Professional Documents
Culture Documents
Biosafety Measures in The Clinical Laboratory
Uploaded by
Denise DeniseOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Biosafety Measures in The Clinical Laboratory
Uploaded by
Denise DeniseCopyright:
Available Formats
overview [generalist | immunology | microbiology and virology | management/administration and training]
Biosafety Measures in the Clinical Laboratory
Peggy Prinz Luebbert, MS, MT(ASCP), CIC, CHSP
From the Department of Risk Management, Alegent Health, Omaha, NE
왘 The Centers for Disease Control and Prevention’s 4 biosafety levels for laboratories handling infectious agents
왘 Basic laboratories, containment laboratories, and maximum containment laboratories
왘 Biologic safety cabinets
Clinical laboratories are special, often unique, work environments that may pose identifiable infectious disease risks to per-
sons in or near them. These infections have been recognized for many years. In a series of published early surveys, Pike and asso-
ciates1-4 reported over 3,000 cases of laboratory-acquired infections, including brucellosis, tuberculosis, typhoid, streptococcal
infections, and hepatitis. These incidents, along with considerable anecdotal information, suggest that most laboratory-acquired
infections occur as a result of error, accident, or carelessness in the handling of a known pathogen; often the mode of transmis-
sion is unknown.
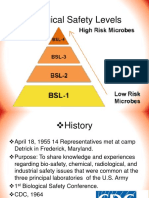
During the 1970s, in an effort to reduce the risks of infection in the laboratory, scientists devised a system for categorizing
etiologic agents into groups based on the mode of transmission, type and seriousness of illness resulting from infection, availabil-
ity of treatment (eg, antimicrobial drugs), and availability of prevention measures (eg, vaccination). The etiologic agent groupings
were the basis for the development of guidelines for appropriate facilities, containment equipment, procedures, and work
practices to be used by laboratorians. These guidelines, now referred to as biosafety levels 1 through 4 [T1], are published and
regularly reviewed by the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH).5
Biosafety level guidelines recognize that facility design is important in providing a barrier to protect persons working in the
facility as well as those in the community. An accidental release of certain airborne infectious agents could be catastrophic. To
assist in planning and managing a laboratory, the CDC describes 3 facility designs based on functions in handling infectious
agents.
Basic Laboratory
The first design, known as the basic laboratory, provides general space in which work is done with viable biosafety level 1
agents (eg, Bacillus subtilis, Naegleria gruberi), which are not associated with disease in healthy adults, and biosafety level 2
agents (eg, hepatitis B, salmonellae), which pose minimal potential aerosol hazard to laboratory personnel and the environment.
Basic laboratories include those that use biosafety levels 1 and 2. While work is commonly conducted on the open bench, certain
operations are confined to biologic safety cabinets. Public areas and general offices to which nonlaboratory staff require frequent
access should be separated from spaces that primarily support laboratory functions. Biosafety level 2 used in the basic laboratory
differs from biosafety level 1 in that:
1. Laboratory personnel have specific training in handling pathogenic agents and are directed by competent scientists;
2. Access to the laboratory is limited when work is being conducted;
3. Extreme precautions are taken with contaminated sharp items; and
4. Certain procedures in which infectious aerosols or splashes may be created are conducted in a biologic safety cabinet or
other physical containment equipment.
There is no specification for single-pass directional inward flow of air (a system in which air goes through the laboratory area
once before being filtered) from a biosafety level 2 laboratory. However, because most microbiology laboratories also work with
potentially hazardous chemicals, negative air pressure is usually present as well. There are published recommendations for pre-
venting buildup of chemical vapors in laboratories, including use of chemical fume hoods and/or single-pass air when recircula-
tion would increase the ambient concentration of hazardous materials.
Containment Laboratory
The containment laboratory has special engineering features that make it possible for laboratory personnel to handle
aerosolized hazardous materials (eg, Mycobacterium tuberculosis, Coxiella burnetii, and St Louis encephalitis virus) without en-
dangering themselves. More emphasis is placed on primary and secondary barriers to protect personnel in contiguous areas and
the community from exposure to potentially infectious aerosols and to prevent contamination of the environment. This laboratory
is usually described as a biosafety level 3 facility.
The unique features that distinguish this laboratory from the basic laboratory are the provisions for access control and a spe- 435
cialized ventilation system. The containment laboratory may be an entire building or a single room (eg, for tuberculosis testing) in
a basic laboratory. A containment laboratory is separated from other parts of the building by an anteroom with 2 sets of doors or
by access through a basic laboratory area. Because of the potential for aerosol transmission, air movement is unidirectional into
the laboratory (ie, from clean areas into the containment area), and all exhaust air is directed outside the building without any re-
circulation, or it undergoes high-efficiency particulate air (HEPA) filtration.
© laboratorymedicine> august 2001> number 8> volume 32
436
laboratorymedicine> august 2001> number 8> volume 32 ©
All procedures involving the manipulation of infectious materials are conducted within biologic safety cabinets or other phys-
ical containment devices. These facilities have solid floors and ceilings and sealed penetrations. They are designed and
maintained to allow appropriate decontamination in the event of a significant spill. All waste from these laboratories must be ren-
dered noninfectious before final disposal.
Maximum Containment Laboratory
The maximum containment laboratory has special engineering and containment features that allow activities associated with
infectious agents (eg, Lassa virus, Ebola virus) that are extremely hazardous to laboratory personnel or that may cause serious
epidemic disease. This laboratory is considered a biosafety level 4 facility. Although the maximum containment laboratory is usu-
ally a separate building, it can be constructed as an isolated area within a building. The laboratory’s distinguishing characteristic
is that is has secondary barriers to prevent hazardous materials from escaping into the environment. Such barriers include sealed
openings into the laboratory, air locks or liquid disinfectant barriers, a clothing-change and shower room contiguous with the lab-
oratory, a double-door autoclave, a biowaste treatment system, a separate ventilation system, and a treatment system to decontam-
inate exhaust air.
Within work areas of the facility, all activities are confined to class III biologic safety cabinets or class II biologic safety cab-
inets used by personnel wearing 1-piece positive-pressure body suits ventilated by a life-support system. Members of the labora-
tory staff have specific and thorough training in handling extremely hazardous infectious agents, and they understand the primary
and secondary containment functions of the standard and special practices, the containment equipment, and the laboratory design
characteristics. They are supervised by competent scientists who are trained and experienced in working with these agents.
All wastes are decontaminated before leaving the maximum containment laboratory, and the exhaust air is passed through
HEPA filters. Except in extraordinary circumstances (eg, suspected hemorrhagic fever), the initial processing of clinical
specimens and identification of isolates can be done safely at a lower level containment. The containment elements are consistent
with the Occupational Safety and Health Administration Bloodborne Pathogen Standard as well as those recommended by the Na-
tional Committee for Clinical Laboratory Standards (M29-A).6,7
Biologic Safety Cabinets
Various laboratory procedures generate aerosols that may spread biohazardous materials in the work area and pose a risk of
infection to personnel. Biologic safety cabinets are used to prevent the escape of aerosols or droplets and to protect the research
product from airborne contamination. These devices are distinct from horizontal or vertical laminar flow hoods, which should
never be used for handling biohazardous, toxic, or sensitizing material. Chemical fume hoods also should not be used for biohaz-
ards as they are solely designed to protect the individual from exposure to chemicals and noxious gases. These chemical fume
hoods are not equipped with HEPA filters. BSCs are designed to protect the individual and the environment from biologic agents
and to protect the specimens and other materials from biologic contamination.
There are 3 general types of BSCs: class I, II, and III [F1] [F2] and [F3].5 There is 1 type of class I BSC. This cabinet is
similar to a chemical fume hood with an inward airflow through the front opening. The exhaust air from the biologic safety cabi-
net is passed through a HEPA filter so that the equipment provides protection for the worker and the public. However, the speci-
mens and other materials are potentially subject to contamination. Class I cabinets are not generally recommended for biohazard
work.
Class II biologic safety cabinets are
designed to protect personnel, the general
public, and the specimen. The
airflow velocity at the face of the work
opening is at least 75 linear feet per minute
(lfpm). Both the supply and the exhaust air
are HEPA filtered. There are 4 types of
class II cabinets (IIA, IIB1, IIB2, and
IIB3). They differ in the amount of recircu-
lation, downflow, and inflow. Usually, all
but IIA are considered satisfactory for bio-
hazard and toxic agents.
Class III cabinets are totally enclosed,
ventilate cabinets of gas-tight construction,
and offer the highest degree of protection 437
from infectious aerosols. They also protect
research materials from biologic contami-
nation. Class III cabinets are most suitable
for work with hazardous agents that require
biosafety level 3 or 4 containment. All op-
erations in the work area of the cabinet are
© laboratorymedicine> august 2001> number 8> volume 32
performed through attached rubber gloves.
The cabinets are operated under negative
pressure. Supply air is HEPA filtered, and
the cabinet exhaust air is filtered by 2
HEPA filters in series or HEPA filtration
followed by incineration, before discharge
outside of the facility.
Every day, new organisms are discov-
ered that could potentially become patho-
genic to the laboratory staff, patients, and
visitors. It is up to the laboratory specialists
in infection control, safety, and microbiol-
ogy to recognize these potential diseases
and handle the organisms according to the
NIH’s most-recent biosafety guidelines.
1. Sulkin SE, Pike RM. Viral infections contracted in the
laboratory. New Engl J Med. 1949;241:205-213.
2. Sulkin SE, Pike RM. Survey of laboratory-acquired
infections. Am J Public Health. 1951;41:769-781.
3. Pike RM, Sulkin SE, Schulze ML. Continuing
importance of laboratory-acquired infections. Am J Public
Health. 1965;55:190-199.
4. Pike RM. Laboratory-associated infections: summary
and analysis of 3921 cases. Health Lab Sci. 1976;13:105-
114.
5. US Department of Health and Human Services,
Biosafety in Microbiological and Biomedical Laboratories.
4th ed. Washington, DC: US Government Printing Office;
1999. Also available at
www.cdc.gov/od/ohs/biosfty/bmbl4/bmbl4toc.htm. Accessed
June 25, 2001.
6. National Committee for Clinical Laboratory Standards
(NCCLS). Protection of Laboratory Workers from Instrument
Biohazards and Infectious Disease Transmitted by Blood, Body
Fluids, and Tissue; M29-A. Wayne: PA: NCCLS; 1997
7. OSHA. Occupational Exposure to Bloodborne
Pathogens; 29 CFR
InterNetConnect
[F2] Class II Cabinets. The Centers for Disease Control and Preven-
tion: <www.cdc.gov>
The National Committee for Clinical Labora-
tory Standards: <www.nccls.org>
438
The Centers for Disease Control and Prevention biosafety Web page: <www.cdc.gov/od/ohs/biosfty/bmbl4toc.htm>
Suggested Reading
laboratorymedicine> august 2001> number 8> volume 32 ©
You might also like
- Pediatric Skills For OT Assistants 3rd Ed.Document645 pagesPediatric Skills For OT Assistants 3rd Ed.Patrice Escobar100% (1)
- Introductory Microbiology Laboratory ManualDocument91 pagesIntroductory Microbiology Laboratory Manualasad bashirNo ratings yet
- BT102 MicrobiologyDocument67 pagesBT102 MicrobiologyHanifullah JanNo ratings yet
- Singapore Electricity MarketDocument25 pagesSingapore Electricity MarketTonia GlennNo ratings yet
- Introductory Microbiology Laboratory Manual PDFDocument91 pagesIntroductory Microbiology Laboratory Manual PDFuti nst100% (2)
- BiosafetyLevels SlidesDocument28 pagesBiosafetyLevels SlidesMazaya's HouseNo ratings yet
- Summary - A Short Course On Swing TradingDocument2 pagesSummary - A Short Course On Swing TradingsumonNo ratings yet
- Practical Manual for Detection of Parasites in Feces, Blood and Urine SamplesFrom EverandPractical Manual for Detection of Parasites in Feces, Blood and Urine SamplesNo ratings yet
- Lecture 1 - Laboratory Management and BiosafetyDocument107 pagesLecture 1 - Laboratory Management and BiosafetyRudairoNo ratings yet
- Chapter 9 Control of Microbial GrowthDocument52 pagesChapter 9 Control of Microbial GrowthMICHELLE GARCIANo ratings yet
- Idmt Curve CalulationDocument5 pagesIdmt Curve CalulationHimesh NairNo ratings yet
- Tekla Structures ToturialsDocument35 pagesTekla Structures ToturialsvfmgNo ratings yet
- Failure of A Gasket During A Hydrostatic TestDocument7 pagesFailure of A Gasket During A Hydrostatic TesthazopmanNo ratings yet
- Biosafety LevelDocument13 pagesBiosafety LevelSunil Bhavsar100% (2)
- Biosafety, Facilities and Design of A Molecular Biology LaboratoryDocument6 pagesBiosafety, Facilities and Design of A Molecular Biology LaboratoryMichal VillanuevaNo ratings yet
- Biorisk Management (Part 2)Document44 pagesBiorisk Management (Part 2)Drafaf MahmoudNo ratings yet
- Biosafety 2020Document37 pagesBiosafety 2020Sara Emad100% (1)
- Module 1 Overview of Biosafety LevelsDocument33 pagesModule 1 Overview of Biosafety LevelsSara Belayineh100% (2)
- Biosafety CabinetDocument32 pagesBiosafety Cabinetvivian kiuNo ratings yet
- Clinical Laboratory Biosafety: Tapeshwar Yadav (Lecturer)Document26 pagesClinical Laboratory Biosafety: Tapeshwar Yadav (Lecturer)Tapeshwar YadavNo ratings yet
- Biosafety BtechDocument3 pagesBiosafety BtechMonika KanojiaNo ratings yet
- Laboratory Biosafety: Pathogenic Microbiology and Virology LaboratoriesDocument27 pagesLaboratory Biosafety: Pathogenic Microbiology and Virology LaboratoriesHafsa SaiyedNo ratings yet
- Biosafety Levels: Submitted To Submitted byDocument16 pagesBiosafety Levels: Submitted To Submitted bySheikh FirdousNo ratings yet
- bmbl5 Sect IIIDocument8 pagesbmbl5 Sect IIIGuillermo GutierrezNo ratings yet
- Adapted From The CDC/NIH 3rd Edition Of: Biosafety in Microbiological and Biomedical LaboratoriesDocument8 pagesAdapted From The CDC/NIH 3rd Edition Of: Biosafety in Microbiological and Biomedical Laboratoriesdipys41No ratings yet
- BIOSAFETYDocument3 pagesBIOSAFETYIbrahim KalokohNo ratings yet
- KCMC Histology Laboratory: Safety ManualDocument12 pagesKCMC Histology Laboratory: Safety Manualdaniel mauyaNo ratings yet
- SOPs and Safety in Microbial Bioenergy and Biofuel LabDocument7 pagesSOPs and Safety in Microbial Bioenergy and Biofuel LabAsad ButtNo ratings yet
- Answer Sheet of BiosafetyDocument3 pagesAnswer Sheet of BiosafetyDebapriya HazraNo ratings yet
- BiosafetyDocument4 pagesBiosafetyDebapriya HazraNo ratings yet
- Lab ManualDocument51 pagesLab ManualGS ShawonNo ratings yet
- Biorisk ManagementDocument1 pageBiorisk Managementhoward.mNo ratings yet
- Biosafety Levels: WWW - Techef.InDocument21 pagesBiosafety Levels: WWW - Techef.InSmk Mahmud KoliNo ratings yet
- Biosafety Ventilation EquipmentDocument53 pagesBiosafety Ventilation EquipmentiqraNo ratings yet
- Module 1 Biosafety Levels PPE EngDocument40 pagesModule 1 Biosafety Levels PPE EngNata ShubladzeNo ratings yet
- Biological Safety Cabinets: By: Ayman FisalDocument49 pagesBiological Safety Cabinets: By: Ayman FisalMojahid Abdelrahman MobarkNo ratings yet
- What Are Biosafety LevelsDocument4 pagesWhat Are Biosafety LevelsBEST DEALS & OFFERSNo ratings yet
- BiohazardsDocument103 pagesBiohazardsAman Preet SinghNo ratings yet
- Microbiology Lab Trans (Prelims)Document35 pagesMicrobiology Lab Trans (Prelims)Dhawell AnnNo ratings yet
- Biological Safety Levels: Endia Ford Lori Gladney Izabella OsakweDocument34 pagesBiological Safety Levels: Endia Ford Lori Gladney Izabella OsakweSheerin Sulthana100% (1)
- Biosafety Levels (BSL-1, BSL-2, BSL-3 and BSL-4) - Microbe NotesDocument23 pagesBiosafety Levels (BSL-1, BSL-2, BSL-3 and BSL-4) - Microbe NotesDr_GSNo ratings yet
- BSL Levels in A LabDocument13 pagesBSL Levels in A LabSyeda Wardah NoorNo ratings yet
- RabinDocument20 pagesRabinKhim AnandNo ratings yet
- BIOSAFETYDocument9 pagesBIOSAFETYYASHIKA raniNo ratings yet
- Bio SaftyDocument4 pagesBio Saftyhawkar omerNo ratings yet
- Fundamental: BiosecurityDocument9 pagesFundamental: BiosecurityAbegail CorpuzNo ratings yet
- Microbiolgy Ii: L. L. Afutu MBCHB, PHDDocument19 pagesMicrobiolgy Ii: L. L. Afutu MBCHB, PHDCosmos OcranNo ratings yet
- Biosafety Cabinet AND Personal Protective EquipmentDocument30 pagesBiosafety Cabinet AND Personal Protective Equipmentgacruz1010No ratings yet
- White Paper: Biosafety and Blood Borne Pathogen Safety in The LaboratoryDocument4 pagesWhite Paper: Biosafety and Blood Borne Pathogen Safety in The LaboratoryDanielleNo ratings yet
- Pubpol122 Presentation1 ContagionDocument67 pagesPubpol122 Presentation1 ContagionKeanu BellamyNo ratings yet
- Basic Concepts On Laboratory Biosafety-Converted - 1040766564Document49 pagesBasic Concepts On Laboratory Biosafety-Converted - 1040766564johaylie porrasNo ratings yet
- BIOSAFETY SEMINAR (Dec10)Document42 pagesBIOSAFETY SEMINAR (Dec10)aprilNo ratings yet
- Good Laboratory PracticesDocument4 pagesGood Laboratory PracticesMd Arifuzzaman ArifNo ratings yet
- Background: Biological LaboratoriesDocument4 pagesBackground: Biological LaboratoriesmuncadamonicaNo ratings yet
- Lecture 6 Laboratory Safety in MicrobiologyDocument47 pagesLecture 6 Laboratory Safety in MicrobiologyPurplesmilezNo ratings yet
- Module 2 Q3 ExperimentingDocument23 pagesModule 2 Q3 ExperimentingSilvina Marie LacierdaNo ratings yet
- 9 BMBL Criteria For BSL-1,2,3 - 0Document40 pages9 BMBL Criteria For BSL-1,2,3 - 0sidparikh254No ratings yet
- bt102 Vu Oxford Handout ShopDocument67 pagesbt102 Vu Oxford Handout ShopHaier GuruNo ratings yet
- Laboratory Safety and Basic Laboratory EquipmentsDocument40 pagesLaboratory Safety and Basic Laboratory EquipmentsAurora Mae AmoresNo ratings yet
- Sanitization TechniquesDocument5 pagesSanitization TechniquesMark BedaniaNo ratings yet
- 3.2.3.P LbHygPPEDocument30 pages3.2.3.P LbHygPPEsayoni.nokia.1998No ratings yet
- BiosafetyDocument6 pagesBiosafetyمصطفى رسول هاديNo ratings yet
- Introduction To BiosafetyDocument45 pagesIntroduction To BiosafetyleejiajingNo ratings yet
- Assignment QMS 1Document3 pagesAssignment QMS 1giripratima379No ratings yet
- Bio SafetyDocument27 pagesBio SafetyShruti VermaNo ratings yet
- Laboratory Biosafety Measures Involving SARS-CoV-2 and The Classification As A Risk Group 3 Biological AgentDocument6 pagesLaboratory Biosafety Measures Involving SARS-CoV-2 and The Classification As A Risk Group 3 Biological AgentDenise DeniseNo ratings yet
- Biosafety Measures at The Dental Office After The Appearance of Covid19 A Systematic ReviewDocument5 pagesBiosafety Measures at The Dental Office After The Appearance of Covid19 A Systematic ReviewMaria SilvaNo ratings yet
- Previous Article Next Article: 10.1039/D0QM00255K Mater. Chem. FrontDocument43 pagesPrevious Article Next Article: 10.1039/D0QM00255K Mater. Chem. FrontDenise DeniseNo ratings yet
- Two-Dimensional Transition Metal Dichalcogenides - Synthesis, Biomedical Applications and Biosafety EvaluationDocument13 pagesTwo-Dimensional Transition Metal Dichalcogenides - Synthesis, Biomedical Applications and Biosafety EvaluationDenise DeniseNo ratings yet
- The 13th Annual Conference of The Asia-Pacific Biosafety Association Was Held in Beijing On August 30, 2018Document1 pageThe 13th Annual Conference of The Asia-Pacific Biosafety Association Was Held in Beijing On August 30, 2018Denise DeniseNo ratings yet
- Esporotricose Zoonótica Procedimentos de BiossegurançaDocument10 pagesEsporotricose Zoonótica Procedimentos de BiossegurançaDenise DeniseNo ratings yet
- Delivery and Biosafety of Oncolytic VirotherapyDocument15 pagesDelivery and Biosafety of Oncolytic VirotherapyDenise DeniseNo ratings yet
- Ijms 20 00929 v2Document30 pagesIjms 20 00929 v2Denise DeniseNo ratings yet
- The 13th Annual Conference of The Asia-Pacific Biosafety Association Was Held in Beijing On August 30, 2018Document1 pageThe 13th Annual Conference of The Asia-Pacific Biosafety Association Was Held in Beijing On August 30, 2018Denise DeniseNo ratings yet
- Previous Article Next Article: 10.1039/D0QM00255K Mater. Chem. FrontDocument43 pagesPrevious Article Next Article: 10.1039/D0QM00255K Mater. Chem. FrontDenise DeniseNo ratings yet
- Two-Dimensional Transition Metal Dichalcogenides - Synthesis, Biomedical Applications and Biosafety EvaluationDocument13 pagesTwo-Dimensional Transition Metal Dichalcogenides - Synthesis, Biomedical Applications and Biosafety EvaluationDenise DeniseNo ratings yet
- Thnov 10 P 8996Document36 pagesThnov 10 P 8996Denise DeniseNo ratings yet
- Biosafety Measures in The Clinical LaboratoryDocument4 pagesBiosafety Measures in The Clinical LaboratoryDenise DeniseNo ratings yet
- 21-Cyto A 24280Document14 pages21-Cyto A 24280Denise DeniseNo ratings yet
- Journal of Biosafety and Biosecurity: Feng W, Haixia Ma, Amei Deng, Zongsheng C, Zhiming YDocument7 pagesJournal of Biosafety and Biosecurity: Feng W, Haixia Ma, Amei Deng, Zongsheng C, Zhiming YDenise DeniseNo ratings yet
- 21 1 s2.0 S2588933819300366 MainDocument1 page21 1 s2.0 S2588933819300366 MainDenise DeniseNo ratings yet
- 21 1 s2.0 S2588933821000066 MainDocument6 pages21 1 s2.0 S2588933821000066 MainDenise DeniseNo ratings yet
- 21 1 s2.0 S2588933819300366 MainDocument1 page21 1 s2.0 S2588933819300366 MainDenise DeniseNo ratings yet
- Potential For Laboratory Exposures To Biohazardous PDFDocument5 pagesPotential For Laboratory Exposures To Biohazardous PDFD 1No ratings yet
- Journal of Biosafety and Biosecurity: Dingzhong Sun, Linhuan Wu, Guomei FanDocument7 pagesJournal of Biosafety and Biosecurity: Dingzhong Sun, Linhuan Wu, Guomei FanDenise DeniseNo ratings yet
- Journal of Biosafety and Biosecurity: Research ArticleDocument4 pagesJournal of Biosafety and Biosecurity: Research ArticleDenise DeniseNo ratings yet
- Journal of Cleaner Production: Ramesh Renganath Rao, Murali Sathish, Jonnalagadda Raghava RaoDocument20 pagesJournal of Cleaner Production: Ramesh Renganath Rao, Murali Sathish, Jonnalagadda Raghava RaoDenise DeniseNo ratings yet
- Journal of Biosafety and BiosecurityDocument5 pagesJournal of Biosafety and BiosecuritypratiwiNo ratings yet
- Potential For Laboratory Exposures To Biohazardous PDFDocument5 pagesPotential For Laboratory Exposures To Biohazardous PDFD 1No ratings yet
- Biossegurança em Laboratórios Biomédicos e de Microbiologia - MS, 2004Document290 pagesBiossegurança em Laboratórios Biomédicos e de Microbiologia - MS, 2004Nathanna MateusNo ratings yet
- 2007 Guideline For Isolation PrecautionsDocument100 pages2007 Guideline For Isolation PrecautionsD 1No ratings yet
- 2007 Guideline For Isolation PrecautionsDocument100 pages2007 Guideline For Isolation PrecautionsD 1No ratings yet
- X HM11 S Manual AUpdfDocument228 pagesX HM11 S Manual AUpdfAntonio José Domínguez CornejoNo ratings yet
- Fcode 54 en El SytucDocument2 pagesFcode 54 en El SytucAga MenonNo ratings yet
- Annisha Jain (Reporting Manager - Rudrakshi Kumar)Document1 pageAnnisha Jain (Reporting Manager - Rudrakshi Kumar)Ruchi AgarwallNo ratings yet
- G JaxDocument4 pagesG Jaxlevin696No ratings yet
- Mathematics 2 First Quarter - Module 5 "Recognizing Money and Counting The Value of Money"Document6 pagesMathematics 2 First Quarter - Module 5 "Recognizing Money and Counting The Value of Money"Kenneth NuñezNo ratings yet
- Ewellery Ndustry: Presentation OnDocument26 pagesEwellery Ndustry: Presentation Onharishgnr0% (1)
- Sikkim Manipal MBA 1 SEM MB0038-Management Process and Organization Behavior-MQPDocument15 pagesSikkim Manipal MBA 1 SEM MB0038-Management Process and Organization Behavior-MQPHemant MeenaNo ratings yet
- Coursework For ResumeDocument7 pagesCoursework For Resumeafjwdxrctmsmwf100% (2)
- The Voice of The Villages - December 2014Document48 pagesThe Voice of The Villages - December 2014The Gayton Group of ParishesNo ratings yet
- S SSB29 - Alternator Cables PM: WARNING: This Equipment Contains Hazardous VoltagesDocument3 pagesS SSB29 - Alternator Cables PM: WARNING: This Equipment Contains Hazardous VoltagesMohan PreethNo ratings yet
- Rideable Segway Clone - Low Cost and Easy Build: Digital MPU6050 Accelerometer/gyro IMU BoardDocument45 pagesRideable Segway Clone - Low Cost and Easy Build: Digital MPU6050 Accelerometer/gyro IMU BoardpaolaNo ratings yet
- Charlemagne Command ListDocument69 pagesCharlemagne Command ListBoardkingZeroNo ratings yet
- Nasoya FoodsDocument2 pagesNasoya Foodsanamta100% (1)
- Brother Fax 100, 570, 615, 625, 635, 675, 575m, 715m, 725m, 590dt, 590mc, 825mc, 875mc Service ManualDocument123 pagesBrother Fax 100, 570, 615, 625, 635, 675, 575m, 715m, 725m, 590dt, 590mc, 825mc, 875mc Service ManualDuplessisNo ratings yet
- A.2 de - La - Victoria - v. - Commission - On - Elections20210424-12-18iwrdDocument6 pagesA.2 de - La - Victoria - v. - Commission - On - Elections20210424-12-18iwrdCharisse SarateNo ratings yet
- Ap06 - Ev04 Taller en Idioma Inglés Sobre Sistema de DistribuciónDocument9 pagesAp06 - Ev04 Taller en Idioma Inglés Sobre Sistema de DistribuciónJenny Lozano Charry50% (2)
- Self-Instructional Manual (SIM) For Self-Directed Learning (SDL)Document28 pagesSelf-Instructional Manual (SIM) For Self-Directed Learning (SDL)Monique Dianne Dela VegaNo ratings yet
- Bell WorkDocument26 pagesBell WorkChuột Cao CấpNo ratings yet
- Gogte Institute of Technology: Karnatak Law Society'SDocument33 pagesGogte Institute of Technology: Karnatak Law Society'SjagaenatorNo ratings yet
- A Perspective Study On Fly Ash-Lime-Gypsum Bricks and Hollow Blocks For Low Cost Housing DevelopmentDocument7 pagesA Perspective Study On Fly Ash-Lime-Gypsum Bricks and Hollow Blocks For Low Cost Housing DevelopmentNadiah AUlia SalihiNo ratings yet
- Drug Study TemplateDocument2 pagesDrug Study TemplateKistlerzane CABALLERONo ratings yet
- 7933-Article Text-35363-1-10-20230724Document8 pages7933-Article Text-35363-1-10-20230724Ridho HidayatNo ratings yet
- ACC403 Week 10 Assignment Rebecca MillerDocument7 pagesACC403 Week 10 Assignment Rebecca MillerRebecca Miller HorneNo ratings yet
- Strength and Microscale Properties of Bamboo FiberDocument14 pagesStrength and Microscale Properties of Bamboo FiberDm EerzaNo ratings yet