Professional Documents
Culture Documents
List Down Interventions/strategies For Fall Prevention.: Nelec: Unit Task 13 - Musculoskeletal System
List Down Interventions/strategies For Fall Prevention.: Nelec: Unit Task 13 - Musculoskeletal System
Uploaded by
Adrian SantosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
List Down Interventions/strategies For Fall Prevention.: Nelec: Unit Task 13 - Musculoskeletal System
List Down Interventions/strategies For Fall Prevention.: Nelec: Unit Task 13 - Musculoskeletal System
Uploaded by
Adrian SantosCopyright:
Available Formats
NELEC : UNIT TASK 13– MUSCULOSKELETAL SYSTEM
1. List down interventions/strategies for Fall Prevention.
1. Make an appointment with your doctor
Begin your fall- prevention plan by making an appointment with your
doctor. Be prepared to answer questions such as:
What medications are you taking? Make a list of your prescription and
over-the-counter medications and supplements, or bring them with you
to the appointment. Your doctor can review your medications for side
effects and interactions that may increase your risk of falling. To help
with fall prevention, your doctor may consider weaning you off
medications that make you tired or affect your thinking, such as
sedatives and some types of antidepressants.
Have you fallen before? Write down the details, including when, where
and how you fell. Be prepared to discuss instances when you almost
fell but were caught by someone or managed to grab hold of
something just in time. Details such as these may help your doctor
identify specific fall- prevention strategies.
Could your health conditions cause a fall? Certain eye and ear
disorders may increase your risk of falls. Be prepared to discuss your
health conditions and how comfortable you are when you walk — for
example, do you feel any dizziness, joint pain, shortness of breath, or
numbness in your feet and legs when you walk? Your doctor may
evaluate your muscle strength, balance and walking style (gait) as
well.
2. Keep moving
Physical activity can go a long way toward fall prevention. With your
doctor's OK, consider activities such as walking, water workouts or tai
chi — a gentle exercise that involves slow and graceful dance-like
movements. Such activities reduce the risk of falls by improving
strength, balance, coordination and flexibility.
If you avoid physical activity because you're afraid it will make a fall
more likely, tell your doctor. He or she may recommend carefully
monitored exercise programs or refer you to a physical therapist. The
physical therapist can create a custom exercise program aimed at
improving your balance, flexibility, muscle strength and gait.
3. Wear sensible shoes
Consider changing your footwear as part of your fall-prevention plan.
High heels, floppy slippers and shoes with slick soles can make you
slip, stumble and fall. So can walking in your stocking feet. Instead,
wear properly fitting, sturdy shoes with nonskid soles. Sensible shoes
may also reduce joint pain.
4. Remove home hazards
Take a look around your home. Your living room, kitchen, bedroom,
bathroom, hallways and stairways may be filled with hazards. To make
your home safer:
Remove boxes, newspapers, electrical cords and phone cords from
walkways.
Move coffee tables, magazine racks and plant stands from high- traffic
areas.
Secure loose rugs with double- faced tape, tacks or a slip- resistant
backing — or remove loose rugs from your home.
Repair loose, wooden floorboards and carpeting right away.
Store clothing, dishes, food and other necessities within easy reach.
Immediately clean spilled liquids, grease or food.
Use nonslip mats in your bathtub or shower. Use a bath seat, which
allows you to sit while showering.
5. Light up your living space
Keep your home brightly lit to avoid tripping on objects that are hard to
see. Also:
Place night lights in your bedroom, bathroom and hallways.
Place a lamp within reach of your bed for middle- of-the-night needs.
Make clear paths to light switches that aren't near room entrances.
Consider trading traditional switches for glow- in-the-dark or
illuminated switches.
Turn on the lights before going up or down stairs.
Store flashlights in easy-to-find places in case of power outages.
6. Use assistive devices
Your doctor might recommend using a cane or walker to keep you
steady. Other assistive devices can help, too. For example:
Hand rails for both sides of stairways
Nonslip treads for bare-wood steps
A raised toilet seat or one with armrests
Grab bars for the shower or tub
A sturdy plastic seat for the shower or tub — plus a hand- held shower
nozzle for bathing while sitting down
2. What are the effects of aging on musculoskeletal function?
Muscles may become rigid with age and may lose tone, even
with regular exercise. Bones become more brittle and may break
more easily. Overall height decreases, mainly because the trunk
and spine shorten. Breakdown of the joints may lead to
inflammation, pain, stiffness, and deformity.
3. Management for the following problems in musculoskeletal system.
a. Osteoporosis- Treatments for established osteoporosis may
include exercise, vitamin and mineral supplements, and medications.
Exercise and supplementation are often suggested to help you prevent
osteoporosis. Weight-bearing, resistance and balance exercises are all
important
b. Rheumatoid Arthritis
Take your pain medication on a schedule and as prescribed.
Use a warm, moist compress to loosen up a stiff joint
Make it a priority every day to relax.
Focus on things you enjoy.
Join a support group.
Exercise. .
Eat a healthy, balanced diet.
Consider talking to a counselor.
c. Gout
Take medicine you have on hand. Start treatment immediately with
over-the-counter ibuprofen (Motrin, Advil) or naproxen (Aleve), but
never take aspirin, which can worsen a flare.
Ice down.
Drink plenty of fluids.
Avoid alcohol.
Get a cane.
Elevate your foot, if affected.
Create gout-friendly socks.
Chill out.
d. Osteoarthritis
Medications (topical pain medicines and oral analgesics including
nonsteroidal anti-inflammatory medications, NSAIDs). Exercise (land- and
water-based). Intermittent hot and cold packs (local modalities). Physical,
occupational, and exercise therapy.
You might also like
- Caregiver ActivitiesDocument8 pagesCaregiver Activitiesrichelle joy reyesNo ratings yet
- Fall PreventionDocument3 pagesFall PreventionEden Rose RiveraNo ratings yet
- Depression and Anxiety: A Practical Guide on How to Cure Depression and Anxiety Without Resorting to Harmful Meds: Collective Wellness, #3From EverandDepression and Anxiety: A Practical Guide on How to Cure Depression and Anxiety Without Resorting to Harmful Meds: Collective Wellness, #3Rating: 5 out of 5 stars5/5 (10)
- Safety TipsDocument16 pagesSafety TipsAnonymous do9rmemPDNo ratings yet
- Overview of Aging ProcessDocument27 pagesOverview of Aging ProcessJoseph Gedeoni ValenciaNo ratings yet
- Anxiety: 3 Manuscripts - Depression and Anxiety, Negative Thoughts and Cognitive Behavioral TherapyFrom EverandAnxiety: 3 Manuscripts - Depression and Anxiety, Negative Thoughts and Cognitive Behavioral TherapyRating: 5 out of 5 stars5/5 (19)
- How To Improve Immunity and Physical Fitness Through SportsDocument38 pagesHow To Improve Immunity and Physical Fitness Through SportsshahulNo ratings yet
- Occupational Therapy For Rheumatoid ArthritisDocument4 pagesOccupational Therapy For Rheumatoid ArthritisRuxiFuxiNo ratings yet
- STROKE CaseDocument14 pagesSTROKE CaseJM MARQUEZNo ratings yet
- English MR - Asmadi. Name Lec Baru Aku LupeDocument7 pagesEnglish MR - Asmadi. Name Lec Baru Aku LupeEzzah SobliNo ratings yet
- Winter 2017Document4 pagesWinter 2017api-306341773No ratings yet
- Healthy AgingDocument7 pagesHealthy AgingAryaa ArrNo ratings yet
- Pe 1 ModuleDocument55 pagesPe 1 ModuleRaella FernandezNo ratings yet
- Discipline and Ideas in The Applied Social Sciences Quarter 1 - Module 8 Professionals and Practitioners in Communication "I Publish My Practices"Document11 pagesDiscipline and Ideas in The Applied Social Sciences Quarter 1 - Module 8 Professionals and Practitioners in Communication "I Publish My Practices"Frelyn R. StellaNo ratings yet
- 7 Tips On Caregiving For A Bedridden LovedDocument3 pages7 Tips On Caregiving For A Bedridden LovedGee LBNo ratings yet
- Back Pain: Your Guide To Prevention and ReliefDocument11 pagesBack Pain: Your Guide To Prevention and ReliefOana HereaNo ratings yet
- Tobias Medical and Diagnostic CenterDocument36 pagesTobias Medical and Diagnostic CenterAhmed Mohamed ElaminNo ratings yet
- What Is Cancer FatigueDocument7 pagesWhat Is Cancer FatigueBucur ClaudiaNo ratings yet
- Module 1 - Different Sports Activities and Energy SystemsDocument10 pagesModule 1 - Different Sports Activities and Energy SystemsDazefulNo ratings yet
- Late-Stage Care: Providing Care and Comfort During The Late Stage of Alzheimer'S DiseaseDocument12 pagesLate-Stage Care: Providing Care and Comfort During The Late Stage of Alzheimer'S DiseaseマガラノチャールNo ratings yet
- Sports InjuriesDocument4 pagesSports InjuriesM.AhsanNo ratings yet
- 2014 Low Back Pain FULLDocument2 pages2014 Low Back Pain FULLmk78_inNo ratings yet
- Fourteen Home Remedies For Knee PainDocument12 pagesFourteen Home Remedies For Knee PainRatnaPrasadNalamNo ratings yet
- How To Keep Healthy: Estefanía Cruz BarriosDocument2 pagesHow To Keep Healthy: Estefanía Cruz BarriosStephanía CruzNo ratings yet
- Exercise Regularly. in Addition To Having Physical Health: What Is Stress?Document4 pagesExercise Regularly. in Addition To Having Physical Health: What Is Stress?strangerNo ratings yet
- OsteoporosisDocument12 pagesOsteoporosisseries recapNo ratings yet
- What Is Stress?: 1. What Is Stress and Its Causes ? How To Overcome or Reduce Stress?Document12 pagesWhat Is Stress?: 1. What Is Stress and Its Causes ? How To Overcome or Reduce Stress?Gauri SawantNo ratings yet
- EdemaDocument5 pagesEdemaLesther Alba Dela CruzNo ratings yet
- Health of Your Body and Self 7-1Document15 pagesHealth of Your Body and Self 7-1karthikxkarthik365No ratings yet
- Chapter III (EXERCISE)Document11 pagesChapter III (EXERCISE)Michelle B. DelmonteNo ratings yet
- How Much Do You Need To Walk Everyday 3Document3 pagesHow Much Do You Need To Walk Everyday 3Ayesha MuberaNo ratings yet
- Back Pain InfoDocument2 pagesBack Pain Infodrhanmantdhage124No ratings yet
- PE Health 11-Week 1Document14 pagesPE Health 11-Week 1China PandinoNo ratings yet
- ACTIVITY - Reflection (Guarino-BSN 101)Document3 pagesACTIVITY - Reflection (Guarino-BSN 101)Mikhaella GwenckyNo ratings yet
- Anky Losing Fact Sheet 2011Document6 pagesAnky Losing Fact Sheet 2011Irwan Santos ONo ratings yet
- Lifestyle Recommendations For Chronic Fatigue and Pain SyndromesDocument2 pagesLifestyle Recommendations For Chronic Fatigue and Pain SyndromesAndrea Granda ValenciaNo ratings yet
- Back Pain Self-Care ApcDocument2 pagesBack Pain Self-Care ApcmustakNo ratings yet
- Ealth Is The Level of Functional orDocument15 pagesEalth Is The Level of Functional orFifi AnnaNo ratings yet
- Ergonomics For Healthy Living!Document9 pagesErgonomics For Healthy Living!ritu_gupta_4No ratings yet
- Nursing Care of Alzheimer Disease: 1. Balanced NutritionDocument5 pagesNursing Care of Alzheimer Disease: 1. Balanced NutritionKelly Koo Pei YuNo ratings yet
- Walking BenefitsDocument3 pagesWalking BenefitsJoycs PintoNo ratings yet
- TakingCare 2008 MayDocument8 pagesTakingCare 2008 MayAB ShawNo ratings yet
- Reader's Digest Everyday Health Hacks: Quick Fixes to Prevent Disease and Improve Your WellbeingFrom EverandReader's Digest Everyday Health Hacks: Quick Fixes to Prevent Disease and Improve Your WellbeingReader's DigestNo ratings yet
- Creating Healthy Lifestyles Preventing Childhood ObesityDocument76 pagesCreating Healthy Lifestyles Preventing Childhood ObesityHana ZdunićNo ratings yet
- As - PD - LFT - 0288 - Sciatica - A4Document12 pagesAs - PD - LFT - 0288 - Sciatica - A4Shamsuddin HasnaniNo ratings yet
- l7 - Active Living ChoicesDocument7 pagesl7 - Active Living Choicesapi-190085695No ratings yet
- Think Positive and Focus On Gratitude: HappyDocument2 pagesThink Positive and Focus On Gratitude: HappySharmine ChavezNo ratings yet
- Ingles TextoDocument2 pagesIngles TextoLizita Peralta TintayaNo ratings yet
- UntitledDocument37 pagesUntitledVevei JaronNo ratings yet
- Healthy Living FactsDocument12 pagesHealthy Living FactshadonghoonNo ratings yet
- Analysis Physiological IndicatorsDocument8 pagesAnalysis Physiological IndicatorsTatadarz Auxtero Lagria100% (1)
- Monologue: How To Improve Your Health: Speaking Practice Tests English C1Document3 pagesMonologue: How To Improve Your Health: Speaking Practice Tests English C1Zuk V CastilloNo ratings yet
- Reflexology BibleDocument84 pagesReflexology BibleenyaNo ratings yet
- Self-Testing Activities Assignment 3, Module 1Document2 pagesSelf-Testing Activities Assignment 3, Module 1Hazel Jane Mejia100% (1)
- BreastDocument2 pagesBreastAdrian SantosNo ratings yet
- Dialysis CareDocument3 pagesDialysis CareAdrian SantosNo ratings yet
- 3Document3 pages3Adrian SantosNo ratings yet
- Nelec Unit Task 13 MusculoskeletalDocument3 pagesNelec Unit Task 13 MusculoskeletalAdrian SantosNo ratings yet
- Charak Samhita P-2 by Dr. Bhagavan DasDocument610 pagesCharak Samhita P-2 by Dr. Bhagavan DasAnshul SharmaNo ratings yet
- Chapter 1 - The Cardiovascular SystemDocument22 pagesChapter 1 - The Cardiovascular SystemHoa LoNo ratings yet
- I. Objectives: C. Practice Consumer Rights When Buying. (Fit This Objective To Your Activities Presented)Document6 pagesI. Objectives: C. Practice Consumer Rights When Buying. (Fit This Objective To Your Activities Presented)Ralph Mariel Rabino GavinoNo ratings yet
- Heavy Metal Water Pollution-A Case Study: Recent Research in Science and Technology 2013, 5 (5) : 98-99 ISSN: 2076-5061Document2 pagesHeavy Metal Water Pollution-A Case Study: Recent Research in Science and Technology 2013, 5 (5) : 98-99 ISSN: 2076-5061Zari Sofia LevisteNo ratings yet
- Sample To Answer LAMP On SmartPhoneDocument18 pagesSample To Answer LAMP On SmartPhonegvstempNo ratings yet
- CryoprecipitateDocument7 pagesCryoprecipitateBrandon BNo ratings yet
- Introduction To Biopsychology - Andrew WickensDocument5 pagesIntroduction To Biopsychology - Andrew WickensnesywebiNo ratings yet
- Clinical Laboratory Immunology 1st Edition Maahon Tice Test BankDocument8 pagesClinical Laboratory Immunology 1st Edition Maahon Tice Test BankBrian Craig100% (37)
- Top 20 Topics For Inicet: Dr. Zainab Vora MBBS, MD Radiology (Aiims)Document26 pagesTop 20 Topics For Inicet: Dr. Zainab Vora MBBS, MD Radiology (Aiims)The Two Kids MomNo ratings yet
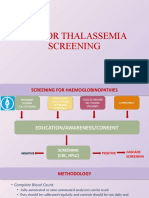
- Sop For Thalassemia Screening Wwith NbsDocument11 pagesSop For Thalassemia Screening Wwith NbsUMMID WashimNo ratings yet
- CHN Rle History of Herbal MedDocument4 pagesCHN Rle History of Herbal MedCarl Josef C. GarciaNo ratings yet
- Interrupted Sutures: Suturing Techniques Simple SuturesDocument5 pagesInterrupted Sutures: Suturing Techniques Simple SuturesMuhammad Ichsan MustariNo ratings yet
- B2 MICROGLOBULINA SiemensDocument31 pagesB2 MICROGLOBULINA SiemensDeborah Gongora100% (1)
- Plant Report Template Class 81Document2 pagesPlant Report Template Class 81Kamran KhanNo ratings yet
- PT1 S12G TendinitisDocument1 pagePT1 S12G TendinitisAdrian AnzanoNo ratings yet
- Rle-Module Final TopicDocument22 pagesRle-Module Final TopicJeonoh FloridaNo ratings yet
- Hinkle PPT CH 01Document23 pagesHinkle PPT CH 01Dennis GallardoNo ratings yet
- Biology Paper 1 November 1999Document30 pagesBiology Paper 1 November 1999k391No ratings yet
- Tips & TricksDocument15 pagesTips & TricksEricNo ratings yet
- Letter To Health MinisterDocument12 pagesLetter To Health Ministerrush999No ratings yet
- Pulmonary Rehabilitation For Cystic FibrosisDocument7 pagesPulmonary Rehabilitation For Cystic FibrosissukiyantoNo ratings yet
- Cell Cycle Pogil AnswersDocument4 pagesCell Cycle Pogil AnswersHaixu Wang100% (1)
- Pregnancy CengizDocument10 pagesPregnancy Cengizkirana_patrolinaNo ratings yet
- A Tale of Twin S TownsDocument4 pagesA Tale of Twin S TownsEunice CameroNo ratings yet
- Epidemiology-Finals ReviewerDocument6 pagesEpidemiology-Finals Reviewereluizamaesipin10No ratings yet
- Autoimmune and Inflammatory Diseases Following COVID-19Document2 pagesAutoimmune and Inflammatory Diseases Following COVID-19ManuelAlbertoBernalCruzNo ratings yet
- BPOC Si SDR MetabolicDocument29 pagesBPOC Si SDR MetabolicMarta DumitracheNo ratings yet
- Classroom Daily Health Monitoring Tool For Covid-19: Symptoms Observed/ReportedDocument2 pagesClassroom Daily Health Monitoring Tool For Covid-19: Symptoms Observed/ReportedJanine Galas DulacaNo ratings yet
- BMLT/BRIT I (First) Year Annual Examination 2015-16Document2 pagesBMLT/BRIT I (First) Year Annual Examination 2015-16Tanveer Abbas JafriNo ratings yet
- Major Causes Hypocalcemia - UpToDate PDFDocument2 pagesMajor Causes Hypocalcemia - UpToDate PDFAnita VásquezNo ratings yet