Professional Documents
Culture Documents
The Shouldice Natural Tissue Repair For Inguinal Hernia
Uploaded by
HardiTariqHammaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Shouldice Natural Tissue Repair For Inguinal Hernia
Uploaded by
HardiTariqHammaCopyright:
Available Formats
SHOULDICE
Surgery Illustrated – Surgical Atlas
BJUI BJU INTERNATIONAL
The Shouldice natural tissue repair for inguinal hernia
Earle Byrnes Shouldice
Shouldice Hospital, Thornhill, Ontario, Canada
ILLUSTRATIONS by STEPHAN SPITZER, www.spitzer-illustration.com
PLANNING AND PREPARATION
5
The finding of a lump is perhaps the best
6
1 7
8
2
9
3
indication of a hernia. A diagnosis by 4
ultrasonography can be misleading and lead
to an unnecessary operation. This introduces
the question of what is an inoperable defect,
as defined by size or symptoms. As to size,
ultrasonography might reveal a very small
finding, causing no symptoms. This is better
left for ‘watchful waiting’, but the patient is 1
burdened with the knowledge he has a 3
4
5
‘hernia’. This finding might be within the
confines of ‘normal’ and best left untouched,
again ‘watchful waiting’.
Discomfort and pain in the groin can be due
to other causes. A tendinitis or tearing of
the insertion of the rectus pyramidalis or
adductor longus a so-called ‘sportsman’s
hernia’ can be improperly diagnosed as a
hernia.
The groin is a complex area, and hernias can
be rather easy or very difficult, according to
the patient’s anatomy, size of the defect and
surgeon’s experience. In the dissection, proper
freeing of the sac and special attention to the
floor of the canal are critical.
There is one critical step in successfully
repairing a hernia, i.e. the dissection. A
particular routine, as described here, has
proven itself over many years. The chances of
success in hernia surgery depend on the
dissection, for without a proper dissection
there can be no proper repair.
Of 1000 recurrences that presented at the
author’s institution for repair, a third were
indirect and two-thirds direct; 12–13% of all
primary inguinal hernias have a secondary
© 2010 THE AUTHOR
428 JOURNAL COMPILATION © 2 0 1 0 B J U I N T E R N A T I O N A L | 1 0 5 , 4 2 8 – 4 3 9 | doi:10.1111/j.1464-410X.2009.09155.x
SURGERY ILLUSTRATED
component. Before suturing, a secondary insurance tables are a reasonable guide. insufficient natural tissue to achieve a
component should be sought, and this will Proper or reasonable weight is a factor in our successful repair. The use of mesh is necessary
lower the recurrence rate. continued success. when the inguinal ligament is missing, but
otherwise it is a very rare situation where
The vast majority of hernia repairs are mesh should be used in the groin. There
operations of election, which presents the SPECIFIC EQUIPMENT/MATERIALS have been too many cases where mesh
opportunity to prepare the patient for complications have left patients with chronic
surgery. Comorbidities are investigated and Stainless steel wire 32–34 G is the suture pain and all of its deleterious effects on
the operating surgeon should be satisfied material of choice, and originally chosen quality of life.
that the possibilities of complications are because it is inert and does not form a nidus
minimal. of infection, should one occur. Initially the SURGICAL STEPS
wire can be difficult to handle but this
Overweight patients are more difficult to problem is soon overcome. Currently there are For all groin hernias, a specific routine of
operate on and this can contribute to several suture materials that could be used. surgical steps enables a smooth-flowing
complications. To provide the best chance Mesh is a great product and certainly presents dissection. It prevents omitting such vital
for success, patients are asked to help by the surgeon with the opportunity to repair features like discovering the secondary hernia,
attaining a reasonable weight; health large and difficult hernias where there is found in 12–13% of cases.
© 2010 THE AUTHOR
JOURNAL COMPILATION © 2010 BJU INTERNATIONAL 429
SHOULDICE
Figure 1
Indirect Inguinal Hernia
1 Indirect hernia
2 Iliohypogastric nerve
3 Cremasteric tissue
4 Shelving border of inguinal ligament
5 External oblique
6 Internal oblique
7 Ilioinguinal nerve
8 Cuff of transversal fascia surrounding the
cord
9 Flap of external oblique
At the internal ring there is a cuff of
transversalis fascia surrounding the spermatic
cord. Free the cord of this tissue. The floor of 5
the canal covered by cremasteric tissue may 6
also hide a second hernia. 1 7
8
2
9
3
© 2010 THE AUTHOR
430 JOURNAL COMPILATION © 2010 BJU INTERNATIONAL
SURGERY ILLUSTRATED
Figure 2
Indirect sac/peritoneal protrusion.
Peritoneum is always present on the cord at
the internal ring either as an indirect hernia or
as a protrusion of peritoneum. In either case
it has to be freed and reduced into the
abdomen. If the sac is difficult to free from
the cord, divide it and leave the distal portion
intact. This prevents unnecessary trauma to
the cord. Some sacs may be very thin and
difficult to find. Freeing the peritoneum and
reducing it assures no missed indirect hernia
which are the findings in a third of all
recurrences.
© 2010 THE AUTHOR
JOURNAL COMPILATION © 2010 BJU INTERNATIONAL 431
SHOULDICE
Figure 3
Divide the cremasterics.
The floor is obscured by cremasteric tissue
(vessels, muscle and genital branch of the
genitofemoral nerve). Removing this tissue
gives an uninhibited view of the posterior wall
where two-thirds of missed hernias are
found. The cremasteric tissue is divided
leaving the distal end long enough to support
the testis, thus avoiding a dependent testis
and the proximal stump reasonably short to
be incorporated to a newly formed internal
ring.
© 2010 THE AUTHOR
432 JOURNAL COMPILATION © 2010 BJU INTERNATIONAL
SURGERY ILLUSTRATED
Figure 4
Splitting the transversalis fascia is rare in
women and essentially never in children. This
fascia needs to be divided far enough to be
able to assure the surgeon of its strength
medially and consequently no missed hernia.
When splitting transversalis fascia remember
it is multilayered. The fascia is split to develop
a wide lateral flap which is necessary for the
repair. It also enables proper viewing of tissue
to be sutured. Beneath this fascia lie small
vessels and the marginal vein which may
require securing.
© 2010 THE AUTHOR
JOURNAL COMPILATION © 2010 BJU INTERNATIONAL 433
SHOULDICE
Figure 5
Transversalis fascia split.
When this fascia is split and its deep surface is
cleaned of adherent fat, suturing can begin.
First check for that elusive secondary hernia,
possibly a femoral or a rare interstitial. In the
medial third of the floor, where most direct
recurrences develop, the transversalis fascia is
of good quality but thins considerably as the
site of the future internal ring is approached.
The initial suture through the transversalis
fascia is placed by the bone; periostium is
avoided. The suture is carried through the
edge of rectus medially.
© 2010 THE AUTHOR
434 JOURNAL COMPILATION © 2010 BJU INTERNATIONAL
SURGERY ILLUSTRATED
Figure 6
First line of the repair
1 Flap of internal oblique, transversus
abdominus and transversalis fascia
2 Epigastric vessels
3 Cremasteric stump
4 Transversalis fascia
5 Shelving border of inguinal ligament
6 Flap of external oblique
This initial suture line, apart from retaining
intra-abdominal fat, anchors the repair very
firmly at its medial and lateral ends. It also
serves to develop an all-important flap of
tissue medially. The lateral flap of transversalis
1
fascia is carried to the deep surface of the
medial lying muscle mass (the triple layer). 2
This develops a flap of tissue used for the
second line of repair.
3
4
5
© 2010 THE AUTHOR
JOURNAL COMPILATION © 2010 BJU INTERNATIONAL 435
SHOULDICE
Figure 7
Finishing the first line of the repair.
The internal ring is formed by picking up
transversalis fascia and the proximal stump of
cremasteric tissue. The latter is formed by an
extension of internal oblique muscle and
transversalis fascia, which becomes the
internal spermatic fascia. These tissues are
carried to the deep surface of the triple layer.
The suture is brought through the full
thickness of the muscle mass ready for the
second line to begin. This helps to create a
cylinder for an internal ring which, upon
contraction of internal oblique, also acts as a
sphincter. There is absolutely no need to try to
close the ring and create strength in the repair
by pulling the suture tight. This only serves to
strangle the tissue. Small bites of tissue are
mandatory; there is no need to make the ring
tight.
© 2010 THE AUTHOR
436 JOURNAL COMPILATION © 2010 BJU INTERNATIONAL
SURGERY ILLUSTRATED
Figure 8
Second line of the repair.
The suture is reversed and the second line
begins by carrying the developed flap
medially to any or all of the iliopubic tract,
transversalis fascia and inguinal ligament
near its shelving or reflected border. Be
careful of the femoral vessels lying just
beneath at the internal ring. Do not use the
needle tip to dig for tissue to be sutured. The
medial lying flap of tissue is carried deeper
as the bone is approached. The floor now
consists of two layers. The original
transversalis fascia and this new reinforcing
flap of tissue form an extension of the triple
layer.
© 2010 THE AUTHOR
JOURNAL COMPILATION © 2010 BJU INTERNATIONAL 437
SHOULDICE
Figure 9
Third line of the repair.
Starting at the internal ring, the lateral flap of
external oblique is replaced over the internal
oblique and covers the previous suture lines. A
small portion of this tissue is left free to
accommodate the spermatic cord. Direct
recurrences occur mainly in the medial
portion of the floor near the bone. Particular
attention is paid to ensure the external
oblique fascia is carried well medially by the
bone to reinforce this area. The fourth line
duplicates the third in reverse. The cord is
then covered by external oblique.
© 2010 THE AUTHOR
438 JOURNAL COMPILATION © 2010 BJU INTERNATIONAL
SURGERY ILLUSTRATED
POSTOPERATIVE CARE others might require acetaminophen 1000 mg local anaesthetic, young muscular cases can
every 6 h, codeine 30–60 mg every 4 h, or be trying. Recurrences where mesh was
Immediate ambulation off the operating large difficult procedures might require previously used can be very difficult. I also
table has both positive physiological and oxycontin 10–20 mg every 12 h. The patient is wait a year after any previous surgery to allow
psychological effects; the former by increasing told to be active within reason, as his repair is the wound to mature. Patient weight loss, as
circulation and the latter reassures the patient firm and discomfort is the only defining noted, can be a major factor in easing the
that all is well, his repair is firm and he should factor. surgeon’s life. Complying with a routine as
move around. However, after returning to his described, with patience, will ensure success.
bed some time is necessary for medications to
wear off and to minimize the risk of falls. FROM SURGEON TO SURGEON Correspondence: Earle Byrnes Shouldice,
Shouldice Hospital, 7750 Bayview Avenue,
Postoperative medication is usually minimal, Overweight patients and larger defects Thornhill, Ontario, Canada.
with 37% of patients requiring nothing, while contribute to difficult surgery and, as I use e-mail: jsears@shouldice.com
© 2010 THE AUTHOR
JOURNAL COMPILATION © 2010 BJU INTERNATIONAL 439
You might also like
- Knots in Orthopedic Surgery: Open and Arthroscopic TechniquesFrom EverandKnots in Orthopedic Surgery: Open and Arthroscopic TechniquesUmut AkgunNo ratings yet
- Removal of Ear, Nose andDocument4 pagesRemoval of Ear, Nose andandinNo ratings yet
- Umbilicalherniarepair: Overview of Approaches and Review of LiteratureDocument16 pagesUmbilicalherniarepair: Overview of Approaches and Review of LiteratureVictor Matias BarriosNo ratings yet
- Cleft Palate Repair, Gingivoperiosteoplasty and Alveolar Bone GraftingDocument10 pagesCleft Palate Repair, Gingivoperiosteoplasty and Alveolar Bone GraftingAndrés Faúndez TeránNo ratings yet
- 11 2 34 PDFDocument3 pages11 2 34 PDFAgusNo ratings yet
- International Journal of Surgery: Sri Vengadesh Gopal, Achuthan WarrierDocument4 pagesInternational Journal of Surgery: Sri Vengadesh Gopal, Achuthan WarrierRon Java FantillanNo ratings yet
- Indications Plexus Reconstr OBPPDocument8 pagesIndications Plexus Reconstr OBPP2w8qg5qwhdNo ratings yet
- 27720150561679Document7 pages27720150561679apryanadarNo ratings yet
- Intimate Examinations and The Use of Chaperones: WWW - Rcr.ac - UkDocument14 pagesIntimate Examinations and The Use of Chaperones: WWW - Rcr.ac - UkMirza BaigNo ratings yet
- Midterm Ngt InsertionDocument5 pagesMidterm Ngt InsertionMaria Kyla VicenteNo ratings yet
- The Digital Rectal ExaminationDocument2 pagesThe Digital Rectal ExaminationGabriela GalvezNo ratings yet
- 0 OP Techniques General Surgery Superficial Parotidectomy OLSEN EXCELLENTDocument13 pages0 OP Techniques General Surgery Superficial Parotidectomy OLSEN EXCELLENTmuhammad ishaqueNo ratings yet
- The Use of Paraglossal Straight Blade Laryngoscopy in Difficult Tracheal IntubationDocument9 pagesThe Use of Paraglossal Straight Blade Laryngoscopy in Difficult Tracheal IntubationJset SixthousandNo ratings yet
- Pediatric Protrusion Mentioned,: Robert M.D. CityDocument2 pagesPediatric Protrusion Mentioned,: Robert M.D. Citybouchra8blsNo ratings yet
- Abdominal Incisions and Sutures in Obstetrics and GynaecologyDocument6 pagesAbdominal Incisions and Sutures in Obstetrics and GynaecologyFebyan AbotNo ratings yet
- Teknik Frenectomy Miller 2020Document4 pagesTeknik Frenectomy Miller 2020yufita fitrianiNo ratings yet
- Clinical Orthopaedic Examination-1 PDFDocument334 pagesClinical Orthopaedic Examination-1 PDFEmil Cotenescu100% (9)
- Arnold L. Freedman, Marc D. Stein, Daniel B. Schneider.Document5 pagesArnold L. Freedman, Marc D. Stein, Daniel B. Schneider.Gloria SequeiraNo ratings yet
- Warthins Tumorof Parotid GlandDocument5 pagesWarthins Tumorof Parotid GlandWahyuni NaharuddinNo ratings yet
- Raoul Tubiana - Jean-Michel Thomine - Evelyn Mackin - F Brunelli - Examination of The Hand and Wrist-CRC PressDocument406 pagesRaoul Tubiana - Jean-Michel Thomine - Evelyn Mackin - F Brunelli - Examination of The Hand and Wrist-CRC PressMaricruzhdezaNo ratings yet
- Journal Plastic - Thenar FlapDocument4 pagesJournal Plastic - Thenar FlapMuhammad WartonoNo ratings yet
- CORMACK, LEHANE - 1984 - Difficult Tracheal Intubation in ObstetricsDocument7 pagesCORMACK, LEHANE - 1984 - Difficult Tracheal Intubation in ObstetricsMubeenRahmanNo ratings yet
- Surgical Techniques in Primary Inguinal Hernia RepairDocument7 pagesSurgical Techniques in Primary Inguinal Hernia RepairNuno AzenhaNo ratings yet
- Urinary Catheterization Procedures With RationaleDocument10 pagesUrinary Catheterization Procedures With RationaleKaye NaigNo ratings yet
- Laparoscopic Hernia Repair in Neonates, Infants and ChildrenDocument9 pagesLaparoscopic Hernia Repair in Neonates, Infants and ChildrenErick OematanNo ratings yet
- Indications and The Diagnosis For Fixed Partial Denture ProsthesisDocument7 pagesIndications and The Diagnosis For Fixed Partial Denture ProsthesisDaniel Espinoza EspinozaNo ratings yet
- Eyelid DisordersDocument6 pagesEyelid DisordersCamilo PerezNo ratings yet
- 295 QsDocument3 pages295 Qsujangketul62No ratings yet
- 3dmax Light Mesh: Technique GuideDocument12 pages3dmax Light Mesh: Technique GuidenautilixxNo ratings yet
- Morphological Study On Torus Palatinus in Adult Human SkullsDocument4 pagesMorphological Study On Torus Palatinus in Adult Human SkullsOttofianus Alvedo Hewick KalangiNo ratings yet
- SteinerDocument23 pagesSteinerAlejandra Zambrano ValeroNo ratings yet
- Rle 107 MTDocument15 pagesRle 107 MTKrizia Claire Marie RedondoNo ratings yet
- Rapid Palatal Expansion in The Young Adult A Case Report: January 2015Document7 pagesRapid Palatal Expansion in The Young Adult A Case Report: January 2015AomChanumpornNo ratings yet
- Clin Experimental Optometry - 2008 - Clinical Medicine in Optometric Practice 2nd EditionDocument2 pagesClin Experimental Optometry - 2008 - Clinical Medicine in Optometric Practice 2nd EditionnicolamihaiuNo ratings yet
- Closed Rhinoplasty The Next Generation - Paul J OKeeffe (2019)Document107 pagesClosed Rhinoplasty The Next Generation - Paul J OKeeffe (2019)poly_paparas100% (1)
- Endodontic SurgeryDocument16 pagesEndodontic SurgeryauntymayaNo ratings yet
- 2014-08-13 Suture Presentation FINAL - SlidesDocument13 pages2014-08-13 Suture Presentation FINAL - SlidesMariana HernandezNo ratings yet
- 2s2022 Ncm109 Rle Learn Mat 1Document18 pages2s2022 Ncm109 Rle Learn Mat 1Guia SalandananNo ratings yet
- Williamson 2014Document7 pagesWilliamson 2014scribd mendeleyNo ratings yet
- Guideline No. 412 Laparoscopic Entry For Gynexological SurgeryDocument16 pagesGuideline No. 412 Laparoscopic Entry For Gynexological SurgeryRaúl MartínezNo ratings yet
- Foresta 2014Document14 pagesForesta 2014stoia_sebiNo ratings yet
- ASSISTING IN BONE MARROW ASPIRATION (2) .Doc Revised. ADocument9 pagesASSISTING IN BONE MARROW ASPIRATION (2) .Doc Revised. ARiza Angela BarazanNo ratings yet
- Histopathology Grossing ProceduresDocument14 pagesHistopathology Grossing ProceduresNico Loko100% (1)
- Editorial: Ó 2002 Blackwell Science LTDDocument5 pagesEditorial: Ó 2002 Blackwell Science LTDpradeep danielNo ratings yet
- Levitt 2002Document7 pagesLevitt 2002Diego ReyNo ratings yet
- Alar Lift: Sail Excision Technique For Alar Overhanging in The Middle Eastern NoseDocument5 pagesAlar Lift: Sail Excision Technique For Alar Overhanging in The Middle Eastern NosejerryimNo ratings yet
- 1 Suhasini SonavdekarDocument6 pages1 Suhasini SonavdekarArlia orohNo ratings yet
- How - To - Determine - Gestational - Age - of - An - Equine - Preg Mcdonell 2006Document7 pagesHow - To - Determine - Gestational - Age - of - An - Equine - Preg Mcdonell 2006kaathydanieelaNo ratings yet
- Diagnostic Laparoscopy: Surgical Endoscopy February 2004Document6 pagesDiagnostic Laparoscopy: Surgical Endoscopy February 2004carmenNo ratings yet
- History Taking: Practical 1 InstructionDocument12 pagesHistory Taking: Practical 1 InstructionDimsyafelNo ratings yet
- ABRAVAS 2 de 9 - Divers 1999 - Reptile EndosDocument8 pagesABRAVAS 2 de 9 - Divers 1999 - Reptile EndosCamilo SantanderNo ratings yet
- Palatally Impacted CaninesDocument5 pagesPalatally Impacted CaninesMoisés MartinsNo ratings yet
- PerforasiDocument3 pagesPerforasiEinz Nur Amalyah IdrusNo ratings yet
- Draping of Tibia: Sandwich TechniqueDocument3 pagesDraping of Tibia: Sandwich Techniquebagus lazuardiNo ratings yet
- Checklist For Vaginal ExaminationDocument7 pagesChecklist For Vaginal ExaminationjoaguilarNo ratings yet
- Invited Discussion On: Concentrated Growth Factors Extracted From Blood Plasma Used To Repair Nasal Septal Mucosal Defect After RhinoplastyDocument2 pagesInvited Discussion On: Concentrated Growth Factors Extracted From Blood Plasma Used To Repair Nasal Septal Mucosal Defect After RhinoplastyHiktor TomNo ratings yet
- Dorsal Ovariectomy in RodentsDocument5 pagesDorsal Ovariectomy in RodentsJavier OjedaNo ratings yet
- Evisceration With Autogenous Scleral Graft and Bioceramic Implantation Within The Modified Scleral Shell 133 Cases Over 17 YearsDocument6 pagesEvisceration With Autogenous Scleral Graft and Bioceramic Implantation Within The Modified Scleral Shell 133 Cases Over 17 YearsSaraelsy MonterrosoNo ratings yet
- Omphalolith Surgical ExtractionDocument2 pagesOmphalolith Surgical ExtractionWei Sheng ChongNo ratings yet
- PerikondritisDocument5 pagesPerikondritisRay RamadhanNo ratings yet
- Urolithiasis - Metabolic Considerations: Case 1Document2 pagesUrolithiasis - Metabolic Considerations: Case 1HardiTariqHammaNo ratings yet
- Urology News Jul Aug 2016 Spot TestDocument2 pagesUrology News Jul Aug 2016 Spot TestHardiTariqHammaNo ratings yet
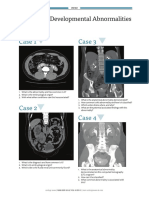
- Case 1 Case 3: Technology - Part 1Document2 pagesCase 1 Case 3: Technology - Part 1HardiTariqHammaNo ratings yet
- Uroma14 Spot Test NewDocument2 pagesUroma14 Spot Test NewHardiTariqHammaNo ratings yet
- Prostate Cancer MRI and Biopsy Spot TestDocument2 pagesProstate Cancer MRI and Biopsy Spot TestHardiTariqHammaNo ratings yet
- Urology Sample MCQ Exam eDocument2 pagesUrology Sample MCQ Exam eHardiTariqHammaNo ratings yet
- Surgical Strategies in Endourology For Stone DiseaseDocument291 pagesSurgical Strategies in Endourology For Stone DiseaseHardiTariqHammaNo ratings yet
- Registration for HoLEP Day Surgery CourseDocument2 pagesRegistration for HoLEP Day Surgery CourseHardiTariqHammaNo ratings yet
- Uroja14 Spot Test NewDocument2 pagesUroja14 Spot Test NewHardiTariqHammaNo ratings yet
- UROLOGY OSCE Skills English NT Version 2Document1 pageUROLOGY OSCE Skills English NT Version 2HardiTariqHammaNo ratings yet
- Uroma16 Spot Test 2Document2 pagesUroma16 Spot Test 2HardiTariqHammaNo ratings yet
- A. Congenital Adrenal HyperplasiaDocument5 pagesA. Congenital Adrenal HyperplasiasewmehondesalegnNo ratings yet
- Urology News Jul Aug 2016 Spot TestDocument2 pagesUrology News Jul Aug 2016 Spot TestHardiTariqHammaNo ratings yet
- Uromj14 Spot Test NewDocument2 pagesUromj14 Spot Test NewHardiTariqHammaNo ratings yet
- A. Congenital Adrenal HyperplasiaDocument5 pagesA. Congenital Adrenal HyperplasiasewmehondesalegnNo ratings yet
- EBU Summative Assessments in UrologyDocument60 pagesEBU Summative Assessments in UrologyHardiTariqHammaNo ratings yet
- Research Protocol Form, Approval Deraw DR - 1Document12 pagesResearch Protocol Form, Approval Deraw DR - 1HardiTariqHammaNo ratings yet
- Urethral Pathology: Case 1 Case 2Document2 pagesUrethral Pathology: Case 1 Case 2HardiTariqHammaNo ratings yet
- 4 5787572421108171420 PDFDocument62 pages4 5787572421108171420 PDFnanda1al1humairahNo ratings yet
- Urology OSCEDocument10 pagesUrology OSCEHardiTariqHammaNo ratings yet
- A. Congenital Adrenal HyperplasiaDocument5 pagesA. Congenital Adrenal HyperplasiasewmehondesalegnNo ratings yet
- Osces For Medical Students, Volume 2 Second EditionDocument41 pagesOsces For Medical Students, Volume 2 Second EditionNaeem Khan100% (3)
- Radiology Quiz: by Jane BelfieldDocument4 pagesRadiology Quiz: by Jane BelfieldHardiTariqHammaNo ratings yet
- LUTS Spot TestDocument2 pagesLUTS Spot TestHardiTariqHamma100% (1)
- Deadly Kidney Infection: Understanding Emphysematous Pyelonephritis (EPNDocument31 pagesDeadly Kidney Infection: Understanding Emphysematous Pyelonephritis (EPNHardiTariqHammaNo ratings yet
- Neurourology: Case 1 Case 3Document2 pagesNeurourology: Case 1 Case 3HardiTariqHammaNo ratings yet
- Uropathology: What's The Diagnosis?: Case 1 Case 2Document2 pagesUropathology: What's The Diagnosis?: Case 1 Case 2HardiTariqHammaNo ratings yet
- Paediatric Urology - Peno-Scrotal: Case 1 Case 2Document2 pagesPaediatric Urology - Peno-Scrotal: Case 1 Case 2HardiTariqHammaNo ratings yet
- Continuing Medical Education: CME Multiple Choice QuestionsDocument1 pageContinuing Medical Education: CME Multiple Choice QuestionsHardiTariqHammaNo ratings yet
- Renal Quiz (12.8.2017)Document3 pagesRenal Quiz (12.8.2017)HardiTariqHammaNo ratings yet
- Saqeeb PPT LiqueurDocument21 pagesSaqeeb PPT LiqueurSæqéëb Æl HæssåñNo ratings yet
- Assignment 6Document2 pagesAssignment 6Rishabh MelwankiNo ratings yet
- The Etherington BrothersDocument30 pagesThe Etherington Brotherstoninho_6660% (1)
- Liturgical Music For LentDocument11 pagesLiturgical Music For LentShirly Benedictos100% (1)
- New Holland E55Bx Tier 4 Compact Hydraulic Excavator Service Repair ManualDocument21 pagesNew Holland E55Bx Tier 4 Compact Hydraulic Excavator Service Repair ManualggjjjjotonesNo ratings yet
- MSC Logic Self Study 2019 CompleteDocument88 pagesMSC Logic Self Study 2019 CompleteAlyssa RenataNo ratings yet
- Negotiation Self-Assessment and Vision Report - by Umang DharDocument1 pageNegotiation Self-Assessment and Vision Report - by Umang Dharumangdhar8No ratings yet
- Well Construction Journal - May/June 2014Document28 pagesWell Construction Journal - May/June 2014Venture PublishingNo ratings yet
- Prabuddha Bharata June10Document58 pagesPrabuddha Bharata June10talk2ankitNo ratings yet
- Unimac Technical Specifications UY180 UY240 UY280Document2 pagesUnimac Technical Specifications UY180 UY240 UY280mairimsp2003No ratings yet
- Awesome Info Lock PickingDocument19 pagesAwesome Info Lock PickingApparatchiki310100% (7)
- Analysis Report Bhuwan BhaskarDocument29 pagesAnalysis Report Bhuwan BhaskarKshitiz LamichhaneNo ratings yet
- Case Study - BIG HIT ENTERTAINMENT AND BTS: K-POP REACHES FOR A GLOBAL BREAKTHROUGHDocument9 pagesCase Study - BIG HIT ENTERTAINMENT AND BTS: K-POP REACHES FOR A GLOBAL BREAKTHROUGHJENEUSE JADE TAGANASNo ratings yet
- Improving Student Vocabulary with Extensive ReadingDocument2 pagesImproving Student Vocabulary with Extensive ReadingSariayumarthatilaarNo ratings yet
- Remedial Law REVIEWER Atty. Tranquil SalvadorDocument61 pagesRemedial Law REVIEWER Atty. Tranquil SalvadorDPMPascua100% (1)
- U2000 & PRS Operation Introduce V1.0Document25 pagesU2000 & PRS Operation Introduce V1.0Nam PhamNo ratings yet
- Horno Industrial HC1 v1.1Document30 pagesHorno Industrial HC1 v1.1Cristian urielNo ratings yet
- Bioworld Naruto Classic Uzumaki Naruto Cosplay Zip-Up Hoodie, Multicolored, Medium Amazon - Ca Clothing, Shoes & AccessoriesDocument1 pageBioworld Naruto Classic Uzumaki Naruto Cosplay Zip-Up Hoodie, Multicolored, Medium Amazon - Ca Clothing, Shoes & AccessoriestonydidlyNo ratings yet
- Describing LearnersDocument29 pagesDescribing LearnersSongül Kafa67% (3)
- DLP Reading Comprehension 15th SeptemberDocument3 pagesDLP Reading Comprehension 15th SeptemberHanaa ElmostaeenNo ratings yet
- VOL. 208, MAY 7, 1992 487 Perla Compania de Seguros, Inc. vs. Court of AppealsDocument9 pagesVOL. 208, MAY 7, 1992 487 Perla Compania de Seguros, Inc. vs. Court of AppealsdanexrainierNo ratings yet
- Around The DubaiDocument11 pagesAround The DubaiGayane HovhannisyanNo ratings yet
- Wax Rolls For Your Success: Yarn Yearns For The One and OnlyDocument9 pagesWax Rolls For Your Success: Yarn Yearns For The One and Onlyangga widayantoNo ratings yet
- PSMB Certified Trainer Curriculum StructureDocument19 pagesPSMB Certified Trainer Curriculum StructureFlankerSparrowNo ratings yet
- Chapter 1:: Grammatical Description of English, Basic TermsDocument6 pagesChapter 1:: Grammatical Description of English, Basic Termsleksandra1No ratings yet
- Catalogo Tecnico Toyota BT Staxio P Series SPE120 200Document4 pagesCatalogo Tecnico Toyota BT Staxio P Series SPE120 200Asesor ComercialNo ratings yet
- Wound Healing PhasesDocument27 pagesWound Healing PhasesAnil BasnetNo ratings yet
- ARTS8 Q4 MOD2Document32 pagesARTS8 Q4 MOD2eoghannolascoNo ratings yet
- Unit 4 Reading Exercise 2Document6 pagesUnit 4 Reading Exercise 2Ivan TamaNo ratings yet