Professional Documents
Culture Documents
Case Report
Uploaded by
muthia khairunnisaOriginal Title
Copyright
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCase Report
Uploaded by
muthia khairunnisaInternational Journal of Science and Research (IJSR)
ISSN: 2319-7064
Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296
Woman with Acute Heart Failure et Causa
Peripartum Cardiomyopathy - A Case Report
Fidiya Septi, MD1, Abaham Ali, MD, FIHA2
Jemursari Islamic Hospital, Surabaya, Indonesia
Abstract: Peripartum cardiomyopathy (PPCM) is a type of dilatative cardiomyopathy, which is characterized by heart failure due to
left ventricular systolic dysfunction at the end of pregnancy or several months after delivery. Incidence of PPCM is low at 0.1% in
pregnancy, but the morbidity and mortality are quite high between 5-32%. In some women, clinical and echocardiography can improve
return to normal conditions, but in some other women can develop into heart failure and sudden cardiac death. This case was reported a
woman with PPCM came with acute heart failure after five months of childbirth. Patients had no complaints of dyspneu before and
during pregnancy, and no previous history of hypertension before. One week after giving birth the patient complained of dyspneu, after
getting therapy the patient never came back to control. Five months later the patient came with a more severe complaint of dyspneu, leg
edema and ascites. Where the results of echocardiography showed a lower ejection fraction that is <32.68%. Changes in normal
pregnancy make PPCM onset easily covered and unknown, because of similar manifestations. Prognosis of PPCM is associated with
improving of ventricular function. Failure of heart size returns to normal is associated with mortality and morbidity. Early diagnosis
and the latest therapies for heart failure have an important role in reducing PPCM mortality and morbidity.
Keywords: cardiomyopathy, peripartum cardiomyopathy, dilatative cardiomyopathy
1. Introduction were obtained; LV dilatation, segmental normokinetic LV
and LV ejection fraction of 60%. After two days of
Peripartum Cardiomyopathy based on the National Heart treatment the patient's condition improved. The patient is
and Blood Institute and the Office of Rare Diseases of the then allowed to go home with oral therapy Digoxin,
National Institute of Healthy Heart failure caused by left Furosemid, Valsartan, Spironolactone. Patient complaints
ventricular systolic dysfunction that occurs during late improved and never came back for follow-up.
pregnancy and five months after postpartum without other
causes of heart failure and disease beforehand.(1) Incidence The patient came to our emergency room complaint a
of PPCM was low at 0.1% in pregnancy, but the morbidity dyspneu. Her vital sign, blood pressure was 120/70 mmHg,
and mortality were quite high between 5-32%. The diagnosis pulse was 120 bpm regular, RR was bpm, temperature was
of PPCM is often late because PPCM symptoms are not 36.2 C, and saturation was 99% with 3 lpm nasal
specific, especially in late pregnancy. In some women, oxygenation. On physical examination there was increased
clinical and echocardiography can improve until returning to jugular venous pressure, wet ronkhi in both lungs, limb
normal conditions, but in some other women can develop edema and ascites. ECG images have sinus tachycardia HR
into heart failure and sudden cardiac death. Therefore bpm, and Left Axis Deviation. X-ray shows cardiomegaly
caution regarding the symptoms of peripartum with pulmonary congestive and pleural effusion. Results of
cardiomyopathy needs to be improved. Early diagnosis and laboratory tests, Leukocytes 8.000 / uL, Hemoglobin levels
the latest therapies for heart failure have an important role in 15.3 g / dl, Thrombocytes 203.000/ uL, Hematocrit 45.1%.
reducing PPCM mortality and morbidity. Sodium electrolyte results of 147.8 meq / L, Potassium 3.5
meq / L, Chloride 108.7 meq / L, Albumin content 3.7 g / dl,
2. Case Report blood urea 7.9 mg / dl, and creatinine clearance 0.78 mg / dl.
The latest echocardiography result was all chamber
A 43-year-old woman came to the emergency room with dilatation, global segmental LV hypokinetic with LV
complaints of dyspneu, leg edema and ascites. Complaints ejection fraction of 32.68%. The patient had acute heart
have become increasingly in the past five months. Patients failure therapy with 3 lpm O2 nasal oxygenation, 0.9% NaCl
complain of fatigue easily during activity, coughing and IVFD 1000cc / 24 hours, and a urine catheter.
waking during sleep due to tightness. History of chest pain Pharmacological therapy is given Furosemid pump 5 mg /
and previous dyspneu is denied. The patient said there had hour, Nitrate 5 mg orally three times a day, and Candesartan
never been a history of hypertension or diabetes mellitus orally 4 mg twice a day. First day of treatment the patient
before, had never found a lump in the neck. The patient five still complained of dyspneu but had begun to diminish, leg
months ago had a labour in a sectarian section at another edema and ascites also diminished. Monitoring urine
hospital. During pregnancy until the last trimester there are production of 650cc / 24 hours. For therapy, diuretics are
no symptoms of pre-eclampsia, only complaints of mild replaced with intravenous diuretics three times a day.
dyspneu such as normal complaints at the end of pregnancy. Second day there were no complaints of dyspneu, swelling
Before surgery the blood pressure rose 150/90 mmHg, and in the legs and ascites. Monitoring of urine production of
occasional PVC images were obtained on 450 cc / 2 hours, patients were given additional Carvedilol
electrocardiography. Then the patient is consulted with a oral therapy of 6.25 mg at night. On the third day the patient
cardiologist. Chest radiography results from cardiomegaly was as stable and improved. Patients go home after three
with pulmonary congestion. From echocardiography results days of hospital treatment with Furosemid home therapy 40
mg in the morning, Candesartan 4 mg twice a day, Nitrate 5
Volume 7 Issue 9, September 2018
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: ART20191433 DOI: 10.21275/ART20191433 1127
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296
mg three times a day, Spironolactone 25 mg in the morning, women with PPCM. However clinically indistinguishable
Carvedilol 6.25 mg at night. between women with or without myocarditis. (7)
3. Discussion Abnormal immune response to fetal microchimerism (fetal
cells in the maternal circulation) is thought to be one of the
Definition causes of PPCM. This theory is supported because during
The commonly used defiition of PPCM from the National pregnancy fetal cells are released into the mother's
Heart and Blood Institute and the Office of Rare Diseases of bloodstream and there is no rejection reaction due to natural
the National Institute of Healthy are heart failure caused by immune suppression that occurs during pregnancy.
left ventricular systolic dysfunction that occurs during late However, after delivery, when fetal cells attach to
pregnancy and 5 months after postpartum without any other myocardial tissue a pathological autoimmune response can
cause of heart failure and other previous illnesses. (1) The occur, causing PPCM in the mother after delivery. (7)
latest definition submitted from the working group on the
PPCM of the Heart Failure Association of European Society During pregnancy, blood volume and cardiac output
of Cardiology is simpler by removing time constraints. increase. Vascular smooth muscles experience relaxation so
Peripartum cardiomyopathy is an idiopathic cardiomyopathy afterload decreases. This causes reversible left ventricular
which shows the presence of heart failure caused by left hypertrophy to meet the needs of the mother and baby.
ventricular systolic dysfunction at the end of pregnancy or Temporary left ventricular dysfunction during the third
several months after delivery, where no other cause of heart trimester and the beginning of the postpartum period, can
failure is found. This is an exclusion criterion. The left return to normal after giving birth in a normal pregnancy.
ventricle can not be dilated but the ejection fraction almost PPCM is thought to occur due to a drastic reduction in
always falls below 45%. (2) ventricular function when there is a change in
hemodynamics during pregnancy. (4)
Epidemiology
Incidence of PPCM is quite low at 0.1% in pregnancy, but Increased plasma concentrations of inflammatory cytokines
the morbidity and mortality are quite high between 5-32%. including tumor necrosis factor α (TNF-α; C-reactive protein
In some women, clinical and echocardiography can improve (CRP); and Fas / Apo-1, plasma markers of apoptosis, have
until returning to normal conditions, but in some other been identified in PPCM. Fas / Apo-1 levels, ligands found
women can develop into heart failure and sudden cardiac on the surface of protein cells that play a key role in
death. Incidence of peripartum cardiomyopathy varies, apoptosis, is higher in women with PPCM compared to
which has been reported in Haiti: 1 in 299 live births, 1 in healthy women. (3)
2229 live births in California and 1 in 4000 live births in the
United States. This wide variation is due to geographical Hilfiker-Kleiner et al found the mechanism of new
differences and reporting patterns, besides access to pathogenesis in PPCM, namely an increase in prolactin
echocardiography causes overestimation of this case. Some production. The amount of prolactin is associated with
risk factors that can cause pregnant women to experience increased blood volume, decreased blood pressure,
PPCM include increased maternal age, multiparity and decreased angiotensin response and decreased amount of
pregnancy with preeclampsia or gestational hypertension. (3) water, sodium and potassium. Research shows that PPCM in
Demakins et al and Brar et al found that African American mice has specific deletions in STAT3 in cardiomyocytes. In
women were 2.9 times more affected by PPCM. compared women with PPCM, the STAT3 protein level is low in the
to white women and 7 times more than Hispanic women. heart and the number of cathepin D serum and 16-kD
Greater incidence of hypertension in African-Americans prolactin increases. (8)
may cause this. (4,5)
The use of prolonged tocolytic is the use of
Etiology and Patophysiology sympathomimetic agents for more than 4 weeks. Lamper et
Peripartum cardiomyopathy is a form of idiopathic primary al found an association between the use of tocolytic therapy
myocardial disease associated with pregnancy. Although and the development of pulmonary edema in pregnant
several etiological mechanisms have been proposed but none women and the relationship between the use of beta
of them are definite etiologies. (6) PPCM is distinguished sympathomimetics and PPCM. (9)
from other cardiomyopathies because of the occurrence
associated with pregnancy. Many etiological processes are Clinical Manifestation and Diagnosis
thought to be the cause of PPCM, namely viral myocarditis, Changes in normal pregnancy such as increased blood
abnormal immune response related to pregnancy, volume, increased metabolic requirements, mild anemia,
maladaptive response to hemodynamic stress during changes in vascular resistance associated with mild
pregnancy, stress-activated cytokines, excessive prolactin ventricular dilatation and increased cardiac output. All of
expression, prolonged use of tocolytic and malnutrition. The these conditions that make PPCM onset can be easily
European Society of Cardiology classifies PPCM as a non- masked and unknown, because of its similar. Women with
familial, non-genetic form of dilatative cardiomyopathy. (3) PPCM are often found to be congested, tired during activity,
dizziness, chest pain, cough, limb edema, increased jugular
Viral myocarditis is the main mechanism thought to be the veins, pulmonary crackles, and heart sounds S3. Symptom
cause of PPCM and was first reported by Goulet and severity varies from New York Association Functional Class
Melvin, who found myocarditis in myocardial biopsy of 3 I to IV. However classes III and IV are the most frequent.
Life-threatening complications include refractory heart
Volume 7 Issue 9, September 2018
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: ART20191433 DOI: 10.21275/ART20191433 1128
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296
failure, cardogenic shock, severe ventricular arrhythmias, differential diagnoses. (10) Cardiac magnetic resonance
multiorgan failure, thromboembolism, and death. (10) imaging (MRI) can be a complement to echocardiography,
especially with suboptimal echocardiographic features.
In this case the patient came to the emergency room with
complaints of dyspeu, swelling of the legs, fatigue easily Management
when active and coughing and tightness if lying down. PPCM management is similar to other forms of heart failure.
Patients come already in a state of increasingly severe heart However, special attention is needed to the safety of women
failure which is found signs of left heart congestion and and the excretion of drugs or metabolites during labor until
right heart. On physical examination there was increased the process of breastfeeding after delivery. The main goal of
jugular venous pressure, wet ronkhi in both lungs, limb managing heart failure is to improve hemodynamic status,
edema and ascites. The patient came already in a state of reduce signs and symptoms, and optimize long-term
heart failure class NYHA III-IV. outcomes. Reducing preload with vasodilators such as
important nitrates which are mostly safe in pregnancy and
The diagnosis of PPCM is often late because PPCM breastfeeding. Diuretics are also important for reducing
symptoms are not specific, especially in late pregnancy. preload, but attention must be given to reducing intavascular
PPCM should be considered in peripartum women with volume, thereby reducing the blood supply to the uterus and
signs and symptoms of heart failure or patients who are long also to the fetus. Management will focus on reducing
recovering. Family history needs to be cultivated further to preload and afterload and increasing inotropic. Management
find out familial patterns in cardiomyopathy. Some non- is generally divided into management when patients with
specific electrocardiograms in PPCM show non-specific compensated heart failure and acute heart failure. Ideal
abnormalities, prolonged QT-intervals, QRS dilation, left management is hidralazine, nitrate, digoxin, and diuretics.
ventricular hypertrophy and atrial fibrillation. Some Angiotensin-converting enzyme inhibitors (ACE-i) are
laboratory tests are also important but not specific to PPCM. contraindicated during labor because of their teratogenicity
(11)
but this therapy is the main PPCM therapy after delivery for
decreased afterload. Aldosterone antagonists are effective
In this case, at early post-partum complaint of the patient when ACE is not tolerated but cannot be given during
was only mild dyspneu, and foot swelling was also pregnancy. (3)
considered a normal complaint in the postpartum mother.
This makes the patient ignore the complaint. Awareness of Beta adrenergic antagonists such as metoprolol and
signs and symptoms and adherence to therapy can affect the carvedilol can be given to PPCM and can increase life
patient's prognosis. At the beginning of echocardiographic expectancy. Beta blockers should not be given in the early
complaints showed LV dilatation, segmental LV stages of PPCM because they can reduce perfusion in acute
normokinetic and 60% Ejection Fraction. Five months heart failure. Digoxin as an inotropic agent is also safe to use
without therapy and monitoring of jatung patients in more during pregnancy, is recommended for pregnant women
severe conditions. Where can we find all chamber dilatation, with left ventricular systolic dysfunction and an ejection
global segmental LV hypokinetic with Ejection Fraction fraction of less than 40% with a failure. The following
<32.68%. guidelines for compensated heart failure on PPCM. The
following guidelines for the management of compensated
Recent studies regarding biomarkers that may be specific to heart failure in PPCM. (3)
PPCM include 16-kDa prolactin, microRNA-146a, soluble-
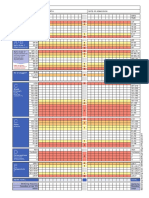
like tyrosine kinase-1 has been found, although the Table 1: Management of peripartum cardiomyopathy with
diagnostic value in clinical practice still requires compensated heart failure(3)
verification. BNP or NT-pro BNP levels (N-terminal pro- Non Pharmaceutical Therapies
brain natriuretic peptide). Plasma BNP or NT-pro BNP Low-sodium diet: limit of 2 g sodium per day
concentrations have high sensitivity to inclusion, and high Fluid restriction: 2 L/day
specificity to exclude heart failure. Despite significant Light daily activity: if tolerated (eg, walking)
hemodynamic stress, BNP or NT pro-BNP does not increase Antepartum Management of PPCM
Beta blocker : Carvedilol, Metoprolol
during normal pregnancy. BNP and NT pro-BNP increased Vasodilator: Hydralazine
not significantly in preeclampsia while in PPCM it increased Digoksin.
significantly. (11) Thiazide diuretic: Hidroklorotiazide
Postpartum Management of PPCM
Chest X-rays should be performed on patients with Angiotensin-converting enzyme (ACE) inhibitor
suspected PPCM. This X-ray can help if there is pulmonary Captopril, Enalapril, Ramipril, Lisinopril
edema, cardiomegaly, pulmonary congestion and pleural Angiotensin-receptor blocker (bila ACE-I tidak mampu
effusion. Echocardiography is a non-invasive examination menoleransi)
and a serial evaluation examination is needed in pregnant Candesartan, Valsartan
Vasodilator
women. In women with PPCM consistently found heart
Hydralazine, Isosorbid Dinitrat
failure, namely a decrease in ejection fraction, global Aldosterone antagonist
dilatation, and thinning of the heart wall. (3) Spironolacton, Eplerenone
Echocardiographic criteria in PPCM namely LV end Beta blockerCarvedilol, Metoprolol
diastolic dimension <2.7 cm / m2 and M-mode Fractional Warfarin (jika fraksi ejeksi <35%)
shortening <30% or left ventricular ejection fraction <45%.
Echocardiography can be used to exclude multiple
Volume 7 Issue 9, September 2018
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: ART20191433 DOI: 10.21275/ART20191433 1129
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296
Management of PPCM patients with acute heart failure starts failure, both left and right heart congestive. The prognosis of
from the airway, breathing and cycles. Assessment of the PPCM is positively associated with improving ventricular
airway is very important because of excessive intravascular function. Women with persistent ventricular dysfunction are
volume pregnancy. Respiratory needs to be assisted with more difficult to survive and return to normal heart function
additional oxygenation to reduce the signs and symptoms of compared to women with increased left ventricular function.
hypoxemia and measure continuous oxygen saturation. Early diagnosis, serial examination, and the latest therapy
Blood pressure monitoring and fetal monitoring need to be for heart failure are expected to play an important role in
done. Pharmacologically can be given intravenous diuretics reducing PPCM mortality and morbidity.
with attention, vasodilators and inotropic agents. Furosemide
is given with consideration of creatinine clearance and References
nitroglycerin given according to clinical status and blood
pressure. [1] Pearson GD, Veille JC, Rahimtoola S et al. 2000.
Peripartum cardiomyopathy: National Heart, Lung, and
In this case, patient had acute heart failure therapy with 3 Blood Institute and Office of Rare Diseases (National
lpm O2 nasal oxygenation, 0.9% NaCl IVFD 1000cc / 24 Institutes of Health) workshop recommendations and
hours, and a urine catheter. Pharmacological therapy is given review. JAMA 283, 1183–1188.
Furosemid pump 5 mg / hour, Nitrate 5 mg orally three [2] Sliwa K, Hilfiker-Kleiner D, Petrie MC et al. 2010.
times a day, and Candesartan orally 4 mg twice a day. First Current state of knowledge on aetiology, diagnosis,
day of treatment the patient still complained of dyspneu but management, and therapy of peripartum
had begun to diminish, leg edema and ascites also cardiomyopathy: a position statement from the Heart
diminished. Monitoring urine production of 650cc/24 hours. Failure Association of the European Society of
Furosemid pump was replaced with intravenous diuretics Cardiology Working Group on peripartum
three times a day. The second day monitoring of urine cardiomyopathy. Eur. J. Heart Fail. 12, 767–778.
production 450 cc/24 hours, patients were given additional [3] Johnson-Coyle, L, Jensen, L, Sobey, A, American
Carvedilol oral therapy of 6.25 mg at night. Patients College of Cardiology, F & American Heart, A, 2012.
discharge after three days of hospitalized with take home Peripartum Cardiomyopathy: review and practice
therapy Furosemid 40 mg in the morning, Candesartan 4 mg guidelines. Am J Crit Care, 21, 89-98.
twice a day, Nitrate 5 mg three times a day, Spironolactone [4] Mielniczuk LM, Williams K, Davis DR et al. 2006.
25 mg in the morning, Carvedilol 6.25 mg at night. This Frequency of peripartum cardiomyopathy. Am. J.
patient showed a good therapeutic response and clinical Cardiol. 97, 1765–1768.
symptoms disappeared for 3 days of treatment. [5] Fett JD, Christie LG, Carraway RD, Murphy JG.
2005. Five-year prospective study of the incidence and
Prognosis prognosis of peripartum cardiomyopathy at a single
The prognosis of PPCM is positively associated with institution. Mayo Clin. Proc. 80, 1602–1606.
improving ventricular function. Failure of heart size to [6] Mishra, VN, Mishra, N & Devanshi, 2013. Peripartum
return to normal size is associated with mortality and Cardiomyopathy. J Assoc Physicians India, 61, 268-73.
morbidity. Women with persistent ventricular dysfunction [7] Anshari, AA, Fett, JD, Carraway, RE, Mayne, AE,
are more difficult to survive and return to normal heart Onlamoon, N & Sundstrom, JB, 2002. Autoimmune
function compared to women with increased left ventricular mechanisms as the basis for human peripartum
function. Sliwa et al said ejection fraction is a strong cardiomyopathy. Clin Rev Allergy Immunol, 23, 301-24.
pedicler of outcomes in women with PPCM. (12) Abboud et [8] Hilfiker-Kleiner, D, Kaminski, K, Podewski, E,
al. reported 50% of women with PPCM returned to normal Bonda, T, Schaefer, A, Sliwa, K, Foster, O, Quint, A,
ventricular function within 6 months after giving birth. (13) Landmesser, U, Doerries, C, Luchtefeld, M, Poli, V,
Medical therapy according to the ACCF / AHA guidelines Schneider, MD, Balligand, JL, Desjardins, F, Ansari,
should continue if the heart function had not returned to A, Struma, I, Nguyen, NQ, Zschemisc, NH, Klein, G,
normal. Early diagnosis and the latest therapy for heart Heusch, G, Schulz, R, Hilfiker, A & Drexler, H,
failure have an important role in reducing PPCM mortality 2007. A cathepsin D-cleaved 16 kDa form of prolatin
and morbidity. Attention must also be given to subsequent mediates postpartum cardiomyopathy. Cell, 128, 589-
pregnancies in patients with improved PPCM. Improvement 600.
of left ventricular function is a predictor for subsequent [9] Lampert, MB, Hibbard, J, Weinert, L, Briller, J,
pregnancy. (14) Lindheimer, M & Lang, RM, 1993. Peripartum heart
failure associated with prolonged tocolytic therapy. Am.
Resume Obstet Gynecol, 168,493-5.
PPCM occurs in women at the end of pregnancy or a few [10] Kim, MJ & Shin, MS, 2017. Practical management of
months after giving birth, which previously had no other peripartum cardiomyopathy. Korean J Intern Md, 32,
heart disease. Changes during normal pregnancy are almost 393-403.
the same as the initial onset of PPCM signs and symptoms [11] Russell, KSaSD, 2015. An Update on Peripartum
so that the diagnosis becomes late. The patient can ignore Cardiomyopathy in the 21st Century. Int J Clin Cardiol
the initial complaint until the complaint becomes more 2015, 2:3.
severe. As in these patients, the initial mild complaint with [12] Sliwa, K, Skudicky D, Bergemann A, Candy G,
ejection fraction was still good at 60%, in five months the Puren A, Sareli P. 2000. Peripartum cardiomyopathy:
complaint became more severe until the ejection fraction analysis of clinical outcome, left ventricle function,
<32.68%. Patients come already in a state of acute heart
Volume 7 Issue 9, September 2018
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: ART20191433 DOI: 10.21275/ART20191433 1130
International Journal of Science and Research (IJSR)
ISSN: 2319-7064
Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296
plasma level cytokines and Fas/Apo-1. J Am Cardiol.
35:701-705.
[13] Abboud J, Murad Y, Chen-Scarabelli C, Saravolatz
L, Scarabelli TM. 2007.Peripartum Cardiomyopathy: a
comprehensive review. Int J Cardiol. 118(3):295-303.
[14] Brar SS, Khan SS, Sandhu GK, et al. 2007.
Incidence, mortality, and racial differences in
peripartum cardiomyopathy. Am J Cardiol. 100(2):302-
304.
Volume 7 Issue 9, September 2018
www.ijsr.net
Licensed Under Creative Commons Attribution CC BY
Paper ID: ART20191433 DOI: 10.21275/ART20191433 1131
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Kjim 2016 360Document11 pagesKjim 2016 360berriandi_arwanNo ratings yet
- News in SurgeryDocument9 pagesNews in Surgerymuthia khairunnisaNo ratings yet
- News in SurgeryDocument9 pagesNews in Surgerymuthia khairunnisaNo ratings yet
- NEWS2 Chart 3 - NEWS Observation Chart - 0Document1 pageNEWS2 Chart 3 - NEWS Observation Chart - 0muthia khairunnisaNo ratings yet
- Peripheral Vascular Disease Surgical PresentationDocument26 pagesPeripheral Vascular Disease Surgical PresentationqreenNo ratings yet
- NEWS2 Chart 1 - The NEWS Scoring System - 0 - 0Document1 pageNEWS2 Chart 1 - The NEWS Scoring System - 0 - 0Flouria Stefanny SimatupangNo ratings yet
- Physical Examination Vascular System: of TheDocument63 pagesPhysical Examination Vascular System: of TheyuniayuuuNo ratings yet
- Neonatal Sepsis Highlighting The Principles of Dia PDFDocument5 pagesNeonatal Sepsis Highlighting The Principles of Dia PDFmuthia khairunnisaNo ratings yet
- Tutor A21Document8 pagesTutor A21muthia khairunnisaNo ratings yet
- Review Article: Postcoital Bleeding: A Review On Etiology, Diagnosis, and ManagementDocument9 pagesReview Article: Postcoital Bleeding: A Review On Etiology, Diagnosis, and ManagementAnonymous i9mBoeOuNo ratings yet
- Jurnal EKG Abnormal Arif Rahman HakimDocument8 pagesJurnal EKG Abnormal Arif Rahman Hakimmuthia khairunnisaNo ratings yet
- Teknik Sungai Dan Rawa-05Document60 pagesTeknik Sungai Dan Rawa-05muthia khairunnisaNo ratings yet
- Lampiran Perhitungan Bab IvDocument5 pagesLampiran Perhitungan Bab Ivmuthia khairunnisaNo ratings yet
- Viral MeningitisDocument6 pagesViral Meningitismuthia khairunnisaNo ratings yet
- 1.c. What's The Impact of Shortness of Breath? AnswerDocument7 pages1.c. What's The Impact of Shortness of Breath? Answermuthia khairunnisaNo ratings yet
- Thacypnea PDFDocument4 pagesThacypnea PDFmuthia khairunnisaNo ratings yet
- Art 40930 PDFDocument13 pagesArt 40930 PDFBrahma MishraNo ratings yet
- SPSSDocument5 pagesSPSSmuthia khairunnisaNo ratings yet
- Jawaban Hakim Sken ADocument3 pagesJawaban Hakim Sken Amuthia khairunnisaNo ratings yet
- MUBESDocument2 pagesMUBESmuthia khairunnisaNo ratings yet
- Laporan Tugas Pengenalan Profesi Blok Xvi Sistem Sensoris Dan Integumentum "Identifikasi Gangguan Pendengaran Di Ypac"Document1 pageLaporan Tugas Pengenalan Profesi Blok Xvi Sistem Sensoris Dan Integumentum "Identifikasi Gangguan Pendengaran Di Ypac"muthia khairunnisaNo ratings yet
- Laporan Penanggungjawaban Lomba Cepat Tepat Spices 2018 FK Um PalembangDocument1 pageLaporan Penanggungjawaban Lomba Cepat Tepat Spices 2018 FK Um Palembangmuthia khairunnisaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Controlled Delivery SystemsDocument12 pagesControlled Delivery SystemsSusan NyaguthiìNo ratings yet
- Clinical Pharmacology of Dobutamine and Dopamine in Preterm NeonatesDocument9 pagesClinical Pharmacology of Dobutamine and Dopamine in Preterm Neonatesmateri posNo ratings yet
- Clinical Research Regulatory Associate in Philadelphia PA Resume Deborah BaldwinDocument3 pagesClinical Research Regulatory Associate in Philadelphia PA Resume Deborah BaldwinDeborahBaldwinNo ratings yet
- Final NeuronotesDocument16 pagesFinal Neuronotesapi-479939114No ratings yet
- Tugas Mandiri Babak 8 Pasien Safety 2Document4 pagesTugas Mandiri Babak 8 Pasien Safety 2Andy NuriyantoNo ratings yet
- Gordon Feldman at 01 - 14 - 2023 09 - 19 PMDocument5 pagesGordon Feldman at 01 - 14 - 2023 09 - 19 PMschoolgirl7796No ratings yet
- Pradeep Project FileDocument25 pagesPradeep Project FilePradeep DhakadNo ratings yet
- Bioisosterismo - RevisãoDocument27 pagesBioisosterismo - RevisãoCLARA VITORIA CAVALCANTE CARVALHONo ratings yet
- Fmge Plan For June 2021Document4 pagesFmge Plan For June 2021holaNo ratings yet
- Drug Study (Aspirin)Document3 pagesDrug Study (Aspirin)Mae Therese B. MAGNONo ratings yet
- Anticoagulant Drugs (HEPARIN)Document1 pageAnticoagulant Drugs (HEPARIN)KyrrielJimenoCeladaNo ratings yet
- Cushing's Syndrome, Addison's Disease and Hyperparathyroidism.Document29 pagesCushing's Syndrome, Addison's Disease and Hyperparathyroidism.pranjl100% (1)
- Phytochemistry and Pharmacology of PhyllanthusDocument25 pagesPhytochemistry and Pharmacology of PhyllanthusGREESTYNo ratings yet
- Sacubitril/Valsartan (Entresto) : Safe Prescribing and Use ofDocument1 pageSacubitril/Valsartan (Entresto) : Safe Prescribing and Use ofpatricia wageyNo ratings yet
- Daftar Penawaran Harga PT Galoeh Husada Farma APRIL 2021Document2 pagesDaftar Penawaran Harga PT Galoeh Husada Farma APRIL 2021puskesmas tarokanNo ratings yet
- Aflac, Lumico, RNA Product InfoDocument12 pagesAflac, Lumico, RNA Product InfoJeromy KovatanaNo ratings yet
- 83 Siadh2 PDFDocument8 pages83 Siadh2 PDFAnonymous QNYOxtHNo ratings yet
- Drugfacts MdmaDocument5 pagesDrugfacts MdmaЕкатерина ДрагомирецкаяNo ratings yet
- Antibiotics FluoroquinolonesDocument35 pagesAntibiotics Fluoroquinolonesmirza_baig_46No ratings yet
- Promotional Medical Education Writer in New York City Resume Louise RozikDocument2 pagesPromotional Medical Education Writer in New York City Resume Louise RozikLouiseRozikNo ratings yet
- Shredder Capacity - Bio Medical WasteDocument3 pagesShredder Capacity - Bio Medical WasteYasser FathiNo ratings yet
- Tocolytic DrugDocument11 pagesTocolytic DrugWan Ahmad FaizFaizalNo ratings yet
- Pengenceran InjeksiDocument6 pagesPengenceran InjeksiMaria Wiji PangestuNo ratings yet
- Drug Lab Interaction FinalDocument133 pagesDrug Lab Interaction FinalJunnin Gay GarayNo ratings yet
- Obsessive-Compulsive Disorder Case Study - Group 3 (REVISED)Document41 pagesObsessive-Compulsive Disorder Case Study - Group 3 (REVISED)Mariah Ainna B. MatienzoNo ratings yet
- Flutivate e CreamDocument9 pagesFlutivate e Creamseema sharmaNo ratings yet
- Central Nervous System Concept Map (Ling)Document1 pageCentral Nervous System Concept Map (Ling)Jacob Kennedy LipuraNo ratings yet
- 2-1 Pharmaceutical Product Development 2340644 - 635535097882656250Document39 pages2-1 Pharmaceutical Product Development 2340644 - 635535097882656250Nadia PerezNo ratings yet
- Literature CitedDocument6 pagesLiterature CitedFlora Fauna FlavourNo ratings yet
- 3/2 CBC - Na - K - Crea - TPAG - CXR Post Intubation - ABG - Eta GscsDocument2 pages3/2 CBC - Na - K - Crea - TPAG - CXR Post Intubation - ABG - Eta GscserikaNo ratings yet