Professional Documents
Culture Documents
Labmed46-0e93 - Case Study 2
Uploaded by
swfsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Labmed46-0e93 - Case Study 2
Uploaded by
swfsCopyright:
Available Formats
Case Studies
Acute Myelogenous Leukemia with Cuplike
Nuclei
Erica Robinson, BS, MLS(ASCP)CM 1* and Carleen Van Siclen, MS, MLS(ASCP)CM 2
Downloaded from https://academic.oup.com/labmed/article/46/4/e93/2937907 by guest on 28 February 2021
Lab Med Fall 2015;46:e93-e97
DOI: 10.1309/LMXC433INJAYLSTD
Clinical History exertion, chest pain, generalized weakness, and malaise, with no other
significant findings.
Patient: 75-year-old white man.
Principle Laboratory Findings: Table 1.
Chief Compliant: Shortness of breath, coughing. After several weeks
with an unrelenting infection and cough, he was referred to the Additional Diagnostic Testing: Flow cytometry and cytogenetic
emergency department by his primary care physician. testing (tachycardia revealed via electrocardiogram [ECG]; chest
X-ray with left pleural effusion; upper right lobe and right middle lobe
History of Present Illness: None reported. pulmonary emboli revealed via computed tomography [CT] angiogram
of chest).
Medical History: Osteoarthritis.
Keywords: acute myelocytic leukemia, acute myeloid leukemia
Family History: Noncontributory.
without differentiation (M1), cuplike nuclei, flow cytometry,
cytogenetics, FLT3 and NPM1 mutation, PML/RARα
Physical Examination: Positive for shortness of breath, dyspnea on
Questions
1. What are the clinically significant laboratory findings for
our patient?
Abbreviations:
2. What do the patient’s peripheral blood smear and bone-
ECG, electrocardiogram; CT, computed tomography; M1, acute myeloid
leukemia without differentiation; WBC, white blood cells; WHO, marrow differential reveal?
World Health Organization; CK-MB, creatine kinase–myocardial band;
CBC, complete blood count; APL, acute promyelocytic leukemia; 3. What is the differential diagnosis?
AML, acute myelocytic leukemia; ALL, acute lymphocytic leukemia;
CD, cluster of differentiation; HLA-DR, human leukocyte antigen–D 4. What do the flow cytometry results reveal?
related; RARα, retinoic acid receptor alpha; FISH, fluorescence in situ
hybridization; PCR, polymerase chain reaction; NPM1, nucleophosmin
5. What other laboratory tests are useful in making a
1; FLT3, FMS-like tyrosine kinase; ITD, internal tandem duplication;
RBC, red blood cells; MCV, mean corpuscular volume; MCH, mean definitive diagnosis?
corpuscular hemoglobin; MCHC, mean cell hemoglobin concentration;
RDW, red blood cell distribution width; MPV, mean platelet volume; PB, 6. What is the patient’s definitive diagnosis, and what
peripheral blood; PT, prothrombin time; INR, International Normalized is the relationship between cuplike nuclei and FLT3 and
Ratio; PTT, partial thromboplastin time; ..., not applicable; Tdt, terminal
deoxynucleotidyl transferase. PML, promyelocytic leukemia; FAB, NPM1 mutations?
French-American-British classification
1
Medical Lab Science, Department of Biology, University of North
Florida Medical Laboratory Science, Jacksonville, FL
Possible Answers
2
Department of Laboratory Medicine and Pathology, Mayo Clinic
College of Medicine, Jacksonville, FL 1. Table 1 demonstrates the patient’s principal laboratory
*To whom correspondence should be addressed. findings. The most clinically significant findings are the
erica.l.robinson22@gmail.com critical laboratory values, including critically high white
www.labmedicine.com Fall 2015 | Volume 46, Number 4 Lab Medicine e93
Case Studies
central pallor that is clefted, indented, folded, or “fish-
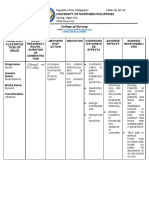
Table 1. Principal Laboratory Findingsa
mouthed,” with loose chromatin and 1 to 3 nucleoli.
Patient
Mehtap et al,2 Kussick et al,3 and Bennett et al4 described
Test Results Reference Interval Interpretation
cuplike nuclei as having a nuclear invagination spanning
Hematology
WBC 354.14 4.50-11.00 x 103/μL Critical
25% or greater of the nuclear diameter and in more than
RBC 3.11 4.30-5.90 x 106/μL L 10% of the blasts. Immunophenotypically, this unusual
Hemoglobin 7.6 13.5-17.5 g/dL L variant is similar to the microgranular variant of acute
Hematocrit 24.6 41.0%-53.0% L promyelocytic leukemia (APL). However, promyelocytes
Downloaded from https://academic.oup.com/labmed/article/46/4/e93/2937907 by guest on 28 February 2021
MCV 85 80-100 fL N
MCH 26.2 25.0-35.0 pg N
do not resemble the blasts because morphologically, they
MCHC 30.8 30.0-37.0 g/dL N have cuplike nuclei.
RDW 19.8 11.5%-15.5% H
Platelets 15 150-450 x 103/μL Critical The bone marrow aspirate and biopsy (Image 2) revealed
MPV 9.5 7.0-11.0 fL N similar cellular distribution and blast morphology (Table
PB Differential
2). We did not perform cytochemical stains.
Neutrophils 1 40%-75% L
Lymphocytes 3 15%-45% L
Bands 2 0-2% N
3. The differential diagnosis includes acute myelocytic
Blasts 94 0% Critical leukemia (AML) and acute lymphocytic leukemia (ALL).
Coagulation Based on the morphology of the blasts, it is difficult
PT 15.5 11.8-15.0 sec H to determine cell lineage. Therefore, we performed
INR 1.2
immunophenotyping by flow cytometry on the peripheral
PTT 30.4 22.9-37.8 sec N
Chemistry blood specimen. The results are displayed in Table 3.
CK-MB 18.4 0-6.3 ng/mL H
Troponin I 4.73 0-.05 ng/mL Critical 4. ALL can be ruled out from the patient’s diagnosis
WBC, white blood cells; L, Low; RBC, red blood cells; MCV, mean corpuscular because of the lack of cell markers for cluster of
volume; N, Normal; MCH, mean corpuscular hemoglobin; MCHC, mean cell differentiation (CD)2, CD3, CD5, CD7, CD8, CD10, CD19,
hemoglobin concentration; RDW, red blood cell distribution width; H, High;
MPV, mean platelet volume; PB, peripheral blood; PT, prothrombin time; INR, CD20, and CD22. The aberrant population of cells
International Normalized Ratio; PTT, partial thromboplastin time; CK-MB, creatinine
kinase–myocardial band.
expresses CD33, whereas a subpopulation expresses
a
Our patient is a 75-year-old white man. CD13. Due to an absence of ALL markers and the
presence of CD33 and CD13, the abnormal cells can be
assigned to the myeloid lineage.
blood cell (WBC) count, critically low platelet count, 94%
blasts in the peripheral blood smear, and critically elevated Table 41,5-8 compares the patient’s immunophenotype
troponin I level. Leukocytosis and thrombocytopenia to the World Health Organization (WHO) classification
accompanied by a finding of 20% or greater blasts is of acute myeloid leukemia (AML) subtypes. The
indicative of acute leukemia, according to the World patient’s immunophenotype is most often observed
Health Organization (WHO) classification.1 Elevated in acute promyelocytic leukemia (APL), in which the
troponin I and creatine kinase–myocardial band (CK-MB) immunophenotypic expression of the abnormal myeloid
levels indicate cardiac muscle damage. The portable chest population is positive for CD33 and negative for human
x-ray and computed tomography (CT) angiogram results leukocyte antigen–D related (HLA-DR) and CD34.1
showed right upper lobe and right middle lobe pulmonary
emboli. However, the electrocardiogram reading was However, APL is typically associated with promyelocytes
normal, revealing no cardiac damage. in the peripheral blood smear. The promyelocytes typically
have heavy granulation and bundles of Auer rods or can
2. The complete blood count (CBC) findings are described be hypogranular with bilobed, angel-winged nuclei.9 APL
in Table 1. The erythrocytes were normocytic and is a subtype of AML characterized by a predominance
normochromic, with moderate anisocytosis. The peripheral of promyelocytes and a diagnostic gene rearrangement,
blood smear revealed approximately 94% blasts. We retinoic acid receptor alpha (PML/RARα).9
observed no Auer rods in the blasts (see Image 1, parts
A-C). The blasts have scant, pale blue-gray, agranular 5. Also, a reference laboratory performed fluorescence
cytoplasm and cuplike nuclei. The cuplike nuclei have a in situ hybridization (FISH) and cytogenetic studies on
e94 Lab Medicine Fall 2015 | Volume 46, Number 4 www.labmedicine.com
Case Studies
Downloaded from https://academic.oup.com/labmed/article/46/4/e93/2937907 by guest on 28 February 2021
Image 1
Acute leukemia as seen in a peripheral blood smear from our
patient, a 75-year-old white man. The smear demonstrates pre-
dominance of blasts, with Auer rods not seen (A; original magni-
fication, ×100); blasts with central indentation (B; original magni-
fication ×1000); and multiple blasts with cuplike nuclei (C; original
magnification, ×1000).
the patient’s bone marrow to differentiate the diagnosis nucleophosmin 1 (NPM1) insertion mutation at position
between APL and another AML subgroup. FISH analysis 959 of exon 12 and negative for FMS-like tyrosine
demonstrated a negative presence for the fusion of kinase (FLT3) mutation. The presence of NPM1 and
promyelocytic leukemia and retinoic acid receptor alpha FLT3 mutations usually co-occur and accompany the
genes (PML/RARα). This fusion is present in approximately variant form of AML that has cuplike nuclei. NPM1 by
97% of patients with APL. Due to a lack of this fusion itself has a positive predictive value of approximately
and a lack of promyelocytes displayed in the patient’s 86%.11 Approximately one-third of adults with AML
peripheral blood and bone-marrow biopsy, APL was thus carry the NPM1 mutation, which is now included in the
excluded from the patient’s diagnosis.10 fourth edition of the World Health Organization (WHO)
classification.5 The immunophenotypes associated with
Further genetic aberrations, NPM1 and FLT3, were this mutation are controversial, but Chen et al11,12 have
investigated. Cytogenetic mutation analysis results discovered in patients with M1 polymorphism who have
via polymerase chain reaction (PCR) were positive for the NPM1 mutation an absence of human leukocyte
www.labmedicine.com Fall 2015 | Volume 46, Number 4 Lab Medicine e95
Case Studies
Table 3. Immunophenotype of Peripheral Blood
via Flow Cytometry
Predominant Approximate %
Variable Reactivity Cells Positive Interpretation
CD3 Mature T cells 0 Negative
CD4 Helper T cells 1 Negative
CD5 T cells 0 Negative
CD7 T cells 1 Negative
Downloaded from https://academic.oup.com/labmed/article/46/4/e93/2937907 by guest on 28 February 2021
CD8 Suppressor T cells 0 Negative
CD10 Common ALL antigen 0 Negative
CD13 Panmyeloid cells 5 Negative (5%+)
CD14 Monocytes 2-3 Negative
CD15 Monocytes 4 Negative (4%+)
Image 2 CD16 Natural killer cells 1 Negative
CD19 Pre-B and B cells 0 Negative
Acute leukemia, as seen in a bone-marrow biopsy smear from our
CD20 B cells 0 Negative
patient, a 75-year-old white man. The smear expresses predomi- CD22 B cells 2 Negative
nantly blasts, which are morphologically similar to those observed CD23 B cells 1 Negative
in the patient’s peripheral blood (original magnification, ×100). CD33 Panmyeloid cells 75 Positive
CD34 Stem cells/blasts 0 Negative
CD36 Monocytes 1 Negative
CD38 General activation/ 46-63 Positive
Table 2. Bone-Marrow Differential in Our plasma cells
Patient, a 75-Year-Old White Man CD45 Total leukocytes 69 Positive
(subpopulation)
Differential % Cells
CD56 Natural killer cells 3 Negative
Blasts 79 HLA-DR … 2 Negative
Granulocytic precursors 17 Tdt … 0 Negative
Lymphocytes 3
CD, cluster of differentiation; ..., not applicable; ALL, acute lymphoblastic leukemia;
Erythrocytes 1 HLA-DR, human leukocyte antigen–D-related; Tdt, terminal deoxynucleotidyl
Segments and bands 0 transferase.
antigen–D related (HLA-DR) and cluster of differentiation less expression of human leukocyte antigen–D related
(CD)34, similar to our patient.13-15 (HLA-DR), and an absence of cluster of differentiation
(CD)34 expression.
6. The definitive diagnosis is acute myeloid leukemia
(AML) without differentiation (M1) with cuplike nuclei. A high correlation of cuplike nuclei and NPM1 mutation
Similarly, Park et al 9 referred to cuplike nuclei as most has been demonstrated by various studies.11-13 NPM1
often occurring in AML M1. Although the relationship mutations are further associated with a normal karyotype,
between cuplike nuclei and nucleophosmin 1 (NPM1) an internal tandem duplication of the FLT3 gene, a higher
and FMS-like tyrosine kinase (FLT3) mutations is highly white blood cell (WBC) count in the peripheral blood,
debated, some studies have demonstrated a correlation a higher fraction of blasts in the bone marrow, lower
with these mutations by themselves or in tandem. expression of CD34 antigen, and female sex.4,9 Many of
Bennett et al4 claim that the NPM1 gene mutation is these characteristics are similar to our patient’s leukemic
the most common genetic alteration in AML. A report expression.
published by the ASCP also reports that as many as
50% to 60% of case individuals with normal karyotypes FLT3-ITD mutations are well documented as being a poor
carry the NPM1 mutation.5 NPM1 encodes for a prognostic indicator rather than a diagnostic factor.5,16
shuttle protein between the nucleolus and cytoplasm, Absence of FLT3-ITD mutations in AML correlates with
which controls cell cycle and regulates centromere an improved outcome.4 NPM1 mutations are favorable
duplication to facilitate mitosis.5 Some studies 4,5,11-13 prognostic indicators in patients with normal karyotypes,
reveal an association of cuplike AML with NPM1 and whereas those with FLT3 mutations have a poor
FLT3–internal tandem duplication (FLT3-ITD) mutations, prognostic factor in AML.9
e96 Lab Medicine Fall 2015 | Volume 46, Number 4 www.labmedicine.com
Case Studies
Table 4. Immunophenotypes Associated with the WHO Classification of AML of Myeloid Origin
Compared with the Patient’s Cuplike AML Varianta
Antigen Markers
AML Group AML Subgroup CD13 CD14 CD15 CD33 CD34 CD36 CD38 CD45 HLA-DR
Patient’s cuplike AML variant +/- - +/- + - - + + -
AML with recurrent APL, AML with PML/RARα, and variants + - - + - - - + -
genetic abnormalities (FAB M3)
Downloaded from https://academic.oup.com/labmed/article/46/4/e93/2937907 by guest on 28 February 2021
AML not otherwise AML minimally differentiated (FAB M0) + - - + + - - + +
categorized
AML without maturation (FAB M1) + - - + + - - + +
AML with maturation (FAB M2) + - + + v - - + V
Acute myelomonocytic leukemia (FAB M4) + + + + v + - + -
WHO, World Health Organization; AML, acute myeloid leukemia; CD, cluster of differentiation; HLA-DR, human leukocyte antigen–D-related; APL, acute promyelocytic leukemia;
PML, promyelocytic leukemia; RARα, retinoic acid receptor alpha; FAB, French-American-British classification; V, variable.
7. Nguyen DT, Diamond LW, Braylan RC. Flow Cytometry in
Hematopathology: A Visual Approach to Data Analysis and
Acknowledgments Interpretation. Totowa, NJ: Humana Press; 2002:187-191.
8. Ismail MA, Hosny SM. Prognostic significance of progenitor
We thank Mark Steciuk, MD, PhD, of, Jacksonville cell markers in acute myeloid leukemia. Life Science Journal.
2011;8(4):680-686.
Pathology Consultants for providing photography and
9. Park BG, Chi H-S, Jang S, et al. Association of cup-like nuclei in
mentoship. blasts with FLT3 and NPM1 mutations in acute myeloid leukemia.
Ann Hematol. 2013;92:451-457.
10. Dekking EHA, van der Velden VHJ, Varro R, et al. Flow cytometric
immunobead assay for fast and easy detection of PML-RARA fusion
proteins for the diagnosis of acute promyelocytic leukemia. Leukemia.
References 2012;26:1976-1985.
11. Chen W, Konoplev S, Medeiros J, et al. Cuplike nuclei (prominent
1. McKenzie SB, Williams JL. Clinical Laboratory Hematology, 2nd nuclear invaginations) in acute myeloid leukemia are highly associated
edition. Upper Saddle River, NJ: Pearson Education. 2010:505-523. with FLT3 internal tandem duplication and NPM1 mutation. Cancer.
2009;115:5481-5489.
2. Mehtap O, Atesoglu E, Gonullu E, Keski H, Hacihanefioglu A. Are
cup-like blasts specific to AML patients with FLT3 ITD and a normal 12. Chen W, Rassidakis GZ, Li J, et al. High frequency of NPM1
karyotype? An ALL case report and review of the literature. Turk J gene mutations in acute myeloid leukemia with prominent nuclear
Hematol. 2011;28:142-145. invaginations (“cuplike” nuclei). Blood. 2006;108:1783-1784.
3. Kussick SJ, Stirewalt DL, Yi HS, et al. A distinctive nuclear 13. Kroschinsky FP, Schakel U, Fischer R, et al. Cup-like acute myeloid
morphology in acute myeloid leukemia is strongly associated with leukemia: new disease or artificial phenomenon? Haematologica.
loss of HLA-DR expression and FLT3 internal tandem duplication. 2008;93:283-286.
Leukemia. 2004;18:1591-1598. 14. Liu Y-R, Zhu H-H, Ruan G-R, et al. NPM1-mutated acute
4. Bennett JM, Pryor J, Laughlin TS, Rothberg PG, Burack WR. Is myeloid leukemia of monocytic or myeloid origin exhibit distinct
the association of “cup-like” nuclei with mutation of the NPM1 immunopheotypes. Leuk Res. 2013;37:737-741.
gene in acute myeloid leukemia clinically useful? Am J Clin Pathol. 15. Syampurnawati M, Tatsumi E, Ardianto B, et al. DR negativity is a
2010;134:648-652. distinctive feature of M1/M2 AML cases with NPM1 mutation. Leuk
5. Foucar K, Reichard K, Czuchlewski D. Chapter 18: Acute Myeloid Res. 2008;32:1141-1143.
Leukemia. ASCP website. http://www.ascp.org/PDF/Books/ 16. Port M, Böttcher M, Thol F, et al. Prognostic significance of FLT3
Chapter-18.pdf. Accessed September 21, 2015. internal tandem duplication, nucleophosmin 1, and CEBPA gene
6. Jaffe E, Harris N, Stein H, Vardiman J. World Health Organization mutations for acute myeloid leukemia patients with normal karyotype
Classification of Tumours: Pathology and Genetics, Tumours of and younger than 60 years: a systematic review and meta-analysis.
Haematopoietic and Lymphoid Tissues. Lyon, France. IARC Press. Ann Hematol. 2014;93(8):1279-1286.
2001:77-95.
www.labmedicine.com Fall 2015 | Volume 46, Number 4 Lab Medicine e97
You might also like
- Tutors Short Cases 1 8 With Answers 2018Document5 pagesTutors Short Cases 1 8 With Answers 2018RayNo ratings yet
- CH 19 Nursing Care of Patients With Immune System DisordersDocument2 pagesCH 19 Nursing Care of Patients With Immune System DisordersZachary T Hall0% (1)
- Case Study For OligohydramniosDocument7 pagesCase Study For Oligohydramniosbjhilario86% (14)
- Labmed46 0e82Document6 pagesLabmed46 0e82FairysparklesNo ratings yet
- Chronic Lymphocytic LeukemiaDocument4 pagesChronic Lymphocytic LeukemiaSantiago López JosueNo ratings yet
- Neutrophilic Leukocytosis, Neutropenia, Monocytosis, and MonocytopeniaDocument7 pagesNeutrophilic Leukocytosis, Neutropenia, Monocytosis, and MonocytopeniaRom ÁlvNo ratings yet
- Ajcpath117 0041Document10 pagesAjcpath117 0041Marco Aurélio SartoriNo ratings yet
- 72_Progressive multifocal leukoencephalopathy in an immunocompetent patientDocument7 pages72_Progressive multifocal leukoencephalopathy in an immunocompetent patientFaras ArinalNo ratings yet
- Case Studies: Recurrent Fever, Chills, and Malaise in A 53-Year-Old ManDocument2 pagesCase Studies: Recurrent Fever, Chills, and Malaise in A 53-Year-Old Mansreeja maragoniNo ratings yet
- CHAPTER-17 NUERO MergedDocument17 pagesCHAPTER-17 NUERO MergedRyn ShadowNo ratings yet
- LNH T PerifericoDocument10 pagesLNH T PerifericopasqualijNo ratings yet
- Leukemia Pada AnakDocument33 pagesLeukemia Pada AnakandrianNo ratings yet
- Acute Lymphoblastic Leukemia Treatment RegimensDocument14 pagesAcute Lymphoblastic Leukemia Treatment RegimensPrashant PandeyNo ratings yet
- Myeloproliferative Neoplasms: Diagnostic Workup of The Cythemic PatientDocument9 pagesMyeloproliferative Neoplasms: Diagnostic Workup of The Cythemic PatientHashim AhmadNo ratings yet
- Aberrations of MYC Are A Common Event in B-Cell Prolymphocytic LeukemiaDocument9 pagesAberrations of MYC Are A Common Event in B-Cell Prolymphocytic LeukemiaRafa AssidiqNo ratings yet
- International Consensus Classification of Myeloid and Lymphoid Neoplasms: Myeloproliferative NeoplasmsDocument16 pagesInternational Consensus Classification of Myeloid and Lymphoid Neoplasms: Myeloproliferative NeoplasmswidweedNo ratings yet
- Clinical Utility of The Band CountDocument36 pagesClinical Utility of The Band CountSergio Alejandro Perez SolisNo ratings yet
- Hom 3Document7 pagesHom 3Mira SrikandiNo ratings yet
- 10 11648 J CRJ 20200802 14Document3 pages10 11648 J CRJ 20200802 14Marj MendezNo ratings yet
- 2020 case report DLBCL CD56Document9 pages2020 case report DLBCL CD56maomaochongNo ratings yet
- 02 ESMO mdx219Document11 pages02 ESMO mdx219Ayten ShirinovaNo ratings yet
- Isolated CNS Relapse in Favourable Acute Myeloid Leukemia Presenting As Cerebello-Pontine Angle TumorDocument3 pagesIsolated CNS Relapse in Favourable Acute Myeloid Leukemia Presenting As Cerebello-Pontine Angle TumorInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bone Marrow Manifestation of Plasmablastic Transformation of Chronic Lymphocytic Leukemia: A Case ReportDocument5 pagesBone Marrow Manifestation of Plasmablastic Transformation of Chronic Lymphocytic Leukemia: A Case ReportTomasz GórskiNo ratings yet
- Nk-Cell Lymphomas of The Head and Neck: AuthorDocument8 pagesNk-Cell Lymphomas of The Head and Neck: AuthorCharmila SariNo ratings yet
- Chronic Myeloid Leukaemia: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDocument11 pagesChronic Myeloid Leukaemia: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpEdwin HadinataNo ratings yet
- Care Plan 3Document30 pagesCare Plan 3Chelsea RuthrauffNo ratings yet
- Alperovich Et Al. - 2015 - Composite Angioimmunoblastic T-Cell and Diffuse Large B-Cell Lymphoma PDFDocument2 pagesAlperovich Et Al. - 2015 - Composite Angioimmunoblastic T-Cell and Diffuse Large B-Cell Lymphoma PDFflashjetNo ratings yet
- Clinical Features of 37 Cardiac Lymphoma CasesDocument13 pagesClinical Features of 37 Cardiac Lymphoma CasesEmirza Nur WicaksonoNo ratings yet
- Neuroasia 2017 22 (1) 015Document9 pagesNeuroasia 2017 22 (1) 015Mazin Al-TahirNo ratings yet
- Tutorial: Section A: Multiple Choice Question (Mcqs T/F)Document7 pagesTutorial: Section A: Multiple Choice Question (Mcqs T/F)Harith AsriNo ratings yet
- Hoelzer, 2016Document14 pagesHoelzer, 2016ValentinaNo ratings yet
- Educational Case: Differentiating Thrombotic Thrombocytopenic Purpura From Other Thrombotic Microangiopathies and Potential Role of The SpleenDocument8 pagesEducational Case: Differentiating Thrombotic Thrombocytopenic Purpura From Other Thrombotic Microangiopathies and Potential Role of The SpleenL ANo ratings yet
- Chaves 2005 PDFDocument5 pagesChaves 2005 PDFWa Nur Arlin RahmadhantyNo ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- Chronic Myeloid Leukemia A Case of ExtremeDocument3 pagesChronic Myeloid Leukemia A Case of ExtremeTumbuh KembangNo ratings yet
- Acute Lymphoblastic Leukemia: John Han-Chih Chang Matthew M. Poppe Chia-Ho Hua Karen J. Marcus Natia EsiashviliDocument7 pagesAcute Lymphoblastic Leukemia: John Han-Chih Chang Matthew M. Poppe Chia-Ho Hua Karen J. Marcus Natia EsiashviliErvanda ZilmiNo ratings yet
- 1150-6162-2-PBDocument10 pages1150-6162-2-PBbella friscaamaliaNo ratings yet
- 722Document7 pages722Cimaie JellyNo ratings yet
- White Paper CPD Sepsis AJCP 2005Document5 pagesWhite Paper CPD Sepsis AJCP 2005jtmchughNo ratings yet
- Muto 2020Document5 pagesMuto 2020pamela queirozNo ratings yet
- Review Series: LGL Leukemia: From Pathogenesis To TreatmentDocument13 pagesReview Series: LGL Leukemia: From Pathogenesis To Treatmentelvis9952No ratings yet
- Burkitts Lymphoma 2015 PDFDocument9 pagesBurkitts Lymphoma 2015 PDFAffra CahyoNo ratings yet
- Study of Correlation Between Imatinib Mesylate Plasma-LinkDocument7 pagesStudy of Correlation Between Imatinib Mesylate Plasma-LinkIvonne Mercedes Gutierrez AtapaucarNo ratings yet
- B-Cell FlowDocument9 pagesB-Cell FlowDaryl FootNo ratings yet
- Q&A OsloDocument9 pagesQ&A OslosyukriNo ratings yet
- Recomendation Deep Molecular ResponsesDocument5 pagesRecomendation Deep Molecular ResponsesRAFANo ratings yet
- Summary of Recent Significant Findings in ME-CFS Research - Updated February 2019 PDFDocument21 pagesSummary of Recent Significant Findings in ME-CFS Research - Updated February 2019 PDFEmilie ChateletNo ratings yet
- AbdfDocument9 pagesAbdfXONNo ratings yet
- Veterinary Clinical Pathology Journal Study of Canine Hematopoietic Neoplasia ImmunophenotypingDocument11 pagesVeterinary Clinical Pathology Journal Study of Canine Hematopoietic Neoplasia ImmunophenotypingJL EulefiNo ratings yet
- Burger 2003Document5 pagesBurger 2003Atria DewiNo ratings yet
- N MZLDocument17 pagesN MZLsnap kingNo ratings yet
- 74 Year Old Woman With Fatigue, Anorexia, and AbdoDocument6 pages74 Year Old Woman With Fatigue, Anorexia, and AbdoRamiro Arraya MierNo ratings yet
- Lupus NefritisDocument13 pagesLupus Nefritisejonhe07No ratings yet
- Management of Acute LeukemiaDocument11 pagesManagement of Acute LeukemiaNicoletta ColomboNo ratings yet
- Cancer - 2004 - Li - Treatment Outcome and Pattern of Failure in 77 Patients With Sinonasal Natural Killer T Cell or T CellDocument10 pagesCancer - 2004 - Li - Treatment Outcome and Pattern of Failure in 77 Patients With Sinonasal Natural Killer T Cell or T Cell2512505993No ratings yet
- Hairy Cell Leukemia-VariantDocument3 pagesHairy Cell Leukemia-VariantInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- American J Hematol - 2006 - Takahashi - Methylprednisolone Pulse Therapy For Severe Immune Thrombocytopenia Associated WithDocument5 pagesAmerican J Hematol - 2006 - Takahashi - Methylprednisolone Pulse Therapy For Severe Immune Thrombocytopenia Associated WithMohan PrasadNo ratings yet
- How We Treat NK/T-cell Lymphomas: Review Open AccessDocument13 pagesHow We Treat NK/T-cell Lymphomas: Review Open AccessRucelia Michiko PiriNo ratings yet
- Guidelines For The Management of Mature T-Cell and NK-cell Neoplasms - Brit J Haem 2011Document35 pagesGuidelines For The Management of Mature T-Cell and NK-cell Neoplasms - Brit J Haem 2011José Antonio Alarcón LeónNo ratings yet
- Hematology Discussion 2011 KPBDocument10 pagesHematology Discussion 2011 KPBtufis02No ratings yet
- Chronic Lymphocytic LeukemiaFrom EverandChronic Lymphocytic LeukemiaMichael HallekNo ratings yet
- Immunosero: Experiment # 1 - Preparation of Red Cell Suspension (Pg. 13-14)Document8 pagesImmunosero: Experiment # 1 - Preparation of Red Cell Suspension (Pg. 13-14)swfsNo ratings yet
- Labmed42-0644 Case Study 3Document5 pagesLabmed42-0644 Case Study 3swfsNo ratings yet
- Choreographer Wilson Regrets 'Transformative' Kim's Early Retirement - The Japan TimesDocument4 pagesChoreographer Wilson Regrets 'Transformative' Kim's Early Retirement - The Japan TimesswfsNo ratings yet
- Bhagavad GitaDocument2 pagesBhagavad GitaswfsNo ratings yet
- Bhagavad GitaDocument2 pagesBhagavad GitaswfsNo ratings yet
- Titration Level 2 LabnotebookDocument1 pageTitration Level 2 LabnotebookswfsNo ratings yet
- Bhagavad GitaDocument2 pagesBhagavad GitaswfsNo ratings yet
- Entrep B2B and B2CDocument3 pagesEntrep B2B and B2CswfsNo ratings yet
- Li Wor RizDocument1 pageLi Wor RizswfsNo ratings yet
- NCP For Pain - Rheumatoid ArthritisDocument5 pagesNCP For Pain - Rheumatoid Arthritisveorjan100% (1)
- Papila DentalDocument6 pagesPapila DentalFedor Rivas MedinaNo ratings yet
- Clinical Case Reports - 2020 - Oliveira - A Normal Motor Development in Congenital Hydrocephalus After Cuevas MedekDocument4 pagesClinical Case Reports - 2020 - Oliveira - A Normal Motor Development in Congenital Hydrocephalus After Cuevas MedekRonaldo Angel VelásquezNo ratings yet
- Wheeless' Textbook of OrthopaedicsDocument6 pagesWheeless' Textbook of Orthopaedicsnurul auliaNo ratings yet
- Allergic Disease: Prof. Rusudan Karseladze Iv. Javakhishvili Tbilisi State University Institute of PediatricsDocument144 pagesAllergic Disease: Prof. Rusudan Karseladze Iv. Javakhishvili Tbilisi State University Institute of PediatricspalNo ratings yet
- Total Shoulder Arthroplasty, An Overview, Indicatins and Prosthetic OptionsDocument4 pagesTotal Shoulder Arthroplasty, An Overview, Indicatins and Prosthetic OptionsYafiahnaf FirdausNo ratings yet
- Juvenile Idiopathic Arthritis (JIA) : Prof Deepthi SamarageDocument20 pagesJuvenile Idiopathic Arthritis (JIA) : Prof Deepthi SamarageTrishenth FonsekaNo ratings yet
- (Kearney & Albano 2004) The Functional Profiles of School Refusal BehaviorDocument15 pages(Kearney & Albano 2004) The Functional Profiles of School Refusal BehaviorHana Lazuardy RahmaniNo ratings yet
- Grade 8 Science Unit 4: "Cells, Tissues, Organs & Organ Systems"Document26 pagesGrade 8 Science Unit 4: "Cells, Tissues, Organs & Organ Systems"api-238589602No ratings yet
- Naplex 1Document7 pagesNaplex 1baniyoNo ratings yet
- The Process of PhlebotomyDocument102 pagesThe Process of PhlebotomyCatherine Merilleno100% (1)
- Objectives and PoaDocument2 pagesObjectives and PoaALIZA BAKILNo ratings yet
- OSCE OphthalmologyDocument15 pagesOSCE OphthalmologyHuzaifa Asif100% (1)
- Natural Cancer Remedies That WorkDocument48 pagesNatural Cancer Remedies That WorkAlessio Anam100% (1)
- CASE REPORT Laser-Assisted Treatment of SialolithiasisDocument2 pagesCASE REPORT Laser-Assisted Treatment of SialolithiasisPeter SalimNo ratings yet
- Erythroblastosis FetalisDocument3 pagesErythroblastosis FetalissolegrinNo ratings yet
- Test Blueprinting II: Creating A Test BlueprintDocument10 pagesTest Blueprinting II: Creating A Test BlueprintDr. Doaa El MorsiNo ratings yet
- Signs and Symptoms of Chest InfectionsDocument10 pagesSigns and Symptoms of Chest InfectionsHussain MirzaNo ratings yet
- Tacata Angeline B. Drug Study For Pt. Supnet J.Document4 pagesTacata Angeline B. Drug Study For Pt. Supnet J.Melrhean GraceNo ratings yet
- Geriatric Pharmacotherapy PDFDocument6 pagesGeriatric Pharmacotherapy PDFverry aswardsNo ratings yet
- Peri ImplantitisDocument12 pagesPeri ImplantitisbobNo ratings yet
- CryotherapyDocument15 pagesCryotherapychaitrareddyNo ratings yet
- Linee Guida Per La Rianimazione Cardiopolmonare Nel Cane e Nel GattoDocument13 pagesLinee Guida Per La Rianimazione Cardiopolmonare Nel Cane e Nel GattoFrancesco NaniaNo ratings yet
- Factors Modifying Drug EffectsDocument47 pagesFactors Modifying Drug EffectsRiddhi Jain100% (1)
- Astro Diagnosis VirgoDocument42 pagesAstro Diagnosis VirgoOvn Murthy100% (1)
- Science: Members:Mikhaila Tunguia Jean R. Bongcawil Kirt Jon Bait-ItDocument10 pagesScience: Members:Mikhaila Tunguia Jean R. Bongcawil Kirt Jon Bait-ItJean BongcawilNo ratings yet
- Skripsi Tanpa Bab PembahasanDocument65 pagesSkripsi Tanpa Bab PembahasanTondi Rosalinda SinagaNo ratings yet
- The Effects of Hypoalbuminaemia On Optimizing.3Document12 pagesThe Effects of Hypoalbuminaemia On Optimizing.3ismaelito22No ratings yet