Professional Documents
Culture Documents
2020 JNM DOPA - Neuroblastoma
Uploaded by
IchaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2020 JNM DOPA - Neuroblastoma
Uploaded by
IchaCopyright:
Available Formats
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
Diagnosis, Treatment Response, and Prognosis: The Role of
18F-DOPA PET/CT in Children Affected by Neuroblastoma in
Comparison with 123I-mIBG Scan: The First Prospective Study
Arnoldo Piccardo1, Giovanni Morana2, Matteo Puntoni3, Sara Campora4, Stefania Sorrentino5, Pietro Zucchetta6,
Martina Ugolini7, Massimo Conte5, Angelina Cistaro1, Giulia Ferrarazzo1, Marco Pescetto8, Marco Lattuada8,
Gianluca Bottoni1, Alberto Garaventa5, Luca Giovanella*9, and Egesta Lopci*10
1Department of Nuclear Medicine, Galliera Hospital, Genoa, Italy; 2Neuroradiology Unit, IRCCS Istituto Giannina Gaslini, Genova,
Italy; 3ClinicalTrial Research Unit, Galliera Hospital, Genoa, Italy; 4Department of Oncology, Galliera Hospital, Genoa, Italy;
5Unit of Pediatric Oncology, Istituto Giannina Gaslini, IRCCS, Genoa, Italy; 6Department of Nuclear Medicine, University Hospital
of Padova, Padova, Italy; 7Medical Physics Department, Galliera Hospital, Genoa, Italy; 8Anaesthesiology Department, Galliera
Hospital, Genoa, Italy; 9Clinic of Nuclear Medicine and Molecular Imaging, Imaging Institute of Southern Switzerland, Bellinzona
and Lugano, Switzerland; and 10Department of Nuclear Medicine, Humanitas Clinical and Research Hospital, IRCCS, Rozzano, Italy
(.7.5) was associated with progression-free survival. Conclusion:
18F-DOPA PET/CT is more sensitive than 123I-MIBG WBS in stag-
Our purpose was to evaluate the diagnostic role of 18F-3,4-dihy-
droxyphenylalanine (DOPA) PET/CT at the time of staging in chil- ing neuroblastoma patients and evaluating disease persistence af-
dren with neuroblastoma and to investigate its ability to assess ter chemotherapy. In a time-to-event analysis, posttherapeutic
18F-DOPA WBMB remained the only risk factor associated with
treatment response. We also investigated the prognostic value of
18F-DOPA PET/CT at the same time points. Methods: We enrolled disease progression.
children with neuroblastoma at onset. Before and after induction Key Words: PET/CT; DOPA; neuroblastoma; chemotherapy;
chemotherapy, all patients underwent 18F-DOPA PET/CT and 123I- prognosis
metaiodobenzylguanidine (MIBG) scanning plus SPECT/CT. 18F- J Nucl Med 2020; 61:367–374
DOPA PET/CT results were compared with those of 123I-MIBG DOI: 10.2967/jnumed.119.232553
whole-body scanning (WBS). For each modality, patient-based
analysis and lesion-based analysis were performed and sensitivity
was calculated. We applied scoring systems to 123I-MIBG scanning
and 18F-DOPA PET/CT (i.e.,123I-MIBG WBS score and whole-body
metabolic burden [WBMB], respectively) and evaluated the associ-
ation between these parameters, the principal neuroblastoma risk
factors, and outcome. Results: We enrolled 16 high-risk and 2 in-
H igh-risk neuroblastoma, commonly defined by metastatic
disease in patients older than 12–18 mo (1,2), by protooncogene
termediate-risk neuroblastoma patients. On patient-based analysis, MYCN amplification in patients at any age, and by unfavorable
sensitivity in detecting primary tumors, soft-tissue metastases, and
histopathologic features (3,4), displays long-term survival rates of
bone or bone-marrow metastases was 83%, 50%, and 92%, re-
spectively, for 123I-MIBG WBS versus 94%, 92%, and 100%, re- approximately 40% (5–7). Internationally agreed-upon treatment
spectively, for 18F-DOPA PET/CT. On lesion-based analysis, the options for high-risk neuroblastoma (NB-AR-01 protocol) include
sensitivity of 18F-DOPA PET/CT in detecting soft-tissue and bone or multiagent induction chemotherapy, surgery, high-dose chemo-
bone-marrow metastases was 86% and 99%, respectively—signif- therapy followed by autologous stem cell transplantation, external-
icantly higher than that of 123I-MIBG WBS, at 41% and 93%, re- beam radiotherapy, radionuclide therapy, differentiation therapies,
spectively. After therapy, on patient-based analysis, the sensitivity and immunotherapy (8). A complete response to induction chemo-
in detecting primary tumors, soft-tissue metastases, and bone or therapy, as evaluated by various diagnostic procedures (e.g., imaging
bone-marrow metastases was 72%, 33%, and 38%, respectively, or bone-marrow biopsy), is one of the main early prognostic factors
for 123I-MIBG WBS versus 83%, 75% and 54%, respectively, for in high-risk neuroblastoma.
18F-DOPA PET/CT. On lesion-based analysis, the sensitivity of 18F-
123I-metaiodobenzylguanidine (MIBG) scintigraphy has long
DOPA PET/CT in detecting soft-tissue and bone or bone-marrow
metastases was 77% and 86%, respectively—significantly higher been recognized as the main imaging procedure for staging of
than that of 123I-MIBG WBS, at 28% and 69%, respectively. During neuroblastoma. More recently, the International Society of Paedi-
follow-up, 8 cases of disease progression and 5 deaths occurred. atric Oncology European Neuroblastoma (SIOPEN) identified the
On multivariate analysis, only posttherapeutic 18F-DOPA WBMB SIOPEN semiquantitative 123I-MIBG skeletal scoring system
(SIOPEN Method 3) as an excellent inter- and intraobserver method
that can estimate the extension of bone or bone-marrow metastases
Received Jun. 18, 2019; revision accepted Aug. 12, 2019. in a reproducible way, thereby providing a reliable prognostic in-
For correspondence or reprints contact: Arnoldo Piccardo, Department of
Nuclear Medicine, E.O. Ospedali Galliera, Mura delle Cappuccine 14, 16128
dicator in neuroblastoma (9). In addition, SIOPEN Method 3 was
Genoa, Italy. validated as a prognostic response predictor in 2 independent tri-
E-mail: arnoldo.piccardo@galliera.it al populations (8). More specifically, a postinduction skeletal
*Contributed equally to this work.
Published online Sep. 20, 2019. score greater than 3 identifies patients with a very poor prognosis
COPYRIGHT © 2020 by the Society of Nuclear Medicine and Molecular Imaging. who require different treatment strategies (9). On the other hand,
18F-DOPA PET/CT AND NEUROBLASTOMA • Piccardo et al. 367
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
123I-MIBG scintigraphy is cumbersome (10), requiring proper pa- chemotherapy, and written informed consent. The exclusion criteria
tient preparation and correct recognition of the distribution pattern, were comorbidity due to other neoplasms, known hypersensitivity to
and is frequently limited by the difficult anatomy in children and the active ingredient or excipients contained in the radiopharmaceu-
low-quality images (11). Various PET tracers have been tested as ticals, and any other medical condition contraindicating the study in
effective substitutes for 123I-MIBG in assessing neuroblastoma (12), the investigator’s judgment.
and 18F-3,4-dihydroxyphenylalanine (DOPA) (13), radiolabeled so-
matostatin analogs (14,15), and 124I-MIBG have proved the most Imaging Modalities
123I-MIBG scintigraphy and 18F-DOPA PET/CT were performed on
promising (16). 18F-DOPA PET/CT has already proved to be more
fasting patients within 10 d of each other; no treatment was adminis-
sensitive than 123I-MIBG scanning in patients with neuroblastoma
tered between the 2 scans. Images were acquired according to standard
relapse (17). Specifically, 18F-DOPA PET/CT has been demon-
procedures (10).
strated to be a reliable diagnostic procedure in detecting small
Whole-body 18F-DOPA PET/CT was performed 60 min after tracer
soft-tissue and bone or bone-marrow metastases that are not accu-
injection according to our previous experience (10,17–19). The activ-
rately detected by 123I-MIBG scintigraphy (17,18). In addition, this ity administered was calculated according to the patient’s body weight
imaging procedure has shown better diagnostic results than conven- (4 MBq/kg), with a minimum activity of 80 MBq (range, 80–185
tional procedures (i.e., CT and MRI), disclosing more neuroblastoma MBq; mean, 110 MBq; SD, 635 MBq).
localizations in bone marrow and lymph nodes and more soft-tissue 123I-MIBG scans were acquired 24 h after injection of the tracer by
recurrences (19). Direct comparison with 18F-FDG PET/CT has also means of a dual-head g-camera (Millennium; GE Healthcare). The
shown that 18F-DOPA PET/CT is the most sensitive and accurate activity administered was calculated according to the patient’s body
method of identifying neuroblastoma localizations, whether weight, with a minimum activity of 80 MBq, as suggested by Lass-
metastases or primary tumors (20). Moreover, its prognostic role mann et al. (range, 80–185 MBq; mean, 110 MBq; SD, 635 MBq)
at the time of recurrence has already been validated by means of (21). Spot views of the various body segments were acquired. Each
an adequate whole-body scoring system, defined as whole-body spot view was acquired for a maximum of 10 min (;500 kilocounts;
metabolic burden (WBMB), which is able to evaluate disease ex- 100 kilocounts for spot views of the lower limbs). Thoracoabdominal
tension (18). In this context, the possibility of disease progression SPECT was performed on all patients at intervals of 24 h, as suggested
and death has been seen to increase in proportion to the WBMB by Matthay et al. (22) and Olivier et al. (23). Fused SPECT/CT images
value (with a cutoff value of .7.5) (18). However, 18F-DOPA PET/ were analyzed on a dedicated workstation (Xeleris; GE Healthcare)
CT has never been tested as a pivotal diagnostic tool for staging of that allowed coregistration of 123I-MIBG and CT images previously
patients affected by neuroblastoma and evaluation of treatment re- acquired during the PET/CT examination.
sponse to induction chemotherapy. Indeed, this diagnostic PET-
Image Interpretation
based approach could help in stratifying patients after induction
Two expert nuclear medicine physicians interpreted separately 18F-
chemotherapy and identify subjects at different risks of disease
DOPA PET/CT and 123I-MIBG SPECT/CT. They were aware of the pa-
persistence or recurrence. The proven ability of 18F-DOPA PET/
tient’s clinical history and anatomical imaging modalities (i.e., MRI/CT)
CT to detect small metastases could be even more important when but blinded to any 18F-DOPA PET/CT or 123I-MIBG SPECT/CT results,
evaluating disease persistence. respectively. Finally, a consensus review of discordant findings was done.
The primary aim of this study was to evaluate the diagnostic On 18F-DOPA PET/CT or 123I-MIBG SPECT/CT, any focal, nonphy-
role of 18F-DOPA PET/CT at the time of first diagnosis in children siologic uptake higher than that of the surrounding background was
with neuroblastoma. We also investigated the ability of this pro- considered pathologic (17,18). The 2 readers analyzed the whole-body
cedure to assess response to chemotherapy. Lastly, we evaluated images by focusing on primary tumors (abdominal or thoracic), lymph
the prognostic role of 18F-DOPA PET/CT in high-risk neuroblas- nodes, lungs, liver, bone, and brain. Both studies were interpreted on a
toma patients on diagnosis and after induction chemotherapy by patient-by-patient basis (patient-based analysis) and a lesion-by-lesion
testing the relationship between WBMB, progression-free survival basis (lesion-based analysis) before and after chemotherapy. In patient-
(PFS), and overall survival (OS). based analysis, the detection rate (DR) was defined as the ability to
detect at least 1 pathologic finding in each subject. In lesion-based
analysis, the DR was defined as the ability to detect suspected lesions
MATERIALS AND METHODS
in relation to the total number of lesions detected by both tracers and
The local ethics committee and the Agenzia Italiana del Farmaco, a by anatomic imaging modalities.
public agency of the Italian Ministry of Health, approved the study.
Written informed consent was obtained from all subjects. The trial Scoring Systems
was registered in the European Clinical Trial Database (EudraCT The effectiveness of 123I-MIBG and 18F-DOPA PET/CT in detect-
number 2012-005398-30). ing neuroblastoma was assessed by reviewing the uptake patterns for
each radiopharmaceutical in the following locations: primary tumor,
Patient Population local and regional soft-tissue metastases, and bone and bone-marrow
From December 2013 to January 2017, we prospectively enrolled metastases. SIOPEN Method 3 was applied to the 123I-MIBG scans to
neuroblastoma patients who were candidates for SIOPEN therapeutic evaluate disease extent in the bone and bone marrow (8). To semi-
protocols and referred for imaging procedures to the Nuclear Medicine quantify soft-tissue neuroblastoma localizations, the modified Curie
Department of Galliera Hospital. Before and within 7 d after chemo- scoring system was applied, based on the methodology of Matthay et
therapy, all patients underwent both 18F-DOPA PET/CT and 123I-MIBG al. (soft-tissue123I-MIBG score) (18,24).
whole-body scanning (WBS) with additional SPECT. The imaging pro- Another scoring system, the WBMB, was applied to 18F-DOPA
cedures were performed within 10 d of each other (range, 1–10 d; mean, PET/CT images to evaluate the extent of bone or bone-marrow in-
4.1 d; SD, 63.3 d). volvement and that of primary tumor and of soft-tissue metastases
The inclusion criteria were histologically proven neuroblastoma at (18). Specifically, for 18F-DOPA PET/CT, SIOPEN Method 3 was
the time of first diagnosis (age . 12 mo and , 18 y), no previous applied to evaluate the extent of bone and bone-marrow disease. To
368 THE JOURNAL OF NUCLEAR MEDICINE • Vol. 61 • No. 3 • March 2020
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
better characterize the intrinsic metabolic burden of each bone seg- or death, and we tested the difference between time-to-event curves by
ment, we multiplied the SUVmean by the score of each bone segment. means of the log-rank test. Cox proportional-hazards modeling was used
The whole-body bone metabolic burden was calculated as the sum of to estimate the risk of disease persistence/progression and death from
the bone-segment metabolic burden of each bone segment in the PET any cause, adjusting for age and other factors that proved to be associ-
image. To determine the extent and load of soft-tissue recurrence or ated with PFS and OS on univariate analyses. Since 123I-MIBG SPECT/
metastases, a whole-body soft-tissue metabolic burden was applied CT and 18F-DOPA PET/CT scores were highly correlated, we used
per patient (18,25). For each tumor lesion, the soft-tissue metabolic different models for each score to avoid collinearity and to test their
burden was calculated as SUVmean multiplied by tumor volume. Tu- independent association with PFS and OS. All analyses were conducted
mor volume was obtained from the CT images of the PET/CT acqui- using Stata software (version 14.2; StataCorp.). Two-tailed probabilities
sitions (26). The whole-body soft-tissue metabolic burden was are reported, and a P value of 0.05 was used to define nominal statistical
calculated as the sum of the metabolic burden of each tumor lesion significance.
in the PET image. Finally, the overall WBMB was calculated as the
sum of whole-body bone metabolic burden plus whole-body soft-tis- RESULTS
sue metabolic burden.
We enrolled 16 high-risk and 2 intermediate-risk patients; their
Risk Stratification main characteristics are summarized in Table 1. For clinical rea-
Each patient was risk-stratified according to age at the time of sons, the 2 intermediate-risk patients and 1 of the high-risk pa-
diagnosis (#18 mo or .18 mo), histopathologic results, stage (3 or 4), tients underwent not NB-AR-01 but different therapeutic protocols
MYCN amplification, lactate dehydrogenase level, homovanillic and with different schemes of induction therapy; they were therefore
vanilmandelic acid levels, 123I-MIBG score before and after induction included only in the diagnostic analysis and were excluded from
chemotherapy, and WBMB before and after induction chemotherapy. the prognostic analysis (Table 1).
At final follow-up, patients were deemed to be disease-free if At the time of first staging, 123I-MIBG SPECT/CT proved pos-
they had less than 10 mm of residual soft tissue at the primary site itive in 17 of 18 patients, whereas 18F-DOPA PET/CT was positive
and in nonprimary lesions and complete resolution of 123I-MIBG in all 18 patients. On patient-based analysis, the DR in detecting
uptake (27). primary tumors, soft-tissue metastases, and bone or bone-marrow
Patients were considered to have disease persistence or partial metastases was 83%, 50%, and 92%, respectively, for 123I-MIBG
response if there was a decrease by more than 30% at the primary and SPECT/CT versus 94%, 92%, and 100%, respectively, for 18F-
nonprimary sites and if 123I-MIBG uptake at the primary site was stable, DOPA PET/CT (Fig. 1; Table 2). On lesion-based analysis, the
improved, or resolved and there was more than a 50% reduction in DR of 18F-DOPA PET/CT in detecting soft-tissue and bone or
123I-MIBG absolute bone score (27).
bone-marrow metastases was 86% and 99%, respectively—signif-
Disease was considered to have progressed if there was a 20% increase
icantly higher (P , 0.001) than that of 123I-MIBG SPECT/CT, at
in longest lesion diameter or any new soft-tissue or bone lesions detected
41% and 93%, respectively (Fig. 2; Table 3).
by CT/MRI that were also 123I-MIBG–avid or were biopsied and
After induction chemotherapy, 123I-MIBG SPECT/CT proved
confirmed to be neuroblastoma (27).
positive in 14 of 18 neuroblastoma patients, whereas 18F-DOPA
Standard of Reference PET/CT was still positive in 17 patients. However, when the anal-
Although only DRs were calculated for each diagnostic modality, ysis did not consider primary tumors but only metastatic sites of
we applied a standard of reference, which was able to provide some disease, 123I-MIBG SPECT/CT proved positive in only 8 patients;
confirmation of the site of disease. The standard of reference for the by contrast, 18F-DOPA PET/CT was still positive in 15.
primary tumor was based on histopathology results (available for all On patient-based analysis, the DR in detecting primary tumors,
patients). The standard of reference for soft-tissue metastases was soft-tissue metastases, and bone or bone-marrow metastases was
based on histopathology results or on diagnostic contrast-enhanced 72%, 33%, and 38%, respectively, for 123I-MIBG SPECT/CT ver-
CT or MRI findings (available for all patients). The gold standards for sus 83%, 75%, and 54%, respectively, for 18F-DOPA PET/CT
bone and bone-marrow metastases were bone-marrow biopsy (avail- (Table 2). On lesion-based analysis, the DR of 18F-DOPA PET/CT
able for all patients), CT, or MRI (available for all patients). A median in detecting soft-tissue and bone or bone-marrow metastases was
clinical and imaging follow-up of 29.3 mo (range, 19–53 mo) was 77% and 86%, respectively—significantly higher than that of 123I-
available for each patient. MIBG SPECT/CT, at 28% and 69%, respectively (P , 0.001 and
Clinical decisions after induction chemotherapy were based on the P 5 0.001, respectively) (Table 3; Fig. 3).
results of 123I-MIBG WBS and conventional radiologic imaging (i.e., Over a median follow-up of 29.3 mo (interquartile range, 19.0–
CT and MRI), not the results of 18F-DOPA PET/CT. 53.1 mo), among the 15 patients considered in the prognostic
analysis, 8 cases of disease progression and 5 deaths occurred.
Statistical Analysis
Kaplan–Meier PFS curves showed that only initial stage (stage 3
Descriptive statistics included mean, SD, and range for data
vs. 4) and the 18F-DOPA WBMB measured after induction che-
involving continuous factors and scores; in the case of categoric factors,
we used absolute and relative frequencies, along with percentage. The
motherapy (WBMB . 7.5; Fig. 4) were associated with progno-
Spearman rank correlation coefficient was adopted to test the correlation sis. However, an important trend toward significance was also
between 123I-MIBG SPECT/CT and 18F-DOPA PET/CT scores. For observed between outcome and pretherapy 123I-MIBG WBS
diagnostic analyses, DRs, defined as the percentage of positive subjects ($46), pretherapy 18F-DOPA WBMB ($45; Fig. 4), and homo-
(in patient-based analysis) or lesions (in lesion-based analysis), were vanillic acid levels ($32 mmol/mmol creatinine) measured before
calculated for each diagnostic modality at each site of disease. We therapy. Finally, risk estimates (unadjusted and adjusted) for dis-
adopted the exact McNemar test to compare DRs between diagnostic ease progression were also calculated from the Cox model. After
modalities. For prognostic analyses, we used Kaplan–Meier estimates of adjustment for all risk factors showing at least a trend toward
the cumulative probability of PFS and OS, defined as the interval be- significance at the univariate level, 18F-DOPA WBMB evaluated
tween initial diagnosis and the onset of disease persistence/progression after induction chemotherapy was the only factor independently
18F-DOPA PET/CT AND NEUROBLASTOMA • Piccardo et al. 369
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
TABLE 1
Main Clinical, Histopathologic, and Biochemical Features of Patients (n 5 18)
Feature Data
Age (mo) 34 ± 19 (12–72)
Sex, male 12 (67)
Histopathology
Undifferentiated 6 (33)
Poorly differentiated 9 (50)
Unknown 3 (17)
Stage
3 4 (22)
4 14 (78)
Treatment
NB AR 01 15 (83)
LINES/personalized 2/1 (17)
MYC amplification 10 (56)
Lactate dehydrogenase (UI/L), median (IQR) median, 2,890 (IQR, 1,506–5,275)
Homovanillic acid levels (μmol/mmol creatinine), median (IQR) median, 66.7 (IQR, 32.0–76.6)
Vanilmandelic acid levels (μmol/mmol creatinine), median (IQR) median 26.1 (IQR, 5.3–123.9)
18F-DOPA WBMB score
Before induction chemotherapy 191.9 ± 349.1 (0–1,120)
After induction chemotherapy 18.2 ± 43.1 (0–169)
123I-MIBG WBS score
Before induction chemotherapy 24.7 ± 20.9 (0–58)
After induction chemotherapy 3.6 ± 9.9 (0–42)
Continuous data are mean ± SD followed by range in parentheses; count data are number followed by percentage in parentheses
(unless otherwise noted).
LINES 5 Low and Intermediate Risk Neuroblastoma European Study; IQR 5 interquartile range.
and directly associated with PFS. More specifically, patients with 7.5 of less (hazard ratio, 10.7; 95% confidence interval, 1.09–104.8;
a 18F-DOPA WBMB score higher than 7.5 displayed a signifi- P 5 0.041). No significant association was found between the risk
cantly higher risk of disease progression than those with a score of factors considered and OS.
Of the 9 patients with completely neg-
ative findings on 123I-MIBG WBS and per-
sistently positive 18F-DOPA WBMB after
induction chemotherapy, 3 showed persis-
tence or progression of disease at the end
of treatment. However, the 6 patients who
did not develop disease progression had an
18F-DOPA WBMB value no higher than 1.
All 5 patients with a WBMB higher than
7.5 after induction chemotherapy devel-
oped persistence or progression of disease,
whereas only 2 of the 10 patients with a
WBMB lower than 7.5 developed persis-
tence or progression of disease (Supple-
mental Fig. 1; supplemental materials are
available at http://jnm.snmjournals.org). By
contrast, although a 123I-MIBG WBS score
higher than 3 identified 3 patients who
FIGURE 1. A 3-y-old child with stage 4 neuroblastoma (MYCN-amplified) of thoracic primary. (A
showed disease persistence or progression,
and B) 18F-DOPA PET/CT (maximum-intensity projection [A] and axial image [B]) showed intense
uptake in primary tumor and identified some bone and bone-marrow metastases (arrows). (C and 4 (33%) of the 12 patients with a 123I-MIBG
123
D) I-MIBG WBS with additional SPECT/CT (axial image [C] and anterior and posterior views [D]) WBS score of 3 or less developed disease
did not identify any site of pathologic uptake. persistence or progression (Fig. 5). Thus,
370 THE JOURNAL OF NUCLEAR MEDICINE • Vol. 61 • No. 3 • March 2020
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
TABLE 2
DRs for Patient-Based Analysis
Timing 123I-MIBG SPECT/CT 18F-DOPA PET/CT P*
Before induction chemotherapy
Primary tumors 15 (83%) 17 (94%) 0.5
Soft-tissue metastases 6 (50%) 11 (92%) 0.06
Bone or bone-marrow metastases 12 (92%) 13 (100%) 1.0
After induction chemotherapy
Primary tumor 13 (72%) 15 (83%) 0.6
Soft-tissue metastases 4 (33%) 9 (75%) 0.06
Bone or bone-marrow metastases 5 (38%) 7 (54%) 1.0
*Exact McNemar significance probability.
DRs (%) were calculated for each single diagnostic modality at each site of disease. Denominator for DRs on primary tumors is total
number of patients (n 5 18), considering that all are subjects with established cancer. For evaluations on soft-tissue and bone or bone-
marrow lesions, denominator is maximum number of patients found to be positive by 2 diagnostic modalities (n 5 12 for soft tissue; n 5 13
for bone or bone-marrow lesions).
123I-MIBG WBS and 18F-DOPA WBMB scores were positively persistent bone and bone-marrow foci of pathologic uptake after
correlated only before induction chemotherapy (before: Spearman chemotherapy. However, it would have been difficult to ascertain
r 5 0.61, P 5 0.007; after: r 5 0.38, P 5 0.11). Specifically, the real clinical impact of this finding if we had not tested the
18F-DOPA WBMB showed greater dispersion than 123I-MIBG prognostic role of 18F-DOPA PET/CT. In other words, the real
WBS, displaying an interquartile range of 20–128 before chemo- issue is whether the higher number of lesions disclosed by 18F-
therapy and 1–9 after chemotherapy, versus respective ranges of DOPA PET/CT after induction chemotherapy was associated with
2–42 and 0–2 for 123I-MIBG (Supplemental Fig. 2). a higher probability of disease persistence or progression at the
end of follow-up or whether the higher number of lesions was a
simple and futile expression of diagnostic sensitivity. Accordingly,
DISCUSSION
we evaluated the prognostic value of 18F-DOPA PET/CT both at
18
First, we found that F-DOPA PET/CT was more sensitive than the time of disease onset and after induction chemotherapy. To
123I-MIBG scanning in detecting neuroblastoma localizations in better understand each patient’s risk, we semiquantified the dis-
a well-selected population of neuroblastoma children analyzed at ease burden by using the previously validated 18F-DOPA WBMB
the time of first diagnosis, as proved by comparing PET/CT and (18) and compared this with the 123I-MIBG WBS and the other
123I-MIBG SPECT/CT images of all patients. This finding is of recognized prognostic factors. Both scores measure the burden of
particular interest, as in the 2 previous studies comparing 18F- the disease, excluding the primary tumor. So far, no reliable and
DOPA and 123I-MIBG (17,20), SPECT/CT images were unavail- validated methods have been used to quantify the extension and
able. In our study, 18F-DOPA PET/CT was even more sensitive in activity of the primary tumor on 123I-MIBG SPECT/CT (8,10)
detecting soft-tissue metastases and small bone or bone-marrow and 18F-DOPA PET/CT images. In this regard, we found that, at
localizations. the univariate level, only disease stage on initial diagnosis (stage 3
Second, we found that 18F-DOPA PET/CT was a reliable di- vs. stage 4) and WBMB measured after induction chemotherapy
agnostic tool for evaluating treatment response after induction (WBMB . 7.5) were associated with prognosis. Notably, neither
chemotherapy and provided important information on disease per- MYCN amplification nor a 123I-MIBG score higher than 3 after
sistence. Specifically, 18F-DOPA PET/CT proved to be more sen- chemotherapy was significantly associated with PFS. By contrast,
sitive than 123I-MIBG SPECT/CT in disclosing small and faint a marked disease burden documented at the time of first diagnosis
by means of 123I-MIBG scanning (123I-
MIBG WBS . 46) and 18F-DOPA PET/
CT (WBMB $ 45) showed an important
trend toward significance (P 5 0.06 and
P 5 0.08, respectively). This finding seems
to be in line with what was reported in a
recent paper by Lewington et al. (9), who
showed that patients with a SIOPEN score
higher than 48 at the time of first diagnosis
had a significantly lower response rate to
induction chemotherapy than patients with
FIGURE 2. A 3-y-old child with stage III neuroblastoma (MYCN-amplified) of abdominal pri-
mary. On axial images, suggestive left paravertebral nodules detected on contrast-enhanced a SIOPEN score of 48 or less.
CT were negative on 123I-MIBG SPECT/CT (A and B) but positive on 18F-DOPA PET/CT (B However, the Cox models showed that
and C). only an 18F-DOPA PET/CT WBMB score
18F-DOPA PET/CT AND NEUROBLASTOMA • Piccardo et al. 371
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
TABLE 3
DRs for Lesion-Based Analysis
Timing 123I-MIBG SPECT/CT 18F-DOPA PET/CT P*
Before induction chemotherapy
Soft-tissue metastases 20 (41%) 42 (86%) ,0.001
Bone or bone-marrow metastases 494 (93%) 522 (99%) ,0.001
After induction chemotherapy
Soft-tissue metastases 11 (28%) 30 (77%) ,0.001
Bone or bone-marrow metastases 54 (69%) 67 (86%) 0.001
*Exact McNemar significance probability.
DRs (%) were calculated for each single diagnostic modality at each site of disease. Denominator for DRs is maximum number of
lesions found to be positive by 2 diagnostic modalities: n 5 49 and n 5 39 before and after induction chemotherapy, respectively, for soft
tissue; n 5 529 and n 5 78 before and after induction chemotherapy, respectively, for bone or bone-marrow lesions.
higher than 7.5 measured after induction chemotherapy was asso- In addition, all 5 patients with 18F-DOPA WBMB scores higher
ciated with PFS. This cutoff had already been validated by our than 7.5 after induction therapy showed disease persistence or
previous study (18), in which patients with a WBMB score higher progression regardless of their 123I-MIBG WBS score. From this
than 7.5 at the time of neuroblastoma relapse had a higher prob- point of view, 18F-DOPA WBMB was the most accurate parameter
ability of disease progression and death. In the present study, we in stratifying the risk of high-risk neuroblastoma patients after
found that, of the 9 patients with negative 123I-MIBG WBS results induction chemotherapy. We could speculate that a greater use of
and persistent positive 18F-DOPA WBMB results after induction sensitive PET tracers, such as 18F-DOPA, could identify patients at
chemotherapy, 3 had disease persistence or progression at the end very high risk for whom a more intense therapeutic regimen is
of follow-up. All 3 of these patients showed at least 4 persistent warranted.
disease localizations on 18F-DOPA PET/CT, and in 2 patients the This study has some limitations: its low statistical power (low
disease burden measured by means of WBMB was scored at number of patients and events) and the fact that the effects of different
higher than 7.5. therapies performed after induction therapy were not considered
FIGURE 3. A 4-y-old child with stage 4 neuroblastoma (not MYCN-amplified) of abdominal primary. (A and C) At time of first staging, both
123 I-MIBG WBS (A) and 18F-DOPA PET/CT with additional SPECT/CT (C) clearly showed primary tumor and diffuse bone or bone-marrow metastases.
(B and D) After induction chemotherapy, both techniques identified some residual bone-marrow metastases (black arrows) but 18F-DOPA
PET/CT (maximum-intensity projection) revealed 3 small, persistent bone-marrow metastases (red arrows) not seen on 123I-MIBG WBS.
372 THE JOURNAL OF NUCLEAR MEDICINE • Vol. 61 • No. 3 • March 2020
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
FIGURE 5. A 2-y-old child with stage III neuroblastoma (MYCN-ampli-
fied) of abdominal primary. Primary tumor was large and calcified at time
of first staging, with major lymph node involvement. On axial images
after induction chemotherapy (A–C; B is the CT component of SPECT/
CT and PET/CT), large residual mass did not show any 123I-MIBG or 18F-
DOPA uptake. However, some calcific lymph nodes negative on 123I-
MIBG SPECT/CT were still evident on 18F-DOPA PET/CT (arrows). After
induction chemotherapy, 123I-MIBG WBS was ,3 (i.e., 0) but WMBM was
.7.5 (i.e., 16). By end of follow-up (19 mo), patient had died of disease
progression.
fused by means of appropriate software but were not acquired by
means of a dedicated hybrid SPECT/CT system. This procedure is
not optimal, as it does not provide the improved image quality
yielded by CT attenuation correction. These issues may have
caused the well-known diagnostic and prognostic power of the
123I-MIBG scanning to be underestimated in this group of patients.
In addition, the 18F-DOPA WBMB score is characterized by high
variability, as a result of the high intrinsic sensitivity of PET/CT
procedures and the possibility of expressing the extent of soft-tissue
metastases and uptake intensity; 18F-DOPA WBMB therefore pro-
vides adequate information about patient risk, which may not be
fully estimated by the 123I-MIBG score.
However, to our knowledge, this is the first paper to prospectively
analyze the diagnostic and prognostic role of 18F-DOPA PET/CT
in a well-selected population of children (median age, 28 mo) with
high- and intermediate-risk neuroblastoma. Indeed, our preliminary
data suggest that this tracer is more effective than 123I-MIBG for the
staging, treatment response evaluation, and prognostication of
neuroblastoma patients.
In any case, to better evaluate the role of these 2 tracers in neuro-
blastoma, a direct comparison between 18F-DOPA and 124I-MIBG
should be conducted. Such an analysis would eliminate any bias re-
lated to the different imaging procedures presented in this study.
Finally, although 123I-MIBG scanning seems to be less sensitive
than 18F-DOPA PET/CT, the principal advantage of 123I-MIBG
remains its intrinsic theragnostic property. Although considering
that the pathologic distribution of the tracers seems to be similar
(17,18,28), there are not sufficient data to support the possibility of
selecting patients for 123I-MIBG therapy by using 18F-DOPA PET/
CT. From this point of view, 18F-DOPA cannot replace 123I-MIBG.
CONCLUSION
Our results confirmed good agreement between 18F-DOPA
FIGURE 4. Kaplan–Meier PFS curves according to 18F-DOPA WBMB # PET/CT semiquantification and 123I-MIBG scanning in neuroblas-
7.5 and . 7.5 after induction chemotherapy (A), 18F-DOPA WBMB (me- toma patients at the time of first staging, in that a positive corre-
dian) # 45 and . 45 before therapy (B), and 123I-MIBG WBS score (third lation between the 2 techniques was observed. However, to stage
quartile) # 46 and . 46 before therapy (C).
neuroblastoma patients and, particularly, to evaluate disease per-
sistence after induction chemotherapy, 18F-DOPA PET/CT appears
in the prognostic analysis. In this context, we did not find any to be more sensitive than 123I-MIBG WBS with additional SPECT/
associations between the different risk factors and OS. Indeed, CT. In time-to-event analyses, 18F-DOPA WBMB, evaluated after
we used PFS alone as a surrogate of prognosis. induction chemotherapy, remained the only risk factor independently
In addition, a single stage 4 123I-MIBG–negative patient was and directly associated with disease progression. Further confirmation
included in the study. SPECT/CT images were coregistered and on a larger group of patient is required.
18F-DOPA PET/CT AND NEUROBLASTOMA • Piccardo et al. 373
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
DISCLOSURE 10. Bar-Sever Z, Biassoni L, Shulkin B, et al. Guidelines on nuclear medicine
imaging in neuroblastoma. Eur J Nucl Med Mol Imaging. 2018;45:2009–
No potential conflict of interest relevant to this article was reported. 2024.
11. Bonnin F, Lumbroso J, Tenenbaum F, Hartmann O, Parmentier C. Refining in-
terpretation of MIBG scans in children. J Nucl Med. 1994;35:803–810.
KEY POINTS
12. Pfluger T, Piccardo A. Neuroblastoma: MIBG imaging and new tracers. Semin
Nucl Med. 2017;47:143–157.
QUESTION: Is 18F DOPA PET/CT able to identify, after induction
13. Piccardo A, Lopci E. Potential role of 18F-DOPA PET in neuroblastoma. Clin
chemotherapy, neuroblastoma patients with persistence of dis- Transl Imaging. 2016;4:79–86.
ease at higher risk of disease progression? 14. Kong G, Hofman MS, Murray WK, et al. Initial experience with gallium-68
DOTA-octreotate PET/CT and peptide receptor radionuclide therapy for pediatric
PERTINENT FINDINGS: In a clinical study including 18 neuro-
patients with refractory metastatic neuroblastoma. J Pediatr Hematol Oncol.
blastoma patients at high and intermediate risk, 18F-DOPA PET/
2016;38:87–96.
CT was a reliable diagnostic tool for evaluating treatment re- 15. Alexander N, Vali R, Ahmadzadehfar H, Shammas A, Baruchel S. Review: The
sponse after induction chemotherapy and provided important in- role of radiolabeled DOTA-conjugated peptides for imaging and treatment of
formation on the presence of disease persistence. Specifically, childhood neuroblastoma. Curr Radiopharm. 2018;11:14–21.
18F-DOPA PET/CT proved to be significantly more sensitive than 16. Cistaro A, Quartuccio N, Caobelli F, et al. 124I-MIBG: a new promising positron-
123I-MIBG SPECT/CT in disclosing small and faint persistent bone emitting radiopharmaceutical for the evaluation of neuroblastoma. Nucl Med Rev
and bone-marrow foci of pathologic uptake after chemotherapy. Cent East Eur. 2015;18:102–106.
17. Piccardo A, Lopci E, Conte M, et al. Comparison of 18F-dopa PET/CT and 123I-
IMPLICATIONS FOR PATIENT CARE: When compared with MIBG scintigraphy in stage 3 and 4 neuroblastoma: a pilot study. Eur J Nucl
other prognostic factors and molecular imaging procedures, 18F- Med Mol Imaging. 2012;39:57–71.
DOPA PET/CT, performed after induction chemotherapy, was able 18. Piccardo A, Puntoni M, Lopci E, et al. Prognostic value of 18F-DOPA PET/CT at
to better identify patients at very high risk amenable to further the time of recurrence in patients affected by neuroblastoma. Eur J Nucl Med
Mol Imaging. 2014;41:1046–1056.
effective treatments.
19. Lopci E, Piccardo A, Nanni C, et al. 18F-DOPA PET/CT in neuroblastoma
comparison of conventional imaging with CT/MR. Clin Nucl Med. 2012;37:
e73–e78.
20. Lu MY, Liu YL, Chang HH, et al. National Taiwan University Neuroblastoma
REFERENCES
Study Group characterization of neuroblastic tumors using 18F-FDOPA PET. J Nucl
1. London WB, Castleberry RP, Matthay KK, et al. Evidence for an age cutoff Med. 2013;54:42–49.
greater than 365 days for neuroblastoma risk group stratification in the Child- 21. Lassmann M, Biassoni L, Monsieurs M, Franzius C, Jacobs F; EANM Dosimetry
ren’s oncology group. J Clin Oncol. 2005;23:6459–6465. and Paediatrics Committees. The new EANM paediatric dosage card. Eur J Nucl
2. Moroz V, Machin D, Faldum A, et al. Changes over three decades in outcome Med Mol Imaging. 2007;34:796–798.
and the prognostic influence of age-at-diagnosis in young patients with neuro- 22. Matthay KK, Shulkin B, Ladenstein R, et al. Criteria for evaluation of disease
blastoma: a report from the international neuroblastoma risk group project. Eur extent by 123I-metaiodobenzylguanidine scans in neuroblastoma: a report for the
J Cancer. 2011;47:561–571. International Neuroblastoma Risk Group (INRG) Task Force. Br J Cancer.
3. Seeger RC, Brodeur GM, Sather H, et al. Association of multiple copies of the 2010;102:1319–1326.
N-myc oncogene with rapid progression of neuroblastomas. N Engl J Med. 23. Olivier P, Colarinha P, Fettich J, et al. Guidelines for radioiodinated MIBG
1985;313:1111–1116. scintigraphy in children. Eur J Nucl Med Mol Imaging. 2003;30:B45–B50.
4. Shimada H, Stram DO, Chatten J, et al. Identification of subsets of neuroblas- 24. Matthay KK, Edeline V, Lumbroso J, et al. Correlation of early metastatic re-
tomas by combined histopathologic and N-myc analysis. J Natl Cancer Inst. sponse by123I-metaiodobenzylguanidine scintigraphy with overall response and
1995;87:1470–1476. event-free survival in stage IV neuroblastoma. J Clin Oncol. 2003;21:2486–
5. Simon T, Hero B, Faldum A, et al. Long term outcome of high-risk neuroblas- 2491.
toma patients after immunotherapy with antibody ch14.18 or oral metronomic 25. Fiebrich HB, Brouwers AH, Kerstens MN, et al. 6-[F-18]fluoro-L-dihydroxyphe-
chemotherapy. BMC Cancer. 2011;11:21. nylalanine positron emission tomography is superior to conventional imaging
6. Valteau-Couanet D, Le Deley MC, Bergeron C, et al. Long-term results of the with 123I-metaiodobenzylguanidine scintigraphy, computer tomography, and
combination of the N7 induction chemotherapy and the busulfan-melphalan high magnetic resonance imaging in localizing tumors causing catecholamine excess.
dose chemotherapy. Pediatr Blood Cancer. 2014;61:977–981. J Clin Endocrinol Metab. 2009;94:3922–3930.
7. Matthay KK, Reynolds CP, Seeger RC, et al. Long-term results for children with 26. Berkowitz A, Basu S, Srinivas S, Sankaran S, Schuster S, Alavi A. Determination
high-risk neuroblastoma treated on a randomized trial of myeloablative therapy of whole-body metabolic burden as a quantitative measure of disease activity in
followed by 13-cis-retinoic acid: a children’s oncology group study. J Clin lymphoma: a novel approach with fluorodeoxyglucose-PET. Nucl Med Commun.
Oncol. 2009;27:1007–1013. 2008;29:521–526.
8. Ladenstein R, Lambert B, Pötschger U, et al. Validation of the mIBG skeletal 27. Park JR, Bagatell R, Cohn SL, et al. Revisions to the International Neuroblastoma
SIOPEN scoring method in two independent high-risk neuroblastoma popula- Response Criteria: a consensus statement from the National Cancer Institute
tions: the SIOPEN/HR-NBL1 and COG-A3973 trials. Eur J Nucl Med Mol clinical trials planning meeting. J Clin Oncol. 2017;35:2580–2587.
Imaging. 2018;45:292–305. 28. Piccardo A, Lopci E, Conte M, et al. Bone and lymph node metastases from
9. Lewington V, Lambert B, Poetschger U, et al. 123I-mIBG scintigraphy in neuro- neuroblastoma detected by 18F-DOPA-PET/CT and confirmed by posttherapy
blastoma: development of a SIOPEN semi-quantitative reporting, method by an 131 I-MIBG but negative on diagnostic 123 I-MIBG scan. Clin Nucl Med.
international panel. Eur J Nucl Med Mol Imaging. 2017;44:234–241. 2014;39:e80–e83.
374 THE JOURNAL OF NUCLEAR MEDICINE • Vol. 61 • No. 3 • March 2020
Downloaded from jnm.snmjournals.org by Infor_Biomed/Rete Ligure on April 16, 2020. For personal use only.
Diagnosis, Treatment Response, and Prognosis: The Role of 18F-DOPA PET/CT in
Children Affected by Neuroblastoma in Comparison with 123I-mIBG Scan: The First
Prospective Study
Arnoldo Piccardo, Giovanni Morana, Matteo Puntoni, Sara Campora, Stefania Sorrentino, Pietro Zucchetta, Martina
Ugolini, Massimo Conte, Angelina Cistaro, Giulia Ferrarazzo, Marco Pescetto, Marco Lattuada, Gianluca Bottoni,
Alberto Garaventa, Luca Giovanella and Egesta Lopci
J Nucl Med. 2020;61:367-374.
Published online: September 20, 2019.
Doi: 10.2967/jnumed.119.232553
This article and updated information are available at:
http://jnm.snmjournals.org/content/61/3/367
Information about reproducing figures, tables, or other portions of this article can be found online at:
http://jnm.snmjournals.org/site/misc/permission.xhtml
Information about subscriptions to JNM can be found at:
http://jnm.snmjournals.org/site/subscriptions/online.xhtml
The Journal of Nuclear Medicine is published monthly.
SNMMI | Society of Nuclear Medicine and Molecular Imaging
1850 Samuel Morse Drive, Reston, VA 20190.
(Print ISSN: 0161-5505, Online ISSN: 2159-662X)
© Copyright 2020 SNMMI; all rights reserved.
You might also like
- Sodium Fluoride PET/CT in Clinical UseFrom EverandSodium Fluoride PET/CT in Clinical UseKalevi KairemoNo ratings yet
- F-FDG Pet/Ct and I-Metaiodobenzylguanidine Imaging in High-Risk Neuroblastoma: Diagnostic Comparison and Survival AnalysisDocument7 pagesF-FDG Pet/Ct and I-Metaiodobenzylguanidine Imaging in High-Risk Neuroblastoma: Diagnostic Comparison and Survival AnalysisManos PanagiotidisNo ratings yet
- Diagnostic Value of F-FDG PET/CT in Paediatric Neuroblastoma: Comparison With I-MIBG ScintigraphyDocument7 pagesDiagnostic Value of F-FDG PET/CT in Paediatric Neuroblastoma: Comparison With I-MIBG ScintigraphyDhruv MahajanNo ratings yet
- Diagnostics 10 00663Document7 pagesDiagnostics 10 00663AdiNNo ratings yet
- Biomedicines 11 00128Document13 pagesBiomedicines 11 00128dmandatari7327No ratings yet
- F DOPA y Otros RF Pet en TNEDocument24 pagesF DOPA y Otros RF Pet en TNEMon Ti TaNo ratings yet
- I-MIBG in The Diagnosis of Primary and Metastatic NeuroblastomaDocument9 pagesI-MIBG in The Diagnosis of Primary and Metastatic NeuroblastomaAdiNNo ratings yet
- The Impact of PETCT On Paediatric OncologyDocument17 pagesThe Impact of PETCT On Paediatric OncologylkitkatgirlNo ratings yet
- 11C MetioninaDocument8 pages11C MetioninaPUIGCOZARNo ratings yet
- 10 1200@jco 20 00386Document12 pages10 1200@jco 20 00386rafaelskpkNo ratings yet
- Recent Advances in Radiological and Radionuclide Imaging and Therapy of Neuroendocrine TumoursDocument14 pagesRecent Advances in Radiological and Radionuclide Imaging and Therapy of Neuroendocrine TumoursrevanthNo ratings yet
- The Role of FDG-PET Scans in Patients With Lymphoma: Review in Translational HematologyDocument11 pagesThe Role of FDG-PET Scans in Patients With Lymphoma: Review in Translational HematologyPunam SinhaNo ratings yet
- 18F FDG PET CT Role in Staging of Gastric CancerDocument8 pages18F FDG PET CT Role in Staging of Gastric Cancermednuclpg mednuclpgNo ratings yet
- Craniotomy For Resection of Meningioma An Age Stratified AnalysisDocument7 pagesCraniotomy For Resection of Meningioma An Age Stratified Analysis49hr84j7spNo ratings yet
- Fluorine 18Document4 pagesFluorine 18Baby DragonNo ratings yet
- J Nucl Med-2009-Putzer-1214-21Document9 pagesJ Nucl Med-2009-Putzer-1214-21Madalina CordonasuNo ratings yet
- Pet Vs Mbgi NeuroblastomaDocument12 pagesPet Vs Mbgi NeuroblastomaItzia VerduzcoNo ratings yet
- TrialllDocument13 pagesTriallljunin_tim4619No ratings yet
- PET in MMDocument8 pagesPET in MMdanishNo ratings yet
- CRITERIOSUSOGA68Document9 pagesCRITERIOSUSOGA68Belen Fdez LlanaNo ratings yet
- Current Radiopharmaceuticals For Positron Emission Tomography of Brain TumorsDocument7 pagesCurrent Radiopharmaceuticals For Positron Emission Tomography of Brain TumorsAl KutbiNo ratings yet
- Jurnal Kanker TiroidDocument6 pagesJurnal Kanker TiroidEkfatil MardiyahNo ratings yet
- New Guidelines For Somatostatin ReceptorsDocument9 pagesNew Guidelines For Somatostatin ReceptorssatyaNo ratings yet
- FDG PET-CT in The Initial Staging and Restaging of Soft Tissue or Bone Sarcoma.Document7 pagesFDG PET-CT in The Initial Staging and Restaging of Soft Tissue or Bone Sarcoma.Anderson Ruben LizcanoNo ratings yet
- FTPDocument5 pagesFTPriezkytrinawatiNo ratings yet
- ch18 6 PDFDocument12 pagesch18 6 PDFomkarNo ratings yet
- PET-CT Radiomics in Breast Cancer - Promising Tool For PredictionDocument10 pagesPET-CT Radiomics in Breast Cancer - Promising Tool For Predictionmazda626 retrocarsNo ratings yet
- Validation of The Meet URO Score in Patients WithDocument9 pagesValidation of The Meet URO Score in Patients Withveaceslav coscodanNo ratings yet
- Cancers 15 00364 v2Document16 pagesCancers 15 00364 v2Raul Matute MartinNo ratings yet
- J Nucl Med-1997-Valdés Olmos-873-9Document8 pagesJ Nucl Med-1997-Valdés Olmos-873-9Mădălina VargaNo ratings yet
- PSMADocument10 pagesPSMADiego GavilanesNo ratings yet
- Nuclear Medicine Imaging in Neuroblastoma: Current Status and New DevelopmentsDocument22 pagesNuclear Medicine Imaging in Neuroblastoma: Current Status and New DevelopmentsAdiNNo ratings yet
- 1 s2.0 S2588931120300900 MainDocument10 pages1 s2.0 S2588931120300900 MainMiro SpiroNo ratings yet
- WBRT Plus SIB With Image Guided Intensity-Modulated Radiotherapy For Multiple Brain MetastasesDocument2 pagesWBRT Plus SIB With Image Guided Intensity-Modulated Radiotherapy For Multiple Brain Metastasessanti lestariNo ratings yet
- 68Ga-DOTATATE PET-Based Radiation Contouring Creates More Precise Radiation Volumes For Patients With MeningiomaDocument7 pages68Ga-DOTATATE PET-Based Radiation Contouring Creates More Precise Radiation Volumes For Patients With MeningiomaandresNo ratings yet
- Artigo de Pet No Monitoramento Precoce Do LinfomaDocument7 pagesArtigo de Pet No Monitoramento Precoce Do LinfomagustavoandradeambrosioNo ratings yet
- JCO 2019 MRD Phéno Myélome PDFDocument20 pagesJCO 2019 MRD Phéno Myélome PDFTony HuynhNo ratings yet
- 10.1007@s00259 019 04298 4Document7 pages10.1007@s00259 019 04298 4CamilleNo ratings yet
- The Place of FDG PET CT in Renal Cell Carcinoma - Value and LimitationsDocument7 pagesThe Place of FDG PET CT in Renal Cell Carcinoma - Value and LimitationslkitkatgirlNo ratings yet
- Diffusion Tensor Imaging, Intra-Operative Neurophysiological Monitoring and Small Craniotomy: Results in A Consecutive Series of 103 GliomasDocument11 pagesDiffusion Tensor Imaging, Intra-Operative Neurophysiological Monitoring and Small Craniotomy: Results in A Consecutive Series of 103 GliomasGeneration GenerationNo ratings yet
- Comparison of 18FDGPETCT and 18FFDGPETMR in Head and Neck 2017Document13 pagesComparison of 18FDGPETCT and 18FFDGPETMR in Head and Neck 2017Victor Alfonso Martinez DiazNo ratings yet
- Gandaglia 2018Document9 pagesGandaglia 2018Arlett Karina Juarez RivasNo ratings yet
- Gandaglia2018 PDFDocument9 pagesGandaglia2018 PDFArlett Karina Juarez RivasNo ratings yet
- Clinical Hepatology: AbstractsDocument2 pagesClinical Hepatology: AbstractssmallheartNo ratings yet
- Intra Individual Comparison of 18F PSMA1007 and 18F-FDG PETCT in The Evaluation of Patients With Prostate CancerDocument8 pagesIntra Individual Comparison of 18F PSMA1007 and 18F-FDG PETCT in The Evaluation of Patients With Prostate CancerJoaquín Escobar FloresNo ratings yet
- JCO 2014 Stary 174 84Document12 pagesJCO 2014 Stary 174 84Ljubisa SavicNo ratings yet
- Neuro OncologyDocument10 pagesNeuro OncologylarissaNo ratings yet
- Clinical Impact of FDG PET-CT On Management Decisions For Patients With Primary Biliary TumoursDocument10 pagesClinical Impact of FDG PET-CT On Management Decisions For Patients With Primary Biliary TumourslkitkatgirlNo ratings yet
- Update On Neuroimaging in Brain Tumours: ReviewDocument8 pagesUpdate On Neuroimaging in Brain Tumours: ReviewYo MismoNo ratings yet
- Letter From The Editors - 2023 - Seminars in Nuclear MedicineDocument2 pagesLetter From The Editors - 2023 - Seminars in Nuclear MedicinePuig CozarNo ratings yet
- Pet ManejoDocument9 pagesPet ManejodrmolinammNo ratings yet
- Magnetic Resonance Imaging - 2023 - Zhang - Artificial Intelligence Applications in Glioma With 1p 19q Co Deletion ADocument15 pagesMagnetic Resonance Imaging - 2023 - Zhang - Artificial Intelligence Applications in Glioma With 1p 19q Co Deletion AMarcNo ratings yet
- Prevalence and Outcomes of Cardiac Amyloidosis in All-Comer Referrals For Bone ScintigraphyDocument6 pagesPrevalence and Outcomes of Cardiac Amyloidosis in All-Comer Referrals For Bone ScintigraphyNadia DuarteNo ratings yet
- Association Between A CTGF Gene Polymorphism andDocument8 pagesAssociation Between A CTGF Gene Polymorphism andAhmad ShamyNo ratings yet
- Ugc Carelist Journals 22novDocument7 pagesUgc Carelist Journals 22novnaresh kotraNo ratings yet
- Neurosurg Focus Article PE4Document8 pagesNeurosurg Focus Article PE4emilyNo ratings yet
- Vander Gee STDocument2 pagesVander Gee STWong Wen JianNo ratings yet
- Chemotherapy Response Evaluation in Metastatic Colorectal Cancer With FDG PET/CT and CT ScansDocument6 pagesChemotherapy Response Evaluation in Metastatic Colorectal Cancer With FDG PET/CT and CT ScansBagus OkaNo ratings yet
- Abordaje de Los Nodulos Pulmonares Indeterminados en El Tamizaje de Cancer de Pulmon Estudio Con PET CTDocument6 pagesAbordaje de Los Nodulos Pulmonares Indeterminados en El Tamizaje de Cancer de Pulmon Estudio Con PET CTAnaNo ratings yet
- Protocol SummaryDocument2 pagesProtocol Summaryapi-642376263No ratings yet
- Tropicalmed 05 00112 v4Document22 pagesTropicalmed 05 00112 v4IchaNo ratings yet
- Tropicalmed 05 00112 v4Document22 pagesTropicalmed 05 00112 v4IchaNo ratings yet
- The Solid Core (Trephine) Bone Marrow Biopsy Needle Advantages of Employing A Biopsy Needle With Core Retention DesignDocument5 pagesThe Solid Core (Trephine) Bone Marrow Biopsy Needle Advantages of Employing A Biopsy Needle With Core Retention DesignIchaNo ratings yet
- Tropicalmed 05 00112 v4Document22 pagesTropicalmed 05 00112 v4IchaNo ratings yet
- Medicine: Clinical Trial/Experimental StudyDocument10 pagesMedicine: Clinical Trial/Experimental StudyIchaNo ratings yet
- Pharmaceutics 12 00210 v2Document10 pagesPharmaceutics 12 00210 v2IchaNo ratings yet
- Predicting Frequent Asthma Exacerbations Using BloDocument13 pagesPredicting Frequent Asthma Exacerbations Using BloIchaNo ratings yet
- Tropicalmed 05 00112 v4Document22 pagesTropicalmed 05 00112 v4IchaNo ratings yet
- Peds 2018-3475 FullDocument30 pagesPeds 2018-3475 FullIchaNo ratings yet
- جورنال جاهزDocument4 pagesجورنال جاهزasrd ramiNo ratings yet
- Medicine: Clinical Trial/Experimental StudyDocument10 pagesMedicine: Clinical Trial/Experimental StudyIchaNo ratings yet
- Urine Cathecolamine Levels As Diagnostic Markers For Neuroblastoma in An Defined Population Implication For Ophthalmic PracticeDocument7 pagesUrine Cathecolamine Levels As Diagnostic Markers For Neuroblastoma in An Defined Population Implication For Ophthalmic PracticeIchaNo ratings yet
- Jurnal Hemato 7Document8 pagesJurnal Hemato 7IchaNo ratings yet
- Jurnal Hemato 8Document13 pagesJurnal Hemato 8IchaNo ratings yet
- Comparisons of The Accuracy of Radiation.5Document8 pagesComparisons of The Accuracy of Radiation.5IchaNo ratings yet
- Done - EDITED-HOPE1 - q1 - Mod5 - ObservesPersonalSafetyProtocolDocument21 pagesDone - EDITED-HOPE1 - q1 - Mod5 - ObservesPersonalSafetyProtocolVivencio Pascual JrNo ratings yet
- Handwashing ProposalDocument2 pagesHandwashing ProposalLevyCastilloNo ratings yet
- Road Traffic Accident: Purpose of Medico-Legal InvestigationDocument33 pagesRoad Traffic Accident: Purpose of Medico-Legal InvestigationAmirul AminNo ratings yet
- Enicillin-Like Antibiotics. Diarrhea, Nausea, Vomiting, HeadacheDocument5 pagesEnicillin-Like Antibiotics. Diarrhea, Nausea, Vomiting, HeadachePauline AñesNo ratings yet
- MEMO - RV RTPCR - MergedDocument5 pagesMEMO - RV RTPCR - MergedMukesh KumarNo ratings yet
- Melba Case Scenario FinalDocument34 pagesMelba Case Scenario FinalAlex Antiporda50% (2)
- Katsuura Et Al (2020) Overlapping, Masquerading, and Causative Cervical Spine and Shoulder Pathology2Document14 pagesKatsuura Et Al (2020) Overlapping, Masquerading, and Causative Cervical Spine and Shoulder Pathology2Miguel Jimenez AlvarezNo ratings yet
- Soal Ujian SekolahDocument47 pagesSoal Ujian SekolahClemens JasonNo ratings yet
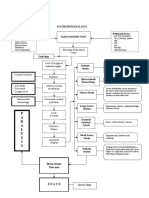
- Pathophysiology: P A R A L Y S I SDocument1 pagePathophysiology: P A R A L Y S I SJordan Garcia AguilarNo ratings yet
- HEALTH-GROUP MEDICLAIM June 2021Document61 pagesHEALTH-GROUP MEDICLAIM June 2021Kishore mohan ManapuramNo ratings yet
- Hyperglycemia Algorithm 2Document1 pageHyperglycemia Algorithm 2damondouglasNo ratings yet
- CHN Health Care Process PDFDocument9 pagesCHN Health Care Process PDFKathleen AngNo ratings yet
- Ingles Parcial Domiciliario 2022Document5 pagesIngles Parcial Domiciliario 2022Macarena zapattaNo ratings yet
- Impaired Posture and MovementDocument40 pagesImpaired Posture and MovementMohamed Magdy ElMeligieNo ratings yet
- Executive Technical Report SHCC 2023Document44 pagesExecutive Technical Report SHCC 2023abdelrahim basheerNo ratings yet
- Family TiesDocument8 pagesFamily TiesCristina Ioana NistorNo ratings yet
- CBC Arikod HoimaDocument37 pagesCBC Arikod Hoimadaniel arikodNo ratings yet
- ECG InterpretationDocument6 pagesECG InterpretationANDREW DEL ROSARIONo ratings yet
- Module 1 in TLE 9 WK 1 2nail CareDocument10 pagesModule 1 in TLE 9 WK 1 2nail CareAdrian AgaNo ratings yet
- 010303A TCCC-MP Tactical Field Care #1 IG 160603Document43 pages010303A TCCC-MP Tactical Field Care #1 IG 160603herralainNo ratings yet
- Life Span Development 16th Edition Santrock Test BankDocument31 pagesLife Span Development 16th Edition Santrock Test Bankbrandoncoletjaxprigfm100% (36)
- Seven Senses Chakra GuideDocument11 pagesSeven Senses Chakra GuidemhliuNo ratings yet
- Nejmoa2035389 ProtocolDocument307 pagesNejmoa2035389 ProtocolRadu FloreaNo ratings yet
- FOLK MEDICINE ExtraDocument22 pagesFOLK MEDICINE ExtraPaul SavvyNo ratings yet
- Covid-19 Ag Rapid Test: OnsiteDocument2 pagesCovid-19 Ag Rapid Test: OnsiteBPG ServiceNo ratings yet
- Falla Cardiaca Consenso 2021Document27 pagesFalla Cardiaca Consenso 2021Medico SantacruzNo ratings yet
- Safety Profile of Rotavac: Observational Prospective StudyDocument7 pagesSafety Profile of Rotavac: Observational Prospective StudyMalook Sekhon100% (1)
- The Art of Surgery: The Strange World of The Placebo ResponseDocument4 pagesThe Art of Surgery: The Strange World of The Placebo ResponseTamsin Athalie NicholsonNo ratings yet
- Handbook of Infant Mental Health Fourth Edition 4th Edition Ebook PDFDocument61 pagesHandbook of Infant Mental Health Fourth Edition 4th Edition Ebook PDFjeffrey.stanton398100% (41)
- 10 Penyakit Terbanyak Di Rawat Jalan Di Puskesmas Provinsi Dki Jakarta TW I Tahun 2019Document9 pages10 Penyakit Terbanyak Di Rawat Jalan Di Puskesmas Provinsi Dki Jakarta TW I Tahun 2019Klinik pratama Iqra' medical centreNo ratings yet