Professional Documents
Culture Documents
Myocardial Infarction
Uploaded by
CM NajitoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Myocardial Infarction
Uploaded by
CM NajitoCopyright:
Available Formats
Myocardial Infarction (Heart Attack) — STEMI vs.
NSTEMI Furthermore, the European Society of Cardiology differentiates
between the following types:
Definition Type 1: The infarction is spontaneous and can be attributed
to a primary coronary incident.
Type 2: The infarction is related to ischemia, the cause of
the ischemia being, for example, coronary embolism or
anemia.
Type 3: The symptoms preceding cardiac death or an
autopsy point to myocardial ischemia.
Type 4a: The myocardial infarction occurs as part of a PCI.
Type 4b: The myocardial infarction is caused by stent
thrombosis.
Type 5: The myocardial infarction develops in connection
with a CABG.
Image: Myocardial Infarction. By: J. Heuser. License: CC BY-SA
3.0 Pathophysiology
The term myocardial infarction refers to ischemia of the myocardial
tissue due to a complete obstruction or drastic constriction of
the coronary artery. This is usually accompanied by an increase in
cardiac enzymes, typical ECG changes, and pain symptoms, or a
thrombus or wall motion abnormality that is detected by means of
medical imaging.
Epidemiology Image: Coronary Artery Disease. By: Bruce Blaus. License: CC
BY 3.0
Spread of myocardial infarction As a result of atherosclerosis, plaques start to form in the coronary
arteries, which are at first still stable. Over time, an unstable
Myocardial infarction is one of the most common causes of death in (vulnerable) plaque forms. The rupturing of this plaque leads to a
industrialized countries. Several million people suffer from thrombotic obstruction of one of the coronary arteries, hypoxia of
myocardial infarction each year. the tissue fed by the coronary artery, and ischemia, followed by the
formation
Regional differences can be observed, with Germany recording a
significantly higher number of infarctions per year (300 infarctions in The rupture can be triggered by e.g. physical or psychological stress,
100,000 inhabitants) compared to Mediterranean countries (100–200 drastic blood pressure fluctuations or in the course of circadian
infarctions in 100,000 inhabitants). Sweden, Belgium, and Japan have rhythms that are accompanied by changes in coagulation activity
an even lower infarction rate of fewer than 100 infarctions in 100,000 (stronger coagulation early in the morning).
inhabitants.
Symptoms
Etiology
Clinical signs of myocardial infarction
Causes of myocardial infarction
The typical symptoms include severe retrosternal pain that typically
The main cause of myocardial infarction is the development of radiates to the left arm (Note: right arm pain is also possible), neck,
atherosclerosis in the coronary arteries; hence, the name coronary and upper jaw and does not improve after nitroglycerin
heart disease. Coronary embolism is a rarer cause. administration. These symptoms are observed in only about 40% of
patients.
Classification
Distinction based on the type of myocardial infarction
Image: Pain in acute myocardial infarction (front). By:
J. Heuser. License: CC BY-SA 3.0
Image: Abbreviations used for ACS (Acute coronary syndrome).
By: J. Heuser. License: CC BY-SA 3.0
Image: Pain in acute myocardial infarction (rear). By:
The general distinction is based on ECG changes: STEMI (ST- J. Heuser. License: CC BY-SA 3.0
segment-elevation myocardial infarction) is distinguished from
NSTEMI (Non-ST-segment-elevation myocardial infarction).
Painless (silent) infarctions especially affect diabetic patients due to
neuropathy or old age. These painless infarctions are present in about
20% of all cases.
However, infarction pain can also be atypical, such as upper
abdominal pain, feeling of faintness combined with fear and
sweating, dyspnea, nausea, or vomiting. These atypical pain
symptoms are frequently found in women, diabetics, or older people.
Diagnostics
ECG diagnostics for myocardial infarction
History and physical examination for myocardial infarction
In the case of NSTEMI, the ST-segment may be temporarily
In the course of the disease, the typical retrosternal pain can be depressed and may be accompanied by a negative pre-terminal T-
evaluated. Physical examination can reveal e.g. signs of cardiac wave. The ECG changes in NSTEMI are often atypical, which means
decompensation or changes in blood pressure. Cardiac risk factors that an infarction can only be ruled out through repeated heart
can be ascertained in the process as well or be unveiled during the enzyme counts.
physical examination.
Noticeable noises, especially in connection with complications, may
be detected in the course of the auscultation. Pericardial rub can be
heard, which suggests underlying pericarditis. Systolic murmur
occurs during ventricular septal perforation or mitral valve
insufficiency. Pulmonary vascular congestion or lung edema can
cause bilateral basal rales.
Laboratory diagnostics for myocardial infarction
The classification of the heart enzymes provides information on the
presence and extent of myocardial damage. The determination of
Troponin I or T (depending on the laboratory) is considered the gold Image: Diagram showing a representation of myocardial infarction
standard. Troponin, as a cardiac marker, is specific to the myocardial on an ECG. By: J. Heuser. License: CC BY-SA 3.0
tissue.
In the case of STEMI, the ECG shows typical changes, such as the
Troponin increases shortly after the infarction. About 70% of patients monophasic ST-segment elevation, which transitions directly into the
show an increase 3 hours after the incident, and that number rises to T-wave, with pathologically enlarged Q-spikes. Other ECG changes
90% 6 hours after the incident. This timeline stresses the necessity of are typical depending on the stage of the infarction:
measuring cardiac enzymes again at a later time even if the initial
result was negative.
Initial stage: Up to 6 hours after the infarction, typically
characterized by pointed elevation of the T-wave, which is
Reinfarction after myocardial infarction cannot be diagnosed by called anoxic T-wave
means of troponin-recording since the troponin concentration only
returns to normal after about 1–2 weeks. In contrast, myoglobin is Acute infarction: Few hours to days after the infarction,
unspecific and increases also when damage to skeletal muscles occurs characterized by the typical monophasic ST-elevation
but goes back to normal after 1 day at the latest. CK-MB is specific to
the infarction, but it only starts to rise 4 hours after the occurrence of Intermediate stage: The ST-elevation and R-spike
ischemia. A CK-MB concentration of between 6–20% of the total CK decrease and so-called poor R-wave progression occurs.
indicates myocardial damage. Moreover, the enlargement of the Q-spike is noted, which,
as a Pardee-Q, signals the end of the myocardium, and
pointed negativity of the T-wave develops.
LDH can serve as a long-term marker of myocardial damage. It starts
to increase only after 6–12 hours, but reaches its maximum after 2–4 Final stage: More than 6 months after the infarction, the
days and stays at an increased level up to 2 weeks following the changes in the QRS complex remain, while the ST-segment
infarction. GOT, which is actually a marker for liver cells, also exists and the T-wave return to normal.
in the heart muscle and can also be used for diagnostics. In that case,
GPT, which is specific to the liver, has to be determined as well in Localization of infarction
order to distinguish heart disease from liver cell damage.
The ECG lead(s) in which changes are detected provide information
on which coronary artery is likely obstructed and where the infarction
is located. In exams, students are often asked to explain how anterior
myocardial infarction leads to ECG changes in leads V1-V6, aVL,
and I. This frequently affects the proximal part of the anterior
interventricular artery. Changes in leads V1 and V2, however,
point to a posterior myocardial infarction, where the posterior
descending artery is being affected frequently.
Medical imaging for myocardial infarction
Image: Typical changes in CK-MB and cardiac troponin in acute Echocardiography as another diagnostic tool helps to detect wall
myocardial infarction. By: J. Heuser. License: CC BY-SA 3.0 motion abnormalities, determine the remaining function, and exclude
complications, such as cardiac valvular defects. Cardiac
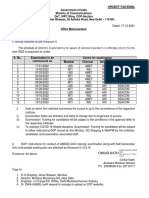
The following table provides an overview of the various catheterization is considered the gold standard and should be
parameters: performed as quickly as possible in the case of STEMI. MRI
cardioangiography serves as another means of detecting wall motion
abnormalities and determining the size of infarction scars.
Pathology has to be continued throughout life, whereas, inhibition by means of
P2Y12 inhibitors is only used for 12 months following the infarction.
The pathology of myocardial infarction can be traced to the
insufficient perfusion of cardiac tissue. At a perfusion rate of less Moreover, all patients should receive cholesterol-lowering agents,
than 25% of the normal blood flow, the tissue is damaged such as statins. The intake of beta-blockers decreases the reinfarction
irreversibly, and after 6–12 hours, damages in the shape of yellowish risk as well as the risk of arrhythmia-related and sudden cardiac
focuses become visible with light microscopy. death.
Complete myocytolysis takes place, the cell nuclei starts to pale, and Complications of Myocardial Infarction
the cross striations get blurred. Granulation tissue with a hemorrhagic
edge and numerous peripheral leukocytes develop a few days later. The complications associated with myocardial infarction are
After only 2 weeks, whitish scar tissue develops. extensive, and their severity depends on the degree of myocardial
damage.
Differential Diagnoses
One can distinguish between early and late complications, the
transition between those phases lying at about 48 hours following the
Symptoms similar to those of myocardial infarction infarction. Early complications include cardiac arrhythmias that
develop when an area of the myocardium is under-supplied.
The typical pain symptoms can also point to unstable angina Ventricular fibrillation, which accounts for 80% of deaths due to
pectoris, with the exception that there is no increase in troponin. myocardial infarction, frequently occurs within the first few four
Particularly, when pain spreads to the upper abdomen, the hours following the infarction. Premature ventricular contractions or
symptoms can be mistaken for an acute abdomen. Another atrial fibrillation can also occur.
differential diagnosis to be considered is Takotsubo
cardiomyopathy, which is often caused by emotional stress.
Depending on what area is damaged, right or left heart failure and
cardiogenic shock may occur, or damage in the papillary
ECG changes can also be caused by other diseases. ST-elevation can muscle may lead to an insufficiency of the atrioventricular
also occur in pericarditis or left ventricular hypertrophy, while valves. After ventricular fibrillation, congestive heart failure due to
low Q-spikes can be noted in lung embolisms, Wolff-Parkinson- cardiac insufficiency is the second most frequent cause of death in
White syndrome, or hypertrophic cardiomyopathies. patients of myocardial infarction.
Furthermore, all other causes of thoracic pain have to be Long-term complications include myocardial aneurysms that can
distinguished from myocardial infarction, including lung embolism, rupture. The myocardium may also rupture. Arterial embolisms,
aortic dissection, tension pneumothorax, and spontaneous rupture of arrhythmias, and insufficiencies also count as long-term
the esophagus (Boerhaave-syndrome). Myocarditis and pericarditis, complications. As a result of the infarction, pericarditis can occur up
as well as musculoskeletal thoracic pain, are also differentials of to 6 weeks later.
myocardial infarction and are possible exam answers on the subject.
Prevention of Myocardial Infarction
Therapy for Myocardial Infarction
Since 95% of the cases of acute coronary syndrome are
Oxygen (4–8 L/min per nasal O2 tube) can be administered from the manifestations of coronary heart disease, the disease can be
initial treatment until the diagnosis is confirmed. Additionally, it is prevented. Thus, risk factors, especially the main risk factors, which
recommended to elevate the upper body for relief (30°) in the case of are high cholesterol, arterial hypertension, diabetes mellitus, and
dyspnea or heart insufficiency. Administering nitroglycerin (1 nicotine abuse must first be addressed. Patients should be advised to
capsule or 2 puffs = 0.8 mg, 1–5 mg intravenously through a perfusor live a healthy lifestyle by paying attention to nutrition and exercise.
(Note: nitroglycerin is contraindicated if systolic blood pressure is 90 However, these approaches can be supported with drugs.
mmHg). The simultaneous administration of PDE-5 inhibitors
and morphine (3–5 mg intravenously every 5–10 minutes) can be
administered when severe pain occurs.
Furthermore, all patients receive aspirin (initial dose 150–300 mg) as
well as heparin (UFH 70 IE/kg, KG or LMWH) and a P2Y12
inhibitor such as clopidogrel (initial dose 300 mg). Intramuscular
injections should be avoided since they lead to a non-specific
increase of CK-levels. The administration of beta-blockers and ACE-
inhibitors and AT1 receptor antagonists is also indicated unless there
is a contraindication.
Cardiac catheterization has to be used for diagnosis of NSTEMI, and
can be performed between 2 and 72 hours after the incident,
depending on the risk factors of the respective patient. In the case of
STEMI, the obstructed coronary vessel has to be revascularized as
quickly as possible by means of PCI. Primary PCI is the therapy of
choice and should be performed within 90 minutes.
Alternatively, a conservative therapy
of fibrinolytics and thrombolytics for reperfusion can be
administered. The substances used are streptokinase, alteplase,
reteplase, and tenecteplase, all of which should accompany heparin
therapy. Alternatively, fondaparinux or enoxaparin may be
administered. It is crucial to ensure that no contraindications such as
hemorrhages exist and that the STEMI is recent, in which case an
acute PTCA is not possible.
Note: Fibrinolytic treatment should not be administered in NSTEMI.
Subsequently, more therapy is necessary to avoid coronary
rethrombosis. Dual platelet inhibition is typically employed in this
process, and in the case of aspirin, it is combined with ticagrelor,
prasugrel, or clopidogrel. Platelet aggregation inhibition using ASA
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Healing Is Voltage - Healing Eye DiseasesDocument219 pagesHealing Is Voltage - Healing Eye DiseasesAndrea Sirah89% (9)
- CH 1 Understanding NutritionDocument30 pagesCH 1 Understanding NutritionAdjannie AndradaNo ratings yet
- Robbins - 12 The HeartDocument5 pagesRobbins - 12 The HeartCM NajitoNo ratings yet
- Exercise Physiology Lab ReportDocument10 pagesExercise Physiology Lab Reportapi-253305501100% (1)
- Respiratory Disorders NCLEXDocument22 pagesRespiratory Disorders NCLEXPotchiee Pfizer50% (2)
- NCP Incarcerated Inguinal HerniaDocument2 pagesNCP Incarcerated Inguinal HerniaJanna Gale Javier76% (25)
- PsychosisDocument4 pagesPsychosisCM NajitoNo ratings yet
- Glutamate: Neurotransmitters Disturbed Increased Sympathetic Stimulation Increased Autonomic StimulationDocument3 pagesGlutamate: Neurotransmitters Disturbed Increased Sympathetic Stimulation Increased Autonomic StimulationCM NajitoNo ratings yet
- 1307 Chest Tube Placement Procedure NoteDocument1 page1307 Chest Tube Placement Procedure NoteRumela Ganguly ChakrabortyNo ratings yet
- Philippine Clinical Practice Guidelines On The Diagnosis and Management of Obstructive Sleep Apnea in AdultsDocument75 pagesPhilippine Clinical Practice Guidelines On The Diagnosis and Management of Obstructive Sleep Apnea in AdultsDiane IsmaelNo ratings yet
- Sample Test Questions: Krok 2Document41 pagesSample Test Questions: Krok 2kjkNo ratings yet
- StrokeDocument5 pagesStrokeCM NajitoNo ratings yet
- Thought DisordersDocument3 pagesThought DisordersCM NajitoNo ratings yet
- Image CC BY-SA 3.0: Term MeaningDocument4 pagesImage CC BY-SA 3.0: Term MeaningCM NajitoNo ratings yet
- Lecturio Schizophrenia QuestionsDocument3 pagesLecturio Schizophrenia QuestionsCM NajitoNo ratings yet
- Image CC BY-SA 4.0: HypertensionDocument3 pagesImage CC BY-SA 4.0: HypertensionCM NajitoNo ratings yet
- Idoc - Pub Sketchy-MicroDocument2 pagesIdoc - Pub Sketchy-MicroCM NajitoNo ratings yet
- Tumor Kidney FailureDocument6 pagesTumor Kidney FailureCM NajitoNo ratings yet
- Childhood EpilepsyDocument3 pagesChildhood EpilepsyCM NajitoNo ratings yet
- How To Interpret An ECG in Seven StepsDocument5 pagesHow To Interpret An ECG in Seven StepsCM NajitoNo ratings yet
- Robbins 15 - Chronic Diffuse Interstitial DiseaseDocument12 pagesRobbins 15 - Chronic Diffuse Interstitial DiseaseCM NajitoNo ratings yet
- Epidemiology and Classification of Diabetic Neuropathy - UpToDateDocument10 pagesEpidemiology and Classification of Diabetic Neuropathy - UpToDateCM NajitoNo ratings yet
- Management of Diabetic Neuropathy - UpToDateDocument19 pagesManagement of Diabetic Neuropathy - UpToDateCM NajitoNo ratings yet
- Diabetic Autonomic Neuropathy - UpToDateDocument27 pagesDiabetic Autonomic Neuropathy - UpToDateCM NajitoNo ratings yet
- Approach To PX With HFDocument1 pageApproach To PX With HFCM NajitoNo ratings yet
- Valvular Aortic Stenosis: Acute Myocardial InfarctionDocument3 pagesValvular Aortic Stenosis: Acute Myocardial InfarctionCM NajitoNo ratings yet
- 2022 Yearly Blank Calendar TemplateDocument1 page2022 Yearly Blank Calendar TemplateCM NajitoNo ratings yet
- Causes Presentation: Staphylococcus AureusDocument3 pagesCauses Presentation: Staphylococcus AureusCM NajitoNo ratings yet
- Prognosis - Rule of 5, 3, and 2:: Image CC BY 3.0Document3 pagesPrognosis - Rule of 5, 3, and 2:: Image CC BY 3.0CM NajitoNo ratings yet
- Image CC By-Sa 3.0: Hypertension Coronary Heart Disease Myocardial InfarctionDocument6 pagesImage CC By-Sa 3.0: Hypertension Coronary Heart Disease Myocardial InfarctionCM NajitoNo ratings yet
- Sign117 TonsillectomyDocument44 pagesSign117 TonsillectomySherynneNo ratings yet
- ECG Rhythm InterpretationDocument21 pagesECG Rhythm Interpretationvanstar7100% (1)
- WWW - Medicalppt.: For More Free Medical Powerpoint Presentations Visit WebsiteDocument15 pagesWWW - Medicalppt.: For More Free Medical Powerpoint Presentations Visit WebsiteJoko Sutrisno,S.Kep,Ns.M.KesNo ratings yet
- For More Free Medical Powerpoint Presentations Visit WebsiteDocument24 pagesFor More Free Medical Powerpoint Presentations Visit Websitevanstar7No ratings yet
- Pharyngitis: Signs and SymptomsDocument26 pagesPharyngitis: Signs and SymptomsCM NajitoNo ratings yet
- Ecg Module 3Document16 pagesEcg Module 3Muhammad BilalNo ratings yet
- Quick Reference Instructions For Patients: Negative ResultDocument5 pagesQuick Reference Instructions For Patients: Negative ResultShifon StareNo ratings yet
- Dog BitesDocument14 pagesDog BitesNdor BariboloNo ratings yet
- BUKU Acute Coronary Syndrome Update 2020Document16 pagesBUKU Acute Coronary Syndrome Update 2020Embun Suci LestariNo ratings yet
- Nursing History FormDocument5 pagesNursing History FormJullie Anne SantoyoNo ratings yet
- GMDSS Exam Schedule For Year 2022Document7 pagesGMDSS Exam Schedule For Year 2022Mani ThapaNo ratings yet
- Parasitlogy FinalsDocument12 pagesParasitlogy FinalsJHODIE LYNNE OLAERNo ratings yet
- FinalDocument45 pagesFinalRanvidsNo ratings yet
- COVID-19 Guidance For Public Pools - 07.08.20Document7 pagesCOVID-19 Guidance For Public Pools - 07.08.20jclark13010No ratings yet
- Biomedical Engineer - UNSEEN HEROES DURING THE PANDEMIC OF COVID-19 by Krushi MehtaDocument4 pagesBiomedical Engineer - UNSEEN HEROES DURING THE PANDEMIC OF COVID-19 by Krushi MehtasamsonNo ratings yet
- AOAC Rapid Method ValidationDocument60 pagesAOAC Rapid Method ValidationPiruzi MaghlakelidzeNo ratings yet
- Bahasa Inggris Kelompok SyahdanDocument11 pagesBahasa Inggris Kelompok SyahdanAji cupleeNo ratings yet
- Article Bladder RetrainingDocument9 pagesArticle Bladder RetrainingRaenette DavidNo ratings yet
- Iron Deficiency Anemia (Ida)Document30 pagesIron Deficiency Anemia (Ida)angel214No ratings yet
- Visualization of EEG Data To Detect ADHD in Children and AdultsDocument5 pagesVisualization of EEG Data To Detect ADHD in Children and AdultsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Secdocument - 813download Goodman and Snyders Differential Diagnosis For Physical Therapists Screening For Referral 7E Jun 2 2022 - 0323722040 - Elsevier 7Th Edition John Heick Full ChapterDocument68 pagesSecdocument - 813download Goodman and Snyders Differential Diagnosis For Physical Therapists Screening For Referral 7E Jun 2 2022 - 0323722040 - Elsevier 7Th Edition John Heick Full Chapterclara.yanez755100% (5)
- The Dogs Learning To Sniff Out DiseaseDocument1 pageThe Dogs Learning To Sniff Out DiseaseMicheleFontanaNo ratings yet
- Ch.11. Transportation in Animals and PlantsDocument3 pagesCh.11. Transportation in Animals and PlantsSharath ChandraNo ratings yet
- DIPHTHERIADocument12 pagesDIPHTHERIANununNo ratings yet
- Health Sector BriefDocument53 pagesHealth Sector Briefecossich123No ratings yet
- Medical Examiner's Report On Daniel PrudeDocument8 pagesMedical Examiner's Report On Daniel PrudePatrick Crozier100% (1)
- GHR Health and Nutrition Capacity Statement 2023Document5 pagesGHR Health and Nutrition Capacity Statement 2023Andre TorresNo ratings yet
- Pattern and Causes of Tooth Extraction in Patients Reporting To A Teaching Dental HospitalDocument6 pagesPattern and Causes of Tooth Extraction in Patients Reporting To A Teaching Dental HospitalAnye PutriNo ratings yet
- Prevalence of Periodontitis in The Indian PopulationDocument7 pagesPrevalence of Periodontitis in The Indian PopulationRohit ShahNo ratings yet