Professional Documents
Culture Documents
Retest Positive For SARS CoV 2 RNA
Retest Positive For SARS CoV 2 RNA
Uploaded by
shofidhiaaaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Retest Positive For SARS CoV 2 RNA
Retest Positive For SARS CoV 2 RNA
Uploaded by
shofidhiaaaCopyright:
Available Formats
DOI: 10.1002/jmv.
26114
COMMENTARY
Retest positive for SARS‐CoV‐2 RNA of “recovered” patients
with COVID‐19: Persistence, sampling issues, or re‐infection?
Hanyujie Kang1 | Yishan Wang1 | Zhaohui Tong1 | Xuefeng Liu2
1
Department of Respiratory and Critical Care Medicine, Beijing Institute of Respiratory Medicine, Beijing Chao‐Yang Hospital, Capital Medical University,
Beijing, China
2
Departments of Pathology and Oncology, Lombardi Comprehensive Cancer Center, Georgetown University Medical Center, Washington, District of Columbia
Correspondence
Zhaohui Tong, Department of Respiratory and Abstract
Critical Care Medicine, Beijing Institute of
Respiratory Medicine, Beijing Chao‐Yang “Retest Positive” for severe acute respiratory syndrome‐related coronavirus‐2
Hospital, Capital Medical University, 100020 (SARS‐CoV‐2) from “recovered” coronavirus disease‐19 (COVID‐19) has been re-
Beijing, China.
Email: tongzhaohuicy@sina.com ported and raised several important questions for this novel coronavirus and
Xuefeng Liu, Departments of Pathology and COVID‐19 disease. In this commentary, we discussed several questions: (a) Can
Oncology, Lombardi Comprehensive Cancer
SARS‐CoV‐2 re‐infect the individuals who recovered from COVID‐19? This question
Center, Georgetown University Medical
Center, Washington DC 20057. is also associated with other questions: whether or not SARS‐CoV‐2 infection in-
Email: xuefeng.liu@georgetown.edu
duces protective reaction or neutralized antibody? Will SARS‐CoV‐2 vaccines work?
(b) Why could some recovered patients with COVID‐19 be re‐tested positive for
SARS‐CoV‐2 RNA? (c) Are some recovered pwith atients COVID‐19 with re‐testing
positive for SARS‐CoV‐2 RNA infectious? and (d) How should the COVID‐19 pa-
tients with retest positive for SARS‐CoV‐2 be managed?
KEYWORDS
coronavirus < virus classification, disease control, immunity/immunization < epidemiology,
persistent infection < infection, SARS coronavirus < virus classification
In December 2019, coronavirus disease 2019 (COVID‐19) caused by However, the recovered (discharged) COVID‐19 patients with retest
severe acute respiratory syndrome‐related coronavirus‐2 (SARS‐ positive for SARS‐CoV‐2 RNA have recently been reported.1‐9 Spe-
CoV‐2) infection emerged in Wuhan, China, and has spread rapidly cifically, A new report on 25 February 2020 indicated that 14% of
worldwide. There are more than 4.7 million confirmed cases and discharged patients were tested positive for SARS‐CoV‐2 RNA in
more than 313 thousand confirmed death in 216 countries by Guangdong province. On 2 February 2020, a woman patient with
16th May 2020. Many countries take very different strategies to COVID‐19 became positive for SARS‐CoV‐2 RNA again during her
control this outbreak including asymptomatic, mild and sever pa- quarantine after hospital discharge because of two consecutively
tients. In China, strict quarantine is needed for all the confirmed negative results on 28 and 30 January, respectively.7 A study from
cases. All patients with COVID‐19 need to meet criteria of recovery Zhongnan Hospital of Wuhan University suggested that four COVID‐
before hospital discharge1: (a) normal temperature for more than 19 patients who met criteria for hospital discharge became positive
3 days, (b) no respiratory symptoms, (c) substantially improved acute for SARS‐CoV‐2 RNA after 5 to 13 days of discharge.1 A single center
exudative lesions on chest computed tomography images, (d) two study reported 38 out of 262 of recovered patients with COVID‐19
consecutively reverse transcription‐polymerase chain reaction (14.5%) became positive for SARS‐CoV‐2 RNA by 10 March 2020,
(RT‐PCR) tests negative for SARS‐CoV‐2 RNA more than 24 hours. during 14 days of further quarantine or isolation.8 A cohort study of
Hanyujie Kang and Yishan Wang contributed equally to this work.
J Med Virol. 2020;1–3. wileyonlinelibrary.com/journal/jmv © 2020 Wiley Periodicals LLC | 1
2 | COMMENTARY
414 confirmed patients with COVID‐19 in a hospital from 11 Jan- restrictive quarantine and follow‐up strategies for all patients with
uary to 23 April 2020 also suggested that 16.7% COVID‐19 patients COVID‐19, suspected cases, and asymptomatic individuals. In the
re‐tested positive for SARS‐CoV‐2 RNA one to three times after 13 discharged patients with retest positive for viral RNA in Guang-
discharge, during 14 days of strict quarantine.9 Another single center dong province on 25 March 2020, follow‐up results demonstrated no
study reported that 8 out of 108 confirmed patients with COVID‐19 new infected cases from 104 close contacts to the original patients.
from 10 February to 13 April 2020 became SARS‐CoV‐2 positive and There was no single family member being infected by the four re-
were re‐admitted in hospital. This “Retest Positive” for SARS‐CoV‐2
6
covered COVID‐19 patients with retest positive for SARS‐CoV‐2
from the discharged COVID‐19 has attracted extra attention and RNA, who were discharged from Zhongnan Hospital of Wuhan Uni-
triggered numerous discussions. In this commentary, we discuss the versity,1 suggesting a relative low or no infectivity of those recovered
following questions: (a) Can SARS‐CoV‐2 re‐infect the individuals patients with retest positive for viral RNA. Researchers in Hong Kong
who recovered from COVID‐19? This question is also associated with have followed up more than 10 recovered, discharged COVID‐19
other questions: whether or not SARS‐CoV‐2 infection induces pro- patients with retest positive for SARS‐CoV‐2 and failed to isolate
tective reaction or neutralized antibody? Will SARS‐CoV‐2 vaccines SARS‐CoV‐2 virus by cell culture in the P3 laboratory due to low viral
work? (b) Why could some recovered patients with COVID‐19 be re‐ loads or no live viruses from the samples. A recent study13 suggested
tested positive for SARS‐CoV‐2 RNA? (c) Are some recovered that the SARS‐CoV‐2 can replicate actively in upper respiratory tract
COVID‐19 patients with re‐testing positive for SARS‐CoV‐2 RNA tissues in the early stage with high infectivity. In the later stage, the
infectious? (d)How should the COVID‐19 patients with retest posi- viral load was relative low in upper respiratory tract.
tive for SARS‐CoV‐2 be managed?
3 | RE ‐IN F E C T I O N W I T H S A RS‐C oV ‐2?
1 | WHY DID SOME RECOVERED COVID‐19
PATIENTS BECOME RETEST POSITIVE FOR Host immune response to pathogens may prevent progression to
SARS‐CoV‐2 RNA? severe illness or reinfection by the same pathogens. Many studies
have shown that recovered patients with COVID‐19 have antibodies
There are several possibilities why the recovered patients with to SASR‐CoV‐2,14‐17 some patients have very low levels of neu-
COVID‐19 became retest positive for SARS‐CoV‐2 RNA: First, tralizing antibodies. These raised possibilities for possible reinfection
two consecutively RT‐PCR tests of pharyngeal swabs might be false‐ of SARS‐CoV‐2 and antibody dependent enhancement.18‐20 As we
negative before the patient was discharged from the hospital, since discussed above, the discharged patients with COVID‐19 in China
overall positivity of RT‐PCR for SARS‐CoV‐2 in COVID‐19 was and elsewhere were re‐testing positive for SARS‐CoV‐2 RNA. It re-
round 30% to 40%.10 The sampling procedures of pharyngeal swabs, mains unclear whether the convalescing patients have risks for an
quality of sampling tube, sample storage temperature and time, “reinfection.” A recent animal study18 may help understanding this
transportation process of samples, and quality of detection reagents situation. They used the SARS‐CoV‐2‐infected monkeys for this
(kits) might result in the false‐negative tests. Second, some COVID‐ study. They found that viral replication in nose, pharynx, lung and gut,
19 patients did not completely meet the discharge criteria. The moderate interstitial pneumonia at 7 days postinfection. After the
interval time between the viral RNA tests before discharge and the symptoms were alleviated and the specific antibody tested positively,
actual discharge date went too long, and viral test was not repeated they rechallenged half of infected monkeys with the same dose of
right before discharge according to the requirements of the SARS‐CoV‐2 strain. They did not observe viral loads in nasophar-
guideline of diagnosis and treatment. Third, positive signal of viral yngeal and anal swabs and viral replication in all primary tissues at
RNA might be from the “dead” viruses or viral gene fragments 5 days post‐reinfection. Thus, SARS‐CoV‐2 infection may protect
without active viral replications. Finally, viral clearance might be from subsequent re‐exposures.18 Previous study showed that
varied from the patient to patient with pre‐existing conditions. For immunoglobulin G (IgG) antibody peaked at month 4 after the onset
example, 48% COVID‐19 patients had a comorbidity (such as hy- of SARS, IgG antibodies persisted for 16 months in all patients. In
pertension, diabetes, etc), 44.9% patients received glucocorticoid patients with COVID‐19, antibodies were also detected in patients'
therapy, and most COVID‐19 patients with critical conditions were blood after being infected by SARS‐CoV‐2, the immunity lasted for at
11,12
older than 50 years and above. All these might delay virus least 7 days following remission of symptoms.21 SARS‐CoV‐2‐specific
clearance. neutralizing antibodies were detected in patients from day 10 to
15 after the onset of the disease and remained thereafter. The titers
of these antibodies among these patients correlated with the
2 | ARE THE PATIE NTS WITH RETE ST spike‐binding antibodies targeting S1, receptor‐binding domain, and
POSITIVE FOR S ARS ‐Co V‐2 I NF ECTI O U S? S2 regions, although antibody titers were variable in different
patients.16 Therefore, it is needed for further studies in animal
Theoretically, COVID‐19 patients with active viral replication are and human for long time follow‐up to rule out the possibility for
infectious. As most already know, China has a very powerful and re‐infection of SARS‐CoV‐2.
COMMENTARY | 3
4 | MANAGEMENT 10. Wang Y, Kang H, Liu X, Tong Z. Combination of RT‐qPCR testing and
clinical features for diagnosis of COVID‐19 facilitates management of
SARS‐CoV‐2 outbreak. J Med Virol. 2020;92:538‐539.
First, the discharge criteria in Novel Coronavirus Pneumonia Diagnosis
11. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality
and Treatment Protocol (7th edition, trial) (http://www.nhc.gov.cn/ of adult inpatients with COVID‐19 in Wuhan, China: a retrospective
yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml.) cohort study. Lancet. 2020;395:1054‐1062.
must be strictly followed. Patients with COVID‐19 (who received 12. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized
patients with 2019 novel coronavirus‐infected pneumonia in Wuhan,
glucocorticoid therapy, had comorbidities, were older than 65) may
China. JAMA. 2020;323:1061.
extend the length of hospital stay because of the prolonged clearance 13. Woelfel R, Corman VM, Guggemos W, et al. Clinical presentation and
of viruses. These discharged patients with COVID‐19 also should be virological assessment of hospitalized cases of coronavirus disease
under quarantine management and health monitoring for 14 days as 2019 in a travel‐associated transmission cluster. medRxiv. 2020. 2020.
2003.2005.20030502.
described in the seventh edition of guidance, instead of “self‐
14. Tian X, Li C, Huang A, et al. Potent binding of 2019 novel coronavirus
monitoring for 14 days” described in previous editions of the Gui- spike protein by a SARS coronavirus‐specific human monoclonal an-
dance. Finally, combination of serology tests for immunoglobulin M tibody. Emerg Microbes Infect. 2020;9:382‐385.
and IgG and viral RNA might be also helpful for surveillance and de- 15. To KK, Tsang OT, Leung WS, et al. Temporal profiles of viral load in
cision making for discharge of patients with COVID‐19.17,22 posterior oropharyngeal saliva samples and serum antibody re-
sponses during infection by SARS‐CoV‐2: an observational cohort
study. Lancet Infect Dis. 2020;20:565‐574.
OR CID 16. Wu F, Wang A, Liu M, et al. Neutralizing antibody responses to SARS‐
Xuefeng Liu http://orcid.org/0000-0002-9922-9627 CoV‐2 in a COVID‐19 recovered patient cohort and their implica-
tions. medRxiv. 2020. 2020.2003.2030.20047365.
17. Zhao J, Yuan Q, Wang H, et al. Antibody responses to SARS‐CoV‐2 in
REFERENC ES
patients of novel coronavirus disease 2019. Clin Infect Dis. 2020.
1. Lan L, Xu D, Ye G, et al. Positive RT‐PCR test results in patients 18. Bao L, Deng W, Gao H, et al. Reinfection could not occur in SARS‐
recovered from COVID‐19. JAMA. 2020. CoV‐2 infected rhesus macaques. bioRxiv. 2020. 2020.2003.2013.
2. Ling Y, Xu SB, Lin YX, et al. Persistence and clearance of viral RNA in 990226.
2019 novel coronavirus disease rehabilitation patients. Chin Med 19. Peron JPS, Nakaya H. Susceptibility of the elderly to SARS‐CoV‐2
J (Engl). 2020;133:1039‐1043. infection: ACE‐2 overexpression, shedding, and antibody‐dependent
3. Qu YM, Kang EM, Cong HY. Positive result of Sars‐Cov‐2 in sputum from enhancement (ADE). Clinics. 2020;75:e1912.
a cured patient with COVID‐19. Travel Med Infect Dis. 2020;34:101619. 20. Fu Y, Cheng Y, Wu Y. Understanding SARS‐CoV‐2‐mediated in-
4. Kipkorir V, Cheruiyot I, Ngure B, Misiani M, Munguti J. Prolonged flammatory responses: from mechanisms to potential therapeutic
SARS‐Cov‐2 RNA detection in anal/rectal swabs and stool specimens tools. Virol Sin. 2020.
in COVID‐19 patients after negative conversion in nasopharyngeal 21. Thevarajan I, Nguyen THO, Koutsakos M, et al. Breadth of con-
RT‐PCR Test. J Med Virol. 2020. comitant immune responses prior to patient recovery: a case report
5. Fu W, Chen Q, Wang T. Letter to the Editor: three cases of re‐ of non‐severe COVID‐19. Nat Med. 2020;26:453‐455.
detectable positive SARS‐CoV‐2 RNA in recovered COVID‐19 pa- 22. Xia, G NW, Gong W. Serological test is an efficient supplement for
tients with antibodies. J Med Virol. 2020. detecting RNA to confirm SARS‐CoV‐2 infection. Preprints. 2020;
6. Cao H, Ruan L, Liu J, Liao W. The clinical characteristic of eight pa- 2020. 2020030184.
tients of COVID‐19 with positive RT‐PCR test after discharge. J Med
Virol. 2020:jmv.26017.
7. Chen D, Xu W, Lei Z, et al. Recurrence of positive SARS‐CoV‐2 RNA in
COVID‐19: a case report. Int J Infect Dis. 2020;93:297‐299.
How to cite this article: Kang H, Wang Y, Tong Z, Liu X.
8. An J, Liao X, Xiao T, et al. Clinical characteristics of the recovered
COVID‐19 patients with re‐detectable positive RNA test. medRxiv. Retest positive for SARS‐CoV‐2 RNA of “recovered” patients
2020. 2020.2003.2026.20044222. with COVID‐19: Persistence, sampling issues, or re‐infection?
9. Huang J, Zheng L, Li Z, et al. Recurrence of SARS‐CoV‐2 PCR posi- J Med Virol. 2020;1–3. https://doi.org/10.1002/jmv.26114
tivity in COVID‐19 patients: a single center experience and potential
implications. medRxiv. 2020. 2020.2005.2006.20089573.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lesson Plan - HPVDocument6 pagesLesson Plan - HPVMonique MavronicolasNo ratings yet
- College of Our Lady of Mt. Carmel (Pampanga) : Course SyllabusDocument4 pagesCollege of Our Lady of Mt. Carmel (Pampanga) : Course Syllabus;'SiLeNt';No ratings yet
- Newly Diagnosed HIV Cases in The Philippines: National Epidemiology CenterDocument4 pagesNewly Diagnosed HIV Cases in The Philippines: National Epidemiology CenterDeden DavidNo ratings yet
- Immunization ChartDocument1 pageImmunization ChartDesilva ThampiNo ratings yet
- Journal of Obstetrics and Gynaecology Canada (JOGC) PDFDocument7 pagesJournal of Obstetrics and Gynaecology Canada (JOGC) PDFgilirNo ratings yet
- An Analysis of Taiwan's Vaccination Services and Applications For Vaccine Injury CompensationsDocument15 pagesAn Analysis of Taiwan's Vaccination Services and Applications For Vaccine Injury CompensationsAnonymous FNZ3uR2AHsNo ratings yet
- Gavrila Catalin 1Document1 pageGavrila Catalin 1Doina RusuNo ratings yet
- K.N.ravichitra, Et AlDocument5 pagesK.N.ravichitra, Et AldindaNo ratings yet
- Bacteriology Ii MCQ:: Prepared By: Srey Viso, Pharmd Medical Biologist & Microbiology, DMM For Pharmacy ClassDocument21 pagesBacteriology Ii MCQ:: Prepared By: Srey Viso, Pharmd Medical Biologist & Microbiology, DMM For Pharmacy ClassPiseth VichhekaNo ratings yet
- Antiviral Therapy PDFDocument438 pagesAntiviral Therapy PDFYOUCEF DHIA ELHAK KOUAOUCINo ratings yet
- Daftar Pustaka Fix GbsDocument2 pagesDaftar Pustaka Fix GbsElizabeth IvanaNo ratings yet
- Zoonoses: Drs. Foster & Smith Educational StaffDocument7 pagesZoonoses: Drs. Foster & Smith Educational StaffTINALEETNT723No ratings yet
- 21-05-2020 05-00 EnglishDocument13 pages21-05-2020 05-00 EnglishRohithNo ratings yet
- VIKKI13Document6 pagesVIKKI13Dillisrinivasarao NNo ratings yet
- Objectives 3Document4 pagesObjectives 3sibugan300No ratings yet
- IMSLP664696-PMLP1066603-The Dilemma All Clarinet Version-Score and PartsDocument12 pagesIMSLP664696-PMLP1066603-The Dilemma All Clarinet Version-Score and PartsJoseph RouquetteNo ratings yet
- Leptospirosis by DR SarmaDocument37 pagesLeptospirosis by DR SarmaTias Diah0% (1)
- Alterations With Infectious Inflammatory and Immunologic ResponseDocument15 pagesAlterations With Infectious Inflammatory and Immunologic Responselaurie.charlynjaneNo ratings yet
- VIRUSESDocument7 pagesVIRUSESJitesh SoniNo ratings yet
- The Correlation Between Basic Immunizations Knowledge and Mothers' Attitude at Basic Immunizations Provision in The House of Vaccination KebagusanDocument1 pageThe Correlation Between Basic Immunizations Knowledge and Mothers' Attitude at Basic Immunizations Provision in The House of Vaccination KebagusanMuhammad Agung WNo ratings yet
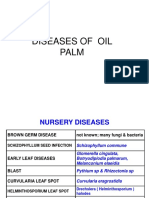
- Diseases of Oil Palm Pictures PpsDocument42 pagesDiseases of Oil Palm Pictures Ppsgafrnce60No ratings yet
- Cutaneous Leishmaniasis: Mark S. Bailey, MRCP, Diana N.J. Lockwood, BSC, MD, FRCPDocument9 pagesCutaneous Leishmaniasis: Mark S. Bailey, MRCP, Diana N.J. Lockwood, BSC, MD, FRCPeva yustianaNo ratings yet
- On The Day of Big Annual SaleDocument7 pagesOn The Day of Big Annual SaleSutin SirisaoNo ratings yet
- Microbial Diseases of The Cardiovascular and Lymphatic SystemsDocument27 pagesMicrobial Diseases of The Cardiovascular and Lymphatic SystemsAbhishek Isaac MathewNo ratings yet
- CarbunclesDocument15 pagesCarbunclesMr DanielNo ratings yet
- Mukesh Kumar,: Municipal CommissionerDocument6 pagesMukesh Kumar,: Municipal CommissionerSSNo ratings yet
- Lymphatic Filariasis SummaryDocument6 pagesLymphatic Filariasis Summaryapi-252809746No ratings yet
- Laboratory Report:: Shaynad Ambalathveettil SharafudheenDocument1 pageLaboratory Report:: Shaynad Ambalathveettil Sharafudheenshaynad binsharafNo ratings yet
- AnaplasmaDocument22 pagesAnaplasmaSomesh SharmaNo ratings yet
- National Immunisation ProgrammeDocument2 pagesNational Immunisation ProgrammeAnonymous whcvnPBeQNo ratings yet