Professional Documents
Culture Documents
Acute Coronary Syndromes: Authors: Tushar Kotecha
Uploaded by
Fauziah TambualaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Coronary Syndromes: Authors: Tushar Kotecha
Uploaded by
Fauziah TambualaCopyright:
Available Formats
Clinical Medicine 2016 Vol 16, No 6: s43–s48 CARDIOVASCULAR
Acute coronary syndromes
Authors: Tushar KotechaA and Roby D RakhitB
In the UK, there are over 80,000 admissions annually with (average age 65 years) compared with patients with NSTE-ACS
ABSTRACT
acute coronary syndromes (ACS). Management of ST-elevation (average age 71 years),3 who also frequently have multi-vessel
myocardial infarction (STEMI) involves primary percutaneous coronary disease and more complex comorbidities. In the UK,
coronary intervention (PCI), which is delivered via dedicated the 30-day mortality associated with STEMI is 8.1%.3 1-year
heart attack centres. Non-ST elevation-ACS (NSTE-ACS) mortality is higher for patients presenting with NSTE-ACS
accounts for two-thirds of ACS presentations, affecting an older compared with STEMI (14.3% versus 9.5%) reflecting the fact
cohort of patients – often with more complex comorbidities. that while patients presenting with NSTE-ACS appear more
Initial management is with anti-thrombotic therapy with stable at presentation, their long-term outcome is worse.4,5
a view to PCI within 24 hours for the most acute cases and The standard of care for patients presenting with ACS includes
within 72 hours for all others. However, varying management early coronary angiography with a view to revascularisation
pathways and access to specialist cardiology services results with percutaneous coronary intervention (PCI) or coronary
in variable times to definitive treatment. Advances in the artery bypass surgery (CABG). Patients with STEMI typically
sensitivity of cardiac biomarkers and the use of risk assessment present acutely with severe ongoing cardiac chest pain and ST
tools now enable rapid diagnosis within a few hours of elevation on 12-lead electrocardiogram (ECG) (Fig 1). In the
symptom onset. Advances in invasive management and drug UK, there is an established STEMI pathway, whereby patients
therapy have resulted in improved clinical outcomes with are taken by the ambulance service directly to a heart attack
resultant decline in mortality associated with ACS. centre where they receive immediate PCI (Fig 2). Patients with
NSTE-ACS usually present more insidiously and are commonly
KEYWORDS: Acute coronary syndrome, non-ST elevation myocardial seen in the local emergency department. This may not be a
infarction, non-ST elevation acute coronary syndrome, ST-elevation PCI-capable centre and patients are frequently admitted under
myocardial infarction the general medical team rather than directly under cardiology.
This may introduce delays in care before the patient receives
definitive treatment.
Introduction
Coronary artery disease (CAD) remains the leading cause Universal definition of myocardial infarction
of death worldwide.1 Clinical manifestations include stable
In 2012, the third universal definition of myocardial infarction
angina, acute coronary syndromes (ACS), heart failure and
was published.6 This update reflects the increasing sensitivity
sudden death. The term ACS encompasses ST-elevation
of biochemical assays and the additional use of imaging
myocardial infarction (STEMI) and non-ST elevation ACS
modalities to diagnose myocardial infarction. The term
(NSTE-ACS), which encompasses non-ST elevation myocardial
myocardial infarction should be used when there is evidence of
infarction (NSTEMI) and unstable angina (UA). Approximately
myocardial necrosis in a clinical setting consistent with acute
two thirds of ACS presentations are with NSTE-ACS and the
myocardial ischaemia. There should be a rise and/or fall of
remainder are STEMI.2,3 Furthermore, with the advent of high
cardiac biomarker value (preferably cardiac troponin) with at
sensitivity troponin assays, many patients previously classified
least one of the following:
as UA are now being diagnosed with NSTEMI. This has resulted
in the incidence of UA to fall while NSTEMI is on the rise.3 > symptoms of ischaemia
While the age- and sex-adjusted incidence of ACS is falling, > new or presumed new significant ST segment or T wave
there remains an associated mortality risk with the condition.2 changes, or new left bundle branch block
In the UK, there are over 80,000 hospital admissions with ACS > development of pathological Q waves on ECG
annually.3 Those presenting with STEMI tend to be younger > imaging evidence of new loss of viable myocardium or new
regional wall motion abnormality
> identification of intracoronary thrombus on angiography or
autopsy.
Authors: Aclinical research fellow, Royal Free Hospital and UCL
Institute of Cardiovascular Science, London, UK; Bconsultant Furthermore, myocardial infarction can be further classified
interventional cardiologist and honorary senior lecturer, Royal Free into five subtypes according to underlying aetiology (Box 1). In
Hospital and UCL Institute of Cardiovascular Science, London, UK clinical practice, type 1 (spontaneous myocardial infarction),
© Royal College of Physicians 2016. All rights reserved. s43
CMJv16n6S-Rakhit.indd 43 23/11/16 9:41 AM
Tushar Kotecha and Roby D Rakhit
Fig 1. Example of 12-lead
electrocardiogram showing
ST-segment elevation in the
inferior leads (II, III and aVF)
with reciprocal ST-segment
depression in leads V1–V4,
I and aVL.
and type 2 (secondary to ischaemic imbalance) are the vessel occlusion. The 12-lead ECG may show ST segment
most commonly encountered. The use of imaging, such as depression, T wave inversion, or be completely normal (Fig 3).
echocardiography or cardiovascular magnetic resonance, NSTEMI is associated with release of cardiac enzymes such as
can be useful to differentiate the two as type 2 is not usually troponin signifying a degree of myocardial necrosis, whereas
associated with loss of viable myocardium or regional wall UA has no enzyme release but the presence of worsening or
motion abnormality. crescendo symptoms. This differentiation of subtypes of ACS
The term ACS encompasses a clinical spectrum of is often used clinically as it allows for diversion of patients to
pathophysiology and presentations of symptomatic coronary different treatment pathways according to clinical urgency.
disease. This is usually due to atherosclerotic plaque rupture,
ulceration or erosion that results in intraluminal thrombus Non-ST elevation acute coronary syndrome
formation and compromises myocardial blood flow leading to
NSTE-ACS may precede STEMI or sudden cardiac death.
myocardial necrosis and release of cardiac enzymes. Usually,
Despite often relatively short-lived symptoms that respond to
STEMI is a manifestation of complete vessel occlusion due to
medical therapy with nitrates and opioids, the risk of death
acute thrombus formation secondary to a ruptured plaque. If
or STEMI in the first 30 days is up to 10%.7 Up to half of
left untreated, this results in transmural infarction and extensive
patients will experience recurrent ischaemia despite initiation
myocardial necrosis. Characteristically, the 12-lead ECG shows
of medical therapy.8,9 The main determinants of prognosis are
ST-segment elevation localised to an epicardial vessel territory.
extent of myocardial injury, extent of coronary artery disease
In contrast, NSTE-ACS results from incomplete or transient
and instability of disease.
Initial assessment of patients with suspected NSTE-ACS is
often performed by emergency department or general medical
physicians. It is important that patients at high risk or those
with ongoing ischaemia receive urgent cardiology review and
definitive treatment with coronary angiography and PCI (Fig 4).
Diagnosis is made from a combination of clinical history, ECG
changes and cardiac troponin release. Troponin is a component
of the myocardial contractile apparatus that is released from
damaged myocytes. It is not detectable in healthy subjects.
There are a number of commercially available assays, most of
which test for troponin T or troponin I. Normal ranges can
vary significantly between assays. Furthermore, some manufac-
turers also quote different cut-off values for males and females.
A number of studies have demonstrated that elevated troponin
is associated with increased risk of mortality.7,10 More recently,
Fig 2. Coronary angiogram of patient presenting with inferior ST- high sensitivity troponin assays have become available, allow-
elevation myocardial infarction. A – occluded right coronary artery (arrow); ing for early diagnosis and ‘early rule out’ of NSTEMI within
B – successful restoration flow following implantation of a drug-eluted stent. 3 hours of onset of chest pain when used appropriately.11,12
s44 © Royal College of Physicians 2016. All rights reserved.
CMJv16n6S-Rakhit.indd 44 23/11/16 9:41 AM
Acute coronary syndromes
Box 1. Subtypes of myocardial infarction6
> Type 1: spontaneous myocardial infarction
Related to atherosclerotic plaque rupture, ulceration, fissuring, erosion or dissection with resultant intraluminal thrombus leading to
decreased myocardial blood flow or distal platelet emboli with ensuing myocyte necrosis.
> Type 2: myocardial infarction secondary to ischaemic imbalance
Myocardial injury with necrosis where a condition other than CAD contributes to imbalance between myocardial oxygen supply and/
or demand, eg coronary endothelial dysfunction, coronary artery spasm, coronary embolus, arrhythmia, anaemia, respiratory failure,
hypotension, hypertension.
> Type 3: myocardial infarction resulting in death when biomarker values are unavailable
Cardiac death with symptoms suggestive of myocardial ischaemia and presumed new ischaemic ECG changes or new left bundle branch
block (LBBB), but death occurring before blood samples could be obtained or before cardiac biomarker could rise.
> Type 4a: myocardial infarction related to PCI
Defined as elevation of troponin more than five times the 99th percentile of upper reference level in patients with normal baseline values, or a
rise in troponin greater than 20% of baseline value. In addition, either (i) symptoms suggestive of myocardial ischaemia, (ii) new ischaemic ECG
changes, (iii) angiographic loss of patency of major coronary artery or side branch or reduced flow, or (iv) imaging evidence of new regional wall
motion abnormality of loss of viable myocardium.
> Type 4b: myocardial infarction related to stent thrombosis
Stent thrombosis on angiography or autopsy with an associated rise and/or fall in cardiac biomarker values.
> Type 5: myocardial infarction related to CABG
Elevation in cardiac biomarkers values more than 10 times with 99th percentile of upper reference level in patients with normal baseline
values. In addition, either (i) new pathological Q waves or LBBB, (ii) angiographic evidence of new graft or native coronary artery
occlusion, or (iii) imaging evidence of new regional wall motion abnormality of loss of viable myocardium.
CABG = coronary artery bypass surgery; CAD = coronary artery disease; ECG = electrocardiogram; PCI = percutaneous coronary intervention
While there is often a reliance on cardiac troponin, it is above upper limit of normal) should prompt investigation for
important to remember that a number of patients may have alternative diagnoses.13 For high sensitivity troponin assays,
unstable coronary disease without troponin release. It is a fivefold increase has greater than 90% positive predictive
therefore important that the result is put into clinical context. value for detection of myocardial infarction, whereas a three
Additionally, troponin may be falsely elevated in conditions fold increase has a positive predictive value of only 50–60%.14
such as renal failure, pulmonary embolism, myocarditis and The next generation of troponin assays have the potential
heart failure. Serial testing at presentation then again after to diagnose myocardial infarction within 1 hour and are
3 hours is now incorporated in many guidelines. Dynamic already in use in some centres.15 These are commonly used
rise in troponin (with or without signs and symptoms of in conjunction with risk scores and, as long as the sample is
myocardial ischaemia) is consistent with a diagnosis of collected more than 2 hours after onset of symptoms, may allow
myocardial infarction, whereas no change (even if elevated for rapid discharge of patients without ACS.
Fig 3. Example of 12-lead
electrocardiogram showing
antero-lateral T wave inversion
(leads V2–V6, I and aVL)
consistent with non-ST
elevation-acute coronary
syndrome.
© Royal College of Physicians 2016. All rights reserved. s45
CMJv16n6S-Rakhit.indd 45 23/11/16 9:41 AM
Tushar Kotecha and Roby D Rakhit
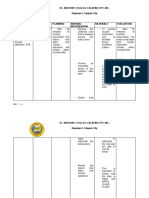
Box 3. Recommendations for timing of coronary
angiography NSTE-ACS according to clinical risk
Very high risk: coronary angiography recommended in <2 hours
> mechanical complications of MI
> dynamic ST/T changes
> acute HF
High risk: coronary angiography recommended in <24 hours
> positive troponin
> dynamic ST/T changes
Fig 4. Coronary angiogram of a patient presenting with non-ST > GRACE score>140
elevation-acute coronary syndrome. Electrocardiogram showed anterior
T wave inversion. A – critical stenosis in proximal left anterior descending Intermediate risk: coronary angiography recommended <72 hours
artery (arrow); B – successful restoration of flow following implantation of a > Diabetes
drug-eluted stent.
> CKD (eGFR<60)
> EF<40% or congestive HF
> prior PCI or CABG
A number of risk scoring systems have been developed
> early post MI angina
to highlight those at highest risk and in need of urgent
intervention. The two most commonly used are GRACE > GRACE score>109 and <140
(Global Registry of Acute Coronary Events) and TIMI Low risk
(Thrombolysis in Myocardial Infarction). GRACE is based
> Any characteristics not mentioned above
on a multinational registry of over 70,000 patients admitted
with ACS.16 The primary endpoint was all-cause mortality at CABG = coronary artery bypass surgery; CKD = chronic kidney disease;
ECG = electrocardiogram; EF = ejection fraction; eGFR = estimated glomerular
6 months. From this, nine predictors of mortality were derived filtration rate; GRACE = Global Registry of Acute Coronary Events; HF = heart
(Box 2). Points are allocated to each of the predictors to give an failure; MI = myocardial infarction; NSTE-ACS = Non-ST elevation-acute
overall score, which correlates to an in-hospital and 6-month coronary syndrome; PCI = percutaneous coronary intervention
mortality risk. A GRACE score above 140 is defined as high risk
and associated with more than 2.8% risk of in-hospital death.16
An early invasive strategy with coronary angiography within arrhythmia or haemodynamic instability, an early invasive
24 hours has been shown to be better than a delayed strategy strategy (within 24 hours) for those with a GRACE score greater
(more than 36 hours) for patients within this group.17 than 140, and coronary angiography within 72 hours for those
Current UK and European guidelines recommend inpatient with low to intermediate risk.13
coronary angiography for patients presenting with NSTE- Contemporary UK data suggest there is room for
ACS. Timing is based on assessment of risk (Box 3). National improvement in timely access to coronary angiography. In
Institute for Health and Care Excellence (NICE) guidelines 2014, only 54% of patients presenting with NSTEMI underwent
recommend urgent coronary angiography within 24 hours for coronary angiography within 72 hours and 67% within
patients who are clinically unstable, for example those with 96 hours.3 These figures are likely to be as a consequence of
ongoing chest pain, and within 72 hours for all other patients.18 many patients being admitted to hospitals without coronary
European Society of Cardiology guidelines recommend intervention facilities and with lack of access to early cardiology
urgent coronary angiography within 2 hours for patients specialist input. Centres have introduced novel pathways to
with refractory angina, associated heart failure, ventricular expedite access to coronary angiography. Examples include
> direct referral of selected patients from the emergency depart-
Box 2. Predictors of 6-month mortality following ACS16 ment in district general hospitals to the cardiology team at the
> Age per 10-year increase above 40 years closest heart attack centre with a 24-hour PCI service
> direct access for the ambulance service to the heart attack
> History of previous myocardial infarction
centre for patients with high-risk NSTE-ACS.19
> Heart failure
> Tachycardia ST-elevation myocardial infarction
> Hypotension
Primary PCI is now established as the optimal revascularisation
> Elevated serum creatinine method for STEMI in the UK. This is as a result of data showing
> Elevated cardiac enzymes improved mortality, non-fatal myocardial infarction and stroke
> ST-segment deviation on ECG compared with fibrinolysis.20 This is based on the ability to
deliver primary PCI in a timely manner. Where primary PCI
> Absence of in-hospital PCI
cannot be reliably delivered within 120 minutes, fibrinolysis may
ACS = acute coronary syndrome; ECG = electrocardiogram; PCI = percutaneous still be considered as an option. Heart attack centres have been
coronary intervention
set up to rapidly mobilise staff and deliver immediate treatment
s46 © Royal College of Physicians 2016. All rights reserved.
CMJv16n6S-Rakhit.indd 46 23/11/16 9:41 AM
Acute coronary syndromes
upon arrival of the patient. Every minute treatment is delayed for the safety of shortening dual antiplatelet therapy to as
results in myocardial damage and consequent increased risk of little as 1 month.30 Therefore, selected patients with high
mortality. A door-to-balloon time of 30 minutes is associated cardiovascular risk or recurrent events may benefit from
with 3% in-hospital mortality compared with 6% mortality at prolonged antiplatelet therapy beyond 1 year whereas those
120 minutes and 9% at 180 minutes.21 In the UK, more than with lower cardiovascular risk and/or high bleeding risk may be
90% of patients receive primary PCI within 90 minutes of treated with a shorter course of dual antiplatelet therapy.
admission to a heart attack centre.3 Door-to-balloon (and call-
to-balloon) times can be reduced by ambulance crews delivering Anticoagulant therapy
patients directly to the cardiac catheterisation laboratory rather
than admitting via the emergency department.22 In addition to antiplatelet therapy, low molecular weight
The majority of routine and primary PCI in the UK is now heparins are recommended in the acute phase of NSTE-
undertaken via the radial rather than femoral route. This has ACS prior to angiography. Commonly used agents include
been shown to reduce mortality and complications such as enoxaparin, dalteparin and tinzaparin. The factor Xa inhibitor
major bleeding.23,24 It also allows for early mobilisation and fondaparinux is now preferred in many centres as it has been
discharge, and is generally preferred by patients. shown to be non-inferior to enoxaparin with 50% reduced
bleeding risk.31 Anticoagulation is not routinely prescribed
Antiplatelet therapy long term following ACS. However, there is evidence that
novel anticoagulants (NOAC), such as rivaroxaban, improve
A key pathological feature of acute coronary syndrome is platelet outcomes following ACS; this is at the expense of increased
activation, which results in thrombin generation, activation of bleeding.32 NICE currently recommends the addition of
the coagulation cascade and release of inflammatory mediators.25 rivaroxaban in selected high-risk patients.33
Anti-thrombotic pharmacotherapy is therefore an important A subset of patients presenting with ACS may have another
adjunct to PCI and an integral part of secondary prevention. indication for long-term anticoagulation, such as atrial
The mainstay of acute and long-term management includes fibrillation. Triple therapy with aspirin, clopidogrel and
aspirin and a P2Y12 inhibitor, such as clopidogrel or ticagrelor. warfarin (or NOAC) is associated with a significantly increased
Clopidogrel is a thienopyridine drug that results in irreversible bleeding risk compared with dual antiplatelet therapy.34
platelet inhibition. It is a pro-drug with an onset of action of However, effective platelet inhibition is essential in the early
2–4 hours and duration of effect of up to 10 days. Ticagrelor is a phase following PCI to reduce the risk of early stent thrombosis.
new P2Y12 inhibitor that does not require metabolism to an active It is therefore suggested that patients with low bleeding risk are
metabolite. It causes reversible platelet inhibition and has a rapid treated with triple therapy for 6 months following PCI, followed
onset of action (approximately 30 minutes). This is theoretically by dual therapy with warfarin (or NOAC) plus aspirin or
advantageous in the acute phase where rapid platelet inhibition clopidogrel for another 6 months.13 Patients with high bleeding
is required. The duration of effect is 3–4 days. The CURE risk should be treated with triple therapy for 1 month, followed
(Clopidogrel in Unstable angina to prevent Recurrent Events) by warfarin (or NOAC) plus aspirin or clopidogrel for the
study initially showed benefit for clopidogrel in addition to remainder of the year.13 After 1 year, treatment with warfarin
aspirin in reducing cardiovascular death, myocardial infarction (or NOAC) alone is recommended.
and stroke for patients with ACS.26 More recently, the PLATO
(PLATelet inhibition and patient Outcomes) study showed Conclusions
benefit for ticagrelor over clopidogrel for the same endpoints
without a significant increase in major bleeding.27 However, there ACS is a common presentation to acute services. There is
was an increase in non-major bleeding with ticagrelor. Cangrelor a clearly defined treatment pathway for STEMI with direct
is a new intravenous reversible antiplatelet agent. It has a rapid admission to heart attack centres with a view to emergency
onset within a few minutes and duration of effect of 1–2 hours. PCI. NSTE-ACS is a more common presentation of ACS,
While not currently used in routine practice in the UK, it has affecting an older cohort of patients – often with more complex
shown potential in the acute phase of STEMI where rapid platelet comorbidities. Management pathways vary, resulting in
inhibition is required.28 variable times to cardiology review and definitive treatment.
Current guidelines recommend dual antiplatelet therapy Initial management is with anti-thrombotic therapy with a
for 1 year following ACS.13 This was partly based on the risk view to PCI in a timely manner. Advances in the sensitivity of
of stent thrombosis with early generation drug eluting stents. cardiac biomarkers and risk assessment tools now enable rapid
However, there is now a move towards tailored antiplatelet diagnosis within a few hours of symptoms onset. Advances
therapy according to the clinical need and bleeding risk of in invasive management and drug therapy have resulted in
the individual patient. The recent DAPT (Dual Antiplatelet improved short-term and long-term clinical outcomes. ■
Therapy) study showed that dual antiplatelet therapy beyond
1 year (compared with aspirin alone) after implantation Conflicts of interest
of a drug eluting stent significantly reduced the risk of
The authors have no conflicts of interest to declare.
stent thrombosis and major adverse cardiovascular and
cerebrovascular events but with an associated increase in risk of
bleeding.29 This bleeding risk is highest in older patients, those References
with existing coagulation defects and those with comorbidities, 1 Murray CJ, Lopez AD. Alternative projections of mortality and
including liver and renal failure. With the introduction of disability by cause 1990–2020: Global Burden of Disease Study.
new generation drug eluting stents, there is emerging evidence Lancet 1997;349:1498–504.
© Royal College of Physicians 2016. All rights reserved. s47
CMJv16n6S-Rakhit.indd 47 23/11/16 9:41 AM
Tushar Kotecha and Roby D Rakhit
2 Yeh RW, Sidney S, Chandra M et al. Population trends in the 18 National Institute for Health and Care Excellence. Unstable angina
incidence and outcomes of acute myocardial infarction. N Engl J and NSTEMI: early management. NICE clinical guideline No 94.
Med 2010;362:2155–65. London: NICE, 2013.
3 Weston C, Gavalova L, Whittaker T, Van Leeven R. Myocardial 19 Koganti S, Rakhit RD. Management of high-risk non-ST elevation
Ischaemia National Audit Project: how the NHS cares for patients myocardial infarction in the UK; need for alternative models of
with heart attack. Annual Public Report April 2013 - March 2014. care to reduce length of stay and admission to angiography times.
London: MINAP NICOR, 2014. www.ucl.ac.uk/nicor/audits/minap/ Clin Med 2015;15:522–5.
documents/annual_reports/minap-public-report-2014 [Accessed 9 20 Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intra-
November 2016]. venous thrombolytic therapy for acute myocardial infarction: a
4 Chan MY, Sun JL, Newby K et al. Long-term mortality of patients quantitative review of 23 randomised trials. Lancet 2003;361:13–20.
undergoing cardiac catheterisation for ST-elevation and non-ST- 21 Rathore SS, Curtis JP, Chen J et al. Association of door-to-balloon
elevation myocardial infarction. Circulation 2009;119:3110–7. time and mortality in patients admitted to hospital with ST elevation
5 Smolina K, Wright L, Rayner M, Goldacre MJ. Determinants of the myocardial infarction: national cohort study. BMJ 2009;338:b1807.
decline in mortality from acute myocardial infarction in England 22 Majumder B, Mavroudis C, Smith C et al. Superior outcome with
between 2002 and 2010: linked national database study. BMJ direct catheter laboratory access versus ED-activated primary percu-
2012:344:d8059. taneous coronary intervention. Am J Emerg Med 2012;30:1118–24.
6 Thygesan K, Alpert JS, Jaffe AS et al. Third universal definition of 23 Mehta SR, Jolly SS, Cairns J et al. Effects of radial versus femoral
myocardial infarction. Circulation 2012;126:2020–35. artery access in patients with acute coronary syndromes with or
7 The Global Use of Strategies to Open Occluded Arteries (Gusto) without ST-segment elevation. J Am Coll Cardiol 2012;60:2490–9.
IIb Investigators. A comparison of recombinant hirudin with 24 Valgimigli M, Gagnor A, Calabro P et al. Radial versus femoral
heparin for the treatment of acute coronary syndromes. N Engl J access in patients with acute coronary syndromes undergoing
Med 1996:335:775–82. invasive management: a randomised multicentre trial. Lancet
8 FRagmin and Fast Revascularisation during InStability in Coronary 2015;385:2465–76.
artery disease (FRISC II) Investigators. Invasive compared with non- 25 Storey RF. New P2Y12 inhibitors. Heart 2011;97:1262–7.
invasive treatment in unstable coronary artery disease: FRISC II 26 The Clopidogrel in Unstable Angina to Prevent Recurrent Events
prospective randomised multicentre study. Lancet 1999;354:708–15. Trial Investigators. Effects of clopidogrel in addition to aspirin
9 Anderson HV, Cannon CP, Stone PH et al. One-year results of the in patients with acute coronary syndromes without ST-segment
Thrombolysis in Myocardial Infarction (TIMI) IIIb clinical trial. A elevation. N Engl J Med 2001;345:494–502.
randomised comparison of tissue-type plasminogen activator versus 27 Wallentin L , Becker RC , Budaj A et al. Ticagrelor
placebo and early invasive versus early conservative strategies in versus clopidogrel in patients with acute coronary
unstable angina and non-Q wave myocardial infarction. J Am Coll syndromes. N Engl J Med 2009 ; 361 : 1045 – 57 .
Cardiol 1995;26:1643–50. 28 Franchi F, Rollini F, Park Y, Angiolillo DJ. A safety evaluation
10 Bohula May EA, Bonaca MP, Jarolim P et al. Prognostic performance of cangrelor in patients undergoing PCI. Expert Opin Drug Saf
of a high sensitivity cardiac troponin I assay in patients with non-ST- 2016;15:275–85.
elevation acute coronary syndrome. Clin Chem 2014;60:158–64. 29 Mauri L, Kereiakes DJ, Yeh RW et al. Twelve or 30 months of
11 Keller T, Zeller T, Peetz D et al. Sensitive troponin I assay in dual anti-platelet therapy after drug eluting stents. N Engl J Med
early diagnosis of acute myocardial infarction. N Engl J Med 2014;371:2155–66.
2009;361:868–77. 30 Urban P, Meredith IT, Abizaid A et al. Polymer-free drug-coated stents
12 Reichlin T, Hochholzer W, Bassetti S et al. Early diagnosis of in patients at high bleeding risk. N Engl J Med 2015;373:2038–47.
myocardial infarction with sensitive cardiac troponin assays. 31 Mehta SR, Granger CB, Eikelboom JW et al. Efficacy and safety of
N Engl J Med 2009;361:858–67. fondaparinux versus enoxaparin in patients with acute coronary
13 Roffi M, Patrono C, Collett JP et al. 2015 ESC guidelines for syndromes undergoing percutaneous coronary intervention: results
the management of acute coronary syndromes in patients from the OASIS-5 trial. J Am Coll Cardiol 2007;50:1742–51.
presenting without persistent ST-segment elevation. Eur Heart J 32 Mega JL, Baunwald E, Wiviott SD. Rivaroxaban in patients with a
2015;320:267–315. recent acute coronary syndrome. N Engl J Med 2012;366:9–19.
14 Giannitsis E, Becker M, Kurz K et al. High-sensitivity cardiac 33 National Institute for Health and Care Excellence. Rivaroxaban for
troponin T for early prediction of evolving non-ST-segment preventing adverse outcomes after acute management of acute coronary
elevation myocardial infarction in patients with suspected acute syndromes. NICE technology appraisal No 335. London: NICE, 2015.
coronary syndrome and negative troponin results on admission. 34 Dewilde WJ, Oirbans T, Verheugt FW et al. Use of clopidogrel with
Clin Chem 2010;56:642–50. or without aspirin in patients taking oral anticoagulant therapy and
15 Reichlin T, Schindler C, Drexler B et al. One-hour rule-out and undergoing percutaneous coronary intervention: an open-label,
rule-in of acute myocardial infarction using high-sensitivity cardiac randomised, controlled trial. Lancet 2013;381:1107–15.
troponin T. Arch Intern Med 2012;172:1211–18.
16 Eagle KA, Lim MJ, Dabbous OH et al. A validated prediction model
for all forms of acute coronary syndrome: estimating the risk of
6-month post-discharge death in an international registry. J Am
Med Assoc 2004;291:2727–33. Address for correspondence: Dr R Rakhit, Cardiology
17 Mehta SR, Granger CB, Boden WE et al. Early versus delayed Department, Royal Free Hospital, Pond Street, London NW3
intervention in acute coronary syndromes. N Engl J Med 2QG, UK.
2009;360:2165–75. Email: Roby.rakhit@nhs.net
s48 © Royal College of Physicians 2016. All rights reserved.
CMJv16n6S-Rakhit.indd 48 23/11/16 9:41 AM
You might also like
- Acute Coronary Syndrome (ACS)Document12 pagesAcute Coronary Syndrome (ACS)swastikNo ratings yet
- Acute Coronary SyndromesDocument8 pagesAcute Coronary Syndromesadek07No ratings yet
- Coronary Artery Disease (Cad)Document4 pagesCoronary Artery Disease (Cad)Freddy PanjaitanNo ratings yet
- ACS ST ElevationDocument5 pagesACS ST ElevationNers BorRegNo ratings yet
- Acute Coronary Syndromes: Unstable Angina and Non-ST Elevation Myocardial InfarctionDocument18 pagesAcute Coronary Syndromes: Unstable Angina and Non-ST Elevation Myocardial InfarctionLOZANO GARCIA PAOLA ALEJADRANo ratings yet
- The Challenge of Acute Coronary Syndromes: Maarten L Simoons, Eric Boersma, Coen Van Der Zwaan, Jaap W DeckersDocument4 pagesThe Challenge of Acute Coronary Syndromes: Maarten L Simoons, Eric Boersma, Coen Van Der Zwaan, Jaap W DeckerssukandeNo ratings yet
- Acute Coronary Syndrome (ACS) Is Usually One of Three Diseases InvolvingDocument7 pagesAcute Coronary Syndrome (ACS) Is Usually One of Three Diseases InvolvingArianne BernardoNo ratings yet
- Acutecoronarysyndromeacs 180106041458Document82 pagesAcutecoronarysyndromeacs 180106041458Razvan SulaimanNo ratings yet
- 2022 JAMA Diagnosis and Treatment of ACSDocument14 pages2022 JAMA Diagnosis and Treatment of ACSPeter Albeiro Falla Cortes100% (1)
- Iam 2022Document14 pagesIam 2022Mateo Daniel Gutierrez CastañedaNo ratings yet
- 201 FullDocument14 pages201 FullMelita Aditya SariNo ratings yet
- It Is Myocardial Infarction With Non-Obstructive Coronary Arteries: A Myth or Reality?Document4 pagesIt Is Myocardial Infarction With Non-Obstructive Coronary Arteries: A Myth or Reality?asclepiuspdfsNo ratings yet
- Atwood Management of Acute Coronary Syndrome 2022Document14 pagesAtwood Management of Acute Coronary Syndrome 2022goten ramirezNo ratings yet
- Management of Cardiogenic Shock After Acute - 2023Document10 pagesManagement of Cardiogenic Shock After Acute - 2023Angy KarakostaNo ratings yet
- Management of Acute Coronary SyndromeDocument14 pagesManagement of Acute Coronary SyndromeMartha Isabel BurgosNo ratings yet
- Acute Coronary SyndromeDocument12 pagesAcute Coronary SyndromeJerick Michael FrancoNo ratings yet
- Treatment of NSTEMI Non-ST Elevation Myocardial inDocument12 pagesTreatment of NSTEMI Non-ST Elevation Myocardial inDavy JonesNo ratings yet
- Piis0140673621023916 2Document12 pagesPiis0140673621023916 2CAMILO FERRERO RESTREPONo ratings yet
- 10.1038@s41572 019 0090 3Document20 pages10.1038@s41572 019 0090 3sari100% (1)
- Acs 33 241Document9 pagesAcs 33 241Ratna AyieNo ratings yet
- Myocardial Infarction, Acute Case FileDocument7 pagesMyocardial Infarction, Acute Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Treatment Strategies of NSTEMI-ACS With Multivessel Disease: Gani Bajraktari, Michael Y. HeneinDocument3 pagesTreatment Strategies of NSTEMI-ACS With Multivessel Disease: Gani Bajraktari, Michael Y. HeneinolisNo ratings yet
- Basra 2014Document18 pagesBasra 2014Pratama InsaniNo ratings yet
- Severe Obstructive Sleep Apnea Is Associated With Coronary Microvascular PDFDocument9 pagesSevere Obstructive Sleep Apnea Is Associated With Coronary Microvascular PDFumyNo ratings yet
- Severe Obstructive Sleep Apnea Is Associated With Coronary Microvascular PDFDocument9 pagesSevere Obstructive Sleep Apnea Is Associated With Coronary Microvascular PDFumyNo ratings yet
- Ekg STDocument23 pagesEkg STisaNo ratings yet
- 2022 Acute Coronary SyndromesDocument13 pages2022 Acute Coronary SyndromesOmar Alejandro Agudelo ZuluagaNo ratings yet
- Troponina predicción oclusión totalDocument5 pagesTroponina predicción oclusión totalmanuel-gnNo ratings yet
- 856 t2sv87Document6 pages856 t2sv87AntonisNo ratings yet
- Strokeaha 120 033994Document8 pagesStrokeaha 120 033994bozasnachoNo ratings yet
- Acute Coronary SyndromeDocument18 pagesAcute Coronary SyndromeKartika RahmawatiNo ratings yet
- Presentasi ACS SHTB - 29 Sept 2018Document58 pagesPresentasi ACS SHTB - 29 Sept 2018Anonymous toclkWvnNo ratings yet
- Cartlidge Timothy Role of Percutaneous CoronaryDocument7 pagesCartlidge Timothy Role of Percutaneous Coronarybruno baileyNo ratings yet
- Acute Coronary Syndrome - StatPearls - NCBI BookshelfDocument5 pagesAcute Coronary Syndrome - StatPearls - NCBI BookshelfYe YulianNo ratings yet
- Pharmacotherapy of Non ST-elevation ACS (Adel Khalil Assignment)Document30 pagesPharmacotherapy of Non ST-elevation ACS (Adel Khalil Assignment)عادل خليلNo ratings yet
- Chapter IDocument36 pagesChapter INaily Nuzulur RohmahNo ratings yet
- Angina Contemporary Diagnosis and ManagementDocument12 pagesAngina Contemporary Diagnosis and Managementalejandro montesNo ratings yet
- 031-035 RevACS NT150217 NEWDocument5 pages031-035 RevACS NT150217 NEWUtari Melinda YanzamiNo ratings yet
- Acute Coronary Syndrome GuideDocument55 pagesAcute Coronary Syndrome GuideShafid HamzabNo ratings yet
- Contemporary Reviews in Cardiovascular Medicine: Cardiogenic ShockDocument13 pagesContemporary Reviews in Cardiovascular Medicine: Cardiogenic ShockIsmi WulandariNo ratings yet
- OMI 2018, MirandaDocument14 pagesOMI 2018, MirandaResidentes UrgenciasNo ratings yet
- Acute Coronary SyndromeDocument45 pagesAcute Coronary SyndromeParsa EbrahimpourNo ratings yet
- Acute Coronary Syndrome ACSDocument9 pagesAcute Coronary Syndrome ACSChen BrionesNo ratings yet
- Principle Management of Acute Coronary Syndrome: Nahar Taufiq Bagian Kardiologi Dan Kedokteran Vaskuler FK UGM YogyakartaDocument57 pagesPrinciple Management of Acute Coronary Syndrome: Nahar Taufiq Bagian Kardiologi Dan Kedokteran Vaskuler FK UGM YogyakartaIntan Farida YasminNo ratings yet
- Managing Ischemic Heart DiseasesDocument14 pagesManaging Ischemic Heart DiseasesNoveno CNo ratings yet
- Chest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsDocument16 pagesChest Pain Evaluation and Management - 2023 - Physician Assistant ClinicsJose AnaconaNo ratings yet
- J Jacadv 2022 100120Document14 pagesJ Jacadv 2022 100120Axel Hiram Hernandez PinedaNo ratings yet
- 6 PDFDocument15 pages6 PDFLivianty HukubunNo ratings yet
- Acute Coronary Syndromes - ClinicalKeyDocument64 pagesAcute Coronary Syndromes - ClinicalKeyERNESTONo ratings yet
- Coronary Microvascular Disease Pathogenic Mechanisms and Therapeutic OptionsDocument17 pagesCoronary Microvascular Disease Pathogenic Mechanisms and Therapeutic OptionsZuleynny TellesNo ratings yet
- 1 Ijmpsdec20171Document12 pages1 Ijmpsdec20171TJPRC PublicationsNo ratings yet
- A Standardized and Comprehensive Approach To The Management of Cardiogenic Shock 2020Document13 pagesA Standardized and Comprehensive Approach To The Management of Cardiogenic Shock 2020gloriaNo ratings yet
- Dogan 2012Document7 pagesDogan 2012Davy JonesNo ratings yet
- Definitions: 1. Patients With Acute Chest Pain and Persistent ( 20 Min) ST-segment ElevationDocument20 pagesDefinitions: 1. Patients With Acute Chest Pain and Persistent ( 20 Min) ST-segment ElevationErick SusantoNo ratings yet
- SVN 2019 000305Document10 pagesSVN 2019 000305zak sutomoNo ratings yet
- Dr. Achmad Lefi, SP JP - Acute Coronary SyndromeDocument43 pagesDr. Achmad Lefi, SP JP - Acute Coronary Syndromek5ng8ntNo ratings yet
- Ersboll LVMD For Early Echocardiographic Prediction of Aritmia and SCDDocument10 pagesErsboll LVMD For Early Echocardiographic Prediction of Aritmia and SCDauliaNo ratings yet
- Anestesia en Ptes Con Enfermedad CardíacaDocument6 pagesAnestesia en Ptes Con Enfermedad CardíacaRalfNo ratings yet
- Understanding Angina Pectoris and the Importance of Assessing Pretest ProbabilityDocument11 pagesUnderstanding Angina Pectoris and the Importance of Assessing Pretest ProbabilityAndi NamirahNo ratings yet
- Sean Jharod C. Bolofer C-Section or Caesarean Section Birth DeliveryDocument2 pagesSean Jharod C. Bolofer C-Section or Caesarean Section Birth DeliveryseanjharodNo ratings yet
- GL On Pertussis Case ManagementDocument32 pagesGL On Pertussis Case Managementnazurah HamidNo ratings yet
- Effect of Steam Inhalation On Nasal Mucociliary Clearance in Normal Individuals and Nasal Disease Sta PDFDocument3 pagesEffect of Steam Inhalation On Nasal Mucociliary Clearance in Normal Individuals and Nasal Disease Sta PDFyolandaNo ratings yet
- Physical Assessment - General Survey GuideDocument2 pagesPhysical Assessment - General Survey GuideDanielle TorresNo ratings yet
- TechTalk Sodium CitrateDocument2 pagesTechTalk Sodium Citrated40sithui50% (2)
- Disease EssayDocument4 pagesDisease Essayapi-280310261No ratings yet
- Postmortem Toxicology - Farmasi ForensikDocument20 pagesPostmortem Toxicology - Farmasi Forensikedrina elfia rosaNo ratings yet
- St. Anthony College Calapan City, Inc. Bayanan I, Calapan CityDocument3 pagesSt. Anthony College Calapan City, Inc. Bayanan I, Calapan CityMike Faustino SolangonNo ratings yet
- Ms - CardiovascularDocument70 pagesMs - CardiovascularMark OngNo ratings yet
- What Are The Symptoms of Frozen Shoulder?Document3 pagesWhat Are The Symptoms of Frozen Shoulder?Georgij VeshoskiNo ratings yet
- Defibrillator: DR Sumanth ReddyDocument39 pagesDefibrillator: DR Sumanth Reddyrohith100% (1)
- Perinatal Mental Health Policy BriefDocument3 pagesPerinatal Mental Health Policy BriefThe Wilson CenterNo ratings yet
- Typhlitis: Clinical Presentation and DiagnosisDocument2 pagesTyphlitis: Clinical Presentation and DiagnosisMUWANGUZI ALEXANDERNo ratings yet
- FNCP OutputDocument6 pagesFNCP OutputRenz AnggoyNo ratings yet
- AS Biology F211 Animal Transport Workbooklet Answers p1-10Document11 pagesAS Biology F211 Animal Transport Workbooklet Answers p1-10T-Jay Ellis-DaleNo ratings yet
- Analisis Kesesuaian Penggunaan Antiinfeksi Pada Infeksi Oportunistik Pasien Hiv/Aids Rawat Inap Di Rsup Dr. Sardjito YogyakartaDocument7 pagesAnalisis Kesesuaian Penggunaan Antiinfeksi Pada Infeksi Oportunistik Pasien Hiv/Aids Rawat Inap Di Rsup Dr. Sardjito YogyakartaindahNo ratings yet
- Therapeutic Drug Monitoring: By: Adewale Akinseloyin Oluwatimilehin Agboola Oluwatosin AjibadeDocument33 pagesTherapeutic Drug Monitoring: By: Adewale Akinseloyin Oluwatimilehin Agboola Oluwatosin AjibadeJoe AjibadeNo ratings yet
- (Pediaii) - 021 - Disorders of The Respiratory TractDocument17 pages(Pediaii) - 021 - Disorders of The Respiratory TractdoktoraronaNo ratings yet
- Oxygen Delivery SystemsDocument9 pagesOxygen Delivery Systemsanon_784834955No ratings yet
- EpidemiologyDocument86 pagesEpidemiologySainab Moohamoud83% (6)
- Feasibility and Efficacy of Home Rectal Irrigation in Neonates and Early Infancy With Hirschsprung DiseaseDocument9 pagesFeasibility and Efficacy of Home Rectal Irrigation in Neonates and Early Infancy With Hirschsprung DiseaseKiki ElvianiNo ratings yet
- Amniotic MembraneDocument8 pagesAmniotic Membraneapi-481789048No ratings yet
- Lourdes College Nursing Program Drug StudyDocument2 pagesLourdes College Nursing Program Drug Studypinksapphire929100% (2)
- Abigail Martin RNDocument2 pagesAbigail Martin RNdesignxtravagantiaNo ratings yet
- Gall Bladder DiseaseDocument11 pagesGall Bladder Diseasedarellejaide100% (1)
- Patient Assessment and Safety Indicators in OphthalmologyDocument34 pagesPatient Assessment and Safety Indicators in OphthalmologyPrabhat GovindanNo ratings yet
- Identifying and Investigating OutbreaksDocument74 pagesIdentifying and Investigating OutbreaksCesarNo ratings yet
- 2 Pathophysiology EpidemiologyDocument36 pages2 Pathophysiology EpidemiologyYosefina CindyNo ratings yet
- Donning and Removing Sterile Gloves (Open Method) Preparation RationaleDocument2 pagesDonning and Removing Sterile Gloves (Open Method) Preparation RationalecharmainchavezNo ratings yet
- Understanding The Carbon Dioxide Gaps: ReviewDocument9 pagesUnderstanding The Carbon Dioxide Gaps: ReviewLaura A M MNo ratings yet