Professional Documents
Culture Documents
Hfo 3
Uploaded by
markus_danusantosoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hfo 3
Uploaded by
markus_danusantosoCopyright:
Available Formats
96 ARTIGO DE REVISÃO
José Roberto Fioretto1, Celso Moura
Rebello2
High-frequency oscillatory ventilation in
pediatrics and neonatology
Ventilação oscilatória de alta freqüência em pediatria e
neonatologia
1. Post-doctorate degree, Adjunct ABSTRACT adjustments relating to oxygenation,
Professor of the Pediatrics Department CO2 elimination, chest radiography,
of the Faculdade de Medicina de This article intends to review lit- suctioning, sedatives and use of neu-
Botucatu da Universidade Estadual erature on high frequency oscillatory romuscular blocking agents were de-
Paulista “Júlio de Mesquita Filho” - ventilation and describe its main clini- scribed. Weaning and complications
UNESP – Botucatu (SP), Brazil. cal applications for children and neo- were also reported. For children, high
2. PhD, Assistant Professor of nates. Articles from the last 15 years frequency oscillatory ventilation is
the Pediatrics Department of the were selected using MedLine and Sci- a therapeutic option, particularly in
Universidade de São Paulo - USP – São Elo databases. The following key words acute respiratory distress syndrome,
Paulo (SP), Brazil. were used: high frequency oscillatory and should be used as early as possible.
ventilation, mechanical ventilation, It may be also useful in the air leak
acute respiratory distress syndrome, syndrome and obstructive pulmonary
children, and new-born. The review disease. Evidence that, in neonates,
describes high frequency oscillatory high frequency oscillatory ventilation
ventilation in children with acute re- is superior to conventional mechanical
spiratory distress syndrome, air leak ventilation is lacking. However there
syndrome, and obstructive lung dis- is evidence that better results are only
ease. Respiratory distress syndrome, achieved with this ventilatory mode to
bronchopulmonary dysplasia, intrac- manage the air leak syndrome.
ranial hemorrhage, periventricular leu-
komalacia, and air leak syndrome were Keywords: High frequency oscil-
reviewed in neonates. Transition from latory ventilation; Mechanical venti-
conventional mechanical ventilation lation; Acute respiratory distress syn-
Received from the Pediatrics to high frequency ventilation and its drome; Child; Infant, newborn
Department of the Faculdade de
Medicina de Botucatu da Universidade
Estadual Paulista “Júlio de Mesquita
Filho” - UNESP - Botucatu (SP), Brazil.
INTRODUCTION
Submitted on July 1, 2008
Accepted on December 24, 2008 One of the mainstays of intensive care in pediatrics and neonatology
is safe control of the ventilatory function achieved by mechanical ventila-
Author for correspondence: tion (MV). Although a life saving procedure, there is growing evidence
José Roberto Fioretto that conventional mechanical ventilation (CMV) may worsen pulmonary
Departamento de Pediatria - Faculdade function and contribute to development of a multiple organ dysfunction
de Medicina de Botucatu - UNESP in the endeavor to warrant normal gas exchange during acute respiratory
Distrito de Rubião Júnior failure.(1-4)
CEP:18618-000 – Botucatu (SP), Several publications call the attention to ventilator induced lung in-
Brasil. jury (VILI). The prevailing opinion is that use of high tidal volumes,
Phone/Fax: +55 (14) 3811-6274.
that generate high inspiratory pressures during MV of patients with acute
E-mail: jrf@fmb.unesp.br
respiratory distress syndrome (ARDS), cause structural injury in, the un-
Rev Bras Ter Intensiva. 2009; 21(1):96-103
High-frequency oscillatory ventilation in pediatrics and neonatology 97
til then, healthy areas of the lung, reproducing the greater in the ventilator circuit and in the tracheal
anatomy-pathological injuries of ARDS, worsening proximal portion, progressively decreasing along the
hypoxemia and patients’ evolution.(5,6) airway, resulting in low pressure amplitude in the al-
Thus VILI may be defined as a simulation of acute veoli.
pulmonary injury taking place in patients submitted Literature review and selection of more relevant
to MV. Repetitive overdistension of the lungs and publications on high frequency ventilation using as
subsequent development of atelectasia contribute to database MedLine and SciElo published in the last 15
pulmonary injury, which is caused by using the ven- years was carried out. The following key words wee
tilator standard for oxygenation and ventilation sup- used: high frequency oscillatory ventilation, mechani-
port. A cyclic change in pulmonary volume may be a cal ventilation, acute respiratory distress syndrome
significant cause of MVIPI, suggesting that a ventila- and new-born.
tion strategy avoiding major pulmonary volume varia-
tions might be beneficial.(7,8) CLINICAL APLICATIONS OF HFOV IN PE-
The concept of protective mechanical ventilation DIATRICS
emerged from the understanding of VILI. It may be
defined as a ventilation that minimizes tidal volume, Acute pulmonary injury and acute respiratory
maintains a low peak inspiratory pressure, offers a distress syndrome
sufficient positive end expiratory pressure (PEEP) to The combination of low volume and pressure vari-
maintain alveolar opening, avoiding alveolar collapse ation and maintenance of constant mean airway pres-
and cyclic opening and closing of the alveolar units, sure (MAP) make use of HFOV attractive for ARDS.
uses non-toxic concentrations of oxygen and permits Maintenance of pulmonary volume avoids pulmonary
hypercapnia.(5,7) overdistension as well as occurrence of atelectasia in
Although CMV is effective for most children, there patients with ARDS and the flow standard may im-
is a significant number of patients with severe respira- prove in relation to ventilation-perfusion. (11,12)
tory failure for whom CMV may not assure oxygen- Successful treatment of ARDS requires a strategy
ation and ventilation. In such cases, when protective to keep the lungs open, the open lung approach. Re-
mechanical ventilation is mandatory, high frequency cruitment of collapsed alveoli reduces intrapulmo-
oscillatory ventilation (HFOV) becomes an attractive nary shunt, reducing the fraction of inspired oxygen
alternative.(9) (FiO2) to less toxic concentrations. It was shown that
HFOV is a ventilation mode that uses a lower tidal children with ARDS have a significant improvement
volume than the anatomic dead space volume (1–3 in oxygenation, lower incidence of barotraumas and
mL/Kg) with a frequency well above the physiologi- better results with use of HFOV, (9) without influenc-
cal one (5–10 Hertz), that is to say, 300-600 cycles/ ing mortality. In adults with ARDS an immediate and
minute). This ventilation mode has been successfully sustained improvement was reported in relation to
used to treat patients with severe respiratory failure partial oxygen pressure (PaO2)/FiO2 when patients
when CMV fails, Furthermore, reports state that were submitted to HFOV combined with alveolar
when HFOV is used earlier, together with a protective recruitment maneuvers.(13) An additional benefit was
strategy, a decrease of the acute or chronic pulmonary shown to be reduction of inflammatory mediators in
injury occurs in patients with ARDS.(5,10,11) samples of bronchoalveolar lavage of patients with
The 3100A by SensorMedics® ventilator is approved HFOV when compared to CMV.(1,6) Further, in these
by Food and Drug Administration (FDA) for use in studies with adults, no statistical difference was ob-
children up to 35 kg. This is a device for mechanical served in mortality when comparing HFOV to CMV.
pulmonary ventilation with a continuous flow of gas It is noteworthy that these studies call attention to
capable of eliminating CO2 and keeping airway pres- early introduction of HFOV in ARDS when benefits
sure constant. The ventilator has an electromagnetic could be more easily demonstrated.
piston that generates high frequency oscillation on To summarize, in cases of ARDS, the HFOV is an
the air flow, establishing pressure oscillation ampli- important therapeutic tool and although, decrease of
tude. Contrary to the CMV, in HFOV tidal volume is mortality with use of this ventilation mode has not
inversely related to frequency and inspiration as well been proven, studies focusing on its early utilization
as expiration is active. The amplitude of pressure is must be implemented.
Rev Bras Ter Intensiva. 2009; 21(1):96-103
98 Fioretto JR, Rebello CM
Air leak syndrome tilator induced injuries (4) were observed. This included
Pneumothorax, mediastinal emphysema and pul- bronchopulmonary displasia (BPD) and occurrence of
monary interstitial air are observed in acute pulmo- air leak (pneumothorax, pneumomediastinum, etc.).
nary injury as a result of base disease as well as venti- To reduce occurrence of BPD various modifications
lation therapy. HFOV has been successfully used for in the ventilation strategies were introduced, and the
these patients(14,15) emphasizing that the strategy must less aggressive MV strategy was implemented. In this
encompass low MAP and use of pressure amplitude at aspect, use of HFOV in neonatology as previously de-
lower values, needed to keep adequate alveolar venti- scribed for older children emerged as an important
lation, resolving the air leak. In such cases a high FiO 2 technique for pulmonary protection.
must be permitted for short periods, accepting arte- Since its introduction in neonatology in 1981,
rial oxygen saturation (SaO 2) > 85% as long as oxygen including 8 new-born with ARDS, various studies
release is adequate, lactic acidosis does not occur and have been carried out to evaluate efficacy and safety
the patient is hemodynamically stable.(1,12) Decrease of of HFOV in relation to CMV in prematures. These
MAP and pressure amplitude lead to hypercapnia and, studies present highly variable results. Since the onset
to maintain adequate elimination of carbon dioxide it was well established that, just as in adults and in
(CO2), frequency may be reduced. However, hyper- older children, MAP applied during HFOV had a di-
capnia must be accepted, because adjustment of the rect correlation with oxygenation, therefore the high
respiratory rate to normalize CO 2 increases tidal vol- values of MAP permitted ventilation with low FiO 2(19)
ume, with a worse air leak.(1,14) and no major hemodynamic aftermaths were observed.
It was noted that in prematures a given MAP needed
Obstructive pulmonary disease to achieve and sustain alveolar expansions, could be
Use of HFOV when facing increased resistance of maintained. The oscillatory drives reopened atelactat-
the airways is controversial.(1,12) For some years HFOV ic areas more efficiently than the same mean pressure
was contraindicated for obstructive pulmonary disease maintained in an static way and that small volumes,
because of high risk of air trapping and dynamic hy- generated a at a respiratory rate of 10 a 15 Hz, pro-
perinsuflation.(1,16) However, successful use of HFOV vided a good safety margin to avoid overdistension of
in children with asthma and brochiolitis has been re- the lung normal areas. (20)
ported. (15) This is probably due to the unique charac- It must be recalled that benefits of HFOV in pre-
teristic of this ventilation mode, active expiration. In matures became evident after establishing a ventilation
this condition, air is actively removed from the lungs strategy based on recovery of the pulmonary volume
without risk of trapping. (16) Thus, in the previously aiming at early reversion of the atelactatic areas by a
described condition, HFOV may be considered as an more aggressive use of MAP and achieving a decrease
alternative when facing refractory respiratory acidosis of FiO2 prior to decrease of pressures.(21)
caused by inadequate alveolar ventilation. A second fundamentally important aspect observed
In one of the largest studies carried out in a in studies comparing efficacy and safety of HFOV in
single center, including 53 patients of which 17 pre- relation to CMV in neonatology, is the strategy used
sented withy obstructive disease, the open airway (17) in CMV, where PEEP used often is relatively low, per-
technique was applied by carefully titrating MAP in mitting alveolar collapse at the end of expiration, al-
HFOV to open airways and adjust ventilation,(18) a though MAP remains at somewhat lower levels than
success for this therapy. those of HFOV. This because the latter modality has
In summary, in situations of obstructive pulmo- the intrinsic advantage of keeping the lung at pres-
nary disease, it is always prudent to evaluate the risk sures above the zone of alveolar collapse, in view of
and benefit of introducing HFOV. the small amplitude of tidal volume utilized. This fa-
cilitates maintenance of the lung at pressures above
CLINICAL APPLICATIONS OF HFOV IN the lower inflection point of the pressure-volume
NEONATOLOGY curve, which is almost impossible in CMV. On the
contrary, especially in earlier studies, there was no
Since introduction of HFOV in neonatology dur- concern about using lower tidal volume values associ-
ing the sixties, a dramatic decrease of mortality (3) as ated to adequate levels of PEEP.(21)
well as establishment of a new category of disease, ven- After almost twenty studies comparing HFOV to
Rev Bras Ter Intensiva. 2009; 21(1):96-103
High-frequency oscillatory ventilation in pediatrics and neonatology 99
CMV in neonatology, it was shown that both treat- lomalacia: RR1.10; 95% CI 0.85-1.43).
ments are comparable in relation to mortality. Ini- Conversely to use of HFOV as a first form of treat-
tially, some studies suggested that HFOV was asso- ment in ARDS, use as a rescue therapy was reported in
ciated to a higher incidence of peri-intraventricular only two controlled studies, (27,28) without evidence of
hemorrhage, (22,23) resulting in some resistance to in- improved evolution in the long term of newborn, be
troduction of HFOV as routine in extreme prema- it in chronic pulmonary disease, occurrence of neuro-
tures. However, in the last five years, strong evidence logical complications, or survival.
has appeared that HFOV and CMV are equivalent Finally, HFOV has only shown a better result than
with regard to risk of evolving into intracranial hem- CMV during the neonatal period in relation to man-
orrhage in prematures. (24,25) agement of extrapulmonary air. The few studies com-
Safety and efficacy of HFOV were reviewed in paring HFOV to CMV in this situation demonstrate
2007 in a meta-analysis with 3585 children in 15 stud- that air leak through the thoracic drain is lower with
ies that compared this ventilation mode with CMV.(26) use of HFOV,(29,30) a fact confirmed in a case report(31)
The authors concluded that there is no evidence that and in an experimental study(32) which disclosed ben-
HFOV used as initial strategy presented advantages efit using HFOV in presence of a tracheoesophageal
in relation to CMV, regarding efficacy of ventilation or bronchopleural fistula.
or mortality at 28-30 days of age or age equivalent to To summarize, data currently available in literature
term. Nevertheless, authors found a small decrease in confirm that HFOV is a safe ventilation mode for use
the incidence of chronic pulmonary disease with 36-37 in neonatology, however there is no evidence proving
weeks gestational age, corrected among survivors with a clear benefit or advantage of HFOV in relation to
use of HFOV. However, this evidence is weakened by CMV in newborn, be as initial or as rescue therapy.
inconsistency of results over the 15 studies and the The only clinical situation where there is evidence of
threshold significance (RR 0.89;95% CI:0.81-0.99). better results with HFOV is extrapulmonary air, espe-
Analyses of subgroups showed that there was a de- cially in bronchopleural fistula.
crease of chronic pulmonary disease when HFOV was
carried out with a high tidal volume strategy, when TRANSITION FROM CONVENTIONAL
piston oscillators were used to perform HFOV, when VENTILATION TO HIGH FREQUENCY VEN-
randomization took place between two to six hours of TILATION
life and when an inspiration/expiration ratio of 1:2
was used for HFOV. Some of the inconsistency of A patient transferred to HFOV must be duly mon-
these results is due to variability of the strategies used itored regarding pulse oxymetry, relation PaO2/FiO2
for HFOV (high volume our reduced volume) as well and capnography. From the cardiovascular point of
as for CMV, over time. view, an adequate intravascular volume must be as-
It is noteworthy that currently when the prenatal sured based upon peripheral perfusion, capillary fill-
use of corticoids to induce pulmonary maturity in the ing, arterial pressure and heart rate. The endotracheal
premature, exogenous surfactant and use of more pro- tube must be correctly positioned and preferably there
tective CMV techniques has become a routine, any should be a closed suction system of the tracheal tube.
benefit from HFOV in relation to CMV, probably will Sedation should be optimized and in some cases cura-
only be proven in new-born with severe pulmonary rization may be needed.
disease. For instance, Courtney et al. (24) showed that As already mentioned, early use of HFOV (24,33,34)
benefit of using HFOV in relation to CMV was only has received considerable attention. As such, for chil-
observed when inclusion was restricted to new-born dren after the neonatal period and with ARDS, when
of very low weight that met criteria of major sever- SaO 2 is below 90%, in FiO 2 higher than 0.6, with
ity, based upon FiO 2 and MAP after administration inspiratory pressure (PIp) of 30-32 cmH2 and PEEP
of surfactant. higher than 10-12 cmH 2O, transfer from convention-
Although the meta-analysis (26) disclosed increased al to HFOV is recommended.
incidence of intreaventricular hemorrhage and of
leukoencephalomalacia with HFOV, in some studies Implementation of HFOV
these were not significant (intraventricular hemor- Initial parameters used in HFOV are: (1,2)
rhage: RR1.05; 95% C.I. 0.96-1.15 – leukoencepha- - sufficient FiO 2 to maintain SaO 2 ≥ 90% (100%
Rev Bras Ter Intensiva. 2009; 21(1):96-103
100 Fioretto JR, Rebello CM
during the transition time from CMV to HFOV; The ability to achieve adequate oxygenation in
- inspiratory time, 33% of the oscillatory cycle; non-toxic FiO2 is the main indicator that MAP is ad-
- frequency of 10 Hz for sucklings and from 5 to equate. In general, chest radiography must be made to
8 Hz for older children or according to the patient’s evaluate the level of pulmonary expansion and pres-
weight < 10kg = 10-12Hz; 11-20kg = 8-10Hz; 21- ence of nine or more intercostal spaces is an indica-
40kg = 6-10Hz; > 40kg = 5-8Hz. For a term newborn tor of superdistension. MAP may be reduced when
= 12 or 15 Hz and for newborn prematures/ very low alveolar recruitment is considered satisfactory and a
weight =15 Hz; lower transpulmoinary pressure is required to main-
- flow must remain between 15 and 20 L/min, tain the lung open. Verification of the level of pulmo-
depending upon the patient’s size and on the MAP nary recruitment includes evaluation of gas exchange
required. In newborn use flow between 8 and 15 L/ efficiency (rate of oxygenation) need for oxygen and
min; chest X-ray exam. (1,2)
- MAP form 2 to 4 cmH2O above that used for In summary, MAP may be increased from 1 to 2
CMV. MAP can later be increased to achieve SaO 2 ≥ cmH2O until FiO2 < 0.6 with SaO2 between 88-92%
90% with FiO 2 ≤ 0.6. For newborn with diffuse al- in cases of ARDS. In cases of air leak syndrome, use of
veolar disease or air leak syndrome use MAP 3-5 cm- a higher FiO2 (between 80% and 100%) is permitted,
H2O above CMV. An early rescue intervention may especially in the first 12-24 hours to minimize MAP,
be made in newborn using MAP of 10-14 cmH2O. while an adequate SaO 2 is achieved.
In newborn as well as in older children, if SaO2 falls
quickly below 90%, recruit manual ventilation and Elimination of carbon dioxide
gradually increase MAP; Ventilation adjustments are achieved by increasing
- pressure amplitude (ΔP) will be that sufficient pressure amplitude or by reducing frequency, although
to achieve perceptible movement of the thoracic wall elimination of CO2 is more related to amplitude and less
(movement of the thigh root which is easily seen) that with frequency. Change of inspiratory time and flow
may be modified to the desired ventilation levels by increase are other maneuvers that may improve ventila-
evaluating PaCO 2. Changes in frequency also define tion. Amplitude may be changed by a button that con-
alteration in PaCO2 and, to the contrary of what takes trols movement of the electromagnetic piston. Increase
place in CMV, in HFOV there is fall of PaCO 2 when of amplitude results in increase of tidal volume. Con-
FR is diminished. In newborn at term the ΔP can be versely, decrease of amplitude supplies lower tidal vol-
≥ 25 cmH2O ands in prematures/ very low weight can ume e reduces the ventilation minute. Increases of ∆P
be ≥ 16 cmH 2O. from 2–5 cmH2O changes PaCO2 by 3–5 mmHg and
increase of ∆P of more than 5 cmH2O changes PaCO2
VENTILATION HANDLING by 5–10 mmHg. It is appropriate to reduce respiratory
rate only if carbon dioxide arterial pressure (PaCO2) is
Oxygenation refractory to changes of the ∆P.(1,2)
Criteria to transfer a patient from CMV to HFOV Choice of adequate amplitude is essentially re-
vary according to the team’s experience. In general, sultant from visual clinical inspection of the level of
transference is based upon clinical judgment, index movement of the patient’s thoracic wall and measure-
of oxygenation pressure peak that has been needed in ment of blood gases. One characteristic of HFOV is
CMV and disease progression.(1,2) that intensity of the piston movement is inversely re-
Because there is a strict relation between pulmo- lated to frequency, that is to say increased frequency
nary volume and surface area of gas exchange, practi- diminishes movement of the piston with an effective
cally all oxygenation in HFOV depends on MAP and decrease of pressure amplitude and of released tidal
FiO2. When MAP is increased the pulmonary volumes volume. Increase of the inspiratory time leads to in-
are recruited and oxygenation improves up to the op- crease of tidal volume and may improve elimination
timal point, beyond which the lungs become hyper of CO2 e oxygenation.(1)
expanded. If there is superdistension, alveolar capillar- Flow is the determinant of MAP and interferes with
ies are compressed, thereby reducing the gas exchange removal of CO2. Typically, the flow needed to achieve
area and of the PaO 2. Furthermore, a more significant adequate mean airway pressure and maintain adequate
hemodynamic impairment may take place.(1) minute ventilation ranges from 20 to 40 L/min.
Rev Bras Ter Intensiva. 2009; 21(1):96-103
High-frequency oscillatory ventilation in pediatrics and neonatology 101
Radiological examination increase of the ∆P.(10)
The exam must be made one or two hours after - Increase of central venous pressure and pulmo-
beginning and as often as 6 or 8 hours until stabiliza- nary artery occlusion pressure: derived from increase
tion. Later, chest X-ray must be performed daily and of MAP and decrease of venous return. Therefore
after significant parameter changes. The ideal number close attention must be paid to volemic reposition of
of intercostal spaces ranges from eight to nine.(1,2) patients that will go from CMV to HFOV.(1)
- Deep sedation and, sometimes curarization: these
Suction of the tracheal tube conditions may lead to an extended mechanical ven-
Suction of the tracheal tube must be restricted as tilation time and LOS, in addition to polyneuropathy
much as possible, especially in the first 24 hours. This inherent to curarization.(38,39)
procedure must be considered if PaCO2 is progressively - Obstruction of the airways and tracheal tube by
increasing. Consider recruitment maneuver after.(1,2) secretions: complications with 4% to 5% incidence(40)
it is important to promote adequate humidification
Sedation and neuromuscular blockade due to high flow of gas and minute ventilation.
Patients must be deeply sedated at onset of HFOV
using an association of benzodiazepines and opioids. RESUMO
Neuromuscular blockade may be necessary and, when
used must be interrupted daily to assess if it must be Este trabalho teve por objetivo rever a literatura e de-
maintained. Remember that small respiratory efforts screver a utilização da ventilação oscilatória de alta freqüên-
cia em crianças e recém-nascidos. Revisão bibliográfica
that alter MAP less than 5 cmH2O do not require
e seleção de publicações mais relevantes sobre ventilação
deeper sedation and/or neuromuscular blockade un-
de alta freqüência utilizando as bases de dados MedLine
less oxygenation or ventilation are impaired. (1,2) e SciElo publicadas nos últimos 15 anos. As seguintes pa-
lavras-chave foram utilizadas: ventilação oscilatória de alta
Weaning from HFOV freqüência, ventilação mecânica, síndrome do desconforto
∆P must be slowly reduced while an adequate respiratório agudo, crianças e recém-nascidos. Descreveu-
PaCO2 is maintained. MAP might be reduced by 1 to se o emprego da ventilação oscilatória de alta freqüência
2 cmH2O to levels between 15 and 20cmH2O with em crianças com síndrome do desconforto respiratório agu-
good recovery after suction. (1,2) do, síndrome de escape de ar e doença pulmonar obstru-
In newborn ∆P must also be slowly reduced, re- tiva. Avaliou em recém-nascidos, síndrome do desconforto
membering that spontaneous breathing may increase respiratório, displasia broncopulmonar, hemorragia peri-
tidal volume. Just as in older children, in newborn intraventricular, leucoencefalomalácia e extravasamento de
ar. Também, abordou a transição da ventilação mecânica
MAP must be reduced by 1 to 2 cmH 2O. Term new-
convencional para a ventilação de alta freqüência e o manu-
born and prematures must return to HFOV when
seio específico da ventilação de alta freqüência quanto à
MAP is at 10 – 12 cmH 2O.(1,2) oxigenação, eliminação de gás carbônico, realização de ex-
ame radiológico, realização de sucção traqueal e utilização
Complications of high frequency oscillatory de sedação e bloqueio neuromuscular. Foram abordados o
ventilation desmame deste modo ventilatório e as complicações. Em
The main complications of HFOV are the following. crianças maiores a ventilação oscilatória de alta freqüência
- Barotrauma and hemodynamic impairment: com- é uma opção terapêutica, principalmente na síndrome do
plications derived from use of high mean airway pres- desconforto respiratório agudo, devendo ser empregada
sures. Mehta et al.(35) reported prevalence of 21.8% of precocemente. Também pode ser útil em casos de síndrome
pneumothorax and in 26% of patients HFOV had to be de escape de ar e doença pulmonar obstrutiva. Em recém-
discontinued because of hemodynamic problems. How- nascidos, não há evidências que demonstram superioridade
da ventilação oscilatória de alta freqüência em relação à
ever, in two randomized controlled studies(36,37) that com-
ventilação convencional, sendo a síndrome de escape de ar
pared HFOV with CMV, prevalence of pneumothorax
a única situação clínica em que há evidência de melhores
and hypertension were comparable between groups. resultados com este modo ventilatório.
It is also noteworthy that it is challenging to rec-
ognize pneumothorax in patients under HFOV. As- Descritores: Ventilação oscilatória de alta freqüência;
sessment relies on reduction or asymmetry of body Ventilação mecânica; Síndrome do desconforto respiratório
vibration in response to the pressure waves or to an agudo; Criança; Recém-nascido
Rev Bras Ter Intensiva. 2009; 21(1):96-103
102 Fioretto JR, Rebello CM
REFERÊNCIAS extubation directly from high-frequency oscillatory ven-
tilation in an infant with cystic lung disease and persis-
1. Lia Graciano A, Freid EB. High-frequency oscillatory ven- tent air leak: a strategy for lung protection. Respir Care.
tilation in infants and children. Curr Opin Anaesthesiol. 2001;46(3):263-6.
2002;15(2):161-6. 15. Duval EL, van Vught AJ. Status asthmaticus treated by
2. Arnold JH. High-frequency oscillatory ventilation in pe- high-frequency oscillatory ventilation. Pediatr Pulmonol.
diatric patients [Intrnet].[cited 2008 Jan 1]. Available from: 2000;30(4):350-3.
http://www.pedsanesthesia.org/meetings/2006winter/ 16. Kneyber MC, Markhorst DG, van Heerde M, Sibarani-
pdfs/A4_Arnold%20Neonatal%20Ventilation.pdf Ponsen R, Plötz FB. Lessons from pediatric high-fre-
3. Henderson-Smart DJ, Wilkinson A, Raynes-Greenow CH. quency oscillatory ventilation may extend the application
Mechanical ventilation for newborn infants with respira- in critically ill adults. Crit Care Med. 2007;35(10):2472-
tory failure due to pulmonary disease. Cochrane Database 3; author reply 2473. Comment on: Crit Care Med.
Syst Rev. 2002:(4):CD002770. 2007;35(7):1649-54.
4. Dreyfuss D, Saumon G. Ventilator-induced lung injury: 17. Kneyber MC, Plötz FB, Sibarani-Ponsen RD, Markhorst
lessons from experimental studies. Am J Respir Crit Care DG. High-frequency oscillatory ventilation (HFOV) faci-
Med. 1998;157(1):294-323. litates CO2 elimination in small airway disease: the open
5. Chan KP, Stewart TE. Clinical use of high-frequency oscilla- airway concept. Respir Med. 2005;99(11):1459-61.
tory ventilation in adult patients with acute respiratory dis- 18. Slee-Wijffels FY, van der Vaart KR, Twisk JW, Markhorst
tress syndrome. Crit Care Med. 2005;33(3 Suppl):S170-4. DG, Plötz FB. High-frequency oscillatory ventilation in
6. Arnold JH. High-frequency ventilation in the pediatric in- children: a single-center experience of 53 cases. Crit Care.
tensive care unit. Pediatr Crit Care Med. 2000;1(2):93-9. 2005;9(3):R274-9.
7. Imai Y, Slutsky AS. High-frequency oscillatory ventilation 19. Marchak BE, Thompson WK, Duffty P, Miyaki T, Bryan
and ventilator-induced lung injury. Crit Care Med. 2005; MH, Bryan AC, Froese AB. Treatment of RDS by high-
33(3 Suppl):S129-34. frequency oscillatory ventilation: a preliminary report. J
8. Malarkkan N, Snook NJ, Lumb AB. New aspects of ven- Pediatr. 1981;99(2):287-92.
tilation in acute lung injury. Anaesthesia. 2003;58(7):647- 20. Byford LJ, Finkler JH, Froese AB. Lung volume recruit-
67. ment during high-frequency oscillation in atelectasis-pro-
9. Arnold JH, Hanson JH, Toro-Figuero LO, Gutiérrez J, Be- ne rabbits. J Appl Physiol. 1988;64(4):1607-14.
rens RJ, Anglin DL. Prospective, randomized comparison 21. Gerstmann DR, deLemos RA, Clark RH. High-fre-
of high-frequency oscillatory ventilation and conventio- quency ventilation: issues of strategy. Clin Perinatol.
nal ventilation in pediatric respiratory failure. Crit Care 1991;18(3):563-80.
Med. 1994;22(10):1530-9. Comment in: Crit Care Med. 22. High-frequency oscillatory ventilation compared with con-
1994;22(10):1521-4. Crit Care Med. 1995;23(8):1443- ventional mechanical ventilation in the treatment of respi-
5. Crit Care Med. 1995;23(8):1445-6. Crit Care Med. ratory failure in preterm infants. The HIFI Study Group.
1995;23(9):1606. N Engl J Med. 1989;320(2):88-93.
10. Chan KP, Stewart TE, Mehta S. High-frequency oscilla- 23. Moriette G, Paris-Llado J, Walti H, Escande B, Magny JF,
tory ventilation for adult patients with ARDS. Chest. Cambonie G, et al. Prospective randomized multicenter
2007;131(6):1907-16. Review. comparison of high-frequency oscillatory ventilation and
11. Matsuoka T, Kawano T, Miyasaka K. Role of high-fre- conventional ventilation in preterm infants of less than
quency ventilation in surfactant-depleted lung injury as 30 weeks with respiratory distress syndrome. Pediatrics.
measured by granulocytes. J Appl Physiol. 1994;76(2):539- 2001;107(2):363-72.
44. 24. Courtney SE, Durand DJ, Asselin JM, Hudak ML, As-
12. Bouchut JC, Godard J, Claris O. High-frequency oscilla- chner JL, Shoemaker CT; Neonatal Ventilation Study
tory ventilation. Anesthesiology. 2004;100(4):1007-12. Group. High-frequency oscillatory ventilation versus con-
13. Mehta S, Lapinsky SE, Hallett DC, Merker D, Groll RJ, ventional mechanical ventilation for very-low-birth-weight
Cooper AB, et al. Prospective trial of high-frequency os- infants. New Engl J Med. 2002;347(9):643-52. Comment
cillation in adults with acute respiratory distress syndrome. in: N Engl J Med. 2002;347(9):630-1. N Engl J Med.
Crit Care Med. 2001;29(7):1360-9. 2002;347(9):682-4. N Engl J Med. 2003;348(12):1181-2;
14. Seller L, Mullahoo K, Liben S, Lands LC. Weaning to author reply 1181-2. N Engl J Med. 2003;348(12):1181-
Rev Bras Ter Intensiva. 2009; 21(1):96-103
High-frequency oscillatory ventilation in pediatrics and neonatology 103
2; author reply 1181-2. distress syndrome and tracheoesophageal fistula: mana-
25. Johnson AH, Peacock JL, Greenough A, Marlow N, Limb gement with high-frequency ventilation. Crit Care Med.
ES, Marston L, Calvert SA; United Kingdom Oscillation 1990;18(4):447-8.
Study Group. High-frequency oscillatory ventilation for 32. Orlando R 3rd, Gluck EH, Cohen M, Mesologites CG.
the prevention of chronic lung disease of prematurity. New Ultra-high-frequency jet ventilation in a bronchopleural
Engl J Med. 2002;347(9):633-42. Comment in: Evid Ba- fistula model. Arch Surg. 1988;123(5):591-3.
sed Nurs. 2003;6(2):41. N Engl J Med. 2002;347(9):630- 33. Hemmila MR, Napolitano LM. Severe respiratory failure:
1. N Engl J Med. 2002;347(9):682-4. N Engl J Med. advanced treatment options. Crit Care Med. 2006;34(9
2003;348(12):1181-2; author reply 1181-2. Suppl):S278-90.
26. Henderson-Smart DJ, Cools F, Bhuta T, et al. Elective high 34. Higgins J, Estetter B, Holland D, Smith B, Derdak S. High-
frequency oscillatory ventilation versus conventional ven- frequency oscillatory ventilation in adults: respiratory the-
tilation for acute pulmonary dysfunction in preterm in- rapy issues. Crit Care Med. 2005;33(3 Suppl):S196-203.
fants. Cochrane Database Syst Rev. 2007;(3):CD000104. 35. Mehta S, Granton J, MacDonald RJ, Bowman D, Mat-
Review. te-Martyn A, Bachman T, et al. High-frequency oscilla-
27. Clark RH, Yoder BA, Sell MS. Prospective, randomized tory ventilation in adults: the Toronto experience. Chest.
comparison of high-frequency oscillation and conventio- 2004;126(2):518-27.
nal ventilation in candidates for extracorporeal membrane 36. Derdak S. High-frequency oscillatory ventilation for acute
oxygenation. J Pediatr. 1993;124(3):447-54. Comment respiratory distress syndrome in adult patients. Crit Care
in: J Pediatr. 1994;124(3):427-30. Med. 2003;31(4 Suppl):S317-23. Review.
28. Engle WA, Yoder MC, Andreoli SP, Darragh RK, Langefeld 37. Bollen CW, van Well GT, Sherry T, Beale RJ, Shah S, Fin-
CD, Hui SL. Controlled prospective randomized compa- dlay G, et al. High frequency oscillatory ventilation com-
rison of high-frequency jet ventilation and conventional pared with conventional mechanical ventilation in adult
ventilation in neonates with respiratory failure and persis- respiratory distress syndrome: a randomized controlled
tent pulmonary hypertension. J Perinatol. 1997;17(1):3- trial [ISRCTN24242669]. Crit Care. 2005;9(4):R430-9.
9. Comment in: Crit Care. 2005;9(4):339-40.
29. Gonzalez F, Harris T, Black P, Richardson P. Decreased gas 38. Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G,
flow through pneumothoraces in neonates receiving high- Shannon W, Kollef MH. Effect of a nursing-implemented
frequency jet versus conventional ventilation. J Pediatr. sedation protocol on the duration of mechanical ventila-
1987;110(3):464-6. tion. Crit Care Med. 1999;27(12):2609-15. Comment in:
30. Donn SM, Zak LK, Bozynski ME, Coran AG, Oldham Crit Care Med. 1999;27(12):2824-5.
KT. Use of high-frequency jet ventilation in the mana- 39. Latronico N, Peli E, Botteri M. Critical illness myopathy
gement of congenital tracheoesophageal fistula associa- and neuropathy. Curr Opin Crit Care. 2005;11(2):126-
ted with respiratory distress syndrome. J Pediatr Surg. 32. Review.
1990;25(12):1219-21. Comment in: J Pediatr Surg. 40. Fort P, Farmer C, Westerman J, Johannigman J, Beninati
1991;26(6):753-4. W, Dolan S, Derdak S. High-frequency oscillatory ventila-
31. Bloom BT, Delmore P, Park YI, Nelson RA. Respiratory tion for adult respiratory distress syndrome - a pilot study.
Crit Care Med. 1997;25(6):937-47. Comment in: Crit
Care Med. 1997;25(6):906-8.
Rev Bras Ter Intensiva. 2009; 21(1):96-103
You might also like
- Lung Injury in NeonatesDocument9 pagesLung Injury in NeonateszunarodriguezleoNo ratings yet
- Nasal high-frequency ventilation overviewDocument22 pagesNasal high-frequency ventilation overviewdragajojicNo ratings yet
- High Frequency Ventilation in Neonates:, TF F, PC N, KL CDocument8 pagesHigh Frequency Ventilation in Neonates:, TF F, PC N, KL CyennyNo ratings yet
- High Frequency Ventilation - 2021 - Clinics in PerinatologyDocument14 pagesHigh Frequency Ventilation - 2021 - Clinics in PerinatologyCamilaNo ratings yet
- Hfo 2Document9 pagesHfo 2markus_danusantosoNo ratings yet
- Ventilatory Strategies in Obstructive Lung. Parrilla2014Document10 pagesVentilatory Strategies in Obstructive Lung. Parrilla2014EzeBorjesNo ratings yet
- Mechanical Ventilation To Minimize Progression of Lung Injury in Acute Respiratory FailureDocument5 pagesMechanical Ventilation To Minimize Progression of Lung Injury in Acute Respiratory FailureGenoveva Navarro SolorzaNo ratings yet
- Mechanical Ventilation of The Neonate Principles and StrategiesDocument6 pagesMechanical Ventilation of The Neonate Principles and StrategiesKelly HoffmanNo ratings yet
- Modes and Strategies For Providing Conventional Mechanical Ventilation in NeonatesDocument6 pagesModes and Strategies For Providing Conventional Mechanical Ventilation in Neonatesbig023296No ratings yet
- NIV and Chronic Respiratory Failure in ChildrenDocument16 pagesNIV and Chronic Respiratory Failure in ChildrenyyullyyannaNo ratings yet
- Acute Medicine Surgery - 2024 - Hoshino - Future Directions of Lung Protective Ventilation Strategies in AcuteDocument8 pagesAcute Medicine Surgery - 2024 - Hoshino - Future Directions of Lung Protective Ventilation Strategies in AcuteDiego AzevedoNo ratings yet
- Ventilación Del Pulmón Sano CC Current 20Document5 pagesVentilación Del Pulmón Sano CC Current 20Silvia Lorena Mireles GonzálezNo ratings yet
- Niv in Pediatric Patients - Book - GarciaDocument62 pagesNiv in Pediatric Patients - Book - GarciaMary ElizabethNo ratings yet
- 07a2 PDFDocument6 pages07a2 PDFDiana Milena Poveda AriasNo ratings yet
- Lung Recruitment Using Oxygenation during HFVDocument7 pagesLung Recruitment Using Oxygenation during HFVGustavo Carhuamaca RoblesNo ratings yet
- Novel Forms of Ventilation in Neonates Neurally Adjusted VentilatoryDocument16 pagesNovel Forms of Ventilation in Neonates Neurally Adjusted VentilatorydocsaravananNo ratings yet
- VitaminaDocument15 pagesVitaminaCarinka VidañosNo ratings yet
- Airway Pressure Release Ventilation and PediatricsDocument12 pagesAirway Pressure Release Ventilation and PediatricsAndres Felipe BarreraNo ratings yet
- Evidence-based role of high-frequency ventilation in neonatal respiratory failureDocument16 pagesEvidence-based role of high-frequency ventilation in neonatal respiratory failureSiska LesnussaNo ratings yet
- Ventilation During Lung Resection and Critical Care ComparativeDocument11 pagesVentilation During Lung Resection and Critical Care Comparativeema moralesNo ratings yet
- Intraoperative Protective Mechanical Ventilation Fact or FictionDocument3 pagesIntraoperative Protective Mechanical Ventilation Fact or Fictionema moralesNo ratings yet
- Ventilator Settings: For Newborn InfantsDocument6 pagesVentilator Settings: For Newborn InfantsRomeo DevNo ratings yet
- Jurnal RespirasiDocument12 pagesJurnal RespirasiwilmaNo ratings yet
- Fessler - 2010Document12 pagesFessler - 2010Cindy KarmilaNo ratings yet
- Pharmacologictreatments Foracuterespiratory DistresssyndromeDocument17 pagesPharmacologictreatments Foracuterespiratory DistresssyndromeLuis HernándezNo ratings yet
- Ventilatorymanagement Ofthenoninjuredlung: David L. Bowton,, Louis Keith ScottDocument10 pagesVentilatorymanagement Ofthenoninjuredlung: David L. Bowton,, Louis Keith ScottGhost11mNo ratings yet
- Initiationofmechanical Ventilationinpatients Withdecompensatedrespiratory FailureDocument14 pagesInitiationofmechanical Ventilationinpatients Withdecompensatedrespiratory FailureCarolina Polo TorresNo ratings yet
- s1013 70252970039 9Document8 pagess1013 70252970039 9ganesh goreNo ratings yet
- Lung Blast InjuryDocument10 pagesLung Blast InjuryHany ElbarougyNo ratings yet
- Laporan PendahuluanDocument8 pagesLaporan Pendahuluancynthia febri kharismaNo ratings yet
- Volume Targeted VentilationDocument28 pagesVolume Targeted VentilationhosnameskarNo ratings yet
- WWW Minervamedica It@r02y2016n01a0058Document11 pagesWWW Minervamedica It@r02y2016n01a0058Gonzalo Venegas RojasNo ratings yet
- HFNC Where Does It FitDocument4 pagesHFNC Where Does It FitTusar KoleNo ratings yet
- High-Frequency Oscillatory VentilationDocument63 pagesHigh-Frequency Oscillatory VentilationAnonymous G20oAbl6p8No ratings yet
- Wormald2009kandidat 2Document4 pagesWormald2009kandidat 2adeNo ratings yet
- Complicaciones en El PreterminoDocument4 pagesComplicaciones en El PreterminonadisjaviNo ratings yet
- Use of Helmet Cpap in COVID-19 - A Practical ReviewDocument10 pagesUse of Helmet Cpap in COVID-19 - A Practical ReviewDoménica SánchezNo ratings yet
- Advances in Emergent Airway Management in PediatricsDocument19 pagesAdvances in Emergent Airway Management in PediatricsLuis Miguel VillanuevaNo ratings yet
- Lung and Diaphragm Protective Ventilation Guided by The EsophagealDocument3 pagesLung and Diaphragm Protective Ventilation Guided by The Esophagealema moralesNo ratings yet
- Fisiologia de Semin - Fetal - Neon - Med - 2016 - Jun - 21 (3) - 174Document7 pagesFisiologia de Semin - Fetal - Neon - Med - 2016 - Jun - 21 (3) - 174MASIEL AMELIA BARRANTES ARCENo ratings yet
- High Frequency Ventilation NeorevDocument16 pagesHigh Frequency Ventilation NeorevLuis Adolfo Gonzalez GomezNo ratings yet
- Preemptive Mechanical Ventilation (VENTILACION M PREVENTIVA)Document26 pagesPreemptive Mechanical Ventilation (VENTILACION M PREVENTIVA)Jesus FrancoNo ratings yet
- 2022-10# (PEERJ) RR in ECMODocument17 pages2022-10# (PEERJ) RR in ECMOjycntuNo ratings yet
- Falla VentilatoriaaaaaaaaDocument6 pagesFalla VentilatoriaaaaaaaaDIANA CAROLINA OTALORA ALVAREZNo ratings yet
- High-Flow Nasal Cannula Recommendations For Daily Practice in PediatricsDocument7 pagesHigh-Flow Nasal Cannula Recommendations For Daily Practice in PediatricsitomoralesNo ratings yet
- VAFO No Invasivo NiñosDocument12 pagesVAFO No Invasivo NiñosRolando Juan Dávila SalcedoNo ratings yet
- The Baby Lung and The COVID-19 EraDocument3 pagesThe Baby Lung and The COVID-19 EraBlueAbeNo ratings yet
- Acute Respiratory Distress Syndrome in The Pediatric Age - An Update On Advanced Treatment. ChJContPed2014Document11 pagesAcute Respiratory Distress Syndrome in The Pediatric Age - An Update On Advanced Treatment. ChJContPed2014Naye ZMNo ratings yet
- What Is New in Refractory Hypoxemia 2013Document4 pagesWhat Is New in Refractory Hypoxemia 2013EN BUNo ratings yet
- RCT of Aprv Vs LPV in Ards PtsDocument11 pagesRCT of Aprv Vs LPV in Ards PtsOldriana Prawiro HapsariNo ratings yet
- Close Lung 2018Document8 pagesClose Lung 2018Sergio CastellanosNo ratings yet
- Hypercapnia and Acidosis in Sepsis: A Double-Edged Sword?Document11 pagesHypercapnia and Acidosis in Sepsis: A Double-Edged Sword?martinivanNo ratings yet
- Monitoring Asynchrony During Invasive Mechanical VentilationDocument23 pagesMonitoring Asynchrony During Invasive Mechanical VentilationLeonardo PgNo ratings yet
- In Preterm Infants Recovering From Respiratory Failure Effects of Volume-Guaranteed Synchronized Intermittent Mandatory VentilationDocument7 pagesIn Preterm Infants Recovering From Respiratory Failure Effects of Volume-Guaranteed Synchronized Intermittent Mandatory VentilationIkayulianiNo ratings yet
- Acuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiesDocument16 pagesAcuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiessamuelNo ratings yet
- Care of neonates on respiratory supportDocument40 pagesCare of neonates on respiratory supportsyedNo ratings yet
- Neonatal VentilationDocument65 pagesNeonatal VentilationBadr Chaban100% (5)
- Bronchopleural Fistula in The Mechanically Ventilated Patient: A Concise ReviewDocument10 pagesBronchopleural Fistula in The Mechanically Ventilated Patient: A Concise Reviewronsua1966No ratings yet
- Manajemen VentiDocument2 pagesManajemen VentiBos AseNo ratings yet
- Which NCT Baby Guide 2013 PDFDocument25 pagesWhich NCT Baby Guide 2013 PDFmarkus_danusantosoNo ratings yet
- Neonatology Today - Oxygen PDFDocument12 pagesNeonatology Today - Oxygen PDFmarkus_danusantosoNo ratings yet
- The Complete Guide To Baby CarryingDocument6 pagesThe Complete Guide To Baby Carryingmarkus_danusantosoNo ratings yet
- Turvallinen Koti Lapselle enDocument24 pagesTurvallinen Koti Lapselle enmarkus_danusantosoNo ratings yet
- Stroller Safety - Tips For Parents - Mayo ClinicDocument4 pagesStroller Safety - Tips For Parents - Mayo Clinicmarkus_danusantosoNo ratings yet
- Baby SlingDocument20 pagesBaby Slingmarkus_danusantosoNo ratings yet
- Treating: Hypoxic Ischemic Encephalopathy With HypothermiaDocument9 pagesTreating: Hypoxic Ischemic Encephalopathy With Hypothermiamarkus_danusantosoNo ratings yet
- High-frequency Ventilation Settings and MeasurementsDocument4 pagesHigh-frequency Ventilation Settings and Measurementsmarkus_danusantosoNo ratings yet
- Attachment Relationships Quality of Care For Young ChildrenDocument33 pagesAttachment Relationships Quality of Care For Young ChildrenGODEANU FLORINNo ratings yet
- 2013 Mother Baby Center Case StudyDocument6 pages2013 Mother Baby Center Case StudyRohan KashikarNo ratings yet
- ENFAMIL - PrematureDocument17 pagesENFAMIL - Prematuremarkus_danusantosoNo ratings yet
- NIH - Patient Info - Prostate Cancer TreatmentDocument19 pagesNIH - Patient Info - Prostate Cancer Treatmentmarkus_danusantosoNo ratings yet
- Health Professionals Guide To Infant FormulaDocument19 pagesHealth Professionals Guide To Infant Formuladaniela18jNo ratings yet
- Baby Development Stages Guide PDFDocument14 pagesBaby Development Stages Guide PDFmarkus_danusantosoNo ratings yet
- HIE - ImagingDocument73 pagesHIE - Imagingmarkus_danusantosoNo ratings yet
- Full Day Care: National Standards For Under 8s Day Care and ChildmindingDocument36 pagesFull Day Care: National Standards For Under 8s Day Care and ChildmindingvaishalikatkadeNo ratings yet
- Procalcitonin Use in Picu 2013Document5 pagesProcalcitonin Use in Picu 2013markus_danusantosoNo ratings yet
- ENFAMIL - Premature PDFDocument17 pagesENFAMIL - Premature PDFmarkus_danusantosoNo ratings yet
- BPD - DART Regiment DexamethasoneDocument4 pagesBPD - DART Regiment Dexamethasonemarkus_danusantosoNo ratings yet
- Procalcitonin Use in PICU 2013Document3 pagesProcalcitonin Use in PICU 2013Nisa UcilNo ratings yet
- VancomycinDocument9 pagesVancomycinmarkus_danusantosoNo ratings yet
- UHT Milk - 1Document7 pagesUHT Milk - 1markus_danusantosoNo ratings yet
- Probiotics 1Document5 pagesProbiotics 1markus_danusantosoNo ratings yet
- NIH - Professional Info - Prostate Cancer TreatmentDocument83 pagesNIH - Professional Info - Prostate Cancer Treatmentmarkus_danusantosoNo ratings yet
- Red FlagsDocument41 pagesRed Flagsmarkus_danusantosoNo ratings yet
- SupervisionDocument8 pagesSupervisionmarkus_danusantosoNo ratings yet
- Resuscitation - NeopuffDocument11 pagesResuscitation - Neopuffmarkus_danusantosoNo ratings yet
- Resuscitation - AdvancedDocument17 pagesResuscitation - Advancedmarkus_danusantosoNo ratings yet
- TFR ExperimentDocument25 pagesTFR ExperimentSiti Norbaya100% (1)
- Paper Lncs PDFDocument57 pagesPaper Lncs PDFNeilNo ratings yet
- Short Questions... DbmsDocument10 pagesShort Questions... DbmsMuhammad Jamal ShahNo ratings yet
- Siahaan V. Data Science Crash Course... With Python GUI 2ed 2023Document610 pagesSiahaan V. Data Science Crash Course... With Python GUI 2ed 2023ArturNo ratings yet
- Locktronics Technical InformationDocument39 pagesLocktronics Technical InformationJulio Gutierrez ReyesNo ratings yet
- Section I Introduction To Magnetic Particle InspectionDocument130 pagesSection I Introduction To Magnetic Particle Inspectionhvu9743No ratings yet
- 3 D Via Composer Error LogDocument9 pages3 D Via Composer Error LogNilesh A. KhedekarNo ratings yet
- Power Control in Ac Isolated Microgrids With Renewable Energy Sources and Energy Storage SystemsDocument1 pagePower Control in Ac Isolated Microgrids With Renewable Energy Sources and Energy Storage SystemssriluNo ratings yet
- IADC Formula Sheet: X X X + + ÷ X + X - ÷ XDocument5 pagesIADC Formula Sheet: X X X + + ÷ X + X - ÷ XMarwa ElghifaryNo ratings yet
- Astm D1014 PDFDocument4 pagesAstm D1014 PDFabilio_j_vieiraNo ratings yet
- Combo FixDocument4 pagesCombo FixJulio Cesar Camones CastilloNo ratings yet
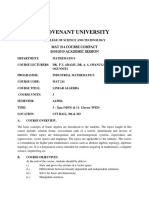
- MAT 214 Course Compact - 18 - 19Document3 pagesMAT 214 Course Compact - 18 - 19seyiNo ratings yet
- Pivot and UnpivotDocument5 pagesPivot and UnpivotSuzan FernandesNo ratings yet
- Soft ComputingDocument38 pagesSoft ComputingGayatri Dilip JuwatkarNo ratings yet
- RPM 00342Document3 pagesRPM 00342Iswahyudi AprilyastonoNo ratings yet
- SmartAir EHVAC System Rev10 Jun2019 2Document40 pagesSmartAir EHVAC System Rev10 Jun2019 2Andy degolNo ratings yet
- Central Corneal Thickness: Ultrasound Pachymetry Verus Anterior Segment Optical Coherence TomographyDocument5 pagesCentral Corneal Thickness: Ultrasound Pachymetry Verus Anterior Segment Optical Coherence TomographybasharatNo ratings yet
- Info - Tech - Uk 09 - 08Document52 pagesInfo - Tech - Uk 09 - 08georossi46No ratings yet
- Bonds Valuation and YtmDocument22 pagesBonds Valuation and YtmarmailgmNo ratings yet
- FPGA Based Implementation of Symmetrical Switching in SVPWM For Three Level NPC ConverterDocument6 pagesFPGA Based Implementation of Symmetrical Switching in SVPWM For Three Level NPC ConvertersateeshNo ratings yet
- Polyethylene Plastic Production ProcessDocument8 pagesPolyethylene Plastic Production Processkiki haikalNo ratings yet
- Design and Analysis of Algorithms Unit IIDocument20 pagesDesign and Analysis of Algorithms Unit IIAyman AymanNo ratings yet
- How To Turn Off or Disable Hardware Acceleration in Windows 11 - 10Document10 pagesHow To Turn Off or Disable Hardware Acceleration in Windows 11 - 10favio lopezNo ratings yet
- Tda2030 PDFDocument6 pagesTda2030 PDFParmeetNo ratings yet
- 1 to 10 DSBDA case studyDocument17 pages1 to 10 DSBDA case studyGanesh BagulNo ratings yet
- MRI ScriptDocument1 pageMRI ScriptPeter BolocelliNo ratings yet
- Introductory Plasma and Fusion Physics: Majid Khan and Muhammad KamranDocument130 pagesIntroductory Plasma and Fusion Physics: Majid Khan and Muhammad Kamrannajeeb ullahNo ratings yet
- Fundamentals of The Analysis of Algorithm EfficiencyDocument38 pagesFundamentals of The Analysis of Algorithm EfficiencyDedi BobNo ratings yet
- 〈1229.8〉 Dry Heat SterilizationDocument2 pages〈1229.8〉 Dry Heat Sterilizationmehrdarou.qaNo ratings yet
- Transformer Winding Resistance and Equivalent CircuitDocument10 pagesTransformer Winding Resistance and Equivalent CircuitM7MD ACADEMIANo ratings yet