Professional Documents
Culture Documents
Disorders of Potassium Homeostasis: Pathophysiology and Management
Uploaded by
abegail eliahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disorders of Potassium Homeostasis: Pathophysiology and Management
Uploaded by
abegail eliahCopyright:
Available Formats
Review Article
Disorders of Potassium Homeostasis: Pathophysiology and
Management
Sumedh S Hoskote*, Shashank R Joshi**, Amit K Ghosh***
Abstract
Disorders of potassium homeostasis are common electrolyte abnormalities encountered in hospitalized patients.
Hypokalemia and hyperkalemia have been estimated to occur in about 21% and 3% of hospitalized patients,
respectively; though the morbidity and mortality associated with the latter is significantly higher. Potassium is a
predominantly intracellular ion and the understanding of its dynamics between intra- and extracellular fluid milieus,
along with its handling by the kidneys, is important in the diagnosis and treatment of potassium disorders. This
article aims to provide a clinically relevant update on management of potassium disorders for internists. ©
INTRODUCTION leading to death. The ECF acts as an intermediary between
the intracellular stores and the input/output mechanisms.
P otassium is the main intracellular ion in the body
and its levels are crucial to normal homeostasis. It is mainly
contained within the intracellular fluid (ICF) compartment,
Potassium excretion matches the dietary intake, in the
absence of disease, and is executed predominantly by
the kidney, with about a 10% contribution from the large
with only about 2% of the total body potassium residing
intestine.
in the extracellular fluid (ECF).1 Nearly 80% of the cellular
stores are present in muscle, with erythrocytes, liver Potassium transfer between the extra- and intracellular
and bone accounting for most of the remainder1 (Fig. 1). milieus is affected by a variety of other endogenous and
The normal ratio between extracellular and intracellular exogenous factors (Fig. 1). Cellular potassium uptake is
concentrations is important for maintenance of the resting promoted by catecholamines and drugs activating β 2
membrane potential and neuromuscular functioning. adrenoceptors, and inhibited by α-antagonist drugs.
Also, intracellularly, potassium participates in several vital States of acidosis and alkalosis affect potassium because
functions, such as cell growth, maintenance of cell volume, it compensates for the movement of protons (hydrogen
DNA and protein synthesis, enzymatic function and acid- ions). In acidosis, H+ ions move into cells and, to maintain
base balance. Disorders of potassium balance are important electrical balance, K+ ions move out into the ECF; and
causes of ambulatory and in-hospital morbidity. In this vice-versa in alkalosis. A hyperosmolar ECF environment
review, we will discuss the pathophysiology of potassium can promote potassium efflux from the cells leading to
transport, mechanisms and management of potassium depletion of intracellular potassium (and, hence, total body
disorders commonly encountered in clinical practice.
PATHOPHYSIOLOGY
Movement of Potassium Between ICF and ECF
Normal daily potassium intake is approximately 40-100
mEq, which is absorbed from the gut, enters the ECF and
is rapidly redistributed into the intracellular compartment
due to the action of post-prandial insulin. This is essential
because an additional 100 mEq of K+ in plasma would
increase plasma K+ concentration several fold, rapidly
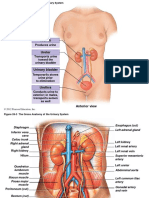
Fig. 1 : Potassium homeostasis: Movement between intra- and
*Research Associate, Joshi Clinic, **Endocrinologist, Lilavati Hospital, extracellular fluids.
Bhatia Hospital and Joshi Clinic; Department of Endocrinology, Seth Movement of potassium between the body compartments is controlled
GS Medical College and KEM Hospital; Mumbai. ***Associate Professor, by various internal and external factors. Potassium predominantly
Mayo Clinic, Rochester, Minnesota. resides intracellularly, with only about 2% being present in the
extracellular fluid. RBCs, red blood cells. Data from Giebisch G.1
© JAPI • VOL. 56 • SEPTEMBER 2008 www.japi.org 685
potassium). Finally, because potassium is predominantly Transtubular Potassium Gradient (TTKG)
contained intracellularly, even if 1% of the cellular K+ content The TTKG is a quick laboratory measure that gives
were to be added to the ECF (due to lysis of cells, such as information about renal K+ secretory function.5 The aim is
rhabdomyolysis or hemolysis), it could result in severe to measure the K+ added into the tubular lumen as it passes
hyperkalemia. through the cortical collecting duct (CCD). Assuming that
Potassium Handling in the Nephron the osmolality of the CCD luminal fluid is equal to that of
Potassium handling by the nephron is unique, in that not plasma, a simple ratio of CCD K+ concentration to the plasma
only is it reabsorbed but it is also secreted by the tubule; and K+ concentration will yield the TTKG.
the amount excreted depends on the dietary intake. TTKG = [K+]CCD / [K+]Plasma
Potassium is freely filtered at the glomerulus and However, because it is clinically impractical to obtain
approximately 65% of the filtered load is reabsorbed in CCD fluid, the parameters are derived using urinary
the proximal convoluted tubule (PCT), which is tied to measurements. TTKG is calculated as:
the reabsorption of sodium and water. This takes place [K]Urine /OSM Urine [K]Urine OSMPlasma
isotonically and the K+ concentration of the fluid entering the TTKG = = X
loop of Henle almost equals that of plasma. In the descending [K]Plasma /OSM Plasma [K]Plasma OSMUrine
part of the loop of Henle, the K+ concentration increases
(greater than that accounted for by the reabsorption of Normal TTKG is about 8-9, which may increase up to 11
water) owing to entry of K+ into the lumen, possibly driven if dietary potassium is increased. The TTKG is applied in the
by the high K+ concentration of the medullary collecting appropriate clinical setting to estimate renal K+ secretion.6
ducts.2 In the thick ascending part of the loop of Henle In the setting of hypokalemia, a TTKG greater than 3 implies
(TALH), the Na+/K+/2Cl- cotransporter present on the luminal renal K+ wastage, while in hyperkalemia, a TTKG lower than
border is responsible for reabsorption of potassium. This 7 implies impaired renal K+ secretion.6
is also the site of action of the loop diuretics, including
furosemide. The next segment, the distal convoluted tubule HYPOKALEMIA
(DCT), has been shown to be involved, to a small extent, in Hypokalemia is defined as a plasma K+ concentration
secretion of K+ into the luminal fluid.3 lower than 3.5 mEq/L. 7 It occurs in about 21% of all
The collecting duct (CD) is responsible for nearly all hospitalized patients8 and goes undertreated in nearly a
the K+ secretion into the urine. The principal cells express fourth of all cases.9 Clinically, diuretic use is the commonest
sodium and potassium ion channels on their luminal cause of hypokalemia.10 Manifestations of hypokalemia
surface. Since the electrochemical force for Na+ entry into are consequences of the effects on the muscle resting
cells is much higher than that for K+, sodium reabsorption membrane potential (RMP) and on the acid-base status
predominates, thus creating a negative charge in the (described above under “Pathophysiology”).
lumen. This negative charge attracts K+ into the lumen and In muscles, low plasma K+ leads to a hyperpolarized
also repels chloride, via the paracellular pathway, into the myocyte that tends to be more refractory to excitation. This
peritubular capillaries. Aldosterone increases the activity of causes fatigue, myalgia and weakness, most pronounced in
the luminal Na+ channels, while also enhancing the function the large proximal skeletal muscles, like those of the hip and
of the basolateral Na+/K+/ATPase pump, thus amplifying the thigh. Worsening hypokalemia produces respiratory muscle
entire process. Also, any factor increasing distal Na+ flow, weakness and, eventually, generalized muscle paralysis,
such as diuretic therapy or osmotic agents (e.g. mannitol, including paralytic ileus.
high glucose in uncontrolled diabetes; which prevent In cardiac myocytes, potassium ion conductance is
absorption of solutes due to increased tonicity of luminal directly related to the plasma K+ concentration.11 Hence,
fluid) can lead to greater K+ secretion. hypokalemia reduces K + conductance and leads to a
Finally, the acid-base status of the body and the prolonged repolarization phase of the cardiac action
extracellular K+ affect each other via renal mechanisms. In potential, reflected in the electrocardiogram (ECG) as a
metabolic alkalosis, excess HCO3- is filtered, which leads prolonged QT (or QU) interval. Other ECG changes include
to increased distal HCO 3- delivery and bicarbonaturia. flattening or inversion of the T wave, a prominent U-wave
Since HCO3- is a poorly reabsorbed anion, it makes the (Fig. 2) and ST-segment depression. Patients receiving
luminal charge more negative and draws out K+ from the digitalis treatment are prone to increased toxicity in the
collecting duct epithelium, leading to increased kaliuresis setting of hypokalemia because digitalis and potassium
and hypokalemia. Hypokalemia increases renal tubular inhibit each other’s binding at the Na+/K+/ATPase pump.12
acid (ammonium ion) generation and, for each mole of Causes
acid generated and excreted in urine, one mole of base
There are many disease processes that lead to or include
(HCO3-) is added to blood. Thus, it contributes towards the
hypokalemia (Table 1). Broadly, hypokalemia can be
metabolic alkalosis. In hyperkalemia, the converse occurs
caused by a shift of K+ into the intracellular compartment,
and renal ammoniagenesis is impaired, leading to metabolic
increased loss from the gut or integument, or from
acidosis.4
686 www.japi.org © JAPI • VOL. 56 • SEPTEMBER 2008
Table 1 : Causes of hypokalemia
Redistribution to ICF
Metabolic alkalosis
Insulin
Autonomic causes
Stress, catecholamines
β2-agonists, α-antagonists
Fig. 2 : Electrocardiogram (ECG) showing effects of hypokalemia.
Anabolic states (Vitamin B12 or GM-CSF therapy)
The left panel shows a normal ECG (serum K+ = 4.4 mEq/L), while
Hypokalemic periodic paralysis the right panel shows the ECG in hypokalemia (serum K+ = 3 mEq/L).
Pseudohypokalemia Flattening of the T wave and a prominent U wave are seen in
Extra-renal Losses hypokalemia.
Secretory diarrhea or laxative abuse
Excessive sweating following exercise or ingestion of a carbohydrate-rich
Intestinal neoplasms meal.15 Both these scenarios normally involve intracellular K+
VIPoma uptake; but this process is abnormally increased in HypoKPP.
Villous adenoma & McKittrick-Wheelock syndrome Serum K+ levels are low during the attack. HypoKPP warrants
Renal Losses
K+ replacement despite being a disorder of transcellular
Primary mineralocorticoid excess
Primary hyperaldosteronism (Conn syndrome) K+ shift. Thyrotoxic periodic paralysis (TPP) is a disorder
Cushing syndrome characterized by elevated thyroxine, hypokalemia and
CAH (CYP 11B1 or CYP 17) paralysis that most commonly occurs in patients of East and
Glucocorticoid-remediable hyperaldosteronism Southeast Asian extraction.16 The importance of recognizing
Hyperaldosteronism due to hyperreninemia this condition is that it is self-limited and administration of
Chronic low circulating volume K+ supplementation can result in rebound hyperkalemia in
Renin secreting tumor
nearly half the patients.16
Renovascular and malignant hypertension
Pseudohyperaldosteronism β2-agonists are potent promoters of cellular K+ uptake
Liddle syndrome and, for this reason, they are important in the management
11 β-HSD2 deficiency or antagonism (licorice, Cd++) of hyperkalemia. Recently, a bizarre cause of hypokalemia
Increased distal Na+ delivery was reported in heroin abusers. Clenbuterol (a drug used
Diuretics to treat airway obstruction in horses) was found to be an
Bartter syndromes
adulterant in heroin, and led to hypokalemia, in addition
Gitelman syndrome
Increased distal delivery of non-reabsorbed anions to the autonomic effects (tachycardia, palpitations).17 This
Renal tubular acidosis – Type 2 drug may also be abused by athletes for its propensity to
Ketoacids (DKA), Penicillins increase lean muscle mass and reduce body fat.
Bicarbonaturia from metabolic alkalosis Losses from the skin and gastrointestinal tract, if severe,
Renal Tubular Acidosis – Type 1
can give rise to significant electrolyte depletion, resulting
Miscellaneous
Reduced dietary intake (<40 mEq/day)
in hypokalemia. Infectious secretory diarrheas account for
Barium toxicity, hypomagnesemia the vast majority of these. A pancreatic tumor secreting
Hypothermia vasoactive intestinal polypeptide (VIPoma) is an exceedingly
rare entity, while a villous adenoma only infrequently
ICF, Intracellular fluid; GM-CSF, Granulocyte-Monocyte Colony
Stimulating Factor; VIPoma, tumor secreting Vasoactive Intestinal produces diarrhea sufficient to cause hypokalemia. Rectal
Polypeptide; CAH, Congenital Adrenal Hyperplasia; CYP 11B1, neoplasms (commonly villous adenomas) producing
11 β-hydroxylase; CYP 17, 17 α-hydroxylase; 11 β-HSD2, 11 electrolyte hypersecretion constitute the McKittrick-
β-hydroxysteroid dehydrogenase-2; DKA, Diabetic ketoacidosis
Wheelock syndrome.18
Diseases causing increased renal K+ loss can be grouped
intrinsic renal disease. Dynamics of K+ exchange between as: (1) those resulting from increased mineralocorticoid
ICF and ECF compartments have already been described effect, (2) those producing increased delivery of Na+ to
(Fig.1). To prevent a spuriously low serum K + reading the distal nephron segments, and (3) those producing
(pseudohypokalemia), blood samples should be maintained increased delivery of unabsorbed anions to the distal
at cool ambient temperatures13 and analyzed without much nephron segments. Some specific renal disorders have been
delay to prevent cellular uptake of K+. A similar phenomenon discussed in detail.
also occurs due to K+ uptake by the abnormal white cells Primary mineralocorticoid excess can result from
in myeloproliferative disorders.14 Several unique causes of primary hyperaldosteronism i.e., Conn syndrome (increased
hypokalemia need special mention. production of aldosterone from a benign or malignant adrenal
Hypokalemic periodic paralysis (HypoKPP) is an neoplasm), or from generalized adrenal hyperfunction
autosomal-dominant inherited disorder involving mutations (Cushing syndrome). Increased mineralocorticoid action
of ion channels present on the muscle sarcolemma. Attacks can occur due to mineralocorticoids produced in congenital
of paralysis occur, beginning in adolescence, after rest adrenal hyperplasia. Inborn deficiencies of the 11
© JAPI • VOL. 56 • SEPTEMBER 2008 www.japi.org 687
β-hydroxylase (CYP 11B1) and 17 α-hydroxylase (CYP 17) its backflow into the lumen is also reduced. Since it is
enzymes lead to increased levels of 11-deoxycorticosterone. this luminal positive charge that drives transcellular
Genetically male children with CYP 17 deficiency manifest reabsorption of other cations like Ca++ and Mg++, Bartter
as pseudohermaphroditism (female genitalia), while syndrome is associated with hypocalcemia (hypercalciuria)
females present in later life with primary amenorrhea. Both and hypomagnesemia. This fact is utilized in differentiating
deficiencies have adult-onset forms as well. Bartter syndrome from Gitelman syndrome, of which
Liddle syndrome is a rare autosomal dominant genetic hypocalciuria is a hallmark.28
disorder manifested by a gain-of-function of the epithelial Gitelman syndrome is an autosomal recessive genetic
sodium channel (ENaC) of the principal cell in the defect resulting in dysfunction of Na + absorption by
collecting duct.19 Excessive Na+ is reabsorbed and, as a the thiazide-sensitive Na + /Cl - cotransporter (NCCT )
direct consequence, excessive K+ is secreted – leading to located in the DCT.29 It is characterized by hypokalemia,
hypokalemia. Patients are volume overloaded, leading metabolic alkalosis, hypomagnesemia, and hypocalciuria.30
to hypertension in the setting of a suppressed renin- Hypomagnesemia is considered the hallmark of NCCT
angiotensin-aldosterone (RAA) axis. A loss-of-function dysfunction31 and is thought to occur due to reduced
mutation of the ENaC produces aldosterone resistance, a activity of epithelial Mg++ receptors,32 while hypocalciuria
syndrome exactly the opposite of Liddle syndrome, which occurs due to increased proximal tubular reabsorption of
is discussed later. Ca++.32
Another condition producing a similar picture to Renal tubular acidosis (RTA) is an umbrella term for
that of Liddle syndrome is the syndrome of apparent the common presentation of hyperchloremic metabolic
mineralocorticoid excess. Cortisol secreted by the acidosis with a normal anion gap, caused by a renal tubular
adrenals possesses some mineralocorticoid action but, in dysfunction. There are four types of RTA and all, except type
aldosterone target tissues, the enzyme 11 β-hydroxysteroid 4, produce hypokalemia.
dehydrogenase-2 (11-βHSD2) converts cortisol to a RTA Type 1, also known as distal RTA, is caused by an
non-mineralocorticoid, cortisone. 20 Symptoms of impairment in acidification of urine due to dysfunctional
hyperaldosteronism develop if the activity of this enzyme acid secretion in the collecting ducts. There is also an
is lacking, or in the presence of inhibitors (licorice 21 or associated defect of K+ conservation, the mechanism of
cadmium from tobacco smoke22). which is uncertain. The urinary excretion of ammonium
Glucocorticoid-remediable hyperaldosteronism is a (NH4+) is disproportionately low compared to the blood
genetic condition wherein the gene for 11 β-hydroxylase pH, which produces the characteristic finding of urine pH
(the enzyme upregulated by corticotropin to synthesize greater than 5.5 even in the setting of acidosis,33 aiding
cortisol) contains the correct promoter but carries the in the differentiation from RTA Type 2. Chronic acidosis is
bases for aldosterone synthase in its coding region (chimeric responsible for the renal calculi formed in Type 1 RTA by
gene duplication).23 Hence, aldosterone synthesis occurs two synergistic mechanisms. Acidosis reduces calcium
in the region of the adrenal (zona fasciculata) responsible reabsorption, increasing the Ca++ concentration in tubular
for cortisol secretion. Administration of dexamethasone fluid, while simultaneously enhancing citrate reabsorption,
can diagnose as well as manage this condition, because reducing its concentration.34 Usually, calcium binds citrate
suppression of corticotropin takes away the stimulus for to form a soluble compound but, due to the imbalance in
excessive aldosterone synthesis. this ratio, calcium binds phosphate to produce a 50-times
Bartter syndrome is a group of genetic conditions less soluble compound that precipitates in the alkaline urine
resulting from defective reabsorption of sodium from the to produce renal calculi.
TALH due to a variety of dysfunctional ion-transport proteins. RTA Type 2, also known as proximal RTA, can occur as a
These include the Na+/K+/2Cl- cotransporter (Bartter I),24 the primary condition, with or without features of generalized
apical (luminal) potassium channel (Bartter II)25 and two proximal tubular dysfunction (Fanconi syndrome), or
defects in the basolateral chloride channel responsible for secondary to drugs such as carbonic anhydrase (CA)
potasium-chloride flux through the tubular cell (Bartter III inhibitors. The result is impaired proximal reabsorption
& IV).26 Recently, a milder variant of Bartter syndrome with of HCO3-. Distal sites in the nephron receive more than
hypocalcemia has also been described (Bartter V). 27 All the usual HCO3- load and, since they are not as adept at
the Bartter syndrome genetic defects are inherited in an its reabsorption, the HCO3- is lost. Bicarbonaturia is the
autosomal recessive fashion, except for Bartter syndrome characteristic of this condition. Eventually, the plasma
V, which follows autosomal dominant inheritance. HCO3- drops to a lower level, at which a new equilibrium
Reabsorption of Na + is impaired and the resultant is established and HCO 3 - is no longer lost in urine.
excessive natriuresis has two important implications – there Bicarbonate replacement therapy is difficult because a
is increased distal Na+ flow and the volume depletion causes fractional HCO3- excretion of more than 15% is observed
activation of the RAA axis. Both factors are responsible and HCO3- may be lost before the desired pH normalization
for the excessive K+ excretion, leading to hypokalemia. is achieved.35 Interestingly, the defect in proximal tubular
In the TALH, K+ absorption is reduced and, consequently, function protects these patients from renal calculi and
688 www.japi.org © JAPI • VOL. 56 • SEPTEMBER 2008
nephrocalcinosis because of the normal/increased citrate
in the tubular fluid. In RTA Type 2, relative to Type 1, a large
quantity of HCO3- needs to be replaced (5-15 mmol/kg/day
vs. 1-2 mmol/kg/day). Since alkali replacement itself causes
hypokalemia, the K+ replacement required in RTA Type 2 is
greater than that required in RTA Type 1.
RTA Type 3 is a rare condition caused by a mutation of
the intracellular form of CA (CA-II).36 The deficiency of a
functional CA-II enzyme gives rise to impaired proximal
HCO3- reabsorption as well as impaired distal acid secretion
i.e. features of both RTA types 1 and 2. Other associated
features are osteoporosis, cerebral calcifications and mental
retardation.
Diagnosis
Hypokalemia should be suspected in any patient
presenting with generalized or proximal muscle weakness
or cardiac arrhythmias. History of gastrointestinal losses, Fig. 3 : Algorithm for diagnosis of hypokalemia.
UK, urinary potassium; GI, gastrointestinal; BP, blood pressure; Aldo,
use of any medications (especially diuretics), renal disease aldosterone; CAH, congenital adrenal hyperplasia; HTN, hypertension;
and history of familial conditions should be actively sought. UCl, urinary chloride; RTA, renal tubular acidosis.
Conditions leading to transcellular K+ shift can be excluded
with a good history and physical examination. Laboratory Hence, plasma renin activity should be tested prior to
values for serum and urinary electrolytes, along with the aldosterone. Conditions like Liddle syndrome give a clinical
blood pressure and plasma renin activity (PRA), are the main picture of hyperaldosteronism despite a suppressed RAA
tools in narrowing down the causes of hypokalemia. axis because their pathophysiology mimics aldosterone
The headings listed in Table 1 (see “Renal losses”) each excess at the level of the target tissues.
represent a pathophysiologic mechanism in the process Treatment
causing hypokalemia and each is a distinct endpoint in the Hypokalemia caused due to true potassium deficit
diagnostic pathway (Fig. 3). should be treated with K+ replacement, though if serious
Once transcellular shift has been excluded, the first complications are expected, hypokalemia resulting from
step is to find out if K+ has been lost via renal or extra- transcellular shifts may also be treated similarly.37 Potassium
renal mechanisms. A daily urinary K+ excretion of > 20 chloride or acetate are used depending on coexistent
mEq suggests renal K+ wastage. If a renal cause has been alkalosis or acidosis, respectively.38 Other modalities can be
found, the next factor to ascertain is the aldosterone employed depending on the specific underlying pathologic
status, since that is the main stimulus for K+ loss. One of condition. If acidosis and hypokalemia coexist, the
the reliable clinical manifestations of hyperaldosteronism hypokalemia must be treated before the acidosis because
is hypertension and, hence, the blood pressure (BP) guides alkali administration can further aggravate hypokalemia.
the further diagnostic course. If the BP is low or normal, we The 2005 American Heart Association (AHA) guidelines
can eliminate aldosterone as the cause for hypokalemia. recommend K+ replacement for serum levels below 2.5
The other reasons for increased K+ loss are increased distal mEq/L to avert risk of cardiac arrhythmias.39 Replacement
delivery of Na+ or HCO3-. These causes are looked for using should be carried out gradually, rather than rapidly, unless
serum HCO3- and urinary chloride. Increased distal Na+ flow the patient’s severity so demands. It is difficult to estimate
is the result of impaired Na+ reabsorption due to an inherited the K+ requirement because the ECF concentration does
defect of the transporters (Bartter and Gitelman syndromes) not reflect body stores. Hence, it is important to frequently
or due to their blockade by diuretics. These disorders monitor serum K+ while administering therapy. Response to
secondarily cause metabolic alkalosis, producing elevated treatment improves with co-administration of magnesium
serum HCO3-. Because Cl- is simultaneously reabsorbed with replacement, especially in hypokalemia that is refractory
Na+, the above conditions lead to Cl- loss as well, causing a to therapy. Care must be taken to avoid overcorrection
high daily Cl- excretion. On the other hand, an extra-renal of the deficit, because rebound hyperkalemia is a serious
cause of metabolic alkalosis (like vomiting or nasogastric complication of therapy.
suction) leads to increased serum HCO3- with a resultant
Some authors recommend that replacement should be
increased tubular HCO3-, whose negative charge repels
initiated with oral potassium chloride because a greater
chloride. The Cl- is driven out of the tubular lumen, leading
rise in ECF potassium can be achieved with this route
to low urinary Cl- excretion. In case the serum HCO3- is low,
at the expense of fewer adverse events and parenteral
renal tubular acidosis is diagnosed.
administration should be reserved for patients unable to
Elevated BP implies excess mineralocorticoid action; take enteral doses.40 According to the AHA guidelines,39
however, this may be due to or independent of renin levels.
© JAPI • VOL. 56 • SEPTEMBER 2008 www.japi.org 689
K + replacement should be empiric, with a maximum Primary aldosterone deficiency can result from either
intravenous potassium chloride infusion rate of 10-20 a generalized adrenal cortex failure (Addison’s disease) or
mEq/L, while continuously monitoring the ECG. If K+ is from an inborn enzyme defect such as the 21-hydroxylase
infused via a central line, it should be ensured that the tip (CYP 21A2) deficiency. The CYP 21A2 deficiency, which
of the catheter is not in the right atrium. If cardiac arrest is may present in childhood or adulthood, causes congenital
imminent, a rapid dose of 10 mEq over 5 minutes is required adrenal hyperplasia and presents with virilization and
and may be repeated once. The therapeutic requirement hypotension. Hyporeninemic hypoaldosteronism is a
for such a rapid infusion must be recorded on the patient’s condition commonly seen in association with diabetic
chart. nephropathy and usually occurs in the presence of some
underlying renal pathology causing volume expansion.46
HYPERKALEMIA The volume expansion secondarily causes suppression of
Hyperkalemia is defined as a plasma K+ concentration the RAA axis, eventually manifesting as hyperkalemia.
greater than 5 mEq/L. It occurs in about 3.3% of all Many drugs interact with the RAA axis. Non-steroidal
hospitalized patients,41 most commonly in patients of anti-inflammatory drugs (NSAIDs) cause hyporeninemia by
chronic renal insufficiency,39 and can carry a high rate impairing prostaglandin synthesis in the juxtaglomerular
of mortality.41 As for hypokalemia, the manifestations of apparatus, which are essential for renin release. Additionally,
hyperkalemia also relate to neuromuscular and acid-base hypoaldosteronism can be caused by fluoride toxicity and
effects. Increased ECF K+ concentration forces K+ into the heparin, which act as inhibitors of aldosterone synthesis,
cells through the always-open leaky potassium channels, or by the angiotensin-converting enzyme inhibitors
leading to a slight depolarization. A constant state of (ACEI) or angiotensin-receptor blockers, which antagonize
depolarization affects excitability and, once again, the angiotensin, the main stimulus for aldosterone release from
effect is fatigue and weakness. If severe, respiratory muscle the adrenals.
weakness can be a life-threatening complication. Impaired K + secretion can result from receptor-
In cardiac myocytes, hyperkalemia causes increased antagonism of aldosterone (spironolactone) or from
K+ conductance.11 Since the K+ current is responsible for blockade of the principal cell Na+ channel (ENaC) by drugs
repolarization, the first manifestation of hyperkalemia is like amiloride, triamterene, amantadine and trimethoprim.
a rapid repolarization, reflected on the ECG as a sharp, RTA Type 4, also known as hyperkalemic distal RTA, is
peaked T wave. Increased K+ conductance also makes the usually the consequence of some other underlying renal
RMP more negative, to a level at which Na+ channels start pathology. There is reduced secretion of K +, leading to
getting inactivated.42 Hyperkalemia can also induce an chronic hyperkalemia. And, as discussed earlier (see
atrioventricular nodal block,43 reflected as a prolonged “Pathophysiology”), hyperkalemia impairs NH4+ production
PR interval and a ventricular rhythm with wide QRS in the collecting duct, leading to defective generation of
complexes.42 P wave amplitude decreases, and may not acid for excretion, and metabolic acidosis. Type 4 RTA should
be detectable, due to an ‘electrical paralysis’ of the atria.44 be taken as a descriptive term rather than as a discreet
With increasing severity of hyperkalemia, the widened QRS pathology, because any condition in which the RAA axis
tends to merge with the peaked T wave (Fig. 4), producing is interrupted can potentially produce Type 4 RTA. Lastly,
a characteristic sine wave pattern.45 Eventually, the cardiac pseudohypoaldosteronism is a rare familial condition in
arrhythmia deteriorates into ventricular fibrillation or which there is a defective gene coding for the ENaC.47 This
asystole, leading to death.
Causes
The various causes of hyperkalemia fall into two main
pathophysiologic groups – movement of K+ from the ICF
to the ECF and impaired renal excretion (Table 2). Factors
causing transcellular shift of K+ have already been discussed
(Fig. 1). Renal causes can, again, be either related to a
defective mineralocorticoid action or due to an intrinsic
tubular inability to secrete potassium. Oliguric renal failure
can, by virtue of reduced renal perfusion and glomerular
filtration rate (GFR), cause reduced K+ secretion. Additionally,
the initiating pathologic process may entail catabolism
and metabolic acidosis, both of which would increase
serum K+. Thus, two separate mechanisms are responsible
for hyperkalemia in oliguric renal failure. This may be Fig. 4 : Electrocardiogram (ECG) of a patient with severe hyperkalemia.
compensated by RAA axis activation, but decompensation The ECG shows a wide QRS complex merging with the peaked T wave,
producing a sine-wave pattern. Right axis deviation (I, aVF) can also be
occurs if GFR falls below a critical value of about 10 mL/ appreciated.
min.
690 www.japi.org © JAPI • VOL. 56 • SEPTEMBER 2008
Table 2 : Causes of hyperkalemia
Redistribution to ECF
Metabolic acidosis
Massive cell rupture
Rhabdomyolysis, burns, hemolysis
Tumor lysis syndrome
Hyperosmolarity (e.g. severe hyperglycemia)
Insulin resistance or deficiency
Drugs
β-blocker therapy
Digitalis
Succinylcholine
Hyperkalemic periodic paralysis
Impaired Renal Excretion
Fig. 5 : Algorithm for approach to hyperkalemia.
Oliguric renal failure DKA, diabetic ketoacidosis; GFR, glomerular filtration rate; ACEI,
Primary mineralocorticoid deficiency angiotensin-converting enzyme inhibitors; NSAIDs, nonsteroidal anti-
Addison’s disease inflammatory drugs; CSA, cyclosporine.
Congenital adrenal hyperplasia (CYP 21A2) * low aldosterone
Secondary mineralocorticoid deficiency
Hyporeninemic hypoaldosteronism should be used. For moderate hyperkalemia (6-7 mEq/L),
NSAIDs an intracellular shift of K+ should be achieved using an
ACE Inhibitors or ARBs insulin-glucose drip, sodium bicarbonate and salbutamol.
Heparin and fluoride In severe hyperkalemia (>7 mEq/L with toxic ECG changes),
Impaired K+ secretion the cardiac toxicity needs to be controlled at the earliest to
Renal tubular acidosis – Type 4 prevent the advent of fatal arrhythmias. Calcium chloride (or
Potassium-sparing diuretics
gluconate) can be used as an infusion to achieve membrane
Amantadine, trimethoprim
Aldosterone resistance
stabilization. In addition to calcium, all the modalities
(pseudohypoaldosteronism) mentioned above should be employed to lower serum K+
Miscellaneous levels. In refractory cases, hemodialysis may be used as a
Pseudohyperkalemia last resort of treatment.
Exercise-induced hyperkalemia (self-limiting)
In summary, disorders of potassium metabolism
ECF, Extracellular fluid; CYP 21A2, 21-hydroxylase; ACE, Angiotensin are commonly encountered in clinical practice. Taking
converting enzyme; ARBs, Angiotensin receptor blockers; NSAIDs, Non-
an excellent clinical history, along with a thorough
steroidal antiinflammatory drugs
understanding of potassium pathophysiology, will help
loss-of-function mutation produces aldosterone resistance the clinician to make an accurate diagnosis and initiate
and, in spite of elevated aldosterone levels, the kidneys appropriate treatment. Additionally, anticipating potassium
continue to lose Na+ and retain K+. disorders in patients receiving medications like diuretics
(hypokalemia) or ACEI (hyperkalemia), especially in patient
Diagnosis
with co-morbid illness and chronic kidney disease, will help
The initial presentation of hyperkalemia can be in ensuring patient safety and optimizing patient care.
paralysis, cardiac arrhythmias or ileus. 48 History of
diabetes, medications and any familial disorders should REFERENCES
be sought. Laboratory values of serum electrolytes, 1. Giebisch G. Renal potassium transport: mechanisms and regulation.
osmolality, blood urea nitrogen (BUN) and creatinine, Am J Physiol Renal Physiol 1998;274:F817-33.
along with urine electrolytes should be obtained. The 2. Jamison RL, Lacy FB, Pennell JP, Sanjana VM. Potassium secretion by
diagnostic approach to hyperkalemia is detailed in the descending limb or pars recta of the juxtamedullary nephron in
vivo. Kidney Int 1976;9:323-32.
Fig. 5.
3. Velázquez H, Ellison DH, Wright FS. Chloride-dependent potassium
Treatment secretion in early and late renal distal tubules. Am J Physiol Renal
Treatment of hyperkalemia involves three major steps: Physiol 1987;253:F555-62
(1) to reverse the cardiac effects, (2) to promote intracellular 4. DuBose TD Jr, Good DW. Chronic hyperkalemia impairs ammonium
transport and accumulation in the inner medulla of the rat. J Clin
uptake, and (3) to remove excess potassium from the body. Invest 1992;90:1443-49.
Later, on subsidence of the acute event, patients need to 5. West ML, Marsden PA, Richardson RM, Zettle RM, Halperin ML. New
be put on a maintenance regimen to prevent episodes of clinical approach to evaluate disorders of potassium excretion. Miner
hyperkalemia. Various treatment modalities and dosages Electrolyte Metab 1986;12:234-8.
are summarized in Table 3.39,48,49 6. Ethier JH, Kamel KS, Magner PO, Lemann J Jr, Halperin ML. The
transtubular potassium concentration in patients with hypokalemia
According to the 2005 AHA guidelines,39 management and hyperkalemia. Am J Kidney Dis 1990;15:309-15.
should be guided by the serum K+ level. In mild hyperkalemia
7. Gennari FJ. Hypokalemia. N Engl J Med 1998;339:451-58.
(5-6 mEq/L), furosemide and sodium polystyrene sulfonate
8. Paice BJ, Paterson KR, Onyanga-Omara F, Donnelly T, Gray JM, Lawson
© JAPI • VOL. 56 • SEPTEMBER 2008 www.japi.org 691
Table 3 : Treatment of hyperkalemia
Therapeutic target Dose and route Onset Duration Comments
and medications of action
Membrane effects
Calcium chloride 5-10 mL of 10% solution Immediate 30 min. Can worsen digitalis toxicity. Monitor
or gluconate IV over 2-5 min. ECG, stop if bradycardia develops.
Intracellular shift of K+
Insulin-glucose drip 10 Units Regular insulin IV 15-30 min. 2-6 h. Glucose unnecessary if
with 50 mL of 50% glucose blood sugar > 250 mg/dl
Salbutamol 2-4 ml of 5 mg/ml salbutamol 15-30 min. 2-3 h. Synergistic with insulin. May cause
by neubulizer over 15 min. a brief rise in plasma K+.
Sodium bicarbonate 50 mEq IV over 5 min. 15-30 min. 1-2 h. Should be used along with insulin
and salbutamol; may be less
effective in ESRD
Removal of excess K+
Furosemide 40-80 mg furosemide IV, with 15-60 min. 4 h. Causes kaliuresis. Only effective if
saline if coexistent adequate renal response to loop diuretics.
valume depletion
Sodium polystyrene 15-30 g in 50-100 mL of 20% 1-2 h. 4-6 h. Sorbitol may be associated with bowel
sulfonate sorbitol, either orally or as a necrosis. May lead to Na+ retention.
retention enema Rectal route acts faster.
Hemodialysis 15-30 min. Avoid ultrafiltration in the first hour
of dialysis
Long-term maintenance therapy
Restriction of K+ intake to < 2-3 g/day
Discontinuation of drugs interfering with K+ homeostasis
Enhanced K+ excretion: furosemide, thiazides
Fludrocortisone (in hypoaldosteronism)
Long-term sodium polystyrene sulfonate therapy
IV, Intravenously; ESRD, End-stage renal disease. Data from: Hollander-Rodriguez JC et al. (48), American Heart Association 2005 Guidelines (39) and
Gennari FJ (49).
DH. Record linkage study of hypokalaemia in hospitalized patients. 20. Hammer F, Stewart PM. Cortisol metabolism in hypertension. Best
Postgrad Med J 1986;62:187-91. Pract Res Clin Endocrinol Metab 2006;20:337-53.
9. Paltiel O, Salakhov E, Ronen I, Berg D, Israeli A. Management of severe 21. van Uum SH, Lenders JW, Hermus AR. Cortisol, 11beta-hydroxysteroid
hypokalemia in hospitalized patients: a study of quality of care based dehydrogenases, and hypertension. Semin Vasc Med 2004;4:121-
on computerized databases. Arch Intern Med 2001;161:1089-95. 28.
10. Knochel JP. Diuretic-induced hypokalemia. Am J Med 1984;77:18- 22. Yang K, Julan L, Rubio F, Sharma A, Guan H. Cadmium reduces 11
27. beta-hydroxysteroid dehydrogenase type 2 activity and expression
11. Sakmann B, Trube G. Conductance properties of single inwardly in human placental trophoblast cells. Am J Physiol Endocrinol Metab
rectifying potassium channels in ventricular cells from guinea-pig 2006;290:E135-42.
heart. J Physiol 1984;347:641-57. 23. McMahon GT, Dluhy RG. Glucocorticoid-remediable aldosteronism.
12. Middleton DA, Rankin S, Esmann M, Watts A. Structural insights into Arq Bras Endocrinol Metabol 2004;48:682-86.
the binding of cardiac glycosides to the digitalis receptor revealed 24. Simon DB, Karet FE, Hamdan JM, DiPietro A, Sanjad SA, Lifton RP.
by solid-state NMR. Proc Natl Acad Sci U S A 2000;97:13602-07. Bartter’s syndrome, hypokalaemic alkalosis with hypercalciuria, is
13. Masters PW, Lawson N, Marenah CB, Maile LJ. High ambient caused by mutations in the Na-K-2Cl cotransporter NKCC2. Nat Genet
temperature: a spurious cause of hypokalaemia. BMJ 1996;312:1652- 1996;13:183-88.
53. 25. Simon DB, Karet FE, Rodriguez-Soriano J, Hamdan JH, DiPietro A,
14. Naparstek Y, Gutman A. Case report: spurious hypokalemia Trachtman H, et al. Genetic heterogeneity of Bartter’s syndrome
in myeloproliferative disorders. Am J Med Sci 1984;288: revealed by mutations in the K+ channel, ROMK. Nat Genet
175-7. 1996;14:152-56.
15. Levitt JO. Practical aspects in the management of hypokalemic 26. Simon DB, Bindra RS, Mansfield TA, Nelson-Williams C, Mendonca E,
periodic paralysis. J Transl Med 2008;6:18. Stone R, et al. Mutations in the chloride channel gene, CLCNKB, cause
Bartter’s syndrome type III. Nat Genet 1997;17:171-78.
16. Manoukian MA, Foote JA, Crapo LM. Clinical and metabolic features
of thyrotoxic periodic paralysis in 24 episodes. Arch Intern Med 27. Vezzoli G, Arcidiacono T, Paloschi V, Terranegra A, Biasion R, Weber
1999;159:601-06. G, et al. Autosomal dominant hypocalcemia with mild type 5 Bartter
syndrome. J Nephrol 2006;19:525-28.
17. Centers for Disease Control and Prevention (CDC). Atypical reactions
associated with heroin use—five states, January-April 2005. MMWR 28. Bettinelli A, Bianchetti MG, Girardin E, Caringella A, Cecconi M, Appiani
Morb Mortal Wkly Rep 2005;54:793-96. AC, et al. Use of calcium excretion values to distinguish two forms of
primary renal tubular hypokalemic alkalosis: Bartter and Gitelman
18. Popescu A, Orban-Schiopu AM, Becheanu G, Diculescu M. McKittrick- syndromes. J Pediatr 1992;120:38-43.
Wheelock syndrome - a rare cause of acute renal failure. Rom J
Gastroenterol 2005;14:63-66. 29. Simon DB, Nelson-Williams C, Bia MJ, Ellison D, Karet FE, Molina AM,
et al. Gitelman’s variant of Bartter’s syndrome, inherited hypokalaemic
19. Warnock DG. Liddle syndrome: genetics and mechanisms of Na+ alkalosis, is caused by mutations in the thiazide-sensitive Na-Cl
channel defects. Am J Med Sci 2001;322:302-07. cotransporter. Nat Genet 1996;12:24-30.
692 www.japi.org © JAPI • VOL. 56 • SEPTEMBER 2008
30. Gitelman HI, Graham JB, Welt LG. A new familial disorder characterized Physician 2006;73:283-90.
by hypokalemia and hypomagnesemia. Trans Assoc Am Phys 49. G e n n a r i FJ . D i s o r d e r s o f p o t a s s i u m h o m e o s t a s i s .
1966;79:221-23. Hypokalemia and hyperkalemia. Crit Care Clin 2002;18:
31. Fukuyama S, Hiramatsu M, Akagi M, Higa M, Ohta T. Novel mutations 273-88.
of the chloride channel Kb gene in two Japanese patients clinically
diagnosed as Bartter syndrome with hypocalciuria. J Clin Endocrinol
Metab 2004;89:5847-50.
32. Nijenhuis T, Vallon V, van der Kemp AW, Loffing J, Hoenderop JG,
Bindels RJ. Enhanced passive Ca2+ reabsorption and reduced Mg2+
channel abundance explains thiazide-induced hypocalciuria and
hypomagnesemia. J Clin Invest 2005;115:1651-58.
33. Halperin ML, Richarson RMA, Bear RA, Magner PO, Kamel K, Ethier
J. Urine ammonium: the key to the diagnosis of distal renal tubular
acidosis. Nephron 1988;50:1-4.
34. Buckalew VM Jr. Nephrolithiasis in renal tubular acidosis. J Urol
1989;141(3 Pt 2):731-37.
35. Ring T, Frische S, Nielsen S. Clinical review: Renal tubular
acidosis—a physicochemical approach. Crit Care 2005;9:
573-80.
36. Shah GN, Bonapace G, Hu PY, Strisciuglio P, Sly WS. Carbonic
anhydrase II deficiency syndrome (osteopetrosis with renal tubular
acidosis and brain calcification): novel mutations in CA2 identified by
direct sequencing expand the opportunity for genotype-phenotype
correlation. Hum Mutat 2004;24:272.
37. Kim HJ, Han SW. Therapeutic approach to hyperkalemia. Nephron
2002;92(suppl 1):33-40.
38. Glover P. Hypokalaemia. Crit Care Resusc 1999;1:239-51.
39. 2005 American Heart Association Guidelines for Cardiopulmonary
Resuscitation and Emergency Cardiovascular Care. Part 10.1: Life-
Threatening Electrolyte Abnormalities. Circulation 2005;112:IV-121-
IV-125.
40. Mount DB, Zandi-Nejad K. Disorders of Potassium Balance. In: Brenner
BM, Rector FC, Livine SA, editors: The Kidney. 7th ed. Philadelphia: WB
Saunders; 2002. p. 1015.
41. Stevens MS, Dunlay RW. Hyperkalemia in hospitalized patients. Int
Urol Nephrol 2000;32:177-80.
42. Mirvis DM, Goldberger AL. Electrocardiography. In: Braunwald E,
Zipes DP, Libby P, editors: Heart Disease: A Textbook of Cardiovascular
Medicine. 6th ed. Philadelphia: WB Saunders; 2001.
43. Ohmae M, Rabkin SW. Hyperkalemia-induced bundle branch block
and complete heart block. Clin Cardiol 1981;4:43-6.
44. Spodick DH. Effects of severe hyperkalemia. Am Heart Hosp
2008;6:68.
45. M a t t u A , B r a d y WJ, Pe r ro n A D. E l e c t ro c a rd i o g r a p h i c
manifestations of hypothermia. Am J Emerg Med 2000;18:
721-29.
46. Oh MS, Carroll HJ, Clemmons JE, Vagnucci AH, Levison SP, Whang ES.
A mechanism for hyporeninemic hypoaldosteronism in chronic renal
disease. Metabolism 1974;23:1157-66.
47. Chang SS, Grunder S, Hanukoglu A, Rösler A, Mathew PM, Hanukoglu
I, et al. Mutations in subunits of the epithelial sodium channel cause
salt wasting with hyperkalaemic acidosis, pseudohypoaldosteronism
type 1. Nat Genet 1996;12:248-53.
48. Hollander-Rodriguez JC, Calvert JF Jr. Hyperkalemia. Am Fam
© JAPI • VOL. 56 • SEPTEMBER 2008 www.japi.org 693
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- 100 General Knowledge Quiz Questions For Entrance ExamsDocument331 pages100 General Knowledge Quiz Questions For Entrance ExamsRamachandran Ram86% (69)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Physiological Regulation of Arterial Blood PressureDocument36 pagesPhysiological Regulation of Arterial Blood PressureFrancesNo ratings yet
- Physiology Question Bank FinalDocument16 pagesPhysiology Question Bank Finalatefmabood100% (2)
- Urinary System Slides Lab 8Document17 pagesUrinary System Slides Lab 8Asad Javed Mehmood100% (1)
- Test Bank Radiographic Pathology For Technologists 8th Edition KowalczykDocument51 pagesTest Bank Radiographic Pathology For Technologists 8th Edition Kowalczykmarcuskenyatta275No ratings yet
- Geochelone Pardalis) : Influence of The Calcium Content of The Diet Offered To Leopard Tortoises (Document5 pagesGeochelone Pardalis) : Influence of The Calcium Content of The Diet Offered To Leopard Tortoises (pzowtNo ratings yet
- Renal and Genitourinary ConditionsDocument139 pagesRenal and Genitourinary ConditionsjustinahorroNo ratings yet
- Frog Dissection HomeworkDocument4 pagesFrog Dissection Homeworkaibiaysif100% (1)
- POTS - Veterinary Anatomy SpecimensDocument92 pagesPOTS - Veterinary Anatomy Specimenssimonsaint100% (1)
- A.S.P.E.N. Clinical Guidelines: Nutrition Support in Adult Acute and Chronic Renal FailureDocument12 pagesA.S.P.E.N. Clinical Guidelines: Nutrition Support in Adult Acute and Chronic Renal FailureCarlos RaiolNo ratings yet
- Chronic Kidney Disease: For The Primary Care PhysicianDocument54 pagesChronic Kidney Disease: For The Primary Care PhysicianFlavia PolodeanuNo ratings yet
- Pa Tho Physiology of GlomerulonephritisDocument1 pagePa Tho Physiology of GlomerulonephritisJhaziel BermejoNo ratings yet
- NEET-SS UrologyDocument59 pagesNEET-SS Urologyadi100% (1)
- Exam Questions AnswersDocument785 pagesExam Questions AnswersLetlet Basabe100% (1)
- PEX-09-01 GGGDocument4 pagesPEX-09-01 GGGDjalika.zNo ratings yet
- Cases in Nephrology by Muhammad Rafiqul AlamDocument9 pagesCases in Nephrology by Muhammad Rafiqul AlamSELLULARNo ratings yet
- Medical Terminology 2Document20 pagesMedical Terminology 2khererer11No ratings yet
- Renal Ultrasound BMUS Study Day: Rosie ConlonDocument72 pagesRenal Ultrasound BMUS Study Day: Rosie ConlonlllorellleiNo ratings yet
- The Animal Organ System - Lesson OutlineDocument5 pagesThe Animal Organ System - Lesson OutlineMa. Cristina UyNo ratings yet
- Sample Questions PNLEDocument12 pagesSample Questions PNLEErika NicaNo ratings yet
- WorksheetsDocument26 pagesWorksheetsw3wzzzNo ratings yet
- Chapter 1: Geriatric Nephrology Has Come of Age: at LastDocument203 pagesChapter 1: Geriatric Nephrology Has Come of Age: at Lastkhangha.ptNo ratings yet
- Keseimbangan Keseimbangan Cairan Cairan Dan Dan Elektrolit ElektrolitDocument6 pagesKeseimbangan Keseimbangan Cairan Cairan Dan Dan Elektrolit Elektrolitbambang ariyantoNo ratings yet
- M 4Document7 pagesM 4Aijem RyanNo ratings yet
- Edexcel IGCSE Checklist Biology 9 1Document17 pagesEdexcel IGCSE Checklist Biology 9 1rehan.akaayubNo ratings yet
- Case Presentation: Patient Chart - Mary JohnsonDocument12 pagesCase Presentation: Patient Chart - Mary Johnsonivoneeh_16100% (1)
- (03241750 - Acta Medica Bulgarica) Horseshoe Kidney With Hydronephrosis - Tales of The UnexpectedDocument3 pages(03241750 - Acta Medica Bulgarica) Horseshoe Kidney With Hydronephrosis - Tales of The UnexpectedTeodorNo ratings yet
- MCQDocument40 pagesMCQLuthie Singh100% (2)
- Renal Doppler Protocol 14 PDFDocument3 pagesRenal Doppler Protocol 14 PDFapi-390240132No ratings yet
- D PharmDocument14 pagesD PharmvikasmaeNo ratings yet