Professional Documents
Culture Documents
Diagnostic Gold Standard of RPOC With Accreta
Uploaded by
Ayu Dyah PrimaningrumOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnostic Gold Standard of RPOC With Accreta
Uploaded by
Ayu Dyah PrimaningrumCopyright:
Available Formats
Diagnostic Gold Standard of RPOC with Accreta
Jauniaux, E., Ayres-de-Campos, D., Langhoff-Roos, J., Fox, K. A., & Collins, S. (2019). FIGO
classification for the clinical diagnosis of placenta accreta spectrum disorders,. International Journal
of Gynecology & Obstetrics, 146(1), 20–24. doi:10.1002/ijgo.12761
Histopathology is considered as the gold standard modality recommended to confirm
clinical diagnosis of PAS, but it is often unavailable in adherent
accreta or conservatively managed cases.
Jauniaux, E., Chantraine, F., Silver, R. M., & Langhoff-Roos, J. (2018). FIGO consensus guidelines on
placenta accreta spectrum disorders: Epidemiology,. International Journal of Gynecology &
Obstetrics, 140(3), 265–273. doi:10.1002/ijgo.12407
The use of standardized protocol and terminology for both the clinical diagnosis and
histopathological confirmation of PAS disorders is essential to obtaining new and more accurate
epidemiological data is recommended by FIGO (2018).
Jauniaux, E., Hussein, A. M., Fox, K. A., & Collins, S. L. (2019). New evidence-based diagnostic and
management strategies for placenta accreta spectrum disorders. Best Practice & Research Clinical
Obstetrics & Gynaecology. doi:10.1016/j.bpobgyn.2019.04.006
The main histopathological criterion used in recent clinical cohorts to confirm the diagnosis
of PAS is the absence of decidual/Nitabuch layer the between the tip of anchoring villi and
superficial myometrium.
Histopathologic diagnosis of PAS, however, can be very difficult if the surgeon has attempted
to remove the placenta, or impossible in cases of conservative management where the
whole placenta is left in situ. Therefore, collaboration between the surgical team and
pathologists to guide the sampling of the hysterectomy specimen is paramount to obtain
accurate grading and extent of the villous invasion.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Spontaneous Preterm Birth - Pathogenesis - UpToDateDocument20 pagesSpontaneous Preterm Birth - Pathogenesis - UpToDateAyu Dyah PrimaningrumNo ratings yet
- Progesterone Supplementation To Reduce The Risk of Spontaneous Preterm Labor and Birth - UpToDateDocument24 pagesProgesterone Supplementation To Reduce The Risk of Spontaneous Preterm Labor and Birth - UpToDateAyu Dyah PrimaningrumNo ratings yet
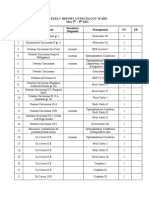
- Weekly RK 3-8 May 2021 Edit 1Document2 pagesWeekly RK 3-8 May 2021 Edit 1Ayu Dyah PrimaningrumNo ratings yet
- Template New Report Akreta Update EropaDocument1 pageTemplate New Report Akreta Update EropaAyu Dyah PrimaningrumNo ratings yet
- Incidence and Mortality of The Preterm Infant - UpToDateDocument29 pagesIncidence and Mortality of The Preterm Infant - UpToDateAyu Dyah PrimaningrumNo ratings yet
- Contoh Mentahan Weekly WordDocument11 pagesContoh Mentahan Weekly WordAyu Dyah PrimaningrumNo ratings yet
- Constipation in PregnancyDocument32 pagesConstipation in PregnancyAyu Dyah PrimaningrumNo ratings yet
- AUB M Ec Hiperplasia Endometrium - Id.enDocument2 pagesAUB M Ec Hiperplasia Endometrium - Id.enAyu Dyah PrimaningrumNo ratings yet
- Beta HCG in RPOCDocument1 pageBeta HCG in RPOCAyu Dyah PrimaningrumNo ratings yet
- "Nausicaa" Compression SutureDocument14 pages"Nausicaa" Compression SutureAyu Dyah PrimaningrumNo ratings yet
- RPOC Treatment Surgery Vs MTXDocument2 pagesRPOC Treatment Surgery Vs MTXAyu Dyah PrimaningrumNo ratings yet