Professional Documents
Culture Documents
Robbins - 12 The Heart
Uploaded by
CM NajitoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Robbins - 12 The Heart
Uploaded by
CM NajitoCopyright:
Available Formats
Robbins Patho, 10 e.
12 The Heart
Table of Contents
12 The Heart.................................................................1
The Heart..................................................................1
Cardiac Structure and Specializations................1
Overview of Cardiac Pathophysiology................3
Heart Failure.........................................................3
Cardiac Development...........................................3
Congenital Heart Disease.....................................3
Ischemic Heart Disease.........................................3
Arrhythmias..........................................................3
Hypertensive Heart Disease.................................3
Valvular Heart Disease.........................................3
Cardiomyopathies.................................................5
Pericardial Disease...............................................5
Tumors of the Heart.............................................5
Cardiac Transplantation......................................5
Cardiac Devices....................................................5
The Heart Both reflect compensatory changes in response to volume and/or
- remarkably efficient, durable, and reliable pump pressure overloads
- propelling more than 7500 L of blood through the body
each day, and beating more than 40 million times a year Cardiomegaly
- wellspring for tissue oxygenation, nutrition, and waste
- Increased cardiac weight / size (or both)
removal
- From hypertrophy and/or dilation
- 8 wks gestation: heart and vasculature are the first fully
functional organ system Myocardium
- pumping function of the heart occurs through coordinated
Cardiovascular disease
contraction (during systole) and relaxation (during
o including coronary artery disease [CAD], stroke, diastole) of cardiac myocytes (the myocardium)
and peripheral vascular disease
Left ventricular myocytes Right ventricular myocytes
o the number-one cause of worldwide mortality - a spiral circumferential - less structured organization,
orientation generating overall less robust
Cardiac Structure and Specializations
- generate vigorous coordinated contractile forces.
- heart weight varies with body habitus waves of contraction - Contraction is achieved by
- Average weight: - spreading from the cardiac shortening of serial contractile
o 0.4% to 0.5% of body weight apex to the base of the heart elements (sarcomeres) within
o M: 300-360 g parallel myofibrils.
o F: 250-320 g Atrial cardiomyocytes Ventricular myocytes
- Hypertrophy: Increased heart weight or ventricular - have cytoplasmic storage - contain B-type natriuretic
thickness granules peptide
- Dilation: enlarged chamber size - contain atrial natriuretic
peptide
- protein hormones that are released in response to
NAJITO, Czarina Marie D. Page 1
Robbins Patho, 10 e.
increased stretch a. (e.g., vagal stimulation)
- promote arterial vasodilation and stimulate renal salt and 2. extrinsic adrenergic agents
water elimination (natriuresis and diuresis) a. (e.g., circulating adrenaline)
3. hypoxia, and potassium concentration
a. (i.e., hyperkalemia can block signal transmission
Valves
altogether)
- maintain unidirectional blood flow
- Valve function depends on the mobility, pliability, and Components of conduction system
structural integrity of the leaflets of the atrioventricular
valves (tricuspid and mitral) or cusps of the semilunar Sinoatrial (SA) node at the junction of the right
valves (aortic and pulmonary) pacemaker atrial appendage and SVC
Atrioventricular (AV) node located in the right atrium
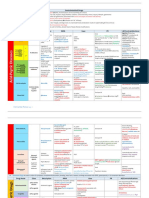
CARDIAC VALVES along the interatrial septum
Atrioventricular valves Semilunar valves Bundle of His (AV bundle) connecting the right atrium to
Tricuspid Valve Aortic Valve the ventricular septum
Mitral Valve Pulmonary Valve Right and Left bundle branch stimulate their respective
Competence depends on the Function depends on the divisions ventricles via further
proper function of the leaflets, integrity and coordinated arborization into the
tendinous cords, and the movements of the cuspal Purkinje network
attached papillary muscles of attachments. The cells of the cardiac conduction system depolarize spontaneously,
the ventricular wall potentially enabling all of them to function as cardiac pacemakers.
Valvular insufficiency Valvular regurgitation
Left ventricular dilation, a dilation of the aortic root SA node
ruptured cord, or papillary
muscle dysfunction that can - 60 to 100 beats/min
interfere with mitral valve - faster than the other components
closure - it normally sets the pace
If nodal tissues become dysfunctional, other cells in the conduction
- Lined by endothelium system can take over, generating, for example, a junctional escape
rhythm (usually at a much slower rhythm).
Layers of cardiac valves
AV node
1. Fibrosa layer
o dense collagenous layer at the outflow surface - has a gatekeeper function
o connected to the valvular supporting structures - by delaying the transmission of signals from the atria to the
o providing mechanical integrity ventricles, it ensures that atrial contraction precedes
ventricular systole
2. Spongiosa layer
o central core of loose connective tissue Blood Supply
3. Ventrucularis or atrialis layer Cardiac myocytes rely almost exclusively on oxidative
o depending on which chamber it faces phosphorylation for their energy needs.
o layer rich in elastin on the inflow surface
o providing leaflet recoil High density of mitochondria (20% to 30% of myocyte
volume)
Cardiac valves Myocardial energy generation also requires a constant
supply of oxygenated blood
thin enough to be nourished by diffusion from the blood
normal leaflets and cusps have only scant blood vessels Myocardium is extremely vulnerable to ischemia.
limited to the proximal portion of the valve
does not express ABO or histocompatibility antigens Nutrients and oxygen are delivered via the coronary arteries with
cryopreserved valvular tissues can be transplanted with ostia immediately distal to the aortic valve
relative impunity
↓
Conduction System
Initially course along the external surface of the heart (epicardial
Coordinated contraction of the cardiac muscle depends on the
coronary arteries)
initiation and rapid propagation of the cardiac initiation and rapid
propagation of electrical impulses ↓
Frequency of electrical impulses is sensitive to: penetrate the myocardium (intramural arteries)
1. neural inputs ↓
NAJITO, Czarina Marie D. Page 2
Robbins Patho, 10 e.
Subsequently branching into arterioles octogenarians (and older) also
frequently have deposition of
↓ extracellular amyloid
- Valvular aging changes are major contributors to
forming a rich arborizing vascular network so that each myocyte
significant valvular disease
contacts roughly three capillaries.
- Progressive atherosclerosis + strong aging component:
- Right and left coronary arteries function as end arteries major cause of IHD
o Even though there are is the presence of collateral
circulation
- Blood flow to the myocardium occurs during ventricular
diastole
o after closure of the aortic valve
o when the microcirculation is not compressed by
cardiac contraction
- At rest, diastole comprises approximately two thirds of the
cardiac cycle
- With tachycardia (increased heart rate), the relative
duration of diastole also shortens, thus potentially
compromising cardiac perfusion.
Cardiac Regeneration
Considerable interest in exploring the possibility of replacing
damaged myocardium by inducing cardiac regeneration in vivo or
implanting stem cell–derived cardiac cells
- myocardium of mammals has a very low replicative
potential after fetal and neonatal life
o less than 1% cardiomyocyte turnover per year in
adult humans
- stimulating cardiac regeneration in vivo in humans could
facilitate recovery of myocardial function after a host of
injurious stimuli
o Implanted cells may show some cardiomyocyte
differentiation
o durability of this benefit has been limited,
o they do not contribute significantly to restoration
of contractile force
o failure to successfully integrate these cells into
Overview of Cardiac Pathophysiology
the conduction pathway of the host heart carries
pathophysiologic pathways that result in a “broken” heart distill down
the very real risk of autonomous arrhythmic foci.
to six principal mechanisms:
Effects of Aging on the Heart
Failure to pump Cardiac muscle contracts
Most forms of heart disease become more prevalent with each
weakly
advancing decade
Systolic dysfunction Chambers cannot empty
- size of the left ventricular cavity, particularly in the base- properly
to-apex dimension, is reduced in later life Diastolic dysfunction Myocardium cannot relax
sufficiently to permit
o exacerbated by systemic hypertension
ventricular filling
as the basal ventricular septum Obstruction to flow Overworked myocardium,
protrudes into the left ventricular which must pump against the
outflow tract (so-called sigmoid obstruction
septum) e.g. calcific aortic valve Lesions that prevent valve
o Elderly heart stenosis opening
Lesser myocytes (degenerative e.g. systemic hypertension, cause increased ventricular
attrition) aortic coarctation chamber pressures
Increased connective tissue Regurgitant flow Backward blood flow
Increased volume workload
May overwhelm the pumping
capacity of the affected
NAJITO, Czarina Marie D. Page 3
Robbins Patho, 10 e.
chambers Sudden Cardiac Death
Shunted flow Divert blood inappropriately
Lead to pressure and volume
overloads Hypertensive Heart Disease
Disorders of cardiac Arrhythmias
conduction Uncoordinated cardiac
impulses or blocked conduction Systemic (Left-Sided) Hypertensive Heart Disease
pathways
Rupture of heart or major Loss of circulatory continuity
vessel Lead to massive blood loss,
hypotensive shock, Pulmonary (Right-Sided) Hypertensive Heart Disease (Cor
and death Pulmonale)
- Most cardiovascular disease results from a complex Valvular Heart Disease
interplay of genetics and environmental factors
o can disrupt signaling pathways that control
morphogenesis Calcific Valvular Degeneration
o affect myocyte survival after injury
o affect contractility or electrical conduction in the
Mitral Valve Prolapse (Myxomatous Degeneration of the Mitral
face of biomechanical stressors.
- Congenital heart defects Valve)
o involves an underlying genetic abnormality
modified by environmental factors. Rheumatic Fever and Rheumatic Heart Disease
- Genes that control the development of the heart may also
regulate the response to various forms of injury including
aging. Infective Endocarditis (IE)
- Subtle polymorphisms can significantly affect the risk of
many forms of heart disease, and
- Adult-onset heart disorders have a fundamentally genetic Noninfected Vegetations
basis.
- Cardiovascular genetics provides an important window on Carcinoid Heart Disease
the pathogenesis of heart disease and molecular diagnoses
are increasingly a critical part of its classification.
Heart Failure
Cardiac Hypertrophy: Pathophysiolgy and Progression to Heart
Failure
Cardiac Development
Congenital Heart Disease
Ischemic Heart Disease
Myocardial Infarction
Chronic Ischemic Heart Disease
Arrhythmias
NAJITO, Czarina Marie D. Page 4
Robbins Patho, 10 e.
Complications of Prosthetic Valves
Cardiomyopathies
Dilated Cardiomyopathy
Arrhythmogenic Cardiomyopathy
Hypertrophic Cardiomyopathy
Restrictive Cardiomyopathy
Myocarditis
Other Causes of Myocardial Disease
Pericardial Disease
Pericardial Effusion and Hemopericardium
Pericarditis
Tumors of the Heart
Primary Cardiac Tumors
Metastatic Neoplasms
Cardiac Transplantation
Cardiac Devices
Ventricular Assist Devices
Electrocardiogram
History
NAJITO, Czarina Marie D. Page 5
You might also like
- Histology - Git Table 1Document1 pageHistology - Git Table 1lcrujidoNo ratings yet
- Trans 1 - Cells As A Unit of Health and DiseaseDocument12 pagesTrans 1 - Cells As A Unit of Health and DiseaseCedrick BunaganNo ratings yet
- WBC Lymph Node SpleenDocument12 pagesWBC Lymph Node Spleendr brijesh TiwariNo ratings yet
- Sources of Parasitic InfectionDocument74 pagesSources of Parasitic InfectionCristy Jean100% (1)
- 07 Pathological ClacificationDocument10 pages07 Pathological Clacificationraanja2No ratings yet
- Malassezia Furfur An-An Ap-Ap Naturally Found On The SkinDocument48 pagesMalassezia Furfur An-An Ap-Ap Naturally Found On The SkinNikki ValerioNo ratings yet
- HAEMOPOIESISDocument6 pagesHAEMOPOIESISDiyana ZahariNo ratings yet
- Patho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Document12 pagesPatho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Grant GarcesNo ratings yet
- Genetic and Pediatric Diseases Chapter SummaryDocument16 pagesGenetic and Pediatric Diseases Chapter SummaryJustine HungNo ratings yet
- Pathology of the Central Nervous System: Edema, Malformations, TraumaDocument6 pagesPathology of the Central Nervous System: Edema, Malformations, TraumaNica Lopez FernandezNo ratings yet
- Pediatrics SamplexDocument6 pagesPediatrics SamplexThea SansonNo ratings yet
- Microbiology: Presented by Alyazeed Hussein, BSCDocument64 pagesMicrobiology: Presented by Alyazeed Hussein, BSCT N100% (1)
- 3 Surgery - Mediastinum and PleuraDocument6 pages3 Surgery - Mediastinum and PleuraCassey Koi FarmNo ratings yet
- Ninja On Fleek - Fern Charts MT2 SLAY Most UpdatedDocument56 pagesNinja On Fleek - Fern Charts MT2 SLAY Most UpdatedyenniNo ratings yet
- Chapter 11 Blood Vessels 8th Ed NotesDocument7 pagesChapter 11 Blood Vessels 8th Ed NotesKyle Christopher SiaNo ratings yet
- Pathology - Lab: Pathology of The HeartDocument8 pagesPathology - Lab: Pathology of The HeartRazel PerezNo ratings yet
- Chapter 10 - Diseases of Infancy and ChildhoodDocument17 pagesChapter 10 - Diseases of Infancy and ChildhoodAgnieszka WisniewskaNo ratings yet
- Reticulo Endothelial SystemDocument15 pagesReticulo Endothelial Systemssdb14No ratings yet
- Sketchy TrackerDocument36 pagesSketchy Trackerpsy killNo ratings yet
- Clinpath - : Red Blood CellsDocument14 pagesClinpath - : Red Blood CellsYolanda Primrosa NurhanNo ratings yet
- Pathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & ThymusDocument5 pagesPathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & Thymusangel_sagun_1No ratings yet
- Systemic Pathology Study NotesDocument33 pagesSystemic Pathology Study NotesLaura BourqueNo ratings yet
- Anti-Anemia and Hematopoietic Growth FactorsDocument8 pagesAnti-Anemia and Hematopoietic Growth FactorsIsabel CastilloNo ratings yet
- Ilovepdf Merged PDFDocument177 pagesIlovepdf Merged PDFNishankumar JhaNo ratings yet
- Fluids and Electrolytes Management in Surgical PatientsDocument4 pagesFluids and Electrolytes Management in Surgical PatientsJanine Maita BalicaoNo ratings yet
- Major Bacterial Genera TableDocument12 pagesMajor Bacterial Genera TablemojdaNo ratings yet
- Heart - PathologyDocument22 pagesHeart - Pathologyjmosser100% (1)
- Hormone Site of Secretion Stimuli For Secretion Actions: BiliaryDocument5 pagesHormone Site of Secretion Stimuli For Secretion Actions: BiliaryLace AzoresNo ratings yet
- Physiologic MonitoringDocument4 pagesPhysiologic MonitoringAimie DagaleaNo ratings yet
- Yeast Invasion of Male's Central Nervous SystemDocument9 pagesYeast Invasion of Male's Central Nervous SystemRomie SolacitoNo ratings yet
- 1 PATHO 2a - Inflammation - Dr. BailonDocument12 pages1 PATHO 2a - Inflammation - Dr. BailontonNo ratings yet
- Parasitic Diseases at a GlanceDocument2 pagesParasitic Diseases at a GlanceStarrie94No ratings yet
- Tissue TableDocument4 pagesTissue TableMarcie BooneNo ratings yet
- Clinical Medicine - Lecture: - Topic: - DateDocument3 pagesClinical Medicine - Lecture: - Topic: - DateqselmmNo ratings yet
- The Kidney: Glomerular Diseases, Nephrotic Syndrome, and Acute Renal FailureDocument11 pagesThe Kidney: Glomerular Diseases, Nephrotic Syndrome, and Acute Renal FailureElina Drits100% (1)
- 3rd Year TipsDocument5 pages3rd Year TipsDianne Joy PascuaNo ratings yet
- The Complement SystemDocument4 pagesThe Complement SystemExamville.com100% (1)
- 3 Year CPC October 8, 20202Document4 pages3 Year CPC October 8, 20202Raian SuyuNo ratings yet
- Bates Outline of Chapter 8Document15 pagesBates Outline of Chapter 8KatherynSotoNo ratings yet
- Robbins Ch. 18 Liver and Biliary Tract Review QuestionsDocument12 pagesRobbins Ch. 18 Liver and Biliary Tract Review QuestionsPA2014No ratings yet
- Hematologymnemonics 151002194222 Lva1 App6891Document8 pagesHematologymnemonics 151002194222 Lva1 App6891padmaNo ratings yet
- Pathology - Chapter 14Document14 pagesPathology - Chapter 14Cory GrayNo ratings yet
- Pathology - Lab: Pathology of The Blood VesselsDocument5 pagesPathology - Lab: Pathology of The Blood VesselsRazel PerezNo ratings yet
- Cardiac Physiology & Pathology TopicsDocument3 pagesCardiac Physiology & Pathology TopicsByeongsu Park100% (1)
- Hemostasis and Thrombosis: OutlineDocument11 pagesHemostasis and Thrombosis: OutlineManila MedNo ratings yet
- Inflammation and Repair OverviewDocument10 pagesInflammation and Repair OverviewMiguel Cuevas DolotNo ratings yet
- Cell Injury & AdaptationDocument22 pagesCell Injury & AdaptationUmam LoyalNo ratings yet
- Small Intestine Lesions Comparison ChartDocument9 pagesSmall Intestine Lesions Comparison ChartfadoNo ratings yet
- Accessory Glands of the Digestive SystemDocument12 pagesAccessory Glands of the Digestive SystemSheena PasionNo ratings yet
- Fatty Liver (1) - General PathologyDocument22 pagesFatty Liver (1) - General PathologyDarien LiewNo ratings yet
- HS202 Pathology ExamDocument6 pagesHS202 Pathology ExamJulio dR AltavasNo ratings yet
- (CLINPATH) Lipids and DyslipoproteinemiaDocument5 pages(CLINPATH) Lipids and DyslipoproteinemiaJolaine ValloNo ratings yet
- Chapter 7 - NeoplasiaDocument23 pagesChapter 7 - NeoplasiaAgnieszka WisniewskaNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Pathology Cell InjuryDocument57 pagesPathology Cell InjuryMajd MustafaNo ratings yet
- Harrisons: Introduction To Infectious DiseasesDocument3 pagesHarrisons: Introduction To Infectious Diseasesapi-3704562No ratings yet
- Robbins Pathology Chapter 17 Liver and Biliary TractDocument2 pagesRobbins Pathology Chapter 17 Liver and Biliary Tractscorpiosphinx79No ratings yet
- Pharmacology of EthanolDocument5 pagesPharmacology of EthanolJoshua RemonNo ratings yet
- PD 17 To 21Document148 pagesPD 17 To 21Loai Mohammed IssaNo ratings yet
- Systemic Effects of Inflammation: The Acute Phase ResponseDocument3 pagesSystemic Effects of Inflammation: The Acute Phase ResponseJenward Hostallero100% (1)
- StrokeDocument5 pagesStrokeCM NajitoNo ratings yet
- Glutamate: Neurotransmitters Disturbed Increased Sympathetic Stimulation Increased Autonomic StimulationDocument3 pagesGlutamate: Neurotransmitters Disturbed Increased Sympathetic Stimulation Increased Autonomic StimulationCM NajitoNo ratings yet
- Thought DisordersDocument3 pagesThought DisordersCM NajitoNo ratings yet
- Idoc - Pub Sketchy-MicroDocument2 pagesIdoc - Pub Sketchy-MicroCM NajitoNo ratings yet
- PsychosisDocument4 pagesPsychosisCM NajitoNo ratings yet
- Image CC BY-SA 4.0: HypertensionDocument3 pagesImage CC BY-SA 4.0: HypertensionCM NajitoNo ratings yet
- Management of Diabetic Neuropathy - UpToDateDocument19 pagesManagement of Diabetic Neuropathy - UpToDateCM NajitoNo ratings yet
- Tumor Kidney FailureDocument6 pagesTumor Kidney FailureCM NajitoNo ratings yet
- Lecturio Schizophrenia QuestionsDocument3 pagesLecturio Schizophrenia QuestionsCM NajitoNo ratings yet
- How To Interpret An ECG in Seven StepsDocument5 pagesHow To Interpret An ECG in Seven StepsCM NajitoNo ratings yet
- Childhood EpilepsyDocument3 pagesChildhood EpilepsyCM NajitoNo ratings yet
- Image CC BY-SA 3.0: Term MeaningDocument4 pagesImage CC BY-SA 3.0: Term MeaningCM NajitoNo ratings yet
- Myocardial InfarctionDocument3 pagesMyocardial InfarctionCM NajitoNo ratings yet
- Robbins 15 - Chronic Diffuse Interstitial DiseaseDocument12 pagesRobbins 15 - Chronic Diffuse Interstitial DiseaseCM NajitoNo ratings yet
- Diabetic Autonomic Neuropathy - UpToDateDocument27 pagesDiabetic Autonomic Neuropathy - UpToDateCM NajitoNo ratings yet
- Prognosis - Rule of 5, 3, and 2:: Image CC BY 3.0Document3 pagesPrognosis - Rule of 5, 3, and 2:: Image CC BY 3.0CM NajitoNo ratings yet
- Epidemiology and Classification of Diabetic Neuropathy - UpToDateDocument10 pagesEpidemiology and Classification of Diabetic Neuropathy - UpToDateCM NajitoNo ratings yet
- Sign117 TonsillectomyDocument44 pagesSign117 TonsillectomySherynneNo ratings yet
- Approach To PX With HFDocument1 pageApproach To PX With HFCM NajitoNo ratings yet
- Classification and Causes of Mitral InsufficiencyDocument3 pagesClassification and Causes of Mitral InsufficiencyCM NajitoNo ratings yet
- Causes Presentation: Staphylococcus AureusDocument3 pagesCauses Presentation: Staphylococcus AureusCM NajitoNo ratings yet
- 2022 Yearly Blank Calendar TemplateDocument1 page2022 Yearly Blank Calendar TemplateCM NajitoNo ratings yet
- Image CC By-Sa 3.0: Hypertension Coronary Heart Disease Myocardial InfarctionDocument6 pagesImage CC By-Sa 3.0: Hypertension Coronary Heart Disease Myocardial InfarctionCM NajitoNo ratings yet
- Ecg Module 3Document16 pagesEcg Module 3Muhammad BilalNo ratings yet
- Pharyngitis: Signs and SymptomsDocument26 pagesPharyngitis: Signs and SymptomsCM NajitoNo ratings yet
- Philippine Clinical Practice Guidelines On The Diagnosis and Management of Obstructive Sleep Apnea in AdultsDocument75 pagesPhilippine Clinical Practice Guidelines On The Diagnosis and Management of Obstructive Sleep Apnea in AdultsDiane IsmaelNo ratings yet
- WWW - Medicalppt.: For More Free Medical Powerpoint Presentations Visit WebsiteDocument15 pagesWWW - Medicalppt.: For More Free Medical Powerpoint Presentations Visit WebsiteJoko Sutrisno,S.Kep,Ns.M.KesNo ratings yet
- ECG Rhythm InterpretationDocument21 pagesECG Rhythm Interpretationvanstar7100% (1)
- For More Free Medical Powerpoint Presentations Visit WebsiteDocument24 pagesFor More Free Medical Powerpoint Presentations Visit Websitevanstar7No ratings yet
- Multi Speciality Hospital: Mr. NishantDocument1 pageMulti Speciality Hospital: Mr. NishantNishant Kumar SinghNo ratings yet
- Genome Analysis Multiple Choice Question (GuruKpo)Document14 pagesGenome Analysis Multiple Choice Question (GuruKpo)GuruKPO93% (15)
- Lesions of The Visual PathwayDocument2 pagesLesions of The Visual PathwayM StojanovskaNo ratings yet
- Sensory DisordersDocument5 pagesSensory DisordersMartin PersianNo ratings yet
- Midterm Examination-BiochemDocument10 pagesMidterm Examination-BiochemRhizel Marie Cauilan FariñasNo ratings yet
- 152 409 1 PBDocument2 pages152 409 1 PBRendra Syani Ulya FitriNo ratings yet
- Identifying Chromosomes 12 and 14Document3 pagesIdentifying Chromosomes 12 and 14AstatinNo ratings yet
- The Emerging Role of Serratiopeptidase in Oral Surgery: Literature UpdateDocument5 pagesThe Emerging Role of Serratiopeptidase in Oral Surgery: Literature UpdatejklhjNo ratings yet
- Herbal - Medicines - in - The - Treatment of Mental IllnessesDocument12 pagesHerbal - Medicines - in - The - Treatment of Mental IllnessesFarash farshiNo ratings yet
- Neural Tube DefectsDocument5 pagesNeural Tube DefectsAnjesh100% (1)
- Manage Cellulitis at HomeDocument2 pagesManage Cellulitis at HomeAnonymous 4txA8N8etNo ratings yet
- Drugs Used in Disorders of The EyesDocument21 pagesDrugs Used in Disorders of The EyesDhea.MutiaraNo ratings yet
- Annals of Medicine and Surgery: SciencedirectDocument4 pagesAnnals of Medicine and Surgery: SciencedirectLee제노No ratings yet
- Managing Health in The Aluminium IndustryDocument346 pagesManaging Health in The Aluminium IndustryWellfro100% (1)
- TUMOR MARKERS (Hand-Out) EDITDocument36 pagesTUMOR MARKERS (Hand-Out) EDITAliza Dewi FortuaNo ratings yet
- Preemptive Cardiac Resynchronization Therapy To Prevent Cardiac Arrest in Peripartum Cardiomyopathy: A Case ReportDocument5 pagesPreemptive Cardiac Resynchronization Therapy To Prevent Cardiac Arrest in Peripartum Cardiomyopathy: A Case Reportvanilla wottledNo ratings yet
- Sturge-Weber Syndrome. Study of 55 PatientsDocument7 pagesSturge-Weber Syndrome. Study of 55 PatientsdzhzrnNo ratings yet
- Super Simplified Pathology Hematology - Dr. Priyanka SachdevDocument500 pagesSuper Simplified Pathology Hematology - Dr. Priyanka SachdevMohd SaquibNo ratings yet
- Emergency Department Chest Pain Evaluation PathwayDocument2 pagesEmergency Department Chest Pain Evaluation Pathwaymuhammad sajidNo ratings yet
- PSSS-1: Christian Rendy C Rendy Andhika Sulaeman Andrianto Susilo Theodorus SuwendiDocument30 pagesPSSS-1: Christian Rendy C Rendy Andhika Sulaeman Andrianto Susilo Theodorus SuwendiSulaeman Andrianto SusiloNo ratings yet
- EEG For DummiesDocument10 pagesEEG For DummiesJosé GuevaraNo ratings yet
- Challenging Cases in Neonatology 2018Document388 pagesChallenging Cases in Neonatology 2018Sabera Kapasi100% (1)
- Understanding Amnestic DisordersDocument31 pagesUnderstanding Amnestic DisordersKhadija ArshadNo ratings yet
- Nonmalignant Leukocyte DisordersDocument30 pagesNonmalignant Leukocyte DisordersKerstine SottoNo ratings yet
- Perception & CoordinationDocument60 pagesPerception & CoordinationRellie CastroNo ratings yet
- Veterinary Internal Medicine Handbook for Field CasesDocument88 pagesVeterinary Internal Medicine Handbook for Field CasesShakil MahmodNo ratings yet
- Differential Diagnosis - NewDocument11 pagesDifferential Diagnosis - NewMøĦãmèd Gämãl GømǮãNo ratings yet
- HSV Lesions and Recurrence RisksDocument24 pagesHSV Lesions and Recurrence RisksMichael Jansen SulaimanNo ratings yet
- Inotropic and Vasoactive Drugs in Pediatric ICUDocument6 pagesInotropic and Vasoactive Drugs in Pediatric ICUCandy RevolloNo ratings yet
- The Perme Scale Score As A Predictor of Functional Status and Complications After Discharge From The Intensive Care Unit in Patients Undergoing Liver TransplantationDocument6 pagesThe Perme Scale Score As A Predictor of Functional Status and Complications After Discharge From The Intensive Care Unit in Patients Undergoing Liver TransplantationKaren MuñozNo ratings yet