Professional Documents
Culture Documents
Posttreatment and Retention Outcomes With and Without Periodontally Accelerated Osteogenic Orthodontics Assessed Using ABO Objective Grading System
Uploaded by
zaidOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Posttreatment and Retention Outcomes With and Without Periodontally Accelerated Osteogenic Orthodontics Assessed Using ABO Objective Grading System
Uploaded by
zaidCopyright:
Available Formats
Original Article
Posttreatment and retention outcomes with and
without periodontally accelerated osteogenic
orthodontics assessed using ABO objective grading
system
Donald J. Ferguson,
Abstract
A. D. Nazarov1, L. Makki,
M. T. Wilcko2,3, W. M. Wilcko4,5 Background: The posttreatment and retention outcomes following nonextraction
orthodontic therapy, with and without corticotomy, were assessed using the American
Department of Orthodontics,
Board of Orthodontists objective grading system (OGS). Purpose: The purpose was to
European University College, Dubai
Healthcare City, UAE, 1Private
determine if the course of retention was any different following alveolar decortication and
Practice in Orthodontics, Parker, augmentation bone grafting, i.e., periodontally accelerated osteogenic orthodontics (PAOO).
Colorado, USA, 2Department of Materials and Methods: Study casts and panoramic radiographs of patients with and without
Periodontology, Case Western PAOO (28 subjects each) were selected on the basis of the following: (1) comprehensive
Reserve University, Cleveland, nonextraction orthodontic treatment using straight wire edgewise appliances for Class I
OH, 4Department of Orthodontics, crowding, (2) availability of immediate posttreatment records and retention records at least
University of Pennsylvania School of 1 year post de‑bracketing, and (3) use of Hawley removable retainers with similar wearing
Dental Medicine, Philadelphia, PA,
instructions. Results: Independent and paired t‑test statistical testing revealed the following:
3
Private Practice in Periodontology,
5
Private Practice in Orthodontics,
(1) Posttreatment orthodontic outcomes were the same, with or without corticotomy.
Erie, Pennsylvania, USA (2) During retention, 5 of 8 ABO grading criteria improved for the sample without
corticotomy, and 6 of 8 ABO grading criteria improved for the group with corticotomy.
(3) Retention outcome scores were lower (better) for alignment and marginal ridges in the
corticotomy‑facilitated group. (4) The total score was significantly lower (better) for the
corticotomy group at retention and the increment of total score change decreased (improved)
significantly more during retention following corticotomy. Conclusions: The retention
phase was more favorable following corticotomy because the amount of OGS total score
change demonstrated a significantly improved retention outcome following PAOO therapy.
Key words: Alveolar corticotomy, orthodontic treatment, retention outcome
INTRODUCTION clinical orthodontist, one very pragmatic goal is to achieve
excellent, long‑term results in as short an active treatment
A primary goal of orthodontic treatment includes excellent time as possible as long as the delivery of services are safe
treatment outcomes that are stable life‑long. For the and comfortable to the patient. Excellent, stable results
delivered in a shorter period of active treatment time means
Access this article online greater patient flow and clinical income. Orthodontic
Quick Response Code: therapy typically requires about 2–3 years of active care
Website:
www.apospublications.com
This is an open access article distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows
DOI: others to remix, tweak, and build upon the work non‑commercially, as long as the
10.4103/2321-1407.186434 author is credited and the new creations are licensed under the identical terms.
For reprints contact: reprints@medknow.com
Address for Correspondence:
Prof. Donald J. Ferguson, Ibn Sina Building, Block D, How to cite this article: Ferguson DJ, Nazarov AD, Makki L, Wilcko MT,
3rd Floor, Office 302, Dubai Healthcare City, P.O. Box 53382, Wilcko WM. Posttreatment and retention outcomes with and without
Dubai, United Arab Emirates. periodontally accelerated osteogenic orthodontics assessed using ABO
E-mail: fergusonloud@gmail.com objective grading system. APOS Trends Orthod 2016;6:194-9.
194 © 2016 APOS Trends in Orthodontics | Published by Wolters Kluwer - Medknow
Ferguson, et al.: Improved retention outcome with PAOO
with fixed appliances. Since early 2000, accelerated tooth versus private practice,[17] mutually exclusive treatment
movements techniques have emerged that have seriously techniques,[18‑25,37] retention techniques[26] plaster versus
challenged the 2+ years active orthodontic treatment time digital study casts,[27‑29] and different cultures.[30]
paradigm.
The specificity and sensitivity of the ABO‑OGS or
Periodontally accelerated osteogenic orthodontics C‑R Eval used for evaluation of orthodontic treatment
(PAOO) is an accelerated tooth movement technique that outcomes are the highest available for discriminating
claims active treatment times 3X to 4X more rapid than differences between treatment strategies. Advocates for
conventional, non‑surgical orthodontics. Moreover, PAOO PAOO claim a more favorable retention course following
outcomes have been shown to increase the posttreatment augmented corticotomy. While degree thesis research
stability of the mandibular anterior segment. Makki[1] has compared immediate and retention outcomes with
compared augmented corticotomy with conventionally and without PAOO therapy using the ABO‑OGS (C‑R
treated patients and demonstrated irregularity index Eval) tool,[31] the data details have not been published
change posttreatment to 5 years was + 0.4 versus + and made accessible through refereed literature. The
2.8 mm (P < 0.000) and posttreatment to 10 years was + null hypothesis tested was no difference in ABO‑OGS
0.9 versus + 2.4 mm (P < 0.000). Hence, irregularity index immediate and retention scores with and without
stability was enhanced 2.8 times at 5‑year and 2.0 times at augmented corticotomy.
10 years. To date, PAOO is the only active orthodontic
therapy shown to increase stability of the mandibular
anterior teeth posttreatment outcome; the effectiveness MATERIALS AND METHODS
of preventing increases in irregularity index compares
favorably with continuous, fixed retainer therapy in the Sample
mandibular anterior segment.[2] The sample was comprised of 56 orthodontically treated
patients with (n = 28) and without (n = 28) a history of
It has also been suggested that PAOO posttreatment PAOO therapy. The group facilitated with augmented
outcomes enjoy a better retention course compared to alveolar corticotomy (Cort+) was selected from the
conventional orthodontic therapy[3,4] but this contention stratified private patient file archives of Dr. William Wilcko,
requires an assessment of orthodontic treatment success orthodontist, Erie, Pennsylvania; average age of the Cort+
using patient posttreatment records and has not, to date, sample was mid‑twenties and mean retention period was
been demonstrated in the scholarly literature. Several 19.6 months. The conventionally treated group without
assessment indexes have been developed to objectively surgery (Conv) was randomly selected from the stratified
evaluate orthodontic treatment results.[5‑9] However, the institutional patient file archives of the Orthodontic
most precise and sensitive method to assess orthodontic Department, Saint Louis University; average Conv sample
outcomes was developed by the American Board of age was mid‑teens and the mean retention period was 16.4
Orthodontics. The ABO objective grading system (OGS) months.[31]
uses a specific instrument to measure dental casts and
uses final panoramic radiographs to judge root paralleling. Orthodontic patient records were selected based on the
Eight criteria are used by the ABO‑OGS index to rate final following criteria:
occlusion: Alignment, marginal ridge height, buccolingual 1. Nonextraction orthodontic edgewise, straight wire
inclination, occlusal relationship, occlusal contact, overjet, therapy for Class I malocclusion in the permanent
interproximal contact, and root angulation.[10] A score dentition
of “0” is given for best occlusion and alignment and for 2. Patient instructed to wear removable Hawley type
each parameter that deviates from the ideal, 1 or 2 penalty retainers full time for 6 months, then nighttime
points are provided. The ABO considers a total score of thereafter
20 points or less “successful” and records scored 30 points 3. Availability of diagnostic quality study casts taken at
or greater as “failed.” posttreatment and retention demonstrating second
molars
The ABO‑OGS renamed the Cast/Radiograph Evaluation 4. Availability of diagnostic quality panoramic radiographs
(C‑R Eval),[11] is an objective clinical examination tool that taken at posttreatment and retention
has been judged reproducible based on extensive inter‑ and 5. Retention records taken at least 1 year following
intra‑examiner reliability testing by various investigators.[12] debanding
In recent orthodontic literature, the ABO‑OGS has been 6. Orthodontic records without evidence of congenitally
used to compare treatment outcomes of postgraduate missing teeth, supernumerary teeth, and/or prosthetic
residents,[13‑16] clinical treatment outcomes of resident bridges.
APOS Trends in Orthodontics | July 2016 | Vol 6 | Issue 4 195
Ferguson, et al.: Improved retention outcome with PAOO
For the Cort+ sample, every record of each nonextraction, during retention: Occlusal contact (3.25 vs. 1.96, P = 0.004),
corticotomy‑facilitated orthodontic patient was reviewed marginal ridges (5.86 vs. 4.86, P = 0.034), interproximal
and excluded from the study based only on the sample contact (1.07 vs. 0.46, P = 0.010), root angulation (4.68
selection criteria; two corticotomy patient files were vs. 3.50, P = 0.000), and total score (30.43 vs. 27.11, P =
excluded because active treatment was terminated 0.005). For Cort+, six scores significantly improved during
prematurely in one patient, and there was a lack of retention: Alignment (2.43 vs. 1.71, P = 0.045), occlusal
compliance in the retention protocol in another patient. contact (3.57 vs. 1.71, P = 0.000), marginal ridges (5.00 vs.
For the Conv sample, patient records were continuously 3.25, P = 0.000), interproximal contact (0.57 vs. 0.11, P =
reviewed, beginning with the patient records most recently 0.010), root angulation (5.54 vs. 3.96, P = 0.000), and total
archived, until 28 subjects were located that fulfilled the score (29.82 vs. 21.79, P = 0.000) [Table 2].
subject selection criteria. Data were collected from the
routine postorthodontic treatment records taken on the day The increment of change per group for each OGS criteria
of fixed appliance removal and the at least 1 year following was calculated and compared. The amount of Cort+
removal of the active, fixed orthodontic appliance. change was insignificantly greater for 7 or the 8 criteria
but not interproximal contact. Total score change was
Procedures significantly greater for Cort+ than Conv, i.e. 8.04 versus
Each set of study casts was measured with the specialized 3.32, P = 0.003 [Table 3].
ABO‑OGS instrument, and the ABO protocol was
followed for scoring alignment, marginal ridge height,
DISCUSSION
buccolingual inclination, occlusal relationship, occlusal
contact, overjet, interproximal contact, and root angulation. No differences were found in posttreatment orthodontic
treatment outcome when Cort+ and Conv were compared.
Experimental error
Removable retention strategies were the same for both
Method error assessment was performed by randomly
groups; however, when ABO‑OGS scores were compared
selecting and re‑measuring 5 sets of study casts from each
approximately 1.5 years later, two OGS criteria scores and
sample. The error method was calculated with Dahlberg
total score differed significantly: Scores were significantly
formula: ΣD ² , where D was the difference between lower for Cort+ than Conv for alignment (1.71 vs. 3.79,
2N P = 0.003) and marginal ridges (3.25 vs. 4.86, P = 0.014).
the repeated measurements and N was the number of
double measurements made. Maximum error was 0.5 score The most dramatic finding in this study was demonstrated
points as determined by repeated measures on two separate in comparing total scores between the groups. Both
occasions as well as separate measures in one setting. groups showed significant total score improvement during
retention although the amount of improvement was
Statistical analysis
substantially greater in Cort+ (8.04 vs. 3.32, P = 0.000).
Statistical analysis of the data was performed using
No differences between the two groups in the total score
Statistical Package for Social Services (SPSS) software,
were found at posttreatment (30.93 vs. 29.82, P > 0.05),
version 15.0.1, IBM, Armonk, NY, USA. Paired t‑test was
but at retention, the total Cort+ score had dropped to be
used to determine intra‑group differences due to therapy
significantly lower (better) than Conv (21.79 vs. 27.21,
(posttreatment to retention comparisons). Independent
P = 0.011).
t‑tests were used to identify intergroup differences with
significance probability set at P ≤ 0.05. It is logical to consider that total score is a reasonable
barometer of overall outcome. While only 2 of the 8 OGS
RESULTS criteria was significantly lower for Cort+ than Conv at 1.5
years posttreatment, all OGS scores were numerically lower
Sample means and standard deviations were computed for (better) than Conv except one (root angulation). All of
the eight criteria of the ABO‑OGS plus total score. No the ABO‑OGS scores decreased (improved) in the Cort+
differences were found at posttreatment, but Cort+ scores sample whereas alignment, anteroposterior relationships,
were significantly lower at retention than Conv for alignment and overjet mean scores increased nonsignificantly in
(1.71 vs. 3.7, P = 0.003) marginal ridges (3.25 vs. 4.86, the Conv sample. Collectively, these differences during
P = 0.014) and total score (21.79 vs. 27.21, P = 0.011) [Table 1]. retention resulted in a dramatic decrease (improvement)
in Cort+ total score. The precipitous drop in total score
Posttreatment and retention scores were compared per group of 8.04 points for Cort+ during the 1.5 years of retention
using paired t‑test. For Conv, five scores significantly improved indicates a more favorable retention phase for PAOO
196 APOS Trends in Orthodontics | July 2016 | Vol 6 | Issue 4
Ferguson, et al.: Improved retention outcome with PAOO
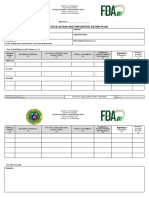
Table 1: Posttreatment and retention score means and standard deviations were computed for each
study group and statistically compared using t‑test
OGS criteria Posttreatment Retention
Conventional Corticotomy P significant Conventional Corticotomy P significant
Mean SD Mean SD Mean SD Mean SD
Alignment 3.32 2.07 2.43 1.62 NS 3.79 3.05 1.71 1.79 0.003
Occlusal contact 3.25 2.05 3.57 2.13 NS 1.96 2.40 1.71 1.80 NS
Marginal ridges 5.86 2.16 5.00 2.06 NS 4.86 2.68 3.25 2.03 0.014
AP relationship 2.75 2.17 2.93 2.80 NS 2.93 3.22 2.21 2.15 NS
Buccolingual inclinations 6.61 2.94 6.64 2.26 NS 6.25 2.95 6.14 1.96 NS
Overjet 2.89 2.33 3.14 2.54 NS 3.36 3.05 2.68 2.25 NS
Interproximal contact 1.07 1.49 0.57 0.92 NS 0.46 1.20 0.11 0.42 NS
Root angulation 4.68 2.64 5.54 3.13 NS 3.50 2.03 3.96 2.58 NS
Total score 30.93 7.33 29.82 7.37 NS 27.21 8.50 21.79 4.95 0.011
Note that no differences were found at posttreatment but retention scores were lower for corticotomy for objective grading system criteria alignment, marginal ridges and
total score. OGS – Objective grading system; SD – Standard deviation; AP – Anteroposterior; NS – not significant (P>0.05)
Table 2: Intra‑group posttreatment and retention score means were compared for each study group
using paired t‑test
OGS criteria Conventional Corticotomy
Posttreatment Retention P significant Posttreatment Retention P significant
(mean) (mean) (mean) (mean)
Alignment 3.32 3.79 NS 2.43 1.71 0.045
Occlusal contact 3.25 1.96 0.004 3.57 1.71 0.000
Marginal ridges 5.86 4.86 0.034 5.00 3.25 0.000
AP relationship 2.75 2.93 NS 2.93 2.21 NS
Buccolingual inclinations 6.61 6.25 NS 6.64 6.14 NS
Overjet 2.89 3.36 NS 3.14 2.68 NS
Interproximal contact 1.07 0.46 0.010 0.57 0.11 0.010
Root angulation 4.68 3.50 0.000 5.54 3.96 0.000
Total score 30.43 27.11 0.005 29.82 21.79 0.000
Note that scores significantly improved for 5 conventional group criteria and 6 corticotomy group criteria. OGS – Objective grading system; AP – Anteroposterior;
NS – not significant (P>0.05)
Table 3: Increment of posttreatment to retention score change for the two groups was compared using
t‑test
OGS criteria Change increment
Conventional (mean) Corticotomy (mean) X different P significant
Alignment −0.46 0.71 1.18 NS
Occlusal contact 1.29 1.86 0.57 NS
Marginal ridges 1.00 1.75 0.75 NS
AP relationship −0.18 0.71 0.89 NS
Buccolingual inclinations 0.36 0.50 0.14 NS
Overjet −0.46 0.46 0.93 NS
Interproximal contact 0.61 0.46 ‑0.14 NS
Root angulation 1.18 1.57 0.39 NS
Total score 3.32 8.04 4.71 0.003
Note that the amount of total score improvement was significantly greater in the corticotomy group. OGS – Objective grading system; AP – Anteroposterior;
NS – not significant (P>0.05)
patients. This evidence strongly suggests that something alignment separately; there was no difference found at
happened following augmented alveolar corticotomy that posttreatment, but alignment of both arches differed
leads to an improved orthodontic outcome at retention. significantly at 1.5 years posttreatment. Alignment scores
at retention were lower (better) for Cort+ than Conv for
To further investigate this notion, the two groups were the maxilla (0.71 vs. 1.96, P = 0.002) and the mandible (1.00
compared for maxillary alignment and mandibular vs. 1.82, P = 0.027). The same was found at posttreatment
APOS Trends in Orthodontics | July 2016 | Vol 6 | Issue 4 197
Ferguson, et al.: Improved retention outcome with PAOO
for marginal ridges as neither maxillary nor mandibular CONCLUSIONS
marginal ridges scores differed (P > 0.05) on the basis
of corticotomy. However, at 1.5 years posttreatment, The purpose of this study was to compare, using the ABO
maxillary marginal ridges score was significantly lower OGS, immediate posttreatment and retention outcomes in
(better) for Cort+ than Conv (1.32 vs. 2.39, P = 0.008) subjects treated with and without corticotomy facilitated
but not mandibular marginal ridges score, i.e., 1.93 versus orthodontic nonextraction therapy. Two samples of Class I
2.46, P > 0.05 (data not shown). crowded malocclusion of 28 each was selected satisfying
given inclusion and exclusion criteria. The OGS criteria
Diminished alveolar bone density (mineralization) at advocated by the American Board of Orthodontics were
posttreatment for Cort+ is a plausible explanation used to evaluate study casts and panoramic radiographs at
facilitating a more favorable retention “settling” phase. posttreatment and 1.5 years posttreatment. Measurements
Alveolar bone turnover with alveolar corticotomy has been were made with a special instrument designed specifically
judged to be 2–3 times greater than without corticotomy,[32] by ABO directors for self‑assessment in preparation
and active orthodontic treatment times average about for the Phase III ABO clinical examination. Study casts
6–8 months.[33] It is anticipated that the alveolar housing and panoramic radiographs had been collected on the
6–8 months following corticotomy is not mineralized to day of appliance removal and at least 1 year following
the same extent and that this lack of mineralization allows de‑bracketing. All subjects had been instructed to wear
greater functional adaptation of the dentition during Hawley type removable retainers in a similar manner. Study
retention. Moreover, the fact that tissues comprising variables were analyzed statistically to identify significant
the periodontium have undergone regional acceleratory differences within and between the two study groups.
phenomena or high turnover after corticotomy[34] suggests
that periodontal tissue memory may have been reduced Parametric statistical testing revealed the following:
or lost. 1. Posttreatment orthodontic outcomes were the same,
with or without corticotomy
Makki [1] reported greater stability of mandibular 2. During retention, 5 of 8 ABO grading criteria improved
irregularity index posttreatment with PAOO citing the for the sample without corticotomy, and 6 of 8 ABO
benefits of augmentation bone grafting as a possible grading criteria improved for the group with corticotomy
contributing factor; other investigators have identified 3. Retention outcome scores were significantly lower
thin alveolar cortices as a risk factor for increased (better) for alignment and marginal ridges in the
postorthodontic mandibular incisor re‑crowding.[35,36] corticotomy‑facilitated group
While the anterior maxillary and mandibular segments 4. The total score was significantly lower (better) in
are taken into account with OGS grading, the primary the corticotomy group at retention. Moreover, the
aim of the ABO postorthodontic treatment evaluation increment of total score change during retention
system is to assess the quality of static orthodontic (effect size) was significantly greater (more improved)
outcome. Subtle posttreatment tooth movements that following corticotomy resulting in significant clinical
lead to improved orthodontic outcomes are quite outcome improvement.
different from lack of tooth movement resulting in
less recrowding. Again, it is entirely conceivable that Based on the conditions of this investigation, orthodontic
the relative state of remineralization in Cort+ was patients facilitated with the alveolar corticotomy and
less than Conv at posttreatment and that the dentition augmentation grafting technique (PAOO) had a more
moved subtly in the direction of improved orthodontic favorable retention course because OGS total score
outcome. improved about 2.4 times more with PAOO than without
during the 1.5 years retention phase.
There were confounding factors associated with the study
that may have influenced results. Although both samples Financial support and sponsorship
were treated with nonextraction orthodontics for Class Nil.
I malocclusion crowding, various aspects of the initial
malocclusion were not matched nor were pretreatment Conflicts of interest
record scores using the ABO Discrepancy Index. There are no conflicts of interest.
Moreover, samples were not matched for age as Cort+
patients averaged mid‑twenties and Conv patients averaged
mid‑teens; it may be argued that younger patients have the REFERENCES
tendency to “relapse” more than older patients, but the
1. Makki L, Ferguson DJ, Wilcko MT, Wilcko WM, Bjerklin K,
10-year mean age difference likely did not play a significant Stapelberg R, et al. Mandibular irregularity index stability following
role in this particular investigation. alveolar corticotomy and grafting: A 10‑year preliminary study.
198 APOS Trends in Orthodontics | July 2016 | Vol 6 | Issue 4
Ferguson, et al.: Improved retention outcome with PAOO
Angle Orthod 2015;85:743‑9. 2015;85:400‑7.
2. Ferguson DJ, Makki L, Wilcko MT, Wilcko WM. Instability of the 21. Detterline DA, Isikbay SC, Brizendine EJ, Kula KS. Clinical outcomes
mandibular dental arch? Look again! Semin Orthod 2016;24. of 0.018‑inch and 0.022‑inch bracket slot using the ABO objective
3. Murphy KG, Wilcko MT, Wilcko WM, Ferguson DJ. Periodontal grading system. Angle Orthod 2010;80:528‑32.
accelerated osteogenic orthodontics: A description of the surgical 22. Farhadian N, Miresmaeili AF, Soltani MK. Comparison of extraction
technique. J Oral Maxillofac Surg 2009;67:2160‑6. and non‑extraction orthodontic treatment using the objective
4. Wilcko MT, Wilcko WM, Pulver JJ, Bissada NF, Bouquot JE. grading system. J Dent Tehran Univ Med Sci 2005;2:91‑5.
Accelerated osteogenic orthodontics technique: A 1‑stage surgically 23. Hsieh TJ, Pinskaya Y, Roberts WE. Assessment of orthodontic
facilitated rapid orthodontic technique with alveolar augmentation. treatment outcomes: Early treatment versus late treatment. Angle
J Oral Maxillofac Surg 2009;67:2149‑59. Orthod 2005;75:162‑70.
5. Andrews LF. The six keys to normal occlusion. Am J Orthod 24. Jain M, Varghese J, Mascarenhas R, Mogra S, Shetty S, Dhakar N.
1972;62:296‑309. Assessment of clinical outcomes of Roth and MBT bracket prescription
6. Daniels C, Richmond S. The development of the index of complexity, using the American Board of Orthodontics objective grading system.
outcome and need (ICON). J Orthod 2000;27:149‑62. Contemp Clin Dent 2013;4:307‑12.
7. Pickering EA, Vig P. The occlusal index used to assess orthodontic 25. Kuncio D, Maganzini A, Shelton C, Freeman K. Invisalign and
treatment. Br J Orthod 1975;2:47‑51. traditional orthodontic treatment postretention outcomes compared
8. Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR index using the American Board of Orthodontics objective grading system.
(peer assessment rating): Methods to determine outcome of Angle Orthod 2007;77:864‑9.
orthodontic treatment in terms of improvement and standards. Eur J 26. Hoybjerg AJ, Currier GF, Kadioglu O. Evaluation of 3 retention
Orthod 1992;14:180‑7. protocols using the American Board of Orthodontics cast
9. Summers CJ. The occlusal index: A system for identifying and and radiograph evaluation. Am J Orthod Dentofacial Orthop
scoring occlusal disorders. Am J Orthod 1971;59:552‑67. 2013;144:16‑22.
10. Casko JS, Vaden JL, Kokich VG, Damone J, James RD, 27. Costalos PA, Sarraf K, Cangialosi TJ, Efstratiadis S. Evaluation of
Cangialosi TJ, et al. Objective grading system for dental casts and the accuracy of digital model analysis for the American Board of
panoramic radiographs. American Board of Orthodontics. Am J Orthodontics objective grading system for dental casts. Am J Orthod
Orthod Dentofacial Orthop 1998;114:589‑99. Dentofacial Orthop 2005;128:624‑9.
11. Greco PM, English JD, Briss BS, Jamieson SA, Kastrop MC, 28. Hildebrand JC, Palomo JM, Palomo L, Sivik M, Hans M. Evaluation
Castelein PT, et al. Posttreatment tooth movement: For better or for of a software program for applying the American Board of
worse. Am J Orthod Dentofacial Orthop 2010;138:552‑8. Orthodontics objective grading system to digital casts. Am J Orthod
12. Lieber WS, Carlson SK, Baumrind S, Poulton DR. Clinical use of the Dentofacial Orthop 2008;133:283‑9.
ABO‑scoring index: Reliability and subtraction frequency. Angle 29. Okunami TR, Kusnoto B, BeGole E, Evans CA, Sadowsky C, Fadavi S.
Orthod 2003;73:556‑64. Assessing the American Board of Orthodontics objective grading
13. Campbell CL, Roberts WE, Hartsfield JK Jr., Qi R. Treatment system: Digital vs plaster dental casts. Am J Orthod Dentofacial
outcomes in a graduate orthodontic clinic for cases defined by the Orthop 2007;131:51‑6.
American Board of Orthodontics malocclusion categories. Am J 30. Song GY, Baumrind S, Zhao ZH, Ding Y, Bai YX, Wang L, et al.
Orthod Dentofacial Orthop 2007;132:822‑9. Validation of the American Board of Orthodontics objective grading
14. Knierim K, Roberts WE, Hartsfield J Jr. Assessing treatment outcomes system for assessing the treatment outcomes of Chinese patients.
for a graduate orthodontics program: Follow‑up study for the classes Am J Orthod Dentofacial Orthop 2013;144:391‑7.
of 2001‑2003. Am J Orthod Dentofacial Orthop 2006;130:648‑55, e1‑3. 31. Ferguson DJ, Makki L, Stapelberg R, Wilcko MT, Wilcko WM.
15. Pinskaya YB, Hsieh TJ, Roberts WE, Hartsfield JK. Comprehensive Stability of the mandibular dental arch following periodontally
clinical evaluation as an outcome assessment for a graduate accelerated osteogenic orthodontics therapy: Preliminary studies.
orthodontics program. Am J Orthod Dentofacial Orthop Semin Orthod 2014;20:239‑46.
2004;126:533‑43. 32. Sebaoun JD, Kantarci A, Turner JW, Carvalho RS, Van Dyke TE,
16. Yang‑Powers LC, Sadowsky C, Rosenstein S, BeGole EA. Treatment Ferguson DJ. Modeling of trabecular bone and lamina DURA
outcome in a graduate orthodontic clinic using the American Board following selective alveolar decortication in rats. J Periodontol
of Orthodontics grading system. Am J Orthod Dentofacial Orthop 2008;79:1679‑88.
2002;122:451‑5. 33. Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics
17. Cook DR, Harris EF, Vaden JL. Comparison of university and with alveolar reshaping: Two case reports of decrowding. Int J
private‑practice orthodontic treatment outcomes with the American Periodontics Restorative Dent 2001;21:9‑19.
Board of Orthodontics objective grading system. Am J Orthod 34. Verna C. Regional acceleratory phenomena. In: Kantarci A, Will L,
Dentofacial Orthop 2005;127:707‑12. Yen S, editors. Tooth Movement Frontiers of Oral Biology. Vol. 18.
18. Anthopoulou C, Konstantonis D, Makou M. Treatment outcomes Basel: Karger; 2016. p. 28‑35.
after extraction and nonextraction treatment evaluated with the 35. Chaison JB, Chen CS, Herring SW, Bollen AM. Bone volume, tooth
American Board of Orthodontics objective grading system. Am J volume, and incisor relapse: A 3‑dimensional analysis of orthodontic
Orthod Dentofacial Orthop 2014;146:717‑23. stability. Am J Orthod Dentofacial Orthop 2010;138:778‑86.
19. Chaison ET, Liu X, Tuncay OC. The quality of treatment in the adult 36. Rothe LE, Bollen AM, Little RM, Herring SW, Chaison JB, Chen CS,
orthodontic patient as judged by orthodontists and measured by et al. Trabecular and cortical bone as risk factors for orthodontic
the Objective Grading System. Am J Orthod Dentofacial Orthop relapse. Am J Orthod Dentofacial Orthop 2006;130:476‑84.
2011;139 4 Suppl: S69‑75. 37. Akinci Cansunar H, Uysal T. Comparison of orthodontic treatment
20. Deguchi T, Terao F, Aonuma T, Kataoka T, Sugawara Y, Yamashiro T, outcomes in nonextraction, 2 maxillary premolar extraction,
et al. Outcome assessment of lingual and labial appliances compared and 4 premolar extraction protocols with the American Board of
with cephalometric analysis, peer assessment rating, and objective Orthodontics objective grading system. Am J Orthod Dentofacial
grading system in angle class II extraction cases. Angle Ortho Orthop 2014;145:595‑602.
APOS Trends in Orthodontics | July 2016 | Vol 6 | Issue 4 199
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Investigation of TMDDocument36 pagesInvestigation of TMDzaidNo ratings yet
- Jva 1Document8 pagesJva 1zaidNo ratings yet
- CBCT of TMDDocument13 pagesCBCT of TMDzaidNo ratings yet
- Corticotomia Indicacion y Efectos PDFDocument14 pagesCorticotomia Indicacion y Efectos PDFNivram Olimac Onaelag ArrapNo ratings yet
- Bracket PlacementDocument102 pagesBracket PlacementzaidNo ratings yet
- Effect of Two Corticotomy Protocols On Periodontal Tissue and Orthodontic MovementDocument10 pagesEffect of Two Corticotomy Protocols On Periodontal Tissue and Orthodontic MovementzaidNo ratings yet
- Maxillary Changes With Bone-Borne Surgically Assisted Rapid Palatal Expansion: A Prospective StudyDocument10 pagesMaxillary Changes With Bone-Borne Surgically Assisted Rapid Palatal Expansion: A Prospective StudyzaidNo ratings yet
- Evolution of Occlusion and TemporomandibularDocument8 pagesEvolution of Occlusion and TemporomandibularAnonymous xKZMORNo ratings yet
- Analysis of The Influences of Bracket and Force System in Different Directions On The Moment To Force Ratio by Finite Element MethodDocument8 pagesAnalysis of The Influences of Bracket and Force System in Different Directions On The Moment To Force Ratio by Finite Element MethodzaidNo ratings yet
- Mini implantappliedprotocoltoMARPEDocument11 pagesMini implantappliedprotocoltoMARPEzaidNo ratings yet
- Davidovitch1995 PDFDocument6 pagesDavidovitch1995 PDFRahulLife'sNo ratings yet
- Expansion of Dog With CorticotomiesDocument14 pagesExpansion of Dog With CorticotomieszaidNo ratings yet
- Analysis of The Influences of Bracket and Force System in Different Directions On The Moment To Force Ratio by Finite Element MethodDocument8 pagesAnalysis of The Influences of Bracket and Force System in Different Directions On The Moment To Force Ratio by Finite Element MethodzaidNo ratings yet
- Won Moon: An Interview WithDocument17 pagesWon Moon: An Interview WithzaidNo ratings yet
- Moment To Force Ratio Center of Rotation and ForceDocument6 pagesMoment To Force Ratio Center of Rotation and ForcezaidNo ratings yet
- Davidovitch1995 PDFDocument6 pagesDavidovitch1995 PDFRahulLife'sNo ratings yet
- PIIS0889540614011548Document8 pagesPIIS0889540614011548zaidNo ratings yet
- Animal and Bird Trade and Hunting in Iraq: Key Biodiversity Areas Project ReportDocument45 pagesAnimal and Bird Trade and Hunting in Iraq: Key Biodiversity Areas Project ReportzaidNo ratings yet
- Skeletal and Dentoalveolar Changes After Miniscrew-Assisted Rapid Palatal Expansion in Young Adults: A Cone-Beam Computed Tomography StudyDocument10 pagesSkeletal and Dentoalveolar Changes After Miniscrew-Assisted Rapid Palatal Expansion in Young Adults: A Cone-Beam Computed Tomography StudyzaidNo ratings yet
- Dental Research Journal: The Effect of Buccal Corticotomy On Accelerating Orthodontic Tooth Movement of Maxillary CanineDocument6 pagesDental Research Journal: The Effect of Buccal Corticotomy On Accelerating Orthodontic Tooth Movement of Maxillary CaninezaidNo ratings yet
- Lingual Orthodontics: Patient Selection and Diagnostic ConsiderationsDocument7 pagesLingual Orthodontics: Patient Selection and Diagnostic ConsiderationszaidNo ratings yet
- 0-Menufacturing and SlotsDocument6 pages0-Menufacturing and SlotszaidNo ratings yet
- Digant Expansion Work FlowDocument5 pagesDigant Expansion Work FlowzaidNo ratings yet
- Head & Face Medicine: Comparative Analysis of Slot Dimension in Lingual Bracket SystemsDocument5 pagesHead & Face Medicine: Comparative Analysis of Slot Dimension in Lingual Bracket SystemszaidNo ratings yet
- Relation Ship Between Tooth Size and Arch DimensionDocument5 pagesRelation Ship Between Tooth Size and Arch DimensionzaidNo ratings yet
- 15 Mixing Medications Using One SyringeDocument2 pages15 Mixing Medications Using One SyringeMarky RoqueNo ratings yet
- Case Study of Placenta PreviaDocument23 pagesCase Study of Placenta PreviaPreeti ChouhanNo ratings yet
- Modelo Baja VisionDocument24 pagesModelo Baja VisioneveNo ratings yet
- Novel Tools and Resources For Evidence-Based Practice in PsychologyDocument10 pagesNovel Tools and Resources For Evidence-Based Practice in PsychologyAndrea Despistes HerreraNo ratings yet
- NUR 320 Fall 2016Document18 pagesNUR 320 Fall 2016Kelechi KaluNo ratings yet
- Directory of Records Index of Personal Information Banks: Administration and Governance 3Document25 pagesDirectory of Records Index of Personal Information Banks: Administration and Governance 3takoda johnstone0% (1)
- Outcomes-based Teaching Learning Plan (OBTL Plan) for Pharmacy Dispensing CourseDocument11 pagesOutcomes-based Teaching Learning Plan (OBTL Plan) for Pharmacy Dispensing CourseJaden GonzagaNo ratings yet
- AV Comment Letter On 2024 MA Advance Notice FINALDocument5 pagesAV Comment Letter On 2024 MA Advance Notice FINALArnold VenturesNo ratings yet
- Susi - Professional Development Power PointDocument10 pagesSusi - Professional Development Power Pointapi-549370844No ratings yet
- Oumme Rushaa Sairally FINAL5PAGEDocument6 pagesOumme Rushaa Sairally FINAL5PAGERushaa SairallyNo ratings yet
- Astigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedDocument12 pagesAstigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedLynden BulanNo ratings yet
- Techniques in Hip Arthroscopy and Joint Preservation SurgeryDocument354 pagesTechniques in Hip Arthroscopy and Joint Preservation SurgeryNoel Alonso Calleros HernandezNo ratings yet
- Cholecystectomy Nursing Care Plan: Risk For InfectionDocument1 pageCholecystectomy Nursing Care Plan: Risk For InfectionBesael BaccolNo ratings yet
- Interview QuestionsDocument7 pagesInterview QuestionsRitesh KumarNo ratings yet
- Exploring Solar Energy Integration in Ugandan Health Centers Evaluating The Implementation of Heliophotovoltaic Solutions For Rural HealthcareDocument10 pagesExploring Solar Energy Integration in Ugandan Health Centers Evaluating The Implementation of Heliophotovoltaic Solutions For Rural HealthcareKIU PUBLICATION AND EXTENSIONNo ratings yet
- Diagnosing and Treating Restricted Mandibular OpeningDocument8 pagesDiagnosing and Treating Restricted Mandibular OpeningAmar BhochhibhoyaNo ratings yet
- Class 7 Social ScienceDocument29 pagesClass 7 Social Sciencesanjay kumar SinghNo ratings yet
- Family Health AssessmentDocument12 pagesFamily Health Assessmentlorelie asisNo ratings yet
- A. B. C. D.: Final CoachingDocument7 pagesA. B. C. D.: Final CoachingRona PieNo ratings yet
- Physical Facilities Designand ManagementDocument14 pagesPhysical Facilities Designand ManagementMAHIR MODYNo ratings yet
- Reaction On The The Philippine Health Agenda 2016Document5 pagesReaction On The The Philippine Health Agenda 2016Jesselle Iquin100% (3)
- Case Study - Business OperationsDocument2 pagesCase Study - Business OperationsSubhajit DeNo ratings yet
- IM EAMC ENDORSEMENT (Updated Feb 2020)Document7 pagesIM EAMC ENDORSEMENT (Updated Feb 2020)Joshua Elijah ArsenioNo ratings yet
- Pregnancy After Kidney Transplantation: Lisa A. Coscia, Dawn Armenti, Serban Constantinescu, and Michael J. MoritzDocument18 pagesPregnancy After Kidney Transplantation: Lisa A. Coscia, Dawn Armenti, Serban Constantinescu, and Michael J. MoritzHuththa pekkdNo ratings yet
- Certificate of Community Service: Mary Ann Janeth AmboDocument46 pagesCertificate of Community Service: Mary Ann Janeth Amboucnursingcesdev2008No ratings yet
- 5a3af95ff1046 Resource Managment Curriculum SternDocument20 pages5a3af95ff1046 Resource Managment Curriculum SternDavid SternNo ratings yet
- DigitDocument180 pagesDigitSapna JhaNo ratings yet
- Latest Resume BuelaDocument3 pagesLatest Resume BuelaCleeve Humprey BuelaNo ratings yet
- 9 - Postterm PregnancyDocument22 pages9 - Postterm PregnancyMara Medina - BorleoNo ratings yet
- Capa 2018Document3 pagesCapa 2018Lexi MontanteNo ratings yet