Professional Documents
Culture Documents
Cardiopulmonary - Resuscitation - in - Prone - Position - A
Uploaded by
DwitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiopulmonary - Resuscitation - in - Prone - Position - A
Uploaded by
DwitaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/6949562
Cardiopulmonary Resuscitation in Prone Position: A Simplified Method for
Outpatients
Article in Journal of the Chinese Medical Association · June 2006
DOI: 10.1016/S1726-4901(09)70219-9 · Source: PubMed
CITATIONS READS
31 816
6 authors, including:
Jeng Wei Sung-how Sue
Cheng Hsin General Hospital Cheng Hsin General Hospital
185 PUBLICATIONS 1,617 CITATIONS 31 PUBLICATIONS 446 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Sung-how Sue on 13 May 2014.
The user has requested enhancement of the downloaded file.
ORIGINAL ARTICLE
Cardiopulmonary Resuscitation in Prone Position:
A Simplified Method for Outpatients
Jeng Wei*, David Tung, Sung-How Sue, Shing-Van Wu, Yi-Cheng Chuang, Chung-Yi Chang
Heart Centre, Cheng-Hsin General Hospital, Taipei, Taiwan, R.O.C.
Background: The efficacy of cardiopulmonary resuscitation (CPR) is vital for saving lives of victims with sudden cardiac
arrest. In 1960, Kuowenhoven and colleagues proposed the method that has become standard for CPR. Despite
vast input of resources for public education and training of this procedure, its success rate outside hospitals remains
poor to dismal. During CPR, restoration of respiration is as important as circulation. But opening the airway and
giving effective mouth-to-mouth respiration is difficult for lay people to learn. Furthermore, most bystanders are reluctant
to do mouth-to-mouth respiration because of the risk of infection. Therefore, the general population needs a more
simplified CPR method for outpatients. The practice of CPR in the prone position, first proposed by McNeil in 1989,
has not been adopted, despite the fact that it meets the desirable requirements of ideal resuscitation: simultaneous
restoration of circulation and respiration with a very simple maneuver.
Methods: Part 1 (circulation test): Eleven patients who expired in the intensive care unit (ICU), with arterial lines
attached, received standard pre-cordial cardiac massage, and the generated blood pressure (BP) was recorded.
They were then turned to the prone position, with the head turned to one side. We compressed the patient’s
thoracic spine with the same force used in standard CPR (rhythm of approximately 60 per minute each time when
the back bounces back), and the BP was also recorded. Part 2 (ventilation test): Ten healthy volunteers (5 doctors
and 5 nurses) were enlisted for respiratory assessment during compression on the back. With the nose clipped
and spontaneous breathing held, the volunteer’s exhaled tidal volume upon compression was measured with a
spirometer.
Results: Standard external cardiac massage of the cadavers generated BPs of 55 ± 20/13 ± 7 mmHg; however,
external compression on the back of the cadavers generated higher BP of 79 ± 20/17 ± 10 mmHg (p = 0.028,
Wilcoxon signed-rank analysis). External compression on the back of the volunteers generated mean tidal volumes
of 399 ± 110 mL.
Conclusion: Our study revealed that prone CPR provides good respiratory and circulatory support at the same time.
It is easy to perform and it may be a good alternative way for bystanders to perform CPR in public surroundings.
We recommend that more investigators do further studies on this topic. [J Chin Med Assoc 2006;69(5):202–206]
Key Words: cardiopulmonary resuscitation, prone position
Introduction and electrical defibrillation introduced by Kuowenhoven
1
et al in 1960 has become the standard method for the
The effectiveness of cardiopulmonary resuscitation past 40 years. However, the success rate for CPR
(CPR) before arrival at hospital is a vital factor in saving outside hospitals remains poor to dismal, despite a vast
2–4
victims of sudden cardiac arrest. The combination of input of resources for its training. Attempts have been
mechanical ventilation, external pre-cordial compression, made to simplify the technique of CPR. The idea of
*Correspondence to: Dr. Jeng Wei, Heart Centre, Cheng-Hsin General Hospital, 45, Cheng-Hsin St., Pei-Tou,
Taipei 112, Taiwan, R.O.C.
E-mail: chghjw@yahoo.com.tw •
Received: July 21, 2005 •
Accepted: December 29, 2005
202 J Chin Med Assoc • May 2006 • Vol 69 • No 5
©2006 Elsevier. All rights reserved.
*050612/Cardio/out/ppp 202 5/10/06, 1:43 PM
Prone CPR
CPR in the prone position (prone CPR) was first Five doctors (including some of the authors) and 5
mentioned by McNeil in 1989,2 and reinforced by nurses also volunteered. They were asked to bite tightly
5
Stewart in 2002. Prone CPR seems to meet the desirable on a mouthpiece that was connected to a spirometer
requirements of ideal resuscitation for outpatients, but (Haloscale, Ferraris Medical, Holland, NY, USA), while
it has not been adopted as the standard method. There in the prone position with the head turned to one side.
6,7
are few clinical studies on prone CPR. More clinical With a nose clip applied, they were asked to hold their
data are necessary to draw support for this ideal CPR spontaneous breathing while a nurse was performing
procedure. Since 1999, we started to collect data on the same massage on their back for 1 minute. The
expired patients in the intensive care unit (ICU) for subject’s exhaled tidal volume upon compression on
clinical study of prone CPR. the back was measured and recorded (Table 2).
Methods Results
With the permission of the families, 11 patients who By external compression on the back of the 11 cadavers
expired in the ICU (Table 1), who had arterial lines whose mean body weight was 65.4 ± 9.0 kg, the mean
attached to physiologic monitors, were included in systolic BP generated was 79.4 ± 20.3 mmHg and
this study. They received standard pre-cordial cardiac diastolic pressure was 16.7 ± 10.3 mmHg. The average
massage for 1 minute, and the BP tracings were rate of back compression was 60 per minute. By pre-
recorded. They then were turned to the prone position cordial compression on 8/11 cadavers, the mean
with the head turned to one side. Similar to standard systolic BP generated was 55.4 ± 20.3 mmHg and
pre-cordial cardiac massage, a nurse was asked to diastolic pressure was 13.0 ± 6.7 mmHg. Wilcoxon
compress the patient’s thoracic spine regularly at a rate signed-rank test of these data yielded a statistically
of about 60 per minute for 1 minute (each time when significant p value of 0.028 (Table 1). By external
the back bounced back), and the generated blood compression on the back of the volunteers whose
pressure (BP) tracing was recorded. Patients who were mean body weight was 63.3 ± 14.7 kg, the mean tidal
severely dehydrated or hypovolemic, such as those volume recorded was 399 ± 110 mL (Table 2).
who died of head injury and sepsis, were excluded Representative arterial BP tracing generated from pre-
from this study. cordial and back compression are shown in Figure 1.
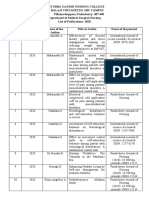
Table 1. Blood pressure measurements in expired patients with supine and prone CPR
BP, supine BP, prone
Case No. Gender Age BW, kg Diagnosis Procedure
mmHg mmHg
1 M 58 60 CAD CABG × 3 N/A* 110/20
2 M 68 62 CAD + RHD CABG + AVR N/A* 70/20
3 F 58 51 RHD MVR N/A* 90/20
4 M 60 65 DCMP Nil 80/25 110/40
5 M 57 67 CAD + ICMP CABG, HTx 60/10 78/10
6 M 78 75 Ao dissection Arch 90/20 90/20
with rupture replacement
7 M 49 78 CAD, AMI HTx 55/5 90/10
8 M 57 80 CAD with CABG 41/15 66/5
RV rupture + RV repair
9 M 50 64 DCMP Nil 39/7 52/4
10 M 75 57 SBE CABG + AVR 43/11 62/24
11 M 39 60 ICMP Nil 35/11 55/11
Mean ± SD 59 ± 11 65 ± 9 (55 ± 20)/(13 ± 7) (79 ± 20) †/(17 ± 10)
AMI = acute myocardial infarction; Ao = aorta; AVR = aortic valve replacement; BW = body weight; CABG = coronary artery bypass grafting;
CAD = coronary artery disease; DCMP = dilated cardiomyopathy; HTx = heat transplantation; MVR = mitral valve replacement; RHD = rheumatic heart
disease; RV = right ventricle; SBE = subacute bacterial endocarditis.
*Blood pressure in supine position was not recorded in the first 3 cases.
†
Statistically significant (Wilcoxon signed-rank test, p = 0.028)
J Chin Med Assoc • May 2006 • Vol 69 • No 5 203
*050612/Cardio/out/ppp 203 5/10/06, 1:43 PM
J. Wei, et al
Table 2. Tidal volume measurements in volunteers Discussion
Volunteer Gender Age Body weight, Tidal volume,
Successful CPR for victims of cardiac arrest outside the
No. kg mL
hospital remains very difficult. According to a report
1 M 53 84 550 by Brison et al,3 the overall survival rate was only 2.5%
2 M 38 77 400
for a consecutive sample of 1,510 primary cardiac
3 M 45 75 450
arrest patients in 5 Ontario communities, although
4 M 52 80 600
the average ambulance response time for witnessed
5 M 32 65 400
6 F 35 51 275
cases was 7.8 minutes.
7 F 32 51 300 Most of the general public is not familiar with the
8 F 28 44 300 standard CPR procedure introduced by Kuowenhoven
1 th
9 F 25 56 400 et al. A recent survey showed that 84% of 6 -year
10 F 23 50 310 medical students in Japan might not perform standard
CPR properly.8 Great effort has been exerted around
Mean ± SD 36 ± 11 63 ± 15 399 ± 110
the world to teach lay people to perform standard
2–4
M = male; F = female. CPR, but the results remain unsatisfactory.
Figure 1. A representative arterial
blood pressure tracing during
chest compression for a 60-year-
old male who died of dilated
cardiomyopathy on March 26,
2000. The upper tracing is EKG
C
and the lower radial arterial blood
pressure (scale: 0/40, 0/80,
and 0/120 mmHg). (A) Cardiac
massage from the anterior chest
wall (standard CPR method). (B)
Cardiac massage from the back
(thoracic spine), gentle force.
(C) Cardiac massage from the
back (thoracic spine), more
forceful.
204 J Chin Med Assoc • May 2006 • Vol 69 • No 5
*050612/Cardio/out/ppp 204 5/10/06, 1:43 PM
Prone CPR
While caring for critical patients in the ICU, we Our volunteers included 5 doctors and 5 nurses. They
have observed that many were still conscious and alert were asked to hold a spontaneous breath during back
despite a systolic BP of 60 mmHg. It is believed that compression. The tidal volume thus generated was
ischemic injury of the kidney, liver, and lungs may surprisingly good and was similar to normal breathing.
occur during prolonged hypotension, but the brain is With regular back compression, the respiratory rate
protected by reactive vasodilatation. Therefore, it is was approximately 60 per minute, which might cause
not direly urgent to generate a high BP during CPR. hyperventilation, but this might compensate for
Our data suggested that the BP generated with back metabolic acidosis during cardiac arrest.
compression is no less than that generated from pre- Vomiting and aspiration pneumonia are serious
cordial compression. Both provided suboptimal, but complications of standard CPR. Stomach content
probably adequate, BP for patients if they can arrive at frequently regurgitates and goes into the airway if the
a hospital without much delay. patient is in the supine position. CPR in the prone
Pre-cordial cardiac massage is also difficult for lay position may prevent these complications.
people to learn. Most people cannot remember which Some other alternative methods of CPR, including
9 10
point of the sternum to compress and how much force vest CPR, interposed abdominal compression, and
11,12
to apply. Excessive force of compression during pre- active chest compression-decompression have been
cordial massage may cause rib fracture and is hazardous introduced, but these methods remain difficult for lay
to the heart. This is especially important, because most people to learn.
bystanders cannot differentiate cardiac arrest from The importance of public-access defibrillators has
other conditions such as shock, bradycardia, or stroke been stressed, and automated external defibrillators
in which pre-cordial cardiac massage is unnecessary or (AED) have been placed in targeted public places,
even harmful. Back compression homogeneously such as airports, shopping centers, and casinos in
shortens the distance between the sternum and the affluent countries.13 The survival rate, however, is not
4
spine and is, thus, less likely to cause rib fracture and any better, as reported in several studies. In most
injury to the heart. instances, bystanders were reluctant to apply immediate
During CPR, effective ventilation is as important as CPR to prehospital victims. We believe that it is most
restoration of blood circulation, and in conventional important to restore the victim’s respiratory and
CPR, the airway must be cleared first. Unfortunately, circulatory functions before arrival at the hospital, and
with the lack of powered suction in public surroundings, defibrillation may even be harmful to the victim if not
it is difficult for bystanders to clear the victim’s airway. done properly.
Besides, if the victim is unconscious, his tongue may Successful CPR in the prone position during
fall back to the larynx and cause airway obstruction intracranial or spinal cord surgery has been reported in
14
while lying in the supine position. Air can be forced the literature. The maneuver, however, is different
into the lungs only when the mandible is held upwards from this proposed prone CPR. In those cases, the
to open the airway during mouth-to-mouth artificial patient was intubated and was placed in the prone
breathing, which is difficult for lay people to learn and position. The ongoing surgery, thus, made changing
can only be performed by trained and experienced of the patient’s position impossible. Surgeons place
rescuers. In most instances, bystanders in public their hands under the sternum to perform the reversed
surroundings cannot perform mouth-to-mouth pre-cordial compression. We believe that back
artificial breathing correctly. Thus, it is only when compression is easier and may have the same effect.
endotracheal intubation is available that standard CPR McNeil listed desirable requirements of an ideal
can be performed effectively. In the prone position, method of CPR as:
the tongue falls by gravity and the airway opens 1. Can be performed by 1 rescuer as effectively as
spontaneously. No endotracheal intubation is needed by 2;
during prone CPR. 2. Does not require mouth-to-mouth contact;
Does prone CPR provide adequate ventilation? At 3. Does not cause gastric distension;
the beginning, we tried to measure the tidal volume 4. Relieves gastric distension;
during back compression in cadavers, but found that 5. Avoids the danger of aspiration of vomitus if
they were not good candidates. The reason is that regurgitation occurs;
most of them died of multiorgan failure and had severe 6. Avoids the necessity for maneuvers to open the
pulmonary complication before death, which is airway;
dissimilar to victims outside the hospital. However, 7. Assists ventilation and circulation with the same
conscious volunteers are ideal for the ventilation test. maneuver;
J Chin Med Assoc • May 2006 • Vol 69 • No 5 205
*050612/Cardio/out/ppp 205 5/10/06, 1:43 PM
J. Wei, et al
8. Can relieve upper airway obstruction by simulating References
a modified Heimlich maneuver, using the same
1. Kuowenhoven WB, Jude JR, Knickerbocker GG. Closed chest
maneuver as is being used for ventilation and
cardiac massage. JAMA 1960;173:1064–7.
circulatory assist; 2. McNeil E. Re-evaluation of cardiopulmonary resuscitation.
9. Should require less than 30 minutes to learn; Resuscitation 1989;18:1–5.
10.The simplicity of the method should promote easy 3. Brison RJ, Davidson JR, Dreyer JF, Jones G, Maloney J,
Munkley DP, O’Connor HM, et al. Cardiac arrest in Ontario:
retention of skills;
circumstances, community response, role of prehospital
11.If commenced in less than 4 minutes from the time defibrillation and predictors of survival. Can Med Assoc J 1992;
of cardiac arrest, it should maintain a circulation 147:1427–8.
that has been oxygenated sufficiently to allow 4. Pell JP, Sirel JM, Marsden AK, Ford I, Walker NL, Cobbe SM.
Potential impact of public access defibrillators on survival after
advanced life support methods to have a reasonable
out of hospital cardiopulmonary arrest: retrospective cohort
chance of success by resuscitation, if available within study. Br Med J 2002;325:515–22.
2
8 minutes from the time of arrest. 5. Stewart J. Resuscitating an idea: prone CPR. Resuscitation
2002;54:231–6.
6. Mazer SP, Weisfeldt M, Bai D, Cardinale C, Arora R, Ma C,
Prone CPR has not attracted the attention of
Sciacca RR, et al. Reverse CPR: a pilot study of CPR in the
program directors who are advocating and promoting prone position. Resuscitation 2003;57:279–85.
CPR by the public, no doubt because they believe the 7. Wei J. Cardiopulmonary resuscitation in prone position: a
back compression would not be effective to generate simplified method for outpatients. Resuscitation 2004;62:
120–1.
adequate BP. From our study, prone CPR seems to
8. Suzuki A, Suzuki Y, Takahata O, Fujimoto K, Nagashima K,
meet all the criteria of the ideal method of CPR. In Mamiya K, Sengoku K, et al. A survey of 3,303 6th-year medical
addition, because of the simplicity of this method, the students from 36 universities concerning knowledge of
cost of teaching may be much less than expected. resuscitation—more than 80% of medical students cannot
perform standard cardiopulmonary resuscitation? Masui 2001;
How should lay people be taught to perform prone
50:316–22.
CPR? It is very simple! 9. Halperin HR, Tsitlik JE, Gelfand M, Weisfeldt ML, Gruben
Step 1: Place the patient in the prone position. KG, Levin HR, Rayburn BK, et al. A preliminary study of
Step 2: Bend either one of the forearms and put it cardiopulmonary resuscitation by circumferential compression
of the chest with use of a pneumatic vest. N Engl J Med 1993;
underneath the forehead or just turn the head to one
329:762–8.
side if you do not remember how to bend and place the 10. Ohomoto T, Miura I, Konno A. A new method of external
forearms. cardiac massage to improve diastolic augmentation and prolong
Step 3: Compress the mid-portion of the thoracic survival time. Ann Thorac Surg 1976;21:284–90.
11. Lurie KG, Lindo C, Chin J. CPR: The P stands for plumber’s
spine with 2 hands of regular force and rhythm (each
helper. JAMA 1990;264:1661.
time when the chest wall bounces back) until arrival at 12. Tang W, Weil MH, Schock RB, Sato Y, Lucas J, Sun S, Bisera
hospital. J. Phased chest and abdominal compression-decompression: a
In conclusion, prone CPR not only may provide new option for cardiopulmonary resuscitation. Circulation
1997;95:1335–40.
good respiratory and circulatory support, but also is easy
13. Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW,
for people to perform. It may also have fewer complications Hardman RG. Outcomes of rapid defibrillation by security
of rib fracture, heart injury, and aspiration pneumonia. officers after cardiac arrest in casinos. N Engl J Med 2000;343:
It is probably a good alternative to conventional CPR for 1206–9.
14. Sun WZ, Huang FY, Kung KL, Fan SZ, Chen TL. Successful
bystanders to perform effective CPR in public
cardiopulmonary resuscitation of two patients in the prone
surroundings. We hope this paper may attract more position using reversed pre-cordial compression. Anesthesiology
investigators to do further studies on this topic. 1992;77:202–4.
206 J Chin Med Assoc • May 2006 • Vol 69 • No 5
*050612/Cardio/out/ppp 206 5/10/06, 1:43 PM
View publication stats
You might also like
- 348-Article Text-1233-1-10-20201221Document5 pages348-Article Text-1233-1-10-20201221Salsabila FitriaNo ratings yet
- Wiga 2011Document9 pagesWiga 2011S4lNo ratings yet
- Trial CPRDocument12 pagesTrial CPRgabriella_jabirNo ratings yet
- Extracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac ArrestDocument10 pagesExtracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac Arrestika nur annisaNo ratings yet
- Referensi 7Document8 pagesReferensi 7Nophy NapitupuluNo ratings yet
- Cardiopulmonary Resuscitation: Unusual Techniques For Unusual SituationsDocument10 pagesCardiopulmonary Resuscitation: Unusual Techniques For Unusual SituationsAmirullah AbdiNo ratings yet
- When Is It Safe To Exercise Mechanically Ventilated Patients HL 2017 BoydDocument6 pagesWhen Is It Safe To Exercise Mechanically Ventilated Patients HL 2017 BoydLeandro MoreiraNo ratings yet
- TugasDocument8 pagesTugasNoviNo ratings yet
- Minimally Invasive Direct Cardiac MassagDocument13 pagesMinimally Invasive Direct Cardiac MassagTM AnNo ratings yet
- Cardiopulmonary Resuscitation: Unusual Techniques For Unusual Situations ConclusionDocument8 pagesCardiopulmonary Resuscitation: Unusual Techniques For Unusual Situations ConclusionIlham AkbarNo ratings yet
- EpinefrinaDocument10 pagesEpinefrinaJorge CamarilloNo ratings yet
- Trombolisis en PCR ExtrahospitalarioDocument12 pagesTrombolisis en PCR ExtrahospitalarioMariangel PerezNo ratings yet
- Research: Cite This As: BMJ 2011 342:c7106Document7 pagesResearch: Cite This As: BMJ 2011 342:c7106rizki heriyadiNo ratings yet
- 2012 ResuscitationDocument5 pages2012 ResuscitationHandrian RahmanNo ratings yet
- 2018 Article 1648Document5 pages2018 Article 1648Dewi NurfadilahNo ratings yet
- Systematic Review Yulia CandraDocument12 pagesSystematic Review Yulia Candrabayu khayudinNo ratings yet
- CPR HSRP BenarDocument8 pagesCPR HSRP Benarrizki heriyadiNo ratings yet
- Anestesiología Anestesiología AnestesiologíaDocument16 pagesAnestesiología Anestesiología AnestesiologíaIqbal HarzikyNo ratings yet
- Chest Physiotherapy After Coronary Artery Bypass Graft Surgery-A Comparison of Three Different Deep Breathing TechniquesDocument6 pagesChest Physiotherapy After Coronary Artery Bypass Graft Surgery-A Comparison of Three Different Deep Breathing TechniquesmadeNo ratings yet
- Perimortem Cesarean Delivery and Subsequent Emergency Hysterectomy: New Strategy For Maternal Cardiac ArrestDocument5 pagesPerimortem Cesarean Delivery and Subsequent Emergency Hysterectomy: New Strategy For Maternal Cardiac ArrestPutri RamadaniNo ratings yet
- Analysis and Results of Prolonged Resuscitation in Cardiac Arrest Patients Rescued by Extracorporeal Membrane OxygenationDocument7 pagesAnalysis and Results of Prolonged Resuscitation in Cardiac Arrest Patients Rescued by Extracorporeal Membrane OxygenationMuhammad RizqiNo ratings yet
- 2017TheSwan GanzCatheterRemainsaCriticallyImpoDocument7 pages2017TheSwan GanzCatheterRemainsaCriticallyImpoCarlos Henrique FerreiraNo ratings yet
- Chest Physical Therapy For Patients in The Intensive Care Unit (APTA Journal)Document19 pagesChest Physical Therapy For Patients in The Intensive Care Unit (APTA Journal)Physio EbookNo ratings yet
- Chest Physical Therapy For Patients in Intensive Care Unit: Key WordsDocument17 pagesChest Physical Therapy For Patients in Intensive Care Unit: Key WordsNeil Francis VillagonzaloNo ratings yet
- Noninvasive Ventilation For Prevention of Post-Extubation Respiratory Failure in Obese PatientsDocument8 pagesNoninvasive Ventilation For Prevention of Post-Extubation Respiratory Failure in Obese PatientsLestat80No ratings yet
- Gasping During Cardiac Arrest in Humans Is Frequent and Associated With Improved SurvivalDocument5 pagesGasping During Cardiac Arrest in Humans Is Frequent and Associated With Improved SurvivalCarla Eliberta ColodroNo ratings yet
- RCP Actaulizacion 2017Document7 pagesRCP Actaulizacion 2017Marisol López HernándezNo ratings yet
- Manejo Postparo Nuevas EstraDocument12 pagesManejo Postparo Nuevas EstraAngela Moreira ArteagaNo ratings yet
- Echocardiography in Hemodynamic MonitoringDocument5 pagesEchocardiography in Hemodynamic MonitoringDr.Biswajit jenaNo ratings yet
- Jurnal KardioDocument5 pagesJurnal KardiomadeNo ratings yet
- Comparative Study of Breathing Techniques After Coronary Artery by Pass GraftingDocument12 pagesComparative Study of Breathing Techniques After Coronary Artery by Pass GraftingJulenda CintarinovaNo ratings yet
- CPR With Chest Compression Alone or With Rescue Breathing: Original ArticleDocument11 pagesCPR With Chest Compression Alone or With Rescue Breathing: Original ArticlePinaDiantiNo ratings yet
- Stiell Et Al 2014 What Is The Optimal Chest Compression Depth During Out of Hospital Cardiac Arrest Resuscitation ofDocument9 pagesStiell Et Al 2014 What Is The Optimal Chest Compression Depth During Out of Hospital Cardiac Arrest Resuscitation oftempeuedanNo ratings yet
- Deep Breathing 9Document9 pagesDeep Breathing 9Asih SulistiyaniNo ratings yet
- Trial of Continuous or Interrupted Chest Compressions During CPRDocument12 pagesTrial of Continuous or Interrupted Chest Compressions During CPRDinar Riny NvNo ratings yet
- Laparoscopic Cholecystectomy Under Spinal Anaesthesia: A Prospective StudyDocument4 pagesLaparoscopic Cholecystectomy Under Spinal Anaesthesia: A Prospective Studyrazaqhussain00No ratings yet
- 1430 FullDocument8 pages1430 Fullganesh goreNo ratings yet
- En V29n2a08Document5 pagesEn V29n2a08Iago DjavanNo ratings yet
- Document Journal Review 4.09Document11 pagesDocument Journal Review 4.09Anonymous diwFs3MsWRNo ratings yet
- Evolution and Revolution in Cardiopulmonary Resuscitation 2Document5 pagesEvolution and Revolution in Cardiopulmonary Resuscitation 2angelama1783riosNo ratings yet
- Crew Size Simulation Cardiac Arrest TapiaiDocument12 pagesCrew Size Simulation Cardiac Arrest TapiaiJamison ParfittNo ratings yet
- Auricchio & Cols. (1999)Document6 pagesAuricchio & Cols. (1999)Luba D'AndreaNo ratings yet
- Improved Oxygenation During Standing Performance of Deep Breathing Exercises With Positive Expiratory Pressure After Cardiac Surgery: A Randomized Controlled TrialDocument5 pagesImproved Oxygenation During Standing Performance of Deep Breathing Exercises With Positive Expiratory Pressure After Cardiac Surgery: A Randomized Controlled TrialVidya UtamaNo ratings yet
- Concord CPR ManualDocument54 pagesConcord CPR ManualtntranNo ratings yet
- AHA Vs ERC GuidelinesDocument39 pagesAHA Vs ERC GuidelinesYoel Harianto100% (2)
- PEEP - Ventilação - Perfusão em Prona e Supino ArtigosDocument9 pagesPEEP - Ventilação - Perfusão em Prona e Supino Artigosle franchiNo ratings yet
- Chest Physical Therapy For Patients in Intensive Care Unit: Key WordsDocument17 pagesChest Physical Therapy For Patients in Intensive Care Unit: Key Wordsketrin maladaNo ratings yet
- International Federation For Emergency Medicine Consensus Statement Sonography in Hypotension and Cardiac Arrest Shoc An InternDocument12 pagesInternational Federation For Emergency Medicine Consensus Statement Sonography in Hypotension and Cardiac Arrest Shoc An InternMai PyonNo ratings yet
- Deep-Breathing Exercises Reduce PDFDocument9 pagesDeep-Breathing Exercises Reduce PDFAde PayNo ratings yet
- 2016 Current Recommendations On Adult Resuscitation BJADocument6 pages2016 Current Recommendations On Adult Resuscitation BJADr.Biswajit jenaNo ratings yet
- Farmacology Del Paro CardiacoDocument14 pagesFarmacology Del Paro CardiacoNicoSwtifNo ratings yet
- Thoracic Epidural For Modified Radical Mastectomy in A High-Risk PatientDocument2 pagesThoracic Epidural For Modified Radical Mastectomy in A High-Risk PatientBianca CaterinalisendraNo ratings yet
- Updates On CPR - AHDocument15 pagesUpdates On CPR - AHsrimegawatihirataNo ratings yet
- Updates On CPR - AHDocument15 pagesUpdates On CPR - AHFaisal ShaldyNo ratings yet
- 1 s2.0 S0735109700007798 MainDocument8 pages1 s2.0 S0735109700007798 MainPaula RNo ratings yet
- Rehabilitacion Pulmonar en La UciDocument19 pagesRehabilitacion Pulmonar en La UcimavhelllinaNo ratings yet
- Borenstein 05Document9 pagesBorenstein 05emmanuel le bretNo ratings yet
- Hands Only Compression Only CardiopulmonDocument7 pagesHands Only Compression Only CardiopulmonMuhammad ArifinNo ratings yet
- Jurnal 3 ACBTDocument4 pagesJurnal 3 ACBTMuhamad Elfitra SalamNo ratings yet
- Endocrine Surgery: Butterworths International Medical Reviews: SurgeryFrom EverandEndocrine Surgery: Butterworths International Medical Reviews: SurgeryI. D. A. JohnstonNo ratings yet
- Clinical Features and Risk Factors of Pancytopenia: A Study in A Tertiary Care HospitalDocument5 pagesClinical Features and Risk Factors of Pancytopenia: A Study in A Tertiary Care HospitalDwitaNo ratings yet
- 3758 5371 1 SM - 2Document8 pages3758 5371 1 SM - 2Nana SetiawanNo ratings yet
- ICH Review Hostettler ExRevNeuroth 062019Document18 pagesICH Review Hostettler ExRevNeuroth 062019DwitaNo ratings yet
- New Variant of SARS-CoV-2 in UK Causes Surge of COVID-19Document2 pagesNew Variant of SARS-CoV-2 in UK Causes Surge of COVID-19DwitaNo ratings yet
- Emergence of A New SARS-CoV-2 Variant in The UKDocument2 pagesEmergence of A New SARS-CoV-2 Variant in The UKDwitaNo ratings yet
- Identification and Computational Analysis of Mutations in SARS-CoV-2Document19 pagesIdentification and Computational Analysis of Mutations in SARS-CoV-2DwitaNo ratings yet
- Severe Acute Respiratory Syndrome Coronavirus 2 - Virus Mutations in Specific European PopulationsDocument4 pagesSevere Acute Respiratory Syndrome Coronavirus 2 - Virus Mutations in Specific European PopulationsDwitaNo ratings yet
- TSANZ AcuteOxygen Guidelines 2016 WebDocument20 pagesTSANZ AcuteOxygen Guidelines 2016 WebArnold BarraNo ratings yet
- Anastesi OJAnes20120500001 - 14738359Document4 pagesAnastesi OJAnes20120500001 - 14738359DwitaNo ratings yet
- Emerging Sars-Cov-2 Mutation Hot Spots Include A Novel Rna-Dependent-Rna Polymerase VariantDocument9 pagesEmerging Sars-Cov-2 Mutation Hot Spots Include A Novel Rna-Dependent-Rna Polymerase VariantFKIANo ratings yet
- Surgical Critical Care Andrew H. Stephen, Charles A. Adams, JR., William G. CioffiDocument30 pagesSurgical Critical Care Andrew H. Stephen, Charles A. Adams, JR., William G. CioffiDwitaNo ratings yet
- Different Mutations in SARS-CoV-2 Associate With Severe and Mild OutcomeDocument5 pagesDifferent Mutations in SARS-CoV-2 Associate With Severe and Mild OutcomeDwitaNo ratings yet
- Intravenous Fluid Therapy in Adults in Hospital Algorithm Poster Set 191627821Document5 pagesIntravenous Fluid Therapy in Adults in Hospital Algorithm Poster Set 191627821Wira Sasmita P100% (1)
- AbortionDocument3 pagesAbortionKim LompotNo ratings yet
- Beasley 2015Document10 pagesBeasley 2015DwitaNo ratings yet
- Anastesi OJAnes20120500001 - 14738359Document4 pagesAnastesi OJAnes20120500001 - 14738359DwitaNo ratings yet
- Prone Cardiopulmonary Resuscitation: A Scoping and Expanded Grey Literature Review For The COVID-19 PandemicDocument9 pagesProne Cardiopulmonary Resuscitation: A Scoping and Expanded Grey Literature Review For The COVID-19 PandemicDwitaNo ratings yet
- Equicover Health Cis PWDocument27 pagesEquicover Health Cis PWLogeshParthasarathyNo ratings yet
- WEBINAR On PEDIATRIC TRAUMADocument44 pagesWEBINAR On PEDIATRIC TRAUMAGovindarajan HariharanNo ratings yet
- Comparison of The Effects of PhotobiomodulationDocument11 pagesComparison of The Effects of PhotobiomodulationJuan AndradeNo ratings yet
- Discover Cyrix-TSL - Your Healthcare Solutions PartnerDocument8 pagesDiscover Cyrix-TSL - Your Healthcare Solutions Partnerabdirahman haadiNo ratings yet
- Comparison of The Effect of Three Treatment Interventions For The Control of Meniere 'S Disease: A Randomized Control TrialDocument6 pagesComparison of The Effect of Three Treatment Interventions For The Control of Meniere 'S Disease: A Randomized Control Trialian danarkoNo ratings yet
- VY-EnFlow Brochure CF805170019 (2) Jul10-FinalDocument8 pagesVY-EnFlow Brochure CF805170019 (2) Jul10-FinalShaikh Emran HossainNo ratings yet
- Chapter 30 Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationDocument23 pagesChapter 30 Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationAbel C. Idusma Jr.No ratings yet
- Bentall Procedure - WikipediaDocument3 pagesBentall Procedure - WikipediaMashudi SyaikhanNo ratings yet
- Spontaneous Tumescence After Implantation of Three-Piece Hydraulic Penile Prostheses: A Short-Term ExperienceDocument4 pagesSpontaneous Tumescence After Implantation of Three-Piece Hydraulic Penile Prostheses: A Short-Term ExperienceAlejandro OlmedoNo ratings yet
- 2.tracheostomy CareDocument48 pages2.tracheostomy Carems khanNo ratings yet
- Position S: Pratiksha RaiDocument49 pagesPosition S: Pratiksha RaiJoanne Cristie TolopiaNo ratings yet
- Comfort Drain Product Brochure English 08 2018Document2 pagesComfort Drain Product Brochure English 08 2018Gino PeñalozaNo ratings yet
- Ojo 2013112116194629 PDFDocument5 pagesOjo 2013112116194629 PDFYash SharmaNo ratings yet
- Oxygenation ChecklistDocument22 pagesOxygenation ChecklistKen Morales Alcantara100% (1)
- Orthopedic InjuriesDocument24 pagesOrthopedic Injuriesamber tariqNo ratings yet
- Library Book List - ENDO, CONSE, NEW, JOURNALSDocument10 pagesLibrary Book List - ENDO, CONSE, NEW, JOURNALSMohammed TarekNo ratings yet
- Analgesia For Iliac Crest Bone GraftDocument9 pagesAnalgesia For Iliac Crest Bone GraftDominik Chirito PastorNo ratings yet
- Naspo Gastric Tube Feeding FinalDocument32 pagesNaspo Gastric Tube Feeding FinalNezuko0% (1)
- Acl Preservation With The Acl Repair Tightrope ImplantDocument15 pagesAcl Preservation With The Acl Repair Tightrope ImplantJose SantiagoNo ratings yet
- Veterinary Officer Exams Preparation by DR HassanDocument8 pagesVeterinary Officer Exams Preparation by DR HassanZohaib AliNo ratings yet
- ELSO Interim Guidelines For Venoarterial.2Document18 pagesELSO Interim Guidelines For Venoarterial.2BiancaPancuNo ratings yet
- SBH/HSC Pre-Angiogram/ Angioplasty/Stent ChecklistDocument2 pagesSBH/HSC Pre-Angiogram/ Angioplasty/Stent ChecklistKena Ben100% (2)
- FILE NO 12 VDocument13 pagesFILE NO 12 VMuthu KumaranNo ratings yet
- Operating Room Form (Major and Minor) : University of The VisayasDocument16 pagesOperating Room Form (Major and Minor) : University of The VisayasJohn Mitchelle NNo ratings yet
- Abdominal Pain Flow ChartDocument1 pageAbdominal Pain Flow ChartJeff ZhouNo ratings yet
- The Management of Compensatory Sweating After Thoracic SympathectomyDocument9 pagesThe Management of Compensatory Sweating After Thoracic SympathectomyJuan David Arboleda LopezNo ratings yet
- 2020 USCLS GP Guide For Dental FeesDocument86 pages2020 USCLS GP Guide For Dental FeesChristieBrownNo ratings yet
- The Children'S Healing Initiative: Brecken Chinn Swartz, Ph.D. Executive Director HandreachDocument26 pagesThe Children'S Healing Initiative: Brecken Chinn Swartz, Ph.D. Executive Director Handreachhehehahee3777No ratings yet
- Standard Operating Procedures For HospitDocument62 pagesStandard Operating Procedures For HospitThanRMNo ratings yet
- Recent Advances in Dental Radiography For Pediatric Patients: A ReviewDocument6 pagesRecent Advances in Dental Radiography For Pediatric Patients: A ReviewFebriani SerojaNo ratings yet