Professional Documents
Culture Documents
Hyperemesis Gravidarum and Puerperal Sepsis
Uploaded by
Blessy Madhuri0 ratings0% found this document useful (0 votes)
13 views4 pagesOBG
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOBG
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
13 views4 pagesHyperemesis Gravidarum and Puerperal Sepsis
Uploaded by
Blessy MadhuriOBG
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
HYPEREMESIS GRAVIDARUM
SIGNS AND SYMPTOMS
1. Signs of dehydration and ketoacidosis
2. Dry coated tongue
3. Sunken eyes
4. Acetone smell in breath
5. Tachycardia and Raise in temperature
6. Postural hypotension
7. Excess vomiting & retching day & night.
8. Epigastric pain
9. Constipation
10.Fatigue
11.Anorexia.
MANAGEMENT
1. Monitor the vitals
2. Open IV line and correct fluids
3. Send for relevant investigations
4. Maintain an intake-output chart
5. Monitor urine output (catheterize the patient)
6. Test the urine periodically for ketone bodies.
DRUGS
1. Antiemetic:
Pro-methazin -25mg IM BD or TDS
Tri-fluopromazine:10mg IM
Meta-chlopromide: 10mg IM
2. Hydro-cortisone: 100mg IV in drip
3. Prednisolone orally
4. Nutritional support:
Vitamin B1, vitamin B6, vitamin B12 & vitamin C.
QUESTIONS:
1. List out the signs and symptoms of hyperemesis gravidarum?
2. What are the drugs used to treat hyperemesis gravidarum?
3. What is the general nursing management?
4. What are the adverse effects of severe vomiting?
5. What for urine analysis is done?
PUERPERAL SEPSIS
ORGANISMS RESPONSIBLE FOR PUERPERAL SEPSIS:
Doderlein’s bacillus
Candida albicans
Staphylococcus aureus
Streptococcus
Escherichia coli
Bacteroides group
Clostridium.
PREDISPOSING FACTORS:
1. Antepartum factors:
Malnutrition and anaemia
Preterm labour
PROM
2. Intrapartum factors:
Repeated vaginal examination
Prolonged rupture of membranes
Traumatic operative delivery
Haemorrhage- antepartum and postpartum
Retained bits of placenta tissue and membranes.
Lscs.
SIGNS AND SYMPTOMS:
Local infection
Uterine infection
Spreading of infections
1. LOCAL INFECTION:
rise of temperature
generalized malaise
Headache
PRISH (pain, redness, immobility, swelling, heat)
Pus
Chills and rigor
2. UTERINE INFECTION
Rise in pulse
Normal lochia discharge
Lochial discharge becomes offensive and copious
Subinvolution of uterus
Measure lochia
lochiometra
3. SPREADING INFECTION:
Parametritis
Pelvic peritonitis
General peritonitis
Thrombophlebitis
Septicaemia
MANAGEMENT:
Isolation of the patient
Adequate fluid and calorie
Correcting Anemia
Indwelling catheter
A chart is maintained to record vitals, lochial discharge, and fluid intake
and output
Ensure that wound is cleaned with sitz bath several times a day and is
dressed with an antiseptic ointment.
Dehiscence of episiotomy or abdominal wound following cesarean
section is managed by scrubbing the wound twice daily, debridement of
all necrotic tissue and then closing the wound with secondary suture.
TREATMENT:
1. Medical management
2. Surgical management
Medical management:
Antibiotics: Ideal antibiotic regimen should depend on the culture and
sensitivity report.
Gentamicin (1.5mg/kg/8 hourly) + Clindamycin (900mg/8 hourly)
Metronidazole (500mg/12 hr) + Penicillin (5 million units/6 hr)
Clindamycin + aztreonam (2 gm/8hr)
Ampicillin (2gm/6hr) + gentamycin
Antibiotic Regimens-A combination of either piperacillin-tazobactam or
carbapenem
Women with MRSA (Methicillin-resistant S. aureus) infection should be
treated with vancomycin or teicoplanin.
Surgical management:
Stitches of the perineal wound
Surgical evacuation
Colpotomy
Laparotomy
Hysterectomy.
QUESTIONS:
1. What are the common causes of puerperal sepsis?
2. What is puerperium and what is sepsis?
3. What is the medical management for sepsis?
4. What are the micro-organisms responsible for puerperal sepsis?
5. What are the predisposing factors for puerperal sepsis?
You might also like
- Procedure Manual For Obstetrics and Gynecological Nursing: Government College of Nursing Somajiguda, Hyderabad, T.SDocument119 pagesProcedure Manual For Obstetrics and Gynecological Nursing: Government College of Nursing Somajiguda, Hyderabad, T.SBlessy Madhuri100% (5)
- Sitz Bath ProcedureDocument6 pagesSitz Bath ProcedureBlessy Madhuri100% (1)
- Clinical Features of APHDocument4 pagesClinical Features of APHBlessy MadhuriNo ratings yet
- Mrs. V. Bhulaxmi M.SC (N) 2 Year Nursing Management Gcon, HydDocument49 pagesMrs. V. Bhulaxmi M.SC (N) 2 Year Nursing Management Gcon, HydBlessy Madhuri100% (1)
- Antenatal-Exercises Health EducationDocument13 pagesAntenatal-Exercises Health EducationBlessy Madhuri100% (2)
- Lesson Plan ON Benign Prostatic HyperplasiaDocument26 pagesLesson Plan ON Benign Prostatic HyperplasiaBlessy Madhuri75% (4)
- BPH and Prostate Cancer 11Document225 pagesBPH and Prostate Cancer 11Blessy MadhuriNo ratings yet
- F W S Ward TeachingDocument40 pagesF W S Ward TeachingBlessy MadhuriNo ratings yet
- Iec Obg CareDocument16 pagesIec Obg CareBlessy Madhuri100% (1)
- Amniotomy ProcedureDocument4 pagesAmniotomy ProcedureBlessy MadhuriNo ratings yet
- Merits and Demerits of Oxytocin and Prostaglandins in Medical Induction of LabourDocument2 pagesMerits and Demerits of Oxytocin and Prostaglandins in Medical Induction of LabourBlessy MadhuriNo ratings yet
- Micro TeachingDocument16 pagesMicro TeachingBlessy Madhuri100% (2)
- Augmentation and IOLDocument24 pagesAugmentation and IOLBlessy MadhuriNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Pharmacology of AntimycobacterialDocument7 pagesPharmacology of Antimycobacterialselflessdoctor100% (1)
- Budesonide (Drug Study)Document3 pagesBudesonide (Drug Study)Franz.thenurse6888No ratings yet
- Common Drugs in SA MedicineDocument8 pagesCommon Drugs in SA MedicineJordan PetersNo ratings yet
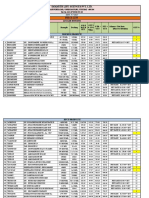
- Obat BPJS SPTDocument11 pagesObat BPJS SPTpoliklinik klungkungNo ratings yet
- Helicobacter Pylori (H. Pylori) Is A BacteriumDocument2 pagesHelicobacter Pylori (H. Pylori) Is A BacteriumnasirkgnNo ratings yet
- HTN PPT - YasDocument18 pagesHTN PPT - YasCiaNo ratings yet
- Drug Study AzithromycinDocument2 pagesDrug Study AzithromycinYamete KudasaiNo ratings yet
- TUBERCULOSISDocument25 pagesTUBERCULOSISManuel Fatima Goncalves83% (6)
- REPORTDocument58 pagesREPORTNisar MarwatNo ratings yet
- Drug Study - DoxycylineDocument3 pagesDrug Study - DoxycylineHaifi Hun100% (1)
- SleDocument893 pagesSleAsma Sikander100% (4)
- Immunisation Form - Greece 0Document0 pagesImmunisation Form - Greece 0Diego_Vitor92No ratings yet
- Logistik Harga Obat (MUTIARA)Document3 pagesLogistik Harga Obat (MUTIARA)EryanaCitaNo ratings yet
- Esophagitis: Preferred By: Daryl S - AbrahamDocument26 pagesEsophagitis: Preferred By: Daryl S - AbrahamBiway RegalaNo ratings yet
- Laporan Penggunaan Juli 2020Document6 pagesLaporan Penggunaan Juli 2020Mas Okta PratamaNo ratings yet
- Methyldopa Drug StudyDocument2 pagesMethyldopa Drug Studymilkv100% (14)
- PriceDocument5 pagesPriceMubarak MHNo ratings yet
- CTC 2020Document850 pagesCTC 2020Mounira75% (4)
- EXISTENCIASDocument2,425 pagesEXISTENCIASOmar BelloNo ratings yet
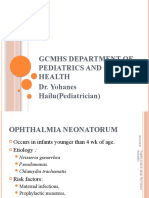
- Ophthalmia NeonatorumDocument12 pagesOphthalmia NeonatorumDemewoz Fikir100% (2)
- ICD X PerfectDocument66 pagesICD X PerfectandrianmaulanaNo ratings yet
- Drug Name Mecahnism of Action Indication Side Effects Nursing Responsibilities Generic NameDocument2 pagesDrug Name Mecahnism of Action Indication Side Effects Nursing Responsibilities Generic NamehahahaNo ratings yet
- Drug List - Medical SchoolDocument33 pagesDrug List - Medical SchoolMatt PrestonNo ratings yet
- What Is Pityriasis Rosea?Document1 pageWhat Is Pityriasis Rosea?andinaNo ratings yet
- HemorrhoidDocument12 pagesHemorrhoidAdelia Maharani DNo ratings yet
- DPDocument28 pagesDPManuel TrujilloNo ratings yet
- Cervical CancerDocument2 pagesCervical CancerLicio LentimoNo ratings yet
- Daftar Nama Obat Dan PengencernyaDocument15 pagesDaftar Nama Obat Dan PengencernyaMeta SuryantiNo ratings yet
- Perencanaan Oktober 2017Document80 pagesPerencanaan Oktober 2017Sri WahyuningsihNo ratings yet