Professional Documents
Culture Documents
Methods Substrate End Products:: Pyridoxal Phosphate
Uploaded by
MUNDER OMAIRA NASRA D.Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Methods Substrate End Products:: Pyridoxal Phosphate
Uploaded by
MUNDER OMAIRA NASRA D.Copyright:
Available Formats
Liver enzymes
Liver function tests
Liver function Liver function tests rationale
Synthetic function - TPAG total protein albumin Test measuring hepatic synthetic function because liver produce proteins, lipoproteins, clotting
- PT prothrombin time because of the clotting factors enzymes, carbohydrates.
factors
Conjugation and excretion - Bilirubin the ability of the liver to metabolized bilirubin
- Urobilinogen
Detoxification - Enzymes like ALP, aminotransferases, 5’N, Used to assess the extent of liver damage
- Liver is a gatekeeper because GGT, LDH - any injury of the liver can lead to liberation of enzyme
it determines if it can be - Ammonia; protein catabolism result or Cytolysis and necrosis
released or not. outcome and it’s very toxic that’s why it’s Differentiate hepatocellular from obstructive disease
converted to urea (non-toxic and can easily be - hepatocellular means that the problem is the hepatocytes (cells from the liver) and
eliminated via kidneys) pertain to functional disorder
Increase ammonia in the blood means - obstructive is mechanical, it may be in the form of gallstones, tumor
problem in the liver
- OCT (liver marker but not commonly
performed)
- Aminotransferases : AST and ALT
No storage function test
Methods Substrate End products OTHER METHODS USED IN ALP DETERMINATION
OBodansky Beta-glycerophosphate Inorganic PO4 + glycerol
Shinowara Same Same
Liver enzyme
Jones Characteristics
Same Same Clinical significance Methods of determination Laboratory Considerations
Reinhart - Catalyzes theSame
same catalytic reaction 1. hepatic disorders
Same o Karmen method 1. Serum or heparinized
ALTKing
alanine
and Armstrong with AST where it transfer an amino
Phenylphosphate InPhenol
almost all of the liver diseases ALT plasma free from
aminotransferase
Bessy, Lowry, and Brock group p-nitro
the onlyphenyl
difference
PO4 is that it’s will
p-nitrophenol also
orelevate.
yellow hemolysis
alanine while in AST is aspartate nitrophenoxide: acute
↑ levels ion inflammatory
OldBowers
name SGPT
and McComb - Cofactor: pyridoxal
Same phosphate (co- condition
Same of the liver 2. Aminotransferases are
serum glutamic factor in amino transferases) present in human plasma,
Huggins Talalay Phenolpthalein diphosphate Phenolphthalein red 1st reaction is the catalytic reaction of the
pyruvic - Major tissue source: liver (liver specific ↑ levels of ALT and AST are seen in bile, CSF and saliva
Moss Alpha napthol PO4 Alpha-naphtol PO4 ALT by which catalyzes the transfer of amino
transaminase enzyme) hepatocellular disorders compared - Running enzyme test for
Klein, babson & read Buffered phenolphthalein Free phenolphthalein group from alanine to a-ketoglutarate
- Minor tissue source: kidney pancreas, to extra/intra hepatic obstruction aminotransferases (ALT,
PO4 producing pyruvate and glutamate
EC 2.6.1.2 RBC, heart, lungs and skeletal muscle - Remain elevated for up to 2-6 AST, Amylase) mask
weeks 2nd reaction the oxidation reduction of NADH should be wear to avoid
Reference value: - Easily detectable to NAD will now be measure. false elevation
6-37 U/L AST/ SGOT ALT/ SGPT o The increase in absorbance of the 3. Vitamin B6
Major organ Heart Liver 2. used to screen blood donors oxidation of NADH to NAD is directly - Vit B6 deficiency patient
affected screen blood donors; not proportional to the activity of the will have falsely low or
Substrate Aspartic alpha Alanine alpha practiced in the Philippines ALT normal ALT because Vit.
ketoglutaric katoglutaric usually analyzed are the o 340 nm B6 is the pyridoxal
acid acid transfusion transmittable o 37°C phosphate which is the
End Glutamic Glutamic infections such as HIV, Hepa cofactor
products acid+ acid+ pyruvic C & A, syphilis and malaria Reitman- Frankel - if absence of cofactor thus
oxaloacetic acid In US ALT is included in Coupled enzymatic reaction slow enzyme reaction
acid screening for the blood 4. Certain drugs and alcohol
Color 2,4 DNPH Same donors as mandated by the may also increase ALT
developer IMCC because ALT is a good activity
Color 0.4N NaOH Same marker for post-transfusion 5. Stability of the enzyme
intensifier hepatitis; if high ALT si donor, activity can be maintained
Methods Reitman and Reitman and thus not qualified by refrigeration of the
frankel, frankel o the change of the absorbance of sample up to 3 days and
karmen freezing the sample for up
colored complex (brown) is to be
measured to 30 days
o The activity of the colored complex is
directly proportional to the ALT
activity.
o 500 nm
Liver Characteristics Clinical significance Methods of determination Laboratory Considerations
enzyme
Catalytic reaction: liberate 1. Evaluation of hepatobiliary disorder 1. Electrophoresis (cathode-anode) - Hemolysis
ALP the inorganic phosphate ion Disorder either in the liver, gallbladder, bile - Liver (fastest) , bone, placenta, and intestine - Serum or heparinized plasma less
Alkaline from the organic duct (slowest) than 3 hours old
phos phosphomonoester via in obstruction: high ALP - Most useful but liver and bone are way too The more mag stand, the
phatase hydrolysis producing alcohol Run together with other enzymes to close, thus difficult to differentiate more mag increase ang pH
EC 3.1.3.1 the catalytic differentiate of its hepatic or fsorder. just add lectin (wheat germ) or the more ma active si ALP
reaction Neuraminidase to improve the - Anticoagulants that remove calcium
happens in 2. Evaluation of bone disorder (Pagets disease) separation of liver and bone and magnesium will prevent produc
pH 9-10 MAJOR ISOENZYMES 2. Heat fractional/stability test formation
that’s why - Liver ALP - 56 C for 10 mins False low
alkaline o Found in biliary duct - Placenta (most heat stable because it can - Lipids, hemoglobin or bilirubin
- Nonspecific enzyme - Bone ALP resist denaturation up to 65 up to 30 mins C) interference
- It can react with a o It takes part in the transport of - intestine, liver and; These can be also absorbed light
number of substrate calcium - bone ( unstable; labile first one to denature in @405 nm
- Activator: o Found in osteoclast; in 56C for 10 mins) - Fasting
magnesium children/older; ALP is higher bc of 3. Chemical inhibition test Ideal if fasting because in intestinal
- ALP contains zinc osteoclastic activity - Phenylalanine – inhibit placenta isoenzyme ALP isoenzyme, after a meal mo
- Major: intestine, - Placental ALP and intestine isoenzyme, and raegan & nagao increase. Thus, false increase
liver, bone, placenta o Detected in pregnant women at the same time.Most common isoenzyme - Temp sensitive
- Isoenzymes are starting from 16-20 weeks after - Synthetic urea –is used to inhibit bone At 4°C false increase ALP
named kung aha sila pregnancy then persist all isoenzyme - Zinc deficiency
nagkita nga organ throughout the pregnancy and will - Levamisole –inhibit liver and bone isoenzyme False low
normalize 3-6 days after nanganak 4. Bower and Mc Comb Hypophosphatasia –genetic disorde
- Intestinal ALP wherein there’s abnormal
o Dependent on the blood group B/O development in the bones and
has higher concentration of - Reaction is based on the breakdown of para- teeth. Low ALP
intestinal ALP than A/AB. Same with nitrophenylphosphate (colorless) because of Low ALP is also found in patients
placental ALP hydrolysis that liberates p-nitrophenol after blood transfusion
o Also involved in the transfer of lipids (yellow) and phosphate ion The ALP tests can be inhibited by
Carcino-placental isoenzyme - p-nitrophenol (yellow) the absorbance is phosphorus
- Carcino because these isoenzymes occur measured at 405 nm Additional information: Placental ALP is a
when there’s neoplasm (active cell division the increase in absorbance of the good tumor marker for germ cell tumor. If
common in cancer) like: liberated p-nitrophenol directly patient is pregnant it’s expected that high
Regan- lung, breast ovarian, and colon CA proportional is to the ALT activity placental ALP.
Nagao –pancreas and bile duct CA - pH 10.15
metastatic CA
Liver enzyme Characteristics Clinical significance Methods of determination Laboratory Considerations
GGT Gamma - Catalytic reaction: 1. evaluation of liver damage; 1. Szass, Rosalki & Tarrow,
Glutamyltransferase Transfers itself to 2. detection of alcoholism; and Orlowski Gamay ra because
amino acids, other 3. the monitoring of alcohol intake by patients o Substrate: gamma- GGT is stable
EC 2.3.2.2 peptides or water - If nag abstain si patient, then GGT will normalize glutamyl-p-nitroanilide Not affected by
molecules after 2-3 weeks o Reaction: when the hemolysis
Reference value: - Distribution: kidney, - In all hepatobiliary disorder, GGT will increase; enzyme acted upon the Can be refrigerated
brain, phosphate, most sensitive liver assay. It may be obstruction substrate it will convert @ 4°C
Male : 6-45 U/L pancreas, and liver (higher elevation) / functional to glycylglycine that
Female: 5-30 U/L - For the patient that’s taking enzyme inducing liberates p-nitroaniline
- Low because female drugs such as phenytoin, barbital, and warfarin. o Product: p-nitroaniline
has estrogen and Will lead to increase in GGT not because of liver o Chromogenic product
progesterone that damage but bc of induction of GGT o Absorbance will be
may suppress the GGT man gud is canaliculi of the liver cells measured at 405 – 420
activity of GGT particularly in the smooth ER. Any nm
mitochondrial induction, will trigger the o Method of testing: end-
GGT’s activity that will lead to false point (only one), fixed
increase time, kinetic or
- GGT is also elevated in Acute Pancreatitis, diabetes continuous (several
mellitus, prostatic disorder absorbance reading)
- In AMI, GGT will also increase for unknown reason
- It is also useful in differentiating the cause of ALP
increase:
ALP GGT
Liver Increase Increase
Bone Increase Decrease
5’ Nucleotidase - A phosphoric 1. Hepatobiliary disease - Dixon and Purdon,
monoester hydrolase 2. Also a marker for infiltrative lesions of the liver Campbell, Goldberg
EC 3.1.3.5 - Predominantly - Also increase in cholestasis. Na stuck or minimized
secreted in the liver production of the bile
Reference value: 0-1.6 U/L - Also help to differentiate between the liver and
bone problem in ALP. Just as the same with GGT
Other clinically Characteristics Clinical significance Isoenzymes Laboratory Considerations
significant
enzymes
ACP Acid - Catalyze same reaction as ALP but active at - Significant levels found in: RBC and Band 1 (B1) - Free from hemolysis because B3 is
phosphatase pH 5 platelet. In adult men, 50% found in - found in found in RBC
prostate gland prostate - Decreases when left at Room
EC 3.1.3.2 Methods Substrate End products - One of its diagnostic value is for Band 2 (B2) Temperature
Gutman Phenyl PO4 Inorganic PO4 detecting prostatic cancer or the - found in WBC - If left at RT for 1-2 hrs., decrease
and recurrence of the Prostatic CA particularly in because the pH will increase thus,
↑ in : thrombocytopenia, problems in the granulocytes became an alkaline pH and ACP is
gutman bone associated with osteoclastic activity, Band 3 (B3) not physiologically active in
Shinowar PNPP p-nitrophenol hemolytic anemias - Found in PLT, alkaline pH
a - Aid in detecting: RBC and - Serum should be frozen or acidify
Babson, Alpha naphthyl Alpha-naphthol metastatic CA monocytes - Prostatic ACP (B1) is inhibited by L-
Read & PO4 (best if other types of CA Band 4 (B4) tartrate ions
Phillips kinetic) bone disease - same as B2 - RBC ACP (B3) is inhibited by
Roy and Thymolphthalein Free forensic (rape cases) Band 5 (B5) formaldehyde
Hillman monophosphate thymolphthalein Because it’s also found in semen. It - found in - TRAP : tartrate resistance ACP so
(best if end- can persist after 4 days after vaginal osteoclast not affected by inhibitions
point) washing, so detectable Present in people having leukemia,
- Nonspecific enzyme, different lymphomas
substrate Elevated serum bilirubin can cause a
falsely low TRAP
MINOR ENZYMES
Aldolase Catalytic reaction: Splits fructose
- EC 4.1.1.13 Three isoenzymes
ALD A –Skeletal muscle
ALD B –WBC , liver, kidney
ALD C –brain tissue
- Clinical significance: increase in problems in skeletal muscle, hepatic diseases, hemolytic anemia, leukemia
Pseudocholinesterase MAJORITY is in Liver and also liver myocardial endo-pancreas
EC 3.1.1.8 - But not a liver enzyme because it reflects more on the synthetic function rather than the detoxification function (assessed by the liver enzyme).
More of a marker for insecticide poisoning
Decrease in acute hepatitis, cirrhosis, carcinoma & malnutrition
ACE - Convert angiotensin I to angiotensin II
Angiotensin-converting - Monitoring and diagnosis of sarcoidosis: abnormal collection of inflammatory cells
enzyme - EC 3.4.15.1
Ceruplasmin Marker for Wilson’s disease: genetic disorder wherein there’s excess storage of copper that ables to lodge to the eyes and brain
Copper carrying protein
Orthinine Carbamoyl - Marker for hepatobiliary diseases
Transferase
G-6-PD o Catalytic reaction: it functions to maintain/ suppress the activity of NADPH in the RBC
o Part of newborn screening
EC 1.1.1.49 o If failure to produce G-6-PD enzyme there might be a problem in the RBC, spleen, adrenal cortex and lymph nodes
o G-6-PD deficiency will lead to hemolysis
o Increase in AMI and megaloblastic anemia
You might also like
- CC - Liver FunctionDocument5 pagesCC - Liver FunctionOrhan AsdfghjklNo ratings yet
- GC Toxicology Case Studies Apr 28 2013Document36 pagesGC Toxicology Case Studies Apr 28 2013Grace Anastasia Ginting SinusingaNo ratings yet
- Montalban-Cc2 Lec EaDocument5 pagesMontalban-Cc2 Lec Eakimmynemil80No ratings yet
- Lesson 5. Enzymology2-LmsDocument14 pagesLesson 5. Enzymology2-LmsJohanna MarieNo ratings yet
- Clinical Enzymology: Enzyme Classification and NomenclatureDocument27 pagesClinical Enzymology: Enzyme Classification and NomenclaturePatrick DazaNo ratings yet
- LABORATORY - ALP DeterminationDocument2 pagesLABORATORY - ALP DeterminationTrisha GarciaNo ratings yet
- 31 Greene Liver LM 428 2017Document59 pages31 Greene Liver LM 428 2017chip_darrisNo ratings yet
- LFTS, Thyroid and Renal Function TestsDocument3 pagesLFTS, Thyroid and Renal Function TestsAminn Alhassan ContehNo ratings yet
- Standard LFT and It's Clinical SignificanceDocument28 pagesStandard LFT and It's Clinical SignificanceanimathzNo ratings yet
- Aplikasi Pemeriksaan EnzimDocument25 pagesAplikasi Pemeriksaan EnzimBaiq NashaNo ratings yet
- Liver Function TestDocument9 pagesLiver Function TestFarah Krisna Sadavao AndangNo ratings yet
- Notes 02 Clinical Chemistry 2Document6 pagesNotes 02 Clinical Chemistry 2Brent LagartoNo ratings yet
- Liver Function Tests LFTsDocument4 pagesLiver Function Tests LFTsDr-Dalya ShakirNo ratings yet
- Clinical Chemistry 2Document6 pagesClinical Chemistry 2Romie SolacitoNo ratings yet
- Enzymes: M. Zaharna Clin. Chem. 2009Document32 pagesEnzymes: M. Zaharna Clin. Chem. 2009Ahmed GaberNo ratings yet
- Lecture Clinical EnzymologyDocument30 pagesLecture Clinical Enzymologychocoholic potchi100% (8)
- Validation & Interpretation of Hepatitis Testing Results MF18092022Document90 pagesValidation & Interpretation of Hepatitis Testing Results MF18092022Laila NihayaNo ratings yet
- Enzymes CC Part 2 PrintDocument6 pagesEnzymes CC Part 2 PrintKrystel Bea DinqueNo ratings yet
- Untitled PresentationDocument8 pagesUntitled PresentationAnand VermaNo ratings yet
- 1.1 Liver Function Tests 15.02.19Document39 pages1.1 Liver Function Tests 15.02.19Syed ArefinNo ratings yet
- A93a01306ben Alp CPDocument4 pagesA93a01306ben Alp CPIbrahimAliNo ratings yet
- A93a01282den Alp CP Rack BiDocument6 pagesA93a01282den Alp CP Rack BilaboratorlisimedNo ratings yet
- Protein Metabolism Dental and Physiotherapy Part 1Document17 pagesProtein Metabolism Dental and Physiotherapy Part 1Nada Atef KoraitemNo ratings yet
- What Are The Classification of ALP?Document4 pagesWhat Are The Classification of ALP?Frances FranciscoNo ratings yet
- Cpliver 1Document4 pagesCpliver 1isahNo ratings yet
- Enzymes of Clinical SignificanceDocument65 pagesEnzymes of Clinical SignificancepaulaOrialNo ratings yet
- 4.6 Alkaline Phosphatase DeterminationDocument9 pages4.6 Alkaline Phosphatase Determinationiridescent brightwinNo ratings yet
- Cyclic 3, 5 - AMP-Stimulated and Non-Stimulated Phosphorylation of Protein Fractions From Rat-Liver Cell Sap On Incubation With ( - P) AtpDocument10 pagesCyclic 3, 5 - AMP-Stimulated and Non-Stimulated Phosphorylation of Protein Fractions From Rat-Liver Cell Sap On Incubation With ( - P) Atpjuan carlos molano toroNo ratings yet
- Assessment of Liver Function: HaeriaDocument16 pagesAssessment of Liver Function: Haeriaria_hai2359No ratings yet
- Protein PlasmaDocument31 pagesProtein PlasmaDimas Adjie Yuda MahendraNo ratings yet
- Interpretación Del Perfil HepáticoDocument10 pagesInterpretación Del Perfil HepáticoEdwin AlvarezNo ratings yet
- Biochemistry Week 8 Amino Acid MetabolismDocument29 pagesBiochemistry Week 8 Amino Acid MetabolismKaren 3No ratings yet
- Urea/ Ammonia Tests: Primary Liver Function TestsDocument6 pagesUrea/ Ammonia Tests: Primary Liver Function TestsMemory MahwendaNo ratings yet
- Liver DiagnosticsDocument10 pagesLiver DiagnosticsTiny Briones-SallomanNo ratings yet
- كيمياء سريرية المحاضرة 2Document19 pagesكيمياء سريرية المحاضرة 2MohamedErrmaliNo ratings yet
- CHY 47 EnzymesDocument143 pagesCHY 47 EnzymesElle BuhisanNo ratings yet
- 13 JCR 015 Neki PhenytoinDocument6 pages13 JCR 015 Neki PhenytoinAnis ThohirohNo ratings yet
- Liver Function Tests (LFTS) : March 2010Document4 pagesLiver Function Tests (LFTS) : March 2010lavanyaNo ratings yet
- Sem2 CC Week2Document13 pagesSem2 CC Week2DENISE MARA�ANo ratings yet
- محاضره ١ كلينيكال د عبدالله القمةDocument11 pagesمحاضره ١ كلينيكال د عبدالله القمةahmed aliNo ratings yet
- Liver Function Test: Maimun ZA Lab Patologi Klinik Fkub-RssaDocument26 pagesLiver Function Test: Maimun ZA Lab Patologi Klinik Fkub-RssaSaifuddin BadarsyahNo ratings yet
- Applications of EnzymesDocument33 pagesApplications of EnzymesRoyal Mind100% (1)
- Porphyria BJH Review PDFDocument12 pagesPorphyria BJH Review PDFNexi anessaNo ratings yet
- Pmls 1 Final Exam Reviewer: Clinical Chemistry ContDocument14 pagesPmls 1 Final Exam Reviewer: Clinical Chemistry ContPlant in a PotNo ratings yet
- Acetaminophen-Induced Nephrotoxicity: Pathophysiology, Clinical Manifestations, and ManagementDocument5 pagesAcetaminophen-Induced Nephrotoxicity: Pathophysiology, Clinical Manifestations, and ManagementanzasmaraNo ratings yet
- 2-LFT Case Report Key AnswerDocument5 pages2-LFT Case Report Key AnswerAbdullah AlthobaitiNo ratings yet
- A Clinician's Guide To Statin Drug-Drug InteractionsDocument17 pagesA Clinician's Guide To Statin Drug-Drug InteractionsPuput mopanggaNo ratings yet
- Liver Function: DRS' NotesDocument13 pagesLiver Function: DRS' NotesVijayabaskaran MNo ratings yet
- Liver Function: DRS' NotesDocument13 pagesLiver Function: DRS' NotesVijayabaskaran MNo ratings yet
- AST and ALTDocument7 pagesAST and ALTTrisha NavarceNo ratings yet
- Principle of Metabolic RegulationDocument27 pagesPrinciple of Metabolic RegulationFlorentNo ratings yet
- Proteins Cclab EnotesDocument30 pagesProteins Cclab EnotesJUSTIN VICTOR ANGNo ratings yet
- Acute PancreatitisDocument13 pagesAcute PancreatitisJacob BorongNo ratings yet
- Professor Dr. Najat A. HasanDocument40 pagesProfessor Dr. Najat A. HasanPeter MungaiNo ratings yet
- A Case Oriented Approach To Liver Laboratory Profiling in Dogs and CatsDocument5 pagesA Case Oriented Approach To Liver Laboratory Profiling in Dogs and CatsAbelantonNo ratings yet
- RFT - Theory Notes-: (Important For Practical Also)Document13 pagesRFT - Theory Notes-: (Important For Practical Also)ammuNo ratings yet
- Medical Use of EnzymesDocument13 pagesMedical Use of EnzymesSamhita ChitturiNo ratings yet
- Restoration of Histoarchitecture in The Paracetamol-Induced Liver Damaged Rat by Earthworm ExtractDocument5 pagesRestoration of Histoarchitecture in The Paracetamol-Induced Liver Damaged Rat by Earthworm ExtractGrace Anastasia Ginting SinusingaNo ratings yet
- Pemeriksaan Fungsi HatiDocument46 pagesPemeriksaan Fungsi HatiNadyaWevtNo ratings yet
- Finding The Standard DeviationDocument2 pagesFinding The Standard DeviationMUNDER OMAIRA NASRA D.No ratings yet
- Agents of Opportunistic MycosesDocument13 pagesAgents of Opportunistic MycosesMUNDER OMAIRA NASRA D.No ratings yet
- Lesson 1 MycologyDocument12 pagesLesson 1 MycologyMUNDER OMAIRA NASRA D.No ratings yet
- RRLDocument4 pagesRRLMUNDER OMAIRA NASRA D.No ratings yet
- RESULTSDocument8 pagesRESULTSMUNDER OMAIRA NASRA D.No ratings yet
- MODULE 8. Ceiling WorksDocument2 pagesMODULE 8. Ceiling WorksAj MacalinaoNo ratings yet
- Job Stress InterventionsDocument5 pagesJob Stress InterventionscocaralucamihaelaNo ratings yet
- MICRF230Document20 pagesMICRF230Amador Garcia IIINo ratings yet
- Traulsen RHT-AHT Reach in Refrigerator WUT Glass DoorDocument2 pagesTraulsen RHT-AHT Reach in Refrigerator WUT Glass Doorwsfc-ebayNo ratings yet
- The Elder Scrolls V Skyrim - New Lands Mod TutorialDocument1,175 pagesThe Elder Scrolls V Skyrim - New Lands Mod TutorialJonx0rNo ratings yet
- Capacitor Trip Device CTD-4Document2 pagesCapacitor Trip Device CTD-4DAS1300No ratings yet
- Chapter 5: Current and Resistance: 5.1 The Motion of Electric ChargeDocument11 pagesChapter 5: Current and Resistance: 5.1 The Motion of Electric Chargeayunna ayunniNo ratings yet
- A Review On PRT in IndiaDocument21 pagesA Review On PRT in IndiaChalavadi VasavadattaNo ratings yet
- First Semester-NOTESDocument182 pagesFirst Semester-NOTESkalpanaNo ratings yet
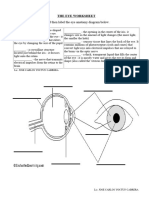
- The Eye WorksheetDocument3 pagesThe Eye WorksheetCally ChewNo ratings yet
- Second Quarter Lesson 4Document7 pagesSecond Quarter Lesson 4Jomarie PauleNo ratings yet
- Title - Dating Virtual To Coffee Table Keywords - Dating, Application BlogDocument3 pagesTitle - Dating Virtual To Coffee Table Keywords - Dating, Application BlogRajni DhimanNo ratings yet
- Solving Systems of Linear Equations in Three Variables: You Should LearnDocument8 pagesSolving Systems of Linear Equations in Three Variables: You Should LearnTheodore JoaquinnNo ratings yet
- Transmittal Sheet 1808-T-RJ-PJ-099SDocument2 pagesTransmittal Sheet 1808-T-RJ-PJ-099SMuhammad AzkaNo ratings yet
- Project - Dreambox Remote Video StreamingDocument5 pagesProject - Dreambox Remote Video StreamingIonut CristianNo ratings yet
- MnemonicsDocument1 pageMnemonicsSunil Boyz-uNo ratings yet
- Microcal P20Document2 pagesMicrocal P20ctmtectrolNo ratings yet
- Time-Temperature Charge Function of A High Dynamic Thermal Heat Storage With Phase Change MaterialDocument15 pagesTime-Temperature Charge Function of A High Dynamic Thermal Heat Storage With Phase Change Materialgassoumi walidNo ratings yet
- ESG Conundrum PDFDocument30 pagesESG Conundrum PDFVijay Kumar SwamiNo ratings yet
- Alliance For ProgressDocument19 pagesAlliance For ProgressDorian EusseNo ratings yet
- LANY Lyrics: "Thru These Tears" LyricsDocument2 pagesLANY Lyrics: "Thru These Tears" LyricsAnneNo ratings yet
- Curry PowderDocument8 pagesCurry PowderMahendar Vanam100% (1)
- 60 Plan of DepopulationDocument32 pages60 Plan of DepopulationMorena Eresh100% (1)
- Jmac TempDocument5 pagesJmac TempDan GerNo ratings yet
- Montessori Vs WaldorfDocument4 pagesMontessori Vs WaldorfAbarnaNo ratings yet
- Curriculum Vitae: Educational Background Certification Major Name of Institute PeriodDocument2 pagesCurriculum Vitae: Educational Background Certification Major Name of Institute PeriodTHEVINESHNo ratings yet
- Tugas Bahasa Inggris: ButterflyDocument4 pagesTugas Bahasa Inggris: ButterflyRiyadi TeguhNo ratings yet
- Def - Pemf Chronic Low Back PainDocument17 pagesDef - Pemf Chronic Low Back PainFisaudeNo ratings yet
- LADP HPDocument11 pagesLADP HPrupeshsoodNo ratings yet
- Applications PDFDocument90 pagesApplications PDFahmedNo ratings yet