Professional Documents
Culture Documents
Pleural Effusion in Dengue: Karachi Perspective: Saudi Medical Journal January 2011
Pleural Effusion in Dengue: Karachi Perspective: Saudi Medical Journal January 2011
Uploaded by
Nico DwikiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pleural Effusion in Dengue: Karachi Perspective: Saudi Medical Journal January 2011
Pleural Effusion in Dengue: Karachi Perspective: Saudi Medical Journal January 2011
Uploaded by
Nico DwikiCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/49735174
Pleural effusion in dengue: Karachi perspective
Article in Saudi medical journal · January 2011
Source: PubMed
CITATIONS READS
9 1,126
3 authors, including:
Kiran Ejaz Munawar Khursheed
54 PUBLICATIONS 311 CITATIONS
National Institute of Cardiovascular Diseases (NICVD)
44 PUBLICATIONS 184 CITATIONS
SEE PROFILE
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Trend over time; A structural review of articles published in Journal of Pakistan Medical Association from 1953-2009 View project
All content following this page was uploaded by Munawar Khursheed on 01 April 2015.
The user has requested enhancement of the downloaded file.
Pleural effusion in dengue
Karachi perspective
Kiran Ejaz, MBBS, Munawar Khursheed, MBBS, DABIM, Ambreen Raza, MBBS.
ABSTRACT Methods: We conducted a cross-sectional study on
patients admitted to Aga Khan University Hospital,
f be
Karachi, Pakistan from January 2005 to September
oo ll
2008. Records of 663 dengue patients were
pr wi
reviewed. Demographic data, respiratory complaints,
al ct
radiographic studies, and final outcome were studied.
fin stra
Presentation and radiological modality confirming the
diagnosis of pleural effusion were noted. Descriptive
on f ab
statistics followed by Chi-Square test were applied,
testing against an alpha of 0.05 and 95% confidence
ere n o
interval (CI).
d h tio
rte la
Results: Three hundred and fifty-four (53%) out
se ns
of a total of 663 dengue syndrome patients did not
in tra
complain of any respiratory symptoms at presentation,
nor did their medical examination elicit any suspicion
ic
of PE. Hence, no radiological study was advised.
ab
Amongst the remaining 309 patients, 299 (97%)
Ar
underwent chest x-ray and 10 (3%) had abdominal
ultrasound. The pleural effusion was noted in 50
(16%) patients (31 male and 19 female patients, with
a mean age of 32±15 years). A right-sided pleural
effusion was found in 23/50 (46%) patients, left sided
in 9/50 (18%), and 18/50 (36%) patients had pleural
effusion on both sides. Out of the radiologically
confirmed pleural effusion dengue patients, 44/50
(88%) showed altered hemo-concentration with
an insignificant odds ratio of 0.7 (p=0.56, 95% CI:
0.263-2.066).
Conclusion: Compared to other studies, fewer
numbers of our patients suffered from pleural effusion.
The diagnostic modality preferred by the physician
was the chest x-ray.
Saudi Med J 2011; Vol. 32 (1):
From the Department of Emergency Medicine, Aga Khan University,
Karachi, Pakistan.
Objectives: To study the presentation of pleural Received 1st August 2010. Accepted 22nd November 2010.
effusion among dengue patients in Pakistan and to
Address correspondence and reprint request to: Dr. Kiran Ejaz, Research
explore limitations in the diagnosis of these patients Associate, Department of Emergency Medicine, Aga Khan University,
by the physicians of a developing country. B-82 Block 10, Federal ‘B’ Area, PO Box 75950, Karachi, Pakistan.
Tel. +92 (213) 6361312. E-mail: drkiranejaz@gmail.com
179
Pleural20100385 179 12/5/10 10:13:02 AM
Pleural effusion in dengue ... Ejaz et al
R esurgence of dengue syndrome (DS) is noted in
most Asian countries.1 A lot has been written in
terms of presentation and management in this context.
after literature search and validated by an expert on the
subject. Demographic data, respiratory complaints,
radiographic studies, and final outcome were studied.
However, physicians miss signs of pleural effusion (PE) Presence or absence of PE in known dengue patients
in differentiating the milder form from severe disease, was noted with respect to clinical examination and
and hence the prognosis profile is affected. Severity radiological modality. Laboratory parameters were also
of disease with an increased percentage of plasma correlated with presence of PE. Dengue severity levels
leakage has been noted. One of the WHO criteria such as DF, DHF and dengue shock syndrome (DSS)
for diagnosing dengue hemorrhagic fever (DHF) were taken as labeled by the attending physician. Altered
is evidence of increased plasma leakage along with hemo-concentration as defined by the WHO criteria is
other criteria.2 Compared to younger adults, elderly thrombocytopenia of <100,000/mm3 and hematocrit
individuals have significantly lower incidences of PE.3 of ≥20% of the baseline for the same age, gender, and
A clinical observation shows the PE in dengue is mostly population.2
mild and self-limiting, requiring only observation Data was double entered and later analyzed using
with no major intervention such as pleural tap. A the Statistical Package for Social Sciences (SPSS Inc,
well-trained clinical hand on initial visit can help such Chicago, IL, USA) version 16. Initially, the complete
patients by avoiding unnecessary radiological exposure data set of 663 was used for analysis. However, to remove
and cost. The types of radiological modalities used for under estimation in calculation, only 50 radiologically
its detection also play an important role. Most studies proven PE cases were used for further statistical analysis.
have shown abdominal, and thorax ultrasound to be Chi-square test with odds ratio was applied according
better in detecting fluid levels.4,5 Guidelines are lacking to nominal variables to test the relation between PE
on what should be the radiological modality of choice and altered hemo-concentration in these DS patients.
in a developing country, where skilled radiologists and Statistical testing was carried out against an alpha of
facilities are limited. Money spent on a radiological 0.05 and 95% confidence interval (CI).
study can and usually is enough to treat the patient
with these milder presentations. Symptoms of effusion Results. According to our data 354 (53%) out
and ascites are noted as early signs of the disease. of a total of 663 DS patients did not complain of
Abdominal ultrasound (U/S) has been recommended as any respiratory symptoms at presentation, nor did
the first-line imaging modality with suspected dengue their medical examination elicit any suspicion of PE.
fever (DF) to detect early signs, even before obtaining Hence, no radiological study was advised. Amongst the
serological confirmation.6 The primary infection or remaining 309 patients, 299 (97%) underwent chest
the first infection with dengue is self-limiting and the x-ray (CXR), and 10 (3%) had abdominal ultrasound.
diagnosis is usually made clinically. Studies leading to The PE was noted in 50 (16%) patients, and was absent
guidelines have been carried out elsewhere,2 but not in 259 (84%). The rest of the analysis was carried out
in the regional setting of South East Asia and Karachi, with only those who had radiologically proven PE. Out
Pakistan. We decided to explore its presentation in our of these 50 patients, 31 (62%) were male and 19 (38%)
patients, with the limitations of our health care system. female. Their mean age was 32±15 years. The severity
Therefore, we studied the presentation of PE among of DS (n=45) was evident as DF in 43 (96%), DHF
dengue patients in Pakistan, to explore limitations in in one (2%), and DSS in one (2%) patient. Dengue
the diagnosis of these patients by the physicians of a IgM was positive in 32/45 (71%), negative in 8/45
developing country. (18%), and laboratory reports were not traceable in
5/45 (11%) patients. Comparison of the severity of
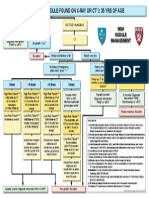
Methods. After acquiring ethical approval from the effusion to side of PE is shown in Figure 1. Out of the
institute’s Ethical Review Committee, we conducted a radiologically confirmed PE dengue patients, 44/50
cross-sectional study. A retrospective chart review of all (88%) showed altered hemo-concentration (p=0.56,
patients was carried out from January 2005 to September 95% CI: 0.263-2.066) with an odds ratio of 0.736.
2008. Patients admitted to Aga Khan University Hospital, Most of the patients were treated and sent home. Table
Karachi, Pakistan with a diagnosis of DS were included. 1 demonstrates the comparison of severity of dengue
A total of 663 patients were identified and included as to PE. Fever was the chief complaint of these patients,
per the hospital’s medical records. Patients not admitted with a mean duration of 6±2 days. No hemorrhagic
to the hospital, or either treated and discharged from manifestation of any form was seen in 47 (94%) out
the Emergency Department (ED), or seen at the of 50 radiological proven PE patients. Complaints of
outpatient clinic for the disease were excluded. Data dyspnea were present in only 2 (4%) (corrections are
was collected with a pretested questionnaire designed made ) patients. Among the patients showing signs or
180 Saudi Med J 2011; Vol. 32 (1) www.smj.org.sa
Pleural20100385 180 12/5/10 10:13:02 AM
Pleural effusion in dengue ... Ejaz et al
detected on CXR as the blunting of costophrenic angle.
It could be inferred that the dengue infection in most
of our patients presented with DF rather than DHF,
as evident by the global data also.7 Physicians dealing
with dengue patients place little significance on imaging
modalities and do not consider them as an important
investigation, especially when it comes to classifying the
disease as DF or DHF.
Theoretically speaking if every patient with suspected
dengue infection undergoes imaging such as CXR
or chest U/S, the results could be different and more
patients with PE could be identified. The timing of
performing a radiological examination is also important.
Figure 1 - Comparison of severity of effusion to side of pleural effusion. When performed much earlier in the disease course, a
CXR may fail to show any effusion patterns. This is the
Table 1 - Comparison of severity of dengue to pleural effusion. time when the patient has a high fever, and the plasma
leakage has not yet begun to produce an effusion.
Variable Dengue severity frequency (%) The site of effusion was recorded in only 43
DF DHF DSS
radiographs we noted, however, 23/43 (53%) of our
patients had pure right sided PE, consistent with the
Presence of effusion (n=45) 43 (96) 1 (2) 1 (2)
Severity of effusion
global data;4,7 bilateral PE was found in 13/43 (30%) of
Mild (n=36) 35 (97) 1 (3) - patients. Right sided effusion has also been observed by
Moderate (n=1) 1 (100) - - Wang et al.8 However, an interesting point that differs
Side of effusion
Right (n=23) 22 (96) 1 (4) - in our patients was the presence of isolated left sided
Left (n=7) 7 (100) - - effusion in 7/43 (16%) cases. However, the difference of
Both (n=13) 12 (92) - 1 (8) right sided 23/50 (46%) effusion versus left sided 9/50
DF - dengue fever, DHF - dengue hemorrhagic fever, (18%) is not that significant. This may be attributed
DSS - dengue shock syndrome
to genetic or anatomical differences, which might have
caused our patients to present differently. It could
Table 2 - Clinical features observed in the sample population. also be argued that perhaps CXR is not as efficient in
detecting PE.
Parameters (unit) Mean ± SD Ultrasound appears to be a significant investigation
Temperature ( C)
o
38±9 in patients with suspected dengue infection. Sonography
Systolic blood pressure (mm Hg) 113±19 has the capacity to detect minor PE.5 It can thus set
Diastolic blood pressure (mm Hg) 73±14 the course of patient management from a much earlier
Pulse pressure (beats/min) 39±16
Hematocrit (gm/dl) 42±9 point, critically before circulatory failure ensues. It
Platelets (x109/L) 37±31 has a value in both accelerating the diagnosis and
Prothrombin time (sec) (n=243) 13±3 directing confirmatory tests. Dengue can be diagnosed
Activated partial thromboplastin time (sec) (n=241) 44±15
earlier using ultrasound compared to other modes of
Sec - seconds
diagnosis.4
This brings to our attention the question of a better
modality to detect PE. In our study, a small percentage
reported respiratory problems, the radiologically study of patients underwent abdominal U/S. It is striking
was carried out within approximately 6±2 days of fever. that all showed right-sided PE. This could be because
A detailed clinical presentation of these patients is it can detect even milder effusion patterns, which are
shown in Table 2. perhaps missed on CXR. Previously, researchers in
2007 specified the limited number of CXR studies, and
we also observed the same difficulty while comparing
Discussion. The efficacy of U/S over CXR is well
our work.8 The results become even more relevant in
documented; a preference for the later over the other is our clinical settings, where we have limited resources
a debatable issue especially in developing countries.4,6 to reach the diagnosis of the disease. However, the
In this retrospective study, CXR was performed on management in all cases is supportive and intervention
most patients with dengue infection. A larger fraction is needed in seldom cases. No intervention was carried
of patients showed no signs of effusion. Small PE is out in any of our patients.
www.smj.org.sa Saudi Med J 2011; Vol. 32 (1) 181
Pleural20100385 181 12/5/10 10:13:04 AM
Pleural effusion in dengue ... Ejaz et al
Limitations to this study include the use of a secondary 2. WHO. Dengue Hemorrhagic Fever: Diagnosis, Treatment, and
data set. The abdominal U/S was performed in only 8 Control. Geneva: World Health Organization; 1997.
patients, and none underwent chest ultrasound as there 3. Lee IK, Liu JW, Yang KD. Clinical and laboratory characteristics
was no clinical indication for it. Ordering an ultrasound and risk factors for fatality in elderly patients with dengue
compared to a CXR does not alter the management, hemorrhagic fever. Am J Trop Med Hyg 2008; 79: 149-153.
and would also increase patients’ cost. Dengue 4. Venkata Sai PM, Dev B, Krishnan R. Role of ultrasound in
classification could be subjecive as the attending dengue fever. Br J Radiol 2005; 78: 416-418.
physician may not have used precise WHO 5. Quiroz-Moreno R, Mendez GF, Ovando-Rivera KM. [Clinical
classification. utility of ultrasound in the identification of dengue hemorrhagic
In conclusion, compared to other studies, fewer fever]. Rev Med Inst Mex Seguro Soc 2006; 44: 243-248.
numbers of our patients suffered from PE. Most of the Spanish
dengue patients had no respiratory complaints. The PE 6. Wu KL, Changchien CS, Kuo CH, Chiu KW, Lu SN, Kuo
was present mostly on the right side, however, it also CM, et al. Early abdominal sonographic findings in patients
showed some atypical presentation, namely, isolated with dengue fever. J Clin Ultrasound 2004; 32: 386-388.
left sided PE. The diagnostic modality preferred by our 7. Wang CC, Wu CC, Liu JW, Lin AS, Liu SF, Chung YH, et
physicians was CXR. al. Chest radiographic presentation in patients with dengue
hemorrhagic fever. Am J Trop Med Hyg 2007; 77: 291-296.
References 8. Chaturvedi UC, Nagar R, Shrivastava R. Dengue and dengue
1. Ahsan T. Dengue fever: a regular epidemic? J Pak Med Assoc haemorrhagic fever: implications of host genetics. FEMS
2008; 58: 1-2. Immunol Med Microbiol 2006; 47: 155-66.
182 Saudi Med J 2011; Vol. 32 (1) www.smj.org.sa
Pleural20100385 182 12/5/10 10:13:04 AM
Pleural effusion in dengue ... Ejaz et al
Dear Author, please read through your article carefully, make a critical review and highlight any changes you require
to be made, please also list these clearly on a separate sheet. Please pay particular attention to all authors’ names
(in English and Arabic if applicable [No changes are allowed after the signed final-galley proof ), the running title
and the footer of the first page. Check the accepted and received dates in this footer. Carefully check all legends
to figures and all column headings in tables, ensuring that total numbers in tables are correct and correspond to
results in the text of your article. Accuracy of all references are the sole responsibility of the author. Please also pay
particular attention to the spelling of all medical and non-medical words.
This is extremely important as mistakes not corrected prior to publication can cause embarrassment, more so to the
authors than the publisher. After you have signed and returned the galley proof of your article, the Journal will not
be held responsible for any errors that appear in the final print. Although erratum notices may be published, this
will only be carried out when the error is the fault of the publisher and not the author.
1. Please amend all the corrections that we did.
2. Figure 1 - this is not clear. Kindly provide the percentage of its data. For example: the grey color in the right
effusion, the black shade in the right effusion.
3. “the clinical basis and WHO guidelines themselves instead of the study investigators”. - this is not clear.
4. 2 (5%) (how did you get the 5%) .
You can pay your offprints online at http://www.smj.org.sa/online/
Please then sign on each and every page of your manuscript and return it to our office together with an indication
of whether to you wish to order re-prints of your article (see below).
Please do not hesitate to call if you have any further queries.
Please note that there is no guarantee that once the Journal is printed offprints can be obtained. The PDF available
on line is protected by password.
Not following the instructions will result in a delay in the publication of your manuscript.
Many thanks.
OFFPRINTS REQUIRED YES NO
(Please tick relevant box)
MS# 20100385
IF YES IS TICKED THEN PLEASE ENSURE
THAT YOU COMPLETE THE ENCLOSED
OFFPRINT FORM OTHERWISE OFFPRINTS
CANNOT BE ORDERED
www.smj.org.sa Saudi Med J 2011; Vol. 32 (1) 183
Pleural20100385 183 12/5/10 10:13:04 AM
Pleural effusion in dengue ... Ejaz et al
SAUDI MEDICAL JOURNAL
(Off-Prints-Original/Uninvited Review/Case Report)
PLEASE COMPLETE THIS SECTION AND RETURN WITH PROOF TO
SAUDI MEDICAL JOURNAL, ARMED FORCES HOSPITAL, PO BOX 7897, RIYADH 11159,
KINGDOM OF SAUDI ARABIA
INSTRUCTIONS FOR ORDER REPRINTS
NUMBER OF MANUSCRIPT: ................................. NO. OF PAGES: ...................................
TITLE OF MANUSCRIPT: ..................................................................................................................
CORRESPONDING AUTHOR: .........................................................................................................
Address:
(of delivery) ....................................................... Tel. No. ...............................................................
..............................................................................
.............................................................................. Fax No. ...............................................................
..............................................................................
I confirm that I wish to purchase __________ off-prints of the above manuscript (minimum is 50).
Offprint Prices
No. of pages Number of Offprints requested 50 100 200 300 400
1-4 pages Price in SR 250 500 1000 1500 2000
0ver 4 pages Price in SR 500 1000 2000 3000 4000
Minimum purchase is 50
METHOD OF PAYMENT
*I enclose a payment of ........................SR, total amount in words ......................................................
(1) Cash
(2) Cheque payable to Saudi Medical Journal
(3) Online payment http://www.smj.org.sa/online/
184 Saudi Med J 2011; Vol. 32 (1) www.smj.org.sa
Pleural20100385 184
View publication stats 12/5/10 10:13:05 AM
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Tea. Jama 2023Document12 pagesTea. Jama 2023Mitchel Cordova Loaiza100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Sem Type Contoh Thesis !Document23 pagesSem Type Contoh Thesis !Anis Syafika86% (7)
- Takeaway & Delivery Menu: Free Delivery Within Dki Jakarta With A Minimum Purchase of Idr 350,000Document10 pagesTakeaway & Delivery Menu: Free Delivery Within Dki Jakarta With A Minimum Purchase of Idr 350,000Nico DwikiNo ratings yet
- Paediatric Sequential Organ Failure Assessment (pSOFA) Score: A New Mortality Prediction Score in The Paediatric Intensive Care UnitDocument9 pagesPaediatric Sequential Organ Failure Assessment (pSOFA) Score: A New Mortality Prediction Score in The Paediatric Intensive Care UnitNico DwikiNo ratings yet
- Review On Hyperemesis GravidarumDocument16 pagesReview On Hyperemesis GravidarumNico DwikiNo ratings yet
- New Doc 2020-03-18 21.49.17Document2 pagesNew Doc 2020-03-18 21.49.17Nico DwikiNo ratings yet
- New Doc 2020-03-21 22.28.32Document3 pagesNew Doc 2020-03-21 22.28.32Nico DwikiNo ratings yet
- CamScanner 04-19-2020 19.30.31Document2 pagesCamScanner 04-19-2020 19.30.31Nico DwikiNo ratings yet
- Scanned With CamscannerDocument2 pagesScanned With CamscannerNico DwikiNo ratings yet
- Nicholas Dwiki Tanong - RSUDBEKASI - 270420Document2 pagesNicholas Dwiki Tanong - RSUDBEKASI - 270420Nico DwikiNo ratings yet
- Gold BergDocument14 pagesGold BergNico DwikiNo ratings yet
- Algorithm For Solitary Lung NoduleDocument1 pageAlgorithm For Solitary Lung NoduleMargaretDeniseDelRosarioNo ratings yet
- Hypertension Pamphlet.Document5 pagesHypertension Pamphlet.Adelerin David OluwatosinNo ratings yet
- GonorrheaDocument2 pagesGonorrheaLeizel ApolonioNo ratings yet
- B1627 Accelerating Genomic Medicine October 2022Document64 pagesB1627 Accelerating Genomic Medicine October 2022Kartik TanejaNo ratings yet
- 2021 Sugar Baby Baby BookDocument27 pages2021 Sugar Baby Baby Bookapi-583733107No ratings yet
- File PDFDocument414 pagesFile PDFAinida FahraafniNo ratings yet
- Mycology-Virology: Reflection Paper JournalDocument6 pagesMycology-Virology: Reflection Paper JournaljeffdelacruzNo ratings yet
- PT of Endotrachealt Tube IntubationDocument28 pagesPT of Endotrachealt Tube IntubationBabita DhruwNo ratings yet
- Name of Drug Mechanism of Action Indication Contraindication Side Effects Adverse Effects Nursing Consideration IndicationDocument2 pagesName of Drug Mechanism of Action Indication Contraindication Side Effects Adverse Effects Nursing Consideration IndicationBrian BaggayanNo ratings yet
- Fundamentals of Nursing Test IiDocument44 pagesFundamentals of Nursing Test IiNOslipperyslopeNo ratings yet
- Duties of Medical Officer of Health (MOHDocument11 pagesDuties of Medical Officer of Health (MOHanojan100% (1)
- Health Insurance Presentation. (Fn-26)Document19 pagesHealth Insurance Presentation. (Fn-26)m_dattaiasNo ratings yet
- Root CariesDocument9 pagesRoot CariesebillNo ratings yet
- 2 Kerala PSC Staff Nurse Previous Solved Papers Part 2 - Kerala PSC QuestionsDocument8 pages2 Kerala PSC Staff Nurse Previous Solved Papers Part 2 - Kerala PSC QuestionsMrudula SureshNo ratings yet
- Community Nutrition Instructional DesignDocument5 pagesCommunity Nutrition Instructional DesignChristine HernandezNo ratings yet
- Medical Certificate Coach Asst Coach Chaperone MC Form 3Document1 pageMedical Certificate Coach Asst Coach Chaperone MC Form 3Jerelyn Maranga MalacasteNo ratings yet
- Down SyndromeDocument9 pagesDown Syndromeapi-479463379No ratings yet
- Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationDocument45 pagesAssessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationCarlos RiosNo ratings yet
- Prenatal Postpartum CareDocument4 pagesPrenatal Postpartum CareJamie PalmeriNo ratings yet
- T2DM Risk Assessment ToolDocument2 pagesT2DM Risk Assessment TooltckhoonNo ratings yet
- Methicillin-Resistant Staphylococcus Aureus (MRSA)Document14 pagesMethicillin-Resistant Staphylococcus Aureus (MRSA)GIST (Gujarat Institute of Science & Technology)100% (1)
- Metronidazole 500mg/tab 1 Tab 3xadayDocument4 pagesMetronidazole 500mg/tab 1 Tab 3xadayCrisyl LipawenNo ratings yet
- Changing Trends in Peptic Ulcer Prevalence in A Tertiary Care Setting in The PhilippinesDocument3 pagesChanging Trends in Peptic Ulcer Prevalence in A Tertiary Care Setting in The PhilippinesRumelle ReyesNo ratings yet
- Nurse 12345: ObjectiveDocument3 pagesNurse 12345: Objectiveapi-469581420No ratings yet
- Hubungan Caring Perawat Dengan Tingkat Kecemasan Pasien Rawat Inap Di Rumah Sakit Umum Gmim Pancaran Kasih ManadoDocument7 pagesHubungan Caring Perawat Dengan Tingkat Kecemasan Pasien Rawat Inap Di Rumah Sakit Umum Gmim Pancaran Kasih ManadoSteffi Eka Nindyastuti WijayaNo ratings yet
- Relationship of Tooth Grinding Pattern During Sleep Bruxism and Temporomandibular Joint StatusDocument9 pagesRelationship of Tooth Grinding Pattern During Sleep Bruxism and Temporomandibular Joint StatusJonathan GIraldo MartinezNo ratings yet
- Handbook8 Fruit - And.vegetables-0 1Document9 pagesHandbook8 Fruit - And.vegetables-0 1Florent MalletNo ratings yet
- Nursing Care Plan Cord CareDocument1 pageNursing Care Plan Cord CareMelanie Bagasol SisonNo ratings yet