Professional Documents
Culture Documents
Preliminary Report of A New Method of Surgical Treatment of Haemorrhoids
Uploaded by
joOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Preliminary Report of A New Method of Surgical Treatment of Haemorrhoids
Uploaded by
joCopyright:
Available Formats
Global Surgery
Research Article ISSN: 2056-7863
Preliminary report of a new method of surgical treatment
of haemorrhoids
Muhammad Assem Kubtan*
Department of surgery, Faculty of medicine, Syrian Private University, Damascus, Syria
Abstract
When conservative treatment fails, many invasive techniques developed to treat hemorrhoids. This study aims to compare the results of method designed by the
author. (Disconnection of Systemic from Visceral Circulation at the anal canal DSVC) with the classical surgery known as Milligan & Morgan approach M&M. We
conducted controlled, non-blinded, randomized study, involved 72 patients, took place under the supervision of one surgeon (the author) in Damascus hospital in
Syria. For DVSC the mean procedures time (10 +/- 0) minutes (ranged between 8-21 minutes) and duration of hospitalization 4 ± 2 hours post operatively.
The mean procedures time for M&M (20 ± 0) minutes (ranged between 18-35 minutes) and hospitalized for two day post-operatively. We recommend DSVC
method for 2nd, 3rd degree and prolapsing hemorrhoids, it is easy to perform, not associated with serious complications and has a good and satisfactory results.
Compared to other surgical procedures, less painful, blood stained anal discharge but no actual bleeding , and does not require specific device (Doppler sounder), or
Stapler, and satisfy the patient.
Introduction a communications between the portal and systemic circulations, and
forming direct arteriovenous communications within the cushions,
Epidemiology and for these reasons, hemorrhoidal bleeding is arterial in nature.
More than 10 million of the population complain of hemorrhoids The submucosal layer of these cushions contains the vessels
in United States Figure 1, more than a million and half are trying mentioned and also rich in muscular fibers, which arise from both
to benefit from different therapeutic modalities, although it has the internal sphincter and the conjoined longitudinal muscle. These
been stated that 50% of the population will experience symptomatic muscular fibers (the muscularis submucosa) help to maintain
hemorrhoid disease at some point in their lives.
Hemorrhoids affect all age groups, peak incidence of symptomatic
disease 45–65 years 2, there is a slightly increased prevalence in women.
Hemorrhoids, exists in healthy people, it become symptomatic when
enlarge, inflamed, bleed, develop prolapses or thrombosis.
An evidence support that hemorrhoidal bleeding is arterial nature,
supported by PO2 calibration.
Anatomical principle
Anal canal 1, is approximately 4 cm in, close to levator - sphincteric
complex. Anus is lined by anoderm, richly innervated with somatic
sensory nerves, and supplied by the inferior hemorrhoidal vessels. The
dentate line is the point at which the squamous anoderm meets the
columnar mucosa it lies about 3 cm above the anal verge. The dentate
line is the major anatomic reference point when considering surgical
treatment. Internal hemorrhoids are cushions of fibrovascular tissue
proximal to the dentate line, with the external hemorrhoid distal to it
Figure 1. Second degree Heamorroids.
[1-5].
The anal canal forms [1,3] a discontinuous layer of thickened tissue,
creating “cushions” found in the left lateral, right lateral anterior, and Correspondence to: Muhammad Assem Kubtan Department of surgery, Faculty
right lateral posterior positions, there are frequent anatomic variations of medicine, Syrian Private University, Damascus, Syria, Tel: 00963944271215;
of this arrangement These cushions receive their blood supply primarily E-mail: makubtan@gmail.com
from the superior hemorrhoidal artery and branches of the middle and Key words: hemorrhoids, hemorrhoids cushions, dentate line
the inferior hemorrhoidal arteries. The venous drainage is provided by
the superior, middle, and inferior hemorrhoidal veins, representing Received: September 05, 2015; Accepted: October 03, 2015; Published: October
07, 2015
Glob Surg, 2015 doi: 10.15761/GOS.1000120 Volume 1(3): 61-64
Kubtan MA (2015) Preliminary report of a new method of surgical treatment of hemorrhoids
adherence of these tissues to the underlying internal sphincter. With
time and aging, starting as early as the second or third decade of life
associated with other factors such as heredity , chronic constipation,
lack of fibers diet etc , this supporting tissue can deteriorate or weaken,
leading to distal displacement of the cushions and venous distention,
erosion, bleeding, thrombosis and hemorrhoids prolapse.
The hemorrhoids have an important role in the maintenance
of anal continence, contributing 15%-20% of resting pressure of the
anal verge. They protect the sphincter mechanism during defecation,
and providing complete closure of anal opening, while performing a
Valsalva maneuver.
Hemorrhoids are formed during the uterine life and continue with
their physiological role in a healthy adult subjects.
The aim of this study is to compare results of DVSC for 2nd, 3rd and
prolapsing hemorrhoids with M&M.
Figure 3. Disconnection of Systemic from Visceral Circulation through the anal
Patients and method canal DSVC.
Between March 2010 to October 2013, after having their consent,
72 patients enrolled in this study. Their ages ranged between 18-70
And the mean procedures time for M&M (20 ± 0) minutes (ranged
years, included 37 (24 males 65%), have been subjected to the method
between 18-35 minutes) and the patient was discharged from the
DVSC, compared with 35 (22 males 63%) treated using the classical
hospital two days post-operation.
procedures M&M.
Both procedures carried out by same surgeon, under caudal
DVSC performed by using PROLINE No. 1 stiches with round
anesthesia to all patients, and tracheal intubation were used only in
twin needles, one of the needles is passed about 5 – 8 mm aside of the
three cases 8.5% of M&M group.
hemorrhoidal cushion from inside the anus above the dentate line
through the ano rectal space heading to outside through para anal All patients received three fingers manual dilatation of anus MDA.
cutaneous area 2 cm proximal to anal orifice , the second needle also
For those who underwent M&M, they suffered 100% from sever
passed in the same manner through the other side of the hemorrhoidal
anal pain after the caudal anesthetic effect have faded, in the first 24
cushion and about 2.5 cm apart between the two needles outlets, the
hours all received Pethidine 100 mg intramuscular injections primarily
two ends ligated tightly together after threading one end of stitches
followed by Pethidine 100 mg diluted in 20 ml N. Saline and given Iv
through a 3 mm diameter of 2.5 cm length of poly ethylene tube
intermittently in divided doses not exceeding 2 ml per hour, followed
producing principally local avascular necrosis and disconnection
by Diclofenac 75 mg injections PRN till discharge. One male (2.8%)
between systemic and portal system and dearterialisation of the
developed retention of urine while in hospital and catheterized for three
hemorrhoidal cushion Figure 2. This procedures were repeated to the
days, one patient (2.8%) developed anal stricture after being discharged
other two hemorrhoidal cushions Figure 3.
from hospital in two weeks requiring readmission for anal dilatation.
The other group of patients treated surgically using the classical
All Patients 100% underwent DVSC received single 100 mg
procedures of M&M.
Pethidine intramuscular injection post operatively when the effect of
Results caudal anesthetic has faded , and discharged from hospital 4 ± 2 hours
and were asked to report to the out patients department OPD three
For DVSC The mean procedures time (10 ± 0) minutes (ranged days post operatively Figure 4 for review and removal of the perianal
between 8-21 minutes) and duration of stay in the hospital 4 ± 2 hours DVSC stitches.
post operatively.
Both groups instructed to attend OPD after 2 weeks, 4 weeks, and
6 months.
Both groups advised to take high fiber diet from the first day post
operatively, also advised to have a lukewarm salted sits bath three times
a day for two weeks.
They were all given a prescription of Potassium Diclofenac 50 mg
orally twice to three times a day with Domperidone 10 mg tablet twice
daily.
Those how suffered from persistent pain in ano were advised to
have more lukewarm salted sits bath and Diclofenac 75 mg injection
IM, PRN not exceeding two injections a day.
It was noticed that patients, who underwent DVSC procedures
Figure 2. Disconnection of Systemic from Visceral Circulation through the anal experienced immediate relief of anal pain Figure 5 following removal
canal DSVC. of stitches. Two weeks later they were seen in the OPD and there were
Glob Surg, 2015 doi: 10.15761/GOS.1000120 Volume 1(3): 61-64
Kubtan MA (2015) Preliminary report of a new method of surgical treatment of hemorrhoids
Discussion
Several options for treating hemorrhoids, including conservative
management, by increasing fiber intake to combat chronic constipation,
encouraging the movement, avoiding prolonged sitting, and in elderly
encouraging the actions of regular fecal evacuation by other means.
Hemorrhoids is considered as a set of arterial-venous vascular complex
residing between the mucous layer the lamina muscularis mucosa
muscle and anal sphincter muscular structure (corpus cavernosum
recti).
Haemorrhoidal cushions share in physiology of anal sphincter
mechanism, but when it became engorged and enlarged it evolves into
clinical condition that requires treatment. Our method described is
effective and eliminates the need for surgical excision.
In our society we deal with people of moderate income who have
Figure 4. 3rd day post operatively before removing prolene sutures. limited access to government services due to lengthy waiting list and
current unrest, and the majorities have no insurances facilities.
DVSC procedures represent an easy way of treating hemorrhoids
leading to immediate arrest of bleeding, regression in size of prolapsed
Figure 5. 3rd day post operatively after removing prolene sutures.
considerable regression in the pain and edema Figure 6, and four weeks Figure 6. Two weeks after surgery.
later they were seen in OPD and were almost completely pain free
without any discomfort in defecation or sitting, and the cushions size
have regressed almost completely with normal anal appearance Figure
7 and without bleeding or other serious symptoms.
The only complication we encountered was cutaneous ulceration
deep to polyethylene tubes seen in 4 patients 10.8% lasted less than a
week and healed completely.
For those who underwent M&M surgery, 18 had residual complaint
51% of pain and discomfort on defecation 2 weeks post operatively
and two of them 5.7% were readmitted for manual dilatation of the
anus, 3 suffered 8.5% from persistent anal bleeding, when reviewed 4
weeks later in OPD 5 patients 14% complained of moderate pain and
discomfort on defecation and 3 had 8, 5% intermittent blood stained
anal discharge.
We fail to see any of both groups six month later in OPD despite
attempting to contact patients by phone, none of the DSVC group had
complaint, while 4 of those 11.4% underwent M&M still c/o discomfort Figure 7. One month after surgery.
on deification.
Glob Surg, 2015 doi: 10.15761/GOS.1000120 Volume 1(3): 61-64
Kubtan MA (2015) Preliminary report of a new method of surgical treatment of hemorrhoids
hemorrhoidal cushions, it is a day case surgery, less complicated, easy hemorrhoids: current incidence and complications of operative therapy. Dis Colon
Rectum 35: 477-481. [Crossref]
to perform, and does not require a special needs such as Doppler
sounder or expensive stapler instruments [6-20]. 4. Loder PB, Kamm MA, Nicholls RJ, Phillips RK (1994) Haemorrhoids: pathology,
pathophysiology and aetiology. Br J Surg 81: 946-954. [Crossref]
We recommend the adoption of the DVSC method, as an easy
5. MacRae HM, McLeod RS (1995) Comparison of hemorrhoidal treatment modalities. A
way not associated with any serious complications, it has a good and meta-analysis. Dis Colon Rectum 38: 687-694. [Crossref]
satisfactory results. Compared to other surgical procedures, easy
6. Dennison AR, Paraskevopoulos JA, Kerrigan DD, Shorthouse AJ (1996) New thoughts
to perform, less painful, blood stained anal discharge but no actual on the aetiology of haemorrhoids and the development of non-operative methods for
bleeding, and achieve satisfaction of the patient and early return to their management. Minerva Chir 51: 209-216. [Crossref]
work.
7. Mehigan BJ, Monson JR, Hartley JE (2000) Stapling procedure for haemorrhoids
versus Milligan-Morgan haemorrhoidectomy: randomised controlled trial. Lancet 355:
We believe that disconnecting the systemic from the visceral
782-785. [Crossref]
circulation process is easy to learn and less invasive than the other
surgical procedures, least in the incidence of recurrence, and we have 8. Rowsell M, Bello M, Hemingway DM (2000) Circumferentialmucosectomy (stapled
haemorrhoidectomy) versus conventional haemorrhoidectomy: randomised controlled
not encounter any relapse three years post operatively, it is least painful trial. Lancet 355: 779-781. [Crossref]
surgical procedures and pain is encountered commonly during the first
9. Ganio E, Altomare DF, Gabrielli F, Milito G, Canuti S (2001) Prospective randomized
three days post operatively . multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg 88: 669-
674. [Crossref]
Pitfalls: We were concerned about the possibility of developing
high fistula in an, and we can state confidently that this worries has no 10. Shalaby R, Desoky A (2001) Randomized clinical trial of stapled versus Milligan-
basis in patients subjected to the DVSC procedures. Morgan haemorrhoidectomy. Br J Surg 88: 1049-1053. [Crossref]
11. Ortiz H, Marzo J, Armendariz P (2002) Randomized clinical trial of stapled
Conclusion haemorrhoidopexy versus conventional diathermy haemorrhoidectomy. Br J Surg 89:
1376-1381. [Crossref]
We recommend DVSC Disconnecting the systemic from visceral
12. Wilson MS, Pope V, Doran HE, Fearn SJ, Brough WA (2002) Objective comparison
circulation it is without complications of value in treatment of of stapled anopexy and open hemorrhoidectomy: a randomized, controlled trial. Dis
hemorrhoids of second and third degree and prolapsed hemorrhoids, Colon Rectum 45: 1437-1444. [Crossref]
it is less painful, satisfactory, the cost is 40% less than other surgical
13. Au-Yong I, Rowsell M, Hemingway DM (2004) Randomised controlled clinical trial
modalities. of stapled haemorrhoidectomyvs conventional haemorrhoidectomy; a three and a half
year follow up. Colorectal Dis 6: 37-38. [Crossref]
Our view that this technique should be considered and require
further study in other centers, to repeat our results and could be 14. Hasse C, Sitter H, Brune M, Wollenteit I, Lorenz W, et al. (2004) [Haemorrhoidectomy:
conventional excision versus resection with the circular stapler. Prospective,
instituted in any societies were short hospitalization and low cost has randomized study]. Dtsch Med Wochenschr 129: 1611-1617. [Crossref]
an important role in choosing the type of surgical treatment instituted.
15. Ganio E, Altomare DF, Milito G, Gabrielli F, Canuti S (2007) Long-term outcome of
Acknowledgments a multicentre randomized clinical trial of stapled haemorrhoidopexy versus Milligan-
Morgan haemorrhoidectomy. Br J Surg 94: 1033-1037. [Crossref]
I would like to extend my appreciation and thanks for the help and 16. Tjandra JJ, Chan MK (2007) Systematic review on the procedure for prolapse and
support provided by Professor Abdul Razak Cheikh Issa the President hemorrhoids (stapled hemorrhoidopexy). Dis Colon Rectum 50: 878-892. [Crossref]
of the Syrian Private University, and a special thanks to my colleague 17. Annals of Surgical Innovation and Research
Professor Yousser Mohammad for her assistance in editing.
18. Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, et al. (2008) Stapled
References haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a
systematic review and economic evaluation. Health Technol Assess 12: iii-iv, ix-x,
1. Milligan ETC, Morgan CN, Jones LE, Officer R (1937) Surgical anatomy of the anal 1-193. [Crossref]
canal and operativetreatment of hemorrhoids. Lancet 2: 1119-1124.
19. Laughlan K, Jayne DG, Jackson D, Rupprecht F, Ribaric G (2009) Stapled
2. Johanson JF, Sonnenberg A (1990) The prevalence of hemorrhoids and chronic haemorrhoidopexy compared to Milligan-Morgan and Ferguson haemorrhoidectomy:
constipation. An epidemiologic study. Gastroenterology 98: 380-386. [Crossref] a systematic review. Int J Colorectal Dis 24: 335-344. [Crossref]
3. Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG (1992) Symptomatic 20. Stapled haemorrhoidopexy for the treatment of haemorrhoids (2011) NICE technology
appraisal guidance 128.
Copyright: ©2015 Kubtan MA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Glob Surg, 2015 doi: 10.15761/GOS.1000120 Volume 1(3): 61-64
You might also like
- APPENDIX C: MONSTROUS GRAFTSDocument5 pagesAPPENDIX C: MONSTROUS GRAFTSLeonardoGuliaNo ratings yet
- ELSC2111 Earth and Life Science Q2 Long Quiz 2 (19) 3Document6 pagesELSC2111 Earth and Life Science Q2 Long Quiz 2 (19) 3Christian TeroNo ratings yet
- Richard McCarty - Stress, Health, and Behavior-The Guilford Press (2023)Document355 pagesRichard McCarty - Stress, Health, and Behavior-The Guilford Press (2023)Mustafa ŞEKERNo ratings yet
- ENT - An Introduction and Practical Guide, Second Edition-CRC Press (2017)Document176 pagesENT - An Introduction and Practical Guide, Second Edition-CRC Press (2017)Marton B.No ratings yet
- SHS STEM Bio1 Q1 Week 1 Module 2 Cell Structure and Functions 1Document17 pagesSHS STEM Bio1 Q1 Week 1 Module 2 Cell Structure and Functions 1Dette Dominic Ballano67% (3)
- Principles of Anatomy and Physiology 15th Edition Tortora Test BankDocument52 pagesPrinciples of Anatomy and Physiology 15th Edition Tortora Test Bankgabrielvanztqro100% (29)
- A Semi-Detailed Lesson Plan in Grade 9 Biology I. ObjectivesDocument3 pagesA Semi-Detailed Lesson Plan in Grade 9 Biology I. ObjectivesCyril Cauilan100% (1)
- Fitting The Task To The Human A Textbook of Occupational Ergonomics by Grandjean, E. Kroemer, K. H. E.Document414 pagesFitting The Task To The Human A Textbook of Occupational Ergonomics by Grandjean, E. Kroemer, K. H. E.Andy Delos ReyesNo ratings yet
- Medip, ISJ-7273 ODocument4 pagesMedip, ISJ-7273 OSharanya Vijay GovindanNo ratings yet
- Hematoma Vulvo-Vaginal: Exceptional Etiology of Obstetrical Near MissDocument4 pagesHematoma Vulvo-Vaginal: Exceptional Etiology of Obstetrical Near MissLova DorlandNo ratings yet
- SWD Wound DehiscenceDocument5 pagesSWD Wound DehiscencealifiaNo ratings yet
- Wjols 15 8Document3 pagesWjols 15 8HERSH NATH AGRAWALNo ratings yet
- Medip, IJOHNS-388 ODocument6 pagesMedip, IJOHNS-388 Onaveed gulNo ratings yet
- Ultrasound-Guided Injection of Polidocanol Microfoam in The Management of Venous Leg UlcersDocument7 pagesUltrasound-Guided Injection of Polidocanol Microfoam in The Management of Venous Leg UlcersAlexandre Campos Moraes AmatoNo ratings yet
- Superficial Wound Healing after Cardiac SurgeryDocument21 pagesSuperficial Wound Healing after Cardiac SurgeryPrimayudha DirgatamaNo ratings yet
- 2011 Journal of Phlebology EliasDocument6 pages2011 Journal of Phlebology EliasronnyNo ratings yet
- Original Article: Burst Abdomen: Is It A Preventable Complication?Document5 pagesOriginal Article: Burst Abdomen: Is It A Preventable Complication?Melisa ClaireNo ratings yet
- Short Term Outcomes of Stapled Hemorrhoidectomy Our Experience at GMC SrinagarDocument4 pagesShort Term Outcomes of Stapled Hemorrhoidectomy Our Experience at GMC SrinagarInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesDocument9 pagesClinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesAndika FahruroziNo ratings yet
- s44215 023 00094 7Document5 pagess44215 023 00094 7charlaayasyafefiNo ratings yet
- SssDocument5 pagesSssDerianti NurhidayahNo ratings yet
- Omentum overlay in laparoscopic treatment of umbilical and incisional herniasDocument10 pagesOmentum overlay in laparoscopic treatment of umbilical and incisional herniasAlin MihetiuNo ratings yet
- Stenosis Baca YaDocument13 pagesStenosis Baca YaDista Yuristia PNo ratings yet
- Abdelhameed Et Al (June 2019)Document6 pagesAbdelhameed Et Al (June 2019)drpklalNo ratings yet
- Difficult Airway Management in Pediatric With A Large Cystic Hygroma Colli Undergoing One-Stage Excision SurgeryDocument4 pagesDifficult Airway Management in Pediatric With A Large Cystic Hygroma Colli Undergoing One-Stage Excision SurgeryDody TamaraNo ratings yet
- Surgical Management of An Extensive Spinal EpiduraDocument5 pagesSurgical Management of An Extensive Spinal EpiduraqrscentralNo ratings yet
- Hemorrhoidal Laser Procedure Help A Painless Treatment For HemorrhoidsDocument4 pagesHemorrhoidal Laser Procedure Help A Painless Treatment For HemorrhoidsIndra YaniNo ratings yet
- 8 Pseudocyst of Pinna and Its Treatment With Surgical Deroofing - An Experience at Tertiary Hospitals 2013Document13 pages8 Pseudocyst of Pinna and Its Treatment With Surgical Deroofing - An Experience at Tertiary Hospitals 2013solikin ikinNo ratings yet
- Management of Pseudoaneurysms in IV Drug Users: Ori Gi Nal Arti CL eDocument4 pagesManagement of Pseudoaneurysms in IV Drug Users: Ori Gi Nal Arti CL eMayur DadhaniyaNo ratings yet
- Kjtcs043 06 09Document7 pagesKjtcs043 06 09정윤형No ratings yet
- Treatment of Sternal Wound Infections After Open-Heart SurgeryDocument6 pagesTreatment of Sternal Wound Infections After Open-Heart SurgeryDennis CobbNo ratings yet
- Jurnal Hemoroid 3Document4 pagesJurnal Hemoroid 3RSU DUTA MULYANo ratings yet
- Eur Surg Res 2008;40:61–183 Abstracts from 20th IPSYS CongressDocument3 pagesEur Surg Res 2008;40:61–183 Abstracts from 20th IPSYS CongressscribullNo ratings yet
- Complete Longitudinal Vaginal Septum Resection. Description of A Bloodless New TechniqueDocument3 pagesComplete Longitudinal Vaginal Septum Resection. Description of A Bloodless New Techniquekellybear775No ratings yet
- Endovenous Microwave Ablation of Great Saphenous VeinDocument3 pagesEndovenous Microwave Ablation of Great Saphenous VeinMalekseuofi مالك السيوفيNo ratings yet
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDocument10 pagesAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahNo ratings yet
- SS 2015052610553699 PDFDocument7 pagesSS 2015052610553699 PDFLeny MeiriyanaNo ratings yet
- Mudavath JournalDocument2 pagesMudavath JournalmmkmedicoNo ratings yet
- Iranjradiol 14 03 21742Document5 pagesIranjradiol 14 03 21742AisahNo ratings yet
- Caldwell Luc IncisionDocument3 pagesCaldwell Luc IncisionabdullahNo ratings yet
- Tau 06 03 510Document7 pagesTau 06 03 510Eko NoviantiNo ratings yet
- VAC System Heals FistulasDocument3 pagesVAC System Heals FistulasYacine Tarik AizelNo ratings yet
- A Prospective Comparative Study of Intestinal Anastomosis, Single LayDocument6 pagesA Prospective Comparative Study of Intestinal Anastomosis, Single LayDumitru RadulescuNo ratings yet
- The Rare TravellersDocument3 pagesThe Rare TravellersPedro TrigoNo ratings yet
- https:grupologsa.eu:wp-content:uploads:2023:01:01_AA_2016_4_ZubilewiczDocument6 pageshttps:grupologsa.eu:wp-content:uploads:2023:01:01_AA_2016_4_Zubilewiczbraulio HuarachaNo ratings yet
- Jandrol 112 016444Document7 pagesJandrol 112 016444Павел ГичакNo ratings yet
- What Is A MicrodebriderDocument7 pagesWhat Is A MicrodebriderIqbalurNo ratings yet
- s-0034-1376262Document14 pagess-0034-1376262NOUF ALDHALAANNo ratings yet
- Moult 2015Document7 pagesMoult 2015Amriansyah PranowoNo ratings yet
- Mucocele: A Rare Complication Following Stapled HaemorrhoidopexyDocument6 pagesMucocele: A Rare Complication Following Stapled HaemorrhoidopexyHafidh HanifuddinNo ratings yet
- Transanal Haemorrhoidal Dearterialisation: Nonexcisonal Surgery For The Treatment of Haemorrhoidal DiseaseDocument7 pagesTransanal Haemorrhoidal Dearterialisation: Nonexcisonal Surgery For The Treatment of Haemorrhoidal DiseasePier Paolo Dal MonteNo ratings yet
- Is Mesh Always Necessary in Every Small UmbilicalDocument8 pagesIs Mesh Always Necessary in Every Small UmbilicalLeonardo RibeiroNo ratings yet
- Treatment of Nipple Hypertrophy by A Simplified Reduction TechniqueDocument7 pagesTreatment of Nipple Hypertrophy by A Simplified Reduction TechniqueАндрей ПетровNo ratings yet
- Analysis of Recurrent Urethral Strictures Due To Iatrogenic Urethral TraumaDocument6 pagesAnalysis of Recurrent Urethral Strictures Due To Iatrogenic Urethral TraumaNur Syamsiah MNo ratings yet
- Preventionofincisionalhernias: How To Close A Midline IncisionDocument14 pagesPreventionofincisionalhernias: How To Close A Midline IncisionRashid Arjona BojorquezNo ratings yet
- Hemorrhoidal Laser Procedure - Short - and Long-Term Results From A Prospective StudyDocument5 pagesHemorrhoidal Laser Procedure - Short - and Long-Term Results From A Prospective StudyagusNo ratings yet
- Jcamr V6i2 42697Document4 pagesJcamr V6i2 42697Anshul ShahNo ratings yet
- Original ArticleDocument9 pagesOriginal ArticleJason HuangNo ratings yet
- 1 Journal of Neurosurgery 3Document5 pages1 Journal of Neurosurgery 3harryNo ratings yet
- Management of Chronic Subdural Haematoma: Burr Hole Drainage, Replacement With Hartmann's Solution, and Closed-System DrainageDocument4 pagesManagement of Chronic Subdural Haematoma: Burr Hole Drainage, Replacement With Hartmann's Solution, and Closed-System DrainageMaenangrybirdNo ratings yet
- Randomized Clinical Trial of Mechanochemical and Endovenous Thermal Ablation of Great Saphenous Varicose VeinsDocument7 pagesRandomized Clinical Trial of Mechanochemical and Endovenous Thermal Ablation of Great Saphenous Varicose VeinsAmade DeaNo ratings yet
- HS Surgical Excision Case SeriesDocument16 pagesHS Surgical Excision Case SeriesMarina StosicNo ratings yet
- (Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsDocument10 pages(Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsAniaNo ratings yet
- Double Lateral Sliding Bridge Flap Technique for Root CoverageDocument4 pagesDouble Lateral Sliding Bridge Flap Technique for Root CoverageHiroj BagdeNo ratings yet
- Epi LepsiDocument6 pagesEpi LepsiFebby Aulia AriefNo ratings yet
- Delineation of de Quervain Tenosynovitis in Saudi Arabia and Literature ReviewDocument6 pagesDelineation of de Quervain Tenosynovitis in Saudi Arabia and Literature ReviewIJAR JOURNALNo ratings yet
- A Comparative Study Between Laser Hemorrhoidoplasty Procedure and Conventional HemorrhoidectomyDocument18 pagesA Comparative Study Between Laser Hemorrhoidoplasty Procedure and Conventional HemorrhoidectomyagusNo ratings yet
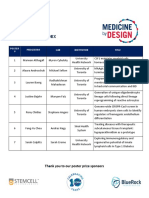
- Poster Index Symposium 2021Document5 pagesPoster Index Symposium 2021Brien WongNo ratings yet
- Respiratory System ExplainedDocument2 pagesRespiratory System ExplainedBryanAngelo Laguilles100% (1)
- Lab Values Memory Trick 1Document2 pagesLab Values Memory Trick 1Mitzi De VeraNo ratings yet
- Neet Wizz Bio Class 12Document89 pagesNeet Wizz Bio Class 12Aarthi T. UNo ratings yet
- Life Processes Notes (Yashvi Modi)Document15 pagesLife Processes Notes (Yashvi Modi)YASHVI MODI60% (5)
- HW-NUR8103 Lecture - Carbohydrate Metabolism IDocument3 pagesHW-NUR8103 Lecture - Carbohydrate Metabolism IyanNo ratings yet
- English 2-09-Structure Transisiton QuestionsDocument8 pagesEnglish 2-09-Structure Transisiton QuestionsDing DongNo ratings yet
- CDI Blood Parameter Monitoring System 550: Real-Time Monitoring of DO As One of 12 Key Blood ParametersDocument5 pagesCDI Blood Parameter Monitoring System 550: Real-Time Monitoring of DO As One of 12 Key Blood ParametersManigandan DhamodhiranNo ratings yet
- 22q11.2 GPC 2023Document24 pages22q11.2 GPC 2023Antoine NinoNo ratings yet
- Anesthetics Drugs - ADocument72 pagesAnesthetics Drugs - Agech yayehNo ratings yet
- Prescotts Microbiology 10Th Edition Willey Solutions Manual Full Chapter PDFDocument25 pagesPrescotts Microbiology 10Th Edition Willey Solutions Manual Full Chapter PDFbob.morris579100% (13)
- Propozitii Scoase Din Cambridge Advanced DictionaryDocument369 pagesPropozitii Scoase Din Cambridge Advanced DictionaryFlorentinoTNo ratings yet
- 4 1Document2 pages4 1Raj BulaNo ratings yet
- Effect of stimulation site on superficial peroneal nerve conduction studiesDocument7 pagesEffect of stimulation site on superficial peroneal nerve conduction studiesfulgencio garciaNo ratings yet
- While Running: An Analysis of Physiological Systems During ExerciseDocument4 pagesWhile Running: An Analysis of Physiological Systems During Exerciseaimi BatrisyiaNo ratings yet
- Mechanisms and Sites of Action for Inhalation AnaestheticsDocument6 pagesMechanisms and Sites of Action for Inhalation Anaestheticsmouxritsa_83No ratings yet
- An RNA Vaccine Drives Expansion and Efficacy of claudin-CAR-T Cells Against Solid TumorsDocument9 pagesAn RNA Vaccine Drives Expansion and Efficacy of claudin-CAR-T Cells Against Solid TumorsYusuf DemirNo ratings yet
- What Is General Adaptation SyndromeDocument3 pagesWhat Is General Adaptation SyndromeCARLOS, Ryan CholoNo ratings yet
- Digestion and AbsorptionDocument16 pagesDigestion and AbsorptionNalla Raghuram ChowdaryNo ratings yet
- 3 Cellular Organization: 3.1 Cells As The Basic Units of LifeDocument6 pages3 Cellular Organization: 3.1 Cells As The Basic Units of LifeVenice Lo100% (1)
- Plant Physiology and BiochemistryDocument4 pagesPlant Physiology and BiochemistryShefira TashaNo ratings yet
- Necrotizing Enterocolitis (Sultn Aiman NeazyDocument59 pagesNecrotizing Enterocolitis (Sultn Aiman NeazyMohammed ElhashimiNo ratings yet