Professional Documents
Culture Documents
Severe Exacerbations and Inhaled Corticosteroid Load With As-Needed Budesonide/formoterol Vs Maintenance Budesonide in Mild Asthma
Severe Exacerbations and Inhaled Corticosteroid Load With As-Needed Budesonide/formoterol Vs Maintenance Budesonide in Mild Asthma
Uploaded by
Victor Martinez HagenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Severe Exacerbations and Inhaled Corticosteroid Load With As-Needed Budesonide/formoterol Vs Maintenance Budesonide in Mild Asthma
Severe Exacerbations and Inhaled Corticosteroid Load With As-Needed Budesonide/formoterol Vs Maintenance Budesonide in Mild Asthma
Uploaded by
Victor Martinez HagenCopyright:
Available Formats
Severe exacerbations and inhaled corticosteroid load with as-needed budesonide/formoterol vs maintenance budesonide in mild asthma
Eric D. Bateman1, Helen K. Reddel2, Paul M. O’Byrne3, Peter J. Barnes4, Nanshan Zhong5, Christina Keen6, Carin Jorup6, Rosa Lamarca7, Agnieszka Siwek-Posluszna8, and J. Mark FitzGerald9
1
Division of Pulmonology, Department of Medicine, University of Cape Town, South Africa; 2Woolcock Institute of Medical Research, University of Sydney, Australia; 3Firestone Institute for Respiratory Health, St Joseph’s Healthcare and Department of Medicine, Michael G.
DeGroote School of Medicine, McMaster University, Hamilton, Canada; 4Airway Disease Section, National Heart and Lung Institute, Imperial College, London, UK; 5State Key Laboratory of Respiratory Diseases, First Affiliated Hospital, Guangzhou Medical University, China;
6
AstraZeneca R&D, Gothenburg, Sweden; 7AstraZeneca, Barcelona, Spain; 8AstraZeneca, Warsaw, Poland; 9Institute for Heart and Lung Health, University of British Columbia, Vancouver, Canada
• The primary analysis used a negative binomial model that • There were fewer participants with high use of as-needed
Introduction included terms for treatment, pre-study treatment, and region,
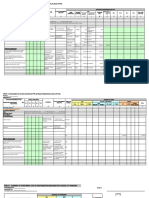
Figure 1. Annualized severe asthma exacerbation rate
(non-inferiority test and superiority test)
Figure 2. Time to first severe exacerbation
Budesonide maintenance (N=2087)
BUD/FORM than as-needed terbutaline: fewer took
and was conducted on the full analysis set population. Non- As-needed BUD/FORM (N=2089) >8 inhalations per day (10.4% vs 15.0%) or >12 inhalations
• Current guidelines recommend that patients with mild 0.10 Number (%) patients with event:
inferiority could be claimed if the upper bound of the 1-sided As-needed BUD/FORM 177 (8.5) per day (4.1% vs 7.4%) at least once.
asthma should be prescribed regular low-dose inhaled Budesonide maintenance 184 (8.8)
95% confidence interval (CI) was less than 1.2.
a severe exacerbation
Probability of having
As-needed Budesonide Rate ratio P value
corticosteroids (ICS) as maintenance medication.1 Test
BUD/FORM maintenance (95% CI)
Hazard ratio (95% CI 2-sided): 0.96 (0.78 to 1.17); p=0.66
Figure 4. Change in ACQ-5 over time
• There was no adjustment for multiplicity testing for
• However, adherence to regular maintenance therapy is
secondary variables. Non-inferiority test 2084 2083 0.97 (NA to 1.16) –
poor,2 and patients tend to rely on and overuse as-needed 0.05 As-needed BUD/FORM (N=2089) Budesonide maintenance (N=2087)
0.2 Change in ACQ-5, from baseline to treatment period average, LS Mean (± 95% CI)
short-acting β2-agonists (SABAs), which do not address
underlying airway inflammation. SABA overuse is associated Results 0.1
As-needed BUD/FORM –0.35
Budesonide maintenance –0.46
Change in ACQ-5 score
Superiority test 2089 2087 0.97 (0.78 to 1.20) 0.75 Treatment difference (95% CI): 0.11 (0.07 to 0.15); p<0.001
with severe exacerbations3 and death.4 0.0
Patients
from baseline
• The SYGMA 2 (SYmbicort Given as needed in Mild Asthma) –0.1
• Of 6634 patients enrolled, 4215 were randomized, and 4176 0.00
study was designed in parallel with SYGMA 1 using a more 0.6 0.8 1.0 1.2 1.4
0 4 8 12 17 20 24 28 34 36 40 44 48 52 –0.2
patients were included in the full analysis set (as-needed Time (weeks)
pragmatic study design, without daily maintenance As-needed BUD/FORM Budesonide maintenance –0.3
BUD/FORM, N=2089; budesonide maintenance, N=2087) (Table 1). better better
medication reminders, to determine whether as-needed Adherence and ICS dose –0.4
budesonide/formoterol (BUD/FORM) is non-inferior to regular Table 1. Baseline demographics and clinical characteristics • Electronically-recorded adherence with blinded maintenance –0.5
budesonide maintenance therapy in preventing severe
As-needed Budesonide • A similar number of patients in both treatment groups had treatment was 63–64% across randomization groups. –0.6
exacerbations in patients with mild asthma. 0 4 8 12 16 20 24 28 32 36 40 44 48 52
BUD/FORM Maintenance Total severe exacerbations requiring emergency department visits or • Median daily ICS dose was 75% lower in the as-needed Time (weeks)
200/6 µg 200 µg BID (N=4176) hospitalizations (Table 2).
(N=2089) (N=2087)
BUD/FORM arm compared with the budesonide maintenance
Methods Age, years, mean (SD) 41.3 (16.8) 40.7 (17.1) 41.0 (17.0) Table 2. Severe asthma exacerbations and exacerbation rate
arm (metered doses 66 µg and 267 µg, respectively). Safety
Lung function and asthma control • One death in each arm, adjudicated as acute asthmatic
• SYGMA 2 was a 52-week, double-blind, randomized, parallel- Female sex, n (%) 1308 (62.6) 1289 (61.8) 2597 (62.2)
As-needed Budesonide exacerbation in the budesonide maintenance arm and
group study (ClinicalTrials.gov identifier: NCT02224157).5 BUD/FORM maintenance • The change in pre-bronchodilator FEV1 from baseline was
200/6 µg 200 µg BID lower with as-needed BUD/FORM compared to budesonide cardiorespiratory arrest in the as-needed BUD/FORM arm.
Time since asthma
• Patients aged ≥12 years with a clinical diagnosis of asthma (N=2089) (N=2087) maintenance (mean difference: -32.6 mL [95% CI -53.7 to
diagnosis, years, 7.9 (0.5 to 62.4) 7.3 (0.4 to 71.2) 7.6 (0.4 to 71.2)
(GINA 2012 criteria6) for ≥6 months, and considered by the
investigator to require GINA Step 2 treatment (regular low-dose
median (range) All severe exacerbations
Patients with at least 177 (8.5) 184 (8.8)
-11.4]) (Figure 3). Conclusions
ICS or LTRA6), were randomized to either twice-daily placebo ACQ-5 score, mean (SD) 1.49 (0.89) 1.53 (0.90) 1.51 (0.90) one exacerbation, n (%) • ACQ-5 score decreased over time for both groups (Figure 4). • In patients with mild asthma, who in this study were
plus as-needed BUD/FORM 200/6 µg (Symbicort® Turbuhaler®, Total number of exacerbations/ 0.11 0.11 moderately adherent with blinded maintenance treatment,
Pre-bronchodilator FEV1, patient-year Figure 3. Change in pre-bronchodilator FEV1 over time as-needed BUD/FORM was associated with a similar
AstraZeneca) or twice-daily budesonide 200 µg (Pulmicort®
% predicted N=2079 N=2075 N=4154 Severe exacerbations requiring
Turbuhaler®, AstraZeneca) plus as-needed terbutaline 0.5 mg Mean (SD) 84.4 (13.9) 84.1 (13.9) 84.3 (13.9)
(non-inferior) rate of severe exacerbations but slightly less
systemic corticosteroid use for symptom control compared to maintenance budesonide.
(budesonide maintenance). at least 3 days
As-needed BUD/FORM (N=2089) Budesonide maintenance (N=2087)
180
Reversibility (%) N=2069 N=2058 N=4127 • This was achieved at 75% less daily ICS dose than
Change in pre-bronchodilator
• Primary objective: to demonstrate non-inferiority of as-needed Patients with at least one 171 (8.2) 173 (8.3)
Mean (SD) 15.1 (12.4) 15.2 (13.0) 15.2 (12.7) 160
FEV1 (mL) from baseline
BUD/FORM to budesonide maintenance for the annualized rate exacerbation, n (%) maintenance budesonide without the need for twice-daily
Total number of exacerbations/ 0.10 0.10 140
of severe exacerbations (worsening asthma leading to systemic Pre-study treatment maintenance dosing.
patient-treatment year 120
corticosteroid treatment for ≥3 days, hospitalization, or subgroup, n (%)
100
emergency department visit leading to systemic Uncontrolled* on BD 959 (45.9) 975 (46.7) 1934 (46.3) Severe exacerbation requiring
Controlled* on ICS 1130 (54.1) 1112 (53.3) 2242 (53.7) emergency department visit and 80 References
corticosteroid treatment). systemic corticosteroids 1. Global Strategy for Asthma Management and Prevention 4. Stanford RH, et al. Ann Allergy Asthma Immunol
or LTRA 60
2018 (http://ginasthma.org/). 2012;109:403-7.
• Secondary objectives included: Patients with at least one 25 (1.2) 36 (1.7) 40
Change in pre-bronchodilator FEV1, from baseline to treatment period average, LS Mean (± 95% CI)
2. Rand C, et al. J Allergy Clin Immunol 2007;119:916-23. 5. O’Byrne PM, et al. Trials 2017;18:12.
As-needed BUD/FORM 104.0 mL
Severe exacerbation in exacerbation, n (%) 20 Budesonide maintenance 136.6 mL
3. Suissa S, et al. J Respir Crit Care Med 1994;149:604-10.
– between-group differences in efficacy assessed as time to first previous 12 months, n (%) Total number of exacerbations/ 0.01 0.02 Treatment difference (95% CI): –32.6 mL (–53.7 to –11.4); p=0.003
0
severe exacerbation; 0 1630 (78.0) 1627 (78.0) 3257 (78.0) patient-treatment year 0 4 8 12 16 20 24 28 32 36 40 44 48 52 Acknowledgments
1 365 (17.5) 362 (17.3) 727 (17.4) Severe exacerbations requiring Time (weeks) We thank the health care providers, research staff, patients, and caregivers who participated in this trial. Sophieanne
– inhaled and systemic corticosteroid use; ≥2 94 (4.5) 98 (4.7) 192 (4.6) hospitalization Wastling of inScience Communications, Springer Healthcare, provided medical writing support, which was funded by
AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
– pre-bronchodilator forced expiratory volume in 1 second *Asthma control on pre-study treatment was physician-assessed. Patients with at least one 17 (0.8) 17 (0.8)
(FEV1); exacerbation, n (%) As-needed medication use Disclosure statement
Exacerbations Total number of exacerbations/ 0.01 0.01 • An average of 0.52 (SD 0.55) inhalations/day of as-needed EDB reports non-financial support from AstraZeneca, and personal fees from AstraZeneca during the conduct of the
study; personal fees from Novartis, Cipla, Vectura, Menarini, ALK, ICON, Sanofi Regeneron, and Boehringer Ingelheim;
– Asthma Control Questionnaire (5-item version; ACQ-5). patient-treatment year BUD/FORM were taken, compared with 0.49 (SD 0.70) and grants to institutions from Novartis, Boehringer Ingelheim, Merck, Takeda, GlaxoSmithKline,
• As-needed BUD/FORM was non-inferior to budesonide Hoffmann-La Roche, Actelion, Chiesi, Sanofi-Aventis, Cephalon, and TEVA, outside of the
• Use of all randomized medications (maintenance and as maintenance for annualized severe asthma exacerbation rate inhalations/day of as-needed terbutaline in the budesonide submitted work; and is a Member of the Global Initiative for Asthma Board and Science
needed) was electronically recorded using Turbuhaler® Usage • There was no difference between the two treatment groups in maintenance group. Patients randomized to as-needed Committee. JMF reports grants and personal fees from AstraZeneca during the conduct of the
(0.11 [95% CI 0.10 to 0.13] and 0.12 [0.10 to 0.14], time to first severe asthma exacerbation (Figure 2).
study; grants to UBC from AstraZeneca, Novartis, Boehringer Ingelheim, GlaxoSmithKline,
Monitors (Adherium). respectively) (Figure 1). BUD/FORM had fewer days with no as-needed use (69.0% Hoffmann-La Roche, Sanofi-Aventis, and TEVA outside the submitted work; personal fees from
Novartis, Sanofi Regeneron, Merck, and Boehringer Ingelheim; and is a Member of the Global
vs 75.9%). Initiative for Asthma Board and Science Committee.
Presented at the ATS International Conference 2018, May 18–23, San Diego, CA, USA
You might also like
- SM JCB 3CX 4CX 328739808-9803-3280-9 PDFDocument1,212 pagesSM JCB 3CX 4CX 328739808-9803-3280-9 PDFСергей Ганкевич97% (31)
- Medication ChartDocument2 pagesMedication Chartmax_21ru100% (1)
- ATS-2023-ePoster D4 16may23 FINALDocument1 pageATS-2023-ePoster D4 16may23 FINAL김현수No ratings yet
- Endo Logbook FormsDocument3 pagesEndo Logbook FormsAmethystVonNo ratings yet
- Recipe Card - TemplateDocument10 pagesRecipe Card - TemplateNiroj AdhikariNo ratings yet
- Classification of Side Effects To Beneficial Organisms: Active IngredientDocument6 pagesClassification of Side Effects To Beneficial Organisms: Active IngredientGaston GarridoNo ratings yet
- SMART Asthma TherapyDocument4 pagesSMART Asthma TherapyKen Won100% (1)
- Appendix 5 Hazmat Inventory SheetDocument1 pageAppendix 5 Hazmat Inventory Sheetaldrb hospitalNo ratings yet
- Fri 394 Ilc2022Document1 pageFri 394 Ilc2022rtthrtfhNo ratings yet
- 6th Annual International Conference On Opioids at Harvard Medical SchoolDocument1 page6th Annual International Conference On Opioids at Harvard Medical Schoolvaluecare1542No ratings yet
- Arts Initial Service Authorization Request Form 06062018 LockedDocument6 pagesArts Initial Service Authorization Request Form 06062018 LockedMistor Dupois WilliamsNo ratings yet
- Thu 348 Ilc2022Document1 pageThu 348 Ilc2022rtthrtfhNo ratings yet
- Bro Van ADocument2 pagesBro Van Asultan_bagadNo ratings yet
- Farmakoterapi Penyakit Paru Obstruksi Kronik (PPOK) : Tinjauan PustakaDocument10 pagesFarmakoterapi Penyakit Paru Obstruksi Kronik (PPOK) : Tinjauan PustakaLilisNo ratings yet
- ICU RehabilitationDocument10 pagesICU RehabilitationKarina Saldivia TecaNo ratings yet
- WHO Model List of Essential Medicines For Children: 2nd List (Updated) March 2010Document36 pagesWHO Model List of Essential Medicines For Children: 2nd List (Updated) March 2010angelitawecNo ratings yet
- Amine Label Nov 2020 - 1332469819Document2 pagesAmine Label Nov 2020 - 1332469819kathygona1980No ratings yet
- AOP Dao 2015 Jan 16, 2015Document63 pagesAOP Dao 2015 Jan 16, 2015geline joyNo ratings yet
- HML - Reporting Templates: List of Material UsedDocument3 pagesHML - Reporting Templates: List of Material UsedALPENGIRLNo ratings yet
- Recipe Card TemplateDocument1 pageRecipe Card TemplateTiago PradoNo ratings yet
- Lung Lab 1Document15 pagesLung Lab 1api-527782385No ratings yet
- Summative Criterion D 2022 3 1Document4 pagesSummative Criterion D 2022 3 1Agus SulfiantoNo ratings yet
- 4 Integrated Incident Severity Matrix Supreme HSE CommiteeDocument1 page4 Integrated Incident Severity Matrix Supreme HSE CommiteeMalik Khuram ShazadNo ratings yet
- Consent TestDocument3 pagesConsent TestMichael EsfahaniNo ratings yet
- BMC Health Services ResearchDocument1 pageBMC Health Services ResearchKris MawantoNo ratings yet
- 2005-2006 Field Guide To Antibiotic Therapy - Kuper AZDocument10 pages2005-2006 Field Guide To Antibiotic Therapy - Kuper AZVeronoasaNo ratings yet
- R&D Hazards Eval Form Ver 3.3Document13 pagesR&D Hazards Eval Form Ver 3.3dleggett5147No ratings yet
- Gems Opt Select Brochure 2021 v6 3Document2 pagesGems Opt Select Brochure 2021 v6 3Bongani West VuthaNo ratings yet
- Asma 101Document43 pagesAsma 101Asfiksia NeonatorumNo ratings yet
- 1667831315mr Chevaugn Witter NHRC 22 p9 pdf1667831315Document1 page1667831315mr Chevaugn Witter NHRC 22 p9 pdf1667831315Kaif AliNo ratings yet
- Prevention & Early Outpatient Treatment Protocol For Covid-19Document4 pagesPrevention & Early Outpatient Treatment Protocol For Covid-19jack mehiffNo ratings yet
- Bbird H NassignmentDocument7 pagesBbird H Nassignmentapi-334644774No ratings yet
- Final HiraDocument39 pagesFinal HiraAnsari HarisNo ratings yet
- ASTHMA - SemisDocument4 pagesASTHMA - SemisInday BertaNo ratings yet
- Haemostasis-Result Sheet-1104Document1 pageHaemostasis-Result Sheet-1104NAKANWAGI JOSLYLINENo ratings yet
- Dubai HSE LAwDocument103 pagesDubai HSE LAwnoufalhse100% (2)
- DKM 377Document2 pagesDKM 377Ngoc NgaNo ratings yet
- Chemistry Risk Assessment UV RadiationDocument3 pagesChemistry Risk Assessment UV RadiationWay to WorldNo ratings yet
- Neo Nic Alternatives NurseriesDocument25 pagesNeo Nic Alternatives Nurseriesdoli simbolonNo ratings yet
- Easy-To-Use Workplace Control Scheme For Hazardous SubstancesDocument1 pageEasy-To-Use Workplace Control Scheme For Hazardous Substancesrahmanshanto623No ratings yet
- SicckKids - PRD - 070 - EFGH - Neyama AlladinDocument1 pageSicckKids - PRD - 070 - EFGH - Neyama AlladinNeyama AlladinNo ratings yet
- CPC Group-3Document1 pageCPC Group-3Jhayber AndradeNo ratings yet
- RECELL Autologous Cell Harvesting Device (RECELL System) Spray-On Skin System For Treating Skin Loss, Scarring and Depigmentation After Burn InjuryDocument1 pageRECELL Autologous Cell Harvesting Device (RECELL System) Spray-On Skin System For Treating Skin Loss, Scarring and Depigmentation After Burn InjuryDaisy Jane KoNo ratings yet
- Lab Values 1Document30 pagesLab Values 1Ezekiel John GarciaNo ratings yet
- Recipe Card SheldonDocument22 pagesRecipe Card SheldonLaone MosweunyaneNo ratings yet
- Screening For Perinatal DepressionDocument3 pagesScreening For Perinatal DepressionZorin SvetlanaNo ratings yet
- Dehydrated Human Amnion Chorion Membrane (dHACM) As Treatment For Pediatric BurnsDocument42 pagesDehydrated Human Amnion Chorion Membrane (dHACM) As Treatment For Pediatric BurnsacanahuateNo ratings yet
- Oral Drug DeliveryDocument13 pagesOral Drug DeliveryHadeelNo ratings yet
- Managing Microbes Poster AIF 00612Document1 pageManaging Microbes Poster AIF 00612Devina Sari PratiwiNo ratings yet
- Bolivar Schedule Aug 4Document1 pageBolivar Schedule Aug 4560107No ratings yet
- Pediatric Liver Transplantation.49Document1 pagePediatric Liver Transplantation.49Raisa Mery Ingunza TapiaNo ratings yet
- Reflection 2 - TranspirationDocument4 pagesReflection 2 - Transpirationfern shirleyNo ratings yet
- Von Willebrand Factor Antigen - 0020002300: Limitations/interfering SubstancesDocument3 pagesVon Willebrand Factor Antigen - 0020002300: Limitations/interfering Substances28850No ratings yet
- AsenapineTransdermalPatchPKPoster CASTELLI NEI2020Document1 pageAsenapineTransdermalPatchPKPoster CASTELLI NEI2020Leslie CitromeNo ratings yet
- American Family Physician Guidelines For AsthmaDocument2 pagesAmerican Family Physician Guidelines For AsthmaEmiliano Salvador EspinozaNo ratings yet
- OHS-PR-09-03-F02 HIRA - 001 Site Survey of Land Rev. 2021Document8 pagesOHS-PR-09-03-F02 HIRA - 001 Site Survey of Land Rev. 2021MuhammadAsimMuneerNo ratings yet
- Pil 8098Document2 pagesPil 8098NE LandlordNo ratings yet
- Cost Effectiveness of Single Inhaler Extrafine Beclometasone Di - 2022 - RespiraDocument8 pagesCost Effectiveness of Single Inhaler Extrafine Beclometasone Di - 2022 - RespiraFernando SarmientoNo ratings yet
- Paper Alumnos 5Document14 pagesPaper Alumnos 5Victor Martinez HagenNo ratings yet
- Paper Alumnos 6Document12 pagesPaper Alumnos 6Victor Martinez HagenNo ratings yet
- Paper Alumnos 3 PDFDocument10 pagesPaper Alumnos 3 PDFVictor Martinez HagenNo ratings yet
- Paper Alumnos 2Document11 pagesPaper Alumnos 2Victor Martinez HagenNo ratings yet
- Prime Factorization of 1400 - Buscar Con Google PDFDocument1 pagePrime Factorization of 1400 - Buscar Con Google PDFVictor Martinez HagenNo ratings yet
- How Should This Medicine Be Used?: Before Taking BudesonideDocument7 pagesHow Should This Medicine Be Used?: Before Taking BudesonideJay RalphNo ratings yet
- Fluticasone Vs BudesonideDocument7 pagesFluticasone Vs Budesonidearie_yuliantoNo ratings yet
- Steroids PDFDocument12 pagesSteroids PDFRahulNo ratings yet
- Aeronid: SSRJVLPHR /JQ K P J/JL FGQDocument1 pageAeronid: SSRJVLPHR /JQ K P J/JL FGQSaifur Rahman SuzonNo ratings yet
- Cost Plus Med ListDocument21 pagesCost Plus Med ListCBS 11 NewsNo ratings yet
- Respiratory Drugs Top 300Document1 pageRespiratory Drugs Top 300Rubina SayedNo ratings yet
- Symbicort Branding Manual PDFDocument79 pagesSymbicort Branding Manual PDFMauricio Gómez100% (1)
- Budesonide Inhalation Drug StudyDocument2 pagesBudesonide Inhalation Drug StudyAijeelene NalapoNo ratings yet
- OBUCORT® Swinghaler® Inhalation Powder Composition 1. CompositionDocument3 pagesOBUCORT® Swinghaler® Inhalation Powder Composition 1. CompositionOka Robi MuhammadNo ratings yet
- DrugsDocument20 pagesDrugsLee Won100% (1)
- Pulmicort Respules (Budesonide Inhalation Suspension) Vs Singulair, Children - Full Text View - ClinicalTrials - GovDocument5 pagesPulmicort Respules (Budesonide Inhalation Suspension) Vs Singulair, Children - Full Text View - ClinicalTrials - GovHanna PurwaningsihNo ratings yet
- ECCO Guideline - IBD 2-2017 PDFDocument16 pagesECCO Guideline - IBD 2-2017 PDFIana CovaliovNo ratings yet
- Budesonide Drug Study COPDDocument2 pagesBudesonide Drug Study COPDNiña Dianne Rubin RustiaNo ratings yet
- SymbicortDocument18 pagesSymbicortkaditasookdeoNo ratings yet
- BudesonideDocument2 pagesBudesonideDiane Bonita HerreraNo ratings yet
- National Pharmaceutical Pricing AuthorityDocument21 pagesNational Pharmaceutical Pricing AuthoritySunil Murkikar (GM - PMI Quality Operations)No ratings yet
- COPD 114554 Comparative Analysis of Budesonide Formoterol and Fluticason 110416Document7 pagesCOPD 114554 Comparative Analysis of Budesonide Formoterol and Fluticason 110416RezaFArthaNo ratings yet
- Inhalers Used in Asthma and COPD PDFDocument1 pageInhalers Used in Asthma and COPD PDFconNo ratings yet
- Nppa Updated Price List As On 01.04.2021Document385 pagesNppa Updated Price List As On 01.04.2021bvs prasadNo ratings yet
- CPT and Nebulizer Preparation Sheet - Student VersionDocument8 pagesCPT and Nebulizer Preparation Sheet - Student Version3mar YasserNo ratings yet
- Drug StudyDocument5 pagesDrug StudyJohn Cyprian AbeloNo ratings yet
- Drug StudyDocument21 pagesDrug StudytyaneoNo ratings yet
- Drug Study MMMCDocument14 pagesDrug Study MMMCKathleen Pagulayan Intalan-GloriosoNo ratings yet
- KYLE OLOR RLE REQS - Docx 1Document14 pagesKYLE OLOR RLE REQS - Docx 1Bernadeth Barrientos ZamoraNo ratings yet
- Market Entry Plan For IndonesiaDocument11 pagesMarket Entry Plan For IndonesiaKiran Manoj100% (2)
- 10.27.08 Isaacs. Treatment of IBDDocument50 pages10.27.08 Isaacs. Treatment of IBDiman naNo ratings yet
- MedicineDocument3 pagesMedicineknhalwarhrNo ratings yet
- S-Bridging The Gap in Asthma Management (In-11244)Document34 pagesS-Bridging The Gap in Asthma Management (In-11244)w5bwmbfrtwNo ratings yet
- Bronchodilators: Uses ActionDocument4 pagesBronchodilators: Uses Actionammar amerNo ratings yet