Professional Documents
Culture Documents
Accelerating Cervical Cancer Control and Prevention
Uploaded by
derr barrCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Accelerating Cervical Cancer Control and Prevention
Uploaded by
derr barrCopyright:
Available Formats
Comment
Accelerating cervical cancer control and prevention
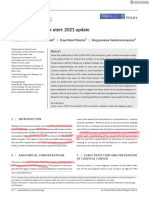
Cervical cancer is probably the best understood and Firstly, vaccination of young girls has no short-term Lancet Public Health 2017
most preventable of all major human malignancies. The effect on cancer rates because of the 30–40 years’ period Published Online
December 18, 2017
progressive steps of this disease—human papillomavirus from first HPV infection to invasive cervical cancer, the http://dx.doi.org/10.1016/
(HPV) infection, progression to precancer, and invasion— reduction of cervical cancer resulting from vaccination S2468-2667(17)30242-6
See Online/Articles
are well described (figure).1 Sexual transmission of causal of girls aged 12–13 years will manifest only decades later.
http://dx.doi.org/10.1016/
HPV infections is ubiquitous but the rates of cervical Secondly, as a direct consequence, screening will remain S2468-2667(17)30222-0
cancer vary widely, inversely related to the effectiveness very important for decades. Lastly, the cancer burden will
of prevention programmes. Almost 90% of deaths occur
in low-income and middle-income countries. In high-
Infection Progression Invasion
income countries, cervical cancer has been relatively Normal HPV Precancer Cervical
well controlled by expensive but effective prevention infection cancer
Clearance Regression
programmes based on cervical cytology screening.2
Discovery of HPV as the causative agent of most
Population prevalence* (%)
cervical cancers has led to two novel and highly
efficacious prevention methods: prophylactic HPV
vaccination to control the early peak of infections and
sensitive HPV-based screening to detect and treat the
secondary peak of precancers.2 With current preventive
0 10 20 30 40 50 60 70
methods, it is technically feasible to control cervical
Age (years)
cancer globally. The speed and degree of control that is
Current approach in high-resource settings
achieved depends on how vaccination and screening is
implemented. Two-dose vaccination
In The Lancet Public Health, Alejandra Castanon and
colleagues3 use a health decision model to estimate HPV screening and triage,
followed by colposcopy
cervical cancer incidence in England, UK, under four and biopsy
different scenarios of implementation of vaccination 0 10 20 30 40 50 60 70
and screening programmes. The authors developed a Age (years)
[multiple screening rounds with intervals varying by age]
pragmatic model, combining age cohort modelling,
observed individual level data, and microsimulation Alternative approach
data for unobservable disease states to estimate future
One-dose vaccination
cancer incidence. The model addresses relatively minor
modifications in the existing, high-quality prevention
HPV screening
programme in England and projects slight changes in (with triage)
the already low cervical cancer burden in the coming
0 10 20 30 40 50 60 70
decades, until vaccinated cohorts reach the age of Age (years)
cancer incidence.3 Most importantly, Castanon and [single screen or few screening rounds]
colleagues show that HPV screening leads to further Figure: Cervical cancer aetiology and prevention approaches
Cervical cancer can arise from infection with one of a dozen carcinogenic HPV types. Infection is sexually acquired,
reduction of cancer incidence compared with cytology,
with a peak transmission of causal infections in late adolescence and early adulthood (green). More than 90% of
and that earlier introduction of HPV screening could infections are suppressed within months to a few years by cell-mediated immunity; the small percentage of
infections that persist lead to typically slow-growing cervical precancers whose incidence peaks from
prevent 1400 cases of cervical cancers. However, the approximately ages 25–40 years (blue). A sizeable minority of precancers eventually acquires invasive potential,
model clearly shows that in places where the cumulative and cancers represent a third peak increasing about age 40 years and extended over the course of decades (red).
Prevention in high-resource countries focuses on the strategies associated with individual-level protection. In the
lifetime incidence is already less than 1%, additional alternative approach, individual efficacy is not the objective; but rather reduced endemicity is the target, which can
substantial reductions are difficult. be achieved without demanding maximum long-term durability of immune response. At the same time,
introduction of at least one or two highly sensitive screens using HPV testing is targeted to the ages of peak
Several findings from this study are important occurrence of cervical precancer, and before the typical ages of invasive cancer. HPV=human papillomavirus.
because they have implications for other settings. *Curves are not to scale and so units are not shown.
www.thelancet.com/public-health Published online December 18, 2017 http://dx.doi.org/10.1016/S2468-2667(17)30242-6 1
Comment
shift to older women because the population is ageing quickly. Importantly, recent data suggest that a single
and older birth cohorts do not receive vaccination. dose of the HPV vaccine might induce a sufficiently
The greatest burden of cervical cancer lies in low- effective and durable immune response against HPV
resource settings that currently have neither vaccination to break transmission networks and rapidly attack the
nor screening programmes. The modelling presented by hyperendemicity of HPV .8
the authors shows that a very different strategy focused This combined cancer control strategy abandons
on cancer reduction is needed in high-risk, low-resource optimal individual-level protection in an HPV-endemic
regions, where waiting decades to control cervical cancer world to protecting individuals as part of the herd
incidences in women is not acceptable. Yet, efforts to (ie, decreasing the chance that a sexual encounter will
introduce vaccination and screening in these settings result in infection). On a global perspective, this strategy
have typically imitated approaches from high-resource will probably save many more lives than introducing
settings. Vaccination programmes are emphasising vaccination to young girls only or than further
maximal individual vaccine efficacy, which is achieved improving screening in high-resource settings such as
when vaccination is administered to young girls before England.
onset of sexual activity. Screening is targeting all dozen
carcinogenic HPV types, despite the strong variation in *Nicolas Wentzensen, Mark Schiffman
risk of individual types4 and the paucity of infrastructure Division of Cancer Epidemiology and Genetics, National Cancer
Institute, Bethesda, MD 20892-9774, USA
to manage all the women testing positive. Without
wentzenn@mail.nih.gov
actually focusing on low-resource settings, the model
We are employed by the National Cancer Institute, which has received cervical
by Castanon and colleagues suggests that such an cancer screening assays in-kind or at reduced cost from Becton Dickinson,
approach will not lead to a reduction of cervical cancer Cepheid, Hologic, and Roche for cervical cancer screening studies.
before decades, failing to address the immediate need Copyright © The Author(s). Published by Elsevier Ltd. This is an Open Access
article under the CC BY 4.0 license.
and the predicted increase of cervical cancer incidences 1 Schiffman M, Wentzensen N. Human papillomavirus infection and the
in countries most at need of control efforts. multistage carcinogenesis of cervical cancer. Cancer Epidemiol Biomarkers
Prev 2013; 22: 553–60.
An alternative approach has been proposed that can 2 Schiffman M, Doorbar J, Wentzensen N, et al. Carcinogenic human
accelerate cancer control in low-resource regions.5,6 papillomavirus infection. Nat Rev Dis Primers 2016; 2: 16086.
3 Castanon A, Landy R, Pesola F, Winridge P, Sasieni P. Prediction of cervical
It focuses on achieving high population coverage of cancer incidence in England, UK, up to 2040, under four scenarios:
vaccination to reduce HPV endemicity in adolescents a modelling study. Lancet Public Health 2017; published online Dec 18.
http://dx.doi.org/10.1016/S2468-2667(17)30222-0.
and young adults, and introduction of HPV screening to 4 Schiffman M, Hyun N, Raine-Bennett TR, et al. A cohort study of cervical
screening using partial HPV typing and cytology triage. Int J Cancer 2016;
detect and treat prevalent precancers in women. Herd 139: 2606–15.
immunity is emphasised and maximised by vaccination 5 Bosch FX, Robles C, Díaz M, et al. HPV-FASTER: broadening the scope for
prevention of HPV-related cancer. Nat Rev Clin Oncol 2016; 13: 119–32.
of a wider age range, during which most causal HPV 6 Salmerón J, Torres-Ibarra L, Bosch FX, et al. HPV vaccination impact on a
infections are acquired, up to age 30 years or even cervical cancer screening program: methods of the FASTER-Tlalpan Study
in Mexico. Salud Publica Mex 2016; 58: 211–19.
older.5,7 Importantly, herd immunity was not considered 7 Burger EA, Kim JJ, Sy S, Castle PE. Age of acquiring causal human
in the model by Castanon and colleagues, highlighting papillomavirus (HPV) Infections: leveraging simulation models to explore
the natural history of HPV-induced cervical cancer. Clin Infect Dis 2017;
a need to adapt this decision model to low-resource 65: 893–99.
settings. Despite lower individual efficacy, population 8 Kreimer AR, Struyf F, Del Rosario-Raymundo MR, et al. Efficacy of fewer
than three doses of an HPV-16/18 AS04-adjuvanted vaccine: combined
effectiveness of vaccination by reduction of endemicity analysis of data from the Costa Rica Vaccine and PATRICIA Trials.
Lancet Oncol 2015; 16: 775–86.
can achieve high coverage and herd immunity
2 www.thelancet.com/public-health Published online December 18, 2017 http://dx.doi.org/10.1016/S2468-2667(17)30242-6
You might also like
- Figo 2018Document15 pagesFigo 2018EJ CMNo ratings yet
- FIGO 2018 - Cervical CADocument15 pagesFIGO 2018 - Cervical CAJP RecioNo ratings yet
- The Management and Prevention of Anal Squamous Cell CarcinomaDocument10 pagesThe Management and Prevention of Anal Squamous Cell CarcinomaGabriela LemNo ratings yet
- 1 s2.0 S2050052119301015 MainDocument10 pages1 s2.0 S2050052119301015 MainELSA DÍAZ LÓPEZNo ratings yet
- Proposal For Cervical Cancer Screening in The EraDocument11 pagesProposal For Cervical Cancer Screening in The EraBushra Altaf ChowdhuryNo ratings yet
- Kyambogo University Faculty of EngineeringDocument17 pagesKyambogo University Faculty of EngineeringiangarvinsNo ratings yet
- 35 CA CervikDocument6 pages35 CA CervikluthfiNo ratings yet
- 242 FullDocument5 pages242 FullsarahNo ratings yet
- Analysis of The Determinants of Low Cervical CanceDocument8 pagesAnalysis of The Determinants of Low Cervical CanceMWANGINo ratings yet
- 1 s2.0 S2666679022000040 MainDocument14 pages1 s2.0 S2666679022000040 MainRahmayantiYuliaNo ratings yet
- Intl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDocument17 pagesIntl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateKim RamirezNo ratings yet
- 1 s2.0 S0140673620300684 MainDocument16 pages1 s2.0 S0140673620300684 MainShabrina Amalia SuciNo ratings yet
- Cervical Cancer ESMODocument12 pagesCervical Cancer ESMOAndrei CorhaNo ratings yet
- Evidence To Recommendation Table 1 Dose Vs 2 DoseDocument12 pagesEvidence To Recommendation Table 1 Dose Vs 2 DoseTân NguyễnNo ratings yet
- OBGYN Invasive Cervical Cancer ArticleDocument7 pagesOBGYN Invasive Cervical Cancer ArticleVanessa HermioneNo ratings yet
- Tatalaksana Dan Pencegahan - Hal 29-38 - Cancer of The Cervix Uteri 2021 UpdateDocument17 pagesTatalaksana Dan Pencegahan - Hal 29-38 - Cancer of The Cervix Uteri 2021 UpdateAl-Amirah ZainabNo ratings yet
- Intl J Gynecology Obste - 2021 - BhatlaDocument17 pagesIntl J Gynecology Obste - 2021 - BhatlaKalaivathanan VathananNo ratings yet
- Artigo Sobre CancerDocument10 pagesArtigo Sobre CancerSérgio Anick da Silva Brito SegundoNo ratings yet
- FIGO CANCER REPORT 2021 - Cancer of The Cervix Uteri 2021 Update 2021Document17 pagesFIGO CANCER REPORT 2021 - Cancer of The Cervix Uteri 2021 Update 2021amrodriguez9No ratings yet
- Pap IntroductionDocument390 pagesPap IntroductionAnish VeettiyankalNo ratings yet
- Oup Accepted Manuscript 2017Document12 pagesOup Accepted Manuscript 2017Yohana Novelia ChristinNo ratings yet
- Cancer de Vulva Revision 2021Document12 pagesCancer de Vulva Revision 2021torresgaliciajesusNo ratings yet
- Development of Electrochemical Biosensor For Breast Cancer Detection Using Gold Nanoparticle Doped CA 15-3 Antibody and Antigen InteractionDocument7 pagesDevelopment of Electrochemical Biosensor For Breast Cancer Detection Using Gold Nanoparticle Doped CA 15-3 Antibody and Antigen InteractionwardaninurindahNo ratings yet
- Cervical Cancer - An Overview of Pathophysiology and ManagementDocument9 pagesCervical Cancer - An Overview of Pathophysiology and ManagementIndah 15No ratings yet
- Seminars in Oncology NursingDocument9 pagesSeminars in Oncology NursingangelitostorresitosNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: Backgroundbehanges71No ratings yet
- 10 1097@aog 0000000000001708Document20 pages10 1097@aog 0000000000001708oodarkfireooNo ratings yet
- Intl J Gynecology Obste - 2021 - OlawaiyeDocument12 pagesIntl J Gynecology Obste - 2021 - OlawaiyeKalaivathanan VathananNo ratings yet
- Ijgo 12193Document5 pagesIjgo 12193Aarthi S JayrajNo ratings yet
- 2020 HSIl en VacunadasDocument7 pages2020 HSIl en VacunadasFrancisco DomínguezNo ratings yet
- Project Title High Risk HPV Genotyping in Patient With Clinically Suspected Precancerous and Cancerous Lesions of CervixDocument16 pagesProject Title High Risk HPV Genotyping in Patient With Clinically Suspected Precancerous and Cancerous Lesions of CervixEmam MursalinNo ratings yet
- Comment: Lancet Oncol 2019Document2 pagesComment: Lancet Oncol 2019Afriade yolandaNo ratings yet
- ACTN4-자궁경부암 관계 입증 논문-2Document17 pagesACTN4-자궁경부암 관계 입증 논문-2김승훈(이과대학 화학)No ratings yet
- e Tarjome E17331Document6 pagese Tarjome E17331فاطمه سادات قربانیNo ratings yet
- Cervical CancerDocument14 pagesCervical CancerAlejandra MurilloNo ratings yet
- 244 FullDocument23 pages244 FullNur Ghaliyah SandraNo ratings yet
- Human Papillomavirus (HPV) Nucleic Acid Amplification Tests (Naats) To Screen For Cervical Pre-Cancer Lesions and Prevent Cervical CancerDocument6 pagesHuman Papillomavirus (HPV) Nucleic Acid Amplification Tests (Naats) To Screen For Cervical Pre-Cancer Lesions and Prevent Cervical CancerDr.Sivakumar SelvarajNo ratings yet
- Intl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDocument17 pagesIntl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDamian BarrancoNo ratings yet
- 1 s2.0 S0002937815014520 MainDocument6 pages1 s2.0 S0002937815014520 Mainilham wildanNo ratings yet
- Will HPV Vaccination Prevent Cervical Cancer?: Claire P Rees, Petra Brhlikova and Allyson M PollockDocument15 pagesWill HPV Vaccination Prevent Cervical Cancer?: Claire P Rees, Petra Brhlikova and Allyson M PollockGina Ionescu AnculeteNo ratings yet
- Intl J Gynecology Obste - 2018 - Adams - Cancer of The VaginaDocument8 pagesIntl J Gynecology Obste - 2018 - Adams - Cancer of The VaginaBattleAppleNo ratings yet
- 2 - Cancer of The Vagina 2021 UpdateDocument9 pages2 - Cancer of The Vagina 2021 UpdateMarcell InfanteNo ratings yet
- Cancer CervicalDocument16 pagesCancer CervicalSilvia Cerda RodríguezNo ratings yet
- Self-Sampling HPV Cervical CancerDocument5 pagesSelf-Sampling HPV Cervical CancerLyka MahrNo ratings yet
- Retrieve 2Document23 pagesRetrieve 2monicayangwNo ratings yet
- Cervical Cancer Research 1Document9 pagesCervical Cancer Research 1tivaNo ratings yet
- Human Papilloma Virus Vaccine For Cervical Cancer PreventionDocument9 pagesHuman Papilloma Virus Vaccine For Cervical Cancer Preventionsayeef khanNo ratings yet
- Knowledge, Attitude and Practice Toward Cervical Cancer and Cervical Cancer Screening and Its Associated Factors Among Women in The City of Bamenda, CameroonDocument17 pagesKnowledge, Attitude and Practice Toward Cervical Cancer and Cervical Cancer Screening and Its Associated Factors Among Women in The City of Bamenda, CameroonEditor IJTSRDNo ratings yet
- Research Paper About Cervical CancerDocument4 pagesResearch Paper About Cervical Cancergw1357jx100% (1)
- Cie 10Document11 pagesCie 10Gabriella MGNo ratings yet
- Bullet Point CANCER CervicouterinoDocument20 pagesBullet Point CANCER CervicouterinoDaniela DuránNo ratings yet
- Ca CervixDocument20 pagesCa CervixNathy MontoyaNo ratings yet
- Density and Tailored Breast Cancer Screening: Practice and Prediction - An OverviewDocument12 pagesDensity and Tailored Breast Cancer Screening: Practice and Prediction - An Overviewelisabeth harahapNo ratings yet
- Journal Pone 0296107Document20 pagesJournal Pone 0296107ayoub.khlifiNo ratings yet
- Pap SmearDocument8 pagesPap Smearvyvie89No ratings yet
- ACOG Cervical Cancer ScreeningDocument20 pagesACOG Cervical Cancer ScreeningAlan Ahlawat SumskiNo ratings yet
- Introducing Human Papillomavirus (HPV) Primary Testing in The Age of HPV VaccinationDocument10 pagesIntroducing Human Papillomavirus (HPV) Primary Testing in The Age of HPV VaccinationIcha NurfaizahNo ratings yet
- Asia Oceania GuidelinesDocument25 pagesAsia Oceania GuidelinesKaily TrầnNo ratings yet
- Pathology of Female Cancers: Precursor and Early-Stage Breast, Ovarian and Uterine CarcinomasFrom EverandPathology of Female Cancers: Precursor and Early-Stage Breast, Ovarian and Uterine CarcinomasTakuya MoriyaNo ratings yet
- BE HE@LTHY BE MOBILE A Handbook On How To Implement MCervicalCanceDocument47 pagesBE HE@LTHY BE MOBILE A Handbook On How To Implement MCervicalCancederr barrNo ratings yet
- ANC Trends Uganda Oct11 2018Document36 pagesANC Trends Uganda Oct11 2018derr barrNo ratings yet
- Pathology-Based Research in AfricaDocument33 pagesPathology-Based Research in Africaderr barrNo ratings yet
- Key Facts: Adolescent PregnancyDocument10 pagesKey Facts: Adolescent Pregnancyderr barrNo ratings yet
- Apac BFP 2015-16Document202 pagesApac BFP 2015-16derr barrNo ratings yet
- The Message Box WorkbookDocument28 pagesThe Message Box Workbookderr barrNo ratings yet
- 10 Tips To Winning A DELTAS Africa Grant - 0Document5 pages10 Tips To Winning A DELTAS Africa Grant - 0derr barrNo ratings yet
- Adult Urology: ElsevierDocument6 pagesAdult Urology: Elsevierderr barrNo ratings yet
- Message Box BlankDocument1 pageMessage Box Blankderr barrNo ratings yet
- DELTAS Africa II Budget Guidelines - Full ApplicationDocument2 pagesDELTAS Africa II Budget Guidelines - Full Applicationderr barrNo ratings yet
- Thomas McKeown A True Public Health PioneerDocument3 pagesThomas McKeown A True Public Health Pioneerderr barrNo ratings yet
- Screening To Prevent Cancer DeathsDocument2 pagesScreening To Prevent Cancer Deathsderr barrNo ratings yet
- Dna Fingerprinting LabDocument37 pagesDna Fingerprinting Labderr barrNo ratings yet
- Cells Structure & FunctionDocument80 pagesCells Structure & Functionderr barrNo ratings yet
- Skin and Epithelial Tissues: Dr. Okello Michael / Dr. Mwaka ErisaDocument44 pagesSkin and Epithelial Tissues: Dr. Okello Michael / Dr. Mwaka Erisaderr barrNo ratings yet
- Protein Structurs and FunctionDocument54 pagesProtein Structurs and Functionderr barrNo ratings yet
- Surgical Treatment For Mammary TumorsDocument5 pagesSurgical Treatment For Mammary Tumorsgrace joNo ratings yet
- Question Paper 1 2018 PDFDocument38 pagesQuestion Paper 1 2018 PDFAyeshaNo ratings yet
- Autacoids: Definition: Chemical Substances Produced LocallyDocument23 pagesAutacoids: Definition: Chemical Substances Produced LocallyAlphahin 17No ratings yet
- HSC 421 Research PaperDocument13 pagesHSC 421 Research Paperapi-502687231No ratings yet
- III Bds II Internal 2023Document5 pagesIII Bds II Internal 2023Sourab KumarNo ratings yet
- Case Presentation OngDocument12 pagesCase Presentation OngRaja Azman Raja AhmadNo ratings yet
- Sr. No. Cghs Treatment Procedure/Investigation List Non-NABH/Non - NABL Rates Nabh/Nabl RatesDocument49 pagesSr. No. Cghs Treatment Procedure/Investigation List Non-NABH/Non - NABL Rates Nabh/Nabl RatesADDECC INFO INDIANo ratings yet
- DNA Replication Study Guide - Biology101Document4 pagesDNA Replication Study Guide - Biology101nandi_scrNo ratings yet
- LDN Information PackDocument17 pagesLDN Information PackkindheartedNo ratings yet
- Worksheet For Perception CoordinationDocument7 pagesWorksheet For Perception CoordinationRiza Angela BarazanNo ratings yet
- Drink Water On Empty StomachDocument4 pagesDrink Water On Empty StomachbabuNo ratings yet
- Contents of Wetland Medicinal Plants in Taiwan: Antioxidant Properties and Total PhenolicDocument12 pagesContents of Wetland Medicinal Plants in Taiwan: Antioxidant Properties and Total Phenolicvaishali shuklaNo ratings yet
- Does WiFi Affect The BrainDocument6 pagesDoes WiFi Affect The BrainrustyNo ratings yet
- Zigmond MJ, Burke RE - Pathophysiology of Parkinson's DiseaseDocument14 pagesZigmond MJ, Burke RE - Pathophysiology of Parkinson's Diseaseursula_ursula100% (1)
- Hyperhidrosis: Management Options: Hyperhidrosis Is Excessive SweatingDocument6 pagesHyperhidrosis: Management Options: Hyperhidrosis Is Excessive SweatingHagane TetsuNo ratings yet
- Lhea's Case StudyDocument14 pagesLhea's Case StudyMelody B. MiguelNo ratings yet
- HomeostasisDocument2 pagesHomeostasisAnn Calindo EstafiaNo ratings yet
- Evaluation of Surgical Glove Integrity and Factors Associated With Glove DefectDocument4 pagesEvaluation of Surgical Glove Integrity and Factors Associated With Glove DefectAdel AdielaNo ratings yet
- SikaForce 010 Part BDocument11 pagesSikaForce 010 Part BAlexander DpsNo ratings yet
- Folic Acid Deficiency Anemia: Prepared By: Arwa, Amna, Kawkab, Ayat, Ghanimah, Madlin, IntelaqDocument10 pagesFolic Acid Deficiency Anemia: Prepared By: Arwa, Amna, Kawkab, Ayat, Ghanimah, Madlin, IntelaqNada MotahharNo ratings yet
- The Conditions of The Small-Scale Miners in Barangay Bukal, Nabunturan Compostela Valley ProvinceDocument24 pagesThe Conditions of The Small-Scale Miners in Barangay Bukal, Nabunturan Compostela Valley Provincexenos19No ratings yet
- Knowledge On Risk Factors of Diabetes Mellitus 2 Among Students in Selected Universities in RwandaDocument6 pagesKnowledge On Risk Factors of Diabetes Mellitus 2 Among Students in Selected Universities in RwandaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Treatment Guidelines For Hyponatremia Stay The.180Document22 pagesTreatment Guidelines For Hyponatremia Stay The.180Carolyn CamposNo ratings yet
- TAMIFLUDocument21 pagesTAMIFLUjaphetnwapiNo ratings yet
- Circular To Dental CollegesDocument3 pagesCircular To Dental CollegesrajeshNo ratings yet
- Ento 365 All Objective Qu.Document30 pagesEnto 365 All Objective Qu.Navneet KumarNo ratings yet
- BodyDocument124 pagesBodygion.nandNo ratings yet
- Congenital Muscular TorticollisDocument5 pagesCongenital Muscular TorticollisKevin Paul ZuñigaNo ratings yet
- Bahasa Inggris Kelas 6Document4 pagesBahasa Inggris Kelas 6Nia Asih KurniasariNo ratings yet
- Potts Spine Case StudyDocument9 pagesPotts Spine Case StudyK. KNo ratings yet