Professional Documents
Culture Documents
ABSTRACTS PRESENTED AT CONCURRENT SESSIONS November 9-10, 2014 Georgia World Congress Center Atlanta, Georgia
Uploaded by
Metallum MarionetteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ABSTRACTS PRESENTED AT CONCURRENT SESSIONS November 9-10, 2014 Georgia World Congress Center Atlanta, Georgia
Uploaded by
Metallum MarionetteCopyright:
Available Formats
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A1
ABSTRACTS
PRESENTED AT CONCURRENT SESSIONS
November 9-10, 2014
georgia world congress center
atlanta, georgia
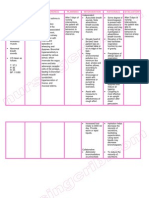
TABLE OF CONTENTS
TOPIC ABSTRACT NUMBERS PAGES
Adverse Food and Drug Reactions, Insect
Reactions, Anaphylaxis and Food Allergy
Pharmacology/Pharmacotherapeutics 1-8 A3-A5
Aerobiology, Allergens, Allergen Extracts
Immunotherapy, Immunizations 9-16 A5-A8
Asthma and Other Lower Airway Disorders 17-24 A8-A10
Basic Science Allergy and Immunology
Clinical Immunology, Immunodeficiency 25-32 A10-A13
Allergy Testing, Clinical Laboratory Immunology
Clinical Case Reports 33-40 A13-A15
Food Allergy
Rhinitis, Other Upper Airway Disorders,
Ocular Disorders 41-48 A15-A18
Other 49-56 A18-A20
Skin Disorders
Asthma, Other Lower Airway Disorders
Clinical Immunology, Immunodeficiency 57-64 A20-A22
VOLUME 113, NOVEMBER, 2014 A1
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A2
ABSTRACTS: CONCURRENT SESSIONS
A2 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A3
ABSTRACTS: CONCURRENT SESSIONS
Characteristics of the caseload of infants with SBS
1
ATYPICAL PRESENTATION OF HONEY BEE STING HYPER-
SENSITIVITY.
S. Melethil*, S. Ho, R.S. Mehta, Galveston, TX.
Introduction: A bee sting can result in a myriad of manifestations ranging
from acute localized cutaneous response to unusual delayed reactions. Here we
report a case of a 15 year old boy who developed bloody diarrhea 72 hours fol-
lowing a bee sting. To the best of our knowledge this is the first such report of
delayed gastrointestinal manifestation. Case Report: A 15 year old male pre-
sented for evaluation of allergy to honey bee. He stated that on 2 occasions he
was stung by a bee resulting in localized swelling of affected area, nausea, vom-
iting and abdominal pain after the sting, then bloody diarrhea approximately
72 hours after. The most recent episode was 1 week prior to clinic visit when
the patient was stung by a bee on his toe, following which he had a local reac-
tion. Then 3 days later he had abdominal pain and loose stools with blood.
Examination revealed a well healed puncture mark on his toe. His vitals were Table legend. SBS: short bowel syndrome. ICV+: preserved ileo-cecal valve.
normal and CBC, ESR, CMP and a stool culture were unremarkable. Skin prick
testing was positive for honey bees. Intradermal testing at lowest concentration
(1/100000) was positive for all other Hymenoptera (wasp, yellow jacket, hor- 3
net) with negative saline. Immunocap showed positivity to all Hymenoptera IMPROVING SURGICAL ANTIBIOTIC OPTIONS WITH PENI-
species. Discussion: Delayed gastrointestinal hemorrhage is an unusual man- CILLIN ALLERGY TESTING.
ifestation after sting by a honey bee that cannot be explained by IgE-mediated T. Pongdee, A. Thethi*, E. Rodrigues, J. Irizarry Alvardo, Jacksonville, FL.
mechanisms. We postulate that this response could be due to a delayed type Background: Resistance to antibiotics is a serious worldwide problem. When
hypersensitivity leading to deposition of immune complexes in the basement antibiotic choices are limited due to resistance, treatment alternatives for resist-
membrane of small blood vessels causing vasculitis. This may explain the ant infections may have higher toxicity, be more costly, and be less effective,
delayed manifestation of bloody diarrhea 72 hours after the sting. It is also pos- and thus patients with resistant infections have higher morbidity and mortal-
sible that the etiology of this unusual reaction may not be immunologically ity. Core methods to prevent antibiotic resistance include the appropriate use
mediated and may be due to a direct cytotoxic effect of honey bee venom com- and choice of antibiotics. Objective: To reduce the use of prophylactic van-
ponent like Melittin on gastrointestinal tissue. Melittin is known to cause com- comycin, levofloxacin, and clindamycin in patients with a history of penicillin
plement cleavage and the release of Bradykinin which are both associated allergy undergoing surgery by implementing a new clinical pathway consist-
with hemolysis. Studies indicate that Melittin and Phospholipase A2 can ing of allergy consultation and penicillin allergy skin testing as part of the pre-
decrease smooth muscular contractility and thus potentially induce hemorrhage. operative evaluation clinic visit. Methods: The participants in this clinical prac-
Conclusion: We report an unusual and rare case of bee sting induced bloody tice improvement project were patients with a history of penicillin allergy who
diarrhea in an adolescent which was reproducible on two different occasions. were scheduled to undergo surgery and referred by the Preoperative Evalua-
We hypothesize that this could be due to a delayed hypersensitivity reaction or tion Clinic team for allergy consultation and penicillin allergy skin testing from
a direct cytotoxic effect of bee venom. August 2012 to August 2013, the first year of this new clinical pathway. The
primary outcomes were the percent reductions in the use of prophylactic van-
comycin, levofloxacin, and clindamycin in patients with a history of penicillin
2 allergy when compared to historical controls. Results: Of the 384 patients
COW’S MILK ALLERGY IN SHORT BOWEL SYNDROME. with a history of penicillin allergy who underwent allergy consultation and
A. Diamanti, A. Fiocchi, L. Dahdah*, O. Mazzina, F. Bellucci, T. Capriati, penicillin allergy skin testing, 360 (94%) had negative penicillin allergy skin
Rome, Holy See (Vatican City State). test results and were given clearance by the allergist to receive penicillin or
Background: Early, massive exposure to milk allergens is traditionally con- cephalosporin antibiotics. For patients who had reported penicillin allergy,
sidered a risk factor for cow’s milk allergy (CMA). Epidemiological studies, within six months of implementation of this new clinical pathway, vancomycin
however, beg the question whether it can be protective; high milk allergen use was reduced by 54%, levofloxacin use was reduced by 40%, and clindamycin
exposure has also been hypothesized as policy for food allergy prevention. In use was reduced by 22% compared to historical controls. Conclusions: Pro-
this context, short bowel syndrome has been anecdotally associated with CMA, phylactic use of vancomycin, levofloxacin, and clindamycin in patients with a
and no studies have used confirmatory milk challenges. Methods: A review history of penicillin allergy undergoing surgery can be reduced by allergy
of consecutive patients followed with short bowel syndrome over a ten-year consultation and penicillin allergy skin testing during the preoperative evalu-
period at a tertiary pediatric institution. Patients included only the patients ation process.
who fulfilled the following criteria: - Intestinal failure following SBS, defined
as dependency on parenteral nutrition providing at least 50% of the total
required intake for at least three months - Clinical follow-up from surgery to 4
the complete introduction of a diversified diet including cow’s milk proteins. A CASE OF NEAR FATAL ANAPHYLAXIS TO ORANGE IN A
Infants with symptoms of CMA underwent a milk-specific IgE sensitization TODDLER.
test and a confirmatory oral milk challenge. Results: Three infants in a case- S.B. Sindher*, S.P. DaVeiga, Philadelphia, PA.
load of 32 eligible patients were confirmed with CMA at challenge (see Table). Introduction: Most fruit allergies manifest as pollen-food allergy syndrome
This 9.4% proportion represents two to ten-folds the incidence of CMA in characterized by pruritus and edema of the lips, tongue, palate and throat usu-
open populations. Conclusion: With its 9.4% incidence, our caseload of SBS ally a few minutes after ingestion of the raw fruit. Orange is among fruits that
children carry a two- to tenfold risk of CMA compared to open populations. are associated with pollen-food allergy syndrome but rarely causes anaphy-
This suggests that a low digestive capacity may play a role in the high inci- laxis. Methods: We review the case of a 31-month-old girl who developed severe
dence of food allergy in children. As their peptic digestion is not complete anaphylaxis after the consumption of one Cutie® orange. Results: A 31-month-
during early life, protein remnants of the diet could act as allergens. If the over- old female presented in anaphylactic shock to an emergency department (ED).
exposure to milk allergens is among the causes of CMA in these children, our Prior to presentation, she was at a supermarket, ate one Cutie® orange and
results warn against the hypothesis of massive antigen exposure as instru- was playing with the orange peel. Within a few minutes she had bilateral peri-
ment of food allergy prevention. orbital swelling and pruritis. She was treated with diphenhydramine at the super-
market. The patient developed lip and tongue swelling and respiratory distress
so her parents drove her to the ED within 10 minutes. Examination was notable
for a pulse oximetry reading of 79% on room air, diffuse wheezing in all lung
fields, lip and tongue angioedema and hives. She was treated with nebulized
albuterol, IV diphenhydramine, ranitidine, 2 doses of subcutaneous epineph-
rine, methylprednisolone and an IV bolus of normal saline. She continued to
VOLUME 113, NOVEMBER, 2014 A3
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A4
ABSTRACTS: CONCURRENT SESSIONS
have worsening respiratory distress and hypoxia and subsequently required laboration with Heinz, using the same rice-free flour to make pasta to which
intubation; she was noted to have significant upper airway edema on intuba- she did not react. Introduction of solids was predicated on a series of OFCs,
tion. After intubation she was transferred via a helicopter to a Pediatric Inten- including wheat, beef, pork, chicken, potato, carrot, spinach, zucchini, toma-
sive Care Unit. A chest x-ray was performed to check endotracheal tube place- toes which were negative. However, each introduction of foods contaminated
ment and revealed right upper lobe atelectasis and pulmonary edema (Figure with rice determined the characteristic symptoms of the syndrome. In one occa-
1). Her symptoms improved overnight and she was discharged home after a 48- sion, a typical FPIES reaction followed the administration of mauve supposi-
hour hospitalization. Her past medical history was notable for a varied diet tories containing rice starch. Conclusion: This case highlights how FPIES onset
and prior consumption of orange juice without reaction. She had reported nightly can be very early and how tiny amount of food can be enough to provoke symp-
cough at baseline with cough on exertion but was not on therapy for asthma. toms, reflecting the degree of hypersensitivity in individual patients. Early
In follow up at Allergy/Immunology as a new patient, she had a positive skin recognition of this condition and the management with cross-contaminant-free
prick test result to orange and peach. She was advised to avoid orange and peach baby foods are crucial in preventing recurrences. The co-operation among pedi-
and also started on asthma therapy. Conclusion: We present the first case report atricians and industry is of outstanding importance.
of near-fatal anaphylaxis to orange in a toddler. This case confirms that poorly
controlled asthma is a risk factor for difficult to treat IgE-mediated reactions
to foods, including orange. 6
EFFECT OF DEVICE AND FORM FACTOR ON AUTO-INJECTOR
APPLICATION FORCE AND EFFICIENCY.
A. Barbir*1, M. Janelli1, M. Lin1, R.A. Wolf2, J. Dennerlein1, 1. Boston,
MA; 2. Plantation, FL.
Introduction: Various auto-injectors differ in their form factor, mechanism
of drug delivery, and user instructions, which can affect the successful use of
the device through applied force capability and consistency of device orienta-
tion during drug delivery. We hypothesized that (1) a device’s form factor will
impact users’ capability of applying force as measured by the maximum applied
force and (2) a device’s form factor, mechanism, and instruction will impact
motor control performance metrics. Methodology: Trainer devices of 3 com-
mercially available epinephrine auto-injectors with 3 different form factors
(cylindrical, elliptical, and prismatic) were tested in a laboratory-based repeated
measures experiment with 20 adult (aged 18-30 years) participants. Partici-
pants performed 2 tasks using a power grip with each of the 3 injectors: a max-
imum force capability task in which they applied their maximum possible force
onto a force plate positioned over their thigh and an application task in which,
after watching the device’s training video, they practiced an injection using the
trainer. For the application task, device performance included time to hold force,
force, and device orientation and its variability during the hold segment. Par-
ticipants rated their force confidence and preference for the 3 devices. Results:
Greatest force capability was exhibited by the device with the elliptical form
factor followed by the prismatic and then the cylindrical, with the difference
between the elliptical and the cylindrical form factors being statistically sig-
nificant. For the application task, the elliptical form factor device had the fastest
time to force. The prismatic form factor device had the largest angle and vari-
ability in the angle of the resultant applied force. Participants reported the high-
est force confidence when using the elliptical and cylindrical form factor
Figure 1: Chest X-ray revealed right upper lobe atelectasis and pulmonary devices, ranking the elliptical as their preferred device. Conclusion: The results
edema. suggest that the elliptical form factor may have better success in drug delivery
in a larger set of the population.
5 Table 1
FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME OF
DIFFICULT MANAGEMENT.
A. Fiocchi*1, L. Dahdah2, O. Mazzina1, S. Corrente2, C. Riccardi1,
S. Salvatore3, 1. Rome, Holy See (Vatican City State); 2. Rome, Italy;
3. Varese, Italy.
Background: Food protein-induced enterocolitis syndrome (FPIES) usu-
ally presents in infancy. In the acute form, when food is ingested on an inter- Parameters measured for (I) maximum force capability task, (II) application
mittent basis or following a period of avoidance, FPIES typically presents task, and (III) self-reported survey. For significant main effects, Tukey’s post
with profuse vomiting, diarrhea, and dehydration, starting 1–3h following hoc groupings are ranked such that A > B. Values with the same superscript
specific food ingestion. FPIES diagnosis is based on history and typical symp- letters indicate no significant difference.
toms that improve with food avoidance, and with the exclusion of other eti-
ologies. Oral food challenge (OFC) remains the gold standard for diagnosis.
Case: A 6-month-old female infant was referred for FPIES of difficult man- 7
agement. The child was admitted to the hospital at 6 weeks of life for suspected INHALED CORTICOSTEROIDS AND INCIDENT PNEUMONIA
sepsis occurred 15 days after receiving milk thickened with rice cream; sepsis IN PATIENTS WITH ASTHMA:SYSTEMATIC REVIEW AND
evaluations were negative. At 5 months, soon after her first rice-containing META-ANALYSIS.
meal, she developped emesis, pallor, followed by diarrhea and lethargy, so she V. Bansal, M. Mangi*, E. Festic, Jacksonville, FL.
was hospitalized for suspected anaphylaxis. Negative allergy tests (SPT, Introduction: As asthma is a chronic inflammatory disease of the airway,
ImmunoCAP for rice, milk, egg, wheat) and the clinical history indicated the affected patients usually require long-term anti-inflammatory therapy. Inhaled
diagnosis of rice-induced FPIES. For the investigation of cereal tolerance she corticosteroids (ICS) are recommended as the first-line treatment for the per-
was challenged with commercial maize to which she reacted with vomiting, sistent disease; however, their routine use might raise certain safety concerns.
hypotonia and bloody diarrhea. Industrial maize food contamination with rice Although an increased risk of pneumonia have been established in patients with
was suspected. We requested a pure whole wheat flour from Heinz Baby Food, COPD on chronic ICS, it is not clear whether this risk pertains to asthma patients,
Italy®, which was tolerated at challenge. A special diet was initiated, in col- as well. Methods: We performed a comprehensive literature search from Jan-
A4 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A5
ABSTRACTS: CONCURRENT SESSIONS
uary 1, 1993, through March 31, 2014, using PubMed, Medline, CENTRAL, sent was obtained from all patients. Results: Among the 75 randomized patients,
EMBASE, Scopus, ISI, Regulatory Documents, Web of Science and manu- the median VAS score at baseline was 76mm. Forty-three patients were deter-
facturers’ web clinical trial registries (GlaxoSmithKline and AstraZeneca) with mined to have severe attacks (rhC1INH: 24; saline: 19). Among patients with
the clinical trial filters using multiple search terms with no language restric- severe attacks, the median (95% CI) time to onset of symptom relief in
tions. We included all studies that compared patients 14 years of age and older rhC1INH- and saline-treated patients respectively, was 90 min (47, 120) ver-
on ICS and not on ICS relative to the risk of incident pneumonia (community sus 334 min (105, not estimable); hazard ratio 2.52, log rank p-value 0.02. The
acquired, lower respiratory tract infection, non-tuberculous mycobacterial pneu- proportion of patients with severe attacks who received open-label rhC1INH
monia). We then summarized individual study estimates into two random-effect as rescue medication was 1/24 (4%) in the rhC1INH group and 10/19 (53%)
meta-analyses, one including randomized controlled trials (RCTs) and another in the saline group. After receiving rescue with rhC1INH, saline-treated patients
one including observational studies (OBS). Results: There were total of 12 stud- with severe attacks had a median time to relief of 60 min, as measured from
ies, 7 RCTs including total of 10,585 and 5 OBS including total of 44,127 par- the time of rescue administration. Conclusions: rhC1INH was effective in resolv-
ticipants. There was no heterogeneity in RCTs and summarized estimated effect ing severe HAE attacks. Patients randomized to saline who had worsening or
of ICS was protective of pneumonia; OR 0.75 (0.57-0.99. p=0.05). On the con- sustained angioedema symptoms had rapid improvement following rescue with
trary, OBS showed moderate heterogeneity (I2 =48%) with resulting summed rhC1INH.
OR of 1.94 (1.42-2.65, p<0.0001), suggesting increased risk of pneumonia with
use of ICS in asthma patients. However, OBS had lower grade of confidence
compared to RCTs. Conclusions: ICS may carry protective effect or at the very 9
least do not have increased risk of incident pneumonia in patients with asthma, THE PREDICTED TREE POLLEN BURST OF 2014 WAS A “BUST”
based on our meta-analysis of available RCTs. While observational studies sug- J.J. Anderson*, P. Pityn, London, ON, Canada.
gested higher risk of pneumonia in similar patients, the observed heterogene-
Introduction: The long harsh winter of 2013-14 prompted allergy experts
ity and inherent methodological limitations confered lower grade of confidence
to predict a “pollen vortex”. They reasoned that delayed antithesis would result
in these studies.
in the sudden release of greater than normal amounts of tree pollen. We eval-
uated the actual tree pollen data for London Ontario (Canada) to determine if
experts had predicted correctly. Methods: Daily samples of airborne pollen
were collected during the 2014 tree season with a Burkard spore trap located
3 stories above grade. The samples were analyzed and compared to our his-
torical 12 year data. The pollen counts were normalized against the 12 year
average count for each of the respective pollen types to assess the 2014 tree
season. The total tree pollen count and preponderance of 15 individual tree
pollen types were examined, along with the start and duration of their pollina-
tion. Results: Contrary to the experts’ predictions, the total seasonal pollen
count was not elevated, but was down considerably and several individual tree
pollen levels were far lower than at any other time in the previous 12 years.
Specifically, pollen levels of maple, juniper, birch, ash, mulberry and walnut
were considerably lower, as much as 4-5 times lower than the average. The other
tree pollen counts were within normal range. Conclusions: Not only did the
forecasted pollen burst fail to materialize this year, but the exact opposite hap-
pened. In 2014, the total tree pollen counts were at historic lows for London,
Ontario. Six major pollen producers of the fifteen tree types were at historic
lows despite otherwise typical duration and start of their respective seasons.
Experts need to refine their modelling skills to better predict pollen in the face
of global climate change.
Meta-analysis of RCTs and OBS for pneumonia (Risk estimates shown are
odds Ratio (OR) for RCTs and OBS.
8
EFFICACY OF RECOMBINANT HUMAN C1 INHIBITOR FOR
THE TREATMENT OF HEREDITARY ANGIOEDEMA PATIENTS
WITH SEVERE ATTACKS.
H. Li*1, A. Reshef2, H. Farkas3, J. Baker4, G. Porebski5, D. McNeil6,
A. Relan7, A. Zanichelli8, 1. Chevy Chase, MD; 2. Tel Hashomer, Israel;
3. Budapest, Hungary; 4. Lake Oswego, OR; 5. Krakow, Poland; 6. Colum-
bus, OH; 7. Leiden, Netherlands; 8. Milan, Italy. 10
Background: Hereditary angioedema (HAE) due to C1 inhibitor deficiency THE ALLERGENICITY OF THE CYANOBACTERIA SPECIE
is characterized by recurrent episodes of disabling and painful tissue swelling. MICROCYSTIS AERUGINOSA IS DEPENDENT ON ITS MICRO-
Although some attacks are self-limiting and may resolve spontaneously, many CYSTIN PRODUCTION.
attacks progress before taking several days to improve. We reviewed the effi-
cacy of recombinant human C1 inhibitor (rhC1INH) in the treatment of severe
E. Geh, D. Ghosh, J.A. Bernstein*, Cincinnati, OH.
HAE attacks in a randomized controlled study. Methods: Seventy-five HAE Background and Purpose: The cyanobacteria specie, Microcystis aerugi-
patients were randomized (3:2) to receive 50 IU/kg of rhC1INH or saline in a nosa (Ma), produces microcystin (MC) and an array of diverse metabolites
multi-center double-blind study. Severity of attack symptoms was assessed at believed responsible for their toxicity and/or immunogenicity. Previously,
baseline using a 100mm visual analog scale (VAS). Patients could be ran- chronic rhinitis patients were demonstrated to elicit a specific IgE response to
domized if the baseline VAS score was ≥50mm. Severe attacks were defined non-toxic strains of Ma by skin-prick testing (SPT) indicating that cyanobac-
as those with a baseline VAS score ≥75mm. The primary endpoint was time to teria allergenicity likely resides in the non-toxin producing component of the
onset of symptom relief, assessed as time from start of study drug infusion to organism. The objective of this study was to investigate the functional inter-
onset of sustained beneficial effect, defined by patient responses demonstrat- actions between cyanobacteria toxins and their co-expressed immunogenic pep-
ing improved symptoms on a Treatment Effects Questionnaire (TEQ). Rescue tides. Methods: Sera collected from chronic rhinitis patients previously found
treatment with open-label rhC1INH was permitted if there was no relief of to be sensitized by SPT to Ma were used to identify sensitizing proteins. Direct
symptoms by 4 hours or in case of life-threatening symptoms; these attacks and indirect IgE-specific ELISAs were used to confirm sensitization to Ma. A
were censored in the primary analysis. IRB approval and written informed con- 2-D gel electrophoresis followed by specific IgE immunoblot and mass spec-
troscopy (MS) was performed to identify the relevant allergenic peptides. Cyto-
VOLUME 113, NOVEMBER, 2014 A5
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A6
ABSTRACTS: CONCURRENT SESSIONS
toxicity and mediator release assays were performed using lysates from Ma
toxic (MC+) and non-toxic strain (MC-). Results: Using lysates from MC+ and
12
CLIMATE CHANGE INDUCED WARMING IMPACTS RAGWEED
MC- Ma strains and sera from Ma sensitized patients, specific IgE was increased
in response to the MC- but not the MC+ strain. In addition, MC- extracts induced POLLINATION IN UKRAINE.
b-hexosaminidase release using rat basophil leukemia cells. 2-D gel elec- V. Rodinkova1, A. Prikhodko2, A. Maleeva2, O. Palamarchuk1, I. Motruk1,
trophoresis followed by MS revealed the relevant sensitizing peptides were phy- L. Kremenska1, K. Musatova1, L.M. DuBuske*3, 1. Vinnitsa, Ukraine; 2.
cocyanin and the core-membrane linker peptide, both components of the Zaporizhzhia, Ukraine; 3. Gardner, MA.
cyanobacteria phycobilisome complex. Of note, the IgE specific response was Background: Ambrosia is increasing in abundance in south and east Ukraine
dose-dependently inhibited by addition of microcystin to the MC- lysate. Con- including Donetsk, Zaporizhzhia, Mykolaiv, Kherson, Kirovograd and Dne-
clusions: The allergenicity of Ma is inversely proportional to its microcystin propetrovsk regions Methods: Pollen collection was done by gravimetric sam-
content suggesting a direct or indirect interaction between microcystin toxin pling in Vinnitsa for years 1999 and 2000. From 2009 to 2013 volumetric meth-
and the allergenic peptides. Further investigation is warranted to understand ods employing a Burkard trap placed at a height of 25 meters above the ground
the interplay between immunogenicity and toxicity of cyanobacteria under on the roof of a Vinnitsa Medical University building were used. Pollen counts
diverse environmental conditions. in Zaporizhya from 2006 to 2013 and in Poltava, Donetsk, Dnepropetrovsk,
Odessa and Simferopol in 2010 used volumetric Burkard spore traps sampling
from the March 1 until October 1. Results: Greatest ragweed pollen counts were
11 in the third ten-day period of August and for the first or second ten-day period
COMPARISON OF OUTDOOR AND INDOOR FUNGAL SPORE of September, seen in Vinnitsa since 1999 and in Zaporizhya from 2006 until
COUNT IN KANSAS CITY. 2010 similar to all other cities in 2010. Ragweed pollen increase occurred in
D.A. Jara*, C.S. Barnes, J. Portnoy, M. Dhar, Kansas City, MO. the third ten-day period of August being maximal August 22 (Zaporizhya) until
Rationale: Fungus can be found outdoors and indoors and can enter the August 29 (Odessa) and August 25 in Vinnitsa for 2011 and 2012. The second
home through multiple mechanisms such as a window, on clothing, or open- period of increased Ambrosia pollen concentrations occurs after September 5
ings in the home. Patients have shown a higher risk of atopy with fungal expo- each year but has been shifting to a later time being September 2, 2010 in
sure. To determine if indoor mold count was elevated in relation to elevated Dnepropetrovsk and September 5 in Vinnitsa in 1999 and Zaporizhya in 2007
outdoor mold counts we conducted the following study. Methods: Data was later occurring September 18, 2012 in Vinnitsa. Greater ragweed counts are
retrieved from the Kansas City mold and spore database for a 15 year period now being seen later in Vinnitsa including 200 p.g./m3 on September 18 ver-
from March 1998 thru August 2013. The community wide outdoor spore count sus 100 August 25, 2012). In 2012 the seasonal peak was observed for the sec-
was performed with a with a Burkard device according to National Allergy ond ten-day period of September in much of Ukraine, something not seen before.
Bureau Protocols. The indoor spore count data was collected from an Aller- In 2010 and 2013 rapid increases of ragweed pollen were seen in the second
genco MK3 or a Buck Bioaire from about 150 homes with a mean of 4 col- ten-day period of August, two weeks earlier than usual being greater than the
lections taken from each home (Basement, Bedrooms, Living Room, Kitchen, mean seasonal maximum on August 27, 2010 (102 p.g./m3 versus 76 p.g./m3)
Bathroom, etc). Outdoor ground level data is the outdoor collection taken at in Vinnitsa with 2013 ragweed pollen count increased to 82 p.g./m3 on August
each home at the time the indoor collections were taken. Data included here 11 peaking at 92 p.g./m3 on August 27. Seasonal maximum in Zaporizhya was
for comparative purposes is for 8 spore types that are easily identifiable indi- on August 19, 2013. Conclusion: The changing pattern of ragweed pollination
vidual genera. Data is reported by percent of collections in which each genera in Ukraine with early ragweed pollen count increases for the second ten-day
was observed. Spore counts were stored in an Access database and analyzed period of August and changes in maximum in September may be evidence of
using Excel. Results: Total spore percentages are seen in table 1. Cladospo- the primary impact of temperature increase on Ambrosia season in Ukraine due
rium was the most common spore collected indoors and outdoors. When com- to global warming.
paring indoor counts, Cladosporium was most commonly seen in basement at
52% followed by child’s bedroom 20%. Alterneria was most commonly seen
in the child’s bedroom at 30% followed by bathroom 19% and master bed- 13
room 15%. Overall spores were most commonly seen in child’s bedroom 16%, THE EVALUATION OF SERUM TRYPTASE LEVELS AFTER SUB-
basement 13% and kitchen 10%. Alternaria was least commonly seen in fam- CUTANEOUS IMMUNOTHERAPY-ASSOCIATED SYSTEMIC
ily room 4% basement 9% and living room 9%. Cladosporium was least com- REACTIONS.
monly seen in family room 2%, master bedroom 3% and living room 6%. Over- P.H. Wong*1, H.C. Crisp2, T.S. Rans3, 1. San Antonio, TX; 2. Andrews AFB,
all spores were least commonly seen in family room 1%, master bedroom 2% MD; 3. Lackland AFB, TX.
and living room 6%. Conclusion: Increased outdoor spore count is associated Background: Elevations in serum tryptase are used to support the diagno-
with higher indoor spore counts but origin could not be inferred from this study. sis of anaphylaxis. Although tryptase has been studied in anaphylaxis to insect
Cladosporium was the most identified fungi both indoors and outdoors in this stings and drugs, it has not been measured systematically in patients who have
study. Interestingly the child’s bedroom seems to be the most susceptible to systemic reactions (SRs) to immunotherapy (IT). Methods: This study was an
indoor mold amplification, while the living room and family room had the low- IRB-approved, prospective cohort study of aeroallergen or venom IT patients
est spore count. This may be secondary to the aesthetic desire most families who experienced SRs during the 30-minute post-IT period and were treated as
put into maintaining a home while negating lesser used rooms. clinically indicated. Consent and serum total tryptase were obtained after a one-
hour observation period when the patient was ready for discharge. A baseline
Table 1 tryptase was drawn 2-7 days post SR. Tryptase levels were determined using
commercially available ELISA kits. Results: Twelve patients had 13 reactions
over a 20-month study period. Patient and SR specifics are shown (Table 1).
All reactions were grade 1 or 2 in severity. Flushing was the most common,
objective symptom. One or 2 doses of epinephrine were administered for all
SRs. All SRs were non-life-threatening and occurred during the build-up phase
of immunotherapy. Median time from SR onset to resolution and from SR onset
to tryptase lab draw was 26 and 85 minutes, respectively. No elevation in tryptase
post-SR or change from reaction to baseline tryptase (>2 ng/ml) was observed.
Discussion: Tryptase is a marker of mast cell degranulation with clinical util-
ity, but it is not consistently elevated in all cases of anaphylaxis. In this study,
Percentage of Total spore counts seen. SRs after IT were of short duration and mild severity. Unlike field anaphylaxis
due to insect stings, post-IT SRs were promptly recognized and treated. The
low total serum tryptase levels may reflect post-epinephrine effects of a ter-
minated systemic reaction. Additionally, IT-associated SRs may represent a
unique or undefined phenomenon involving complement, anaphylatoxins,
kinins, or lipid mediators. Basophils rather than mast cells may be activated in
the early stages of IT-associated SRs. These data suggest that tryptase is of lim-
A6 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A7
ABSTRACTS: CONCURRENT SESSIONS
ited utility in identifying patients with higher risk of IT-associated SRs or assist-
ing in the diagnosis of grade 1 or 2 SRs. Conclusion: No elevation or change
15
OCCURRENCE AND DURATION OF LOCAL ALLERGIC REAC-
in total tryptase was observed in the first prospective cohort study of IT-asso-
ciated SRs. Tryptase appears to be of little clinical utility in evaluating mild TIONS IS SIMILAR FOR RAGWEED, GRASS, AND HOUSE DUST
SRs to IT, however larger studies are needed. MITE SUBLINGUAL IMMUNOTHERAPY TABLETS AND CON-
SISTENT WITH AN IMMEDIATE IGE-MEDIATED REACTION.
Patient and Systemic Reaction Characteristics with associated Tryptase and H.S. Nelson*1, J. Maloney2, M.A. Calderon3, J.A. Bardelas4, A. Kaur2,
Histamine Levels H. Nolte2, 1. Denver, CO; 2. Whitehouse Station, NJ; 3. London, United
Kingdom; 4. High Point, NC.
Introduction: The most common adverse events (AEs) with sublingual
immunotherapy tablets (SLIT-T) are local allergic reactions of the mouth and
throat. These AEs are expected as the allergen extract presumably elicits an
IgE-associated mediator release from mast cells located in oral tissues. Our
objective was to report the duration of local allergic reactions in response to
SLIT-T for 3 different allergens to characterize the reaction patterns. Meth-
ods: Symptoms and duration in minutes of local allergic reactions after SLIT-
T administration were collected during phase 1 studies of Timothy grass SLIT-
T 2800 BAU (MK-7243) and short ragweed SLIT-T 12 Amb a 1-U (MK-3641),
and during phase 1 and 2b studies for house dust mite (HDM) SLIT-T 12 DU
(MK-8237; all Merck/ALK-Abelló). Additionally, the duration in days (num-
ber of days that an event recurs) was collected for local allergic reactions dur-
ing the phase 3 trials for each of these tablets. IRB approval and informed con-
sent was obtained from all subjects. Results: The median durations in minutes
a. Severity based on WAO Subcutaneous Immunotherapy reaction grading
for the most common local adverse reactions after SLIT-T or placebo admin-
system scores Grade 1-5.
istration are shown in the Table. For each of the events, reactions typically
b. Same patient who experienced a post-IT SR on two separate dates.
resolve within minutes. Events generally recur over several days prior to reso-
Symptoms codes: F=flushing; C=conjunctivitis; G=globus sensation; D=dys-
lution of the events. The median recurrence of symptoms after active treat-
pnea; A=angioedema; P=pruritis; CT=chest tightness; W=wheezing;
ment varies in duration, ear pruritus (4 to 14 days); oral pruritus (5 to 8 days);
UC=uterine cramping; U=urticaria
throat irritation (5 to 9 days). Conclusions: The occurrence and duration of local
NA = Not available data in patient 3.
adverse reactions related to SLIT-T were similar across studies, and appear to
be a class effect consistent with an IgE-mediated response. Although cautious
interpretation is required due to the limited sample size, the data reveals that
14 the reactions generally resolve within minutes of SLIT-T administration and
EFFICACY, IMMUNOLOGIC RESPONSE, AND SAFETY OF RAP-
are experienced for less than 2 weeks.
IDLY-DISSOLVING SUBLINGUAL IMMUNOTHERAPY TABLETS
IN SUBJECTS OVER 50 YEARS OF AGE WITH ALLERGIC Median Duration of Most Common Local Allergic Reactions in Response to
RHINITIS. SLIT-T
P. Creticos*1, D.I. Bernstein2, R. Weber3, N.J. Amar4, Z. Li5, A. Kaur5,
J. Maloney5, H. Nolte5, 1. Baltimore, MD; 2. Cincinnati, OH; 3. Denver,
CO; 4. Waco, TX; 5. Whitehouse Station, NJ.
Introduction: Use of allergen immunotherapy in older adults with allergic
rhinitis (AR) has been questioned because of age-related dampening of immuno-
logic responses. Efficacy, immunologic response, and safety in subjects ≥50
years and/or 18 to <50 years receiving rapidly-dissolving sublingual
immunotherapy tablets (SLIT-T) approved for treatment of Timothy grass- (and
related grasses) or short ragweed-induced AR was analyzed. Methods: Data
pools were constructed from phase 2/3 trials (24-wk to 1-yr duration) of grass
SLIT-T 2800 BAU (MK-7243; Merck/ALK-Abelló; 4 phase 3 trials for effi-
cacy, 6 phase 2/3 trials for safety) or ragweed SLIT-T 12 Amb a 1-U (MK-3641;
Merck/ALK-Abelló; two 28-day safety trials and two 52-wk trials). Efficacy
was assessed by total combined symptom and medication scores (TCS). The
ragweed SLIT-T efficacy trials excluded subjects ≥50 years, thus no efficacy *Sum of daily durations throughout entire 28-day trial.
or immunologic data are available for this subgroup. Results: TCS improved †Duration on day 1 of treatment.
by 20% with grass SLIT-T vs placebo (mean difference: −1.36, 95% CI −1.74, AE=adverse event; ND=not determined; SLIT-T=sublingual immunotherapy
−0.97) in subjects <50 years (n=1988), and 15% vs placebo (mean difference: tablet.
−0.86, 95% CI −1.84, 0.13) in subjects ≥50 years (n=311). TCS improved by
23% with ragweed SLIT-T vs placebo (mean difference: −2.02, 95% CI −2.87,
−1.17) in subjects <50 years (n=311). Consistent increases in IgG4 from base- 16
line were observed in both age groups for grass SLIT-T; a similar increase was JTF PRACTICE PARAMETER-COMPLIANT SUBCUTANEOUS
observed with ragweed SLIT-T in subjects <50 years. The overall treatment- IMMUNOTHERAPY FOR ALLERGIC RHINITIS DUE TO MOUN-
emergent adverse event (TEAE) rate with grass SLIT-T was 83.4% in subjects TAIN CEDAR INDUCES SKIN TEST ANERGY AND LONG-TERM
<50 years (n=1468) and 78.6% in subjects ≥50 years (n=201). The overall TEAE CLINICAL REMISSIONS.
rate with ragweed SLIT-T was 56.7% in subjects <50 years (n=841) and 55.6%
in subjects ≥50 years (n=216). The most common treatment-related AEs were M.P. Vaughn*, San Antonio, TX.
local application site reactions for both tablets, regardless of age. Conclu- Rationale:The 2010 Joint Task Force (JTF) Practice Parameters on Aller-
sions: Efficacy and immunologic data for grass SLIT-T reveal similar response gen Immunotherapy (www.AAAAI.org) recommends subcutaneous
patterns in subjects <50 and ≥50 years. Although not studied, it may be inferred immunotherapy (IT) for allergic rhinitis (AR) with aeroallergen extracts given
that ragweed SLIT-T would result in similar efficacy and immunologic changes at “probable effective doses” (Table IX.) beginning weekly, from a 1000-fold
in ragweed allergic patients ≥50 years. No new safety concerns were revealed dilution of the maintenance vial (1:1), and incrementally progressing to a goal
in subjects ≥50 years for either tablet. These data suggest that patients ≥50 years of 0.5cc of the (1:1) concentrate (Appendix 1). Per the JTF guidelines for “con-
with AR may benefit from grass and ragweed SLIT-T. ventional” IT, “the intervals between the maintenance injections generally range
from every 2-4 weeks”. We have previously reported that 3 years of “conven-
tional” IT is typically sufficient to induce the loss of skin test reactivity to
aeroallergens however; this result appears to be highly dose-dependent. A ret-
VOLUME 113, NOVEMBER, 2014 A7
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A8
ABSTRACTS: CONCURRENT SESSIONS
rospective survey was used to evaluate the association between the loss of skin
test reactivity during IT and long-term clinical efficacy. Methods: Patients (Age
18
LOCAL REACTIONS DURING IMMUNOTHERAPY AND THEIR
18-65) were mailed a follow-up survey if they had stopped IT prior to 2010 and
met the following criteria: Skin test (+) to mountain cedar (MC) with ≥ mod- IMPACT ON DOSE ADJUSTMENT.
erate AR during MC pollinations. Achieved 1:1 vial dosing for > 12 months Q. Kamili*, A.C. Gavino, R. Rossen, F. Orson, A. Casillas, Houston, TX.
and had repeated skin testing prior to IT discontinuation. Results: Of 200 sur- Introduction: Local reactions are commonly noted during allergen
veyed, 28 of 40 respondents met inclusion criteria. Among the 14 patients reach- immunotherapy (IT) administration. These are usually mild and self-limiting;
ing the monthly goal of 0.5cc (mode volume), 100% reported “significant with more than 80% of reactions smaller than the size of a palm (8-10 cm).
improvement” of AR while receiving IT and a fall in skin test grading by ≥ 2 Studies have shown that local reactions may not be predictive of subsequent
grades was seen in 93%. A sustained complete remission (CR) of symptoms systemic reactions. A common practice to empirically enhance safety is to repeat
was reported by 43% while off IT for 5 to 10.1 years (median 6.9 yrs). In con- or reduce the IT dose based on the size of the post-administration wheal. Con-
trast, among those who had received a lower maintenance dose (Mean = 0.22 servative management of local reactions less than 25 mm in size may lead to
± 0.17cc.), a fall in skin test reactivity was seen in only 42% and CR was reported inadequate therapy. We report the incidence of local and systemic reactions
in only 21% (n=14). No differences between groups were observed for: initial with IT administration and the time taken to reach maintenance therapy at our
symptom severity or skin test grading, subjective treatment efficacy (while on institution which follows a conservative management of local reactions less
IT), or the IT duration. Conclusion: “Real-world” JTF-compliant IT is highly than 25 mm in size. Methods: We reviewed data on patients receiving aeroal-
effective, both during and after treatment courses. Aeroallergen IT, formulated lergen immunotherapy at an academic medical center where dosing practices
and administered per JTF-recommendations, can induce allergen-specific skin are based on a protocol that is altered according to local wheal size after IT
test anergy in a dose-dependant manner. The induction of a persistent remis- administration. Patients on immunotherapy for 23 weeks or more were included.
sion was significantly more common among those in whom the loss of skin Post injection reactions were graded from 1-5, and dose adjustments were made
test reactivity was observed. accordingly (see table). Other factors which led to dosage changes were a change
to a new vial and time delays over two weeks since last dose. Results: Fifty-six
patients received 6633 IT injections over 0.5- 7 years (mean of 2.1years ±1.2
17 years). Local reactions were observed in 89% of patients with an incidence rate
POPULAR ON YOUTUBE: A CRITICAL APPRAISAL OF THE of 13% (grade 2 = 37%, grade 3=15% & grade 4=48%). Half of the reactions
EDUCATIONAL QUALITY OF INFORMATION REGARDING (52%) were less than 25 mm. Thirty-eight percent of the reactions occurred
ASTHMA. during build up phase delaying the initiation of maintenance therapy. The mean
A. Gonzalez-Estrada*, L. Cuervo Pardo, B. Ghosh, F. Pazheri, M. Smith, time taken to reach maintenance (1:1 concentration) was 7.6 ± 3.4 months with
K. Zell, X. Wang, D.M. Lang, Cleveland, OH. 61% of all patients reaching this level over 5-22 months. Only 4 patients (7%)
reached the final therapeutic IT dose. Conclusions: We note that more than half
Background: Asthma affects over 300 million people globally, including of the reactions were smaller than 25 mm in size. Most (93%) patients did not
25 million in the US. Patients with asthma frequently use the internet as a source achieve the prescribed maintenance IT dosage over the time period studied. It
of information (Cabana MD, Le TT. J Allergy Clin Immunol. 2005). YouTube, may be possible to increase efficacy of IT by changing the dose adjustment cri-
a video sharing website, is one of the three most popular websites teria for reactions that are smaller than 25 mm in size.
(http://www.alexa.com/topsites). We sought to determine the educational qual-
ity of asthma YouTube videos. Methods: We performed a YouTube search using Protocol for Dose Adjustment During Immunotherapy Administration
the keyword “asthma” from June 4-8, 2014. The 200 most viewed relevant
videos were included in the study. Asthma videos were analyzed for charac-
teristics, source and content. Source was further classified as asthma health-
care provider, other health-care provider, patient, pharmaceutical company, and
professional society/media. A scoring system was created to evaluate quality
(-10 to +30 points). Negative points were assigned for misleading informa-
tion. Five blinded reviewers scored each video independently; a mean score
was calculated by video source. Two-tailed analysis was performed for video
characteristics, ANOVAs were performed to compare scores by video type, and
intraclass correlation was used to assess similarity in scoring by reviewers. 19
Results: Two hundred videos were analyzed, with a median of 18,073.5 views, THE HEDIS MEDICATION MANAGEMENT FOR PEOPLE WITH
31.5 likes, 2 dislikes, and lasted a median of 172 seconds. More video presen- ASTHMA MEASURE DOES NOT CORRELATE WITH
ters were male (60.5%). The most common type of video source was other IMPROVED ASTHMA OUTCOMES.
health-care providers (34.5%). The most common video content was alterna- A. Crans Yoon*1, W. Crawford1, J. Sheikh1, A. Gong1, R. Nakahiro2,
tive treatments (38.0%), including live-fish ingestion, reflexology, acupres- M. Schatz2, 1. Los Angeles, CA; 2. San Diego, CA.
sure/acupuncture, ayurveda, yoga, raw food/vegan/gluten free diets, marijuana, Introduction: A new Healthcare Effectiveness Data and Information Set
Buteyko breathing, salt therapy, etc. Scores for videos supplied by asthma health- (HEDIS) asthma measure has been implemented, however it is unknown if
care providers were statistically significantly different from all other sources meeting this care measure is associated with improved asthma outcomes. We
(p < 0.001) and had the highest average score (9.91). Table 1 summarizes all examined if the HEDIS Medication Management for people with Asthma meas-
scores by video source. Overall, there was a high degree of agreement among ure (“MMA measure”) associates with asthma outcomes. Methods: Adminis-
reviewers (rho = 0.847; p < 0.001). Conclusion: We found that YouTube videos trative data was used to identify 30,040 patients who met the HEDIS criteria
on asthma are frequently viewed, but are a poor source of health care infor- for persistent asthma during 2012. They were classified as meeting or not meet-
mation. Videos by asthma health-care providers were rated highest in quality. ing the MMA measure at the 75% and 50% adherence thresholds. Association
The Allergy/Immunology community has a clear opportunity to enhance the between MMA adherence in 2012 and asthma outcomes in 2013 was assessed.
value of educational materials via YouTube. Patients who were not MMA adherent but met the HEDIS asthma medication
ratio measure were compared to those adherent to the MMA measure. Results:
Table 1. Scores by video source Patients who met the 75% or 50% MMA measure in 2012 had no difference
in asthma related hospitalizations, ED visits, short-acting beta agonist (SABA)
dispensing, and oral steroid dispensing events in 2013 compared to those who
did not meet the measure. Stepwise comparison of patients who were 75% com-
pliant, 50-75% compliant and < 50% compliant also showed no difference in
these outcomes. To address confounding by patients who met the measure due
to having a later index date, patients who met the 75% MMA measure with
index dates late in the year were compared to those who did not meet the 75%
measure whose index dates were early in the year and no difference was found
in their 2013 asthma outcomes. Additionally, patients who met the 75% and
50% MMA measures were compared to those who did not but had an asthma
medication ratio of >0.5. Asthma outcomes of hospitalization, ED visits and
greater than 6 SABA canisters dispensed were higher in the 75% adherent group
A8 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A9
ABSTRACTS: CONCURRENT SESSIONS
compared to the non-adherent but ratio >0.5 group. No difference in hospital- more controlled than what the child reports. In children ages 4-11 years, 39%
izations or ED visits was found between the groups at the 50% adherence thresh- with uncontrolled asthma received an appropriate increase in medications, while
old; however the 50% adherent group had more patients who required greater 76% with controlled asthma were maintained on their medication or decreased.
than 6 SABA canisters. Conclusions: The HEDIS MMA measure does not cor- In children > 12 years of age, 36% with uncontrolled asthma received an increase
relate with asthma-related hospitalizations, ED visits, SABA dispensing, or in medications, while 81% with controlled asthma were maintained on their
oral steroid dispensing. Alternate measurements of asthma outcomes, such as medication or decreased. Conclusion: Although results suggest a discrepancy
the asthma medication ratio and its correlate, the number of SABA canisters between ACT scores for uncontrolled asthma and subsequent step-up in asthma
dispensed, may better identify patients at risk for adverse asthma outcomes. management, there are other objective factors which play a role in determin-
ing asthma management, such as the pulmonary function test and physical
exam. Analysis of these measures along with the ACT should be considered
20 for asthma management. A communication gap about asthma symptom sever-
ALLERGY IMMUNOTHERAPY ADHERENCE: DOES RUSH ity might exist between caregiver and child, which may be mitigated through
MAKE A DIFFERENCE? patient education.
S.P. Raschal, J.M. Holcombe, B.G. Carlton*, Chattanooga, TN.
Traditionally, immunotherapy consisted of regular (weekly/bi-weekly) injec-
tions over several months until a maintenance stage was reached. Rush
22
UTILITY OF HIGH ATTENUATING MUCUS AND OTHER RADI-
immunotherapy (RIT) allows the patient to achieve a maintenance stage much
OLOGIC FEATURES IN DIAGNOSED CASES OF ALLERGIC
quicker than traditional immunotherapy. The purpose of the current study was
to identify whether patients were more or less adherent to treatment when they BRONCHOPULMONARY ASPERGILLOSIS.
received RIT. A systematic chart review was conducted on all new patients who P. Agarwal*, A. Chowdhary, S. Gaur, Delhi, India.
started immunotherapy in 2011. Variables of interest included demographic Background: High attenuating mucus (HAM) impaction and other radio-
factors (age, gender, etc.), potential control variables (systemic reactions, prick logic features (ORF) have been considered as important radiologic parameters
test results, and asthma diagnosis), RIT (hours), and duration of treatment while diagnosing and classifying patients of Allergic bronchopulmonary
(months). Overall, 199 patients began allergy immunotherapy at the clinic in aspergillosis (ABPA). However, the exact significance of these radiologic find-
2011. The average patient was 33 years old, female (65.3%), and Caucasian ings is controversial. Method: A total of 63 patients diagnosed as ABPA based
(81.9%). The majority of patients had systemic reactions during their initial on the Rosenberg-Patterson criteria were categorized on the basis of HRCT
screening (92.4%) and was also prick test positive (96.0%). The patients were findings into 4 groups; ABPA-S (Serological), ABPA-CB (Central bronchiec-
almost evenly divided by asthma diagnosis (yes=59.1%; no=40.9%), but analy- tasis), ABPA-CB-HAM and ABPA-CB-ORF. These groups were studied for
ses showed no significant differences between these two groups in regards to their baseline characteristics at initial visit and their clinical, serological and
RIT hours and treatment duration. Patients were classified into one of three functional severity were assessed on follow up visits and ABPA exacerbations.
groups at the time of chart review – (1) still on treatment, (2) stopped treatment IEC approval and informed consent was obtained from all research subjects.
without restart, and (3) stopped treatment with restart(s). Of the 199 patients Results: The prevalence of HAM and ORF was found to be 9.5% and 41.3%
who started treatment in 2011, 97 (48.7%) were still receiving treatment with respectively. A statistically significant higher correlation was observed for
an average therapy duration of 14 months. Eighty patients (42.2%) had stopped expectoration of brownish black mucus plugs (P < 0.03), anorexia (P<0.05),
treatment and had not restarted while 18 patients (9.0%) had stopped treatment weight loss (P<0.008), mean number of ward admission per year (P<0.015),
and subsequently restarted, some on several occasions. The average number of mean number of ABPA exacerbations per year (P<0.001), mean total IgE lev-
RIT hours for patients still on treatment (M=13.37) was significantly higher els (P<0.001) in patients with HAM on the initial visit. Also, significantly more
than for patients who had stopped treatment (M=8.20) even if they restarted number of ORF patients had history of anti tubercular treatment for sputum
(M=2.64) [F(2, 196) = 15.57, p = .000]. Further analyses were conducted clas- positive tuberculosis (P<0.01). Furthermore, severe and very severe grades of
sifying patients into groups dependent upon the number of RIT hours they obstruction on spirometry were observed in ORF group. The prospective analy-
received, if any. Patients receiving 1-10 RIT hours had significantly lower treat- sis revealed mean serum total IgE levels (P<0.03) to be significantly high in
ment duration (M=8.3) than patients receiving no RIT (M=14.4), 11-20 RIT HAM group, whereas, mean specific IgE levels against Aspergillus fumigatus
hours (17.2), or more than 20 RIT hours (18.77) [F(3,195) = 14.17, p = .000]. were found to be significantly higher (P<0.007) in patients with central
While RIT hours do play a role in treatment duration, results of these analyses bronchiectasis . The follow up HRCT done during exacerbations detected pres-
suggest that another variable, possibly related to commitment to treatment, may ence of HAM in 3 patients of ABPA-CB, 1 of ABPA-CB-ORF and 4 of ABPA-
also be involved in the prediction of adherence. CB-HAM. A high serum total IgE and specific IgE values were found in HAM
impaction but were not statistically significant. Finally, comparisons made in
the exacerbation group between HAM positive and HAM negative patients
21 were also statistically insignificant. Conclusion: HAM and ORF appear to be
ASSESSING SUBJECTIVE MEASURES OF ASTHMA CONTROL associate findings in ABPA patients which may or may not influence the sever-
IN AN INNER CITY PEDIATRIC AND ADOLESCENT POPULA- ity of the disease. Also, these findings could not be used as a diagnostic tool
TION. independently and do not predict the outcome. .
P.J. Patel*1, N. Abou Baker2, R. Travis2, A. Tentler2, E. Montalvo Stanton2,
Comparison of ABPA exacerbation data among study groups,
1. North Brunswick, NJ; 2. Newark, NJ.
Introduction: In clinical practice where time and resources are limited, the
asthma control test (ACT) and the childhood asthma control test (C-ACT) were
developed by Nathan et al and Liu et al, respectively, to identify poorly con-
trolled asthma. The ACT contains questions for the patient >12 yrs of age and
the C-ACT contains questions for the caregiver and child 4-11 years of age.
The goal of this study was to evaluate whether patients are on optimal asthma
treatment based on subjective reporting of asthma control from the child and
the parent as assessed by the ACT/C-ACT. Methods: A random selection of
office visits made by children, ages 4-20 years, with asthma during 2013 was
surveyed. We reviewed 171 charts: 114 children 4-11 years completed the C-
ACT with their caregivers; 57 children 12-20 years completed the ACT. For
children ages 4-11 years old, a comparison was made between the responses
of children and their caregivers on their measure of asthma control. All sur- * = Statistically significant data
veyed charts were examined for step-up in medications if they had uncontrolled
asthma (ACT/C-ACT score < 20) or appropriate maintenance or decrease in
medications if controlled. Results: In children ages 4-11 years, it was noted
that while caregivers’ ACT scores had a moderate correlation (R2 = 0.52) with
their child’s score, the caregiver’s score was, on average, 7% higher than the
child’s score, suggesting that caregivers may perceive their child’s asthma as
VOLUME 113, NOVEMBER, 2014 A9
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A10
ABSTRACTS: CONCURRENT SESSIONS
nosis of persistent asthma who were started on inhaled corticosteroids were
23 prospectively enrolled with informed consent. Each subject completed the
ASTHMA ALLY: TAKING ADVANTAGE OF THE CLOUD TO
PAAT. The PAAT was scored such that a higher score suggested better adher-
UNDERSTAND ENVIRONMENTAL TRIGGERS OF ASTHMA ence. Refill history was assessed through phone calls to the subject’s pharmacy
AND ALLERGIES. at 1 week, 3 months, and 6 months after initial visit. Adherence was defined
R. Lucas*1, J. Dees2, R. Reynolds2, B. Rhodes3, N. Allen3, R.W. Hender- as 4 or more medication refills at 6 months. IRB approval and informed con-
shot4, 1. Phoenix, AZ; 2. Salt Lake City, UT; 3. Provo, UT; 4. North Salt sent was obtained from all research subjects. Results: At 6 months, only 10/74
Lake, UT. subjects (13.5%) of patients filled 4 or more controller inhalers. The median
Asthma and allergies represent a substantial cost to society. Cloud com- number of refills for controller medication at 6 months was higher for subjects
puting and mobile-based client technologies have the potential to improve dis- who answered “agree or strongly agree” compared to “neutral” to the question
ease control as well as expand the scientific and medical community’s insight regarding if their controller was necessary (median 3 vs. 2, p=0.028). There
into these diseases. We report the results of a case series study in which we was no difference in total PAAT score between the adherent and non-adherent
employed a cloud computing and mobile phone-based platform, Asthma Ally, group (20 vs 18.5, p=0.406). Additionally, there were no clinically significant
in order to track patients’ asthma and allergy symptoms and automatically com- differences in refill history for subjects for all other questions. Conclusions:
pile temporally and spatially appropriate environmental data that are useful We have demonstrated that the vast majority of patients receiving a new con-
for understanding individual triggers exacerbating their asthma and allergy troller medication for their asthma are non-adherent. The PAAT was able to
events. Participating patients used a cell phone application to interface with identify that adherence is better in patients who believe that their controller was
Asthma Ally and log symptom information regarding their individual asthma necessary for their asthma. Asking this question during a pediatric visit may
and allergy episodes and composite measures of asthma control based on a indicate a patient at higher risk for non-adherence, and may improve patient
questionnaire instrument. Approximately two years of anonymous patient data outcome through early intervention focusing on essential role of medication
were used for this study in addition to research subjects granting informed con- education. Unfortunately, total PAAT score failed to identify adherent versus
sent. For every participating individual, environmental data (e.g. air quality, non-adherent patients in our asthma patient population. Further investigation
ambient pollen counts, climate data, etc.) were regressed against individual is necessary to determine the validity of the tool to predict a child’s adherence
asthma or allergy symptoms. Where pollen data were available, grass pollen to a controller medication.
counts were consistently the strongest covariate in individual regression mod-
els, contributing as much as 41.7 – 76.1% of the explained variation for all
asthma and allergy events. The covariates particulate matter size 2.5 mm (PM2.5) 25
and wind speed also commonly had high relative importance values in indi- ASSOCIATION BETWEEN MOUSE AND COCKROACH SKIN
vidual regression models, contributing as much as 7.3 – 33.2% of the explained PRICK TEST, SERUM SPECIFIC IGE, ENVIRONMENTAL EXPO-
variation. The strength of the coefficient of determination varied by individ- SURE AND ASTHMA MORBIDITY IN ATOPIC CHILDREN <4
ual, ranging from 0.053 – 0.730. During well controlled periods, asthma events YEARS OF AGE IN THE BRONX, NEW YORK.
tended to not be significantly related to environmental variables. During uncon- A.L. Richler*1, Y. Jorge2, Y. Pichardo2, P. Polanco3, K. Achar2, R. Nazari4,
trolled periods, however, asthma events tended to be more strongly related to G. de Vos2, 1. Brooklyn, NY; 2. Bronx, NY; 3. San Juan, Puerto Rico;
environmental variables, the strength of the relationships increasing with increas- 4. Philadelphia, PA.
ing lack of asthma control. Asthma Ally can improve asthma and allergy out-
comes because both healthcare providers and patients are better able to under- Background: Epidemiologic studies have found inconsistent associations
stand specific environmental factors triggering asthma and allergy events at between cockroach and mice exposure, allergic sensitization and asthma mor-
an individual level and each can make treatment or behavior changes to improve bidity. Such studies used either skin prick testing (SPT) or serum specific IgE
control and quality of life. testing (ssIgE) to determine allergic sensitization, possibly contributing to the
inconsistency of the results. Objective: To determine the association between
environmental roach and mice exposure, SPT and ssIgE results and asthma
morbidity in a population of atopic, asthmatic inner-city children < 4 years of
age residing in the Bronx, New York. Methods: Forty-nine (49) atopic asth-
matic children between 18 – 48 months of age were enrolled. An extensive
health interview was conducted with the parents, including questions about the
visual presence of mice and roaches at their home. Children underwent SPT
(ComforTen®) and ssIgE testing (Immulite 2000) with a cut-off ssIgE level of
≥ 0.35 kU/l considered as positive. IRB approval and informed consent was
obtained from all research subjects. Results: Reported mice infestation at home
was associated with a positive SPT to mouse (OR=5.0, 95% CI 1.6-54.3,
p=0.01), but not with mouse ssIgE (OR=3.1, 95% CI 0.7-13.8, p=0.12). In addi-
tion, children sensitized to mouse based on either testing method appeared to
be more likely to have at least 1 asthma related ED visit in the past 12 months
Example of longitudinal environmental exposures and asthma event data for compared to children not sensitized to mouse (OR= 3.5, 95% Cl, 0.9.-13.9,
an individual. Environmental data compiled by automated algorithms of p=.075). In contrast, we did not find an association between reported roach
Asthma Ally. Rose shaded area highlights uncontrolled asthma events. Trends infestation at home and roach sensitization based on SPT (OR=1.5, Cl 0.4-5.7,
are indicated using loess regression with a weighting factor of 0.1. p=0.59) or ssIgE (OR=1.7, Cl 0.5-6.3, p=0.43). Roach sensitization based on
either testing method did not predict asthma related ED visits in the past 12
months, regardless if roach infestation was reported or not. Conclusion: Our
pilot study suggests that mice infestation is a strong predictor of mouse spe-
24 cific sensitization and asthma morbidity in young inner-city children, stronger
than roach infestation and roach sensitization. SPT appears to correlate stronger
THE PEDIATRIC ASTHMA ADHERENCE TEST (PAAT): A SUR-
with mouse exposure than ssIgE testing
VEY FOR PEDIATRIC PATIENT PROPENSITY TO ADHERE TO
CONTROLLER MEDICATIONS.
B.T. Kelly*1, W. An1, C. Bauer2, H. Zafra1, L. Gimenez1, L. Crandall1,
P. Simpson1, M. Nugent1, P. Vargas2, K.J. Kelly3, 1. Milwaukee, WI; 2.
Phoenix, AZ; 3. Chapel Hill, NC.
Introduction: Medication non-adherence leads to increased pediatric emer-
gency visits and hospitalizations. Tools to predict adherence in adults with
asthma have been successfully validated. No tool currently exists in pediatrics
that reliably predicts adherence to use of controller asthma medications. We
developed a PAAT to quantitatively predict adherence in children with per-
sistent asthma. Methods: Patients between ages of 2 and 18 with a new diag-
A10 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A11
ABSTRACTS: CONCURRENT SESSIONS
27
MACROPHAGE PHENOTYPE SHIFT TOWARD M1 AFTER
IGG STIMULATION WITH OMALIZUMAB IN AN IGE FREE
SYSTEM.
R. Steele*, M. Littlefield, I. Voloshyna, M. Davis-Lorton, M. Aquino,
L. Fonacier, A. Reiss, Mineola, NY.
Introduction: Classically activated M1 macrophages drive Th1 responses,
while alternatively activated M2 macrophages drive Th2 responses. A shift away
from Th2 toward Th1 is associated with decreased incidence of atopy. Anti-IgE
monoclonal antibody (mAb) therapy (omalizumab; a humanized IgG1 mAb)
is an FDA approved treatment for allergic asthma and chronic urticaria. In recent
studies, patients with non-allergic asthma and those with low serum IgE showed
improvement in clinical measures with omalizumab treatment independent of
IgE level. This may represent an unrecognized immunomodulatory effect of
Graph, Results of exposure, allergen sensitivity and morbidity. (+) ssIgE was omalizumab. IgE-independent effects of this mAb in antigen presenting cells
determined as ≥ .35 kU/L.” were examined in polarization of the THP-1 human monocytic cell line in an
Group 1 is made up of children with reported exposure to roach and positive IgE free system. Methods: THP1 were differentiated into adherent macrophages
roach SPT. Group 2 is made up of children with reported exposure to mouse (PMA), then stimulated with IFNγ/LPS and IL-4 to polarize them into the M1
and positive mouse SPT. Group 3 is made up of children with positive roach and M2 state, respectively. Cells were stimulated with omalizumab at varying
SPT but without reported exposure to roach. Group 4 is made up of children concentrations (0.1, 1, 10 mg/mL) ± IFNγ/LPS and IL-4 (during and after polar-
with positive mouse SPT but without reported exposure to mouse. Group 5 ization). Then mRNA was isolated and subjected to QRT-PCR to examine pro-
is made up of children with reported exposure to roach and positive roach file markers for M1 (CCR7 and IL12), and M2 (CD163 and CCL17). Results
ssIgE. Group 6 is made up of children with reported exposure to mouse and were normalized to GAPDH. Results: Costimulation with mAb-IFNγ/LPS
positive mouse ssIgE. Group 7 is made up of children with positive roach upregulated M1 markers CCR7 (17-fold) and IL12 (3-fold) above polarization
ssIgE but without reported exposure to roach. Group 8 is made up of chil- with IFNγ/LPS alone. Treatment of already polarized cells with mAb did not
dren with positive mouse ssIgE but without reported exposure to mouse. significantly impact transcription of CCR7 or IL12. The M2 marker CD163
was downregulated by costimulation by mAb-IFNγ/LPS (15-fold) vs. IFNγ/LPS
alone (8-fold) compared to PMA controls. IL-4 did not significantly affect M1
26 or M2 markers. M2 marker CCL17 transcription was enhanced by omalizumab
TARGETED GENE THERAPY IN THE TREATMENT OF alone (11-fold) and with IFNγ/LPS (9-fold) over PMA controls. Conclusions:
X-LINKED HYPER-IGM SYNDROME. This proof-of-concept study suggests that IgG mAB enhances transcription of
M1 markers in THP1 cells and attenuates transcription of some M2 markers.
C.Y. Kuo*1, M.D. Hoban1, A.V. Joglekar2, D.B. Kohn1, 1. Los Angeles,
This effect may be due to the Fab portion (omalizumab specific) or be isotype
CA; 2. Pasadena, CA.
specific (IgG1). Interestingly, CCL17 is an inducer of chemotaxis in T-cells,
Introduction: X-linked hyper-IgM syndrome (XHIM) is a primary immun- particularly Th2 cells that play a critical role in atopic disease and this was
odeficiency with absent IgG, IgA, IgE and normal/elevated IgM due to defects upregulated by our mAb. The interaction of the mAb may represent a point of
in the CD40 ligand (CD40L) gene. Hematopoietic stem cell transplantation immunomodulation by omalizumab not previously recognized, or a novel
(HSCT) is the only curative modality, but it carries significant risks, suggest- immunomodulatory effect of IgG1.
ing the need for improved methods of treatment. Previous studies using CD40L-
/- bone marrow corrected by retroviral-vector transfer of CD40L cDNA in
mouse models resulted in abnormal lymphoproliferation due to unregulated
expression of the gene. Hypothesis: Custom TAL effector nucleases (TALENs)
or Clustered Regularly Interspaced Short Palindromic Repeats (CRISPRs),
combined with the effective delivery of a homologous donor sequence con-
taining normal CD40L DNA, will allow for targeted integration and provide
physiologic expression of the endogenous CD40L gene to safely provide long-
term immune reconstitution. Methods/Data: TALENs targeting the 5’ UTR of
the CD40L gene were created and their function validated using a surveyor
endonuclease assay. Allelic disruption of up to 31% at the target locus in K562
cells was achieved. In order to evaluate the capacity for targeted integration of
a cassette at the cut site, K562 and Jurkat cells were electroporated with the
TALEN pair and a donor molecule with a promoterless GFP reporter gene
flanked by homology arms that parallel the cut site. In/Out PCR using a for-
ward primer within the GFP region and a reverse primer in the genomic DNA
outside the donor molecule demonstrated proper integration into K562 cells.
Targeted insertion of the GFP reporter into the CD40L locus should also pro-
vide a measure of physiologic induction of CD40L expression. Thus, expres-
sion of the GFP reporter was evaluated in Jurkat cells (which naturally express
60% CD40L), with up to 10% detected by FACs and increasing to 22% upon
PHA activation. In addition, CRISPRs targeting a patient-specific mutation in
intron 3 achieved >50% gene disruption in K562 cells. Co-electroporation with
a template donor modified to contain a unique restriction enzyme site demon-
strated site-specific gene integration by enzyme digest and gel electrophore-
28
sis. Conclusion: These results demonstrate that site-specific modification at ASSOCIATION OF VDR GENETICS VARIANTS TO PEDIATRIC
CD40L is achievable and that physiologic expression of the endogenous CD40L ASTHMA: A CASE CONTROL STUDY IN A POOR COMMUNITY
gene could provide a viable therapy for immune reconstitution in XHIM. OF THE COLOMBIAN CARIBBEAN AREA.
E. Egea1, G. Garavito de Egea*1, L. Visbal1, N. Lecompte1, G.E. Egea1,
M. Sanchez Borja2, L. Fang3, 1. Barranquilla, Colombia; 2. Caracas, Boli-
varian Republic of Venezuela, 3. Cartagena, Colombia.
Background: Vitamin D and its nuclear receptor (VDR) have been associ-
ated with asthma. Single nucleotide polymorphisms (SNPs) in the VDR gene
may alter the actions of vitamin D, and could influence the development and
severity of asthma. Objectives: To analyze the genetic association of the TaqI
VOLUME 113, NOVEMBER, 2014 A11
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A12
ABSTRACTS: CONCURRENT SESSIONS
SNP [rs731236 A> G], ApaI [rs7975232 A> C], BsmI [rs1544410 C> T] and & M2 (Fizz, Arg1) markers in obese-HDM vs. lean-HDM mice in comparison
FokI [rs2228570 A> G] with susceptibility to asthma in children from the to their controls. Finally, DEX-significantly reduced M2 marker expression but
Caribbean Coast Colombian. Methods: This was a case-control study that did not reduce M1 expression in obese-HDM mice. Discussion: Using a novel
included 1000 individuals : 500 asthmatic children belonging to a poor com- model of obesity & asthma our findings suggest a potential role of dex-resist-
munity and 500 non asthmatic children from the same socioeconomic charac- ant M1 MΦ in the etiology of steroid resistance in the obese asthmatic. Because
teristic living in Barranquilla a city on the north of the Caribbean coast of these findings are consistent with what has been observed in the obese popu-
Colombia. The SNPs were genotyped by RT-PCR and TaqMan ® probes. Allelic lation, this model might be useful to test new treatments that target reducing
and genotypic frequencies were estimated using a Arlequin v3.5 software; D’and MΦ infiltration or shifting M1 pro-inflammatory to M2-antiiinflammatory
r2 statistic Linkage disequilibrium (LD) were studied using Haploview v4.2 MΦ.
software and associated haplotypes were identified by haplo.stats v1.6.8 soft-
ware package R v3.0.2. Results: Our results showed that only the SNP BsmI
[rs1544410 C> T] was associated with the disease with a significantly higher 30
frequency of the CC genotype (57%, n = 280) in the asthmatic groups com- LONGITUDINAL STUDY OF CVID ILD.
pared with controls(49.2% n = 244)It was also found that the frecuency of CT P.J. Maglione*, C. Cunningham-Rundles, New York, NY.
genotype was 35.6% in cases, n = 175, compared with the controls (43.8%, n
Introduction: Evidence of interstitial lung disease (ILD) is a frequent radi-
= 217), p = 0.031. Haplotype analysis showed that the haplotype A / C / T / G
ologic finding in common variable immunodeficiency (CVID), however, the
was found to be a protective factor for asthma (OR = 0.49, 95% CI = 0.26 to
long-term consequence is unclear. We retrospectively examined CVID patients
0.88, P = 0.028), while haplotype A / C / C / G was showed as a risk factor for
who had pulmonary function testing (PFT) over the duration of 20 months or
disease susceptibility (OR = 1.28, 95% CI = 1.03 - 1.60, p = 0.049). The LD
more to gain insight into the natural history of CVID ILD. Methods: Retro-
analysis showed that the best D’and r2 found in SNPs block understood by TaqI,
spective chart review and statistical analysis was performed for 10 subjects
ApaI and BsmI; was D ‘= 0.753 and r2 = 0.565. Conclusion: This is the first
with CVID who had CT chest evidence of ILD and PFT covering at least 20
study conducted in asthmatic Colombian children searching for the associa-
months. CT evidence of ILD was defined as the presence of numerous pul-
tion of the VDR polymorphisms with pediatric asthma. Our results demonstrate
monary nodules, ground glass opacity, or interstitial infiltrate as noted by board-
that the VDR gene locus is associated with susceptibility of asthma in this spe-
certified radiologists in the medical record. Patients who received rituximab
cific admixed ethnic group of children seated in the Colombian Caribbean
had PFT measured 6-12 months after the completion of a single course of treat-
Coast.
ment. Results: Of the 10 patients studied, 5 had evidence of progressive ILD
indicated by (1) DLCO less than 50% of predicted, (2) DLCO less than 80%
of predicted that decreased by 20% or more during the duration of the study,
or (3) FVC that decreased by 20% or more during the duration of the study.
Initial PFT parameters and conventional laboratory tests (quantitative
immunoglobulins, CBC with differential, alkaline phosphatase) did not statis-
tically differentiate these two groups, however initial serum IgM trended higher
in patients with progressive ILD (68±28 mg/dL vs. 13±4, P = 0.08). Four of
the 5 patients with progressive ILD received treatment with rituximab and had
a significant improvement in FVC (73±1% vs. 62±2%, P = 0.01), but no sig-
nificant restitution of other PFT parameters. Conclusions: Half of the CVID
patients with CT evidence of ILD in this retrospective study had worsening of
PFTs suggestive of progressive lung disease. Initial serum IgM trended higher
in patients with progressive ILD, but other conventional laboratory parame-
ters did not significantly differentiate those who went on to have worsening
PFT. Treatment with a single course of rituximab in patients with progressive
ILD resulted in improvement of FVC. Larger studies are indicated to define
the natural history of CVID ILD and determine the optimal indication and mode
of treatment
29
M1 MACROPHAGES: A POTENTIAL ROLE IN THE DEVELOP-
MENT OF STEROID RESISTANT ASTHMA IN OBESE MICE. 31
MULTIPLE UNRELATED HETEROZYGOUS GENE DEFECTS
J.M. Diaz*1, X. Xue2, M. Solanki2, M. Gupta2, P. Chatterjee2,
PRESENTING AS A PRIMARY IMMUNODEFICIENCY.
V.R. Bonagura2, C. Metz2, 1. North Bellmore, NY; 2. Manhasset, NY.
P. Abghari*, E. Secord, P. Poowuttikul, Detroit, MI.
Background: The obesity epidemic has contributed to the development of
a new phenotype of “obese asthmatics” who are steroid resistant. To develop Introduction: Many syndromes of primary immunodeficiencies (PID) are
more effective treatments for these asthmatics, it is important to understand the well described and have been identified by genetic analysis. We present a case
etiology of this resistance. Using a mouse model of obese asthma, we previ- of a boy with hypogammaglobulinemia, malabsorption and recurrent skin
ously reported a macrophage- (MΦ) predominant infiltrate in the lungs. We lesions with multiple heterozygous defects on genotyping; any of these alone
hypothesize this non-eosinophilic cell composition contributes to steroid resist- would not likely be clinically significant, but together constitute an immune
ance. Because MΦ can be pro-inflammatory (M1) & anti-inflammatory (M2), deficiency. Case Description: A 2 year old Chaldean boy was born full-term to
we examined the infiltrating MΦ in lean vs. obese asthmatic mice. Methods: consanguineous parents. At approximately 7 weeks of age he presented with
Mice (C57BL/6, males) were fed a regular “lean” or high fat chow (60% fat). skin lesions over the umbilicus and buttock. Biopsy revealed exuberant epithe-
After 6 months, mice were given intranasal saline or house dust mite extract lial hyperplasia. By 6 months of age he developed chronic diarrhea, oral thrush,
(HDM), 5 days/week for 4 weeks. During the last 2 weeks, mice were given bacteremia, failure to thrive, poor wound healing and wound dehiscence. Lab-
either saline or dexamethasone (dex) (1 mg/kg, IP) 5 days/week. After pento- oratory evaluation at 6 months revealed hypogammaglobinemia, inadequate
barbital euthanasia, bronchoalveolar lavage (BAL) and lungs were collected. pneumococcal titers, normal oxidative burst, normal CD11, CD18, CD54 lev-
Differentials were established using Modified Wright stain. Quantitative PCR els, normal T, B and NK cell populations and normal mitogen proliferation
(qPCR) using lung tissue was performed using F4/80 (MΦ marker), Fizz (M2), assays. Intravenous immunoglobulin (IVIG) infusions were initiated. The diar-
Arg1 (M2) & Nos2 (M1) primers. Results: The absolute cell count in the BAL rhea and skin lesions responded to low dose prednisone, however despite the
was low in untreated obese & lean mice (<1x106 cells/mL), while HDM expo- response, total parenteral nutrition was necessary for nutrition. Genetic testing
sure significantly increased cell count in both (3x106). Dex significantly revealed a negative panel for SCID, agammaglobulinemia, and chronic gran-
decreased BAL counts in lean-HDM mice (<1x106) but not in obese-HDM ulomatous disease. Whole exome sequencing revealed multiple mutations of
mice (2.5x106). Both HDM groups had a significant increase in eosinophils unknown clinical significance. Two defects in DOCK 8 were detected, how-
when compared to saline control mice. BAL of lean-HDM mice was comprised ever protein was demonstrated to be present and functional. A heterozygous
of equal numbers of MΦ & eosinophils, while obese-HDM mice had more MΦ mutation for microvillus inclusion disease and a separate heterozygous defect
& fewer eosinophils. Obese-HDM-dex mice had almost no eosinophils, but for congenital malabsorption type 4 were identified as well. In addition, a het-
high levels of MΦ. qPCR revealed increased expression of F4/80, M1 (Nos2) erozygous mutation of PRKDC, which has been linked to severe combined
A12 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A13
ABSTRACTS: CONCURRENT SESSIONS
immunodeficiency when homozygous defects are present and a heterozygous icillin challenge following a negative skin test. A cost analysis was performed
mutation of the IKBKB gene which has also been linked to an immune defi- in 29 patients who had antibiotics switched to a beta-lactam after negative PST.
ciency when homozygous defects were identified. Finally, a heterozygous muta- Fourteen patients (48%) were switched to a narrow-spectrum agent (i.e.
tion of the IGFB2 gene, which codes for CD18 was identified. All were sepa- aminopenicillins, oxacillin, and non-pseudomonal cephalosporins). Total cost
rately reported as of unknown significance. Conclusion: This case illustrates of therapy with a beta-lactam after PST was $3,518. Total cost of therapy if
that multiple heterozygous defects, although not previously reported as related, initial BS/HC abx prior to PST were continued was $14,670. Approximate cost
together can present as a PID. Whole genome sequencing was able to provide for PST materials for 38 patients was $3,631. Overall cost savings was
us with results and should be considered more often in PID cases that are not $7,521.The additional savings of impact on developing adverse reactions and
straightforward and not easily diagnosed by immunology workup. superinfections (i.e. C. difficile) was not assessed. Conclusions: Following the
implementation of a PST protocol, we observed a decrease in BS/HC antibi-
otic use in patients with previously documented PA. PST is a safe and cost-
32 effective procedure to serve as a negative predictor test for penicillin hyper-
NOVEL CLINICAL DATA ACQUISITION TECHNOLOGY FOR sensitivity mediated by IgE.
MONITORING OF HOME IG INFUSION FOR PIDD.
T. Walton1, J. Ney2, D. Schaefer1, B. Geng*3, 1. Lenexa, KS; 2. Boston, MA;
3. Los Angeles, CA. 34
SEVERE THROMBOCYTOPENIA WITH UPPER GI BLEED
PIDD patients are frequently managed by several physicians and care set-
AFTER MMR VACCINATION.
tings, and usually only see Immunologist 1-4 times per year. Given increased
scrutiny on number of infections per year as a determinant of therapy and patient K. Winkler*, T. Abramowitz Saadia, J. Moallem, New York, NY.
success, with risk that more frequent infections may contribute to more severe Adverse effects of MMR vaccination, mostly self-limited and benign, are
outcomes, we asked if present care model is sufficient for collecting rate of reported. Fever in up to 15% of vaccinees 6 to 12 days after vaccination(1, 2),
infection data and whether new data acquisition technology could improve data transient rash in up to 5%, febrile seizure 5 to 12 days after immunization, as
collection. We compared sample of 16 PIDD patients from 4 physicians in sin- well as mild lymphadenopathy (2) are reported. Thrombocytopenia after MMR
gle academic immunology clinic by conducting chart review of office visit vaccination is reported in 1:25,000 to 1:2,000,000 (1). There is no report of
encounters, with sample of 40 PIDD patients from 23 physicians and 266 data thrombocytopenia resulting in severe hemorrhagic complications or death in
collection points on CareExchange®, to compare time between data collec- immunocompetent recipients (2).Infrequency with which it occurs makes it a
tions, frequency of reported infections, and infection rates per year. CareEx- challenging diagnostic task for practitioners. 13 month old African American
change® is data collection software with multiple parameters focusing on the male presented to the emergency department due to two episodes of bloody
patient’s infection rate, antibiotic use, provider visit, and overall health assess- vomitus.Two days prior he had fallen from a height of two stairs and sustained
ment. Chart review of PIDD patients on IG replacement from single academic a rapidly enlarging hematoma on his forehead. A hematoma to the lip was noted
center showed mean time between visits was 5.2 (1-24 months) and the mean on the day of presentation.10 days prior to presentation he was vaccinated
number of infections/year was 1.2 (0-5). Mean age for this group was 21 (8- with the MMR vaccine. There was no reported history of fever, recent upper
39 years). Primary diagnosis for single academic center was: 31.3% Bruton’s, respiratory illness or other illness.Physical examination in the ED demonstrated
43.8% CVID, 12.5% SCID, 6.3% Hyper-IgM. CareExchange patients had data a fussy but alert child, HR 145, RR 36, T 100.2F, with a five centimeter
collected on average 6.7 (1-15 times/year) and mean infection rate of 0.69 hematoma on the forehead, hemorrhagic lesion on the upper lip, gingival bleed-
between infusions. Mean sum of infections from all sources at any one time ing and multiple petechiae on the upper and lower extremities.The rest of the
between infusions was 1.38. Mean acute health care used between infusions physical examination was unremarkable.Laboratory investigation was signif-
was 0.4, and mean rate of new antibiotic usage between infusions was 0.25. icant for platelet count of 5K/uL, Hgb 8.4 g/dL and Hct of 24.7% on CBC.
Mean age for the CareExchange group was 39.2 years (range 5-75). Primary Indirect Coombs test and Stool Guaiac were positive.In PICU his hemoglobin
diagnoses for the group was: 48% CVID, 28% Hypogammaglobulinemia NOS further dropped to 4.0 g/dL, requiring transfusion. Bone marrow aspiration
28%, 10% Congenital Hypogammaglobulinemia. This pilot study was lim- revealed absence of lymphoblasts with increased megakaryocytes and red blood
ited, but revealed known gap in data collection, challenge of patient recall, and cell precursors. He was treated with IVIG 1g/kg/day for 2 days and Methyl-
variability of physician questions/notes/visit schedule as compared to an auto- prednisolone 4mg/kg/day for 4 days then continued on PO prednisone
mated system which can collect patient infection data as frequently as needed. 2mg/kg/day to be continued for one week. CBC on the seventh day of admis-
There’s no established acceptable rate of infections for a patient to be deemed sion showed platelets of 311 K/uL, and increase of hemoglobin hematocrit to
well controlled. There is no well-validated system of acquiring data from home 9.4 g/dL and 28%. ITP after MMR vaccination typically occurs within 6 weeks
infusion patients. Further study is needed to validate utility of this automated of vaccination (3).Mild bruising and petechiae are common (4). Hospitaliza-
uniform system of clinical data collection. tion is rarely required.Transfusion is required in 1 of 1.8 million vaccinees
(5).Platelet counts are typically >20,000 K/uL, higher than non-vaccine asso-
ciated ITP (6).This is the first report of thrombocytopenia resulting in severe
33 hemorrhagic complications in an immunocompetent recipient of the MMR vac-
IMPACT OF PENICILLIN SKIN TESTING (PST) ON ANTIBIOTIC cine.
(ABX) USE IN PATIENTS WITH A PENICILLIN ALLERGY (PA).
S. Challa*1, E. King2, K. Patel2, S. Anghel2, J. Brensilver2, L. Bielory2,
1. Springfield, NJ; 2. Summit, NJ.
35
B-CELL IMMUNOPHENOTYPING IN PATIENTS WITH GL-ILD
Rationale: PA generally leads to the use of broad-spectrum abx that may (GRANULOMATOUS INTERSTITIAL LUNG DISEASE) ASSO-
increase complications and cost. A PST pilot protocol was developed at Over-
CIATED WITH CVID (COMMON VARIABLE IMMUNE
look Medical Center to help reduce the use of broad-spectrum/high-cost
DEFICIENCY).
(BS/HC) abx and determine the cost effectiveness of PST. Methods: A retro-
spective analysis was conducted on patients who had PST performed by an E. Willits*, A. Joshi, Rochester, MN.
allergist between November 2013 – May 2014. PST included prick and intra- Introduction: Granulomatous interstitial lung disease (GL-ILD) develops
dermal testing with major (Pre-Pen™) and minor (penicillin G) determinants in a subset of patients with common variable immunodeficiency (CVID) and
followed by an oral amoxicillin challenge. Abx were de-escalated based on is commonly confused with sarcoidosis. Little is known about the immunophe-
results of PST. Reduction in cost of abx, and adverse reactions were assessed. notyping of T and B lymphocyte subsets in GL-ILD. We reviewed the charts
Cost analysis was based on the material cost of abx and skin testing compo- of four patients with CVID and GL-ILD. Methods: The presentation, labora-
nents. Study was IRB approved. Results: A total of 38 adult patients had PST. tory and imaging studies, and treatment recommendations were reviewed. Each
Median age was 64 yrs; 97%(n=37) were allergic to penicillin alone; patient presented with thrombocytopenia and splenomegaly, and was subse-
piperacillin/tazobactam (n=1), and a history of multiple abx allergies (n=9). quently found to have CVID and GL-ILD. Two patients, an 18 yr/M (#1), and
Sixty three percent had a reaction >20yrs ago with cutaneous reaction being a 12 yr/M (#2), presented with Evan’s Syndrome. Results: All patients demon-
the most common reaction (45%). Aztreonam was the most common initial abx strated significant hypogammaglobulinemia. Chest CTs were obtained in all
used prior to PST (55%).Urinary tract (26.3%) and intra-abdominal infections patients and demonstrated diffuse nodular opacities. All patients underwent
(18%) were the most common indications for abx treatment. Skin testing was BAL and bronchoscopy to rule out an acute or chronic infection in addition to
negative in 38 (100%) patients but one patient had anaphylaxis to oral amox- immunostaining and pathology studies on a lung biopsy sample. Tissue sam-
VOLUME 113, NOVEMBER, 2014 A13
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A14
ABSTRACTS: CONCURRENT SESSIONS
ples were obtained to confirm the diagnosis of GL-ILD in three out of four what concentrations rituximab achieves in neonates in utero, and if breast feed-
patients. Finally, B-Cell Immunophenotyping was obtained for all patients ing after rituximab treatment is safe. Methods: Rituximab was quantified by
and showed decrease in total memory B-Cells (CD27+),especially low class mass spectroscopy (MS) from serum of mother and infant. Results: A 31 year
switched memory B Cells (CD27+M-D-). Conclusions: These four cases illus- old primigravid woman with GPA required a fourth cycle of rituximab (375
trate the association between low class switched memory B Cells with GL-ILD mg/m2) weekly for four weeks starting at 30 weeks gestation for management
in CVID patients. Specifically, it was found that all patients had decreased of headache stemming from pituitary involvement by GPA. She delivered a
percent (3/4) or decreased absolute number (4/4) of class switched memory B healthy term infant by cesarean section at 40 weeks gestation. The baby was
Cells. B cell immunophenotyping may therefore be a useful tool for identify- exclusively breast fed without major health issues. Cord blood samples were
ing patients with CVID and granulomatous disease. Implications for early iden- not taken at the time of delivery. At four months post-partum, serum samples
tification include early initiation of specific treatment regimens, since this sub- from the infant and mother were checked and shown in Table 1. Trace amounts
set of patients may have a poorer prognosis and decreased survival when of peptides corresponding to both the heavy chain and light chain of rituximab
compared to their granuloma-free CVID counterparts. In this specific popula- were detected in the infant’s and mother’s serum by MS. Conclusions: Ritux-
tion of CVID patients, the combination of Rituximab and Azathioprine has imab peptides were detected in the serum of an infant who was exposed to rit-
been shown in preliminary studies to result in improvement in pulmonary func- uximab in utero and exclusively breast fed. The infant’s B-cell population and
tion tests and lung disease. The combination of low serum IgA levels, immunoglobulin levels did not appear to be affected at four months of age
splenomegaly and low class switched memory B cells can be used to create a (approximately 6 months after initial rituximab exposure). Measuring ritux-
prediction model for the diagnosis of GL-ILD in CVID patients in future. imab concentrations in breast milk may help to clarify if rituximab is secreted
into breast milk.
Immunoglobulin and B-Cell Phenotyping in four patients with Common
variable immunodeficiency and Granulomatous interstitial lung disease Laboratory results from infant and mother at 4 months post-partum
37
DIAGNOSTIC DILEMMA: PRIMARY IMMUNODEFICIENCY IN
A 3 YEAR-OLD PATIENT WITH GUILLAIN-BARRé SYNDROME.
S. Rogers*1, L. Potter2, 1. Kailua, HI; 2. Portsmouth, VA.
Background: X-linked agammaglobulinemia (XLA) is a primary immun-
odeficiency characterized by low immunoglobulins and an absence of B-lym-
phocytes. XLA is secondary to a mutation of the Bruton tyrosine kinase (BTK)
gene, which prevents the maturation of B cell lineages. Patients with XLA most
commonly present with recurrent sinopulmonary infections and are at risk for
severe enteroviral infections. We report the case of a 3 year old patient with a
history of recurrent infections, treated for atypical Guillain-Barré syndrome
(GBS), who was later discovered to have XLA. Case Report: The patient ini-
tially presented to our facility with proximal upper and lower extremity weak-
ness, which progressed to near complete flaccid paralysis. After initial labora-
tory and radiographic studies were unremarkable, he was diagnosed with an
axonal variant of Guillain-Barré syndrome. Empiric treatment with intravenous
immunoglobulin (IVIG) was initiated. Despite therapy, his weakness progressed
and the patient underwent plasmapheresis. After plasmapheresis he continued
to receive pulse doses of IVIG for residual neurologic deficits. Prior to his diag-
36 nosis of GBS our patient had recurrent otitis media. In the following 24 months,
IN UTERO RITUXIMAB: DETECTION OF RITUXIMAB IN AN he experienced recurrent infections such as sinusitis, pneumonia and an episode
INFANT AT 4 MONTHS OF AGE. of S. pneumoniae bacteremia. Infections often occurred 4-6 months after receiv-
J. Jin*, J. Mills, E. Conboy, M. Snyder, D. Murray, U. Specks, A. Joshi, ing IVIG. He was thereafter found to have low total immunoglobulin levels.
Rochester, MN. Flow cytometry revealed a total absence of CD19 B lymphocytes and non-
protective antibody responses to vaccination. Mutation analysis detected a
Background: Rituximab is a chimeric anti-CD20 antibody used in the treat- c.595A>T nonsense mutation of the BTK gene, confirming the diagnosis of
ment of non-Hodgkin lymphomas, chronic lymphocytic leukemia, rheuma- XLA. He was begun on monthly IVIG replacement therapy and transitioned
toid arthritis, granulomatosis with polyangiitis (GPA), and microscopic to weekly subcutaneous immunoglobulin replacement. He has remained infec-
polyangiitis. Rituximab is comprised of human IgG1(κ) heavy and light chain tion free since beginning a regular replacement program. Discussion: Patients
constant regions with murine anti-human CD20 IgG1κ variable regions. Treat- with X-linked agammaglobulinemia often present with recurrent sinopulmonary
ment with rituximab results in complement-dependent cytotoxicity, antibody- infections. However, this patient presented with atypical GBS that required
dependent cellular toxicity and direct cytotoxicity to CD20-expressing B-lym- plasmapheresis and IVIG. Pulse IVIG therapy inadvertently resulted in inter-
phocytes. Pharmacokinetic studies suggest that serum levels of rituximab can vals without recurrent infection that likely contributed to a delay in his diag-
still be detected 3 to 6 months after treatment with a half-life of elimination nosis of XLA. This case demonstrates the importance of considering primary
ranging from 5 to 78 days. As an IgG antibody, rituximab may cross the pla-
centa and be secreted into human breast milk. However, it remains unknown
A14 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A15
ABSTRACTS: CONCURRENT SESSIONS
immunodeficiency in pediatric patients with a history of recurrent or severe and the last case did not show any effect on solar urticaria. To our knowledge,
infections and atypical neurologic syndromes. this is the first case reporting rapid symptom improvement within 7 days of
initiating therapy. Although the evidence is limited, Omalizumab may be con-
sidered in patients with solar urticaria that is refractory to standard therapies
38 with anti-histamines and sunscreen.
RESOLUTION OF ALCOHOL-INDUCED RESPIRATORY REAC-
TION FOR ASPIRIN EXACERBATED RESPIRATORY DISEASE
FOLLOWING ASPIRIN DESENSITIZATION. 40
C.J. Calais*, Rockville, MD. IGG4-RELATED DISEASE IN A PATIENT WITH ALLERGIC
RHINITIS, EOSINOPHILIA AND CHRONIC URTICARIA.
Introduction: The purpose of this case is to shed more light on the link of
alcohol-induce respiratory symptoms with aspirin exacerbated respiratory dis- V. Bundy*, B. Geng, R. Kachru, M. Garcia-Lloret, Los Angeles, CA.
ease(AERD). Rationale: There is a distinct link between alcohol-induced res- Introduction: The term Immunoglobulin G4-related disease (IgG4-RD)
piratory symptoms in patients with AERD. A recent questionnaire based study refers to a newly recognized collection of fibroinflammatory disorders char-
of 50 patients which consisted of (4) clinical types (aspirin challenge confirmed acterized by tissue infiltration of IgG4-positive plasma cells and eosinophils,
AERD, aspirin tolerant asthma, aspirin tolerance with chronic rhinosinusitis, obliterative phlebitis and elevated serum IgG4. While the clinical presentation
and a healthy control), characterized the prevalence of alcohol-induced reac- of IgG4-related disease will depend on the affected organ(s), the histopatho-
tions to be highest in patients with AERD. We present a case of a patient with logical features, which are the cornerstone of the diagnosis, are strikingly sim-
confirmed AERD/Samter’s triad and alcohol-induced respiratory reaction that ilar. Little is known about the pathogenesis of IgG4-RD, but TH2 cell responses
experienced resolution of alcohol-induced symptoms with aspirin (ASA) desen- are activated at the affected sites and patients may present with concomitant
sitization therapy. Methods: Review of clinical course, documentation as well atopic symptoms. Case Presentation: A 66-year old Vietnamese man with a his-
as ASA desensitization/challenge was conducted at Walter Reed National Mil- tory of allergic rhinitis and chronic urticaria presented with a one year history
itary Medical Center Allergy Clinic. Results: Our 56 year old patient had a of worsening neck lymphadenopathy and bilateral parotid gland swelling. Lab-
history of facial flushing and profuse rhinorrhea with ingestion of alcoholic oratory evaluation showed serum eosinophils 18.2%, IgE 270 mg/ml, total IgG
beverages, which arose concurrently with his diagnosis of severe recurrent nasal 2870 mg/L, IgG1 640mg/dL, IgG2 1240mg/dL, IgG3 245mg/dL, IgG4
polyposis, asthma, allergic rhinitis, anosmia, and ageusia. He first experi- >300mg/dL, ESR 37mm/hr. Serum protein electrophoresis resulted in a total
enced hypersensitivity to motrin in 2008 followed by ASA hypersensitivity in protein 8.1gdL, albumin 52.7%, alpha 2 globulins 7.5%, beta globulins 6.3%,
2012 for which he related the symptoms of cephalic flushing, profuse rhinor- gamma globulins 31.7%, with a possible monoclonal band present in the gamma
rhea and ocular watering all of which mirrored his symptoms with alcohol region. Histopathological analysis of lymph node biopsy found plasma cell
ingestion. ASA challenge/desensitization in 2014 elicited upper respiratory dyscrasia arising in the background of IgG4-related sclerosing sialadenitis.
symptoms and a reversible decline in FEV1 of >10% from baseline. Since the Immunohistochemical studies detected sheets of monotypic plasma cells pos-
desensitization therapy, he has remained on ASA 650mg twice daily and has itive for IgG4 (IgG4 infiltrate >150/hpf), IgG (IgG4/IgG ratio 80-90%), CD138,
regained his sense of smell, taste, and can now tolerate alcohol consumption. and Kappa light chain restriction, with periductal and perivascular onion-skin-
Conclusions: The pathogenesis of alcohol-induced respiratory symptoms asso- ning fibrosis. The lymphadenopathy and parotid swelling improved following
ciation with AERD is unknown; however, current thought postulates that alco- oral corticosteroid treatment. Discussion: Because of the intrinsic TH2 bias
hol may have an inhibitory effect on the catabolism of leukotriene E4. This case that characterizes IgG4-related disease, patients’ initial clinical features may
lends clinical evidence that bolsters the idea of a common pathway for both suggest an allergic condition. The presence of lymphadenopathy, swollen parotid
conditions since ASA desensitization improved both disease processes. Clini- or salivary glands or evidence of organ dysfunction should raise suspicion for
cally, allergists should be cognizant of this link and the possibility that such IgG4-RD. Prompt recognition is key because, if untreated, the expanding inflam-
patients may be able to tolerate alcohol following successful aspirin desenti- matory lesions can potentially destroy the involved organ. Moreover, up to 16%
zation . of patients develop malignancies during the course of the disease.
39 41
A SUCCESSFUL TREATMENT OF SOLAR URTICARIA WITH EOSINOPHILIC ESOPHAGITIS: IS THERE A FOOD ALLERGY
OMALIZUMAB. CONNECTION?
M. Chong*, M. Aquino, M. Davis-Lorton, L. Fonacier, Mineola, NY. T.M. Nsouli*1, F.H. Al-Kawas2, N.Z. Diliberto2, C.M. Davis2, S.T. Nsouli2,
Background: Solar urticaria is a rare physical urticaria caused by ultravio- J.A. Bellanti2, 1. Burke, VA; 2. Washington, DC.
let radiation. Managing solar urticaria can be challenging as treatment options Rationale: Eosinophilic esophagitis (EoE) is a clinicopathological Th2-
are limited to anti-histamines, sunscreen and UV light-hardening therapy, which driven atopic disorder with an escalating prevalence. The condition is charac-
are usually ineffective. As Omalizumab has been shown to effectively treat terized by esophageal mucosal eosinophilic inflammation. Untreated EoE can
refractory chronic urticaria, we hypothesized that Omalizumab may be effec- lead to irreversible damage of the esophagus. Random food elimination appears
tive in the treatment of solar urticaria as well. We present a case of solar urticaria to be effective; however, this regimen is empiric and is not evidence-based. The
treated successfully with Omalizumab. Case Report: A 29 year old male was goal of the present study was to investigate the association of EoE and food
evaluated for a 9 year history of solar urticaria involving both exposed and allergy by means of an allergy evaluation, in order to determine the potential
lightly covered skin areas. He noted improvement in his symptoms while work- pathogenic role of specific food allergen(s), and to avoid prolonged random,
ing as a construction worker in Florida for 4 years. However, upon return to unnecessary, and unsubstantiated empiric food elimination diet(s). Method: We
New York 1 year ago he began to experience urticarial lesions every time he evaluated 54 patients (n=54; mean age= 43 years) with the diagnosis of EoE
was exposed to sunlight despite the use of high-dose antihistamines (Zyrtec based on clinical history of dysphagia, esophagogastroduodenoscopies (Fig-
40mg or Allegra 360 mg daily) and sunscreen. His urticaria was not exacer- ure 1), biopsies with > 15 eosinophils/high-power field. Patients underwent
bated by other physical factors. Challenge tests were negative to visible and food allergy evaluation by means of clinical history, allergy skin testing, and
laser light. However, multiple erythematous macules developed within 15 min- in vitro specific IgE ImmunoCAP testing. Study participants eliminated the
utes of sun exposure through a window pane and 5 minutes of direct sun expo- putative offending specific food allergen for 16 weeks. Clinical and patholog-
sure on a different site. A skin biopsy of the macular lesion revealed a super- ical improvement was assessed by a patient symptom scoring system (PSSS)
ficial to deep perivascuar inflammatory cell infiltrate consisting of lymphocytes, and by upper GI endoscopy with esophageal biopsy to monitor treatment
histiocytes, neutrophils and eosinophils. The biopsy and clinical findings were response. Results: The primary symptoms of EoE in our study included dys-
consistent with a diagnosis of solar urticaria. The patient was placed on a phagia (94%), food impaction (35%), and heartburn (96%). The common food
monthly trial of Omalizumab 300 mg SQ for a total of 3 doses. With daily chal- allergens detected included wheat (58%), dairy (53%), egg (35%), soy (28%),
lenges of sun exposure, the frequency of urticarial lesions significantly decreased peanut (25%) and tree nuts (21%). Avoidance of the above offending food aller-
7 days after the first dose with complete control of urticaria after an additional gens for a 16-week period resulted in improvement of symptoms, with a decrease
two doses of Omalizumab. Discussion: Omalizumab is a monoclonal anti-IgE (PSSS) of 98%, 100% and 90% in dysphagia, food impaction, and heartburn,
antibody that is FDA-approved for allergic asthma and chronic urticaria. A respectively. Mean average density esophageal eosinophilic infiltration (eos/hpf)
few case reports have shown variable effectiveness of Omalizumab in the treat- from mid-esophageal biopsies before and after specific food elimination diet
ment of solar urticaria; one case showed resolution, one showed improvement decreased from 36 to 6 eos/hpf. Amelioration and sustained remission occurred
VOLUME 113, NOVEMBER, 2014 A15
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A16
ABSTRACTS: CONCURRENT SESSIONS
in 82% of patients. Conclusion: The results of this study support the role of dren with peanut allergy, delayed anaphylaxis to mammalian meat, or esophageal
food allergy in EoE and illustrate the need for a collaborative gastroentero- biopsy-diagnosed EoE. Assay methods included: ImmunoCAP (CAP) using
logic/allergic approach not only for successful management of EoE, but also whole and component extracts, CAP assays on serial dilutions (1:2 to 1:8) of
for avoidance of unnecessary and potentially harmful, unsubstantiated exclu- sera, and ImmunoCAP ISAC (biochip assay for 112 purified allergens).
sion diets. This requires a multidisciplinary collaboration of gastroenterolo- Results:Analysis with ISAC correlated well with results using component-spe-
gists, allergist-immunologists, pathologists, and nutritionists. cific CAP assays for both peanut allergens (peanut allergy) and inhalant aller-
gens (EoE). By contrast, no positive results for food allergens were found by
ISAC in EoE sera that were positive for milk, wheat, or soy by CAP. Dilution
assays showed no change (undiluted value vs. calculated titer) for peanut in
peanut allergy sera or inhalants (dust mite and cat) in EoE sera in contrast, cal-
culated titers up to six times the undiluted value were noted for foods in EoE
sera (milk, wheat, and peanut) and in mammalian meat allergy sera (beef and
pork). CAP assays for 5 milk components revealed positivity to minor com-
ponents in over 50% of EoE sera. CAP assays for αgal revealed positivity in
100% of patients presenting with delayed anaphylaxis to mammalian meat.
Conclusion: Differences in the results of the dilution assays demonstrate that
assaying undiluted sera can significantly underestimate IgE Ab levels if the IgE
Ab are directed against a quantitatively minor component of the extract on the
solid phase. These results strongly suggest that the IgE Ab to milk and other
foods in EoE sera are directed against a minor component that has not yet
been identified.
44
Endoscopic Esophageal View:
EMERGENCY EPINEPHRINE USE FOR FOOD ALLERGY REAC-
Multiple Rings suggestive of EoE
TIONS IN CHICAGO PUBLIC SCHOOLS.
R. Gupta*1, L. DeSantiago-Cardenas2, V. Rivkina1, 1. Chicago, IL;
2. Phoenix, AZ.
According to the CDC, food allergy prevalence has increased by 50%
between 1997 and 2011. Currently, approximately 1 out of every 13 children,
42 or 2 children per classroom, has a food allergy. In addition, it is estimated that
THE PREVALENCE OF PEDIATRIC FOOD ALLERGY IN URBAN more than 15% of school aged children with food allergies have had a reaction
KANSAS CITY. in school and that 20-25% of epinephrine administrations in schools involve
A.L. Humphrey*, M. Reddy, J. Shroba, C. Ciaccio, Kansas City, MO. individuals whose allergy was unknown at the time of the reaction. For this rea-
Introduction: The prevalence of food allergy has been difficult to assess, son, it is important for schools to have undesignated emergency epinephrine
but previous studies report a range of 3.4%-8% in the pediatric population. It available for use in the event of an anaphylactic reaction. Purpose: The aim of
is unclear how or if geographic factors affect the prevalence of this disease. As this presentation is to demonstrate how Chicago Public Schools (CPS) was the
our institution is the primary provider of pediatric allergy/immunology con- first large urban school district in the United States to develop and implement
sultation within the urban core of Kansas City, we aimed to estimate the preva- a comprehensive stock epinephrine policy in accordance with state guidelines
lence of food allergy in children residing in this region. Methods: This study and present Year 1 findings. Significance: Understanding how CPS developed
was approved by the local Institutional Review Board. Pediatric outpatient clinic and implemented their Emergency Epinephrine Initiative will help districts
data from 2004-2014 was obtained through our hospital’s electronic medical across the United States appreciate the benefits and challenges of such an under-
record. Patients with ICD-9 codes 995.3, 995.60-995.69, 995.7, 693.1, 708, taking. Methodology: After updating a key health-related policy to include Dis-
V15.01-V15.05, and V15.09 were selected. United States Census data was used trict Issued Emergency Epinephrine, EpiPens were distributed to all schools in
to estimate total population by ZIP code. Multiple encounters by the same the district prior to the beginning of the 2012/2013 school year. Data was col-
patient were consolidated. Results: Representing 545 unique ZIP codes, 12,612 lected on District Issued EpiPen usage based on school nurse progress notes
distinct food allergic children were seen from 2004-2014. Two thousand six and principal reporting mechanisms. Findings: During Year 1 of the CPS Dis-
hundred and fifty nine children were identified within the city’s urban core trict Issued Emergency Epinephrine Initiative, 38 lives were saved because of
(26 ZIP codes). The average prevalence of food allergy in this urban core was the availability of stock epinephrine in schools across Chicagoland. Of these
5.2% with the range being 1.6%-10.3%. Conclusion: The prevalence of pedi- 38 individuals, 2 were school staff, and 36 were students between the ages of
atric food allergy in urban Kansas City over the past decade is consistent with 3 and 19, with more than half of the reactions being first time incidents. Con-
previously reported values. Further investigation is needed to determine if vari- clusion: After evaluating the distribution and tracking the usage of District
ations exist between urban, suburban, and rural settings. Issued EpiPens, the CPS Office of Student Health and Wellness has learned
key lessons which will inform the strategy for future years of the District Issued
Emergency Epinephrine Initiative. As the first large urban school district to
43 implement such a project, CPS is poised to be a national model of what a school
district can do to save the lives of its students.
CHALLENGES WITH MEASUREMENT OF IGE ANTIBODIES IN
EOSINOPHILIC ESOPHAGITIS, PEANUT ALLERGY, AND MAM-
MALIAN MEAT ALLERGY.
A. Tripathi*1, L.J. Workman1, S.P. Commins1, R. Hamilton2, E.A. Erwin3,
45
OCCUPATIONAL AND ENVIRONMENTAL RISK FACTORS FOR
T.A. Platts-Mills1, 1. Charlottesville, VA; 2. Baltimore, MD; 3. Columbus, CHRONIC RHINOSINUSITIS: A SYSTEMATIC REVIEW.
OH.
A. Sundaresan*1, A. Hirsch1, M. Storm1, B. Schwartz2, 1. Danville, PA;
Background: In the investigation of food allergy syndromes, serum assays 2. Baltimore, MD.
detecting IgE antibodies (Ab) to food allergens use whole extracts on the solid
phase, which contain specific allergen components in varying amounts. The Introduction: Chronic rhinosinusitis (CRS) is a heterogeneous inflamma-
interpretation of results assumes that the causative allergen components are tory upper airway disease of significant morbidity. Environmental exposures
adequately represented in the extract and that the presence and level of specific are thought to trigger sinonasal inflammation but no prior studies have sys-
IgE titer to the whole extract of the relevant food(s) are diagnostic of the syn- tematically reviewed what is known about key exposures and how these influ-
drome. IgE assays for beef or pork can underestimate the IgE Ab to a minor ence CRS. Methods: We searched PubMed database for relevant peer-reviewed
component of mammalian meat, αgal. The inciting food allergens in articles. We included articles if they assessed associations of occupational and
Eosinophilic Esophagitis (EoE) remain unclear, although IgE Ab to milk, wheat, environmental exposures with “chronic” sinusitis. Results: Literature search
soy, and peanut are frequently present in low titer. Method: IgE Ab to relevant yielded 1080 references and 48 articles met the inclusion criteria. Of these 37,
allergens and their components were measured in the sera of adults and chil- 8 and 3 studies assessed occupational or environmental exposures or both,
A16 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A17
ABSTRACTS: CONCURRENT SESSIONS
respectively. The quality of exposure assessment ranged from measured expo- gest that an IgE-independent mechanisms could also be involved. High-mobil-
sure by validated questionnaire (n=2) to exposure surrogates, including plant ity group box protein 1 (HMGB1) has been recently identified as an important
(30 exposures), job title linked to job exposure matrices (n=3), geographic infor- proinflammatory mediator with many characteristics similar to classic proin-
mation system (n=2) to self-reported exposures without validation (n=16). Con- flammatory cytokines The aim of our study is to investigate serum levels of
cerning outcome definition, no studies used the current clinical EPOS CRS HMGB1 and circulating sRAGE in children affected by VKC before and after
definition (symptoms plus objective evidence of inflammation). Studies were treatment with cyclosporine A (CsA) eye drops and in a group of otherways
thus classified based on the likelihood that their CRS definition represented healthy children. Methods Twenty-four children affected by VKC aged between
true CRS: “probable” n = 17 for objective criteria; “possible” n = 8 for vali- 5 and 12 yrs of life were enrolled. Twenty-four healthy children without atopy,
dated definition without objective evidence; and “least likely” n = 23 for vary- ocular, and systemic disease, cross-matched for sex and age to patients affected
ing definitions. Associations were assessed for the “probable” or “possible” by VKC, represented the controls. All children affected by VKC were treated
studies. Fishing, grain farming, diving, cotton, pickling and glass blowing, with CsA 1% eye drops for 4 wks, and blood samples were collected before
World Trade Center rescue work (n=1 study for each), self-reported work expo- and 2 wks after the end of treatment while the controls underwent to a single
sure (n=5), second hand smoking (n=5), wood stove use (n=1) and air pollu- blood sample at the time of enrollment. Statistical analyses were performed
tion (n=2) were the exposures that showed a positive association with CRS. using SPSS (Statistical Package of Social Sciences, Chicago, IL, USA) soft-
Since most exposures were only evaluated by one study, no between-study ware version 19. Ethical Committee approuved the study. Results Serum basal
evidence could be assessed. Among exposures with 3 or more studies, unclear levels of HMGB1 and sRAGE were higher in children with VKC when com-
or non-quantitative exposure assessment, biased study design, varied outcomes pared with controls while, in patients affected by VKC, no difference was
(eg. second hand smoking n=1 incident CRS, n=3 difficult-to-treat CRS with detected between atopic and non-atopic, and between ANA-positive and ANA-
3 different outcomes), and approach to analysis did not allow rigorous com- negative children. A significant reduction in serum HMGB1 and sRAGE lev-
parison or meta-analysis Conclusions: The published literature offers little els was found after the therapy while CsA serum levels were negative. Dis-
evidence of whether and how occupational and environmental exposures may cussion Our study gives a support to the definition of VKC as a systemic
be associated with CRS. Studies are needed using current clinical case defini- inflammation in which HMGB1 and its soluble receptors could play a role. We
tions and rigorous approaches to exposure assessment. did not find any detectable levels of systemic CsA at the end of our study, but
serum levels of HMGB1 and sRAGE showed a significant reduction after 4
wks of therapy. Our findings lead us to hypothesize that the topical adminis-
46 tration of CsA may influence not only the ocular immunological responses but
EFFECT OF NASAL POLYPOSIS ON NOCTURNAL SLEEP DIS- also the regulation of systemic inflammation.
TURBANCES, DAYTIME SLEEPINESS, AND SLEEP SPECIFIC
QUALITY OF LIFE DISTURBANCES IN PATIENTS PRESENT-
ING WITH ALLERGIC RHINITIS. 48
K. Kumar*, A. Shah, Delhi, India. PERIOSTIN TISSUE EXPRESSION AND ITS POTENTIAL VALUE
AS A SERUM BIOMARKER IN ALLERGIC RHINITIS.
Introduction: Allergic rhinitis (AR), chronic rhinosinusitis (CRS) and nasal
polyposis (NP) are known to coexist frequently. AR and CRS impair the qual- R. Patel*1, P. Howarth1, E. Beattie2, R. Modeste2, A. Salapatek2,
ity of life (QoL) and also adversely affect the quality of sleep. NP remains 1. Southampton, United Kingdom; 2. Mississauga, ON, Canada.
largely undiagnosed and is thought to independently affect negatively the qual- Background: Serum periostin (SP) has been proposed as a potential bio-
ity of sleep in patients with AR. Methods: The study comprised 106 consecu- marker of TH2-related airway inflammation in asthma. However, allergic rhini-
tive patients with AR (males/females, 60/46), between 18 to 60 years, enrolled tis (AR), another TH2 disease, commonly co-exists with asthma. There is lim-
from outpatients department of VP Chest Institute, University of Delhi. IRB ited information on periostin expression in rhinitis and whether this could
approval and informed consent was obtained from all research subjects. AR confound the use of SP as a biomarker in allergic asthma. Here, we aimed to
was diagnosed according to “Allergic Rhinitis and its Impact on Asthma” guide- 1) To compare the presence and extent of periostin immuno-expression in nasal
lines. CT-PNS, done in all patients, assessed the presence of CRS/NP. The biopsies from subjects with both IN and OUT-OF-season (grass pollen) AR,
patients were divided into three groups: AR alone (group 1), AR with CRS perennial (house dust mite, HDM) AR, healthy subjects and in subjects with
without NP (group 2) and AR with CRS and NP (group 3). To assess the sever- non-atopic rhinitis; 2) To assess whether airborne ragweed challenge affects
ity of the disease and impact on QoL, patients responded to Visual Analogue SP levels in OUT-OF-Season ragweed-allergic subjects. Methods: Periostin
Scale (VAS) and Sinonasal Outcome Test 22 (SNOT-22) respectively. To study immunostaining was assessed in nasal biopsies obtained from subjects with
the effect of NP on sleep, patients responded to Nocturnal Rhinoconjunctivi- IN-season AR (n=17), perennial AR (n=13), non-atopic rhinitis (NAR, n=9),
tis Quality of Life Questionnaire (NRQLQ), the Epworth Sleepiness Scale OUT-OF-Season subjects 6hrs after a nasal allergen challenge (NAC) (n=9)
(ESS) and the Pittsburgh Sleep Quality Index (PSQI). Results: The 106 patients and healthy (n=9) and non-rhinitic subjects (n=9) (Figure 1). Serum SP was
were categorised as follows: group 1 with 34 (32%), group 2 with 36 (34%) evaluated in subjects with ragweed-induced seasonal AR (n=15) and healthy
and group 3 with 36 (34%) patients. Mean global VAS score increased from (non-rhinitic, HNV) controls (n=5) before and after a 4 hour exposure to rag-
7.12 in group 1 to 7.66 in group 2 and 8.03 in group 3 (P=0.004). Mean SNOT- weed allergen in an environmental exposure chamber (EEC) on 2 consecutive
22 score increased from 45.47 in group 1 to 66.83 in group 2 and 70.22 in group days. Results: The extent of nasal biopsy periostin immuno-expression was sig-
3 (P=0.001). Similarly, mean NRQLQ score increased from 32.94 in group 1 nificantly increased IN-Season AR (p<0.05), OUT-OF-Season NAC AR
to 49 in group 2 and 63.19 in group 3 (P=0.002). Mean ESS score too increased (P<0.05) and perennial AR (p<0.05) compared to non-allergic rhinitis and
from 9.76 in group 1 to 11.14 in group 2 and 12.24 in group 3 (P=0.001). Mean healthy subjects. No significant differences were noted between seasonal and
global PSQI score also increased from 7.17 in group 1 to 9.67 in group 2 and perennial AR groups (p=0.950) or between healthy and non-atopic rhinitis
13.58 in group 3 (P=0.001). Conclusions: NP occurs in half of the patients with groups (p=0.233) (Figure 1). There were no significant differences seen in SP
AR and associated CRS. The presence of NP significantly increased the sever- after ragweed challenge compared to HNV studied in the EEC. Conclusion:
ity of the disease and negatively impacted the QoL. Instruments to assess the Mucosal but not SP expression is increased in both seasonal and perennial AR
effect on sleep highlighted the significant adverse impact of NP on the qual- compared to non-atopic rhinitis and HNV controls. This suggests SP does not
ity of sleep. Its presence denotes a more severe form of the disease, thus empha- reflect local nasal inflammation and is therefore not a reliable systemic bio-
sising the need for early diagnosis. marker for AR. Concomitant nasal disease should thus not interfere with the
value of SP as a biomarker in asthma.
47
VERNAL KERATOCONJUNCTIVITIS AS A SYSTEMIC DISEASE.
M. Duse*, A. Zicari, M. Nebbioso, F. Occasi, L. Leonardi, A. Zicari, Rome,
Italy.
Vernal keratoconjunctivitis (VKC) is a chronic disease affecting conjunc-
tiva even though the immunopathogenetic mechanisms underlying this inflam-
mation are unclear. Although many clinical and laboratory findings support the
presence of an IgE-dependent immediate hypersensitivity reaction in VKC [2],
the conflicting results concerning the association between VKC and atopy sug-
VOLUME 113, NOVEMBER, 2014 A17
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A18
ABSTRACTS: CONCURRENT SESSIONS
rubella (MMR)=18%, varicella=8%, rabies=4%. Ped physicians answered cor-
rectly regarding influenza (not CI) and yellow fever (CI) (49,50%) more than
IM physicians (12,16%)(p<0.05). IM residents (22%) answered MMR more
than any other group (p<0.05). Only 27% of all Ped physicians correctly iden-
tified common causes of IgE mediated food allergy in children <4 years old:
egg=69%, milk=40%, whereas strawberry=34%, artificial food coloring=13%.
The majority of Ped physicians (47%) responded that skin prick testing for food
or inhalant allergens is not accurate or reliable until 3 years old. Of all physi-
cians, 58% answered that medications may interfere with serum IgE results and
38% felt serum IgE testing was a useful screening test to detect the presence
of food allergy. Our survey identified substantial knowledge gaps regarding
common A/I conditions among IM and Ped faculty and residents at academic
medical centers. Improved education and quality improvement strategies are
needed to help provide the most accurate and up to date medical care for patients.
Figure 1: Periostin staining in Allergic Rhintis Phenotypes.
51
INCREASED COMORBIDITY OF ANTERIOR SEGMENT DIS-
49 EASE IN AN ALLERGIC POPULATION.
SERUM 25-HYDROXYVITAMIN D LEVELS IN PATIENTS WITH B.P. Bielory*1, J. Pepose2, E. Donnenfeld3, M. McDonald3, K. Nichols4,
EOSINOPHILIC ESOPHAGITIS. L. Bielory5, 1. Valhalla, NY; 2. St Louis, MO; 3. Lynbrook, NY;
M. Slack*1, P.U. Ogbogu1, T.A. Platts-Mills2, E.A. Erwin1, 1. Columbus, 4. Houston, TX; 5. Springfield, NJ.
OH; 2. Charlottesville, VA. Rationale: The purpose of this study was to evaluate the prevalence and
Rationale: Studies have suggested that vitamin D deficiency is associated severity of dry eye disease (DED) in a consecutive series of patients present-
with increased prevalence of atopic disorders such as asthma, food allergy, ing to an allergy practice. Methods: 68 consecutive patients were tested for tear
and atopic dermatitis; however it has never been assessed in eosinophilic hyperosmolarity and polled for binary DED symptoms: fluctuating vision, lens
esophagitis (EoE). Our objective was to determine the levels of 25-hydrox- discomfort, light sensitivity, watery eyes, tired eyes, redness, burning, itching
yvitamin D in a cohort of patients with EoE. Methods: We measured total serum and grit. Data were compared to 9,407 subjects polled nationally across oph-
25-hydroxyvitamin D using liquid chromatography with tandem mass spec- thalmologist and optometrist practices. Results: Of the patients reporting to the
trometry in adults (n=35) and children (n=34) with EoE. We compared the allergy clinic, 42.6% were highly symptomatic (reporting ≥ 5 symptoms), while
results to our patient demographics, EoE specific disease parameters, and mark- 15.8% reported ≥ 5 symptoms nationally. However, only 37.5% of the symp-
ers of allergy using multiple logistic regression. Results: The median vitamin tomatic subjects were hyperosmolar in the allergy clinic, compared to 51.6%
D level was 29 ng/ml. Patients with insufficient vitamin D (<30 ng/ml) were nationally. Although a smaller prevalence, the hyperosmolar subjects present-
older (age 25.5 compared with 16.2 years) and had a higher body mass index ing to the allergy center displayed a significantly higher severity, averaging
(BMI) (median 25.2 compared with 19.8, p<0.001). Peak esophageal eosinophil 337±28 mOsm/L vs. 323±16 mOsm/L nationally (p < 0.0001). Non-DED sub-
counts were not different in vitamin D insufficient and sufficient patients; how- jects were clinically identical, averaging 295.7 mOsm/L vs. 297.8 mOsm/L
ever, higher vitamin D levels were associated with higher tissue eosinophil nationally, which ruled out the possibility of instrumental variation or analyt-
counts (R=0.26, p<0.05). While there were no differences in total IgE or titers ical drift accounting for the difference in severity. These data suggest that dry
of specific IgE in insufficient and sufficient patients, positive skin prick test eye in the presence of allergy may be more severe than dry eye alone, and that
to peanut was more common in patients who were vitamin D insufficient with symptoms alone were insufficient to determine diagnosis. Conclusions: There
odds ratio (O.R.) 5.98 (95% CI 1.51-23.7). This result remained significant in is a significant overlap in symptoms of both allergy and dry eye disease. Objec-
a logistic regression model in which the results were adjusted for age and BMI tive testing can help differentiate between the two etiologies. Further, con-
(O.R. 7.57 (95% CI 1.66-34.6). Conclusions: In our group of adult and pedi- comitant DED in the presence of allergy may be more severe than DED alone.
atric patients with EoE, vitamin D levels were low overall (median <30 ng/ml)
indicating that this is a population at risk for vitamin D insufficiency. Inter-
estingly lower vitamin D levels were not associated with higher esophageal 52
eosinophil counts. The only marker of allergy associated with having an insuf- CORRELATION OF HOUSE DUST NICOTINE WITH REPORTED
ficient level in EoE patients was positive skin prick test to peanut. SMOKING HISTORY.
C.S. Barnes*, F. Pacheco, R. Allenbrand, L. Gard, C. Ciaccio, Kansas
City, MO.
50 Introduction: Exposure to cigarette smoke is a major asthma trigger and
ALLERGY MISCONCEPTIONS AMONG PHYSICIANS AT ACA- has a detrimental impact on pediatric asthma. Allergists frequently estimate
DEMIC MEDICAL CENTERS. pediatric exposure to cigarette smoke through questions directed to parents or
K.J. Wada*1, S. Montandon2, T. Green2, D. Stukus1, 1. Columbus, OH; care givers. To evaluate the relationship of reported indoor smoking to actual
2. Pittsburgh, PA. levels of nicotine measured in house dust we performed the following studies.
Poor understanding of allergic conditions can influence patient care through Methods: Dust was collected from homes enrolled in the Kansas City Safe
unnecessary diagnostic testing and/or management thus negatively impacting and Healthy Homes Project. Project enrollees were asked a series of questions
quality of care, cost, and outcomes. We conducted an anonymous electronic concerning smoking in the home including the number of persons in the home
survey of pediatric (Ped) and internal medicine (IM) residents and faculty physi- who smoke and if anyone was allowed to smoke inside the house. A conven-
cians at two tertiary care academic medical centers. Participants completed a ience sample of 58 homes containing 0 to 5 individuals who declared they
6 (IM) or 9 (Ped) item questionnaire regarding allergy evidence and/or guide- smoked cigarettes was selected for analysis. For all samples, nicotine was
lines. 409 surveys were collected (Ped faculty=129, Ped residents=106, IM fac- extracted from 0.2 grams of dust and analyzed by immunoassay using com-
ulty=78, IM residents=96). An elective rotation in allergy (A/I) was completed mercially available reagents. For conformation in one-third of samples nico-
by <50% of faculty and <20% of residents. When asked for the best first treat- tine was extracted from 0.5 grams of dust and analyzed for nicotine by gas chro-
ment for a patient experiencing urticaria and emesis immediately following matography mass spectroscopy (GCMS). Results: Enzyme immunoassay results
ingestion of a known food allergen, physicians reported: epinephrine=64%, 1st indicated nicotine values for the 58 dusts ranged from 0 to 330 nanograms per
generation antihistamine=31%, H2 antagonist=3%, prednisone=1%. Only 50% gram of dust. GCMS analysis results ranged from 0 to 340 nanograms per gram
of all IM physicians answered epinephrine (p<0.0001). Regarding allergies that of dust. Correlation between the two methods was strong (r = 0.90). The lower
should be inquired about prior to ordering an imaging study with radiocon- limit of detection for the immunoassay was calculated at 4.0 nanograms per
trast media: iodine=80%, shellfish=40%, artificial dye=21%. IM physicians gram of dust and for the GCMS at 100 nanograms per gram of dust. Dust-
reported iodine (89 vs 73%) and shellfish (47 vs 34%) more than Ped physi- borne nicotine concentrations were greatest in homes where up to 3 declared
cians (p<0.05). Regarding contraindicated (CI) immunizations in egg allergic smokers resided. The highest nicotine concentrations came from houses with
patients, they answered: influenza=85%, yellow fever=49%, measles, mumps, declared smokers who smoked in the home. Dustborne nicotine concentrations
A18 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A19
ABSTRACTS: CONCURRENT SESSIONS
in homes where smoking was not permitted inside the house ranged from 0 to by A/I Providers were 123.34 (SD±178.5) for an average of 69.1 (SD±77.1)
50 nanograms per gram of dust. Conclusion: Nicotine concentration in house unique Medicare beneficiaries. Conclusions: The Physician and Other Supplier
dust can be measured by commercially available immunoassay methods. Homes PUF provides a unique opportunity to better understand how Allergy/Immunol-
where smoking was permitted had higher dust nicotine than homes where smok- ogy providers fit into the overall healthcare landscape. Allergy/Immunology
ing was not permitted. However, homes where smoking was declared not per- providers can use this data better to understand how their practice compares to
mitted were not without nicotine in house dust. national norms.
53 55
DEVELOPMENT OF A NONINVASIVE SCREENING ASSAY FOR PRENATAL AND EARLY LIFE DETERMINANTS OF ATOPY:
EOSINOPHILIC ESOPHAGITIS. PRELIMINARY FINDINGS OF THE KINGSTON ALLERGY
K.M. Maples*, T.C. Burch, A.M. Perkins, K.M. Cunnion, N.K. Krishna, BIRTH COHORT.
H. Minto, L.K. Willis, J.O. Nyalwidhe, Norfolk, VA. M.L. North, J. Thiele, V. Omana, M. Soliman, A.K. Ellis*, Kingston, ON,
Introduction: Currently there is no noninvasive assay to evaluate for the Canada.
possibility of eosinophilic esophagitis (EoE) in patients with suggestive symp- Background: Many authorities have recognized that gene-environment inter-
toms. The current standard of diagnosis and monitoring is endoscopy but this actions likely play a key role in the developmental origins of allergy, now known
is an imperfect approach. Endoscopy is invasive, esophageal epithelial to be mediated largely by epigenetic modifications. Prospective epigenetic stud-
eosinophilia is not uniform, there is not a standardized high-power field (hpf) ies, beginning in utero involving the collection of umbilical cord blood pro-
size and current diagnostic thresholds for eosinophils per hpf correlate poorly vides a window into the prenatal environment and a prospective sample to iden-
with clinical measures of disease. Identification of a truly noninvasive bio- tify epigenetic markers that precede the development of allergy. Methods: The
marker for EoE and a standardized, reliable assay is an important unmet med- Kingston Allergy Birth Cohort (KABC) now includes over 400 children born
ical need. Methods: Urine samples were obtained from patients with biopsy in Kingston, Ontario, and surrounding rural areas with mother/child pairs
proven EoE (n=27) and from atopic controls (n=24) without eosinophilic recruited during the prenatal period, many of whom are between 18mo to 3y
esophagitis. We used a targeted Single Ion Monitoring LC-MS-MS strategy to of age. 60 mother/child pairs thus far have returned to undergo skin testing
quantify the levels of 3-Bromotyrosine (3-BrTyr) in creatinine-normalized urine (common environmental and food panel) and surveys completed regarding
samples. Descriptive statistical analysis was performed for 3-BrTyr level fol- symptoms of potential atopic disease in the child as well as relevant home and
lowing stratification and compared using the Mann-Whitney U test. Results: dietary exposures in the first 2y of life. Some children have also been evalu-
The median urine 3-BrTyr level was 12-fold higher for all subjects with EoE ated in local Allergists offices for suspected allergy. Results: Of 60 children
(169.50 picograms 3-BT/400 mg creatinine/dL, IQR 40.74-412.86) compared evaluated thus far, 11 (18.3%) demonstrated at least one positive SPT: 8 had
with atopic controls (12.87, IQR 3.51-114.69 (P=.01)). In order to evaluate positive SPT to a food allergen, only 4 of whom had a clinical history of sup-
the potential utility of urine 3-BrTyr as a screening test we performed a subset porting food allergy, however. 5 children had at least one positive environmental
analysis evaluating only newly diagnosed and untreated patients with EoE com- SPT, 2 of which had symptoms suggestive of early asthma. On preliminary
pared with atopic controls. The median urine 3-BrTyr level was 13-fold higher analysis, factors associated with, or trending with, positive SPT include furry
for untreated subjects with EoE (172.62, IQR 81.30-327.60) compared with pet ownership (P=0.038; Fisher’s Exact Test), early-life second hand smoke
atopic controls (12.87, IQR 3.51-114.69 (P=.0459)). Using a threshold cutoff exposure (P=0.1) and breastfeeding for less than 3 months (P=0.074). Con-
of 145 yields a sensitivity of 67% and a specificity of 79%. Thus, a 3-BrTyr clusions: Data collection is ongoing. Our early high rate of atopy likely reflects
level<145 yields a negative predictive value of 90.48% in atopic individuals. interest-bias from parents concerned about allergies. Pets, second-hand smoke
Conclusions: This proof-of-concept study demonstrates a reliable assay for uri- and breastfeeding will be further explored. We anticipate epigenetic analysis
nary 3-BrTyr. Further, urinary 3-BrTyr has the potential to be a useful, nonin- of cord blood from atopic children compared to age/gender-matched controls
vasive biomarker in the diagnosis and management of EoE. will provide a window into the prenatal environment and potentially identify
biomarkers that precede allergic disease
54
ANALYSIS OF THE 2012 US MEDICARE REIMBURSEMENT 56
DATA: PUTTING ALLERGY/IMMUNOLOGY DATA INTO CON- THE ASSOCIATION OF HOUSEHOLD AIR POLLUTION WITH
TEXT. ALLERGIC RESPIRATORY DISEASES IN CHILDREN.
A.S. Nickels*, G. Volcheck, Rochester, MN. R. Kumar*, K. Singh, U. Mehto, S. Nagar, R. Prasad, Delhi, India.
Introduction: Released in April 2014 by the Center for Medicare and Med- Background: Indoor air pollution is the third leading cause of disease bur-
icaid Services (CMS),the Provider Utilization and Payment Data Physician and den in South East Asia as per Global burden of disease study 2010. Children
Other Supplier Public Use File includes reimbursement information on 6000 are much more susceptible to household air pollutants as they spend most of
different procedures/ services reimbursed to over 880,000 healthcare providers their time indoors. The present study was thus planned to assess the effect of
in 2012. We have analyzed this database hoping to better understand how indoor air pollution on childhood asthma and/or allergic rhinitis. Methods: The
Allergy/Immunology providers are contributing to the care of the Medicare present study is a cross sectional study to assess the difference in household
population. Methods: Using the Physician and Other Supplier PUF Aggregate air quality in houses having children (<17 years age) with or without asthma
file, the average number of unique beneficiaries seen, total paid by medicare and/or allergic rhinitis in a rural setting (Village Khanpurjupti, Loni, Ghazi-
to each physician, and the average amount paid per unique beneficiary was cal- abad) of Delhi NCR region. Seventy households were selected in which none
culated. These values were calculated for the other provider types for contex- of the child had symptoms of asthma and/or rhinitis while the other seventy
tualization of the results across the healthcare field. We excluded any organi- households had at least one child with asthma and/or rhinitis. A standard ques-
zational provider types, non-MD/DO provider types, non-face-to-face diagnostic tionnaire was filled for all children enrolled in study, information was collected
specialties, as well as specialties with less than 100 providers. Eighty nine from parents of child during the study and potential pollutant sources were
providers types are included in the Physician and Other Supplier PUF with 53 identified in their residence. PM 2.5 was measured by using UCB Particle and
provider types included in the final analysis. Focusing on Allergy/Immunol- Temperature Sensor (UCB-PATS) from Berkley Air monitoring group,
ogy providers only, we calculated the average number of unique beneficiaries USA.VOCs were measured by using Phocheck Tiger PID, Ion Science limited,
seen as new or established patients was also calculated from the database. UK. The measurements of PM 2.5 and VOC were done at an interval of 10 min-
Results: A total of 3119 Allergy/Immunology providers saw for an average of utes in each of 140 households for a day. Result: There were a total of 108 chil-
160.4 (SD ±179.6) unique Medicare beneficiaries and collected an average of dren (52 asthma alone, 20 allergic rhinitis alone and 36 with co-existent asthma
$52,762 (SD ± $103,425). Among Allergy/Immunology providers, the average and allergic rhinitis) in the 70 houses having children affected with asthma
amount paid per unique beneficiary was $313 (SD ±$449). Of the 53 provider and/or rhinitis. The level of pollutants was found to be twice higher in affected
types included in the final analysis, Allergists ranked 45th in average number children houses as compared to control houses. The average PM2.5 levels were
of unique beneficiaries seen, 40th in average amount collected from CMS, and significantly higher (9.68mg/m3vs 4.31mg/m3; p 0.011) in affected houses as
16th in average amount paid per beneficiary in 2012. Allergy/Immunology compared to controls. Similarly VOCs levels were higher in these houses (2.222
providers billed for an average of 35.2 (SD ± 31.9) unique Medicare benefici- ppm vs 1.161 ppm; p 0.128) but could not reach statistical significance. It was
aries for new patient visits (all types). The average number of established visit also seen that houses of children with asthma and/or rhinitis had higher sec-
VOLUME 113, NOVEMBER, 2014 A19
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A20
ABSTRACTS: CONCURRENT SESSIONS
ond hand smoke, kerosene and biomass fuel use. Conclusion: Household air
pollution from smoking, kerosene and biomass fuel combustion results in an
58
DO PARENTS INFLUENCE HEALTH LITERACY AND IMPACT
increased levels of PM2.5and VOCs in household air, which may be responsi-
ble for increased level of asthma and/or allergic rhinitis in children. ASTHMA SELF-MANAGEMENT IN RURAL GEORGIA HIGH
SCHOOL STUDENTS?
J.S. Bush*, J.L. Waller, D.R. Ownby, M.S. Tingen, Augusta, GA.
57 Introduction: Patients with lower health literacy (HL) have poorer under-
PATTERNS OF RESPONSE IN CHRONIC IDIOPATHIC/SPON- standing and self-management of chronic diseases, including asthma. We
TANEOUS URTICARIA (CIU/CSU) PATIENTS TREATED WITH hypothesized that parents/caregivers were an important source of HL for teenage
OMALIZUMAB IN TWO RANDOMIZED DOUBLE-BLIND students, which would be indicated by agreement between student and care-
PLACEBO-CONTROLLED CLINICAL TRIALS (ASTERIA I AND giver HL scores on standard instruments. Methods: HL status was assessed as
ASTERIA II). part of Puff City, a randomized controlled trial of a web-based asthma educa-
A. Kaplan*1, E. Antonova2, B. Trzaskoma2, K. Raimundo2, S. Khalil3, tion intervention in four rural Georgia high schools. Baseline sociodemographic
data was obtained. Due to the small percentage of “other race,” whites and other
T. Omachi2, J. Zazzali2, 1. Charleston, SC; 2. South San Francisco, CA;
races were combined for analyses. Three validated instruments were used:
3. Basel, Switzerland. REALM (Rapid Estimate of Adolescent/Adult Literacy in Medicine) and SILS
Introduction: Little is known about how quickly chronic idiopathic/spon- (Single Item Literacy Screener). To examine agreement between scores,
taneous urticaria (CIU/CSU) patients respond to omalizumab treatment and weighted kappa statistics were calculated. Bowker’s test of symmetry was used
for how long they maintain their response. We report patterns of treatment to examine equality of disagreement in scores. Differences in REALM and
response from ASTERIA I and ASTERIA II (pooled). Methods: Subjects were SILS scores were examined with t- and chi-square tests. Results: 243 students
randomized 1:1:1:1 and received placebo (PLB) or omalizumab 75, 150, or 300 and 203 caregivers completed HL assessments yielding 198 paired observa-
mg (OMA75, OMA150, OMA300) every 4 weeks for 3 (ASTERIA II, n=322) tions. The students attended grades 9-12, were 60.6% female, 72.7% African
or 6 (ASTERIA I, n=318) doses. Patients completed the Urticaria Patient Daily American (AA), with mean age of 15.3 (SD 0.9) years. Parent education ranged
Diary (twice-daily), from which a daily Urticaria Activity Score (UAS) was from less than high school diploma (19.1%) to college graduate (24.0%). Sig-
calculated; the 7-day sum of UAS is given as UAS7. Response was defined in nificant differences of REALM scores were seen between AA and white stu-
two ways: (1) well-controlled urticaria (UAS7≤6) and (2) complete response dents, 56.2 (10.6) vs 60.8 (6.8), p<0.0005, respectively. Agreement between
(itch and hive free, UAS7=0). The duration of response was defined as the student and caregiver REALM categories was poor (κw=0.26) while disagree-
percentage of the treatment period, during which patients experienced their ment did not significantly differ by scores or demographic variables. There was
responses. IRB approval and informed consent were obtained from all research significant disagreement between student and caregiver scores on SILS and
subjects. Results: From baseline to week 12, UAS7≤6 was achieved at some this differed by caregiver race, with students having higher scores when their
point in time by 28% of PLB, 49% of OMA75, 56% of OMA150, and 73% of caregiver was AA. Agreement in SILS scores between student and caregiver
OMA300 patients; for UAS7=0: 13% of PLB, 26% of OMA75, 33% of was poor for both caregiver race groups, but whites/other race caregivers had
OMA150, and 53% of OMA300 patients. During the 12-week treatment period, a higher weighted kappa (κw=0.31) than AA caregivers. Conclusion: The poor
patients who reached a UAS7≤6 at some point in time, had this level of response agreement between student and caregiver HL scores suggest that teens do not
for a mean percent of time of 45% (PLB), 42% (OMA75), 54% (OMA150) or primarily acquire HL from caregivers. Consistent with previous adult litera-
65% (OMA300); for UAS7=0 the mean percent of time was 34% (PLB), 29% ture, there appears to be a disparity in adolescent HL between AA and whites.
(OMA75), 37% (OMA150), or 52% (OMA300). The median time to achieve The lower HL among AA teens suggests that they are likely to require more
UAS7≤6 was 10 weeks (OMA150) and 4 weeks (OMA300) and to achieve physician effort to become proficient in asthma self-management.
UAS7=0 was 10 weeks (OMA300). Less than 50% of patients achieved UAS7≤6
in PLB and OMA75 and UAS7=0 in PLB, OMA75, and OMA150, thus we
did not calculate their median time to respond. Conclusion: More CIU/CSU
patients in OMA300 achieved well-controlled or complete responses than
59
PROFILING AND VISUALIZING UTILIZATION AND COST FOR
patients in other treatment arms. OMA300 patients achieved their responses PEDIATRIC ASTHMA CARE IN THE MEDICAID SYSTEM.
sooner and maintained them for longer than those in any other arm. These results
provide additional insights about how CIU/CSU patients might respond to oma- R.P. Hilton1, N. Serban1, Y. Zheng*2, 1. Atlanta, GA; 2. Smyrna, GA.
lizumab therapy over time. These data can help healthcare providers by setting Introduction: The aim of this study is to summarize and visualize the uti-
expectations of likelihood of response in CIU/CSU patients at different time lization and cost relational system between providers for pediatric asthma care
points after omalizumab initiation. in the Medicaid system using large patient-level claims data. We investigate
an inferential and graphical approach for uncovering patterns in the healthcare
Number and percentage of patients who achieved the state of well-con- utilization within the Medicaid system. We pilot this study for pediatric asthma
trolled urticaria or complete response by week and study arm. patients in Georgia and North Carolina using the 2009 patient-level claims data.
Methods: We apply sequence clustering analysis (SCA) to classify patients
according to their utilization profiles, and for each cluster, we derive a proba-
bilistic network of care where the probabilities are determined based on the
patient-level utilization across providers of different types. The underlying
utilization networks are the basis in deriving the cost relational system between
providers. Results: We use the Markov chain representation of the utilization
profiles to visualize the network model for each profile as derived from the
SCA with three profiles. Profile 1 is dominated by patients primarily utilizing
Emergency Department (ED) care services with a small proportion referred to
primary care. Profile 2 is dominated by patients primarily utilizing primary
care once or multiple times with a small proportion visiting ED. Profile 3 has
a high variation in utilization. Among the children with asthma in the 2009
Medicaid system of Georgia, about half of the patients utilize primary care
BSL = baseline; PLB = placebo; OMA = omalizumab, UAS7 = Weekly whereas the other half either seek care through ED or from multiple providers.
Urticaria Activity Score. The cost analysis shows that the distribution of cost-per-visit for ED visits is
similar across the three profiles with a higher median for the ED-care preva-
lent profile. The costs for other provider types have similar symmetrically-
shaped distribution but with some differences in the median across all three
profiles. Conclusion: It is not surprising to find that ED visits contribute to a
large portion of the cost for pediatric asthma care where most of the ED cost-
per-visit values are in the range of other care visit types suggesting that many
ED visits are for routine care. However, we also find that about half of the
A20 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A21
ABSTRACTS: CONCURRENT SESSIONS
children in the Medicaid system in Georgia do utilize primary care, they stay
on this path, and thus cost less.
61
A RANDOMIZED PHASE 3 STUDY ASSESSING PATIENT-
REPORTED OUTCOMES AND SAFETY OF RESLIZUMAB IN
PATIENTS WITH ASTHMA WITH ELEVATED EOSINOPHILS.
J. Maspero*1, L. Bjermer2, C. Lemiere3, M. Ciesielska4, C. O’Brien4,
J. Zangrilli4, 1. Buenos Aires, Argentina; 2. Lund, Sweden; 3. Montreal,
Canada; 4. Frazer, PA.
Introduction: Reslizumab (RES), a humanized anti-human interleukin-5,
is in development for patients with moderate to severe persistent asthma with
elevated eosinophils (EOS). We compared patient-reported outcomes (PROs)
and safety of RES vs placebo (PBO) in patients with asthma and elevated EOS.
Methods: This multicenter, double-blind, 16-week study (NCT01270464)
included patients (N=311), 12-75 years of age, with uncontrolled asthma on at
least medium-dose inhaled corticosteroids with/without additional controllers,
Asthma Control Questionnaire score ≥1.5, and blood EOS level of ≥400/mL.
Randomization was to intravenous RES 0.3 mg/kg (n=104) or 3.0 mg/kg
(n=106) or PBO (n=105) once every 4 weeks. PROs included Asthma Quality
of Life Questionnaire (AQLQ) (7-point scale, 1 [all of the time]; 7 [none of
the time]; minimal important difference [MID], 0.5 U), and Asthma Symptom
Utility Index (ASUI) (0 [worst possible symptoms]; 1 [no symptoms]). Results:
Baseline clinical characteristics were similar among treatment groups. At 16
weeks, RES 0.3 mg/kg and 3.0 mg/kg improved AQLQ from baseline (mean
treatment difference vs PBO 0.278 and 0.359, respectively). The difference
between RES 3.0 mg/kg and PBO was statistically significant (P=0.0241). The
percentage of patients with a MID in AQLQ at week 16 was 59%, RES 0.3
mg/kg; 64%, RES 3.0 mg/kg; and 48%, PBO. The difference between RES 3.0
mg/kg and PBO was statistically significant (P=0.0189). RES-treated patients
had statistically significant (P≤0.016) ASUI improvements vs PBO (mean treat-
ment difference vs PBO: 0.51, RES 0.3 mg/kg; 0.47, RES 3.0 mg/kg). Most
(86%) patients received 4 complete infusions of RES. Incidence of adverse
events (AEs) was similar among treatment groups. Serious AEs for RES
occurred in the 3.0 mg/kg group (1 patient with pneumonia, road accident/rib
fracture, and asthma exacerbation; 1 patient with sinusitis; 2 patients with
60 asthma exacerbations). AEs led to discontinuation in 10%, <1%, and 6% of
TRENDS OF ATTENTION OF ASTHMA AT THE INSTITUTO PBO, RES 0.3 mg/kg, and RES 3.0 mg/kg patients, respectively. Conclusions:
MEXICANO DEL SEGURO SOCIAL 2007-2012. In patients with uncontrolled asthma and elevated blood EOS, 4 monthly doses
M. Nunez*, M. Becerril-Angeles, V.H. Borja-Aburto, A. Rascon-Pacheco, of RES were well tolerated and associated with improvements in PROs of qual-
U. Angeles-Garay, M. Vargas-Becerra, Mexico City, DF, Mexico. ity of life and symptoms. This study was sponsored by Teva Pharmaceuticals.
Introduction: The prevalence of asthma in Mexico is about 10%. The Insti-
tuto Mexicano del Seguro Social (IMSS) attends a population of 58 millions,
and one third of the new cases of asthma coming from public hospitals around 62
the country. Methods: The registries of consultations, emergencies, discharges, DEVELOPING A RISK STRATIFICATION MODEL TO ALLO-
and deaths, due to asthma of all medical units of the IMSS in the period 2007- CATE LIMITED ASTHMA RESOURCES.
2012 were analized. Results: There was an annual average of 839, 363 con- J. Hanson*, H. Murphy, D. Williams, B. Lee, M. Reddy, Kansas City, MO.
sultations, including new cases and subsequent cases of asthma. The consul- Background: Current models for calculating asthma related risk require
tations increased 31%, from 720, 041 in 2007 to 947, 452 in 2012. The average clinical parameters or administrative data. Often, programs that conduct dis-
incidence was 236 cases per 100, 000 patients covered by Social Security. The ease management, community outreach and environmental assessment do not
state with the highest rate of cases was Yucatan (3625.9); and the state with the have access to either. The aim of this study is to develop a simple risk stratifi-
lowest rate was Hidalgo (697.6). The 10 states with the highest rates are located cation model to help allocate limited resources to children with high risk asthma.
on the coast, and 9 of the 10 states with the lowest rates are away from the coast. Methods: This is an IRB approved retrospective study of 11,915 patients <18
There was an annual average of 265, 425 cases of asthma in the emergency years seen for an asthma diagnosis at one of 23 outpatient clinics at our insti-
room. The emergency cases decreased from 37.3% in 2007 to 28.2% in 2012. tution between 1/1/10 and 5/31/12, regardless of whether asthma was the prin-
The hospital discharges decreased 9.3%, from 14, 313 in 2007 to 12, 987 in cipal diagnosis (PD). The frequency of asthma related acute care visits (ACVs)
2012. Five percent of the attended cases in the emergency room were hospi- in the 12 months prior to the outpatient visit was determined and a risk score
talized. The mortality from asthma around the country was 2.36 per million of calculated based on ACV type (ED/UCC visit=1 point, inpatient admission=2
patients covered by Social Security. The states with the highest mortality and points, PICU admission=3 points). The total risk score was used to create four
incidence of asthma were Yucatan and Campeche. Conclusions: The consulta- risk categories: Very Low (0 points), Low (1-2 points), Medium (3-6 points)
tions for asthma have increased nearly one third since 2007. The highest inci- and High (≥7 points). The odds of an asthma related ACV in the 12 months
dence of asthma was observed in the states located at the sea level. The rate of following the outpatient visit were then compared across risk categories using
visits to the emergency room and of hospital discharges showed a decreasing logistic regression. Results: Our study sample included 27,083 outpatient vis-
trend. The rate of mortality found in this report was low in relation to that found its representing 11,915 unique patients. Of these visits, 74% were Very Low
in other countries. risk, followed by approximately 19%, 6% and 1% for Low, Medium and High
risk, respectively. Eighty-two percent of High, 57% of Medium, 36% of Low
and 11% of Very Low risk patients had an asthma related ACV in the 12 months
following the outpatient visit. After accounting for clustering of visits by patient,
the odds of a future ACV was significantly higher for High risk (odds ratio
(OR)=36.8; p<0.001), Medium risk (OR=10.6; p<0.001) and Low risk (OR=4.5;
p<0.001) patients, when compared to Very Low risk patients. The odds of a
future ACV was significantly higher for High (OR=8.2; p<0.001) and Medium
(OR=2.4; p<0.001) risk patients, as compared to Low risk patients. High risk
patients had 3.5 times greater odds of having a future ACV than Medium risk
patients (p=0.001). Conclusion: This scoring algorithm effectively stratified
VOLUME 113, NOVEMBER, 2014 A21
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A22
ABSTRACTS: CONCURRENT SESSIONS
asthmatic patient risk for future asthma related ACVs. The potential utility
and scope of this model could be significant in the allocation of asthma resources
64
FINANCIAL AND MORBIDITY IMPACT OF ADDING TRECS TO
to those who need them most, particularly when access to detailed clinical
data is limited. NBS.
S.E. Henrickson*1, J. Heimall2, S. Jyonouchi2, 1. Haddonfield, NJ;
2. Philadelphia, PA.
63 Introduction: TREC based NBS identifies newborns with asymptomatic
NEWBORN SCREENING FOR SEVERE COMBINED IMMUN- SCID and allows HSCT with lower morbidity, mortality and cost. TREC NBS
ODEFICIENCY IN IOWA: RESULTS OF A ONE YEAR PILOT started in PA statewide July 2013, but hospitals can opt out. We review the cases
STUDY. of 4 PA born infants who recently presented: 2 via positive NBS and 2 who
S. Aleem*1, E. Phillips1, T. Henry1, C. Johnson1, P. Ferguson1, were born in hospitals not participating in TREC NBS and developed oppor-
S. Rumelhart1, C. Kremer1, K. Piper1, M. Fasano2, 1. Iowa City, IA; tunistic infections. Results: Patients identified by positive NBS: Pt 1: Outpa-
2. Des Moines. tient phenotyping showed T-B+NK- SCID; confirmed as X-SCID. Prophylac-
tically admitted for 9d due to sibling illness. Readmitted DOL26 for 48h for
Introduction: Early recognition of severe combined immunodeficiency unconditioned MRD PBSC transplant (PBSCT). Readmitted with emesis and
(SCID) is integral in the adoption of timely life-saving interventions, like blood streaked stools (15d), asymptomatic CMV and EBV reactivation (48h).
hematopoietic stem cell transplantation for an infant born with the disorder. Total admissions 28d. Now well day+106. Pt 2: Outpatient phenotyping demon-
Population-based, inexpensive, and sensitive newborn screening (NBS) for strated T+B-NK+; found to have RAG1 mutation. Admitted DOL120 for mye-
SCID involves measurement of T-cell receptor excision circles (TRECs) via a loablative conditioned UCB transplant (UCBT), hospitalized 39d, including
quantitative polymerase chain reaction (qPCR) assay. Here we summarize the transplant associated microangiopathy. Readmitted with fever (7d), poor weight
results of Iowa’s one year SCID NBS pilot program. Methods: A TREC qPCR gain (6d). Total admissions 52d. Now well day+175. Patients identified by
assay using DNA isolated from dried blood spots was developed by the State severe infections: Pt 3: Transferred from OSH at DOL154 with fevers,
Hygienic Lab and ran on all infants born in Iowa during the June 3, 2013-June pseudomonas UTI, pneumocystis pneumonia and CMV viremia. Found to have
31, 2014 pilot year. Samples with initial abnormal results were repeated and T-B+NK+ SCID; confirmed as X-SCID. Received unconditioned MMRD
immunophenotyping was performed on all infants with abnormal results. PBSCT at DOL167, hospitalized to day +8. 2 admissions for symptomatic CMV
Results: Of 43,930 infants screened, 13 were presumptive positive for SCID; viremia (20d), required CMV+ CTLs twice. Total admissions 41d. Now day+119
one remained indeterminate on repeat screening. Threshold for abnormal results with asymptomatic CMV viremia. Pt 4: At birth admitted to OSH NICU (14d).
was revised twice during the pilot. Of these 14 infants, 6 were identified in the DOL 18 admitted with ALTE and UTI (11d). DOL59 admitted with FTT/
first month of the pilot and 8 were identified after cut-offs were revised in chronic diarrhea, diagnosed with ADA SCID. During 221d admission, aspira-
February 2014; 10 (71%) were male, 8 (57%) were in an intensive care unit, 3 tion and pneumocystis pneumonia, chronic respiratory failure. Treated with
(21%) were Hispanic, 3 (21%) were infants of diabetic mothers and 2 (14%) PEG-ADA and developed autoreactive T cells. Received myeloablative condi-
had congenital heart disease. Immunophenotyping was without significant T- tioned UCBT DOL178. Total admissions 232d, with168d NICU/PICU. Now
cell lymphopenia ( CD3 < 1500 cells/ml, or absence/marked reduction in CD4 well at day+155. Conclusion: Patients identified with SCID via NBS are healthy
naïve T cells [CD4/CD45RA] < 5% of total CD3 T cells) in 11 infants, includ- at diagnosis and have shorter hospital stays with less morbidity and mortality.
ing one with 22q11.2 deletion syndrome. Significant T-cell lymphopenia was From 2000-2010, 11 SCID patients were identified at our institution. SCID
found in 3 (21%) infants; however, T-cell function (assessed as lymphocyte pro- diagnosis at < 3 m/o cost an average of $460K, diagnosis at >3 m/o cost an
liferation to phytohemagglutinin) was normal and none was found to have SCID. average of $1.5M. The cost of a single TREC screen is ~$4-5. With ~150K
Three infants with significant T-cell lymphopenia underwent additional testing babies born annually in PA, 1 SCID patient identified via NBS pays for a year
and clinical outcomes were monitored. One infant was diagnosed with Jacob- of screening. This supports the national inclusion of TRECs in NBS on a manda-
sen syndrome with associated cytopenias, one with 18p deletion syndrome and tory participation basis.
complex congenital heart disease and one with no causative genetic mutation
yet identified. Conclusion: In the first year of Iowa’s SCID NBS program no
SCID babies were identified; however, a variety of other conditions with T-
cell lymphopenia were found. This finding is similar to that of other states
reporting TREC NBS and may help to improve our understanding of other con-
ditions that present with T-cell lymphopenia.
A22 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A23
ABSTRACTS
PRESENTED AT POSTER SESSIONS
November 8-9, 2014
georgia world congress center
atlanta, georgia
TABLE OF CONTENTS
TOPIC ABSTRACT NUMBERS PAGES
Adverse Food and Drug Reactions,
Insect Reactions, Anaphylaxis P1 – P26 A25-A32
Aerobiology, Allergens, Allergen Extracts P27 – P38 A32-A35
Allergy Testing, Clinical Laboratory
Immunology P39 – P42 A35-A36
Asthma and Other Lower Airway Disorders P43 – P80 A36-A47
Basic Science Allergy and Immunology P81 – P93 A48-A50
Clinical Case Reports P94 – P207 A50-A84
Clinical Immunology, Immunodeficiency P208 – P242 A84-A93
Food Allergy P243 – P256 A93-A97
Immunotherapy, Immunizations P257 – P270 A97-A101
Other P271 – P284 A101-A104
Pharmacology and Pharmacotherapeutics P285 – P295 A104-A108
Rhinitis, Other Upper Airway and
Ocular Disorders P296 – P310 A108-A112
Skin Disorders P311 – P331 A112-A118
VOLUME 113, NOVEMBER, 2014 A23
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A24
ABSTRACTS: POSTER SESSIONS
A24 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A25
ABSTRACTS: POSTER SESSIONS
viduals or families. We present the case of a 7 year old girl with severe atopic
P1 dermatitis that was controlled with topical steroids and the soak and seal method.
A CASE OF SUCCESSFUL DESENSITIZATION TO ALGLU-
She had a history of multiple food reactions consistent with IgE mediated
COSIDASE ALFA IN A 7 WEEK-OLD WITH INFANTILE-ONSET food allergy. At 18 months, she ingested sweet potato, resulting in profuse vom-
POMPE DISEASE. iting that was diagnosed by her pediatrician as anaphylaxis. Methods: Skin
C. Adkins*1, C.M. Makris2, S. Kankirawatana2, 1. Hoover, AL; prick and ImmunoCapp testing was performed followed by a food challenge
2. Birmingham, AL. to sweet potato in an observed medical setting. Results: Skin prick testing
Introduction: Pompe disease (PD) is an inherited disorder caused by a defi- with commercial extracts revealed sensitivity to multiple foods including peanut,
ciency of the lysosomal enzyme alpha-1,4-glucosidase and characterized by tree nuts, milk, egg, shellfish and wheat but was negative to sweet potato. The
accumulation of lysosomal glycogen in many organs, including the heart and patient’s total serum IgE was 4504 kUA/L, and ImmunoCapp to sweet potato
skeletal muscle, leading to myopathy. Patients with infantile-onset PD can was 2.73. In comparison, her milk IgE was >100. Based on these results an oral
develop severe cardiomyopathy, which if left untreated, may result in death food challenge was performed. There was no immediate reaction (within 20
within the first year of life. A recent breakthrough treatment with recombinant minutes) to sweet potato given in increasing doses over 2 hours. One hour
enzyme replacement has significantly improved patients’ survival, but is often after the full serving, she began to vomit profusely, and continued to vomit over
complicated by the development of enzyme specific antibodies precluding fur- the following 3 hours, despite treatment with diphenhydramine, IM epineph-
ther administration. Here we report a case of successful desensitization to alglu- rine and IV ondansetron. IV fluid resuscitation was also performed. A com-
cosidase alfa in an infant who previously developed a systemic allergic reac- plete blood count obtained during the reaction revealed a significantly elevated
tion during enzyme replacement therapy. Methods: Specific IgE to alglucosidase neutrophil count of 17,100, compared to baseline of 2,800. She also had a nor-
alfa was obtained and reported to be negative. The patient underwent desensi- mal tryptase. These results are consistent with an FPIES reaction to sweet potato.
tization using our protocol starting approximately at a 1:10,000 dilution of the Conclusion: FPIES is generally considered in the differential diagnosis when
therapeutic dose, with doubling of the dose every 15 minutes until the cumu- infants and toddlers present with acute reactions to food ingestion, but not in
lative dose approximated the therapeutic dose (See Table 1). Results: Patient older children. This child posed a further diagnostic challenge given her con-
was a 7 week-old neonate with infantile-onset PD receiving weekly intravenous comitant IgE mediated food allergies to multiple foods. This unusual case, never
infusions of alglucosidase alfa at 20mg/kg. He developed a diffuse urticarial reported in the literature, demonstrates the potential for distinct pathogenic
rash, respiratory distress with wheezing, and periorbital and oral angioedema mechanisms in children with multiple food sensitivities. Physicians should con-
approximately 5 minutes into his 4th infusion. The following day, we proceeded sider in the differential diagnosis and be prepared to treat FPIES in any child
with desensitization. He developed two generalized cutaneous allergic reac- with a history of profuse vomiting after ingestion of certain foods.
tions during dose titration, but was able to complete the protocol. He was con-
tinued on dose escalation weekly and was eventually able to transition to his
former outpatient infusion protocol. Discussion: The incidence of anaphylaxis P3
from administration of this medication has been reported in the range of 1- ENZYME REPLACEMENT THERAPY: A CASE OF SUCCESSFUL
14%. It is unclear if these cases are truly IgE vs. non-IgE mediated. Our patient’s ELOSULFASE ALFA DESENSITIZATION IN A MORQUIO A
clinical history and cutaneous reactions during his desensitization suggest an SYNDROME PATIENT.
IgE mediated mechanism. The specific IgE blood sample was obtained within A. CaJacob*1, C. Adkins2, M. Descartes1, C. Allen1, J. Anderson1,
hours of his anaphylactic reaction and thus may have caused a false-negative 1. Birmingham, AL; 2. Hoover, AL.
result. We report our case to illustrate a protocol that was effective in inducing
Introduction: Morquio A Syndrome (also known as mucopolysaccharidase
temporary drug tolerance to alglucosidase alfa, allowing continuation of life-
type IVA deficiency) is an autosomal-recessive lysosomal storage disease char-
sustaining treatment for this patient.
acterized by a deficiency of the N-acetylgalactosamine-6 sulfatase enzyme.
Until the recent FDA-approval of elosulfase alfa (Vimizim™) enzyme replace-
Table 1: Alglucosidase alfa desensitization protocol
ment therapy (ERT) in February 2014, treatment of this progressive, multior-
gan disease had been symptomatic care. In pre-market clinical trials it was
determined to carry a 7.7% risk of anaphylaxis. We present a patient who was
successfully desensitized to elosulfase alfa after an anaphylactoid reaction.
Methods: An nine hour desensitization protocol was devised. We began with
an approximate initial dose of 1/10,000, with doubling of the dose until the
patient received her goal dose of 200mg. Results: A 54 year old female with
Morquio A syndrome began elosulfase alfa ERT in October 2013. She toler-
ated weekly infusions without difficulty until March 2014 when after approx-
imately 2.5 hours into her twenty-third infusion she developed a reaction char-
acterized by fever to 102.7, tachycardia, hypotension, wheezing and hypoxia
(O2 sat 75%). Reaction was treated with intravenous fluids, antihistamines,
nebulized albuterol and methylprednisolone. She was referred to the Allergy
service one week later for evaluation. Skin prick testing (patient and control)
was negative to 1:1, 1:10 and 1:100 dilutions with good histamine control. The
patient’s intradermal testing was positive at a 1:10 dilution. The control’s intra-
dermal testing was negative at 1:10 and 1:1 dilutions. One month after her
reaction, we proceeded with the above desensitization protocol. The desensi-
tization was well-tolerated. After its completion, the patient resumed her weekly
infusions at a slower rate without further reactions. Repeat skin testing four
months from initial desensitization was negative at 1:10 and 1:1 dilutions.
Conclusions: Vimizim™ is an FDA-approved ERT for Morquio A syndrome
patients which carries an anaphylaxis risk. The immunologic basis of our
patient’s anaphylactoid reaction is unclear, particularly given the fever and the
absence of any skin manifestations. After desensitization, she had conversion
P2 to negative skin testing. No antibody assay is currently available. To our knowl-
FOOD PROTEIN INDUCED ENTEROCOLITIS SYNDROME edge, this case represents the only elosulfase alfa ERT desensitization in pub-
(FPIES) TO SWEET POTATO IN A HIGHLY ATOPIC CHILD. lished literature.
B.J. Lanser*, N. Rabinovitch, Denver, CO.
Background: Food Protein Induced Enterocolitis Syndrome (FPIES) is a
rare, but increasingly prevalent non-immunoglobulin E (IgE) mediated gas-
trointestinal reaction to food proteins. It is outgrown in the majority of chil-
dren by 30 months of age, and does not show predominance for atopic indi-
VOLUME 113, NOVEMBER, 2014 A25
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A26
ABSTRACTS: POSTER SESSIONS
Vimizim™ Desensitization Protocol desquamation on her torso and arms. Her initial laboratory evaluation showed
WBC 21,700 cells/mm3, AEC 10,200 cells/mm3, normal C3 and C4. With three
days of systemic steroids, her AEC improved to 8650 cells/mm3. The edema
was not improved and she developed hepatic injury (AST 215, ALT 242, Alk
Phos 1201) with mild hepatitis suggested on ultrasound. Phenytoin and Lisino-
pril were discontinued as her picture was consistent with DRESS. She quickly
improved and was extubated 4 days following Phenytoin discontinuation. Dis-
cussion: Facial edema is common in DRESS however oropharyngeal and laryn-
geal involvement have not been described. Tongue edema has been reported
previously in a patient concomitantly on an ACE inhibitor, as was our patient.
This may implicate a synergistic effect of ACE inhibitors and DRESS presen-
tation. To our knowledge this is the first report of DRESS presenting with laryn-
geal involvement and intubation.
P4
FIRST STUDY OF PATTERN OF EPINEPHRINE AUTO INJEC-
TOR PRESCRIPTIONS FOR ANAPHYLAXIS IN A LARGE TER-
TIARY CARE HOSPITAL IN SAUDI ARABIA.
S. Al Gazlan*, R. Amin, A. Khaliq, T. Al Otaibi, S. Alhashim, F. Sheikh,
Riyadh, Saudi Arabia.
Anaphylaxis is a serious allergic reaction that may cause death. The pres-
ent study examined the symptoms, triggers and demographic patterns of patients
treated for anaphylaxis at a large tertiary care hospital in Riyadh, Saudi Ara-
bia. The protocol was approved by the Institutional Review Board of the hos-
pital. All the patients who were prescribed Epinephrine auto-injectors ( EA )
between 1/1/2010 and 31/12/2011 were included in this study. 238 new patients
were identified using hospital pharmacy database and the medical records of
these patients were reviewed. To date, Epinephrine auto-injectors ( EA ) are
available at very few hospitals in Saudi Arabia. Since our hospital is the main
tertiary care hospital with allergy&immunology service in the Kingdom, these
data may reflect Anaphylaxis presentations in our region. The mean age at the
time of first EA prescription was 22.9 years, (2years to 73 years). SD +/- 18.2
Female to male ratio was 52:48. 54% for subjects were less than 18 years of
age. 18 % were Non Saudis living in the Riyadh region. Most of these were
employees of the hospital or their dependents. Although most of the signs and
symptoms were similar to other published data, there were some differences
observed in our population. Urticaria and angioedema was the most common
presentation accounting for 70% in adults and children followed by shortness
of breath in 33% in adults and 23% in children. Food was the commonest trig-
ger for anaphylaxis with Tree Nuts and Egg the most frequent, followed by
Sesame and Peanut. Drug Allergy was also a common trigger, with Penicillins
and NSAIDs being the commonest. Regarding Insect allergy, Samsum Ant was
the commonest trigger in our population. This is the first such study on Ana-
phylaxis in Saudi Arabia. While there are many similarities, some of the pre-
senting signs, symptoms, and triggers of anaphylaxis are significantly differ-
ent in our population than in others. While treating Anaphylaxis, we should be
mindful of these differences. This improved understanding should help reduce
the morbidity and mortality associated with Anaphylaxis in our region.
P6
PEANUT IGE THRESHOLD FOR REFLEX PEANUT COMPO-
P5 NENT TESTING.
PHENYTOIN INDUCED DRESS PRESENTING WITH LARYN- M. Altrich*1, H.D. Wells1, J.C. Thompson2, 1. Lee’s Summit, MO;
GEAL EDEMA REQUIRING INTUBATION. 2. Atlanta, GA.
H.N. Hartman*, L. Gimenez, Milwaukee, WI. Introduction: Patients with suspected peanut allergy (PA) come to medical
Introduction: DRESS is a severe and potentially fatal drug reaction char- attention following an adverse food reaction or in the course of in vivo or in
acterized by fever, rash, lymphadenopathy and visceral organ damage. We vitro testing. An IgE level of 15 kU/L or above has been suggested as 95%
describe the case of a patient with Phenytoin induced DRESS presenting as likelihood of PA, however the majority of patients sensitized to peanut have an
eosinophilia and laryngeal edema. Case Report: The patient is a 59 yo AA IgE level below this cut off. As some patients avoid peanut after initial symp-
Female with Hypertension, Type 2 Diabetes, Hyperlipidemia, Hypothyroidism toms, a negative history of systemic reaction to peanut has uncertain predic-
and a history of Cerebral Vascular Event and subsequent seizure. She has no tive value. This creates a diagnostic dilemma for clinicians who wish to rec-
history of previous angioedema. Her home medications include alendronate, ommend avoidance, consumption or the option of a food challenge. At what
atorvastatin, cholecalciferol, folic acid, insulin, levothyroxine, lisinopril, omepra- lower limit of peanut IgE should component testing be considered? Peanut com-
zole and phenytoin which was initiated 2-3 months prior. Initially she presented ponent testing provides a more certain decision point; sensitization to peanut
to the ED for fever and an urticarial and maculopapular rash on her neck, chest seed storage proteins (SSP), Ara h 2 in particular, correlates well with symp-
and abdomen. She was placed on antimicrobial therapy for presumed UTI for tomatic peanut allergy. Based on food challenges, Codreanu proposed an IgE
which she took for two days before returning to the ED with worsening rash threshold for Ara h 2 of 0.23 kU/L for identifying peanut allergic subjects, Nico-
and desquamation. At this evaluation she was given oral prednisone burst. laou and Custovic proposed 0.35 kU/L as a threshold. This study considers the
Five days following completion of steroids she again presented to the ED with peanut IgE level that may be used as a decision point for reflex component test-
fever and facial edema. She was emergently intubated by ENT for oropharyn- ing. Methods: This prospective study utilized sera with de-identified patient
geal edema. She was started on Dexamethasone 8mg q8 for edema and a CT health information. Samples from 25 peanut sensitized subjects, age 12 years
obtained demonstrated extensive angioedema of her tongue and larynx with and younger with specific IgE 0.35-15 kU/L, were assayed for peanut SSP Ara
cervical lymphadenopathy. On exam she had no rash, but was noted to have h 1, Ara h 2, Ara h 3, for PR-10 Ara h 8, and lipid transfer protein (LTP) Ara
A26 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A27
ABSTRACTS: POSTER SESSIONS
h 9. Results: 76% of the subjects were sensitized to peanut SSP, 56% to Ara h mumab (Humira) for his RA 7 wk & 1 wk before the rash started. On presen-
2, 20% were sensitized to PR-10, Ara h 8 and 12% to LTP, Ara h 9. Ara h 2 of tation, his VS & PE were normal except for generalized ulcerated bullous pus-
at least 0.35 kU/L was seen at the lowest extent of the peanut IgE data set. In tular eruption without facial or mucous membranes involvement. Lab findings:
one sample a value for Ara h 2 of 0.44 kU/L corresponded to a peanut IgE of WBC 23000 with 95% N, ESR 81mm/hr, CRP 45mg/dl & normal CMP. Lesion
0.41 kU/L. Within the complete data set it was not possible to predict sensiti- smear showed neutrophils with negative culture & no fungi or AFB. Blood
zation to Ara h 2 or SSP based on peanut IgE as the profile may contain IgE culture was also negative. He was treated with hydrotherapy, wound care, and
to SSP or cross-reactive proteins. Conclusions: There is not a lower peanut IV methylprednisolone 60mg daily & diphenhydramine 25mg q 6 hr. Biopsy
IgE threshold for component testing and it is not possible to predict the com- showed dermal microabscesses & leukocytoclastic vasculitis consistent with
ponent profile based on the peanut IgE alone. Peanut IgE values <15 kU/L may pyoderma gangrenosum (PG). Methylprednisolone was increased to 1 g daily
be associated with values of Ara h 2 exceeding peanut challenge decision points. for 5 d then switched to PO prednisone 60 mg daily. Further evaluation showed
Component testing has improved in availability and affordability. Medical deci- positive ANA with no specific pattern, and negative RF, CCP, Ds-DNA, anti-
sion-making based on the component profile allows a more accurate risk assign- Smith Abs, ANCA & PSTPIP1 mutation. Serum & urine electrophoresis and
ment than decisions based on peanut IgE alone. C3 & C4 were normal. Serum Humira Abs (IgG) was 15.8 U/ml. The rash grad-
ually improved until completely resolved over 3 wk while prednisone was being
gradually tapered to 20 mg daily on discharge. Conclusion: PG was diagnosed
P7 based on biopsy & negative workup for other bullous pustular disorders. Humira
UTILITY OF PATCH TESTING IN FIXED DRUG ERUPTION. was the most suspect because it was the most recent medication received, ele-
D.A. Cariño Cartagena*, A.A. Velasco-Medina, J.C. Fernández de vated serum Humira IgG Abs, and resolution while on all his other medica-
Córdova-Aguirre, S. González-Flores, M.E. Arroyo-Cruz, G. Velázquez- tions. This may be the first reported PG case caused by Humira. PG is uncom-
mon neutrophilic dermatosis affecting mainly young adults; > 50% of cases
Samano, Mexico City, DF, Mexico.
have an associated systemic inflammatory disease (e.g., IBD, hematologic or
Introduction: Fixed drug eruption is characterized by the sudden onset of rheumatologic). Most patients achieve remission on immunosuppressants but
a single or few circular macular erythematous-violaceous lesions, that could relapse can occur.
happen in a specific location repeatedly after exposure to a particular drug in
85 to 100 % of cases; drugs most often involved are sulfonamides, NSAIDs,
tetracyclines, paracetamol, anticonvulsants and other anecdotal drugs as anti-
fungal. There are five clinical forms: a) classic characterized by an asymmet-
P9
AN UNUSUAL PRESENTATION OF DRESS SYNDROME IN A
ric and erythematous pigmented shape b) symmetrical form with erythema-
POST-TRANSPLANT PATIENT: A CASE REPORT.
tous unpigmented plaques, c) is minor or individual lesion, d) Disseminated
bullous form, e) linearly. The responsable drug was identified through patch S.B. Sindher*, J. Heimall, Philadelphia, PA.
test. Case Presentation: Thirty eight years old female presents multiple slim, Introduction: Drug reaction with eosinophilia and systemic symptoms
erythematous, assymetrical lesions 24 hours after treatment with Trimethoprim (DRESS) is a severe acute drug reaction with a highly variable clinical pres-
- Sulfamethoxazole located in the back with regular discoid margins with slow entation. It is characterized by a polymorphic skin eruption associated with
progressive involution. After suspension of TMP-SMZ exposure the patient fever, eosinophilia, lymphadenopathy and the involvement of multiple organs
preserved a lesion in the calf with residual pigmentation. She had a history of (liver, kidney and lung) along with a long latency (two to eight weeks) between
previous similar episodes with unspecified drug exposure, 6 weeks later fixed drug exposure and disease onset. Methods: We evaluated a 14-year-old boy
drug eruption by TMP-SMZ was confirmed with patch testing. Discussion: with history of allogenic peripheral blood stem cell (PBSC) transplant for acute
Fixed drug eruption has a better prognosis than other drug induced skin lesions myelogenous leukemia (AML). He presented to Allergy clinic for evaluation
and is considered a form of delayed hypersensitivity mediated by T cells CD8 of rash and eosinophilia. Results: The patient received a matched unrelated
+, the disease could determine important physical and psychological impair- donor PBSC transplantation for high-risk AML 7 months prior to his presen-
ment due to discomfort and cosmetic appearance, thereby physicians should tation. He had history of chronic skin graft-versus-host disease requiring long-
be alert of this possibility to avoid subsequent recurrent episodes. The litera- term therapy with prednisone. Daily medications also included lisinopril, acy-
ture indicates that patch testing is less dangerous than oral challenge to iden- clovir, cetirizine, vitamin D, omeprazole and sulfamethoxazole/trimethoprim.
tify the responsible drug with positivity of 23.6% to 20%, which proved effec- After 6 months of therapy, prednisone was slowly weaned to a physiologic dose
tiveness in the presented case, thereby this diagnostic tool should be considered of hydrocortisone. Within a week of stopping prednisone he developed inter-
as a first step approach for fixed drug eruption. mittent low-grade fevers and an erythematous and pruritic rash on his legs that
progressively worsened despite treatment with topical triamcinolone 0.1% oint-
ment and oral diphenhydramine. Over a period of 2 months he had 3 hospital
admissions for work-up of fever and worsening rash. Blood cultures were neg-
ative. During his 3rd admission new-onset eosinophilia and worsening
transaminitis were noted. Based on these findings he was diagnosed with
DRESS. Therapy with sulfamethoxazole/trimethoprim was stopped and he
received 7 days of prednisone resulting in improvement of his rash. Within a
few days of completing the prednisone course he developed recurrence of his
fever and rash and was readmitted. A skin biopsy confirmed a drug reaction.
He was initiated on a 3-month course of prednisone with complete resolution
of his symptoms. Conclusions: Our case report highlights the difficulty of diag-
nosing DRESS syndrome. Though the syndrome is known for its long latency
between exposure and symptom onset, the diagnosis and symptoms in our
P8 patient were likely initially masked by his chronic prednisone use.
UNUSUAL SEVERE RASH CAUSED BY ADALIMUMAB.
A.A. Mourad*, S.L. Bahna, Shreveport, LA. P10
Introduction: Rashes are common in patients receiving multiple medica- SUCCESSFUL MYCOPHENOLATE MOFETIL DESENSITIZA-
tions. Most rashes are benign but some can be life-threatening and require TION IN A DOUBLE HEART-KIDNEY TRANSPLANT RECIPIENT.
urgent identification & discontinuation of the culprit which can be difficult.
Case: A 49-y-o AA man was transferred from another hospital because of severe M.A. Smith*1, A. Gonzalez-Estrada2, E. Glancy2, D. Fernandez2,
generalized rash started 2 wk earlier as pustules on legs then spread as bul- A. Subramanian2, 1. South Euclid, OH; 2. Cleveland, OH.
lous-pustular all over his body except the face; accompanied by on-off fever Introduction: Mycophenolate mofetil (MMF) is increasingly being used in
up to 101F. He did not improve on TMP/SMX & rifampicin or on IV van- place of azathioprine in organ transplantation, as it is associated with less
comycin, piperacillin-tazobactam & prednisone 20 mg daily. Review of sys- bone marrow suppression, fewer opportunistic infections, and a lower incidence
tems revealed HTN, RA, gout, obstructive sleep apnea & peptic ulcer; on of acute rejection. MMF, a purine nucleotide analogue, blocks lymphocyte pro-
amlodipine, olmesartan, aliskiren, nebivolol, clonidine, methotrexate, allop- liferation by inhibiting guanine nucleotide synthesis in lymphocytes. Methods:
urinol, modafinil, pantoprazole, iron and folic acid. He was started on adali- A case report Results: A 46-year-old African-American female with systemic
VOLUME 113, NOVEMBER, 2014 A27
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A28
ABSTRACTS: POSTER SESSIONS
lupus erythematosus (SLE) induced dilated cardiomyopathy and end stage renal
disease underwent double heart-kidney transplant. Following the transplant the
P12
CATAMENIAL ANAPHYLAXIS: A RARE CASE.
patient was placed on azathioprine, tacrolimus and methylprednisolone. MMF
was not included in her immunosuppressive regimen due to a previous episode N. Kharod*1, M. Sands2, 1. Orchard Park, NY; 2. Buffalo, NY.
of oral pruritus within minutes after the first dose for lupus nephritis approxi- Introduction: Catamenial anaphylaxis, a.k.a. cyclical anaphylaxis, is char-
mately 10 years ago. A second trial of MMF three weeks after the first resulted acterized by recurrent episodes of serious, possibly fatal, multisystem allergic
in urticaria, pruritus and angioedema. MMF was discontinued and her symp- reactions occurring at the time of menstruation. It is an uncommon clinical
toms subsided within 3 days.Allergy and Immunology was consulted to evalu- entity with few reports. Presentation: A 38-year-old Caucasian female patient
ate for possible reinitiation of MMF. Skin testing to MMF was performed, how- with recurrent anaphylaxis: abdominal cramping, diarrhea, injection and
ever the patient had a blunted response to the histamine control. Given the urgency swelling of the eyes, nasal congestion, wheezing, respiratory distress, throat
of the situation and inability to interpret our skin tests, we designed a novel 12- closing. First episode occurred while she was working at a breakfast restau-
step desensitization protocol (Table I) adapted from current Drug practice param- rant. She had worked there on and off for 4 years previously without any such
eters1. In an intensive care unit setting, an oral desensitization with MMF was issues. Continued to have recurrent episodes x 2 over the next three months,
performed with diphenhydramine 25 mg IV and famotidine 20 mg IV given as then every 4 weeks. Each time, the episodes resolved with oral antihistamine.
premedications. She completed the desensitization without adverse reactions. The patient never used epinephrine and never sought medical attention after
Conclusion: The use of MMF has become standard practice in many solid organ the episodes. No identifiable food or medication triggers. CBC and CMP within
transplant recipients due its efficacy and favorable risk profile compared to other normal limits. RAST IgE positive for dog, cat, ragweed, total IgE 179. Base-
immunosuppressants. There has been a single case report of successful MMF line tryptase normal at 3.2; did not get acute tryptase drawn. No prior medical
desensitization2. However, this protocol did not follow current Drug practice history other than asthma and allergic rhinitis. On questioning, patient noted
parameters and was done over a three-day period. We report a successful desen- that she had very good control of asthma symptoms except during her peri-
sitization to MMF in a double heart-kidney transplant recipient. menstrual period, when she would have wheezing and dyspnea on otherwise
normal exertion. Patient also noted that all anaphylactic episodes were occur-
Table I. Mycophenolate Mofetil Oral Desensitization ring on/around Day 1 of menses and that she was completely asymptomatic in
between. Patient was successfully treated with hormonal suppression of menses.
Discussion: Catamenial anaphylaxis is a rare, possibly underdiagnosed clini-
cal condition. It is a diagnosis of exclusion which can be identified after an
appropriate evaluation, and when conditions such as mastocytosis and C1-
esterase inhibitor deficiency/dysfunction have been ruled out. No obvious patho-
genesis identified, but possible theories include hypersensitivity to proges-
terone, hypersensitivity to estrogen, prostaglandins in menstrual fluid. There
is no one universal method of treatment, as several of these pathways require
different interventions.
P13
TREE NUT ALLERGY AND ANAPHYLAXIS: A CASE OF
DELAYED DIAGNOSIS.
S. Joychan*1, K. Dass2, 1. Kalamazoo, MI; 2. Chicago, IL.
P11 Anaphylaxis is an acute, potentially life-threatening systemic hypersensi-
AMPHOTERICIN DESENSITIZATION. tivity reaction, resulting from exposure to an allergen. Classically, this occurs
A. Ravi*, D. Maddox, Rochester, MN. when an individual is exposed to an allergen, leading to sensitization and sub-
Rationale: Although rare, amphotericin adverse reactions may occur. Meth- sequent exposures result in an immunologic response. A 22-year-old female
ods: Report of a case and review of the literature. Case Presentation: A 39 year with a history of polysubstance abuse presented with anaphylaxis. The patient
old male with disseminated cryptococcus meningitis infection after exposure had a history of frequently presenting to the emergency room (ER) with vague
to deceased birds and feces presents with rash. His only new medications were complaints of abdominal pain, nausea, and vomiting usually after meals. No
flucytosine and liposomal amphotericin. The rash presented as itchy, slightly cause had been found for her symptoms, which were attributed to drug-seek-
raised, diffuse erythema most consistent with an urticarial lesion on bilateral ing behavior. She presented to the ER one day prior to admission with mild
knees on Day 7 of antifungal therapy. No lip/tongue swelling, difficulty breath- uvular swelling, tachycardia, diffuse urticaria, and voice hoarseness. Her symp-
ing, abdominal pain, or vomiting. No oral ulcers or skin peeling. Flucytosine toms were attributed to an allergic reaction of unknown etiology. She was given
was continued and liposomal amphotericin was held to help further determine intravenous (IV) methylprednisolone, IV famotidine, IV diphenhydramine, and
the causative agent. On Day 8 of antifungal therapy, he tolerated flucytosine. two doses of intramuscular (IM) epinephrine. The patient was monitored and
The rash was nearly resolved. On Day 9, flucytosine was continued and lipo- discharged when symptoms resolved. The next day, she presented again with
somal amphotericin re-initiated. 1 hour into liposomal amphotericin infusion, dyspnea, nausea, and urticaria after consumption of garlic bread. She reported
he developed a similar rash on bilateral knees. Thirty minutes after the infu- “outgrowing” a childhood peanut allergy. She also reported having recently
sion, he developed chest tightness lasting 30 minutes. On Day 10, he under- started working at an Italian restaurant but denied workplace exposure to
went liposomal amphotericin desensitization with an initial concentration of 1 peanuts. She was unaware of any new exposures. IV methylprednisolone, IV
ng/ml infused at 1.67 ml/min rate with 3 fold increments in concentration every famotidine, IV diphenhydramine and IM epinephrine were given, in addition
30 minutes for a cumulative dose of 300mg. There were a total of 14 incre- to aggressive IV hydration. Tree nut panel confirmed allergy to almond, Brazil
ments. 4 hours after completing the desensitization, he developed a similar rash nut, cashew, coconut, hazelnut, macadamia nut, pecan, pine nut, pistachio,
on his bilateral knees, left calf, and right foot. On Day 11, rash was nearly peanut, sweet chestnut, and walnut. Upon further questioning, the patient noted
resolved. On Day 11 evening, he underwent a conventional amphotericin (with- pine nuts on her garlic bread. All other allergy tests were negative. The patient
out liposomal component) desensitization with a similar protocol except to a received extensive counseling regarding her allergies and risk for anaphylaxis.
cumulative dose of 0.7mg/kg (54mg). There were a total of 10 increments. She was provided with a prescription for an epinephrine auto-injector and rec-
Results: He was successfully desensitized to conventional amphotericin B after ommended to follow up with an allergist outpatient. This case demonstrates the
failing desensitization with liposomal amphotericin. Discussion: Amphotericin importance of taking a detailed allergy history and performing a thorough exam-
is the drug of choice for treatment of severe invasive fungal infections. The ination when presented with a case of anaphylaxis. Clinicians should be con-
use of liposomal amphotericin has increased given the less adverse side effects. scientious about recognizing vague symptoms that might precede an allergic
In review of the literature, there was a case of a child who had urticaria to lipo- reaction. This case also highlights the importance of differentiating signs and
somal amphotericin but tolerated conventional amphotericin. In patients who symptoms related to a patient’s substance abuse from similar symptoms that
adversely react to liposomal amphotericin, one may consider desensitization can represent a true allergic reaction.
to conventional amphotericin B, as the patient may be reacting to the liposo-
mal component or to an epitope array of amphotericin that only gets presented
by a liposomal formulation.
A28 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A29
ABSTRACTS: POSTER SESSIONS
P14 P15
POSITIVE PATCH TEST TO LAMOTRIGINE IN A PEDIATRIC TREATMENT OF DRUG REACTION WITH EOSINOPHILIA AND
PATIENT WITH DRESS SYNDROME. SYSTEMIC SYMPTOMS (DRESS) WITH MYCOPHENOLATE
J.A. Mendez*, C. Acantilado, S. Nazario, San Juan, Puerto Rico. MOFETIL AS A STEROID-SPARING AGENT.
Introduction: Drug reaction with eosinophilia and systemic symptoms M. Mortezavi*, J.M. Lomas, R.J. Looney, Rochester, NY.
(DRESS) is a rare and life threatening delayed hypersensitivity reaction caused Introduction: Drug reaction with eosinophilia and systemic symptoms
by exposure to certain medications. However, identification of the culprit drug (DRESS) is a drug-induced hypersensitivity reaction that includes skin erup-
may be challenging, particularly in patients receiving multiple medications. tions, eosinophilia, lymphocytosis, lymphadenopathy and internal organ involve-
Patch testing is a well-known method used to identify the culprit drug in delayed ment. First line therapy includes high dose corticosteroids, however, patients
Type IV hypersensitivity reactions. Here, we report the case of a pediatric patient with DRESS often require a slow, prolonged taper to prevent relapse. Here, we
in whom lamotrigine-induced DRESS syndrome was successfully confirmed describe the case of a patient with DRESS effectively treated with mycophe-
through patch testing. Case description: A 5 year-old boy with epilepsy had nolate mofetil as a steroid sparing drug. Case Presentation: Our patient is a
been receiving valproic acid for over 1 year to control seizures. He had per- 14-year-old white female, previously in good health. She developed a cough,
sisted with symptoms despite medical therapy and a follow-up electroen- malaise and sore throat treated at home with ibuprofen and pseudoephedrine.
cephalogram (EEG) still revealed abnormal electrical activity. A decision was Her father also gave her one dose of amoxicillin left over from an old pre-
made to change his antiepileptic therapy to lamotrigine 125mg daily. Two weeks scription. A few days later her symptoms subsided. Four weeks after the onset
after starting therapy with lamotrigine, the patient experienced the sudden onset of the initial illness, she developed a flat pink rash, joint pains, fever, and cer-
of fever of 103° F and a diffuse maculopapular skin rash. Laboratory workup vical lymphadenopathy. Her symptoms continued to escalate until she became
was remarkable for an elevated eosinophil count of 0.86x109/L. A hypersensi- lethargic, had altered mental status and dyspnea. She was brought to the hos-
tivity reaction to lamotrigine was suspected and the medication was stopped pital hypotensive and required intubation. A CT scan revealed diffuse cervi-
immediately. A complete resolution of symptoms was observed after 2 weeks. cal, axillary, hilar, intra-abdominal, pelvic mesenteric and inguinal lym-
He was referred to our clinics due to suspected drug allergy. Patch testing was phadenopathy. She had leukocytosis of 80 K/ml, 20% bands, eosinophilia of
performed to lamotrigine 30% in water and in petroleum jelly. Patch test read- 28 K/mL, lymphocytosis 29 K/mL, acute hemolytic anemia, thrombocytopenia,
ing at 72 hours revealed a positive result to lamotrigine in water. Conclusion: elevated creatinine, ferritin of 5500 ng/ml, and sIL2R 79,000 pg/ml. A bone
Patch testing of medical products is a useful tool in the evaluation of patients marrow and lymph node biopsy showed no evidence of hemophagocytosis or
with delayed Type IV hypersensitivity drug reactions. In this case, patch test- malignancy. Workup for lupus, vasculitis, and infection was negative. She was
ing was successfully used to confirm lamotrigine-induced DRESS syndrome diagnosed with DRESS. She received 1gm IV steroids for three days with
in a pediatric patient with epilepsy. remarkable recovery of pulmonary, renal and hepatic function and normaliza-
tion of labs. She was transitioned to oral prednisone at 1mg/kg and started on
mycophenolate mofetil 500 mg bid before discharge. Her steroid dose is tapered
without relapse. Conclusion: DRESS is characterized by a profound immuno-
logic response involving overproduction of multiple cell lines including T-cells,
B-cells, eosinophils and production of abnormal antibodies. Mycophenolate
mofetil is a non-competitive inhibitor of inosine monophosphate dehydroge-
nase that inhibits T and B Cell proliferation. To our knowledge, this is the first
described case of using this agent to successfully treat a patient with DRESS.
P16
PREVALENCE OF ALLERGY TO HYMENOPTERA STING
AMONG SCHOOLCHILDREN IN MONTERREY, MEXICO.
H. Hernandez-Sanchez*, A. Arias Cruz, S.N. Gonzalez Díaz, L. Leal
Villarreal, M. Hernandez Robles, J.A. Buenfil Lopez, I.V. Yanez Perez,
Monterrey, Nuevo Leon, Mexico.
Background: Hymenoptera stings can cause allergic reactions in individu-
als sensitized to their venom. There is few epidemiological data on the preva-
lence of this type of allergy in children in México. The aim of this study is to
know the prevalence of Hymenoptera sting allergy in school children of Mon-
terrey, Mexico. Method: We conducted a transversal and observational study
where hymenoptera allergy was surveyed among children attending to ele-
mentary school. The study was divided into two phases. First phase consisted
in design and validation of a questionnaire to survey hymenoptera allergy. In
the second phase, questionnaire was applied to parents whose children attended
to any of the different elementary schools of the city. Finally, questionnaires
were collected and submitted to analysis. The clinical reactions and epidemi-
ological characteristics to ant bites, bee and wasp were investigated. Allergy to
hymenoptera sting was correlated with personal history of atopy. Results: A
total of 323 questionnaires were completed and selected for analysis. The age
of the students ranged from 5-13 years (mean 9.6 ± 21) and 162 (50.2%) were
female. Ninety-three children (28.8%) had a personal history of atopy and 23%
had some clinical suspicion of atopy. Of the total sample, 217 children (67%)
had a history of at least one wasp sting. The 10.5% of children had large local
reactions and 6.5% systemic reactions. Anaphylaxis occurred in 0.9% of the
children. We found no significant difference in the prevalence of allergy to
Positive patch test to lamotrigine 30% in water at 72 hours. Hymenoptera between atopic and non-atopic subjects (p = 0.09). Conclusions:
The prevalence of large local reactions and systemic reactions found in this
study was similar to what has been reported by other authors. However, the
prevalence of anaphylactic reactions was lower than what has been reported in
other epidemiological studies in the pediatric population.
VOLUME 113, NOVEMBER, 2014 A29
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A30
ABSTRACTS: POSTER SESSIONS
angioedema of her face and fingers. The patient had no other systemic symp-
P17 toms. The medication was discontinued and the patient responded to oral pred-
SUCCESSFUL MEROPENEM CHALLENGE IN A PATIENT WITH
nisone and hydroxyzine. After a few weeks, her cardiologist started her on a
FULMINANT PIPERACILLIN-INDUCED IMMUNE HEMOLYTIC different beta blocker (carvedilol). The patient had a similar cutaneous reac-
ANEMIA. tion with angioedema on the third day without anaphylaxis, again responding
B. Prince*, A. Peters, Chicago, IL. to prednisone and hydroxyzine. Results: We believed her cutaneous reactions
Introduction: Drug induced immune hemolytic anemia (DIIHA) is a rare were not IgE-mediated; rather they were T-cell mediated, occurring within a
but often severe cause of hemolysis that was first described in the 1950’s. Cur- few days of the initiation of two beta blockers. There are no validated skin test-
rently, there are more then 125 different drugs known to cause DIIHA with ing or in vitro serum testing assays available for proving beta-blocker sensi-
cephalosporin and penicillin antibiotics being the most common agents. A diag- tivity. We empirically suggested the patient start a low dose beta-blocker under
nosis of DIIHA is made by a clinical history of drug associated hemolysis and cover of oral cyclosporine in an attempt to abrogate the cutaneous reaction.
positive serologic testing. Once DIIHA is identified, the causal drug should be With the reinitiation of carvedilol the patient developed no rash, dermal pru-
discontinued, and avoidance of similar classes of medications is generally rec- ritus, or angioedema. After two months the cyclosporine dose was slowly
ommended since the cross reactivity between related medications is not well tapered, the carvedilol dose was escalated, and such was well tolerated. After
established. Methods: Case Report Results: A 43 year old female with cystic 6 months, we recommended that the patient discontinue the low dose
fibrosis (CF) and a history of life-threatening, piperacillin-induced immune cyclosporine (25 mg twice daily) while continuing the carvedilol (12.5 mg twice
hemolytic anemia was hospitalized with worsening productive cough and short- daily), but the patient relocated to Europe prior to dose changes. Conclusions:
ness of breath refractory to tobramycin, aztreonam, and azithromycin. Sputum Cyclosporine has been used off-label for the treatment of various inflamma-
cultures were notable for persistent pseudomonas aeruginosa infection sensi- tory and autoimmune skin conditions. This is a prime example of successful
tive to piperacillin/tazobactam (PT) and meropenem (MP); however, two years use of cyclosporine to prevent a drug-induced skin reaction. Further studies
prior to admission, the patient developed severe hemolytic anemia with her need to be performed to evaluate the efficacy of cyclosporine in T cell-medi-
hemoglobin reaching a nadir of 2.7gm/dL 5 days after starting PT. Laboratory ated, drug-induced allergic dermatoses, wherein the use of such drug is deemed
evaluation at that time was significant for an elevated LDH and bilirubin, an necessary.
undetectable haptoglobin, and a strongly IgG positive DAT. The patient was
admitted to the ICU and required multiple blood transfusions but improved
within a few days of stopping PT. Given the patient’s history of DIIHA to P20
piperacillin and serious nature of her current CF exacerbation, MP was deemed IN VITRO CHARACTERIZATION OF A DELAYED HYPERSEN-
medically necessary for treatment, and informed consent was obtained. A 16 SITIVITY REACTION TO DOCETAXEL USING GENE EXPRES-
day graded dose challenge was performed starting at 1mg IV to a goal dose of SION PROFILING IN A PATIENT WITH STAGE 3 BREAST CAN-
2 grams IV q8hrs without any evidence of hemolysis. The patient has contin- CER.
ued to tolerate subsequent courses of MP without any adverse events. Con- T. Kelbel*, F. Ishmael, Hershey, PA.
clusion: This is the first known report of a patient with a history of piperacillin-
induced immune hemolytic anemia tolerating meropenem through a cautious Introduction: The diagnosis of T-cell mediated drug hypersensitivity reac-
graded dose challenge. tions is challenging due to lack of sensitive and specific assays. We describe a
case of delayed hypersensitivity reaction to docetaxel and use of an in vitro
assay using T-cell gene expression response to characterize the reaction and
P18 preemptively test navelbine as a safe, alternative chemotherapy treatment. Patient
History: A 59 year old woman with stage 3 breast cancer developed whole body
NSAIDS ARE THE MOST COMMON CAUSE OF DRUG INDUCED
erythematous rash shortly followed by desquamation about 24 hours after
ANAPHYLAXIS AT A VILNIUS UNIVERSITY HOSPITAL.
cyclophosphamide and docetaxel treatment. It was not clear whether the reac-
A. Blaziene1, N. Buterleviciute1, V. Paltarackiene1, K. Linauskiene1, tion was caused by cyclophosphamide or docetaxel. Methods: An in vitro T-
L.M. DuBuske*2, 1. Vilnius, Lithuania; 2. Gardner, MA. cell assay was used to quantify gene expression changes in a panel of cytokines
Background: Anaphylaxis is a life threatening condition. NSAIDs a most and inflammatory mediators (IL-2, -4, -5, -6, -8, -10, -13, -17a, GM-CSF, TNF-
common pain relief medicine, may induced anaphylaxis. Methods: 70 patients α, CCL2, IFN-γ, Fas ligand) when exposed to docetaxel and cyclophosphamide.
(38 women (54.3%) and 32 men (45.7%) with anaphylaxis hospitalized in a Additionally, her oncologist requested navelbine be preemptively tested as it
Vilnius University Hospital from 2009 to 2012 were assessed. The mean age would be indicated as her next chemotherapeutic option. Results: In vitro test-
of patients was 47.31 ± 17.63 (range 20-83) years old. A total of 26 patients ing showed significant elevation of T-cell response of IL-6 and CCL2 to doc-
with drug-induced anaphylaxis were included in this study. The causes, symp- etaxel compared to cyclophosphamide and navelbine (Figure). These results
toms and diagnosis of anaphylaxis were analyzed using WAO criteria. Results: suggest that the reaction was a type IVa delayed hypersensitivity reaction to
NSAIDs were the main suspected cause of anaphylaxis for 10 (38.5%) patients. docetaxel. The patient was successfully treated with navelbine and cyclophos-
Other triggers of anaphylaxis were antibiotics (30.8%), local anesthetics (3.8%) phamide and is currently in remission. Conclusion: In vitro T-cell response test-
and other drugs (26.9%). 9 cases of NSAIDs induced anaphylaxis fulfilled the ing may be used to characterize docetaxel allergy while also predicting the
second WAO criteria for anaphylaxis diagnosis and 1 met the third criteria. absence of a type IVa reaction to navelbine. This is a novel approach to
90.0% of patients had cardiovascular symptoms, 70.0% had skin symptoms, chemotherapeutic drug reactions with significant clinical application poten-
60.0% had respiratory symptoms and 40.0% had gastrointestinal symptoms. tial. Nevertheless, more research is needed before mainstream application.
One patient experienced NSAID induced anaphylaxis twice. Provocation tests
were performed and safe alternative NSAIDs were chosen for 2 patients. Con-
clusion: Drug induced anaphylaxis was most commonly induced by NSAIDS.
Anaphylaxis manifestation typically involved the cardiovascular system, fol-
lowed by skin and respiratory systems.
P19
TREATMENT OF BETA BLOCKER-INDUCED CUTANEOUS
REACTION AND ANGIOEDEMA WITH SYSTEMIC
CYCLOSPORINE.
M. Imran*, Y. Zgherea, S. Gierer, J. Martinez, Kansas City, MO.
Introduction: Cyclosporine is an immunosuppressive and immunomodu-
latory drug that acts selectively on T-cells by inhibiting calcineurin. It has been
used in the treatment of a variety of T cell-mediated inflammatory and immune-
mediated skin diseases. Methods: A 40 year old Caucasian female was started
on a beta adrenergic receptor blocker (metoprolol) for ischemic cardiomyopa-
thy. On the third day, the patient developed a non-urticarial, pruritic and vesic-
ular rash on her upper chest and extensor surface of her hands, along with
A30 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A31
ABSTRACTS: POSTER SESSIONS
P21 P22
DRUG INDUCED HYPERSENSITIVITY WITH USE OF RECURRENT DRUG REACTION WITH EOSINOPHILIA AND
AMLODIPINE. SYSTEMIC SYMPTOMS (DRESS) TRIGGERED BY A STRUC-
P. Oza*, Ann Arbor, MI. TURALLY UNRELATED DRUG.
Introduction: Drug induced hypersensitivity reaction to amlodipine is rare. S. Spriet*, T. Banks, T. Love, Bethesda, MD.
We present a 59 year old woman who presented with a 3 month history of a Introduction: Drug reaction with eosinophilia and systemic symptoms
cutaneous manifestation drug induced hypersensitivity which started 2 days (DRESS) is a rare, drug-induced reaction characterized by rash, fever, lym-
after she was re-started on Amlodipine. Methods: Evaluation, diagnosis, and phadenopathy, elevated liver enzymes, and leukocytosis with eosinophilia and
treatment of a patient with serum sickness secondary to amlodipine. Results: has a long latency period between exposure and disease onset. We describe a
A 59 year old woman presented with a 3-month history of severe rash which case of recurrent DRESS triggered by a structurally unrelated drug. Case Pres-
started 2 days after being placed on Amlodipine for uncontrolled hypertension. entation: A 54-year-old female with Neurofibromatosis type I and seizure dis-
The patient recalls taking the drug before, but did not know the duration or why order presented to her primary physician with a diffuse morbilliform eruption
she stopped the therapy. Her rash was located primarily on her palms and soles. and facial edema approximately 4 weeks after transitioning from levetirac-
It was painful, pruritic, showed significant desquamation and was associated etam to lamotrigine. As a result, lamotrigine was discontinued; however, the
with a constant burning sensation. She also had swelling of her legs. Amlodip- patient was soon admitted due to persistent cutaneous symptoms and new fever,
ine was discontinued after 2 weeks, but the rash persisted. She was treated abdominal pain and dyspnea. Laboratory studies were significant for a leuko-
with a Medrol dose pack which improved her symptoms, but the lesions recurred cytosis of 35,000 cells/mcL, an absolute eosiniphilia count of 7500 cells/mcL,
despite follow on therapy with Clobetasol cream BID, Vaseline, Vitamin E, and elevated liver enzymes and an increase in serum creatinine from a baseline of
Benadryl. Her pain was debilitating and prevented her from walking. Derma- 0.7 to 2.7 mg/dL. Bilateral pulmonary infiltrates were noted on chest radiog-
tology obtained a punch biopsy of her hands and feet revealed eczematous raphy. There was no mucosal involvement. Intravenous corticosteroids were
dermatitis, and was noted to have mild largely perivascular dermal lymphoid initiated and the patient’s symptoms and laboratory values steadily improved.
infiltrate. She was prescribed modified Goeckerman regimen which was not Following discharge, the patient continued on a planned oral steroid taper. Three
helpful. Upon presenting to our clinic, her rash was clearly demarcated by ery- weeks later she was started on a ten day course of clindamycin (1200mg/day)
thematous marginal lines present on both palms and soles (see image). Her for treatment of a newly diagnosed cellulitis. This process quickly resolved, but
ESR was noted to be elevated at 30. She was started on a prednisone taper. At on day 10 of the antibiotic course she developed a recurrence of her morbilli-
her 2 week follow up visit, she showed resolution of the cracking on the palms form rash, evolving to significant erythroderma that resolved with an increase
and burning sensation, with presence of mild residual erythema. Conclusion: in the daily dose of prednisone from 50 to 60mg. Due to the clinical course
There have been only 3 case reports suggesting a cutaneous reaction to amlodip- and temporal relation to clindamycin, the patient was diagnosed with recur-
ine use. The cutaneous manifestations of serum sickness are variable. Promi- rent DRESS triggered by the antibiotic. Discussion: Antibiotics are the most
nent skin changes at the lateral aspect of the feet and hands, especially at the commonly implicated drugs in cases of recurrent DRESS however, the mech-
junction of the sole and side of the foot and at the junction of palm and dorsal anism by which these or other structurally unrelated agents trigger the abnor-
skin surface has been noted to be unique to serum sickness. Given that amlodip- mal immune response remains unclear. As in our case, recurrent reactions
ine is lipid-soluble, it can take months for the body to clear, which explains the tend to be limited to cutaneous findings. Providers should be aware of this
persistent nature of the rash. Conclusion This case demonstrates Amlodipine potential complication in patients with a history of DRESS and recognize the
induced drug hypersensitivity can present as an isolated cutaneous manifesta- need for prompt treatment.
tion that is responsive to treatment with oral steroid.
P23
BACITRACIN IRRIGATIONS AS A CAUSE OF ANAPHYLAXIS
AND RASH.
S.E. Chiarella*, D. Nayak, N. Fenny, C. Saltoun, Chicago, IL.
Bacitracin is a polypeptide antibiotic that was approved by the FDA in 1948.
Topical bacitracin ointment has traditionally been used to prevent skin infec-
tions. More recently prophylactic bacitracin irrigations are being used during
surgical procedures. Seven cases of intraoperative anaphylaxis after exposure
to bacitracin irrigations have been previously reported. Here we present the
cases of two patients who developed hypersensitivity reactions after receiving
prophylactic bacitracin irrigations. The first case is a 47 year-old female with
a history of breast cancer status post mastectomy and prior patch testing that
was positive for bacitracin who presented for breast revision. Upon starting
the procedure, lidocaine 1% with epinephrine was employed for local anes-
thesia and the surgical wound was irrigated with a bacitracin solution. A few
minutes after receiving these medications, she developed generalized erythema
and hypotension. Intravenous hydrocortisone, diphenhydramine, and famoti-
dine were given with improvement in her blood pressure. Full recovery ensued.
Laboratory tests done later that day were all normal, except for an elevated
serum tryptase at 77.9 mg/L (normal <11 mg/L). Subsequent skin testing for
lidocaine and latex was negative. The second case is a 51 year-old female with
a history of breast cancer status post mastectomy who also presented for a breast
revision. She was given cefazolin before the procedure, prepped with chlorhex-
idine and, as in the prior case, the surgical wound was irrigated with a baci-
tracin solution. No immediate complications were noted. One day after the pro-
cedure she developed a pruritic erythematous papular rash over the left breast
that later spread to her back and abdomen. The rash resolved after completing
a short course of oral prednisone. Bacitracin patch testing done in our clinic
was positive. In addition, skin testing for penicillin and chlorhexidine was
negative. In summary, these are two very interesting cases of patients who devel-
oped hypersensitivity reactions after intraoperative exposure to a bacitracin
solution. This problem is particularly relevant since prophylactic bacitracin irri-
gations of clean surgical wounds are becoming more common.
VOLUME 113, NOVEMBER, 2014 A31
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A32
ABSTRACTS: POSTER SESSIONS
lines. Materials and Methods: We will review the medical record of this patient,
P24 including results of laboratory and RAST testing. We conducted a MeSH search
DRESS IN A PEDIATRIC PATIENT TO MEXILETINE.
for “anaphylaxis”, “rat”, “mouse”, “murine”, and “bite”. Results: Review of
C. Collins*1, J. Sherr2, A. Liu2, 1. Cupertino, CA; 2. Palo Alto, CA. literature revealed 7 previously reported cases of severe allergic reaction after
DRESS (drug reaction with eosinophilia and systemic symptoms) is a seri- rat or mouse bites. One case was an anaphylactoid reaction in a 9-year-old that
ous and sometimes fatal drug reaction that is difficult to diagnose. Mexiletine was bitten by a pet mouse. 6 other cases of true anaphylaxis involved labora-
has been reported as a cause of DRESS in case reports in the adult literature. tory workers. 5 of the 7 previously reported reactions occurred in patients with
Here we report the first case of drug reaction with eosinophilia and systemic atopy exacerbated by murine exposure. Our patient was evaluated in the ER for
symptoms (DRESS) in a pediatric patient caused by the antiarrhythmic drug an episode of anaphylaxis that occurred minutes after sustaining a rat bite to
mexiletine. Our patient developed DRESS on mexiletine started for non-sus- the finger. He was treated with epinephrine, prednisone, and antihistamines
tained ventricular tachycardia associated with nonischemic idiopathic car- with prompt recovery and referred to our clinic for follow up. We used RAST
diomyopathy. Her symptoms included fever, rash and facial swelling, lym- testing to assess for sensitization to laboratory animals, and he was found to
phadenopathy, and peripheral eosinophilia approximately 6 weeks after starting have strongly positive IgE to rat and mouse urine and epithelium (rat urine
mexilitene. Though mexilitene was initially discontinued with improvement IgE>100). Recommendations were made for avoidance of laboratory animals,
in reaction symptoms, it was restarted when the patient had multiple PVCs and he was provided with an epinephrine autoinjector. Conclusion: Murine
and there was concern for the subsequent development of ventricular tachy- anaphylaxis is an unusual but important entity to recognize in the workplace.
cardia, for which she did not have good long-term alternatives. This case is Laboratory workers who develop allergic sensitization to animals as evidenced
unusual and significant because a re-exposure was associated with syndrome by exacerbation of asthma and rhinoconjunctivitis should be aware of the risks
recurrence, confirming the culprit medication. of development of serious reactions, and career counseling may be indicated.
Murine specific immunotherapy can also be considered. The genetic and molec-
ular bases of murine anaphylaxis are unknown and require further study.
P25
SUSPECTED METHYLPREDNISOLONE SUCCINATE ANAPHY-
LAXIS CONFIRMED WITH SKIN TESTING. P27
L.M. Cristiano*, J.W. Caldwell, Winston Salem, NC. COMPATIBILITY OF SHORT RAGWEED EXTRACTS IN CON-
CENTRATED MIXTURES WITH HIGH-PROTEASE AND LOW-
Perioperative anaphylaxis is often a difficult diagnostic dilemma as multi-
ple medications are administered in a short timeframe. Considering all agents
PROTEASE GLYCERINATED EXTRACTS AT REFRIGERATION
in this setting is prudent. Anaphylaxis due to corticosteroids is rare with only OR AMBIENT TEMPERATURES.
about 100 case reports available. Hydrocortisone, prednisolone, and methyl- T.J. Grier*, D. Hall, E. Duncan, T. Coyne, Lenoir, NC.
prednisolone are the formulations most often implicated in anaphylactic reac- Background: The stability of short ragweed allergens in immunotherapy
tions. We present a case of near-fatal anaphylaxis attributed to methylpred- vaccines can be compromised by mixing with other extracts, particularly those
nisolone succinate. A 45-year-old female presented for ophthalmological surgery containing active hydrolytic enzymes. Delivery of inaccurate or inconsistent
requiring general anesthesia. Within 30 minutes, the patient suffered severe allergen levels can reduce the effectiveness of patient treatment regimens using
hypotension and cardiac arrest with pulseless electrical activity. She was resus- these mixtures. Objectives: To confirm the compatibilities of standardized short
citated and transferred to the ICU. The Allergy/Immunology service was asked ragweed extracts in mixtures with a variety of other phenolated, glycerinated,
to confirm anaphylaxis and identify the culprit. Our institution has recently high-protease (mold, cockroach) and low-protease (tree, grass, cat, dog epithe-
adopted a new electronic medical record system (EMR). The system allows lia, dust mite) extracts at concentrations targeted for maintenance immunother-
recording of operative events which are presented in graphical format includ- apy administrations. Methods: Two-part and three-part mixtures containing
ing vital signs and medication administration in the context of time. This for- short ragweed and other glycerinated extract concentrates were analyzed by
mat proved helpful in identifying the causative agent of anaphylaxis in this case. Amb a 1 radial immunodiffusion assay, the method currently used for short
According to the operative record, the patient entered the OR in stable condi- ragweed extract standardization, after storage for up to 12 months at 2-8°C or
tion. Induction of anesthesia included propofol, rocuronium, and fentanyl. up to 6 months at 20-25°C. Results: Short ragweed extract controls and all mix-
She also received ocular lidocaine. Approximately 30 minutes later, a second tures displayed favorable Amb a 1 recoveries during storage at either temper-
dose of rocuronium was administered with 500mg of IV methylprednisolone. ature. Control sample recoveries ranged from 90-107 (2-part) and 49-72 (3-
Vital signs were stable prior to dosing; however, within minutes, severe hypoten- part) Amb a 1 U/mL, and mixtures retained 85-117% (2-part) and 70-116%
sion and cardiac arrest ensued. The patient received epinephrine and CPR with (3-part) of control values in these analyses. There was no evidence of pro-
return of spontaneous circulation. There were no reports of rash or flushing. gressive changes in short ragweed extract potency in the stored samples. Con-
Using information from the EMR graph, skin testing was planned for rocuro- clusions: Diverse combinations of short ragweed and other glycerinated extracts
nium, cisatracurium, fentanyl, and methylprednisolone. SPT and intradermal frequently used for immunotherapy displayed very stable ragweed allergen lev-
testing to rocuronium, cisatracurium, and fentanyl were negative. SPT to methyl- els under all conditions examined. These data support refrigerated storage of
prednisolone was positive with wheal/flare of 10/35mm. Positive and negative these and related extract mixtures for up to 12 months in clinical settings. Ambi-
controls had wheal/flare of 10/30mm and 0/5mm, respectively. This case illus- ent temperatures (20-25°C) were evaluated as an accelerated (worst-case) exper-
trates the need to consider corticosteroids as a cause of anaphylaxis. The EMR imental condition, and are not recommended for storage of actual patient
and graphical record are useful tools in recognizing the timing of anaphylaxis immunotherapy formulas.
and guided drug testing. The EMR in combination with positive and negative
SPT results helped in making a diagnosis of methylprednisolone anaphylaxis.
P28
STABILIZATION OF LABILE GRASS-FUNGAL AND GRASS-
P26 INSECT EXTRACT MIXTURES DURING STORAGE AT
ANAPHYLACTIC REACTIONS TO MURINE BITES: A CASE SUB-ZERO (CONVENTIONAL FREEZER) TEMPERATURES.
REPORT AND REVIEW OF THE LITERATURE FOR MANAGE- T.J. Grier*, D. Hall, E. Duncan, T. Coyne, Lenoir, NC.
MENT GUIDELINES.
Background: Preparation of optimal extract mixtures for allergen
L.M. Cristiano*, G. Krishnaswamy, Winston Salem, NC. immunotherapy can be restricted by changing regulations or limits for reim-
Background: Anaphylaxis is a severe and potentially life-threatening reac- bursement. Stabilization of allergen combinations known to be incompatible
tion caused by an IgE-mediated systemic response to drugs, foods, and other under conventional storage conditions, such as pollens mixed with protease-
allergens. Anaphylaxis associated with laboratory animal exposure is a recog- rich fungi or insects, can provide viable alternatives to help allergists admin-
nized but rare occurrence. The development of atopic symptoms such as ister the desired immunotherapy formulations to their patients. Objectives: To
rhinoconjunctivitis and asthma is common among those who work with labo- examine the compatibilities of standardized Meadow fescue and Timothy grass
ratory animals, estimated to affect 11-44% in close contact with rats or mice. pollen extracts in mixtures containing fungal or insect extracts at elevated glyc-
However, only a few cases of true anaphylaxis have been reported. Objective: erin concentrations after storage for up to 12 months at refrigerator (2-8°C) or
To report a case of anaphylaxis which occurred after rat bite in a laboratory freezer (-15 to -20°C) temperatures. Methods: Meadow fescue and Timothy
worker with history of atopic disease exacerbated by rat exposure. We will extracts were combined with individual fungal (Alternaria, Aspergillus, Peni-
review this case and published literature for diagnosis and management guide- cillium) or insect (American cockroach, German cockroach, fire ant) extracts
A32 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A33
ABSTRACTS: POSTER SESSIONS
at glycerin concentrations ranging from 25-50%, in 5% increments. Extract pollen season with very high tree pollen counts. Late summer-fall pollen sea-
levels corresponded to those producing effective maintenance doses for sub- son in past years is less intense and characterized by a ragweed bloom. How-
cutaneous immunotherapy. Grass extract potencies were determined by IgE ever, through 2009-2013, there were very high levels of Cedar Elm during
ELISA inhibition assay, the same method used to standardize these products. August and September. The pollen counts were consistently within the mod-
Results: Grass allergens in mixtures with fungal or insect extracts were stabi- erate range as determined by NAB criteria as greater than 15 grains per cubic
lized considerably by storage in a conventional freezer. Several mixtures at meter. Peak counts ranged between 39.1- 475.2 grains/cubic meter and 4-day
25-30% glycerin were partially frozen, but those at 35-50% glycerin remained average ranged between 23.5- 206.2 grains/cubic meter. Notable, was the
in liquid phase. All combinations exhibited significant improvements in grass increasing duration of the season and days spent within the moderate pollen
allergen potency relative to identical mixtures maintained at 2-8°C (up to 10- range. Conclusions: Cedar Elm has not been a dominant local aeroallergen in
fold for Meadow fescue; up to 16-fold for Timothy). Recoveries for most mix- Atlanta, Georgia. It appears that due to a variety of climatic and environmen-
tures at 25% glycerin in freezer exceeded those at 50% glycerin in refrigera- tal factors over the last several years, the prevalence of Cedar Elm pollen in
tor. Conclusions: Storage of glycerinated extract mixtures at freezer temperatures metro-Atlanta has increased. The change of positioning of the pollen collec-
stabilizes labile allergens, supporting formulation of specific product combi- tion device may also be a factor for these extremely high counts, nevertheless
nations that must currently be separated into different treatment vial sets. Cedar Elm is an important aeroallergen and should be considered in patients
having predominant summer-fall symptoms, especially if they fail to respond
to Ragweed testing or immunotherapy which presents during the same time of
P29 year.
CORRELATION OF POLLEN COUNT WITH NEW ALLERGY
AND ASTHMA VISITS. Cedar Elm Pollen Counts in the Fall in Atlanta, Georgia: 2005-2013
J. Turbyville*1, R. Arora2, P. Hall3, S. Pollard3, 1. Fort Knox, KY;
2. Lexington, KY; 3. Louisville, KY.
Background: Aeroallergen surveys help clinicians select appropriate aller-
gens for skin testing and immunotherapy.Knowing local pollen and spore pat-
terns might also help optimize access to care and scheduling for patients. Objec-
tives: To evaluate patterns of pollen and spore dispersal in Louisville, Kentucky
and correlate these with the number of new appointments scheduled with an
Allergist-Immunologist and with the number of acute visits for pediatric asthma.
Methods: A National Allergy Bureau certified counter in Louisville, Kentucky
performed daily pollen and spore counts.The mean daily pollen/spore count
was determined and graphs were generated indicating the onset, peak, and dura-
tion of total tree, grass, and weed pollen and mold spores.These graphs were
compared to the number of monthly new office visits in a large Allergy-
Immunology practice.In addition, the pollen counts were compared to the P31
monthly emergency room visits and admissions for asthma in a large children’s ANAPHYLAXIS FROM COMPRESSION BANDAGE POST
hospital. Results: Daily pollen/spore counts were available for 7 of 10 years DIALYSIS.
from 2003-2013. Tree pollen was present from mid-February through mid-June K. Chotikanatis*, A. Mathew, R. Barth, R. Joks, Brooklyn, NY.
with a bimodal peak; the first in mid-March dominated by juniper and the sec- Introduction: Medical adhesive bandages frequently cause irritant contact
ond in mid-May dominated by oak. Grass pollen was present from April through dermatitis, occasionally allergic contact dermatitis. Systemic hypersensitivity
August with a peak in mid-May. Weed pollen increased in mid-August with a reactions from the adhesive bandages are exceptionally rare. We report algi-
peak in early September and resolution by late-October. Mold spores were pres- nate, a component of compression bandages used after hemodialysis (HD), as
ent year round, but began rising around the first week of April, with maximum causing anaphylaxis. Case: A 31-year-old woman with end stage renal disease
levels occurring from June 01 through October 01, and decreasing to baseline due to prolong hypertension, received HD therapy via arteriovenous fistula for
winter levels in early December. New allergy visits showed a bimodal peak 8 years, presented with 5-months of recurrent generalized pruritus urticarial
with the first occurring in early May and the second in late September. These eruption, along with shortness of breath immediately after hemodialysis ses-
peaks occurred approximately 4 weeks later than peak pollen and the adjusted sions. She had no history of angioedema; and no history of chemical, medica-
total monthly pollen curve demonstrated significant correlation with new office tion or food allergies. Skin prick testing to hydrocolloid gel from TipStop®
visits (R2 =0.725). The pollen curve also correlated with total monthly asthma (Gambo, Hechingen, Germany) bandage was positive and negative to medica-
visits from March through September (R2=0.77), but asthma visits and pollen tions administered at the time of HD including intravenous iron, erythropoi-
count did not correlate when including the winter months in the data set etin and paricalcitol. Total IgE, latex IgE and tryptase levels were unremark-
(R2=0.03). Conclusions: Acute asthma visits correlate with the pollen count able. The patient was advised to avoid TipStop® bandage and became symptoms
during the pollen season and demand for new office Allergy-Immunology vis- free for 3-month follow up. Discussion: TipStop® is one of the modern com-
its correlates with peak pollen counts with a lag time of about 4 weeks. pression bandage that claims to be hypoallergenic. The Bandage has hydro-
colloid gel in the center made from alginate which is designed to stop bleed-
ing after vascular punctures and to protect the fistula. Alginate, an extract
P30 from brown seaweed, is used extensively in medical devices and products such
HIGH CEDAR ELM POLLEN COUNTS IN THE FALL IN as dental impressions, prosthetics, soft tissue dermal fillers, dressings and com-
ATLANTA, GEORGIA: 2009-2013. pression bandages. It is also used in food industry, for thickening soups and
M.R. Shams*1, S. Fineman2, 1. Atlanta, GA; 2. Marietta, GA. jellies. This is the first case of anaphylaxis to bandages. The more severe reac-
Rationale: Hayfever symptoms directly correlate with atmospheric pollen tion in our case might be caused by direct contact of alginate with vascular
concentrations. Climatic and environmental factors have the ability to influ- system. Conclusion: The allergenic potential of modern wound dressings should
ence local botany and aerobiology. National Allergy Bureau pollen count sta- not be underestimated.
tions determine the presence of local, clinically relevant allergens and track
patterns of prevalence. This data is extremely valuable to treating allergists as
knowledge regarding yearly and seasonal fluctuations in pollen counts is impor- P32
tant in the managing patients with allergic rhino-conjunctivitis, in order to RELATIONSHIP BETWEEN POLLEN COUNTS AND EMER-
provide appropriate treatment regimens. Methods: Atmospheric sampling for GENCY DEPARTMENT VISITS FOR ASTHMA.
aeroallergens in Atlanta, GA was preformed over a nine-year interval accord- O. Gourgy-Hacohen*, J. Jacobs, Walnut Creek, CA.
ing to National Allergy Bureau standards using Rotorod sampler. Samples were Background: Asthma exacerbations triggers include environmental factors.
collected each morning by trained observers and various pollens are counted. Objective: The objective of this study was to investigate the relationship between
Atmospheric concentrations are determined by calculation from the raw counts. Emergency Department visits for asthma and pollen counts. Methods: The num-
The pollen counting station was moved a distance of 2.2 miles in 2010. The ber of emergency department visits for Asthma between the years 2008-2013
staff is certified through the American Academy of Allergy, Asthma and was recorded at John Muir Hospital in Walnut Creek, California. Pollen counts
Immunology Aeroallergen Network. Results: The southeast has an intense spring were collected in Pleasanton, California during the same time period. Results:
VOLUME 113, NOVEMBER, 2014 A33
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A34
ABSTRACTS: POSTER SESSIONS
The number of emergency department (ED) visits for Asthma varied through-
out the year with a peak number of visits occurring in May. We found a sig-
P34
A QUALITATIVE ANALYSIS OF A NEW ROTOROD SYSTEM UTI-
nificant correlation between the number of Asthma ED visits and: 1. The
monthly averaged total pollen counts (rho=0.629, p<0.05) and 2. The monthly LIZING MICROCONTROLLERS AND OPTICAL SENSOR TECH-
averaged tree pollen counts (rho=0.678, p<0.05). The daily ED visits for Asthma NOLOGY IN THE ENVIRONMENTAL EXPOSURE UNIT (EEU).
significantly correlated with: 1. The total pollen counts (rho=0.212, p<0.0001), T.J. Walker*, L.M. Steacy, B. Hobsbawn, A.K. Ellis, Kingston, ON, Canada.
2. The grass pollen counts (rho=0.192, p<0.0001) and 3. The tree pollen counts Background: Certainty of continual Rotorod® impact sampler revolutions
(rho=0.201, p<0.0001). There was a significant difference in the number of per minute(RPM) is unknown during normal operation using accepted tradi-
daily visits between days with high grass pollen counts vs. low grass pollen tional design and RPM calibration techniques; only during RPM calibration
counts (Mann Whitney. p<0.0005. High grass pollen days: Mean=2.024 visits can one be definitive. As EEU pollen concentration levels are monitored and\or
per day. Low grass pollen days: Mean=1.302 visits per day). A significant dif- adjusted based on accurate sampling, monitored constant RPM values are pre-
ference in the number of daily visits was also observed when comparing days ferred. Methods: Custom programmable microcontroller boards, optical encoder
with high tree pollen counts vs. low tree pollen counts (Mann Whitney. p<0.001. technology, secure digital(SD) storage, wireless connectivity, and touch screen
High tree pollen days: Mean=1.894 visits per day. Low tree pollen days: control are combined to provide real time monitoring, alerts, and data storage.
Mean=1.312 visits per day). Conclusions: ED Asthma visits in this study were Pulse width modulation(PWM) using the proportional-integral-derivative con-
associated with tree pollen counts and with grass pollen counts. troller(PID) and encoder feedback ensure accurate motor control. The 2400
RPM speed is calculated and recorded per second and stored along with device
name, date, time, and user stamp on the onboard storage or wirelessly to a sep-
arate location. A standard 30 second spin cycle was initiated multiple times
over a 15 minute period while simultaneously taking RPM measurements with
a handheld National Institute of Science and Technology(NIST) certified opti-
cal tachometer. Voltage was monitored until the rotorod system was unable to
sustain the minimum RPM and noted. All data was stored and then compared
in our central database. Results: The RPM comparison speeds captured by the
new system averaged 2380.90 RPM, st dev 35.86. Readings from the hand-
held tachometer averaged 2394.52 RPM, st dev 9.65. The minimum voltage
causing RPM under tolerance was 11.85 volts. The new design allows for con-
tinual, noncontact, real time monitoring and storage of data from multiple
devices simultaneously, therefore, lessoning labor time requirements.
Conclusions: The redesigned rotorod particle sampler will allow for real-time
verification feedback and alerts for all particle sampling in the EEU. This
advancement assures that all particle sampling using rotorod impact sampling
is accurate for the entire duration of all duty cycles. Qualification/ validation
of these devices addresses any mitigations deemed necessary to meet regula-
tory guidelines.
Monthly averages of the different pollen types and ED Asthma visits between
the years 2008-2013 with SEM. Pollen data presented as pollen grains per
cubic meter. Asthma visits data presented as the monthly averaged number of P35
visits. OCCUPATIONAL ALLERGY TO PEACH (PRUNUS PERSICA)
POLLEN AND CROSS-REACTIVITY BETWEEN ROSACEAE
FAMILY POLLENS.
P33 N. Jiang*, L. Wen, J. Yin, Beijing, China.
ALLERGEN EXTRACT STABILITY: NON-STANDARDIZED
Background: Orchard workers are highly exposed to several allergic agents,
EXPIRATION DATING.
especially peach pollen and other Rosaceae family pollens. However, no occu-
G. Plunkett*, B. Mire, Round Rock, TX. pational allergy in this branch has been described before. Methods: First, skin
Introduction: In the US, the standardized extracts, grass pollen, dust mite, tests, serum-specific IgE tests with home-made extracts of peach pollen and
short ragweed, cat hair/pelt, and venoms have expiration dating determined by other four Rosaceae family pollens (apricot pollen, cherry pollen, apple pollen
formal manufacturer studies and approved by the FDA. Non-standardized and pear pollen) of the working environment were executed. Furthermore, con-
extracts have expiration dating specified by the FDA. 50% glycerin extracts junctival challenge with peach pollen was performed, western immunoblots
are dated for 6 years from extraction, but only 3 years from shipping, and non- with these five Rosaceae family pollens were performed. In addition, ELISA
glycerin extracts are dated for 3 years and 1.5 years from shipping. Little evi- inhibition and western blotting and inhibition experiments among five Rosaceae
dence is available to support this dating, so the purpose of this study is to eval- family pollens were performed. Result: Skin prick tests with five Rosaceae pol-
uate various extracts produced over the last 10 years for protein and allergen lens extracts were positive in patient. Specific IgE against three pollens (peach
content. Methods: Allergen extract concentrates were analyzed for protein diver- pollen, apricot pollen and cherry pollen) could be demonstrated in the patient
sity by SDS-PAGE. Potency of some extracts was determined by IgE binding by ELISA. Cross reactivity studies by ELISA inhibition performed with the
and major allergen assays such as Bet v 1 in Birch, Pla l 1 in English plantain, patient’s sera, when peach pollen used as solid phase, IgE binding to peach
Ara h 1,2,6 in peanut and tropomyosin in shrimp. The commercial extract lots pollen could be inhibited by precubation the other four pollens with inhibition
were manufactured over a 10 year period and were stored in their final con- rate ranging from 45% to 87%, the strongest inhibitor was apricot pollen extract.
tainer vials at 2-8C. Results: SDS-PAGE protein patterns generally maintain Sera from patient showed clear IgE binding to 20kD,60kD,80kD proteins in
consistent patterns for the mandated expiration dating. Most aqueous extracts peach pollen extract, similarly the patient’s sera recognized apricot pollen pro-
began to show changes after the 3 year expiration and most glycerin extracts teins of 20KD,55kD,80kD, the sera showed weak IgE binding to 20KD,80KD
showed little change over 6 years. Remarkably, some extracts maintain con- component of cherry pollen, and the IgE reactivity protein in apple pollen
sistent patterns for up to 10 years. Potency assays helped support the gel data. appeared to be 80kD and 110 kD. The 20KD IgE binding component in patient’s
Conclusion: The characterization methods used in this study provide evidence serum could be demonstrated with peach pollen, apricot pollen and cherry
for the expiration dating for many non-standardized allergen extracts. The sta- pollen. The IgE binding to the 20kD protein in peach pollen extract was com-
bility enhancing ability of glycerin has been confirmed. pletely inhibited with apricot pollen (10mg/ml) as inhibitor. When cherry, apple,
and pear pollen were used as inhibitors, 20kD band was partly inhibited. Con-
clusion: We conclude that peach pollen is a potential cause of IgE mediated
occupational respiratory disease, extensive cross reactivity among Rosaceae
pollens. An increasing number of patients are needed to confirm these inter-
esting preliminary finding, and epidemiologic studies are necessary to assess
the importance of this aeroallergen among exposed orchard workers.
A34 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A35
ABSTRACTS: POSTER SESSIONS
tant trends were noted. Study participants with early life exposure to high lev-
P36 els of dog allergen had a nearly 50% reduction in levels of the following
UNIQUE ALLERGY AND ASTHMA SMARTPHONE APP.
cytokines compared to those with exposure to low levels of dog allergen: G-
S. Kagen*, Appleton, WI. CSF, IL-10, MCP-3, TGFalpha, IL-9, and IL-3. No cytokine was elevated in
Smartphone applications are now playing a new and critical role in mon- participants with exposure to high levels of dog allergen compared to the low
itoring the success or failure of allergy and asthma treatments, especially as dog allergen level group. In contrast, study participants with early exposure to
new healthcare reforms reward successful patient outcomes and performances. high levels of cat allergen had significantly higher levels of the following
Monitoring allergy patients has been difficult, but a new and unique Smart- cytokine compared to those with exposure to low levels of cat allergen: IL-
phone software application (KagenAir®) enables consumers to simultaneously 12p70, G-CSF, Mip-1alpha, IL-9, and TNFbeta. Only VEGF was substantially
monitor their allergy and asthma symptoms and discover local environmental elevated in participants with exposure to low levels of cat allergen. Conclu-
factors that affect how they feel using patent pending methodologies and com- sions: The observed trends support that early exposure to high levels of dog
puter generated animated maps and graphics. The KagenAir App is unique in allergen is immunoprotective and associated with lower serum levels of
that it measures symptoms scores and also directly connects consumers with cytokines in later childhood. Notably, a similar relationship was not found with
uncontrolled allergy and asthma symptoms to Board Certified Allergy-Asthma- high cat allergen exposure at a young age. In contrast, early exposure to high
Immunology Specialists within their communities using both cell phone and levels of cat allergen was associated with higher cytokine levels.
video-chat technologies. Beta testing on allergy and asthma patients established
the KagenAir App to be easy to understand, simple to use and helpful in con-
necting consumers with local allergy specialists. P39
THE CORRELATION OF BODY MASS INDEX (BMI) TO ALLER-
GEN SKIN TESTING AND SERUM SPECIFIC IGE.
P37 M.Z. Braunstein*, R. Joks, Brooklyn, NY.
GRASS POLLINATION OCCURS EARLIER AND IS MORE ABUN-
Background: Obesity has been linked to asthma exacerbations, total serum
DANT IN CENTRAL UKRAINE LIKELY DUE TO CLIMATE
IgE, and severity of atopic dermatitis. The correlation of obesity on allergy test-
CHANGE. ing responsiveness has not been well studied. Objective: We sought to investi-
V.V. Rodinkova1, O.O. Palamarchuk1, I.I. Motruk1, L.V. Kremenska1, gate the relationship of BMI to allergen skin prick tests and serum specific
K.V. Musatova1, L.M. DuBuske*2, 1. Vinnitsa, Ukraine; 2. Gardner, MA. allergen IgE levels of common aeroallergens and foods. Methods: We reviewed
Background: Recent pollen seasons in Ukraine have demonstrated rapid adult patient charts (n=288) who presented to the allergy and immunology clinic
changes in the pollination patterns of key taxa producing allergenic pollen. from 1998-2013. Data from patients with physician diagnosed allergic rhinocon-
Poaceae is one of the pollen types causing severe symptoms for patients in junctivitis or asthma who underwent routine epicutaneous skin prick testing
Ukraine. Method: Pollen collection from 2009 to 2014 used volumetric meth- (SPT) for common environmental allergens (n=124) or who had allergen spe-
ods employing a Hirst Burkard trap placed at a height of 25 meters above the cific IgE levels (FEIA) to common environmental and food allergens (n=92)
ground on the roof of a Vinnitsa Medical University building. All samples were were included for analysis. Spearman coefficients were generated to determine
taken from March 1 until October 31. Results: Poacea pollen season start has an association of BMI with the number of positive SPT, the mean wheal diam-
shifted at least 10 days earlier for the 2013 and 2014 year seasons than seen in eter, and the maximum specific IgE class. Results: BMI significantly corre-
2009 to 2012. Thus, year 2009 and 2011 were characterized for the latest sea- lated with the number of positive SPT (p=0.01) and inversely with the mean
sonal start in the third ten-day-period of May. Years 2010 and 2012 were char- wheal diameter (p=0.05). There was no significant correlation with the maxi-
acterized with the season start in the second ten-day-period of May. Poaceae mum specific IgE class. Conclusions: Obesity, as measured by BMI, is asso-
pollination was seen during the first ten-day period of May for both 2013 and ciated with increased specific cutaneous allergic responses. However, the cuta-
2014. However, the season end is always the first ten-day period of September neous response to allergen decreases with increasing BMI, suggesting an
in each year. Interestingly, May 24, 2014 was characterized by a significant attenuated response to allergic mediators released during immediate hyper-
pollen count increase to 73 pollen grains per cubic meter of air (p.g./m3). The sensitivity reactions with increasing BMI.
grass pollen season for 2009 and 2011 had just begun around this date. The
pollen count increase exceeded seasonal peak values seen in 2009, 2012 and Spearman correlation (r) of BMI with:
2013 (71, 62 and 43 p.g./m3 respectively). Total pollen number collected in
2014 by June 18 in Vinnitsa is already comparable with the total annual val-
ues recorded in years 2012 and 2013 (819 p.g versus 911 and 896 respectively).
Conclusion: Poaceae pollination has became more abundant and starts early in
recent years in Central Ukraine. This phenomenon may be related to climate
change and global warming. *statistically significant
P38 P40
INFLUENCES OF EARLY PET EXPOSURE ON CYTOKINE LEV- THE ASSOCIATION BETWEEN SERUM IGE, EOSINOPHIL LEV-
ELS IN LATER CHILDHOOD. ELS AND CANCER, NHANES 2005-2006.
H. Nguyen*, J.M. Biagini Myers, U. Sivaprasad, G.K. LeMasters, S. Nagarajan*1, Q. Meng1, L. Bielory*2, 1. Piscataway, NJ; 2. Springfield,
D.I. Bernstein, T. Reponen, P.H. Ryan, G.K. Hershey, Cincinnati, OH. NH.
Background: Though exposure to pets is a known trigger of allergic dis- Background: Cancer is an important cause of health morbidity in adults.
ease, it has been shown that such exposures, particularly at a young age, can One in four deaths are due to cancer (ACS, 2014). There is little published lit-
be immunoprotective. Early dog exposure especially has been associated with erature of serum IgE and eosinophil level associations with cancer on a national
decreased risk of wheezing and atopic dermatitis. Methods: Data from the level. Objective: To examine the association between serum IgE, eosinophil %
Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS) provided cat and the overall vs. type-specific prevalence of cancer. Methods: Data from a
and dog allergen levels contained within dust samples collected from the homes nationwide survey conducted by the Centers for Disease Control and Preven-
of infants born between the years of 2001 and 2003 with at least one atopic par- tion, National Health and Nutrition Examination Survey (NHANES 2005-2006)
ent. Cytokine levels were measured from blood samples obtained when was used. Bivariate analyses with chi-square tests, logistic regression and strat-
CCAAPS study participants were 11-12 years of age. IRB approval and ified models assessed the relationship between serum IgE and eosinophil %)
informed consent was obtained from all research subjects. The study data from and the overall prevalence of cancer (defined as ever having been diagnosed
the first 40 participants with available serum samples were included in this by a physician with cancer of any kind) versus the type-specific prevalence of
study, and levels of cytokines were measured via a Luminex® multiplex cytokine cancer. Results: A total of 4,893 adults constituted our study population. After
assay. High allergen level was defined as a level at or above the calculated controlling for age, gender, ethnicity, education and income, smoking status
median. High cytokine level was also defined as a level at or above the calcu- and duration of cancer diagnosis, subjects with high serum IgE had a negative
lated median. Differences in the proportions of high and low allergen levels odds of overall cancer (OR = 0.83, 0.64-1.09), as did subjects with higher
with high and low cytokine levels were tested by Chi-square. Results: Although eosinophil levels (OR = 0.90, 0.82-0.99). Interaction models demonstrated the
the differences in cytokine levels did not reach statistical significance, impor- significant protective effect of cancer for IgE for males (OR= 0.85, 0.74-0.99)
VOLUME 113, NOVEMBER, 2014 A35
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A36
ABSTRACTS: POSTER SESSIONS
and eosinophil levels in females (OR= 0.73, 0.54-0.98). Finally, IgE levels had cryoglobulins in association with characteristic clinical signs and symptoms.
a negative odds of lung (OR= 0.28, 0.15-0.52) and cervical cancers (OR= 0.84, Prognosis is generally dependent on the degree of resolution of the underlying
0.61-0.16). High eosinophil levels also had negative odds of lung (OR=0.39, condition. This case marks the importance of an infectious work-up and vas-
0.15-1.00) and cervical cancers (OR=0.57, 0.41-0.78). Conclusion: This study culitic evaluation in a patient with non-remitting urticarial lesions.
shows that atopy and eosinophilia were associated with a decreased preva-
lence of overall cancer after covariate adjustment, using a large, nationally
representative dataset. This suggests the need for continued allergy surveillance P43
and longitudinal studies of the possible protective role of serum IgE and IMPACT OF WEIGHT LOSS ON MARKERS OF SYSTEMIC
eosinophil levels in lung and cervical cancers. INFLAMMATION IN OBESE SAUDI CHILDREN WITH ASTHMA.
O.H. Al Jiffri*, Jeddah, Saudi Arabia.
P41 Background: Weight loss studies were conducted in children without asthma
have demonstrated a reduction in systemic inflammation. However, the impact
CONTACT SENSITIVITY TO METAL AND ACRYLATES IN
of weight loss in the obese paediatric population with asthma has not been
PATIENTS UNDERGOING JOINT REPLACEMENT.
investigated. Objective: To measure the effects of weight loss on markers of
M. Goebel, J. Tan*, D. Bernstein*, Cincinnati, OH. systemic inflammation in obese children with bronchial asthma. Methods:
Introduction: Allergy to metals and acrylates in bone cement have been Eighty obese children with bronchial asthma (42 boys, and 38 girls) with mean
implicated in joint implant failures. Over 900,000 hip and knee replacement age 13.86± 3.21 years were divided into two equal groups. The training group
surgeries are performed annually in the US. The purpose of this study was to received diet regimen, exercise training in addition to the medical treatment for
evaluate contact hypersensitivity to metals and acrylates in patients undergo- two months, where the control group received the medical treatment only.
ing joint replacement. Methods: Sixty-five subjects were referred for evalua- Results: There was a 17.5%, 15.5%, 22.4%, 14.1% and 15.9% reduction in
tion of possible allergy to metal between 2012-2014. Subjects underwent either mean values of tumor necrosis factor-alpha (TNF-alpha), interleukin-6 (IL-6),
pre-operative (N=46) or post-operative (N=19) patch testing to a standard panel interleukin-8 (IL-8), Leptin and body mass index (BMI) respectively and 38.7%
of metal salts (nickel, cobalt, chromium, palladium, vanadium, and zirconium) increase in mean values of adiponectin in the training group. While, there was
and methyl and ethyl acrylate. Patients and referring providers were contacted a 0.7%, 9.0%, 2.8%, 1.6% and 1.2% increase in mean values of TNF-alpha,
for information regarding component materials in the prostheses and postsur- IL-6, IL-8, Leptin and BMI respectively and 3.9% decrease in mean values of
gical outcomes. Results: Of 65 patients, 46 with a self-reported history of metal adiponectin in the control group. The mean values of TNF-alpha, IL-6, IL-8,
allergy were tested pre-operatively (PRE) and 19 patients were referred post- Leptin and BMI was decreased and adiponectin was increased significantly in
operatively (POST) for implant failure. Thirty-five (76%) of the PRE group the training group, however the results of the control group were not signifi-
had a positive patch test; all these patients had an alternative material (eg zir- cant. Also, there were significant differences between both groups at the end
conium, polyethylene, ceramic, or titanium) implanted. Fourteen of POST of the study. Conclusion: Weight loss improves markers of systemic inflam-
patients had positive patch tests (74%); 8/14 (57%), however, gave no prior mation in obese Saudi children with bronchial asthma. Key words: obesity,
metal allergy history. Nickel was the most common offending antigen in both asthma, weight loss, cytokines.
groups with 54% of PRE and 32% of POST patients reacting to nickel. Rare
metals such as palladium caused several reactions with 8 PRE and 4 POST pos- Mean value and significance of TNF- α, IL-6, IL-8, Leptin, Adiponectin
itive patch tests. Two PRE and 3 POST patients, all female, reacted to ethyl and BMI in group (A) and group (B) after treatment.
acrylate as well. Conclusion: A history of metal allergy and/or contact hyper-
sensitivity confirmed by patch testing may influence choice of implant mate-
rial. In addition to infection and biomechanical failure, metal allergy should
be considered as a potential cause of prosthetic joint failure.
P42
HEPATITIS C VIRUS-ASSOCIATED CRYOGLOBULINEMIA PRE- TNF- α = tumor necrosis factor – alpha. IL-6 = Interleukin-6
SENTING AS CHRONIC URTICARIA. IL-8= Interleukin-8 BMI= Body Mass Index
S. Bantz, M. Rodenas*, New Haven, CT.
Introduction: A 48 year old male presents with a 20 year history of chronic
urticaria that has been worsening in severity for the past 4 years. He reports a P44
long-standing pruritic urticaria that comes and goes on his arms, legs, abdomen, THE USEFULNESS OF SERUM HIGH SENSITIVITY C-REAC-
and back. For the past 4 years he has had more painful lesions occurring over TIVE PROTEIN AS A MARKER OF AIRWAY INFLAMMATION
a greater area and with increased frequency, almost daily. The pain and itch are IN BRONCHIAL ASTHMA.
relieved by oral steroids and antihistamines, but he has been requiring greater T. Shimoda*1, Y. Obase2, M. Imaoka1, R. Kishikawa1, T. Iwanaga1,
doses of short-acting antihistamines recently. On review of systems, he also 1. Fukuoka, Japan; 2. Nagasaki, Japan.
reports nasal congestion, cough, abdominal pain, BRBPR due to hemorrhoids, Rationale: Serum high sensitivity C-reactive protein (hs-CRP) has been
joint aches and swelling. Social history revealed a 25 pack-year smoking his- shown to be useful as a marker of airway inflammation in bronchial asthma.
tory, heavy alcohol consumption, and previous incarceration for ten years. Phys- However, various factors have been reported to affect hs-CRP levels. We con-
ical examination revealed raised, erythematous, circumscribed lesions that are ducted a study in patients with mild bronchial asthma without complications
not blanchable on his upper and lower extremities, abdomen, and back. Results: to determine whether hs-CRP could serve as a useful indicator in assessing air-
Laboratory evaluation revealed mild anemia Hb13.1g/dL, Hct 39.6%. IgE 28 way inflammation. Methods: The subject population consisted of 40 healthy
kU/L. CMP unremarkable. Absent CH50 and C4. Low C2 (0.9mg/dL) and C3 volunteer (HV) controls, and 45 patients with bronchial asthma (BA). Induc-
(36mg/dL). Rheumatoid factor positive. C1q, ANA, ANCA, ESR (2mm/hr), tion of sputum with the use of inhaled 3% hypertonic saline and bronchial
anti-Smith, anti-dsDNA and anti-RNP antibodies were normal. SPEP unre- hyperresponsiveness test were performed, in addition to serum hs-CRP. Results:
markable. Quantiferon Gold negative. HIV negative. Hepatitis C antibody reac- The log serum hs-CRP levels were higher in BA patients (2.49 ± 0.41) com-
tive, HCV Quantitative 1,160,000 IU/mL and HCV Quantitative Log 6.06. Hep- pared with healthy subjects (2.21 ± 0.39) (p=0.002). When receiver operator
atitis C genotype 1b. Biopsy was consistent with vasculitis. Cryoglobulins characteristic (ROC) analysis was performed to compare healthy subjects and
positive. The patient is scheduled to start anti-viral therapy. Discussion: Cryo- BA patients, the sensitivity was 0.64 and specificity was 0.71 at a log serum
globulinemia is a systemic inflammatory syndrome that involves small-to- hs-CPR of 2.3. The log serum hs-CRP levels were negatively correlated with
medium vessel vasculitis due to immune complexes. Clinical presentations of FEV1.0,%pred (r = -0.31, p = 0.04), positively with sputum eosinophils (r = 0.34,
cryoglobulinemia vary widely. Cryoglobulinemia has different underlying eti- p = 0.02), but not with log PC20 (r = -0.09, p = 0.56). Multiple regression analy-
ologies, and is associated with up to 65% of patients with hepatitis C virus. sis demonstrated that the log serum hs-CRP concentrations were significantly
Cryoglobulinemia can cause a triad of palpable purpura, arthralgia, and myal- correlated with both eosinophils (p = 0.004) and neutrophils (p = 0.011) in spu-
gia when viral associated, while cryoglobulinemia due to monoclonal tum. Conclusions: Serum hs-CRP is useful in assessing airway inflammation
immunoglobulins or hematological malignancies is generally associated with in BA patients without complications such as heart disease, hypertension, hyper-
hyperviscosity. Cryoglobulinemia is diagnosed by the demonstration of serum lipidemia, chronic obstructive pulmonary disease, and infections.
A36 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A37
ABSTRACTS: POSTER SESSIONS
controlled withdrawal study of patients with moderate-to-severe persistent aller-
P45 gic asthma receiving long-term therapy with OMA for ≥5 years. Patients were
ASTHMA SEVERITY AND INCREASED RISK OF CARDIOVAS-
randomized to either continue the same dose of OMA (n=88) or switch to
CULAR AND CEREBROVASCULAR OUTCOMES IN PATIENTS placebo (PLB, n=88) and were followed every 4 weeks for 1 year. Patients com-
WITH MODERATE-TO-SEVERE PERSISTENT ASTHMA. pleted the Asthma Control Questionnaire (ACQ) and the Asthma Control Test
T.A. Omachi*1, T. Haselkorn1, D.P. Miller2, M. Shah2, M.D. Eisner1, (ACT) at baseline (BSL) and every 4 weeks until week 52. High ACQ (range
H. Chen2, C. Iribarren3, 1. South San Francisco, CA; 2. San Francisco, CA; 0-6) and low ACT (range 0-25) scores indicate poor asthma symptom control.
3. Oakland, CA. We compared changes in ACT and ACQ scores from BSL to week 52 and
Introduction: Studies have shown higher risk of cardiovascular disease ACT and ACQ scores at each time point against the BSL (ANOVA tests). We
(CVD) in asthma than non-asthma populations. However, there are limited data compared the percentage of PLB and OMA patients (chi-square test) whose
examining whether asthma severity is linked to CVD incidence within asthma decline reached minimal important difference (MID) from BSL to Week 52 on
populations. Methods: The Evaluating Clinical Effectiveness and Long-Term ACT and ACQ. IRB approval and informed consent were obtained from all
Safety in Patients with Moderate-to-Severe Asthma study (EXCELS) is a mul- research subjects. Results: On average, patients had good asthma symptom con-
ticenter, prospective, 5-year, observational cohort study of patients with mod- trol at the BSL (Table). Patients randomized to continue OMA maintained
erate-to-severe persistent asthma, including cohorts treated and not treated with better asthma symptom control than patients randomized to PLB. The mean
omalizumab. This post hoc analysis examined the association between base- change from BSL to Week 52 for ACT score was -2.88 for the PLB arm and -
line asthma severity factors and longitudinal outcomes over 5 years in the non- 1.16 for the OMA continuation arm [p=0.0188]. The mean change from BSL
omalizumab cohort. Cardiovascular- and cerebrovascular-related events were to Week 52 for ACQ score was 0.63 in the PLB arm and 0.22 in the OMA con-
combined into a single endpoint of arterial thrombotic events (ATE), defined tinuation arm [p = 0.0039]. Compared to the BSL, the decline in asthma symp-
as the first of the following: cardiovascular death, myocardial infarction, tom control in ACT and ACQ was statistically significant for the PLB arm start-
ischemic stroke, transient ischemic attack, or unstable angina. An independent ing at week 4. There was no statistically significant change for the OMA arm
expert panel blindly adjudicated all ATEs. Asthma severity measures included at any time point (Table). By week 52, the percentage of patients whose decline
spirometry, physician-assessed asthma severity, oral steroid usage, and the of asthma control reached MID comprised 28.4% (OMA) vs. 43.2% (PLB) on
Severity of Asthma Score (SOA), a validated instrument that assesses asthma ACQ (p = 0.041) and 23.9% (OMA) vs. 39.8% (PLB) on ACT (p=0.024). Con-
symptoms, asthma medication burden, and asthma emergency utilization his- clusions: Patients with allergic asthma who continue on OMA therapy main-
tory (range 0-28). Multivariable Cox models were used to assess risk of ATE tain asthma symptom control. However, patients who discontinue OMA ther-
for each individual asthma severity measure, controlling for potential con- apy report significant decline in asthma symptom control, and this is evident
founders. Results: A total of n=2,829 patients in the non-omalizumab cohort as early as week 4.
were analyzed. Baseline mean age was 46.2±17.1 years, 66.5% were female,
and 82.2% were white. Mean pre-bronchodilator % predicted forced expira- ACQ and ACT scores by study visits and treatment arms
tory volume (FEV1) was 80.0±21.6 and mean SOA was 10.0±4.5. After con-
trolling for potential confounders, lower pre-bronchodilator FEV1 % predicted,
higher SOA, and chronic oral corticosteroid usage were each statistically sig-
nificantly associated with increased risk of ATE (Table). Conclusions: Multi-
ple asthma severity measures were associated with increased risk of ATE in
this cohort. Further work is required to delineate mediators, but this analysis
utilizing a large cohort followed over an extended timeframe provides some of
the most robust evidence linking higher asthma severity to greater risk of car-
diovascular and cerebrovascular outcomes.
Adjusted Predictions for Time to First ATE Event (n=2,829 Patients)
PLB = placebo; OMA = omalizumab.
High ACQ and low ACT scores indicate poor asthma symptom control.
* P < 0.05. ** P < 0.01. P-values were derived from ANOVA, comparing
against baseline.
P47
ASTHMA KNOWLEDGE AND DISEASE CONTROL.
M. Stevens*1, J. Stokes1, A. Bewtra1, M. Fasano2, 1. Omaha, NE; 2. Iowa
City, IA.
Background: Multiple studies have shown inadequate parental knowledge
ATE, arterial thrombotic event; FEV1, forced expiratory volume in 1 second about asthma is common among pediatric patients seen in Emergency Rooms
a) Analyses of FEV1 % predicted controlled for tobacco history (none, cur- (ER) for acute asthma. Furthermore educational interventions have resulted in
rent, former) and education but not age, gender or race/ethnicity because improvements in both the asthma knowledge of parents, as well as disease con-
these demographic factors are included in the calculation of percentage pre- trol of patients. However in adult populations there are conflicting data regard-
dicted. ing the relationship between asthma knowledge and disease control. Methods:
b) Controlling for age, gender, race/ethnicity, education, and tobacco history We measured asthma knowledge with the Asthma Self-Management Ques-
(none, current, former). tionnaire, a validated 24 item true/false instrument, in 49 adult asthmatics while
visiting any of 3 primary care clinics at a single tertiary referral center. Asthma
control was measured by Asthma Control Test (ACT), mini- Asthma Quality
P46 of Life Questionnaire (m-AQLQ), as well as patient reported: monthly short
LONGITUDINAL CHANGE IN ASTHMA SYMPTOM CONTROL acting beta-agonist (SABA) use, ER visits for asthma in the past year, and life-
IN PATIENTS WHO CONTINUED VS. DISCONTINUED OMAL- time hospitalizations for asthma. Other demographic, socioeconomic, includ-
IZUMAB: RESULTS FROM THE XPORT STUDY. ing literacy as measured by the Newest Vital Sign (NVS), and asthma care
J. Antonova, B. Trzaskoma, K. Raimundo, P. Solari*, J. Zazzali, South San data were also collected. Results: Asthma knowledge was correlated with asthma
Francisco, CA. control as measured by monthly SABA use (r=-0.29 p=0.05) but was not with
Introduction: Little is known about the effect of omalizumab (OMA) con- ACT (r=0.17, p=0.24), m-AQLQ (r=0.19, p=0.19), ER visits (r=-0.13, p=0.13),
tinuation vs. discontinuation after its long-term use on patient-reported asthma and hospitalization (r=-0.11, p=0.47). Asthma knowledge was correlated with
symptom control. XPORT was the first rigorous study of long-term benefit of specialist referral (r=0.41, p=0.003) and patient literacy (r=0.37, p=0.01), but
OMA continuation. Methods: XPORT was a randomized, double-blind, placebo- not with the patient’s reported highest level of formal education (r=0.19, p=0.20),
patient income (r=0.08, p=0.60), time since asthma diagnosis (r=0.22, p=0.13),
VOLUME 113, NOVEMBER, 2014 A37
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A38
ABSTRACTS: POSTER SESSIONS
and controller medication prescription (r=0.04, p=0.8). Discussion: In this pop- (261/787) of families required 〈15 minutes of bedside education, compared to
ulation asthma knowledge was correlated with SABA use, patient literacy and 48% (75/157) when the IAC was offered five days a week (p=0.0005). Over-
specialist referral, but did not correlate with other measures of asthma control, all, 8% (75/944) of families required ≥30 minutes of bedside education with
socioeconomic status, and asthma management. However this was a small parental attendance in the IAC, compared to 17% (172/1042) of patients with-
survey conducted in a single facility and the study population had significantly out parental attendance in the IAC (p〈0.0001). Conclusion: Expanding the IAC
higher scores than the population in which the knowledge measurement tool from three days a week to five days a week increased parental attendance, result-
was validated. Consequently further investigation into adult patient knowledge ing in a reduction in bedside education time. This time-savings has allowed re-
and asthma control is warranted. allocation of RRT’s to more urgent clinical needs throughout the hospital. The
increasing importance of cost-efficient, value-based care supports the future
provision of educational programs such as the IAC.
P48
THE ASSOCIATION OF BLOOD EOSINOPHIL LEVELS AND
SEVERE ASTHMA DEFINED BY NEW GUIDELINES. P50
J. Casciano*1, J. Krishnan2, M. Buatti Small3, S. Bajpai1, C. Li4, EFFECTS OF BUDESONIDE/FORMOTEROL ON FIXED AIR-
Z. Dotiwala1, 1. White Plains, NY; 2. Chicago, IL; 3. Frazer, PA; 4. Little FLOW OBSTRUCTION STATUS AND EARLY STUDY WITH-
Rock, AR. DRAWAL DUE TO PREDEFINED ASTHMA EVENTS IN
PATIENTS WITH MODERATE TO SEVERE ASTHMA.
Background: Recently published European Respiratory Society (ERS) and
American Thoracic Society (ATS) asthma guidelines provide a new definition B.E. Chipps*1, D.P. Tashkin2, M. DePietro3, F. Trudo3, 1. Sacramento, CA;
of severe asthma based on control measures and medication use. The relation- 2. Los Angeles, CA; 3. Wilmington, DE.
ship between asthma severity and blood eosinophils (EOS) was examined using Background: The effect of budesonide/formoterol (BUD/FM), BUD, or FM
this new guideline definition. Objective: To study the association of asthma on fixed airflow obstruction (FAO) and withdrawal due to predefined asthma
severity defined by ERS/ATS guidelines with blood EOS levels. Methods: events (PAEs) is unclear. Methods: This was a post-hoc analysis of a 12-week,
Records of patients at least 12 years of age with at least two medical claims randomized, placebo (PBO)-controlled study (NCT00652002) of patients aged
with a primary or secondary diagnosis of asthma defined by ICD-9-CM code ≥12 years with moderate–severe asthma. After 2-week run-in with twice-daily
493.xx between January 2004 and July 2011, were extracted from the EMR- BUD 160 mg via pressurized metered dose inhaler (pMDI), patients received
Claims+ database (eMAX Health, White Plains NY) containing electronic med- twice-daily BUD/FM pMDI 320/9 mg, BUD pMDI 320 mg, FM 9 mg via dry-
ical records linked to insurance claims across 6 Midwestern states in the U.S. powder inhaler, or PBO. Worsening asthma event criteria were predefined
The date of first diagnosis was defined as the ‘index date’. Patients were required (PAEs; Drugs. 2006;66:2235-54). Postbronchodilator FAO status was assessed
to have at least 1 peripheral blood EOS test in the 12 month ‘assessment’ period at screening, weeks 2, 6, and 12 via forced expiratory volume (FEV1)/forced
following the index date. Patients’ asthma was classified as severe or non-severe vital capacity (FVC) ratio for patients who completed the study. This analysis
using intensity of treatment and level of asthma control during the assessment excluded patient withdrawals for any reason before week 2. Persistent FAO−
period, as recommended by the 2014 ERS/ATS guidelines. An elevated EOS (FEV1/FVC ≥ lower limit of normal [LLN]) and persistent FAO+ (FEV1/FVC
was defined as > 400 cells/mL. Chi-square tests were utilized to compare the 〈 LLN) patients retained their FAO status at all visits. FAO status of variable
proportion of patients with elevated EOS between the two severity groups. Mul- patients was not consistent on all visits. FAO status and withdrawals due to
tivariable logistic regression was used to assess the relationship between asthma PAEs were assessed. Results: In 258/389 patients (66%), FAO status was per-
severity and EOS, after controlling for potential confounders. Results: Among sistent throughout the study (135 FAO− and 123 FAO+). The remaining 131
the 2,164 patients with asthma and EOS test results in the assessment period, patients (34%) had variable FAO, changing status after screening. The per-
9% (n=184) had severe asthma according to ERS/ATS guidelines. A signifi- centage of patients with persistent FAO− (44%, 37%, 28%, and 30%), persist-
cantly greater proportion of patients with severe asthma had elevated EOS, ent FAO+ (30%, 29%, 35%, 33%), and variable FAO (26%, 34%, 38%, and
compared to patients with non-severe asthma (30% vs. 19%, p=0.0002). In 37%) differed in the BUD/FM, BUD, FM, and PBO groups, respectively. Over-
multivariable analysis, severe asthma was associated with an 83% increased all, persistent FAO− patients had fewer PAEs than FAO+ or FAO variable
odds of elevated EOS (Odds Ratio = 1.83, p=0.0005), compared to those with patients. The numbers of patients who withdrew due to PAEs in the persistent
non-severe asthma after adjusting for differences in patient demographic char- FAO− (n = 2, 4, 3, and 7), persistent FAO+ (n = 1, 4, 15, and 15), or FAO vari-
acteristics and comorbidities. Conclusion: An elevated EOS is associated with able (n = 6, 8, 15, and 12) classifications also differed for the BUD/FM, BUD,
nearly double the odds of severe asthma. FM, and PBO groups, respectively. Conclusions: Patients with moderate to
severe asthma treated with BUD/FM are most likely to remain persistent FAO−,
least likely to become FAO variable, and least likely to withdraw from the study
P49 if FAO+. Patients who were persistent FAO− vs persistent FAO+ or FAO vari-
REDUCING BEDSIDE EDUCATION TIME BY EXPANDING able had fewer withdrawals due to PAEs. Irrespective of FAO status, patients
PARENTAL ACCESS TO AN INPATIENT ASTHMA CLASS. receiving BUD/FM experienced the fewest withdrawals due to PAEs. Supported
H. Murphy*, D. Williams, J. Wolverton, M. Reddy, Kansas City, MO. by AstraZeneca LP
Background: Prior to 2011, patients admitted with asthma to this tertiary
care children’s hospital received bedside education from a registered respira-
tory therapist (RRT) with variable intensity and consistency. To address this
P51
EFFECT OF FIXED AIRFLOW OBSTRUCTION STATUS ON
problem, an Inpatient Asthma Class (IAC) was implemented three days a week
in 2011, which was increased to five days a week in 2014. Our specific aim PEAK EXPIRATORY FLOW AND RESCUE MEDICATION USE
was to evaluate the relationship between expanding parental access to an IAC IN RESPONSE TO BUDESONIDE/FORMOTEROL TREATMENT
and RRT time spent on bedside education. Methods: ORI determination was IN PATIENTS WITH MODERATE TO SEVERE ASTHMA.
obtained for non human subjects research. The study population included chil- B.E. Chipps*1, D. Tashkin2, M. DePietro3, F. Trudo3, 1. Sacramento, CA;
dren with asthma admitted from February 2011 to May 2014. RRT’s were asked 2. Los Angeles, CA; 3. Wilmington, DE.
to document in the electronic medical record (EMR) the amount of time spent Background: The effects of fixed airflow obstruction (FAO) on peak expi-
on bedside education with each family as: 〈15 minutes, 15 minutes, 30 min- ratory flow (PEF) and rescue medication (RM) use with budesonide/formoterol
utes, or 〉30 minutes. Data was extracted from the EMR to investigate RRT time (BUD/FM) in patients with moderate to severe asthma is unclear. Methods: In
spent on bedside education when the IAC was offered three days a week, com- a 12-week, double-blind, double-dummy, placebo (PBO)-controlled study
pared to five days a week. Analyses were performed in Stata 11.2 and Excel (NCT00652002), moderate to severe asthma patients aged ≥12 years were
(.xlsx) using chi-squares and differences in proportions. Results: About 100 randomized to twice-daily BUD/FM via pressurized metered dose inhaler
RRT’s provided bedside education for 2546 patients and their families during (pMDI) 320/9 mg, BUD pMDI 320 mg, FM dry powder inhaler 9 mg, or PBO
the study period. When the IAC was offered three days a week, 21% (469/2197) after a 2-week run-in with twice-daily BUD pMDI 160 mg. In a post-hoc analy-
of patients did not have documentation of time spent on education, similar to sis, postbronchodilator FAO status was assessed via forced expiratory volume
26% (91/349) who did not have documentation when the IAC was offered five in 1 second/forced vital capacity (FEV1/FVC) ratio at screening and weeks 2,
days a week. When the IAC was offered three days a week, 46% (787/1728) of 6, and 12 for patients who completed the study, excluding patient withdrawals
parents attended; whereas 61% (157/258) attended when the IAC was offered for any reason before week 2. Persistent FAO− (FEV1/FVC ≥ lower limit of
five days a week (p〈0.0001). When the IAC was offered three days a week, 33%
A38 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A39
ABSTRACTS: POSTER SESSIONS
normal [LLN]) and persistent FAO+ (FEV1/FVC〈 LLN) patients remained 6 months and peak flow meter measured at home. The main objective was to
FAO− or FAO+ throughout the study. FAO variable patients had inconsistent measure the ACT, the second objective was to assess mini-AQLQ, FEV1 and
FAO status at different visits. Percentage of patients with ≥30-L/min increase peak flow. Results: Mean age was 48 years. 65% were women. ACT <16: 10
in morning and evening PEF and ≥0.5-inhalation/d (inh/d) decrease in RM uncontrolled patients and between 16 and 19 ACT: 20 patients partially con-
use from baseline were evaluated. Results: Of 389 patients, 135 had persistent trolled. The mean duration of asthma was 11 years. Fifteen patientys received
FAO−, 123 persistent FAO+, and 131 FAO variable. More BUD/FM vs BUD, tiotropium, 10 patients Roflumilast and 5 theophylline. 3 patients discontinued
FM, and PBO patients, respectively, improved ≥30 L/min in morning PEF treatment during the 6 months. In all 3 groups improved ACT and mini-AQLQ
(55.3% vs 14.7%, 22.2%, and 11.1% for FAO−; 56.3% vs 18.5%, 5.9%, and (p <0.0001). The total values of lung function with tiotropium improved FEV1
6.7% for FAO+; 46.4% vs 21.9%, 16.2%, and 5.9% for FAO variable) and 2.46 ± 0.89 L at baseline to 2.60 ± 0.92 L at 6 months (p <0.0001); with rof-
evening PEF (51.1% vs 20.6%, 33.3%, and 7.4% for FAO−; 46.9% vs 11.1%, lumilast 2.50 ± 0.90 L at baseline to 2.63 ± 0.96 L at 6 months (p <0.0001);
8.8%, and 3.3% for FAO+; 39.3% vs 18.8%, 8.1%, and 8.8% for FAO variable). and 2.43 ± 0.84 theophylline L at baseline to 2.53 ± 0.91 L at 6 months (p
The percentage of patients decreasing RM use ≥0.5 inh/d was greater with <0.0001). PEF with tiotropium increased from 5.76 ± 2.38 to 6.22 ± 2.47 L /
BUD/FM vs BUD, FM, and PBO, respectively (57.4% vs 35.3%, 51.9%, and s (p <0.0001); with roflumilast increased from 4.65 ± 2.22 to 5.11 ± 2.32 L /
22.2% for FAO−; 65.6% vs 40.7%, 38.2%, and 43.3% for FAO+; 53.6% vs s (p <0.0001); and theophylline increased from 5.13 ± 2.17 to 6.01 ± 2.31 L /
53.1%, 40.5%, and 23.5% for FAO variable). Conclusions: The percentages of s (p <0.0001). Conclusion: It is premature to ensure that these drugs are safe
patients who experienced ≥30-L/min morning and evening PEF increases and and effective. We conclude that adding tiotropium, theophylline and roflumi-
≥0.5-inh/d decreased RM use were similar for BUD/FM in FAO+ and FAO− last achieves a better disease control, increases FEV1, PEF and improves qual-
patients and numerically greater than BUD, FM, or PBO, irrespective of FAO ity of life.
status. Increased responses occur with the combination of BUD and FM in
FAO+ patients. Supported by AstraZeneca LP
P54
CHRONIC COUGH WITH RESTRICTIVE CHANGES ON
P52 SPIROMETRY DIAGOSED AS HYPERSENSITIVITY PNEU-
A PERSISTENT ASTHMATIC PATIENT AFTER LOVEBIRD CON- MONITIS FROM EXPOSURE TO NYMPHICUS HOLLANDICUS
TACT: CASE REPORT. (COCKATIEL).
S. Kaygusuz, M. Nursoy*, A. Gedik, S. Uzuner, E. Cakir, Istanbul, Turkey. R. Harris*, Beverly Hills, CA.
Introduction and Aim: Asthma is chronic respiratory disease characterized This a case report of a 59 year old female presenting with a persistent severe
with recurrent episodes where environmental factors are important. An asth- cough of 10 months duration. She had multiple evaluations for asthma, GERD,
matic patient whose clinical and radiological findings persisted after lovebird and treament with multiple inhalers and antibiotics without response. History
contact was presented. Case: A nine-years-old allergic asthmatic patient was was negative for occupational exposures to known agents causing hypersensi-
admitted due to persistant cough and wheezing for 1 months. Her complaints tivity pneumonitis such as gases, paints (TDI) or other agents. There was no
increased after living with a lovebird at home. Her father, aunt, and cousins had history of emphysema in non smokers in her family and she is a lifelong non
asthma, tuberculosis (TB) contact wasn’t mentioned. Bilateral roncus and pro- smoker. When asked about pets previously she stated that she had no cats or
longed expiration were found in examination. Inflammation in chest X-ray and dogs. When questioned in detail about bird exposure such as pigeons close to
mite-allergy in prick test (eosinophil 3.9%, ImmunglobulinE 92 mg/dl) were her windows, etc,she stated that she had a Cockatiel that she purchased 12
determined. Asthma and allergic rhinitis were treated with inhaled steroid, long- months before her presentation to our office. On further history she stated that
acting beta-2 agonist, leucotrien antagonist, nasal steroid. Macrolid was given she was the one who cleaned the cage of droppings and that no mask was worn.
for atypical Mycobacteria. Symptoms persisted after two weeks of these ther- On physical exam she had no dyspnea she did have cough ( with no inspira-
apies. Computarized tomography revealed atelectasis, infiltrations and frosted- tory stridor), no clubbing, pO2=95, she had diffuse crackling breath sounds on
glass appearance. Extrinsic allergic alveolitis due to lovebird was thought. Bird auscultation. Her Spirometry showed FVC=59% predicted and FEV1=69%
feather specific IgE, Aspergillus antigen, Chlamydia and Mycoplasma serol- predicted. We ordered chest xray, arranged for a Spirometry with DLCO gas
ogy, and sputum cultures were negative, Quantiferon test was positive. Fiberop- exchange, titers for Chlamydia pneumonia and Mycoplasma pneumonia,hyper-
tic bronchoscopy was normal, ARB in BAL and gastric aspirates were nega- sensitivity pnuemonitis panel plus titers and precipitins for parrot/cockatiell (
tive. Anti-TB therapy was begun due to resistant clinical and radiological if available) and alpha 1- antitrypsin was considered if the above was negative.
symptoms and positive Quantiferon test. During the follow-up, Mycobacterium Unfortunately due to the expense after insurance the patient declined the test-
complex was obtained from BAL culture. Family screening was negative, after ing. She removed the Cockatiel from the home and within 3 months her cough
a while her adolescent neighbour had TB was told by the family. Clinical and totally abated. She declined followup spirometry and was lost to followup. In
radiological complete improvement was seen after therapy. Conclusion: The patients with chronic respiratory issues or chronic cough a thorough investi-
diagnosis of TB disease should be excluded in the patients where clinical and gation of pets, including birds, and fish ( we had one patient with HSPneu-
radiological symptoms and findings are resistant to therapy. monitis to silkworm powder used to feed fish). In this case she refused to do
diagnostic studies but our clinic suspicion was that her Cockateil and her expo-
sure to the cage droppings were considered highly likely to be the cause. There
P53 are studies showing Cockatiel to be an antigen stimulating precipitins.
POORLY CONTROLLED ASTHMA: NEW THERAPEUTIC McClusky, et.al. published on a case where a similar patient showed positive
OPTIONS. precipitating antibody to cockatiel dropping mix (CDM) .
J. Fernandez de Cordova Aguirre*, A. Velasco-Medina, D. Carino-
Cartagena, M.E. Arroyo-Cruz, S. Gonzalez Flores, G. Velazquez-Samano,
Mexico City, DF, Mexico. P55
PHARMACOKINETICS, SAFETY, AND TOLERABILITY OF FLU-
Poorly controlled asthma is diagnosed when despite high doses of inhaled
TICASONE PROPIONATE MULTIDOSE DRY POWDER
corticosteroids daily plus short and long acting β-2-agonists, and other thera-
pies, symptoms interfere significantly with daily activities, frequent exacer-
INHALER AND FLUTICASONE DISKUS® ADMINISTERED IN
bations need to be solved with the administration of corticosteroids, frequent HEALTHY SUBJECTS: AN OPEN-LABEL, RANDOMIZED,
emergency room visits or hospital admissions and the need for oral corticos- THREE-PERIOD CROSSOVER, SINGLE-DOSE STUDY.
teroids. Material and Methods: We performed a pilot, prospective, open study A.B. Vutikullird1, M. Gillespie2, S. Song2, J. Steinfeld*2, 1. Cypress, CA;
from June to December 2013. We included 30 asthmatic patients who signed 2. Frazer, PA.
informed consent and were over 18 years old. They were clasified according Introduction: Fluticasone (Fp), an inhaled corticosteroid, was approved in
to GINA in partly controlled or uncontrolled and treated with inhaled steroids 1993 for the maintenance treatment of asthma. It has well-established safety
at high doses plus long acting β-2-agonist. In the first visit we registered a and efficacy profiles and is available as a dry powder inhaler formulation and
spirometry with bronchodilator, asthma control test of 5 questions (ACT) and a hydrofluoroalkane inhalation aerosol. In the present study, Fp is delivered via
the quality of life of asthma (mini-AQLQ). We then indicated ICS and LABA a novel, inhalation-driven multidose dry powder inhaler (MDPI) that eliminates
plus tiotropium 2.5 mcgs a day or roflumilast 500 mcgs a day or theophylline the need to coordinate actuation with inhalation. Methods: This was a single-
200 mg every 12 hours. ACT were evaluated and mini-AQLQ once a month center, open-label, randomized, 3-period crossover, single-dose study in healthy
via phone and on 2 visits at 3 and 6 months, spirometry with bronchodilator at Japanese and Caucasian subjects aged 20-45 years, inclusive. Subjects (N=30)
VOLUME 113, NOVEMBER, 2014 A39
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A40
ABSTRACTS: POSTER SESSIONS
were randomized to 1 of 6 treatment sequences including combinations of 4 maintained through 30 minutes; recovery was complete for both groups at 60
inhalations of Fp MDPI 100 mg (total dose of 400 mg), Fp MDPI 200 mg (total minutes. Median time to recovery for AB MDPI was 5.07 minutes vs PBO,
dose of 800 mg), and Fp-DISKUS® (GlaxoSmithKline, Research Triangle Park, 30.07 minutes (p<0.0001). Adverse events (AEs) included severe migraine
NC) 100 mg (total dose of 400 mg). The primary objective was to assess phar- (n=1, PBO) and moderate sinus bradycardia (n=1, AB MDPI). No serious AEs,
macokinetics (PK) (maximum plasma concentration and time, terminal rate discontinuations due to AEs, or deaths occurred. Conclusions: AB MDPI pro-
constant and half-life for plasma elimination, area under concentration-vs-time vided clinically significant protection from EIB in adolescents and adults with
curve) for each treatment; safety and tolerability also were assessed. Results: a history of EIB. There were no safety issues with short-term AB MDPI use.
Over the range of all Fp doses evaluated, PK parameters were similar in Japan- This study was sponsored by Teva Pharmaceuticals.
ese and Caucasian subjects. Differences were observed between the systemic
exposures produced by each of the 3 doses, with the Fp plasma concentration-
vs-time curves being highest for the Fp MDPI 800 mg total dose and lowest for P57
the Fp DISKUS 400 mg total dose (Figure). The most frequently occurring RESULTS FROM TWO TRIALS EVALUATING THE POTENTIAL
adverse event was presyncope, which occurred in 2 Caucasian subjects, 1 treated EFFECTS OF FLUNISOLIDE HFA (AEROSPAN) ON GROWTH
with Fp MDPI 400 mg total dose and 1 treated with Fp MDPI 800 mg total dose. IN PEDIATRIC PATIENTS WITH MILD-TO-MODERATE
There were no clinical laboratory, electrocardiographic, vital signs, or physi- ASTHMA.
cal examination findings that were considered clinically significant. Conclu-
G. Bensch*1, L. Greos2, N. Ruiz3, J. Karafilidis3, 1. Stockton, CA;
sions: The PK profiles for Fp MDPI 400 mg, Fp MDPI 800 mg, and Fp DISKUS
400 mg were similar in Japanese and Caucasian subjects; however, there were 2. Centennial, CO; 3. Somerset, NJ.
differences in the systemic exposures dependent on total dose, with Fp MDPI Introduction: While recognized as the most effective maintenance treat-
800 mg being highest and Fp DISKUS 400 mg being lowest. The safety and ment for mild-to-moderate persistent asthma, inhaled steroids have the poten-
tolerability profiles of all treatments were consistent with the known profile of tial to cause growth suppression in children. Several studies performed with
Fp. This study was sponsored by Teva Pharmaceuticals inhaled corticosteroids demonstrated an impact on growth velocity (ranging
from -0.3 cm/yr to -1.8 cm/yr) with recent studies suggesting that this effect is
not reversible once treatment with the inhaled steroid is stopped. Two 1-year
trials were performed with flunisolide HFA (Aerospan), a small-particle inhaled
corticosteroid with a built-in spacer for the treatment of asthma in asthmatics
6 years and older, to evaluate growth velocity changes in pre-pubescent chil-
dren 4 to 11 years of age. Methods: The first study was an open-label, ran-
domized, 1-year safety study of flunisolide HFA, inhaled beclomethasone (BDP)
CFC, and inhaled cromolyn (as a negative control) in children 4 to 11 years of
age with mild-to-moderate asthma. The second study was a double-blind ran-
domized 1-year safety study of flunisolide HFA and placebo in children 4 to 9
years of age with mild-to-moderate asthma. Each study was analyzed simi-
larly for growth velocity (via stadiometry assessments) and change in height
over 1 year (measured as cm/yr). The dose of flunisolide HFA in both studies
was 160 mcg (2 puffs) twice daily, which represents the maximum FDA-
approved dose of flunisolide HFA for children. Results: In the open-label study,
206 patients age 6-11 years, were analyzed for growth and growth velocity.
Mean changes from baseline height were 6.2 cm for the flunisolide HFA and
cromolyn groups versus 5.1 cm for the BDP group. Mean growth velocity was
6.2 cm/yr for the flunisolide HFA group versus 5.3 cm/yr (BDP) and 6.9 cm/yr
(cromolyn). In the double-blind study, of 218 evaluable patients age 4-10 years,
the mean growth velocity was 6.01 cm/yr for flunisolide HFA versus 6.19 cm/yr
for placebo, a non-significant difference (P=.425). Conclusion: The results from
P56 two trials demonstrated that flunisolide HFA did not result in significant growth
A NOVEL ALBUTEROL MULTIDOSE DRY POWDER INHALER suppression in pre-pubescent pediatric asthma patients 4 to 11 years of age
IN ADULT AND ADOLESCENT PATIENTS WITH EXERCISE- when compared to placebo or the negative control (cromolyn).
INDUCED BRONCHOCONSTRICTION: A SINGLE-DOSE STUDY.
N. Ostrom*1, H. Taveras2, H. Iverson2, D. Pearlman3, 1. San Diego, CA;
2. Miami, FL; 3. Denver, CO. P58
Introduction: A novel, inhalation-driven, multidose dry powder inhaler INHALER-DEVICE SATISFACTION, SMOKING HISTORY,
(MDPI) has been developed that eliminates the need to coordinate actuation ALLERGIC RHINITIS AND ADHERENCE IN US ADULT
with inhalation and may reduce administration errors in comparison with con- ASTHMA PATIENTS: RELATIONSHIP TO HEALTH-RELATED
ventional metered-dose inhalers. Studies show that albuterol (AB) is effective OUTCOMES.
and well tolerated for the prevention of exercise-induced bronchoconstriction D. Price1, B. Harrow*2, L. Gever*2, J. Pike3, M. Small3, V. Higgins3,
(EIB). Methods: This single-dose, double-blind, 2-way crossover study 1. Aberdeen, Scotland, United Kingdom; 2. Somerset, NJ; 3. Macclesfield,
(NCT01791972) randomized adolescents and adults with EIB (≥20% fall from United Kingdom.
pre-exercise challenge FEV1) to treatment sequences AB MDPI 180 mg/placebo
Improving asthma control has focused on potentially modifiable clinical
(PBO) MDPI (n=19) or reverse sequence (n=19). IEC/IRB approval and
and behavioural characteristics including correct inhaler technique, allergic
informed consent from all subjects were obtained. FEV1 was measured at 30
rhinitis (AR), adherence and smoking. This research aims to establish these
minutes post-dose, 5 minutes before treadmill exercise challenge (baseline) and
relationships with asthma control, outcomes and quality of life. A US cross-
5, 10, 15, 30, and 60 minutes after exercise challenge. The primary efficacy
sectional survey of adult asthma patients seeking routine care, informed Par-
endpoint was maximum percentage fall from baseline in FEV1 up to 60 min-
tial Least Squares Path Modelling to quantify inner model relationships between
utes post-exercise challenge. Secondary efficacy endpoints included percent-
latent variables of patient-reported satisfaction of drug delivery, device func-
age of patients whose maximum percentage fall from baseline FEV1 post-exer-
tionality, device feedback, concomitant AR, adherence (Morisky Medication
cise challenge was <10% (protected by treatment) and time to recovery (from
Adherence Scale), smoking history, patient-reported outcomes (Asthma Con-
exercise challenge completion to the first measured post-challenge FEV1 within
trol Test, Jenkins Sleep Questionnaire, EuroQol-5D-3L) and physician-reported
10% of the pre-challenge baseline FEV1). Results: Age, gender, and baseline
asthma exacerbations in last 12 months. Patients not receiving inhaled main-
FEV1 were comparable between subjects in both sequences. Mean maximum
tenance therapy were excluded. 243 patients were included. All actual variables
percentage fall in FEV1 within 60 minutes post-exercise challenge for AB MDPI
were positively correlated with the appropriate latent variable. Cronbach’s Alpha,
was 6.21±1.44% (95% CI, 3.28%-9.14%) vs PBO, 22.38±1.44% (95% CI,
a measure of consistency for a group of variables, measured at least 0.659 for
19.44%-25.31%; p<0.0001). Thirty-two (84.2%) AB MDPI subjects had a <10%
latent variables indicating that the hypothetical variables of inhaler satisfac-
maximum FEV1 fall post-exercise challenge vs 6 (15.8%) PBO subjects. Pro-
tion, smoking history, concomitant AR, adherence and outcomes were well
tection with AB MDPI was significant (p<0.001) vs PBO within 5 minutes and
reflected by the composition of the actual variables in the dataset. Cross-load-
A40 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A41
ABSTRACTS: POSTER SESSIONS
ings were also supportive of the hypothesized outer model. Better patient out-
comes were significantly associated with patient satisfaction regarding drug
P60
CHILDHOOD OBESITY IN DIFFICULT TO CONTROL PEDI-
delivery attributes related to the inhaler (p=0.002). A negative smoking his-
tory coupled with absence of concomitant AR were also significantly associ- ATRIC ASTHMA PATIENTS IN A TERTIARY PEDIATRIC SUB-
ated with better patient outcomes (both p<0.001). Improved adherence did result SPECIALTY CLINIC.
in enhanced outcomes, but this relationship was not statistically significant Y. Hamzavi Abedi*, A.M. Perkins, M.B. Morales, Norfolk, VA.
(p=0.060). The R2 value for outcomes was 14.6% and pseudo goodness of fit, Introduction: It is important to identify clinical features associated with
measuring overall prediction performance of the path model, was 20.56% indi- asthma for the development of new interventions to be most effective. Our clin-
cating a fifth of the variance was explained by this model. Improving patient ical observation suggested the hypothesis that the proportion of overweight/obe-
satisfaction with inhaler drug delivery parameters represents one modifiable sity is significantly higher in difficult to control (DTC) than in well-controlled
aspect of asthma management contributing to better control. Interventions based asthmatics. Methods: This was a retrospective chart review of 100 patients,
on improved recognition of impact of severe AR, allergy phase and smoking aged 5 to 18 years, who were seen in a CHKD or one of the CSG Allergy out-
on patient’s asthma control are also likely to have a positive impact on asthma patient clinics between 5/1/2013 and 3/31/2014, and diagnosed with asthma.
patient health-related outcomes. Cases (n = 50) were identified as severe persistent DTC asthmatics based on
their required high dose of ≥1000 mg/day of inhaled corticosteroids (ICS). The
control group (n = 50) included subjects with well-controlled mild or moder-
ate persistent asthma defined by a dose of ≤ 500 mg/day of ICS. A subject’s
weight status was classified by the BMI percentile for age as normal weight
(BMI < 85%), overweight (BMI 85-94%), or obese (BMI ≥ 95%). The chi-
square test was used to assess the relationship between overweight / obesity
status and DTC asthma status. IRB and HRC approval and waivers of consent
and authorization to access protected health information were obtained. Results:
The BMI percentile in the DTC asthma group was significantly higher than in
the well-controlled group (75.74 ± 25.63 vs. 51.69 ± 24.43, p < 0.001). 36 %
of the DTC asthmatics were obese (vs. 0% of the well-controlled asthmatics,
p < 0.001), 14% overweight (vs. 10% of the well-controlled asthmatics, p =
0.99) and 50% normal weight (vs. 90% of the well-controlled asthmatics, p <
0.001). Mean age in the DTC asthmatics was 13.2 ± 3.3 vs. 10.0 ± 3.2 in the
well-controlled group (p < 0.001). Notably, a significant difference was observed
in the race between the DTC and the well-controlled asthma group. 74% of the
DTC asthmatics were African American (AA) (vs. 30% AA in the well-con-
trolled asthma group, p < 0.001), 14% were White (vs. 66% in the well-con-
trolled group, p < 0.001). There was no significant difference in gender between
the DTC and well-controlled asthmatics. (Table 1). Conclusion: The results of
this study suggest that there is a significant association between obesity and
severe persistent DTC asthma. This finding underlines the need for new treat-
ment approaches for DTC asthmatics involving a simultaneous treatment of
P59 asthma and obesity.
EVALUATION OF RECURRENT RESPIRATORY INFECTIONS
IN PATIENTS WITH ALLERGIC RHINITIS, ASTHMA, AND/OR TABLE 1. Demographics by difficult to control asthma status
COPD PRE- AND POST-TREATMENT WITH BACTERIAL
LYSATE VACCINES.
A.M. Koatz*, Buenos Aires, Argentina.
Introduction: Recurrent acute infections of the upper and lower airways are
frequent and often require multiple therapies. This is especially true for patholo-
gies such as allergic rhinitis and/or asthma and/or COPD. The etiology of recur-
rent infections is generally viral, but the additional complication of bacterial
infection worsens the symptoms of the underlying pathology. For these rea-
sons, preventive measures should be considered when treating acute infections.
Methods: a randomized, double-blind, placebo-controlled clinical trial was con-
ducted. Patients aged 16-65 years who had not received a lysate vaccine in the
previous year were included. Eighty-four (84) patients were randomly assigned
to 2 groups of 42 subjects each one :- Group A (active) – receive either OM-
85 bacterial lysate vaccine capsule or equivalent placebo. Capsules were admin-
istered daily for 10 consecutive days per month for a duration of 3 consecutive
months..Group C (healthy controls) serologic studies were performed in 10
subjects. Serum and secretory IgA levels were determined before and after
treatment along with symptom score and the number of infections and exac-
erbations. Written informed consent was obtained from all study participants.
Results: Eighty-four (84) patients were enrolled and 42 patients that received
OM-85 had a decrease in the number of recurrent infections from 82% to 45.5% SD – standard deviation; a P value calculated using two-sample t test; b P
(p< 0.05) compared to 78.9% in the placebo group. Similarly, the exacerba- value calculated using Fisher’s exact test; c P value calculated using chi-
tions of the underlying pathology decreased from 65.7% to 34.9% with OM- square test
85 versus 62.3% in the placebo group (p<0.05) There was also a substantial
reduction of the symptoms of the underlying pathology. (p<0.01) A signifi-
cant increase in serum and secretory IgA levels was observed only in the OM- P61
85 group (both p<0.001) during which parallels the 3 cycles of therapy. Con- INHALED MOMETASONE FUROATE-INDUCED ADRENAL SUP-
clusion: This study demonstrated a clinical benefit of OM-85 for reducing PRESSION IN AN ADOLESCENT.
reinfections and exacerbations in patients with allergic rhinitis and/or asthma M. Hanna*1, D.P. Mack2, 1. Oakville, ON, Canada; 2. Burlington, ON,
and/or COPD. The use of OM-85 lead to an increase in serum and secretory Canada.
IgA levels which provides a new perspectives regarding the immunological Introduction: High dose inhaled corticosteroids have been increasingly rec-
mechanism of action, namely immunostimulation and immunodesviation. Fur- ognized to cause adrenal suppression. Patients reported in the literature typi-
ther investigation is warranted to better understand these encouraging outcomes. cally have presented in the first decade of life. We report on the first case of
VOLUME 113, NOVEMBER, 2014 A41
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A42
ABSTRACTS: POSTER SESSIONS
mometasone furoate (MF) induced adrenal suppression on MF therapy. Case with antibiotics and oral corticosteroids. Chest x-rays were clear in January and
Description: A sixteen-year-old female with asthma and allergic rhinitis since March, 2014. She was started on inhaled fluticasone-salmeterol by a pulmo-
the age of five was initially maintained on a regimen of FP 500mcg per day nologist and referred for allergy evaluation after minimal improvement of res-
and MF nasal spray 50-100 mcg per day. As she had uncontrolled symptoms piratory symptoms. She had a course of allergen immunotherapy in the early
she was changed to MF/formoterol fumarate 800/ 20 mcg per day in addition ‘90s and surgery to remove nasal polyps in 1992. Findings: On initial visit, she
to her nasal spray. She was more stable in follow-up but presented with increas- had end-expiratory wheezing auscultated in the right lung. FEV1 was 100%,
ing fatigue, weight loss and nausea. She also reported striae. Extensive initial and FeNO was 30 ppb. Allergy skin tests were positive to multiple inhalant
hospital investigations were normal. A random glucose was 5.0 (3.4-7.0) and allergens. In-office nasopharyngoscopy showed purulent sinus discharge and
an AM cortisol was reported at < 50 nmol/L (170-540). She was started on scarring from previous nasal surgery. She was treated with cefdinir and started
hydrocortisone therapy and changed to ciclesonide, as well as montelukast on inhaled budesonide, montelukast, mometasone intranasal sprays, sinus irri-
and formoterol. Her energy and weight have improved after initiation of replace- gations, and allergen immunotherapy. Her cough improved somewhat after cef-
ment hydrocortisone therapy with plans for an ACTH stimulation test after dis- dinir, but she reported a persistent nighttime cough and had end-expiratory
continuation of oral corticosteroids. Discussion: While inhaled FP has been wheeze on exam on follow-up. In May 2014, CT chest showed calcified gran-
most commonly implicated in adrenal suppression, to our knowledge this is the uloma in the intra-inferior aspect of the right lower lobe. Subsequent bron-
first reported case of symptomatic MF-induced adrenal suppression. Despite choscopy identified a foreign body (suspicious for peanut) that was removed
having high protein binding, we hypothesize that the pharmacokinetics of MF from the right bronchus intermedius. Pathology reported a foreign degraded
with a high receptor affinity, long half-life and decreased hepatic clearance organic material. The patient subsequently recalled an episode of choking on
when used at a high dose result in similar adrenal suppression as has been peanuts in January 2014. Conclusion: This is a report of an adult with previ-
reported in FP. Physicians need to remain aware of the possibility of adrenal ously diagnosed allergic asthma, rhinitis, and nasal abnormalities that con-
suppression in any patient on high dose inhaled corticosteroid. founded the diagnosis of FBA. Although initial history and diagnostic evidence
did not suggest FBA, FBA should be considered in adult patients with persist-
ent wheezing unresponsive to asthma therapy. CT imaging and bronchoscopy
P62 are sometimes necessary for a conclusive diagnosis.
EFFICACY OF FLUNISOLIDE HFA (AEROSPAN) IN ADULT AND
ADOLESCENT PATIENTS 12 YEARS AND OLDER WITH
ASTHMA BY BASELINE INHALED STEROID. P64
L. Greos*1, J. Corren2, N. Ruiz3, J. Karafilidis3, 1. Centennial, CO; 2. Los EYE SYMPTOMS CORRELATE WITH ASTHMA SEVERITY.
Angeles, CA; 3. Somerset, NJ. M. Chen*1, E. Rael2, 1. State College, PA; 2. Hershey, PA.
Introduction: Inhaled steroids (ICSs) are the most effective maintenance Rationale: Eye symptoms are commonly seen in patients with allergic
treatment for mild-to-moderate persistent asthma. Flunisolide HFA, a small asthma and the combination can have significant effects on quality of life and
particle ICS with a built-in spacer, is approved for treatment of asthma in patients work productivity. Common allergic eye conditions include allergic conjunc-
12 years and older at doses of 160 mcg (2 puffs) and 320 mcg (4 puffs) BID. tivitis, vernal keratoconjunctivitis and atopic keratoconjunctivitis. Here we
Efficacy and safety comparisons to each patient’s prior ICS offer important report amongst a cohort of asthmatics at a university based allergy, asthma, and
perspective. Methods: This was a multi-center, double-blind, placebo-controlled immunology specialty clinic, correlations between subjective eye symptoms
trial consisting of a 2-week run-in with flunisolide CFC (500 mcg BID), fol- and asthma symptoms. Methods: After informed consent and IRB approval,
lowed by double-blind treatment with placebo, flunisolide HFA (80, 160 and 370 asthmatics, recruited to the study between 2011 and 2014, underwent
320 mcg BID), or flunisolide CFC (250, 500 and 1000 mcg BID) for 12 weeks clinical assessment including review of the Eye Symptom Score as part of the
in patients 12 and older with mild-to-moderate asthma. The primary efficacy mini RQLQ score, the total mini RQLQ score, and ACQ quality of life asthma
endpoint was change from baseline in % predicted FEV1. A retrospective analy- symptom score to determine whether there is a correlation between eye symp-
sis of the primary efficacy endpoint by baseline ICS (all patients were previ- toms and asthma severity. The mean assessment divided the cohort by ACQ
ously treated with an ICS) was performed to evaluate potential differences in scores into group 1, low risk asthmatics for future asthma events in the next 2
efficacy in patients previously treated with another ICS. The most commonly weeks as demonstrated by ACQ < 1.50 and group 2, high risk asthmatics for
used previous ICSs were: fluticasone (FP-195 patients), beclomethasone (BDP- future asthma events in the next 2 weeks as demonstrated by ACQ > 1.50.
190 patients), triamcinolone acetonide (TAA-174 patients) and flunisolide Results: Group 1 asthmatics represented 243 subjects and group 2 asthmatics
(FLN-98 patients). Patients were required to be on a stable dose of ICS for at represented 127 subjects. Subjects in group 1 had a mean mini RQLQ eye symp-
least 30 days prior to trial entry. Results: Of the 669 randomized patients, 548 tom score of 4.4 in comparison to a higher score of 7.1 amongst group 2 sub-
(82%) completed the trial. Compliance was >90% at all visits in each treatment jects. The average total mini RQLQ score in group 1 subjects was 25.9, versus
group. Patients experienced about a 12% improvement in FEV1 after the 2- 41.9 amongst group 2 subjects. Conclusions: This study shows that patients
week run-in with flunisolide CFC. After 12 weeks of treatment, patients treated who have higher immediate risk for asthma flares concurrently have higher
with flunisolide HFA 160 mcg BID maintained the 12% improvement achieved ocular and total upper airway symptoms scores further validating the one air-
during run-in, patients treated with 320 mcg BID had a 0.4% improvement over way hypothesis. Further studies are necessary and future research could assess
run-in, and patients treated with placebo had a 4.5% decrease (p<0.007; active whether there are different ocular phenotypes associated with asthma severity.
HFA treatments vs placebo). LS mean changes from baseline in % predicted
FEV1 did not significantly differ based on previous ICS, with the most sig-
nificant improvements seen with the 160 and 320 mg BID doses of flunisolide P65
HFA compared with placebo. Conclusion: The results from this retrospective SERUM LEVELS OF VITAMIN D AND IGE IMMUNE RESPONSE
evaluation by baseline ICS suggest that the efficacy with flunisolide HFA 160 TO ALLERGENS IN PEDIATRICS ASTHMATIC CHILDREN:
and 320 mcg BID is at least equivalent to other ICSs, as demonstrated by sim- CONTROVERSIAL RESULTS FROM A POOR CARIBBEAN
ilar % improvements in FEV1 for each of the baseline ICS subgroups. COLOMBIAN COMMUNITY.
E. Egea*1, G. Garavito de Egea1, L. Fang1, G. Egea1, L. Visbal1,
N. Lecompte1, J. Escamilla2, 1. Barranquilla, Colombia; 2. Cartagena,
P63 Colombia.
PEANUT ASPIRATION IN AN ADULT WITH ALLERGIC
Background: Humans have the ability to synthesize vitamin D during the
ASTHMA.
action of ultraviolet (UV) radiation upon the skin. The term “vitamin D insuf-
A.P. Nguyen*, K.G. Clay, S.M. Fineman, Atlanta, GA. ficiency” has been associated with asthma. However, little is known about the
Rationale: Foreign body aspiration (FBA) occurs more commonly in chil- link between total and serum specific IgE levels and vitamin D in asthmatic
dren than adults. Diagnosing FBA in adults with allergic asthma and allergies children. Today dust mite allergens and cockroach are the most important sources
is challenging because patients may not remember choking and there may be of clinically relevant allergens sensitizing patients with asthma in the tropics,
confounding symptoms. Case: A 41 year old female with history of allergic Objective: To investigate the relevance of Vit D levels on the total Ig E and
asthma, rhinitis, and nasal polyps was seen for evaluation in March 2014. She allergen-specific sensitization(Cr and Mite) in asthmatic children living a poorer
complained of cough and intermittent wheezing that had worsened since Thanks- communities within a Barranquilla, a city on the Colombian Caribbean Coast.
giving 2013. Her symptoms began with bronchitis that developed into chronic Method: A case-control study with 1000 individuals, which included 500 asth-
wheeze and productive cough; she had minimal improvement after treatment matic children and 500 healthy children from the Colombian Caribbean coast
A42 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A43
ABSTRACTS: POSTER SESSIONS
was made. Serum 25-hydroxy vitamin D was measured by a EIA. Total IgE, Baseline risk factors associated with >400 blood eosinophils/ml
specific IgE to Dermatophagoides farinae-D f- and Blomia tropicalis-B t.-
and Periplaneta americana –Cr-were determinated by ELISA (ImmunoCAP ®
Phadia AB, Sweden technology). The independent effects of these variables
were estimated from obtaining odd ratios (OR) trough logistic regression mod-
els adjusted for sex and age. Results: Elevated total IgE (> 100UI/mL) were
observed in both study group. Showing as a risk factor for susceptibility to
childhood asthma (OR = 1.63, 95% CI = 1.08 - 2.46). Serum levels of vitamin
D were found normal or insufficient in both groups (52.21 ng / mL and 52.2
ng / mL, P = 0.907). Also, insufficient vitamin D was associated with elevated
levels of Total Ig E (15% vs 8.7%, P = 0.037); showing a negative correlation
(Spearman r = -0.28, p = 0.00). However, our data is not clear regarding what
effect it may have the insufficient levels of vitamin D on the IgE immune
response (OR = 1.84, 95% CI = 0.9 - 3.6). On the other hand, elevated Total
IgE levels were associated with specific IgE sensitization to B. tropicalis, D.
farinae and P. americana. Conclusion: Despite the growing evidence of the role
of vitamin D in incident asthma and asthma exacerbation, studies are not all
consistent Taking together our results are showing that insufficient serum lev-
els of vitamin D is not a risk factor for developing asthma in poores comuni-
ties children of the Caribbean area.
(Reference category=1.00)
P67
CORRELATION BETWEEN GASTROESOPHAGEAL REFLUX
DISEASE AND ASTHMA SYMPTOMS.
A. DeWaters*1, M.P. Henao2, E. Rael2, 1. Hummelstown, PA;
2. Hershey, PA.
P66 Rationale: Gastroesophageal reflux disease and asthma are both among the
IDENTIFYING RISK FACTORS ASSOCIATED WITH ELEVATED most common diseases treated in the outpatient setting. Studies suggest that
BLOOD EOSINOPHIL COUNTS IN PATIENTS WITH ASTHMA asthma and gastroesophageal reflux disease are comorbid conditions and con-
FROM PRIMARY CARE CLINICAL RECORDS. trol of gastroesophageal reflux disease may lead to improvement of asthma
D.B. Price*1, E.R. Bleecker2, J.D. Campbell3, C.J. Corrigan4, I.D. Pavord5, symptoms. Therefore, it was hypothesized that the presence of gastroesophageal
A. Rigazio6, A. Burden6, J. von Ziegenweidt6, V.L. Ashton6, G.H. Gopalan7, reflux disease would be associated with less control of asthma symptoms. Here
M. Buatti Small7, 1. Aberdeen, United Kingdom; 2. Winston-Salem, NC; we report the correlation between the presence of gastroesophageal reflux dis-
ease and the severity of asthma symptoms, as measured by the Asthma Con-
3. Denver, CO; 4. London, United Kingdom; 5. Oxford, United Kingdom;
trol Questionnaire. Methods: After informed consent and IRB approval, 389
6. Cambridge, United Kingdom; 7. Frazer, PA. asthmatics recruited to the study between 2011 and 2014 underwent clinical
Introduction: A previous study concluded that blood eosinophil counts in assessment including review of the ACQ quality of life, and assessment of
patients with asthma could be used as an indicator of prospective asthma out- gastroesophageal reflux disease. The independent sample t-test divided the
comes. We aimed to identify risk factors associated with elevated blood cohort by ACQ scores into group 1 (ACQ < 1.50) and group 2 (ACQ > 1.50).
eosinophil counts in patients with asthma from UK primary care clinical records. Results: 63 percent of 257 asthmatics in group 1 reported having a diagnosis
Methods: Retrospective, observational study using the Clinical Practice of gastroesophageal reflux disease versus 65 percent of group 2 subjects. Group
Research Datalink and the Optimum Patient Care Research Database. Patients 1 asthmatics with gastroesophageal reflux disease had an average ACQ score
were aged 12-80 years with asthma and no other chronic respiratory disease. of 0.63, whereas group 1 asthmatics without gastroesophageal reflux disease
Study period was 1 year before (baseline period) date of last recorded blood had an average ACQ score of 0.56. Group 2 asthmatics with and without gas-
eosinophil count. Comparison at date of last recorded blood eosinophil count: troesophageal reflux disease had an identical average ACQ score of 2.6. Con-
≤400 eosinophils/ml (low) vs. >400 eosinophils/ml (elevated). Baseline char- clusion: Among asthmatics with well-controlled symptoms, the presence of
acteristics: biomarkers, demographics, comorbidities and markers of disease gastroesophageal reflux disease resulted in a slightly increased ACQ score.
severity. Univariable logistic regression was used to identify baseline charac- However, among asthmatics with uncontrolled symptoms, the presence of gas-
teristics associated with >400 eosinophils/ml (p≤0.05). These characteristics troesophageal reflux disease did not result in any increase in the ACQ score.
were then included in a multivariable model and reduced to a list of noncollinear There was no statistically significant correlation between the presence of gas-
factors. Results: Of 130,248 patients, 16% had >400 eosinophils/ml. Thirty- troesophageal reflux disease and more severe asthma symptoms in patients with
nine percent of the patients with ≤400 eosinophils/ml and 31% with >400 were uncontrolled asthma.
male. Median age (Interquartile range) was 45 (31-61) and 50 (37-63) for ≤400
and >400 eosinophils/ml, respectively. Table shows baseline risk factors asso-
ciated with >400 eosinophils/ml (Reference category=1.00). Conclusion: In this
study, several clinical and demographic features were predictive of elevated
P68
ASSOCIATION BETWEEN ASTHMA CONTROL AND BODY
blood eosinophil counts in asthma patients. These data could be used to strat- MASS INDEX IN ASTHMATICS.
ify patients who could benefit from more intensive and/or targeted asthma ther-
apies, potentially improving control and reducing costs. P.K. Gleeson*, E. Rael, Hershey, PA.
Rationale: Emergency room visits and hospitalizations due to acute asthma
exacerbations result in substantial healthcare costs and loss of productivity in
the workforce. Although hospitalizations and deaths due to asthma have steadily
declined since the 1980s, asthma prevalence is increasing. Obesity is also on
the rise, and several studies have shown that obesity is a risk factor for asthma
and poor asthma control. The Asthma Control Questionnaire (ACQ) is a vali-
VOLUME 113, NOVEMBER, 2014 A43
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A44
ABSTRACTS: POSTER SESSIONS
dated instrument for measuring asthma control in adults, with a score greater
than 1.5 predicting a higher risk of visiting an emergency department in the
P70
TRENDS IN THE USE OF ASTHMA MEDICATIONS IN MEXICO.
subsequent two weeks. We hypothesized that in a cohort of asthmatics at a
university-based allergy, asthma, and immunology specialty clinic, body mass M. Becerril-Angeles*, M. Vargas-Becerra, J.L. Estrada-Aguilar,
index (BMI) would correlate with ACQ score. Methods: After informed con- V. Borja-Aburto, Mexico City, DF, Mexico.
sent and IRB approval, 356 asthmatics recruited to the study between 2011 and Introduction: Asthma guidelines recommend controller medications for per-
2014 underwent clinical assessment including review of BMI and ACQ-7 scores. sistent asthma, plus short-acting bronchodilators in case of symptoms. It has
The independent sample t-test divided the cohort by ACQ scores into group 1 been shown a greater use of rescue medications than controllers, which asso-
(ACQ < 1.5) and group 2 (ACQ > 1.5). Results: Groups 1 and 2 had 236 sub- ciates with poor asthma control. The Instituto Mexicano del Seguro Social
jects and 120 subjects, respectively. The average ACQ score for group 1 was (IMSS) provides medical care to 58 million people and has a group of med-
0.6, and for group 2 was 2.6. Group 1 had a lower average BMI (27.1, 95% CI ications for asthma treatment. Objective: To know the trend of the use of con-
26.2 – 28.0) than Group 2 (29.9, 95% CI 28.2 – 31.5). Conclusions: Asthmat- troller, rescue and emergency medications for asthma during a 6-year period.
ics with ACQ scores less than 1.5 had a lower BMI than asthmatics with ACQ Methods: The use of controller (fluticasone, salmeterol/fluticasone, budes-
scores greater than 1.5. This finding contributes to the growing body of evi- onide/formoterol, beclomethasone, montelukast, zafirlukast), rescue (salbuta-
dence showing a link between BMI and asthma. Further research is needed to mol, salbutamol/ipratropium) and emergency (aminophyline, nebulized: salbu-
elucidate this relationship. tamol, salbutamol/ipratropium, beclomethasone and budesonide) medications
for asthma was analyzed according to the nationwide registries of the IMSS
from 2007 to 2012. Results: In the analyzed period, the rescue medications
P69 increased from 2,537,882 to 3,205,101 units (26.3%), and controllers from
IMPROVING DOCUMENTATION OF THE ASTHMA CONTROL 1,702,606 to 3,565,548 units (109.4%). The controllers with greater incre-
TEST™ USING PATIENT/CAREGIVER ELECTRONIC ENTRY. ment were: salmeterol/fluticasone (702%), montelukast (79%) and beclometha-
H. Murphy*, L. Harte, J. Parker, M. Reddy, 1. Kansas City, MO. sone (77%). Between 2010 and 2011 the trend in the use of controllers was
greater than that of rescue medications. In the emergency medications there
Introduction: The NHLBI recommends ongoing assessment of asthma con-
was a 56.8% decrease in the use of aminophyline, and a 320% and 244%
trol using a validated self-assessment questionnaire such as the Asthma Con-
increase in the use of salbutamol/ipratropium and budesonide, respectively. In
trol Test™ (ACT). Variable use and poor electronic medical record (EMR) doc-
2009 we developed and communicated our institutional asthma clinical prac-
umentation of the ACT prompted an organization-wide quality improvement
tice guidelines. Conclusion. Although both types of medications for chronic
project. Methods: Use of the ACT has been advocated for all children ≥4 years
asthma increased within the studied period, the trend in the use of controllers
presenting with asthma to clinics within this tertiary care children’s hospital.
greatly surpassed the increase in rescue drugs. As to the emergency medica-
In 2011, a process was initiated to facilitate consistent completion at outpatient
tions, the antiinflammatory drugs revealed an increased tendency. Spreading
visits and subsequent documentation in the EMR, with an iPad version of the
of the institutional asthma guidelines might partially explain these trends.
ACT created in 2012. Electronic data reports guided monthly assessment of
barriers. Plan-Do-Study-Act (PDSA) cycles facilitated local improvement.
Interventions were spread from the pilot clinic to a total of seven clinics in 2013.
Data was analyzed using Excel QI Macros. The Office of Research Integrity
P71
ASTHMA BASELINE FOR CHILDREN IN THE GEORGIA AND
determined that this project does not involve human subjects research. Results:
In 2011, age appropriate paper questionnaires were programmed to print out NORTH CAROLINA MEDICAID PROGRAM.
with registration paperwork for patient/caregiver completion. Providers man- K.E. Johnson*, J. Swann, N. Serban, Atlanta, GA.
ually entered calculated ACT scores into EMR-based Asthma Action Plans. In Research Objective: Pediatric asthma affects 10% of children age 0-10
September 2012, a pilot clinic began patient/caregiver completion of the ACT and 15% of middle and high school students and is a significant contributor to
on iPads with the score auto-populating the EMR. This clinic increased ACT morbidity in children covered by public insurance. To evaluate the impact of
documentation from an average of 17% to 75% by May 2014, with one month interventions, or to design interventions to have the greatest impact with lim-
as high as 92%. Iterative PDSA cycles focused on reducing variation and embed- ited resources, it is useful to understand the status quo within a system. This
ding process changes into daily activities. Survey results uncovered barriers. study uses retrospective Medicaid claims data to develop and quantify a set of
Provider support tools, such as pictorial EMR guidance, were created. Ongo- measures around pediatric asthma in Georgia geographically and over time.
ing refinement of electronic reports optimized the approach for identifying Methods and Data: The baseline measures were calculated using Medicaid
the appropriate patients for the iPad–based ACT. Sharing incremental results MAX claims data for children age 4-17 on Medicaid in Georgia and North Car-
fostered competition that drove improvement. The ACT was also set up on each olina from 2005-2009. We quantify asthma-related visits by race, age group,
exam room computer in case of a lapse in iPad connectivity. Once these location, provider type, and the costs of those services. We also identify patients
processes spread to six more clinics, the aggregate EMR documentation by all with persistent asthma and develop measures around medication adherence and
clinics improved to 62% by May 2014. Conclusion: Facilitating PDSA cycles the use of long term controller medication. We use ICD-9-CM codes to extract
aimed at addressing obstacles and adapting processes can improve completion the relevant data, and we generate measures within areas such as counties and
and documentation of the ACT. The goal of 75% was achieved and sustained by subpopulations. Results: The findings include a set of baseline measures for
for 12 months in the pilot clinic, but the overall goal of 90% for all clinics may pediatric asthma in Georgia and North Carolina 1) overall, 2) by geographical
depend on more direct engagement of providers. area, and 3) over time. For utilization, we find the highest percentage of patients
with an asthma diagnosis among blacks but the highest number of visits in the
population that is non-black and non-white. The number of patients per 1000
children decreases with age but the cost per visit increases slightly with age.
On treatment measures, we find no differences with respect to age but statis-
tically lower adherence to medication among the black patients. Measures of
utilization, cost, and treatment varied significantly across the state, with a few
areas identified as extreme on each. Some results varied over time. Conclu-
sions: Significant variations in pediatric asthma measures exist geographi-
cally within Georgia and North Carolina, and some measures show changes
over time. The cost measures tend to be higher in some urban and rural areas
and may be driven by different underlying factors.
The pilot clinic increased EMR documentation of the ACT from an average
of 17% to 45% by March 2013, but with wide variation in results. Iterative
PDSA cycles focused at reducing variation and embedding the process
changes into daily activities resulted in improvement to an average of 75% by
May 2014.
A44 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A45
ABSTRACTS: POSTER SESSIONS
P73
ALBUTEROL MULTIDOSE DRY POWDER INHALER IN
PATIENTS 12 YEARS AND OLDER WITH PERSISTENT ASTHMA:
12 AND 52 WEEK SAFETY.
C. LaForce*1, D. Miller2, H. Taveras3, H. Iverson3, C. O’Brien4, G. Raphael5,
1. Raleigh, NC; 2. North Dartmouth, MA; 3. Miami, FL; 4. Frazer, PA;
5. Bethesda, MD.
Introduction: A novel, inhalation-driven albuterol (AB) multidose dry pow-
der inhaler (MDPI) has been developed that eliminates the need to coordinate
actuation with inhalation. Methods: Subjects aged 12 years and older with
persistent asthma were enrolled in 1 of 3 studies: two 12-week, multicenter,
randomized, double-blind, repeat-dose, parallel-group studies (NCT01424813
and NCT01747629) to evaluate the efficacy and safety of AB MDPI 180 mg
vs placebo MDPI (PBO) administered 4 times a day (QID) and one 52-week
study (NCT01698320) that included a 12-week, double-blind phase during
which subjects were randomized to receive either AB MDPI 180 mg or PBO
QID followed by a 40-week, open-label phase during which all subjects received
AB MDPI as needed. Safety results from the 12-week phases of all 3 studies
were pooled for evaluation. IRB approval and informed consent from all sub-
jects were obtained. Primary efficacy endpoints are reported elsewhere. Results:
Overall, adverse events occurred in 50% of patients in the PBO group (n=333)
and 40% of patients in the AB MDPI group (n=321) during the pooled 12-week
dosing period; upper respiratory tract infections (11% PBO and 10% AB MDPI),
nasopharyngitis (6% and 5%), and headache (6% and 4%) occurred most fre-
quently. The incidences of β2-agonist–related events during the pooled 12-week
dosing period were low (<1%) in both groups. The most frequent adverse events
reported in patients treated with AB MDPI during the 40-week open-label phase
were nasopharyngitis (12%), sinusitis (11%), and upper respiratory tract infec-
tion (9%). There were no clinically meaningful trends in clinical laboratory
P72 variables and vital signs from screening to week 52 in those who remained on
SHORT-TERM IMPROVEMENT OF ASTHMA KNOWLEDGE IN AB MDPI for the entire study. There were no electrocardiographic findings
ASTHMATIC CHILDREN FOLLOWING ASTHMA CAMP ATTEN- considered clinically relevant in AB MDPI-treated subjects at any time point
DANCE. in the 52-week study; no subject had a QTc interval length (Bazett or Frideri-
J. Olsen*, M. Stevens, P. Foster, R. Hopp, Omaha, NE. cia) >500 msec at any time point. Conclusions: The safety profile of AB MDPI
in these studies was comparable to PBO and consistent with that of the well-
Introduction: Asthma camp allows children with asthma to participate in characterized profile of AB in subjects with asthma. This study was sponsored
camp activities while providing medical support to ensure a safe environment by Teva Pharmaceuticals.
for their camp experience. There is minimal data on the ability of asthma camp
to increase asthma knowledge in children with asthma. This study evaluated
the effectiveness of a local asthma camp in increasing asthma knowledge in
children ages 7-17 who have asthma. Methods: The Asthma Self-Management
P74
EFFICACY OF ALBUTEROL MULTIDOSE DRY POWDER
Questionnaire (ASMQ), previously validated in adults, was given to 40 chil-
INHALER VERSUS PLACEBO IN SUBJECTS 12 YEARS OF AGE
dren attending asthma camp. The survey was given on the first and sixth day
of camp. IRB approval and informed consent was obtained from all research
AND OLDER WITH PERSISTENT ASTHMA.
participants. Statistical significance was determined by a paired-samples t-test. G. Raphael*1, H. Taveras2, H. Iverson2, C. O’Brien3, D. Miller4, 1. Bethesda,
Results: Topics covered in the curriculum during asthma camp included the MD; 2. Miami, FL; 3. Frazer, PA; 4. North Dartmouth, MA.
definition of asthma, proper inhaler use, asthma symptoms and triggers, and Introduction: A novel, inhalation-driven, multidose dry powder inhaler
the difference between controller and rescue medications. Initial analysis of the (MDPI) has been developed that eliminates the need to coordinate actuation
full ASMQ demonstrated no significant change between pre- and post-camp with inhalation. Methods: Data from subjects 12 years of age and older with
scores (p = 0.14). Further analysis of the questions from the ASMQ that were persistent asthma who were enrolled in two 12-week, multicenter, random-
not covered in the curriculum during asthma camp was performed. There was ized, double-blind, repeat-dose, parallel-group studies (NCT01424813 and
no significant change between pre- and post-camp scores (p = 0.34). Analysis NCT01747629) were pooled to evaluate the efficacy and safety of albuterol
of the questions from the ASMQ that were covered in the curriculum during (AB) MDPI 180 mg compared with placebo MDPI (PBO) administered 4 times
asthma camp demonstrated a significant increase in the scores between pre- a day (QID). IRB approval and informed consent from all subjects were
and post-camp t(39) = 2.32, p < 0.05, with a mean score increase of 0.53, 95% obtained. Safety endpoints are reported elsewhere. The primary efficacy end-
CI for difference = 0.07 to 0.98. Conclusion: With improvement between pre- point was baseline-adjusted FEV1 area-under-the-effect curve over 6 hours post-
and post-camp test scores, our data suggests that asthma camp can improve dose (FEV1 AUC0-6) over 12 weeks. Results: AB MDPI-treated subjects (n=153)
short-term asthma knowledge in asthmatic children attending camp. It is not experienced significantly (p<0.0001) greater improvements in baseline-adjusted
possible to draw conclusions regarding which aspect of asthma camp led to FEV1 AUC0-6 compared with PBO subjects (n=163) over the 12-week study
the observed improvement. Asthma camp may provide opportunities for chil- period (AB MDPI, 1.20 L x hr vs PBO 0.33 L x hr; mean difference 0.87±0.10
dren to understand their disease better. Caution should be used when inter- L x hr). The mean change from baseline in FEV1 for the pooled population is
preting these results as the ASMQ has not been validated in children. Further shown in the Figure. Significant (p<0.0001) increases in baseline-adjusted
studies are needed to investigate other potential benefits that could be provided FEV1 AUC0-6 in AB MDPI-treated subjects were apparent on days 1 and 8 and
by attending asthma camp. maintained through day 85 compared with PBO subjects (mean differences of
1.06, 0.75, and 0.81 L x hr vs PBO for these 3 time points, respectively). Of
the 153 subjects treated with AB MDPI, 110 (72%) achieved a 12% increase
in FEV1 within 30 minutes postdose on day 1 with a median time to onset of
5.2 minutes, and median duration of effect (12% increase) of @3 hours for
one study and 4 hours for the other. Ninety-one AB MDPI-treated subjects
(59%) achieved a 15% increase in FEV1 within 30 minutes postdose on day 1
with a median time to onset of 5.4 minutes, and median duration of effect (15%
increase) of @2 hours for one study and 3 hours for the other. Conclusions:
AB MDPI was consistently superior to PBO over the 12-week treatment period
on spirometry-based measures. These data confirm that during periods of reg-
VOLUME 113, NOVEMBER, 2014 A45
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A46
ABSTRACTS: POSTER SESSIONS
ular usage over 12 weeks, AB MDPI continued to produce clinically signifi-
cant bronchodilation compared with PBO. This study was sponsored by Teva
Pharmaceuticals.
Mean Change from Baseline in FEV1
P75 P76
CUMULATIVE DOSE COMPARISON OF THE EFFICACY AND
IMPACT OF OBESITY ON PULMONARY FUNCTION: PROSPEC-
SAFETY OF ALBUTEROL-MULTIDOSE DRY POWDER
TIVE STUDY IN YOUNG ADULTS.
INHALER AND ALBUTEROL-HYDROFLUOROALKANE
S. Melendez*, B. Del Río, J. Del Río, E. Navarrete, Mexico City, METERED DOSE INHALER IN ADULTS WITH ASTHMA.
DF, Mexico.
D. Miller1, D. Wayne2, T. Ferro*3, H. Taveras2, H. Iverson2, 1. North Dart-
Asthma and obesity are chronic disorders, and are increased in prevalence mouth, MA; 2. Miami, FL; Frazer; PA.
among young people. It is proposed that obesity and overweight has an inde-
pendent effect on lung function in asthmatic patients. We barely know long- Introduction: Albuterol (AB) delivered via a novel, inhalation-driven, mul-
term obesity effects in this patients. Methodology: The study was conducted tidose dry powder inhaler (MDPI) eliminates the need to coordinate actuation
in our Hospital. The study group where obese or overweight with or without with inhalation. In a separate study, treatment of adolescents and adults with
asthma. It was performed spirometry with reversibility in a baseline measure- persistent asthma with AB MDPI was well tolerated and demonstrated efficacy
ment and after 5 years follow-up, besides weight, height and BMI (Body Mass significantly greater than placebo and comparable to AB hydrofluoroalkane
Index). Symptoms of asthma conducted through validated questionnaires: metered dose inhaler (HFA) at the intended doses of 90 and 180 mg. Methods:
ISAAC Questionnaire and Asthma Control Test. Results: We invited to partic- This multicenter, randomized, double-blind, double-dummy, cumulative-dose,
ipate 90 patients, of whom 5 decided not participate. 85 patients were included 2-period crossover study (NCT01056159) evaluated the efficacy, pharmaco-
but cannot schedule appointment to 35, because change of residence and phone kinetics (PK), extrapulmonary pharmacodynamics (PD), and safety of cumu-
number. We studied a total of 50 patients, of whom 33 realize spirometer, and lative doses (1440 mg) of AB via MDPI or HFA to subjects (aged 18-45 years;
17 is still pending. Institutional Review Board approval and informed consent N=47) with asthma. IRB approval and informed consent from all subjects were
was obtained from all research subjects.Of the 50 patients studied, 22 were obtained. Subjects were treated with AB MDPI or AB HFA (90 mg/inhalation)
women and 28 men, the average age, after 5 years of follow-up for both groups and respective placebo in a randomized-sequence, two-period crossover. At
was 18.7. Within the studied groups compared with the 5-year follow-up, sig- each treatment visit, study drug was administered by cumulative dosing of
nificant difference was observed: in weight (p= 0.000), height (p= 0.000) and 1+1+2+4+8 inhalations (separated by 30 minutes) from each device. Treatment
BMI (p= 0.000). In spirometric values, the comparison group at baseline and visits were separated by 3 to 14 days of washout. The primary efficacy end-
follow-up, significant differences was found in forced vital capacity (p= 0.000), point was baseline-adjusted FEV1 at 30 minutes after each of the cumulative
forced expiratory volume in one second (FEV1 p= 0.000), after bronchodila- doses. Results: Thirty-eight subjects received both AB MDPI and AB HFA and
tor FEV1 (p= 0.004), reversibility (p= 0.009), (PEF expiratory flow p=0.001).Of experienced increases in FEV1 over baseline at each cumulative dose level. The
the 50 patients evaluated, at the beginning of the follow up 12 patients (24%) differences between treatments in FEV1 at 30 minutes ranged from −0.07 to
had asthma. There were 6 patients who were monitoring newly diagnosed asthma −0.03 L and were not clinically meaningful. Mean systemic exposure over 14
(33%). Of the 18 asthmatic patients in total, we classify according to symp- hours was comparable (AUC0-t, 23,227 for AB MDPI and 20,939 for AB HFA),
toms, through the ACT questionnaire, 5 patients were in poor control, 7 with Cmax was higher for AB MDPI (4422.8 pg/mL) vs AB HFA (3303.8 pg/mL),
partly controlled asthma and 6 with well-controlled asthma. Initial asthmatic and Tmax occurred earlier with AB MDPI (2.48 h) vs AB HFA (3.05 h). Extra-
patients significant differences were found in weight and in spirometric values pulmonary PD differences between treatments were not considered clinically
in FVC, FEV1, and PEF (Table no. 1). Conclusion: In this study we found that meaningful. Adverse events reported by ≥5% of subjects treated with AB (cumu-
obese patients with asthma, they referred to be controlled and partially con- lative dose of 1440 mg) included tremor (17% AB MDPI and 13% AB HFA),
trolled. We found that obese asthma patients remained with better spirometric palpitations (9 and 2), and headache (9 and 4). Conclusions: The overall effi-
values compared to baseline values. In patients with newly found diagnosis cacy, PK, PD, and safety profile of AB MDPI and AB HFA were generally sim-
were in ranges of overweight and obesity. ilar. The results of this and previous AB MDPI studies support evaluation of a
dose of 180 mg in adults with asthma. This study was sponsored by Teva Phar-
maceuticals.
P77
POLYMORPHISM IN THE CD14 PROMOTER (CD14-C159T) IN
CRIMEAN ADULTS WITH EARLY AND LATE-ONSET ASTHMA.
Y. Bisyuk1, V. Beloglazov1, A. Dubovyi1, L.M. DuBuske*2, 1. Simferopol,
Ukraine; 2. Gardner, MA.
Introduction: The CD14 gene is located on chromosome 5q31-32, consid-
ered a critical region for asthma. The association of the CD14 C-159T SNP in
early and late-onset asthma patients remains to be determined. Methods: 262
early-onset and 69 late-onset persistent asthma patients were studied. Early-
A46 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A47
ABSTRACTS: POSTER SESSIONS
onset asthma was diagnosed when first episodes of symptoms occurred before dioxide, carbon monoxide and PM10), temperature and relative humidity, from
40 year old and late onset one after 40 according to GINA 2012 guidelines. The 2009 to 2013, were analyzed. IRB/HAC approval was obtained. Results: Dur-
control group included 285 non-atopic volunteers. Single nucleotide poly- ing these five years there were 5331 visits for asthma exacerbations, with an
morphisms of CD14 C-159T were detected by PCR. Patients and volunteers annual average of 1066. There was a gradual decrease in cases, from 2363 in
were recruited at the Crimean State Medical University, Simferopol, Crime, 2009 to 505 (21%) in 2013. There was a male predominance in all ages (ratio
and provided written informed consent for the genetic study. Results: In early- 1.7 : 1). The age groups 24-71 months and 6-12 years had the highest number
onset asthma patients CC genotype was detected in 74 patients, CT in 142 and of cases, 1766 (33.1%) and 1827 (34.3%), respectively. During fall there was
TT in 46; in late-onset asthma: CC in 31, CT in 27, and TT in 11; while in the the highest number of visits 2069 (39%), and the lowest was in spring, 801
control group CC in 97, CT in 146, and TT in 42. The allele frequencies were (15%). The correlation between asthma and environmental factors was: CO:
55 % (n=290) for the C allele and 45 % (n=234) for the T allele in the early- R=0.242, NO2: R=0.175, SO2: R=0.092, PM10: R=0.056, O3: R=-0.062, rela-
onset asthma c (OR, 1.19; 95% CI, 0.94-1.52; P=0.15); 64% (n=89) for the C tive humidity R=-0.106 and temperature R=-0.36. Conclusions: A gradual and
allele and 36% (n=49) for the T allele in the late-onset asthma (OR, 0.81; 95% significant reduction in the number of asthma visits to the emergency room
CI, 0.55-1.99; P=0.29); and 60% (n=340) for the C allele and 40% (n=230) was observed during the period of five years. There was a significant increase
for the T allele in the controls. Conclusion: CD14-C159T polymorphism is in asthma exacerbations related to seasonal effect. There was a predominance
not associated with adult early and late-onset asthma in Crimean population. of male pre-school and school children in relation to asthma exacerbations. The
The polymorphism in this population did not differ from that seen in healthy highest correlation between atmospheric pollutants and asthma cases was related
control subjects. to carbon monoxide. There was inverse correlation between asthma exacerba-
tions and weather factors (humidity and temperature).
P78
CLINICAL FEATURES OF ALLERGIC RHINITIS IN INTER- P80
MITTENT AND MILD PERSISTENT ALLERGIC ASTHMA. LAPSES IN ASTHMA CONTROL IN PATIENTS WHO CONTIN-
V. Tsybulkina1, N. Kurmaeva1, N. Tsybulkin1, L.M. DuBuske*2, 1. Kazan, UED VS. DISCONTINUED OMALIZUMAB IN A REAL-WORLD
Russian Federation; 2. Gardner, MA. SETTING.
Introduction: Allergic rhinitis (AR) is frequently encountered in patients G. Sun1, E. Antonova2, E. Chang1, M. Broder1, P. Solari2, J. Zazzali*2,
with atopic asthma (AA). The influence of allergic rhinitis on clinical symp- 1. Beverly Hills, CA; 2. South San Francisco, CA.
toms in asthmatics depends significantly on asthma severity. Methods: Con- Introduction: Little is known about benefits of continuous omalizumab
secutive patients 17-26 years of age with mild intermittent (MI) and mild per- (OMA) treatment to asthma patients in real world. We examined the lapses in
sistent (MP) allergic asthma were enrolled in the study with informed consent asthma control in patients who continued vs. discontinued OMA treatment in
obtained. Evaluation included lung function assessment, skin prick tests, bron- a real-world setting. Methods: This retrospective cohort study used a large
cho-provocation tests,(BPTs), bronchodilator (BDT) response, total and aller- HIPAA-compliant commercial healthcare claims database (1/1/08 to 12/31/10).
genspecific IgE levels. Results: Patients in both groups, 63 in MI and 72 in MP, Identified patients were ≥12 years old, had ≥2 medical asthma-associated claims,
had similar age(mean 19 years) and AA duration (mean 5 versus 6 years in MI filled ≥2 asthma controller medications in the identification period (1/1/09-
and MP groups) and were equally of rural and urban origin. Prevalence of per- 12/31/09), and used OMA continuously for ≥6 months. After ≥6 months of
sistent AR (P-AR) was significantly greater in MP asthma (54% in MI asthma OMA therapy, patients were stratified as continuers (continued OMA until
and 78% in MP asthma, p<0.05). Patients with persistent AR had on average dropout or 12/31/10) or early discontinuers (stopped OMA for >90 days) and
higher rate of exacerbations independent of asthma severity: more than 1 exac- followed for ≥3 months after the index date. The primary outcome was the risk
erbation per month occurred in 26% of patients with intermittent AR (I-AR) of lapse in asthma control during follow-up, reported as episodes per 100 patient-
or without AR versus 68% of patients with persistent AR (p<0.05) in the MI years (PY), measured as any asthma-related hospitalization or emergency room
asthma group. More then 1 exacerbation per month was seen in 44% of patients visit, ≥2 oral corticosteroid (OCS) or ≥6 short-acting beta-agonists filled in 1
with I-AR or without AR versus 86% of patients with P-AR (p<0.05) in the year. We used Cox regression models to assess risk of the outcome, adjusted
MP asthma group. Patients with persistent AR had much higher rates of symp- for baseline patient characteristics (e.g., demographics and the number of
toms in relation to overall dust load both in MP asthma (95% in P-AR patients chronic conditions). The study did not involve human subjects, thus IRB review
versus 25% in all others, p<0,05) and MI asthma (95% in P-AR versus 68% in was not needed. Results: We identified 414 continuers and 240 discontinuers
all others, p<0,05). In MI asthma patients presence of persistent AR was also among eligible patients; mean age: 46.2 years, 62.5% women, and 15.6% had
associated with a higher mean number of relevant non-specific triggers COPD. At baseline, the groups were balanced by demographics and asthma
(1.76±0.93 in P-AR versus 0.97±0,84 in all others, p<0.05), clinical reaction control. Patients were followed for a median 415 days; the discontinuers had
to cold air (27% in P-AR patients versus 3% in all others, p<0.05) and exer- no OMA use after the discontinuation date. Overall, there were 32.5 episodes
cise-related symptoms (81% in P-AR versus 48% in all others, p<0.05). Con- of lapses in asthma control per 100 PY of follow-up: 27.9 per 100 PY for con-
clusion: Allergic rhinitis has significantly higher prevalence in MP asthma. tinuers vs. 43.3 per 100 PY for discontinuers (p = 0.002, Table). Discontinuers
Patients with persistent allergic rhinitis have two-fold or higher rate of exac- had worse individual clinical outcomes that defined lapses in asthma control
erbations independent of asthma severity. Among non-specific asthma trig- than did continuers (Table). Adjusting for patient characteristics, discontin-
gers the most clinically relevant for all patients with persistent allergic rhinitis uers had a significantly higher risk of having lapses in asthma control than con-
was the total dust load. The number of non-specific asthma triggers was also tinuers (adjusted hazard ratio 1.66, p<.001). Conclusions: Real-world evidence
greater in patients with persistent allergic rhinitis in both mild intermittent and suggests that asthma patients who receive continuous (>6 months) OMA treat-
mild persistent asthma. ment may have fewer lapses in asthma control than those who prematurely
discontinue OMA after 6 months.
P79 Lapses in Asthma Control in Patients who Continued vs. Discontinued
CORRELATION BETWEEN ATMOSPHERIC POLLUTANTS, Omalizumab after ≥6 Months of Treatment
CLIME AND ASTHMA EXACERBATIONS IN CHILDREN OVER
A FIVE YEAR PERIOD IN MEXICO CITY.
C. Hernandez-Ramirez*, J. Vidal-Guzman, U. Angeles-Garay, A. Ortega-
Gonzalez, M. Becerril-Angeles, Mexico City, DF, Mexico.
Background: There is a relationship between atmospheric pollutants and
climatic factors and visits to the emergency room for asthma, however there is
lack of knowledge on the situation of this phenomenon in Mexico City. Objec-
tive. To assess the correlation of atmospheric pollutants and some climatic a Number of events per 100 patient-years
factors with the number of cases of asthma exacerbations in children in a third
level hospital in Mexico City during the last five years. Methods: Case reg-
istries of asthma exacerbations at pediatric emergency room, stratified by age
(0-23 months, 24-71 months, 6-12 years, 12-17 years), and their correlation
with daily values of atmospheric pollutants (ozone, sulphur dioxide, nitrogen
VOLUME 113, NOVEMBER, 2014 A47
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A48
ABSTRACTS: POSTER SESSIONS
P81 P84
INHIBITORY EFFECTS OF SALIDROSIDE ON INFLAMMA- EVALUATION OF GENES INVOLVED IN TRANSITION FROM
TORY RESPONSES IN RAT ALVEOLAR MACROPHAGES. AUTOIMMUNE DISEASE TO LYMPHOMA.
X. Hu*, Hangzhou, China. R. Anand*1, E. George2, M. Yu2, J.L. Ambrus2, L. Shen2, 1. Getzville, NY;
The genus Rhodiola is important herb used for thousands of years in Tra- 2. Buffalo, NY.
ditional Chinese Medicine for treating various kinds of diseases, including Introduction: There is a high incidence of secondary lymphomas in patients
inflammation-related diseases such as pneumonia, chronic bronchitis, asthma, with autoimmune diseases, especially Sjogren’s syndrome (SS). We have devel-
and rheumatoid arthritis. Salidroside (p-hydroxyphenethyl-beta-d-glucoside, oped an animal model, the IL-14alpha transgenic mouse (IL14aTG) that repro-
C14H20O7, molecular weight 300.30), which is one of the most potent ingre- duces all the features of SS seen in patients in the same relative time frame,
dients of the genus Rhodiola, has been reported to have a broad spectrum of including the development of lymphoma. We have evaluated genetic changes
pharmacological properties. Recent study indicates an anti-inflammatory role in the spleens of these mice during different stages of the disease to determine
for salidroside in lipopolysaccharide (LPS)-induced acute lung injury (ALI), when genes characteristic of SS lymphoma are aberrantly expressed in the
but the mechanisms of anti-inflammatory action are not clear. In the present animals with the disease. Methods: QPCR was performed on the splenic RNA
study, anti-inflammatory activity of salidroside was analyzed in vitro using of IL14aTG mice and control C57BL/6 mice for bcl-6 and bcl-10 at 6, 10 and
LPS-induced inflammatory reactions in rat alveolar macrophages. Inflamma- 14 months of age. In this animal model, disease involving the salivary and
tory mediators such as TNF-α, IL-6, and NO were measured by the Griess reac- lacrimal glands starts at 6 months of age while systemic disease starts at 10
tion for NO and Enzymelinked immunosorbent assay (ELISA) for other inflam- months of age. Some mice will start developing lymphoma at 14 months of age
matory mediators. QRT-PCR was used to measure the mRNA expression of while the majority of mice develop lymphoma only by 18-20 months of age.
TNF-α, IL-6, and iNOS, and the protein levels of iNOS, p65, p-p65, IκB-α, Results: In IL14aTG mice but not C57BL/6 mice, expression of bcl-6 and bcl-
and p-IκB-α were analyzed by western blot. EMSAs and reporter gene assays 10 decreased at 14 months of age, but not at earlier time points. None of the
were used to evaluate DNA binding and transcriptional activities of NF-κB. mice with these genetic changes had yet developed lymphoma.
ChIP analysis was used to detect the binding of p65 to the iNOS promoter.
NF-κB nuclear translocation was analyzed by western blot. Salidroside sig-
nificantly inhibited LPS-stimulated production of NO by suppressing the expres- P85
sion of iNOS. EMSA demonstrated that LPS treatment increased p65-DNA CUTANEOUS NON-TUBERCULOUS MYCOBACTERIAL INFEC-
binding, whereas this interaction was decreased by salidroside. ChIP analysis TION IN A PATIENT WITH SEVERE T-CELL LYMPHOPENIA
revealed that salidroside markedly inhibited LPS-induced p65 binding to the AND SELECTIVE IGM DEFICIENCY.
iNOS promoter. Western blotting confirmed that salidroside effectively inhib-
A. Gharib*1, A. Gupta Louis2, S. Agrawal2, S. Gupta2, 1. Los Angeles, CA;
ited the nuclear translocation of p65. We also examined the effect of salidro-
side on the induced degradation and phosphorylation of IκBα protein by LPS. 2. Irvine, CA.
The results showed that salidroside could change the kinetics of IκBα phos- Background: Detailed immunological analyses have not been reported in
phorylation and degradation. Salidroside also suppressed TNF- and IL-6 at recently recognized Non-tuberculous mycobacterial infection of the skin. The
the mRNA level, and then reduced the release of TNF-α and IL-6 induced by main purpose of this investigation is to present extensive immunological analy-
LPS. In conclusion, our results suggest that salidroside can block LPS stimu- sis of a patient with cutaneous non-tuberculous mycobacterial infection
lated inflammatory responses, and may be used as a potential anti-inflamma- (mycobacterium avium complex). Material and Methods: Peripheral blood from
tory agent for the prevention and treatment of inflammation-related diseases. the patient and healthy controls were analyzed for CD3+, CD4+, CD8+ T cells,
regulatory T cells (FoxP3+CD4+CD25+), naïve, transitional, marginal zone,
IgM memory, switched memory B cells and plasmablasts, expression of TACI
P82 and BAFF-R on naive and memory B cells, expression of IFN-γ receptor and
REGULATION OF AIRWAY EOSINOPHILIA IN A MODEL OF IL-12 receptor on lymphocytes and monocytes, NK cell phenotype and cytox-
FELINE ALLERGIC ASTHMA BY KTN0158, A HUMANIZED icity against K562 target cells using various effector:target ratio. Lymphocyte
ANTI-KIT MONOCLONAL ANTIBODY. functions were measured by in vitro response to mitogens (PHA, ConA, PWM)
and recall antigens (mumps, candidate, PPD, and tetanus toxoid) by 3H incor-
E.M. Mandel*1, C.R. Reinero2, R.W. Gedrich1, C. Chang2, J. Trzil2, poration. Toll-like receptors (TLR) were analyzed on monocytes. Results: Analy-
J. Dodam2, L.A. Cohn2, C. Lubeski1, Y. Hadari1, T. LaVallee1, 1. New Haven, sis of lymphocyte subsets showed severe T cell lymphopenia of CD3+, CD4+
CT; 2. Columbia, MO. and CD8+ T cells) and an impaired response to mitogens and antigens. T reg-
Immune response and pathologic events in allergic asthma are regulated by ulatory cells were significantly reduced. Analysis of B cells revealed low serum
specific T cell subsets and the cytokines that they secrete. Mast cells and IgM and an increased transitional B cells with normal marginal zone, IgM mem-
eosinophils are key effectors in the cascade of airway inflammatory events ory and class switch memory B cells, and marginal zone B cells. Expression
which induce bronchoconstriction, influx of inflammatory cells and airway of TACI and BAFF receptor on both naiive and memory B cells, and expres-
remodeling. KIT, the receptor for Stem Cell Factor (SCF), is expressed on mast sion of and IFN -γ receptor and IL-12 receptor on lymphocytes and monocytes
cells and eosinophils in the lung, and for that reason, we are examining inhi- were normal. TLR4 expression was increased, whereas the expression of TLR5,
bition of SCF/KIT signaling as a possible therapeutic in allergy and inflam- TLR7, and TLR9 was decreased. NK activity was found to be decreased. Con-
mation. KTN0158 is a humanized IgG1 monoclonal antibody that inhibits clusion: This patient illustrates that cutaneous non-tuberculous mycobacterium
signaling through KIT. This antibody specifically binds the Ig-like domain 4 infections may be associated with severe immune deficiency including T cell
of KIT, and blocks SCF binding and receptor dimerization and activation. In lymphopenia, impaired cell mediated immunity, deficiency of T regulatory
vitro studies demonstrate that KTN0158 is a potent inhibitor of SCF-depend- cells, alterations in transitional B cells, selective IgM deficiency, altered TLR
ent KIT activation and of degranulation enhanced by SCF in the human LAD2 expression, and an impaired NK cell cytotoxicity.
mast cell line. KTN0158 has similar binding affinity for human, monkey, dog
and cat KIT, but does not cross-react with murine KIT. A placebo-controlled,
cross-over design pilot study was conducted to evaluate the ability of KTN0158 P86
to reduce airway eosinophilia and airway reactivity in experimentally asthmatic COMPLEMENT DEFICIENCY PRESENTING AS GROUP A
cats sensitized with Bermuda Grass Antigen (BGA). Cats received 20 mg/kg STREPTOCOCCAL (GAS) SEPSIS WITH TOXIC SHOCK SYN-
KTN0158 or placebo on days -1 and 14, and airway reactivity was assessed DROME AND ESCHERICHIA COLI UROSEPSIS IN INFANCY.
using BGA or methacholine bronchoprovocation (day 0 or day 28) and venti-
L. Helfner*, A.M. Jongco, Great Neck, NY.
lator-acquired pulmonary mechanics, as well as bronchoalveolar lavage to assess
airway inflammation. Cats treated with KTN0158 had significant reduction in Introduction: Complement component deficiencies are rare, and predis-
airway eosinophilia during the early- (p=0.009) and late-phase (p=0.032) asth- pose to autoimmunity or increased susceptibility to recurrent infections with
matic reactions, suggesting further investigation of KIT inhibition with encapsulated bacteria. The types of infection relate to the function of the miss-
KTN0158 in allergic asthma is warranted. To this end, studies to investigate the ing components. For example, terminal complement component deficiency fre-
potential benefit of KTN0158 in mast cell-related diseases and to evaluate quently presents with Neisseria species infections. Methods: We describe an
safety are ongoing. 11-month old male who presented originally with lethargy and fever that devel-
oped into GAS sepsis with toxic shock syndrome. He received a 10-day course
of IV antibiotics and was discharged on oral cephalexin. Shortly after discharge,
A48 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A49
ABSTRACTS: POSTER SESSIONS
he was re-admitted with fever and found to have extended-spectrum beta lac- soft. Results: CDA activity in pneumonia (8.14±2.72 U), as well as in infec-
tamase producing (ESBL) E. coli urosepsis, which responded well to a 10-day tious mononucleosis (4.37±2.22 U) was found to be high in comparison with
course of IV ertapenem. For UTI prophylaxis, the patient now receives trimetho- the control groups: 1.1±0.4 U for the wide cohort and 2.29±0.5 U for the nar-
prim-sulfamethoxazole daily, and has done well following his second hospi- row cohort. In contrast, chronic HCV patients had no increased CDA levels
talization. He is currently receiving routine vaccinations as per CDC guide- (1.21±0.17 U). A polyclonal pattern was seen in both wide and narrow con-
lines. Results: Laboratory evaluation was remarkable for undetectable CH50 trols, IM and chronic HCV infection patients. Both control cohorts show sim-
on two separate occasions, as well as mild T cell lymphocytosis (CD3+ of ilar ADA activity levels: 12.08±5.24 U for wide and 11.10±2.2 U for narrow
8326/uL (reference range 1700-3600), CD4+ of 6285/uL (range 1700-2800), cohort. A two-fold increase in ADA activity in IM patients (27.56±9.87 U)
and CD8+ of 1654/uL (reference of 800-1200)). B and NK cells were unre- and the absence of significant deviations in ADA levels for chronic HVC (14.53
markable for age. Lymphocyte proliferation to pokeweed and phytohemag- U) were seen. Despite the low absolute values, CDA and ADA enzymatic activ-
glutinin was normal. G6PD was mildly depressed at 3.5 U/g Hb (range 4.6- ity proved itself to be among the most individually variable immunologic param-
13.5). Myeloperoxidase stain was normal. HIV serologies were negative, and eters. Conclusions: CDA and ADA enzyme activity is an informative parame-
he had detectable hepatitis B surface antibody. Total IgE was elevated at 323 ter with potential to be a biomarker of hidden immunodeficiency status.
IU/mL (range 0-15), with normal IgA, IgM, and IgG for age. Levels of C2,
C3, C4, C5, C7, C9, C1q, mannose binding lectin and AH50 were normal. C8
was decreased at 20 ug/mL (range 33-58). Further investigation of other com- P89
plement components is underway. Conclusion: This patient had mildly decreased ASSESSMENT OF SELECT SERUM CYTOKINES IN ORAL
G6PD and C8 with undetectable CH50 but normal AH50, suggesting that other LICHEN PLANUS PATIENTS.
complement components are deficient in quantity and/or function, likely G. Drannik1, A. Kurchenko1, R. Rehuretska1, L.M. DuBuske*2, 1. Kiev,
upstream of the membrane attack complex. Physicians must remain vigilant
Ukraine; 2. Gardner, MA.
and include complement deficiency in the differential diagnosis. These patients
should receive routine vaccinations, especially against diseases for which they Introduction: Oral lichen planus (OPL) is the most common immune dis-
are at increased risk. ease of oral mucosa, having an increased risk of malignancy. Cytokines (IL-1,
TNF-α, TGF-β) in blood may impact disease progression in erosive oral lichen
planus. Methods: 97 patients aged 18 to 60 years were studied including 35
P87 with erosive oral lichen planus, 32 with non-erosive oral lichen planus and 30
healthy control subjects of similar age. The levels of serum cytokines IL-1,
GUANYLYL CYCLASE-CGMP PATHWAY MEDIATES MITOGE-
NESIS INHIBITION BY NATRIURETIC PEPTIDES AND SODIUM TNF-α, TGF-β were determined by enzyme-linked immunosorbent assay
(“Immunotech”; France). Results: During relapse of erosive oral lichen planus
NITROPRUSSIDE IN RAT AIRWAY SMOOTH MUSCLE CELLS.
there is change in select cytokines compared with control group levels includ-
F.A. Placeres-Uray*, R. Gonzalez de Alfonzo, I. Lippo de Becemberg, ing IL-1 (0.6±1.5 pg/ml) being 2- fold increased versus the healthy controls
M. Alfonzo, Caracas, Bolivarian Republic of Venezuela. and TNF-α being 4.3- fold increased (0.3±1.6 pg/ml versus 1.3±1.2 pg/ml).
The airway smooth muscle cells (ASMC) hyperplasia is a central feature TGF-β ( 3.2±1.2 pg/ml) however is reduced 3.8- fold versus healthy controls
of airway remodeling. ASMC mitogenesis is promoted by several mediators (12.3±1.1 pg/ml). In erosive chronic OLP there is an increase in IL-1 by 1.8-
such as epidermal growth factor (EGF) and tumor necrosis factor-α (TNF-α), fold, an increase of TNF-α by 1.8- fold and an increase of TGF-β (29.6±2.2
which are countered by activators of guanylyl cyclases (GC)-cGMP pathway. pg/ml) compared to healthy controls (12.3±1.1 pg/ml). In chronic OLP IL-1
This study evaluated the effect of sodium nitroprusside (SNP), an oxide nitric indexes were increased 3.7- fold in comparison to OLP relapse and TNF-α
(NO) donator, and natriuretic peptides (ANP, CNP) on rat ASMC proliferation. increased 7.7- fold and TGF-β increased 9.2 – fold compared to disease
Cells were isolated from tracheal fragments and were characterized using relapse(p<0.05). Conclusions: Acute relapse and chronic stages of lichen planus
immunochemistry with specific antibody anti-α smooth muscle actin, indi- of the oral mucosa are characterized by immunological changes detectable in
cating that after 3rd passage were 100% positive. Proliferation assays were per- peripheral blood serum including increases in concentrations of IL-1, TNF -α,
formed by MTS-PMS method. Viability was confirmed by trypan blue exclu- TGF-β, characteristic of development of a recurrent inflammatory immune
sion method. To determined GC enzyme activity, cells were pre-incubated with response and chronic persistent erosive disease.
100 M IBMX (PDEs inhibitor) and cGMP was measured using Amersham kit.
SNP (10-5M; n=6), ANP and CNP (n=3) in a doses-dependent manner inhib-
ited ASMC proliferation induced by fetal bovine serum (FBS), EGF and TNF- P90
α (p <0.05). ODQ (sGC inhibitor) reversed the action of SNP (p <0.05, n=3) IMMUNOSUPRESSIVE PROPERTIES OF HUMAN OLFACTORY
and improved basal proliferation and mitogenesis induced by FBS (p <0.05, EPITHELIUM-DERIVED ECTOMESENCHYMAL STEM CELLS
n=3). We found increased of cGMP levels in response to SNP, ANP and CNP. CULTURED EX VIVO.
cGMP synthesis induced by SNP, but not by natriuretic peptides, was inhib- A. Hancharou1, N. Antonevich1, V. Chekan1, L.M. DuBuske*2, 1. Minsk,
ited by 100nM ODQ (p <0.05, n=3). NO, ANP and CNP increase cGMP lev-
Belarus; 2. Gardner, MA.
els by different transduction systems and inhibit ASMC proliferation. More-
over, basal activity of sGC regulates ASMC mitogenesis. This signaling pathway Introduction: Nasal mucosa contains olfactory epithelium-derived ectomes-
might be altered in airway remodeling and represent an important therapeutic enchymal stem cells (hOE-EMSC), which are similar to mesenchymal stem
target to ASMC hyperplasia. cells derived from bone marrow and adipose tissue and which may have
immunosuppressive properties. Methods: Nasal mucosa samples were taken
from 4 patients with non-inflammatory diseases of the nasal cavity. Explant
P88 culture methods were used to obtain hOE-EMSC cells. Cells were assayed for
phenotype (CD90, CD105, CD45, CD273, CD274, CD80, CD86, CD40,
CYTIDINE DEAMINASE AND ADENOSINE DEAMINASE ARE
HIGHLY SENSITIVE ENZYMATIC REGULATORS OF IMMUNE nestin). Culture media from hOE-EMSC were collected and used in further
experiments. PBMC isolated from donor blood were primed with CFSE, co-
RESPONSE INTENSITY AND SPECIFICITY.
cultured with hOE-EMSC for 3 days plus PHA, and then assayed for prolifer-
L. Titov1, K. Pavlov1, A. Hancharou1, O. Yanovitch1, S. Javoronok1, ation. PBMC were also cultured without hOE-EMSC with the addition of PHA
L.M. DuBuske*2, 1. Minsk, Belarus; 2. Gardner, MA. (positive control), and with the addition of hOE-EMSC conditioned media.
Background: Cytidine deaminase (CDA) and adenosine deaminase (ADA) Results: Cells obtained were CD90+CD105+nestin+CD45–. The ability of hOE-
basal serum activity may be impacted by acute and chronic infection states. EMSC to inhibit mitogen-induced proliferation of CD4+ T cells was shown.
Methods: Two groups formed on a wide (n = 10, male and female, 24-31 age) The immunosuppressive effect did not depend on soluble factors produced by
and narrow (n = 19, only male, 18-25 age) principle of sampling as controls stem cells, including interleukin-10. Direct contact of hOE-EMSC with lym-
were compared to infectious mononucleosis (IM) patients (n = 10, male and phocytes was required to exhibit immunosuppressive properties. HOE-EMSC
female, 18-34 age), chronic HCV infection patients (n=29, male and female, expressed the co-inhibitory molecules CD273 and CD274 but were negative
27-70 age), and patients with pneumonia developing in the 2012-13 influenza for CD80 and CD86. Immunosuppressive properties were dependent on CD273
epidemic season (n=10, male and female, 6-16 age) by assessing CDA and and CD274 expression. Conclusion: The hOE-EMSC possesses immunosup-
ADA activity (indophenol colorimetric test), CD19 + cells content (flow cytom- pressive properties and may possibly be used in cellular immunotherapy of
etry), B-cells clonal status (immunoglobulin heavy chains rearrangement) and immune system disorders including autoimmune diseases and could possibly
PCR analysis using ISH assay (InVivoscribe, USA) and GelAnalyzer 2010a assist in prevention of organ and tissue rejection.
VOLUME 113, NOVEMBER, 2014 A49
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A50
ABSTRACTS: POSTER SESSIONS
P91
ALTERATIONS IN MINOR SUBSETS OF PERIPHERAL BLOOD
LEUKOCYTES IN INFECTIOUS MONONUCLEOSIS PATIENTS.
A. Hancharou1, G. Davidovich1, I. Ramanava1, E. Duzh1, L.M. DuBuske*2,
1. Minsk, Belarus; 2. Gardner, MA.
Introduction: The content of minor leukocyte subsets in the patients with
infectious mononucleosis (IM) may be altered including monocyte, dendritic
cell (DC) and myeloid-derived suppressor cells (MDSC). Methods: 12 patients
with acute IM, confirmed by blood serum and saliva PCR analysis, were selected
for investigation. Whole blood from 10 healthy volunteers matched by age and
sex was used as a control. Relative and absolute counts of leukocyte subsets
were assayed using FACSCanto II cytometer: CD1c+ and CD141+ myeloid DC,
plasmacytoid DC, CD14+/CD16+ blood monocytes and monocytic (M-MDSC)
and granulocytic (CD15+ and CD33+) G-MDSC. Results: In patients with IM
statistically significant myeloid DC subset redistribution was seen with increase
of CD141+ cells (CD1c/CD141 index in patients: 1.9(1.4–2.6), versus in con-
trols: 6.2(5.6–7.3), =0.00013), suggesting a role in the pathogenesis IM.
Decrease of plasmacytoid dendritic cell counts in IM was observed (patients:
0.04(0.02–0.11)% versus controls: 0.4(0.250–0.520)%, p=0,000001; patients:
0.003(0.002–0.01)×106/ml versus controls: 0.022(0.013–0.032)×106/ml,
p=0.00017), suggesting migration to lymphoid tissue or selective depletion.
Monocytic myeloid-derived suppressor cell counts were reduced in acute IM
(patients: 0.075(0.05–0.135)% versus controls: 0.32(0.23–0.37)%, p=0.011),
explaining EBV-induced immune system hyper-stimulation and increase of
HLA-DR expression on virtually all APC and T-cells. Increase of absolute
(p=0.052) and relative (p=0.09) CD15+ G-MDSC counts were seen in IM but
P93
no statistically significant differences in the number of CD33+ G-MDSC cells. CREST SYNDROME IN AN 8 YEAR OLD AFRICAN AMERICAN
Significant variability of content of G-MDSC and “intermediate” and “non- GIRL.
classical” monocyte subsets were noted such as in IM with CD15+ G-MDSC I. Katayeva*1, K. Chotikanatis2, S. Glick3, J. Moallem2, 1. Forest Hills,
minimum of 0.01% and maximum of 0.22% versus controls minimum of NY; 2. Brooklyn, NY; 3. New York, NY.
0.022% and maximum of 0.167%. Conclusion: Significant changes in the num- Introduction: CREST syndrome (Calcinosis, Raynaud’s phenomenon,
ber of minor leukocyte subsets in blood are seen in IM. These changes may esophageal dysmotility, sclerodactyle, and telangiectasia) or systemic sclero-
explain some of the clinical immune manifestations of IM. sis with limited scleroderma is very rare in children, and mainly involves skin,
subcutaneous tissues, muscle and bones, and does not involve internal organs.
The usual onset of scleroderma is approximately 30-65 years of age. Its inci-
P92 dence in children is one per one million. Case Description: An 8 year old African
THE EFFECT OF GENDER ON THE PERIPHERAL BLOOD B American girl with past medical history significant for being born at 28 weeks
CELLS MATURATION. GA, via C-section due to abruptio placenta and pre-eclampcia, intubated right
A. Khojah*1, A. Bukhari1, O. Alpan2, 1. Chicago, IL; 2. Vienna, VA. after delivery, required 3 months of NICU care, with multiple blood transfu-
Rationale: Despite the growing use of flow cytometry in evaluation of var- sions, PDA closed with indomethacin, pubarche at 5 years of age, with nega-
ious immunodeficiency disorders, there are limited number of studies that dis- tive work up, who presented with over all 10 months history of non-pruritic,
cuss the gender effect on the reference range of different B cell subsets, espe- off white, rashes on elbows, knees that over the course of few months had turned
cially in the pediatric age group. The aim of this study was to evaluate the effect hard and looked as if they were warts and finally calcified over the next few
of gender on B cell maturation in different age groups. Methods: Total of 988 months . Also 10 months history of “icy cold” fingers and toes with bluish dis-
subjects were included in this study. We excluded all adults whose age is 22 or coloration. On physical examination there were multiple calcified nodules on
older, all subjects with known primary or secondary immunodeficiency and extensor surfaces of the elbows, finger tips with protruding calcified papules,
patients with incomplete work up. All Subjects had normal evaluation includ- sclerodactily of fingers, and telangiectasia along with bluish discoloration of
ing CBC, serum immunoglobulin, antibody response to vaccine especially pneu- finger tips to the level of PIPs. Biopsy of the lesions confirmed calcinosis cutis.
mococcal titers (for subjects more than 2 years). Clinical and laboratory data Laboratory investigation including CBC, ESR, CMP, ANA with reflex remained
including B cell subset were obtained from patients’ records. Subjects were inconclusive. Chest x-ray did not indicate any pathology. Treatment: She was
divided into seven groups based on their age. Using T test, we compared between started on monthly IVIG infusion along with daily PO Prednisolone, weekly
males and females in each age group in terms of different B cell sub-popula- PO Methotrexate and daily folic acid. Her symptoms greatly improved over 4-
tions. Data was analyzed using SPSS, version 22. Results: Both, the absolute 5 month, calcinosis of the finger tips resolved, while the rate of eruption of the
B cell count and the percentage of B cell, drop significantly in the first 7 years new calcified lesions slowed .and resolved. Discussion: CREST syndrome is
of life. That drop was equal in the male and female groups. The mean of CD5+ a very rare disease in children, our patient had 4 out of 5 findings and improved
B cell was 4 to10 % higher in males versus females in all age categories except after outlined therapy. Treatment for scleroderma needs to be started promptly
in subjects between 19 and 21 years of age. This difference reaches statistical to avoid future complications. In general prognosis of sclerosis in children is
significance in the age groups between 13 and18 years, which might suggest better than in adults.
a possible, but not previously described, hormonal effect on the B cell matu-
ration. Overall, females have higher mean of switched B cell (IgG+, IgA+)
and lower mean of IgM+, IgD+ B cell. Yet, these differences are more signif- P94
icant between 10 to18 years of age. Conclusion: These graphs highlight the dif- ASEPTIC MENINGITIS WITH INTRAVENOUS GAMMAGLOB-
ference between males and females in terms of B cell sub-populations, and the ULN ADMINISTRATION.
importance of having gender-specific reference ranges especially in the ado- C.C. Randolph*, D.H. Dreyfus, Waterbury, CT.
lescent age group. Our results suggest a possible hormonal influence on B cell Rationale:Intravenous gammaglobulin(IVIG) administration for immun-
maturation. Further research is needed to investigate this theory. odeficiency disease is rarely associated with a delayed serious, adverse reac-
tion of aseptic meningitis.This condition is usually related to high doses of
IVIG (1-2gm/kg).The pathogenesis is postulated to be an osmotic shift caused
by small amounts of IVIG penetrating the cerebrospinal fluid and/or antineu-
trophil antibodies in some IVIG products activating neutrophils in the central
nervous system.(1) Methods :Case Report We present a 36 year old white female
with 1) selective antibody deficiency and hypogammaglobulinemia 2)car-
A50 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A51
ABSTRACTS: POSTER SESSIONS
diomyopathy with implanted pacemaker (2009)and recurrent pericaridi- a medical mission trip to Kenya. Upon his return, he develops an eruptive rash
tis3)moderate persistent asthma on Advair and Alvesco 4)depression and 5) a on his abdomen that is self-limiting after 3 months. He also develops a cough
migraine condition admitted with aseptic meningitis after first infusion of IVIG and worsening dysphagia and is initially treated medically for acid reflux.
400mg /kg over 3 hours in a monitored setting.She develped a severe,pulsat- Despite treatment, these symptoms worsen. He also experiences intermittent
ing, diffuse occipital, temporal and parietal headaches with retro orbital pain diarrhea, ranging from loose to watery bowel movements. Labs display
beginning 6 hours post infusion.The pain exacerbated with any motion of the eosinophilia (eosinophil count 600 c/mL (10.2%) (normal 500 c/mL)) and nor-
head or neck,cough or bearing down and was associated with visual alter- mal immunoglobulin E (IgE) level (93 kU/L). Results: After months of wors-
ations and inability to register words or numbers.She experienced dull pain ening dysphagia and cough, an esophagogastroduodenoscopy reveals mucosal
radiating down the neck to left precordial area and left shoulder and arm with changes including longitudinal furrows and circumferential folds in the entire
fever,nausea and diarrhea 24 hours prior to admision.CT scan of the head esophagus. Pathology displays squamous mucosal eosinophilia with 57 in 1
demonstrated right maxillary sinus air fluid levels.Lumbar puncture(LP) high power field (normal <15 per high power field), seen superficially and deep
revealed normal glucose 49mg/dl,normal protein 36mg/dl,WBC 512/mm3 and with no microabcesses. A diagnosis of eosinophilic esophagitis is made. After
RBC 59/mm3 47%segmented neutrophils,51%mononuclear cells and one month of no resolution with swallowed corticosteroid solution, his aller-
2%eosinophils with negative cerebrospinal fluid cultures and relief of gist is prompted to pursue a parasitic work up. A strongyloides immunoglob-
symptoms consistent with aseptic meningitis . She had a history of recurrent ulin G (IgG) antibody (Ab) ELISA is elevated at 1.22 units/mL (normal, <1.00).
sinusitis and admissions for “pneumonia” 2009-13 .Her original immune Ova and parasite stool test is negative. Treatment with ivermectin is initiated.
evaluation demonstrated IgG 651mg/dl(694-1618mg/dl),normal His dysphagia resolves after anti-parasitic treatment, but his shortness of breath
IgM(132mg/dl),A(298mg/dl), and protective tetanus titers but nonprotective continues. Labs show persistent eosinophilia, and he is given a second treat-
pneumococcal titers( 13/14) despite recurrent immunizations and varicella ment of ivermectin with resolution of respiratory symptoms. Conclusion: EoE
zoster titers were nonprotective. Results:Aseptic meningitis was treated with is a condition that can lead to permanent sequelae including esophageal scar-
systemic steroids and Omnicef for sinusitis. IgG replacement was subsequently ring and fibrosis. Strongyloides infection can cause a systemic eosinophilia,
changed to subcutaneous route without further complications. Conclusion Asep- and in this patient the eosinophilia from the untreated Strongyloides infection
tic meningitis is a rare delayed adverse event following IVIG administration. was associated with esophageal infiltration of eosinophils. Strongyloides is
Reference:Stiehm ER :Adverse effects of human immunoglobulin treated with anti-parasitic agents, and can be monitored by symptom resolu-
therapy.Transfusion Medicine Reviews 2013:27:171-8 tion, eosinophilia on labs, or repeat strongyloides Ab.
P95 P97
HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS: MAKING A COMBINED IMMUNODEFICIENCY IN WOLF-HIRSCHHORN
CHALLENGING DIAGNOSIS. SYNDROME.
A. Mathur*, L. Yao, Phoenix, AZ. S. Galowitz*, M. DeFelice, Wilmington, DE.
Rationale: Hemophagocytic lymphohistiocytosis (HLH) is a rare clinical Rationale: Wolf-Hirschhorn syndrome (WHS) is a genetic disorder due to
syndrome characterized by uncontrolled activation of lymphocytes and partial deletion of the distal short arm of chromosome 4, with characteristic
macrophages producing elevated levels of cytokines. A clinically challenging features including facial, cardiac and skeletal abnormalities, developmental
diagnosis to make, HLH manifests as fevers, cytopenias, hepatosplenomegaly, delay, growth retardation, and a high mortality rate in the first two years of
hyperferritinemia, elevated IL-2, hepatic failure, and neurologic symptoms. We life. Though no known genes associated with immunodeficiency reside on the
present a case of a patient with persistently high fevers, pancytopenia, hyper- short arm of chromosome 4, these patients can present with immune dysregu-
ferritinemia that was diagnosed as HLH. Methods: A 28 year old Native Amer- lation. Limited data shows patients with WHS most commonly have defects in
ican male presented with fever, chills, myalgias, arthralgias, bilateral lower humoral immunity, while T-cell immunity remains intact. To date, there has
extremity edema, and a fifty-six pound unintentional weight loss in three been one reported case of an isolated T-cell defect. We present the first reported
months. Neither high dose prednisone for Adult Onset Still’s disease, nor broad case of a child with WHS with deficiencies in both humoral and cellular immu-
spectrum antibiotics for an infectious etiology improved the fever or hepatic nity. Methods: The patient is a 2 year old female with 4p16.3 chromosomal
synthetic function. Results: Ferritin was extremely elevated to 16,173 ng/mL deletion and characteristic clinical findings consistent with WHS. She was
(reference range 22-322). Serum immunoglobulins, including IgG, IgA, and referred to us for severe hypogammaglobulinemia noted on hospital admis-
IgM, were within normal limits. Concentration of sCD25 and IL-2 receptor sion for acute respiratory failure secondary to parainfluenza virus. Results: The
were elevated. Fibrinogen was low and triglycerides were high. Infectious serolo- patient has a history of methicillin sensitive S. aureus bacteremia, two episodes
gies and cultures including EBV and CMV were negative. Autoimmune mark- of pneumonia requiring intravenous antibiotics, recurrent acute otitis media
ers were negative. White blood cell count with differential was normal. Liver infections requiring two sets of myringotomy tubes, and bacterial colonization
biopsy showed steatohepatitis with stage 2 fibrosis. Flow cytometry showed of her bladder. Her childhood vaccinations are up to date. Immunologic eval-
normal phenotype. Bone marrow biopsy showed prominent hemophagocyto- uation revealed low IgG (185 mg/dL), IgM (13 mg/dL) and IgA (24 mg/dL),
sis consistent with hemophagocytic lymphohistiocytosis. Conclusion: Our poor antibody response to diphtheria vaccination (0.02 IU/mL), and absent anti-
patient met seven of the eight diagnostic criteria for HLH, including fever, body response to tetanus (<0.1 IU/mL) and Prevnar 13 (0/23 serotypes pro-
splenomegaly, cytopenias, hypofibrinogenemia and hypertriglyceridemia, ele- tective) vaccines. Lymphocyte subset enumeration demonstrated decreased
vated ferritin, elevated sCD25 and hemophagocytosis in the bone marrow. absolute CD3 (998 cells/mcL; normal 1400-3700), CD19 (154 cells/mcL;
Delays in this challenging diagnosis can result in high mortality rates due to normal 390-1400) and CD8 (240 cells/mcL; normal 490-1300) counts. Mito-
multisystem organ failure. Because biopsies of affected sites may be normal gen stimulation, CH50, AH50 and MBL were normal. Random stool alpha 1-
or misinterpreted, repeat biopsies are sometimes necessary if clinical suspicion antitrypsin level was normal. She began monthly immunoglobulin replacement
remains high. We suspect hepatic involvement in our patient despite the lack and the severity of her infections has improved, with no further hospital admis-
of hemophagocytosis on liver biopsy. Treatment algorithms include etoposide, sions for bacterial illness. Conclusions: Immunodeficiency is a possible cause
dexamethasone, antithymocyte globulin, cyclosporine A, intravenous of early mortality in patients with WHS. This is the first report of a patient with
immunoglobulin, alemtuzumab, and hematopoietic cell transplant. In patients WHS with deficiencies in both B- and T-cell lineages. Thorough immunologic
with persistent fever, hepatosplenomegaly and cytopenias, the challenging diag- evaluation and appropriate management for combined immunodeficiency may
nosis of HLH should be considered for prompt therapy. drastically improve survival and quality of life for affected patients.
P96 P98
A CASE OF EOSINOPHILIC ESOPHAGITIS IN A PATIENT WITH IGE-MEDIATED ALLERGY TO BACITRACIN: KEY CONCEPTS
STRONGYLOIDES STERCORALIS. ILLUSTRATED VIA A CASE SERIES.
A. Ali*, M. Segal, Philadelphia, PA. E. Glancy*, C. Radojicic, Cleveland, OH.
Introduction: Eosinophilic esophagitis (EoE) is a condition in which inflam- Bacitracin is often considered to be an innocuous over-the-counter med-
matory cells invade the mucosa of the esophagus. Few cases have described the ication. However, both T cell-mediated and IgE-mediated allergic reactions
association of EoE with parasitic diseases. We present a case of EoE in a young have been reported with increasing frequency, presumably due to its widespread
man with Strongyloides infection. Methods: A 21 year old male returns from use. We describe two cases of IgE-mediated reactions to bacitracin confirmed
VOLUME 113, NOVEMBER, 2014 A51
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A52
ABSTRACTS: POSTER SESSIONS
by positive skin prick testing (testing for second case in figure below). The first for throat swelling, hives, fevers, chills, night sweats, or weight loss. He was
case is of a 53-year-old female who developed diffuse hives following baci- initially placed on high dose prednisone which only temporarily improved his
tracin irrigation during breast augmentation surgery. The second case describes swelling. Shortly after the steroids were discontinued the swelling reappeared.
a 40-year-old man who developed anaphylaxis following the application of a MRI showed symmetric bilateral lacrimal gland enlargement. Labs including
topical bacitracin ointment to blistered skin. In both cases, the patient had a ESR, CRP, ANCA, ANA, and IgG4 level were within normal range. He had
history of prior reaction to a triple antibiotic preparation before reacting to bac- peripheral eosinophilia with absolute eosinophil count of 830. Initial lacrimal
itracin alone. This case series demonstrates the variable routes of exposure caus- gland biopsy was read as non-necrotizing perivascular granulomatous infiltrate
ing allergic reactions, initially suspected neomycin allergy with resultant rec- that involves small arteries and veins. He was initially diagnosed with
ommendation to use bacitracin alone, and the utility of skin prick testing to Eosinophilic Granulomatosis with Polyangiitis. He had no other medical his-
confirm bacitracin as the culprit allergen. Physicians need to be cognizant of tory or organ involvement suggestive of small vessel vasculitic syndromes.
the potentially serious consequences of using topical antibiotics on damaged Biopsy slides were sent to a specialty laboratory who reported fibrosis, oblit-
skin and mucosal surfaces, and furthermore, consider bacitracin as equally erative phlebitis, as well as 174 IgG4 plasma cells/high powered field consis-
important as neomycin in causing allergic reactions. Allergists can provide skin tent with the diagnosis of IgG4-Related Disease. He was subsequently treated
prick testing to the components of triple antibiotic ointments to confirm an IgE- with azathioprine and had significant improvement of his periorbital swelling.
mediated mechanism for allergic reactions. Conclusion: Integration of clinical, radiographic, and histopathologic data is
necessary to diagnose IgG4-related disease. Biopsy with special staining for
IgG4 plasma cells interpreted by an experienced pathologist is an important
part of diagnosis and should be considered in any patient with bilateral lacrimal
gland swelling to identify IgG4-related disease.
P100
COMMON VARIABLE IMMUNODEFICIENCY IN A PATIENT
WITH SYSTEMIC LUPUS ERYTHEMATOSUS: CASE REPORT.
E. Sandoval*1, C. Quezada-Chalita1, C. Cunningham-Rundles2, S. Enciso-
Pelaez1, M. Gutiérrez-Ceniceros1, 1. Mexico City, DF, Mexico; 2. New York,
NY.
Introduction: Common variable immunodeficiency (CVID) is the most
common clinically significant primary immune defect. Although 70% to 80%
of patients have had recurrent sinopulmonary infections, auto-immunity and
inflammatory complications are also common. Case Report: We present the
case of a 16 years old girl, who was admitted with a history of fatigue, weak-
ness, pallor, edema of lower limbs. Physical examination was positive for Ray-
naud phenomenon. The diagnosis of systemic lupus erythematosus (SLE) was
made based on 1. Proteinuria cellular casts, nephritis with low glomerular fil-
tration rate, requiring replacement management with hemodialysis, 2. Hemolytic
anemia and lymphopenia, 3. Pericardial effusion, 4. Central nervous system
disorder with acute confusional state with cerebral MRI angiography showing
irregular contours in distal segments and beading trend in vessels of medium
and small size . Laboratory work-up showed Antinuclear antibody with a speck-
led pattern at a low titer; ANCA, anti DNA, lupus anticoagulant, B2GP1 were
negative. Hypogammaglobulinemia and hypocomplementemia were found.
Antibodies in the urine were positive for anti DNA at high titers, 333.2 U/ml
(0-9.6U/ml): supporting the diagnosis of SLE.The patient had a torpid evolu-
tion, with severe sepsis, pancreatitis and gastrointestinal bleeding. She devel-
oped neurological impairment, seizures and Broca’s aphasia, an MRI revealed
ischemia in temporal and generalized vasospasm. Given the persistence of
hypogammaglobulinemia at the expense of IgG and IgM as well as a history
of multiple infectious events including pneumonia requiring mechanical ven-
tilation, urinary tract infection by Pseudomonas aeruginosa and Serratia
marscenses. Flow cytometry showing impaired lymphocyte subpopulation B
(marked decrease in CD19 and CD20), lymphopenia at the expense of the
Positive skin prick tests to bacitracin and bacitracin/polymixin subpopulation of T lymphocytes CD3 +, CD4 +. NK cells without alteration.
Isohemagglutinins (anti A1) for blood groups reported in 1:16 dilution, and no
response to immunization of Streptococcus pneumoniae. Conclusions: Clini-
P99 cians should be aware about the relation between immunodeficiency and autoim-
munity. Autoimmune diseases affect about 20% of CVID patients and are com-
IGG4-RELATED DACRYOADENITIS IN YOUNG MALE.
monly the first manifestations of immune deficiency. The pathogenesis of
V. Reddy*, T. Craig, Hershey, PA. autoimmunity in immune deficiency is unclear for the most part, further inves-
Introduction: Bilateral periorbital swelling raises a wide differential diag- tigation must be done.
nosis that includes both benign inflammatory conditions and malignant disor-
ders. It may be a presentation of IgG4-related disease which is a recently
emerged systemic condition characterized by unique lymphoplasmacytic infil-
tration of soft tissues by IgG4 plasma cells that can affect a wide variety of
organs. Histopathologic and immunohistochemical analysis is important in the
diagnosis of this disease and to differentiate it from other inflammatory and
malignant conditions. We present a case of bilateral periorbital swelling which
was initially diagnosed as organ limited vasculitis. However with further inves-
tigation he was diagnosed with IgG4-related disease. Case Report: Patient is a
21 year old male with no significant past medical history who presented with
fluctuating bilateral eyelid swelling for 1 year. The swelling was associated with
pain and redness isolated to around the eyes. Review of systems was negative
A52 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A53
ABSTRACTS: POSTER SESSIONS
P102
A CASE OF IRBESARTAN-INDUCED ANGIOEDEMA WITH
SEVERE LARYNGEAL EDEMA.
R. Rishi*1, S. Ringwala1, S. Fatteh2, 1. Fort Lauderdale, FL; 2. Plantation,
FL.
Objective: To assess the safety of replacing angiotensin-converting enzyme
inhibitors (ACEI) with angiotensin II receptor blockers (ARBs) in patients with
a history of ACEI induced angioedema. Angioedema has been associated with
ACEI use in hypertension treatment. Angiotensin II receptor blockers have long
been considered a safe alternative treatment for hypertension in cases of ACEI
induced angioedema. Angiotensin II receptor blockers selectively block the
binding of angiotensin II to the AT1 receptor and therefore do not cause accu-
mulation of kinins which subsequently lead to angioedema. Methods: Case
Report Results: A 57 yr old Caucasian male experienced an acute episode of
angioedema with laryngeal edema. He experienced swelling of his tongue,
lips and larynx. The angioedema failed to respond to two doses of epinephrine
and IM diphenhydramine. He required a tracheostomy and ICU admission for
14 days. The patient was discontinued from his home medications, which
included irbesartan (Avapro). The angioedema persisted for 7 days, and failed
to respond to I.V. corticosteroids and antihistamines. His history revealed acute
episode of angioedema 5 years prior during a surgical procedure. The patient
was under conscious sedation, and he experienced unilateral tongue swelling
upon awakening. He was being treated with lisinopril at the time for hyper-
tension and was switched to irbesartan. Subsequently, the patient claimed he
experienced intermittent episodes of lip swelling. He was evaluated for Hered-
itary Angioedema, and all labs were within normal limits. Immunocap to food
Fig 1. MRI angiography showing irregular contours in distal segments and and environmental allergy was unremarkable as well. An autoimmune panel
beading trend in vessels of medium and small size. was also negative. He has not experienced any episodes of angioedema since
being discontinued from irbesartan. Conclusions: The patient’s angioedema
appeared to be related to his ARB therapy. In the ONTARGET trial, the inci-
P101 dence of ARB induced angioedema was 0.1 % compared to 0.3% for ACEI
associated angioedema. Although the incidence of ARB induced angioedema
CASE REPORT: SUCCESSFUL BRONCHIAL THERMOPLASTY
IN A CASE OF SEVERE PERSISTENT ATOPIC ASTHMA. is lower than ACEI, life-threatening complications such as laryngeal edema
may result. The mechanism of ARB associated angioedema has not been clearly
C. Lee-Kim*1, S. Patel2, 1. Buffalo, NY; 2. Los Angeles, CA. established, but studies have shown that ARBs may also increase bradykinin
Introduction: Bronchial thermoplasty (BT), approved by the US Food and levels. Therefore, other classes of anti-hypertensive medications should be con-
Drug Administration in 2010, is a novel technique that uses radiofrequency sidered as first line replacements in patients with a history of ACEI induced
energy during bronchoscopy to reduce the amount of built-up excess smooth angioedema.
muscle tissues and spasms in the airways of asthmatic patients. Several ran-
domized clinical trials (AIR, RISA, AIR2 Trials) have reported the efficacy of
BT on patients that have been unable to attain adequate control of their disease P103
with high doses of inhaled corticosteroids and long-acting beta-agonists. The BLACK RUBBER AND P-PHENYLENEDIAMINE CONTACT
results from these studies demonstrated overall reduction of symptoms, reduc- DERMATITIS.
tion in the number of asthma attacks requiring emergency room care, and
C. Lin*, M. Frieri, East Meadow, NY.
improvement in patients’ AQLQ scores. Recently, the Global Initiative for
Asthma has recognized BT as an add-on treatment option at the GINA Step 5 Introduction: Contact dermatitis is a common skin inflammation that occurs
level for select adults with severe persistent asthma. We report a successful case when foreign substances irritate the skin, characterized by erythematous and
of bronchial thermoplasty in a patient with severe-persistent atopic asthma. pruritic lesions. Contact dermatitis has been well documented in over 3000
Case Report: We present a 47 year old Iranian American male with allergic chemical triggers. P-Phenylenediamine, as a chemical substance is widely used
rhinitis, nasal polyposis, obstructive sleep apnea, reflux disease, and severe per- in hair dye. Its partially oxidized state can cause allergic reactions in sensitive
sistent allergic asthma who underwent bronchial thermoplasty. Previously, his individuals. Case: A 61 year old white female was referred to the allergy clinic
asthma remained difficult to control despite multi-drug therapy [mon- from the emergency department for an intensely diffuse rash on her skin dis-
telukast,mometasone furoate/ formoterol fumarate dihydrate, theophylline, seminated from the neck to waist for 2 weeks. She also complained of a pin
tiotropium bromide, loratadine, olopatadine nasal spray, fluticasone furoate and needle sticking pain within the rash area. She had hair dye at a salon 2
nasal spray, and omalizumab]. Prior to the procedure, he had an average FEV1 days before she developed the pain and skin reaction. There was no shortness
of 40%, ACT scores <19, and levalbuterol use 3-6 times a day for relief. Since of breath, stridor or throat symptoms. Past medical history included seasonal
the completion of the BT procedure 1 year ago, the patient has been able to allergy and food allergy. Skin prick tests revealed positive for grass, trees and
decrease his levalbuterol use to about once a day, improve his latest FEV1 to dust mite. She takes cetirizine all year around for allergy prophylaxis. On phys-
70%, and ACT score to 25. He has not experienced severe exacerbations requir- ical examination, she was alert, oriented, and afebrile with stable vital signs.
ing ER visits or hospitalization over the past 12 months. Furthermore, he has Her skin showed an extensively maculopapular rash randomized throughout
been able to discontinue several of his previous medications, such as mon- from her neck to chest and back area. Methods: A skin patch test disclosed a
telukast, tiotropium, and theophylline. Conclusion: This is the first case report positive test for p-Phenylenediamine and black rubber mix. sIgE testing for
of an atopic asthmatic patient successfully treated by bronchial thermoplasty latex was negative. She was advised to avoid known allergic related chemi-
after failure of conventional and several non-conventional therapies. This case cals, continue to take cetirizine or fexofenadine. The rash and pain gradually
demonstrates that for some highly-select adult patients with difficult to man- improved. Conclusion: Contact dermatitis can result from hair dye hypersen-
age allergic asthma, a referral to an asthma specialty center with bronchial ther- sitivity. Its severity ranges from a mild localized rash to a widespread allergic
moplasty should be considered dermatitis reaction or even rarely, anaphylaxis. The diagnosis relies upon a
detailed history and physical examination. The skin patch test remains the
gold standard to confirm contact allergic reactions. Avoidance of exposure to
rubber products, causative hair dye should be withdrawn. Systemic anti-hista-
mines are often needed and in severe patients, a short course of systemic steroids
may be required. Prevention could be achieved by testing oxidative dyes before
use or switched to non-oxidative hair dye. Patients should also be careful with
VOLUME 113, NOVEMBER, 2014 A53
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A54
ABSTRACTS: POSTER SESSIONS
rubber products and cross- reacting chemicals or drugs such as printing inks, tions R257X and c.967_979del13 in the AIRE gene. The patient’s clinical man-
temporary black henna tattoos ifestations included chronic mucocutaneous candidiasis, hypoparathyroidism,
adrenal insufficiency with positive 21-hydroxalase antibodies, vitiligo, hypoplas-
tic dental and nail enamel, and delayed growth. At age 13 she developed chronic
urticaria despite high dose antihistamines and daily montelukast. Laboratory
workup revealed the presence of anti-FceRI autoantibodies without progres-
sion of autoimmune disease. Treatment with omalizumab 150mg led to reso-
lution of symptoms after one month and reduction of daily oral medications.
The patient is currently under treatment every 8 weeks with omalizumab and
will stop therapy soon to evaluate for possible remission of her urticaria. Con-
clusions: Omalizumab appears to be an effective therapy for CIU in APECED;
however, questions remain regarding its underlying mechanism of action. The
rare appearance of CIU in this patient population seems to run counter to the
hypothesis that CIU is associated with autoimmune disease. Our patient high-
lights the need for further research to better characterize the relationship of
CIU with immune dysregulation and how therapy with omalizumab influ-
ences this process.
P106
REFRACTORY HYPOTENSION IN A PATIENT WITH SYSTEMIC
MASTOCYTOSIS UNCOVERED AFTER ACUTE MYELOID
LEUKEMIA TREATMENT.
D. Ferastraoaru*, M. Janakiram, G. Hudes, Bronx, NY.
Representative photograph. From: Patricia Norris M.D., Allergy Clinic
Portland Contact Dermatitis Background: Systemic mastocytosis (SM) can be associated with clonal
hematological disorders like myelodysplastic syndrome (MDS) and acute
myeloid leukemia (AML). Most of the SM-AML cases have translocation
P104 t(8;21) and mutation of c-kit gene. Rarely, specific SM treatment is required.
We present a patient with SM-AML without t (8; 21) and c-kit mutation who
SUCCESSFUL MONOCLONAL ANTIBODY DESENSITIZATION
IN A PEDIATRIC PATIENT WITH HYPERSENSITIVITY TO RIT- developed refractory hypotension due to mast cells mediators release. Meth-
ods: case report; review of literature Case Report: 53 year old female was diag-
UXIMAB.
nosed with myeloproliferative-myelodysplastic syndrome which evolved to
S. Logsdon*, L. Schneider, Boston, MA. high risk MDS with complex cytogenetics (deletion of chromosomes 5,7 and
Introduction: Drug allergy can limit essential therapeutic options for patients. trisomy 8) for which she received induction chemotherapy. After discharge
Hypersensitivity to monoclonal antibodies has been documented in adult she developed urticaria that slowly responded to daily antihistamines and was
patients, but desensitization to this class of drugs has not been well described thought to be medication related. She relapsed with AML (similar cytogenet-
in the pediatric population. Here, we present a pediatric patient with hyper- ics) in 3 months and received re-induction therapy. The course was complicated
sensitivity to rituximab who underwent successful drug desensitization. Meth- by Enterobacter bacteremia that cleared with daptomycin. However, she devel-
ods: Desensitization to rituximab was completed via a modified 12-step, 3-bag oped severe persistent hypotension along with new diffuse pruritic maculo-ery-
method in an inpatient unit. The protocol started at an initial dose of .0057 mg thematous rash. Skin biopsy showed spongiosis. The patient was transferred
with doubling of the dose at 20-minute intervals, with the proposed final step to intensive care unit requiring vasopressors which were difficult to taper off.
to be infused at 75 cc/hr to provide at total therapeutic dose of 285 mg. The Cardiac and septic shock were excluded as causes for refractory hypotension.
child developed significant rash prior to the last step, and thus future protocols Repeat BM biopsy for induction response revealed clearance of myeloid blasts
reduced the infusion rate of the last step. The patient was monitored after com- but showed 20% CD 117+ oval spindle-shaped mast cells, which were positive
pletion of each desensitization protocol. Results: A 7-year-old boy with neona- for tryptase and negative c-kit mutation. Serum tryptase level was 42 ng/ml.
tal biliary atresia status post remote liver transplant developed EBV negative The patient was diagnosed with SM-AML and started on histamine-1, hista-
post transplant lymphoproliferative disease (PTLD). Rituximab were required mine-2 and leukotriene receptors blockers with significant improvement in
for treatment of the child’s PTLD, but he developed urticaria and cough with blood pressure and skin rash. After 2 weeks she died from multiorgan failure.
infusions despite premedication with antihistamines. As rituximab was a crit- Conclusion: This is the first reported case of refractory hypotension due to mast
ical part of the child’s chemotherapy, urgent desensitization was required. The cells mediators release in a patient with SM-AML. Moreover, no cases of SM-
patient underwent the desensitization protocol, but developed diffuse skin ery- AML without t(8;21) or c-kit mutation were previously reported. From the
thema prior to completion of the last dose. The protocol was therefore modi- sequence of clinical events we believe that the mast cells were uncovered by
fied as described above, with increased premedication. The child tolerated sub- the treatment for AML. As a result, the diagnosis of SM was made after cytore-
sequent desensitization protocols, and completed his chemotherapeutic regimen. ductive therapy. It is imperative that clinicians are aware of coexistence of SM
Conclusions: This is one of the only reported cases of successful desensitiza- in clonal malignant hematological disorders. If clinically suspected, prompt
tion to rituximab monoclonal antibody in a pediatric patient, and includes strate- treatment improves the SM-related symptoms.
gies for patients who have reactions during the procedure. This protocol will
be beneficial for future patients with rituximab hypersensitivity.
P107
SEED ALLERGY: WHEN NATURAL COLORS ARE DANGEROUS.
P105 K. Tuano*, C. Hanson, K. Dillard, Houston, TX.
CLEARING THE AIRE.
Color additives are frequently used in processed foods to impart color and
C. Lundberg*1, T. Banks2, 1. Silver Spring, MD; 2. Bethesda, MD. enhance its appearance. The US Food and Drug Administration (FDA) is respon-
Introduction: Autoimmune polyendocrinopathy-candidiasis-ectodermal sible for regulating color additives in commercial foods to ensure safety and
dystrophy (APECED) is a primary immune deficiency (PID) associated with accurate labeling of approved ingredients. Synthetically produced colors are
autoimmune sequelae; however, chronic idiopathic urticaria (CIU) is a very FDA-certified and listed in food labels. However, natural color additives are
rare manifestation. While omalizumab is effective in patients with CIU, its exempt from FDA-certification and labeled as natural color. Annatto is a nat-
mechanism of action in these patients is not completely understood and its ural color additive extracted from the seeds of Bixa Orella trees that imparts
role in autoimmunity and anti-FceRI autoantibodies is unclear. We present a an orange-yellow color to foods. The prevalence of adverse reactions to food
case of CIU in an APECED patient refractory to standard therapy that resolved additives in the US is less than 1% in adults but 2-7% in children and higher
with omalizumab. Case: APECED was diagnosed at age 9 after an ICU admis- in those with atopy. We present an IgE mediated reaction to annatto in a 4 y/o
sion for severe hypocalcemia and tetany secondary to hypoparathyroidism. atopic child. She developed urticaria within minutes of eating mac and cheese
Genetic testing revealed the patient was a compound heterozygote with muta- at a chain restaurant on two separate occasions. She also had urticaria with
A54 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A55
ABSTRACTS: POSTER SESSIONS
angioedema immediately after eating ice cream sandwiches, pasteurized cheese torso to her hands and feet and then became generalized with sparing of the
and boxed cheeseburger pasta. She tolerates chocolate, peanut, hazelnut, milk, head and neck. Symptoms started about 2 hours after coming out of the ocean.
wheat and egg ingredients in above foods without reaction. Ingredient review Patient had gone into the ocean previously even swimming at the same general
for the mac and cheese and ice cream sandwiches both contained annatto seed. beach area without incident. Patient also claimed that her family was with her
The boxed cheeseburger pasta only listed natural flavors and coloring. Skin in the same ocean water and did not develop the same symptoms. Crusting of
prick test to annatto extract was positive (8x30 mm) compared to negative the rash with associated blistering with additional pruritis and discomfort fol-
control (5x9 mm). Use of annatto as natural alternative to artificial color is lowed over the next 3-4 days. Vital signs were stable. There was blistering and
exempt from FDA certification and gaining popularity. It is labeled as all nat- crusting noted on the skin on physical exam. Patient was given hydrocortisone
ural, no artificial food coloring, achiote, pimentao, bixin or norbixin. Annatto 2.5% ointment to be applied topically in a thin layer to the affected areas as
is used in cheeses, dairy spreads, rice, custard powder, baked goods, snacks, needed only and placed on cetirizine 10 mg po daily for 2 weeks duration. Dis-
cereals and smoked fish. Despite its widespread use, there have only been 2 cussion: Seabather’s eruption is a self limited reaction that results in a highly
cases in adults of IgE mediated reaction to annatto. We present the first case pruritic papular rash on exposure to seawater. It results from a hypersensitiv-
of IgE mediated reaction to annatto in a child. Our patient had no other food ity to thimble jellyfish larva (Linuche Unguiculata). Cases are noted from March
allergies and the timing of ingestion of annatto-containing food and develop- to August but peak incidence is in May and June. The eruption is seen in the
ment of symptoms with a positive immediate hypersensitivity skin test to annatto United States east coast of Florida. Bathing suits are believed to trap the lar-
extract is highly suggestive of an IgE mediated reaction. It is increasingly impor- vae which then discharge a venom, the significance of which is unknown. Swim-
tant to investigate reactions to natural food coloring in patients with symp- mers washing themselves off with fresh water with their bathing suits off and
toms to multiple unrelated foods. As advocates for our patients, allergists should those that refrain from wearing their bathing suits for an extended period of
advocate for FDA certification and specific labeling for all natural flavors and time are found to be better protected against Seabather’s Eruption. Conclusion:
coloring. Providers should be careful to avoid narrow differential diagnoses when patients
present with rashes. Seabather’s eruption should be considered in the differ-
ential in patients presenting with pruritus and papular rash and proper history
P108 and physical exam should be conducted to ascertain relevant information for
EXTRAOVARIAN PRIMARY PERITONEAL CARCINOMA AND this diagnosis. Supportive measures with symptomatic care is the treatment of
ABDOMINAL COCOON SYNDROME INITIALLY PRESENTED choice.
AS DERMATOMYOSITIS: A CASE REPORT.
N.F. Morgal*, M. Patrimonio, S. Sonza, A. Jesena, M. Tupas, V. Gasataya,
Iloilo, Philippines.
Background: Dermatomyositis (DM) is an idiopathic autoimmune myopa-
thy that predominantly targets the skin and skeletal musculatures. This report
describes an unusual case of a patient having both Extraovarian Primary Peri-
toneal Carcinoma (EOPPC) and Abdominal Cocoon Syndrome (ACS) who ini-
tially presented with Dermatomyositis. Case Summary: This is a case report
of 47-year old woman admitted due to rashes. History revealed that 7 months
prior to admission, there was note of multiple, pruritic erythematous macula
rashes prominent on the face, neck and chest. She was admitted and managed
as case of hypersensitivity reaction. Six months prior to admission, the skin
lesions over the face and chest recurred associated with raised violaceous, scaly
papules on the metacarpophalangeal, proximal interphalangeal and distal inter-
phalangeal joints on both hands and erythematous, cracked and roughened peri-
ungal areas. Patient was readmitted and diagnosed with dermatomyositis. She
was started on prednisone and methotrexate. Three months prior to admission,
an abdominal distention associated with difficulty of breathing was noted and
underwent abdominal CT scan revealing moderate ascites thus paracentesis
was done. Ascitic fluid analysis was positive for malignant cells. Medical onco-
logic consult was sought. Patient came in with BMI of 18.3 kg/m2, pale con-
junctivae, macular hyperpigmented lesions at the neck and shoulder area, scaly FIG1 - Seabather’s Eruption Rash.
papules at the MCP, PIP, DIP of both hands, distended abdomen with shifting
dullness and grade 1 pitting bipedal edema. CA-125 was elevated among the
requested tumor markers. Exploratory laparotomy with tenckhoff catheter inser-
tion was done with. intraoperative findings of encapsulated mass, thick walled
P110
UTILITY OF A WEBSITE BASED DATABASE OF DRUG
containing the bowels adherent to the anterior abdominal wall and sidewalls ALLERGY: AMERICAN IMPRESSIONS.
and foul smelling ascitic fluid. Uterus and both ovaries were atrophic. Biopsy
of peritoneal tissue revealed psammoma bodies. With these pertinent find- N.P. Joshi*1, T. Pun2, V. Jain3, M. Sidhu4, L. Miller1, 1. St. John’s, NF,
ings, EOPPC and ACS were considered. Patient endured cycles of chemother- Canada; 2. Toronto, ON, Canada; 3. Winnipeg, MB, Canada; 4. London,
apy using Carboplatin and Paclitaxel. Conclusion: The incidence of classic DM ON, Canada.
is 5.5 cases per million per year. The reported frequency of malignancy varied Rationale: Drug allergy consults are challenging due to the dearth of pub-
from 6% to 60% with most large population based cohort studies revealing a lished data. Furthermore, there are few international journals who publish
frequency of about 20 to 25%. case reports of drug allergies. This study aims to determine the utility of a web-
site-based database of drug allergy case reports and desensitization protocols
among American allergists. An online survey was administered to American
P109 allergists, who are members of the American Academy of Allergy, Asthma and
A CASE OF A HYPERSENSITIVITY REACTION SECONDARY Immunology (AAAAI). Methods: A semi-structured survey was created and
TO SEABATHER’S ERUPTION. administered to members of the AAAAI. The questions were split into two
S. Ringwala*1, R. Rishi1, S. Fatteh2, 1. Fort Lauderdale, FL; 2. Plantation, parts: demographics and database design. The demographics section of the sur-
vey strives to ascertain the types of drugs commonly consulted for and the fre-
FL.
quency of these consults. The next section attempts to elucidate how Ameri-
Objective: To assess the appropriate evaluation and management options can allergists proceed with desensitization protocols- earlier research with
for a patient with Seabather’s Eruption (Sea Lice). Seabather’s Eruption is an Canadian allergists showed that personal experience was the most used resource.
entity that should be included in the differential diagnosis of patients present- Results: 193 members of the AAAAI answered the survey. In terms of what
ing with rashes and appropriate supportive care should be offered. Methods: percentage of consults were related to drug allergies 62.1% estimated 1-10%,
Case Report Results: This is a 12 year old female from South Florida that pre- with 22.6% estimating 10-25%. When discussing which drugs patients are con-
sented with a rash that started under her bathing suit top after going swimming sulted about- the vast majority (>95%) said they had been consulted for Peni-
in the ocean. The rash was maculopapular and pruritic. It spread from her
VOLUME 113, NOVEMBER, 2014 A55
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A56
ABSTRACTS: POSTER SESSIONS
cillins, and Cephalosporins. Similarly when asked which drugs they had been cromolyn, monteleukast and omalizumab more than three years ago. This
consulted for a desensitization protocol 93.1% of respondents named penicillin. resulted in sustained weight gain, improved tolerance to previously sensitive
When asked what resources they use for researching desensitization protocols foods and aeroallergens, minimal hair regrowth, and decreased frequency and
82.8% said specific E-Journals, 76.6% said E Journal search database, and severity of urticaria. Despite improvements on optimal medical therapy, over-
69.3% use online search databases such as google or Uptodate. When asked if all symptom control and quality of life remain poor. The patient is considering
they would utilize a website database of case reports on drug hypersensitivity other treatment modalities including allogeneic hematopoietic stem cell trans-
reactions and desensitization protocols 82.9% responded yes with 54.1% of plantation, which has been described in two small series for SM with variable
respondents also being interested in submitting to the database. In discussing outcomes. Conclusions: MCAS is a diagnosis of exclusion that warrants con-
the characteristics that would be most important in the database respondents sideration in patients with chronic multisystem complaints of unclear etiol-
felt overwhelmingly (>85%) that it should be structured and contain informa- ogy. MCAS diagnosis and management are evolving; additional research is
tion pertaining to patient demographics, medication usage, desensitization pro- necessary for understanding the etiology and natural history of this disease.
tocols and patient presentation. Conclusion: There is widespread support among
American Allergists for the creation of a database of drug allergy. The next log-
ical step is to gather support to create this database, which will require a mul- P113
tistakeholder approach. A RARE CASE OF BREASTFEEDING ANAPHYLAXIS.
A. Speck*, M. McMorris, Ann Arbor, MI.
Introduction: Breastfeeding anaphylaxis is rare, but potentially fatal. Symp-
P111 toms range from urticaria to hypotension and syncope and occur in close rela-
OLIVE OIL SENSITIVITY AND DESENSITIZATION: A NON-IGE
tion to lactation. The pathogenesis of the reaction remains unclear; however,
MEDIATED MECHANISM. hormone shifts related to the end of gestation and the beginning of lactation
M. Karam*1, T. Franxman2, M. McMorris1, J. Baldwin1, 1. Ann Arbor, MI; seemingly play a role. Waning levels of progesterone postpartum and loss of
2. Lexington, KY. its mast cell stabilizing effect has been one hypothesized mechanism, though
Introduction: The pungency of extra virgin olive oil (EVOO) is attributed the roles of oxytocin, prolactin, adrenocorticotrophic hormone (ACTH), cor-
to one of its phenolic compounds called oleocanthal (OC) and is mediated ticotropin-releasing hormone (CRH) and increased numbers of antepartum
through the transient receptor channel potential cation channel ankyrin sub- mammary and uterine mast cells have also been questioned. In addition, NSAIDs
type 1 (TRPA1) expressed in the posterior oropharynx. EVOO also mimics may also be a contributing factor. Methods: Presentation, evaluation, diagno-
the pharmacology of ibuprofen in that both agents cause a dose-dependent inhi- sis and management of a patient with breastfeeding anaphylaxis. Data: A 25
bition of cyclooxygenase enzymes COX-1 and COX-2. EVOO sensitivity has year old gravida 3 para 3 woman was admitted with anaphylaxis on postpar-
been described in the literature previously however EVOO desensitization has tum day 3 following the birth of her third child. She had breastfed her first child
not. Herein we report the first case of successful EVOO desensitization using for 2 months without difficulty. Three days after the delivery of her second
a novel EVOO desensitization protocol. Case Description: A 25-year-old patient child, she developed isolated urticaria after breastfeeding. She discontinued
with medical history significant for aspirin sensitivity, exercise induce asthma breastfeeding and symptoms resolved. Her third child was born via uncompli-
and mixed vasomotor and allergic rhinitis presented with a history of facial and cated vaginal delivery. She had been taking 600 mg of ibuprofen every 8 hours
tongue pruritus, throat irritation, coughing and hives within minutes of olive following the delivery, but was on no other medications. Breastfeeding was
oil consumption. Symptoms required diphenhydramine however several prior uneventful for the first 48 hours after delivery. On postpartum day 3, however,
episodes required epinephrine. A series of food and drug challenges were enter- with the first breastfeeding after generation of mature milk, she developed dif-
tained to establish the mechanism of EVOO sensitivity in this patient. Also a fuse urticaria, tongue swelling, emesis, and dizziness. On admission, she was
novel EVOO desensitization protocol was devised. Discussion: EVOO desen- tachycardic, tachypneic, and hypotensive. A tryptase level obtained 6 hours
sitization has not been attempted previously in the literature and in this report after the episode was elevated at 14.6 ng/mL (normal < 11.5 ng/mL). The patient
we describe the first case of successful EVOO desensitization using a novel desired to continue breastfeeding. She was placed on prophylactic cetirizine
EVOO desensitization protocol. Furthermore the patient continues to be in a 10 mg BID and all NSAIDs were discontinued. She subsequently breastfed
desensitized state 2 years after the procedure maintained with daily doses of successfully for 24 hours while under close observation. Conclusions: Our
10 ml EVOO. Although the mechanism of her reaction is likely due to OC stim- patient had anaphylaxis with breastfeeding on postpartum day 3 when lacto-
ulation of TRPA1, the mechanism of desensitization and maintenance of the genesis was established. She subsequently tolerated 24 hours of breastfeeding
desensitized state is unclear and requires further study. without difficulty with the use of cetirizine 10 mg BID and avoidance of
NSAIDs. Our case suggests that mothers with a history of breastfeeding ana-
phylaxis and a desire to breastfeed can likely do so with appropriate treatment
P112 and counseling.
LONGITUDINAL MULTIMODAL THERAPY IN A PATIENT WITH
MAST CELL ACTIVATION SYNDROME.
A.S. Chau*1, L. Helfner2, V.R. Bonagura2, A.M. Jongco2, 1. Mineola, NY;
P114
CROSS-REACTIVITY TO BALSALAZIDE IN A MESALAMINE
2. Great Neck, NY.
HYPERSENSITIVE PATIENT.
Background: Mast cell activation disorders (MCAD) affect multiple sys-
tems and are caused by episodic mast cell mediator release. Intrinsic defects R. Rishi*1, H. Nasir2, S. Ringwala1, S. Fatteh3, 1. Fort Lauderdale, FL;
in mast cell proliferation or activation are found in primary MCAD such as sys- 2. Miami, FL; 3. Plantation, FL.
temic mastocytosis (SM) and monoclonal mast cell activation syndrome. In Objective: To determine the safety of replacing mesalamine with other 5-
secondary MCAD such as allergic disorders, mast cells that are normal in quan- aminosalicylic (5-ASA) formulations in patients with hypersensitivity to
tity and function respond to external stimuli (i.e., allergens). In idiopathic mesalamine. Patients with inflammatory bowel disease (IBD) such as ulcera-
MCAD, such as mast cell activation syndrome (MCAS), there is no identifi- tive colitis are usually treated with 5-ASA preparations such as mesalamine.
able cause of mast cell activation. We describe the longitudinal clinical course These drugs are first line medications used to treat mild to moderate ulcera-
and management of a patient with MCAS. Methods: A 49-year-old woman tive colitis due to their steroid-sparing effects. Balsalazide is a dimerized 5-
diagnosed with autoimmune disorder, not otherwise specified, status post ASA preparation that may be tolerated in patients with hypersensitivity to
thymectomy originally presented with chronically elevated IgE and ANA, alope- mesalamine. Due to its structural differences, dimerized 5-ASA medications
cia universalis, weight loss, chronic idiopathic urticaria and multiple food sen- may be considered to be safe alternatives due to a presumed lack of cross-
sitivities. Extensive evaluation revealed multiple aeroallergen hypersensitivity reactivity. Methods: Case Report Results: A 39-year-old Caucasian female pre-
and unremarkable bone marrow studies. There was no evidence of immune sented to our service after experiencing anaphylaxis following use of
deficiency, autoimmunity, IgE-mediated food allergies, SM and celiac disease. mesalamine (Asacol). She had been using mesalamine for 19 years to control
Results: Urine histamine and histamine release assay were normal. Serum her mild to moderate ulcerative colitis. Six months ago, she experienced dif-
tryptase was unremarkable repeatedly. Her symptoms did not improve after tri- fuse urticaria and generalized pruritus one hour after taking her morning dose
als of immunosuppressive and immunoglobulin replacement therapy. In col- of mesalamine. She took diphenhydramine, and her symptoms resolved within
laboration with the Center of Excellence for Mastocytosis and Mast Cell Acti- hours. The next day, she took her morning dose of mesalamine and experienced
vation Disorders at Brigham and Women’s Hospital, she was started on an immediate anaphylaxis. She developed laryngeal edema, diffuse urticaria, and
aggressive anti-inflammatory regimen including H1 and H2 antihistamines, generalized pruritus. The patient was treated with epinephrine, and her symp-
A56 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A57
ABSTRACTS: POSTER SESSIONS
toms resolved. The patient underwent a provocative drug challenge with bal-
salazide (Giazo) in our clinic over two days. The patient reacted on the second
day when she experienced swelling of her hands and generalized pruritus. The
patient was administered oral antihistamines and corticosteroids and her symp-
toms resolved within four hours. Conclusions: Cross-reactivity may occur
between different 5-ASA preparations despite their structural differences.
Patients with inflammatory bowel disease who are hypersensitive to mesalamine
may also react to balsalazide and olsalazine. Mesalamine hypersensitive patients
should not be started on these medications without undergoing a provocative
drug challenge. We designed an outpatient protocol that will safely enable
patients to undergo testing in an office setting.
Balsalazide (Giazo) Provacative Challenge Protocol
P115 Tongue swelling in endotracheally-intubated patient
A CASE OF TONGUE SWELLING CAUSED BY ENDOTRA-
CHEAL TUBE-INDUCED VASCULAR OBSTRUCTION.
M. Saifi*, J.A. Bird, Dallas, TX. P116
HYPERSENSITIVITY REACTION TO SUBCUTANEOUS
Introduction: Allergists are commonly asked to evaluate the etiology of IMMUNOGLOBULIN.
tongue swelling. We report a case of a woman with 16 days of tongue swelling
secondary to endotracheal tube (ETT)-induced vascular obstruction of the base Q. Rashid*, A. Grant, Galveston, TX.
of the tongue. Methods: Case Report. Data: A 55 year-old female with systemic Introduction: Immunoglobulins (Ig) are routinely used in management of
lupus erythematosis, end-stage renal disease, hypertension, and congestive heart Primary Immune Deficiency diseases (PIDD). Ig formulations differ based on
failure presented to the emergency department with acute onset shortness of the content of IgG, IgA, osmolality and stabilizer. Most adverse reactions to
breath and somnolence. MRI revealed bilateral intraventricular hemorrhage IVIG are either due to a rapid rate of infusion or IgA deficiency. We report a
and chest imaging revealed pneumonia. She was intubated secondary to res- case of hypersensitivity reaction to the stabilizer in the Ig formulation. Meth-
piratory distress. Tongue swelling was reported 2 days after intubation and wors- ods: A 50 year old female with a 3-year history of CVID was referred by her
ened over the next 2 days. Physical examination revealed a swollen tongue, allergist for management of hypersensitivity reaction to subcutaneous
which was at least 2-3 times the size of normal, protruding out of her mouth. immunoglobulin. She had been treated with subcutaneous hizentra weekly for
Pressure ulcers were noted on the base of the tongue. Laboratory evaluation 2 years; however, 2 months ago she developed an urticarial rash 20 minutes
revealed normal C3 and C4. Due to concern for oropharyngeal edema, a tra- after taking her usual dose. Subsequent doses caused immediate symptoms of
cheostomy was performed. Swelling had not improved 14 days after intuba- throat closure, difficulty breathing, swallowing and low blood pressure requir-
tion and a 4 day course of dexamethasone was administered without improve- ing treatment with epinephrine, prednisone and antihistamine in the ER. She
ment in swelling. Tongue swelling improved 1 day post-extubation and resolved denied symptoms of nausea, vomiting, fever, chills or headache. Hizentra was
within 2 days. Past medical history was significant for lisinopril-induced subsequently discontinued and she was referred to UTMB for further evalua-
angioedema. The patient did not receive an ACE-inhibitor or ARB prior to or tion. On evaluation, her history was negative for allergic or anaphylactic reac-
during admission and medication regimen did not change prior to or post-res- tions to other medications and IgA deficiency was ruled out. Skin prick test-
olution of swelling. The differential diagnosis of tongue swelling includes hered- ing to Ig was not helpful due to dermatographism. The patient was treated
itary angioedema (AE), acquired AE, medication-related AE, mechanical with Gammagard, chosen for the differences in osmolality and stabilizer con-
obstruction, and sublingual hematoma secondary to a difficult intubation. tent vs. Hizentra. Patient received a slow infusion of Gammagard and was
Tongue swelling was attributed to venous obstruction secondary to local subsequently switched to SC administration without further reactions. Dis-
mechanical compression of the base of the tongue by ETT. This is supported cussion: Hizentra contains the stabilizers L-proline and polysorbate 80, whereas
by a normal C4, onset of swelling after ETT placement and resolution after Gammagard contains only glycine. Polysorbate 80 is commonly used in vac-
ETT removal, and the prolonged course of swelling (16 days). Conclusion: cines, chemotherapy and tablet formulations. It has been reported to cause non
Mechanical obstruction of venous drainage should be considered as an etiol- IgE mediated anaphylactic reactions in patients receiving Docetaxal and is the
ogy of prolonged tongue swelling in intubated individuals. most likely cause of hypersensitivity reaction in our patient. No hypersensi-
tivity reactions with L-proline have been reported in literature. Hizentra also
has higher osmolality as compared to Gammagard but the adverse reactions
due to high osmolality usually include thrombosis and kidney injury which
were not present in our patient. Conclusion: We report a rare case of hyper-
sensitivity reaction to a stabilizer in Hizentra, an Ig formulation used for treat-
ment of PIDD. This report alerts the allergist/immunologist about work up and
VOLUME 113, NOVEMBER, 2014 A57
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A58
ABSTRACTS: POSTER SESSIONS
management of patient’s with hypersensitivity reaction to an immunoglobulin sideration of CF as an explanation of recurrent sinopulmonary disease in a pre-
formulation. viously “healthy” adult is certainly unusual. Growing evidence of the diverse
genotype-phenotype relationships in CF and reported variability in disease-
onset suggests that a diagnosis of CF be evaluated in adults with recent-onset
P117 pneumonia, bronchiectasis, and sinopulmonary disease.
EOSINOPHILIC CHOLECYSTITIS IN AN ASPIRIN EXACER-
BATED RESPIRATORY DISEASE (AERD) PATIENT.
L. Finkas*, R. Katial, Denver, CO.
Introduction: A rare case of eosinophilic cholecystitis in a patient with
AERD Case: 50-year-old male with past medical history of asthma, chronic
sinusitis with nasal polyps, and AERD. He underwent aspirin desensitization
a few years prior and had improvement in both his asthma and sinus disease.
Following desensitization, he was maintained on aspirin 650 mg BID and was
subsequently decreased to 325 mg BID. He presented for routine 6 month fol-
low up at which time he had been experiencing significant gastrointestinal
symptoms for the previous 3 weeks. His symptoms began as indigestion and
heartburn and progressed to diarrhea and vomiting. His PMD had placed him Image 1: Chest CT (left) revealing cylindrical and varicoid bronchiectasis;
on a course of antibiotics, but despite antibiotics, he continued to have symp- sinus CT (right) revealing chronic maxillary sinusitis.
toms. Stool studies were obtained and C-diff was negative. His aspirin dose
was decreased to 81 mg without improvement in GI symptoms. Further diag-
nostics were pursued and complete blood count was notable for an elevated P119
WBC of 14,000 with an absolute eosinophil count of 6100. Liver function tests, PROTRACTED ANGIOEDEMA IN A 9-YEAR-OLD GIRL: PROPO-
ESR and CRP were within normal limits. He was evaluated in the emergency FOL AND FOOD ALLERGY.
room given his persistent symptoms and was found to have cholecystitis. He S.K. Lin*, T.B. Fausnight, Hershey, PA.
underwent a cholecystectomy and pathology revealed transmural inflamma-
Introduction: According to package inserts, use of Diprivan brand propo-
tory cell infiltrate composed predominantly of eosinophils. Bone marrow biopsy,
fol or Fresenius brand propofol is contraindicated in patients with soy or egg
EGD and colonoscopy were performed for possible hypereosinophilic syn-
allergy. This is due to the use of soybean oil and egg lecithin as excipients and
drome. His bone marrow biopsy was negative for FIP1L1/PDGFRA mutation
the potential for soy or egg protein contamination. Fresenius is additionally
and was only notable for mild eosinophilia. EGD and colonoscopy were neg-
contraindicated in peanut allergic patients due to potential cross-reactivity
ative for eosinophilic infiltrate. He remained on aspirin during this time and
between peanut and soy. Case Report: A 9-year-old girl with history of Chiari
following his surgery increased to 325 mg daily. Following cholecystectomy,
malformation was noted to have swelling of her face, lips, and tongue after neu-
the patient had significant improvement in his peripheral eosinophilia and his
rosurgery. She had a history of identical reactions to fresh egg and peanut, and
eosinophil count retuned to his baseline of 400. His gastrointestinal symptoms
anesthesiology suspected her reaction was due to Fresenius and her peanut
resolved. Conclusion: This is the first case of a rare eosinophilic process iso-
allergy. She had tolerated Diprivan at least 7 times before, most recently 2
lated to the gallbladder in a patient with AERD, which in itself is manifested
months prior. She was given H1 and H2-blockers and was extubated postop-
by increased circulating eosinophils in over half the patients. The authors have
eratively, but then developed stridor, wheezing, desaturations, and again had
previously reported rare complication of pancreatitis after aspirin desensitiza-
lip and tongue swelling. She continued to be symptomatic despite anaphylaxis
tion and a few unpublished cases of increased GI symptoms with eosinophilia.
management and required an epinephrine drip and nasal intubation. She required
This shows another possible complication in AERD patients with underlying
a slow 7 day wean off epinephrine. Results: Total tryptase level drawn at hour
eosinophilia.
four was 4 ng/mL. C4 and C1 esterase inhibitor levels were normal. IgE lev-
els for egg white, egg yolk, and soy were negative, while peanut was positive
at 1.27 kU/L. Follow up skin testing to egg and soy were negative, and peanut
P118 was positive (5 mm wheal). Discussion: After literature review, we found that
DIAGNOSIS OF CYSTIC FIBROSIS IN 59-YEAR-OLD WOMAN
the vast majority of patients with soy, egg, or peanut allergy receive propofol
REFERRED FOR IMMUNE DEFICIENCY. without issue. In one study, there were no adverse reactions to propofol amongst
C. Dutmer*, E. Gelfand, Denver, CO. 45 food allergic patients. Despite its contraindication in peanut allergic patients,
Introduction: Cystic fibrosis (CF) is a disease caused by mutations in the Fresenius does not contain any ingredients which make it more allergenic than
CF transmembrane conductance regulator (CFTR) gene, resulting in deleteri- Diprivan in patients with egg, soy, or peanut allergy. While we have not yet been
ous effects on epithelia of various tissues. Though the classic CF phenotype is able to identify the cause of our patient’s protracted reaction, we do not sus-
characterized by progressive pulmonary disease and associated exocrine pan- pect it was related to her peanut allergy. Conclusion: Care should be taken to
creatic insufficiency in childhood, disease phenotype varies greatly by specific understand the reasoning behind food allergy contraindications of medications,
CFTR mutations, associated genetic modifiers, and environmental factors. as these can often be given to food allergic patients without issue. Such con-
Nearly 2,000 CFTR gene mutations have been identified, highlighting the allelic traindications may cause unnecessary avoidance of medications and/or may
heterogeneity in the CFTR gene. Discovery of new mutations (and associated distract from the identification of a true medication allergy.
factors) may explain the diverse nature of CF-related disease phenotypes with
varying age of onset and recognition. We describe a 59-year-old woman eval-
uated for immune deficiency in whom CF was diagnosed. Case Description: P120
A 59-year-old Caucasian woman with chronic obstructive pulmonary disease MANAGEMENT OF HYPOGAMMAGLOBULINEMIA DURING
and a 40 pack-year cigarette smoking history presented with an 18-month his- MEASLES AND MUMPS OUTBREAK IN PATIENTS TRANSI-
tory of recurrent pneumonia and sinus disease as well as an episode of pan- TIONING OFF IMMUNOGLOBULIN REPLACEMENT.
creatitis. Prior history was notable for the absence of significant infection. She K. Strothman*, R. Scherzer, Columbus, OH.
recently required numerous hospitalizations and had subsequently required sup-
plemental oxygen while suffering from chronic dyspnea and cough. Expecto- Introduction: In a country where the transmission of many diseases has
rated sputum and bronchoalveolar lavage bacterial cultures revealed mucoid been largely eliminated by vaccination, the widespread outbreak of preventa-
Pseudomonas aeruginosa. Cylindrical and varicoid bronchiectasis as well as ble illness could modify management and treatment options of patients with
chronic maxillary sinusitis were evident on CT (Image 1). Quantitative serum hypogammaglobulinemia. We describe two patients with a history of hypogam-
immunoglobulin levels were normal as was the remainder of her immune eval- maglobulinemia who were in the process of transitioning off IgG replacement.
uation. Family history identified a paternal first cousin once removed with CF In light of the measles and mumps outbreak in Ohio, these patients were either
as well as carrier status for a CF gene mutation in the patient’s daughter. Sweat continued or restarted on IgG replacement. This was due to their unvaccinated
chloride testing was elevated at 72 mmol/L and CFTR gene sequencing analy- status and the recommended interval between receiving antibody-containing
sis revealed two mutations: deltaF508 and R117H. Discussion: New-onset products and administration of a measles-containing vaccine. Case Reports:
sinopulmonary infections in the 6th decade of life of a long-standing smoker Case 1 involves a 5 year-old female who was introduced to the Immunology
prompted initial concern for secondary or acquired immune deficiency. Con- service at 5 weeks of age during an admission for bronchiolitis. Immunology
A58 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A59
ABSTRACTS: POSTER SESSIONS
was consulted for recurrent respiratory infections. Her clinical course was com- gitis and subsequent left-sided stroke, allergic rhinitis (based on positive skin
plicated by pneumothorax, bronchopleural fistula, and necrotizing pneumonia. testing), and asthma, who presented to the hospital for headaches and vomit-
Her immune workup was normal except for a gradually declining IgG level. ing after two minor head traumas at daycare. Because of her history, CSF stud-
Stool α-1-antitrypsin initially high, favoring the diagnosis of hypogamma- ies were obtained and revealed recurrent meningitis, which prompted further
globulinemia secondary to a protein-losing enteropathy. She started IgG replace- workup confirming the CSF leak. She was found to have a congenital cochlear
ment at 15 months. By 4 years of age, there was discussion to begin weaning malformation, which was then repaired by otolaryngology. Outcome & Dis-
IgG replacement. This was halted due to concern about the measles and mumps cussion: Retrospectively, her history and various hospital visits were all con-
outbreak. Case 2 is that of a 2 year-old male who presented in the first month sistent with CFS leakage. The patient actually presented to the hospital at 9
of life with enterocolitis and dehydration. He had a low total protein, albumin, months of age after a minor fall with reported vomiting and lethargy. After-
and IgG level thought to be due to GI losses, although stool α-1-antitrypsin wards, she was seen at various points for upper respiratory infections, allergic
negative. Work-up for a unifying diagnosis was negative. History now thought rhinitis, as well as meningitis with stroke, and asthma with hypoxia. She was
to be most consistent with transient hypogammaglobulinemia of infancy. He also seen by an allergist/immunologist for workup of her food allergies and
was started on IgG replacement at 4 months. At 2 years he was weaned off IgG asthma. She was diagnosed with allergic rhinitis based on clinical history of
replacement and remained off for 6 weeks. Secondary to concern over the rhinorrhea and mildly positive environmental skin testing. The rhinorrhea
increased risk of exposure to measles or mumps through his particular daycare showed moderate improvement with intranasal corticosteroid treatments. Dur-
setting, IgG replacement was restarted. Conclusions: These cases highlight ing her first episode of meningitis, she had a basic immunological workup
the challenges that exist for our patient population with Immunoglobulin Defi- including immunoglobulin and complement levels and vaccine titers, which
ciency due to the reemergence of vaccine-preventable illness. As these expo- were all normal. It was not until her second episode of known meningitis that
sures continue to increase, we must modify our treatment plans to provide opti- there were considerations for CSF leak as a source of her infections. Both
mal care and ensure patient safety. instances of meningitis were only suspected because of acute neurological signs.
Conclusion: Though rare, CSF leakage should always be considered in the dif-
ferential for clear rhinorrhea and recurrent meningitis. In our case, there were
P121 several clues for CSF leakage including: history of head trauma, persistent clear
MUSTARD SEED ANAPHYLAXIS. rhinorrhea despite appropriate therapy for allergic rhinitis, and recurrent menin-
L. Cuervo-Pardo*, A. Gonzalez-Estrada, J. Fernandez, Cleveland, OH. gitis despite a normal immune evaluation.
Introduction: Food is the most common cause of anaphylaxis (Lieberman
P et al. J Allergy Clin Immunol. 2010). Very few cases of mustard seed induced P123
anaphylaxis have been reported. We present a case of mustard seed anaphy-
OMALIZUMAB MAY PREVENT PERFUME TRIGGERED
laxis. Methods: A case report Results: 29 year old man presented to our depart-
ment for evaluation of anaphylaxis. He had an episode of generalized urticaria LARYNGEAL ANGIOEDEMA.
(Figure A), chest tightness, vomiting, facial flushing and angioedema (Figure R.M. Young*, P. Ciminera, East Meadow, NY.
B), within 30 minutes of eating a prepared quinoa dish at home. He did not Introduction: Omalizumab is a monoclonal antibody to IgE indicated for
seek medical attention and his symptoms resolved within hours of self-admin- use in asthma but also used in other IgE mediated conditions i.e.Allergic Rhini-
istration of loratadine and diphenhydramine. He had no relevant past medical tis and recently indicated for use in chronic urticaria. But could it have a role
history of previous adverse reactions to foods. Upon further questioning, the in irritant induced angioedema? Methods: N/A Case Report: This is a 16yr old
ingredients in the quinoa dish included: chicken, rice, avocado, ginger, onion, female who had multiple hospitalizations for status asthmaticus x 2 yrs. Sinusi-
potatoes, tomato, nutmeg, yeast, soy, wheat, black pepper, thyme, and mustard tis, GERD, allegies to environment/foods were diagnosed as well as Paradox-
seed. He had previously tolerated quinoa without adverse reactions. However, ical Vocal Cord (PVC) dysfunction by ENT via rhinoscopy. On exposure to
the two last ingredients were obtained from a new brand. His physical exam dust, acid reflux, chlorine in a pool or indoor pollutants like perfumes, she’d
was unremarkable. Percutaneous skin testing was positive to soy and prick- develop nasal congestion, hoarseness, a barking cough, and throat tightness.
prick testing to mustard seed. He was instructed on avoidance measures includ- She was placed on maximal medicines of steroid inhaler/LABA, montelukast,
ing food label reading and prescribed epinephrine auto injector. Conclusions: oral antihistamines, steroid nasal spray, pantoprazole, and oral steroids in an
This case report demonstrates the importance of an adequate clinical history effort to control these symptoms. But since PVC was also a problem, speech
and detailed content of ingredients. therapy/counseling were started as well as immunotherapy (IT). Despite this
regimen, when the patient was exposed to perfume in school, she required
Epinephrine, Diphenhydramine, and Albuterol for symptoms of cough, throat
closure and syncope with eventual admittance to the Pediatric ICU. This reac-
tion was so severe that the child became home tutored due to the fear of per-
fume exposure. A similar reaction but milder to dust mite IT was witness and
quickly reversed with Epinephrine and Diphenhydramine IM. The patient had
an IgE level of 1033 IU/ml, so Omalizumab was started. For the past 1 year,
she has received 375mg SQ every 2 weeks. She has returned to school and
normal activities and hasn’t had any symptoms requiring Epinephrine or
Albuterol on exposure to perfumes. Conclusion: Since the patient was on med-
icines to control asthma, GERD, and sinusitis, it was thought that her throat
closure was due to PVC triggered by the perfume. But Laryngeal angioedema
seem to be the culprit. Irritants like perfume may have an IgE mediated process
or a mechanism of destablizing mast cells similar to idiopathic anaphylaxis that
hasn’t been identified. Therefore, Omalizumab should be considered as a trial
therapy. More studies are needed using omalizumab for these cases.
P122 P124
ALLERGIC RHINITIS: UNASSUMING UNTIL MENINGITIS UNCONTROLLED ASTHMA IN A PRIMARY CILIARY
RECURRED. DYSKINESIA PATIENT TREATED SUCCESSFULLY WITH
OMALIZUMAB.
P. Uong*, R. Casper, Phoenix, AZ.
J.X. Lee*, A. Rafi, W.B. Klaustermeyer, J.S. Yusin, Los Angeles, CA.
Introduction: We present a case of a toddler with recurrent bacterial menin-
gitis of unclear etiology, various upper respiratory infections, allergic rhinitis, Primary cilia dyskinesia (PCD) is an autosomal recessive genetic disorder
and persistent cough who was eventually found to have a cerebral spinal fluid characterized by recurrent and chronic infections of the upper and lower res-
(CSF) leak. The case is interesting in that there were vague clues to her CSF piratory tract due to impaired mucociliary clearance. Patients with PCD can
leak over the years, but it was not until her second case of meningitis that have co-existing asthma. Omalizumab is a high affinity recombinant human-
prompted a cisternogram, which confirmed the diagnosis of a Mondini defor- ized monoclonal anti-IgE antibody which is commonly used to treat uncon-
mity. Case History: A 3 year-old female with a past history of bacterial menin- trolled moderate to severe allergic asthma. We report a case of 58 year old
VOLUME 113, NOVEMBER, 2014 A59
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A60
ABSTRACTS: POSTER SESSIONS
female with known diagnosis of PCD and persistent allergic asthma who pre- PTA when he started Interferon gamma (IFN-g) for asymptomatic hepatitis C.
sented with symptoms consistent with infections and expected course of PCD One week post IFN-g therapy, patient developed dyspnea and fatigue. Two
but were in fact due to uncontrolled asthma and successfully treated with Oma- weeks PTA, patient self discontinued IFN-g and then one week PTA devel-
lizumab. At the time of presentation, she was already on maximal therapy for oped a rash. Patient noted a pruritic rash starting on his scrotum which he ini-
airway clearance for her PCD. She had been treated with numerous courses of tially attributed to tinea cruris. He used nystatin powder, which temporarily
antibiotics for infection without improvement for the previous 5 years. At her relieved the itching however the rash began to spread to his bilateral lower
initial visit, her pulmonary function test revealed component of obstruction extremities and then to his upper body. During the three months preceding
with airway hyper-responsiveness that was reversible. Her physical exam admission, HIV regimen was also adjusted multiple times for increase in HIV
revealed coarse breath sounds and wheezing that improved after bronchodila- viral load. Review of laboratory studies showed peripheral eosinophilia (absolute
tion. Despite PCD being her dominant disease pathology, she was thought to eosinophil count: 1.8 K/cumm), peripheral smear with atypical lymphocyto-
have a component of uncontrolled allergic asthma. As she was maximized on sis, and stool examination for ova and parasites as well as serum testing for
Beta 2 agonist and inhaled corticosteroid therapy, the decision was made to Strongyloides were negative. Patient suffered from acute renal insufficiency.
start Omalizumab given her elevated total serum IgE level. Within 3 months Liver involvement was not detected. Patient was diagnosed with DRESS. Diag-
of starting Omalizumab, the patient reported significant improvement in her nostic criteria included fever, acute rash, hypereosinophilia, lymphadenopathy,
shortness of breath from baseline and her appetite. At the time of this report, and atypical lymphocytosis. DRESS was likely attributed to abacavir; however,
approximately 2 years after starting Omalizumab, she has an overall improve- other HIV medications or IFN-g could not be ruled out definitively as the cause.
ment in FEV1, improved symptoms of shortness of breath, and decreased exer- Patient required large doses of steroids to control symptoms and had an exten-
cise induced bronchospasm symptoms. In summary, due to their motile cilia sive hospital course. Post-mortem exam revealed cause of death to be gram-
disorder, PCD patients have variable degrees of decline in their pulmonary negative sepsis (Acinetobacter baumannii) without evidence of hepatic necro-
function. While a majority of their respiratory symptoms are likely due to struc- sis. Conclusion: In general, DRESS carries a mortality rate of 5-10%, which
tural lung damage related to recurrent infections, other etiologies for short- is in patients without co-morbid conditions. This case is unique because it illus-
ness of breath such as concomitant allergic asthma should not be overlooked. trates patients with DRESS and underlying HIV maybe suspect to even higher
In addition, the use of Omalizumab in the treatment of allergic asthma as add- mortality rates.
on therapy should be considered in patients with elevated total IgE level even
in the setting of significant structural lung disease.
P125
A RARE CASE OF FOOD INDUCED ANAPHYLAXIS TO BEET-
ROOT.
F. Pazheri*1, B. Schroer2, 1. Shaker Heights, OH; 2. Cleveland, OH.
Background: Beetroot is a common food ingredient and are consumed all
over the world. It is used as a food additive in many food products. Allergy to
beetroot (Beta Vulgaris) is rare. Until now only one case of apparent anaphy-
laxis to beet root consumption has been reported (de Oliveira et al, Clinical
and Translational Allergy 2011) ; there are a few reports of asthma and rhinocon-
junctivitis induced by inhaling the vapor of cooked beet. Methods: We report
a case of a 17 year old young man who had an anaphylactic reaction after eat- P127
ing beetroot. His medical history was notable for anaphylaxis to tree nuts, aller- PERSISTENT HIGH IMMUNGLOBULIN E LEVELS AND TUBER-
gic rhinitis, Latex allergy and a subsequent diagnosis of Crohn’s disease. The CULOSIS: A CASE REPORT.
patient had oral and throat itching, vomiting, and a sensation of throat closing
up within one minute after ingestion of one shot glass amount of a juice smoothie M. Yuksel, M. Nursoy*, A. Gedik, E. Cakir, Istanbul, Turkey.
containing ¼ of a beet, carrots, and apples in 16 Oz glass of juice smoothie Introduction: T helper1 (Th1) lymphocytes have important role in immune
made at home. Symptoms slowly resolved over the next hour after 50 mg of response against Tuberculosis(TB). Relationship between TB and high
diphenhydramine and monitoring in an urgent care clinic. He had never eaten immunoglobulin E(Ig E) levels with Th1 related mechanism was told in recent
beets before and there are no tree nuts in his home due to his tree nut allergy. studies and reduction in high Ig E levels was noted with TB therapy. Aim: To
He has safely eaten carrots and apples after the reaction. He was evaluated for discuss relationship between high and persistant Ig E levels and TB. Case:
possible allergy to beetroot with blood testing and skin prick testing. Results: Twelve-years-old female patient who have had chronic productive cough, fre-
Food specific IgE to beet root were positive at 2.52 KU/L. Skin prick test quent otitis and sinusitis since 6 months-old and was followed-up with asthma,
using fresh beetroot juice using a prick-prick method with a bifurcated needle resistant atelectasis of right middle lobe, bilateral bronchiectasis was admitted.
on the forearm was positive with a 9 mm wheal and 20 mm flare (Negative con- Previous tests were normal except high IgE (494 mg/dl), TB history of her uncle
trol 0/0 mm wheal/flare, histamine 6/20 mm wheal/flare). Beet sugar prick- 5 years ago. After admission, atelectasis was found in computarized tomogra-
prick skin testing and food challenge was negative. Patient has not had a sub- phy (CT) and bronchoscopy revealed dense purulent mucus. Aspergillus fumi-
sequent allergic reaction to any food since the reaction. Conclusion: Anaphylaxis gatus and Hemophilus influenzae were observed in BAL culture. Symptoms
to beetroot is very rare and this is the first case reported with positive fresh persisted and total IgE increased (1750 mg/dl) despite appropriate therapy.
food prick-prick testing that we could find. Refined beet sugar may not lead Aspergillus fumigatus in prick test, Aspergillus spesific IgE, control sputum
to reactions in beet allergic patients. culture, and immune deficiency tests were negative. PPD, Quantiferon test, and
ARB in gastric aspiratation were 20mm, positive and negative, respectively.
Control CT revealed multiple intrathoracic conglomerated lymph-nodes (30x25
P126 mm). Mediastinoscopic biopsy for Lyphoma resulted reactive hyperplasia. Anti-
DRUG REACTION WITH EOSINOPHILIA AND SYSTEMIC TB therapy was given to patient who had TB disease contact, PPD and quan-
SYMPTOMS (DRESS) PRESENTING IN AN HIV PATIENT tiferon positivity, infiltration and conglomerated lymph-nodes resistant to ther-
TREATED WITH INTERFERON AND ANTIRETROVIRALS. apy. Clinical and radiological improvement and reduction of IgE (289 mg/dl)
were seen in second months of therapy. Conclusion: This case was presented
S. Hamadani*, A. Wong, C. Parrish, S. Thobani, L. Scott, M. Li, Los due to rare presentation TB with high Ig E levels with almost complete improve-
Angeles, CA. ment.
Introduction: DRESS is a potentially life-threatening hypersensitivity reac-
tion associated with a variety of medications, generally anti-epileptics. Patients
present with rash, fever, hypereosinophilia, lymphadenopathy, and internal
organ involvement, often hepatitis, usually within two months after initiation
of a medication. Methods: Case report Results: A 50 year old African Ameri-
can Male with HIV (CD4=400), HCV Genotype 1a, and HTN, presenting with
rash for one week prior to admission (PTA). Patient was in his usual state of
stable health, with undetectable HIV viral load on HIV treatment, until 3 months
A60 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A61
ABSTRACTS: POSTER SESSIONS
P128 P130
EVALUATION OF EOSINOPHILIA: HYPEREOSINOPHILIC SYN- FIRST REPORTED CASE OF ANAPHYLAXIS INDUCED BY
DROME. POGONOMYRMEX SPP BITE IN MEXICO.
G. Rosner*1, D.W. Rosenthal2, 1. New York, NY; 2. Great Neck, NY. J. Fernandez de Cordova Aguirre*, A. Velasco-Medina, M.E. Arroyo-Cruz,
Background: Eosinophilia can have multiple etiologies including atopy, S. Gonzalez Flores, D. Cariño-Cartagena, G. Velazquez-Samano,
parasitic infections and Churg-Strauss. Hypereosinophilic syndrome(HES) can Mexico City, DF, Mexico.
be initiated by myeloproliferative and lymphocytic causes. Case Report: A 16 Stings and bites are a common cause of allergic reactions. We report a case
year old male was admitted for a 2-week history of new onset chest pain and of anaphylaxis by Pogonomyrmex ant bite. It was diagnosed by clinical fea-
shortness of breath. Four months prior to admission(PTA), the patient presented tures and confirmed with skin tests. Currently in treatment with specific
with transaminitis and peripheral eosinophilia to another academic medical immunotherapy. Case Report: Fifty-six years old male. A year ago, while work-
center, where corticosteroids were tapered over 2 months. Two weeks PTA, the ing in the garden home, he is bitten by an ant on his right hand presenting ery-
patient developed intermittent, severe, mid-sternal chest pain, shortness of thematous, pruritic confluent hives, swelling of eyelids, face and hands with-
breath, a racing heart, blurred vision, and dizziness, which progressively wors- out cough or respiratory distress. He improved with oral antihistamines. Six
ened as he developed bilateral joint pain. Results: Upon admission the patient months ago he suffers again an ant bite and besides the previous symptoms, he
had eosinophilia(3.9x109/L), ESR 38, IgE 130, LDH 375. Results from the has nasal obstruction, rhinorrhea, fatigue. He received treatment with intra-
prior admission showed an ultrasound with hepatic inflammation, and a liver muscular antihistamine and steroids. A month ago, he is bitten a third time by
biopsy with fibrosis, and rare portal and lobular eosinophils(Eos). Esophageal an ant. He presented confluent pruritic erythematous rash, eyelids, mouth and
biopsy revealed mild Eos infiltrates and bone marrow biopsy showed myeloid hands edema, cough and dyspnea, within minutes he had loss of conscious-
hyperplasia with increased Eos. Cytogenetic studies for FIP1L1-PDGFRA were ness. He treated with oxygen, 0.5 ml intramuscular epinephrine, intravenous
negative. During this admission, transaminases, bilirubin, alkaline phosphatase, steroids and intramuscular antihistamines, intravenous fluids and improves
cardiac enzymes, ANCA, tryptase, vitamin B12 and IL- 5 were all normal. CTA gradually until he is discharged. Complementary studies show 7100 leukocytes
chest and cardiac MRI were unremarkable. Chest X-ray showed bibasilar small with 59% neutrophils (4200), 30% lymphocytes (2200), 2.3% eosinophils (200),
pleural effusions, spirometry showed restrictive lung disease, and bronchial 0.4% basophils (4), blood chemistry, renal function tests and liver function tests
biopsy had mild Eos infiltrate. Infectious disease studies were unremarkable. are normal, nasal cytology with eosinophils, serum total IgE 1220 IU / ml. Skin
The patient was restarted on corticosteroids and Eos decreased(1.8x109/L). As tests were performed with the criteria AAAIC at a dilution of 1: 10,000 with a
corticosteroids were tapered over weeks, chest pain recurred with associated positive result for Pogonomyrmex harvester ants. Nonpharmacological therapy
increased Eos, C-reactive protein and LDH, which resolved with increased cor- (information, “allergic to ant” bracelets and emergency actions) and pharma-
ticosteroids. Discussion: Multiple etiologies of eosinophilia were considered cological (epinephrine, steroids, antihistamines, and albuterol) was initiated.
including infection, hematopoietic clonal eosinophilic proliferation, over-pro- Immunotherapy starting at 1:1,000,000 dilution was indicated. He is currently
duction of eosinophilic cytokines, Churg-Strauss and others. Symptoms were asymptomatic and in a dose escalating immunotherapy protocol. Discussion:
controlled with corticosteroids. The diagnosis of HES remains without a spe- We show allergic reaction to Pogonomyrmex spp ant with positive intradermal
cific molecular or laboratory biomarker. Thus, it remains essential to diagnose skin test. Immunotherapy is safe so far. Although it is still not established the
and treat HES when patients present with peripheral hypereosinophilia(>1.5x positive predictive value of a skin test, the combination of symptoms and skin
109/L on 2 examinations separated in time by at least 1 month) with tissue test reaction indicated an IgE-mediated reaction. Pogonomyrmex allergy could
hypereosinophilia(20% eosinophils on bone marrow biopsy, or significant be deadly. The immunological mechanism of anaphylaxis in this patient is
eosinophilic tissue infiltration) and with organ damage or dysfunction. caused by a type I hypersensitivity reaction.
P129 P131
TERMINAL ILEUM PERFORATION IN A PATIENT WITH THE DIAGNOSIS IS IN THE HISTORY: A CASE OF DRESS IN A
HYPER IGE SYNDROME. PEDIATRIC PATIENT.
J. Jiao*, C.C. Horner, A.L. Kau, St Louis, MO. B.J. Buelow*1, H.T. Zafra2, 1. Menomonee Falls, WI; 2. Milwaukee, WI.
Introduction: Autosomal dominant hyper IgE syndrome (HIES) is a com- Background: Drug reaction with eosinophilia and systemic symptoms
plex primary immunodeficiency disorder characterized by recurrent skin and (DRESS) is a rare, possibly life-threatening drug reaction typically consisting
sinopulmonary infections, eczematoid dermatitis, and elevated serum IgE lev- of recent exposure to a high-risk medication (initiation weeks to months prior
els. Disseminated infections by endemic dimorphic fungi have been reported to symptoms) accompanied by skin eruption, systemic symptoms (fever, lym-
to affect patients with HIES. However, invasive histoplasmosis rendering a cat- phadenopathy, hematologic abnormalities like eosinophilia) and end-organ
astrophic terminal ileum perforation has not been previously described. Case involvement. Failure to recognize this disease, especially with a history of expo-
Description: We present the case of a 21-year-old man with HIES who devel- sure to a high-risk medication, may lead to significant morbidity and mortal-
oped recurrent episodes of diffuse abdominal pain, low-grade fever, intermit- ity while removal of the offending agent can be lifesaving. Case: A 9 year-old
tent emesis and unintentional weight loss. CT of the abdomen and pelvis on African American male with a history of cerebral palsy, epilepsy, and GERD
admission revealed partial small bowel obstruction. Laboratory findings demon- presented with a diffuse erythematous rash along with fever, cough and pro-
strated significantly elevated urine histoplasma antigen (15.82 ng/mL) and pos- gressive dyspnea. His medications included phenobarbital and valproic acid
itive serum histoplasma antibody, implying a disseminated infection by H. cap- started two weeks prior to presentation with long-term use of omeprazole. Fam-
sulatum. He responded well to fluid resuscitation, GI decompression, and ily and social history were unremarkable. Initial physical exam was signifi-
intravenous liposomal amphotericin B which was later transitioned to oral cant for a diffuse maculopapular rash without mucosal involvement and coarse
itraconazole 200 mg twice a day after the acute episode resolved. While he breath sounds. His chest x-ray demonstrated patchy airspace opacities bilater-
was maintained on itraconazole over the following year, the level of urine histo- ally. He was admitted to the hospital with continuation of his home medica-
plasma antigen was assessed periodically. The level was trending down grad- tions and initiation of ampicillin for possible pneumonia. He clinically wors-
ually but still remained detectable, likely due to his noncompliance to the anti- ened. He required CPAP for respiratory support. He developed facial edema,
fungal therapy. The patient ultimately developed terminal ileum perforation eosinophilia (max AEC of 1560) and a transaminitis. His renal function
which was successfully treated with partial small bowel resection and primary remained normal. Differential diagnosis included drug reaction such as DRESS,
anastomosis. GMS staining of the resected small intestine revealed H. capsu- infection or hypereosinophilic syndrome. His phenobarbital and valproic acid
latum within histiocytes. He recovered well after the surgery and continued were discontinued four and six days later, respectively. He concomitantly
the antifungal therapy. Discussion: In HIES, STAT-3 mutations result in an aber- received high-dose corticosteroids. His clinical status and laboratory findings
rant TH17 cell response and impaired β-defensin production and neutrophil traf- returned to baseline with a slow corticosteroid taper over the next eight weeks.
ficking. These defects likely account for the susceptibility to invasive fungal Conclusion: A history of high-risk medication use as well as clinical manifes-
infections. Ileocecal histoplasmosis may clinically mimic inflammatory bowel tations of skin eruption with systemic symptoms and end-organ involvement
disease. Thus clinicians should be vigilant for the development of histoplam- should prompt the possible diagnosis of DRESS. The most effective treatment
osis in HIES patients. Timely diagnosis and adequate antifungal therapy are is to remove the offending agent along with supportive treatment. The use of
crucial in preventing severe complications. systemic corticosteroids is typically implored in patients with severe end-organ
involvement. Laboratory abnormalities should be monitored closely until nor-
VOLUME 113, NOVEMBER, 2014 A61
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A62
ABSTRACTS: POSTER SESSIONS
malized. Importantly, the allergist should be familiar with and serve as a knowl- cause and effect is not definitive, the patient had not previously responded to
edgeable resource for the diagnosis and treatment of DRESS. five days of aggressive conventional therapies. Review of the literature indi-
cates that this may be the first successful treatment of severe acute urticaria
with omalizumab. The cause of this patient’s outbreak remains unclear, but
P132 might be associated with chemicals used in the furniture, as indicated by other
CRYPTOCOCCUS MENINGITIS AS THE FIRST MANIFESTA- reports in the literature.
TION OF IDIOPATHIC CD4 LYMPHOCYTOPENIA.
J. Brooks*1, G. Ghaffari2, 1. Lititz, PA; 2. Hershey, PA.
Introduction: Idiopathic CD4 lymphocytopenia (ICL) is a rare disorder of
P134
A RARE CASE OF ACUTE COMPARTMENT SYNDROME SEC-
unknown etiology. Diagnostic criteria include a persistent CD4 T cell lym-
ONDARY TO INSECT BITE.
phopenia with no underlying primary or secondary immunodeficiencies, with
a CD4 T cell count < 300 cell/mL or a CD4 T cell count < 20% total lympho- F. Farri*1, T. Akande2, S. Baghian2, Y.K. Persaud2, 1. Ossining, NY; 2. Bronx,
cytes on multiple occasions. Case Report: 52 year old Caucasian female, with NY.
history of SLE controlled on plaquinil, presented with a 2 month history of Introduction: Acute compartment syndrome (ACS) is a surgical emergency,
headaches associated with confusion, dizziness, nausea/vomiting, and right eye mostly seen as a rare but severe complication of trauma; however there are non-
pain. Upon admission, an MRI revealed leptomeningeal enhancement. Cryp- traumatic causes. ACS secondary to insect bite is very rare; to our knowledge,
tococcus neoformans grew on CSF culture. Amphotericin B and flucytosine there is only one previously reported case of ACS due to a mosquito bite. Case
were initiated. An absolute CD4 count was 86 (normal (N): >500). HIV test- Report: A 21-month old female with past medical history of recurrent insect
ing with PCR, HSV, hepatitis panel, PPD, HTLV, and histoplasmosis and blas- bites presented with extensive swelling of the hand and forearm. She had a
tomycosis antigen tests were all negative. Immunology consult was obtained. small pruritic bump on dorsum of the left hand from a witnessed flying insect
B cell lymphocytes, NK cells, immunoglobulin levels, mitogen proliferation bite a few days prior. Subsequently, she developed decreased movement of the
studies, CH50 and C2 were normal. Antibody titers for diphtheria, tetanus, left wrist and tenderness with passive extension of the digits. There was no
and streptococcus pneumonia revealed protective levels. Based on the presen- improvement of the swelling with topical antibiotic ointment and oral antihis-
tation, lab findings, and no identifiable cause for low CD4 count, the patient tamine. X-rays of the wrist and forearm showed soft tissue swelling, but was
was diagnosed with ICL. She was discharged on amphotericin and flucytosine negative for fractures and or dislocations. A diagnosis of Acute Comparte-
and prophylactic treatment with trimethoprim/sulfamethoxazole was initiated. ment Syndrome was made and immediate surgical intervention was undertaken.
The patient was medication compliant and asymptomatic at her 2 week fol- Intra-operative findings showed maximally elevated pressures (45mmHg) in
low-up visit. The repeat labs revealed an absolute CD4 and CD8 count of 37 the adductor-pollicis compartment of the left upper limb. Surgical decom-
and 91 (N: >200), and a CD4/CD8 ratio of 0.41. Discussion: Patients with ICL pression of the affected area was performed with subsequent resolution of the
are usually identified when the CD4 count is less than 200 and complications pain and swelling. Diagnostic evaluation showed normal white blood cell counts
develop. Opportunistic infections are the most common initial manifestations. with differential, complement levels, total tryptase levels, total serum IgE, and
Patients also present with autoimmune conditions or malignancies. The inci- IgE to mosquito and house fly. Blood and wound cultures showed no growth
dence of asymptomatic patients with ICL is unknown. Currently, there are no during both episodes, she did however have significantly elevated serum his-
specific treatment guidelines. Therapies used to increase CD4 levels, IL-2, tamine levels Discussion: Most reaction’s to insect bites are non-allergic man-
interferon-gamma, and IL-7 or allogeneic hematopoietic stem cell transplan- ifestations of the venom’s toxic effect, and present as erythema, pain and
tation, have variable results. In children, immunoglobulin replacement is con- swelling. Insect bite hypersensitivity, may be mediated by immunologic mech-
sidered. Prophylactic treatments for opportunistic infections based on the CD4 anisms (IgE-mediated or non-IgE-mediated venom allergy) but also by non-
cell count should be considered. Conclusion: ICL is a diagnosis of exclusion immunologic mechanisms. An important question in the clinical management
when there is no identifiable underlying cause for a low CD4 count. A thor- of the patient was: did an infectious process (i.e. cellulitis) contribute to the ini-
ough immune system evaluation is necessary when contemplating this diag- tial clinical presentation of ACS? The absence of fever, the short duration from
nosis. time of bite to presentation, the absence of differential warmth, the normal
white cell count as well as negative blood and wound cultures made a bacter-
ial super-infection unlikely. The patient was placed on daily antihistamines and
P133 the parents were instructed to be vigilant in accessing immediate medical care
SUCCESSFUL TREATMENT OF ACUTE URTICARIA WITH during each subsequent reaction.
OMALIZUMAB.
K. Patel*, R. Ten-Boquera, K. Gundling, San Francisco, CA.
Introduction: Omalizumab is a monoclonal antibody that binds free IgE
and is used in treatment of allergic asthma and chronic idiopathic urticaria. We
report the first case of acute urticaria refractory to maximal conventional ther-
apy that responded to omalizumab therapy. Methods: A case report and review
of the literature. Data: A previously healthy 36 year old woman presented with
an acute episode of facial edema and full body hives 24 hours after receiving
new furniture in her home. She presented to the ED where she received epi-
nephrine, solumedrol, diphenhydramine and ranitidine; she was discharged
home after symptomatic improvement. The following day she had recurrent
symptoms; she was treated similarly as her prior episode with overall improve-
ment. She was discharged home on prednisone and loratadine. The next day
she again had similar symptoms and was admitted for management. During the
next 3 days of her admission, she received the following daily medications: 150
to 200 mg of diphenhydramine, 60mg prednisone, 150mg ranitidine, 25 to 50
mg hydroxyzine, 10 to 40 mg cetirizine, and 10 to 20 mg of montelukast. Despite
this maximal therapy, she continued to have full body urticaria with facial and
pedal edema. A skin biopsy confirmed acute urticaria. Due to ongoing severe
symptoms, she was given omalizumab (300mg), and within 24 hours had rapid
resolution of disease. A large panel of laboratory studies was negative, except
for elevated levels of plasma histamine (3.6 ng/mL) and total tryptase (12
ng/mL), supporting mast cell mediator release. To further evaluate the furni-
ture as a possible cause, fabric was ground with sterile water; the skin prick
test was negative. Patch testing was also negative. Her medications were tapered
over a month, and she continued to be symptom free at her 3 month follow up
off of all medications. Conclusion: A trial of omalizumab for severe, refrac-
tory acute urticaria was associated with rapid resolution of disease. Although
A62 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A63
ABSTRACTS: POSTER SESSIONS
P135 P137
A YOUNG IMMUNOCOMPETENT FEMALE WITH ASTHMA MASTOCYTIC ENTEROCOLITIS: CHRONIC INTRACTABLE
AND ALLERGIC RHINITIS FOUND TO HAVE RARE FUNGAL DIARRHEA, ABDOMINAL PAIN, WITH INCREASED MUCOSAL
RHINOSINUSITIS WITH SKULL EROSION, SCHIZOPHYLLUM MAST CELLS.
RADIATUM. A.C. Netterville*, A. Ochoa, New Orleans, LA.
R. Gupta*1, M. Segal2, 1. Vernon Hills, IL; 2. Philadelphia, PA. Introduction: Mastocytic enterocolitis is a proposed term for cases of diar-
Rationale: Fungal sinusitis is generally limited to immunocompromised rhea-predominant irritable bowel syndrome (IBS) with elevated numbers of
hosts including those with hematological malignancies, diabetes, and chronic mucosal mast cells. GI mast cells excess is defined as the presence of greater
steroid use. The most responsible culprits include Aspergillus, Fusarium, Muco- than 20 mast cells per high-power field of microscopy in the GI tract mucosa.
rales, and dermatiaceous molds. Here we present a young female found to have Presentation is chronic intractable diarrhea, often associated with abdominal
a rare fungal species causing maxillary sinusitis requiring long term fungal pain with unremarkable colonic or duodenal biopsy specimens on routine hema-
treatment. Methods: Computed Tomography of Sinuses, Magnetic Resonance toxylin-eosin staining, but increased numbers of mast cells on immunohisto-
Imaging of Head, and sinus biopsies with gram stain and culture. Results: Our chemistry for mast cell tryptase. Case Description: This is a 6 year old male
patient has a longstanding history of allergic rhinitis and asthma with 3-4 hos- who initially presented at 23 months with chronic diarrhea and abdominal pain.
pital visits a year never requiring intubation. She presented with complaints He was evaluated by GI with an upper and lower endoscopy, and was found on
of severe sinus symptoms and subsequently had a CT scan demonstrating immunohistochemical stains for CD117 to have greater than 20 mast cells per
sinusitis with bony erosion at the base of the skull. Endoscopic surgery and high power field. Elevated numbers were found throughout the colon and rec-
maxillary sinus biopsies revealed fungal species of Schizophyllum radiatum. tum. He had extensive additional evaluation which revealed normal total
Itraconazole treatment was started with frequent monitoring of QT-interval immunoglobulins, IgG subclasses, tryptase, C1 esterase inhibitor level and
and drug levels, with microbiology confirming adequate susceptibility of treat- function, and complete blood count. He also had negative immunocaps to all
ment. Clinically her sinusitis continued to improve. She remained on Itra- foods and inhalant allergens tested. He was initially treated with hydroxyzine
conazole for 6 months, with total resolution of symptoms. Conclusion: We and singulair with little improvement. He was later started on gastrocrom four
believe this patient’s case demonstrates two facets of rarity. One, our patient times a day, and at that time demonstrated significant improvement, with near
does not fit the typical demographic of those who acquire fungal sinusitis. resolution of his symptoms of diarrhea and abdominal pain. Upon evaluation
Second, Schizophyllum radiatum is an unfamiliar species to cause infection by us we recommended adding an H2 receptor antagonist. Conclusion: Mast
and bony destruction. This case provides insight into evaluation of patients cells play an important role in the regulation of GI visceral sensitivity and vas-
deemed minimal risk for fungal sinusitis and the rare although morbid com- cular permeability. Increased numbers of GI mucosal mast cells has been doc-
plications of fungal sinusitis. umented in several studies in patients with irritable bowel syndrome, masto-
cytic enterocolitis, systemic mastocytosis, mast cell activation syndrome, and
allergic mastocytic gastroenteritis and colitis. Patients with chronic unexplained
P136 diarrhea should undergo colonoscopic biopsies with special mast-cell stains.
TREATMENT OF GRANULOMATOUS-LYMPHOCYTIC INTER- If elevated mast cells are demonstrated on biopsies patients should be treated
STITIAL LUNG DISEASE (GLILD) IN CVID WITH RITUXIMAB with H1 and H2 receptor antagonist and also a mast cell stabilizing agent. In
AND MYCOPHENOLATE. more severe cases it has been proposed to add an antileukotriene or a 5-lipoxy-
genase inhibitor.
J.M. Lomas*, M. Mortezavi, R.J. Looney, Rochester, NY.
Introduction: Granulomatous-lymphocytic interstitial lung disease (GLILD)
is a non-infectious pulmonary complication of common variable immune defi-
ciency (CVID) that can have a profound impact on the quality of life and sur-
P138
COW’S MILK PROTEIN ALLERGY PRESENTING WITH
vival of affected patients. Combination chemotherapy with rituximab and aza- HYPEREOSINOPHILIA AND ELEVATED BRAIN NATRIURETIC
thioprine has been previously shown to improve pulmonary function and
PEPTIDE.
imaging in this subgroup ofthese patients. We describe a case of CVID with
GLILD treated with rituximab and oral mycophenolate mofetil that had a sim- C. Parrish*, A.K. Wong, S. Thobani, M. Li, L. Scott, Los Angeles, CA.
ilar positive outcome. Case Description: A 37 year-old female with history of Introduction: Cow’s milk protein allergy is common in infancy. About half
idiopathic thrombocytopenic purpura (ITP), initially presented to our clinic for of all cases are non-IgE-mediated, and allergic proctocolitis with bloody stools
evaluation of a chronic cough and shortness of breath. Pulmonary function test- is considered the most benign form. Methods: Case Report. Results: A 4-month-
ing showed a restrictive pattern, without evidence of obstruction or reversibil- old Hispanic female presented with complex febrile seizure and was inciden-
ity. Laboratory results were remarkable for profound hypogammaglobulinemia tally noted to have grossly bloody stools. After a full-term delivery, she had
(IgG 75, IgA < 5, IgM 13) with normal numbers of T and B cells on flow cytom- been treated with prophylactic antibiotics due to maternal chorioamnionitis.
etry. Computed tomography (CT) of the chest showed extensive interstitial dis- During the NICU stay she was breastfed with cow’s milk formula supplemen-
ease, including innumerable bilateral pulmonary nodules, as well as multiple tation, and had intermittent heme-positive stools. Grossly bloody stools first
enlarged mediastinal lymph nodes and splenomegaly. She was started on occurred at 1 month of age, after which the mother eliminated cow’s milk for-
monthly intravenous immunoglobulin (IVIG) therapy and underwent wedge mula and began to exclusively breastfeed. Over the subsequent months, the
biopsy of the lung for diagnostic purposes. Pathology reported follicular bron- patient had multiple episodes of grossly bloody stools after maternal dairy
chiolitis, lymphocytic interstitial pneumonia, and non-necrotizing granuloma- ingestion, but was otherwise thriving. Serum IgE to milk protein was negative.
tous inflammation as well as areas with fibrin deposition and organizing pneu- Review of laboratory studies showed peripheral eosinophilia (1.9k/mm3) 4 days
monia. She was treated with 2 doses of rituximab (2g) two weeks apart and after birth and at time of presentation (3.3k/ mm3). Stool examination for ova
1000mg of oral mycophenolate mofetil twice daily. The therapy was well tol- and parasites as well as serum testing for Strongyloides and Toxocara were neg-
erated. Six months following initiation of therapy, repeat imaging showed near ative. Given severe eosinophilia over a 4-month period beginning shortly after
resolution of pulmonary nodules with significant improvement in mediastinal birth, screening was done for target organ damage. Urinalysis and liver tests
lymphadenopathy and ground-glass opacities. Pulmonary function had returned were normal, but Brain Natriuretic Peptide (BNP) was elevated at 626 pg/mL,
to normal and the patient’s cough and shortness of breath had resolved. Con- (no cardiac symptoms and echocardiogram normal). All dairy products were
clusions: Multiple authors have previously documented that monotherapy for eliminated from the maternal diet, with subsequent resolution of eosinophilia
treatment of GLILD in CVID is not effective. Combination chemotherapy using (absolute eosinophils 100/ mm3) and significant decrease in BNP (211 pg/mL).
rituximab and azathioprine has previously been shown to be effective. This is Conclusions: Milk protein allergy presenting with bloody stools is common
the first case describing case describing successful treatment of GLILD with and generally considered benign. The diagnosis is based upon clinical presen-
a combination of rituximab and mycophenolate mofetil. tation and resolution of symptoms upon withdrawal of the presumed food anti-
gen, and therefore labs are not routinely checked. However, this case illus-
trates that even intermittent exposure to cow’s milk protein over several months
may lead to persistent eosinophilia, which in other conditions has been shown
to cause target organ damage. Elevated BNP levels have not previously been
reported in hypereosinophilia. This case suggests that BNP may be a sensitive
VOLUME 113, NOVEMBER, 2014 A63
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A64
ABSTRACTS: POSTER SESSIONS
early marker for eosinophilic myocardial insult, although further studies would glycine and have similar osmolarity and content. Gamunex uses bromobutyl
be needed to support this hypothesis. rubber stoppers in their vials while Gammagard liquid utilizes halobutyl or
chlorobutyl rubber stoppers. Currently no comparative data exist describing
the side effect profile in terms of appearance of dyshidrotic eczema among dif-
P139 ferent IVIG formulations.
RASH ASSOCIATED WITH ANGIOIMMUNOBLASTIC T-CELL
LYMPHOMA MISTAKEN FOR DRESS.
A.K. Wong*, C. Parrish, S. Thobani, M. Li, L. Scott, Los Angeles, CA. P141
LöFFLER SYNDROME IN AN EIGHT-YEAR-OLD PIG FARMER.
Introduction: Angioimmunoblastic T-cell Lymphoma (AITL) is a periph-
eral T-cell lymphoma which presents with non-specific systemic illness includ- H. Shah*1, K. Gipson2, L. Wall2, 1. Yorba Linda, CA; 2. New Orleans, LA.
ing lymphadenopathy, hepatosplenomegaly, B-symptoms, rash, and/or ane- Löffler syndrome is a hypersensitivity response to parasite larval migration
mia. Rash is present in 20-60% of patients, and they are usually pruritic with through the lungs, and is rare in the modern United States. It is classically attrib-
lymphohistiocytic vasculitis seen on biopsy. Methods: Case Report Results: A uted to Ascariasis, but can occur with other parasites. A previously healthy 8-
64 year-old Hispanic male with no prior medical history presented to an out- year-old male was hospitalized with tachypnea, cough, and fever of one week’s
side clinic with a 2-week history of generalized, erythematous, papular, non- duration. History revealed exposure to pigs on his family’s farm in southern-
blanching, pruritic rash over his trunk and extremities. After a 5-day steroid most Louisiana, no travel, no asthma or atopy, and normal review of systems.
burst, the rash did not improve. 2 weeks later, he presented for evaluation. He He was hypoxemic and imaging revealed diffuse reticulonodular lung opaci-
was noted to have lymphadenopathy. Lymph node and bone marrow biopsies ties. He demonstrated leukocytosis, peripheral eosinophilia (39%), and high
yielded a diagnosis of AITL. He received 1 round of chemotherapy with com- serum IgE (3,480 IU/mL). Given his acute respiratory failure, systemic corti-
plete resolution of his rash. He was well for 2 weeks until he presented to the costeroids were initiated. He was treated empirically for atypical pneumonia
emergency room with fever of 101.3°F and neutropenia of 700/mm3. Cefepime while undergoing diagnostic evaluation. Despite increasing serum IgE levels
and vancomycin were started on admission, and 2 days later he developed gen- (peaking at 12,700 IU/mL), he demonstrated rapid clinical improvement and
eralized facial swelling with a maculopapular erythematous rash over his trunk was weaned off of supplemental oxygen. Pulmonary function testing demon-
and extremities. The patient developed a fever of 101.8°F around the time of strated a mixed obstructive and restrictive pattern. Broncho-alveolar lavage
rash onset, and on physical exam, he was noted to have axillary and inguinal fluid showed profound pulmonary eosinophilia (86%). Subsequent evaluation
lymphadenopathy. Review of laboratory studies showed peripheral eosinophilia of his eosinophilia revealed highly elevated serology to both Ascaris and Tox-
which increased from 0/mm3 on admission to 1100/mm3 on hospital day 7. ocara, which was treated with albendazole. Strongyloides serology was nega-
Allergy and Immunology was consulted to evaluate for drug reaction with tive, as was an extensive evaluation for other infectious and allergic etiologies.
eosinophilia and systemic symptoms (DRESS). Conclusions: Allergists/Immu- This case demonstrates that Löffler syndrome may be severe, yet elusive. It
nologists are commonly consulted for rashes, especially in relation to drug hyper- may present with pulmonary involvement and fever without the involvement
sensitivities. While DRESS is a potentially life-threatening adverse reaction to of other organs expected from larval migration, requiring a high degree of sus-
medications, the onset of DRESS is typically 2-8 weeks after initial exposure picion to make the diagnosis. One should consider it even in the absence of
to the offending medication. The time course of this patient’s rash was not con- travel history, especially in endemic areas for Ascaris such as southeastern
sistent with DRESS. This case illustrates the importance of maintaining a broad United States. Strikingly elevated eosinophils in the lung washings should
differential diagnosis including infection or malignancy in the evaluation of a prompt evaluation for parasites. Other aspects unique to our patient include liv-
patient with rash of unknown origin. Generalized non-specific rash is a com- ing in close association with pigs and being seropositive to both Ascaris and
mon presenting feature of AITL, and in this particular patient, his DRESS-like Toxocara. Moreover, Ascaris suum is known to infect pigs and has rarely been
symptoms of fever, lymphadenopathy, and eosinophilia and systemic symptoms reported with visceral larva migrans in humans. Systemic corticosteroids were
were explained by his underlying malignancy. His rash and DRESS-like symp- effective in treating the patient’s respiratory compromise, despite concern for
toms improved after starting his second round of chemotherapy. dissemination of the parasite when host immunity is suppressed.
P140 P142
DYSHIDROTIC ECZEMA INDUCED BY GAMUNEX INTRA- AN ATYPICAL PRESENTATION OF GIANT CELL ARTERITIS.
VENOUS IMMUNOGLOBULIN THAT RESOLVED WITH GAM- J.R. Zaragoza*, N. Vernon, G. Ghaffari, Hershey, PA.
MAGARD IN A PATIENT WITH MYASTHENIA GRAVIS. Giant cell arteritis (GCA) is a chronic vasculitis of large and medium cal-
M. Shtessel*, D. Ferastraoaru, J. Graber, G. Hudes, Bronx, NY. iber blood vessels, mostly affecting individuals in the fifth decade of their life.
Rationale: Dyshidrotic eczema is a known rare side effect of intravenous It is caused by arterial wall inflammation that leads to the clinical manifesta-
immunoglobulin (IVIG) therapy in patients who are most commonly treated tions of vasculitis and tissue ischemia such as jaw claudication, temporal
for neurologic diseases. Its pathophysiology is not clear. Eczematous eruption headache and visual loss. Although it may be generalized, vessel inflamma-
has never been reported in patients treated with IVIG for immunodeficiency tion most prominently involves the cranial branches of the arteries originating
states, highlighting the role of high doses of IVIG in this peculiar side effect. from the aortic arch. We present an uncommon manifestation of GCA in a
The skin changes usually respond well to topical steroids and some patients patient with tongue swelling. Case Report: A previously healthy 68-year-old
may improve with continuation of the IVIG. Methods: Review of the literature female was presenting submandibular swelling a month prior to evaluation. She
and case report of a patient in which the use of Gamunex resulted in appro- was treated with antibiotics and intermittent doses of steroids for suspected
priate myasthenia gravis control but intolerable dyshidrotic eczema, which sialadenitis. Despite therapy, the patient presented increased swelling of the
resolved when the formulation was switched to the Gammagard liquid form. tongue and pain with minimal headache, but had no blurred vision or jaw clau-
Results: 37 year-old female with history of myasthenia gravis was started on dication. She was admitted to the hospital where a lingual biopsy revealed no
Gamunex 2g/kg over 3 days, every six weeks. After the first infusion she devel- amyloidosis or malignancies. Upon further testing, hereditary angioedema
oped dryness and scaling lesions over hands, scalp and chest which were diag- screening was negative but she still had elevated C-reactive Peptide (1.3 mg/dL).
nosed as dyshidrotic eczema. Patient did not have a history of eczema prior to A trial of icatibant was administered for suspected bradykinin-induced
receiving Gamunex. She was started on topical corticosteroids without much angioedema. With no improvement of the symptoms, the patient was trans-
improvement in her skin lesions. Patch testing with common contact allergens ferred to our institution for further evaluation. A biopsy of the temporal arter-
and Gamunex was negative at 48 and 96 hours. Drug reaction was suspected ies revealed GCA and treatment was initiated with high-dose corticosteroids.
and the patient’s formulation of IVIG was switched from Gamunex to Gam- Unfortunately, the necrosis of the tongue led to its eventual self-amputation.
magard 2g/kg over 3 days every 6 weeks. The skin changes remitted with the Conclusion: Lingual swelling and necrosis are extremely rare complications
new product, but she developed 2 flairs of myasthenia gravis. The decision in GCA. That atypical presentation may mimic an angioedema episode when
was made to switch back to Gamunex. Unfortunately, the patient’s eczema reoc- classic symptoms of GCA are subtle. This case reinforces the importance of
curred but her treatment with Gamunex was continued for optimum myasthe- suspecting GCA upon evaluating elderly individuals that present lingual swelling
nia gravis control. Conclusions: This is the first reported case of dyshidrotic as to avoid a delay in diagnosis and treatment. We conducted a literature search
eczema in a patient receiving Gamunex IVIG that did not improve with topi- review using Ovid. A search using the keywords “Giant Cell Arteritis and tongue
cal steroids but resolved after switching to an alternative formulation. It is necrosis” resulted in 43 published cases dating back to 1967. All cases were
unclear why the eczema improved with Gammagard. Both formulations use almost identical in clinical presentation to our case with the exception of some
A64 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A65
ABSTRACTS: POSTER SESSIONS
subtle differences. Six of the published GCA and lingual necrosis cases were bronchiectasis causes worsening inflammation, airway obstruction, morbidity
triggered by ergotamine use. Also, the severity and extent of necrosis varied and mortality. Methods: We review a case of an adolescent female who pre-
among cases, ranging from unilateral partial lingual necrosis to extensive necro- sented with uncontrolled asthma and seasonal allergies to the Allergy/Immunol-
sis of the tongue, scalp or bilateral vision loss. ogy Division. Results: A 17 year old female presented with “uncontrolled
asthma” and seasonal allergies. She had transient tachypnea of the newborn
and RSV bronchiolitis at 2 months of age. At 1 year of age, she had her first
episode of pneumonia. She then had pneumonia about once a year, requiring
antibiotics. She had required high dose inhaled steroids and frequent oral steroid
courses for asthma. She reported wheezing when recumbent and a feeling of
fullness in her left lung with inability to sleep on her left side. Her examina-
tion was significant for crackles and inspiratory wheeze with dullness to per-
cussion at the left lung base. Spirometry demonstrated reversible airway obstruc-
tion. Skin prick tests were positive to pollens. Sweat test was negative and
immunologic evaluation demonstrated increase in antibody levels to pneumo-
coccus following booster vaccination. Chest CT scan showed bronchiectasis
in the left lower lobe. Bronchoscopy demonstrated narrowing of the orifice of
the left lower lobe due to collapsibility of the posterior wall of the bronchus
and thick, white secretions within the left lower lobe. Biopsy of the bronchus
demonstrated chronic inflammation with ciliary disorientation. She was diag-
nosed with impaired mucociliary clearance and retained secretions due to left
lower lobe bronchomalacia. She started an airway clearance regimen with sig-
nificant clinical improvement and capacity to wean asthma therapy. Conclu-
sion: In an asthmatic with wheezing, chronic cough, sputum production and
focal findings on examination, bronchiectasis should be considered. Missed
diagnosis, can create undue burden of disease and significant sequelae from
excess asthma therapy.
P143
ADULT FEMALE WITH SERUM SICKNESS SECONDARY TO
MUPIROCIN.
A. Asawa*1, R. Bonds2, 1. Sugar Land, TX; 2. Galveston, TX.
Introduction: Serum sickness is a type III hypersensitivity reaction caused
by antigen-antibody complexes and presents with fever, urticaria, poly-arthral-
gia/poly-arthritis, and/or acute glomerulonephritis. In this type of reaction an
antigen binds to antigen specific IgG forming immune complexes. These then
bind to IgG receptors on inflammatory cells and activate complement causing
an inflammatory reaction. Methods: We report the case of a 44 year old female
referred to Allergy/Immunology clinic for hives and arthralgias. Patient first
noted symptoms 4 years ago after she was treated with trimethoprim-sul-
famethoxazole and mupirocin for cellulitis of her right foot. Two weeks later
she noted diffuse erythematous, well defined, burning, circular skin lesions that
blanched. She also had swelling and increased warmth in both knees and arthral-
gias in her knees, neck, elbows, and hands. Numerous antihistamines were tried,
but not helpful. The symptoms gradually resolved in a few months. She was
asymptomatic for four years. In April 2014 she treated blisters at the base of
her right foot with mupirocin. One day later she noted a return of her diffuse
urticaria, arthralgias, and fever. She was treated with a corticosteroid injection
which did not alleviate her symptoms. Subsequently, she was started on
cyclosporine which has provided her with moderate relief of symptoms. Dis-
cussion: The patient’s history of repeat episodes of arthralgias, fever, urticar-
ial rash triggered by a medication raises concern for serum sickness versus drug
induced lupus. Laboratory evaluation revealed normal levels of C3 (123 mg/dl;
reference range 86-184 mg/dl) and C4 (26.5 mg/dl reference range 20.0-59.0 Chest CT: Airway dilatation in the left lower lobe
mg/dl), elevated C1Q binding (4.7 ugE/mL; reference range 0.0 –3.9 ugE/mL),
and ESR (45 mm/hr; reference rage 0-20 mm/hr) suggesting evidence of cir-
culating immune complexes supporting the diagnosis of serum sickness over P145
drug induced lupus. In our literature search, we did not identify any previous UNUSUAL CASE OF ACQUIRED ANGIOEDEMA PRESENTING
reports of mupirocin causing serum sickness. Conclusion: We report a 44 year INITIALLY AS HEREDITARY ANGIOEDEMA.
old female old presenting with elevated C1Q binding and ESR along with recur-
rent fevers, arthralgias, and urticarial rash most likely secondary to serum sick- M. Joseph*, Saginaw, MI.
ness induced by mupirocin. 51 year-old female suffered from recurrent lip, tongue and laryngeal
angioedema for almost 2 years and she required two tracheostomies. Her daugh-
ter had a history of lip swelling. Laboratory reports: C4 undetectable, C1 esterase
P144 low, C1 esterase function was 40% and C1q normal. She was diagnosed with
WHEN WHEEZE IS MORE THAN ASTHMA: A CASE REPORT. HAE. Danazol was started. Because of persistent cramping abdominal pain,
and because she was going to start danazol, a CT of the abdomen was obtained;
M. Gupta*, S.P. DaVeiga, Philadelphia, PA.
it showed mild splenomegaly. She was then evaluated by the oncologist who
Introduction: Bronchiectasis can occur in children due to cystic fibrosis, entertained the possibility of hereditary versus acquired angioedema (AAE).
primary ciliary dyskinesia, infections, immunodeficiency, and anatomic eti- A bone marrow biopsy revealed the presence of a small CD5 negative, CD10
ologies. Primary symptoms include productive cough, chest pain, dyspnea, and negative, CD19 & CD 20 positive Lambda restricted B-cell population. The
fatigue. High-resolution computed tomography (HRCT) is the diagnostic imag- pathologist felt that the presence of a small abnormal monoclonal B-cell pop-
ing modality of choice. Management involves treatment of the underlying dis- ulation was suspicious but not definitive for the diagnosis of lymphomatous
ease process, mucociliary clearance, and treatment of infections. Untreated, involvement of the bone marrow. Given the non-definitive bone marrow diag-
VOLUME 113, NOVEMBER, 2014 A65
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A66
ABSTRACTS: POSTER SESSIONS
nosis, the oncologist and the patient decided to observe with close follow up.
Despite danazol, she suffered from continued life threatening attacks of
angioedema. Two months later, C1 Esterase Inhibitor (Cinryze) infusion ther-
apy was started in an attempt to prevent episodes of angioedema. By this time,
her spleen was found be palpably enlarged. Repeat complement studies showed
C1q to be low, in contrast to a normal C1q previously. After 2 months of Cin-
ryze therapy, the patient underwent a splenectomy for Non-Hodgkin’s lym-
phoma. During the period she received Cinryze, she did not have angioedema.
One month post splenectomy, Cinryze was stopped. She continued to be free
from episodes of angioedema. Four months later, C4 and C1q remained
depressed, but C1INH function recovered nicely. This patient had an initial
diagnosis of HAE. Later, the low C1q and palpably enlarged spleen prompted
a diagnosis of AAE secondary to non-Hodgkin’s lymphoma. This was an unusual
presentation with an initially normal C1q in this patient with AAE. Cinryze
therapy is not approved for use in acquired angioedema but was necessary in
this patient with life threatening episodes. Cinryze therapy prevented further
episodes of life-threatening angioedema until definitive therapy with a splenec-
tomy was performed. Our patient has been completely free of angioedema for
more than one year after splenectomy and discontinuation of cinryze therapy.
Figure 1: Persistent lip swelling.
P146 P147
OROFACIAL GRANULOMATOSIS IN A PATIENT WITH HERED-
ITARY ANGIOEDEMA. TREATMENT OF POST-TRANSPLANT ACUTE REJECTION
WITH SUBCUTANEOUS IMMUNOGLOBULIN REPLACEMENT.
S.P. Brady*1, H.J. Wedner2, 1. Clayton, MO; 2. St. Louis, MO.
Z. Pirani, MD*, J. Shih, MD, Atlanta, GA.
Introduction: Orofacial granulomatosis (OFG) is a rare, disfiguring illness
of unknown etiology characterized by the development of non-caseating gran- Introduction: Acute antibody mediated rejection (AMR) is characterized
ulomas in the oral and maxillofacial area. OFG can manifest as Melkersson- by graft dysfunction manifesting over months or years. It is a result of donor
Rosenthal syndrome, which is a triad of persistent lip or facial swelling, recur- specific antibodies that usually develop de novo after transplantation. A diag-
rent facial paralysis and fissured tongue, or as cheilitis granulomatosa of nosis of AMR typically indicates an increased incidence of allograft dysfunc-
Miescher, which primarily affects the lips. Although OFG can be associated with tion and mortality. IVIG has been cited in previous studies as being used suc-
systemic diseases such as tuberculosis, Crohn’s disease and sarcoidosis, it has cessfully to treat AMR in cardiac transplant patients. However, there are
not been reported with hereditary angioedema (HAE). Case: A 43-year-old currently no studies that investigate the use of SCIG in the management of acute
woman presented with complaints of recurrent swelling of the face, lips, uvula, AMR, which has shown in this case to be a promising treatment. Case Descrip-
neck, tongue and limbs. The episodes occurred twice weekly and resolved over tion: Patient is a 68 year old female who is currently being treated for hypogam-
2-4 days. High-dose antihistamines were not beneficial. Laboratory work-up maglobulinemia (HGG) and acute rejection s/p cardiac transplant in 2008. Mul-
revealed normal C4 level and normal C1 inhibitor level and function. She was tiple biopsies of the endomyocardium post-transplant from 2008-2009 showed
diagnosed with HAE with normal C1 inhibitor level and successfully treated evidence of Grade 1A and 1B rejection. In 2010, the patient was found to have
with C1 inhibitor concentrate, ecallantide and icatibant. However, six months multiple grade 3A rejections, and received 3 days of IV Solu-Medrol and 7-
after her initial presentation, the episodic lip swelling progressed to persistent days of Thymoglobulin for presumed T-cell mediated acute rejection. She was
lip swelling despite resolution of other symptoms. Physical exam revealed dif- subsequently admitted for photopharesis for 2 days and plasmapheresis with
fusely edematous upper and lower lips with mild overlying maceration. A lip concomitant IVIG for 3 days the following month. In March 2013, the patient
biopsy demonstrated diffuse, submucosal infiltrate of lymphocytes, histiocytes, was admitted for another episode of 3A rejection, at which time she was also
and multinucleated giant cells forming non-caseating granulomas, as well as found to have low Ig levels: IgG 326, IgA 119, IgM 41, and IgE 1.9 with
negative Congo red stain, Periodic Acid-Schiff stain, and Fite stain. These find- increased BUN/Cr. Patient was given IVIG, 1 gm/kg x 2 days. Subsequent
ings were consistent with cheilitis granulomatosa. Oral and intravenous corti- biopsy revealed grade 1B rejection, and the patient had much improvement in
costeroids led to only mild temporary improvement, while dietary modifica- her IgG levels. Patient was continued on monthly subcutaneous immunoglob-
tion and topical corticosteroids were ineffective. The patient is scheduled to ulins (SCIG) at 500 mg/kg for treatment of acute antibody mediated rejection
undergo intralesional corticosteroid injections. If these are unsuccessful, the and HGG. She continued to maintain IgG levels within normal range in spite
next management consideration would be topical and/or systemic immunosup- of end stage renal disease. Her subsequent pathology specimen reports, with
pressants. Conclusion: Orofacial granulomatosis is rare illness that can signif- the most recent from 4/2014, show grade 1B rejection, which is much improved
icantly affect patients’ quality of life. Our case describes a unique presentation from previous 3A rejections. Discussion: This case illustrates the potential ben-
of OFG in the setting of HAE. Delay in recognition and diagnosis can result in efit of using SCIG as part of the management for recurrent AMR. Early insti-
permanent disfigurement and impairment in eating and drinking. Therefore, it tution of this form of treatment could reduce the incidence of AMR, and there-
is imperative for clinicians to consider OFG in their differential diagnosis for fore, prevent its complications including allograft dysfunction and mortality.
orofacial edema, and recognize that it can develop in the setting of HAE. Research on this topic is warranted.
P148
ATYPICAL CASE OF KABUKI SYNDROME WITH INDETER-
MINATE IMMUNODEFICIENCY, LOW B CELLS AND AUTOIM-
MUNE ENTEROPATHY.
M. Gogna*, Glenshaw, PA.
Kabuki syndrome (KS) is a multiple malformation/mental retardation syn-
drome with an estimated frequency of 1/32,000 that is characterized by dis-
tinctive facial features, skeletal anomalies, short stature, and mental retarda-
tion. Increased infections especially otitis media, URIs, and Pneumonia have
been identified in 60-70%patients. It is unclear if these infections are due to
Immune problems (Hypogammaglobulinemia is a frequent finding in Kabuki
syndrome) or craniofacial abnormalities. We present the case of a 15 year old
female with Kabuki syndrome who presented with persistently low B cells
and Autoimmune enteropathy. Both these findings have previously not been
reported in KS. Her Immunoglobulins have been trending down since last 5
A66 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A67
ABSTRACTS: POSTER SESSIONS
years (table 1) Our patient gets mostly line infections with MSSA, CONS, Ecoli
and Klebsiella and not sinopulmonary infections. This can possibly be explained
P150
WEST NILE VIRUS ENCEPHALITIS IN GATA2 DEFICIENCY:
by a disruption in skin barrier and disruption in GI barrier(h/o chronic diar-
rhea). Her Memory B cells and Mitogen assays were wnl which is very reas- CLINICAL IMPROVEMENT AFTER IVIG AND INTERFERON
suring. She had significantly low B cells over the course of atleast 5years. ALFA-2B THERAPY.
Low B cells cannot be explained by chronic diarrhea or use of Tacrolimus ( J.S. Rosa*1, S. Kappagoda1, A. Hsu2, S. Holland2, A.Y. Liu1, 1. Stanford,
started on Tacrolimus for Autoimmune-enteropathy). She was diagnosed with CA; 2. Bethesda, MD.
Autoimmune enteropathy based on the following 1.Inflammation and increased Introduction: A twenty-four-year-old male was admitted to the ICU with
intraepithelial lymphocytes and numerous apoptoses on biopsy and 2.positive deteriorating mental status and cogwheel movements. Two healthy individuals
anti-enterocyte antibody and 3. anal fissures on exam. who accompanied the patient on a recent trip to Wyoming had spontaneous res-
olution of similar prodromal symptoms after exposure to mosquito bites. He
TREND OF IMMUNOGLOBULINS AND LYMPHOCYTE SUBSETS was subsequently found to have neuroinvasive West Nile virus infection with
OVER 5YEARS positive IgM antibodies in his CSF and serum, and detectable serum RNA. The
patient had a history of recurrent sinopulmonary infections, chronic warts,
and leukopenia with monocytopenia. His father and grandfather died before
50 years of age due to viral illnesses. There was no known family history of
leukemia or nontuberculous mycobacterial infections. Methods: Peripheral
blood was analyzed by flow cytometry. NK cell function was measured by the
release of radioactive chromium from lysis of the erythroleukemia cell line,
Recommendations: We recommend that a basic Immunological work up K562. DNA amplification of all exons, flanking splice sites, and intronic non-
–quantitative Immunoglobulins, Specific antibody titers be done in all coding regulatory regions of GATA2 was performed on whole blood. The patient
patients with KS. If the Initial work up is abnormal, we recommend further received 1.2 g/kg IVIG divided over 3 days and 3 million units of subcutaneous
work up including Lymphocyte subsets, Mitogen assays and B CELL panel. interferon alfa-2b daily for 14 days. Results: Monocytes (0), B lymphocytes
An index of suspicion should be kept for Autoimmune enteropathy leading to (8), CD4+ and CD8+ T lymphocytes (161 and 68), and NK cells (13) (/mL)
Chronic Diarrhea. were low. Absolute CD16+56+ and CD56bright NK cell counts were markedly
reduced, with relative frequency within normal limits. NK cell function was
normal. Genomic sequencing revealed a heterozygous single base deletion,
P149 c.1021delG; p.A341Pfs, causing the loss of the highly conserved second zinc
A CASE OF HASHIMOTO’S ENCEPHALOPATHY TREATED finger of GATA2. DNA sequencing for the same mutation in his mother was
WITH IMMUNOMODULATION AND THYROIDECTOMY WITH negative. The patient had a significant improvement in his neurologic function
INCIDENTAL FINDING OF THYROID CANCER. and most of his warts subsided after IVIG and interferon alfa-2b. He was referred
to our Hematopoietic Stem Cell Transplantation Program for bone marrow aspi-
J.A. Quirt*1, O. Perlov2, D.A. Haaland1, 1. Hamilton, ON, Canada; ration/biopsy and evaluation for bone marrow transplantation. Conclusions:
2. Barrie, ON, Canada. This is the first report of a patient with GATA2 deficiency presenting with West
Background: Hashimoto’s encephalopathy is a rare and likely under rec- Nile virus encephalitis. Patients with heterozygous GATA2 mutations may be
ognized immune-mediated neurologic syndrome. While the exact pathophys- more susceptible to neuroinvasive disease from West Nile virus infection, even
iology remains unclear, the encephalopathy itself appears to be independent of in the absence of a nontuberculous mycobacterial infection or familial history
the biochemical thyroid status. Due to the rarity of the syndrome, minimal evi- of leukemia. IVIG and interferon alfa-2b may have been beneficial for this
dence is available to guide treatment decisions. The mainstay of treatment is patient with impaired viral immunity.
corticosteroids, with some patients requiring other immunosuppressive agents.
Cases of success with use of IVIG have been published. Few case reports exist
in the literature of successful treatment involving thyroidectomy, with the P151
rational of removing the thyroid as an antigenic stimulus. Case Presentation: EPOETIN ALFA HYPERSENSITIVITY REACTION AND SUC-
We report a case of a 39 year old man who initially presented with a goiter and CESSFUL DESENSITIZATION IN A CHILD.
non-specific symptoms of dizziness, palpitations and general malaise. He was
found to be hypothyroid and started on replacement therapy. He subsequently J.S. Rosa*, A.Y. Liu, Stanford, CA.
developed ataxia, thought to be cerebellar in nature with head titubation, gait Introduction: Erythropoietin replacement is a key therapy of anemia asso-
dysfunction, cognitive impairment and inappropriate emotional responses. The ciated with chronic kidney disease. Rapid desensitization has been successful
severity of his symptoms caused him to be bed-bound. He had a reassuring in patients with immediate type I hypersensitivity to epoetin alfa, and a slower
MRI head, LP, and CT of his chest, abdomen and pelvis as well as a negative two-day protocol has been described in an adult patient who had delayed type
paraneoplastic antibody work-up. His anti-thyroid peroxidase antibodies and hypersensitivity reactions to the same agent. An eleven-year-old girl with a his-
anti-thyroglobulin antibodies were significantly elevated. The treatment regi- tory of end stage focal segmental glomerulosclerosis on hemodialysis devel-
men initiated included high dose corticosteroids, with a prolonged taper as well oped a diffuse, pruritic, maculopapular rash one day after starting epoetin alfa,
as IVIG, addition of mycophenolic acid and thyroidectomy. Interestingly, pathol- which recurred when darbepoetin alfa was subsequently administered. She then
ogy from the thyroidectomy revealed micropapilary cancer with local micro- failed a two-day epoetin alfa desensitization protocol but subsequently toler-
metastases in the lymph nodes. The patient returned to his baseline status, and ated epoetin alfa after a seventeen-day desensitization. Methods: Binding and
presently is continued on monthly IVIG, mycophenolic acid and a continued neutralizing anti-epoetin alfa and anti-darbepoetin alfa antibodies were meas-
prednisone taper. He has not had recurrence of his symptoms. Conclusion: ured using biosensor immunoassay (GE Healthcare-Biocare, Uppsala, Swe-
The above case highlights a rare and likely under-diagnosed immunologic den). A two-day subcutaneous epoetin alfa (Epogen, Amgen) desensitization
syndrome for which little guidance in the literature exists with respect to treat- schedule, adjusted by weight, was modeled after a previously published adult
ment beyond corticosteroids. This case report serves to review the clinical pres- epoetin alfa desensitization protocol. The patient developed an intensely pru-
entation, pathogenic theories, diagnosis and management options for ritic, maculopapular rash prior to the first dose of day two. She was started on
Hashimoto’s encephalopathy. The case also adds support to previous cases of prednisone 0.3 mg/kg (10 mg) daily and a prolonged protocol was designed.
successful treatment with thyroidectomy. Results: Anti-epoetin alfa and anti-darbepoetin alfa antibodies were absent. On
day 4, the patient’s rash resolved, and desensitization was resumed. She did
not have pruritic rashes prior to subsequent doses. On day 17, she reached her
target dose of 700 IU, and the prednisone was discontinued. At her three-month
follow-up visit, she continued to tolerate the epoetin alfa without adverse reac-
tion. Conclusions: To our knowledge, this is the first epoetin alfa desensitiza-
tion for a child with delayed type hypersensitivity who experienced an adverse
reaction to a two-day regimen. Subsequently, a slower dose escalation (seven-
teen days), with the support of a low dose systemic steroid, was successful at
building a desensitized state to epoetin alfa. This case corroborates the princi-
VOLUME 113, NOVEMBER, 2014 A67
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A68
ABSTRACTS: POSTER SESSIONS
ple that slower desensitization may increase tolerability in delayed type hyper- mon adverse reactions including fever, chills, rash, nausea, arthralgia, headache,
sensitivity reactions. and phlebitis. Skin testing evaluates the potential for a type I hypersensitivity
reaction. Despite a positive skin test, there are circumstances in which receiv-
Desensitization Protocol ing ATG is deemed necessary and in such circumstances, ATG desensitization
is recommended. Previous ATG desensitizations in adults have been unsuc-
cessful. Clinical Vignette: The patient was a 43 year old male with aplastic ane-
mia and mild intermittent asthma. His treatment started with cyclosporine and
ATG. On the first dose of ATG, he developed dyspnea, fevers, hypotension,
and tachycardia, which were treated with infusion cessation, acetaminophen,
morphine, and hydrocortisone, with relief of his symptoms. A second infusion
was attempted the next day per his initial protocol and again symptoms devel-
oped including dyspnea, tachypnea, chest tightness, fevers, and hypotension.
The infusion was stopped, supplemental oxygen given, and a CT chest with
contrast was obtained, which showed bilateral scattered ground glass opacities
with a few areas of focal consolidation. Given the possibility of ATG-induced
lung toxicity, no further ATG was given and the patient was maintained on
cyclosporine. Eighteen months later, the patient was found to have worsening
pancytopenia despite therapeutic cyclosporine serum levels. Given failure of
treatment with cyclosporine, treatment with ATG was deemed necessary. As
skin testing results would not have changed the plan for desensitization, skin
testing was deferred. The patient underwent the ATG desensitization protocol
outlined in Table I which was based on the protocol put forth by Ferdman and
colleagues. He tolerated the protocol well without symptoms except fever on
day 2 of the protocol which resolved with acetaminophen. Conclusion: Suc-
cessful desensitization to ATG has been documented in only pediatric patients
as adult patients have developed symptoms necessitating cessation of the desen-
sitization. This case illustrates a successful desensitization to ATG in an adult
patient with aplastic anemia.
P152
NICKEL AND COBALT ALLERGY: THE IMPORTANCE OF
PATIENT HISTORY.
P154
INTRANASAL MOMETASONE AS AN ALTERNATIVE TO FLU-
P. Naik*, R. Steele, M. Aquino, L. Fonacier, Mineola, NY. TICASONE IN AN HIV PATIENT ON RITONAVIR.
Rationale: Contact dermatitis (CD) is one of the most common inflamma- S. Deol*, D.A. Khan, Dallas, TX.
tory skin diseases diagnosed by allergists, dermatologists, and primary care
providers. The presentation of CD is variable based on its time course; it can Introduction: Adrenal suppression and Cushing’s syndrome have been
range from red clustered vesicles to bullae with both scaling and pruritus. Aller- reported due to the interaction between ritonavir and intranasal fluticasone. We
gic CD can complicate or co-exist in the patient with atopic dermatitis (AD). report the successful use of an alternative intranasal steroid (INS) in a patient
Methods: An 11 year old female with a history of AD was referred to the who previously had adrenal suppression due to ritonavir and intranasal flutica-
Allergy/Immunology Clinic at Winthrop University Hospital for evaluation of sone. Methods: Case report. Data: A 50 yo M with HIV on a boosting dose of
persistent chelitis despite evaluation and management by her primary care physi- ritonavir 100 mg BID as well as emtricitabine-tenofavir, raltegravir, and darunavir
cian and dermatologist. Over the last four years, the patient reported worsen- was treated with fluticasone intranasal spray 2 sprays per nostril daily for aller-
ing of perioral and lip lesions. She had been treated with topical tacrolimus and gic rhinitis. After 6 months, he reported good control of rhinitis and lacked signs
corticosteroids with minimal improvement. She denied any perioral pruritis, or symptoms of adrenal suppression. Three months later he was noted to have
worsening of lesions with food ingestion, or use of any cosmetic or lip balm abdominal striae and easy bruising. Early morning cortisol was <1.0 and ACTH
products. She reported using the same toothpaste on a regular basis and denied was found to be <5. He was started on a tapering dose of hydrocortisone and
licking her lips. She reported skin irritation with costume jewelry and hobbies intranasal fluticasone was discontinued. Upon further inquiry, on some occa-
included flute playing. Physical examination revealed dyshidrosis and chelitis sions the patient self-increased his INS dose up to 2 sprays tid. After comple-
(dry cracked lips and perioral erythema with no other active eczematous lesions tion of the hydrocortisone taper, early morning cortisol and ACTH were within
present). Suspicion for allergic CD exacerbating atopic dermatitis. The patient normal range and his Cushingoid appearance resolved. After 9 months of treat-
was treated with emollients and continued use of a low potency topical CS. ment with intranasal antihistamines, oral antihistamines, as well as leukotriene
Results: The patient underwent patch testing with the North American Contact antagonist therapy, his rhinitis symptoms were still not controlled and were
Dermatitis panel which included a total of 69 allergens including metals, cos- greatly affecting his quality of life. A baseline morning cortisol and ACTH were
metics, fragrances, preservatives and medications. She had positive results to normal. Intranasal mometasone was prescribed and he was counseled on the
nickel (3+), cobalt (2+), and neomycin(2+). The nickel and cobalt were deter- strict usage of mometasone 1 spray per nostril daily. After 4 weeks of continu-
mined to be of probable relevance as they were likely components of her flute. ous therapy, early morning cortisol and ACTH remained normal. After 6 months
The neomycin was considered to be of unknown or past relevance. She was of follow-up, he continues to have excellent symptom control and absence of
counseled on a trial avoidance of her metallic flute. Conclusions: Nickel remains Cushing’s syndrome on repeat examinations. Conclusion: Our case demonstrates
the most common allergen obtained from patch testing. In patients with lip der- that adrenal suppression with the concomitant use of intranasal fluticasone and
matitis one must consider allergens including lip balms, lipsticks, toothpastes, ritonavir can also occur while on the lower boosting dose of ritonavir. This case
gums and hobbies including playing an instrument. In patients with co-exist- also suggests that intranasal mometasone is safe and effective with concomi-
ing AD consider allergic CD, if there is not a response to medical pharma- tant ritonavir 100 mg twice a day in a patient with HIV.
cotherapy and interventions, identification and avoidance of relevant aller-
gens is the mainstay treatment of CD.
P155
THE POTENTIAL EFFECTS OF ALLERGY IMMUNOTHERAPY
P153 ON EOSINOPHILIC ESOPHAGITIS.
SUCCESSFUL DESENSITIZATION TO ANTITHYMOCYTE V. Miller*, E. Lanford, J. Kurz, S. Shah, G. Patel, Dublin, OH.
GLOBULIN IN AN ADULT PATIENT WITH APLASTIC ANEMIA. Background: We will describe two unique cases regarding the potential
K. Lindgren*1, K. Conner2, B. Yu2, 1. Elmhurst, IL; 2. Chicago, IL. effects of allergy immunotherapy (IT) on eosinophilic esophagitis (EE). Meth-
Background: Antithymocyte globulin (ATG) is a lymphocyte-selective ods: Patients underwent a complete history, physical exam, skin prick testing
immunosuppressant indicated for the management of allograft rejection in renal (SPT) by classical method, and an accelerated IT program. Both patients reached
transplant patients and aplastic anemia. ATG has the potential for adverse reac- their maintenance doses, which was 0.5ml of a 1:1 concentration. EE was diag-
tions including type I hypersensitivity reactions as well as other more com- nosed via EGD and biopsy. Results: Case 1: Patient presented for evaluation
A68 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A69
ABSTRACTS: POSTER SESSIONS
of seasonal allergy symptoms and food allergies. Patient had a known history ness, TL was not on coagulation factor IX, the one protein that he was miss-
of EE that was previously controlled with an elimination diet. SPT revealed ing, because of multiple instances of anaphylaxis and inhibitors to it. Interest-
positive results to dust mites, cat, dog, grass, trees, weeds, milk, egg, peanut, ingly, he had undergone two desensitizations as a toddler with eventual fair
multiple tree nuts, and sesame. Patient was started on IT for allergic rhinitis, control of his bleeding despite high inhibitor levels. However, in recent years,
and after six months of treatment the patient reported that dysphagia had pro- allergic symptoms to factor IX started to escalate, requiring change of therapy
gressively worsened despite avoidance of all known food triggers. Case 2: to factor VII, which bypassed the factor IX-dependent step in the coagulation
Patient presented with complaints of dysphagia and seasonal allergy symp- cascade and kept his bleeding under variable control. Outcome: TL continues
toms. SPT revealed positive results to trees, grass, weeds and cockroach. Daily to struggle with allergies to factor IX, acute on chronic pain exacerbations,
symptoms of dysphagia were uncontrolled on a proton pump inhibitor alone. and ongoing complications including a recent large deep venous thrombosis
The patient was referred to a GI specialist for a definitive diagnosis, and EE (DVT) in his left arm. He is now undergoing desensitization to factor IX again
was confirmed with an EGD and biopsy. An elimination diet was not initiated. but is now using Rixubis instead of BeneFIX, with the addition of rituximab.
Patient was prescribed a daily swallowed budesonide and Splenda mixture for Because the protocol by Sarah Alexander was denied by insurance, TL is now
three months after which treatment was stopped with improvement in symp- desensitizing according to the protocol by Dioun et. al at Boston’s Children’s
toms. Three months after swallowed budesonide was discontinued, allergy IT Hospital. Advantages for rituximab include lowering inhibitor levels and bleed-
was initiated for treatment of allergic rhinitis. IT was continued for 1.5 years ing symptoms with a reported beneficial change in factor kinetics. The disad-
until discontinued by the patient. Upon completion, the patient reported that vantage, however, is that rituximab can be associated with anaphylaxis, and in
dysphagia had continued to improve since starting IT. Conclusions: The inhala- rare cases, multifocal leukoencephalopathy. With his debilitating disorder,
tion of aeroallergens may have an effect on the inflammation occurring in the depression is certainly a concern, but TL is now doing better than ever before,
esophagus of EE patients. It is hypothesized that using IT to reduce sensitiza- and hope exists for even newer therapies on the horizon, including several long-
tion would greatly impact this inflammatory response, however, there are no acting formulations of factor IX. Conclusion: Hemophilia B is a chronic, life-
controlled studies on allergy IT as an adjunctive treatment for EE. Our case threatening, debilitating condition, but with a history of allergies and anaphy-
reports indicate that there is conflicting data on whether or not IT can impact laxis to the one protein that is missing, treatment and management becomes
EE, and if this impact is harmful or beneficial. Our recommendations are to much more complex. This case report is an important reminder of the need for
continue research on the role of aeroallergens in the pathogenesis of EE, to con- a strong interdisciplinary team to stay involved and to stay abreast of new
sider the effects of IT on EE, and to assess the risks and benefits of continu- medical advances to help maximize care for this patient.
ing IT on patients with EE.
P158
P156 A NAVAJO INFANT WITH SCID PRESENTS WITH HYPOXIA,
FUNCTIONAL ABDOMINAL PAIN OR MAST CELL GI DISOR- SEVERE NEUTROPENIA AND A NORMAL IGG LEVEL.
DER: A STAIN AWAY. P. Uong*1, N. Jain2, 1. Phoenix, AZ; 2. Gilbert, AZ.
K. Anthony*, L. Wild, New Orleans, LA. Introduction: Defects in the gene Artemis are known to result in a form of
Introduction: Chronic abdominal pain associated with bowel dysfunction severe combined immune deficiency (SCID). The incidence of this defect in
affects 15% of the general population. These patients often undergo extensive the Athabascan-speaking Native American population is about 1/2000 live
negative work-ups and are diagnosed with functional pain disorders. Gas- births. Here, we describe a case of an infant with SCID with the Artemis gene
trointestinal mast cell disorders are not always considered in the differential defect who presented with severe neutropenia despite a normal IgG level. Case:
diagnosis; however, recent studies suggest patients with chronic abdominal pain A 5-month-old Navajo female with a history of poor weight gain and frequent
may have an underlying gastrointestinal mast cell disorder that will improve respiratory tract infections was admitted to the hospital due to hypoxemia and
with appropriate therapy. We present a case suggesting these patients should respiratory distress. Initial chest radiograph from the ED revealed bilateral infil-
be evaluated for a gastrointestinal mast cell disorder. Methods: A 32 y.o. male trates, and the child was placed on supplemental oxygen via nasal cannula. Res-
with allergic rhinitis presented with a 3 year history of diffuse abdominal pain, piratory culture was positive for respiratory syncytial virus (RSV) and rhi-
diarrhea, and a sensation of “itching” inside the abdomen. He denied any asso- novirus. Initial lab work up revealed an abnormal complete blood count (CBC)
ciated flushing, rash, wheezing, difficulty breathing, syncope, or dizziness. with leukopenia, lymphopenia, and profound neutropenia (absolute lympho-
He had undergone an extensive evaluation including endoscopy, colonoscopy, cyte count approximately 1000/mm3 and an absolute neutrophil count of
CT abd/pelvis, CBC, CMP, ESR, and celiac screening. Given his persistent 300/mm3). HIV screen was negative. IgG was preserved at 811 mg/dL, IgA
symptoms, he underwent a repeat endoscopy/colonoscopy with biopsies and was < 8 mg/dL, and IgM was 301 mg/dL. IgG subclasses revealed a total IgG
staining for CD 117+ cells. Results: CT abd/pelvis, CBC, CMP, ESR, and celiac at 799 mg/dL (IgG1 681mg/dL, IgG2 8 mg/dL, IgG3 6 mg/dL, and IgG4
screening were normal. Previous endoscopy and colonoscopy were negative. undectable). The patient developed ecthyma gangrenosum of the nose secondary
Repeat endoscopy and colonoscopy with staining for CD 117+ cells was sig- to infection at the site of nasal cannula with culture positive for pseudomonas
nificant for >20-40 mast cells per hpf in the stomach, duodenum, terminal species. The patient was put on anti-pseudomonal therapy with meropenum
ileum, and colon. Systemic mastocytosis was ruled out with normal serum and ciprofloxacin. Immunology consult was obtained due to persistent severe
tryptase and normal bone marrow biopsy. He was started on daily H1 and H2 neutropenia of unclear etiology. Recommendations were made for bronchoscopy,
blockers with significant improvement in abdominal pain and diarrhea. Con- which revealed P. jirovici pneumonia and the patient was started on sul-
clusion: Chronic abdominal pain and diarrhea in this patient were likely sec- famethoxazole/trimethoprim. T-cell receptor excision circles (TREC) assay
ondary to mast cell gastroenterocolitis. Treatments for mast cell gastrointesti- revealed <74 TREC/106 cells suggestive of SCID. Due to her Navajo back-
nal disorders including oral antihistamines and oral mast cell stabilizers are ground, the patient was suspected of having a defect in the Artemis gene and
available and usually effective. Accurate diagnosis enables patients to start was transferred to the University of California at San Francisco Medical Cen-
appropriate treatment, leading to improved symptom control and quality of life. ter for further management including a bone marrow transplantation. Conclu-
This case suggests patients with persistent abdominal pain and bowel dys- sion: This is the first reported case of a child with a defect in the Artemis gene
function may need evaluation for a mast cell GI disorder, even in the absence presenting with severe neutropenia and a normal IgG level. This unusual lab
of symptoms of systemic mastocytosis. presentation led to a delay in immunology consultation and a definitive diag-
nosis. Although the patient’s absolute lymphocyte count was also low, initial
work up focused on the patient’s neutropenia.
P157
ANAPHYLAXIS TO A LIFE-SAVING REMEDY.
P. Uong*1, K. Christine1, D. Wong2, 1. Phoenix, AZ; 2. Mesa, AZ. P159
METAL HYPERSENSITIVITY AS A CAUSE OF RECURRENT
Introduction: We teach patient with allergies to avoid allergen as the first
step in treatment, but what if that allergen is a life-saving treatment? We pres- INFECTIONS AFTER JOINT REPLACEMENT.
ent a case of a child with severe hemophilia B who developed anaphylaxis to D. Hirsch*, V. Bonagura, Great Neck, NY.
coagulation factor IX with subsequent desensitization attempts and associated Rationale: Hip replacement surgery is an increasingly common procedure
medical complications. Case: TL is a 15 year-old male with severe hemophilia in the United States, as more than 300,000 individuals undergo total hip replace-
B who presented to the hospital for severe right arm pain and swelling, found ment (THR) yearly. Common causes of joint replacement failure have histor-
to be compartment syndrome requiring an urgent fasciotomy. Despite his ill- ically included mechanical loosening, infection, fractures around the implant,
VOLUME 113, NOVEMBER, 2014 A69
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A70
ABSTRACTS: POSTER SESSIONS
and joint instability. Failure rates are as high as 6.1% for metal-on-metal THR diagnosis of linear scleroderma. She presented with facial and both proximal
and 3.3% for ceramic-on-ceramic articulations[i]. In the general population, and distal extremity angioedema that was poorly responsive to oral corticos-
10-15% of individuals have metal hypersensitivity[ii], which may represent an teroids, antihistamines and plaquenil. There was no associated urticaria or pru-
increasing cause of joint replacement failure. We describe the presentation, ritus and no identifiable exacerbating factors. C4 complement (44 mg/dL), C1
clinical course, and evaluation of a patient with recurrent infections after THR Esterase inhibitor (40 mg/dL), and C1q (8.3 mg/dL) were all normal. Quanti-
who was ultimately diagnosed with metal hypersensitivity. Methods: A 48-year- tative immunoglobulins (IgG 1010 mg/dL, IgM 206 mg/dL, IgA 141 mg/dL)
old man presented for an immunological evaluation because of recurrent infec- were normal. Serum protein electrophoresis was normal. Auto-antibodies (anti-
tions after a THR. Three days after the operation, he developed a fever and DNA, anti-SCL70, anti-nuclear, anti-TPO, anti-TG) were negative. Over a period
underwent a washout and temporary insertion of a spacer. A few weeks later, of 2 months, serum IgG decreased from 1010 mg/dL to 659 mg/dL and serum
he underwent re-implantation of hardware, but the wound did not heal prop- IgG2 from 206 mg/dL to 153 mg/dL. Serum histamine was elevated (8.7ng/mL)
erly so a spacer was inserted and he had another re-implantation of hardware and tryptase was slightly elevated at 13 ng/mL. She acutely developed a marked
3 months later. One year after the original procedure, he developed an abscess hypereosinophilia, AEC 3200/mL up from a baseline of 400/mL, 2 months ear-
and a fistula in the hip. He was treated with intravenous antibiotics and had lier. Parasitic workup was unremarkable. Bone marrow and cytogenetic evalu-
another re-implantation of hardware. One year later, he again developed a ations for hypereosinophilic syndrome, mastocytosis, and myeloproliferative
joint infection which required removal of the hardware and implantation of a disorders was negative. She was started on hydroxyzine 200 mg daily and a low
temporary spacer. Prior to the hip replacements, he had been very healthy with histamine diet with resolution of the angioedema, tryptase levels dropped to
no significant infections. Results: After an immunological workup was unre- 6ng/ml and serum histamine to 2.2 ng/mL and eosinophils decreased to 400/ml.
markable, patch testing to metals contained in the prosthetics elicited positive Conclusions: We report a case of atypical angioedema, mildly elevated tryptase
responses to nickel and chromium. Conclusions: It is important to include metal levels and histaminemia which has been responsive to high dose antihistamines
hypersensitivity in the differential diagnosis of individuals presenting with and modified histamine-restricted diet. Evaluations for mastocytosis and neo-
recurrent infections after joint replacement. plasias have been unremarkable.
P160 P162
USE OF IVIG IN PATIENTS WITH SHWACHMAN-DIAMOND USE OF RITUXIMAB TREATMENTS FOR ACQUIRED DEFI-
SYNDROME. CIENCY OF C1 ESTERASE INHIBITOR.
J.M. Zibert*1, M. Scotten2, S. Gierer2, 1. Kansas City, MO; 2. Kansas T. Lee*, P. Busse, New York, NY.
City, KS. Acquired deficiency of C1 esterase inhibitor (ACID) is a rare disorder with
Introduction: Shwachman-Diamond Syndrome (SDS) is a rare, autosomal recurrent episodes of self-limited angioedema that typically affects the skin or
recessive disorder characterized by pancreatic dysfunction, hematologic abnor- mucosal tissues of the upper respiratory and gastrointestinal tracts. An under-
malities, small stature, and recurrent infections. Dysgammaglobulinemia in lying defect of ACID may be an undiagnosed malignancy or autoimmune dis-
SDS has been reported, but the use of Intravenous Immunoglobulin (IVIg) to ease, therefore further investigation to rule out these disorders is critical. The
reduce infection rate has not been studied. We present siblings with SDS treated management of a patient with ACID involves education about potential trig-
with (IVIg) whose rate of hospitalization was dramatically reduced. Case gers (including surgery, trauma, medications), ready access to acute treat-
Description: We present brothers, ages 15 and 17, diagnosed with SDS in early ment, and in some patients consideration of a prophylactic treatment. We pres-
childhood, who have exocrine pancreatic dysfunction, small stature, and recur- ent an 82 year old male that developed multiple episodes of angioedema of his
rent infections. Since diagnosis, they have required repeated hospitalizations extremities and in an episode of airway swelling around age 75 years. A diag-
for infections. Both had normal immunoglobulin levels, MBL function, total nosis of ACID was made by a decreased C4, C1-inh function, C1-inh protein
complement, neutrophil oxidative burst, and post-vaccination antibody levels. level and a low C1Q. There was no evidence of an underlying malignancy. He
Between 2007 and 2013, the 15 year old had an average of 2 hospitalizations was initially given C1 inhibitor concentrate (C1INHRP) for treatment of acute
per year for fever or infections. After initiation of IVIg in March 2013, he has attacks and danazol for prophylaxis as his attacks were becoming more fre-
had no hospitalizations for fever or infections. Between 2007 and 2013, the 17 quent. Initially his attack rate and severity decreased, but over the following
year old averaged 1.86 hospitalizations per year for fevers or infections. After years, he required nearly weekly rescue dosing of C1INHRP for acute attaks.
initiation of IVIg in March 2013, has had only one hospitalization for fever. His danazol was changed to aminocaproic acidwithout improvement. A high
Since initiation of IVIg, both patients reported significant improvement in their antibody titer to C1-inh was detected and the patient was also given icatibant
quality of life with improved fatigue and less missed school days. Discussion: for rescue medication. He was subsequently given a round of rituximab which
SDS is a rare congenital disorder with limited data on treatment options. Recur- significantly decreased his frequency of attacks and need for rescue therapy.
rent respiratory infections, beginning early in childhood, are frequently reported After approximately 1 year, his angioedema symptoms increased in frequency
and often require hospitalization to rule out sequelae. While SDS may be asso- and he was given another course of rituximab with improvement again, which
ciated with immunoglobulin deficiencies, a literature search did not reveal waned over the following year. A third course of rituximab was administered.
any publications documenting the use of IVIg to reduce infection rate in patients The patient has been monitor for lymphocyte numbers and specific antibody
with SDS. In the two patients presented, the use of monthly IVIg has shown responses. In conclusion, treatment of ACID can be difficult and may require
objective health benefits including decreased overall infection rate and decreased rituximab. Although additional courses of rituximab may be warranted, it should
hospitalization rate; as well as subjective improvement in quality of life, be done with careful monitoring of the patient’s immune status.
improved fatigue, and decreased number of missed school days. This unique
case study supports the use of monthly IVIg infusions in patients with SDS by
providing objective data. It also supports the important need for the develop- P163
ment of more scientifically supported clinical guidelines in the treatment of EVALUATING THE USE OF ICATIBANT INJECTIONS
rare genetic conditions causing immune deficiencies. (FIRAZYR®) WITH C1 ESTERASE INHIBITORS (CINRYZE®
AND BERINERT®) DURING PREGNANCY OF A TYPE III
HEREDITARY ANGIOEDEMA PATIENT.
P161 F.F. Ansary*1, T.J. Craig2, 1. Hummelstown, PA; 2. Hershey, PA.
STEROID REFRACTIVE ANGIOEDEMA ASSOCIATED WITH
Background: Hereditary angioedema (HAE) is a rare disease, character-
MILD MAST CELL ACTIVATION AND HISTAMINEMIA.
ized by localized swelling, inflammation, and pain. It is the over production of
J. Dara*1, A. Rubinstein2, 1. New York, NY; 2. Bronx, NY. bradykinin that leads to the angioedema. Icatibant (FIRAZYR®) is used to
Introduction: 65-year-old female with linear scleroderma was evaluated for treat acute attacks of hereditary angioedema by inhibition of the bradykinin
recurrent angioedema refractory to high dose steroids and antihistamines. She receptor. Icatibant is approved for use in type I and II, but is often used off label
was initially found to have a mildly elevated serum tryptase, elevated serum his- for type III. Icatibant is contraindicated in pregnancy and at this time no data
tamine, and eosinophilia. Bone marrow analysis and cytogenetic studies were are available on the safety of using icatibant in pregnancy. We report a case of
unremarkable. Serum abnormalities and angioedema resolved on high dose anti- type III HAE with frequent use of icatibant that suggests icatibant may be safe
histamines and a modified mastocytosis diet. Methods: Immunological, genetic, during pregnancy. Methods: The patient was first diagnosed with type III hered-
and pathological evaluations of a patient, LL, with atypical angioedema were itary angioedema based on her history and normal compliment blood tests. C1-
performed. Results: LL had a history of benign multinodular goiter and recent inhibitor was given for prophylaxis. Icatibant was used frequently for attacks
A70 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A71
ABSTRACTS: POSTER SESSIONS
and continued to be used despite onset of pregnancy without the prescribers’ was initiated. Xolair and montelukast were discontinued. He was subsequently
knowledge. During the first two trimesters, icatibant was used multiple times treated with Rituxumab 375mg/m2 for four weeks. Six weeks following dis-
a week. Results: Despite the use, two births resulted in normal fetuses without charge, he developed severe abdominal pain and presented with an acute
apparent teratogenic effects. One fetus was premature by 2 weeks and slightly abdomen. Exploratory laparotomy revealed full thickness perforation of the
below gestational weight; however, is physically normal and up to date on devel- proximal jejunum. Histopathological evaluation of the resected segment was
opmental skills. Conclusions: It appears that the use of icatibant early during consistent with eosinophilic vascultitis. Post-operatively, prednisone 25 mg and
pregnancy is safe; however, additional cases of accidental use during pregnancy cyclophosphamide 100 mg daily have resulted in resolution of eosinophilia and
are needed to confirm this suspicion. improvement in symptoms. Conclusion: EGPA may be precipitated by CS with-
drawal in patients with adult onset, steroid-dependent asthma. Consequently,
clinicians should cautiously monitor for signs of EGPA when tapering CS in
P164 severe asthma patients, especially in those with eosinophilia.
THE PERPLEXING NATURE AND CLINICAL PROGRESSION
OF EOSINOPHILIC GRANULOMATOSIS WITH POLYANGITIS
IN A PREVIOUSLY HEALTHY ELITE ATHLETE. P166
T. Ocampo*, T. Rans, San Antonio, TX. TREATMENT OF REFRACTORY MACROPHAGE ACTIVATION
SYNDROME IN SYSTEMIC JUVENILE IDIOPATHIC ARTHRI-
Eosinophilic granulomatosis with polyangitis (EGPA), formerly known as
TIS WITH HIGH DOSE ANAKINRA.
Churg-Strauss syndrome, is a rare multisystem, antineutrophil cytoplasmic anti-
body (p-ANCA) associated vasculitis characterized by asthma and hypere- J. Kwong1, T. Peng*2, A. Mohiuddin1, P.F. Weiss3, R.Q. Cron4, D. Chefitz1,
osinophilia. Its clinical manifestations are variable and often develop over years, V. Craig1, D. Weissmann1, J. Andujar-DeLaCruz1, L.N. Moorthy1, 1. New
making diagnosis challenging. We present a previously healthy 30 year old Brunswick, NJ; 2. Edison, NJ; 3. Philadelphia, PA; 4. Birmingham, AL.
female marathon runner with abrupt onset rhinitis without polyps, productive Background: Macrophage Activation Syndrome (MAS), a potentially fatal
cough of mucus plugs, intermittent dyspnea, and chest tightness while living complication of sJIA (systemic juvenile idiopathic arthritis), is characterized
in Missouri. Although diagnosed clinically with allergic rhinitis and asthma, by high persistent fevers, hepatosplenomegaly, lymphadenopathy, pancytope-
antihistamines and inhaled corticosteroid (ICS) use provided minimal relief. nia, hyperferritinemia, hypertriglyceridemia and liver dysfunction. Objective:
Symptoms initially improved upon relocation to Texas, but occasional respi- To describe a case of sJIA and MAS requiring high dose anakinra (interleukin-
ratory exacerbations occurred over the following year. Abruptly, during a bout 1 receptor antagonist). Case Description: An 8-year-old female with sJIA
of sinusitis, she endorsed fatigue, weight loss, burning leg pain, facial improved with pulse methylprednisolone (30 mg/kg/day IV x 3 days), anakinra
angioedema, and a blistering rash. Routine CBC demonstrated marked (3 mg/kg/day SQ), and tocilizumab (monoclonal interleukin-6 receptor anti-
eosinophilia (AEC 16,100) prompting hospital admission. Initial investigation body) infusion. Two weeks later, she developed unremitting fevers (105°F)
of primary (FIP1L1-PDGFRA) and secondary (medications, infectious, malig- and MAS was suspected. Results: She had hyperferritinemia, elevated d-dimers,
nancy, rheumatologic) etiologies of eosinophilia were unrevealing. Rheuma- transaminitis, and hypertriglyceridemia. Bone marrow biopsy revealed hemo-
toid factor (RF), antineutrophil antibody (ANA), and ANCA (PR3 Ab 0.5, MPO phagocytosis and anti-CD163 staining identifying activated histiocytes. She
Ab 0) were negative. Sinus CT revealed extensive paranasal sinus disease. Chest received high dose methylprednisolone (30 mg/kg/day IV x 6 days, then tapered
CT revealed tree in bud and ground glass opacities, mucus plugging, and lym- over 7 months), cyclosporine, intravenous immunoglobulin, and anakinra (Table
phadenopathy (normal chest CT the year prior). Serum IgE (3901 IU/ml) and 1) for MAS. Anakinra was increased from 3 mg/kg/day to 12 mg/kg/day. Fever
CRP (1.4mg/dL) were elevated. Aspergillus precipitans were negative. Skin resolved in 4 days, laboratory markers improved and she was discharged home
biopsy revealed eosinophil infiltration and findings consistent with vasculitis, in 14 days. Medications were tapered over 12 months. She subsequently flared
which along with her constellation of symptoms led to the diagnosis of EGPA. and was controlled on daily anakinra. She was then switched to monthly
Prednisone (75mg daily) was started with rapid resolution of peripheral Canakinumab, and her disease continues to be in remission on Canakinumab.
eosinophilia and she has continued to clinically improve on a prolonged steroid Discussion: We report a case of MAS occurring during the initial presentation
taper. Retrospectively, this patient demonstrated the prodromal, eosinophilic, of sJIA. Excess interleukin-1 can lead to the clinical and laboratory findings
and vasculitic phases described in EGPA. However, her diagnosis was elusive of sJIA and MAS, and the up regulation of interleukin-6. Uncontrolled pro-
to her multidisciplinary team until a rapid surge of symptoms prompted a skin duction and activation of macrophages and T lymphocytes lead to MAS man-
biopsy. This case reminds the practicing Allergist of the importance of frequent ifestations, including prolonged high fever, pancytopenia, coagulopathy, lym-
reassessments and to maintain a high index of suspicion for alternative diag- phadenopathy, hepatic insufficiency, and neurologic dysfunction. MAS can
noses in patients with emerging presentations. rapidly progress to multi-organ failure and death if not treated aggressively.
Anakinra is a recombinant interleukin-1 receptor antagonist with a short half-
life (~ 4-6 hours). The usual dosage of anakinra is 1-2mg/kg/day. Our patient
P165 responded to a 4-fold increase in standard dosing, without adverse events. Our
EOSINOPHILIC GRANULOMATOSIS WITH POLYANGIITIS experience suggests that high dose anakinra is effective and safe in refractory
PRECIPITATED BY CORTICOSTEROID WITHDRAWAL. MAS secondary to sJIA.
J.L. Hill*, S. Patel, D. Sudano, T.F. Carr, Tucson, AZ.
Table 1 – Response after Increased Anakinra Dosing
Introduction: Eosinophilic granulomatosis with polyangiitis (EGPA) is a
rare, systemic vasculitis characterized by a prodromal phase of chronic rhi-
nosinusitis, asthma, and eosinophilia. Treatment of asthma with CS (corticos-
teroids) may suppress clinical signs of EGPA. Further, agents such as omal-
izumab or leukotriene modifiers may enable weaning from CS, subsequently
unmasking EGPA. We report a case of EGPA with onset following cessation
of systemic CS and complicated by mesenteric vasculitis with bowel perfora-
tion. Case Presentation: A 56-year-old man with allergic rhinitis, chronic sinusi-
tis, one-year history of steroid-dependent asthma, and eosinophilia (0.4-
1.9K/uL) was hospitalized with severe epigastric abdominal pain, worsening
dyspnea, and left upper extremity weakness and numbness that developed one
week after abrupt discontinuation of oral prednisone. Asthma therapies included
inhaled CS, long-acting bronchodilators, montelukast, systemic CS, and oma-
lizumab. Extensive eosinophilia workup was previously negative. Physical
examination on presentation was significant for bibasilar crackles, periumbil-
ical tenderness, and decreased sensation to and weakness of the left hand. Data:
WBC 26K/uL, absolute eosinophil count 15.2K/uL, CT chest: peribronchial
ill-defined ground glass opacities and tree in bud nodules, BAL: 35%
eosinophils, EGD: patchy erosions from distal duodenum to the middle jejunum,
C-ANCA positive with a titer 1:256, Myeloperoxidase antibody elevated at 111
AU/mL. A diagnosis of EPGA was made and pulse dose methylprednisolone
VOLUME 113, NOVEMBER, 2014 A71
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A72
ABSTRACTS: POSTER SESSIONS
P167 P168
PRIMING OF ANAPHYLAXIS WITH SEQUENTIAL ALLERGEN PANCYTOPENIA IN A PATIENT WITH GOOD’S SYNDROME.
EXPOSURE IN A 35 YEAR-OLD MALE. J. Regan*, W. Stevens, B. Stein, P. Avila, Chicago, IL.
R.S. Paul1, L. Anderson2, A. Rafi2, J. Yusin*2, 1. San Francisco, CA; 2. Los Good’s Syndrome is a rare disorder associated with thymoma, hypogam-
Angeles, CA. maglobulinemia, low peripheral B cells, and abnormal cell-mediated immu-
Background: The clinical evolution of anaphylaxis is highly variable, nity. Complications from this disease include increased incidence of infec-
depending on the volume of antigen exposure and degree of sensitization tions and autoimmune diseases. Since the discovery of Good’s Syndrome in
amongst other factors. Such a reaction may even progress in a stepwise fash- 1955, the prevalence of this disease is estimated to be only approximately 5%
ion with sequential allergen exposures. A phenomenon of “anaphylactic prim- of patients with thymomas. We present a case of a 62 year-old male with a his-
ing” can be conceived given that the magnitude of basophil, Langerhans and tory of Good’s Syndrome status post thymectomy receiving intravenous
mast cell activation is quantitatively linked to the degree of IgE binding via immunoglobulin replacement who presented with mild dyspnea on exertion
FcεRI, FcεRII and Galactin 3 receptors. It thus follows that an intimate series and right arm swelling. The patient was found to have a right upper extremity
of individually small allergen challenges may translate into a summation of deep venous thrombosis (DVT). Interestingly, he was also incidentally found
effector cell activation and ‘readiness’ for histamine and vasoactive mediator to be pancytopenic with a white blood cell count of 3, hemoglobin of 4.9, and
release. We report a case of anaphylaxis that likely exemplifies this phenome- platelets of 27. A bone marrow biopsy showed normocellular marrow with lack
non. Case presentation: A healthy 35 year-old male with no prior atopic his- of red blood cell precursors and very rare megakaryocytic precursors concerning
tory was outdoors when he was bitten on the left leg by a fire ant. The reaction for developing aplastic anemia or pure red cell aplasia. Infectious workup includ-
that ensued was limited to local swelling and irritation of the affected extrem- ing screening for human immunodeficiency virus, parvovirus, herpes virus,
ity. A few hours later, he ate lunch consisting of beef, sea bass and pesto. After Epstein-Barr virus, and cytomegalovirus was unremarkable. Hypercoagula-
15 minutes, he developed facial and lip swelling, throat closure and dyspnea bility workup for the DVT was negative including screening for Factor V Lei-
and heralded emergency medical services. His management in the field and in den, Prothrombin, Protein S, Protein C, Lupus Anticoagulant, and Antithrom-
the emergency room entailed intramuscular epinephrine and intravenous diphen- bin III dysfunction. The patient was started on prednisone 100mg daily and
hydramine with relief of symptoms. Work-up in the allergy clinic found him cyclosporine 250mg twice a day with improvement in anemia but very little
to have an obstructive pattern on spirometry with reversibility. Skin prick test- response in his thrombocytopenia. Unfortunately, the patient re-presented 1
ing demonstrated significant reactions to peanut, tree nut, dust mite, grass mix, month later with hearing loss, elevated liver function studies, and acute renal
Bermuda mix, weed mix, fire ant, horse, dog and cat. He was advised to avoid failure attributed to cyclosporine toxicity and this medication was subsequently
NSAIDs, sulphites, peanuts, tree nuts, fish and exposure to fire ant venom. He discontinued. As he continued to be thrombocytopenic, the patient was then
was prescribed oral cetirizine 10 mg with an epinephrine auto-injector and an started on N-plate weekly. The patient’s condition continued to deteriorate with
albuterol inhaler to use as needed for anaphylaxis and/or bronchospasm. Con- multiple hospitalizations for failure to thrive. His poor performance status
clusion: Anaphylaxis due to immediate hypersensitivity represents a state of precluded aggressive treatments including immunosuppression and the patient
clinically significant histamine and inflammatory mediator release from effec- ultimately passed away. In summary, this is a very interesting case of a patient
tor cells upon binding and cross-linking of IgE. The short chemical half-life with Good’s syndrome found to have pancytopenia.
argues that such mediators are released not only in remarkable quantity but in
synchrony in this setting. Recent allergen exposure in the form of fire ant venom
in this case may have recruited effector cells into a state of readiness, thereby P169
orchestrating a more profound level of mediator release following the second MINOCYCLINE-INDUCED ANAPHYLAXIS IN AN ADOLESCENT
allergen challenge. FEMALE.
T. Peng*1, A. Ettinger2, C. Maccia2, A. Weller2, L. Moorthy2, 1. Edison, NJ;
Skin Prick Results 2. New Brunswick, NJ.
Introduction: Minocycline is a semisynthetic tetracycline derivative used
in the treatment of acne vulgaris. It is associated with several adverse effects
including drug-induced lupus erythematosus, drug reaction with eosinophilia
and systemic symptoms, and serum sickness. There are few reported cases of
anaphylaxis to minocycline. Objective: To describe a patient with acne vulgaris
who developed minocycline-induced anaphylaxis. Case Description: A 16 year
old female with acne vulgaris treated with minocycline presented with a 2 day
history of diffuse, erythematous and pruritic rash, and fever (maximum tem-
perature of 38.8°C). Symptoms began approximately one hour following
minocycline ingestion and progressed to the development of arthralgias, eme-
sis, edema of the hands and feet and throat swelling. Patient was tachycardic
upon presentation in the emergency department. She received a 1 liter normal
saline bolus, diphenhydramine and was admitted. Results: Patient had ele-
vated c-reactive protein (12.6mg/dL) and sterile pyuria. Complete blood count,
complete metabolic panel C1 Esterase inhibitor functional assay, antinuclear
antibody (ab), anti-neutrophilic cytoplasmic ab, anti-double stranded DNA
ab, complements C3 and C4, were within range. Blood and urine cultures were
negative. Patient discontinued minocycline 2 days prior upon onset of symp-
toms when rash appeared. Patient was started on Solumedrol (2 mg/kg/day
divided every 6 hours). On HD (hospital day) #2, she was switched to Pred-
nisone 20 mg BID. Patient complained of “scratchy” throat, shortness of breath
and flushing concerning for anaphylaxis. 0.3 mg of Epinephrine was adminis-
tered intramuscularly. Patient’s rash continued to improve and symptoms of
edema, shortness of breath and fever resolved. Patient was discharged on HD#3
with Cetirizine, Ranitidine, 7-day steroid taper and EpiPen prescription. Dis-
cussion: Minocylcine-induced anaphylaxis has been discussed in a few case
reports in the existing literature. Our patient developed symptoms 1 month after
the initiation of minocycline. Patient’s symptoms partially improved after treat-
ment with antihistamines and steroids, but she required an intramuscular dose
of epinephrine, and was continued on an oral steroid course. As minocycline
continues to be one of the important treatments for acne vulgaris, clinicians
must be vigilant for its potential adverse effects.
A72 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A73
ABSTRACTS: POSTER SESSIONS
phocytes, 10% monocytes, 2% eosinophils. His LFTs were significant for an
P170 elevated AST of 80 U/L, and ALT of 100 U/L. Sepsis workup including blood
DRESS FOLLOWING PRES.
cultures was negative. Skin biopsy was consistent with the diagnosis of drug
S.M. May*, N.L. Ott, A. Joshi, M. Hartz, Rochester, MN. hypersensitivity reaction. Discussion: The time from starting phenytoin and
Introduction: Drug Related Eosinophilia with Systemic Symptoms (DRESS) appearance of rash with other positive findings noted above were all consis-
is a rare reaction to medications that occurs 2-6 weeks after drug exposure and tent with AHS. The patient was treated with intravenous steroids and improved.
typically presents with fever, rash, facial edema, lymphadenopathy, eosinophilia AHS is unusual in that it occurs later than most other drug reactions; about 2-
and transaminitis. Common medications are aromatic anti-convulsants, sul- 6 weeks after initiation of the offending agent. Frequently, the hallmark fea-
fonamides, and Dapsone with immunosuppression being a risk factor. Reacti- tures of fever, rash, and lymphadenopathy are accompanied by multiorgan-sys-
vation of herpes virus family is seen in 60-75% of the cases. The mainstay treat- tem decompensation. Recognition of this syndrome, which may have variable
ment is removal of the offending agent and high-dose steroids. Case Description: presentations, is the key to prompt discontinuation of the drug and further man-
17 year-old white male with history of sideroblastic anemia status post bone agement. This case demonstrates one such variable presentation and stresses
marrow transplant, immunosuppression, Posterior Reversible Encephalopathy the importance of recognizing a symptom free period prior to progression of
Syndrome (PRES) since January, adrenal insufficiency and atopic diseases that the disease to the state of shock. Furthermore, it reinforces the importance of
presented to the hospital with a very pruritic, bright red rash, shaking chills and including AHS and DRESS in the differential diagnosis of sepsis.
fevers. He was admitted for presumed adrenal insufficiency and graft-versus-
host disease leading to the rash. Rash was biopsied, he was started on hydro-
cortisone 15 mg TID and cefepime. Family remarked that the fevers and chills P172
have been present since diagnosis of PRES that was being treated with leve- FOOD PROTEIN INDUCED ENTEROCOLITIS SYNDROME
tiracetam, amlodipine, furosemide. Patient was also on Dapsone for prophy- (FPIES) IN A PATIENT WITH PRIOR IGE MEDIATED FOOD
laxis. He continued to have fevers and absolute eosinophil count was noted to ALLERGY.
be 5,420 on steroids with elevated liver enzymes. Allergy was consulted, viral J. Giacinto Lawrence*1, P. Ponda2, 1. Roslyn, NY; 2. Manhasset, NY.
titers at this time were negative. All the mentioned drugs were discontinued and
prednisone 100 mg daily was started with resolution of symptoms and labora- Introduction: FPIES is a disorder presenting as repeated bouts of emesis
tory abnormalities. A few months later, the patient had reactivation of EBV within 1-3 hours with or without subsequent diarrhea 5-8 hours after ingestion
treated with Rituximab and developed erythroderma, mild transaminitis and of an offending food. It is primarily a non-IgE-mediated hypersensitivity dis-
later eosinophilia (1,240). Prednisone was increased back to 50 mg daily and order commonly diagnosed during infancy. The pathophysiology although not
symptoms resolved. Conclusion: DRESS is a rare reaction to drugs that can be yet fully defined, likely involves stimulation of antigen-specific T cells and a
difficult to diagnose and even more difficult to determine the culprit medica- resulting proinflammatory cytokine cascade inducing increased permeability
tion due to the delayed timing. There are common drugs associated with this of intestinal mucosa. The gold standard for diagnosis is the oral food chal-
disorder, such as dapsone and amlodipine, but multiple medications have been lenge (OFC). The most common food triggers are milk and soy though solid
reported as individual cases including Levetiracetam and furosemide. Our foods can also induce FPIES. We present a case of IgE-mediated soy allergy
patient was taking all four of these. Reactivation of herpes viruses is common treated with years of avoidance that presented as FPIES upon re-introduction
and should be evaluated. Finally, immunosuppression is thought to be a risk of soy. Methods: A 6 month old female with eczema who developed a facial
factor and DRESS should be included in the differential in these patients pre- rash after drinking soy formula was found to have positive serum and skin prick
senting with rash, systemic symptoms and especially if eosinophilia is pres- tests (SPT) to soy, milk and eggs (see Figure 1). She had an OFC for baked egg
ent. at approximately 3 years old and passed. One year after incorporating baked
egg into the diet, the patient presented for a soy OFC. Results: The patient tol-
erated 5oz. (150mL) of liquid soy challenge without reaction and was subse-
quently discharged. She returned approximately 2 hours after initiation of the
soy challenge due to emesis. The patient’s vital signs remained stable; exam
was unremarkable with the exception of pallor; no rash was present. She
remained alert, responsive and talking with continued repetitive nausea and
vomiting. She received IM Benadryl and Epinephrine and was subsequently
transferred to the ER by ambulance for continued monitoring where she received
fluids, steroids and an antiemetic. The patient recovered and continues to avoid
soy. Conclusion: Although rare, cases of IgE-mediated allergy converting to
FPIES have been reported. Although FPIES is thought to be a predominantly
non-IgE-mediated reaction, the role of IgE remains unclear. A future role for
Rash biopsy site. other diagnostic measures, such as patch testing, to quantify the risks of food
challenge has been suggested however more research is necessary before these
tests can be recommended. Given these rare cases, there should be a higher
P171 awareness and vigilance when diagnosing or challenging a patient with prior
ANTICONVULSANT HYPERSENSITIVITY SYNDROME ASSO- IgE-mediated food allergy for possible non-IgE mediated reactions.
CIATED WITH A SYMPTOM FREE PERIOD.
S. Patel*1, E. Nwaobasi-Iwuh2, A. Wolff3, 1. Summit, NJ; 2. Morristown, Figure 1: Serum IgE and skin testing over time.
NJ; 3. Newark, NJ.
Introduction: Anticonvulsant hypersensitivity syndrome (AHS) is a known
potentially life-threatening complication of phenytoin, carbamazepine and phe-
nobarbital therapy. Although its occurrence is rare, when AHS occurs, it often
results in hospitalization and even death. Although the exact mechanism is
unknown, it is thought to be an immunologic adverse drug event that is a T-
cell–mediated, delayed hypersensitivity reaction. Case: An 8 year old male with
a history of seizure disorder maintained on phenytoin for 10 days, presented
to the ED with high fevers and a pruritic rash on his trunk, extremities and face.
On exam, pertinent positives included a temperature of 102F and a general-
ized erythematous, maculopapular rash. Phenytoin was discontinued. His fevers P173
and rash resolved within 48 hours without steroids. He was subsequently dis- AN ATYPICAL PRESENTATION OF CHRONIC EOSINOPHILIC
charged only to return to the ED 24 hours later with worsening rash and a PNEUMONIA.
fever of 103F. On examination, he appeared ill with tachycardia and hypoten-
sion. His pharynx was erythematous with cervical lymphadenopathy and he A. Yang*, R. Ganim, J. Mueller, P. Gurung, Springfield, MA.
had a generalized maculopapular, nonblanching rash. He was started on a Introduction: Chronic Eosinophilic Pneumonia (CEP) is an eosinophilic
dopamine drip, vancomycin and ceftriaxone for presumed sepsis. Results: His lung disease that is idiopathic and progressive. It is an uncommon disorder
CBC revealed a WBC count of 14,000/ml, with 73% neutrophils, 11% lym- affecting females, usually of the fifth decade, who present with chronic respi-
VOLUME 113, NOVEMBER, 2014 A73
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A74
ABSTRACTS: POSTER SESSIONS
ratory and systemic symptoms. An atopic history is common but may not be
present.The diagnosis is supported by eosinophilia greater than 1000cells/uL,
P175
A CASE OF HYPEREOSINOPHILIC SYNDROME PRESENTING
biopsy or bronchoalveolar lavage, pulmonary function tests (PFT), imaging
and the exclusion of other causes for eosinophilic lung disease. We present a WITH MYOCARDITIS.
case of an uncommon condition with an atypical presentation which illus- N. Fenny*, K. McGrath, A. Peters, Chicago, IL.
trates the importance of having a differential diagnosis in cases that may seem Hypereosinophilic syndromes (HES) are characterized by persistent hyper-
ordinary. Case Presentation: A 64 year old female without a smoking history eosinophilia with eosinophilic infiltration and mediator release that cause dam-
presented to clinic with a four month history of left posterior cervical painless age to multiple organs. The peripheral blood hypereosinophilia is defined as
lymphadenopathy. She denied any weight changes, fever, chills, hemoptysis, eosinophils exceeding 1.5 x 10 9/L on two separate occasions separated by at
poor appetite, dyspnea or cough. Physical examination showed she was breath- least one month. We describe a 53 year old female with a history of ovarian
ing on room air at 97% with clear lungs sounds bilaterally without egophony cancer, asthma, chronic rhinosinusitis with nasal polyps (CRSwNP) and
nor dullness to percussion. There were two lymph nodes which were smooth, eosinophilia who presented with chest pain of 4 days duration and was found
nontender and mobile of 1cm. HRCT showed multiple mediastinal, and bilat- to have an absolute eosinophil count (AEC) of 15. 4 x 10 9/L. Her troponins
eral hilar lymphadenopathy measuring 1.3 to 2.2 cm with groundglass opaci- and CKs were elevated. She denied initiation of any new medications. She was
ties in subpleural distribution with basilar predominance. No honeycombing, previously seen as an outpatient for eosinophilia, asthma and CRSwNP. At her
bronchiectasis, pleural effusion, consolidation, nodules nor masses were noted. most recent clinic visit 18 months ago, while undergoing chemotherapy with
She was referred to pulmonary clinic for workup for an inflammatory lung steroids for the ovarian cancer, her eosinophil count was 0. Her highest previ-
process. PFT showed a FEV1/FVC ratio of 82% and a diffusion capacity of ous AEC was 8.85 x 10 9/L. Previous workup for Churg Strauss and skin test-
59%. Additional findings showed eosinophilia of 43.4%, with absolute ing for Aspergillus fumigatus to evaluate for ABPA was negative. Workup
eosinophil count of 5,000cells/uL. Hypersensitivity pneumonitis panel, ANA, included a peripheral smear showing absolute eosinophilia with normal mor-
ANCA, and anti-CCP were negative. IgE was elevated at 838IU/mL. She had phology. ANA, cANCA, pANCA, tryptase and quantitative immunoglobulins
a right lung wedge resection which showed patchy eosinophilic infiltrates and were normal. She was HIV negative. Strongyloides serology as well as stool
intra-alveolar macrophages indicative of chronic eosinophilic pneumonia. Dis- O &P were negative. An echocardiogram showed an ejection fraction (EF) of
cussion: The initial presentation of posterior cervical lymphadenopathy and 59% and a small pericardial effusion. A cardiac MRI revealed a normal EF,
lack of respiratory symptoms presented a diagnostic challenge. CEP shows subtle evidence of edema and diffusely elevated gadolinium ECV fractions
peripheral consolidation with upper lobe predominance. Although the pattern thought consistent with myocarditis. FISH analysis was negative for the pres-
of HRCT indicated an interstitial lung pneumonia such as usual or fibrotic sub- ence of a deletion of CHIC2, or translocations involving the FIP1L1 and
type, biopsy confirmed it to be CEP. The combination of clinical history and PDGFRA genes. She was treated with methylprednisolone 60mg IV every 6
supporting clinical studies will guide the clinician towards a diagnosis for appro- hours with decline of her AEC to 0.4 x 10 9/L She was discharged home on
priate management. prednisone 60 mg daily for 1 week with follow up with hematology for possi-
ble bone marrow biopsy and cardiology for a cardiac catheterization with biopsy.
However, she was unable to follow up and presented 1 month later with chest
P174 pressure. She was found to have an AEC of 11.5 x 10 9/L. She underwent an
IGM DEFICIENCY PRESENTING AS STRONGYLOIDES HYPER- endomyocardial biopsy that showed eosinophilic myocarditis and was treated
INFECTION. with high dose steroids with improvement. The most likely diagnosis is idio-
J.G. Ghably*1, A. Kapila1, G. Shaw1, T. Roy1, R. Byrd1, K. Guha2, pathic HES. A bone marrow biopsy is pending to exclude other etiologies such
1. Johnson City, TN; 2. Winston-Salem, NC. as primary HES due to myeloproliferative disorder or systemic mastocytosis.
A 59 year old male with a history of type 2 diabetes, peripheral vascular
disease, chronic kidney disease, and multiple lacunar infarcts is hospitalized
for pontine stroke and treated for klebsiella and enterococcus pneumonia and
P176
EMERGING TREND OF HENNA TATTOOS CAUSING A CLINI-
Clostridium difficile colitis. He was readmitted following month for oxygen
CAL CONTACT DERMATITIS.
desaturation and altered mental status eventually requiring intubation and
mechanical ventilation. EEG and lumbar puncture revealed normal findings. P. Buddiga*, Fresno, CA.
Cultures of sputum and bronchial washings grew Klebsiella pneumonia, van- Introduction: Henna painting or temporary Henna tattooing traditionally
comycin resistant enterococcus, candida, HSV1 and he was placed on appro- known as “Mehndi” is a custom used for centuries in the eastern world for bridal
priate antibiotics. Stool studies were positive for C. difficile and he was con- parties or other celebratory occasions. The dyeing agent is Hennotannic acid
tinued on oral vancomycin. Patient developed transient eosinophilia that was and very rarely leads to an allergic reaction or an adverse skin hypersensitiza-
initially attributed to underlying infection. Eventually, tracheotomy was per- tion. Nevertheless Henna tattoos or painting are usually mixed with para-
formed and patient was placed on chronic mechanical ventilation. After com- phenylenediamine [PPD] to assist with drying as well as darkening the color
pletion of antibiotics, he continued to exhibit leukocytosis and eosinophilia, hence beautifying the different patterns of Henna art. Methods: A 21 year old
chest infiltrates remained stable, and his diarrhea had not resolved despite con- girl with history of allergic rhinitis on Allergen Immunotherapy presents for
tinued vancomycin treatment. Strongyloides titer tested normal so further infec- her weekly allergy shot and complains that 6 weeks ago she attended a bridal
tive workup was pursued revealing sinusitis, otitis media, and candida cystitis. shower for one of her friends and along with another 6 girls in the same age
Despite receiving appropriate treatments, leukocytosis and diarrhea persisted. range had Henna tattoos painted on their hands and feet. She noticed that a
Stool was tested for ova and parasites and results were positive for Strongy- week later after placement it started to itch, burn and started to swell only at
loides stercoralis. After receiving 3 doses of invermectin, his diarrhea and the site of the tattoo. She immediately applied itch cream and 1% Hydrocorti-
encephalopathy resolved and he was able to be weaned completely off venti- sone with no resolution. She did not seek any professional medical care hop-
lator. Immunodeficiency evaluation revealed elevated IgE levels, low IgM ing it would resolve on its own. Henna tattoos usually dissipate by themselves
levels, and normal IgG and IgA levels. Hyperinfection with Strongyloides ster- on their own in 2 weeks. This case is clearly abnormal since the swelling and
coralis is generally seen in immunocompromised hosts with prolonged steroid coloring is still very distinct at 6 weeks out from application. Upon a serende-
therapy, acquired immune deficiency, malignancy, or chronic illness. Since pity consultation in the Allergy shot room she was given high dose topical cor-
the disseminated infection has a high mortality rate, it is imperative to recog- ticosteroid plus dimethicone and wrapping at the site with periodic ice com-
nize the disease and offer early treatment. Ivermectin is the treatment of choice. presses for comfort. No blisters or other adverse events occured and the lesion
This nematode primarily affects the gastrointestinal system and the lungs, but dissipated in 10 days with treatment. Conclusion: Henna is a potent contact
may rarely manifest in the central nervous system as mycotic aneurysm, intracra- dermatitis agent and must be skin tested or patch tested prior to application. It
nial hemorrhages, or vasculitis. Primary selective Ig M deficiency is a rare form contains paraphenyldiamine that can be a significant trigger. Recommenda-
of the immune disorder associated with severe life threatening infections and tions are to patch test this agent prior to use and if the Henna artwork does not
severe allergic reactions. Intravenous immunoglobulin is the only treatment dissipate in 2 weeks to see your local allergist or dermatologist for relief and
modality available without clear benefits. resolution.
A74 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A75
ABSTRACTS: POSTER SESSIONS
noses. Cerebrospinal fluid (CSF) leak could be classified as traumatic and non-
traumatic causes, it’s considered idiopathic when no cause is identified, and
benign conditions of elevated intracranial pressure are ruled out. The cardinal
clinical presentation is persistent rinorraquia confirmed by cytology/cyto-
chemical detection of CSF or ß2-transferrin as part of the diagnostic approach.
Case Report: Female of 52 years old with 1 year of evolution with hyaline ante-
rior rhinorrhea, persistent nasal pruritus, without identificable pattern of pres-
entation, coughing and wheezing exacerbated with the intake of ASA; spirom-
etry with bronchodilator reversibility of 14%, partial response to conventional
therapy for persistent rhinorrhea, no trauma history, CT scan of nose and
paranasal sinuses showed soft tissue density in entire left maxillary sinus, with
concommitant occupation of anterior left ethmoid cells in intimate contact with
cribriform plate. Cytochemical and cytological study confirms the presence
of CSF. As intraoperative finding concommitant maxillary chronic rhinosi-
nusitis were identified due to sinonasal polyposis, after endoscopic closure of
CSF leak total control of symptoms were achieved. Discussion: AERD is a per-
sistent inflammation condition of nasal mucosa, that has been linked to asthma
exacerbations, sometimes sinonasal polyps are not evident clinically or endo-
scopically, its important to assess the specific anatomy of patients with sub-
optimal control sino-nasal symptoms. The non-traumatic CSF leak is one of
the differential diagnoses that should be considered in patients with persistent
rhinorrhea.
Contact Dermatitis due to Henna Tatoo Six weeks from Application
P177
GRANULOMATOUS DISEASE ASSOCIATED WITH IMMUNOD-
EFICIENCY.
D. Shah*, T. Truong, Denver, CO.
Introduction: Granulomatous disease is a well-documented complication
of Common Variable Immunodeficiency, primarily seen in lung, but can also
involve skin, liver, spleen, and the GI tract. Autoimmune and lymphoprolifer-
ative disorders are common associations. We present a case of unexplained
granuloma involvement of skin and bone marrow in the setting of selective anti-
body deficiency and MGUS. Case Report: A 56 year-old man with history of
vitiligo, shingles, and pneumonia presented with a 9-year history of chronic Sinus CT Scan. Box: Polyps in Left Maxillary Sinus; Arrow: cerebrospinal
leg ulceration after falling on a boat anchor. Vascular work-up was negative. fluid fistula, Oval: Fluid-Air Level suggestive of Chronic Rhinosinusitis
Lesions were recurrent despite wound care, antibiotics for secondary infections
and hyperbaric oxygen, but were prednisone responsive. Exam showed numer-
ous pustular ulcers on legs and was otherwise normal. Studies for HIV, hepa- P179
titis, cryogloblulins, ANA, RF, anti-SSA, anti-SSB, and ACEI were negative. SUCCESSFUL APPROACH TO A PATIENT WITH MULTIPLE
MRI was negative for osteomyelitis. Multiple ulcer biopsies showed extensive DRUG REACTIONS (INCLUDING SERUM SICKNESS) TO RIT-
granulomatous process with no vasculitis. Bacterial, fungal and mycobacter- UXIMAB.
ial cultures were negative. Immune evaluation showed low IgA and IgM and J.K. Kim*1, S. Deol2, C. Wysocki2, D.A. Khan3, 1. Dallas, IL; 2. Dallas,
high IgG levels. SPEP/IFE was positive for IgG lambda monoclonal protein.
TX; 3. Grapevine, TX.
Antibody titers to H. Influenzae, diphtheria, and tetanus were normal. Strep-
tococcus titers were low despite repeated vaccination with Pneumococcal and Introduction: We report a case of a patient with 3 mechanistically different
Prevnar vaccines. Lymphocyte subsets showed low lymphocytes and NK cells reactions to rituximab and a successful management approach. Methods: Case
and stimulation was low with PHA and tetanus. IL-1 and IFN-gamma responses report Results: A 30 year old male with steroid-dependent oral pemphigus
were low. Complement levels, toll-like receptor, and IL-12 receptor assay were vulgaris developed subjective chest and throat tightness, hoarseness, and dif-
normal. CT chest did not show any ILD or lymphadenopathy, including medi- ficulty breathing 1 hour after his first rituximab infusion at an outside facility,
astinal. Subsequent work-up for myeloma revealed normal bone scan and flow which resolved within 15 minutes of stopping the infusion and treatment with
cytometry. However, bone marrow biopsy revealed numerous non-caseating intramuscular (IM) epinephrine. He was evaluated by us 2 years later for rit-
granulomas and 15 % plasma cells with normal cytogenetic studies and nega- uximab desensitization. Based on his symptoms, we considered the possibil-
tive cultures for bacteria, fungus, AFB and mycobacteria. Patient responded to ity of drug-induced vocal cord dysfunction, and he received his rituximab
treatment with prolonged steroids and IVIG for selective antibody deficiency. dose after premedication with H1/H2 antagonists and oral corticosteroids with-
Trial off IVIG after six months resulted in increased sinus and wound infec- out any initial reactions. Eleven days later, he noted a pruritic, red facial and
tions and thus was resumed. Conclusion: Diminished cellular responses with truncal rash along with severe joint pain which he self-treated by increasing his
IL-1 and IFN-gamma have been implicated in host defenses against mycobac- daily steroid dose. Serum sickness-like reaction was diagnosed, and he was rec-
terium; however numerous biopsy cultures in this case were unrevealing. Fur- ommended to receive high-dose corticosteroids post-infusion. He developed
ther studies are needed to elucidate the underlying etiology of granulomatous objective tongue, soft palate, lip, and facial swelling; pruritus; and throat tight-
disease in immunodeficiency states. ness within 30 minutes of his next dose, which resolved over 1 hour with stop-
ping the infusion and treatment with IM epinephrine, IV methylprednisolon,
and diphenhydramine. Due to the immediacy of the visible angioedema, an
P178 IgE-mediated reaction was diagnosed. He underwent a 17 step rapid desensi-
tization protocol to rituximab. The infusion was briefly halted at step 11 (32.5
ASPIRIN EXACERBATED RESPIRATORY DISEASE (AERD) AND
CEREBROSPINAL FLUID RHINORRHEA: CASE REPORT. cc/hr at 4mg/ml) after he experienced subjective chest tightness. It was restarted
30 minutes later at 20 cc/hr when the patient noted subjective lip edema and
D.A. Carino Cartagena*, A.A. Velasco-Medina, J.C. Fernandez de palmar pruritus without objective evidence of rash, angioedema, or wheezing.
Cordova-Aguirre, M.E. Arroyo-Cruz, S. Gonzalez-Flores, G. Velazquez- He was treated with IV diphenhydramine and lorazepam with improvement of
Samano, Mexico City, DF, Mexico. symptoms. At a maintenance dose of 20 cc/hr, he developed 2 urticarial episodes
Introduction: Aspirin-exacerbated respiratory disease (AERD) usually join that resolved with IM epinephrine, antihistamines, and montelukast. After desen-
sinonasal polyposis and bronchial asthma exacerbated by ASA. Given the per- sitization, he completed 10 days of prednisone 60 mg with no recurrence of
sistence of symptoms like rhinorrea is important to consider differential diag- the serum sickness-like reaction. Conclusions: Allergists should be familiar
VOLUME 113, NOVEMBER, 2014 A75
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A76
ABSTRACTS: POSTER SESSIONS
with the various adverse reactions to rituximab. This case illustrates a patient likely secondary to autoantibodies against C1-INH that are produced by aber-
with multiple reactions (including serum sickness) who successfully received rant plasma cells. Mechanistically, it is believed that autoantibodies bind to and
rituximab via desensitization and post-infusion corticosteroid therapy. destabilize the C1-INH complex, leading to proteolytic cleavage and inactiva-
tion of C1-INH and downstream generation of bradykinin. Conclusion: To our
knowledge, this is the first reported case of AAE due to MM. This case high-
P180 lights the principle that the management of AAE requires treatment of its under-
AN UNUSUAL CASE OF RECURRENT ABDOMINAL PAIN SIM- lying cause, which may be an autoimmune disorder or a malignancy.
ULATING ANGIOEDEMA.
L. Rampur, A. Rubinstein, Z. Ren*, Bronx, NY.
Introduction: Recurrent abdominal pain is frequent in patients with hered-
P182
FATAL ASEPTIC MENINGITIS DUE TO COXSACKIE B3 VIRUS
itary and acquired angioedema. We present a case of recurrent abdominal pain
INFECTION IN A PATIENT WITH ACQUIRED HYPOGAMMA-
presumed to have abdominal angioedema, found to have eosinophilic segmental
serosal and muscular enteritis. Methods: Case description Results: 31 year GLOBULINEMIA.
female was referred for episodic abdominal pain since 2007, recurring every T.V. Palacios*, M. Lawrence, L. Borish, Charlottesville, VA.
3 to 6 months lasting several days. She was presumed to have abdominal vis- Introduction: Human enteroviral infections are the most common cause of
ceral angioedema in 2009 treated with systemic steroids with relief of symp- meningoencephalitis in the United States. Enteroviral infection is usually a self-
toms within 2-3 days. MRI during several episodes was consistent with local- limited disease. However, in an immunocompromised patient, infections can
ized Jejunal wall edema in the same 5-6” segment. Lab work at baseline and be fatal. We present a case of an adult female patient with a history of Evan’s
during attacks revealed normal C1 esterase inhibitor function of 102%, nor- syndrome treated with prior splenectomy and rituximab who subsequently
mal C4 (20mg/dl), C3 (97mg/dl), Tryptase (5.9 ug/L), autoimmune antibody developed panhypogammaglobulinemia after which, despite receiving antibody
panel, Celiac panel, alpha 1 anti-trypsin and quantitative immunoglobulin assay replacement, she developed a progressive and ultimately fatal meningoen-
including ESR, electrolytes, liver and renal function and stool examination. But cephalitis due to human Coxsackie B3 virus. Case Description: A 28-year-old
C1q level was low (< 1.2 ugeq/ml). Absolute Eosinophil count was1400k/ul white female presented to the University of Virginia with a 4-month history of
(15%) when she was asymptomatic and as high as 3500k/ul (33%) during an progressive encephalopathy. She had a history of Evan’s Syndrome (autoim-
episode. IL-5 levels were normal. FISH analysis did not detect translocations mune hemolytic anemia and idiopathic thrombocytopenia purpura) for which
or deletions of the chromosome 4q12 resulting fusion of FIP1L1 and PDGFRA she had received treatment with rituximab and splenectomy 5 years prior to
genes and rearrangement of PDGFRB and FGFR1. Peripheral blood did not presentation. 5 months previously, she was hospitalized for Influenza A with
show a mutation for JAK2 V617F myeloproliferative disorder and and molec- concurrent facial Pseudomonas cellulitis and bacteremia. During that admis-
ular analysis showed normal alleles detected RT-PCR for BCR-ABL P210. Mul- sion, she was found to have severe panhypogammaglobulinemia with 0% cir-
tiple upper endoscopies and colonoscopies including capsule endoscopy have culating CD19+ B cells and intravenous immunoglobulin (IVIG) was started.
been unremarkable. In a recent admission a MRI showed further spread of the Her exam on admission was also consistent with aseptic meningitis. She was
jejunal thickening to around 10”. A laparoscopic jejunal biopsy of the edema- subsequently readmitted with worsening encephalopathy and repeat lumbar
tous region showed dense serosal and muscularis propria eosinophil infiltrates puncture and MRI were negative for an infectious process. A stereotactic brain
suggestive of eosinophilic enteritis, not involving the jejunal mucosa. Conclu- biopsy was obtained, which was also negative for infection. Despite empiric
sion: This patient’s presentation of recurrent abdominal pain with localized treatment with broad-spectrum antibiotics, she continued to decline neu-
jejunal wall edema was suggestive of abdominal angioedema attacks. Work up rocognitively and hospice care was pursued. The patient expired and subse-
for hereditary or autoimmune angioedema was negative. The only clue for the quent post-mortem brain biopsy identified human Coxsackie virus B3, on the
diagnosis was the fluctuating peripheral eosinophilia albeit with absence of basis of positive viral protein (VP)2, VP4 and VP 5` untranslated region (UTR)
increased eosinophil infiltrates in mucosal jejunal biopsies. Hyper eosinophilic by PCR. Conclusion: Previous treatment of this patient with rituximab for Evan’s
syndrome was excluded by the absence of the relevant mutations in syndrome was associated with persistent profound B cell lymphopenia and sec-
FIP1L1/PDGRA. Diagnosis was obtained by serosal and muscularis biopsy of ondary hypogammaglobulinemia. Given the observation that some patients
the edematous jejunal segment. treated with rituximab will develop persistent lymphopenia and hypogamma-
globulinemia, and the increasing use of rituximab in the treatment of malig-
nancies and autoimmune disorders, physicians must have increased awareness
P181 of the risk of secondary B cell and antibody deficiency and susceptibility to
A CASE OF MULTIPLE MYELOMA MANIFESTING AS LIFE- enteroviral meningeal infections in this population.
THREATENING ANGIOEDEMA.
S. Bose*, D. Nayak, C. Saltoun, Chicago, IL.
Introduction: A deficiency in C1 esterase inhibitor (C1-INH) can be caused
P183
PREVENTION OF KOUNIS SYNDROME EPISODES USING A
by hereditary angioedema (HAE) or acquired angioedema (AAE). HAE occurs
from a gene mutation that leads to either lack of C1-INH or production of non- COMBINATION OF KETOTIFEN AND NON-SEDATING ANTI-
functional C1-INH. AAE results from consumption or inactivation of C1-INH, HISTAMINES.
usually in the setting of lymphoproliferative disorders. Several cases of AAE J. McCracken*1, C. Schlegel2, S. Sur2, 1. League City, TX; 2. Galveston,
have been reported in conjunction with monoclonal gammopathy of undeter- TX.
mined significance (MGUS) and non-Hodgkin’s lymphoma. We report a rare Introduction: Kounis syndrome is a rare condition when allergy or hyper-
case of a patient, who presented with AAE, leading to a diagnosis of multiple sensitivity can lead to cardiovascular symptoms. Symptoms are caused by the
myeloma (MM). Case: A 70-year-old male with asthma and chronic idiopathic release of inflammatory mediators from mast cells which can have cardiovas-
urticaria presented to the ED with tongue and right anterior neck swelling with- cular effects including coronary spasm. Methods: We report the case of a 61
out urticaria. Because his uvula could not be visualized on presentation, he was year old male with a history of allergic rhinitis, asthma, monoclonal gam-
intubated. The patient’s admission laboratory results were indicative of anemia, mopathy of undetermined significance (MGUS) and eosinophilic esophagitis
acute kidney injury and hypercalcemia. They also showed an increased glob- who was referred to us for evaluation of urticaria, chest pain and shortness of
ulin gap, an elevated serum IgG level, high serum free lambda light chains and breath (SOB). His symptoms have been occurring over the past 2.5 years and
a low C4. The patient’s presentation was concerning for AAE due to an under- rash typically precedes the cardiac symptoms. Six months prior to his first visit
lying malignancy. His angioedema did not improve approximately 12 hours in our clinic, he had an acute myocardial infarction requiring stent placement.
after administration of intravenous steroids in the ED. The patient received 1 Physical exam was normal. Laboratory work-up was significant for elevated
dose of C1-INH concentrate and within a few hours his angioedema rapidly eosinophils, elevated IgE, and intermittently elevated tryptase with these
regressed. C1-INH and C1-INH functional levels were normal, but the C1q episodes. Skin prick testing was positive for trees, weeds, grass, dust mite, cock-
level was found to be low, suggestive of AAE. A bone marrow biopsy revealed roach, and cat. Bone marrow biopsy was c-kit negative. He was started on fex-
~35% plasma cells, consistent with a diagnosis of MM. The patient’s ofenadine 180 mg in the morning, cetirizine 10 mg in the evening, and keto-
angioedema resolved after administration of C1-INH concentrate and initia- tifen 1 mg twice a day. Two weeks later, he again had chest and jaw pain
tion of treatment for his MM. Discussion: The most common malignancies associated with development of a rash on his palms that required hospitaliza-
known to cause AAE are indolent lymphomas. However, we report a unique tion. Angiography showed patent stent. His medications were increased to fex-
case of MM manifesting as AAE. The patient in our case suffered from AAE ofenadine 180 mg 2 tabs in AM, cetirizine 10 mg 2 tabs in PM and ketotifen
A76 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A77
ABSTRACTS: POSTER SESSIONS
2 mg twice a day. He was unable to tolerate the increased doses of fexofena- deaminase (ADA), purine nucleoside phosphorylase (PNP), DNA ligase 4,
dine and cetirizine so he resumed his initial dosing of those medications. He TAC1, BTK, and 22q11 deletion studies were negative and telomeres were
now reports symptoms improved since last follow-up. Discussion: We believe not consistent with dyskeratosis congenita. Thymus was identified on ultra-
his presentation of urticaria associated with severe chest pain and SOB is sug- sound. Conclusion: Early detection of T cell lymphopenia has led to early treat-
gestive of Kounis syndrome. Current literature focuses more on the acute treat- ment and improved prognosis of severe combined immune deficiency. We pres-
ment of the allergic and cardiac symptoms, and less on the prevention of symp- ent a case of T and B lymphopenia and IgM and IgA deficiency of unclear
toms. In this patient, ketotifen, a mast cell stabilizer, and non-sedating etiology to date. Further studies including whole exome sequencing may reveal
antihistamines were utilized to control symptoms. Conclusion: We present a the etiology.
case of possible Kounis syndrome in a patient who is successfully being treated
with non-sedating antihistamines and ketotifen. This reports to the allergists
that this combination therapy can be a useful management option when treat- P186
ing patients with Kounis syndrome. PROLACTINOMA MIMICKING REFRACTORY RHINITIS.
M.S. Motosue*, Rochester, MN.
A 24 year old male presented to the allergy clinic with a four month his-
P184 tory of persistent clear left nasal drainage. Patient denied any history of facial
RECURRENT PERIOPERATIVE ANAPHYLAXIS IN A 24 YEAR
trauma, facial surgery, nasal polyps, or nasal deviation. Beyond the rhinor-
OLD FEMALE WITH UNTREATED ASTHMA. rhea, the review of systems was otherwise negative. Prior to presenting to allergy
J. Kannan, J. Bernstein*, Cincinnati, OH. clinic, the patient was seen by his primary care physician and was on daily cet-
Introduction: Perioperative anaphylaxis is a life threatening IgE or non-IgE irizine, montelukast, and fluticasone nasal spray without any symptom improve-
mediated condition presenting with symptoms including urticaria, angioedema, ment. Given the persistent unilateral rhinorrhea without history of trauma or
bronchospasm, arrhythmias, and hypotension.1 Its prevalence has been reported surgery, further diagnostic workup was pursued. Computed tomography sinus
from 1:3,500 to 1:20,000 with a mortality rate of 3 to 9%. The most common imaging revealed a 6.5 x 5.6 x 4.4 cm infiltrative, destructive mass centered in
culprits include antibiotics, neuromuscular blocking agents, latex, hypnotics, the sella turcica with intracranial nasopharyngeal extension which was subse-
opioids, colloids, dyes, and nonsteroidal anti-inflammatory medications. Case quently confirmed by MRI. Laboratory results were remarkable for a positive
Description: The patient was a 24 year old female with a history of asthma, beta-2 transferrin and an elevated prolactin (532, normal range 3-13 ng/mL).
rhinitis, egg allergy, eczema, and prior tonsillectomy who presented after two An endoscopic left nasopharyngeal biopsy was performed with pathology con-
episodes of anaphylaxis while undergoing oral jaw surgery. During the first sistent with an atypical pituitary adenoma. The staining profile of the ade-
surgery she developed hypotension, wheezing, and hypoxia leading to car- noma was of a prolactinoma. The patient subsequently underwent neurosurgery
diopulmonary arrest. She was treated with epinephrine, fluids, and corticos- for repair of the CSF leak followed by treatment with cabergoline. Conclu-
teroids. Skin prick testing was found positive to vecuronium, succinylcholine, sion:Nasal symptoms such as rhinorrhea are commonly encountered in both
rocuronium, cisatracurium, penicillin, sulfa, ciprofloxacin, and cefazolin. These the allergy and primary care clinics. Frequently, these symptoms are related to
agents were avoided during the next operation, but systemic symptoms recurred. inflammatory conditions such as sinusitis, rhinitis, and nasal polyps. How-
Further evaluation showed a normal FEV1 with 14% reversibility post bron- ever, rarely they may be related to malignant lesions. Red flags of a unilateral
chodilator and an exhaled nitric oxide (eNO) of 52ppb indicative of airway distribution along with a refractory response to standard medical treatment
inflammation. Urine tryptase and thyroid stimulating hormone (TSH) were nor- should prompt the physician to examine for other differentials including sinus
mal. She was started on an inhaled corticosteroid. Twenty four hours prior to masses.
her third surgery she was treated with corticosteroids and antihistamines, and
neuromuscular blocking agents and beta blockers were avoided. She tolerated
her subsequent surgeries without complication. Discussion: This case illus-
trates the serious nature of perioperative anaphylaxis. Despite avoidance of
the sensitized agents, anaphylaxis reoccurred. This led to further exploration
discovering poorly controlled asthma which is a known risk factor for ana-
phylaxis.2
P185
LYMPHOPENIA AND AGAMMAGLOBULINEMIA OF UNCLEAR
ETIOLOGY.
L. Bornstein*, R. Herzog, New York, NY.
Introduction: Early diagnosis of severe combined immune deficiency has
led to timely treatment and improved prognosis for patients. We present a 17
month old male with lymphopenia and agammaglobulinemia of unclear etiol-
ogy identified by TREC assay on newborn screen. Case Report: The patient
was a full term newborn with low T-cell receptor excision circle (TREC) lev-
els. The patient was well until 53 days of age, when he developed fever to 38.5C
and upper respiratory infection symptoms. Labs revealed low T and B cell
counts and agammaglobulinemia, and he was treated with antibiotics and intra-
venous gamma globulin (IGIV). Cultures and viral PCR were negative. There-
after, the patient developed recurrent otitis media and viral infections due to
RSV, coronavirus, rhinovirus, enterovirus, and metapneumovirus. In addition
to IGIV, the patient has been given prophylaxis with palivizumab, acyclovir,
pentamidine (due to intermittent neutropenia on TMP-SMX), and filgrastim
as needed. The patient has been developing normally for his age. Results: New-
born TREC was 132, 132, 164 (nl>200/ml), with repeat of 0, 0, 0, 31, 33/ml.
Naïve CD45RA+ CD4 count was normal. Absolute lymphocyte count (ALC)
was 900/ml (1,000-4,800), CD4+CD3+ 468/mm, 48% (2,780-3,908, 50-57%), MRI demonstrating a infiltrating mass in the sella turcica with biopsy and
CD8+CD3+ 127/mm, 13% (351-2,479, 8-31%), CD19+ 63/mm, 7% (432- pathology consistent with a prolactinoma.
3,345, 11-45%), normal NK function, IgG 522, IgA: <7, IgM 9 (20-87 mg/dl).
T cell proliferative response to phytohemagglutinin (PHA), Concanavalin (con
A), OKT3, and mixed lymphocyte culture was normal. Responses to Candida
and Tetanus were low normal. There was no evidence of maternal engraftment
or clonal T or B cells. Immunization with DTaP did not result in increased titers.
Anti-neutrophil antibodies were negative. Artemis, RAG1, RAG2, adenosine
VOLUME 113, NOVEMBER, 2014 A77
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A78
ABSTRACTS: POSTER SESSIONS
used to eradicate the inhibitor in some patients. As B-cells recover, the inhibitor
P187 may reappear in selected patients, and maintenance rituximab may need to be
CASE OF HYPOGAMMAGLOBULINEMIA FOLLOWING RIT-
considered.
UXIMAB THERAPY.
M. Egan*, C. Cunningham-Rundles, New York, NY.
Rituximab is a B cell depleting anti-CD20 monoclonal antibody often used P189
in the setting of malignancy or autoimmune conditions. Transient B cell deple- A COMMON SKIN ERUPTION WITH AN UNCOMMON CAUSE.
tion is often seen but immunoglobulin levels are not often affected 1. However, J.T. Abraham*, J. Fernandez, Cleveland, OH.
there is growing literature documenting hypogammaglobulinemia requiring
Background: Autoimmune Progesterone Dermatitis is an IgE mediated reac-
intravenous immunoglobulin following rituximab therapy1,2. In some cases, the
tion to endogenous or exogenous progesterone. Clinical presentations are
presentation of hypogammaglobulinemia was years after completion of ritux-
described as varied, with cutaneous lesions mostly on abdomen and lower
imab therapy3. We present the case of a 71 year old female with a history
extremities. The rash occurs cyclically, typically during the luteal phase of the
microvascular polyangiitis treated with rituximab, cyclophosphamide and pred-
menstrual cycle when progesterone levels are high. Methods: A 28 year-old
nisone who was diagnosed hypogammaglobulinemia, specifically IgG defi-
healthy Caucasian female presents to Allergy and Immunology clinic with inter-
ciency, two years after completing therapy. The patient had a history of recur-
mittent lower extremity and abdominal rash since May 2013. The erythema-
rent pneumonias preceding the immune modulating regiment, however all
tous maculopapular rash occurred every 4-6 weeks initially, then increased in
episodes required only outpatient antibiotic therapy. After completion of treat-
frequency. It normally lasted three days and self-resolved. The rash progres-
ment the patient required frequent inpatient admissions for pulmonary infec-
sively became associated with myalgias and malaise. She had been using a
tions, including three to the intensive care unit. Subsequent evaluation revealed
NuvaRing for contraception during this time. Results: The patient was initially
an IgG of 412 mg/dL, IgM of 31mg/dL and IgA level of 129 mg/dL. She had
evaluated by rheumatology with concern for the rash being consistent with vas-
an appropriate antibody response to pneumococcal polysaccharide vaccine with
culitis. Skin biopsy was performed, demonstrating perivascular dermatitis with
11 of 23 titers positive. B cells were present in normal numbers. Thus, a diag-
eosinophils and neutrophils as well as extravasation. Laboratory evaluation was
nosis of IgG deficiency was made4,5. She was started in intravenous
remarkable for elevated IgG levels (2960 mg/dL), a speckled pattern ANA
immunoglobulin therapy and has been well since initiation of treatment. This
(1:1280), positive SSA (122 units) and SSB (75 units) antibodies. She was sent
patient adds to the cases in the literature of hypogammaglobulinemia requir-
to Allergy and Immunology for evaluation due to the cyclical nature of her rash
ing immunoglobulin therapy after rituximab treatment. In our patient the
and concurrent use of hormonal contraception. Epicutaneous and intradermal
immunoglobulin levels prior to initiation of therapy are not available so it is
skin testing was performed with progesterone (50mg/ml) as well as positive
not known if treatment accelerated an already existing condition or represents
(histamine) and negative (normal saline) controls. Epicutaneous testing with
a truly new illness following therapy. There are case reports of clinically asymp-
1:1 concentration was negative. Intradermal injection of 1:1000 and 1:100 dilu-
tomatic patients with reduced immunoglobulin prior to rituximab treatment
tions showed positive wheal/flare reactions of 5mm x 12mm and 8mm x 15mm,
that experienced clinical deterioration after therapy1. It is possible a similar sce-
respectively. Intradermal injections were also placed in three healthy subjects
nario occurred in our patient given the history of frequent, though milder, infec-
to ensure the dilutions used were not irritant doses. The healthy controls showed
tions prior to therapy. Retrospective studies have shown that only a small minor-
minimal to no reaction to these dilutions. Conclusions: Autoimmune Proges-
ity of patients develop hypogammaglobulinemia following rituximab therapy
terone Dermatitis is a rare condition, however it should be considered in women
indicating there is likely a specific subset of patients at risk6. More research is
of child bearing age who present with cutaneous lesions in a cyclic pattern.
needed to determine if this association is due to an aggravation of an existing
condition and the utility of screening.
P188
USE OF RITUXIMAB IN HEMOPHILIA B PATIENTS WITH ANA-
PHYLAXIS AND FACTOR IX INHIBITOR.
J. Kiehm*1, N. Qamar2, S. Acharya3, B. Kaplan1, 1. Great Neck, NY;
2. Manhasset, NY; 3. New Hyde Park, NY.
Introduction: The development of Factor IX (FIXi) inhibitor (antibodies)
in severe Hemophilia B (FIX deficiency) patients is a rare phenomenon (1%-
6% incidence), increasing morbidity and mortality. Treatment of these patients
can be complicated by the association of FIX inhibitor (FIXi) with anaphylaxis
to FIX replacement therapy. More recently, the use of rituximab to eradicate
inhibitors has been reported. Methods: We describe two Hemophilia B patients
(Pt#1-8 year old and Pt#2-4 year old males) who developed anaphylaxis to
recombinant FIX replacement product, BeneFIX (RFIX), in the setting of an
inhibitor. Results: After 9 months of RFIX therapy for the treatment and pre-
vention of bleeding episodes, Pt#1 developed anaphylaxis shortly after RFIX
infusion. FIXi titer was 4.3 BU. Pt#2 was receiving RFIX therapy that was dis-
continued due to detection of a FIXi of 0.6 BU on routine screening. After his
inhibitor titer became undetectable, he was re-challenged with RFIX. He devel-
oped an anaphylactic reaction after 5 weeks of RFIX therapy. FIXi was 2.4
BU. Skin testing to RFIX and plasma derived FIX, Mononine (PFIX), was
performed for both patients. Pt#1’s skin test was negative to RFIX but positive P190
to PFIX. Pt#2’s skin test was negative to both products. The patients were treated IGE MEDIATED ALLERGIC REACTION TO METHIMAZOLE IN
with rituximab 375mg/m2/dose weekly x 4 and successfully completed desen- A PEDIATRIC PATIENT WITH SUBSEQUENT SUCCESSFUL
sitization to RFIX. Pt#1’s FIXi decreased to 0, and he has been tolerating RFIX DESENSITIZATION.
with no resurgence of his inhibitor for 9 months thus far. Pt#2’s FIXi and B- E. Akl*, B. Ward, A. Kumar, W. Zhao, Richmond, VA.
cells dropped from 6.3 BU to 0 and 603 cells/uL to 0 respectively. After 6 months
Introduction: Methimazole is a common reagent used to treat hyperthy-
of tolerance, Pt#2 developed diffuse urticaria and dyspnea within minutes of
roidism. Its side effects such as rash, vasculitis, have been widely reported but
completing his RFIX infusion. FIXi was 0.8 BU, and B-cells were 270 cells/uL.
rarely has an IgE mediated reaction been reported in a child and no desensiti-
Repeat skin testing was minimally positive to RFIX and negative to PFIX. Sub-
zation protocol exists for this medication. We present a case of IgE mediated
sequently, patient failed graded challenge to PFIX (generalized hives). Con-
allergic reaction after administration of methimazole on two occasions along
clusion: These cases highlight the importance of recognizing that an inhibitor
with a successful desensitization to the medication with subsequent treatment
can play a role in anaphylaxis to biologic agents. Skin testing to FIX prepara-
of hyperthyroidism. Case Description: A 7 year old Hispanic female with a his-
tions is not necessarily predictive of systemic reaction. Rituximab has been
tory of intermittent asthma and hyperthyroidism treated with methimazole
A78 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A79
ABSTRACTS: POSTER SESSIONS
and developped a generalized itchy rash and hives with myalgias and arthral- markable and there was no swelling or edema noted. A rapid strep test was
gias. Her symptoms resolved within 1 day after stopping the medication. She performed. Approximately 30 minutes passed and on reexamination the uvula
was then switched to propylthiouracil (PTU) and had no issues. Another trial was noted to be edematous. The patient then began to have progressive palatal
of methimazole lead to the same symptoms and the patient was again switched edema that involved the entire posterior oropharynx. The patient had no respi-
to PTU which result in elevated liver enzyme within a few months. The patient ratory distress and continued to have stable vital signs, however the decision
presented to our allergy clinic for evaluation. Skin prick testing showed a pos- was made to electively intubate him to protect his airway. C1 esterase inhibitor
itive reaction to methimazole at 100 mcg/ml concentration. Intradermal test- therapy was initiated at this time. On direct laryngoscopy, the patient’s palate
ing showed a 6 mm wheal to the 1 mcg/ml concentration. The starting dose of was noted to be edematous, however the glottis, trachea and larynx were all
desensitization was calculated to be 100 fold less than that which yielded a 5- normal. The patient remained intubated for less than 24 hours, was success-
8 mm wheal by skin testing. Patient was monitored in our clinic for possible fully extubated and discharged to home within 72 hours. Our case of an HAE
local and systemic reaction. Desensitization was started at a concentration of attack with isolated palatal edema after the rapid strep test was performed raised
10 ng/ml in a volume of 0.3 ml (dose of 3 ng) with no reaction. The dose was the unique question: did the rapid strep test incite enough trauma to the poste-
increased half log every 15 minuntes until a cumulative dose of 29.5 mg was rior oropharynx to provoke an attack of HAE? Our case suggests that the patient
reached. Our patient had no reactions during the desensitization and was started was at the beginning of an attack and the trauma of the rapid strep test may
on a dose of 5 mg daily and increased to therapeutic dose for her hyperthy- have caused him to have isolated angioedema to the posterior oropharynx.
roidism. Conclusion: Drug desensitization protocols exist for a few medica-
tions mainly beta lactam antibiotics, vancomycin, aspirin, NSAIDS and some
chemotherapy reagents and monoclonal antibodies. To our knowledge, no methi- P192
mazole desensitization case has been reported. Our report provides a useful A CURIOUS COUGH.
tool in treating hyperthyroism of patients with allergic reaction to methimazole C. Caruthers*, J. Vitale, M. Warrier, St. Louis, MO.
who are not tolerating PTU.
41-year-old female with past medical history of Gastroesophageal Reflux
(GERD) well-controlled on famotidine and obesity status post lap-band sur-
gery three years prior presented with a one year history of cough. Her cough
was intermittently productive of yellow (morning) to clear sputum (later in the
day) alternating with dry cough that was worse with exertion and associated
with wheezing and dyspnea. She had frequent nocturnal awakenings. She also
had perennial clear rhinorrhea with postnasal drip, nasal and ocular pruritus
and sneezing. Social history was notable for cat and dog at home and tobacco
use. Physical exam was unremarkable except for obesity, clear rhinorrhea, post-
nasal drainage and non-productive cough. Percutaneous skin testing was pos-
itive for cat and dog. Pulmonary function tests (PFTs), chest x-ray, and sinus
CT were normal. She was diagnosed with perennial allergic rhinitis, cough and
GERD. Initial treatment included environmental controls, a nasal steroid and
albuterol for rescue. She continued to have nocturnal rhinitis and a wet cough.
Pulmonary function tests progressively declined and demonstrated a positive
bronchodilator response. Management over the next few years included trials
of immunotherapy for cat and dog, high dose proton pump inhibitor, antibi-
otics, montelukast, steroids (nasal, inhaled and oral) and omalizumab. Cough
with frequent nocturnal awakenings continued to be her main complaint. GERD
was repeatedly assessed and reported to be well-controlled by the patient.
Approximately four years after initial presentation, chest CT and esopha-
gogastroduodenoscopy (EGD) were performed due to worsening of symp-
toms and oral steroid dependence. The CT showed a fluid distended thoracic
esophagus, and EGD revealed food in her esophagus despite being NPO the
night prior to the procedure. She recalled two episodes over the past several
months of coughing up food that she had eaten 24-48 hours earlier. It was sub-
sequently realized that her lap-band was inflated one to two years prior to the
initial onset of her symptoms. Her lap-band was deflated with dramatic improve-
Desensitization protocol ment in symptoms and PFTs. She was able to discontinue oral steroids and
maintenance asthma medications. There is one other report of chronic cough
and nocturnal rhinorrhea following lap-band surgery. Chronic cough is a com-
P191 plication of lap-band that may be under-recognized outside the general sur-
WAS TRAUMA THE CAUSE? A CASE OF HEREDITARY gery community.
ANGIOEDEMA.
M.B. Reddy*, Denver, CO.
A 15-year-old male with a history of hereditary angioedema (HAE) type 1
P193
presented to the local children’s hospital emergency department (ED) with a NON-TUBERCULOUS MYCOBACTERIA (NTM) INFECTION
chief complaint of 4 days of sore throat and abdominal pain. He had 7 prior PRESENTING AS DIFFICULT-TO-CONTROL ASTHMA.
admissions for HAE attacks, with 2 in the past year. His typical attacks included J.M. Rodrigues*, A. Katta, R. Nayak, R. Slavin, St Louis, MO.
angioedema of his feet and face, and occasionally abdominal pain. He was Introduction: Although NTM infection is known to exist in patients with
always treated with C1 esterase inhibitor. Preventative therapy had been dis- chronic lung diseases, it is seldom considered in the evaluation of severe or dif-
cussed at his prior allergy clinic visits, however he had been lost to follow-up ficult-to-control asthma. Case Report: A 66 year old woman was referred to
prior to this presentation. On his current presentation, the patient noted that the allergy clinic with difficult-to-control asthma. She had recurrent daytime
his abdominal pain was similar to prior flares, but denied any emesis, dysp- productive cough with yellow sputum and frequent nocturnal awakening. She
nea, or angioedema. He had multiple sick contacts at home with similar symp- described repeated use of short acting β agonist despite compliance with com-
toms. On exam, the patient had stable vital signs. He appeared to be in no bination (high dose) inhaled corticosteroids (ICS)/long acting β agonist and
acute distress. On HEENT examination he had clear tympanic membranes, leukotriene receptor antagonist. Pulmonary function tests were consistent with
PERRLA, clear oropharynx with 2+ tonsils with mild erythema and without severe obstructive ventilatory limitation. A High resolution chest CT scan
palatal, tongue, or uvula edema, moist mucous membranes, and supple neck. showed multiple bilateral pulmonary nodules. She had two positive sputum cul-
His lungs were clear to auscultation, and heart had regular rate and rhythm with- tures for Mycobacterium avium-intracellularae and was started on ethambutol,
out any murmurs. His abdominal examination was positive for mild tenderness rifabutin and azithromycin. She has had marked improvement in symptoms and
to palpation diffusely without rebound or guarding. His skin exam was unre- decrease in albuterol use since starting treatment. Discussion: A recent study
VOLUME 113, NOVEMBER, 2014 A79
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A80
ABSTRACTS: POSTER SESSIONS
showed that the estimated prevalence of NTM infections among asthmatic drome in response to azithromycin, so it was stopped. Symptoms progressed
patients was 1.7% with an average interval of 2 years from symptom change and he was seen in allergy/immunology clinic 1 day later where he was thought
to diagnosis. Patients commonly present with symptoms of worsening lung dis- to have herpetic stomatitis and was started on valaciclovir. Oral swab for HSV-
ease including progressive dyspnea, productive cough and frequent asthma 1/2 was sent. He was seen 2 days later when he had hives. He continued to
exacerbations. Imaging studies may reveal bronchiectasis, nodules < 5 mm or have oral mucositis with improving facial swelling. His HSV-1/2 PCR were
fibrosis. American Thoracic Society (ATS)/ Infectious Diseases Society of negative, so valaciclovir was stopped. Mycoplasma IgG and IgM were sent.
America (IDSA) guidelines require at least two positive expectorated sputum After consultation with dermatology, his mucositis, which was characterized
cultures for diagnosis of NTM infection. Recent studies have indicated that by extensive ulcerations covered with a pseudomembrane on the buccal mucosa,
older patients with severe airflow limitation receiving long term high dose labial mucosa, tongue, and palate as well as with bloody crusted lip ulcerations,
ICS are at a higher risk of acquiring NTM infection. The current recommended was determined to be diagnostic of oral EM. Positive Mycoplasma IgM and
treatment for pulmonary disease comprises a triple drug regimen with IgG titers confirmed the infection as the trigger for oral EM. He was treated
azithromycin, ethambutol and rifabutin for duration of at least 12 months after with topical and systemic steroids with rapid improvement. Conclusion: Oral
conversion of sputum to negative. It is imperative to consider NTM infection EM is a unique and much less described variant of EM. It is most often trig-
in the differential of difficult-to-control asthma that has been unresponsive to gered by HSV infections, less commonly by drug reactions, and rarely by
conventional therapy. Mycoplasma infection. Unlike acute herpetic stomatitis, which involves kera-
tinized mucosa and which can be confused with oral EM, our patient devel-
oped lesions only on nonkeratinized tissues. The triggers of oral EM and its
P194 characteristic presentation are important to recognize as repeated attacks often
AN EARLY PRESENTATION OF DRUG REACTION WITH result in more severe forms of EM involving both the oral mucosa and skin.
EOSINOPHILIA AND SYSTEMIC SYMPTOMS.
S. Waqar*1, S. Farzan2, 1. Dix Hills, NY; 2. Great Neck, NY.
Introduction: Drug Reaction with Eosinophilia and Systemic Symptoms
(DRESS) is a rare, but potentially life-threatening syndrome, which typically
presents two to eight weeks after drug exposure. It is characterized by multi-
ple system involvement, which may include skin eruption, hematologic abnor-
malities, lymphadenopathy, and affect internal organs such as the liver, kid-
neys, and lungs. Patients usually face several relapses despite discontinuation
of the drug. Here we describe the presentation, diagnosis, and clinical course
of a patient with early-onset DRESS. Methods: A 15-year-old male, with past
medical history of hypertension presents with recurrent pruritic rash and short-
ness of breath two weeks after treatment of a MRSA skin infection with
trimethoprim-sulfamethoxazole (TMP-SMX). He reports initial development
of a rash on day 4 of TMP-SMX. The rash was a full-body pruritic erythema-
tous papular rash sparing the mucus membranes and most prominent on the
face. TMP-SMX was discontinued. He was treated with an oral prednisone
taper, as well as intravenous fluids for acute kidney injury with a creatinine of
1.5. The rash resolved within two days but reappeared on day 6. He was read-
mitted approximately 10 days after initial TMP-SMX treatment with fever, rash,
and shortness of breath. On readmission, his physical exam was notable for
fever of 39.4 degrees C and a pruritic full-body morbilliform erythematous rash
including the palms and soles, and again sparing the mucus membranes. Results:
Laboratory work-up showed eosinophilia (1200 per microliter; 13.9%) with
an elevated C-reactive protein of 18.7. ESR, hepatitis panel, liver function tests,
Lyme screen, rapid plasma reagin were normal. HIV was non-reactive. EBV
P196
A SUCCESSFUL PRE-MEDICATION PROTOCOL FOR A
testing was consistent with a past infection. ANA, dsDNA, and histone anti-
PATIENT WITH ANAPHYLATOID REACTION TO INTRA-
bodies were normal. Chest X-ray revealed small bilateral pleural effusions. Uri-
nalysis, respiratory viral panel, throat culture and blood cultures were negative.
VENOUS RADIOCONTRAST MEDIA IN SPITE OF STANDARD
He was started on a very slow taper of prednisone for early-onset DRESS. On PRE-MEDICATION PROTOCOL.
follow-up, rash had not recurred and eosinophilia had resolved. Conclusion: M.H. Chong*, S.L. Mawhirt, J. Sher, M. Aquino, M. Davis-Lorton,
In patients with recurrent rash and multiple system involvement, DRESS should L. Fonacier, Mineola, NY.
be considered. Early-onset DRESS should be in the differential in cases con- Background: Immediate hypersensitivity reactions (IHR) to low osmolar
sistent with the syndrome but with presentation of symptoms earlier than radiocontrast media (RCM) have an overall reported incidence of up to 3%.
expected, and after exclusion of other etiologies. Pre-medication regimens reduce IHR rates in subsequent studies requiring
RCM. However, breakthrough IHR (BIHR) may occur despite the use of pre-
medication and low osmolar RCM. Consensus on successful pre-medication
P195 protocols for patients requiring RCM after BIHR is lacking. Case Report: A
DIAGNOSIS OF ORAL ERYTHEMA MULTIFORME IN A 50 year old male with a history of asthma presented for elective cardiac catheter-
PATIENT WITH MYCOPLASMA PNEUMONIA. ization for unstable angina. He reported one previous RCM reaction with sneez-
K.R. Brown*1, D. Eisen2, J. Li2, A. Assa’ad2, 1. Lakeside Park, KY; ing, hives, and ocular pruritis. Prior to catheterization, the patient received a
2. Cincinnati, OH. modified Greenberger pre-medication protocol with oral prednisone 50mg (13,
7, and 1 hr pre-procedure), oral diphenhydramine 50mg and methylprednisolone
Introduction: Erythema multiforme (EM) is an immune-mediated hyper-
125mg 1 hour pre-procedure. Despite pre-medication, the patient developed
sensitivity reaction typically presenting with cutaneous and mucous membrane
generalized urticaria, periorbital angioedema, nasal congestion, and wheezing
involvement. EM is known to be associated with exposure to drugs and viral
upon administration of a 3cc dose of low osmolar iohexol (640 mosm/kg). The
pathogens. The most commonly associated pathogen is herpes simplex virus
procedure was immediately terminated and albuterol, diphenhydramine, and
(HSV). However, there are reports of EM in patients diagnosed with
methylprednisolone were administered at that time and for two days post pro-
Mycoplasma pneumonia. We describe a case of oral EM, a distinct but less
cedure. As the patient still required catheterization, a subsequent pre-medica-
well-recognized variant of EM, presenting as isolated oral mucositis in a patient
tion protocol was implemented: prednisone 80mg daily, montelukast 10mg
with Mycoplasma pneumonia. Clinical Case: A 10 year old previously healthy
daily, cetirizine 10mg and famotidine 20mg twice daily for four days prior to
male presented to his pediatrician with fever, cough, and lip swelling. Crack-
the subsequent study. Additionally, he received methylprednisolone 125mg,
les were found on exam and he was prescribed azithromycin for treatment of
diphenhydramine 75mg, and albuterol 1 hour pre-procedure. The patient under-
atypical pneumonia. His facial swelling spread and he presented to the emer-
went second cardiac catheterization one week later with successful placement
gency department. He had buccal mucosal lesions with sloughing of oral mucous
of two drug-eluting stents using lower osmolar iodixanol (290 mosm/kg) with-
membranes without skin rash. There was concern for Stevens Johnson Syn-
A80 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A81
ABSTRACTS: POSTER SESSIONS
out any adverse effects. Discussion: Breakthrough IHR to RCM are reported was diagnosed with GPA and started on high dose steroids and cyclophos-
to occur at a rate of 0.11-18% and patients may experience symptoms compa- phamide. Relapses were treated with rituximab. Currently he has hemodialy-
rable to their index reaction. Successful pre-medication regimens to prevent sis dependent end stage renal disease, hypertension, dilatation of coronary
repeat BIHR in patients requiring utilization of RCM for subsequent imaging artery, pericardial effusion required pericardiocentesis, concentric left ven-
studies are not well documented. We describe a regimen which allowed our tricular hypertrophy, hypogammaglobinemia secondary to chemotherapy, on
patient to receive critical coronary intervention. Further investigation into effec- IVIG infusion, bilateral cataract secondary to chronic use of prednisone and
tive pre-medication in patients who successfully receive RCM may elucidate posterior reversible encephalopathy syndrome. Conclusion: GPA is extremely
optimal regimens which may be most beneficial. rare in children and aldolescents especially of African descendant. Attributing
symptoms of GPA to more common but less harmful disease processes, espe-
cially in areas of the world where it is less prevalent may occur. Earlier diag-
P197 nosis and treatment is extremely important in preventing permanent renal dam-
POST-INFUSION MYOCARDIAL INFARCTION IN A PATIENT age.
RECEIVING IVIG.
S. Draikiwicz*1, S. Arakali2, E. Capitle3, 1. Scotch Plains, NJ; 2. New
Brunswick, NJ; 3. Newark, NJ. P199
CASE REPORT: A PATIENT WITH ACQUIRED C1-INH DEFI-
Adverse reactions have been reported in up to twenty percent of all patients
CIENCY (ACID) AND HYPOGAMMAGLOBULINA.
receiving IVIG infusion.1 From October 1997 through July 2007, there were
10 reports of stroke, 6 reports of thrombosis, 4 reports of myocardial infarc- E. Schussler*, P. Busse, New York, NY.
tion, 2 reports of pulmonary embolus and 1 report of transient ischemic attack Introduction: Acquired angioedema with C1 inhibitor deficiency is a rare
suspected of being associated with IVIG.2 While multiple known factors such disease characterized by recurrent episodes of angioedema without urticaria or
as hypertension and diabetes contribute to the development of coronary artery pruritis. Attacks may be triggered by trauma, psychological stress, or infection,
disease and myocardial infarction (MI), it is also important to acknowledge but may also occur without an identifiable trigger. The etiology of ACID is
the association of IVIG and post-therapy myocardial infarction. Our case is a frequently due an underlying malignancy (lymphatic or adenocarcinoma), a
48 year-old man with a history of diet-controlled hypertension, steroid induced monoclonal gammunopathy of uncertain significance or an autoimmune con-
diabetes mellitus and polymyositis who developed a MI following IVIG. The dition. Case Presentation: A 70 year old female was referred for evaluation after
patient was diagnosed with polymyositis in August 2013. His initial CPK was a recent onset of recurrent episodes of angioedema without urticaria. Her ini-
10,000, elevated ANA titer at 1:640, and with a positive single-stranded DNA tial episode developed in her lip approximately 24 hours after cataract surgery.
antibody. His polymyositis was refractory to multiple therapies including pred- A subsequent episode of angioedema occurred in her neck and jaw after a res-
nisone and mycophenolate mofitil. He was then started on IVIG therapy. He piratory tract infection. Treatment with anti-histamines and corticosteroids
completed a three day course of IVIG from July 7 through July 10. On the morn- did not improve symptoms. Blood work revealed a C4 <5 mg/dL (normal 10-
ing of July 16th, he developed severe, constant, non-radiating chest pain. He 40 mg/dL), C1-INH function=23% (normal >41%), C1-INH protein=6 mg/dL
presented to the ED more than 12 hours later and was diagnosed with a myocar- (normal 21-39 mg/dL) and a C1q < 3.6 mg/dL (normal 5.0-8.6 mg/dL) and a
dial infarction. He had no history of cigarette smoking or prior cardiac history. diagnosis of ACID was made. The patient was started on Aminocaproic acid
His admission troponin T was elevated to 7.29 and he had a CPK of 2315. Car- 1gm TID to prevent attacks and Icatibant to treat acute attacks. To evaluate for
diac catheterization revealed a 100% occlusion of the mid left circumflex artery a possible underlying malignancy, the patient had a CBC, lymphocyte profile,
for which he underwent angioplasty. We believe that IVIG caused a MI in this and a MRI of her abdomen, all of which were unremarkable except for a mildly
patient due to his lack of prior cardiac disease, relatively short term course of elevated B-cell number at 482/cu mm (normal range 75 – 375). Her ANA titer
steroid induced diabetes mellitus (approximately 6-12 months), and a time was 1:320 (normal 1:40). As part of the evaluation a SPEP and immunofixa-
course consistent with prior reported thromboembolic events caused by IVIG.3 tion was performed which revealed an IgG at 438 (normal 700-1600 mg/dL),
This case is important because the application of IVIG continues to grow and and IgA 59 (normal 70-400 mg/dL), and normal IgM 81 (normal 40-230 mg/dL)
providers need to be aware of the possible risks associated with this therapy. with a polyclonal pattern. On review of symptoms, the patient reported 2
References: 1.Pierce LR, Jain N. Risks associated with the use of intravenous episodes of pneumonia, confirmed on CXR. Specific IgG to pneumococcal
immunoglobulin. Transfus Med Rev. 2003;17(4):241. 2.WHO Drug Informa- antigens was detectable for 7/14 serotypes, which decreased 5 months later (to
tion Vol 22, No. 1, 2008 3. Rajabally YA, Kearney DA. Thromboembolic com- 6/14 seropyes) after Pneumovax administration. Conclusion:To our knowledge,
plications of intravenous immunoglobium therapy in patients with neuropathy: this is the first reported patient with ACID and a specific antibody deficiency
a two-year study. J Neurol Sci. 2011;308(1-2):12-7. Epub 2011 Jun
P200
P198 A DELAYED PRESENTATION OF SEVERE COMBINED IMMUN-
GRANULOMATOSIS WITH POLYANGITIS IN AN ADOLESCENT ODEFICIENCY.
BOY. J. Bergerson*, B. Pelz, B. Prince, R. Fuleihan, Chicago, IL.
S. Burke-Mcgovern*, Middle Village, NY. Introduction: Severe combined immunodeficiency (SCID) syndromes are
Introduction: Granulomatosis with Polyangiitis (GPA) is an antineutrophil primary immunodeficiencies that result from the absence or diminished func-
cytoplasmic antibody (ANCA)-associated vasculitis (AAVs) with hallmark fea- tion of T cells and are classified by the presence or absence of B and NK cells.
tures of necrotizing granulomatous inflammation and pauci-immune vasculi- T-B-NK+ SCID occurs with autosomal recessive genetic defects involving
tis in small- and medium-size blood vessels. It has a predilection for the res- V(D)J recombination or DNA repair mechanisms necessary to produce diverse
piratory system and kidneys. GPA is extremely rare in children and adolescents T and B cell receptors and ultimately mature T and B cells. We present a case
especially of African American descent. Here we report a case of Granulo- of T-B-NK+ SCID presenting with microcephaly, growth retardation, hypogam-
matosis with Polyangiitis in an African American teen. Case Report: 13 year maglobulinemia, and recurrent infections. Case: An 18 month old female with
old black boy born and lived in Grenada, in his usual state of health began to a history of a multicystic, dysplastic right kidney, microcephaly, failure to thrive,
experience productive cough, blood tinged sputum, dyspnea, chest pain, malaise, and eczema presented with hypogammaglobulinemia identified while inpatient
and intermittent fevers. Chest x-ray (CXR) showed bilateral infiltrates, cystic for a recurrent sinopulmonary infection and chronic diarrhea. History was
changes and a 2.3 cm RUL cavitary lesion. Intradermal tuberculin test as well significant for oral candidiasis at 8 months of age, sinusitis, recurrent acute oti-
as sputum and gastric aspirate for acid fast bacilli (AFB) and HIV / HTV anti- tis media, and diaper dermatitis since 16 months. Physical examination was
body were negative. Despite a 2 weeks course of antibiotics and 18 months notable for a small female with microcephaly, and xerotic, excoriated skin on
empiric treatment for tuberculosis in Grenada his symptoms persisted. 17 the trunk and lower extremities, as well as inguinal erythroderma. Previous lab-
months after initial symptoms he demonstrated microscopic hematuria along oratory evaluation was significant for lymphopenia on CBC, undetectable IgG,
with rising serum creatinine. Five months later, in USA, his chest CT revealed IgA, and IgE, low IgM, and stool culture positive for yeast and rare
a large thick walled cavity with an air fluid level in the RUL, tree and bud for- Pseudomonas aeruginosa. Results: Repeat analysis confirmed hypogamma-
mation and a thin walled cavity in the left upper lobe. Laboratory investigation globulinemia and lymphopenia. T, B, and NK cell quantification revealed low
was significant for serum BUN / Creatinine of 65/4.1, positive ANA, and anti- T and B cell counts with an increased number of activated, memory T cells
Proteinase 3 .Renal biopsy revealed pauci-immune diffuse sclerosing and cre- and NK cell numbers that were low normal. T cell receptor analysis showed a
sent glomerulonephritis with severe tubular atrophy and interstial fibrosis. He polyclonal V beta repertoire for both CD4+ and CD8+ T cell subsets. The
VOLUME 113, NOVEMBER, 2014 A81
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A82
ABSTRACTS: POSTER SESSIONS
patient’s lymphocytes did not proliferate in response to mitogens, confirming eral arms and legs. The rash first appeared approximately four weeks previ-
a diagnosis of T-B-NK+ SCID. Genetic testing revealed a previously reported ously; six days after the rash appeared, the patient presented to a local emer-
H282R missense mutation and a novel L242IfsX5 frameshift mutation in the gency department for evaluation and was prescribed benadryl and instructed to
LIG4 gene producing a truncated DNA ligase IV protein. Conclusion: Hypo- be evaluated in an allergy clinic. Over the next three weeks, the rash gradually
morphic mutations in DNA ligase IV are a rare cause of radiosensitive, SCID resolved with benadryl, and subsequently recurred four days prior to her initial
that can have a delayed clinical presentation from classic forms. Patients with clinic visit. The patient reported no history of food, environmental, or seasonal
LIG4 mutations typically have microcephaly and growth retardation, but can allergies. The patient works as a housecleaner, and reported a history of con-
have a wide range in phenotype from mild immune deficiency to embryonic tact exposure to various household chemicals on regular a regular basis. Review
lethality depending on the residual function of the DNA ligase IV protein. of systems was positive for throat soreness which preceded the appearance of
the rash. Physical examination revealed 1-2 cm erythematous blanching mac-
ules on the bilateral lower extremities with sparing of the soles, with scattered
P201 overlying excoriations. Erythematous papules were noted on the bilateral upper
G6PC3 DEFICIENCY AND POLAND SYNDROME IN A THREE extremities, with a follicular eruption noted on the back. Areas of periungual
YEAR OLD. desquamation (not present during the initial episode of rash) were noted on the
G. Coscia*, M. Foca, K. Anyane-Yeboa, K. Ender, Y. Demirdag, New York, hands bilaterally. Results: Laboratory studies included a comprehensive meta-
bolic panel, as well as a complete blood count with differential, both of which
NY.
were within normal limits. An anti-streptolysin O screen was elevated at 1220
Introduction: Mutations in glucose-6-phosphatase catalytic subunit 3 IU/mL (ref 0-408 IU/mL). A throat culture grew Streptococcus pyogenes and
(G6PC3) are characterized by syndromic and non-syndromic severe congeni- mixed upper respiratory flora. The patient was treated with a five-day course
tal neutropenia. The syndromic form is associated with a wide spectrum of clin- of amoxicillin; her rash gradually improved but was still present ten weeks fol-
ical findings, including thymic hypoplasia, primary pulmonary hypertension, lowing its initial appearance. Conclusion: Streptococcal infection may cause
cardiac, urogenital, and musculoskeletal abnormalities. Dursun Syndrome, a prolonged and recrudescent exanthem in affected patients. While a range of
rare condition characterized by familial primary pulmonary hypertension, diagnoses may be considered, Streptococcal pharyngitis should remain a lead-
leukopenia, and atrial septal defect (ASD), is in the spectrum of G6PC3 defi- ing suspicion for both adult and pediatric patients with atypical dermatologic
ciency. To date, over 60 patients with G6PC3 mutation have been reported. Here findings when there is a clear clinical history of antecedent pharyngitis.
we present a patient with G6PC3 mutation associated with severe congenital
neutropenia, lymphopenia, pulmonary hypertension, ASD and Poland syn-
drome. To our knowledge this is the first reported case of G6PC3 mutation
and Poland syndrome. Case Report: A 3-year-old boy from non-consanguineous
P203
DELAYED HYPERSENSITIVITY REACTIONS TO ADHD MED-
parents of Dominican descent with leukopenia and recurrent infections pre-
ICATIONS: A CASE SERIES.
sented to our clinic at 8 months of age. He also has Poland syndrome (associ-
ated with absence of left pectoralis muscle, shortened left upper extremity, S. LaBarba*, P. Ponda, Great Neck, NY.
and syndactyly of the 3rd and 4th fingers of the left hand), a large secundum Rationale: Attention Deficit Hyperactivity Disorder (ADHD) is character-
atrial septal defect, pulmonary hypertension, chronic lung disease, failure to ized by hyperactivity, impulsivity and/or inattention. ADHD affects 8-10% of
thrive, aspiration, grade III vesicoureteral reflux, hydronephrosis and an inguinal all children, making it one of the most common childhood disorders. In the
hernia. He has had recurrent pneumonia as well as cellulitis and skin abscesses 2011 National Survey of Children’s Health, the prevalence of ADHD in U.S
caused by S. aureus (MRSA), P. aeruginosa, E. coli, S. maltophilia, and E. cloa- children ages 4-17 years was 11%. This is a 42% increase from a prevalence
cae. These illnesses have prompted many hospitalizations including ICU admis- of 7.8% in 2003. Up to 70% of children with this diagnosis have persistent
sions for septic shock. Laboratory analysis is summarized in Table 1. Genetic symptoms into adulthood. Currently, ADHD is treated with 3 different types
analysis revealed a homozygous G6PC3 mutation c.218+1G>A which was pre- of medications: phenylphenidates, amphetamines and “other” class. These med-
viously reported. He continues to have recurrent skin infections requiring hos- ications work to various degrees to inhibit norepinephrine and dopamine reup-
pitalizations despite filgastrim treatment. Discussion: Dursun Syndrome is a take, thereby increasing the concentration of these neurotransmitters in the
rare condition recently linked to G6PC3 deficiency associated with severe con- synaptic cleft. This in turn improves executive functioning, motivation, and
genital neutropenia. Here we report a case of G6PC3 deficiency, Dursun syn- reward perception. We describe three patients who had delayed reactions to dif-
drome, and Poland syndrome. Our patient’s findings emphasize the wide clin- ferent classes of ADHD medications. Methods: A 9 year old boy with ADHD
ical spectrum of G6PC3 deficiency. was started on amphetamine and developed diffuse urticaria one week later.
The rash resolved within two days of stopping the medicine. He then tried
Laboratory Analysis methylphenidate and lisdexamfetamine dimesylate respectively and developed
urticaria one week after starting each medication. The rash resolved one day
after stopping the medication on both occasions. Skin prick testing to all three
drugs was negative. The patient was then placed on guanfacine and tolerated
this drug without reaction. A 5 year old boy developed diffuse urticaria one
week after starting guanfacine. This resolved two days after the medication was
discontinued. A 34 year woman developed generalized pruritis five days after
starting bupropion for ADHD. This resolved one day after stopping it. She
then started lisdexamfetamine dimesylate and developed generalized erythema,
pruritis, and sensation of throat closure one week later. These symptoms resolved
after this medication was discontinued. Conclusions: Given the increasing fre-
quency of ADHD in the U.S. population and the persistence into adulthood, it
is important for clinicians to recognize ADHD medications as a possible source
of delayed cutaneous reactions. Therefore skin testing may not be predictive in
these cases. Both IgE mediated and non-IgE mediated reactions to these med-
ications should be considered when the appropriate clinical history is elicited.
P202 P204
RECRUDESCENT EXANTHEM SECONDARY TO STREPTO- EOSINOPHILIC CYSTITIS: A RARE CAUSE OF DYSURIA AND
COCCUS PYOGENES PHARYNGITIS. HEMATURIA IN CHILDREN.
G. Imperato*1, A. Khokhar2, S. LaBarba1, P. Ponda1, 1. Great Neck, NY; I.R. Bachove*, Philadelphia, PA.
2. Manhasset, NY.
Rationale:Eosinophilic cystitis (EC) is an inflammatory condition, often
Introduction: Streptococcus pyogenes pharyngitis causes an associated exan- misrepresented as a bladder tumor due to its presenting symptoms of
them in a minority of cases. Here we report a patient with an atypical prolonged gross/microscopic hematuria, urinary frequency, dysuria and suprapubic abdom-
and recrudescent exanthem secondary to Streptococcus pyogenes infection. inal pain. It is a rare condition seen in children and is thought to be caused by
Methods: A 51 year-old Hispanic female with no significant past medical his- antigenic stimulation of IgE-mediated activation of eosinophils causing mast
tory presented for evaluation of an erythematous and pruritic rash on her bilat-
A82 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A83
ABSTRACTS: POSTER SESSIONS
cell degranulation. This accounts for much of the inflammation and fibrosis to could not finish his 4 hours treatment. His Vitals remained stable and he denied
the bladder wall. We review our experience of treating patients with this con- any respiratory symptoms such as difficulty breathing, wheezes and cough.
dition in our allergy clinic. Methods:Two children with a history of acute onset There was no angioedema, headache, blurry vision or GI complaints. He denied
of urinary frequency, suprapubic abdominal pain and gross hematuria were any history of medication, food, contact or environmental allergies. Past med-
referred to allergy with the diagnosis of eosinophilic cystitis for the evaluation ical history: End-stage renal disease from IgA nephropathy, hypertension. Cur-
of potential allergens as a cause of eosinophilic cystitis. Results:Our patients rent medications: Procardia XL 30mg daily. Physical examination: He was alert,
include a 4 year old female and a 17 year old male who present with a history BP: 126/84 mm Hg, pulse 96/min, RR: 16/min. Cardiopulmonary and neuro-
of hematuria referred for evaluation after routine urine and microscopy showed logical examinations were normal. Skin revealed diffuse urticarial rash with
> 50 RBC’s/high power field. Urine culture was negative. Both patients were blanching wheals on the face, trunk and upper extremities [Fig]. Methods: Lab-
diagnosed via cystourethroscopy with biopsy demonstrating a prominence of oratory data showed WBC: 5.2K/mm3 with 10% eosinophil. Serum tryptase
eosinophils with scattered neutrophils and lymphocytes. Allergic disease level: 22.8mg/L (2hours after rash started); IgE-EIA: 44 U/ml, CH50: 57U/ml
(asthma, allergic rhinitis, etc) was present in both patients. The 4 year old female and C1Q binding: <1.2 Eq/ml. We suspected that the reaction was dialyzer
had skin testing to common indoor and outdoor allergens which was negative. related. We contacted the dialysis center and suggested that dialyzer be changed
She was treated with antihistamines with resolution by 2 months follow-up. or reused. Prewashing the dialyzer with the patient’s blood temporarily helped
The 17 year old male did not have skin testing although immunocap testing to alleviate his symptoms. We then prescribed Prednisone PO 40mg the night
showed egg IgE 38, milk IgE 52, peanut IgE 14, wheat IgE >100 and total IgE before, and 2 hours before dialysis. PO Benadryl 50mg just prior to dialysis.
1156. He was not started on any medications and had spontaneous resolution On follow up visit, the patient did very well with premedication, even when
at 3 months follow-up. Conclusion: Eosinophilic cystitis is a rare inflamma- prednisone dose was tapered down to 10 mg. Conclusion: Common causes for
tory disorder of the urinary bladder. The exact etiology of eosinophilic esophagi- dialysis resulted reactions include sensitivity to dialyzer. However, some patients
tis remains elusive though an allergic response has been proposed. Manage- continue to exhibit hypersensitivity reaction despite dialyzer changes. Pre-
ment comprises of removal of any suspected allergen, followed by antihistamine medication with steroid can successfully prevent the reactions. More studies
and corticosteroids. The course is usually benign and self-limited in children, are needed to better identify the cause of hemodialysis reactions in order to
although progression to fibrosis of the bladder with obstructive uropathy has develop better management strategies to treat affected patients.
been reported in some cases.
P205
CASE REPORT: CASHEW AS AN INCITING FOOD FOR FPIES.
E.J. Feuille*, New York, NY.
Food Protein-Induced Enterocolitis (FPIES) is a non-IgE mediated food
hypersensitivity that typically presents in infancy with vomiting and diarrhea.
The diagnosis is made based on history and clinical presentation, and is con-
firmed by a supervised oral food challenge; there is no specific laboratory test
to aid in diagnosis or in identifying the inciting food. Knowledge of potential
trigger foods for FPIES thus is important in making the diagnosis, and subse-
quently counseling patients appropriately on food avoidance. In young infancy,
the most common triggers are cow milk and soy formula. In older infants and
children, FPIES may occur with ingestion of solid foods such as grains (most
commonly rice and oat), meat and poultry, egg white, vegetables, fruit, legumes,
and seafood. FPIES to cashew, however, has not been previously reported in
the literature. In this report, we present the case of a 2.5 year-old boy who devel-
oped FPIES to cashew. His allergic history includes infantile FPIES to cow
milk, which transitioned to development of IgE mediated allergy to cow milk
at 9 months of age. After ingesting several cashews at 2.5 years of age, he had
one episode of emesis. When skin testing with an allergist was negative for
cashew, the mother was advised to reintroduce cashew. On re-introduction of
cashew however, the patient had a reaction consistent with FPIES 2 hours after- P207
wards: he developed repetitive emesis, lethargy, cyanosis, and diarrhea, notably
INFECTION AS THE CULPRIT IN ANGIOEDEMA.
without any cutaneous or respiratory symptoms. He was brought by ambulance
to the emergency department for treatment, where he improved rapidly after M.L. Curtiss*, J.T. Anderson, T. Hwangpo, Birmingham, AL.
administration of intravenous fluids. On repeat testing 3 months after this reac- Background: Angioedema causes self-limited, localized subcutaneous
tion, he was found to have small wheal in response to cashew on skin testing swelling especially likely to affect the periorbital and circumoral areas. Here
with diameter of induration 3 mm and diameter of erythema 0 mm. He also we report a case of lip swelling in the context of angiotensin-converting-enzyme
had mildly elevated specific IgE to cashew at 0.75 kIU/L. In conclusion, here inhibitor (ACEi) use caused by extensive odontologic, maxillary and parasep-
we present the first reported case of atypical (older age of onset and associa- tal abscesses. Case: A 44-year-old African American female smoker with a his-
tion with detectable serum cashew-specific IgE) FPIES to cashew, adding to tory of obstructive lung disease, atopy, hypertension on ACEi for 2 months,
the list of potential allergic triggers for FPIES. Though rare, tree nuts such as and diabetes mellitus type 2 was admitted to the hospital for her eighth pul-
cashew should be considered when identifying potential inciting food in chil- monary exacerbation in one year. She was treated with IV steroids and antibi-
dren infants presenting with symptoms consistent with FPIES. otics, her second course of high dose IV steroids in six weeks. One week later,
she reported sore throat and right ear pain, nasal discharge, pain in upper teeth,
fevers, chills, neck tenderness and progressive swelling of nose, cheeks and
P206 upper lip. Allergy consult was made to evaluate patient’s facial swelling. Results:
HYPERSENSITIVITY REACTION DURING HEMODIALYSIS. Physical exam showed swelling of upper lip, nostrils and cheeks. Laboratory
Z. Li*, J. Celestin, M. Pasha, Albany, NY. results significant for normal C1 esterase level but WBC elevated to 34,000.
Sinus CT scan done 3 days prior to lip swelling showed a maxillary periapical
Introduction: Dialyzer reactions refer to all of the abnormal sequelae result- abscess. Lip swelling and pain persisted for several days in spite of stopping
ing from the interaction between blood constituents and the hemodialysis (HD) ACEi and starting oral antibiotics. She then had spontaneous eruption of a large
membrane. There are two types of reactions: type A (0.004%) and type B (3- foul-smelling fluid collection from her nostrils. Subsequent maxillary-facial
5%). In the past, these reactions were grouped under the term “first use syn- CT demonstrated cortical breakthrough of maxillary periapical abscess and
drome” because they primarily occurred with new dialyzers. Here we present interval development of septal abscess extending down into the philtrum with
a case of hypersensitivity reaction during hemodialysis. Case: A 28 year old likely phlegmonous infection of the upper lip. She underwent I&D of septal
male was referred to the allergy clinic for diffuse urticarial rash during HD for abscess with aspiration of frank purulent material and placement of septal
the past 2 months. The pruritic rash starts within 2 hours of HD, on his face, splints. She received more aggressive antibiotic treatment thereafter. Discus-
chest and back sparing his lower extremities. The discomfort was such that he sion: ACEi involvement is the culprit of the majority of drug-induced
VOLUME 113, NOVEMBER, 2014 A83
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A84
ABSTRACTS: POSTER SESSIONS
angioedema. However, angioedema that persists and worsens over time after and infection rates and quality-of-life assessments over time. Patients from our
ACEi discontinuation may point to other causes. In this case, a severe sinus 140 investigators are eligible. IRB approval was obtained, as well as informed
infection with multiple abscesses led to inflammatory changes resulting in local consent from all subjects. Information collected by Coram nurses and phar-
facial swelling. Propensity toward development of this infection is likely mul- macists was entered into the IDEaL database. Additionally, patients were asked
tifactorial, including high dose steroids and poor oral hygiene, and protracted to complete an SF-36 questionnaire and a Life Quality Index Questionnaire
use of IV steroids likely made control of her sinus infection more difficult. (LQIQ) every six months. Currently 310 subjects are enrolled in the Registry.
The average age for diagnosis of adult patients was 59 years, and their average
serum IgG level was 508 mg/dL. The average dose for subcutaneous Ig (SCIg)
was 134 mg/kg/week; for intravenous Ig (IVIg), it was 465 mg/kg/month. In
patients who switched from IVIg to SCIg, the average conversion ratio was
1:1.21. The average annual number of infections was three, with no significant
difference between administration routes. Similar side-effect incidence rates,
with differences in specific side effects depending on route, were noted. LQIQ
results showed that most patients had a positive perception of their treatment,
including how worthwhile and effective they felt it was, but were evenly split
on how expensive they felt it was. These results from the IDEaL Registry sug-
gest an overall profile of PID patients receiving Ig. Key findings include that
adult patients were diagnosed later in life, SCIG dose was toward the lower end
of the recommended dose range, and in patients switched from IVIg to SCIg,
the dose conversion was 1:1.21. Patients appeared to have good infection con-
trol; however, with a limited dose spread, we could not demonstrate a strong
P208 dose response curve. Side effects were generally mild. Patients reported gen-
ANTERIOR UVEITIS IN A PATIENT WITH UNDERLYING erally positive quality-of-life perceptions. Continued data collection will allow
IMMUNODEFICIENCY. for further long-term data analysis on outcomes of patients on Ig treatment.
R. Kreiner*1, R. Rosenbaum1, A. Rubinstein2, 1. New York, NY;
2. Bronx, NY.
Introduction: Anterior uveitis is the process of intraocular inflammation P210
that results most commonly from a systemic immune-mediated disease. Meth- FREQUENCIES OF AUTOIMMUNE DISEASES ASSOCIATED
ods: We evaluated a 9 year old previously healthy female who presented with POLYMORPHISMS IN MEXICAN POPULATION.
anterior uveitis poorly responsive to conventional medical management and B. Esquivel*, Mexico City, DF, Mexico.
subsequently found to have an underlying familial immunodeficiency. Results: Aim: This study was aimed to determine the allelic frequencies of 22 related
9-yr-old female BZ was referred for immunologic evaluation after developing immune polymorphism (10488631, 1061170, 1265159, 12722489, 1799964,
acute anterior uveitis presenting as red right eye, absent pupillary reaction to 1800629, 1800630, 2187668, 2476601, 3087243, 3135388, 3761847, 3890745,
light and blurred vision. Initial diagnosis was made by ophthalmology on slit 4112788, 4140564, 6457617, 6822844, 6897932, 725613, 7574865, 800292,
lamp examination. She was seen by multiple specialists including rheumatol- 9888739) in Mexican population and estimated the risk for immune diseases.
ogy for a suspicion of JIA as she briefly complained of joint pain. She also had These polymorphism have been commonly associated whit 9 immune dis-
a history of a mycoplasma pneumonia affecting several family members. BZ, eases as; rheumatoid arthritis, macular degeneration, Type 1 diabetes, celiac
however, had a persisting IgM response to Mycoplasma with a delayed class disease, graves’ disease, multiple sclerosis, lupus, osteoarthritis and psoriasis,
switch to IgG. At the onset of uveitis BZ was otherwise asymptomatic and and also are located in several of the most important immune genes as; HLA,
afebrile. She was started on ophthalmic steroid drops for 6 weeks with resolu- STAT4, TNF, TNPO3, IL21, IL2RA, IL7R, MHC, C2, CFH among others.
tion of symptoms and decreased signs of inflammation on slit lamp exam. Method: Genotyping was carried out in 100 genomic DNA samples from dried
Several weeks later she was found to have recurrent insidious inflammation. blood spots supplied by the Mexican patients of Gene Test TQMedicine using
She was placed back on steroid ophthalmic drops with a marked improve- custom made multiplex array in Sequenom Massarray System technology.
ment. Upon further analysis she was found to have low serum immunoglobu- Results: The frequency for all the polymorphism was calculated and previous
lins. The family history revealed that her paternal grandfather and a paternal risk alleles for autoimmune diseases determined in Mexican population. Our
aunt suffer from Common Variable Immunodeficiency (CVID) who presented data shows similarities with those frequencies founded in human genome proj-
with recurrent infection and are being treated with periodic intravenous gam- ect and suggest an increase genetic probability for psoriasis and lupus in Mex-
maglobulin (IVIG). BZ had no history of infections other than recurrent otitis ican population. Patients with several risk alleles show an exacerbated immune
in infancy. Conclusion: This is the first case report describing a patient with response for several clinical conditions. For this patients that shown genetic
an underlying immune deficiency and family history of CVID. Her immune risk for immune diseases, relevant clinical events were not observed since nutri-
parameters do not completely fulfill the criteria for CVID. She presented with tional and clinical care were established to avoid the previous calculated genetic
a persisting IgM to Mycoplasma infection with delayed class switch to IgG as risk.. Conclusion: The Mexican population showed a slight frequency of immune
well as an autoimmune uveitis. BZ responded well to topical and systemic associated diseases polymorphism, however those who have several risk alle-
steroids but the uveitis recurred promptly with a decrease of or discontinua- les shown an exacerbated immune response. Follow up with immune modula-
tion of steroids. She had a sustained response after 3 doses of IVIG at 1 gram/Kg tors should be perform in this population to control this conditions.
and is now on prophylactic periodic treatment. Uveitis is a challenging disease
as the differential is largely idiopathic. Early diagnosis is key as untreated uveitis
can result in severely impaired vision. P211
ARE PATIENTS WITH PRIMARY IMMUNODEFICIENCY (PID)
AT GREATER RISK OF INFECTION AFTER CARDIOPUL-
P209 MONARY BYPASS FOR HEART VALVE REPLACEMENT?
THE IMMUNOGLOBULIN DIAGNOSIS, EVALUATION, AND KEY
LEARNINGS (IDEAL) PATIENT REGISTRY: RESULTS FROM M. Stein1, R. Price2, A. Koterba*1, W. Tuer3, 1. North Palm Beach, FL;
OUR PRIMARY IMMUNE DEFICIENCY POPULATION 2. Palm Beach Gardens, FL; 3. West Palm Beach, FL.
TREATED IN ALTERNATE SITES OF CARE. Reports from JS Rankin in the surgical literature suggest that cardiopul-
S. Kearns*1, L. Kristofek1, B. Bolgar1, L. Seidu2, 1. Denver, CO; monary bypass (CPB) may have immune depleting effects with some patients
2. Atlanta, GA. having low IgG levels. He reports that this in turn leads to pulmonary dys-
function which improves with intravenous immune globulin (IVIG). In our
The IDEaL Patient Registry collects longitudinal information on subjects practice in the past 3 years, 3 patients with PID have undergone aortic valve
receiving immunoglobulin (Ig) replacement therapy from Coram CVS/spe- replacements. One patient had significant post operative pulmonary prob-
cialty infusion services in an alternate care setting. Long-term outcomes and lems. Case Reports: Case 1, 61 year old female with PID was receiving IVIG
patient-reported quality-of-life assessments are not widely available for patients 25 gm every 5 weeks with trough IgG = 866 mg/dl on12/12/12. The next dose
on Ig therapy for different disease types. In the IDEaL primary immune defi- of IVIG was increased to 35 gm on 1/14/13. Aortic valve was replaced on
ciency (PID) population, we examined baseline lab values for treated patients, 1/22/13, and she was on CPB for 87 mins. On 1/25/13 respiratory distress
A84 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A85
ABSTRACTS: POSTER SESSIONS
with a small infiltrate on chest X-ray leading to reintubation. On 1/29/13 IgG describe the case of a 21 year old male who was diagnosed with CVID at the
= 490 mg/dl and patient received IVIG 30 gm. There was subsequent rapid age of 17 years after an episode of prolonged diarrhea and weight loss that
improvement over the next 48 hours. Two other females with PID had aortic required total parenteral nutrition. His quantitative Immunoglobulins were
valve replacement with no pulmonary or infectious complications. Case 2, 72 decreased (IgG 146 mg/dl (700-1600 mg/dL) IgA= <7 mg/dl (70-400 mg/dL)
year old on 30 gm IVIG with trough IgG = 799 mg/dl and was on CPB for 85 (IgM=<5 mg/dl (40-230 mg/dL)). He had protective antibody levels to measles,
mins. Case 3, 58 year old was on subcutaneous immune globulin 29.7 gm every mumps, rubella and varicella but absent antibodies to tetanus vaccine. Replace-
2 weeks. IgG trough was 1300mg/dl and she was on CPB for 64 mins. Con- ment with intravenous immunoglobulins (IVIG) was started; because of low
clusion: Reports from the surgical literature suggest that CPB may lead to a trough levels dose increases were necessary. A biopsy of his Duodenum showed
decrease in IgG. In one of three patients with therapeutic levels of IgG preop- complete absence of plasma cells, several non-necrotizing microgranulomata
eratively, there was a significant drop in IgG after CPB and aortic valve replace- were found in gastric samples. Diphenoxylate and atropine was started for treat-
ment. Multiple factors could contribute to this drop including dilutional effects ment of diarrhea. In the following the patient continued to have daily exten-
of intravenous fluids, active bacterial infection, and the use of CPB. The pul- sive diarrhea that prevented weight gain. Giardia was identified by stool cul-
monary infection and respiratory distress were accompanied by the decrease ture. Despite prolonged treatment with various antibiotic regimens no
in IgG. A prospective study is needed in patients with and without PID, with eradication could be achieved. Treatment with Metronidazole, Tinidazole, Nita-
measurement of IgG before surgery and 24,48 and 72 hours post CPB. At the zoxanide, Paromomycin, Quinacrine alone and in different combinations was
present time it is important to consider whether there is a need for an extra load- attempted for 2 years. Oral Budesonide and Loperamide were needed for con-
ing dose of IVIG before surgery or whether careful monitoring of IgG levels trol of his diarrhea on most days. Control of inflammation was also attempted
after surgery will help assure that the PID patient will not have serious post- with oral prednisone intermittently. Environmental precautions as avoidance
operative infections. of tap water were advised. A prolonged course of Quinacrine and Tinidazole
cleared the infection and has kept him in remission for almost 11 months. Dif-
ferent components of CVID at interplay in the gastrointestinal tract required a
P212 delicate balance of controlling inflammation with corticosteroids and treatment
MOWAT-WILSON SYNDROME (MWS) WITH ASPLENIA AND of infection with antibiotics. Increased protein loss necessitated various dose
LOW IMMUNOGLOBULIN LEVELS. adjustments of IVIG to allow adequate protection of reinfection.
S. Wu*1, C.M. Bollard2, B.S. Vartabedian1, K. Paull3, B.P. Chumpitazi1,
I.C. Hanson1, 1. Houston, TX; 2. Washington, DC; 3. Bryan, TX.
Introduction: MWS is characterized by peculiar facial appearance, heart
P214
TSUKAMURELLA SPECIES INFECTION PROMPTING DIAG-
defects, Hirschsprung disease (HD), genitourinary anomalies and brain anom-
NOSIS OF CHRONIC GRANULOMATOUS DISEASE IN A 17
alies. It is caused by mutation of ZEB2 gene. Pons et al have described con-
YEAR OLD MALE.
genital hypo/asplenia in 4 patients with MWS and ZEB2 mutation, and sug-
gest ZEB2 as a candidate gene for asplenia. Immune abnormalities have not C.D. Kubiak*, J.R. Trotter, J.K. Potthast, A. Petrovic, J.W. Leiding,
been reported in MWS patients. Here we report two unrelated patients with St. Petersburg, FL.
MWS, ZEB2 mutation, congenital and/or functional asplenia and immune Chronic granulomatous disease (CGD) is an innate defect caused by muta-
abnormalities. Methods: Chart and literature review Results: Patient 1 is a 6- tions in any of the five subunits of the NADPH oxidase leading to impaired
year-old boy with MWS, HD, heart defects, and congenital asplenia. He had superoxide production and reduced intracellular killing of certain bacteria and
no significant infection history. His immunological studies showed low IgG, fungi. Recurrent infections of the skin, lungs, lymph nodes, and liver are caused
IgA and IgM, but normal response to vaccination. T&B cell phenotyping showed by a narrow spectrum of bacteria and fungi with particular susceptibility to
normal percentages and numbers of mature B cells (CD19/CD20), but low per- catalase positive organisms. We report a case of Tsukamurella species pneu-
centages of CD19/27+ memory B cells. CD3 and CD8 T cell numbers were monia prompting diagnosis of p47 deficient CGD in a 17 year old male. A 17
low but lymphoproliferative studies showed normal responses to mitogen and year old Hispanic male developed cough, fever, and fatigue over one week.
specific antigen. He lacked serologic evidence for past viral infection. In vitro Cavitary necrotic lobar pneumonia of the right upper lobe, left lower lobe, and
cytotoxic-T-lymphocyte (CTL) function appeared normal with cellular ability lingula was found on computed tomography. Sputum culture yielded Tsuka-
to release interferon g in response to autologous EBV-transformed B cells murella species and methicillin-sensitive Staphylococcus aureus. Prolonged
(Elispot assay) and kill EBV-transformed B cells in cytotoxicity assay docu- treatment with meropenem and trimethoprim-sulfamethoxazole led to clinical
mented. In sum, no T cell defect was identified. Patient 2 is a 4-year-old girl improvement and resolution of consolidations. Past history included bacterial
with MWS, malrotation, hypogangolionosis, developmental delay, seizure dis- lymphadenitis at 18 months and 12 years, recurrent viral upper respiratory
order, and minimal splenic function from presumed splenic infarct. She had infections, and ulcerative colitis diagnosed at 17 years. In addition he had recur-
recurrent infections of URI, otitis, and sinusitis. Her immunological studies rent granulomatous skin disease with slow wound healing. Infection with Tsuka-
showed low IgG and IgA, and normal response to vaccination. T&B cell phe- murella, an opportunistic organism, prompted immune evaluation. Dihy-
notyping showed normal percentages and numbers of T (CD3, CD4, CD8) drorhodamine assay revealed abnormal oxidative burst pattern consistent with
and B (CD19, CD20, CD19/27+) cells including transitional and class-switched autosomal recessive CGD. Analysis of NCF1 showed a 2 base pair deletion
B cells. This child received empiric immunoglobulin supplementation and then (c.75_76delGT ) confirming the diagnosis of autosomal recessive CGD. Tsuka-
antibiotic prophylaxis. Conclusion: Like the MWS patients reported by Pons murella species are partially acid fast, aerobic, castalase positive, Gram-posi-
et al, our 2 subjects also had congenital and/or functional asplenia associated tive rods found in soil. Infections with Tsukamurella typically occur in immuno-
with ZEB2 mutation. Both patients had evidence of immune discrepancies with compromised hosts, particularly when neutropenia is present. Indwelling central
low immunoglobulin levels. Physicians caring for patients with MWS should venous catheter placement is also a risk factor. Cases of Tsukamurella have
be aware of asplenia risk and possible immune abnormalities specifically B been reported in patients with severe combined immunodeficiency, leukemia,
cell defects. Abdominal ultrasound and immune evaluation are recommended myelodysplasia, and in those receiving immunosuppressive chemotherapy.
to reduce infectious morbidity. We report the first case of Tsukamurella infection in a patient with CGD.
P213 P215
BALANCING INFLAMMATION AND INFECTION IN A PATIENT RENAL COMPLICATION OF COMMON VARIABLE IMMUN-
WITH COMMON VARIABLE IMMUNODEFICIENCY (CVID) ODEFICIENCY.
AND CHRONIC GIARDIASIS. H.M. Tartibi*, S.L. Bahna, Shreveport, LA.
D.A. Andreae*, C. Cunningham-Rundles, New York, NY. Introduction: Primary immunodeficiency diseases can have a variety of
CVID is a collection of diverse and distinct diseases characterized by pri- complications, mostly infections. We report a case with a renal complication.
mary antibody deficiency (hypogammaglobulinemia). Clinical manifestations Case: A 26-y-o male presented with fever, pleuritic pain & productive cough
include autoimmunity, inflammatory disease, recurrent infections and increased for 1 d. He had adenotonsillectomy as a child and multiple pneumonias over
malignancies, especially lymphoproliferative disorders. Inflammatory disease the past 4 y. He appeared ill, in mild respiratory distress, T 1010F, RR 20/min,
of the gastrointestinal tract is seen in about 50 % of patients and lymphocytic HR 118/min, BP 134-151/70-89 mmHg, Wt 97.5 kg, with dry mucous mem-
intraepithelial infiltration is common. Gastrointestinal infections, especially in branes, decreased breath sounds on the right lower lung field, and mild lower
patients with absent IgA are common and Giardia is a recognized culprit. We extremity edema. CXR showed RUL & RLL infiltrate with right-sided pleu-
VOLUME 113, NOVEMBER, 2014 A85
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A86
ABSTRACTS: POSTER SESSIONS
ral effusion. CBC: Hgb 10.1 g/dL, Hct 29.9%, Platelets 310 K/uL, WBC 20.12
K/uL, N 16.86 K/uL (84%), L 1.7 K/uL (8.4%), M 1.15 K/uL (5.7%), E 0.3
P217
IDENTIFICATION OF GATA2 MUTATION IN ASYMPTOMATIC
K/uL (1.6%). Serum protein was 4.5 g/dL, with albumin 1.1 g/dL. He was rehy-
drated with IVF & started on antibiotics (blood culture grew S. pneumoniae). PATIENT.
His BUN 13 mg/dL & Cr 2.1 mg/dL increased to BUN 48 mg/dL and Cr 6.5 M.R. Shams*, L. Kobrynski, Atlanta, GA.
mg/dL by day 10. UA showed 500 mg/dL protein, Pr/Cr ratio 7.9 (nl <0.2). Rationale: Whole exome sequencing (WES) is being used as a screening
Renal biopsy demonstrated post-infectious glomerulonephritis (secondary to and diagnostic test for a number of rare diseases. The significance of mutations
S. pneumoniae). Our evaluation showed IgG 102 mg/dL, IgM 31 mg/dL, IgA identified through WES requires interpretation by experts with knowledge of
<8 mg/dL, IgE <0.3 IU/mL. He had nonprotective Ab titers to diphtheria (<0.1 disease causing mutations. Methods: A 22 month old male presented to the
IU/mL) & tetanus (<0.1IU/mL). Pneumococcal Abs were not done due to lab Immunology clinic after WES revealed a mutation in GATA2. Genetic testing
error. We administered IVIG 1g/kg. Upon obtaining his past medical records, was performed because of a history of mild dysmorphic features, laryngoma-
we discovered that 3 y ago he had IgG 169 mg/dL, IgM 2 mg/dL, & IgA <5 lacia, and obstructive sleep apnea. The only infectious history was recurrent
mg/dL without intervention. At that time had normal BP and renal function. acute otitis media requiring tympanostomy tubes and severe gingiva-stomati-
HIV test was negative. Flow cytometry was WNL. UPEP was consistent with tis. Results: WES revealed a 3 distinct mutations; COMP R381H heterozygous
non-selective proteinuria & SPEP was suggestive of acute inflammatory mutation, TMCO C35Y heterozygous mutation and a de novo GATA2 R396W
response. His stool α-1-ATP was negative. For glomerulonephritis, he was heterozygous mutation associated with known disease. GATA 2 defects are
started on high dose steroid therapy with gradual reduction to 60 mg/day pred- inherited in an autosomal dominant and cause increased susceptibility to severe
nisone & anti-hypertensives. His findings were compatible with CVID com- viral infections, the development of mononuclear cytopenias, myelodysplastic
plicated by nephrotic syndrome. IVIG continued (500 mg/kg) every 2-3 wk syndrome/acute myeloid leukemia and lymphedema. GATA2 R396W has been
with peak 1280 mg/dL & troughs 370-662; and IgG half-life 6.3 d. His renal previously reported in 2 patients, who developed symptoms in late childhood
function fluctuated depending on his adherence to Lisinopril; with Cr 1.3 mg/dL with infections with Epstein-Barr virus, herpes-simplex virus, human papil-
& Pr/Cr ratio 2.3. He has remained infection-free with radiographic resolution loma virus, mycobacterium avium intracellulare and the development of
of his pneumonia & pleural effusion. Conclusion: To our knowledge, this is myelodysplastic syndrome. Our patient had a history of oral herpetic lesions
the first reported case of CVID complicated with post-streptococcal glomeru- due to herpes simplex but had no other significant viral infections. T, B, NK
lonephritis possibly due to marked delay in IVIG therapy. lymphocyte enumeration was normal. Neither parent had the R396W mutation.
The other two identified mutations were carried by his father but are of unknown
significance. Conclusions: WES is a useful testing modality to confirm sus-
P216 pected diagnoses. However, providers should use caution when interpreting
SARCOIDOSIS WITHOUT GRANULOMA PRESENTING AS genetic reports, especially if used as a screening modality, as many genetic vari-
LYMPHOPENIA. ations are benign polymorphisms. It is critical to perform WES on both par-
A. Kleva*, A. Jongco, Great Neck, NY. ents and, if available, affected family members to confirm the pathogenicity of
a mutation.
Introduction: Sarcoidosis is a granulomatous disorder of unclear etiology
that affects multiple systems. Monocytes, macrophages, and activated T cells
increase production of inflammatory mediators in noncaseating granulomas.
Peripheral lymphopenia correlates with disease severity. Methods: We report
P218
EFFECTIVE USE OF 20% SUBCUTANEOUS IMMUNOGLOBU-
a relatively healthy 22-year old male with a history of psoriasis who presented
with fever, cough, malaise after traveling to Cancun. He was diagnosed with LIN THERAPY IN AN ADULT MALE WITH PRE-EXISTING
bibasilar pneumonia and treated with levofloxacin. He was readmitted for fever, THROMBI.
abdominal pain, diarrhea, hypoxia and neutropenia requiring filgrastim. Hos- C.M. Duff*1, M. Sher2, J. Leiding2, 1. Parrish, FL; 2. St. Petersburg, FL.
pitalization was complicated by pneumothorax after bronchoscopy. Bron- Rationale: Immunoglobulin replacement therapy is prescribed for patients
choalveolar lavage showed Balantidium coli that was treated with doxycycline with immunodeficiency characterized by hypogammaglobulinemia and/or the
and metronidazole. After a few days, he was readmitted with fever, hypoten- inability to make antibodies to recall antigens. Administration can occur intra-
sion, hypoxia, diarrhea, and a new purpuric rash on the extremities. High dose venously or subcutaneously. Currently there is a black box warning on all
steroids, imipenem, vancomycin and levofloxacin improved respiratory status immunoglobulin replacement products indicating a possible increased risk of
and rash. He returned soon after discharge with pneumothorax needing a chest thrombogenic events. Data regarding the use of subcutaneous immunoglobu-
tube. As outpatient, prednisone was titrated to 40 mg daily without exacerbat- lin (SCIG) therapy in patients with known thrombotic events is limited. Meth-
ing rash or respiratory status. Bactrim prophylaxis was started. Results: At first ods: A 36 year old Caucasian male with cystic fibrosis was diagnosed with
readmission, T-cell lymphopenia was found (CD4+ = 83/uL, CD8+ = 35/uL). selective antibody deficiency based on absent pneumococcal responses (0/14
Bone marrow biopsy and extensive autoimmune and infectious workup were protective serotypes) with intact tetanus and diphtheria responses and normal
nondiagnostic. On readmissions, he had low IgG of 547 mg/dL. Open lung immunoglobulin profile (IgG 1020mg/dl, IgA, IgM). He is the survivor of a
and skin biopsies showed a predominantly T-cell lymphohistiocytic infiltrate double lung transplant at 24 years and a single lung transplant at 33 years. A
with CD4+>CD8+. Noncaseating granulomas were absent in both biopsies. As left leg deep vein thrombosis and sagittal vein thrombosis developed two years
outpatient, lymphopenia persisted (CD4+ = 112/uL, CD8+ = 54/uL, CD19+ after second transplant. Causes of primary thrombophilia were excluded. In
=6/uL, and CD 16+/56+ = 20/uL). Lymphocyte proliferation to PHA, IgG, IgA, parallel recurrent bacterial pneumonias, primarily caused by S. pneumonia led
IgM, CH50, and G6PD level were normal. He had protective titers to MMR, to multiple hospitalizations. Based on poor antibody responses and clinical sta-
tetanus, diphtheria, pertussis and polio, but not to pneumococcus or varicella. tus, immunoglobulin replacement therapy was initiated. Results: To decrease
A skin biopsy performed 6 months later showed noncaseating granulomas con- the potential risk of a thrombotic event, 20% SCIG was administered more
sistent with sarcoidosis. Lymphopenia persists (CD4+ = 82/uL, CD8+ = 32/uL frequently at twice weekly. Concurrent treatment of thrombi continued with
and CD16+/56+ = 33/uL) while on weekly low-dose methotrexate, daily dap- warfarin maintaining INR at a therapeutic level of 2-3 units. No bleeding or
sone and prednisone 10 mg. Conclusion: Whether an underlying immune defi- bruising occurred at infusion sites. A magnetic resonance angiogram performed
ciency was present is unclear, but medication-induced immune suppression 6 months after starting SCIG showed no increase in size or new thrombi. Pro-
does not adequately explain his course. This case underscores the need for re- tective pneumococcal titers were measured and were found to be protective to
evaluation of affected systems. Sarcoidosis should be considered in the differ- 10/14 serotypes and the patient has had only one hospitalization for bacterial
ential diagnosis of lymphopenia. pneumonia since starting SCIG. Conclusion: SCIG can be safely and effec-
tively administered to patients with thrombi receiving anticoagulant therapy.
Concurrent use of anticoagulant medications did not increase the occurrence
of local site reactions with the use of 20% SCIG treatment in this patient.
A86 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A87
ABSTRACTS: POSTER SESSIONS
domain, leading to a malformation of the functional enzyme similarly found
P219 in homozygous mutation. Our patient does not have microcephaly or growth
DIVERGENT PHENOTYPES IN SIBLINGS WITH X-LINKED
retardation, but does show clear evidence of radiosensitivity and T cell lym-
CGD. phopenia, which we suspect will worsen with age.
F. Alkhatib*1, D.M. Robertson2, 1. Holyoke, MA; 2. Hadley, MA.
Introduction: CGD is a rare immunodeficiency of phagocytes character-
ized by increased susceptibility to bacterial and fungal pathogens. We describe P221
the first report of two siblings with X-linked CGD due to the same mutation STAT3 MUTATION IN GOOD SYNDROME.
with significant variation in phenotype. Methods: A 6 week-old full term boy L. Buyantseva*, T. Craig, Hershey, PA.
presented with fever, lymphadenopathy, and dyspnea. Imaging showed multi-
Background: Good syndrome is a rare cause of combined immune defi-
focal pneumonia. His hospital course was complicated by ARDS, septic shock,
ciency that occurs in association with thymoma. TACI and BAFF-R receptor
Candida lusitaniea fungemia, a cutaneous Candida and Rhizomucor abscess,
mutations have been described in association with this syndrome. Signal trans-
multi-organ dysfunction, and HLH (Hemophagocytic Lymphohistoiocytosis).
ducer and activator of transcription 3 (STAT3) is a transcription factor essen-
The “healthy” 18-month old brother of patient 1 was considered as a stem cell
tial for differentiation of the TH17 helper T cells. Mutation of STAT3 gene has
donor, but was found to have CGD caused by the same mutation. He was thriv-
been described in association with HyperIgM syndrome and a variety of autoim-
ing with no major illnesses, but serological evaluation revealed systemic inflam-
mune diseases. We present a case of STAT 3 mutation associated with Good
mation, normalizing on triple prophylaxis of Bactrim, Itraconazole and INF-
syndrome. Case Presentation: A 73-year-old female with Common Variable
gamma. Results: In patient 1, Immunoglobulin B & T cells levels were normal,
Immunodeficiency (CVID) and thymoma removed 20 years ago. She presented
while NK cells were slightly low (92 c/mm3). DHR showed absent neutrophil
with chronic watery diarrhea, 20 pound weight loss and frequent sinus infec-
function: genetic testing revealed a hemizygous mutation in the CYBB gene
tions. Her physical exam was remarkable for extensive onycomycosis. Immune
of gp91phox, consistent with X-linked CGD. After stabilizing medically, he under-
workup showed lymphopenia, deficiency of B and T absolute cell counts (<1%
went hematopoietic stem cell transplant (HSCT) from an unrelated donor com-
and 58% respectively), normal NK cells count, and low IgA, IgG and IgM lev-
plicated only by mild cutaneous GVHD. The second sibling had a negative DHR
els (<33 mg/dL, 6.7 mg/dL and 4.2 mg/dL respectively). Gastroenterology
assay and the same mutation. ESR was >120, Plt 719, Hct 26.3, Alk Phos 310
workup revealed celiac disease as a cause of her diarrhea. Gluten-free diet was
and immunoglobulins were elevated. Screening CT showed 2-3 <1cm non-
initiated and her diarrhea resolved. Patient was started on Atovaquone for pro-
enhancing hepatic hypodensities, not amenable to biopsy. Lab abnormalities
phylaxis of opportunistic infections and IVIG replacement. Genetic analysis
normalized within weeks of starting prophylactic therapy. At age 3, he remains
identified STAT 3 mutation. Conclusions: This is a first published report of a
free of recurrent bacterial and fungal infection. Discussion: CGD is caused by
patient with Good syndrome associated with STAT 3 mutation. This case
mutations in phagocyte NADPH oxidase, with considerable variability in dis-
demostrates the variability of phenotypic responce to STAT 3 mutations.
ease severity. For many years, treatment consisted primarily of antimicrobial
prophylaxis. Recently, HSCT has emerged as an attractive alternative, though
there is debate about candidates for transplant. Generally, patients with very
low super oxide production have worse long-term survival. Previous cases of
P222
siblings with AR-CGD have shown variable phenotype, presumably due to pen-
MANNOSE BINDING LECTIN DEFICIENCY WITH A CONCUR-
etrance of the functional allele. Our cases are unique in that the patients have RENT ESOPHAGEAL CANDIDIASIS AND RECURRENT HER-
the same level of phagocyte function but very different phenotypes and high- PES GINGIVALIS.
light the potential difficulty in using level of super oxide production to assess K. Achar*1, D. Ferastraoaru2, D.L. Rosenstreich2, 1. New York, NY;
patients for HSCT. 2. Bronx, NY.
Introduction: Mannose binding lectin (MBL) recognizes carbohydrate pat-
terns found on the surface of pathogenic microorganisms leading to activation
P220 of the lectin pathway of the complement system and contributing to ultimate
NEWBORN TREC SCREENING IDENTIFIED AN INFANT WITH pathogen elimination. MBL plays an important role in the first-line defense
NHEJ1 HETEROZYGOUS MUTATION LEADING TO THE DIAG- against Candida albicans and its deficiency is associated with herpes virus sim-
NOSIS OF ATYPICAL RADIOSENSITIVE SCID. plex (HSV) infection in mice. Method: Review of the literature and case report
H. Bhatti*, P. Poowuttikul, E. Secord, Detroit, MI. of a patient with MBL deficiency, esophageal candidiasis and recurrent oral
herpes virus simplex infection. Results: 50 yo male with well controlled sea-
Background: Radiosensitive forms of SCID are due to defects in compo-
sonal allergies was referred for evaluation of a possible immune deficiency
nents of the NHEJ DNA repair mechanism during the process of V(D)J recom-
after he was found to have one episode of esophageal candidiasis that resolved
bination. Mutations in several genes involved in the NHEJ mechanism result
with oral fluconazole treatment. The patient did not have any other factors that
in a T-B-NK+ SCID. About 1/3 of patients with SCID have the T-B-NK+ phe-
could predispose to candidiasis, predisposing factors such as diabetes mellitus
notype, which is associated with a poorer prognosis after receiving hematopoi-
or treatment with oral or inhaled corticosteroids, and was HIV antibody neg-
etic cell transplantation in various studies. The components of DNA repair
ative. Further history revealed that he had been experiencing recurrent oral
that are known to lead to radiosensitive SCID include Artemis, DNA Ligase
ulcers for the past 10 years the worst of which were over the lip, with more fre-
IV, DNA-PKcs, Ku70, Ku80, XRCC4 and Cernunnos-XLF or NHEJ1. Patients
quent and longer episodes for the past year. A repeat immunological evalua-
with NHEJ1 deficient SCID typically have microcephaly with growth retar-
tion revealed normal lymphocyte subsets, serum immunoglobulin levels, anti-
dation; however there are a few cases who do not. Objective: We report the case
body responses (tetanus toxoid and pneumococcal titers), complement levels
of 21-month old female with a heterozygous NHEJ1 defect and T cell defi-
and a negative repeat HIV test. The serum MBL level on the first visit was low
ciency identified on newborn TREC screening. Case Report: A full term new-
(12ng/ml ; normal: >100 ng/ml) and when repeated 3 months later was less
born was found to have very low TREC on newborn screening leading to sus-
than 0.5 ng/ml. The patient did not have any recurrence of esophageal can-
pected SCID versus a combined immunodeficiency. Exam of the baby revealed
didiasis and he was prescribed acyclovir for recurrent oral HSV which reduced
normal growth parameters and no dysmorphism. Subsequent testing revealed
the frequency and severity of the oral lesions. Conclusion: This is the first
T and B cell lymphopenia (CD4 = 750/mm3, CD19 = 75/mm3) with normal
documented case of associated esophageal candidiasis and recurrent oral HSV
IgG and IgM with low IgA. Genetic testing revealed a heterozygous defect in
infection in a patient with MBL deficiency. The exact mechanism through which
the NHEJ1 gene. The lymphoblastoid cells revealed abnormal radiosensitivity
MBL deficiency predisposes to mucosal infections in patients with an other-
of 15%. The T cell lymphopenia progressed until our last labs at 16 months.
wise normal immune system is not completely understood. We would like to
Testing for 22q11 deletion was normal. PHA was initially low but was ade-
highlight the importance of maintaining a high level of suspicion for MBL defi-
quate at 16 months and the child experienced no serious infection during that
ciency in these challenging cases. Making a correct diagnosis will help to pre-
time. The family refused further care and the patient remains lost to follow up.
vent possible future complications by keeping these patients under closer obser-
Discussion: Deficiency of NHEJ1 is one of the variants of radiosensitive SCID.
vation. At the present there is no specific treatment available for MBL deficiency.
Five SCID patients reported to date have homozygous mutation of NHEJ1. Typ-
ically patients with this variant exhibit severe recurrent infections, microcephaly
and growth retardation. Mild to severe T and B cell lymphopenia have been
reported with progressive lymphopenia over time. We report a patient with het-
erozygous NHEJ1 deficiency in which the defect involves the dimerization
VOLUME 113, NOVEMBER, 2014 A87
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A88
ABSTRACTS: POSTER SESSIONS
P223 P224
RISK FACTORS RELATED TO MORTALITY IN CHILDREN NEUTROPENIA: A CLUE FOR THE DIAGNOSIS OF X-LINKED
WITH HAEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS IN A AGAMMAGLOBULINEMIA.
CHILDREN’S HOSPITAL FROM MEXICO CITY. M. Tallar*1, M. Hintermeyer1, H.N. Hartman2, J. Verbsky1, J. Casper1,
L.I. Calderon*, A. Partida, B.E. Del Rio, O. Saucedo, C. Cicero, Mexico J. Routes1, 1. Wauwatosa, WI; 2. Milwaukee, WI.
City, DF, Mexico. Background: X-linked Agammaglobulinemia (XLA) is a primary immun-
Introduction: Haemophagocytic lymphohistiocytosis is a life-threatening odeficiency secondary to a mutation in the gene coding for the Bruton’s tyro-
disease of immuneregulation. A large proportion of deaths occur early into sine kinase (Btk) protein, which is essential for the differentiation of B cells.
treatment. We investigated association with early death for laboratory and clin- Immunological evaluation typically demonstrates a low/absent CD19+ B cells
ical parameters. Methods: A total of 45 children from Federico Gómez Chil- and agammaglobulinemia/severe hypogammaglobulinemia. The clinical pres-
dren’s Hospital in Mexico city wich fulfill the diagnostic criteria and/or with entation of XLA is usually between 6-18 months of age and is characterized
familiar disease, receiving diferent treatments were included. We discribed by recurrent upper and lower respiratory tract infections gastrointestinal tract
demographic, clinical and laboratory data with frecuencies and proportions and infections, conjunctivitis, skin infections/pyoderma, meningitis and sepsis. Ten
also stadistics with central tendancy and dispersión tendancy. We made a risk to 20% of patients have neutropenia at the time of initial diagnosis. Case Descrip-
analysis in two steps. The first was about an univariated análisis with propor- tion: An 18 month old male with a history of atopic dermatitis was admitted
tional diferences in the survivor group and in non-survivers, using X2 or exact to hospital for a rash concerning for bullous impetigo. He had an absolute
Fisher test acording to the number of observations. From the variables that show neutrophil count of 0/mm3 on admission which improved to 3500/mm3 after
statisticaly significant diferences, they were introduced in a model of multiple starting antibiotics for methicillin sensitive staphylococcal aureus (MSSA).
OR, in wich we also include time in months until clinical presentation, genus Quantitative immunoglobulins were obtained revealing IgG<80 mg/dL (431-
and etary group, getting a statisticaly significant model (LR X2 (6g-l) = 13.32; 1109), IgA<6 mg/dL (20-100), and IgM<5 mg/dL (19-146). Vaccination titers
p=0.038). Results: We observed a significant relation of risk for mortality for to tetanus, diphtheria, haemophilus, and pneumococcus were absent. Flow
neutropenia (OR 8.96 IC95% 1.08 a 74.49, p = 0.042). The presence of clini- cytometry on peripheral blood revealed no CD19+ B Cells and absence of BTK
cal infection at the time of diagnosis show a relation with mortality without expression in monocytes. Conclusions: Although there are several proposed
significant relevance (OR 7.17 IC95% 0.97 a 53.16; p= 0.054). The presence mechanisms for neutropenia in XLA, two non-mutually exclusive mechanisms
of hepatomegaly and absence of epistaxis are perfect predictors of surveillance. have recently gained prominence. One proposed mechanism is that Btk is nec-
The surveillance curves point out the group between 1 and 4.9 years to be the essary for PMN function and development. In mouse models, neutrophils defi-
more vulnerable with a higher mortality get in the first month after diagnosis cient in Btk have decreased expression of granular proteins (elastase, myeloper-
of 50% and 70% thereafter. The group of less than 1 year show a mortality of oxidase, gelatinase, and neutrophilic granular protein) and arrest of maturation
62%. The group of 5 to 10.9 years show a mortality rate of 66%. Finally the at the myelocyte/promylocyte stage. Another proposed mechanism is that Btk
group of 11years and older, get a mortality rate of 55% at 3 months after diag- negatively regulates cytokine and Toll Like Receptors (TLR) induced Reduced
nosis. Conclusión: In 45 patients with the diagnosis of haemophagocytic lym- Oxygen Intermediates (ROI) production. In studies using human PMNs, a defi-
phohistiocytosis in the Hospital Infantil de México Federico Gomez, we found ciency in Btk results in the overproduction of ROI during infection leading to
a mortality of 53%. The risk factor asociated to mortality was the presence of increased neutrophil apoptosis compared to neutrophils from normals. How-
neutropenia. We also found a relationship with the presence of infection, but ever, neither of these mechanisms explains why neutropenia only occurs with
it wasn’t statistically relevant. Moreover, in this study, we found posible pro- infection prior to diagnosis and not subsequently following administration of
tector factors related to mortality like the abscence of epistaxis and presence replacement antibody. Regardless, XLA should be on the differential diagno-
of hepatomegaly. sis of males between the ages of 6-18 months of age presenting with neutropenia.
Table 4. Differences between survivours and non-survivours & univariate
risk analysis. P225
LONG-TERM PROPHYLACTIC TREATMENT OF HEREDITARY
ANGIOEDEMA: FINDINGS FROM AN INTERNATIONAL
HEREDITARY ANGIOEDEMA EXPERT SURVEY.
B. Zuraw*1, T. Craig2, J.A. Bernstein3, H. Farkas4, I. Boccon-Gibod5,
L. Bouillet5, M. Cicardi6, M. Cancian7, A. Reshef8, M. Stobiecki9,
P. Nordenfelt10, H. Longhurst11, M. Guilarte12, T. Caballero13,
M.B. Ferreira14, K. Bork15, M. Magerl16, I. Martinez-Saguer17,
E. Aygören-Pürsün18, A. Bygum19, 1. La Jolla, CA; 2. Hershey, PA;
3. Cincinnati, OH; 4. Budapest, Hungary; 5. Grenoble, France; 6. Milan,
Italy; 7. Padova, Italy; 8. Tel Hashomer, Israel; 9. Cracow, Poland;
10. Jönköping, Sweden; 11. London, United Kingdom; 12. Barcelona,
Spain; 13. Madrid, Spain; 14. Lisbon, Portugal; 15. Mainz, Germany;
16. Berlin, Germany; 17. Frankfurt- Mörfelden, Germany; 18. Frankfurt,
Germany; 19. Odense, Denmark.
Introduction: Orally administered attenuated androgens (AAs) have been
used since the 1970s for prophylactic treatment of hereditary angioedema (HAE)
attacks, although they may be associated with dose-dependent undesirable side
effects. Intravenous plasma derived C1-INH (C1-INH) has become available
for prophylaxis in the last 5 years in some countries. However, long-term expe-
rience and safety data on this therapy is limited and its use varies by region
and country. Our aim was to assess AA use across several international HAE
centers and identify medical reasoning which may support switching patients
from AAs to C1-INH prophylaxis. Methods: An 8-question survey exploring
physician opinions on the use of prophylactic medications for HAE was sent
to 17 HAE experts’ in Europe (EU) and 3 in the United States (US). Experts
reported on the percentage of patients receiving prophylaxis with AAs, side
effects observed in patients receiving AAs and barriers preventing the switch-
ing of patients to alternative therapies. Results: The use of AAs varied among
the HAE experts surveyed being most common in the EU compared to the US
(Fig 1), and was more common in men (27.6%) than women (13.4%). Other
therapies used included C1-INH, antifibrinolytics and progestin (Fig 1). Side
effects reported in males receiving AAs included weight gain, lipid abnormal-
A88 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A89
ABSTRACTS: POSTER SESSIONS
ities and hypertension. Most reported side effects in females were menstrual
irregularities, virilization and weight gain. A small number of patients discon-
P227
RECOMBINANT HUMAN HYALURONIDASE [RHUPH20]-
tinued AAs due to side effects (12%) while some patients (12%) switched to
alternative treatments, e.g., C1-INH. Physicians reported that barriers pre- FACILITATED SUBCUTANEOUS (SC) INFUSION OF IMMUNO-
venting patients switching to prophylactic C1-INH included AA efficacy (n=10), GLOBULIN G (IGG) (HYQVIA; IGHY) IN PATIENTS AGED ≥16
ease of oral administration (n=10) and cost (n=7). Conclusions: The HAE expert YEARS WITH PRIMARY IMMUNODEFICIENCIES (PI): LONG
survey demonstrates that AAs are widely used for prophylaxis in many coun- TERM SAFETY, EFFICACY, AND TOLERABILITY.
tries. Experts noted that while AAs are effective they may be associated with R.L. Wasserman1, M. Stein2, I. Melamed3, L. Kobrynski4, J.A. Grant5,
side effects; however, at low doses (i.e., 50–100 mg/day) they may be well tol- S. Gupta6, W. Engl7, H. Leibl7, L.Yel*8, R.I. Schiff8, 1. Dallas, TX; 2. North
erated. In the absence of objective, comparative, randomized, controlled stud- Palm Beach, FL; 3. Centennial, CO; 4. Atlanta, GA; 5. Galveston, TX;
ies of the benefit/risks of new prophylactic therapies compared to AAs no 6. Irvine, CA; 7. Vienna, Austria; 8. Westlake Village, CA.
consensus could be reached regarding switching patients from AAs to other Introduction: IGHy allows for SC administration of IgG at a similar fre-
prophylactic modalities. quency (every 3–4 weeks) and bioavailability to that of intravenous (IV) IgG
(IGIV). Compared with conventional SC-administered IgG (IGSC), IGHy
requires fewer infusions per month (median 1.09 in the pivotal phase 3 study)
using one or occasionally two sites. We report efficacy, safety and tolerability
of IGHy in patients aged ≥16 years who were treated with IGHy for up to 3
years. Methods: Sixty-one patients aged ≥16 years received IGIV for 3 months
followed by IGHy at 3-or 4-week intervals for approximately 18 months; 55
were treated for up to an additional 21 months at the same dose and interval.
rHuPH20 was infused at 75U/g IgG followed by IgG at 108% of the IV dose.
rHuPH20 was discontinued after up to 3 years of exposure; patients were fol-
lowed for an additional 6–12 months. Assessments included rates of adverse
events (AEs), serious AEs (SAEs), and infections; tolerability; and rHuPH20
antibody levels. These studies were approved by the appropriate ethics com-
mittees. Results: The maximum IGHy exposure for patients aged ≥16 years
was 3 years (144 patient-years). Over the full study course, rates of temporally-
Figure 1: Use of attenuated androgens and other therapies for the prophylac- associated AEs/patient-year were 2.99 (local) and 2.78 (systemic; excluding
tic treatment of HAE attacks across centers in US and Europe infections). No SAEs were related to IGHy. The annual infection rate was 3.05
(95% CI: 2.63–3.52)/patient-year, including ramp-up. Of 2307 IGHy infusions
administered (including ramp-up), 98% required no administration changes
P226 due to tolerability concerns or AEs. Thirteen patients ≥16 years developed non-
A CASE OF GATA2 MUTATION PRESENTING WITH CRYPTO- neutralizing anti-rHuPH20 antibody titers ≥1:160 on 1 or more occasion with
COCCAL MENINGITIS. no associated AEs; titers declined despite continuing rHuPH20 in 12 of 13
K. Welch*, New York, NY. patients. No patients developed neutralizing anti-rHuPH20 antibodies. Con-
Introduction: Mutations of the GATA2 gene have recently been implicated clusion: In patients with PI who were treated with IGHy for up to 3 years, infec-
as causes of MonoMAC syndrome, a primary immunodeficiency associated tion rates were low and AE rates were comparable to previously reported rates
with monocytopenia and B and NK cell lymphopenia. The clinical ramifica- for patients treated with IGSC, but with infusion volumes and rates equivalent
tions are broad and include mycobacterial, viral and fungal infections, as well to that of IGIV.
as pulmonary alveolar proteinosis and myelodysplasia. Long-term complica-
tions of the genetic defect include recurrent infections and likely leukemia.
Case Presentation: A 33 year-old Hispanic woman presented to the emergency P228
department with intermittent fever and a severe frontal headache of one week NEW COMPLEX CHROMOSOME ABNORMALITY IN A
duration. Imaging revealed enhancing leptomeningeal nodules, and subsequent PARTIAL DIGEORGE PATIENT ASSOCIATED WITH LATE
lumbar puncture identified cryptococcal meningitis. Her labs were notable for PRESENTATION OF IMMUNE ALTERATIONS.
a white count of 6.3x103 and a monocyte count of zero. On further review, the V. Cavero Chavez*, S.A. Schwartz, Buffalo, NY.
patient’s history was notable for interstitial fibrosis with pulmonary alveolar
Introduction: DiGeorge syndrome (DGS) is characterized by defective
proteinosis, characterized by intermittent hemoptysis for the past 6 years. She
development of the pharyngeal pouch system. The triad is: cardiac anom-
also notes a varied infectious history, including Mycobacterium avium and
alies, hypoplasic thymus and hypocalcemia. Patients are divided in two sub-
Aspergillus fumigatus pneumonias as well as HPV infection with cervical
types: complete DGS, with total absence of thymic tissue that is a type of SCID
intraepithelial neoplasia. A unifying diagnosis had not been offered in the past
and fatal within the first year of life unless treated, and partial DGS which
6 years since she became symptomatic. There was no family history of immun-
usually have not severe variable immunologic defects. The typical deletion
odeficiency. Taking into consideration her disseminated fungal infection and
associated is 22q11.2. Methods: We describe a 26 year old male patient with
monocytopenia, as well as the history of mycobacterial infection, PAP and HPV,
partial DGS and Tetralogy of Fallot surgically corrected, who presented with
GATA2 deficiency was suspected and genetic analysis revealed a frameshift
new recurrent sino-pulmonary infections for the past 8 months requiring mul-
mutation in the gene leading to MonoMAC syndrome. Conclusions: GATA2
tiple courses of antibiotics. He underwent immunological studies including:
deficiency is a relatively newly identified genetic mutation that can lead to a
Lymphocyte subset counts, lymphocyte mitogens an antigen stimulation test,
characteristic presentation of pathologic changes and infectious disease. Patients
quantification of specific antibody titers for S. pneumoniae pre and post
in whom this defect is suspected should undergo genetic sequencing to con-
vaccination, immunoglobulin levels. Results: Immunological evaluation
firm the diagnosis. Ultimate treatment involves bone marrow transplant to pre-
revealed Lymphopenia: Absolute lymphocyte count: 487/mcl(NR:1400-3300),
vent the likely long-term outcome of hematologic malignancy.
CD3:409/mcl(NR: 1000-2200), CD4:143/mcl(NR:530-1300), CD8:231/mcl(NR:
330-920), CD19:25/mcl(NR:110-570), CD56:53/mcl(NR:70-480). Mitogen
stimulation of mononuclear cells revealed a normal response to Pokeweed,
decreased response to PHA and CON-A. Antigen studies included positive
responses to Tetanus and Streptolysine O antigens, decreased responses to MMR
and Candida. Serum immunoglobulins included low IgG (396 mg/dL), low IgA
(59 mg/dL), normal IgM (55mg/dL). Serum antibody responses revealed base-
line S. pneumoniae titers: 8/23 non–protective and post vaccination S. pneu-
moniae titers: 7/23 non-protective. Tetanus toxoid, varicella and Polio anti-
bodies, were protective. Karyotype 45, XY, der (19) t(19;22) (p13.3, q11.2),
-22, no previously described. Conclusions: Our 26 year old partial DGS patient
with complex chromosome abnormality presented with late onset of humoral
deficiency, lymphopenia and impaired T cell function. He required immunoglob-
VOLUME 113, NOVEMBER, 2014 A89
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A90
ABSTRACTS: POSTER SESSIONS
ulin replacement and prophylaxis for opportunistic infections. In this particu-
lar case genetic heterogeneity may play a significant role in time of presenta-
P231
OPTIC NEURITIS IN A 29-YEAR-OLD WITH COMMON VARI-
tion, manifestations and severity of impaired immunity. More understanding
of this genetic variations will help to better know about prognosis of Partial ABLE IMMUNODEFICIENCY TREATED WITH INFLIXIMAB.
DGS patients and continue close follow up even during adulthood. M. Mortezavi*, E. Weis, R.J. Looney, Rochester, NY.
Introduction: Non-infectious complications are now the major cause of mor-
bidity and mortality in patients with Common Variable Immunodeficiency
P229 (CVID). We describe the case of a young woman with CVID who has both
IGG4-RELATED DISEASE PRESENTING AS ABDOMINAL PAIN granulomatous-lymphocytic interstitial lung disease (GLILD) and unilateral
WITH MASS. optic neuritis. Case Presentation: Our patient is a white female who was diag-
L. Zhou*, G.D. Marshall, Jackson, MS. nosed with CVID at age 16 but was not treated due to lack of insurance. At age
26, she presented with headaches, difficulty walking and profound hyopgam-
Introduction: IgG4-related disease is a systemic malady that has been
maglobulinemia (IgG 75, IgA < 5, IgM 32). She had multifocal brain lesions,
reported to involve multiple organ systems, especially the pancreas with plasma
which on biopsy were non-specific lymphoid tissue. Her symptoms and lesions
cell infiltrates. It has also been found to affect skin, lacrimal glands, salivary
resolved after treatment with maintenance IVIG and oral corticosteroids. At
glands, thyroid, pericardium, aorta, lungs, kidneys, pancreas, liver, retroperi-
age 28, she developed dyspnea, a restrictive pattern on spirometry and ground
toneum, breast, and prostate. Regardless of which organ is involved, tissue biop-
glass opacity on CT thorax. She underwent an open lung biopsy, which showed
sies show great histopathological similarities such as diffuse lymphoplasma-
GLILD. All her biopsies stained negative for viral and bacterial agents, and for
cytic infiltrates, abundant IgG4 positive plasma cells, and extensive fibrosis.
IgG4 plasma cells. She was treated with four weekly rituximab infusions for
Methods: Case files of patient was reviewed. Literature reviewed was perofmed
GLILD. She improved symptomatically, but a CT two months later showed sev-
using PubMed searches with the terms “IgG4” and “abdomen”. Results: A 53
eral new lung nodules. Soon after, she developed complete loss of vision in
year old African American female presented to her primary care physician with
her left eye. Ophthalmologic examination showed a bulging optic disc and MRI
chronic abdominal pain. She was referred for specialty care and had unre-
of the orbit showed enhancing optic nerve consistent with optic neuritis. She
markable esophagogastroduodenoscopy and colonoscopy. Subsequent CT scan
improved after three doses of 1 gm IV methylprednisolone and mycophenolic
revealed finding a 28x28x33mm soft tissue mass in the right lower
acid, but relapsed shortly after. MRI of the brain and spine did not show any
abdomen/pelvis mesentery anteriorly abutting several loops of small bowel.
evidence of a demyelinating central nervous system disease. She was treated
Exploratory surgery was performed with abdominal wall mass and partial small
with pulse dose steroids and infliximab. She has regained her vision and con-
bowel resection. The pathological report of the mass showed a storiform pro-
tinues to do well as her steroids are being tapered. Conclusion: There is only
liferation of dense fibrous tissue with marked infiltration by plasma cells.
one previously reported case of optic neuritis in CVID. Patients with CVID can
Immunohistochemistry for IgG4 showed up to 60 plasma cells staining per high
present with granulomatous lesions of the lung, skin and other organs. Optic
power field. There was an associated phlebitis with infiltration by plasma cells.
neuritis is usually seen in demyelinating neurologic disease, such as multiple
Blood IgG4 level was increased. These findings are consistent with IgG4-related
sclerosis (MS). Patients with MS-related optic neuritis usually show a quick
disease. Conclusions: IgG4-related disease is a disease that can involve a wide
and sustained response to pulse treatment with steroids. Given the quick relapse
range of organ systems. The pathological findings of IgG4-related disease have
after stopping steroids and lack of evidence for demyelinating disease, we extrap-
striking similarities. IgG4-related disease has broad clinical heterogeneity with
olated that her optic neuritis may be due to a granulomatous process. We
multi-system involvement. Differentiation of IgG4 related disease from malig-
employed infliximab due to its success in treatment of neurosarcoidosis and
nancy and other autoimmune disorder along with more clinical insight into the
had positive results.
management of this disease are needed. More details of the radiologic mani-
festations of this disease aided by clinical and laboratory findings maybe essen-
tial for the accurate diagnosis of this disease and avoiding unnecessary inva-
sive procedures.
P232
TOPICAL GM-CSF FOR WOUND-HEALING IN LYMPHOPENIC
PATIENT WITHOUT KNOWN NEUTROPHILIC DYSFUNCTION.
P230 B. Geng*, M. Breslin2, M. Garcia-Lloret, R. Roberts, Los Angeles, CA.
OUTCOMES OF SPLENECTOMY IN CVID: A SURVEY OF Neutrophil and monocyte function is crucial for normal wound healing.
44 PATIENTS. GM-CSF enhances function of both neutrophils and monocytes, and has been
J.M. Camacho*, C. Cunningham-Rundles, New York, NY. shown to improve wound healing in neutrophil dysfunction patients. Use of
GM-CSF in wounds of normal patients has produced mixed results. We pres-
Introduction: Common Variable Immunodeficiency (CVID) is a heteroge-
ent case of successful treatment of refractory post-surgical wound with lym-
neous group of disorders characterized by low levels of serum IgG, IgA and
phopenia but without any known neutrophilic defects. 18 month old male with
/or IgM and with loss of antibody production. The diagnosis is most commonly
truncus arteriosus s/p failed surgical repair and subsequent heart transplant
made between the ages of 20 and 40 years of age but children and older adults
developed refractory non-healing post-operative wounds. He had history of
can also be diagnosed with this condition. There are many known clinical man-
recurrent fevers with persistent Coagulase-negative Staph Aureus bacteremia,
ifestations associated with CVID that include acute and chronic infections,
but otherwise negative bacterial, fungal and viral cultures. He received multi-
inflammatory and autoimmune disease as well as an increased incidence of
ple courses of empiric broad-spectrum antibiotics as well as antifungals and
cancer and lymphoma. For patients with inflammatory and hematologic com-
remained afebrile while on therapy, but was unable to stay afebrile off antimi-
plications, there is a risk of developing lymphadenopathy, splenomegaly, autoim-
crobials. Prior to transplant he presented with initial IgG 249, IgA 53 and IgM
mune cytopenia, and/or granulomatous disease. Splenectomy has been used in
23. He had hypoalbuminemia and high alpha-1-antitrypsin in stool(220 mg/dL)
patients with CVID often in the case of refractory autoimmune cytopenia or
suggesting protein-losing enteropathy. He also had severe lymphopenia(200
malignancy. Aside from a recent European report, there is limited information
cells/ml) with CD4 46 cells/ml, CD8 8 cells/ml, CD 19 25 cells/ml and NK 99
as the medical reasons and outcomes have not been well defined. Methods: A
cells/ml. He received IVIG weekly to keep IgG>1000. PMN oxidative index
retrospective chart review on patients seen at an Immunology clinic based a
was 60 ruling out Chronic Granulomatous Disease. Whole Exome Sequenc-
tertiary academic center. The IRB approved chart review encompassed patients
ing found compound heterozygous c.422C>G and c.6064T>C variants of uncer-
seen over the last 20 years and includes 43 patients with CVID and a history
tain significance in PRKDC gene. Mutations of this gene have been impli-
of a splenectomy. Results: The most common reasons for splenectomy in our
cated in forms of autosomal recessive SCID due to defects in DNA repair. No
patient cohort included hypersplenism (n=14), ITP (n=14), AIHA (n=8), pre-
mutations were found in any genes associated with neutrophil defects. GM-
sumed lymphoma (n=2), staging of Hodgkins disease (n=2) and lymphoma
CSF aqueous solution was applied to 2 refractory surgical wounds 3 times daily
(n=1). These were not mutually exclusive reasons. Twenty-five patients had res-
over 2 weeks. Significant improvement in color, size and degree of healing was
olution of their symptoms at some point after splenectomy for either hyper-
observed by multiple physicians and nurses. GM-CSF leads to enhancement
splenism, AIHA or ITP. There were 13 significant complications after splenec-
of granulation tissue development in wound healing, and has been shown to be
tomy in this cohort, which included pulmonary hypertension (n=4),
beneficial for wounds in neutrophil dysfunction patients. Very little data exists
hepatopulmonary syndrome (n=2), sepsis/infection (n=3) fistulae development
in its efficacy in patients with immunodeficiencies other than primary neu-
(n=2), liver decompensation (n=2). Conclusion: There are significant risks asso-
trophil defects. Given that T-cells are a significant source of GM-CSF, and the
ciated with splenectomy in patients with CVID. Splenectomy has been used in
observed improvement in wound healing seen in this patient, use of GM-CSF
patients with CVID and its role needs to be re-examined.
A90 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A91
ABSTRACTS: POSTER SESSIONS
may be considered in refractory wounds in patients with severe primary or
acquired lymphopenia.
P235
INTERACTION BETWEEN SPERM AND MUCOSAL IMMUNITY
AS ASSESSED BY REACTIVE OXYGEN SPECIES GENERATION
P233 IN SEMINAL FLUID OF CHRONIC ABACTERIAL PROSTATITIS
PATIENTS.
CYTOKINE AND SLPI LEVELS IN BLOOD AND URINE OF
PATIENTS WITH CHRONIC CYSTITIS AND PYELONEPHRITIS. G.N. Drannik1, T.V. Poroshina1, V.S. Savchenko1, K.R. Nyrimanov1,
G. Drannik1, F. Gaisenyuk1, V. Driyanska1, N. Stepanova1, L.M. DuBuske*2, L.M. DuBuske*2, 1. Kiev, Ukraine; 2. Gardner, MA.
1. Kiev, Ukraine; 2. Gardner, MA. Background: Spermatozoa and leukocytes in semen may produce reactive
Introduction: Cytokines are key factors in pathological processes includ- oxygen species (ROS) which may have and importance in chronic abacterial
ing urinary tract diseases. Urinary tract mucosa contains various protective prostatitis. Methods: Reactive Oxygen species can be assessed by using nitrob-
effector molecules including antimicrobial peptides and inhibitory proteinases lue tetrazolium (NBT). Levels of ROS can be measured by chemiluminescence.
such as secretory leukocyte protease inhibitor (SLPI) produced by mucosa cells, The NBT test was performed according to the method adapted to ejaculate. In
macrophages and neutrophils which assists in defense against elastase secreted the light microscope with an increase in x 100 counted stained percentage of
by activated neutrophils, and has antibacterial and anti-inflammatory proper- neutrophils and spermatozoa in the ejaculate. To avoid additional procedures,
ties. Levels of cytokines and SLPI in plasma and urine of the patients with determination of ROS in cells was performed using native ejaculate without
chronic infections of urinary system (USCI) including cystitis and pyelonephri- using a density gradient. Cells that had large and small dark blue deposits occu-
tis may be critical in disease pathogenisis. Methods: Levels of interleukin pying more than 50% of the sperm cytoplasm were called positive. Results:
(IL)-1, -4, -6, -10, TNF-, TGF- 1 in peripheral blood of 12 patients with chronic Based on leukocyte concentrations in semen,patients samples were classified
cystitis ( 1st group) and 25 patients with chronic pyelonephritis (2nd group) were into 2 separate groups: leukocytic -sperm group (leukocytic count > 1 x 106
assessed by ELISA methods using STAT FAX-303 PLUS (“Immunotech”, peroxidase-positive leukocytes[PPL]/mL semen; n = 20) and non-leukocytic
“Diaclon”, France; “DRG”, Germany and “Hycult biotechnology” for Human sperm group(leukocytic count 1 x 106 PPL/mL; n = 63). In Group 1 the NBT-
SLPI (Netherlands). Results: Patients in both groups showed high levels of test showed that the overwhelming number of patients (75%) had 60% of sperm
cytokines compared with normal persons (p<0.05). Serum TNF- levels were producing reactive oxygen species (ROS), more than in healthy men with sperm
greater in Group 1 99.6±6.5 versus Group 2 43.5±2.0 pg/ml (p<0,001) but the ejaculate normally characterized by low ROS generation; percentage of NBT
urine levels in Group 1 exceeded the levels in Group 2 by 3-fold (p<0.001); positive sperm is 15.5 ± 4.2%). Antioxidant properties of ejaculate based upon
IL-1, IL-4, IL-6, IL-10, IL-17, IFN-γ, TGF-, though exceeding normal levels, NBT test in 75% of patients was decreased by 90%. Group 2 had ROS pro-
did not differ between Groups 1 and 2. The SLPI level in urine from Group 1 duction by sperm by NBT test in 75% of patients with 56% of sperm produc-
was greater (4171±225) than in Group 2 (1857±203 pg/ml; <0.05). SLPI lev- ing ROS. Antioxidant properties of the ejaculate by NBT test in 75 patients was
els in serum of Group 1 (2052+378) and Group 2 (2240+178) were greater than decreased by 70%. Conclusions: The NBT test can be used to assess the con-
normal but did not differ( 2240±178 versus 2052±316 pg/ml; P>0.05). Con- tribution of seminal leukocytes and defective spermatozoa towards ROS gen-
clusion: TNF-, that was greater in cystitis than in pyelonephritis, The elevated eration in semen. In infertile patients with a chronic abacterial prostatitis pro-
SLPI-levels were seen in urine with levels >3200 pg/ml typical for the pres- duction of ROS by seminal spermatozoa is increased and does not depend on
ence of cystitis. Cytokines and SLPI have an important role in immunity of the quantity of leukocytes in the ejaculate.
the urinary bladder mucosa and antibacterial immunity in USCI.
P236
P234 CONCENTRATION OF TGF-β1 IN URINE OF CHILDREN WITH
OBSTRUCTIVE AND REFLUXING MEGAURETER.
INTERRELATION OF ANTIENDOTOXIN AND HUMORAL
IMMUNITY IN PATIENTS WITH SYSTEMIC LUPUS ERYTHE- G.N. Drannik1, N.A. Kalinina1, V.F. Peterburgskiy1, T.V. Poroshina1,
MATOSUS. V.S. Savchenko1, L.A. Mygal1, L.M. DuBuske*2, 1. Kiev, Ukraine;
D.V. Shaduro1, V.A. Beloglazov2, A.I. Gordienko2, L.M. DuBuske*3, 2. Gardner, MA.
1. Minsk, Belarus; 2. Simferopol, Ukraine; 3. Gardner, MA. Background: Obstruction of the upper urinary tracts results in the re-mod-
Background: Lipopolysaccharide (LPS) or endotoxin of Gram-negative ulation of the tubulointerstitial tissue that is a precondition for nephrosclero-
enterobacteria may help to maintain autoimmune inflammatory responses in sis. TGF-β1 influences each stage of development of tubulointerstitial and
SLE. One indicator of the strength of immunity is antiendotoxin CD14 expres- glomerular lesions. Levels of TGF-β1 in the urine of children with obstructive
sion. Methods: 48 SLE patients were studied. Levels of potential of specific and refluxing megaureter (MU) may be critical in disease development. Meth-
receptors to endotoxin (CD14) on granulocytes in peripheral blood were deter- ods: The TGF-β1 level in urine was assessed in 54 children (1 – 9 years old)
mined by laser double staining flow cytometry using monoclonal antibodies with obstructive (23) and refluxing (31) MU; with or without pyelonephritis
to anti-CD14-REIO-Test® (CD14). Levels of general Ig, IgM and IgG anti- (PN). The control group consisted of 10 healthy children. The TGF-β1 con-
bodies were assessed by ELISA. Circulating immune complexes (CIC) were centrations were assessed by the immuno-enzymatic method with “DRG” (USA)
determined spectrophotometrically by precipitation with polyethyleneglycol test system. Results: TGF-β1 concentration in urine taken from the urinary
(PEG). Results: The levels of CD14 receptors in SLE patients on granulocytes bladder of children with obstructive and refluxing MU statistically exceeded
was 18.57 ± 0.502 fluorescence units (UF). The level of total IgA was 2.041 ± the values in the control group being 15.3 ± 4.35 pg/ml (P<0.001). The distri-
0.059 g/l, IgM was 1.927 ± 0.087 g/l and IgG was 11.34 ± 0.171 g/l. CIC level bution of values in controls was 0 to 5.4 pg/ml, while in children with MU it
was 19.288 ± 1.546 conventional units (CU). In studying the relations of these was 8.8 – 50,9 pg/ml. There was an increase in MU when compared with the
parameters an inverse relationship between CD14 receptor level and the level control of TGF-β1 excretion in the patients with obstructive (15.7 ± 2.1 pg/ml)
of total IgA was found with R= –0.404 (Pearson correlation) at a significance and refluxing MU (16.9 ± 3.8 pg/ml) (P<0.001); no difference was noted
level of p = 0.004. Dependence was described by the formula: IgA = –1.734 * between the groups and was similar to the TGF-β1 excretion in urine of groups
CD14+3.258. There was also a direct significant correlation of receptors CD14 of MU patients complicated by pyelonephritis (16.6 ± 1.6 pg/ml) (P<0.05 ver-
and CIC (R = +0.371; p = 0,009) expressed by the formula: CIC = 41.47 * sus controls). Conclusion: Increase in the TGF-β1 level above normal at the
CD14 – 9.81. Significant relationships between CD14 and IgM and IgG anti- first examination, or continuous increase during examination every 3 to 4
bodies were detected. Conclusions: An association of cellular anti-endotoxin months in comparison with the values of the first examination, are considered
immunity as represented by the CD14 receptor with humoral immunity (IgA, evidence of aggravation of the functional state of the kidney due to the active
CIC) was seen in patients with SLE. This support s arole for LPS of Gram-neg- fibrotic processed in patients with megaureter. TGF-β1 plays a role in the patho-
ative intestinal flora in modulating the immune status of SLE patients. genesis of renal disease in these patients.
P237
RECURRENT LUNG ABSCESSES.
L. Bornstein, R. Herzog*, New York, NY.
Background: The spectrum of autoinflammatory disorders has broadened
in recent years, and interleukin-1 inhibitors have been introduced as success-
VOLUME 113, NOVEMBER, 2014 A91
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A92
ABSTRACTS: POSTER SESSIONS
ful treatment options. We present a 9 month old patient with recurrent lung
abscesses who was successfully treated with an interleukin-1 antagonist. The
P239
ANTI-NEUTROPHIL ANTIBODY POSITIVITY IN SEVERE CON-
case illustrates the importance of early diagnosis and treatment of autoinflam-
matory disorders. Case Report: A female patient presented in the newborn GENITAL NEUTROPENIA.
period with recurrent sterile skin abscesses that resolved after antifungal and S.E. Henrickson*1, S. Jyonouchi2, 1. Haddonfield, NJ; 2. Philadelphia, PA.
antibiotic therapy. She was then well until 9 months of age, when she devel- Introduction: Two toddlers presented with skin abscesses, recurrent acute
oped recurrent sterile lung abscesses which were unresponsive to trials of anti- otitis media (AOM) and neutropenia with both weakly positive anti-neutrophil
bacterial and antifungal treatment, but which resolved completely with Anakinra antibodies and ELANE mutations consistent with severe congenital neutrope-
and Canakinumab therapy. Results: Laboratory testing revealed negative cul- nia (SCN). Here we consider when it may be necessary to consider genetic test-
tures with persistent leukocytosis, thrombocytosis, and elevated acute phase ing even after anti-neutrophil antibodies are positive. Clinical Cases: Patient
reactants. Lung biopsy was sterile and without granulomas, and lung 1: 17-month-old female presented with neutropenia, delayed umbilical cord
parenchyma showed reactive type 2 pneumocyte hyperplasia, chronic intersti- separation, recurrent AOM, oral ulcers and progressive, refractory skin
tial inflammation, and detached acute inflammatory debris. The drained abscess abscesses. She was referred to Infectious Disease where an assessment yielded
showed evidence of acute inflammation and debris with 90% neutrophils, 12% appropriate humoral immune responses, normal B and T cell flow cytometry
macrophages, 4% eosinophils and 4% small lymphocytes. Skin biopsy showed and CBC with ANC 126. With persistent skin abscesses, she was referred to
neutrophilic folliculitis with organizing dermal abscess. Conclusions: The spec- Dermatology and then Immunology. A repeat CBC with ANC of 0 led to urgent
trum of clinical presentations of autoinflammatory disorders is growing. Low referral to hematology and BM biopsy with evidence of blockade in granulo-
threshold for early treatment initiation with IL-1 antagonists is necessary in the cyte development. She was had weakly positive anti-neutrophil antibodies and
setting of persistently elevated inflammatory markers and sterile neutrophilic an ELANE mutation consistent with severe congenital neutropenia (SCN).
biopsy without evidence of infectious etiology. Patient was started on G-CSF and required high dose G-CSF (15mcg/kg/day),
with a full sibling match identified for BMT. Patient 2: 8-month-old male pre-
sented with a history of chronic AOM, perirectal abscess complicated by fis-
P238 tula formation and pneumonia requiring prolonged IV antibiotic therapy. Based
NONCASEATING GRANULOMATOUS DISEASE WITH on recurrent infections, he was referred to Immunology and labs showed per-
EOSINOPHILIC SPONGIOSIS ASSOCIATED WITH POTENTIAL sistent neutropenia, with referral to Hematology and a bone marrow biopsy
COMMON VARIABLE IMMUNODEFICIENCY (CVID). with decreased granulocyte maturation, consistent with severe congenital neu-
B. Patel*, A.S. Nickels, G.W. Volcheck, A.Y. Joshi, Rochester, MN. tropenia. He was found to have weakly positive anti-neutrophil antibodies and
an ELANE mutation consistent with severe congenital neutropenia (SCN). He
Background: Diagnosis of CVID presents a diagnostic challenge given vari- was started on G-CSF, requiring high doses (10mcg/kg/day), with only mod-
able interpretation of the diagnostic criteria. Clinical findings are not included est increases in his neutrophil count. He received an identically matched sib-
as part of the diagnostic criteria, however they can be helpful in further sup- ling bone marrow transplant. Conclusion: We have not identified any prior case
porting or refuting the diagnosis. CVID is associated with many other dis- reports of anti-neutrophil antibody positivity in patients who have SCN. Patients
eases including granulomatous disease, though the mechanism of association with autoimmune neutropenia do not generally have difficulty with recurrent
is unclear. Case Presentation: 47 year old female presented with a progressive infections. Therefore, In neutropenic patients with multiple, severe, recurrent
rash for 2.5 years, lymphopenia and hypogammaglobulinemia, though she infections at an early age and weakly positive anti-neutrophil antibodies, SCN
denied an infectious history. Rash consisted of well circumscribed plaques with should be fully evaluated.
lichenification and mild scaling on the face and trunk. Biopsy of her rash demon-
strated eosinophilic spongiosis and noncaseating dermal granulomatous inflam-
mation with eosinophils. Staining for an infectious etiology was negative. Exam
demonstrated axillary lymphadenopathy and follow up PET/CT demonstrated
P240
A CASE OF IDIOPATHIC CD4 LYMPHOPENIA WITH CUTA-
mild uptake in areas of thickened skin overlying the right breast and left axilla
NEOUS HPV INFECTION.
and multiple prominent right axillary lymph nodes. An excisional right axil-
lary lymph node biopsy demonstrated non-necrotizing granulomatous lym- J. Toh*1, J. Dara1, A. Rubinstein2, 1. New York, NY; 2. Bronx, NY.
phadenitis. Bone marrow biopsy and peripheral flow for lymphoma/leukemia Introduction: Idiopathic CD4 Lymphopenia (ICL) is a disorder defined by
were negative. An angiotensin-converting enzyme (ACE) level was elevated at persistently low CD4 T-lymphocyte count (CD4 < 300/mm3) or CD4 count less
68. Blood work demonstrated a low IgG of 587 (reference range 767-1590mg/dl) than 20% of total lymphocytes on more than one occasion with no evidence of
and a low IgA of 50 (reference range of 61-356mg/dl) but normal IgM and human immunodeficiency virus (HIV-1/2) or human T-cell lymphotropic 1/2
IgE levels. She had a mildly reduced response to the pneumococcal vaccina- (HTLV-1/2) infection and no other secondary causes of immunosuppression.
tion as defined by the 2012 AAAAI working group statement, but she had Other features include high serum IL-7 levels, but poor signaling through IL-
protective titers to diphtheria and tetanus vaccination. A lymphocyte flow report 7. ICL patients can present with autoimmune disease, malignancies or oppor-
demonstrated a decrease in the class switched memory B cells (CD27+M-D- tunistic infections. The most common infections include Cryptococcus, non-
). Conclusion: This case describes granulomatous disease as the primary pres- tuberculosis mycobacterial infection and human papilloma virus (HPV). Very
entation of possible CVID. This patient meets the least stringent diagnostic low CD4 counts (< 150/mm3), low CD8 counts (< 180/mm3; normal 212 –
criteria for CVID, but interestingly does not have an infectious history. How- 1007/mm3) and low natural killer (NK) cell counts (< 100/mm3; normal 97 –
ever, recurrent infections can develop over time in patients who meet criteria 421/mm3) are all associated with increased morbidity. Treatment options con-
for CVID and would not be uncommon in patients who initially present with sidered were immunomodulators such as interleukin-2 (IL-2), interleukin-7
granulomatous or autoimmune disease. Therefore, this patient should be closely (IL-7) and interferon-gamma. We describe a case of cutaneous HPV infection
monitored for infection and consideration of treatment with IVIG. in ICL treated with interferon-gamma. Methods: Case Report Results: A 34
year-old female with known ICL presented to Immunology clinic with digital
warts and severe plantar warts on her left sole which were scraped monthly.
Her previous treatment with IL-7 was ineffective. Warts were unresponsive to
Imiquimod and Urea 40% gel. Laboratory results were significant for a very
low CD4 count at 18/mm3, low NK cells 86/mm3, low CD8 count 69/mm3.
Mitogen and antigen-induced lymphocyte proliferation profile was decreased
to candida, tetanus toxoid, tuberculin purified protein derivative (PPD), phy-
tohemagglutinin (PHA), pokeweed mitogen (PWM) and concanavalin A (Con
A). Serum immunoglobulins and mannose-binding lecithin (MBL) levels were
within normal range. We started treatment with Interferon-gamma-1b 100mcg
three times a week for one month. Our patient’s digital warts resolved and the
plantar warts significantly decreased after one month of treatment with Inter-
feron-gamma-1b. Conclusion: ICL is a rare immunodeficiency that can pres-
ent with HPV infection. Severe cases of cutaneous HPV infection with very
depressed T-lymphocyte counts may be unresponsive to topical or destructive
therapy. However, treatment with immunomodulators such as Inteferon-gamma-
1b may be promising.
A92 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A93
ABSTRACTS: POSTER SESSIONS
this diagnosis should be considered in very young infants with severe infec-
P241 tions and persistent leukocytosis even in the face of largely normal immuno-
EARLY ONSET OF MARKED LYMPHOPENIA, NEUTROPENIA
logic testing.
AND MILD THROMBOCYTOPENIA IN AN AFRICAN-AMERI-
CAN GIRL.
L.E. Moore*1, L. Zhou2, A.B. Yates2, 1. Navarre, FL; 2. Jackson, MS. P243
Rationale: The prevalence of lymphopenia, neutropenia and thrombocy- EOSINOPHILIC ESOPHAGITIS SECONDARY TO FRESH
topenia in children without HIV infection, malignancy, or aplastic anemia is CILANTRO INGESTION.
rare. Frequent infections are the primary clinical manifestation. Methods: An K. Cook*, Orange, CA.
8 year old (yo) African American female with recurrent infections since 1 yo
Introduction: Spice allergy is relatively rare accounting for approximately
was monitored with serial CBC’s, immunoglobulins, lymphocyte subsets, spe-
2% of all observed food allergy. Cilantro has been implicated in IgE mediated
cific antibody titers, and bone marrow biopsies. Results: From 1 yo, this patient
hypersensitivity reactions varying from mild cases of urticaria to anaphylaxis.
had recurrent otitis media, pneumonia, and skin abscesses. She had diffuse ver-
To our knowledge this is the first reported case of eosinophilic esophagitis sec-
rucae plana for the last 2 years. Serial CBCs showed intermittent neutropenia
ondary to cilantro. Case Description: A 31 year old man with no prior medical
(ANC ranging 570-6248 cells/uL), marked lymphopenia (ALC 272-943
history initially presented to gastroenterology clinic with episodic dysphagia
cells/uL), and thrombocytopenia (platelet counts 54,000-120,000 cells/uL).
and food impaction for approximately 7 years. Five years prior, an EGD revealed
Lymphocyte subsets (CD3, CD4, CD8, CD19, and CD3-CD16+CD56+) were
a Schatzki ring which was treated with dilation. He was maintained on Omepra-
persistently very low, as well as low CD27+ B cells (memory B cells). HIV
zole daily but subsequently self discontinued as he was relatively asympto-
PCR, HIV-1/2 antibody, and Parvovirus antibody were negative. Neutrophil
matic. The patient returned after experiencing 6 distinct episodes of dyspha-
associated antibody was negative. Specific antibody titers to Streptococcus
gia associated with increased mucous production over a 2 year period. Repeat
pneumoniae and Haemophilus influenzae b normalized following booster vac-
EGD with biopsy of the lower esophagus showed “strikingly abundant
cines, with fairly good amnestic titers. Quantitative immunoglobulins were nor-
eosinophils, consistent with eosinophilic esophagitis”. He was started on Lan-
mal, until recent onset of low IgM levels. Lymphocyte response to mitogens
soprazole by his gastroenterologist. The patient was asked to record a food diary
and specific antigens were normal. Flow cytometry for paroxysmal nocturnal
of all foods he consumed in relation to episodes of dysphagia. He underwent
hemoglobinuria was negative. 1,2:3,4-diepoxybutane (DEB) clastogen assay
skin prick testing for corn, potato, soy, wheat, chicken, pork, egg, milk, almonds
for Fanconi anemia was negative. Chromosomal study showed 46, XX, with
and peanuts with commercial extracts, all of which were negative. Skin prick
no clonal abnormality. Fluorescent in situ hybridization (FISH) for Myelodys-
testing to aeroallergens was positive for dust mites only. As he noted symptoms
plasia panel and DiGeorge (22q11 and 10p13p14) were negative. Bone mar-
with intake of fresh salsa, the patient later underwent fresh food skin prick test
row at 1 yo showed normocellular trilineage marrow with erythroid and
to tomato and cilantro, which was positive to cilantro. ImmunoCAP testing for
megakaryocytic hyperplasia, and at 5 yo showed hypocellular marrow (60-80%
cilantro/coriander was negative at <0.1kU/L. Lansoprazole was changed to
cellularity) with trilineage maturation and mild 1+ fibrosis. Megakaryocytes
Omeprazole which has been shown to decrease IL-13 and eotaxin 3 levels as
were normal in number and morphology. Chromosomal microarray analysis
additional benefit. With strict cilantro avoidance measures and omeprazole
showed duplication at 10q26.3, confirmed by FISH and a deletion at 11p11.12.
the patient noted no further episodes of dysphagia at three month follow up.
She began daily trimethoprim/sulfamethoxazole prophylaxis 3 years ago, with
Conclusion: This case illustrates the importance of fresh food skin prick test-
very few bacterial infections since then. Conclusions: Patients with lymphopenia
ing in evaluating eosinophilic esophagitis associated with intake of foods and
and frequent infections may benefit from antibiotic prophylaxis. Monitoring
spices. Although skin prick with commercial extracts and ImmunoCAP test-
with appropriate lab tests can guide the treatment plan. Given this patient’s
ing are used as first line in diagnostic work ups, fresh food skin prick testing
onset of verrucae plana, additional evaluation for WHIM syndrome may be
with cilantro should be considered with a suggestive history.
warranted.
P242 P244
AN UNUSUAL CASE OF ASPARAGUS ALLERGY.
SEVERE AND EARLY PRESENTATION OF NEMO/IKBKG
DEFICIENCY. K.M. White1, P.H. Wong*2, R.A. Gomez1, M.H. Tucker3, 1. Lackland AFB,
TX; 2. San Antonio, TX; 3. Bonita, CA.
V. Nayima*, P. Atkinson, Birmingham, AL.
Rationale: Asparagus food allergy is rare and usually associated with pos-
Rationale: Nuclear factor-κB essential modulator (NEMO) deficiency is a
itive skin or serum IgE testing. Methods: A 26 year-old male reported urticaria
combined immunodeficiency due to hypomorphic mutations in the X-linked
over 3 years associated with eating asparagus. He had no history of atopy.
IKBKG gene. Symptoms include antibody deficiency, susceptibility to nontu-
Skin testing with fresh asparagus was negative. An open challenge resulted in
berculous mycobacteria, and ectodermal dysplasia. Female carriers of severe
a diffuse urticarial rash within minutes of ingestion. Serum IgE via Immuno-
loss of function mutations in IKBKG have a condition called incontinentia pig-
CAP was less than 0.35 KU/L. Serum was analyzed using ELISA testing.
menti. Case description: A Caucasian male infant (36.5wga) presented to clinic
Asparagus was lyophilized and protein content determined by a modified Lowry
at one week after circumcision with MRSA infection of the penis. Five weeks
technique. The food extract was added to ELISA plate wells, incubated, washed,
later he again presented for evaluation with thrush, severe eczema, bloody stools,
blocked, and re-washed. Serum was then added and the plate was incubated,
and a submandibular mass that grew MSSA. At 12 weeks of age he was admit-
washed, and anti-human IgE antibody was added. After incubation, plate was
ted for fever, diarrhea, and leukocytosis (WBC 40K) and was found to have
washed and pNPP AP substrate was added. Optical density readings were taken
significant eosinophilia ( 24%) and severe panhypoimmunoglobulinemia. He
at 30 minutes and at 1,2,3, and 20 hours. Inhibition ELISA testing was also
was treated with empiric antibiotics and IVIG. At 14 weeks the patient was
performed, with asparagus inhibited by itself. Controls included cord blood as
admitted for weight loss and leukocytosis (WBC 45K) and was found to have
well as serum from an atopic patient. The assay was performed in triplicate.
a right inguinal abscess that grew MSSA and multiple bowel flora. He was re-
Results: The patient’s serum exhibited IgE binding to asparagus antigens at a
admitted at 5 months for a planned bone marrow transplant after positive genetic
ratio of 2.5 times that of the cord blood control. The binding was completely
tests. He continued to have poor weight gain and experienced multiple infec-
inhibited by preincubation of the serum with asparagus. An atopic control exhib-
tions during the pre-transplant interval with MSSA, MRSA, coagulase nega-
ited binding to asparagus which was also inhibited by asparagus. Immunoblot
tive staphylococci. Results: Complement tests, CD11/CD18 protein expres-
was performed and was negative. Conclusions: To our knowledge this is the
sion, mitogen stimulation, neutrophil respiratory burst, FOXP3 protein
first patient with asparagus allergy manifesting as systemic urticaria with neg-
expression, NK cell function, T and B cells and subsets including Th17 cells
ative fresh asparagus skin testing and negative commercial serum IgE testing
by flow, and HHV 6/7/8 PCR testing were all normal/negative. CD45 RO (naïve)
demonstrated to have specific IgE to asparagus via an IgE-ELISA inhibition
CD4+ T cells were decreased by flow. During his evaluation it was discovered
assay. Further testing is needed to identify the specific allergens involved.
that his mother had an extensive patchy hyperpigmented birthmark that was
consistent with incontinentia pigmenti. Gene sequencing revealed a hemizy-
gous IKBKG gene (H413D) variant which has not been published as mutation
or benign polymorphism, not identified in 1200 individuals with Euro-
pean/African American ancestry, and predicted to be pathogenic. Conclusion:
This early and severe presentation of NEMO/IKBKG deficiency suggests that
VOLUME 113, NOVEMBER, 2014 A93
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A94
ABSTRACTS: POSTER SESSIONS
listlessness and non-bloody diarrhea requiring ICU admission status post inges-
P245 tion of homemade sweet potatoes. The first instance occurred at 6.5 months of
PINEAPPLE ANAPHYLAXIS.
age for which she was diagnosed with a viral sepsis syndrome in the setting of
K.E. Bruner*1, R. Gomez2, J. Freiler2, K. White2, A. White3, 1. Lackland a positive parainfluenza culture. Symptoms then reoccurred at 7.5 months of
AFB, TX; 2. San Antonio, TX; 3. San Diego, CA. age when she was fed sweet potato mixed with pear, and then she was diag-
Introduction: Pineapple is rarely reported to cause anaphylaxis. We pres- nosed with FPIES. She had already been consuming cheerios, oatmeal, banana,
ent two cases of pineapple anaphylaxis with evidence of IgE antibodies to peas, and broccoli. The patient’s mom had questions regarding the proper tim-
pineapple. Methods: Two patients with histories consistent with pineapple ana- ing to introduce new foods. Results: There are no specific recommendations
phylaxis underwent ImmunoCAP and immunoblot testing to pineapple and one regarding introduction of new foods for patients with FPIES. Among infants
underwent skin prick testing. Results: Both patients reported regularly eating with solid food FPIES in one study, 80% reacted to more than one food and
pineapple prior to their initial episode of anaphylaxis. Pt 1 initially experienced 65% were previously diagnosed with cow’s milk and/or soy FPIES. Typically,
a feeling of throat swelling, lip numbness and unsettled stomach after eating if a patient is tolerating foods from one group then other foods of that group
pineapple but did not associate it as an allergic reaction. Three weeks later, he are considered OK to eat. It is suggested that in children with solid food FPIES,
ate 4-5 pieces of pineapple and experienced generalized sweating, prolonged the introduction of grains, legumes and poultry should be delayed until the first
abdominal cramping and recurrent vomiting that lasted approximately one hour. year of life. Conclusions: It was recommended to our patients mother that she
He had no rash or angioedema. His skin testing revealed a 15x40mm wheal continue foods she is currently tolerating. It was also recommended that mom
and flare to fresh pineapple, 15x50mm to pineapple extract. He was skin test can introduce other fruits one at a time. Since she was eating peas, it was sug-
negative to bromelain, other fruits including fig, kiwi and papaya, and an aeroal- gested that she try lentils as her next legume. Since she was eating oat, quinoa
lergen panel. An immunoblot was performed which revealed a faint band at 23 was recommended as her next grain. Mom was instructed to continue breast
kD consistent with bromelain and correlated with a weak positive Immuno- feeding. She was instructed to wait to until one year of age to consume soy and
CAP of 0.42 kU/L. Patient 2 developed generalized hives, angioedema, throat milk. Approximately two weeks later she had tolerated lentils, quinoa and blue-
closing, diarrhea and a sense of impending doom shortly after ingesting pineap- berries at home without any issues. She still had not exposed her to dairy.
ple. She received steroids, epinephrine and IV fluids in the emergency depart-
ment with resolution of symptoms over 90 minutes. Her initial ImmunoCAP
to pineapple was 2.24 kU/L. She deferred pineapple skin prick testing due to P247
fear of recurrent reaction. Repeat ImmunoCAP was obtained one year later and ANAPHYLAXIS DUE TO TOPICAL PRAMOXINE.
was negative at <0.35 kU/L. Immunoblot performed at that time was also neg- S.J. Kim*, C.K. Lin, B.J. Goldberg, Los Angeles, CA.
ative suggesting that her sensitivity may have waned over the intervening 12
Introduction: Pramoxine is a local anesthetic agent that has long been used
months. She was not interested in food challenge. Conclusion: Pineapple can
in various surgical specialties. A few cases of contact dermatitis have been
cause anaphylaxis with presence of IgE demonstrated on skin prick testing,
described; however anaphylaxis has not been reported. Though pramoxine has
ImmunoCAP and immunoblot. Bromelain was identified on immunoblot as
low sensitizing potential, it was implicated in our case of anaphylaxis. Case
the reactive substance. One patient’s ImmunoCAP converted to negative after
Description: A 47-year-old Caucasian man was brought to our emergency
one year indicating that sensitivity to pineapple may decrease over time.
department with a widespread pruritic rash, generalized edema, chest pain, dys-
pnea, nausea, and diaphoresis. An acute anaphylactic reaction was suspected,
and treated immediately. Serum laboratories revealed tryptase 2.6 (< 15.8
mcg/L), total IgE 44.5 (< 113 kU/L), and WBC 14.7 (4-11 x 1000/mcL) with
no eosinophils. He had applied Neosporin + Pain Relief® cream (active ingre-
dients neomycin, polymyxin B, and pramoxine) to a cut on his hand minutes
prior to his anaphylactic event. He had applied topical Neosporin® ointment
(without the Pain Relief component) numerous times previously without any
adverse reaction. At allergy clinic follow-up 5 weeks later, topical application
of Neosporin + Pain Relief® cream to the patient’s forearm produced a 30 x
30-mm wheal. Skin prick testing revealed a 7 x 9-mm wheal to histamine and
to pramoxine. Testing of neomycin and polymyxin B were negative. In vitro
assays were performed (ImmunoCAP 1000 System, Thermo Fisher Scientific,
Waltham, MA). Direct coupling of pramoxine to the solid phase was not fea-
sible as there was no free amine or hydroxyl group available on this compound.
Specific IgE against polymyxin B, neomycin, and bacitracin were not detected
in the patient’s serum (< 0.1 KUA/L). Therefore, of the 3 active components in
Neosporin + Pain Relief® cream, pramoxine was the culprit. Discussion:
Pramoxine is used only for surface anesthesia; therefore sensitization should
not entail any risk of future systemic reaction. Low sensitization potential has
been demonstrated, and patients sensitive to other topical anesthetics showed
no sensitization to pramoxine. To our knowledge, ours is the first report describ-
ing anaphylaxis to topically applied pramoxine. Ready access to the systemic
circulation seems to be a prerequisite for the development of anaphylaxis. In
contemplating topical therapy, patients should consider the integrity of the skin.
Patient 1 skin prick test. Pin=pineapple extract, F.P.=fresh pineapple
If the skin barrier is compromised, an anaphylactic reaction is possible. Physi-
cians should be aware that topical pramoxine may give rise to life-threatening
anaphylaxis.
P246
A CASE OF FPIES TO SWEET POTATO.
B. Navetta*, Manhasset, NY. P249
Introduction: FPIES is a non-immunoglobulin E (IgE) mediated GI food CHARACTERISTICS OF FOOD ALLERGY IN AN ADULT POP-
hypersensitivity which presents with profuse, repetitive vomiting, often with ULATION.
diarrhea leading to dehydration and lethargy after ingestion of a food allergen. T. Shankar*, A. Petrov, M. Fajt, Pittsburgh, PA.
The exact mechanism is unknown, however it is thought that the ingestion of
Introduction: Food allergies appear to be increasing in prevalence (Boyce,
an allergen causes local inflammation (mediated by T cells) leading to increased
JACI 2010), and aside from physical effects, lead to poor quality of life. Epi-
intestinal permeability and fluid shift. The most common allergens are cow’s
demiologic studies to date have focused on the pediatric population, and as a
milk or soy protein, however solid food proteins can also elucidate these symp-
result, there is limited data on food allergies in adults, with available data sug-
toms. The common solid food that has been known to cause FPIES is rice.
gesting differences in both presentation of allergy and underlying causative
Methods: An 8 month old female with a history of atopic dermatitis presented
agents in these two groups. This study aimed to evaluate the characteristics of
for initial consultation after she developed two episodes of profuse vomiting,
A94 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A95
ABSTRACTS: POSTER SESSIONS
patients presenting to an adult Allergy/Immunology clinic with food allergy as testinal disorders, the most frequent was esophageal and functional dyspepsia.
well as to determine the most prevalent food allergies reported. Methods: We Positive test to aeroallergens were 76.19% Betulaceae (Birch 45.2%, Alnus
conducted a retrospective analysis of demographic and clinical data from adult 30.95%), 78.57% Oleaceae (42.5% Fraxinus, Olive 35.09%), 38.09% Aster-
patients seen in an outpatient university Allergy/Immunology Clinic from June aceae (Red Oak 38.09%), 38.9% Fagaceae (Thistle 38.09%). For food were
2010-June 2014 for a complaint of food allergy as evidenced by ICD-9 code positive test were peach, orange and plum 38.09%, raw apple, 35.7% raw broc-
of 995.7. Data: Preliminary results from evaluation of 10 patients demonstrated coli, celery, 33.3% raw carrot, strawberry, 30.95% raw onion, corn, banana,
a female predominance (90%) with onset of symptoms in adulthood (age >18 kiwi, hazelnut and almond 28.57%. Positivity LTP extract 14% and 12% were
yrs) in 80%. Concomitant environmental allergy was present in 80% of patients positive to profilins. Conclusion: In our populations, 12% of patients were pos-
and drug allergy, most commonly penicillin, was present in 40% of patients. itive to profilins and 14% to LTPs. 100% was positive to multiple pollens which
Though nearly all of the patients (70%) had previously sought medical care is similar to the prevalence reported worldwide 10-30% patients with pollen
for food allergy, only 1 patient had injectable epinephrine previously prescribed allergy react to profilin. This is of great importance since it is considered a
at the time of visit. The most common food allergen reported and confirmed risk factor for developing food allergies as well as most of these patients with
was shrimp (40%). Other confirmed food allergies were fish (salmon), peanuts oral allergy syndrome. Also it has been reported that anaphylaxis is more com-
and tree nuts. 80% of patients reported allergy to >3 foods, but only 30% had mon in patients with only sensitization to LTPs.
positive serum specific IgE testing to >3 foods. Of the 10 patients evaluated,
40% opted to have no further testing beyond the initial visit and were discharged
with injectable epinephrine prescription, training for use if needed, and an action
plan for food avoidance. Conclusion: Our preliminary data suggests that onset
of food allergy can occur in adulthood and is under-recognized and undertreated
by the medical community. Specific features such as female gender and co-
existence of both environmental and drug allergies may help to identify adult
patients with food allergy. Additional analysis with larger sample sizes is needed
to confirm these associations.
P250
RITUXIMAB AND FOOD ALLERGY IN A PEDIATRIC LIVER
TRANSPLANT PATIENT.
W.M. Rassbach*, J. Wang, New York, NY.
As a monoclonal antibody to CD20 on B lymphocytes, rituximab is used
to treat a variety of lymphoproliferative disorders, including post-transplant
lymphoproliferative disorder (PTLD). It is unknown to what degree this ritux-
imab-induced B cell depletion could affect pre-existing IgE-mediated food
allergy in children. We report a case of a three year-old patient who developed
hives and lip swelling to peanut butter after receiving tacrolimus immunosup-
pression for a living-related liver transplant performed for biliary atresia. She
subsequently developed PTLD and underwent treatment with rituximab, lead- P252
ing to B cell depletion. In the allergy evaluation that followed, her skin prick DIFFERENCES IN COMMON FOOD ALLERGENS, FOOD
testing revealed a negative histamine control, and her serum food-specific IgE ALLERGY SEVERITY AND THRESHOLDS IN 16 COUNTRIES.
levels were undetectable. As the patient had demonstrated clinical reactivity to R. Gupta*1, J. Blumenstock1, L. Bilaver2, L. Harada3, M. Marchisotto4,
peanut despite a negative serum peanut IgE, her case raises the question as to 1. Chicago, IL; 2. DeKalb, IL; 3. Toronto, ON, Canada; 4. New York, NY.
whether rituximab could have played a role in masking her IgE-mediated sen- Introduction: Food allergy prevalence is increasing globally in developed
sitivity to peanut and other foods. Rituximab targets actively dividing B cells, and developing countries especially in children. Avoidance is still the best rec-
particularly those present in the peripheral blood, and as such her case may indi- ommendation for management; however, strict avoidance impacts quality of
cate that the IgE active in food allergy is being produced by B cells in a body life. Recent research has focused on food allergen threshold levels, the lowest
compartment other than the peripheral blood. amount of an allergen that causes a reaction. After years of recommendations
to avoid allergens at any level, it is unknown how families feel about thresh-
olds. This would be the first international study of its kind to examine differ-
P251 ences in food allergy types, severity, diagnosis, and opinions about food allergy
FREQUENCY OF SENSITIZATION TO FOODS RICH IN LIPID thresholds between countries. Methods:A survey prepared by FARE gathered
TRANSFER PROTEINS AND PROFILIN IN PATIENTS OF THE consumer comments on allergen thresholds and was distributed by patient organ-
NATIONAL INSTITUTE OF RESPIRATORY DISEASES. izations in 16 countires to 10,225 respondents. The survey was designed for
R.D. Ruiz Morales*, M.D. García Cruz, V.A. Maldonado Ríos, F. Ramírez people with food allergies, family members, and caregivers who purchase their
Jiménez, G.F. Pavon Romero, M. Molina Macip, N. Camacho Ordonez, food. The public was asked to comment on opinions of food allergen thresh-
P. Sanchez de la Vega Reynoso, Z. Perez Estrella, L.M. Teran Juarez, olds, current approaches to managing food allergies through food selection,
Mexico City, DF, Mexico. and knowledge of thresholds. The results from these surveys were compiled
and analyzed by country. Results: Differences were observed by country in per-
Background: Food allergy affects many millions of people. May develop
cent of respondents with food allergy to each of the common food allergens,
allergy to almost any food, but in some cases it may be result of cross-reactiv-
percent of respondents with history of severe reaction, source of diagnosis,
ity between food and inhalant allergens. Clinical manifestations can be included
knowledge of food allergy thresholds, and willingness to consume food that
in the pollen-food syndrome sometimes leading to trigger anaphylaxis. These
contains varying amounts of food allergen. Overall, while 73% of respondents
syndromes are related to proteins like pathogenesis related protein family (PR-
said they had some knowledge about allergen thresholds, only 21% said they
10), profilin, lipid transfer proteins (LTPs) and storage proteins. Objective:
would buy a product that contained levels of an allergen low enough that it
Determine the frequency of sensitization to food rich in LTPs and profilin in
would not trigger a reaction and 4% would purchase a product with levels only
patients of the National Institute of Respiratory Diseases of Allergy and
capable of triggering a mild reaction. Responses to all threshold opinion ques-
Immunology Department. Methods: Patients were seen at the Allergy and
tions varied by country. Conclusion: There are clear differences in food allergy
Immunology Department with suggestive symptoms of oral allergy syndrome
in each of the countries participating in the survey. This is the first study of its
or food anaphylaxis underwent questionnaire to determine functional gas-
kind to analyze the breakdown of food allergy by common allergen and sever-
trointestinal disorders with subsequent skin testing to aeroallergens and food
ity in each country and opinions about the emerging topic of food allergen
with LTPs and profilins. Results: 42 patients were included, 75.6% were female
thresholds. It is apparent that if a food contains an allergen a family is avoid-
and 26.1% male, mean of IgE levels were 506 IU / L, average eosinophils in
ing, they may avoid the food regardless of thresholds and allergen levels. As
peripheral blood 422 cells/mm3. 71% of patients had symptoms of oral allergy
this topic develops, patient input is crucial as industry labeling policy shifts.
syndrome, 19% anaphylaxis to food intake and 60% had functional gastroin-
VOLUME 113, NOVEMBER, 2014 A95
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A96
ABSTRACTS: POSTER SESSIONS
P253 P255
FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME A SPOONFUL OF SUGAR HELPS BUDESONIDE GO DOWN.
(FPIES) CAUSED BY AVOCADO. J. Lee*, M.M. Shuker, T.F. Brown-Whitehorn, A. Cianferoni, L.M. Gober,
A. Doshi*, S. Leonard, San Diego, CA. C.A. Liacouras, R. Verma, J.M. Spergel, Philadelphia, PA.
Introduction: FPIES is a non-IgE mediated gastrointestinal food hyper- Introduction: Two methods for treating Eosinophilic Esophagitis (EoE)
sensitivity that is characterized by delayed profuse, repetitive vomiting and are off-label use of swallowed steroids and dietary therapy. For swallowed
often diarrhea. Severe cases can also lead to acute dehydration; weight loss and steroids, the two main options are swallowing MDI actuated inhaled corticos-
failure to thrive can result if chronic. We present 2 cases of FPIES caused by teroids or mixing budesonide into a slurry with sucralose (Splenda®). How-
avocado, a trigger that has not previously been reported. Case 1: A breastfed ever, some patients do not like sucralose. We describe our treatment success
10-month-old male presents with a history of reflux, failure to thrive, and inter- with other agents used to mix budesonide. Methods: We retrospectively reviewed
mittent vomiting, which improved with restricted maternal diet. Solids were data from EoE patients treated with swallowed budesonide at our institution.
introduced at age 6 months, one new food every 3 days. At age 7 months, 4 EoE was defined using the standard consensus criteria of > 15 eosinophils/hpf
hours after the second introduction of peas, zucchini and avocado he experi- (eos/hpf) on esophageal biopsy after ruling out gastroesophageal reflux. A value
enced 2 episodes of emesis and appeared lethargic, returning to baseline by of < 15 eos/hpf was considered adequate improvement. IRB approval and
the next morning. Shortly thereafter he developed repetitive vomiting, pale- informed consent was obtained from all subjects. Results: Fifty-four children
ness, limpness and lethargy 3 hours after the second introduction of sweet potato between ages 2 and 18 years (mean 6 years) were treated with swallowed budes-
and squash, separately. He was treated in the emergency room with ondansetron onide over a 5 year period and had sufficient data to review. The most com-
and intravenous fluids for the sweet potato episode, but recovered at home after mon delivery vehicle for budesonide was sucralose (n=32, 59%). A variety of
the squash reaction. At this point he was diagnosed with sweet potato and squash other agents were also used: 11 patients used apple sauce; 3-honey; 1-alter-
FPIES. At age 10 months, avocado was ingested again, and 3 hours later he nating apple sauce and ice cream; 1-banana puree; 1-pear sauce; 1-hot cocoa
developed vomiting, limpness, paleness and lethargy. He recovered at home mix; 1-rice cereal; 1-tapioca starch; 1-xanthan gum; and 1-compounded for-
after 3 hours. Case 2: A 9-month-old female was diagnosed with rice and milk mulation. Of the patients using sucralose, 30 of 32 patients had improvement
FPIES after presenting with a history of repetitive vomiting 2 hours after inges- on their esophageal biopsy (down to mean 1.27 eos/hpf). Of the 11 apple sauce
tion of rice and milk-based formula, separately, at age 7 months. When avo- patients, 7 had improvement (down to mean 2.86 eos/hpf); 2 had no repeat
cado was introduced at age 12 months, she developed repetitive episodes of biopsy data, 1 did not respond adequately to budesonide, and 1 improved after
vomiting 5 hours after ingesting a few bites. She was back to baseline a few switching to honey as the vehicle. The patient on alternating apple sauce and
hours later. Discussion: These cases highlight avocado as an unreported trig- ice cream went from 60 eos/hpf to 20 eos/hpf. All 3 honey patients had improve-
ger of FPIES. The most common causative foods are milk, soy, rice, and egg; ment (down to mean 3.33 eos/hpf). The patients using banana puree, pear sauce,
reactions to meats, nuts, and other fruits/vegetables have also been reported. hot cocoa mix, xanthan gum and the compounded formulation as the vehicle
To our knowledge, there have not been any other published accounts of avo- all had improvement to 0 eos/hpf. The patients using rice cereal or tapioca starch
cado FPIES. There is often a delay in FPIES diagnosis due to the lack of bio- did not have improvement on their biopsies. Conclusion: Splenda® (sucralose)
markers and because symptoms overlap with other more common disease is the most commonly used delivery vehicle for swallowed budesonide in EoE
processes, such as gastroenteritis. FPIES is a clinical diagnosis based on his- patients. Various other vehicles can also be effective, including apple sauce,
tory and it is important to not overlook uncommon or unreported triggers. pear sauce, honey, banana puree, hot cocoa mix, xanthan gum, and a com-
pounded formulation. Certain other agents, however, may not work.
P254
SEVERE SEQUELLAE OF DEHYDRATION IN A FOOD PRO- P256
TEIN-INDUCED ENTEROCOLITIS PATIENT. WHEN IGE CRASHES THE PARTY: A CASE OF BEER ALLERGY.
M.A. Ruffner*1, J. Fiedler2, 1. Rutledge, PA; 2. Philadelphia, PA. J.D. Waldram*1, K.M. Woessner2, 1. La Jolla, CA; 2. San Diego, CA.
Introduction: Food protein-induced enterocolitis syndrome is a non-IgE Case Presentation: An 18-year-old female presented to the allergy clinic
mediated food allergy which usually presents in infancy as severe vomiting and with concern for beer intolerance. She drank beer for the first time at age 14
diarrhea. Onset of symptoms are delayed and occur 2-4 hours after ingestion and did not develop symptoms. Recently she has begun experiencing lip and
of a food. FPIES patients often experience delayed diagnosis due to the simi- mouth tingling and numbness within minutes of drinking beer, followed by nau-
larity of its presentation with gastroenteritis, surgical abdominal processes, and sea and vomiting within an hour. She denied additional skin or mucosal symp-
sepsis. This case illustrates that acute FPIES can be accompanied by profound toms, and never experienced respiratory symptoms. Her symptoms occur with
dehydration and a high clinical suspicion should be maintained for the poten- a single sip of beer and are present with every exposure, regardless of the type
tial clinical sequelae of severe dehydration. Case Summary: An exclusively of beer. She has consumed wine, champagne and distilled spirits without any
breastfed 6 week old full-term male was transferred to our institution for the adverse reactions, both before and since her symptoms with beer. She also
management of hyponatremia and severe dehydration in the setting of one week reports developing a localized, urticarial rash if beer is splashed on her skin.
of worsening vomiting and diarrhea. He had been breastfeeding and gaining Her past medical history is remarkable for migraine headaches for which she
weight appropriately until six days prior to admission. He presented with 6 days takes sumatriptan as needed. She has no history of atopic diseases. She has no
of multiple episodes of nonbloody, nonbilious emesis and four days of loose known drug allergies. Her mother has allergic rhinitis. Review of systems and
nonbloody diarrhea. He had 0.52 kg weight loss over one week’s time, with physical examination were unremarkable. Skin prick test was adequate for inter-
exam notable for sunken fontanel, delayed capillary refill and dry mucous mem- pretation with a histamine control of 10mm/34mm and a negative glycerin con-
branes and laboratory workup notable for hyponatremia to 128. He required trol. She reacted to barley extract (5mm/17mm), malt extract (10mm/32mm)
rehydration with IV fluids, and during the hospitalization he developed per- and Pabst Blue Ribbon beer (10mm/40mm). She did not react to corn, hops,
sistent rightward eye deviation which progressed to apnea and bradycardia wheat or yeast (Saccharomyces cerevisiae) extracts. She was instructed to avoid
requiring resuscitation. Electrolytes were normal and brain MRI/MRV revealed beer and food or beverages containing barley or malt. Follow up was arranged
thrombosis of the medullary vein. Hypercoagulable workup was negative. to perform oral food challenges to barley and malt, in order to determine whether
Workup of his vomiting and diarrhea was negative, including: LFTs, lipase, she can safely consume foods containing these ingredients. Conclusion:
infectious stool studies, testing for neurometabolic disorders, anti-enterocyte Although uncommon, beer allergy should be suspected in a patient who reacts
and FoxP3 staining as well as normal IgA staining of intestinal biopsies. His adversely to beer and whose presentation is consistent with an allergic reac-
hospital course was significant for multiple attempts to restart breastmilk or tion. Several beer components have the potential to cause IgE-mediated reac-
alimentum complicated by recurrence of vomiting and diarrhea; he was even- tions, including barley, hops and yeast, in addition to various other starches.
tually able to tolerate NeoCate with resolution of GI symptoms and was dis- [3] Identifying a specific allergen, although often difficult, will assist in aller-
charged home on NeoCate. At followup visits he demonstrated normal growth gen avoidance and prevent unnecessary dietary restrictions.
pattern and stooling pattern on NeoCate, but at 28 months had accidental expo-
sure to a small amount of milk and developed diarrhea secondary to this expo-
sure. Although FPIES is a diagnosis of exclusion given the severity of symp-
toms in this patient, and the reproducibility of his symptoms, FPIES to milk
seems is the most likely diagnosis.
A96 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A97
ABSTRACTS: POSTER SESSIONS
year. Patient demographics were analyzed to see if specific populations were
less likely to achieve goal. Methods: An IRB approved retrospective chart review
of all current immunotherapy patients at one allergy clinic was conducted. Only
patients on standardized dust mite mix immunotherapy for at least 1 year were
included. One year was chosen as the inclusion time because it would take 32-
43 weekly incremental dosage steps to achieve maintenance goal if there were
no gaps or skipped doses, assuming a starting dose of 0.05cc of 0.001AU-0.1AU
and a goal maintenance dose of 0.20cc of 10,000AU using our standard pro-
tocol for dose advancement. Patients were excluded if they received combina-
tion shots with other allergens in the same extract vial or were on house dust
immunotherapy. Chi-square analysis was used to determine if differences were
significant. Results: There were 36 females and 46 males that met criteria for
the study. Of the 82 patients, 41 (50%) achieved their pre-set maintenance
goal target in 1 year. 41.7% of females achieved goal maintenance compared
to 56.5% of males. However, chi-square analysis found no significant gender
difference in achieving goal (p=0.182). Participants were also stratified into 3
different age groups: young (0-39 years), n=35, middle aged (40-59 years),
n=32, and elderly (60+ years), n=15. The age group differences were statisti-
cally significant (p=0.003). Odds ratio showed middle aged patients were 3.2
times and elderly patients 6.0 times more likely to achieve goal when compared
to young patients. Also, patients with no reactions to immunotherapy were
significantly more likely to achieve maintenance goal than those who had reac-
tions (p=0.027). Patients who consistently visited clinic for immunotherapy
treatments were more likely to achieve goal than those who missed appoint-
P257 ments (p≤0.000). Conclusion: Patients who consistently visit clinic for
QUANTITATIVE BENEFIT AND RISK ASSESSMENT OF TIMO- immunotherapy treatments, have no major reactions to treatments, and are older
THY GRASS AND SHORT RAGWEED SUBLINGUAL are more likely to achieve maintenance goal in a timely manner. Patients younger
IMMUNOTHERAPY TABLETS IN THE TREATMENT OF ALLER- than age 40 are at high risk of not meeting goal. Improving success for this pop-
GIC RHINITIS. ulation may indicate a need for more resources for them such as special adher-
A. Kaur1, G. Koch2, S. Durham3, J.M. Portnoy4, Z. Li1, J. Maloney1, ence counseling on each injection visit and visit reminders.
H. Nolte*1, 1. Whitehouse Station, NJ; 2. Chapel Hill, NC; 3. London, United
Kingdom; 4. Kansas City, MO.
Introduction: Number needed to treat (NNT) and needed to harm (NNH)
is a quantitative approach to assess relative efficacy and safety of a treatment.
Lower NNT indicates more effective treatment, and higher NNH indicates safer
treatment. NNTs for allergic rhinitis (AR) treatments depend on the clinical
response definition and range from 3–34.5; NNHs depend on the frequencies
and types of adverse events and range from 13–167. We determined the NNT
and NNH to quantify benefit-risk for 2 sublingual immunotherapy tablets (SLIT-
T) approved for Timothy grass- (and related grasses) or short ragweed (RW)-
induced AR. Methods: For grass SLIT-T 2800 BAU (MK-7243; Merck/ALK-
Abelló), efficacy data vs placebo from 3094 subjects was used for NNT; safety
data from 4195 subjects was used for NNH evaluation. For RW SLIT-T 12 Amb
a 1-U (MK-3641; Merck/ALK-Abelló), efficacy data vs placebo from 644 sub-
jects was used for NNT; safety data from 1814 subjects was used for NNH eval-
uation. In the absence of an established responder definition, NNT was based
on 2 exploratory post-hoc responder definitions. Definition 1 required the sub-
ject to achieve ≥50% well days during the pollen season (grass full season,
RW peak season). Well days were days with no rescue medication use, and with
the worst score as none or mild for each of the 6 symptoms measured. Miss-
ing data were considered non-well days. Definition 2 required the subject’s total
combined symptom and medication score (TCS) to be ≤3 (~10% of the observed
endpoint range to be considered a responder). NNH was based on the adverse
event rate for epinephrine use and treatment-related systemic allergic reactions,
the safety endpoints of clinical concern. IRB approval and informed consent
was obtained from all subjects. Results: For grass SLIT-T, the NNT was 7.9 P259
using the ≥50% well days definition and 9.4 using the TCS ≤3 threshold. NNH GASTROINTESTINAL ADVERSE EVENTS IN SUBJECTS
was 305 based on epinephrine use and 303 based on systemic allergic reac- RECEIVING RAPIDLY DISSOLVING TIMOTHY GRASS OR
tions. For RW SLIT-T the NNT was 10.3 using the ≥50% well days definition SHORT RAGWEED SUBLINGUAL IMMUNOTHERAPY
and 16.4 using the TCS ≤3 threshold. NNH was 230 based on epinephrine use TABLETS.
and no harmful effect could be determined based on systemic allergic reac-
tions. Additional sensitivity analysis corroborated the NNT results. Conclu-
J. Maloney*1, D. Skoner2, G. Berman3, B.Q. Lanier4, A. Kaur1, H. Nolte1,
sions: Grass SLIT-T and RW SLIT-T have favorable benefit-risk ratios based 1. Whitehouse Station, NJ; 2. Pittsburgh, PA; 3. Minneapolis, MN; 4. Fort
on NNT and NNH. Worth, TX.
Introduction: Saliva may carry concentrated allergen extract to areas of
the gastrointestinal (GI) tract distal to the mouth and throat when swallowed
P258 after administration of sublingual immunotherapy tablet (SLIT-T) or liquid.
ANALYSIS OF DUST MITE IMMUNOTHERAPY MAINTENANCE Unabsorbed contents of a rapidly dissolving SLIT-T may be swallowed fewer
GOAL ACHIEVEMENT. times than that of a SLIT-T that takes minutes to dissolve or liquid extracts,
minimizing allergen exposure contact with the non-mouth/throat GI tract. There-
N. Khoiny*1, J. Chase2, J. Sheikh2, M. Kaplan2, 1. Long Beach, CA; fore, it is important to characterize the non-mouth/throat GI adverse events
2. Los Angeles, CA. (AEs) associated with each SLIT product. We report the GI AEs associated
Introduction: This study investigated the percentage of patients who with 2 SLIT-T products approved for the treatment of Timothy grass (and cross-
achieved their pre-set dust mite immunotherapy maintenance goal within 1 reactive grasses) or short ragweed (RW)-induced allergic rhinitis that dissolve
VOLUME 113, NOVEMBER, 2014 A97
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A98
ABSTRACTS: POSTER SESSIONS
within seconds under the tongue. Methods: AE data from 8 randomized, dou- failed to respond to multiple courses of destructive modes of treatment, includ-
ble-blind, placebo-controlled trials (24-week to 1-year) of daily Timothy grass ing cryotherapy, salicylic acid 6%, imiquimod 5%, and electrodessication These
SLIT-T 2800 BAU (MK-7243; Merck/ALK-Abelló) were combined into adult patients were started on immunotherapy consisting of intralesional injections
and pediatric safety pools. AE data from 4 randomized, double-blind, placebo- of 0.4 mL of a Candida albicans antigen preparation (Hollister-Stier) with a
controlled trials (two 52-week trials and two 28-day trials) of daily RW SLIT- concentration of 1,000 PNU/mL. This treatment was given at 3-week intervals
T 12 Amb a 1-U (MK-3641; Merck/ALK-Abelló) were combined into a 28- with an average of 3.5 sessions. Results: The patients’ plantar warts achieved
day safety pool. Results: A total of 3173 subjects received grass or RW SLIT-T complete and striking resolution without scarring (Figure 2a, 2b) following
and 2836 subjects received placebo (Table). The majority of treatment-related immunotherapy with multiple intralesional injections of Candida albicans anti-
GI AEs were associated with the oral mucosa (Table). Dysphagia and dyspep- gen. No relapses have been reported to date (average follow-up ~2.3 years).
sia did not affect a large number of subjects but did occur at a numerically The mechanism of action is still uncertain, but most likely due to the stimula-
higher rate than in the placebo group for each pool (Table). Abdominal pain tion of a T-helper type 1 (Th1) cell cytokine response leading to induction of
and gastroesophageal reflux disease (GERD) occurred in ≤1% of subjects receiv- local and distal cell-mediated immune responses. The most common side effect
ing grass or RW SLIT-T. Only 1/2116 (0.05%) subjects receiving grass SLIT- was pain during intralesional injections. Conclusion: The striking favorable
T (none for RW SLIT-T) reported eosinophilic esophagitis; this AE was mild response to multiple stratified intralesional immunotherapeutic injections of
in intensity, did not result in study discontinuation, and was not assessed as Candida albicans antigen in these 4 patients with recalcitrant warts unrespon-
treatment-related by the investigator. No serious GI AEs were reported in any sive to usual destructive forms of treatment, provides support for a promising
subject receiving grass or RW SLIT-T. Only 2/2116 (0.09%) subjects receiv- effective and safe mode of immunomodulator therapy.
ing grass and 1/1057 (0.09%) receiving RW SLIT-T discontinued due to treat-
ment-related abdominal pain or GERD. Conclusions: GI AEs associated with
grass SLIT-T and RW SLIT-T treatment predominately affected the oral mucosa.
Non-mouth/throat GI AEs were infrequent and rarely resulted in study dis-
continuation.
Treatment-related GI AEs in ≥1% of Subjects in Any Treatment Group
P261
THE EFFICACY OF THE UNITED ALLERGY SERVICES SELF-
ADMINISTERED IMMUNOTHERAPY PROTOCOL.
F.M. Schaffer*1, L. Garner1, M. Ebeling2, T. Hulsey2, A. Naples1, 1. San
Antonio, TX; 2. Charleston, SC.
Introduction: Controversy exists about the efficacy of self-administered
SCIT protocols. We previously reported the safety study results of the United
Allergy Service (UAS) self-administered SCIT protocol (WAO J 2014, 7 (Suppl
1), 24). We now report the results of the efficacy trial. Methods: An IRB/HAC
approval and informed consent was obtained from all research subjects. A ret-
rospective efficacy study was completed for 56 control patients and 60 SCIT
patients (in accordance with the UAS protocol). Enrollment criteria in part
included only patients: who demonstrated positive SPTs to at least 3 of 6 com-
AE=adverse event; GI=gastrointestinal; SLIT-T=sublingual immunotherapy mon study site geographic allergens (Timothy, Bermuda, Cedar, Oak, Ragweed,
tablet. and Cocklebur) and had associated seasonal symptomology. The study con-
trasted statistical assessment of pretreatment and ongoing symptom scores (SS),
medication scores (MS), SS + MS, and quality of life scores (QOL). Results:
P260 Assessment demonstrated significantly improved SS (SMD: -1.74; 95% CI: -
IMMUNOMODULATORY THERAPY OF RECURRENT AND 2.15, -1.34; p< 0.0001), MS (SMD: -1.17; 95% CI: -1.50, -0.84; p< 0.0001),
RECALCITRANT WARTS: EFFICACY USING CANDIDA SS+MS (SMD: -1.61; 95% CI: -2.01, -1.21 ; p< 0.0001) and QOL (SMD: -
ALBICANS ANTIGENS. 1.01; 95% CI: -1.40, -0.63; p< 0.0001) for the treatment group during
T.M. Nsouli*1, L.E. Firestone2, N.Z. Diliberto2, S.T. Nsouli2, J.A. Bellanti2, immunotherapy (mean of 16 months) compared to pre-immunotherapy scores.
1. Burke, VA; 2. Washington, DC. A comparison of SS, MS, SS+MS, and QOL scores demonstrated significant
treatment group improvement in contrast to the control group (p<0.0001). There
Rationale: Recalcitrant warts are benign epidermal cutaneous skin lesions
was a 41% improvement in SS+MS for the treatment group compared to the
caused by human papillomavirus (HPV), commonly seen in clinical practice.
control group (p< 0.0001) and a comparison to a recently published meta-analy-
Plantar warts are associated with severe pain and tenderness when walking or
sis of 12 SCIT studies (DiBona et al, JACI 2012; 130: 1097-1107) demonstrated
standing and are not only particularly bothersome for patients, but can also sig-
equivalent efficacy. Conclusions: These efficacy results, and our previously
nificantly affect their quality of life. The treatment of recurrent plantar warts
reported safety results, demonstrate that a carefully designed and implemented
usually poses a therapeutic challenge to the clinician and is often difficult,
self-administered SCIT protocol is safe and efficacious.
painful, time-consuming and, in some cases, unsatisfactory. Optimal treat-
ment with absence or low recidivism has not yet been established for recurrent
and recalcitrant warts. (Nofal A, et al. Am J Clin Dermatol 2013;14:253) Meth-
ods: Four patients (27 y/o WM, 24 y/o WF, 33 y/o WF and 44 y/o WF), each
with severe and recalcitrant plantar warts affecting their ambulation due to
significant pain (Figure 1), were studied. Immunologic assessment of all patients
revealed normal humoral and cell-mediated immune function. The warts had
A98 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A99
ABSTRACTS: POSTER SESSIONS
clusions: The incidence, nature and severity of adverse reactions reported dur-
P263 ing treatment with the 300IR (9,000 BAU) 5-grass pollen sublingual tablet were
SAFETY OF SUBCUTANEOUS SPECIFIC ALLERGIC
similar in the adult and pediatric populations.
IMMUNOTHERAPY IN PATIENTS WITH ALLERGIC RHINITIS
FROM THE NATIONAL INSTITUTE OF RESPIRATORY DIS-
EASES FROM 2005 TO 2014. P265
G.F. Pavon Romero, J.I. Rodríguez Gaspar*, M.E. Cervantes Malagon, SAFETY OF THE 5-GRASS POLLEN SUBLINGUAL TABLET IN
F. Ramírez Jimenez, M.H. García Cruz, L.M. Teran Juarez, Mexico City, MONO- AND POLY-SENSITIZED PATIENTS WITH GRASS
DF, Mexico. POLLEN-INDUCED ALLERGIC RHINOCONJUNCTIVITIS.
Background: Subcutaneous specific allergic immunotherapy (SSAI), in D.B. Golden*1, K. Abiteboul2, R.K. Zeldin2, 1. Baltimore, MD; 2. Antony,
conjunction with drug therapy and patient education, is the cornerstone for the France.
treatment of allergic diseases. So far SSAI is the only treatment able to mod- Background: The efficacy of the 5-grass pollen sublingual tablet has been
ify the allergic disease in addition to helping prevent the development of asthma. demonstrated in both mono- and poly-sensitized patients with grass pollen-
Complications of SSAI are rare but possible. Currently there is insufficient induced allergic rhinoconjunctivitis. Using pooled data from across the devel-
information to describe the incidence of adverse reactions in daily clinical prac- opment program, we report the safety profile according to the sensitization sta-
tice. Collecting information that assesses SSAI’s safety could help us to iden- tus of patients at study entry. Methods: Eight double-blind, placebo-controlled
tify allergens, dose, time of administration, and other factors in order to reduce studies were conducted worldwide. Patients (age 5-65 years) with medically
the incidence of potentially serious reactions. Objective: To assess the safety confirmed grass pollen-induced allergic rhinoconjunctivitis for at least 2 years
of SSAI in patients with allergic rhinitis from 2005-2014. Methods: Patients were enrolled. IRB/EC approval and informed consent was obtained from all
with Allergic rhinitis who received SSAI between 2005-2014 were included. patients. At entry, all patients underwent skin testing to 5-grass mix or timo-
SSAI was performed using Alk-Abello® allergens with monthly applications thy and a panel of geographically relevant aeroallergens. Mono-sensitized
according to Mexican guidelines for immunotherapy. An adverse reaction to patients had a positive test to 5-grass mix/timothy alone and poly-sensitized
SSAI (AR) was considered as the presence of any clinical manifestation pro- ones had a positive test to 5-grass/timothy and at least one other aeroallergen.
posed by the European Academy of Allergy and Clinical Immunology. Fre- Of note, these other sensitizations were not to cause potential confounding
quency analysis and survival curve were performed using the software SPSS symptoms of allergy during the period of evaluation. Adverse events were mon-
v. 21. Results: 1,923 patients were included, 3.7% (72) had AR, the average age itored throughout the study. Treatment-emergent adverse events (TEAEs) were
of the patients was 19 years, 63% were female and 37% male, 67%(48) were analyzed descriptively. Results: A total of 951 patients were mono-sensitized
children and 33% (24) adults. The most frequent allergens detected by skin (active=587; placebo=364) and 1,560 were poly-sensitized (active=927;
test and reported as managed with SSAI were Dpt (94%) and Ash (25%). Of placebo=633). Similar incidences of TEAEs were reported in active and placebo
the 72 patients with AR, 66% were polisensitized (POL) and 34% monosensi- groups, whether patients were mono-sensitized (77.2% vs. 67.9%) or poly-sen-
tized (MONO); 39% received SSAI with standardized allergens (E), 25% with sitized (76.7% vs. 70.9%) and the most frequently reported TEAEs (i.e., appli-
non-standard () and 26% a combination. The average duration of the SSAI treat- cation site reactions such as oral pruritus, throat irritation, mouth edema) were
ment was 15 months, and the AR was presented during the build up phase at reported at similar incidences in actively-treated mono- and poly-sensitized
1:1 concentration in E and 1:200000 in . POL patients developed AR earlier patients. Mono- and poly-sensitized patients receiving active treatment reported
than MONO patients, and the same phenomenon was observed when compar- serious TEAEs with similar frequencies (1.5% and 1.4%, respectively). Actively-
ing vs E. Of those with AR 65% of the cases had mild reactions, 24% moder- treated patients withdrew due to TEAEs with similar frequencies whether mono-
ate and 11% severe. Conclusion: The polisensitized pediatric patients who sensitized (31 patients [5.3%]) or poly-sensitized (46 patients [5.0%]). Con-
received SSAI with non-standardized allergen had mild adverse reactions that clusions: Treatment with the 5-grass pollen sublingual tablet was similarly well
were presented earlier in our population. tolerated in mono-sensitized and poly-sensitized patients.
P264 P266
SAFETY OF THE 5-GRASS POLLEN SUBLINGUAL TABLET IN EFFICACY OF HOUSE DUST MITE SUBLINGUAL
ADULT AND PEDIATRIC POPULATIONS WITH GRASS IMMUNOTHERAPY TABLET ON OCULAR SYMPTOMS USING
POLLEN-INDUCED ALLERGIC RHINOCONJUNCTIVITIS. AN ENVIRONMENTAL EXPOSURE CHAMBER.
R.K. Zeldin*1, Y. Amistani1, L. Paolozzi1, U. Wahn2, 1. Antony, France; H. Nolte*1, J. Maloney1, H.S. Nelson2, D.I. Bernstein3, Z. Li1,
2. Berlin, Germany. R. Zieglmayer4, P. Zieglmayer4, P. Lemell4, F. Horak4, 1. Whitehouse
Background: The efficacy and safety of the 5-grass pollen sublingual tablet Station, NJ; 2. Denver, CO; 3. Cincinnati, OH; 4. Vienna, Austria.
has been demonstrated in patients with grass pollen-induced allergic rhinocon-
Rationale: Allergic rhinitis is frequently associated with ocular symptoms
junctivitis. Using pooled data from across the development program, we eval-
which can have a significant impact on quality of life and daily activity. The
uated the safety by age group. Methods: Patients (age: 5-65 years) with med-
effect of house dust mite (HDM) sublingual immunotherapy tablet (SLIT-T)
ically confirmed grass pollen-induced allergic rhinoconjunctivitis for at least
on ocular symptoms is unknown; therefore, the efficacy on ocular symptoms
2 years were included in one of eight double-blind, placebo-controlled studies
of MK-8237 (Merck/ALK-Abelló), a HDM SLIT-T currently under clinical
conducted worldwide. IRB/EC approval and informed consent was obtained
development, was evaluated in an environmental exposure chamber trial. Meth-
from all patients. Those who received 300IR (9,000 BAU) 5-grass pollen sub-
ods: Adults with HDM-induced allergic rhinitis with/without conjunctivitis
lingual tablet or placebo were considered for the age subgroup (i.e., chil-
and/or asthma (n=124) received daily MK-8237 12 DU, 6 DU, or placebo for
dren/adolescents [5-17 years] and adults [≥18 years]) analysis. Adverse events
24 weeks in this randomized, placebo-controlled, double-blind, single-site trial.
were monitored throughout the studies. Treatment-emergent adverse events
HDM exposure challenges of 6 hours duration were conducted at screening
(TEAEs) were analyzed descriptively. Results: 1,878 adults (300IR=1,038;
and weeks 8, 16, and 24. The total ocular symptom score (TOSS) was assessed
placebo=840) and 312 children/adolescents (300IR=154; placebo=158) were
and was the sum of 2 scores: gritty/red/itchy eyes and watery eyes, scored on
included in the analysis. TEAEs were reported by 78% of adults and 84% of
a 0 to 3 point scale (maximum=6). Total nasal symptom score (TNSS) was also
children/adolescents receiving active treatment and 66% and 79% of those
assessed and was the sum of scores for runny nose, blocked nose, sneezing,
receiving placebo. The most commonly reported TEAEs by both actively-treated
and itchy nose, scored on a 0 to 3 point scale (maximum=12). IEC approval
subgroups were application site reactions (e.g., oral pruritus, throat irritation,
and informed consent was obtained from all subjects. Results: Overall 83% of
mouth edema), with similar incidences. The incidence of severe TEAEs was
subjects reported ocular symptoms at the screening chamber challenge. Improve-
similar in actively-treated adults (102 patients [9.8%]) and children/adolescents
ments of 34.1% and 67.9% in TOSS with MK-8237 12 DU versus placebo were
(17 patients [11.0%]). Similar percentages of adults and children/adolescents
observed at week 8 (mean difference: −0.61; P=0.023) and week 24 (mean
receiving the 300IR sublingual tablets withdrew from the studies due to TEAEs
difference: −1.27; P<0.001), respectively. Similarly, an improvement of 41.2%
(49 [4.7%] adults and 7 [4.5%] children/adolescents), mainly as a result of
with MK-8237 6 DU was observed at week 24 (mean difference: −0.77;
application site reactions. Three serious TEAEs (hypersensitivity, angioedema
P=0.023). Efficacy for nasal symptoms was also demonstrated with improve-
and diarrhea) considered related to the study drug by the investigator were
ments of 20.4%, 30.1%, and 48.6% in TNSS with MK-8237 12 DU versus
reported in adults; none were reported in children/adolescents. No actively-
placebo observed at week 8 (mean difference: −1.37; P=0.007), week 16 (mean
treated patients received epinephrine and there were no ICU admissions. Con-
difference: −2.08; P<0.001), and week 24 (mean difference: −3.62; P<0.001),
VOLUME 113, NOVEMBER, 2014 A99
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A100
ABSTRACTS: POSTER SESSIONS
respectively. Similarly, improvements of 17.8% and 26.6% with MK-8237 6 treatment and had not restarted while 18 patients (9.0%) had stopped treatment
DU were observed at week 16 (mean difference: −1.23; P=0.032) and week 24 and subsequently restarted, some on several occasions. The average number of
(mean difference: −1.98; P=0.003), respectively. Both MK-8237 doses were RIT hours for patients still on treatment (M=13.37) was significantly higher
well tolerated. No anaphylactic reactions or reactions requiring epinephrine than for patients who had stopped treatment (M=8.20) even if they restarted
were reported. Conclusions: A dose- and time-dependent effect of HDM SLIT- (M=2.64) [F(2, 196) = 15.57, p = .000]. Further analyses were conducted clas-
T MK-8237 on ocular and nasal symptoms was observed, with maximum effi- sifying patients into groups dependent upon the number of RIT hours they
cacy of 67.9% for ocular symptoms observed at week 24 with the 12 DU dose. received, if any. Patients receiving 1-10 RIT hours had significantly lower treat-
ment duration (M=8.3) than patients receiving no RIT (M=14.4), 11-20 RIT
hours (17.2), or more than 20 RIT hours (18.77) [F(3,195) = 14.17, p = .000].
P267 While RIT hours do play a role in treatment duration, results of these analyses
SAFETY OF THE SUBLINGUAL TABLET OF HOUSE DUST MITE suggest that another variable, possibly related to commitment to treatment, may
ALLERGEN EXTRACTS IN AN ENVIRONMENTAL EXPOSURE also be involved in the prediction of adherence.
CHAMBER STUDY: FOCUS ON ASTHMA-RELATED
SYMPTOMS.
M. Roux*1, W.H. Yang2, P. Devillier3, R.K. Zeldin1, 1. Antony, France;
P269
EFFICACY OF SUBCUTANEOUS IMMUNOTHERAPY IN
2. Ottawa, ON, Canada; 3. Suresnes, France.
PATIENTS POLYSENSITIZED COMPARED TO PATIENTS
Background: The efficacy and safety of a sublingual tablet of house dust MONOSENSITIZED WITH ALLERGIC RHINITIS AND ASTHMA.
mite (HDM) allergen extracts was tested in an environmental exposure cham-
ber (EEC) study, in which patients were exposed to a stable concentration of D. Rivero Yeverino, M. Molina Macip*, M.H. García Cruz, G. Pavon
HDM allergens. Here, we focus on asthma-related symptoms. Methods: Adults Romero, F. Ramírez Jimenez, L. Teran Juarez, Mexico City, DF, Mexico.
(18-55 years) with medically confirmed HDM-associated allergic rhinitis were Background: The World Health Organization estimates that 40% of the
randomized in this double-blind study to receive either placebo or active treat- world population suffers any type of allergic disease lilke allergic rhinitis (AR),
ment at the doses of 500IR, 300IR or 100IR with daily administration for 6 currently the mainstay of treatment of AR is the use of topical steroids, how-
months. Patients with intermittent asthma controlled with therapies consistent ever the specific allergy immunotherapy (SAIT) is the only treatment capable
with GINA treatment step 1 could be enrolled. IRB approval and informed con- of modifying the natural course of the disease. Currently the studies that eval-
sent was obtained from all patients. During the study, patients participated in uate the SAIT in patients with AR describes a favorable clinical efficacy, how-
five 4-hour allergen challenges in the environmental exposure chamber. Analy- ever the are performed in monosensitized patients, the results of these investi-
ses were performed to evaluate the incidence of bronchospasm, asthma and gations have traspolated to polysensitized, without having assessed the same
asthma-related symptoms, such as dyspnea, cough, wheezing, occurring in rela- clinical consistency and biological support. Objective: To evaluate the effi-
tion to the EEC challenges (i.e., peri-EEC periods defined as the day of and cacy of subcutaneous immunotherapy in patients polysensitized (POL) versus
the day after an allergen challenge) and that occurring outside of these peri- monosensitized (MONO) with allergic rhinitis and asthma. Methods: We
ods. Results: 355 patients received at least 1 dose of the investigational prod- enrolled asthmatic patients with AR; skin prick test were developed with ALK-
uct and comprised the safety set (500IR=93; 300IR=86; 100IR=89; bello allergens classifying the groups of study in POL if there are two or more
placebo=87); 12.7% had asthma. During the peri-EEC periods, the incidence allegens positives in the test and MONO if only has a one. SAIT was devel-
of bronchospasm, asthma and asthma-related symptoms was similar across oped according Mexican guideline for immunotherapy. All participants real-
treatment groups (range: 36.6%-44.9%). The incidence of these symptoms out- ized spirometry, Asthma Control Test, control of AR symptoms with statement
side of the peri-EEC periods was approximately half of that during these peri- of ARIA in each phase of build up and measure of eosinophils, levels of Ig E
ods (range: 16.1%-21.3%). The majority of patients experiencing these events and inhaled steroids dosage at the begging and end of this phase. Statics was
did not have asthma at study entry. Seven patients in the 3 active treatment developed using Wilcoxon test compared 0 time vs 4 time in each grupo and
groups (none with asthma at baseline) withdrew due to peri-EEC asthma symp- U Mann Whitney between the groups with SPSSv21. Results: 23 patients par-
toms. No Patients withdrew outside of these periods. All events were of mild ticipated, were xx female and xx male, the average of age was xx years old, 12
or moderate intensity; 2 resolved without treatment, 4 with inhaled β2-agonist, patients integrated monosensitized group and 11 polysensitized, the principal
and 1 with an OTC treatment. Conclusions: Treatment with sublingual tablet allergen was Dpt in both groups, the average of allergens in POL group were
of house dust mite allergen extracts tested in an environmental exposure cham- 5; FEV1 increases in each group (p = 0.006), there were decrease of 32 % in
ber was generally well tolerated and without adverse effects on respiratory func- the dosage of inhaled steroid (p = 0.001) and increased of ACT questionnaire
tion. During the challenges, asthma-related symptoms of mild-moderate sever- score (p = 0.001),there were not differences in these variable when comparing
ity were reported in patients receiving placebo or active treatment. POL vs MONO. The levels of IgE,eosinophils and evaluation of symptoms of
AR were similar in 0 vs 4 time in each and both groups. Conclusions:
Immunotherapy has the same efficacy in polysensitized patients as in mono-
P268 sensitized
ALLERGY IMMUNOTHERAPY ADHERENCE: DOES RUSH
MAKE A DIFFERENCE?
S.P. Raschal, J.M. Holcombe, B.G. Carlton*, Chattanooga, TN. P270
SAFETY OF SUBCUTANEOUS SPECIFIC ALLERGIC
Traditionally, immunotherapy consisted of regular (weekly/bi-weekly) injec-
IMMUNOTHERAPY IN PATIENTS WITH ALLERGIC RHINITIS
tions over several months until a maintenance stage was reached. Rush
FROM THE NATIONAL INSTITUTE OF RESPIRATORY DIS-
immunotherapy (RIT) allows the patient to achieve a maintenance stage much
quicker than traditional immunotherapy. The purpose of the current study was EASES FROM 2005 TO 2014.
to identify whether patients were more or less adherent to treatment when they G. Pavon, I. Rodriguez*, M. Cervantes, F. Ramirez, M. Garcia, L. Teran,
received RIT. A systematic chart review was conducted on all new patients who Mexico City, DF, Mexico.
started immunotherapy in 2011. Variables of interest included demographic Background: Subcutaneous specific allergic immunotherapy (SSAI), in
factors (age, gender, etc.), potential control variables (systemic reactions, prick conjunction with drug therapy and patient education, is the cornerstone for the
test results, and asthma diagnosis), RIT (hours), and duration of treatment treatment of allergic diseases. So far SSAI is the only treatment able to mod-
(months). Overall, 199 patients began allergy immunotherapy at the clinic in ify the allergic disease in addition to helping prevent the development of asthma.
2011. The average patient was 33 years old, female (65.3%), and Caucasian Complications of SSAI are rare but possible. Currently there is insufficient
(81.9%). The majority of patients had systemic reactions during their initial information to describe the incidence of adverse reactions in daily clinical prac-
screening (92.4%) and was also prick test positive (96.0%). The patients were tice. Collecting information that assesses SSAI’s safety could help us to iden-
almost evenly divided by asthma diagnosis (yes=59.1%; no=40.9%), but analy- tify allergens, dose, time of administration, and other factors in order to reduce
ses showed no significant differences between these two groups in regards to the incidence of potentially serious reactions. Objective: To assess the safety
RIT hours and treatment duration. Patients were classified into one of three of SSAI in patients with allergic rhinitis from 2005-2014. Methods: Patients
groups at the time of chart review – (1) still on treatment, (2) stopped treatment with Allergic rhinitis who received SSAI between 2005-2014 were included.
without restart, and (3) stopped treatment with restart(s). Of the 199 patients SSAI was performed using Alk-Abello® allergens with monthly applications
who started treatment in 2011, 97 (48.7%) were still receiving treatment with according to Mexican guidelines for immunotherapy. An adverse reaction to
an average therapy duration of 14 months. Eighty patients (42.2%) had stopped SSAI (AR) was considered as the presence of any clinical manifestation pro-
A100 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A101
ABSTRACTS: POSTER SESSIONS
posed by the European Academy of Allergy and Clinical Immunology. Fre- 8/55), and Gastroenterology (13%, 7/55). The remaining 50% of consults were
quency analysis and survival curve were performed using the software SPSS placed by 11 other subspecialty services. Outpatient A/I follow up was rec-
v. 21. Results: 1,923 patients were included, 3.7% (72) had AR, the average age ommended for 31 (56%) of the 55 new patients evaluated in the hospital. Of
of the patients was 19 years, 63% were female and 37% male, 67%(48) were these 31 patients, 55% (17/31) presented to our clinic for scheduled follow up
children and 33% (24) adults. The most frequent allergens detected by skin evaluation. Established patients of the A/I service accounted for 27 inpatient
test and reported as managed with SSAI were Dpt (94%) and Ash (25%). Of consults on 22 unique patients. Fifty-two percent (14/27) of these consults were
the 72 patients with AR, 66% were polisensitized (POL) and 34% monosensi- for co-management related to a previously diagnosed immunodeficiency. The
tized (MONO); 39% received SSAI with standardized allergens (E), 25% with majority (67%, 18/27) of consults for established A/I patients were placed by
non-standard () and 26% a combination. The average duration of the SSAI treat- ID (20%, 11/55) and Hospital Pediatrics (13%, 7/55). Conclusions: Our review
ment was 15 months, and the AR was presented during the build up phase at of inpatient A/I consultations demonstrates the need for expert evaluation of
1:1 concentration in E and 1:200000 in . POL patients developed AR earlier both allergic and immunologic disorders in the inpatient setting. Additionally,
than MONO patients, and the same phenomenon was observed when compar- inpatient evaluation by the A/I service is helpful for establishing outpatient A/I
ing vs E. Of those with AR 65% of the cases had mild reactions, 24% moder- follow-up for patients new to the A/I service. Understanding the inpatient con-
ate and 11% severe. Conclusion: The polisensitized pediatric patients who sultation patterns has implications for A/I fellow training, resident and med-
received SSAI with non-standardized allergen had mild adverse reactions that ical student education, as well as patient care.
were presented earlier in our population.
P273
P271 ASSESSING EPIPEN® PROFICIENCY AMONG INTERNAL MED-
GASTROESOPHAGEAL REFLUX DISEASE (GERD) THERAPY ICINE INTERNS.
DOSING MISSES THE MARK. S. Bodner*, S. Akbar, R. Sejour, S. Chaudhry, M. Tamuz, A.M. Jongco,
J.L. Mutnick*, Morris, MN. Manhasset, NY.
Rationale: Gastroesophageal reflux disease (GERD) is a chronic disease Introduction: Many clinicians under-utilize and incorrectly dose epineph-
and very common in the evaluation of chronic cough. Oftentimes, GERD is rine in anaphylaxis. Residents report being confident in diagnosing and man-
silent and patients do not realize they are experiencing symptoms. When treated, aging anaphylaxis despite limited clinical experience with this relatively uncom-
the dosing of medication is often a significant component in ensuring improve- mon condition. We designed a simple training module to teach interns how to
ment and efficacy in therapy. Yet, under-dosing seems to be a common prob- use an EpiPen®, as well as developed and validated a scoring tool to reliably
lem that is not meeting the needs of appropriate therapy. Methods: 28 patients measure an intern’s autoinjector proficiency. Methods: We developed the
with GERD (diagnosed by EGD or classic symptoms) were evaluated in clinic. EpiPen® proficiency assessment tool (E-PAT), a two-part tool including a
The patients had failed conventional proton-pump inhibitor therapy with checklist that outlines 8 steps of proper autoinjector use and questions about a
omeprazole 20mg once daily. Patients were randomized to two groups. 14 clinician’s prior EpiPen® experience. We recruited 58 interns from an ACGME-
patients were placed on omeprazole 20mg twice daily; the remaining 14 patients accredited internal medicine training program at an academic medical center
were placed on omeprazole 40mg once daily. 12 weeks of therapy were per- during orientation where they underwent skills training. This study was IRB
formed and the REFLUX-QUAL (RQS) quality of life (QoL) questionnaire approved. Each intern participated in a 30-minute training module, followed
was used to evaluate symptom improvement. Results: The REFLUX-QUAL by an assessment. First, the interns watched a part of the manufacturer’s instruc-
(RQS) questionnaire is a validated and simple tool consisting of 8 items cov- tional video. Second, an allergist recapped the key points in the video and
ering the principal domains of the patients’ QoL. A score is rapidly obtained encouraged questions. Third, the interns used EpiPen® trainers to practice on
ranging from 0 to 100; the higher the score, the better the QoL. The median themselves and their colleagues, with the opportunity to receive feedback from
score amongst both groups at Week 0 was 36. Patients in the Omeprazole 20mg the observing allergist. Finally, two independent coders (an allergist and a sen-
twice daily group had RQS scores improve by an average of 16 points at Week ior resident with allergy training) used the E-PAT to individually assess each
12 whereas the 40mg once daily group RQS scores improved by an average of intern’s EpiPen® proficiency. Results: All 58 interns participated in the study.
44 points at Week 12, an almost three-fold improvement. Conclusions: GERD Prior to this activity, 74% of the interns reported having never used an EpiPen®
is a common diagnostic consideration in the Allergy and Asthma practice. It trainer, none have used an EpiPen® in the past year and 7% have ever used an
has been my finding that increased frequency (qday vs. BID) of failed omepra- EpiPen®. Over one-third (37%) of the interns knew someone who uses an epi-
zole doses do not alleviate or improve symptoms. Rather, it appears that an nephrine autoinjector. After the training, the interns’ mean EpiPen® proficiency
increased dose of omeprazole is associated with much improved REFLUX- score was 7.5±0.85 out of a maximum of 8 points (range 6-8), suggesting that
QUAL symptoms scores and quality of life (QoL). A steady state of the same this module was effective. Inter-rater reliability for each item on E-PAT was
failed dose is not appropriate to control symptoms. It is likely that this might high and the overall kappa was 0.63, p<0.0001. Conclusion: Interns reported
be a class finding and relatable to other proton pump inhibitors. limited experience with epinephrine autoinjectors prior to starting residency.
Our brief training module resulted in high, measurable EpiPen® proficiency
immediately. E-PAT demonstrated substantial inter-rater reliability. Future stud-
P272 ies will assess whether residents retain proficiency longitudinally and if E-PAT
INPATIENT CONSULTATIONS TO THE ALLERGY AND is equally reliable when used by non-clinician coders.
IMMUNOLOGY SERVICE AT A TERTIARY CARE PEDIATRIC
REFERRAL CENTER.
E.E. Kempe*1, D. Stukus1, K. Strothman2, R. Scherzer1, 1. Columbus, OH; P274
2. Dublin, OH. SUCCESSFUL SWITCH FROM LONG-TERM PROPHYLAXIS
WITH DANAZOL TO ACUTE TREATMENT WITH C1 ESTERASE
Background: There is a paucity of data examining patterns for inpatient
INHIBITOR CONCENTRATE (BERINERT) IN A PATIENT WITH
pediatric Allergy and Immunology (A/I) consultations. Objective: This analy-
sis was to determine the reasons for inpatient consultation to the A/I service at HEREDITARY ANGIOEDEMA.
a tertiary care pediatric referral center. Patient demographics and patterns for I. Martinez-Saguer*, W. Kreuz, Moerfelden-Walldorf, Germany.
establishing A/I follow-up (if recommended) were also examined. Methods: Background: Several treatment options exist for the treatment of heredi-
We performed a retrospective chart review of all inpatient A/I consults from tary angioedema (HAE), a rare genetic disease that manifests in episodes of
January 1, 2013 to December 31, 2013. Results: In 2013, 82 inpatient consults swelling in different parts of the body. Attenuated androgens, including dana-
were placed to the A/I service, with 76 unique patients. Of these, 55 represented zol, are well established for long-term use but are associated with multiple side
patients who had not previously been evaluated by the Section of Allergy and effects and contraindications. C1 esterase inhibitor concentrate (C1-INH)
Immunology. Fifty-six percent (31/55) of new patient consults were to assess replaces the missing or dysfunctional protein and is recommended as a first-
for possible immunodeficiency, 16% (9/55) for angioedema/anaphylaxis, 13% line treatment by international guidelines. Case Description: A 51-year-old
(7/55) for possible food allergy, 7% (4/55) for adverse drug reactions, 5% (3/55) male patient with HAE had his first symptoms of HAE (abdominal pain) at an
to assist with immunoglobulin replacement therapy, and 2% (1/55) for rash. age of 13 years. He was initially misdiagnosed with indigestion and allergies.
Of the consultations placed for possible immunodeficiency, 71% (22/31) were His first laryngeal attack occurred at an age of 23 years. Upon diagnosis of
for patients under 2 years of age. The majority of new inpatient consults were HAE, the patient received a daily dose of 200 mg danazol for long-term pro-
requested by Infectious Disease (ID) (23%, 13/55), Hospital Pediatrics (14%, phylaxis. During danazol therapy, he experienced side effects, including
VOLUME 113, NOVEMBER, 2014 A101
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A102
ABSTRACTS: POSTER SESSIONS
increased transaminases, and arterial hypertonia. Reduction to a daily dose of lected included basic demographics, penicillin allergy test results, current allergy
100 mg danazol triggered HAE attacks (≥ 1 attack per week). When the patient status on the EMR, readmission rates, prescribed antibiotics and discharge sum-
expressed the wish to switch from danazol to C1-INH, he was trained in intra- mary contents. Results: 146 patients were tested for penicillin allergy in 2012.
venous self-infusion and learned how to recognize early symptoms of HAE Of these, 144 (98.6%) were not allergic to penicillin. Although orders were
attacks. Danazol was then reduced stepwise (tapering down over several weeks). written in the charts of 145 (99.3%) patients to update their allergy status after
During this period, recurrent attacks occurred approximately every 8 days and testing, 32 (22.23%) of these patients with negative tests were still listed as
were successfully treated with self-infusion of human pasteurized nanofil- allergic to penicillin in the EMR. Only 19 (15.2%) discharge summaries noti-
tered C1-INH (pnf-C1-INH, Berinert®; CSL Behring, Marburg, Germany). fied family physicians of the allergy testing results and discharge summaries
Currently, the patient experiences HAE attacks every 5 days. All attacks are were missing for 25 (20%) patients. Further assessment of 50% of the charts
treated successfully with self-infusion of pnfC1-INH. The patient has no side revealed that in 41% of cases the negative allergy test resulted in a change of
effects and transaminases have returned to normal. Arterial hypertonia is ongo- antibiotics to penicillin or its derivative. Of the 60 readmitted patients, 20 (33%)
ing but is well-controlled with lercanidipine. Conclusions: Self-infusion of were still listed as allergic to penicillin in the EMR (only one patient tested pos-
pnfC1-INH is an effective and safe alternative for patients with severe HAE itive on skin testing) and 14 (70%) of the 20 patients required antibiotics. 12
who experience side effects or show lack of response to attenuated androgens. of the 14 patients (86%) were prescribed antibiotics in the penicillin family
Before switching from long-term prophylaxis with danazol to acute treatment despite their positive allergy status. Conclusions: A significant proportion of
with pnfC1-INH, we inform the patient about a possible increase of attack fre- health records were not amended following antibiotic allergy testing and the
quency and train the patient in intravenous self-administration techniques. We patient’s new allergy status was not communicated to the majority of general
do not stop androgens immediately and taper down danazol over several weeks. practitioners in the discharge summary. A more efficient and reliable system
needs to be implemented to ensure changes to allergy status are communi-
cated to all members of the healthcare team.
P275
THE PRACTICAL USE OF A REAL WORLD DATA BASE IN CLIN-
ICAL PRACTICE. P277
G. Steven*, Milwaukee, WI. USE OF A PRIVATE PRACTICE ALLERGY SPECIALTY HEALTH
CARE DATA BASE IN IDENTIFICATION OF PATIENTS THAT
Objectives: Health decision-makers involved with treatment, coverage and
payment policies are increasingly developing policies that seek information MAY BENEFIT FROM NEW THERAPIES.
on “real-world” (RW) data base outcomes. Motivated by these initiatives, we G. Steven*, Greenfield, WI.
have begun to develop a framework to assist health-care decision-makers in Clinical and demographic data have been entered in a diagnosis-related
dealing with RW clinical data, especially related to treatment, coverage and administrative database (P4P) at AASC since 2008. This database was used to
payment decisions. Methods: Since 2008, a relational database has been devel- estimate the prevalence of ragweed seasonal allergic rhinitis and to examine
oped and refined to complement the EHR by providing clinical decision sup- the capture of data in P4P, considered in different time frames. Methods: A
port in ways that are not currently possible in most certified software. Data case-finding algorithm identified patients with a positive skin test to ragweed
from skin testing, spirometry, eNO analysis, impulse oscillometry are com- among those who had had skin testing done since 1996 and healthcare contact
bined with medication lists, immunotherapy formularies and injection admin- at AASC within the last six years for whom we had current and correct con-
istration records, smoking history, demographics, quality of life assessments tact information. Prevalence rates were calculated as the ratio of the number
and immunization status. Results: We defined RW clinical information (P4P) of identified patients to the total number of allergic rhinitis patients tested.
as data used for decision-making in day-to-day clinical care that are more prac- Results: Of the 6877 skin test records in the database, 534 patients were iden-
tical than the low-level paradigms formulated by data collected in conventional tified who had at least a moderate SPT to short ragweed (approximately an
randomized controlled trials (RCTs) “evidence-based medicine.” We consid- 8mm wheal or greater), had a diagnosis of allergic rhinitis, were not already
ered several characterizations: by type of outcome (clinical, economic, and on SCIT, had a current email address on file and, based on the prescribing infor-
patient-reported), by hierarchies of evidence (which rank evidence according mation of the recently approved sublingual ragweed extract tablet, were between
to the strength of research design), and by type of data source (supplementary the ages of 18 and 65. Only 42 of these patients called in to request more infor-
data collection alongside RCTs, large simple trials, patient registries, admin- mation about this new treatment option. Since this medication had been only
istrative claims database, surveys, and medical records). P4P data base key recently approved, we found lack of formulary coverage to be a significant
issues: 1) the importance of RW data; 2) limitations of RW data; 3) data depends obstacle to getting patients treated with this new therapy. Nonetheless, although
on the circumstance; 4) good practices for collecting and reporting RW data; there was only about 2 weeks’ time between the drug appearing in pharmacies
5)good process in using RW data in coverage and reimbursement decisions; 6) and the last day to start therapy this year (12 weeks prior to the start of the RW
the need to consider costs and benefits of data collection; 7) need for model- season, per the package insert), we were able to initiate treatment with 12
ing; and 8) the need for continued stakeholder dialogue. Conclusions: Real- patients. Conclusions: Clinical and administrative healthcare databases in pri-
world databases are essential for sound coverage and reimbursement decisions. vate practice today can be important tools in identifying populations that may
Of greatest utility is our use of clinical data to provide high-level treatment benefit from new therapies, notifying patients of new information (e.g., boxed
decisions that maximize outcomes. It is critical that policymakers recognize warnings) regarding medications they are currently taking, as well as identify
the benefits, limitations, and methodological challenges in using RW data from potentially eligible patients for clinical research trials as part of the drug devel-
private practice data bases (P4P), and the need to consider carefully the costs opment process. However, data collection needs to be judicious, relevant and
and benefits. used on a daily basis in order to have a positive impact on clinical care.
P276 P278
RECONCILIATION OF HEALTH RECORDS FOLLOWING PENI- ALLERGIC DISEASES AND CORRELATED RISK FACTORS IN
CILLIN ALLERGY TESTING OF HOSPITALIZED PATIENTS. PRESCHOOL CHILDREN.
R. Pratt*1, A. Romanova2, J. Greenbaum3, M. Cyr3, 1. Stoney Creek, ON, M. Duse*, G. Forastiere, D. Porta, T. Melengu, A. Di Coste, L. Indinnimeo,
Canada; 2. Ottawa, ON, Canada; 3. Hamilton, ON, Canada. Rome, Italy.
Background: Medication errors are a very common problem, which can Background: Allergic diseases affect 40% of the population with an increas-
lead to a range of sequela, including disclosure with no harm to a substantial ing prevalence. In the SIDRIA study, prevalence of allergic diseases changed
degree of morbidity. As a result, medication reconciliation is being implemented with the age: asthma and rhinitis raised (respectively from 9.3% to 10.3% and
as a formal process in many hospitals. Similarly, inaccurate medication allergy 12.3% to 20.9%), while eczema decreased (from 15.9% to 11.9%). However,
lists can lead to increased cost to the system, unnecessary repeat allergy test- data on younger children are lacking. The aim of the present study is to assess
ing, inappropriate or inferior antibiotics being prescribed on readmission or the prevalence of allergic and respiratory diseases as well as related risk fac-
even allergic reactions. We hypothesized that the majority of inpatients tested tors in a population of 3 to 5 years old preschool children. Methods: The study
for penicillin allergy were not allergic and that this information was not ade- includes children attending 4 Nursery Schools in an urban district of Rome.
quately documented in the EMR or communicated to the general practitioner. Data on the allergic diseases were collected using standardized questionnaire
Methods: We retrospectively reviewed the charts of all inpatients at a teaching (SIDRIA-2) and Skin prick tests (SPT) was performed. We investigated the
hospital that were seen by a consultant allergist over the year of 2012. Data col- association of atopy, rhinitis, wheezing and asthma with a list of potential deter-
A102 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A103
ABSTRACTS: POSTER SESSIONS
minants, calculating the Odds Ratios (OR) and 95% Confidence Limits (95%CI) esize a correlation between the presence of TMJ symptoms and the Epworth
from logistic regression models. Results: 494 children (46% male) aged 3-6 sleep score which measures degree of daytime drowsiness during a variety of
years were studied. More than 75% were breastfed (> 2 months) and 87% activities. Methods: After informed consent and IRB approval, 44 subjects were
were weaned after the 5th month of life. Most of them started attending school identified to have doctor diagnosed TMJ consisting of a constellation of ten-
after the 11th months and 64% had previously attended daycare. Sixty-seven derness to palpation over the TMJ with joint movement. 763 subjects did not
percent of children had at least 1 sibling; 72.3% lived at home with at least have clinically diagnosed TMJ in a university academic allergy/immunology
other 3 persons; 42% reported to live in a street with heavy traffic; 20.6% had clinic. Results: The average Epworth Sleepiness Scale (ESS) score amongst
a pet at home, and 22.9% had smoking parent. SPT was positive in 12% of chil- subjects with TMJ was 7.8 in comparison to controls with an average ESS score
dren. Asthma was positively associated with nationality not Italian (OR: 2.54, of 7.1. Conclusions: Our results show a positive correlation between the pres-
95%CI: 1.09-5.92), breastfeeding >1 month (OR: 2.78, 95%CI: 0.97-7.97), ence of TMJ symptoms and Epworth sleep score. Our findings indicate a need
daycare attendance (OR: 2.26, 95%CI: 1.14-4.52), mother’s atopy (OR: 2.04, to further evaluate the relationship between TMJ symptoms, day time sleepi-
95%CI: 1.13-3.66), and dermatitis (OR: 2.02, 95%CI: 1.13-3.61). Allergic rhini- ness, and the role of sleep hygiene in symptomatic TMJ patients to improve
tis was positively associated with father’s atopy (OR: 3.11, 95%CI: 1.30-7.44), patient quality of life.
and dermatitis (OR: 11.6, 95%CI: 4.52-29.6). Atopic status was positively asso-
ciated with mother’s atopy (OR: 2.09, 95%CI: 1.15-3.77). Conclusion: Our
study found a high prevalence of atopic sensitization in children under five P281
years, and confirms the high prevalence of allergic diseases, to an extent com- THE ASSOCIATIONS OF ALLERGY SKIN TEST, OCULAR AND
parable to those seen later in life. The mother’s atopy increases the risk of devel- NASAL SYMPTOMS AND ASTHMA DURING NHANES II (N-II)
oping asthma, father’s atopy increases the risk of allergic rhinitis while pollu- AND NHANES III (N-III).
tants (smoke and vehicular traffic) are not significant risk factors in these setting.
Q. Meng*1, S. Nagarajan1, L. Bielory2, 1. Piscataway, NJ; 2. Springfield,
NJ.
P279 Background: The prevalence of allergy skin test (IST), ocular and nasal
symptoms (ONS), and asthma has been reported from N-II and N-III. How-
EFFECTS OF DELIVERY AND FEEDING ON INCIDENCE OF
ATOPIC DISORDERS. ever, the associations of among these symptoms over time are unknown. Meth-
ods: N-II (1976-1980) and N-III (1988-1994) collected allergy IST data, ONS
M. Hauk1, B.A. McGoey2, M. Michelis*2, 1. Mahwah, NJ; and asthma prevalence. IST, ONS and asthma results were assessed for 6 com-
2. Hackensack, NJ. mon allergens (Ags) to N-II and N-III: cat, ragweed, perennial rye, oak, Bermuda
Introduction: Breastfeeding and vaginal delivery are known to be benefi- grass, and A. alternata. The IST+ (sensitized for 1 or more Ags) populations
cial to a child’s health. This study investigates the prevalence of atopic disor- were then assessed for ONS, and asthma status. ONS was identified using sur-
ders in children who are breastfed versus bottle fed and method of delivery, vey responses and asthmatics based on having a history and still having asthma.
spontaneous vaginal delivery (SVD) or cesarean section (C-section). Methods: The associations among IST, ONS and asthma were characterized with con-
A retrospective chart review was conducted on 100 patients 0.5 to 17 years of tingency tables and correlation analyses. Results: IST+, ONS, and asthma sta-
age (average 6.3 years of age ± 4.3). Patients were separated by duration of tus were collected from N-II (n=11,044) and N-III (n=10,833). The number of
breastfeeding or formula fed with no breastfeeding. Breastfed infants and tod- IST+(n=2144), ONS(n=991), and asthma(n=275) from N-II; and IST+(n=4538),
dlers were subdivided into 5 groups based on length of feeding, <3 months, 3- ONS(n=3242), and asthma(n=547) from N-III. Comparing N-II to N-III, the
<6 months, 6-<9 months, 9-<12 months, and 12 or more months. Prevalence prevalence increased: asthma 2.0 times, IST+ 2.2 times, ONS 3.3 times. The
of atopic skin disorders, such as eczema and atopic dermatitis (AD), concurrent prevalence of asthma, ONS, and +IST increased 5.3 times (all p<
Immunoglobulin E (IgE) disorders, such as food allergies, asthma, allergic 0.0001; Χ2 test). From N-II to N-III, sensitivity increased to an increasing num-
rhinitis (AR), and a family history of pertinent atopic diseases (FHX) were ber of Ags. ONS prevalence in N-III was 2-3 times > N-II (p< 0.0001, except
identified in each patient. Student’s t test was performed. Results: Out of the for all 6 Ags, p=0.069). Within each NHANES survey, the associations among
100 children, 52 were males and 48 were females. The children breastfed for +IST, ONS and asthma were all statistically significant with stronger associa-
9-<12 months and born via SVD group had the lowest atopic skin disorders, tions observed in N-III vs. N-II. Correlation coefficients between asthma and
but had a low FHX. The 6-<9 months breastfed and born via C-section group positive skin tests doubled or tripled in N-III (r=0.04 in N-II & 0.12 in N-III
had the lowest amount of IgE disorders, but the highest amount of atopic skin for oak). A linear association (p< 0.0001) between the cumulative number of
disorders. The 6-<9 months breastfed SVD group had the highest FHX. The IST+ (ranging from 0-6) and the prevalence of ONS or asthma was stronger in
12+ months breastfed SVD group had the highest number of IgE disorders. N-III. Conclusion: From N-II to N-III, the prevalence of asthma, ONS, and IST
All breastfed children had a lower occurrence of atopic skin disorders with a increased with greatest associated with more than one symptom. From N-II to
p value of 0.02. With regards to breast fed versus formula fed, the 9-<12 months N-III, sensitivity increased to an increasing number of Ags. The associations
breastfed group had the lowest atopic skin disorders, IgE disorders, and FHX among IST, ONS, and asthma became stronger during N-III vs. N-II. Supported
prevalence. The 6-<9 months breastfed group had the highest atopic skin dis- in part by US EPA STAR Grant #: RD834547; Observational, Laboratory, and
orders and FHX. The <3 months breastfed group had the highest occurrence Modeling Studies of the Impacts of Climate Change on Allergic Airway Dis-
of IgE disorders. Conclusion: Breastfeeding for 9-<12 months seemed to reduce ease; PI: Leonard Bielory, M.D.
the amount of atopic skin disorders and IgE disorders; however, the genetic
lack of prevalence of atopy may explain this observation. Children breastfed
for <3 months had higher incidence of atopy. Patients that were born via SVD P282
were shown to have a less likely occurrence of atopic skin disorders and FHX PEDIATRIC ALLERGY AND GI COMBINED CARE IMPROVES
and a higher occurrence of an IgE disorder when compared to patients born EOSINOPHILIC ESOPHAGITIS SYMPTOM CONTROL IN
via C-section. A future study with a larger population size is needed to con- CHILDREN.
firm these results.
M. Hogan1, A. Wonnaparhown2, R. Scherr*2, N. Wilson2, 1. Reno, NV;
2. Las Vegas, NV.
P280 Introduction: Eosinophilic esophagitis (EE) is an inflammatory esophagi-
TEMPOROMANDIBULAR JOINT DISEASE AND ITS RELA- tis which can be associated with IgE sensitization to food and aeroallergens.
TIONSHIP TO SLEEP HYGIENE AND SLEEP DEPRIVATION. Food avoidance, swallowed glucocorticosteriods, and proton pump inhibitors
have been utilized therapeutically in pediatric EE patients. Information regard-
C. DiMaio*1, P. Henao2, E. Rael2, 1. Palmyra, PA; 2. Hershey, PA. ing pediatric follow-up of EE is limited. Methods: Patients (1-18 years) with
Rationale: TMJ, or temporo-mandibular joint disease, is a common disor- biopsy proven EE co-managed with pediatric GI from 2010-2013 in the
der with significant morbidity affecting the quality of life for many people in UNSOM A/I clinic and having at least one follow-up visit were evaluated ret-
the United States. TMJ is more common in non-hispanic Caucasian women and rospectively for skin test IgE sensitization to food, aeroallergens, and EE symp-
has been attributed to pain threshold, behavioral factors, and past trauma. How- toms. Statistics were performed with Fischer’s exact test with graphpad.com.
ever, to date no clear etiology has been identified and this disease is likely IRB exclusion was obtained. Results: 23 children with EE meeting study cri-
multifactorial. Characterized primarily by pain, headache, and ear pain, TMJ teria were identified. IgE sensitization occurred to food in 87%, aeroallergens
is very difficult to treat given the complex nerve root anatomy of the skull and 96% and 87% of children had sensitization to both. A/I and GI therapy for EE
foramina. Given the significant morbidity TMJ carries on patients, we hypoth- and AR increased after the first A/I visit with 9/23 swallowing GCS, 3/23 on
VOLUME 113, NOVEMBER, 2014 A103
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A104
ABSTRACTS: POSTER SESSIONS
proton pump inhibitors, 8/23 avoiding most likely contributing foods and 16/23 of breath, mucus/phlegm and cough occurring in ≥70% entries while chest
with prescribed aeroallergen avoidance or immunotherapy for allergic rhinitis tightness and wheezing occurring in ≥60% of entries over the 26-week study
or/asthma. Most common food sensitizations identified were legumes (14/23) period. Exploratory factor analysis gave a single factor, including both symp-
and tree nuts (8/20). Other foods were noted at lesser frequencies. Common toms and the BD items. Internal consistency was extremely high, being >0.95
aeroallergens identified in the population in order of frequency were cat 69%, for all three assessment points (M1, M2 and E) at baseline, Week 12 and Week
sagebrush 63%, maple 61%, dog 57% and timothy 54% of the study popula- 26. Thus the scale is unidimensional, so that the overall mean of the seven items
tion. Eosinophilic esophagitis symptoms of stomachache (p<0.037) and (OM7) could be used as a summary measure. Test-retest reliability was assessed
GERD/heartburn (p<0.033) improved with this comprehensive care. Conclu- in 44 patients who showed no change in their symptoms between baseline and
sion: Pediatric EE is a complex inflammatory disease with multiple possible Week 1. The intraclass correlation coefficients (ICC) for OM7 were 0.97 for
triggers and follow-up information after initial evaluation is limited. Aeroal- M1 and M2 and 0.96 for E. The lower 95% confidence limit was >0.92 in all
lergens and food IgE sensitization was notable in this population. Compre- cases. The eDiary was sensitive to change: the effect size for change over 26
hensive care in this population resulted in decreased GI symptoms of pain and weeks in patients identified as having improved on both clinical and patient
should be studied further as a working model to improve pediatric EE care. global measures, was large (0.79) as compared to a minimal change in patients
classified as uncertain/no change (0.16). Anchor-based comparison suggests
that a change of 0.6 on the OM7 Score of the eDiary (range 0-10) represented
P283 a meaningful change for patients. Conclusion: The new COPD eDiary showed
HYPERSENSITIVITY COURSE: EMPOWERING FELLOWS good measurement properties, being valid, reliable, internally consistent, and
TO DESIGN/CONDUCT THEIR OWN EFFECTIVE ALLERGY sensitive to change.
CURRICULUM.
A.C. Gavino*, Q. Kamili, Z. Maskatia, N. Chokshi, D. Bayer, K. Tuano,
S. Wu, S. Hasan, M. Garcia Buheis, L.M. Noroski, Houston, TX.
P285
THE CHARACTERIZATION OF RPC4046, A NOVEL ANTI-IL13
Introduction: National training programs answer to the Accreditation Coun- MONOCLONAL ANTIBODY THAT BLOCKS BINDING TO IL-13
cil for Graduate Medical Education (ACGME) to meet competency require-
RECEPTOR α1 AND α 2 IN DEVELOPMENT FOR
ments. Allergy and Immunology (AI) requirements include core competency
EOSINOPHILIC ESOPHAGITIS: RESULTS OF A FIRST-IN-
achievements in allergy (hypersensitivity). Methods that empower learners to
take ownership in their own course curriculum are not standard, yet can max- HUMAN STUDY.
imize content retention important for accreditation, exam scores and practice C. Tripp*1, A. Campbell2, B. Hendrickson2, C. Cuff1, R. Miller1, C. Wu1,
performance. Our objective was to develop an innovative and effective Hyper- K. Kim3, 1. Worcester, MA; 2. North Chicago, IL; 3. Cypress, CA.
sensitivity Course (HSC) by/for AI fellows. Methods: Needs assessment was Eosinophilic esophagitis (EoE) is a chronic, immune/food antigen-medi-
performed for actual competence and perceived efficacy in aeroallergen diag- ated disease characterized clinically by esophageal dysfunction and histologi-
nostics, allergic disorders and procedures, based on in-training exam results, cally by eosinophil-predominant inflammation with overexpression of cytokines,
patient/procedure logs and confidence/experience/satisfaction. Gaps in allergy including interleukin 13 (IL-13). RPC4046 (previously known as ABT-308) is
knowledge, practice and self-efficacy were identified and fellows became part- a humanized, high-affinity, neutralizing antibody that prevents IL-13 binding
ners in creating an allergy-focused and shared-group interactive course with to both IL-13Rα1 and IL-13Rα2. The first-in-human (FIH) study
expert oversight. Modified flipped design with project-based learning and real- (NCT00986037) was a single center, randomized, double-blind, placebo-con-
life applications to master allergy was applied. Results: AI fellows successfully trolled, 3-part, dose escalation study. RPC4046 was administered to healthy
designed (2008-2009) and implemented (2009-2014) their own HSC course volunteers (HV) and patients with mild to moderate, controlled asthma to assess
to master ACGME AI competencies in allergic diseases/procedures, aeroaller- the safety, tolerability and PK of single escalating intravenous (IV) doses or
gen identification and desensitizations, and continue to modulate it (by prac- multiple escalating subcutaneous (SC) doses. Twenty HV and 15 asthma patients
tice parameters/literature updates and learner needs) and teach it (weekly-10 received single IV infusions of RPC4046 (0.3 to 10 mg/kg) or placebo. Sub-
months/year). All HSC AI fellows (2008-2014) reached increased in-training sequently, 12 asthma patients received 3 weekly SC doses of RPC4046 (0.3 or
exam scores and board pass rates (100%), met log requirements to 50%ile 3.0 mg/kg) or placebo. IRB approval and informed consent was obtained from
(2013-2014), ranked it highest among courses, achieved increased allergy self- all research subjects. RPC4046 pharmacokinetic (PK) parameters were simi-
efficacy and, in 2013, earned the ACGME David Leach Award for a trainee- lar after a single IV infusion between HV and asthma patients. Following mul-
driven educational program. Conclusion: HSC AI fellows conquered compre- tiple SC administration, Tmax was ~4 days, exposure was dose-proportional and
hension-performance in allergic diseases and procedures with confidence and the absolute bioavailability was ~70%. In 27.8% of subjects receiving RPC4046,
competence through becoming teachers while learners. They became empow- measurable anti-drug antibodies were detected transiently, which did not appear
ered as leaders in their own sustainable curriculum for themselves and their to affect PK or safety. The AE profile was similar in HV and asthma patients
clinical team. Their HSC methods may serve as a feasible and effective model and with different administration routes. For RPC4046 subjects, all AEs were
not only for meeting AI training requirements but also for those seeking mas- mild to moderate in severity, with none reported as probably related to study
tery in allergy practice and knowledge. drug. There were no dose-related increases in AEs and no discontinuations
due to AEs. The proportion of subjects reporting an upper respiratory tract
infection was greater among those receiving RPC4046 compared to placebo.
P284 A single SAE of worsening foot bunion was reported in Group 1 HV and con-
EVALUATION OF AN ELECTRONIC DAILY DIARY FOR MEAS- sidered not related to study drug by the investigator. There were no study drug
URING SYMPTOMS AND IMPACT OF CHRONIC OBSTRUCTIVE related infusion-related reactions and no suggestion of worsening asthma. These
PULMONARY DISEASE. results support further investigation of RPC4046 for allergic/inflammatory dis-
K. Kulich1, B. Tiplady*2, D. Banerji3, 1. Basel, Switzerland; eases involving IL-13, including the ongoing phase 2 clinical trial in adults with
2. Peterborough, United Kingdom; 3. East Hanover, NJ EoE (NCT02098473).
Introduction: Patient-reported outcomes are increasingly important in eval-
uating the severity and impact of chronic conditions such as chronic obstruc-
tive pulmonary disease (COPD). Electronic patient diaries (eDiaries) have been
found to be highly acceptable to patients, who often prefer them to paper.
Also, eDiaries allow time-stamping of entries, automatic tailoring of entries to
the time of day, and limit entries to valid options. Methods: Qualitative patient
interviews have been used in the development of a new COPD eDiary, which
includes five symptom items and two impact items rating bother and diffi-
culty (BD). Two morning assessments (since awakening, M1; since last assess-
ment, M2) and one evening assessment (E) were made each day. The eDiary
was completed by a subset of 209 patients (140 males, aged 44 - 86) in a 26-
week QVA149 SHINE study. Results: Patient compliance with the eDiary was
90.1% over the 7-day baseline period, and 80.0% at Week 26. The frequencies
of reporting of each of the 5 symptoms were ≥60% of baseline, with shortness
A104 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A105
ABSTRACTS: POSTER SESSIONS
PK Parameters (Mean ± SD) of RPC4046 Following a Single IV Infusion in obtained from all research subjects (or parents for adolescents). Results: Of 51
Healthy and Asthma Subjects subjects included, 47 (92.1%) experienced a warming sensation within 60 sec-
onds of ingestion. The median duration of the sensation was 100 seconds (95%
Confidence Interval: 82, 112 seconds). Most subjects (71%) liked the warm-
ing sensation; no subjects expressed significant dislike (i.e., very much or
extreme dislike) of the sensation. About 67% thought the strength of warming
was “just about right.” There were no safety concerns, and the syrup was well
tolerated and effective for treating cough and cold symptoms. Conclusions: The
flavour agent 316282 is associated with a warming sensation, which may be a
desirable attribute for a cough and cold product for some patients. Lack of a
control group – i.e., unflavored syrup – limits interpretation of the findings.
More data are needed to overcome the challenge of appropriate controls for
these types of studies.
a N = 4 for Cmax and Cmax/Dose for Groups 2 and 3 P288
b Mean ± SD ONCE-DAILY TIOTROPIUM RESPIMAT® ADD-ON TO MAIN-
c Harmonic mean ± pseudo-standard deviation TENANCE THERAPY IMPROVES LUNG FUNCTION IN
PATIENTS WITH MODERATE OR SEVERE SYMPTOMATIC
ASTHMA, INDEPENDENT OF T HELPER 2 INFLAMMATORY
P286 STATUS.
EFFICACY OF SULFASALAZINE, AN ANTI-INFLAMMATORY M.L. Vandewalker*1, J. Karpel2, G. Bensch3, L. Ford4, M. Engel5,
AGENT, FOR THE TREATMENT OF SEVERE CHRONIC IDIO- R. Sigmund5, P. Moroni-Zentgraf 5, H. Kerstjens6, 1. Columbia, MO;
PATHIC URTICARIA PATIENTS NOT CONTROLLED ON ORAL 2. New York, NY; 3. Stockton, CA; 4. Bellevue, NE; 5. Ingelheim am Rhein,
ANTIHISTAMINES. Germany; 6. Groningen, Netherlands.
S. Nsouli*, Danville, CA. Background: In many patients (pts) current asthma control is inadequate,
Previously, we have shown the efficacy of Omalizumab, a recombinant, resulting in impaired quality of life and increased risk of exacerbations. T helper
humanized, chimeric anti-IgE monoclonal antibody, for the treatment of Severe 2 (TH2) immune response mediates allergic airway inflammation, may influ-
Chronic Idiopathic Urticaria (CIU) patients not controlled on oral antihista- ence individual asthma expression, and is the target of many asthma treatments.
mines. Clinical observations have led us to believe that sulfasalazine, an anti- Once-daily tiotropium Respimat® add-on to at least medium-dose inhaled cor-
inflammatory agent, composed of a sulfapyridine covalently linked to 5-aminos- ticosteroid (ICS) ± long-acting β2-agonist (LABA) maintenance therapy pro-
alicylic acid, may provide additional efficacy in sub optimally controlled Chronic vides sustained lung function improvements in pts with symptomatic asthma.
Idiopathic Urticaria (CIU) patients that remain symptomatic on an H1-Recep- Pre-specified analyses of pooled data from replicate Phase III, randomized,
tor Antagonist, Cetirizine. In this open labeled 16 week trial, 60 adult patients double-blind, placebo-controlled, parallel-group trials were performed to assess
with symptomatic Severe Chronic Idiopathic Urticaria using Cetirizine, 10 whether tiotropium Respimat® treatment response was dependent on TH2 inflam-
mg orally QD, were randomized to continue the existing therapy Cetirizine or matory status. Methods: Pts with severe symptomatic asthma (PrimoTinA-
to add on Sulfasalazine 500 mg oral tablets (increased by 500mg weekly) until asthma®, n=912) from two 48-week trials of tiotropium Respimat® 5 mg add-
control of clinical symptoms occurred or until reaching a maintenance dose on to high-dose ICS (≥800 mg budesonide or equivalent) + LABA, and pts with
according to patient’s weight, 30 to 50 mg/kg per day, in 2 evenly divided doses, moderate symptomatic asthma (MezzoTinA-asthma®, n=2100) from two 24-
not to exceed 2g per day to the existing therapy Cetirizine. The end points of week trials of tiotropium Respimat® 5 mg or 2.5 mg or salmeterol add-on to
the trial include: weekly itch severity score on a scale. The mean of measure- medium-dose ICS (400-800 mg budesonide or equivalent), were evaluated. Peak
ments at the end of the 16-week trial revealed a significant improvement in all and trough forced expiratory volume in 1 second (FEV1) were assessed (pooled
parameters examined in the treatment group receiving Sulfasalazine (as add- data) in the TH2-low and TH2-high subgroups according to baseline total serum
on to the existing therapy), compared to the other group. In conclusion, the IgE ≤ or >430 mg/L, blood eosinophils ≤ or >0.6×109/L, and clinical judgment
addition of Sulfasalazine to the combination of Cetirizine is more effective than of allergic asthma as “no” or “yes”. COPD was excluded. Results: 3012 pts
Cetirizine, for the treatment of Severe Chronic Idiopathic Urticaria patients. It were included in the treated set, with baseline demographics and disease char-
appears that when Sulfasalazine is added to the combination H1-receptor antag- acteristics balanced between treatment regimens and subgroups. Peak and trough
onist, Cetirizine, the end points and symptom scores are significantly improved. FEV1 responses were improved with tiotropium Respimat® versus placebo,
independent of total serum IgE level, blood eosinophil count, and clinical judg-
ment of allergic asthma (Table). Safety and tolerability of tiotropium Respi-
P287 mat® were balanced compared with placebo. Conclusion: Once-daily tiotropium
PATIENT ACCEPTANCE AND PREFERENCE FOR THE WARM- Respimat® add-on to at least medium-dose ICS ± LABA maintenance therapy
ING SENSATION ACCOMPANYING FLAVOUR AGENT 316282 IN provides sustained improvements in lung function, independent of TH2 inflam-
AN OVER-THE-COUNTER COUGH AND COLD SYRUP. matory status, in pts with moderate or severe symptomatic asthma. Tiotropium
Respimat® add-on therapy may therefore be beneficial in both allergic and non-
R. Furcha1, A. Amin*2, 1. Nyon, Switzerland; 2. Parsippany, NJ. allergic asthma.
Introduction: An over-the-counter (OTC) cough and cold syrup containing
paracetamol, phenylephrine, and guiafenesin was reformulated with flavour
agent 316282, which has been shown to cause a warming sensation in the mouth
and back of the throat. This agent is included for the taste of the product, but
also may have a soothing effect appropriate to the indication. The ability of a
warming sensation to help patients suffering from cough, cold, and flu feel bet-
ter is well known anecdotally. However, there are no studies to date that have
evaluated the warming sensation of liquids, rubs, or drug ingredients in terms
of patient acceptability and preference. Objective: We sought to assess the
warming sensation associated with the flavour agent 316282 in terms of patient
acceptability. Methods: This was a single dose, single cohort, single treatment
arm, open-label study. Subjects received one 30 mL dose of syrup containing
paracetamol (500 mg), phenylephrine (10 mg), guaifenesin (200 mg) and flavour
agent 316282 (0.15% weight/volume). Onset and duration of the warming sen-
sation in the mouth/throat were recorded, and subjective assessments of strength
and appeal of the sensation and overall acceptability of the product as a cough
and cold remedy were surveyed. IRB/HAC approval and informed consent was
VOLUME 113, NOVEMBER, 2014 A105
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A106
ABSTRACTS: POSTER SESSIONS
Adjusted mean difference for tiotropium Respimat® versus placebo at Week
24 (mL)
P290
REVIEW OF HISTAMINE RECEPTOR (H1, H2, AND H3) ANTAG-
ONIST BINDING AFFINITIES YIELDS THREE TRENDS OF
BINDING PROPERTIES.
J. Maik*1, L. Bielory2, 1. New York, NY; 2. Springfield.
Introduction: Histamine receptor antagonists bind to several types of recep-
tors causing various wanted and unwanted physiological responses. By iden-
tifying the affinity levels (Ki) of ligands to three Histamine receptors (H1, H2,
H3), one could utilize a given antagonist by identifying low Ki values to
unwanted ligand-receptor binding (H3 which is consider to be an itch ago-
nist), and high Ki values for wanted ligand-receptor binding (H1, H2). Meth-
ods: A review of literature of Histamine antagonist affinities was performed to
tabulate affinity values for H1, H2, and H3 receptors. 12 chemicals were iden-
tified with affinity values for the receptors. Ki corresponds to [M] of the given
ligand when 50% of receptors are occupied. Results: Ki [M] for Pheniramine:
H1=34, H2=14567, H3=10567. Pyrilamine; H1=.8 H2=9510 H3=1016. Diphen-
hydramine; H1=14 H2=1600 H3=25000. Emedastine: H1=1.3 H2=49067
H3=12430. Levocabastine; H1=56 H2=23500 H3=4597. Antazoline; H1=160
H2=44483 H3=42400. Chlorpheniramine; H1=1.4 H2=7980 H3=3103. Keto-
tifen H1=1.3 H2=1115 H3=2277. Histamine; H1=180000 H2=18350 H3=4.6.
Methylhistamine; H1=138000 H2=72100 H3=1.4. Thioperamide; H1=28000
H2=57967 H3=1.1. Cimetidine; H1=6190 H2=2377 H3=20750. Ranitidine;
H1=46100 H2=187 H3=10537 Summary: Using Ki=1000 as a cutoff for high
aValues for active and placebo groups combined. Pts may be included in more or low affinity, three trends of Histamine receptor affinity emerge. Low H1
than one subanalysis; bFor treatment × subgroup interaction BID, twice-daily; affinity, High H2 affinity, and High H3 affinity that includes Pheniramine,
QD, once-daily Pyrilamine, Diphenhydramine, Emedastine, Levocabastine, Antazoline, Chlor-
pheniramine and ketotifen; high H1 affinity, high H2 affinity, and low H3 affin-
ity that includes Methyl histamine, Thioperamide, and Histamine; high H1
P289 affinity, low H2 affinity, and high H3 affinity that includes Cimetidine, and
PHARMACOLOGIC MODELING TO GUIDE THE DX-2930 DOS- Ranitidine. Conclusion: Different antihistamines have different effects that may
ING REGIMEN IN INVESTIGATING LONG-TERM PROPHY- further guide the improved used of these agents in the care of patients with
LAXIS OF HEREDITARY ANGIOEDEMA. histamine related disorders.
Y. Chyung*, D. Sexton, C. TenHoor, J. Kenniston, R. Faucette, R. Iarrobino,
J. Biedenkapp, B. Adelman, Burlington, MA. P291
DX-2930 is a fully human monoclonal antibody inhibitor of plasma TREATMENT WITH RECOMBINANT HUMAN C1 INHIBITOR
kallikrein (pKal) under investigation for prophylaxis against acute attacks of SHORTENS DURATION OF HEREDITARY ANGIOEDEMA
hereditary angioedema (HAE). It is well established that pKal plays a critical ATTACK SYMPTOMS.
role in HAE pathogenesis but the minimum level of pKal inhibition necessary
to prevent attacks is unknown. We hypothesize that continuously maintaining M. Riedl*1, D. Moldovan2, W.Yang3, H. Wedner4, M. Stobiecki5, A. Relan6,
levels of pKal inhibition associated with peak plasma drug levels (80 nM) of M. Cicardi7, 1. San Diego, CA; 2. Tirgu-Mures, Romania; 3. Ottawa, ON,
ecallantide (approved in the US to treat acute HAE attacks) would prevent Canada; 4. St. Louis, MO; 5. Krakow, Poland; 6. Leiden, Netherlands;
attacks (mid-dose hypothesis). Alternatively, lower or higher levels may be nec- 7. Milan, Italy.
essary. To inform future clinical trial design we performed analyses to evalu- Background: Hereditary angioedema (HAE) due to deficiency in C1
ate these low, mid, and high-dose hypotheses. Publicly available data from inhibitor is characterized by recurrent attacks of tissue swelling affecting mul-
OPuS-1, a clinical study of the pKal inhibitor BCX-4161 for HAE prophy- tiple anatomic regions. Recombinant human C1 esterase inhibitor (rhC1INH)
laxis (BioCryst Pharmaceuticals Inc.), was reviewed. In vitro inhibition of pKal was previously shown effective for treatment of angioedema attacks in patients
by ecallantide and DX-2930 was assessed using a synthetic substrate assay. with HAE by reducing the time to symptom relief. In addition to onset of relief,
Modeling was conducted using pharmacokinetic (PK) data from a single ascend- the duration of attack symptoms is recognized as a clinically meaningful end-
ing dose study of subcutaneous DX-2930 in healthy subjects. IRB approval and point. The current analysis reviews the time to reach minimal symptoms after
informed consent was obtained from all subjects. Review of the OPuS-1 data treatment with rhC1INH across six clinical studies. Methods: HAE patients
suggested that therapeutic response correlated with higher plasma drug con- treated with rhC1INH for acute angioedema attacks in three randomized-con-
centrations of BCX-4161 and that pKal inhibitor levels below 80 nM might trolled trials (RCT) and three open-label (OL) studies were reviewed. Patients
offer only partial prophylactic effect, lending further credence to the mid- and treated in the RCTs received rhC1INH or placebo (saline) for a single
high-dose hypotheses over the low-dose hypothesis. In an in vitro pKal assay, angioedema attack. In the OL studies, patients could be treated with rhC1INH
DX-2930 and ecallantide displayed comparable pharmacodynamic activity at multiple times for repeated attacks. Severity of attack symptoms at each affected
80 nM concentrations. Thus, continually maintaining DX-2930 drug levels anatomical location was assessed using a 100 mm visual analog scale (VAS)
above 80 nM should attain the level of pKal inhibition delineated by the mid- prior to treatment and at regular intervals following administration of study
dose hypothesis. PK modeling predicts that chronic DX-2930 dosing will yield medication. Time to minimal symptoms was defined as occurring when VAS
steady state plasma drug concentrations above 80 nM with 100 mg every 2 scores were <20 mm at all attack locations. Data were analyzed by study. IRB
weeks (or 300 mg every 4 weeks) and above 200 nM with 300 mg every 2 approval and written informed consent was obtained from all patients. Results:
weeks. Available data support the mid- and high-dose hypotheses for long-term In the three RCTs, a total of 145 patients were randomized to receive either
prophylaxis of HAE with DX-2930. Chronic dosing with 100 mg and 300 mg rhC1INH at doses of 50-100 IU/kg or saline. The median time to minimal symp-
is estimated to provide therapeutic coverage relevant to testing the mid and toms for patients in rhC1INH 50 IU/kg groups (240, 247 min) and 100 IU/kg
high-dose hypotheses in an efficacy and safety study. Plans for future clinical groups (245, 480 min) was significantly shorter than for patients in the saline
trial efforts will further be refined by PK and biomarker data from an ongoing groups (362, 1101, 1440 min), p<0.05 for all within study comparisons. In the
Phase 1b study in HAE subjects. OL studies patients were treated with an initial dose of 2100 IU or 50 IU/kg
with an option for a second dose. Data were available on 171 patients who
received rhC1INH for 449 acute attacks. Across the three studies, the median
time to minimal symptoms was 241 minutes for the 2100 IU dose group, and
240 and 243 minutes for the 50 IU/kg groups. Conclusions: In addition to pro-
viding rapid onset of relief, as previously shown, treatment with rhC1INH
resulted in consistently short duration of attack symptoms in HAE patients with
acute angioedema attacks across six clinical studies.
A106 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A107
ABSTRACTS: POSTER SESSIONS
P292 P294
GLOBAL AVAILABILITY OF HEREDITARY ANGIOEDEMA ONCE-DAILY TIOTROPIUM RESPIMAT® ADD-ON TO INHALED
DRUGS. CORTICOSTEROIDS ± LONG-ACTING β2-AGONISTS
N. Onyango*, K. Karikari, T. Craig, Hershey, PA. IMPROVES LUNG FUNCTION AND ASTHMA CONTROL AND
Rationale: Hereditary Angioedema (HAE) is a rare autosomal dominant REDUCES RISK OF ASTHMA WORSENING IN PATIENTS WITH
disease that is caused by a deficiency in C1, a serine protease inhibitor. It is MODERATE OR SEVERE ASTHMA.
currently estimated that the prevalence of HAE worldwide is 1:50000. There K. Murphy*1, G. Bensch2, W.E. Berger3, M. Engel4, H. Schmidt5,
are several drugs that have been developed to prevent and/or treat HAE. We P. Moroni-Zentgraf4, H.A. Kerstjens6, 1. Boys Town, NE; 2. Stockton, CA;
report on most of these drugs in order to highlight the challenges of treating 3. Mission Viejo, CA; 4. Ingelheim Am Rhein, Germany; 5. Biberach an
HAE in some parts of the world and to provide awareness of this condition, der Riss, Germany; 6. Groningen, Netherlands.
especially to help assess travel risks for patients with diagnosed HAE and to Background: The goal of asthma treatment is to achieve control and min-
advocate for patients in areas without sufficient HAE drugs. Methods: The imize future risk. Here we assess the efficacy of once-daily tiotropium Respi-
study was conducted by literature reviews, case reports and by obtaining rele- mat® add-on to inhaled corticosteroid (ICS) ± long-acting β2-agonist (LABA)
vant information from the manufacturers. Results: We identified the main cat- maintenance therapy in patients with symptomatic asthma: lung function, asthma
egories of drugs that are in current use in the treatment of hereditary angioedema. control, and asthma worsening data are presented. Methods: Four Phase III,
The therapies used to treat HAE focus: on either replacing the deficient or randomized, double-blind, placebo-controlled, parallel-group trials were eval-
dysfunctional C1 protein; or, on blocking the activation of specific pro-inflam- uated: two 48-week trials of tiotropium Respimat® 5 mg add-on to high-dose
matory proteins. These include: recombinant human C1 inhibitors (INH), ICS (≥800 mg budesonide or equivalent) + LABA (PrimoTinA-asthma®) in
bradykinin antagonists, and kallekrein inhibitors. Bradykinin B2 antagonists patients with severe symptomatic asthma; two 24-week trials of tiotropium
were widely available in most of Europe and in the US. Plasma kallekrein Respimat® 5 mg or 2.5 mg or salmeterol add-on to medium-dose ICS (400-800
inhibitors are only available in Israel and in the US. Plasma derived C1-INH mg budesonide or equivalent) in patients with moderate symptomatic asthma
products are available in the US for HAE prophylaxis; but are approved for (MezzoTinA-asthma®). Lung function was assessed as peak forced expiratory
both propylaxis and treatment in eleven European countries. The most widely volume in 1 second (FEV1) within 3 hours post-dosing (0-3h) and trough FEV1.
available drug was a human C1-esterase inhibitor; which was found in the US, Asthma symptoms and control were assessed as responder rate (percentage of
Europe, parts of South America and Asia. A recombinant human C1 inhibitor patients with minimally important change of ≥0.5) using the seven-question
is available in all 27 European Union countries, plus Norway, Iceland and Liecht- Asthma Control Questionnaire (ACQ-7). Time to first episode of asthma wors-
enstein. Conclusions: Overall, there is a distribution differential in the avail- ening (pre-specified as exacerbation) was also assessed. Results: Tiotropium
ability of hereditary angioedema drugs. These drugs are mostly available in the Respimat® provided statistically significant and sustained improvements in
European Union and in the United States. Most other countries outside these both peak FEV1(0-3h) and trough FEV1. A higher proportion of patients achieved
zones have either one or none of the therapies that are available for the pro- an ACQ-7 response with tiotropium Respimat® compared with placebo (Table).
phylaxis and treatment of HAE. Patients should take precautions when travel- Risk of asthma worsening was reduced with tiotropium Respimat® compared
ing to countries without HAE therapies and have a plan of care available in case with placebo: 31% risk reduction [RR] with 5 mg (hazard ratio [HR] 0.69;
of an exacerbation. Also, since ill-health seems to be a trigger for HAE, patients 95% confidence interval [CI] 0.58, 0.82; p<0.001) in PrimoTinA-asthma® at
should ensure that vaccinations and preventive medications are up to date, in Week 48; 13% RR with 5 mg (HR 0.87; 95% CI 0.69, 1.08; p=0.211) and 34%
addition to having their HAE medications available with them. RR with 2.5 mg (HR 0.66; 95% CI 0.52, 0.84; p<0.001) in MezzoTinA-asthma®
at Week 24. Safety and tolerability of tiotropium Respimat® were balanced
compared with placebo. Conclusion: Once-daily tiotropium Respimat® add-on
P293 to at least medium-dose ICS ± LABA provided significant and sustained
SAFETY EVALUATION OF OLOPATADINE HCL OPHTHALMIC improvements in lung function, improved asthma control, and reduced risk of
SOLUTION 0.77%, A TOPICAL OCULAR ANTI-ALLERGIC asthma worsening in adults with moderate or severe symptomatic asthma.
AGENT, IN ASYMPTOMATIC SUBJECTS.
E.J. Meier*, Mason, OH. ACQ-7 response with tiotropium Respimat® compared with placebo
Introduction: The objective of this study was to evaluate the safety of a new
topical ocular anti-allergic formulation, Olopatadine HCl, 0.77% in subjects 2
years of age and older. Methods: This was a multicenter, double-masked, vehi-
cle-controlled, parallel-group safety study. Asymptomatic adult and pediatric
subjects were randomized in a 2:1 ratio to receive Olopatadine 0.77% or vehi-
cle once daily in both eyes for 6 weeks. Safety assessments were conducted at
Day 0, weeks 1, 3 and 6. Safety assessments and parameters included adverse
events (AEs), best-corrected visual acuity (BCVA), ocular signs, intraocular
pressure (IOP), dilated fundus exam and vital signs (blood pressure, heart rate).
Results: The safety population included a total of 499 subjects ranging from 2
to 74 years of age; 330 subjects were in the Olopatadine 0.77% group and 169
subjects were in the vehicle group. Treatment-related adverse events occur-
ring in ≥ 1% subjects included blurred vision (4.5% vs 4.1%), abnormal sen-
sation in eye (2.1% vs 4.1%), dry eye (2.4% vs 3%), eye irritation (0.3% vs
3%), and dysgeusia (2.4% vs 0%), in olopatadine and vehicle groups, respec-
tively. No deaths or serious adverse events were reported during the study. No
subjects with exposure to Olopatadine 0.77% discontinued study participation
due to an adverse event. Based upon analysis and review of safety parameters
measured over the course of this trial, no clinically meaningful differences were
noted between the treatment groups. Conclusion: Olopatadine 0.77% was well-
tolerated in the overall safety population and no safety concerns were observed
with the higher concentration of Olopatadine.
VOLUME 113, NOVEMBER, 2014 A107
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A108
ABSTRACTS: POSTER SESSIONS
P295 P296
24-HOUR LUNG FUNCTION RESPONSE TO TIOTROPIUM CETIRIZINE-PSEUDOEPHEDRINE COMBINATION EFFEC-
RESPIMAT® ADD-ON TO MAINTENANCE THERAPY IN SYMP- TIVELY RELIEVES BOTH OCULAR AND NASAL ALLERGY
TOMATIC PATIENTS WITH MODERATE PERSISTENT SYMPTOMS IN SUBJECTS WITH SEASONAL ALLERGIC
ASTHMA. RHINITIS.
T. Casale*1, W.W. Carr2, L. Greos3, M. Engel4, L.J. Bour5, P. Moroni- E.R. Urdaneta*1, X. Tian2, M. Wu3, Q. Du2, K.B. Franklin1, M.K. Patel1,
Zentgraf4, H.A. Kerstjens6, 1. Tampa, FL; 2. Mission Viejo, CA; 1. Fort Washington, PA; 2. Shanghai, China; 3. MorrisPlains, NJ.
3. Centennial, CO; 4. Ingelheim am Rhein, Germany; 5. Biberach an der Objective: Evaluate the efficacy of combination cetirizine-pseudoephedrine
Riss, Germany; 6. Groningen, Netherlands. (CTZ-PSE) for ocular and nasal allergy symptom relief in subjects with sea-
Background: Tiotropium Respimat® is a once-daily long-acting bron- sonal allergic rhinitis (SAR). Methods: Two randomized placebo-controlled
chodilator currently being investigated as a potential treatment option in asthma. SAR studies of subjects aged ≥12 years taking CTZ-PSE 5mg/120mg twice
Tiotropium Respimat® add-on to medium-dose inhaled corticosteroids (ICS) daily were evaluated post hoc. The studies were approved by institutional review
has previously been shown to improve both peak forced expiratory volume in boards; informed consent was obtained from all research subjects. Total ocu-
1 second (FEV1) within 3 hours post-dosing (0-3h) and trough FEV1, compared lar symptom score (TOSS) was sum of severity scores for itchy eyes and watery
with placebo, in patients (pts) with moderate symptomatic asthma. Here we eyes. Total nasal symptom score (TNSS) was sum of severity scores for sneez-
evaluate the degree to which these improvements in lung function are sustained ing, runny nose, itchy nose, postnasal drip, and nasal congestion. Individual
over 24 hours in a subset of these pts. Methods: 24-hour spirometric pulmonary symptom scores were rated on 4-point scale (0=none to 3=severe). TOSS
function tests (PFTs) were performed on a subset of pts from two 24-week, changes were assessed for subjects with any baseline ocular symptom score
Phase III, randomized, double-blind, placebo-controlled, parallel-group trials ≥1 and TNSS changes were assessed for subjects with any baseline nasal symp-
(MezzoTinA-asthma®). Pts were required to be symptomatic (seven-question tom score ≥1. Changes from baseline in TOSS and TNSS over a 2-week treat-
Asthma Control Questionnaire score ≥1.5), to have pre-bronchodilator FEV1 ment period, by day in first week, and weekly were assessed. Results: In the
60-90% of predicted, never to have smoked, or to be ex-smokers for ≥1 year CTZ-PSE group, TOSS (N=605) improved 36.8% and 36.2% from baseline
(with <10 pack-years). Pts with chronic obstructive pulmonary disease were and TNSS (N=682) improved 32.4% and 31.6% over 2 weeks (adjusted mean
excluded. Pts received once-daily tiotropium Respimat® 5 mg or 2.5 mg, sal- change: -1.29 and -1.25 for TOSS and -3.02 and -2.89 for TNSS, respectively).
meterol, or placebo, each as add-on to medium-dose ICS (400-800 mg budes- Compared with placebo (TOSS, N=627; TNSS, N=683), TOSS and TNSS
onide or equivalent) maintenance therapy. PFTs were performed at Week 24, improvements in the CTZ-PSE groups were statistically superior in both stud-
10 minutes pre- and post-dose and at intervals throughout the 24-hour period. ies over 2 weeks (P<0.001) (95% CI for difference: TOSS, [-0.69, -0.33] and
Results: Overall, 580 pts were included in the 24-hour PFT subset (pooled data). [-0.70, -0.33]; TNSS, [-1.77, -1.03] and [-1.79, -1.05], respectively). Effect
At 24 weeks, tiotropium Respimat® 5 mg and 2.5 mg add-on to medium-dose sizes were 0.44 and 0.45 for TOSS and 0.56 and 0.58 for TNSS. Conclusion:
ICS significantly improved lung function responses compared with placebo CTZ-PSE 5mg/120mg twice daily effectively relieved both ocular and nasal
(Table), as did treatment with salmeterol. Results for all three active treatment allergy symptoms in subjects with SAR.
arms were comparable versus placebo. Both doses of tiotropium Respimat®
provided sustained and similar improvements in FEV1 at all time points
throughout the 24-hour dosing interval at Week 24. Safety and tolerability of P297
tiotropium Respimat® were comparable with placebo. Conclusion: Once-daily CETIRIZINE-PSEUDOEPHEDRINE COMBINATION EFFEC-
tiotropium Respimat® add-on to medium-dose ICS maintenance therapy pro- TIVELY RELIEVES OCULAR ALLERGY SYMPTOMS IN SUB-
vided significant and sustained improvements in lung function throughout the JECTS WITH SEASONAL ALLERGIC RHINITIS.
24-hour dosing interval in pts with moderate symptomatic asthma. These M.K. Patel*1, E.R. Urdaneta1, K.B. Franklin1, X. Tian2, M. Wu3, Q. Du2,
data support the previously reported improvements in both peak FEV1(0-3h) and 1. Fort Washington, PA; 2. Shanghai, China; 3. Morris Plains, NJ.
trough FEV1 in pts from the same studies following add-on treatment with
tiotropium Respimat®. Objective: To evaluate the efficacy of combination cetirizine-pseu-
doephedrine (CTZ-PSE) for ocular allergy symptom relief in subjects with sea-
Adjusted mean difference versus placebo (95% CI) at Week 24 (mL) sonal allergic rhinitis (SAR). Methods: Two randomized placebo-controlled
SAR studies of CTZ-PSE 5mg/120mg administered twice daily to subjects
aged ≥12 years were evaluated post hoc. The studies were approved by insti-
tutional review boards; informed consent was obtained from all research sub-
jects. Total ocular symptom score (TOSS) was the sum of severity scores for
itchy eyes and watery eyes in both studies. Individual symptom scores were
rated on a 4-point scale (0=none to 3=severe). Subjects with a baseline ocular
symptom score ≥1 were included in the analysis. Changes from baseline in
TOSS over a 2-week treatment period, by day in the first week, and weekly
were assessed. Results: Over 2 weeks in the two studies, TOSS improved 36.8%
and 36.2% from baseline in CTZ-PSE subjects (N=605), with adjusted mean
changes of -1.29 and -1.25, respectively. TOSS improvements in the CTZ-PSE
groups were statistically superior (P<0.001) to those in the placebo groups
(N=627) in both studies (95% CI for difference: [-0.69, -0.33] and [-0.70, -
0.33], respectively). The effect sizes were 0.44 and 0.45 for the CTZ-PSE groups
in the two studies. After the first dose, the daily TOSS for the CTZ-PSE groups
showed significant improvements compared with the placebo groups in Week
1 in both studies (P<0.001). Weekly TOSS for the CTZ-PSE groups was sig-
nificantly reduced compared with the placebo groups in both studies (P<0.001).
Conclusion: CTZ-PSE 5mg/120mg twice daily effectively relieves ocular allergy
symptoms in subjects with SAR.
P298
24-hour PFT subset from full analysis set (pooled data); placebo (n=146) ALLERGIC RHINITIS IN THE ELDERLY: A PILOT STUDY OF
AUC, area under the curve; BID, twice-daily; CI, confidence interval; QD, VITAMIN D SUPPLEMENTATION.
once-daily
M. Columbo*, A. Rohr, Bryn Mawr, PA.
Allergic rhinitis in the elderly is poorly understood as very few studies have
investigated this patient group. VitD insufficiency and deficiency are very com-
mon and VitD appears to play a role in respiratory disease. We studied the effect
of VitD supplementation for 6 weeks in elderly subjects with perennial aller-
A108 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A109
ABSTRACTS: POSTER SESSIONS
gic rhinitis (PAR).This is a double-blind, placebo controlled, cross-over study.
Fifteen subjects with symptomatic PAR (Total Nasal Symptom Score, TNSS≥5
P300
RANDOMIZED, DOUBLE-BLIND, PLACEBO-CONTROLLED
out of 12) received VitD (4,000 I.U./day) and placebo each for 6 weeks. TNSS
(reflective and in the previous 3 weeks) and Rhinitis Related Quality of Life TRIAL OF THE SAFETY AND EFFICACY OF ASTEPRO
Questionnaire (RQLQ) were evaluated at 5 study visits (baseline, and 3, 6, 9, (AZELASTINE 0.15% SOLUTION AND 0.10% SOLUTION) IN
and 12 weeks later). This study was performed in the period November 1, CHILDREN AGES ≥6 TO <12 WITH PERENNIAL ALLERGIC
2013 to March 20, 2014, to try to avoid seasonal fluctuations of serum VitD RHINITIS.
due to sun exposure. All study subjects signed an informed consent and this J.A. Bernstein*1, S. Meltzer2, L. Gever3, N. Ruiz3, J. Blessing-Moore4,
study was approved by the Main Line Hospitals Institutional Review Board. 1. Cincinnati, OH; 2. Long Beach, CA; 3. Somerset, NJ; 4. Palo Alto, CA.
Data were analyzed by the two-tail t test for unpaired data and the Pearson cor- Introduction: Astepro 0.10% and 0.15% are currently approved for use in
relation coefficient. The study subjects’ average age was 77.5±7.3 years, the patients 6 years and older with seasonal allergic rhinitis (SAR) or perennial
Body Mass Index (BMI) was 26.5±4.9, the duration of rhinitis was 57.9±17.8 allergic rhinitis (PAR). The objective of this clinical trial was to evaluate the
years, the total medication score (TMS) was 1.9±1.1. Baseline serum vitamin safety and efficacy of the 0.10% and 0.15% azelastine formulations compared
D was 29.7±10.6 I.U. and serum calcium was 9.6±0.5 mg/dl. TNSS was 7.3±2.2 to placebo at a dosage of 1 spray per nostril twice daily in pediatric patients ≥6
(reflective) and 8±2.6 (3 week). RQLQ score was 58.3±30.9. After the 6 week to <12 yrs with perennial allergic rhinitis (PAR). The results of this study were
VitD supplementation, its serum levels increased significantly (to 39.7±8.9 the basis of approval for the pediatric indication. Methods: This was a 4-week,
I.U., p<0.01), whereas serum calcium remained unchanged. Reflective TNSS randomized, double-blind, parallel-group study in patients ≥6 to <12 years of
(4.6±2.7 and 4.3±3.4 for placebo and VitD at 3 weeks, respectively), 3 week age with moderate-to-severe PAR. The studies were IRB-approved and all
TNSS, and RQLQ (including its individual values) remained unchanged com- patients or guardians signed written, informed consent before participation.
pared to placebo (p>0.4). There was no association between serum VitD and The 12-hour reflective Total Nasal Symptom Score (rTNSS), consisting of nasal
age, BMI, duration of rhinitis, or TMS (p≥0.57). However, in subjects with congestion, runny nose, sneezing and nasal itching, was the primary efficacy
poorly controlled symptoms (TNSS ≥8 of 12, RQLQ for nasal symptoms ≥16 variable. Symptoms were scored twice daily on a 0 to 3 scale (0=none, 1=mild,
of 24), there was an inverse association with serum vitamin D (r>-0.55) that 2=moderate, 3=severe) such that the maximum daily rTNSS was 24. Treatment
was significant for the 3 week TNSS (r=-0.81, p=0.008, n=8). In summary, group comparisons were made by analysis of covariance (ANCOVA). Results:
VitD supplementation for 6 weeks did not improve nasal symptoms or RQLQ A total of 489 patients were randomized to treatment and >90% of patients in
in elderly subjects with PAR. These results and the inverse association between each treatment group completed the study. The change from baseline in rTNSS
VitD and nasal symptoms will require confirmation in larger studies. was statistically significant compared to placebo for both formulations (0.15%;
P = .005 and 0.10%; P = .015). Treatment with the 0.15% formulation resulted
in a mean change of -3.45 rTNSS points from a baseline value of 16.60. The
P299 0.10% formulation resulted in a mean change of -3.37 points from a baseline
DEPOSITION CHARACTERISTICS OF DYMISTA NASAL SPRAY value of 16.35. The mean change with placebo was -2.48 from a baseline value
(AZELASTINE HCL 137 mG / FLUTICASONE PROPIONATE of 16.09. The most frequently reported adverse events with the 0.15% formu-
50 mG) IN AN ANATOMICAL MODEL OF THE HUMAN NASAL lation were epistaxis (4.3%), nasal discomfort (4.3%), dysgeusia (3.7%), and
CAVITY. sneezing (2.5%). The most frequently reported adverse events with the 0.10%
A. D’Addio*1, N. Ruiz1, M. Mayer2, L. Gever1, E.O. Meltzer3, formulation were epistaxis (4.8%), dysgeusia (2.4%), URI (2.4%), and sneez-
1. Somerset, NJ; 2. Baltimore, MD; 3. San Diego, CA. ing (1.8%). There were no serious or unexpected adverse events. Conclusions:
Both the 0.10% and 0.15% Astepro formulations were effective and well tol-
Introduction: Intranasal antihistamines or steroids must be delivered in a
erated in this pediatric study population.
volume and with a technique that allows optimal deposition and distribution
within the nasal cavity. Too little spray volume may not cover the entire nasal
cavity, whereas excess volume may result in outflow from the front of the
nasal cavity or backflow into the throat. In the case of Dymista (AZ/FP) Nasal
P301
Spray, it has been suggested that two generic sprays of the components is equiv- RANDOMIZED TRIAL OF THE SAFETY OF DYMISTA NASAL
alent to the single AZ/FP product, although no evidence exists to support that SPRAY COMPARED WITH FLUTICASONE PROPIONATE
approach. This in vitro evaluation simulated nasal deposition and distribution NASAL SPRAY IN CHILDREN AGES ≥4 YEARS TO <12 YEARS
of AZ/FP compared to sequential sprays of the commercially available AZ and WITH ALLERGIC RHINITIS.
FP components. Methods: A model of a normal adult human nasal cavity was W. Berger*1, P. Ratner2, D. Soteres3, L. Gever4, N. Ruiz4, 1. Mission Viejo,
used to visualize deposition and distribution of nasal spray products. A single CA; 2. San Antonio, TX; 3. Colorado Springs, CO; 4. Somerset, NJ.
spray of Dymista (0.137 mL [137 mg of azelastine/50 mg of fluticasone propi- Introduction: Azelastine hydrochloride (AZ) with fluticasone propionate
onate]) or single sequential sprays of azelastine nasal spray (0.137 mL) fol- (FP) in a single nasal spray (Dymista) is approved for the treatment of patients
lowed by either Flonase or generic fluticasone propionate nasal spray (0.100 12 years of age and older with seasonal allergic rhinitis. The objective of this
mL) were manually actuated into the model. The interior of the cast was coated study was to evaluate the safety of AZ/FP Nasal Spray compared to FP Nasal
with a water-sensitive dye that changes color when exposed to aqueous-based Spray, administered as 1 spray per nostril twice daily in pediatric subjects ≥4
formulations. A slight vacuum (15 L/min) was applied during spray delivery years to <12 years with allergic rhinitis (AR). Methods: This randomized, open-
to simulate inhalation. Results were photographed using anterior and lateral label, 3-month study was conducted at 42 investigational sites in the US. The
views. Results: Three replicates of Dymista showed no dripping or back flow study was approved by a central IRB and informed consent (from caregiver)
from the nasal cavity. Visually, the turbinates in the anterior third of the nasal and pediatric informed assent (from subjects 7 years and older) were obtained
cavity were coated with nasal spray. In contrast, three replicates of azelastine before participation. Qualified subjects had a history of AR, were in good health,
nasal spray followed in 1 minute by either Flonase or generic fluticasone nasal and had no evidence of nasal mucosal erosion, nasal ulceration, nasal septum
spray showed significant dripping from the nostril and toward the back of the perforation, or any significant nasal disease. Subjects were randomized in a 3:1
nasal cavity. Visually, the turbinates were coated with nasal spray as was the ratio to AZ/FP (n=304) and FP (n=101) and were stratified by age as follows:
top portion of the nasopharynx. Conclusions: A single spray of Dymista resulted (1) ≥4 years to <6 years; (2) ≥6 years to <9 years; and (3) ≥9 years to <12
in retention in the nasal cavity compared to sequential administration of the years. Safety was assessed by subject and/or caregiver-reported adverse events
two component products, which caused dripping from the front of the nostril (AEs), nasal examinations, vital signs, and laboratory assessments. Results:
and run-off to the nasopharynx. The two components of AZ/FP Nasal Spray Overall, 94% of subjects treated with AZ/FP and 92% treated with FP com-
delivered sequentially provide a spray volume that exceeds the volume of the pleted the study. Completion rates were similar in each age strata. The per-
nasal cavity and therefore may negatively impact therapeutic efficacy and patient centage of subjects with AEs was comparable between treatment groups and
tolerability. across the age strata. The most frequently reported AEs with AZ/FP and FP,
respectively, were: epistaxis (10% and 9%), headache (7% and 3%), cough (4%
and 3%) and pyrexia (3% and 2%). The discontinuation rate due to AEs was
2% with AZ/FP and 4% with FP. Laboratory parameters showed no meaning-
ful increase in mean or median values in either treatment group. Improve-
ments in nasal examination findings were observed in both treatment groups
and in each age stratum and there were no findings of nasal mucosal ulcera-
VOLUME 113, NOVEMBER, 2014 A109
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A110
ABSTRACTS: POSTER SESSIONS
tion or septal perforation. The two treatment groups were comparable for mean showed no differences between two groups as in vitro test, total IgE and blood
changes in vital sign measurements regardless of age stratification. Conclu- eosinophil count. Conclusion: Symptom severities of allergic rhinitis patients
sions: AZ/FP and FP were well-tolerated during this 3-month study when admin- sensitive to multiple allergens showed no differences with those of patients sen-
istered as 1 spray per nostril twice daily in pediatric subjects ≥4 years to <12 sitive only to house dust mite.
years with AR.
P304
P302 THE EFFICACY OF A NASAL ANTIHISTAMINE AZELASTINE
EFFICACY OF AZELASTINE HCL AND FLUTICASONE PROPI- HYDROCHLORIDE AND CORTICOSTEROID FLUTICASONE
ONATE IN A SINGLE NASAL SPRAY (DYMISTA) IN TREATING PROPIONATE FOR THE TREATMENT OF SEROUS OTITIS
OCULAR SYMPTOMS OF SEASONAL ALLERGIC RHINITIS. MEDIA.
B. Stanaland*1, R. Settipane2, S. Gawchik3, N. Ruiz4, F. Hampel5, S. Nsouli*, Danville, CA.
1. Naples, FL; 2. Providence, RI; 3. Upland, PA; 4. Somerset, NJ; 5. New Since chronic inflammation is the histopathologic landmark of otitis media
Braunfels, TX. with effusion, clinical observations have led us to believe that the combination
Introduction: The efficacy of azelastine HCL (AZ) and fluticasone propi- of a nasal antihistamine Azelastine and corticosteroid Fluticasone propionate,
onate (FP) in a single nasal spray (Dymista [AZ/FP]) for treating nasal symp- with an oral antibiotic may be more effective than monotherapy with an oral
toms of seasonal allergic rhinitis (SAR) has been demonstrated in four well- antibiotic in the treatment of serous otitis media. We studied forty adult patients
controlled clinical trials of 2 weeks duration.1,2,3 The reflective total ocular in a randomized open labeled 2-week trial to compare the efficacy of the com-
symptom score (rTOSS), consisting of itching, watering, and redness, was a bination nasal Azelastine and Fluticasone propionate (137mcg/50 mcg), one
secondary variable in the studies. This post-hoc analysis compared the efficacy spray per nostril twice daily, with an oral antibiotic Amoxicillin/Clavulanate
of AZ/FP to monotherapy with AZ, FP, and placebo for the treatment of ocu- potassium (875mg/125mg) every 12 hours, for the treatment of otitis media
lar symptoms of SAR. Methods: A total of 3996 patients 12 years of age and with effusion. The efficacy of the treatment options was assessed using pneu-
older with moderate-to-severe SAR were included in the analyses. The studies matic otoscopy, impedance tympanometry, and audiometry to monitor the clin-
were IRB-approved and all patients signed written, informed consent before ical course of the middle ear effusion in both treatment groups. In the combi-
participation. Patients were randomized to AZ/FP, AZ, FP or placebo nasal nation group nasal Azelastine and Fluticasone with oral antibiotic, a resolution
spray administered 1 spray/nostril twice daily (total daily doses: AZ=548 mg; of otitis media with effusion occurred at the 8th day. In contrast in the group
FP=200 mg). The three ocular symptoms were scored twice daily on a 4-point treated with monotherapy with the oral antibiotic, the resolution of otitis media
scale (0=no symptoms; 1=mild, 2=moderate, 3=severe) such that the maximum with effusion occurred on the 14th day. In conclusion, the combination of nasal
daily score was 18. Treatment group comparisons of change from baseline in Azelastine and Fluticasone plus an oral antibiotic may be a safer and shorter
rTOSS were made by analysis of covariance (ANCOVA). Time to response therapy than monotherapy with an oral antibiotic in the treatment of serous oti-
(defined as a ≥50% change from baseline) was evaluated by log-rank test. tis media, given the safety issues with long-term use of systemic antibiotics.
Results: Overall, patients treated with AZ/FP had a significantly greater
improvement from baseline in rTOSS compared to AZ (P=.048), FP (P<.0001),
and placebo (P<.0001). Patients treated with AZ/FP achieved at least a 50% P305
reduction in rTOSS significantly sooner than patients treated with FP (P=.02) EFFICACY AND SAFETY OF BECLOMETHASONE DIPROPI-
or placebo (P≤.0001). The difference approached significance versus AZ ONATE NASAL AEROSOL IN CHILDREN (4-11 YEARS OF AGE)
(P=.08). When patients with baseline rTOSS ≥8 were analyzed (n=3341; rep- WITH PERENNIAL ALLERGIC RHINITIS.
resenting 84% of the total population), significant differences were seen com- W. Berger*1, R. Jacobs2, N. Amar3, S. Tantry4, J. Li4, C. Small4, 1. Mission
pared to AZ (P=.04) as well as to FP (P<.01) and placebo (P<.001). Conclu-
Viejo, CA; 2. San Antonio, TX; 3. Waco, TX; 4. Frazer, PA.
sions: In this population of patients with moderate-to-severe SAR, AZ/FP
improved ocular symptoms to a significantly greater extent than AZ or FP alone. Introduction: Beclomethasone dipropionate (BDP) nasal aerosol (non-
1
Hampel FC et al. Ann Allergy Asthma Immunol. 2010;105:168-173; 2Carr W aqueous) is approved for management of seasonal and perennial allergic rhini-
et al. JACI. 2012;129:1282-1289; 3Meltzer EO et al. Allergy Asthma Proc. tis (SAR/PAR) in adolescents and adults. This study evaluated the efficacy
2012;33:324-332 and safety of 80 mg/d BDP nasal aerosol in children with PAR. Methods: A
12-wk, phase 3, randomized, double-blind, placebo-controlled, parallel-group,
clinical trial was conducted at 62 US centers to investigate the efficacy and
P303 safety of BDP nasal aerosol in children (4-11 y of age) with PAR. A total of
547 patients were randomized (2:1) to receive 2 actuations of BDP nasal aerosol
ASSESSMENT OF SYMPTOM SEVERITIES OF ALLERGIC
(1 actuation/nostril; 40 mg/actuation) or placebo nasal aerosol once daily. The
RHINITIS PATIENTS SENSITIVE TO MULTIPLE ALLERGENS
primary end point was change from baseline in average morning (am) and
COMPARED TO SINGLE ALLERGEN IN MAST.
evening (pm) reflective total nasal symptom score (rTNSS) over the first 6 wk
B. Yu*1, J. Lee2, D. Lee2, 1. Uijeongbu, Republic of Korea; 2. Daejeon, of treatment in patients 6-11 y of age. Additional efficacy end points included
Republic of Korea. change from baseline in average am and pm instantaneous TNSS (iTNSS) in
Background and Objectives: To assess the symptom severities of allergic children 6-11 y of age, and change from baseline in average rTNSS and iTNSS
rhinitis patients sensitive to multiple allergens compared to single house dust in children 4-11 y of age. Results: Improvement was significantly greater with
mite allergen. Subjects and Method: Total 56 allergic rhinitis patients were clas- BDP nasal aerosol (80 mg/day) than with placebo over the first 6 wk of treat-
sified into 2 groups. The multiple allergens group was defined as patients sen- ment in children 6-11 y of age in average am and pm rTNSS and iTNSS (mean
sitive to multiple allergens including house dust mite in MAST. The single aller- [95% CI] treatment difference: –0.66 [–1.08, –0.24], P = 0.002 and –0.58 [–0.99,
gen group was defined as patients sensitive only to house dust mite. Symptom –0.18], P = 0.004, respectively). Improvement in average am and pm rTNSS
severity was evaluated with visual analogue scale (VAS) for following symp- and iTNSS was significantly greater in patients 4-11 y of age receiving BDP
toms: postnasal drip, anosmia, sneezing, itching, nasal obstruction, cough, spu- nasal aerosol than in those receiving placebo over the first 6 wk of treatment
tum, headache, and rhinorrhea. For in vitro test, total IgE and blood eosinophil (P = 0.002 and P = 0.004, respectively). Similar results were observed over 12
count were also analysed. IRB approval and informed consent was obtained wk of treatment (P < 0.001). Improvement in average am and pm reflective
from all research subjects. Results: Among 56 patients, 32 patients were clas- individual nasal symptoms over the first 6 wk of treatment in 6-11 y olds was
sified to the multiple allergens group and 24 patients were classified to the significantly greater for rhinorrhea (P = 0.004), nasal congestion (P = 0.001),
single allergen group. The mean symptom scores of multiple allergens group and sneezing (P = 0.002) with BDP nasal aerosol than with placebo. BDP nasal
for postnasal drip, anosmia, sneezing, itching, nasal obstruction, cough, spu- aerosol was well-tolerated in children, with a safety profile comparable to
tum, headache, rhinorrhea were 4.56±3.4, 1.25±2.40, 1.25±3.40, 4.25±3.11, placebo. Conclusions: This study showed that once-daily treatment with 80 mg
3.44±3.56, 5.75±3.30, 3.87±3.25, 3.50±3.45 and 5.21±3.17. On the other hand, BDP nasal aerosol (nonaqueous) in children 4-11 y of age was safe and effec-
the mean symptom scores of single allergen group for postnasal drip, anos- tive in controlling nasal symptoms associated with PAR, suggesting that BDP
mia, sneezing, itching, nasal obstruction, cough, sputum, headache, rhinorrhea nasal aerosol is effective for children with PAR.
were 2.75±2.77, 1.29±3.01, 1.29±3.01, 4.46±3.60, 3.41±3.67, 5.75±3.13,
2.88±3.03, 2.75±3.57 and 3.70±3.22. Total summation of symptom scores for
two groups was 33.75±22.24 and 37.75±16.89 each. Statistically these scores
A110 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A111
ABSTRACTS: POSTER SESSIONS
matophagoides pt., found in 21.0 % (8/38) patients. Positive skin prick tests
P306 with Candida albicans occurred in 18.4% (7/38), with Alternaria alternata in
COMPLEMENTARY THERAPY FOR TREATMENT OF ALLER-
18.4% (7/38), with Cladosporium herbarium in 10.52% (4/38), with Aspergilus
GIC RHINTIS. fumigatus in 5.26 % (2/38), and with Botrytis cinerea in 2.63 % (1/38). None
J. Kern*1, L. Bielory2, S. Luster2, 1. Newark, NJ; 2. Springfield, NJ. of these patients had sensitization to other mold allergens. Elevated allergen
Introduction: Allergic rhinitis is a prevalent condition impacting approxi- specific IgE was seen for Candida in 24% (9/38) patients, Alternaria alternata
mately 20% of the US population. There is a growing section of the popula- 26% (10/38), and Cladosporium herbarium in 8% (3/38). Conclusion: Nearly
tion, up to 50% in some surveys, who are turning to alternative therapies for half of chronic sinusitis patients had sensitization to at least one allergen. Mold
the treatment of their allergic rhinitis. Methods: A literature search was per- allergy was commonly seen in chronic sinusitis patients requiring surgery, being
formed utilizing keywords rhinitis acupuncture, rhinitis traditional Chinese comparable in occurrence to dust mite sensitization.
medicine (TCM), and rhinitis alternative therapy. Randomized control trials
were reviewed in regards to their impact on symptom scores and objective equiv-
alents and are displayed in table 1. Results: Decrease in total IgE: 39% from P308
Yang et al. correlating with symptom improvement using various TCM for- EPIDEMIOLOGY OF ALLERGY IN VARIOUS CHILDREN OF
mulations. 13.7% reduction in Zhang et al. Jung et al. showed a 3% increase VARIOUS AGE GROUPS IN WESTERN HUNGARY FROM 2002
in IgE levels in the group receiving TCM. Yang et al. demonstrated a 15% reduc- TO 2005 AND FROM 2006 TO 2009.
tion in specific IgE to dust mites (p<.05). Acupuncture has been shown to L. Soti1, Z. Petz1, L.M. DuBuske*2, 1. Szombathely, Hungary; 2. Gardner,
have an impact on patient symptom scores as evidenced in table 1. In a ran- MA.
domized control trial by Brinkhaus et al. there was a minimal, however statis-
tically significant, improvement in symptom score with acupuncture compared Background: The onset allergic diseases by age and gender may vary in
to sham therapy and medication alone. A follow up study comparing the com- childhood. The prevalence of various allergic diseases in patients stratified by
bination of acupuncture with medication versus sham therapy with medica- gender into age groups who presented at the Allergy Outpatient Clinic of West-
tion showed a reduction of 9% in the utilization of medication [p=0.01]. A large ern Hungary from 2002-2005 and from 2006-2009 were assessed. Methods:
portion of studies were poorly constructed with significant bias given the oper- Only patients with newly diagnosed allergic diseases confirmed by skin prick
ators’ awareness of real versus sham therapy when applying acupuncture. Home- tests and/or allergen specific IgE were assessed, being stratified by age into
opathic therapy has been evaluated in several studies demonstrating mixed groups from newborn to 20 years old. From 2002 to 2005, there were 10,018
results in regards to its impact on allergic rhinitis. Several have found signifi- patients and from 2006 to 2009, there were 13,125 patients included in this epi-
cant improvement. Taylor et al. demonstrated nasal airflow mean difference demiologic study. Results: The total number of allergic patients increased from
19.8 L/min [p=0.0001], visual analogue score showed a symptom reduction of 0 through 5 years of age, then declined until adulthood in both investigated
28% in homeopathic group vs 3% reduction in placebo group [p=0.0007]. A periods. There were more male patients under the age of 15, especially in the
larger study conducted by Aabel et al found no difference in symptom scoring 5 year old age group in every year of the investigated period. After 15 years of
from placebo. Conclusion: The evidence regarding the utilization of traditional age the female/male patient ratio increases rapidly. At 20 years of age, females
Chinese medicine is mixed. Complementary therapy for allergic rhinitis demon- are twice as likely to present with allergic diseases. Both the female and male
strates a potential benefit to patients in addition to current medical therapies. patients in the age group analysis of various allergic diseases demonstrated
Alternative therapy studies revealed mixed results, however safety studies have the pattern of the “allergic march”. Conclusion: Peak incidence of various aller-
shown minimal to no risk making them a safe addition to the treatment regime gic diseases occurred in the 5 years old age group. In early childhood the
in select patients. male/female ratio among allergic patients is high, this ratio being reversed in
later adolescence. Patterns of prevalence of various childhood and adolescent
Table 1 allergic disease in Western Hungary demonstrated the progression from der-
matologic to respiratory allergy characteristic of the allergic march.
P309
CEREBROSPINAL FLUID (CSF) RHINORRHEA PRESENTING
THREE YEARS AFTER HEAD TRAUMA.
M. Shum*1, K. Chotikanatis2, T.A. Saadia2, R. Joks2, 1. New York, NY;
2. Brooklyn, NY.
Background: The time interval from diagnosis of pseudotumor cerebri to
development of CSF rhinorrhea is quite variable in literature. It can be inter-
mittent and undetected for many years or may be the presenting symptom. We
report a case of CSF rhinorrhea presenting three years after head trauma and
pseudotumor cerebri. Methods: A 35-year-old woman with a five-year history
of perennial allergic rhinitis to cat and mouse and moderate persistent asthma
complained of intermittent persistent unilateral clear rhinorrhea, without any
nasal congestion, sneezing or pruritus of six months duration. She denied any
associated headache or wheezing. Results: Further review of systems was
P307 notable for history of head trauma three years prior to presentation, with devel-
PREVALENCE OF MOLD SENSITIZATION IN CHRONIC RHI- opment of pseudotumor cerebri, sinovenous thrombosis, papilledema, and mac-
NOSINUSITIS PATIENTS REQUIRING SURGERY. ular degeneration. However, there was no skull fracture. Nasal examination was
R. Gawlik1, E. Czecior1, W. Scierski1, L.M. DuBuske*2, 1. Katowice, remarkable for swollen bilateral inferior turbinates. She was able to produce
Poland; 2. Gardner, MA. left sided nasal clear rhinorrhea by leaning forward. Fluid was tested for glu-
cose and was found to be 307 mg/dL. She was promptly referred to neuro-
Background: Mold sensitization is a risk factor for development and dete- surgery. Confirmatory tests for new onset diabetes were performed given the
rioration of upper airway allergy, especially chronic rhinosinusitis including degree of elevated glucose in the CSF. Discussion: Etiology of CSF rhinorrhea
those requiring surgery. Methods: 38 chronic sinusitis patients after surgery is classified as traumatic (>90%) or nontraumatic (<10%). Accidental head
were included into the study. Routine medical examination, skin prick tests injury accounts for most traumatic cases, followed by iatrogenic etiology sec-
with common inhaled allergens an extended mold panel (Alternaria alternate, ondary to neurosurgical or rhinologic procedure. Nontraumatic causes are
Cladosporium herbarium, Aspergilus fumigatus, Candida albicans, Mucor typically due to high intracranial pressure, tumors, erosive diseases, congeni-
mucedo, Botrytis cinerea, Rhisopus nigricans, Penicilliumi notatum, Fusarum tal defects of base of skull, or spontaneous without a specific etiology. Though
moniliforme Pullularia pullulans (Allergopharma, Germany) was done and our patient had no history of skull fracture to account for a CSF leak, she did
IgE and allergen specific IgE measurement (Phadia, Sweden). All subjects were have a history of pseudotumor cerebri after the trauma. While CSF rhinorrhea
seen by an otolaryngologist and mycological examination was performed. is a relatively rare entity in comparison to other common sinonasal inflamma-
Results: Sensitization to at least one allergen was present in 44.7% (17/38) of tory conditions such as the allergic rhinitis in our patient, this case illustrates
sinusitis patients. The most prevalent was sensitization to house dust mite Der- the importance of maintaining a high index of clinical suspicion when encoun-
VOLUME 113, NOVEMBER, 2014 A111
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A112
ABSTRACTS: POSTER SESSIONS
tering a complaint of unilateral clear rhinorrhea with a remote history of trauma was positive in 11.4% patients, negative antinuclear antibodies in all cases but
and/or increased intracranial pressure. This will ensure timely diagnosis and the antibodies anti thyroid (AAT) positive in 11.4% of LE cells, lupic antico-
proper neurosurgical management that can ultimately prevent further compli- agulant and D dimer were negative in all patients and rheumatoid factor was
cations such as bacterial meningitis or other serious intracranial infections. positive in 1 patient. Positive patients AAT 100% were women and 75% of them
had negative PSA. Tests of correlation between ASST and antibodies, was not
significant. Conclusion: Patients with UCE most are women and only 11% had
P310 positive ASST but this does not correlate with anti thyroid antibodies or other
CHALLENGES OF CHRONIC COUGH. common parameters of autoimmunity
V. Ta*1, K. Woessner2, 1. Redondo Beach, CA; 2. San Diego, CA.
Introduction: Establishing gastroesophageal reflux disease (GERD) as the
cause of chronic cough is challenging despite a careful history and initial eval-
P312
A RETROSPECTIVE REVIEW OF CHRONIC URTICARIA AND
uation because not all patients present with the usual symptoms of GERD. The
term supraesophageal reflux disease (SERD) has been used to describe GERD BODY MASS INDEX (BMI) IN A HISPANIC COHORT.
with additional symptoms such as sore throat, hoarseness, globus, and exces- M. Rodríguez-Roa*, C.M. Pimentel, B.K. Di Giorgi, J. Méndez,
sive throat clearing. It should be emphasized that these laryngeal findings are I. Malinow, C. Ramos, S. Nazario, San Juan, Puerto Rico.
not specific for SERD as a causative factor and the precise pathophysiologic Background: Chronic urticaria (CU) is a benign, idiopathic and disturbing
mechanism responsible for the production of supraesophageal symptoms condition affecting a significant proportion of patients. A state of obesity has
remains contentious. Case: The patient is a 60 year old male who presented been linked with atopic diseases such as asthma. The association of obesity and
with throat clearing and nonproductive chronic cough of one year duration. The CU has not been established. Methods: We performed a retrospective analysis
cough occurs daily and is associated with the sensation of postnasal drip of 86 Hispanic patients with CU visiting an Allergy and Immunology Clinic
although he is unable to expectorate mucus. His symptoms are not positional from June 2012 - August 2013 in Puerto Rico. Cases were stratified between
or triggered by fumes or exercise. He denies food impaction or heartburn symp- physical urticaria (PU) and idiopathic urticaria (CIU). Demographic charac-
toms. The patient has tried various nasal corticosteroids, antihistamines, sys- teristics, comorbid diseases, and associated symptoms were compared. Data
temic corticosteroids and proton pump inhibitors (PPI) but these interventions was analyzed using SPSS v19. Results: Subjects mean age was 32 ± 20 years,
failed to control his symptoms. His workup included negative skin prick, intra- 77% were female. Concurrent atopic diseases were reported in 48% of patients,
dermal, and serum specific IgE testing to aeroallergens. His nasal cytology was 31% had asthma. Most commonly associated symptom was angioedema (38%).
negative for eosinophils. His CT sinus showed maxillary sinus mucosal thick- Forty-four (51%) patients had CIU, while 41 (48%) had PU. 56% of the patients
ening. He underwent an upper esophagogastro-duodenoscopy that showed no with PU reported more than one physical trigger. No significant associations
furrows, white patches, or ulcers. However, mid/proximal esophagus biopsy were found between gender, thyroid disease, allergic rhinitis or food allergy
showed greater than 50 eosinophils on high power field. He also underwent a and type of urticaria. Thyroid disease was more prevalent in adult participants
24 hour pH probe which showed a supine pH average of 4.75. Discussion: Ini- (16/66; 24%), while allergic rhinitis was more common in adolescents and chil-
tial treatments include PPI and head of bed elevation even though acid sup- dren (19/27; 70%). Patients with BMI > 25 were significantly more likely to
pressing medications have been shown to be only partially effective in treating have PU (20/31 (65%); p = 0.025), while subjects with a BMI <25 were two
SERD. Other options include surgery such as the Nissen fundoplication or the times more likely to suffer from CIU (29/49 (59%); p = 0.039). Conclusions:
LINX System. Although 50 eosinophils/HPF was observed histologically, the A significant association was found between increased BMI and PU com-
patient denied any EoE symptoms and on these grounds the possibility of EoE pared to CIU. Studies are needed to evaluate the modulation of adipose tissue
was dismissed. The more likely explanation for this patient’s cough is SERD, on mast cells and basophil degranulation.
evident by his positive 24 hour pH probe. The patient tried and failed a short
course of PPIs, however, a longer trial of a PPI is warranted. If ineffective, sur-
gery will be considered.
24 hour pH probe
P311
EVIDENCE OF AUTOIMMUNITY IN PATIENTS WITH SPONTA-
NEOUS CHRONIC URTICARIA (SCU).
M.I. Rojo-Gutierrez, C.N. Flores Ruvalcaba*, J. Mellado Abrego,
G. Castillo Narvaez, P. Ramirez Rojo, Mexico City, DF, Mexico.
Spontaneous Chronic Urticaria (SCU ) is a common condition in adults and
mainly among women, which coincides this phenomenon with autoimmunity.
Our objective was assessed through laboratory studies whether patients with
CUS presented autoimmunity data. Material and Methods: Cross-sectional
study that 35 patients from the Allergy and Immunology at Juarez Hospital of
Mexico diagnosed with CUS included, to which complete blood count CBC,
thyroid antibodies (anti peroxidase and thyroglobulin), nuclear antibodies,
rheumatoid factor, lupus anticoagulant and autologous serum skin test (ASST).
Results: We evaluated 35 adult patients, 77.1% female and 22.9% male, ASST
A112 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A113
ABSTRACTS: POSTER SESSIONS
patients to unnecessary medications and stress for months before reaching a
P313 diagnosis or worse delay a diagnosis of underlying malignancy. Case Descrip-
EFFICACY OF ANTI-IGE MONOCLONAL ANTIBODIES AT A
tion: Patient was a 52 year old female with past medical history of hyperten-
DOSE OF 150 TO 300MG IN PATIENTS WITH CHRONIC sion who was in her usual state of health until July 2013.She started having
URTICARIA SPONTANEOUS (CUS) WITH FAILURE IN THE raised, painful, edematous and erythematous lesions. The tended to appear first
EFFICACY OF ANTIHISTAMINE. in her hands and feet then rapidly spread to her forearms, legs and face. She
M.I. Rojo-Gutierrez*, C.N. Flores Ruvalcaba, J. Mellado Abrego, occasionally had them in her chest. These lesions would appear every 7-8 days.
G. Castillo Narvaez, M. Gonzalez ibarra, Mexico City, DF, Mexico. They would last for 3-4 days then disappear, mostly spontaneously. She noticed
Urticaria is a very common disease of skin, characterized by rapid onset of that they were preceded almost always by fever. The patient initially went to
hives with or without angioedema. It is classified by etiology ; in spontaneous the emergency room after the lesions first appeared. She was told that the lesions
and inducible urticaria, and evolution in acute and chronic. IgE. CSU is more were likely hives and she was discharged home to follow up with her primary
common in women and international management guidelines recommend 2nd care physician. Her primary care physician switched her medication for hyper-
generation antihistamines regulate dose or higher doses and in cases of failure tension (lisinopril) to another drug but that did not help. Later she was started
suggest the use of monoclonal antibodies against IgE. Monoclonal antibodies on a short course of prednisone 40mg daily for 10 days. She also was prescribed
are effective at doses of 150 and 300 mg so our aim was to determine their topical corticosteroid and anesthetic creams. Patient did not have any relief
effectiveness at doses of 150mg and 300mg in patients with CSU. Materials with any of these interventions. Lesions continued to be a major concern for
and methods: We evaluated 35 patients who failed UCE in conventional anti- her. So, she was referred to a dermatologist and biopsy was performed for one
histamine therapy .Two groups were randomly performed where the group : of these lesions. The biopsy was consistent with “neutrophilic dermatitis”.
A) 20 patients received 150 mg single subcutaneous dose of omalizumab and Patient later was referred to a hematologist/oncologist to rule out underlying
B) 300mg 20 patients . Evaluate effectiveness by measuring frequency and malignancy. She was also referred to an Allergy-Immunology clinic where we
intensity of the lesions with a baseline measurement UAS7 (Urticaria activity had the chance to see her. She did not have active lesions at the time we saw
score 7 days) and weekly reviews and quality of life questionnaire (CUQ2oL) her in the clinic but she showed us pictures she took for them at different sites
on arriving a week 1, 2 and 3. Results: we evaluated 40 patients 22.5 % (9) were of her skin. Our plan was to start the patient on colchicines as prednisone failed
male and 78.5 % (31) females. The mean was 226.93 CUQ2oL at baseline, 93.7 to show any improvement in her symptoms. Conclusion: It is crucial for gen-
at the first week, 57 the second and the third 44.33. Hives/ pruritus in stock- eral practitioners and allergists to keep sweet syndrome in the differential diag-
ings 2.2/2.5 at startup, the first week 1.35/1.45, 0.9/1.1 second and 0.98 / 1.08 nosis of acute skin eruptions. As long as it is in the differential, the diagnosis
the third, we find highly significant differences when comparing home against can be confirmed with a skins biopsy. However, management can be as easy
1st week, 2nd week and 3rd week p < 0.0001 . Conclusions: Omalizumab is as discontinuing a causative drug or gets more complicated if there was an
highly effective in controlling symptoms of chronic spontaneous urticaria. underlying malignancy. That’s why it is important to increase awareness of
this rare condition.
P314 P316
SEVERE ATOPIC DERMATITIS EXACERBATED BY STAPHY-
LOCOCCUS INTERMEDIUS. ATOPIC DERMATITIS IN CHILDREN: COST-EFFECTIVENESS
COMPARATIVE ESTIMATION OF VARIOUS IMMUNOTROPIC
V. Bozoghlanian*, D. Levy, R. Gutta, Irvine, CA.
THERAPY PROGRAMMES.
Introduction: Staphylococcus aureus is known to exacerbate atopic der-
matitis with production of bacterial enterotoxins and superinfection of lesions. T. Slavyanskaya*1, V. Derkach2, B. Sangidorj1, 1. Moscow, Russian Feder-
We report the first case of severe atopic dermatitis in a human exacerbated by ation; 2. Vladivostok, Russian Federation.
Staphylococcus intermedius, which has been associated with exacerbation of The study was aimed at conducting a comparative cost-effectiveness (CE)
atopic dermatitis in dogs. Case Description: A 26 year old Hispanic man pre- analysis of various immunotropic therapy (IT) programmes of atopic dermati-
sented with a 6-year history of extremely pruritic diffuse rash consistent with tis (AD) in children. 94 children at the age of from 3 to 18 with AD having
atopic dermatitis. He was referred for total IgE >16,000 IU/ml and failure to lasted for 1-15 years were examined. All the patients received routine clinical
respond to high-dose topical and oral corticosteroids, methotrexate, and immuno-allergological examinations. The treatment was conducted in
cyclosporine, and phototherapy. In our clinic, an immunodeficiency evaluation two stages: background therapy (BT) and IT. The patients were divided into
was normal. Workup for hyper-IgE syndrome, including STAT-3 and Dock-8 three groups: the 1st group (n=30) received immunomodulator (IM) on a step-
gene mutations, was normal. Skin biopsies were negative for malignancy, fun- by-step basis in the course dose of 20 mg; the 2nd group (n=31) received an
gal staining, or vasculitis, and suggestive of severe atopic dermatitis with nor- accelerated course of parenteral allergen-specific IT (PASIT); in the 3rd group
mal immunofluorescence and immunophenotyping. Workup for a 70-pound (n=33) a combination IT (CIT) - IM+PASIT at an accelerated pace was applied.
unintentional weight loss was performed, with negative SPEP, UPEP, HIV, HTLV, The CE comparative estimation of IT in the treatment of children with AD has
bone marrow biopsy, flow cytometry, CT chest/abdomen/pelvis, endoscopies, shown the most optimal ratio in the 3rd group of patients receiving CIT. How-
and autoimmune evaluation. The patient had multiple severe exacerbations ever, in the 1st and the 2nd groups in which IM and PASIT were applied, AD
requiring several hospitalizations. Aggressive skin care measures (including was not monitored well enough, that resulting from considerable expenses for
wet/dry wraps), high-dose antihistamines, gabapentin, oral antibiotics, a one- hospital care. The ratio of costs for treating children with AD in hospital envi-
month trial of terbinafine, and a five-month trial of omalizumab were not effi- ronment who received IM (the 1st group) was 42.95% of the total cost of AD
cacious. Multiple skin cultures identified highly-resistant Staphylococcus inter- treatment per year within direct expenses; the medicinal treatment was 48.12%.
medius. The patient developed malignant otitis externa treated with daptomycin Among expenses for medications, 30.6% were for IM, and the other ones were
and meropenem. Cultures from the ear also grew Staphylococcus intermedius. associated with conducting BT for improving AD monitoring. In the 2nd group
His skin lesions improved on the IV antibiotics, but he continued to have a of children receiving PASIT, the principal item of direct expenses was the
relapsing-remitting course when the antibiotics were withdrawn. Discussion: amount spent for visiting the allergologist for administering injections. The
Staphyloccocus intermedius has been associated with exacerbation of atopic expenses for hospital care were 15.1%. In the 2nd group, the principal costs
dermatitis in dogs. It may be transmitted to humans with close contact to dogs. were associated with medicinal treatment of infectious complications. In the
In patients with severe atopic dermatitis refractory to first and second line ther- 3rd group of children receiving CIT, the percentage of direct expenses for hos-
apies, it may be prudent to investigate for Staphyloccocus intermedius colo- pital care was 8.92%, thus, being insignificant. Expenses for outpatient care
nization and/or infection, and if identified, should be treated with tailored antibi- (5.95%) and BT (8.95%) in this group were much lower than in the 1st and the
otic therapy based on drug sensitivity. 2nd groups due to the absence of infectious complications and reduction of
BT volume. Inclusion of CIT in the integrated programme of therapy of chil-
dren with AD resulted in reduction of BT volume, less admissions to hospital,
P315 prevention of secondary infection overlay; moreover, the disease was moni-
WHY IS IT IMPORTANT TO KNOW ABOUT SWEET SYN- tored efficiently at the same time. Thus, the CE ratio of the treatment was
DROME? more rational.
A. Hamad*, Madison Heights, MI.
Introduction: Sweet syndrome has a presentation that is not uncommon;
acute skin eruptions. It could be mistaken for many other conditions and expose
VOLUME 113, NOVEMBER, 2014 A113
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A114
ABSTRACTS: POSTER SESSIONS
P317 P319
CHRONIC IDIOPATHIC/SPONTANEOUS URTICARIA: PATIENT AN UNUSUAL PRESENTATION OF TOXIC EPIDERMAL
CHARACTERISTICS AND RESOURCE USE. NECROLYSIS IN A PATIENT WITH SYSTEMIC LUPUS ERY-
G. Sun1, K. Raimundo2, E. Antonova3, E. Chang1, M. Broder*1, 1. Beverly THEMATOSUS.
Hills, CA; 2. South San Francisco, CA; 3. San Francisco, CA. R. Patel*1, G. Jyothirmayi2, E. Capitle2, 1. Long Island City, NY;
Introduction: Chronic idiopathic (spontaneous) urticaria (CIU) is a rare and 2. Newark, NJ.
symptomatic skin condition affecting patient health-related quality of life. Data Introduction: Toxic Epidermal Necrolysis (TEN) is a dermatologic disor-
on CIU-related healthcare resource use (HCRU) are old. We examined HCRU der characterized by diffuse erythema and necrosis of the epidermis. TEN can
and costs in CIU patients using a healthcare claims database. Methods: We used occur secondary to drugs, infections or autoimmune disorders (1). Methods:
a HIPAA-compliant fully de-identified commercial healthcare claims database This is a 43 year old female,with a history of SLE maintained on hydroxy-
from 2012 for this retrospective cohort study. We identified CIU patients with chloroquine and azathioprine, hypertension and hypothyroidism, who presented
a previously validated ICD-9-CM coding algorithm. We examined patient char- with a progressively worsening erythematous and tender skin rash affecting her
acteristics, HCRU, and costs. Outcomes were stratified by demographics. We entire body. She was seen prior for a similar skin rash under the breast and dis-
used chi-square tests and F-tests to conduct bivariate analyses. Because the charged on cephalexin and fluconazole for possible cellulitis vs a fungal infec-
study did not involve human subjects, IRB review was not needed. Results: The tion. She reported myalgias but denied any fever, vision changes, chest pain,
prevalence of CIU was 0.1% among all continuously enrolled patients. We iden- shortness of breath, or genitourinary complaints. On physical examination,
tified 6,350 CIU patients with mean age 42.4 years, 68.3% women, and mean the patient was afebrile, with a blood pressure of 81/57, heart rate of 106, and
Charlson Comorbidity Index 0.9. CIU-related comorbidities included allergic a diffuse, erythematous, exudative, desquamating rash over 70 percent of her
rhinitis (43.2%), angioedema (23.5%), and asthma (18.3%). The most com- body including mucous membranes but no ocular involvement. Results: Fur-
monly prescribed drug classes were oral corticosteroids (OCS; 54.7%), anti- ther work up revealed leucocytois on CBC. The severity of illness score for
histamines (24.0%), and leukotriene receptor antagonists (17.5%). Mean all- TEN (SCORTEN) was 5 out 7 indicating a 90% mortality rate. Her acute symp-
cause total annual healthcare costs were $9,142 per CIU patient; outpatient toms were managed with intravenous (IV) fluids and broad spectrum antibi-
services accounted for 43.0% of the costs. Per year, CIU patients averaged 15.1 otics. Infectious work up was negative. Skin biopsy was indicative of TEN and
physician office visits, 7.3% of patients had at least one hospitalization, and she was treated with IV Immunoglobulin and steroids. Discussion: TEN is a
15.9% – at least one emergency department (ED) visit. Total costs and HCRU life threatening skin disease and must be managed rapidly. This disorder belongs
increased significantly with age. Women accrued higher costs and had more on a spectrum of skin diseases, which also involve Erythema Multiforme Major
hospitalizations and ED visits than men. CIU-specific annual costs totaled $997 and Minor and Steven’s Johnson Syndrome. History is an important aspect in
per patient, and outpatient services accounted for about 2/3 of costs. Patients the diagnosis of this condition. Details involving medication history, recent
averaged 3.4 office visits for CIU-specific claims; 0.1% of CIU patients had infections, and underlying autoimmune diseases must be thoroughly reviewed.
at least one CIU-specific hospitalization and 1.9% at least one CIU-specific In this patient, the rash was present prior to the start of antibiotic therapy, thus
ED visit. Costs associated with CIU-based claims increased with age and were her underlying autoimmune disease of lupus most likely was the cause of TEN.
higher in women than in men; otherwise few consistent trends in HCRU
emerged. Conclusions: Despite being otherwise relatively healthy, CIU patients
had frequent HCRU, the majority of which were outpatient visits. CIU-specific
HCRU was small compared with the total use, which also primarily comprised
office visits. This indicates that CIU patients often see physicians for reasons
not directly related to their urticaria.
P318
TREATMENT OF CHRONIC URTICARIA WITH IMMUNOSU-
PRESSORS: CASE REPORT.
M.E. Arroyo-Cruz, A.A. Velasco-Medina, S. Gonzalez-Flores,
J.C. Fernandez-Cordova*, D.A. Cariño-Cartajena, G. Velazquez-Samano,
Mexico City, DF, Mexico.
Introduction: Chronic urticaria (CU) has a prevalence of 30%. It is a con-
dition that does not endanger life but has great impact on the quality of life.
Sometimes, its management is difficult. Case 1: 33 year old female with urticaria
for 1 year, and 2 months ago she has an exacerbation with the presence of ede-
matous-erythematous, pruritic plaques, positive dermatographism and insom-
nia; eyelid edema and arms, she was treated with multiple antihistamines with-
out success, we initiate methotrexate. We achieve a good control of symptoms.
Case 2: 60 years old female, with urticaria for 3 years, which exacerbates in Image 1: Our patient with a diffuse erythematous, exudative, and desquamat-
the past 3 months without responding to the multiple tratments, predominantly ing rash involving more than 70% of her body surface area.
generalized pruritus and rash on both arms and abdomen; we indicate methotrex-
ate with an good clinical response. Discussion: Urticaria management includes
H1 antihistamines as the first option. Recent studies have reported the useful-
ness of methotrexate at a dose of 10-15mg per week, due to its anti-inflam-
P320
IMPROVEMENT OF SLEEP IN PATIENTS WITH CHRONIC IDIO-
matory effect rather than immunosuppression, proving to be effective in chronic PATHIC/SPONTANEOUS URTICARIA (CIU/CSU) TREATED
idiopathic and autoimmune urticaria. Its mechanism of action is unclear, it
WITH OMALIZUMAB: RESULTS OF A RANDOMIZED,
increases adenosine levels, inducing apoptosis of activated CD4 lymphocytes
and decreases neutrophil chemotaxis. It has an estimated response time of 3
DOUBLE-BLIND, PLACEBO-CONTROLLED CLINICAL TRIAL
weeks to 6 months. We report two cases of patients with urticaria with good (GLACIAL).
response to methotrexate. It is a good option for patients with no response to J. Antonova, K. Raimundo*, B. Trzaskoma, P. Solari, T. Omachi, J. Zazzali,
antihistamines and other therapies. South San Francisco, CA.
Introduction: Chronic idiopathic/spontaneous urticaria (CIU/CSU) symp-
toms interfere with patient sleep. Omalizumab has been shown to reduce dis-
ease activity in patients with CIU/CSU. We describe patient-reported data on
sleep from GLACIAL - a large randomized double-blind placebo-controlled
clinical trial. Methods: Subjects were randomized 1:3 and received placebo
A114 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A115
ABSTRACTS: POSTER SESSIONS
(PLB, n=83) or omalizumab 300 mg (OMA300, n=252) every 4 weeks for 6 claimers, and therefore a review of the full ingredient list of any hair dyes is
doses. Sleep was assessed in: Urticaria Patient Daily Diary (UPDD; sleep inter- required prior to use.
ference question; possible range 0-21), Chronic Urticaria Quality of Life Ques-
tionnaire (CU-Q2oL; sleep problems dimension; possible range 0-100), and a
Medical Outcomes Study Sleep Scale (MOS-SS; sleep problem index II [SPI- P322
II]; possible range 0-100). IRB approval and informed consent were obtained USEFULNESS OF A PURINE BIOSYNTHESIS INHIBITOR IN
from all research subjects. Results: On average, at baseline patients reported ATOPIC DERMATITIS.
substantial sleep impairment (Table). Patients in both arms experienced improve- J. Fernandez de Cordova Aguirre*, A. Velasco-Medina, M.E. Arroyo-Cruz,
ment in sleep by week 12 compared with baseline. Comparing week 12 with
S. Gonzalez Flores, D. Cariño-Cartagena, G. Velazquez-Samano, Mexico
baseline, OMA300 arm demonstrated a larger reduction in patient-reported
City, DF, Mexico.
sleep problems than the PLB arm (mean, % reduction): MOS-SS SPI-II: -19.0
(-39%) for OMA300 vs. -13.4 (-28%) for PLB; UPDD sleep interference item: We report a case of a patiente with atopic dermatitis and allergic rhinitis
-9.2 (-77%) for OMA300 vs. -5.0 (-44%) for PLB; CU-Q2oL Sleep Problems: with bad control with standard therapy. We added mycophenolate mofetil with
- 29.4 (-64%) for OMA300 vs. -18.3 (22.2%) for PLB. Conclusion: CIU/CSU good results, assessed by SCORAD scale. Case Presentation: Twenty-eight
patients receiving OMA300 achieved greater reduction in sleep problems than years old male from Veracruz. Since childhood, he has had pruritic erythema-
those in the PLB arm. OMA300 helps reduce sleep impairment in patients with tous scaly lesions scattered across the whole body surface, especially in the
CIU/CSU. flexurar folds of the elbows, popliteal and ankle regions, creases of the neck
and on the face; he also has extremely dry scaly skin. Symptoms have periods
Sleep problems reported by CIU/CSU patients in GLACIAL of remission and exacerbation. He also has hyaline anterior rhinorrhea, nasal
obstruction, nasal pruritus and sneezing. He received moisturizers, topical and
systemic steroids and calcineurin inhibitors without improvement. At initial
assessment he has a SCORAD of 60. He has pruritic erythematous scaly papules
with impetiginization. Studies show 9400 leukocytes, 3500 (38%) neutrophils,
2500 (27%) lymphocytes, 2400 (26%) eosinophils, 90 (1%) basophils. Blood
chemistry, stool test, acute phase reactants (CRP and ESR), IgG, IgM, IgA
and complement were normal. Total serum IgE 7830 IU /ml. Positive nasal
eosinophils. Skin prick test was positive for Fraxinus and Dermatophagoides
farinae. The diagnosis of severe atopic dermatitis and mild intermittent aller-
gic rhinitis is confirmed by clinical and complementary studies. We started
treatment for allergic rhinitis and atopic dermatitis based on intranasal saline
*Larger numbers indicate worse sleep solution, intranasal steroids, oral antihistamines, skin hydration, specific
**Larger negative numbers represent higher degree of improvement immunotherapy and added mycophenolate mofetil 1 g orally daily for 60 days.
BSL = baseline; W12 = week 12; SPI II = Sleep Problem Index II, MOS-SS Clinical response of both allergic rhinitis and skin pathology was successful
= Medical Outcomes Study Sleep Scale; UPDD = Urticaria Patient Daily (SCORAD of 10). Discussion: Atopic dermatitis is a chronic inflammatory skin
Diary, CU-Q2oL = Chronic Urticaria Quality of Life Questionnaire. disease commonly associated with allergic rhinitis. The goals of treatment are
to improve pruritus, papules, erythema, edema, vesicles and prevent impetigo
and lichenification of the skin. Treatment was established with skin hydration,
P321 topical steroids, antihistamines and mycophenolate mofetil 1 g orally for 60
ALLERGIC CONTACT DERMATITIS TO HENNA HAIR DYE. days. We conclude that mycophenolate mofetil is an effective treatment for dif-
Q. Kamili*, Q.L. Nguyen, R. Katta, J. Schmidt, Houston, TX. ficult to control atopic dermatitis.
Introduction: Henna, derived from the plant Lawsonia inermis, has been
used for centuries in India as a hair dye. In recent years, it has experienced
resurgence, as consumers are increasingly drawn to natural products, includ-
P323
PSORIASIFORM SPONGIOTIC DERMATITIS AND AUTOIM-
ing natural hair dyes. Interest in henna has also arisen as it is an exceedingly
rare cause of allergy. Traditional hair dyes, on the other hand, make use of p- MUNE DISEASE.
phenylenediamine (PPDA). This is a common cause of allergic contact der- S. Sran*, M. Taborga, M. Frieri, East Meadow, NY.
matitis, and is found in almost all permanent, semi-permanent, and demi-per- Inflammatory skin diseases manifest via reactive physiological pathways
manent hair dyes in the United States. Because of the extremely low risk of to pathogens. Epidermal keratinocytes play a major role in skin inflammation.
allergy, henna hair dyes are often recommended by physicians as appropriate In acute eczematous dermatitis, activated dermis-infiltrating T cells secrete
alternate hair dyes for those allergic to PPDA. Case: A 50 year old male pre- proinflammatory cytokines that direct epidermal keratinocytes to undergo either
sented to dermatology clinic with a rash of the frontal hairline, eyebrows, and apoptosis or survival. Tumor necrosis factor may promote keratinocyte apop-
beard area. He reported that months earlier he had experienced an allergic reac- tosis and limit the spread of keratinocyte damage, leading to the formation of
tion several days following the use of a drugstore brand of hair dye. His physi- spongiosis, the histopathological hallmark of acute eczematous dermatitis. A
cian had diagnosed allergic contact dermatitis, likely due to p-phenylenedi- 76 year old female presented to the allergy clinic with intermittent lesions in
amine in the hair dye. He was instructed to use only henna hair dyes in the her left lower extremity. The patient had similar lesions in her chest and upper
future. He then purchased a henna hair dye at an ethnic grocery store and applied extremity in the past which resolved spontaneously. Her medical history is
it to his hair, eyebrows, and the beard area. Within three days he developed significant for rheumatoid arthritis, Sjogren’s disease, fibromyalgia, breast can-
erythema, itching and swelling in each of these areas. A review of the ingredi- cer with bilateral mastectomy, gastroesophageal disease, myocardial infarction,
ent list on the henna hair dye package revealed the presence of PPDA. Given neuropathy, depression, anxiety disorder, COPD, dyslipidemia, and hypothy-
his history, he declined patch testing. Conclusion: Henna is often recommended roidism. Physical examination was significant for a 6.4cm discoid ulcer near
as an alternate hair dye in patients with PPDA allergy. For patients reporting the left ankle. RF, CCP, B cell markers, CD19, CD29, CD23, CD10, surface
PPDA allergy, henna has been recommended by physicians and hairstylists, as immunoglobulin, myeloid, platelet and natural killer cell, stem cell, erythroid
well as via multiple outlets on the internet. This case demonstrates that this is cell markers and NBT were within normal limits. Allergen testing by sIgE was
not always a safe strategy. Patients must be informed that some henna hair dyes normal. Immunoglobulin A and M, as well as complement levels were nor-
may contain additional PPDA. This may be due to the fact that henna naturally mal; however immunoglobulin G levels were decreased. Biopsy of the area
produces a reddish tint to the hair. In order to produce a darker color, additional revealed spongiosis, epidermal hyperplasia, and a superficial perivascular and
ingredients may be added in commercially available henna hair dyes; in this interstitial mixed inflammatory cell infiltrate. Sjögren’s syndrome is a systemic
case PPDA. Patients must also be advised that packaging may not include dis- autoimmune disease characterized by dry oral mucosa, dry eyes, and arthritis.
Skin manifestations in Sjögren’s syndrome occur in half of the affected patients.
VOLUME 113, NOVEMBER, 2014 A115
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A116
ABSTRACTS: POSTER SESSIONS
There are reports of atopic dermatitis complicated by Sjögren’s syndrome and
these patients present with persistent itchy dry skin and eczematous lesions.
Perivascular infiltrates of lymphocytes, histiocytes, and occasional eosinophils
can occur in dyshidrotic eczema in rheumatoid arthritis. Drug eruptions may
present in virtually all patterns of cutaneous inflammation including spongi-
otic, lichenoid, and psoriasiform dermatitis. In psoriasiform dermatitis, the
microenvironment of interacting inflammatory cells, antigen presenting cells,
and epithelial cells is disturbed, leading to stereotyped reaction patterns in
inflammatory skin diseases.
P324
THE HAZARDS OF HENNA: AN EVALUATION OF COMMER-
CIALLY AVAILABLE HENNA HAIR DYES.
Q. Kamili*, R. Katta, Q.L. Nguyen, Houston, TX.
Introduction: The chemical p-phenylenediamine (PPDA), found in almost
all permanent hair dyes, is a common cause of allergic contact dermatitis. As
the treatment of PPDA allergy centers on avoidance, the identification of a safe
alternate hair dye is important. Henna is frequently recommended as an alter-
nate, as allergy to henna is exceedingly rare. Derived from the plant Lawsonia
inermis, henna has been used for centuries. This study was undertaken to eval-
uate commercially available henna hair dyes to determine their suitability as
hair dyes in PPDA-allergic patients. Methods: A cross-section of local stores,
including ethnic grocery stores, were surveyed in order to evaluate any henna
hair dyes. Products were included if they contained the word “henna” in the
name or on the package. The ingredient lists of all products were reviewed.
Packaging was reviewed for any other indicators of PPDA presence. Results:
A total of 6 stores were surveyed, and 25 brands of henna hair dyes identified.
Of these, 21 contained the word “henna” in the name of the product, 2 used
alternate words such as “mehandi” and 2 used the word “henna” elsewhere on
the packaging. Eight of the 25 products lacked an ingredient list. Of the remain-
ing 17 dyes, 7 listed PPDA as an ingredient and one contained disperse dyes.
Only 3 of the 7 dyes containing PPDA provided disclaimers; the remainder dis-
played no notification of the presence of PPDA apart from the ingredient list.
Conclusion: This analysis finds that multiple commercially available henna
hair dyes could prove hazardous to patients with PPDA allergy. Almost half of
labeled henna hair dyes in local stores contained PPDA, and the majority con-
tained no notification of the presence of PPDA apart from the ingredient list.
One additional product contained disperse dyes, a potential cross-reactor to
PPDA. Another notable hazard was our finding that almost 1/3 of products con-
P325
A CHALLENGING CASE OF ACUTE GENERALIZED EXAN-
tained no ingredient listing at all. This analysis makes clear that recommend- THEMATOUS PUSTULOSIS.
ing henna hair dyes to patients with PPDA allergy is not sufficient. Many of
the commercially available products would result in allergic reactions if used A. Kim*, San Diego, CA.
by those with PPDA allergy. Patients must therefore be advised to purchase Introduction: Acute generalized exanthematous pustulosis (AGEP) is a rare
only products that contain a full listing of ingredients, and to review the ingre- self-limiting drug eruption that classically presents with sterile pustules on an
dients carefully prior to use. edematous and erythematous base. Diagnosing AGEP can be challenging due
to potentially overlapping clinical features shared with septic shock, chronic
blistering diseases, Stevens Johnson syndrome (SJS) and toxic epidermal necrol-
ysis (TEN). Methods: Clinical case presentation. Results: A 49 year old woman
was admitted to the intensive care unit for multi-organism urosepsis and started
on vancomycin and ertapenem. Due to preexisting drug allergies, antimicro-
bial resistance and ertapenem-induced thrombocytopenia, Allergy/Immunol-
ogy was consulted to facilitate Ceftriaxone desensitization. Prior to desensiti-
zation, the patient had stable hemodynamics and absent history of AGEP,
DRESS, SJS/TEN, and visceral involvement from prior antibiotic administra-
tion. 2 hours following desensitization, the patient became febrile and tachy-
cardic. Clinical deterioration progressed to profound hypotension overnight
requiring initiation of two vasopressors. Infectious Disease evaluated the patient
for urosepsis recurrence, but cultures were unremarkable. 96 hours following
desensitization the patient developed erythema, edema, blistering, and desqua-
mation on the dorsal feet with progression to her neck, perioral region, chest
and upper back. Flaccid bullae and Nikolsky sign were present on the anterior
thighs. Dermatology and Burn teams were emergently consulted and IVIG was
initiated due to concerns of SJS/TEN. Skin biopsy revealed subcorneal neu-
trophilic pustular dermatitis with negative immunofluorescence. Blood analy-
sis did not reveal eosinophilia or liver abnormalities and diagnosis of presumed
AGEP secondary to Vancomycin was made. Conclusion: AGEP is a self-lim-
iting and acute cutaneous eruption that typically presents with fever, pustules
and erythema. Although AGEP generally has a clinical presentation distinct
from SJS/TEN, there can be considerable clinical overlap necessitating care-
A116 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A117
ABSTRACTS: POSTER SESSIONS
ful histopathologic evaluation. As in our patient, AGEP can manifest with skin diet but subsided with antihistamines alone.Conclusion:The urticaria started
desquamation and positive Nikolsky sign, as well as profound disruption in with food supplemental pill which contained shrimp and shell fish proteins
hemodynamics. Given that the prognosis and management of AGEP is notably but undiagnosed gluten enteropathy became obvious during the treatment.
different from SJS/TEN, it is vital that physicians are aware of the diagnosis The urticaria also can be a cutaneous manifestation of gluten-sensitive enteropa-
and its myriad clinical features. thy aside from the food allergy. Therefore, the clinician should be aware of the
role of concomitant underlying gluten-sensitive enteropathy in the treatment
of urticaria.
P326
ACQUIRED ACRODERMATITIS ENTEROPATHICA AND
HYPOTHYROIDISM IN A SEVERELY ATOPIC INFANT. P328
N.N. Shah*, K. Paris, New Orleans, LA. A NOVEL HUMAN-DERIVED PROBIOTIC EXTRACT WITH
FILAGGRIN PROMOTING THERAPEUTIC EFFECT.
Introduction: It is important to evaluate the nutritional deficiencies in
severely atopic infants in order to treat possible non-atopic causes of persist- B. Subhadra*, S. Shastri, M. Henson, J. Krier, N. Monsul, E. Berkes, Sara-
ent dermatitis. We describe a case of acquired acrodermatitis enteropathica and sota, FL.
endocrinopathy in an atopic child. Case Description: A full term 11 month old Introduction: Skin health, especially in atopic dermatitis (AD), relies on
male with history of failure to thrive, GERD, and atopic dermatitis presented an intact skin barrier, a critical component of which is the protein filaggrin. If
to our hospital with fever, dehydration, edema, and dermatitis. At 6 months of filaggrin production is impaired, skin barrier function is also dysfunctional and
age, the patient’s mother elected to feed with rice milk exclusively due to pos- can lead to xerosis, infection, inflammation and allergic sensitization. Com-
itive serum specific IgE testing to various foods. Our initial laboratory evalu- mensals may help support a healthy skin barrier by helping support normal
ation revealed anemia, lymphopenia, hypoalbuminemia, and transaminitis. His filaggrin function. Using a patent-pending bio-extract from a novel probiotic
growth parameters were less than the 3rd percentile, and he had anasarca. Skin human commensal organism, we examined whether the extract could be used
exam revealed denuded, scaly, well demarcated erythematous plaques over the to increase skin filaggrin protein levels. Methods: Using an ex vivo skin explant
diaper area and erythematous crusted lesions around the mouth and eyes. The culture model with normal excised skin from plastic surgery patients, filaggrin
rash appeared 1 month prior to admission, and was not responsive to topical induction by the proprietary bio-extract was tested via filaggrin antibody
steroids. Skin biopsy was consistent with acrodermatitis enteropathica. Inpa- immunohistochemistry, rtPCR and ELISA. Normal skin explants were also
tient evaluation of his malnutrition further revealed markedly elevated thyroid used in a dry skin model induced by SDS treatment, with skin barrier
stimulating hormone, and low serum zinc. An elemental diet and levothyrox- integrity/hydration assessed via skin conductance; bio-extract effect was com-
ine were started, and the patient’s symptoms improved. Appropriate re-evalu- pared against dexamethasone. Results: Filaggrin immunohistochemistry: pro-
ation of his food hypersensitivity was performed and reintroduction of solids prietary bio-extract at 0.05% and 0.1% increased filaggrin staining vs control.
was successful. Discussion: This report highlights the potential morbidity of Filaggrin mRNA: filaggrin mRNA expression did not increase with bio-extract
overly restrictive diets in children with severe atopic dermatitis. Patients with treatment at 0.25% and 0.1% vs control. Filaggrin ELISA: proprietary bio-
atopic dermatitis may have positive sensitization to various foods without his- extracts at 0.05% and 0.1% increased filaggrin protein levels by over 2-fold vs
tory of clinical reaction. Foods used in lieu of infant formula may have vary- control. Skin barrier function: after SDS treatment, 30 minute proprietary bio-
ing levels of carbohydrates, fats, proteins, and minerals. These differences must extract treatment increased skin conductance to or above normal levels; this
be considered when dietary counseling takes place. Conclusion: Acquired acro- improvement lasted for all time points measured and performed at least as
dermatitis enteropathica should be considered in malnourished infants with well as dexamethasone. Conclusion: Patients look for “natural” disease treat-
steroid resistant dermatitis. Minerals are important co-factors in hormone pro- ment options but often fail to find effective choices. Even small increases in
duction and function. Nutritionally appropriate alternatives should be recom- filaggrin have the potential to significantly improve AD clinical symptoms.
mended when discussing food elimination. The 2-fold increase in filaggrin protein levels accompanied by normalization
of skin barrier function in human skin explants induced by a novel human-
probiotic derived bio-extract hold significant clinical promise in the treatment
P327 of skin diseases characterized by low filaggrin expression and skin barrier
OVERLAPPING URTICARIC SKIN MANIFESTATION IN FOOD defects, such as AD.
ALLERGY AND GLUTEN- SENSITIVE ENTEROPATHY.
J. Baik*, A.B. Kim, Los Angeles, CA.
Introduction:Treatment for urticarial rash could be frustrating if the con-
P329
A NOVEL HUMAN-DERIVED PROBIOTIC EXTRACT WITH
ventional treatment fails but the side effect of medication seems to rise. We
report a case of urticaria secondary to food allergy along with concomitant ANTI-METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS
undiagnosed gluten-sensitive enteropathy.Methods: A 23 year old oriental (MRSA) BIOFILM THERAPEUTIC EFFECT.
female presented with 1 week history of the generalized urticaria including E. Berkes, B. Subhadra*, M. Henson, J. Krier, N. Monsul, Sarasota, FL.
face and both palms. There were no GI symptoms at the initial presentation. Introduction: It is increasingly recognized that maintenance of skin health,
She took a chitosan pill which is a product of shrimp and shell fishes as a food particularly in patients with atopic dermatitis (AD), requires homeostasis among
supplement prior to onset of the rash. There was a history of premenstrual the microbes comprising the dermatologic microbiome. Biofilms are the com-
pain which required high doses of advil. She had a frequent indigestion with munal phenotype preferred by most microbes, including pathogens, and form
unknown origin during chidhood. Initially,her urticarial rash responded well on most surfaces. Commensals may help support a healthy skin barrier by
to IM steroid with IM Benadryl, followed by oral prednisone, hydroxyzine. But inhibiting pathogenic biofilms such as MRSA. Using a patent-pending bio-
few days later, the patient started to have severe intermittent colicky abdomi- extract from a novel probiotic human commensal organism, we defined MRSA
nal pain with recurrent urticaria in spite of the treatment.The patient was seen anti-biofilm activities of potential clinical utility in the prevention and treat-
at ER, started on hydrocodone-acetaminophen for pain without relief.Oral ment of MRSA biofilms. Methods: Using a 96-well biofilm microplate assay,
steroid was discontinued after the onset of the abdominal pain and changed to proprietary bio-extracts were tested against clinical MRSA isolates for 2 anti-
IM steroid which controlled urticaria but abdominal pain persisted. The patient biofilm activities: anti-biofilm adhesion and detachment of MRSA biofilm.
was evaluated by two different gastroenterologists. The gastroendoscopy find- Results were compared against vancomycin and meropenem. Results: Anti-
ing was negative. The blood test was positive for t- transglutaminase IgA: 5u/ml adhesion: The bio-extract was 2-3x more effective than antibiotic controls, with
(0-3).The percutaneous skin test revealed multiple hypersensitivities to clam, 35% anti-adhesion at 0.01 mg/ml, 50% at 0.05 mg/ml, 58% at 0.1 mg/ml, 85%
shrimp, oyster, barley, celery, coconut, sweet potato, salmon, squash, straw- at 0.5 mg/ml and 90% at 1 mg/ml when compared against untreated growth
berry, string bean, tomato, dust mites and chinese elm tree pollen but negative control. Biofilm detachment: The bio-extract was up to 10 times more effec-
for wheat. Result:The gluten-free diet resulted in prompt remission of the recur- tive than antibiotic controls: 0.05 mg/ml detached 50% of MRSA biofilm; van-
rent colicky abdominal pain. The urticaria was under control with antihista- comycin and meropenem both detached only approximately 5%. Unlike the
mine along with elimination diets, allowing complete discontinuation of sys- anti-adhesive assay, there was no apparent dose-dependence, as percent detach-
temic steroids. Urticaria came back twice over 2 months in spite of gluten-free ment declined as bio-extract concentration increased. Lack of dose dependence
VOLUME 113, NOVEMBER, 2014 A117
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A118
ABSTRACTS: POSTER SESSIONS
may reflect non-metabolic mechanisms of action and/or brief application time.
Conclusion: We have discovered a novel human-derived probiotic extract with
P331
ELEPHANTIASIS NOSTRAS OF THE LIP.
anti-MRSA biofilm therapeutic effect. Skin of patients with AD is diffusely
colonized by Staphylococcus aureus and MRSA. Increased microbial burden K. Dass*, A. Ditto, Chicago, IL.
is associated with acute exacerbations, and chronically, these microbes are asso- Elephantiasis nostras (EN) occurs secondary to a recurrent lymphangitis
ciated with inflammation, decreased skin immune defense and a weakened skin often introduced by trauma. Rarely, EN can affect the lips, with only four
barrier. MRSA biofilms are a key factor in the persistence of these microbes reported cases in literature. A 27 year old female presented to our allergy-
in AD patients. This human probiotic-derived bio-extract with the dual anti- immunology outpatient office with complaints of painful edema, erythema,
biofilm activities of inhibition of biofilm adhesion as well as detachment of peeling, and scabbing of her upper and lower lips. Her symptoms began 6 months
already formed pathogenic biofilm, could synergistically both treat and pre- prior to her visit. There was no history of drug allergy or prior history of
vent MRSA biofilms in chronic skin diseases, such as AD. angioedema. She denied any constitutional symptoms. Her symptoms were
worse in the morning or when any food touched her lips. She denied any globus,
tongue swelling, dyspnea. She denied any new medications or exposure to any
P330 new detergents or bathing products. Examination was notable for erythema-
DELAYED DIAGNOSIS OF ERYTHROPOIETIC PROTOPOR- tous, edematous, painful lips with fissures at the vermillion border. There was
PHYRIA: A 36 YEAR OLD HISPANIC FEMALE WITH SUN- no cervical or post-auricular lymphadenopathy. She was concerned about her
INDUCED ANGIOEDEMA. appearance and lack of resolution of her symptoms. Elephantiasis nostras was
M. Rodríguez-Roa*1, S. Nazario2, 1. San Juan, Puerto Rico; 2. Hato Rey, considered as a diagnosis. The patient was treated with five days of prednisone
and twenty-one days of amoxicillin clavulanate with complete resolution of her
Puerto Rico.
symptoms. Unfortunately, she was lost to follow up. With recurrence of symp-
Rationale: Angioedema is a self-limited, localized swelling of the skin or toms, the patient followed with a dermatologist. She was treated for contact
mucosal tissues resulting from the extravasation of fluid into the interstitium. dermatitis despite avoiding all makeup or other skin products in the affected
Although angioedema is a common condition in allergy practices, solar induced area. After testing positive for a nickel allergy, she also followed a low nickel
angioedema has a narrower differential diagnosis, including phototoxic drug diet. Despite her efforts, her symptoms persisted. . The patient returned to the
reactions, solar urticaria, contact dermatitis, autoimmune inflammatory disor- allergy and immunology outpatient office, where she was successfully treated
ders and in rare cases metabolic disorders, such as cutaneous porphyrias. We with a second course of 5 days of prednisone and 21 days of amoxicillin-clavu-
present a case of erythropoietic protoporphyria (EPP) presenting as sun- induced lanate. Elephantiasis nostras can lead to permanent swelling, hypertrophic fibro-
angioedema in a 36 y/o Hispanic female. Methods: Case Report. Results: A sis, and facial disfigurement with repeated attacks. Suspicion of EN as a clin-
36 y/o female G1P1A0 presents to the clinic with burning, itching and swelling ical entity may arise with unrelenting edema. Other disorders that should be
within minutes upon sun-exposed areas since her childhood. These episodes considered include angioedema, contact dermatitis, erysipelas, granulomatous
last several days, do not leave residual hyperpigmentation, but interfere sig- cheilitis, Melkersson’s syndrome, superior vena cava syndrome, and sclero-
nificantly in her quality of life. Neither antihistamines nor sunscreens have derma. Treatment focuses on long-term antibiotic administration with plastic
been helpful to control her symptoms. Denies associated blisters, hives, hyper- surgery occasionally required. This case illustrates the importance of main-
trichosis, anemia, exacerbation or provocation by any other physical stimuli, taining elephantiasis nostras as a differential diagnosis in patients with chronic
anemia, concomitant liver disease, family history of sun induced angioedema, edematous lips.
nor NSAIDs use. Also denies gastrointestinal or respiratory complains or any
comorbid conditions. Her family emigrated from Cuba and there is no history
of intermarriage. Her only medication is vitamin D replacement. Past medical
history was remarkable for chemical hepatitis after surgery for an ovarian cyst
at 12 y/o and cholecystectomy for gallstones when she was 27 y/o. On physi-
cal exam a pale short size woman was noted without any visible eczema, hives,
blisters or organomegaly. Initial laboratories were significant for mildly ele-
vated liver function tests as well as elevated coproporphyrin and heptacarboxyl
in urine. Anemia was not present. A preliminary diagnosis of EPP was made
awaiting confirmatory porphyrin and protoporphyrin levels in RBC, which will
be available for the presentation. Conclusion: Although EPP is a rare cause of
sun- induced angioedema, it is important for allergists to consider it in the dif-
ferential diagnosis in order to diagnose at an early age and prevent life-threat-
ening complications such as hepatitis and hepatic failure requiring liver trans-
plant, and to initiate appropriate sun avoidance recommendations.
A118 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A119
SPEAKER DISCLOSURES
Disclosures
Oral and Poster Abstract Presenters
American College of Allergy, Asthma & Immunology
Annual Scientific Meeting
Continuing Medical Education
November 6-10, 2014
Atlanta, Georgia
Disclosure Policy and Disclosures
As required by the Accreditation Council for Continuing Medical Education (ACCME) and in accordance with the American
College of Allergy, Asthma and Immunology (ACAAI) policy, all educational planners, presenters, instructors, moderators,
authors, reviewers, and other individuals in a position to control or influence the content of an activity must disclose all rele-
vant financial relationships with any commercial interest that have occurred within the past 12 months. All identified conflicts
of interest must be resolved and the educational content thoroughly vetted for fair balance, scientific objectivity, and appropri-
ateness of patient care recommendations. It is required that disclosure be provided to the learners prior to the start of the activ-
ity. Individuals with no relevant financial relationships must also inform the learners that no relevant financial relationships
exist. Learners must also be informed when off-label, experimental/investigational uses of drugs or devices are discussed in an
educational activity or included in related materials. Disclosure in no way implies that the information presented is biased or of
lesser quality. It is incumbent upon course participants to be aware of these factors in interpreting the program contents and
evaluating recommendations. Moreover, expressed views do not necessarily reflect the opinions of the ACAAI. (Please note
that posters were not certified for credit.)
Abiteboul, K. – P265 Bajpai, S. – P48 Bernstein, D. – 14, P266
Employee: Stallergenes Consultant/Advisory Board: Teva Consultant/Advisory Board:
Circassia, Merck; Research Grant:
Adelman, B. – P289 Baker, J. – 8 Greer, Merck, Stallergenes
Employee: Dyax Research Grant: Amgen, Amphastar,
Array, AstraZeneca, Asubio, Celgene, Bernstein, J. – P225, P300
Allen, N. – 23 Circassia, CSL Behring, Dyax, Consultant/Advisory Board: CSL
Consultant/Advisory Board: OSIA Galderma, Genentech, Behring
Medical GlaxoSmithKline, Kythera, Maruho,
Meda, Merck, Mylan, Novartis, Pearl Biedenkapp, J. – P289
Amar, N. – P305, 14 Therapeutics, Pfizer, Pharming, Employee: Dyax
Research Grant: AstraZeneca, Pulmagen, Sanofi, Merck, Shire,
GlaxoSmithKline, Merck, Teva; Data Teva, Tigercat Bielory, L. – P40, P306
Monitoring Committee: Merck Research Grant: EPA
Banerji, D. – P284
Amin, A. – P287 Employee: Novartis Bjermer, L. – 61
Employee: Novartis Consultant/Advisory Board:
Barbir, A. – 6 AstraZeneca, Airsonette, Aerocrine,
Amistani, Y. – P264 Research Grant: Mylan Specialty ALK-Abello, Almirall, Boerhringer
Employee: Stallergenes Ingelheim, Chiesi, GlaxoSmithKline,
Bensch, G. – P57 Meda, Merck, Mundipharma,
Antonova, E. – 57, P80, P317 Research Grant: Meda Nigaard, Novartis, Orion, Sandoz,
Employee: Genentech Teva; Speaker: AstraZeneca,
Berger, W. – P301, P305 Airsonette, Aerocrine, ALK-Abello,
Antonova, J. – P46, P320 Consultant/Advisory Board, Research Almirall, Boehringer Ingelheim,
Employee: Genentech Grant: Meda Chiesi, GlaxoSmithKline, Meda,
Merck, Mundipharma, Nigaard,
Aquino, M. – 39 Berkes, E. – P328, P329 Novartis, Orion, Teva
Research Grant: Genentech Co-founder: Quorum Innovations
Blessing-Moore, J. – P300
Ashton, V. – P66 Berman, G. – P259 Consultant/Advisory Board, Research
Employee: Research in Real Life Research Grant: AstraZeneca, Grant: Meda
Cerecor, Circassia, Forest, Genentech,
Aygören-Pürsün, E. – P225 GlaxoSmithKline, Janssen, Mylan, Boccon-Gibod, I. – P225
Consultant/Advisory Board: CSL Novartis, Perrigo, Roche, Sunovion, Consultant/Advisory Board: CSL
Behring Teva Behring
VOLUME 113, NOVEMBER, 2014 A119
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A120
SPEAKER DISCLOSURES
Borish, L. – P182 Carr, W. – P295 Davis-Lorton, M. – 39
Consultant/Advisory Board : Allakos, Consultant/Advisory Board and Research Grant: Novartis
Genentech, Novartis, Pluristem; Speaker: Alcon, Allergan,
Research Grant/Clinical Trials: AstraZeneca, Boehringer Ingelheim, Dees, J. – 23
Allakos, Dupont, Genentech, Knopp, Meda, Mylan, Teva Consultant/Advisory Board: OSIA
National Institutes of Health (NIH) Medical
Novartis Casale, T. – P295
Consultant/Advisory Board and Dennerlein, J. – 6
Bork, K. – P225 Research Grant: Boehringer Research Grant: Mylan Specialty
Consultant/Advisory Board: CSL Ingelheim
Behring DePietro, M. – P50, P51
Casciano, J. – P48 Employee, Stocks: AstraZeneca
Bouillet, L. – P225 Consultant/Advisory Board: Teva
Consultant/Advisory Board: CSL Devillier, P. – P267
Behring Chang, E. – P80, P317 Consultant/Advisory Board,
Employee: Partnership for Health Honorarium, Research Grant: ALK,
Bour, L. – P295 Analytic Research AstraZeneca, Chiesi,
Employee: Boehringer Ingelheim GlaxoSmithKline, Merck, Menarini,
Chen, H. – P45 Pierre Fabre, Sanofi, Stallergenes
Broder, M. – P80, P317 Employee, Stocks: Genentech
Employee: Partnership for Health Dotiwala, Z. – P48
Analytic Research Chipps, B. – P50, P51 Consultant/Advisory Board: eMAX
Consultant/Advisory Board: Health
Buatti Small, M. – P66 AstraZeneca, Genentech,
Employee: Teva GlaxoSmithKline, Meda, Merck, Du, Q. – P296, P297
Novartis, Sunovion; Speaker: Employee: Johnson & Johnson
Burden, A. – P66 AstraZeneca, Bausch & Lomb, Consumer Products
Employee: Research in Real Life Genentech, GlaxoSmithKline, Merck,
Novartis, Sunovion Duff, C. – P218
Busse, P. – P162, P199 Consultant/Advisory Board: Baxter,
Consultant/Advisory Board: Dyax, Chyung, Y. – P289 CSL Behring, Immune Deficiency
Shire; Grant: CSL Behring, Dyax, Employee: Dyax Foundation
Shire
Cicardi, M. – P225, P291 Duncan, E. – P27, P28
Bygum, A. – P225 Consultant/Advisory Board: CSL Employee: Greer
Consultant/Advisory Board: CSL Behring
Behring Durham, S. – P257
Ciesielska, M. – 61 Consultant/Advisory Board: ALK-
Caballero, T. – P225 Employee: Teva Abello, Circassia, Merck,
Consultant/Advisory Board: CSL Stallergenes: Research Grant: ALK-
Behring Corren, J. – P62 Abello, Merck, Stallergenes
Research Grant: Meda
Calderon, M. – 15 Ebeling, M. – P261
Consultant/Advisory Board and Coyne, T. – P27, P28 Statistical Analysis: United Allergy
Speaker: ALK-Abello, Employee: Greer Services
Allergopharma, Hal Allergy,
Stallergenes Craig, T. – P225 Eisner, M. – P45
Consultant/Advisory Board: CSL Employee, Stocks: Genentech
Campbell, A. – P285 Behring
Employee and Stocks: AbbVie Engel, M. – P288, P295
Creticos, P. – 14 Employee: Boehringer Ingelheim
Campbell, J. – P66 Consultant/Advisory Board and
Consultant/Advisory Board: Teva Research Grant: Circassia, Greer, Engl, W. – P227
Merck Employee : Baxter
Cancian, M. – P225
Consultant/Advisory Board: CSL Cuff, C. – P285 Farkas, H. – 8, P225
Behring Employee, Stocks: AbbVie Consultant/Advisory Board: CSL
Behring, Shire; Travel Grants: CSL
D'Addio, A. – P299 Behring, Shire, Swedish Orphan
Employee: Meda Biovitrum
A120 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A121
SPEAKER DISCLOSURES
Faucette, R. – P289 Gupta, S. – P227 Kaplan, A. – 57
Employee: Dyax Consultant/Advisory Board and Consultant/Advisory Board:
Speaker: Baxter Genentech, Novartis: Research Grant:
Fernandez, J. – P121, P189 CSL Behring, Dyax, Shire; Speaker:
Speaker: Baxter Hadari, Y. – P82 Shire
Stocks: Kolltan
Ferreira, M. – P225 Karafilidis, J. – P57, P62
Consultant/Advisory Board: CSL Hall, D. – P27, P28 Employee: Meda
Behring Employee: Greer
Kaur, A. – 14, 15, P257, P259
Fonacier, L. – 39 Hampel, F. – P302 Employee: Merck
Research Grant: Genentech Research Grant: Meda
Kenniston, J. – P289
Ford, L. – P288 Harrow, B. – P58 Employee: Dyax
Research Grant: Boehringer Employee: Meda
Ingelheim Kerstjens, H. – P288, P294, P295
Haselkorn, T. – P45 Consultant/Advisory Board: Almirall,
Franklin, K. – P296, P297 Consultant/Advisory Board: Boehringer Ingelheim, Novartis,
Consultant/Advisory Board: McNeil Genentech Pfizer; Research Grant: Boehringer
Ingelheim, Chiesi, GlaxoSmithKline,
Furcha, R. – P287 Hendershot, R. – 23 Pfizer
Employee: Novartis Consultant/Advisory Board: OSIA
Medical; Speaker: AstraZeneca, Khalil, S. – 57
Garner, L. – P261 Merck Employee: Novartis
Consultant/Advisory Board: United
Allergy Services Hendrickson, B. – P285 Kobrynski, L. – P227
Employee and Stocks: AbbVie Consultant/Advisory Board: Baxter,
Gawchik, S. – P302 CSL Behring
Consultant/Advisory Board, Research Henson, M. – P328, P329
Grant: Meda Clinical Research Advisor: Quorum Koch, G. – P257
Innovations Principal Investigator: Merck
Gedrich, R. – P82
Employee: Kolltan Horak, F. – P266 Krier, J. – P328, P329
Employee: Vienna challenge chamber Microbiologist: Quorum Innovations
Gever, L. – P299, P300, P301
Employee: Meda Hulsey, T. – P261 Krishnan, J. – P48
Statistical Analysis: United Allergy Consultant/Advisory Board: eMAX
Gillespie, M. – P55 Services Health
Employee: Teva
Iarrobino, R. – P289 Kulich, K. – P284
Golden, D. – P265 Employee: Dyax Employee: Novartis
Consultant/Advisory Board:
Stallergenes; Speaker: Genentech; Iribarren, C. – P45 LaForce, C. – P73
Research Grant: Genentech, Merck, Consultant/Advisory Board: Consultant/Advisory Board: Novartis
Siemens Diagnostics Genentech
Lang, D. – 17
Gopalan, G. – P66 Iverson, H. – P56, P73, P74, P76 Consultant/Advisory Board: Hycor,
Employee: Teva Employee: Teva Merck, Quest: Honorarium: Merck,
Research Grant: Genentech, Novartis
Grant, J. – P227 Jain, N. – P158
Consultant: Baxter Consultant/Advisory Board: Lanier, B. – P259
Aerocrine; Speaker, Honorarium: Research Grant: Genentech, Merck;
Grier, T. – P27, P28 Abbott, AstraZeneca, Speaker: Novartis
Employee: Greer GlaxoSmithKline, Novartis
LaVallee, T. – P82
Guilarte, M. – P225 Janelli, M. – 6 Employee: Kolltan
Consultant Advisory Board: CSL Research Grant: Mylan Specialty
Behring Lawrence, M. – P182
Consultant/Advisory Board: Regado
VOLUME 113, NOVEMBER, 2014 A121
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A122
SPEAKER DISCLOSURES
Leibl, H. – P227 Melamed, I. – P227 Ostrom, N. – P56
Employee: Baxter Consultant/Advisory Board: Baxter, Consultant/Advisory Board: Allergan,
BPL, ADMA; Investigator: CSL, AstraZeneca, Meda, Merck, Novartis,
Lemell, P. – P266 ADMA, BPL, Baxter, Octapharma Teva; Speaker, Honorarium:
Employee: Vienna Challenge AstraZeneca, GlaxoSmithKline,
Chamber Meltzer, E. – P299 Meda, Merck, Novartis, Sunovion,
Consultant/Advisory Board, Research Teva, Sunovion; Research Grant:
Lemiere, C. – 61 Grant: Meda Actavis, Alcon, Amgen, AstraZeneca,
Consultant/Advisory Board: Apotex, Boehringer Ingelheim, Cytos,
Aerocrine, AstraZeneca, Meltzer, S. – P300 Genentech, GlaxoSmithKline, HRA,
GlaxoSmithKline; Speaker: Research Grant: Meda Johnson & Johnson, MedImmune,
AstraZeneca, Merck; Research Grant: Merck, Mylan, Nestle, Novartis,
Aerocrine, GlaxoSmithKline Miller, D. – P45, P73, P74, P76 Proctor & Gamble, Rigel, Sunovion,
Employee: ICON Clinical Research; Teva
Li, C. – P48 Research Grant: Genentech
Consultant/Advisory Board: eMAX Paolozzi, L. – P264
Health Miller, R. – P285 Employee: Stallergenes
Employee and Stock: AbbVie
Li, H. – 8 Patel, M. – P296, P297
Consultant/Advisory Board: CSL Mire, B. – P33 Employee: McNeil Consumer
Behring, Dyax, Salix, Shire; Speaker: Employee: ALK Healthcare
CSL Behring, Dyax, Shire; Research
Grant: Shire Moldovan, D. – P291 Pearlman, D. – P56
Research Grant: CSL Behring, Shire; Research Grant: AstraZeneca,
Li, J. – P305 CSL Behring, Pharming, Shire Genentech, Novartis, Optinose,
Employee: Teva Sanofi, Teva
Monsul, N. – P328, P329
Li, Z. – 14, P257, P266 Co-Founder: Quorum Innovations Plunkett, G. – P33
Employee: Merck Employee: ALK
Moroni-Zentgraf, P. – P288, P295
Lin, M. – 6 Employee of Boehringer Ingelheim Porebski, G. – 8
Research Grant: Mylan Specialty Speaker: CSL Behring, Swedish
Murphy, K. – P294 Orphan Biovitrum; Research
Longhurst, H. – P225 Consultant/Advisory Board: Investigator: CSL Behring
Consultant/Advisory Board: CSL AstraZeneca, Genentech, Greer,
Behring Meda, Merck, Novartis, Teva; Price, D. – P58, P66
Speaker, Honorarium: AstraZeneca, Consultant/Advisory Board:
Lubeski, C. – P82 Genentech, Merck, Mylan, Novartis, Aerocrine, Almirall, Amgen,
Employee: Kolltan Teva AstraZeneca, Boehringer Ingelheim,
Chiesi, GlaxoSmithKline, Meda,
Magerl, M. – P225 Naples, A. – P261 Mundipharma, Napp, Novartis,
Consultant/Advisory Board: CSL Employee: United Allergy Services Pfizer, Teva; Speaker: Almirall,
Behring AstraZeneca, Boehringer Ingelheim,
Nelson, H. – 15, P266 Chiesi, Cipla, GlaxoSmithKline,
Maloney, J. – 14, 15, P257, P259, Consultant/Advisory Board: Kyorin, Meda, Mundipharma,
P266 Circassia, Merck: Research Grant: Novartis, Pfizer, Skyepharma, Takeda,
Employee: Merck Circassia Teva; Honorarium: Aerocrine,
Boehringer Ingelheim, Mundipharma,
Mandel, E. – P82 Nolte, H. – 14, 15, P257, P259, P266 Napp, Novartis; Research Grant Peer
Employee: Kolltan Employee: Merck Reviewer: Aerocrine, AstraZeneca,
Boehringer Ingelheim, British Lung
Martinez-Saguer, I. – P225 Nordenfelt, P. – P225 Foundation, Chiesi, Eli Lilly,
Consultant/Advisory Board: CSL Consultant/Advisory Board: CSL GlaxoSmithKline, Meda,
Behring Behring Mundipharma, Novartis, Orion,
Pfizer, Respiratory Effectiveness
Meier, E. – P293 O'Brien, C. – 61, P73, P74 Group, Takeda, Teva, UK National
Research Grant: Alcon Labs Employee: Teva Health Service, Zentiva, Medical
Research Council, HTA; Stock
Omachi, T. – 57, P320, P45 Ownership: AKL, Research in Real
Employee: Genentech Life, Optimum Patient Care
A122 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A123
SPEAKER DISCLOSURES
Raimundo, K. – 57, P46, P317, P320 Sexton, D. – P289 Tashkin, D. – P51, P50
Employee, Stocks: Genentech Employee: Dyax Consultant/Advisory Board:
AstraZeneca, Pearl, Sunovion,
Ratner, P. – P301 Shah, M. – P45 Theravance; Research Grant:
Consultant/Advisory Board and Employee: ICON Clinical Research GlaxoSmithKline, Pearl, Sunovion;
Research Grant: Meda Speaker: AstraZeneca, Boehringer
Shastri, S. – P328 Ingelheim, Forest
Reinero, C. – P82 Laboratory Investigator: Quorum
Research Grant: Kolltan Innovations Taveras, H. – P56, P73, P74, P76
Employee: Teva
Relan, A. – 8, P291 Sigmund, R. – P288
Employee, Stocks: Pharming Employee: Boehringer Ingelheim TenHoor, C. – P289
Employee: Dyax
Reshef, A. – 8, P225 Skoner, D. – P259
Consultant/Advisory Board: CSL Consultant/Advisory Board, Research Tian, X. – P296, P297
Behring, Shire; Research Grant, Grant: Greer, Merck; Speaker: Merck Employee: Johnson & Johnson
Speaker, Honorarium: CSL Behring,
Pharming, Shire, Teva Small, C. – P305 Tiplady, B. – P284
Employee: Teva Employee: ERT
Reynolds, R. – 23
Consultant/Advisory Board: OSIA Solari, P. – P46, P80, P320 Tripp, C. – P285
Medical Employee, Stocks: Genentech Employee, Stocks: AbbVie
Rhodes, B. – 23 Song, S. – P55 Trudo, F. – P50, P51
Consultant/Advisory Board: OSIA Employee: Teva Employee, Stocks: AstraZeneca
Medical
Soteres, D. – P301 Trzaskoma, B. – 57, P46, P320
Riedl, M. – P291 Research Grant: Meda Employee: Genentech
Consultant/Advisory Board:
BioCryst, CSL Behring, Dyax, Isis, Stanaland, B. – P302 Urdaneta, E. – P296, P297
Salix, Shire; Research Grant: Speaker: Meda Employee: McNeil Consumer
BioCryst, CSL Behring, Dyax, Salix, Healthcare
Shire: Speaker: CSL Behring, Dyax, Stein, M. – P227
Shire Consultant/Advisory Board, Speaker: Vandewalker, M. – P288
Baxter, CSL Behring; Research Grant: Boehringer
Rigazio, A. – P66 Research Investigator: ADMA, Ingelheim
Employee: Research in Real Life Baxter, BPL, CSL Behring, Green
Cross, Kedrion von Ziegenweidt, J. – P66
Roux, M. – P267 Employee: Research in Real Life
Employee: Stallergenes Steinfeld, J. – P55
Employee: Teva Wahn, U. – P264
Ruiz, N. – P57, P62, P299, P300, Consultant/Advisory Board, Speaker:
P301, P302 Stobiecki, M. – P225, P291 Allergopharma, Danone, Merck,
Employee: Meda Consultant/Advisory Board: CSL Novartis; Speaker: GlaxoSmithKline,
Behring Nestle, Nutricia, Stallergenes, Thermo
Schaffer, F. – P261 Fisher Scientific
Employee/Chief Medical Officer: Subhadra, B. – P328, P329
United Allergy Services Employee/Research Director: Quorum Wasserman, R. – P227
Innovations Consultant/Advisory Board: ADMA,
Schiff, R. – P227 Baxter, CSL Behring, BPL, Korean
Employee: Baxter Sun, G. – P80, P317 Green Cross, Kedrion, Therapure;
Employee: Partnership for Health Speaker: Baxter, CSL Behring;
Schwartz, S. – P228 Analytic Research Investigator : ADMA, Baxter, CSL
Stocks: Merck, Pfizer Behring, BPL, Kedrion
Tantry, S. – P305
Seare, J. – 5 Employee, Stocks: Teva Wayne, D. – P76
Research Grant: Mylan Specialty Employee: Teva
Settipane, R. – P302 Weber, R. – 14
Consultant/Advisory Board and Speaker: Merck
Research Grant: Meda
VOLUME 113, NOVEMBER, 2014 A123
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A124
SPEAKER DISCLOSURES
Wedner, H. – P291 Wu, M. – P296, P297 Zazzali, J. – 57, P46, P80, P320
Consultant/Advisory Board: Employee: Johnson & Johnson Employee, Stocks: Genentech
BioMarin, CSL Behring, Genentech;
Speaker: CSL Behring, Dyax, Yang, W. – P291, P267 Zeldin, R. – P264, P265, P267
Genentech, GlaxoSmithKline, Merck, Consultant/Advisory Board: CSL Employee: Stallergenes
Mylan, Novartis, Shire, Teva; Behring, Shire; Research Grant: CSL
Research Grant: CSL Behring, Dyax, Behring; Zieglmayer, P. – P266
Genentech, Mankind, Merck, Employee: Vienna Challenge
Pharming, Shire, Teva; Advisory Yel, L. – P227 Chamber
Committee: Baxter, Genentech, Employee: Baxter
MedImmune, Shire Zieglmayer, R. – P266
Zangrilli, J. – 61 Employee: Vienna Challenge
Wolf, R. – 6 Employee: Teva Chamber
Employee: Mylan Specialty
Zanichelli, A. – 8 Zuraw, B. – P225
Wu, C. – P285 Consultant/Advisory Board: Shire; Consultant/Advisory Board: CSL
Employee, Stock: AbbVie Speaker: CSL Behring, Shire, Behring
Swedish Orphan Biovitrum
The following have no relevant financial relationships with commercial interests to disclose:
Abou Baker, N. – 21 Allenbrand, R. – 52 Arroyo-Cruz, M.E. – P7, P53, P130,
P178, P318, P322
Abraham, J.T. – P189 Alpan , O. – P92
Asawa, A. – P143
Abramowitz Saadia, T. – 34 Altrich, M. – P6
Assa'ad, A. – P195
Acantilado, C. – P14 Ambrus, J.L. – P84
Atkinson, P. – P242
Achar , K. – 25, P222 Amin, R. – P4
Avila, P. – P168
Acharya, S. – P188 An, W. – 24
Bachove , I.R. – P204
Adkins, C. – P1, P3 Anand, R. – P84
Baghian, S. – P134
Agarwal, P. – 22 Anderson, J.J. – 9
Bahna, S.L. – P8, P215
Agrawal, S. – P85 Anderson, J.T. – P3, P207
Baik, J. – P327
Akande, T. – P134 Anderson, L. – P167
Baldwin, J. – P111
Akbar, S. – P273 Andreae, D.A. – P213
Banks, T. – P22, P105
Akl , E. – P190 Andujar-DeLaCruz, J. – P166
Bansal, V. – 7
Al Gazlan, S. – P4 Angeles-Garay, U. – 60, P79
Bantz, S. – P42
Al Jiffri, O. H. – P43 Anghel, S. – 33
Bardelas, J.A. – 15
Al Otaibi , T. – P4 Ansary, F.F. – P163
Barnes, C.S. – 11, 52
Aleem, S. – 63 Anthony, K. – P156
Barth, R. – P31
Alfonzo, M. – P87 Antonevich, N. – P90
Bauer, C. – 24
Alhashim, S. – P4 Anyane-Yeboa, K. – P201
Bayer, D. – P283
Ali, A. – P96 Aquino, M. – 27, 39, P152, P196
Beattie, E. – P48
Al-Kawas, F.H. – 41 Arakali, S. – P197
Becerril-Angeles, M. – 60, P70, P79
Alkhatib, F. – P219 Arias Cruz, A. – P16
Bellanti, J.A. – 41, P260
Allen, C. – P3 Arora, R. – P29
Bellucci, F. – 2
A124 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A125
SPEAKER DISCLOSURES
Beloglazov, V. – P77, P234 Buelow, B. J. – P131 Chefitz, D. – P166
Bensch, G. – P288, P294 Buenfil Lopez, J.A. – P16 Chekan, V. – P90
Berger, W.E. – P294 Bukhari, A. – P92 Chen, M. – P64
Bergerson, J. – P200 Bundy, V. – 40 Chiarella, S.E. – P23
Bernstein, D. – P38, P41 Burch, T.C. – 53 Chokshi, N. – P283
Bernstein, J. A. – 10, P184 Burke-Mcgovern , S. – P198 Chong, M.H. – 39, P196
Bewtra, A. – P47 Bush, J.S. – 58 Chotikanatis, K. – P31, P93, P309
Bhatti, H. – P220 Buterleviciute, N. – P18 Chowdhary, A. – 22
Biagini Myers, J.M. – P38 Buyantseva, L. – P221 Christine, K. – P157
Bielory, B.P. – 51 Byrd, R. – P174 Chumpitazi, B.P. – P212
Bielory, L. – 33, 51, P40, P281, P290 CaJacob, A. – P3 Ciaccio, C. – 42, 52
Bilaver, L. – P252 Cakir, E. – P52, P127 Cianferoni, A. – P255
Bird, J. A. – P115 Calais, C.J. – 38 Cicero , C. – P223
Bisyuk, Y. – P77 Calderon, L.I. – P223 Ciesielska, M. – 61
Bjermer, L. – 61 Caldwell, J.W. – P25 Ciminera, P. – P123
Blaziene, A. – P18 Camacho Ordonez, N. – P251 Clay, K.G. – P63
Bleecker, E.R. – P66 Camacho, J.M. – P230 Cohn, L.A. – P82
Blumenstock, J. – P252 Capitle, E. – P197, P319 Collins, C. – P24
Bodner, S. – P273 Capriati, T. – 2 Columbo, M. – P298
Bolgar, B. – P209 Carino Cartagena, D.A. – P7, P53, Commins, S.P. – 43
P130, P178, P318, P322
Bollard, C.M. – P212 Conboy, E. – 36
Carlton, B.G. – 20, P268
Bonagura, V.R. – 29, P112, P159 Conner, K. – P153
Carr, T.F. – P165
Bonds, R. – P143 Cook, K. – P243
Caruthers, C. – P192
Borja-Aburto, V.H. – 60, P70 Corrente, S. – P248
Casillas, A. – P262
Bornstein, L. – P185, P237 Corrigan, C.J. – P66
Casper, J. – P224
Bose, S. – P181 Coscia, G. – P201
Casper, R. – P122
Bozoghlanian, V. – P314 Craig, T.J. – P99, P163, P221, P292
Castillo Narvaez, G. – P311, P313
Brady, S.P. – P146 Craig, V. – P166
Cavanaugh, P. – 5
Braunstein, M.Z. – P39 Crandall, L. – 24
Cavero Chavez, V. – P228
Brensilver, J. – 33 Crans Yoon, A. – 19
Celestin, J. – P206
Breslin, M. – P232 Crawford, W. – 19
Cervantes, M. – P263, P270
Brooks, J. – P132 Crisp, H.C. – 13
Challa, S. – 33
Brown, K.R. – P195 Cristiano, L.M. – P25, P26
Chang, C. – P82
Brown-Whitehorn, T.F. – P255 Cron, R.Q. – P166
Chase, J. – P258
Bruner, K.E. – P245 Cuervo Pardo, L. – 17, P121
Chatterjee, P. – 29
Buatti Small, M. – P48 Cunningham-Rundles, C. – 30,
Chau, A.S. – P112 P100, P187, P213, P230
Buddiga, P. – P176
Chaudhry, S. – P273 Cunnion, K.M. – 53
VOLUME 113, NOVEMBER, 2014 A125
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A126
SPEAKER DISCLOSURES
Curtiss, M.L. – P207 DuBuske, L.M. – 12, P18, P77, P78, Finkas, L. – P117
P89, P90, P91, P233, P234, P235,
Cyr, M. – P276 P236, P237, P307, P308 Fiocchi, A. – 2, P248
Czecior, E. – P307 Duff, C. M. – P218 Firestone, L.E. – P260
Dahdah, L. – 2, P248 Duse, M. – 47, P278 Flores Ruvalcaba, C.N. – P311,
P313
Dara, J. – P161, P240 Dutmer, C. – P118
Foca, M. – P201
Dass, K. – P13, P331 Duzh, E. – P91
Fonacier, L. – 27, 39, P152, P196
DaVeiga, S.P. – 4, P144 Egan, M. – P187
Forastiere, G. – P278
Davidovich, G. – P91 Egea, E. – 28, P65
Foster, P. – P72
Davis, C.M. – 41 Egea, G.E. – 28, P65
Franxman, T. – P111
Davis-Lorton, M. – 27, 39, P196 Eisen , D. – P195
Freiler, J. – P245
de Vos , G. – 25 Ellis, A.K. – 55, P34
Frieri, M. – P103, P323
DeFelice, M. – P97 Enciso-Pelaez, S. – P100
Fuleihan, R. – P200
Del Rio, B.E. – P75, P223 Ender, K. – P201
Gaisenyuk, F. – P233
Del Río, J. – P75 Engel, M. – P294
Galowitz, S. – P97
Demirdag, Y. – P201 Erwin, E.A. – 43, 49
Ganim, R. – P173
Deol, S. – P154, P179 Escamilla, J. – P65
Garavito de Egea, G. – 28, P65
Derkach, V. – P316 Esquivel, B. – P210
Garcia Buheis, M. – P283
DeSantiago-Cardenas, L. – 44 Estrada-Aguilar, J.L. – P70
García Cruz, M.H. – P251, P263,
Descartes, M. – P3 Ettinger, A. – P169 P269
DeWaters, A. – P67 Fajt, M. – P249 Garcia, M. – P270
Dhar, M. – 11 Fang, L. – 28, P65 Garcia-Lloret, M. – 40, P232
Di Coste, A. – P278 Farri, F. – P134 Gard, L. – 52
Di Giorgi, B.K. – P312 Farzan, S. – P194 Gasataya, V. – P108
Diamanti, A. – 2 Fasano, M. – 63, P47 Gaur, S. – 22
Diaz, J.M. – 29 Fatteh, S. – P102, P109, P114 Gavino, A.C. – P262, P283
Diliberto , N.Z. – 41, P260 Fausnight, T.B. – P119 Gawlik, R. – P307
Dillard, K. – P107 Fenny, N. – P23, P175 Gedik, A. – P52, P127
DiMaio, C. – P280 Ferastraoaru, D. – P106, P140, P222 Geh, E. – 10
Ditto, A. – P331 Ferguson, P. – 63 Gelfand, E. – P118
Dodam, J. – P82 Fernandez, D. – P10 Geng, B. – 32, 40, P232
Donnenfeld, E. – 51 Fernandez, J. – P121 George, E. – P84
Doshi, A. – P253 Fernandez de Cordova Aguirre, J. – Ghably, J.G. – P174
Draikiwicz, S. – P197 P7, P53, P130, P178, P318, P322
Ghaffari , G. – P132, P142
Drannik, G.N. – P89, P233, P235, Festic, E. – 7
Gharib, A. – P85
P236 Feuille, E.J. – P205
Ghosh, B. – 17
Dreyfus, D. – P94 Fiedler, J. – P254
Ghosh, D. – 10
Driyanska, V. – P233 Fineman, S.M. – P30, P63
Giacinto Lawrence, J. – P172
Dubovyi, A. – P77
A126 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A127
SPEAKER DISCLOSURES
Gierer, S. – P19, P160 Hamad, A. – P315 Holland, S. – P150
Gimenez, L. – 24, P5 Hamadani, S. – P126 Hopp, R. – P72
Gipson, K. – P141 Hamilton, R. – 43 Horner, C.C. – P129
Glancy, E. – P10, P98 Hamzavi Abedi, Y. – P60 Howarth, P. – P48
Gleeson, P.K. – P68 Hancharou, A. – P88, P90, P91 Hsu, A. – P150
Glick, S. – P93 Hanna, M. – P61 Hu, X. – P81
Gober, L.M. – P255 Hanson, I.C. – P107, P212 Hudes, G. – P106, P140
Goebel, M. – P41 Hanson, J. – 62 Humphrey, A.L. – 42
Gogna, M. – P148 Harada, L. – P252 Hwangpo, T. – P207
Goldberg, B.J. – P247 Harris, R. – P54 Imaoka, M. – P44
Gomez, R.A. – P244, P245 Harte, L. – P69 Imperato, G. – P202
Gong, A. – 19 Hartman, H.N. – P5, P224 Imran , M. – P19
Gonzalez de Alfonzo, R. – P87 Hartz, M. – P170 Indinnimeo, L. – P278
Gonzalez Díaz, S. N. – P16 Hasan, S. – P283 Irizarry Alvardo, J. – 3
Gonzalez Flores, S. – P53, P130, Hauk, M. – P279 Ishmael, F. – P20
P322
Heimall, J. – 64, P9 Iwanaga, T. – P44
Gonzalez ibarra, M. – P313
Helfner, L. – P112 Jacobs, J. – P32
Gonzalez-Estrada, A. – 17, P10,
P121 Helfner, L. – P86 Jacobs, R. – P305
Gonzalez-Flores, S. – P7, P178, P318 Henao, M.P. – P67, P280 Jain, V. – P110
Gordienko, A.I. – P234 Henrickson, S.E. – 64, P239 Janakiram, M. – P106
Gourgy-Hacohen, O. – P32 Henry, T. – 63 Jara, D.A. – 11
Graber, J. – P140 Hernandez Robles, M. – P16 Jesena, A. – P108
Grant, A. – P116 Hernandez-Ramirez, C. – P79 Jiang, N. – P35
Green, T. – 50 Hernandez-Sanchez, H. – P16 Jiao, J. – P129
Greenbaum, J. – P276 Hershey, G.K. – P38 Jin, J. – 36
Greos, L. – P57, P62, P295 Herzog, R. – P185, P237 Joglekar, A.V. – 26
Guha, K. – P174 Higgins, V. – P58 Johnson, C. – 63
Gundling, K. – P133 Hill, J.L. – P165 Johnson, K.E. – P71
Gupta Louis, A. – P85 Hilton, R.P. – 59 Joks, R. – P31, P39, P309
Gupta, M. – 29, P144 Hintermeyer, M. – P224 Jongco, A.M. – P86, P112, P216,
P273
Gupta, R. – 44, P135, P252 Hirsch, A. – 45
Jorge , Y. – 25
Gupta, S. – P85 Hirsch, D. – P159
Joseph, M. – P145
Gurung, P. – P173 Ho, S. – 1
Joshi, A.Y. – 35, 36, P170, P238
Gutiérrez-Ceniceros, M. – P100 Hoban, M.D. – 26
Joshi, N.P. – P110
Gutta, R. – P314 Hobsbawn, B. – P34
Joychan, S. – P13
Haaland, D.A. – P149 Hogan, M. – P282
Jyonouchi, S. – 64, P239
Hall, P. – P29 Holcombe, J.M. – 20, P268
Jyothirmayi, G. – P319
VOLUME 113, NOVEMBER, 2014 A127
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A128
SPEAKER DISCLOSURES
Kachru, R. – 40 King, E. – 33 LeMasters, G.K. – P38
Kagen, S. – P36 Kishikawa, R. – P44 Lemiere, C. – 61
Kalinina, N.A. – P236 Klaustermeyer, W.B. – P124 Leonard, S. – P253
Kamili, Q. – 18, P283, P321, P324 Kleva, A. – P216 Leonardi, L. – 47
Kankirawatana, S. – P1 Koatz, A.M. – P59 Levy, D. – P314
Kannan, J. – P184 Kobrynski, L. – P217 Li, J. – P195
Kapila, A. – P174 Kohn, D.B. – 26 Li, M. – P126, P138, P139
Kaplan, B. – P188 Koterba, A. – P211 Li, Z. – P206
Kaplan, M. – P258 Kreiner, R. – P208 Liacouras, C.A. – P255
Kappagoda, S. – P150 Kremenska, L.V. – 12, P237 Lin, C.K. – P103, P247
Karam, M. – P111 Kremer, C. – 63 Lin, S.K. – P119
Karikari, K. – P292 Kreuz, W. – P274 Linauskiene, K. – P18
Karpel, J. – P288 Krishna, N.K. – 53 Lindgren, K. – P153
Katayeva, I. – P93 Krishnaswamy, G. – P26 Lippo de Becemberg, I. – P87
Katial, R. – P117 Kristofek, L. – P209 Littlefield, M. – 27
Katta, A. – P193 Kubiak, C.D. – P214 Liu, A. Y. – P24, P150, P151
Katta, R. – P321, P324 Kumar, A. – P190 Logsdon, S. – P104
Kau, A.L. – P129 Kumar, K. – 46 Lomas, J.M. – P15, P136
Kaygusuz, S. – P52 Kumar, R. – 56 Looney, R.J. – P15, P136, P231
Kearns, S. – P209 Kuo, C.Y. – 26 Love, T. – P22
Kelbel, T. – P20 Kurchenko, A. – P89 Lucas, R. – 23
Kelly, B.T. – 24 Kurmaeva, N. – P78 Lundberg, C. – P105
Kelly, K.J. – 24 Kurz, J. – P155 Luster, S. – P306
Kempe, E.E. – P272 Kwong, J. – P166 Maccia, C. – P169
Kern, J. – P306 LaBarba, S. – P202, P203 Mack, D.P. – P61
Kerstjens, H.A. – P294 Lanford, E. – P155 Maddox, D. – P11
Khaliq, A. – P4 Lang, D.M. – 17 Maglione, P.J. – 30
Khan, D.A. – P154, P179 Lanser, B.J. – P2 Maik, J. – P290
Kharod, N. – P12 Leal Villarreal, L. – P16 Makris, C.M. – P1
Khoiny, N. – P258 Lecompte, N. – 28, P65 Maldonado Ríos, V.A. – P251
Khojah, A. – P92 Lee, B. – 62 Maleeva, A. – 12
Khokhar, A. – P202 Lee, D. – P303 Malinow, I. – P312
Kiehm, J. – P188 Lee, J. – P255, P303 Mangi, M. – 7
Kim, A.B. – P325, P327 Lee, J.X. – P124 Maples, K.M. – 53
Kim, J.K. – P179 Lee, T. – P162 Marchisotto, M. – P252
Kim, K. – P285 Lee-Kim, C. – P101 Marshall, G.D. – P229
Kim, S.J. – P247 Leiding, J.W. – P214, P218 Martinez, J. – P19
A128 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A129
SPEAKER DISCLOSURES
Martinez-Saguer, I. – P274 Morales, M.B. – P60 Nugent, M. – 24
Maskatia, Z. – P283 Morgal, N.F. – P108 Nunez, M. – 60
Maspero, J. – 61 Moroni-Zentgraf, P. – P294 Nursoy, M. – P52, P127
Mathew, A. – P31 Mortezavi, M. – P15, P136, P231 Nwaobasi-Iwuh, E. – P171
Mathur, A. – P95 Motosue , M.S. – P186 Nyalwidhe, J.O. – 53
Mawhirt, S.L. – P196 Motruk, I.I. – 12, P237 Nyrimanov, K.R. – P235
May, S.M. – P170 Mourad, A.A. – P8 Obase, Y. – P44
Mayer, M. – P299 Mueller, J. – P173 O'Brien, C. – 61
Mazzina, O. – 2, P248 Murphy, H. – 62, P49, P69 Ocampo, T. – P164
McCracken, J. – P183 Murray, D. – 36 Occasi, F. – 47
McDonald, M. – 51 Musatova, K.V. – 12, P237 Ochoa, A. – P137
McGoey, B.A. – P279 Mutnick, J.L. – P271 Ogbogu, P.U. – 49
McGrath, K. – P175 Mygal, L.A. – P236 Olsen, J. – P72
McMorris, M. – P111, P113 Nagar, S. – 56 Omana, V. – 55
McNeil, D. – 8 Nagarajan, S. – P40, P281 Onyango, N. – P292
Mehta, R.S. – 1 Naik, P. – P152 Orson, F. – P262
Mehto, U. – 56 Nakahiro, R. – 19 Ortega-Gonzalez, A. – P79
Melendez, S. – P75 Nasir, H. – P114 Ott, N.L. – P170
Melengu, T. – P278 Navarrete , E. – P75 Ownby, D.R. – 58
Melethil, S. – 1 Navetta, B. – P246 Oza, P. – P21
Mellado Abrego, J. – P311, P313 Nayak, D. – P23, P181 Pacheco, F. – 52
Mendez, J.A. – P14, P312 Nayak, R. – P193 Palacios, T.V. – P182
Meng, Q. – P40, P281 Nayima, V. – P242 Palamarchuk, O. – 12, P37
Metz, C. – 29 Nazari , R. – 25 Paltarackiene, V. – P18
Michelis, M. – P279 Nazario, S. – P14, P312, P330 Paris, K. – P326
Miller, L. – P110 Nebbioso, M. – 47 Parker, J. – P69
Miller, V. – P155 Netterville, A.C. – P137 Parrish, C. – P126, P138, P139
Mills, J. – 36 Nguyen, A.P. – P63 Partida , A. – P223
Minto, H. – 53 Nguyen, H. – P38 Pasha, M. – P206
Moallem, J. – 34, P93 Nguyen, Q.L. – P321, P324 Patel, R. – P48, P319
Modeste, R. – P48 Nichols, K. – 51 Patel, B. – P238
Mohiuddin, A. – P166 Nickels, A.S. – 54, P238 Patel, G. – P155
Molina Macip , M. – P251, P269 Noroski, L.M. – P283 Patel, K. – 33, P133
Montalvo Stanton , E. – 21 North, M.L. – 55 Patel, P.J. – 21
Montandon, S. – 50 Nsouli, S.T. – 41, P260, P286 Patel, S. – P101, P165, P171
Moore, L.E. – P241 Nsouli, S. – P304 Patrimonio, M. – P108
Moorthy, L.N. – P166, P169 Nsouli, T.M. – 41, P260 Paul, R.S. – P167
VOLUME 113, NOVEMBER, 2014 A129
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A130
SPEAKER DISCLOSURES
Paull, K. – P212 Pratt, R. – P276 Rivero Yeverino, D. – P269
Pavlov, K. – P88 Price, R. – P211 Rivkina, V. – 44
Pavon Romero, G.F. – P251, P263, Prikhodko, A. – 12 Roberts, R. – P232
P269, P270
Prince, B. – P17, P200 Robertson, D.M. – P219
Pavord, I.D. – P66
Pun, T. – P110 Rodenas, M. – P42
Pazheri, F. – 17, P125
Qamar, N. – P188 Rodinkova, V.V. – 12, P37
Pelz, B. – P200
Quezada-Chalita, C. – P100 Rodrigues, E. – 3
Peng, T. – P166, P169
Quirt, J.A. – P149 Rodrigues, J.M. – P193
Pepose, J. – 51
Rabinovitch, N. – P2 Rodríguez Gaspar, J.I. – P263
Perez Estrella , Z. – P251
Radojicic, C. – P98 Rodriguez, I. – P270
Perkins, A.M. – 53, P60
Rael, E. – P64, P67, P68, P280 Rodríguez-Roa, M. – P312, P330
Perlov, O. – P149
Rafi, A. – P124, P167 Rogers, S. – 37
Persaud, Y.K. – P134
Ramanava, I. – P91 Rohr, A. – P298
Peterburgskiy, V.F. – P236
Ramírez Jiménez, F. – P251, P263, Rojo-Gutierrez, M. – P311, P313
Peters, A. – P17, P175 P269
Romanova, A. – P276
Petrov, A. – P249 Ramirez Rojo, P. – P311
Rosa, J.S. – P150, P151
Petrovic, A. – P214 Ramirez, F. – P270
Rosenbaum, R. – P208
Petz, Z. – P308 Ramos, C. – P312
Rosenstreich, D.L. – P222
Phillips, E. – 63 Rampur, L. – P180
Rosenthal, D.W. – P128
Pichardo , Y. – 25 Randolph, C.C. – P94
Rosner, G. – P128
Pike, J. – P58 Rans, T. – 13, P164
Rossen, R. – P262
Pimentel , C.M. – P312 Raphael, G. – P73, P74
Routes, J. – P224
Piper, K. – 63 Raschal, S. P. – 20, P268
Roy, T. – P174
Pirani, Z. – P147 Rascon-Pacheco, A. – 60
Rubinstein, A. – P161, P180, P208,
Pityn, P. – 9 Rashid, Q. – P116 P240
Placeres-Uray, F.A. – P87 Rassbach, W.M. – P250 Ruffner, M.A. – P254
Platts-Mills, T.A. – 43, 49 Ravi, A. – P11 Ruiz Morales, R.D. – P251
Polanco , P. – 25 Reddy, M. – 42, 62, P49, P69, P191 Rumelhart, S. – 63
Pollard, S. – P29 Reddy, V. – P99 Ryan, P.H. – P38
Ponda, P. – P172, P202, P203 Regan, J. – P168 Saadia, T.A. – P309
Pongdee, T. – 3 Rehuretska, R. – P89 Saifi, M. – P115
Poowuttikul, P. – 31, P220 Reiss, A. – 27 Salapatek, A. – P48
Poroshina, T.V. – P235, P236 Ren, Z. – P180 Saltoun, C. – P23, P181
Porta, D. – P278 Reponen, T. – P38 Salvatore, S. – P248
Portnoy, J.M. – 11, P257 Riccardi, C. – P248 Sanchez Borja, M. – 28
Potter, L. – 37 Richler, A.L. – 25 Sanchez de la Vega Reynoso, P. –
P251
Potthast, J.K. – P214 Ringwala, S. – P102, P109, P114
Sandoval, E. – P100
Prasad, R. – 56 Rishi, R. – P102, P109, P114
A130 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A131
SPEAKER DISCLOSURES
Sands, M. – P12 Sherr, J. – P24 Strothman, K. – P120, P272
Sangidorj, B. – P316 Shih, J. – P147 Stukus, D. – 50, P272
Saucedo , O. – P223 Shimoda, T. – P44 Subramanian, A. – P10
Savchenko, V.S. – P235, P236 Shroba, J. – 42 Sudano, D. – P165
Schaefer, D. – 32 Shtessel, M. – P140 Sundaresan, A. – 45
Schatz, M. – 19 Shuker, M.M. – P255 Sur, S. – P183
Scherr, R. – P282 Shum, M. – P309 Swann, J. – P71
Scherzer, R. – P120, P272 Sidhu, M. – P110 Ta, V. – P110
Schlegel, C. – P183 Simpson, P. – 24 Taborga, M. – P323
Schmidt, H. – P294 Sindher, S.B. – 4, P9 Tallar, M. – P224
Schmidt, J. – P321 Singh, K. – 56 Tamuz, M. – P273
Schneider, L. – P104 Sivaprasad, U. – P38 Tan, J. – P41
Schroer, B. – P125 Slack, M. – 49 Tartibi, H.M. – P215
Schussler, E. – P199 Slavin, R. – P193 Ten-Boquera, R. – P133
Schwartz, B. – 45 Slavyanskaya , T. – P316 Tentler , A. – 21
Scierski, W. – P307 Small, M. – 17, P10, P58 Teran Juarez , L.M. – P251, P263,
P269, P270
Scott, L. – P126, P138, P139 Snyder, M. – 36
Thethi, A. – 3
Scotten, M. – P160 Solanki, M. – 29
Thiele, J. – 55
Secord, E. – 31, P220 Soliman, M. – 55
Thobani, S. – P126, P138, P139
Segal, M. – P96, P135 Son, H. – P83
Thompson, J.C. – P6
Seidu, L. – P209 Sonza, S. – P108
Tingen, M.S. – 58
Sejour, R. – P273 Soti, L. – P308
Titov, L. – P88
Serban, N. – 59, P71 Speck, A. – P113
Toh, J. – P240
Shaduro, D.V. – P234 Specks, U. – 36
Travis, R. – 21
Shah, A. – 46 Spergel, J.M. – P255
Tripathi, A. – 43
Shah, D. – P177 Spriet, S. – P22
Trotter, J.R. – P214
Shah, H. – P141 Sran, S. – P323
Truong, T. – P177
Shah, N.N. – P326 Steacy, L.M. – P34
Trzil, J. – P82
Shah, S. – P155 Steele, R. – 27, P152
Tsybulkin, N. – P78
Shams, M.R. – P30, P217 Stein , B. – P168
Tsybulkina, V. – P78
Shankar, T. – P249 Stein, M. – P211
Tuano, K. – P107, P283
Shaw, G. – P174 Stepanova, N. – P233
Tucker, M.H. – P244
Sheikh, F. – P4 Steven, G. – P275, P277
Tuer, W. – P211
Sheikh, J. – 19, P258 Stevens, M. – P47, P72
Tupas, M. – P108
Shen, L. – P84 Stevens, W. – P168
Turbyville, J. – P29
Sher, J. – P196 Stokes, J. – P47
Uong, P. – P122, P157, P158
Sher, M. – P218 Storm, M. – 45
Uzuner, S. – P52
VOLUME 113, NOVEMBER, 2014 A131
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A132
SPEAKER DISCLOSURES
Vargas, P. – 24 Warrier, M. – P192 Wu, S. – P212, P283
Vargas-Becerra, M. – 60, P70 Wedner, H.J. – P146 Wysocki, C. – P179
Vartabedian, B.S. – P212 Weis, E. – P231 Xue, X. – 29
Vaughn, M.P. – 16 Weiss, P.F. – P166 Yanez Perez, I.V. – P16
Velasco-Medina, A. – P7, P53, P130, Weissmann, D. – P166 Yang, A. – P173
P178, P318, P322
Welch, K. – P226 Yanovitch, O. – P88
Velazquez-Samano, G. – P7, P53,
P130, P178, P318, P322 Weller, A. – P169 Yao, L. – P95
Verbsky, J. – P224 Wells, H.D. – P6 Yates, A. B. – P241
Verma, R. – P255 Wen, L. – P35 Yin, J. – P35
Vernon , N. – P142 White, A. – P245 Young, R.M. – P123
Vidal-Guzman, J. – P79 White, K.M. – P244, P245 Yu, B. – P153, P303
Visbal, L. – 28, P65 Wild, L. – P156 Yu, M. – P84
Vitale, J. – P192 Williams, D. – 62, P49 Yuksel , M. – P127
Volcheck, G. – 54, P238 Willis, L.K. – 53 Yusin, J.S. – P124, P167
Voloshyna, I. – 27 Willits, E. – 35 Zafra, H.T. – 24, P131
Vutikullird, A.B. – P55 Wilson, N. – P282 Zangrilli, J. – 61
Wada, K.J. – 50 Winkler, K. – 34 Zaragoza , J.R. – P142
Waldram, J.D. – P256 Woessner, K.M. – P110, P256 Zell, K. – 17
Walker, T.J. – P34 Wolf, R. A. – 5 Zgherea, Y. – P19
Wall, L. – P141 Wolff, A. – P171 Zhao, W. – P190
Waller, J.L. – 58 Wolverton, J. – P49 Zheng, Y. – 59
Walton, T. – 32 Wong, A.K. – P126, P138, P139 Zhou, L. – P229, P241
Wang, J. – P250 Wong, D. – P157 Zibert, J.M. – P160
Wang, X. – 17 Wong, P.H. – 13, P244 Zicari, A. – 47
Waqar, S. – P194 Wonnaparhown, A. – P282 Zicari, A. – 47
Ward, B. – P190 Workman, L.J. – 43
A132 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A133
INDEX OF ORAL AND POSTER ABSTRACT AUTHORS AUTHOR INDEX
A Atkinson, P. P242 Borja-Aburto, V.H. 60, P70 Casper, R. P122
Avila, P. P168 Bork, K. P225 Castillo Narvaez, G. P311,
Abghari, P. 31* Aygören-Pürsün, E. P225 Bornstein, L. P185*, P237 P313
Abiteboul, K. P265 Bose, S. P181* Cavero Chavez, V. P228*
Abou Baker, N. 21 Bouillet, L. P225 Celestin, J. P206
Abraham, J.T. P189* B Bour, L.J. P295 Cervantes, M. P270
Abramowitz Saadia, T. 34 Bozoghlanian, V. P314* Cervantes Malagon, M.E. P263
Acantilado, C. P14 Bachove, I.R. P204* Brady, S.P. P146* Challa, S. 33*
Achar, K. 25, P222* Baghian, S. P134 Braunstein, M.Z. P39* Chang, C. P82
Acharya, S. P188 Bahna, S.L. P8, P215 Brensilver, J. 33 Chang, E. P80, P317
Adelman, B. P289 Baik, J. P327* Breslin, M. P232 Chase, J. P258
Adkins, C. P1*, P3 Bajpai, S. P48 Broder, M. P80, P317* Chatterjee, P. 29
Agarwal, P. 22* Baker, J. 8 Brooks, J. P132* Chau, A.S. P112*
Agrawal, S. P85 Baldwin, J. P111 Brown, K.R. P195* Chaudhry, S. P273
Akande, T. P134 Banerji, D. P284 Brown-Whitehorn, T.F. P255 Chefitz, D. P166
Akbar, S. P273 Banks, T. P22, P105 Bruner, K.E. P245* Chekan, V. P90
Akl, E. P190* Bansal, V. 7 Buatti Small, M. P48, P66 Chen, H. P45
Al Gazlan, S. P4* Bantz, S. P42 Buddiga, P. P176* Chen, M. P64*
Al Jiffri, O.H. P43* Barbir, A. 6* Buelow, B.J. P131* Chiarella, S.E. P23*
Al Otaibi, T. P4 Bardelas, J.A. 15 Buenfil Lopez, J.A. P16 Chipps, B.E. P50*, P51*
Al-Kawas, F.H. 41 Barnes, C.S. 11, 52* Bukhari, A. P92 Chokshi, N. P283
Aleem, S. 63* Barth, R. P31 Bundy, V. 40* Chong, M.H. 39*, P196*
Alfonzo, M. P87 Bauer, C. 24 Burch, T.C. 53 Chotikanatis, K. P31*, P93,
Alhashim, S. P4 Bayer, D. P283 Burden, A. P66 P309
Ali, A. P96* Beattie, E. 48 Burke-Mcgovern, S. P198* Chowdhary, A. 22
Alkhatib, F. P219* Becerril-Angeles, M. P70*, Bush, J.S. 58* Christine, K. P157
P79, 60 Chumpitazi, B.P. P212
Allen, C. P3 Busse, P. P162, P199
Bellanti, J.A. 41, P260 Chyung, Y. P289*
Allen, N. 23 Buterleviciute, N. P18
Bellucci, F. 2 Ciaccio, C. 42, 52
Allenbrand, R. 52 Buyantseva, L. P221*
Beloglazov, V. P77, P234 Cianferoni, A. P255
Alpan, O. P92 Bygum, A. P225
Bensch, G. P57*, P288, P294 Cicardi, M. P225, P291
Altrich, M. P6* Byrd, R. P174
Berger, W.E. P294, P301*, Cicero, C. P223
Amar, N.J. 14, P305
P305* Ciesielska, M. 61
Ambrus, J.L. P84
Bergerson, J. P200* C Ciminera, P. P123
Amin, A. P287*
Berkes, E. P328, P329 Clay, K.G. P63
Amin, R. P4
Berman, G. P259 Caballero, T. P225 Cohn, L.A. P82
Amistani, Y. P264
Bernstein, D.I. 14, P38, P41*, CaJacob, A. P3* Collins, C. P24*
An, W. 24 P266
Anand, R. P84* Cakir, E. P52, P127 Columbo, M. P298*
Bernstein, J.A. 10*, P184*, Calais, C.J. 38*
Anderson, J.J. 9* Commins, S.P. 43
P225, P300* Calderon, L.I. P223*
Anderson, J. P3 Conboy, E. 36
Bewtra, A. P47 Calderon, M.A. 15
Anderson, J.T. P207 Conner, K. P153
Bhatti, H. P220* Caldwell, J.W. P25
Anderson, L. P167 Cook, K. P243*
Biagini Myers, J.M. P38 Camacho, J.M. P230*
Andreae, D.A. P213* Corren, J. P62
Biedenkapp, J. P289 Camacho Ordonez, N. P251
Andujar-DeLaCruz, J. P166 Corrente, S. 5, P248
Bielory, B.P. 51* Campbell, A. P285
Angeles-Garay, U. 60, P79 Corrigan, C.J. P66
Bielory, L. 33, 51, P40*, P281, Campbell, J.D. P66
Anghel, S. 33 P290, P306 Coscia, G. P201*
Ansary, F.F. P163* Cancian, M. P225 Coyne, T. P27, P28
Bilaver, L. P252
Anthony, K. P156* Capitle, E. P197 Craig, T.J. P99, P163, P221,
Bird, J.A. P115
Antonevich, N. P90 Capitle MD, E. P319 P225*, P292
Bisyuk, Y. P77
Antonova, E. 57, P80, P317 Capriati, T. 2 Craig, V. P166
Bjermer, L. 61
Antonova, J. P46, P320 Carino Cartagena, D.A. P7, Crandall, L. 24
Blaziene, A. P18 P53, P130, P178*, P318,
Anyane-Yeboa, K. P201 Crans Yoon, A. 19*
Bleecker, E.R. P66 P322
Aquino, M. 27, 39, P152, P196 Crawford, W. 19
Blessing-Moore, J. P300 Carlton, B.G. 20*, P268*
Arakali, S. P197 Creticos, P. 14*
Blumenstock, J. P252 Carr, T.F. P165
Arias Cruz, A. P16 Crisp, H.C. 13
Boccon-Gibod, I. P225 Carr, W.W. P295
Arora, R. P29 Cristiano, L.M. P25*, P26*
Bodner, S. P273* Caruthers, C. P192*
Arroyo-Cruz, M.E. P7, P53, Cron, R.Q. P166
Bolgar, B. P209 Casale, T. P295*
P130, P178, P318, P322 Cuervo-Pardo, L. 17, P121*
Bollard, C.M. P212 Casciano, J. P48*
Asawa, A. P143* Cuff, C. P285
Bonagura, V.R. 29, P112, P159 Casillas, A. 18
Ashton, V.L. P66 Cunningham-Rundles, C. 30,
Bonds, R. P143 Casper, J. P224
Assa’ad, A. P195 P100, P187, P213, P230
Borish, L. P182
VOLUME 113, NOVEMBER, 2014 A133
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A134
AUTHOR INDEX
Cunnion, K.M. 53 E Furcha, R. P287 Grant, A. P116
Curtiss, M.L. P207* Grant, J.A. P227
Cyr, M. P276 Ebeling, M. P261 Green, T. 50
Czecior, E. P307 Egan, M. P187* G Greenbaum, J. P276
Egea, E. 28, P65* Greos, L. P57, P62*, P295
Egea, G.E. 28*, P65 Gaisenyuk, F. P233 Grier, T.J. P27*, P28*
D Eisen, D. P195 Galowitz, S. P97* Guha, K. P174
Eisner, M.D. P45 Ganim, R. P173 Guilarte, M. P225
D’Addio, A. P299* Ellis, A.K. 55*, P34 Garcia, E. 18* Gundling, K. P133
Dahdah, L. 2*, P248 Enciso-Pelaez, S. P100 Garcia, M. P270 Gupta, M. 29, P144*
Dara, J. P161*, P240 Ender, K. P201 Garcia Buheis, M. P283 Gupta, R. P135*, 44*, P252*
Dass, K. P13, P331* Engel, M. P288, P294, P295 García Cruz, M.D. P251 Gupta, S. P85, P227
DaVeiga, S.P. 4, P144 Engl, W. P227 García Cruz, M.H. P269, P263 Gupta Louis, A. P85
Davidovich, G. P91 Erwin, E.A. 43, 49 Garcia-Lloret, M. 40, P232 Gurung, P. P173
Davis, C.M. 41 Escamilla, J. P65 Gard, L. 52 Gutiérrez-Ceniceros, M. P100
Davis-Lorton, M. 27, 39, P196 Esquivel, B. P210* Garner, L. P261 Gutta, R. P314
de Vos, G. 25 Estrada-Aguilar, J.L. P70 Gasataya, V. P108
Dees, J. 23 Ettinger, A. P169 Gaur, S. 22
DeFelice, M. P97 Gavino, A.C. 18, P283* H
Del Rio, B.E. P75, P223 Gawchik, S. P302
Del Río, J. P75 F Gawlik, R. P307 Haaland, D.A. P149
Demirdag, Y. P201 Gedik, A. P52, P127 Hadari, Y. P82
Dennerlein, J. 6 Fajt, M. P249 Gedrich, R.W. P82 Hall, D. P27, P28
Deol, S. P154*, P179 Fang, L. 28, P65 Geh, E. 10 Hall, P. P29
DePietro, M. P50, P51 Farkas, H. 8, P225 Gelfand, E. P118 Hamad, A. P315*
Derkach, V. P316 Farri, F. P134* Geng, B. 32*, 40, P232* Hamadani, S. P126*
DeSantiago-Cardenas, L. 44 Farzan, S. P194 George, E. P58*, P84 Hamilton, R. 43
Descartes, M. P3 Fasano, M. 63, P47 Gever, L. P58*, P299, P300, Hampel, F. P302
Devillier, P. P267 Fatteh, S. P102, P109, P114 P301 Hamzavi Abedi, Y. P60*
DeWaters, A. P67* Faucette, R. P289 Ghably, J.G. P174* Hancharou, A. P88, P90, P91
Dhar, M. 11 Fausnight, T.B. P119 Ghaffari, G. P132, P142 Hanna, M. P61*
Di Coste, A. P278 Fenny, N. P23, P175* Gharib, A. P85* Hanson, I.C. P107, P212
Di Giorgi, B.K. P312 Ferastraoaru, D. P106*, P140, Ghosh, B. 17 Hanson, J. 62*
Diamanti, A. 2 P222 Ghosh, D. 10 Harada, L. P252
Diaz, J.M. 29* Ferguson, P. 63 Giacinto Lawrence, J. P172* Harris, R. P54*
Diliberto, N.Z. 41, P260 Fernandez, D. P10 Gierer, S. P19, P160 Harrow, B. P58
Dillard, K. P107 Fernández de Córdova- Gillespie, M. P55 Harte, L. P69
DiMaio, C. P280* Aguirre, J.C. P7, P53*, Gimenez, L. 24, P5 Hartman, H.N. P5*, P224
Ditto, A. P331 P121, P130*, P178, Gipson, K. P141 Hartz, M. P170
Dodam, J. P82 P189, P318*, P322* Glancy, E. P10, P98* Hasan, S. P283
Donnenfeld, E. 51 Ferreira, M.B. P225 Gleeson, P.K. P68* Haselkorn, T. P45
Doshi, A. P253* Festic, E. 7 Glick, S. P93 Hauk, M. P279
Dotiwala, Z. P48 Feuille, E.J. P205* Gober, L.M. P255 Heimall, J. 64, P9
Draikiwicz, S. P197* Fiedler, J. P254 Goebel, M. P41 Helfner, L. P86*, P112
Drannik, G.N. P235, P236 Fineman, S.M. P30, P63 Gogna, M. P148* Henao, M.P. P67
Drannik, G. P89, P233 Finkas, L. P117* Goldberg, B.J. P247 Henao, P. P280
Dreyfus, D.H. P94 Fiocchi, A. 2, 5, P248* Golden, D.B. P265* Hendershot, R.W. 23
Driyanska, V. P233 Firestone, L.E. P260 Gomez, R.A. P244, P245 Hendrickson, B. P285
Du, Q. P296, P297 Fitzpatrick, A. 18 Gong, A. 19 Henrickson, S.E. 64*, P239*
Dubovyi, A. P77 Flores Ruvalcaba, C.N. P311*, Gonzalez de Alfonzo, R. P87 Henry, T. 63
P313
DuBuske, L.M. 12*, P18*, Gonzalez Díaz, S.N. P16 Henson, M. P328, P329
P37*, P77*, P78*, P88*, Foca, M. P201 Gonzalez ibarra, M. P313 Hernandez Robles, M. P16
P89*, P90*, P91*, P233*, Fonacier, L. 27, 39, P152, Gonzalez-Estrada, A. 17*, P10, Hernandez-Ramirez, C. P79*
P234*, P235*, P236*, P196 P121 Hernandez-Sanchez, H. P16*
P307*, P308* Forastiere, G. P278 Gonzalez-Flores, S. P53, P130, Hershey, G.K. P38
Duff, C.M. P218* Ford, L. P288 P178, P318, PP322 Herzog, R. P185, P237*
Duncan, E. P27, P28 Foster, P. P72 González-Flores, S. P7 Higgins, V. P58
Durham, S. P257 Franklin, K.B. P296, P297 Gopalan, G.H. P66 Hill, J.L. P165*
Duse, M. 47*, P278* Franxman, T. P111 Gordienko, A.I. P234 Hilton, R.P. 59
Dutmer, C. P118* Freiler, J. P245 Gourgy-Hacohen, O. P32* Hintermeyer, M. P224
Duzh, E. P91 Frieri, M. P103, P323 Graber, J. P140 Hirsch, A. 45
Fuleihan, R. P200
A134 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A135
AUTHOR INDEX
Hirsch, D. P159* K Krishna, N.K. 53 Longhurst, H. P225
Ho, S. 1 Krishnan, J. P48 Looney, R.J. P15, P136, P231
Hoban, M.D. 26 Kachru, R. 40 Krishnaswamy, G. P26 Love, T. P22
Hobsbawn, B. P34 Kagen, S. P36* Kristofek, L. P209 Lubeski, C. P82
Hogan, M. P282 Kalinina, N.A. P236 Kubiak, C.D. P214* Lucas, R. 23*
Holcombe, J.M. 20, P268 Kamili, Q. 18*, P283, P321*, Kulich, K. P284 Lundberg, C. P105*
Holland, S. P150 P324* Kumar, A. P190 Luster, S. P306
Hopp, R. P72 Kankirawatana, S. P1 Kumar, K. 46*
Horak, F. P266 Kannan, J. P184 Kumar, R. 56*
Horner, C.C. P129 Kapila, A. P174 Kuo, C.Y. 26* M
Howarth, P. 48 Kaplan, A. 57* Kurchenko, A. P89
Kaplan, B. P188 Kurmaeva, N. P78 Maccia, C. P169
Hsu, A. P150
Kaplan, M. P258 Mack, D.P. P61
Hu, X. P81* Kurz, J. P155
Kappagoda, S. P150 Kwong, J. P166 Maddox, D. P11
Hudes, G. P106, P140
Karafilidis, J. P57, P62 Magerl, M. P225
Hulsey, T. P261
Karam, M. P111* Maglione, P.J. 30*
Humphrey, A.L. 42*
Karikari, K. P292 L Maik, J. P290*
Hwangpo, T. P207
Karpel, J. P288 Makris, C.M. P1
Katayeva, I. P93* LaBarba, S. P202, P203* Maldonado Ríos, V.A. P251
I Katial, R. P117 LaForce, C. P73* Maleeva, A. 12
Katta, A. P193 Lanford, E. P155 Malinow, I. P312
Iarrobino, R. P289 Katta, R. P321, P324 Lang, D.M. 17 Maloney, J. 14, 15, P257,
Imaoka, M. P44 Kau, A.L. P129 Lanier, B.Q. P259 P259*, P266
Imperato, G. P202* Kaur, A. 14, 15, P257, P259 Lanser, B.J. P2* Mandel, E.M. P82*
Imran, M. P19* Kaygusuz, S. P52 LaVallee, T. P82 Mangi, M. 7*
Indinnimeo, L. P278 Kearns, S. P209* Lawrence, M. P182 Maples, K.M. 53*
Iribarren, C. P45 Kelbel, T. P20* Leal Villarreal, L. P16 Marchisotto, M. P252
Irizarry Alvardo, J. 3 Kelly, B.T. 24* Lecompte, N. 28, P65 Marshall, G.D. P229
Ishmael, F. P20 Kelly, K.J. 24 Lee, B. 62 Martinez, J. P19
Iverson, H. P56, P73, P74, P76 Kempe, E.E. P272* Lee, D. P303 Martinez-Saguer, I. P225,
Iwanaga, T. P44 Lee, J. P303 P274*
Kenniston, J. P289
Lee, J.X. P124* Maskatia, Z. P283
Kern, J. P306*
Lee, J. P255* Maspero, J. 61*
Kerstjens, H. P288
J Lee, T. P162* Mathew, A. P31
Kerstjens, H.A. P294, P295
Lee-Kim, C. P101* Mathur, A. P95*
Khalil, S. 57
Jacobs, J. P32 Leibl, H. P227 Mawhirt, S.L. P196
Khaliq, A. P4
Jacobs, R. P305 Leiding, J. P218 May, S.M. P170*
Khan, D.A. P179, P154
Jain, N. P158 Leiding, J.W. P214 Mayer, M. P299
Kharod, N. P12*
Jain, V. P110 LeMasters, G.K. P38 Mazzina, O. 2, 5, P248
Khoiny, N. P258*
Janakiram, M. P106 Lemell, P. P266 McCracken, J. P183*
Khojah, A. P92*
Janelli, M. 6 Lemiere, C. 61 McDonald, M. 51
Khokhar, A. P202
Jara, D.A. 11* Leonard, S. P253 McGoey, B.A. P279
Kiehm, J. P188*
Javoronok, S. P88 Leonardi, L. 47 McGrath, K. P175
Kim, A. P325*
Jesena, A. P108 Levy, D. P314 McMorris, M. P111, P113
Kim, A.B. P327
Jiang, N. P35* Li, C. P48 McNeil, D. 8
Kim, J.K. P179*
Jiao, J. P129* Li, H. 8* Mehta, R.S. 1
Kim, K. P285
Jin, J. 36* Li, J. P305, P195 Mehto, U. 56
Kim, S.J. P247*
Joglekar, A.V. 26 Li, M. P126, P138, P139 Meier, E.J. P293*
King, E. 33
Johnson, C. 63 Li, Z. P206*, 14, P257, P266 Melamed, I. P227
Kishikawa, R. P44
Johnson, K.E. P71* Liacouras, C.A. P255 Melendez, S. P75*
Klaustermeyer, W.B. P124
Joks, R. P31, P39, P309 Lin, C.K. P247 Melengu, T. P278
Kleva, A. P216*
Jongco, A.M. P86, P112, P216, Lin, C. P103* Melethil, S. 1*
Koatz, A.M. P59*
P273 Lin, M. 6 Mellado Abrego, J. P311, P313
Kobrynski, L. P217, P227
Jorge, Y. 25 Lin, S.K. P119* Meltzer, E.O. P299
Koch, G. P257
Joseph, M. P145* Linauskiene, K. P18 Meltzer, S. P300
Kohn, D.B. 26
Joshi, A.Y. 35, 36, P170, P238 Lindgren, K. P153* Mendez, J.A. P14*
Koterba, A. P211*,
Joshi, N.P. P110* Lippo de Becemberg, I. P87 Méndez, J. P312
Kreiner, R. P208*
Joychan, S. P13* Littlefield, M. 27 Meng, Q. P40, P281*
Kremenska, L.V. 12, P37
Jyonouchi, S. 64, P239 Liu, A.Y. P24, P150, P151 Metz, C. 29
Kremer, C. 63
Jyothirmayi PA-C, G. P319 Logsdon, S. P104* Michelis, M. P279*
Kreuz, W. P274
Lomas, J.M. P15, P136* Miller, D.P. P45
Krier, J. P328, P329
VOLUME 113, NOVEMBER, 2014 A135
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A136
AUTHOR INDEX
Miller, D. P73, P74, P76 Nolte, H. 14, 15, P257*, P259, Pavon Romero, G. P251, P263, Ramanava, I. P91
Miller, L. P110 P266* P269 Ramirez, F. P270
Miller, R. P285 Nordenfelt, P. P225 Pavord, I.D. P66 Ramírez Jimenez, F. P251,
Miller, V. P155* Noroski, L.M. P283 Pazheri, F. 17, P125* P263, P269
Mills, J. 36 North, M.L. 55 Pearlman, D. P56 Ramirez Rojo, P. P311
Minto, H. 53 Nsouli, S. P286*, P304* Pelz, B. P200 Ramos, C. P312
Mire, B. P33 Nsouli, S.T. 41, P260 Peng, T. P166*, P169* Rampur, L. P180
Moallem, J. 34, P93 Nsouli, T.M. 41*, P260* Pepose, J. 51 Randolph, C.C. P94*
Modeste, R. 48 Nugent, M. 24 Perez Estrella, Z. P251 Rans, T.S. 13, P164
Mohiuddin, A. P166 Nunez, M. 60* Perkins, A.M. 53, P60 Raphael, G. P73, P74*
Moldovan, D. P291 Nursoy, M. P52*, P127* Perlov, O. P149 Raschal, S.P. 20, P268
Molina Macip, M. P251, P269* Nwaobasi-Iwuh, E. P171 Persaud, Y.K. P134 Rascon-Pacheco, A. 60
Monsul, N. P328, P329 Nyalwidhe, J.O. 53 Peterburgskiy, V.F. P236 Rashid, Q. P116*
Montalvo Stanton, E. 21 Nyrimanov, K.R. P235 Peters, A. P17, P175 Rassbach, W.M. P250*
Montandon, S. 50 Petrov, A. P249 Ratner, P. P301
Moore, L.E. P241* Petrovic, A. P214 Ravi, A. P11*
Moorthy, L.N. P166, P169 O Petz, Z. P308 Reddy, M. 42, 62, P49, P69
Morales, M.B. P60 Phillips, E. 63 Reddy, M.B. P191*
Morgal, N.F. P108* O’Brien, C. 61, P73, P74 Pichardo, Y. 25 Reddy, V. P99*
Moroni-Zentgraf, P. P288, Obase, Y. P44 Pike, J. P58 Regan, J. P168*
P294, P295 Ocampo, T. P164* Pimentel, C.M. P312 Rehuretska, R. P89
Mortezavi, M. P15*, P136, Occasi, F. 47 Piper, K. 63 Reinero, C.R. P82
P231* Ochoa, A. P137 Pirani, MD, Z. P147* Reiss, A. 27
Motosue, M.S. P186* Ogbogu, P.U. 49 Pityn, P. 9 Relan, A. 8, P291
Motruk, I. 12 Olsen, J. P72* Placeres-Uray, F.A. P87* Ren, Z. P180*
Motruk, I.I. P37 Omachi, T.A. 57, P45*, P320 Platts-Mills, T.A. 49, 43 Reponen, T. P38
Mourad, A.A. P8* Omana, V. 55 Plunkett, G. P33* Reshef, A. 8, P225
Mueller, J. P173 Onyango, N. P292* Polanco, P. 25 Reynolds, R. 23
Murphy, H. 62, P49*, P69* Orson, F. 18 Pollard, S. P29 Rhodes, B. 23
Murphy, K. P294* Ortega-Gonzalez, A. P79 Ponda, P. P172, P202, P203 Riccardi, C. 5, P248
Murray, D. 36 Ostrom, N. P56* Pongdee, T. 3 Richler, A.L. 25*
Musatova, K.V. 12, P37 Ott, N.L. P170 Poowuttikul, P. 31, P220 Riedl, M. P291*
Mutnick, J.L. P271* Ownby, D.R. 58 Porebski, G. 8 Rigazio, A. P66
Mygal, L.A. P236 Oza, P. P21* Poroshina, T.V. P235, P236 Ringwala, S. P102, P109*,
Porta, D. P278 P114
Portnoy, J.M. 11, P257 Rishi, R. P102*, P109, P114*
N P Potter, L. 37 Rivero Yeverino, D. P269
Potthast, J.K. P214 Rivkina, V. 44
Nagar, S. 56 Pacheco, F. 52
Prasad, R. 56 Roberts, R. P232
Nagarajan, S. P40*, P281 Palacios, T.V. P182*
Pratt, R. P276* Robertson, D.M. P219
Naik, P. P152* Palamarchuk, O.O. 12, P37
Rodenas, M. P42*
Price, D.B. P58, P66*
Nakahiro, R. 19 Paltarackiene, V. P18
Price, R. P211 Rodinkova, V.V. 12, P37
Naples, A. P261 Paolozzi, L. P264
Prikhodko, A. 12 Rodrigues, E. 3
Nasir, H. P114 Paris, K. P326
Prince, B. P17*, P200 Rodrigues, J.M. P193*
Navarrete, E. P75 Parker, J. P69
Pun, T. P110 Rodriguez, I. P270*
Navetta, B. P246* Parrish, C. P126, P138*, P139
Rodríguez Gaspar, J.I. P263*
Nayak, D. P23, P181 Partida, A. P223
Rodríguez-Roa, M. P312*,
Nayak, R. P193 Pasha, M. P206 Q P330*
Nayima, V. P242* Patel, B. P238* Rogers, S. 37*
Nazari, R. 25 Patel, G. P155 Qamar, N. P188 Rohr, A. P298
Nazario, S. P14, P312, P330 Patel, K. P133*, 33 Quezada-Chalita, C. P100 Rojo-Gutierrez, M.I. P311,
Nebbioso, M. 47 Patel, M.K. P296, P297* Quirt, J.A. P149* P313*
Nelson, H.S. 15*, P266 Patel, P.J. 21* Romanova, A. P276
Netterville, A.C. P137* Patel, R. 48* Rosa, J.S. P150*, P151*
Ney, J. 32 Patel, S. P171*, P165, P101 R Rosenbaum, R. P208
Nguyen, A.P. P63* Patel MD, R. P319* Rosenstreich, D.L. P222
Nguyen, H. P38* Patrimonio, M. P108 Rabinovitch, N. P2
Rosenthal, D.W. P128
Nguyen, Q.L. P321, P324 Paul, R.S. P167 Radojicic, C. P98
Rosner, G. P128*
Nichols, K. 51 Paull, K. P212 Rael, E. P64, P67, P68, P280
Rossen, R. 18
Nickels, A.S. 54*, P238 Pavlov, K. P88 Rafi, A. P124, P167
Routes, J. P224
Pavon, G. P270 Raimundo, K. 57, P46, P317,
Roux, M. P267*
P320*
A136 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A137
AUTHOR INDEX
Roy, T. P174 Shaw, G. P174 T Verbsky, J. P224
Rubinstein, A. P161, P180, Sheikh, F. P4 Verma, R. P255
P208, P240 Sheikh, J. 19, P258 Ta, V. P310* Vernon, N. P142
Ruffner, M.A. P254* Shen, L. P84 Taborga, M. P323 Vidal-Guzman, J. P79
Ruiz, N. P57, P62, P299, P300, Sher, J. P196 Tallar, M. P224* Visbal, L. 28, P65
P301, P302 Sher, M. P218 Tamuz, M. P273 Vitale, J. P192
Ruiz Morales, R.D. P251* Sherr, J. P24 Tan, J. P41* Volcheck, G.W. 54, P238
Rumelhart, S. 63 Shih, MD, J. P147 Tantry, S. P305 Voloshyna, I. 27
Ryan, P.H. P38 Shimoda, T. P44* Tartibi, H.M. P215* von Ziegenweidt, J. P66
Shroba, J. 42 Tashkin, D.P. P50, P51 Vutikullird, A.B. P55
Shtessel, M. P140* Taveras, H. P56, P73, P74, P76
S Shuker, M.M. P255 Ten-Boquera, R. P133
Shum, M. P309* TenHoor, C. P289 W
Saadia, T.A. P309
Sidhu, M. P110 Tentler, A. 21
Saifi, M. P115* Wada, K.J. 50*
Sigmund, R. P288 Teran, L. P270
Salapatek, A. 48 Wahn, U. P264
Simpson, P. 24 Teran Juarez, L.M. P251,
Saltoun, C. P23, P181 Waldram, J.D. P256*
Sindher, S.B. 4*, P9* P263, P269
Salvatore, S. 5, P248 Walker, T.J. P34*
Singh, K. 56 Thethi, A. 3*
Sanchez Borja, M. 28 Wall, L. P141
Sivaprasad, U. P38 Thiele, J. 55
Sanchez de la Vega Reynoso, P. Waller, J.L. 58
Skoner, D. P259 Thobani, S. P126, P138, P139
P251 Walton, T. 32
Sandoval, E. P100* Slack, M. 49* Thompson, J.C. P6
Slavin, R. P193 Tian, X. P296, P297 Wang, J. P250
Sands, M. P12 Wang, X. 17
Sangidorj, B. P316 Slavyanskaya, T. P316* Tingen, M.S. 58
Small, C. P305 Tiplady, B. P284* Waqar, S. P194*
Saucedo, O. P223 Ward, B. P190
Small, M. P58 Titov, L. P88
Savchenko, V.S. P235, P236 Warrier, M. P192
Smith, M.A. 17, P10* Toh, J. P240*
Schaefer, D. 32 Wasserman, R.L. P227
Snyder, M. 36 Travis, R. 21
Schaffer, F.M. P261* Wayne, D. P76
Solanki, M. 29 Tripathi, A. 43*
Schatz, M. 19 Weber, R. 14
Solari, P. P46*, P80, P320 Tripp, C. P285*
Scherr, R. P282* Wedner, H.J. P146, P291
Soliman, M. 55 Trotter, J.R. P214
Scherzer, R. P120, P272 Weis, E. P231
Song, S. P55 Trudo, F. P50, P51
Schiff, R.I. P227 Weiss, P.F. P166
Sonza, S. P108 Truong, T. P177
Schlegel, C. P183 Weissmann, D. P166
Soteres, D. P301 Trzaskoma, B. 57, P46, P320
Schmidt, H. P294 Welch, K. P226*
Soti, L. P308 Trzil, J. P82
Schmidt, J. P321 Weller, A. P169
Schneider, L. P104 Speck, A. P113* Tsybulkin, N. P78
Specks, U. 36 Tsybulkina, V. P78 Wells, H.D. P6
Schroer, B. P125 Wen, L. P35
Spergel, J.M. P255 Tuano, K. P283, P107*
Schussler, E. P199* White, A. P245
Schwartz, B. 45 Spriet, S. P22* Tucker, M.H. P244
Sran, S. P323* Tuer, W. P211 White, K.M. P244, P245
Schwartz, S.A. P228 Wild, L. P156
Scierski, W. P307 Stanaland, B. P302* Tupas, M. P108
Steacy, L.M. P34 Turbyville, J. P29* Williams, D. 62, P49
Scott, L. P126, P138, P139 Willis, L.K. 53
Scotten, M. P160 Steele, R. 27*, P152
Stein, B. P168 Willits, E. 35*
Seare, J. 5 U Wilson, N. P282
Secord, E. 31, P220 Stein, M. P211, P227
Steinfeld, J. P55* Winkler, K. 34*
Segal, M. P96, P135 Uong, P. P122*, P157*, P158* Woessner, K.M. P256, P310
Seidu, L. P209 Stepanova, N. P233
Urdaneta, E.R. P296*, P297 Wolf, R.A. 6
Sejour, R. P273 Steven, G. P275*, P277*
Uzuner, S. P52 Wolff, A. P171
Serban, N. 18, 59, P71 Stevens, M. P47*, P72
Stevens, W. P168 Wolverton, J. P49
Settipane, R. P302 Wong, A.K. P126, P138, P139*
Sexton, D. P289 Stobiecki, M. P225, P291 V
Stokes, J. P47 Wong, D. P157
Shaduro, D.V. P234 Wong, P.H. 13*, P244*
Shah, A. 46 Storm, M. 45 Vandewalker, M.L. P288*
Strothman, K. P120*, P272 Wonnaparhown, A. P282
Shah, D. P177* Vargas, P. 24
Stukus, D. 50, P272 Workman, L.J. 43
Shah, H. P141* Vargas-Becerra, M. 60, P70
Subhadra, B. P328*, P329* Wu, C. P285
Shah, M. P45 Vartabedian, B.S. P212
Subramanian, A. P10 Wu, M. P296, P297
Shah, N.N. P326* Vaughn, M.P. 16*
Sudano, D. P165 Wu, S. P212*, P283
Shah, S. P155 Velasco-Medina, A.A. P7, P53,
Sun, G. P80, P317 Wysocki, C. P179
Shams, M.R. P30*, P217* P130, P178, P318, P322
Shankar, T. P249* Sundaresan, A. 45* Velazquez-Samano, G. P7,
Shastri, S. P328 Sur, S. P183 P53, P130, P178, P318,
Swann, J. 18, P71 P322
VOLUME 113, NOVEMBER, 2014 A137
ACAAIAbstractAnnals14v4_ACAAI Abstract Book 9/25/14 9:29 AM Page A138
AUTHOR INDEX
X
Xue, X. 29
Y
Yanez Perez, I.V. P16
Yang, A. P173*
Yang, W.H. P267, P291
Yanovitch, O. P88
Yao, L. P95
Yates, A.B. P241
Yel, L. P227*
Yin, J. P35
Young, R.M. P123*
Yu, B. P153, P303*
Yu, M. P84
Yuksel, M. P127
Yusin, J.S. P124, P167*
Z
Zafra, H. 24
Zafra, H.T. P131
Zangrilli, J. 61
Zanichelli, A. 8
Zaragoza, J.R. P142*
Zazzali, J. 57, P46, P80*, P320
Zeldin, R.K. P264*, P265,
P267
Zell, K. 17
Zgherea, Y. P19
Zhao, W. P190
Zheng, Y. 59*
Zhou, L. P229*, P241
Zibert, J.M. P160*
Zicari, A. 47, 47
Zieglmayer, P. P266
Zieglmayer, R. P266
Zuraw, B. P225
A138 ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Michael S. Niederman Severe Pneumonia Lung Biology in Health and Disease, Volume 206Document450 pagesMichael S. Niederman Severe Pneumonia Lung Biology in Health and Disease, Volume 206Alirio Bastidas0% (1)
- Pil 880 PDFDocument6 pagesPil 880 PDFBobbyNo ratings yet
- Nursing Exam For Review With RationaleDocument39 pagesNursing Exam For Review With RationaleKeizha Ronatay100% (2)
- Nursing Care Plan Bronchial AsthmaDocument2 pagesNursing Care Plan Bronchial Asthmaderic93% (60)
- Haad Exam 7Document22 pagesHaad Exam 7MallikarjunNo ratings yet
- Foreign Body Aspiration in Children-A Diagnostic ChallengeDocument3 pagesForeign Body Aspiration in Children-A Diagnostic ChallengeViany RehansyahNo ratings yet
- Community Health ProfileDocument16 pagesCommunity Health ProfilecrainsnewyorkNo ratings yet
- Asthma in Children CMEDocument37 pagesAsthma in Children CMEGideon K. MutaiNo ratings yet
- Bronchial Asthma Nursing Care PlansDocument2 pagesBronchial Asthma Nursing Care PlansdeincediannaNo ratings yet
- Autacoid PharmacologyDocument38 pagesAutacoid PharmacologyAakkkNo ratings yet
- HONKA Brochure Lowres Bypage PDFDocument76 pagesHONKA Brochure Lowres Bypage PDFCamila LopezNo ratings yet
- July PNLE 2011 PreBoard ExamDocument9 pagesJuly PNLE 2011 PreBoard ExamRon KimNo ratings yet
- Children's Hospital Association of Texas Asthma Management Pathway (ED and IP) Asthma ScoresDocument4 pagesChildren's Hospital Association of Texas Asthma Management Pathway (ED and IP) Asthma ScoresMumunni MoretzNo ratings yet
- Atopic EczemaDocument251 pagesAtopic EczemaxandinhagNo ratings yet
- Utility of The Sputum Cytology Applying MGG and Pap Stains in Monitoring Sudanese Patients Complaining of Bronchial AsthmaDocument6 pagesUtility of The Sputum Cytology Applying MGG and Pap Stains in Monitoring Sudanese Patients Complaining of Bronchial AsthmaDr. Asaad Mohammed Ahmed BabkerNo ratings yet
- 1000 Drug CardsDocument33 pages1000 Drug Cardstfish106588% (90)
- 7081 - PHARMA - AnnualReport - 2001-12-31 - Pharma-OpsActivities-Achievements (795KB) - 583228015Document35 pages7081 - PHARMA - AnnualReport - 2001-12-31 - Pharma-OpsActivities-Achievements (795KB) - 583228015surayaNo ratings yet
- A Descriptive Study To Assess The Knowledge and Practices Regarding COPD Prevention and Management Among Staff Nurses in Selected Hospital of District PatialaDocument27 pagesA Descriptive Study To Assess The Knowledge and Practices Regarding COPD Prevention and Management Among Staff Nurses in Selected Hospital of District PatialaEditor IJTSRD100% (1)
- Care of Patients On Lower Respiratory System Drugs Presented by Donnahae Rhoden SalmonDocument39 pagesCare of Patients On Lower Respiratory System Drugs Presented by Donnahae Rhoden SalmonKishi CopelandNo ratings yet
- What Are Dust MitesDocument4 pagesWhat Are Dust MitesNada PetrovićNo ratings yet
- AsthmaDocument3 pagesAsthmaAnjana BasilNo ratings yet
- Block - 3 - 2014 Block 3 BookDocument197 pagesBlock - 3 - 2014 Block 3 BookhappyhappylandNo ratings yet
- Water Cures - F. Batmanghelidj, M.DDocument22 pagesWater Cures - F. Batmanghelidj, M.DEric Callahan100% (1)
- PSYCHOIMMUNOLOGYDocument23 pagesPSYCHOIMMUNOLOGYHemant100% (1)
- Dissertation Allergic RhinitisDocument8 pagesDissertation Allergic RhinitisWritingPaperServicesReno100% (1)
- Treating Acute BronchiolitisDocument3 pagesTreating Acute BronchiolitisHajar Hanis SofiaNo ratings yet
- Reviewer For OediaDocument19 pagesReviewer For Oedias9crhvrymhNo ratings yet
- AguidetorespiratorycodingDocument16 pagesAguidetorespiratorycodingSusan GleesonNo ratings yet
- Pharmacology, 2nd Semester - Sollas NotesDocument224 pagesPharmacology, 2nd Semester - Sollas NotesTovin NguyenNo ratings yet
- Final Test FK - 1 - Ang - 2019 - Juli 2020Document3 pagesFinal Test FK - 1 - Ang - 2019 - Juli 2020CahayaNo ratings yet