Professional Documents
Culture Documents
DEFIBRILLATION
Uploaded by
Funi PesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DEFIBRILLATION
Uploaded by
Funi PesCopyright:
Available Formats
DEFIBRILLATION • Junctional ectopic tachycardia (JET) Electrocution of the by-standers
DEFIBRILLATION • The patient has a valid do-not-resuscitate order (DNR) Formation of short circuits between paddles due to excessive amount of conduction jelly applied on the
- electrical current administered to stop a dysrhythmia. It is used in emergency situations as the treatment of • The patient is wet and lying in water (outside hospital setting) paddles. This causes loss of electrical energy.
choice for ventricular fibrillation and pulseless VT. • Multifocal atrial tachycardia Dysrhythmias Pulmonary edema
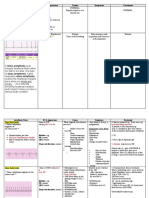
DEFIBRILLATOR • Presence of a pulse Cardiac arrest Pulmonary or systemic emboli
– are devices that restore a normal heartbeat by sending an electric pulse or shock to the heart. They are used to • Obvious signs of death Respiratory arrest Equipment malfunction
prevent or correct an arrhythmia, a heartbeat that is uneven or that is too slow or too fast. Defibrillators can also FACTORS AFFECTING DEFIBRILLATION ANALYSIS Neurologic impairment Death
restore the heart's beating if the heart suddenly stops. Electrode position Altered skin integrity
CARDIAC ARREST Hand-held versus patch electrodes
– a sudden loss of blood flow resulting from the failure of the heart to pump effectively. Signs include loss of Electrode position PARTS OF DEFIBRILLATOR
consciousness and abnormal or absent breathing. Some individuals may experience chest pain, shortness of breath, Electrode pad size
or nausea before cardiac arrest. Automated rhythm analysis
VENTRICULAR FIBRILLATION Device maintenance and quality assurance
- is a rapid but disorganized ventricular rhythm that causes ineffective quivering of the ventricles. There is no atrial CAUTION AND REMINDERS IN OPERATIBNG DEFIBRILLATION
activity seen on the ECG. Maintain good contact between the pads or paddles (with a conductive medium) and the patient’s skin to
RESPIRATORY ARREST prevent electrical current from leaking into the air (arcing) when the defibrillator is discharged
- cessation of breathing. Respiratory arrest is usually the endpoint of respiratory distress that leads to respiratory The defibrillator is discharged. Ensure that no one is in contact with the patient or with anything that is
failure touching the patient when the defibrillator is discharged, to minimize the chance that electrical current will be
HEART conducted to anyone other than the patient.
- is a muscular organ about the size of a fist, located just behind and slightly left of the breastbone. The heart pumps Place paddles or pads so that they do not touch the patient’s clothing or bed linen and are not near
blood through the network of arteries and veins called the cardiovascular system. medication patches or direct oxygen flow.
CARDIOVASCULAR COLLAPSE If cardioverting, ensure that the monitor leads are attached to the patient and that the defibrillator is in sync
- Sudden loss of effective blood flow due to cardiac and/or peripheral vascular factors that may reverse mode. Ifdefibrillating, ensure that the defibrillator is not in sync mode (most machines default to the “not-sync”
spontaneously. mode). Basic Parts of Defibrillator
VENTRICULAR TACHYCARDIA Use multifunction conductor pads or paddles with a conducting agent between the paddles and the skin (the
- is defined as three or more PVCs in a row, occurring at a rate exceeding 100 beats per minute. The causes are conducting agent is available as a sheet, gel, or paste).
similar to those for PVC. VT is usually associated with coronary artery disease and may precede ventricular Do not charge the device until ready to shock; then keep thumbs and fingers off the discharge buttons until
fibrillation. VT is an emergency because the patient is usually (although not always) unresponsive and pulseless. paddles or pads are on the chest and ready to deliver the electrical charge.
PURPOSE OF DEFIBRILLATION Exert 20 to 25 pounds of pressure on the paddles to ensure good skin contact.
To treat a tachycardia (atrial or ventricular) Before pressing the discharge button, call “Clear!” three times: As “Clear” is called the first time, ensure that
To disrupt a chaotic rhythm and allow the heart's normal pacemakers to resume effective electrical activity you are not touching the patient, bed or equipment; as “Clear” is called the second time, ensure that no one
It reverses the cardiac arrest by sending an electrical current through the heart muscle cells, momentarily is touching the bed, the patient, or equipment, including the endotracheal tube or adjuncts; and as “Clear” is
stopping the abnormal electrical energy and allowing the normal heart beat to resume called the third time, per-form a final visual check to ensure you and everyone else are clear of the patient
Treatments for tachydysrhythmias and anything touching the patient.
INDICATIONS
Record the delivered energy and the results (cardiac rhythm,
• Patient who has tachydysrhythmias pulse).
• Ventricular tachycardia or pulseless VT
After the event is complete, inspect the skin under the pads or paddles for burns; if any are detected, consult
• Ventricular fibrillation with the physician or a wound care nurse about treatment.
• Atrial fibrillation TYPES OF DEFIBRILLATORS
• Atrial flutter
COMPLICATIONS 1. MANUAL EXTERNAL DEFIBRILLATOR
CONTRAINDICATIONS
Damage to myocardium due to repeated high energy electrical shocks
An advanced life support medical device that monitors the heart rhythm and allow the user to manually set
• Digitalis induced dysrhythmias
Chest burns due to repeated high-energy discharges and poor contract between the paddles and the skin
the energy delivery and deliver a shock.
2. MANUAL INTERNAL DEFIBRILLATOR 14. Continue resuscitative efforts until patient regains pulse or until physician determines death.
Deliver the shock through paddles placed directly on the heart. They are mostly used in the operating room
and, in rare circumstances, in the emergency room during an open heart procedure.
3. SEMI-AUTOMATED EXTERNAL DEFIBRILLATOR
Used by lay responders to treat someone in cardiac arrest. The user pushes. the on button, pulls a handle or
opens the lid and the AED starts to talk to you. The user will open the pads and place them on the patient as
indicated by pictures on the pads.
4. AUTOMATED EXTERNAL DEFIBRILLATOR (AED)
AEDs are considered a public access device designed to be used by anyone, whether they are trained or
not. The device walks the user through the rescue until EMS arrives or the person is revived.
5. IMPLANTABLE CARDIOVERTER DEFIBRILLATOR (ICD)
A device implantable inside the body, able to perform cardioversion, defibrillation, and pacing of the heart.
The device is therefore capable of correcting most life-threatening cardiac arrhythmias.
6. WEARABLE CARDIAC DEFIBRILLATOR
A device worn by patients who are at risk for sudden cardiac arrest. A WCD allows physicians time to assess
for their patient's arrhythmic risk and make appropriate plans. A WCD is lightweight and easy to wear.
STEPS AND GUIDELINES IN OPERATING DEFIBRILLATOR
STEPS
1. Establish unresponsiveness and call for help.
2. Establish absence of respirations and lack of circulation: no pulse, no respirations, no movement.
3. Activate code team in accordance with hospital policy and procedure.
4. Start chest compressions and continue until defibrillator is attached to patient and verbal prompt of device
advises you, “Do not touch the patient.
5. Place defibrillator next to patient near chest or head.
6. Turn on power
7. Attach device. Place the first pad on the upper right sternal border directly below the clavicle. Place the second pad
lateral to the left nipple with the top of the pad a few inches below the axilla. Ensure that cables are connected to the
machine.
8. When defibrillator prompts you, stop touching patient. Do NOT touch patient after this prompt. Direct rescuers or medical
professionals to avoid touching patient by announcing “Clear!” Allow the defibrillator machine to analyze the rhythm. Some
devices require that an analysis button be pressed. The defibrillator takes approximately 5 to 15 seconds to analyze the
rhythm.
9. Before pressing the shock button, announce loudly to clear the victim and perform a visual check to ensure that no one is
in contact with victim.
10. Immediately begin chest compression (CPR) after the shock and continue for 2 minutes.
11. Deliver two breaths using mouth-to-mouth with barrier device or mouth-to mask device or bag-mask device. Watch for
chest rise and fall. Deliver 10 to 12 breaths/min.
12. After 2 minutes of CPR, the defibrillator will prompt you not to touch patient and will resume analysis of patient’s rhythm.
This cycle will continue until patient regains a pulse or physician determines death.
13. Inspect pad adhesion to chest wall. If pads are not in good contact with chest wall, remove them and apply a new set.
Attach new set of pads to the defibrillator.
You might also like
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- DefibrillatorsDocument54 pagesDefibrillatorsAli Al-AhmedyNo ratings yet
- Decoding Cardiac Electrophysiology: Understanding the Techniques and Defining the JargonFrom EverandDecoding Cardiac Electrophysiology: Understanding the Techniques and Defining the JargonAfzal SohaibNo ratings yet
- Defibrillatorppt 131028115457 Phpapp01Document41 pagesDefibrillatorppt 131028115457 Phpapp01Simon JosanNo ratings yet
- DefibrillatorDocument8 pagesDefibrillatorJisha JanardhanNo ratings yet
- DC ShockDocument8 pagesDC Shockرافت العواضيNo ratings yet
- Defibrillator: DR Sumanth ReddyDocument39 pagesDefibrillator: DR Sumanth Reddyrohith100% (1)
- Cheat ECG-2Document3 pagesCheat ECG-2Neil Emman BotardoNo ratings yet
- Cardiology Medsurg LectureDocument9 pagesCardiology Medsurg LectureTine GuibaoNo ratings yet
- DefibrillatorDocument10 pagesDefibrillatorMakhanVermaNo ratings yet
- ETD-DefibDocument58 pagesETD-DefibFarah Najwa GhazaliNo ratings yet
- Defibrillatorppt 131028115457 Phpapp01Document41 pagesDefibrillatorppt 131028115457 Phpapp01Qweku BlackNo ratings yet
- Basic Principle, Operation and Maintenance: Aqeel Ahmed KhanDocument18 pagesBasic Principle, Operation and Maintenance: Aqeel Ahmed KhanchanlalNo ratings yet
- Defibrillation TypedDocument8 pagesDefibrillation TypedValarmathiNo ratings yet
- Troubleshootingcardiac Monitor Problems: Don't Forget Toassess The Patient First!Document2 pagesTroubleshootingcardiac Monitor Problems: Don't Forget Toassess The Patient First!Melinia HdyNo ratings yet
- Defibrillator1 200806145633Document28 pagesDefibrillator1 200806145633harpreetNo ratings yet
- Cardiac Electrical Assistive DevicesDocument14 pagesCardiac Electrical Assistive DevicesaprnworldNo ratings yet
- Atrial FlutterDocument38 pagesAtrial FlutterLady AngodNo ratings yet
- Defibrillation and Electrical CardioversionDocument27 pagesDefibrillation and Electrical CardioversionYui Hirasawa100% (1)
- Cardiac PacingDocument4 pagesCardiac PacingmrygnvllNo ratings yet
- Defibrillation and Cardioversion: Dr. Asim BiswasDocument32 pagesDefibrillation and Cardioversion: Dr. Asim BiswasAsim Kumar BiswasNo ratings yet
- Chapter 125. CardioversionDocument21 pagesChapter 125. CardioversionZoe VelasquezNo ratings yet
- Defibrillation ChecklistDocument4 pagesDefibrillation ChecklistCzarina100% (1)
- Basics of Ecg InterpretationDocument76 pagesBasics of Ecg InterpretationDennis MiritiNo ratings yet
- ECG Monitor and RhythmDocument9 pagesECG Monitor and Rhythmboxed juiceNo ratings yet
- Overdrive PacingDocument24 pagesOverdrive PacingWilliam Perero RodríguezNo ratings yet
- Pacemaker Therapy: Prepared by Zahra A.M Ahmed Supervisor by Dr. Hassan Abdullah AthbiDocument27 pagesPacemaker Therapy: Prepared by Zahra A.M Ahmed Supervisor by Dr. Hassan Abdullah AthbiZahraa A.M AhmedNo ratings yet
- DefibrillatorDocument5 pagesDefibrillatorgurneet kourNo ratings yet
- DC ShockDocument8 pagesDC ShockMeidita Annisa PurmanNo ratings yet
- Cardiorespiratory Arrest (FS)Document55 pagesCardiorespiratory Arrest (FS)Ahmad AzharNo ratings yet
- DefibrillatorDocument20 pagesDefibrillatorJasmine KaurNo ratings yet
- Cardiac Pacing and ICDDocument74 pagesCardiac Pacing and ICDBernadixta Winda Dwi Cahyani100% (3)
- PACEMAKERDocument5 pagesPACEMAKERPoonam ThakurNo ratings yet
- Cardio ExpoDocument35 pagesCardio Expoapi-667225436No ratings yet
- DefibrillatorDocument85 pagesDefibrillatorDhruv DesaiNo ratings yet
- Presentation1 DefibDocument60 pagesPresentation1 DefibRoshani sharmaNo ratings yet
- DefibrillationDocument9 pagesDefibrillationJara Maris Moreno BudionganNo ratings yet
- Arrhythmia: Andi Wahjono Adi, MD, FihaDocument37 pagesArrhythmia: Andi Wahjono Adi, MD, FihaChechyl MilianiNo ratings yet
- Pacemaker Therapy-1Document30 pagesPacemaker Therapy-1shejila c hNo ratings yet
- Transe 1Document2 pagesTranse 1lija.medija.swuNo ratings yet
- Pacemaker 180508042454Document86 pagesPacemaker 180508042454padmaNo ratings yet
- Defibrillation and Cardioversion Monette NCM 118 SL PDFDocument40 pagesDefibrillation and Cardioversion Monette NCM 118 SL PDFSam VeraNo ratings yet
- DefibrillationDocument9 pagesDefibrillationWilson Tadeu Assis100% (2)
- Defibrillation: DR Ezechiel NteziryayoDocument31 pagesDefibrillation: DR Ezechiel NteziryayoNteziryayo EzechielNo ratings yet
- Cardiac PacingDocument4 pagesCardiac PacingmrygnvllNo ratings yet
- 12 Lead ECGDocument9 pages12 Lead ECGVinz Khyl G. CastillonNo ratings yet
- DefibrillationDocument13 pagesDefibrillationKristine VedadNo ratings yet
- Design of DC Shock Simulator: 0Xkdppdg $plu 0D Uxi, Bambang Guruh Irianto, Tri Bowo IndratoDocument7 pagesDesign of DC Shock Simulator: 0Xkdppdg $plu 0D Uxi, Bambang Guruh Irianto, Tri Bowo IndratoنزیرNo ratings yet
- Early Management: Admit To Burns UnitDocument1 pageEarly Management: Admit To Burns UnitErica A. Gallegos AriasNo ratings yet
- Instrument - Automated External DefibrillatorDocument2 pagesInstrument - Automated External DefibrillatorJulio ArgañarazNo ratings yet
- Defibrillation and CardioversionDocument51 pagesDefibrillation and CardioversionChinju Cyril100% (2)
- DefibrilationDocument4 pagesDefibrilationDrmirfat AlkashifNo ratings yet
- Atrioventricular Conduction During Atrial FlutterDocument4 pagesAtrioventricular Conduction During Atrial FlutterTaynan MassaroNo ratings yet
- Defibrillation & DC Shock: Ns. Retno Setyawati, M.Kep., SP - KMBDocument34 pagesDefibrillation & DC Shock: Ns. Retno Setyawati, M.Kep., SP - KMBdanur ciyeeNo ratings yet
- Health Problem Addressed: Umdns GMDNDocument1 pageHealth Problem Addressed: Umdns GMDNHaerul ImamNo ratings yet
- Cardioversion & DefibrillationDocument14 pagesCardioversion & DefibrillationbajaocNo ratings yet
- Cardioversion and DefibrillationDocument24 pagesCardioversion and Defibrillationrona-chanNo ratings yet
- Sinus Bradycardia: I. Sinus Dysrhythmias Description ManagementDocument4 pagesSinus Bradycardia: I. Sinus Dysrhythmias Description ManagementMargueretti Delos ReyesNo ratings yet
- Defibrillators 1Document1 pageDefibrillators 1Nirmal Kumar PandeyNo ratings yet
- ECG ExamplesDocument25 pagesECG Examplesvinsonpeng26No ratings yet
- Nur 111 Session 10 Sas 1Document9 pagesNur 111 Session 10 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Cardio QuizDocument100 pagesCardio QuizEvidence ChaibvaNo ratings yet
- Touch and Step PotentialsDocument10 pagesTouch and Step PotentialsMirela JakNo ratings yet
- Touchcardio HRC Abstracts 2022 Final 3Document149 pagesTouchcardio HRC Abstracts 2022 Final 3Cristina AdamNo ratings yet
- Roberto Santilli - Electrocardiography of The Dog and Cat - Diagnosis of Arrhythmias-Edra (2018)Document348 pagesRoberto Santilli - Electrocardiography of The Dog and Cat - Diagnosis of Arrhythmias-Edra (2018)Juan DuasoNo ratings yet
- Essay About GardeningDocument5 pagesEssay About Gardeningfesehos0tej2100% (2)
- Mark K Audio LecturesDocument62 pagesMark K Audio LecturesMelissa Sapp100% (6)
- Medical Electronics - SKP 116 135Document20 pagesMedical Electronics - SKP 116 135Mohammed Mian ANo ratings yet
- Cardiology-5 DysrhythmiaDocument16 pagesCardiology-5 DysrhythmiaMahmoud RamadanNo ratings yet
- 2021 ESC Guidelines On Cardiac Pacing and Cardiac Resynchronization TherapyDocument107 pages2021 ESC Guidelines On Cardiac Pacing and Cardiac Resynchronization TherapyLourdes FrancoNo ratings yet
- Arrythmia Name: Normal Sinus RhythmDocument7 pagesArrythmia Name: Normal Sinus RhythmJulx0No ratings yet
- Antiarrhythmic DrugsDocument42 pagesAntiarrhythmic DrugsRamadi PrameelaNo ratings yet
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyNo ratings yet
- Adult 3 FinalDocument29 pagesAdult 3 Finalأبوأحمد الحكيم100% (1)
- Tintinalli - Chapter 11 Sudden Cardiac DeathDocument3 pagesTintinalli - Chapter 11 Sudden Cardiac DeathGelo JosonNo ratings yet
- PRN2158 ASHI G2015 BLS SB 081016 DigitalDocument64 pagesPRN2158 ASHI G2015 BLS SB 081016 DigitalJampol BalganionNo ratings yet
- 2019 Catheter Ablation of VA PDFDocument153 pages2019 Catheter Ablation of VA PDFyusupNo ratings yet
- Electric Shocks and Electrocution, Clinical Effects and PathologyDocument9 pagesElectric Shocks and Electrocution, Clinical Effects and PathologyYosuaNo ratings yet
- Atrial Fibrillation - Diagnosis and Treatment - AAFP PDFDocument8 pagesAtrial Fibrillation - Diagnosis and Treatment - AAFP PDFNaufal AmanullahNo ratings yet
- Chapter 47 - Antidysrhythmic DrugsDocument10 pagesChapter 47 - Antidysrhythmic Drugsdlneisha61100% (1)
- Epilepsy & Behavior: Gaetano Zaccara, Simona LattanziDocument9 pagesEpilepsy & Behavior: Gaetano Zaccara, Simona Lattanziricky hutagalungNo ratings yet
- International Conference On Application of Recent Technologies in Science, Engineering, Management For Societal and Industrial Development ProceedingsDocument9 pagesInternational Conference On Application of Recent Technologies in Science, Engineering, Management For Societal and Industrial Development ProceedingsjanurangNo ratings yet
- Worker Death Due To ElectrocutionDocument702 pagesWorker Death Due To ElectrocutionRajuNo ratings yet
- Pre-Excitation Syndromes in Children: Dr.K.MaheshDocument105 pagesPre-Excitation Syndromes in Children: Dr.K.MaheshNischal ShahNo ratings yet
- Questions & Answers: CardiologyDocument77 pagesQuestions & Answers: CardiologyDev Yadav100% (1)
- Dysrhythmias: Normal Electrical ActivityDocument32 pagesDysrhythmias: Normal Electrical ActivityLarisse de LeonNo ratings yet
- Electrical InjuriesDocument5 pagesElectrical InjuriesFalon PapalangiNo ratings yet
- Peralatan Sistem Tenaga ListrikDocument13 pagesPeralatan Sistem Tenaga ListrikHarfiana MaharaniNo ratings yet
- Ehra Position Paper: Europace (2020) 00, 1-48 Doi:10.1093/europace/euaa065Document48 pagesEhra Position Paper: Europace (2020) 00, 1-48 Doi:10.1093/europace/euaa065Catherine MorrisNo ratings yet