Professional Documents
Culture Documents
Stroke On Call, by Ahmed Koriesh: Stroke Timeline: Paged: Bedside: Exam: CT: Iv Tpa
Uploaded by
pattumkp0 ratings0% found this document useful (0 votes)
26 views2 pagesOriginal Title
Stroke-On-Call-new.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views2 pagesStroke On Call, by Ahmed Koriesh: Stroke Timeline: Paged: Bedside: Exam: CT: Iv Tpa
Uploaded by
pattumkpCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
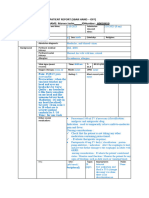
Stroke timeline: Stroke On Call, by Ahmed Koriesh Last seen normal:
First time seen with stroke:
Paged: Past medical history: DM – HTN – Cardiac – Hepatic - Other:
Bedside: Past surgical history: any recent surgery?
Exam: Medications: Antiplatelets? Anticoagulants? Other home meds:
CT: Allergy to contrast? To drugs?
IV tPA:
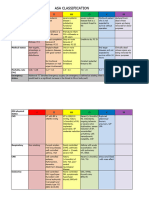
1a. Level of Consciousness(LOC) Alert (or awakens easily and stays awake) 0 ICH Scale
Drowsy (Responds to minor stim. but falls back asleep) 1 GCS: Volume: IVH: Infratentorial: Age:
Obtunded (Responds only to deep pain or vigorous stim) 2 3-4: 2 points ≥30: 1 point Yes: 1 point Yes: 1 point ≥80: 1 point
Comatose 3 5-12: 1 point <30: 0 points No: 0 points No: 0 points <80: 0 point
1b. LOC- Questions Month? Age? Both correct 0 - One answer correct 1 - Neither question answered correctly 2 13-15: 0 points
Mortality: 1 point: 13% 4 points: 97% 6 points: 100%
1c. LOC– Commands Both correct 0 - One correct 1 - Neither performed correctly 2 0 points: 0% 2 points: 26% 3 points: 72% 5 points: 100%
Opens/closes eyes - Opens/closes hands
2. Eye Movements: Normal 0 - Mild gaze paralysis (can bring eyes only over to midline) 1 - Complete 2
Horizontal eye movements Hunt and Hess scale Survival
3. Visual fields: Normal 0 - Partial (quadrant) 1 - Complete hemianopia 2 - Bilateral hemianopia 3 1 Asymptomatic, mild headache, slight nuchal rigidity 70%
2 Moderate to severe headache, nuchal rigidity, no neurologic deficit other than CN palsy 60%
3 Drowsiness / confusion, mild focal neurologic deficit 50%
4. Facial: Normal 0
4 Stupor, moderate-severe hemiparesis 20%
Minor paralysis (flattening of nasolabial folds) 1
5 Coma, decerebrate posturing 10%
Partial paralysis (near or total paralysis lower face) 2
Complete paralysis (Of upper and lower face) 3 Fischer Grade score
5a. Motor – Left Arm Normal (No drift at all) 0 Grade 1: No blood
Hold arm straight out from chest Drift (Drifts downward but NOT to bed before 10 sec.) 1 Grade 2: Diffuse or thin layer of blood less than 1 mm thick
Amputation or joint fusion (N/A) Drifts to bed within 10 sec 2 Grade 3: Localized clots and/or layers of blood greater than 1 mm thick in the vertical plane
Movement, but not against gravity 3 Grade 4: Intracerebral or intraventricular clots with diffuse or absent blood in basal cisterns
Complete paralysis (No movement at all) 4
tPA
5b. Motor – Right Arm Normal (No drift at all) 0
Inclusion Criteria:
Hold arm straight out from chest Drift (Drifts downward but NOT to bed before 10 sec.) 1
- Onset of symptoms <3 hours - ischemic stroke causing measurable neurological deficit - Aged ≥18 years
Amputation or joint fusion (N/A) Drifts to bed within 10 sec 2
Exclusion Criteria
Movement, but not against gravity 3
Significant head trauma or prior stroke in previous 3 months
Complete paralysis (No movement at all) 4
Symptoms suggest subarachnoid hemorrhage
6a. Motor – Left leg Normal (No drift at all) 0
History of previous intracranial hemorrhage
Drift (Drifts downward but NOT to bed before 5 sec.) 1
Keep leg off bed
Intracranial neoplasm, AVM, or aneurysm
Amputation or joint fusion (N/A) Drifts to bed within 5 sec 2
Recent intracranial or intraspinal surgery
Movement, but not against gravity 3
Arterial puncture at noncompressible site in previous 7 days
Complete paralysis (No movement at all) 4
Elevated blood pressure (systolic >185 mm Hg or diastolic >110 mm Hg)
6b. Motor – Right leg Normal (No drift at all) 0 Active internal bleeding
Keep leg off bed Drift (Drifts downward but NOT to bed before 5 sec.) 1 Blood glucose concentration <50mg/dl (2.7mmol/L)
Amputation or joint fusion (N/A) Drifts to bed within 5 sec 2 Acute bleeding diathesis, including but not limited to: Platelet count <100 000/mm³
Movement, but not against gravity 3 Heparin received within 48 hours, resulting in abnormally elevated aPTT
Complete paralysis (No movement at all) 4 Current use of anticoagulant with INR >1.7 or PT >15 seconds
7. Limb Ataxia: Finger-Nose - Heel-Knee Absent (OR pt cannot move arm/leg) 0 - in one limb 1 - in two limbs 2 Current use of direct thrombin inhibitors or direct factor Xa inhibitors
CT demonstrates multilobar infarction (hypodensity >1/3 cerebral hemisphere)
8. Sensory : (Test on face, arm & thigh) Normal 0 - Mild to moderate loss 1 - Severe (unaware of being touched) 2 Relative Exclusion Criteria
Only minor or rapidly improving stroke symptoms (clearing spontaneously)
9. Language/Aphasia Normal ability use words and follow commands 0 Seizure at onset with postictal residual neurological impairments
Repetition & Comprehension Mild to Moderate (Repeats / names with some difficulty) 1 Major surgery or serious trauma within previous 14 days
“Today is a bright sunny day” Severe Aphasia (very few words correct or understood) 2 Recent gastrointestinal or urinary tract hemorrhage (within previous 21 days)
Mute (no ability to speak or understand at all) 3 Pregnancy
10. Dysarthria (slurred) Normal 0 Mild to moderate 1 Severe (none understandable) 2 To extend IV tPA to 4.5 hours, the following additional criteria MUST be met:
Intubated or other physical barrier (N/A) Patient is < 80 years of age
11. Neglect : Ignores touch or vision Normal 0 - Mild (partial) 1 - Profound (Visual and tactile – complete) 2 Patient does not have a history of both diabetes AND stroke
Patient is not taking Warfarin (Coumadin) or any other anticoagulant regardless of INR/coagulation results
Total Score 0 = Best, 42 = Worst NIHSS is < 25
Written informed consent obtained from patient and/or family – required
You might also like
- Cheatsheet 2Document1 pageCheatsheet 2Rick Frea86% (7)
- DR Vineet SuriDocument45 pagesDR Vineet SuriPushpanjali Crosslay HospitalNo ratings yet
- RT Consult Form Side #2Document1 pageRT Consult Form Side #2Rick Frea100% (1)
- Arterial Lines Mark Hammerschmidt, RN FromDocument9 pagesArterial Lines Mark Hammerschmidt, RN FromMark Hammerschmidt100% (3)
- Components of Selected Prehospital Assessment ToolsDocument11 pagesComponents of Selected Prehospital Assessment ToolsRenzho OyeNo ratings yet
- Neuro NihstrokescaleDocument1 pageNeuro NihstrokescaleVictorine Levana PudjiadiNo ratings yet
- NE For StrokeDocument22 pagesNE For StrokeJacky LinNo ratings yet
- Presentation 3 - DR Curran - 0Document41 pagesPresentation 3 - DR Curran - 0শরীফ উল কবীরNo ratings yet
- Ischemic Stroke Case SummaryDocument31 pagesIschemic Stroke Case SummaryHariniNo ratings yet
- Appendix A National Institutes of Health Stroke.22Document1 pageAppendix A National Institutes of Health Stroke.22mhd.mamdohNo ratings yet
- ESRSDocument5 pagesESRSIshita DhyaniNo ratings yet
- Senior Lawyer Stroke CaseDocument4 pagesSenior Lawyer Stroke CaseAlessandra Dominique MarianoNo ratings yet
- Neecham Confusion ToolDocument3 pagesNeecham Confusion Tooli love garfieldNo ratings yet
- 4 Abdominal+ExaminationDocument9 pages4 Abdominal+Examinationمرتضى حسين عبدNo ratings yet
- Approach To Seizures in ChildrenDocument12 pagesApproach To Seizures in ChildrenShamen KohNo ratings yet
- 2015 355 Moesm1 EsmDocument3 pages2015 355 Moesm1 EsmIvan BurgosNo ratings yet
- Post-Anesthesia Recovery Scoring SystemsDocument3 pagesPost-Anesthesia Recovery Scoring SystemsChia VioletNo ratings yet
- Med CnsDocument23 pagesMed CnsPrakruti VaghaniNo ratings yet
- Chapter 48B - Critical Care of Cerebrovascular DiseaseDocument26 pagesChapter 48B - Critical Care of Cerebrovascular DiseaseDragutin PetrićNo ratings yet
- Management of Acute StrokeDocument57 pagesManagement of Acute StrokeariffurqaniNo ratings yet
- Spinal Cord InjuryDocument17 pagesSpinal Cord InjuryTom MallinsonNo ratings yet
- 2011国际学院意识障碍头痛Document67 pages2011国际学院意识障碍头痛Wai Kwong ChiuNo ratings yet
- EpilepsyDocument4 pagesEpilepsyWardah AliNo ratings yet
- PEDIATRIC ASSESSMENT OVERVIEWDocument2 pagesPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- Adult vital signs chart neurological assessmentDocument9 pagesAdult vital signs chart neurological assessmentEmma NuroNo ratings yet
- NIH Stroke Scale for Diagnosing Stroke SubtypeDocument23 pagesNIH Stroke Scale for Diagnosing Stroke SubtypekNo ratings yet
- Pediatric Pain ScaleDocument2 pagesPediatric Pain ScaleSathish HaranNo ratings yet
- To RememberDocument2 pagesTo RememberMes KimNo ratings yet
- Person Assessment TemplateDocument10 pagesPerson Assessment TemplateCassandra LeeNo ratings yet
- CRAMS Score: Call AIR for 8 or LessDocument1 pageCRAMS Score: Call AIR for 8 or LessIGDNo ratings yet
- SeizuresDocument14 pagesSeizuresGidu SaidNo ratings yet
- Determinants:: Blood PressureDocument3 pagesDeterminants:: Blood PressureYmon TuallaNo ratings yet
- Clinical Skills - Neurology Exam TechniquesDocument34 pagesClinical Skills - Neurology Exam TechniquesHassen Kavi IsseNo ratings yet
- Case 2Document9 pagesCase 2Sofia Ranada LamosteNo ratings yet
- Localising CNS LesionsDocument3 pagesLocalising CNS LesionsDeeWallyNo ratings yet
- ASACLASS Renew3Document3 pagesASACLASS Renew3docwepNo ratings yet
- Management of Unconscious Patient-Document2 pagesManagement of Unconscious Patient-chesang507No ratings yet
- Health Assessment Reviewer DiagaoDocument3 pagesHealth Assessment Reviewer DiagaoJohana Pinagayao AngkadNo ratings yet
- Neurological Examination SignsDocument71 pagesNeurological Examination SignsDaniel DiduNo ratings yet
- NEUROLOGI - NEUROEMERGENCY - COMA AND BRAIN DEATH - DR - Yovita Andhitara, SP.S, FINS, MSi - Med - Kelas B Dan DDocument38 pagesNEUROLOGI - NEUROEMERGENCY - COMA AND BRAIN DEATH - DR - Yovita Andhitara, SP.S, FINS, MSi - Med - Kelas B Dan DFini AndrianiNo ratings yet
- 1-General ExaminationDocument5 pages1-General Examinationalmatrim10No ratings yet
- Ver Tigo A ND Dizziness in The Emergenc y Depar TmentDocument12 pagesVer Tigo A ND Dizziness in The Emergenc y Depar TmentEko SaputraNo ratings yet
- 5-Lump ExaminationDocument4 pages5-Lump Examinationdzidek7No ratings yet
- The Fetus and The Neonatal Infant: Figure 99-5Document1 pageThe Fetus and The Neonatal Infant: Figure 99-5Raian SuyuNo ratings yet
- COMFORT ScaleDocument7 pagesCOMFORT ScaleALDO STEFANUZ (STIK)No ratings yet
- Psyche DrugsDocument9 pagesPsyche DrugsJc EvaristoNo ratings yet
- Anti ArrhythmicsDocument32 pagesAnti ArrhythmicsdNo ratings yet
- Illness Trajectory in Palliative Care: SudirmanDocument62 pagesIllness Trajectory in Palliative Care: SudirmanMarlina SaputriNo ratings yet
- SheetDocument3 pagesSheetapi-3853070No ratings yet
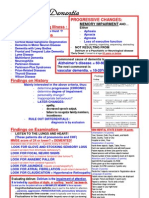
- Alzheimers Dementia Alzheimers Dementia Alzheimers Dementia Alzheimers DementiaDocument5 pagesAlzheimers Dementia Alzheimers Dementia Alzheimers Dementia Alzheimers DementiaTom Mallinson0% (1)
- Left Hemiplegia Case StudyDocument98 pagesLeft Hemiplegia Case StudyMuhammad Jawa'd AnwarNo ratings yet
- Pediatric Assessment: General ImpressionDocument4 pagesPediatric Assessment: General Impressiondanx finNo ratings yet
- Optic AtrophyDocument36 pagesOptic Atrophysajjad hossainNo ratings yet
- IM Equine. Revision T.W 0 Vet. SourseDocument50 pagesIM Equine. Revision T.W 0 Vet. SourseMohamed KhaledNo ratings yet
- Carpal Tunnel Syndrome PowerPointDocument15 pagesCarpal Tunnel Syndrome PowerPointRadja DhilahNo ratings yet
- Case Report EpilepsyDocument47 pagesCase Report EpilepsySonya HyekyoNo ratings yet
- Newborn Assessment ChartDocument1 pageNewborn Assessment ChartRupert AsesorNo ratings yet
- Clinical Symptom Score of The Japanese Orthopaedic Association PDFDocument3 pagesClinical Symptom Score of The Japanese Orthopaedic Association PDFJoanne NgimNo ratings yet
- Stroke Assessment: For NursesDocument60 pagesStroke Assessment: For NursesMatt Joseph Cabanting100% (1)
- Sbar 6Document3 pagesSbar 6marwajr2509No ratings yet
- Hidden Disabilities and Conditions: Creating an Inclusive WorkplaceFrom EverandHidden Disabilities and Conditions: Creating an Inclusive WorkplaceNo ratings yet
- Assesment of Respiratory DistressDocument2 pagesAssesment of Respiratory DistresspattumkpNo ratings yet
- ICU Rounding Template - v. WebsiteDocument2 pagesICU Rounding Template - v. Websitepattumkp0% (1)
- Preanesthetic Evaluation Down's Syndrome PDFDocument11 pagesPreanesthetic Evaluation Down's Syndrome PDFpattumkpNo ratings yet
- Intubation PDFDocument80 pagesIntubation PDFEdson Llerena SalvoNo ratings yet
- Emergency Drug ListDocument1 pageEmergency Drug Listpattumkp50% (2)
- CT Goalsobj2014 PDFDocument7 pagesCT Goalsobj2014 PDFpattumkpNo ratings yet
- Hypertension 5 Minutes PDFDocument7 pagesHypertension 5 Minutes PDFpattumkpNo ratings yet
- Emergency Drug ListDocument1 pageEmergency Drug Listpattumkp50% (2)
- Anesthesia GuideDocument84 pagesAnesthesia GuideRaisa Paz RamosNo ratings yet
- Teething Trouble in ChildrenDocument3 pagesTeething Trouble in ChildrenpattumkpNo ratings yet
- Emergency Drug ListDocument1 pageEmergency Drug Listpattumkp50% (2)
- Emergency Drug ListDocument1 pageEmergency Drug Listpattumkp50% (2)
- 07 Guidelines For ManagementDocument6 pages07 Guidelines For ManagementNuwanda GoreNo ratings yet
- Vasopressors: Jennifer & Joshua Chalk Talk 1/17/2014 Go Hawks!Document44 pagesVasopressors: Jennifer & Joshua Chalk Talk 1/17/2014 Go Hawks!pattumkp100% (1)
- Havells - E-Plus Electrician PointsDocument1 pageHavells - E-Plus Electrician Pointspattumkp83% (60)
- Pocket Tutor Understanding ABGs and Lung Function Tests (2012) (PDF) (UnitedVRG)Document170 pagesPocket Tutor Understanding ABGs and Lung Function Tests (2012) (PDF) (UnitedVRG)pattumkpNo ratings yet
- D. P. Laporta MD SMBD-JGH Dept of Adult Critical CareDocument40 pagesD. P. Laporta MD SMBD-JGH Dept of Adult Critical CarepattumkpNo ratings yet
- Vaso Pressors and I NotRopesDocument12 pagesVaso Pressors and I NotRopesBea Marie Deocampo EsportonNo ratings yet
- Cardiovascular SystemDocument624 pagesCardiovascular Systempattumkp100% (1)
- Central Nervous SystemDocument0 pagesCentral Nervous SystempattumkpNo ratings yet
- Relieving Respiratory Distress with EpinephrineDocument91 pagesRelieving Respiratory Distress with EpinephrineJimmalyn Santos100% (1)
- OCR Scheme of Work SupportDocument48 pagesOCR Scheme of Work SupportijemikinNo ratings yet
- Leadership & Management Assignment - DelegationDocument87 pagesLeadership & Management Assignment - Delegationamasoud96 amasoud96No ratings yet
- High blood pressure readingsDocument2 pagesHigh blood pressure readingsEniamrahs DnalonNo ratings yet
- Fundamentals of NursingDocument220 pagesFundamentals of NursingdgratyNo ratings yet
- MCQs On CVS Pharmacology by Medical Study CenterDocument47 pagesMCQs On CVS Pharmacology by Medical Study CenterLin YunNo ratings yet
- SGLT2 Inhibitors and MechanismsDocument7 pagesSGLT2 Inhibitors and MechanismseswaynedNo ratings yet
- INTERSALT Study Findings Public Health and Medical Care ImplicationsDocument9 pagesINTERSALT Study Findings Public Health and Medical Care ImplicationsMore Force CompanyNo ratings yet
- Clinical Management GuidelineDocument246 pagesClinical Management GuidelineKyaw Htet KhaingNo ratings yet
- Kul Sistem CV Ut Prodi FarmasiDocument34 pagesKul Sistem CV Ut Prodi FarmasiMicho Zhii IntelNo ratings yet
- 10 1161@hypertensionaha 119 14240 PDFDocument8 pages10 1161@hypertensionaha 119 14240 PDFAbidia KamilNo ratings yet
- Pcol Cover To CoverDocument214 pagesPcol Cover To CoverJec OcampoNo ratings yet
- Nutrition in Pregnancy and LactationDocument84 pagesNutrition in Pregnancy and LactationJustin Ahorro-DionisioNo ratings yet
- Summary TechnicalOnly Patient MonitorDocument40 pagesSummary TechnicalOnly Patient MonitorFidaa JaafrahNo ratings yet
- ScoreDocument43 pagesScorepokharelriwaj82No ratings yet
- General Surgery: Aiims MedeasyDocument19 pagesGeneral Surgery: Aiims Medeasyvk100% (2)
- Vital SignsDocument131 pagesVital SignskasingaNo ratings yet
- How I Personalize Fluid Therapy in Septic Shock?: Review Open AccessDocument11 pagesHow I Personalize Fluid Therapy in Septic Shock?: Review Open AccessGian CarloNo ratings yet
- Health 2NDDocument21 pagesHealth 2NDJulie AlayonNo ratings yet
- Citricare 506DN ManualDocument100 pagesCitricare 506DN Manualmaria jose rodriguez lopezNo ratings yet
- Aldomet: (Methyldopa)Document6 pagesAldomet: (Methyldopa)Riska AuliahNo ratings yet
- Blood VesselsDocument43 pagesBlood VesselsJessica AcostaNo ratings yet
- Safe Tourniquet Use A Review of The Evidence JAAOSDocument10 pagesSafe Tourniquet Use A Review of The Evidence JAAOSAzmi FarhadiNo ratings yet
- BP Pump 2: Operators ManualDocument82 pagesBP Pump 2: Operators ManualomerNo ratings yet
- JPCC January - March 2016 PDFDocument70 pagesJPCC January - March 2016 PDFseema sharmaNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4jamie carpioNo ratings yet
- EMS Field Handbook (Revision 1) PDFDocument61 pagesEMS Field Handbook (Revision 1) PDFAnonymous qAEhQo1No ratings yet
- Eclampsia Severe Pre-Eclampsia 5.1Document37 pagesEclampsia Severe Pre-Eclampsia 5.1MarsyaNo ratings yet
- Hypertension ReportDocument16 pagesHypertension ReportAxl SalimoNo ratings yet