Professional Documents
Culture Documents
Neuro Aging
Neuro Aging
Uploaded by
psy0 ratings0% found this document useful (0 votes)
5 views1 pageOriginal Title
Neuro_Aging.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views1 pageNeuro Aging
Neuro Aging
Uploaded by
psyCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 1
Describe expected and uncommon physical changes associated with the aging neuro system.
How do
these impact the patient?
Physiologic Changes Implications
More permeable blood-brain barrier There will be an increased medication and toxin sensitivity
Less neurons and nerve fibers Changes in pain sensation and not as able to localize pain
Reaction time is slower and lower limbs There is an increased risk of falls and accidents.
have decreased proprioception Encourage patient to wear sensible shoes and look where
at feet when walking.
Change patient position at least every 2 hours if unable to
move.
Neurotransmitter system decrease Slower processing speed
(receptors, enzymes, neurotransmitter) Older adults need time to respond to directions and/or
questions. This time for processing will differentiate
normal form neurologic deterioration.
Possible memory changes or loss White matter in frontal lobe has the greatest loss.
Intellect not impaired but there is a slow learning process.
Memory loss in older adults needs reinforced teaching and
repetition.
Perception of pain change; possible loss May lead to falls or accidents.
of vibration sense (ankles or feet) Ask patient about quality and characteristic of pain.
Decrease in pupil size. Amount of light entering eye is restricted and vision
adaption is slow.
Make sure patient has safe environment to avoid falls and
injury
Sleep pattern changes (reduced sleep, Older adults need less sleep.
daytime naps, circadian rhythm changes) Assess sleep habits and bedtime routines.
Calming, relaxing environment with noise reduction could
help older adults have better sleep.
Decreased coordination and balance Coordination and reflex decrease in older adults.
alteration Can cause falls if patient moves too quickly.
Older adults would need ambulatory aids and adaptive aids
for support.
Risk for infection There is a structural deterioration of microglia (responsible
for cell-mediated response of CNS)
Older adult patients need to be periodically monitored for
infection and also there is a need to stop infection from
happening.
Real life scenario:
Most patients I have seen in the hospital are older adults and they come in with all kinds of
disorders or illness. Especially in the SNF, I noticed older adults have most of the physiologic changes
mentioned above. For example, they have decreased need for sleep and are usually up very early in the
morning. They have a slower pain reception even when you would expect them in so much pain after
surgery or experiencing chronic illness. They have unsteady gait and have an increased risk for falls.
Short term memory loss is also common, as well as an increased risk for infection.
You might also like
- Neurological DisorderDocument10 pagesNeurological DisordersonyNo ratings yet
- Scrib AssignmentDocument9 pagesScrib AssignmentShayne Jessemae AlmarioNo ratings yet
- Multiple Sclerosis: Saadia Perwaiz, PT BSPT, M. Phil-MskDocument39 pagesMultiple Sclerosis: Saadia Perwaiz, PT BSPT, M. Phil-MskArslan Aslam100% (2)
- Assessment of Neurologic Function: Dr. Lubna DwerijDocument41 pagesAssessment of Neurologic Function: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Sleep Physiology and Disorders in Aging and DementiaDocument17 pagesSleep Physiology and Disorders in Aging and DementiaJúlio EmanoelNo ratings yet
- DRUG STUDY CefuroximeDocument2 pagesDRUG STUDY CefuroximeLyana Stark92% (39)
- Narcolepsy, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandNarcolepsy, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (2)
- Theories of AgingDocument2 pagesTheories of AgingJeremiah JustoNo ratings yet
- Intestinal ObstructionDocument52 pagesIntestinal ObstructionAsfandyar Khan100% (2)
- 118a - Alteration in Neurologic FunctionDocument35 pages118a - Alteration in Neurologic FunctionJoanna TaylanNo ratings yet
- Amyotrophic Lateral Sclerosis: Daga, Joel Andrew BSN 3DDocument17 pagesAmyotrophic Lateral Sclerosis: Daga, Joel Andrew BSN 3DJoel Andrew Java Daga100% (2)
- Cushing's SyndromeDocument4 pagesCushing's SyndromeZainab AliNo ratings yet
- Surgery MCQDocument24 pagesSurgery MCQMoiz Khan88% (8)
- Guided Meditations for Anxiety, Insomnia and Sleep: Have a Full Night's Rest with Sleeping Techniques and Deep Relaxation, Which Can Help Adults and Kids Wake up More Happier and Become More Energized!From EverandGuided Meditations for Anxiety, Insomnia and Sleep: Have a Full Night's Rest with Sleeping Techniques and Deep Relaxation, Which Can Help Adults and Kids Wake up More Happier and Become More Energized!No ratings yet
- Angiography (Cardiac Catherization) : Patient Teaching/preparationDocument2 pagesAngiography (Cardiac Catherization) : Patient Teaching/preparationpsyNo ratings yet
- Neurologic Assessment Physiologic Changes With AgingDocument4 pagesNeurologic Assessment Physiologic Changes With AgingDarl Dacdac100% (1)
- OB-GYN Board Exam QuestionsDocument11 pagesOB-GYN Board Exam QuestionsJo Anne94% (17)
- Unconsciousness SeminarDocument23 pagesUnconsciousness SeminarJosh100% (3)
- CCNDocument39 pagesCCNMann TSha100% (1)
- Multiple SclerosisDocument35 pagesMultiple SclerosisJc SeguiNo ratings yet
- Types of Seizure & Status Epilepticus: Prepared By: Ivy Joy A. Benitez, BSN 4-ADocument28 pagesTypes of Seizure & Status Epilepticus: Prepared By: Ivy Joy A. Benitez, BSN 4-AyviyojNo ratings yet
- Alteration in Neurologic FunctionDocument35 pagesAlteration in Neurologic FunctionJoanna Taylan100% (1)
- NCP ON MenopauseDocument12 pagesNCP ON MenopauseNancy Singh100% (1)
- 3.chronic IllnessesDocument51 pages3.chronic IllnessesJonalyn EtongNo ratings yet
- Presentation EpilepsyDocument38 pagesPresentation EpilepsypertinenteNo ratings yet
- Advance Nursing Practice Presentation On Sensory DeprivationDocument22 pagesAdvance Nursing Practice Presentation On Sensory DeprivationLaveena Aswale67% (3)
- Unconciounsness & Sensory DepDocument92 pagesUnconciounsness & Sensory DepSimran SimzNo ratings yet
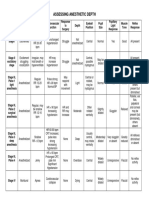
- Anesthesia-Assessing Depth PDFDocument1 pageAnesthesia-Assessing Depth PDFAvinash Technical ServiceNo ratings yet
- Nursing Diagnosis: AdvertisementsDocument7 pagesNursing Diagnosis: AdvertisementsJamea TumbagaNo ratings yet
- Neurologic Chnages (Geriatric Patient)Document2 pagesNeurologic Chnages (Geriatric Patient)Havier EsparagueraNo ratings yet
- NCM116 Finals Assessment of The Nervous SystemDocument9 pagesNCM116 Finals Assessment of The Nervous SystemRachelle DelantarNo ratings yet
- Vestibular NeuritisDocument2 pagesVestibular NeuritisElsa Nabila YumezaNo ratings yet
- Degen 1Document21 pagesDegen 1KoRnflakesNo ratings yet
- Diagnostic EvaluationDocument67 pagesDiagnostic EvaluationMyzing OraaNo ratings yet
- Comatose PatientDocument11 pagesComatose PatientUWIMANA Jean ClaudeNo ratings yet
- NCM 114 Module 3Document30 pagesNCM 114 Module 3leinneleinneNo ratings yet
- Epilepsy and Its ManagementDocument2 pagesEpilepsy and Its Managementlmra89No ratings yet
- NCM 116a: Skills Learning Material 4Document17 pagesNCM 116a: Skills Learning Material 4Ryrey Abraham PacamanaNo ratings yet
- Lewis: Medical-Surgical Nursing, 10 Edition: Sleep and Sleep Disorders Key Points SleepDocument4 pagesLewis: Medical-Surgical Nursing, 10 Edition: Sleep and Sleep Disorders Key Points Sleepsophia onu100% (2)
- Multiple Sclerosis: Demyelination-Damages The Myelin Sheath and Neurons This Damage Slows Down orDocument6 pagesMultiple Sclerosis: Demyelination-Damages The Myelin Sheath and Neurons This Damage Slows Down orNorhana ManasNo ratings yet
- Cognitive and Neurologic FunctionDocument38 pagesCognitive and Neurologic Functioncoosa liquorsNo ratings yet
- Sequelae of Trumatic Brain InjuryDocument19 pagesSequelae of Trumatic Brain InjuryAnurag SuryawanshiNo ratings yet
- Question Mphill VivaDocument2 pagesQuestion Mphill Vivaali imranNo ratings yet
- Advanced Nursin-Wps Office RachelDocument14 pagesAdvanced Nursin-Wps Office RachelRachel GeddamNo ratings yet
- CM3 Cu13Document10 pagesCM3 Cu13AengewycaNo ratings yet
- DevPsy 8 OldAgeDocument5 pagesDevPsy 8 OldAgekaren gempesawNo ratings yet
- Herniated Nucleus Pulposus 1Document17 pagesHerniated Nucleus Pulposus 1Ivan OngNo ratings yet
- Week 4 NotesDocument27 pagesWeek 4 NotesRayNo ratings yet
- Neuro Study GuideDocument19 pagesNeuro Study GuideMelissa SmirnowNo ratings yet
- Altered Mental Status: by Diana King, MD, and Jeffrey R. Avner, MDDocument9 pagesAltered Mental Status: by Diana King, MD, and Jeffrey R. Avner, MDchintya claraNo ratings yet
- ND Chapter 1Document5 pagesND Chapter 1Rome OlaNo ratings yet
- Sleep PresentationDocument16 pagesSleep Presentationapi-627301337No ratings yet
- NEUROLOGICDocument11 pagesNEUROLOGICinah krizia lagueNo ratings yet
- CHN 2 ElderlyDocument25 pagesCHN 2 Elderlynimila gopiNo ratings yet
- DementiaDocument27 pagesDementiaNina OaipNo ratings yet
- Ayurvedic Home Remedies For ParalysisDocument2 pagesAyurvedic Home Remedies For ParalysisPravin BholeNo ratings yet
- Loss of Mental Abilities & Most Commonly Occurs Late in Life A Brain Disorder That Seriously Affects A Person'S Ability To Carry Out Daily ActivitiesDocument29 pagesLoss of Mental Abilities & Most Commonly Occurs Late in Life A Brain Disorder That Seriously Affects A Person'S Ability To Carry Out Daily ActivitiesPatrick PantuaNo ratings yet
- Subject Seminar On COMA by DR - Mohan T Shenoy On 24-8-2009 & 31-8-2009Document146 pagesSubject Seminar On COMA by DR - Mohan T Shenoy On 24-8-2009 & 31-8-2009Aimhigh_PPMNo ratings yet
- Seizure: Focal/partial SeizuresDocument7 pagesSeizure: Focal/partial SeizuresMauren DazaNo ratings yet
- MS Neuro (Lab) Sas 1Document4 pagesMS Neuro (Lab) Sas 1Jake Yvan DizonNo ratings yet
- Alterations in Neurological, Mental Health and Cognition FunctionsDocument133 pagesAlterations in Neurological, Mental Health and Cognition Functionsthe4gameNo ratings yet
- Disorders of The Nervous System: Vascular DisorderDocument3 pagesDisorders of The Nervous System: Vascular DisorderHetty100% (1)
- UnconsciousnessDocument80 pagesUnconsciousnessDivya SomanNo ratings yet
- Presbyastasis A Multifactorial Cause of Balance Problems in The ElderlyDocument5 pagesPresbyastasis A Multifactorial Cause of Balance Problems in The Elderlydarmayanti ibnuNo ratings yet
- Physiologic Changes IN Aging: (Nervous System)Document17 pagesPhysiologic Changes IN Aging: (Nervous System)Yamete KudasaiNo ratings yet
- Ad HD MSDocument16 pagesAd HD MSangelaNo ratings yet
- MidtermDocument4 pagesMidtermJennica BubanNo ratings yet
- Geriatric NursingDocument46 pagesGeriatric NursingQuolette Constante100% (2)
- Anaphylactic Shock Due To Contrast Dye Allergy HF Due To Left Ventricle Damage and MIDocument3 pagesAnaphylactic Shock Due To Contrast Dye Allergy HF Due To Left Ventricle Damage and MIpsyNo ratings yet
- ParkinsonsDocument2 pagesParkinsonspsyNo ratings yet
- ECG Description:: Ventricular FibrillationDocument2 pagesECG Description:: Ventricular FibrillationpsyNo ratings yet
- Physiological Integrity: Draw A Quick Concept Map Comparing Right Vs Left Heart FailureDocument1 pagePhysiological Integrity: Draw A Quick Concept Map Comparing Right Vs Left Heart FailurepsyNo ratings yet
- List, Prioritize, Discuss Care For Patients Suffering An Acute Critical Neuro Emergency. Pick A Condition From This Chapter. and Create A Quick Concept MapDocument2 pagesList, Prioritize, Discuss Care For Patients Suffering An Acute Critical Neuro Emergency. Pick A Condition From This Chapter. and Create A Quick Concept MappsyNo ratings yet
- ParkinsonsDocument2 pagesParkinsonspsyNo ratings yet
- Myasthenia GravisDocument2 pagesMyasthenia GravispsyNo ratings yet
- HyperparathyroidismDocument2 pagesHyperparathyroidismpsyNo ratings yet
- Gather Patient HistoryDocument1 pageGather Patient HistorypsyNo ratings yet
- Nutrition Self-Monitored Blood GlucoseDocument3 pagesNutrition Self-Monitored Blood GlucosepsyNo ratings yet
- AIIMS PG 2005 Question Paper PDFDocument26 pagesAIIMS PG 2005 Question Paper PDFramNo ratings yet
- Nursing Diagnosis Cues Rank Justification According To ABC or Maslow'sDocument3 pagesNursing Diagnosis Cues Rank Justification According To ABC or Maslow'sShaina MillanNo ratings yet
- Long Case PresentationDocument3 pagesLong Case PresentationAkshat WaranNo ratings yet
- Form Ringkasan Perawatan Pasien Pulang (Resume Medis)Document1 pageForm Ringkasan Perawatan Pasien Pulang (Resume Medis)gandi mahardika muktiNo ratings yet
- Clonidine Stimulation For GH Secretion in ChildrenDocument2 pagesClonidine Stimulation For GH Secretion in ChildrenMulyono Aba AthiyaNo ratings yet
- Pulse TerapiDocument4 pagesPulse TerapiZuldan KaramiNo ratings yet
- 32) How To Do and Interpret A Rectal Examination PDFDocument3 pages32) How To Do and Interpret A Rectal Examination PDFAndres Gómez AldanaNo ratings yet
- Introduction To First Aid: American Red Cross St. John AmbulanceDocument5 pagesIntroduction To First Aid: American Red Cross St. John AmbulanceВалентина Василівна Банилевська0% (1)
- Combined Orthokeratology With Atropine For Children With Myopia: A Meta-AnalysisDocument9 pagesCombined Orthokeratology With Atropine For Children With Myopia: A Meta-AnalysiskarakuraNo ratings yet
- 10 Communicable DiseasesDocument3 pages10 Communicable DiseasesPauline de VeraNo ratings yet
- Guidelines For Management of Spontaneous ICH-2015Document30 pagesGuidelines For Management of Spontaneous ICH-2015Jerry John OforiNo ratings yet
- DSM 5 - Motor DisorderDocument5 pagesDSM 5 - Motor DisorderjackyploesNo ratings yet
- ARMD M Optom 4 TH SemesterDocument78 pagesARMD M Optom 4 TH Semestertanishqa eye careNo ratings yet
- In Primary Care: Chronic Kidney Disease (CKD)Document4 pagesIn Primary Care: Chronic Kidney Disease (CKD)NotForAbuseNo ratings yet
- What Is Alopecia Areata?Document2 pagesWhat Is Alopecia Areata?dincajeanNo ratings yet
- Lecture VIII - PdfpedoDocument13 pagesLecture VIII - PdfpedoNoor Abdullah AlNo ratings yet
- EndophthalmitisDocument30 pagesEndophthalmitisNazmiNo ratings yet
- Understanding KwashiorkorDocument7 pagesUnderstanding KwashiorkorpraneethNo ratings yet
- Eating Disorder WebQuestDocument2 pagesEating Disorder WebQuestFiona Wang100% (1)
- Lu 2014Document6 pagesLu 2014Yanet FrancoNo ratings yet
- Bacterio BilityDocument8 pagesBacterio BilityAbdul Rehman SafdarNo ratings yet
- PEH 3 Lesson 2Document3 pagesPEH 3 Lesson 2ShaineMaiko MarigocioNo ratings yet
- Eiparm Pdskji MakassarDocument15 pagesEiparm Pdskji MakassarArya Utama Timur Galang AdilNo ratings yet