Professional Documents
Culture Documents
GTH Stellungnahme AstraZeneca Engl. 3 22 2021
GTH Stellungnahme AstraZeneca Engl. 3 22 2021
Uploaded by
Nicolás SilvaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GTH Stellungnahme AstraZeneca Engl. 3 22 2021
GTH Stellungnahme AstraZeneca Engl. 3 22 2021
Uploaded by
Nicolás SilvaCopyright:
Available Formats
GTH Geschäftsstelle – Gertrudenstr.
9 - 50667 Köln / Germany GTH
Gesellschaft
für Thrombose- und
Hämostaseforschung
e.V.
___________________
GTH Geschäftsstelle
Haus der Verbände Köln
Gertrudenstr. 9
50667 Köln / Germany
Telefon +49 221 423346 26
mail@gth-online.org
www.gth-online.org
Cologne, 03/22/2021
___________________
Vorstand
Updated GTH statement on vaccination with the AstraZeneca COVID-19 Vorsitzender
vaccine, as of March 22, 2021 Prof. Dr. J. Oldenburg
Stellvertr. Vorsitzender
PD Dr. R. Klamroth
On Friday, March 19, 2021, vaccinations with the COVID-19 vaccine from Sekretär
AstraZeneca were resumed in Germany. The Paul Ehrlich Institute (PEI) had Prof. Dr. F. Langer
previously reported on 13 cases of sinus or cerebral vein thrombosis with > 1.6 Schatzmeisterin
million AstraZeneca COVID-19 vaccine doses administered. The thromboses Dr. C. von Auer
Weitere Mitglieder
occurred 4–16 days after vaccination with the AstraZeneca COVID-19 vaccine in Prof. Dr. M. Albisetti
twelve women and one man aged 20–63 years. The patients also had PD. Dr. C. Ay
thrombocytopenia, which indicates an immunological event as the cause of the Prof. Dr. W. Korte
tendency to thrombosis.
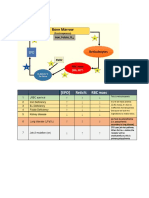
An important pathomechanism has meanwhile been clarified within the GTH
under the leadership of the Greifswald working group around Andreas
Greinacher. The vaccination is likely to lead to the formation of antibodies
against platelet antigens as part of the inflammatory reaction and immune
stimulation. Depending on or independently of heparin, these antibodies then
induce massive platelet activation via the Fc receptor in analogy to heparin-
induced thrombocytopenia (HIT). This mechanism (HIT mimicry) could be
demonstrated in four patients with a sinus / cerebral vein thrombosis after
vaccination with the AstraZeneca COVID-19 vaccine in the laboratory of Andreas ___________________
Greinacher in cooperation with other GTH members. As with classical HIT, these Amtsgericht München
antibodies appear 4–16 days after vaccination. This pathomechanism does not Vereinsregister Nr. 5945
rule out that the sinus / cerebral vein thromboses after vaccination with the
Finanzamt Frankfurt/Main
AstraZeneca COVID-19 vaccine also have other causes. However, it forms the Steuer Nr.
basis for the following updated statements and recommendations of the GTH: 45 255 50797
___________________
On a population basis, the positive effects of vaccination with the Bankverbindung
AstraZeneca COVID-19 vaccine outweigh the negative effects, so that Frankfurter Sparkasse
the resumption of vaccinations in Germany with this vaccine is to be
IBAN: DE73 5005 0201 0000 2729 49
welcomed. SWIFT/BIC: HELADEF1822
According to the current state of knowledge, there is no evidence that
thromboses at typical locations (leg vein thrombosis, pulmonary
embolism) are more common after vaccination with the AstraZeneca
COVID-19 vaccine than in the age-appropriate normal population.
Due to the immunological genesis of thromboses in intracranial veins or
other (atypical) locations, patients with a positive history of thrombosis
and / or known thrombophilia do not have an increased risk of
developing this specific and very rare complication after vaccination
with the AstraZeneca COVID-19 vaccine.
Flu-like symptoms such as joint, muscle and headache that persist for 1–
2 days after vaccination are a common side effect and are not a cause
for concern.
In the event of side effects that persist or recur > 3 days after
vaccination (e.g., dizziness; headache; visual disturbances; nausea /
vomiting; shortness of breath; acute pain in chest, abdomen, or
extremities), further medical diagnostics should be carried out to clarify
a thrombosis.
Important examinations are, in particular, the blood count with
determination of the platelet count, blood smear, D-dimers and, if
necessary, further imaging diagnostics (e.g., cMRI, ultrasound, CT of
chest / abdomen).
In the event of thrombocytopenia and / or evidence of thrombosis,
testing for pathophysiologically relevant antibodies should be carried
out regardless of previous exposure to heparin. The first test in the
diagnostic algorithm is a screening test for heparin-induced
thrombocytopenia (HIT), which is based on the immunological detection
of antibodies against the platelet factor 4 (PF4) / heparin complex. In
case this test is negative, an HIT-like specific immunological cause of
thrombosis / thrombocytopenia can be ruled out. In case this test is
positive, a classical HIPA assay (HIPA, heparin-induced platelet
activation) or SRA (serotonin-release assay) should be ordered as a
functional confirmatory test. These assays detect pathophysiologically
relevant antibodies, which activate platelets dependent (typical HIT) or
independent of exogenous heparin (autoimmune HIT). A positive test
result thus establishes the diagnosis of (autoimmune) HIT. In case the
classical HIPA (or SRA) is negative, a modified HIPA assay, which has
been established in the laboratory of Andreas Greinacher, Greifswald,
should be ordered. This assay detects pathophysiologically relevant
antibodies, which show a reaction pattern different from that observed
in (autoimmune) HIT. A positive test result thus establishes the diagnosis
of vaccine-induced prothrombotic immune thrombocytopenia (VIPIT).
Until (autoimmune) HIT is ruled out, if the clinical situation, availability
and experience permit, anticoagulation with heparins should be avoided
and alternative, HIT-compatible anticoagulants should be used.
In patients with confirmed (autoimmune) HIT or VIPIT and critical
thromboses such as sinus / cerebral or splanchnic vein thrombosis, the
prothrombotic pathomechanism can very likely be interrupted by the
administration of high-dose intravenous immunoglobulins (IVIG), e.g., at
a dose of 1 g per kg of body weight daily on two consecutive days.
Regardless of (autoimmune) HIT and VIPIT test results, alternative
causes of thrombocytopenia and / or thrombosis must be considered
and further clarified accordingly. These include, for example, thrombotic
microangiopathy (iTTP, aHUS), antiphospholipid syndrome, paroxysmal
nocturnal hemoglobinuria and underlying malignant (haematological)
diseases.
With friendly recommendation
Chairman of the Board of GTH Vice Chairman of GTH Secretary
Prof. Dr. med. Priv.- Doz. Dr. med. Prof. Dr. med.
Johannes Oldenburg Robert Klamroth Florian Langer
Chairman and Director Chefarzt der Klinik für Innere Leiter des Bereichs
Medizin Angiologie und Hämostaseologie
University Clinic Bonn AöR Hämostaseologie (Gerinnungsambulanz und
Institute of Experimental Hämophiliezentrum)
Haematology and Transfusion Zentrum für Gefäßmedizin
Medicine Vivantes Klinikum im Universitätsklinikum
Friedrichshain Hamburg-Eppendorf
II. Medizinische Klinik und
Poliklinik
(Onkologie, Hämatologie
und KMT mit der Sektion
Pneumologie)
Prof. Dr. med. Prof. Dr. med.
Bernd Pötzsch Andreas Greinacher
Stv. Leiter Leiter der Abteilung
Institute of Experimental Transfusionsmedizin am Institut
Haematology and Transfusion für Immunologie und
Medicine Transfusionsmedizin
University Clinic Bonn AöR Universitätsmedizin Greifswald
You might also like
- Routine Blood Results Explained 3/e: A guide for Nurses & Allied Health ProfessionalsFrom EverandRoutine Blood Results Explained 3/e: A guide for Nurses & Allied Health ProfessionalsRating: 3 out of 5 stars3/5 (2)
- Human Performance and Limitations: Atpl SummariesDocument59 pagesHuman Performance and Limitations: Atpl SummariesAlex Dominguez MiguezNo ratings yet
- Clinical Pathology: Essentials ofDocument8 pagesClinical Pathology: Essentials ofAhmed BahaaNo ratings yet
- Standard Operating Procedure Blood Bank/ Blood Station: Approval SheetDocument28 pagesStandard Operating Procedure Blood Bank/ Blood Station: Approval Sheetddophlaak labdeptNo ratings yet
- Blood Transfusion On Dialysis Guidelines Aug 2017 PDFDocument5 pagesBlood Transfusion On Dialysis Guidelines Aug 2017 PDFYolanda IrawatiNo ratings yet
- English: Quarter 4 - Module 2Document28 pagesEnglish: Quarter 4 - Module 2Janrex Karl FaelagmaoNo ratings yet
- 43ttkxj2joqnljbdueumkilwDocument4 pages43ttkxj2joqnljbdueumkilwDivyansh SinghNo ratings yet
- The Human Body Final DraftDocument3 pagesThe Human Body Final DraftPratyush AcharyaNo ratings yet
- Guideline Massive PPHDocument27 pagesGuideline Massive PPHSarah SabrinaNo ratings yet
- Limitations and Pitfalls of FDG-PET/CT in Infection and InflammationDocument13 pagesLimitations and Pitfalls of FDG-PET/CT in Infection and InflammationTurki100% (1)
- Deep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edFrom EverandDeep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edRating: 5 out of 5 stars5/5 (1)
- Test Bank For Pathophysiology 6th Edition Jacquelyn L BanasikDocument3 pagesTest Bank For Pathophysiology 6th Edition Jacquelyn L BanasikKenneth Maestas100% (27)
- 2021 Thrombocytopenia and Intracranial Venous Sinus Thrombosis AfterDocument10 pages2021 Thrombocytopenia and Intracranial Venous Sinus Thrombosis AfterBeatriz VásquezNo ratings yet
- Tuberculosis-Associated HLH in An 8-Month-Old Infant: A Case Report and ReviewDocument8 pagesTuberculosis-Associated HLH in An 8-Month-Old Infant: A Case Report and Reviewnia nofilia widartoNo ratings yet
- Coronavirus VipitguidanceDocument5 pagesCoronavirus VipitguidanceVijay ShankarNo ratings yet
- Anticoagulation Guidance Emerging For Severe COVID-19Document11 pagesAnticoagulation Guidance Emerging For Severe COVID-19danielaNo ratings yet
- tmp9204 TMPDocument4 pagestmp9204 TMPFrontiersNo ratings yet
- Nice Guidelines For VteDocument512 pagesNice Guidelines For VtesilcmtgNo ratings yet
- Developments and Quality Assurance in Stem Cell TransplantationDocument7 pagesDevelopments and Quality Assurance in Stem Cell TransplantationDenySidiqMulyonoChtNo ratings yet
- JTH 14879Document5 pagesJTH 14879miNo ratings yet
- 2018 - Chronic Thromboembolic Pulmonary HypertensionDocument10 pages2018 - Chronic Thromboembolic Pulmonary HypertensionSebastian PuertoNo ratings yet
- Fa y StrokeDocument11 pagesFa y StrokeCatherine Galdames HinojosaNo ratings yet
- Brain Behavior and ImmunityDocument4 pagesBrain Behavior and ImmunityRached ZeghlacheNo ratings yet
- AnalitikDocument17 pagesAnalitikwecytriaNo ratings yet
- 9515-Article Text-70471-1-10-20200725Document20 pages9515-Article Text-70471-1-10-20200725cristina_zaharia865440No ratings yet
- NICE 2010 Guidelines On VTEDocument509 pagesNICE 2010 Guidelines On VTEzaidharbNo ratings yet
- Pulmonary Embolism - European Heart Journal 2012Document12 pagesPulmonary Embolism - European Heart Journal 2012Andreas IoannouNo ratings yet
- Critical Care and Emergency Medicine Neurology in StrokeDocument3 pagesCritical Care and Emergency Medicine Neurology in StrokeAnca GuțuNo ratings yet
- Guidance Sponsors How Manage Clinical Trials During Covid 19 Pandemic - enDocument2 pagesGuidance Sponsors How Manage Clinical Trials During Covid 19 Pandemic - enSerban RosuNo ratings yet
- Pseudothrombocytopenia-A Review On Causes, Occurrence and Clinical ImplicationsDocument19 pagesPseudothrombocytopenia-A Review On Causes, Occurrence and Clinical ImplicationsGABRIELA HERRERANo ratings yet
- American J Hematol - 2023 - PanseDocument14 pagesAmerican J Hematol - 2023 - PanseMaria GarciaNo ratings yet
- Amniotic Fluid Embolism: About A CaseDocument4 pagesAmniotic Fluid Embolism: About A CaseIJAR JOURNALNo ratings yet
- Use of Chloroquine in Asymptomatic Elderly Covid19 Patients, A Placebo or Rather A Source of Complications: A Case ReportDocument8 pagesUse of Chloroquine in Asymptomatic Elderly Covid19 Patients, A Placebo or Rather A Source of Complications: A Case ReportIJAR JOURNALNo ratings yet
- Main PDFDocument8 pagesMain PDFrubramNo ratings yet
- Thrombosis Research: A B C D e F G A e A A 1 F 1Document3 pagesThrombosis Research: A B C D e F G A e A A 1 F 1Natasya IntanNo ratings yet
- Ddesewfaegftsegrhdtr 64 Ty 3 HyDocument1 pageDdesewfaegftsegrhdtr 64 Ty 3 Hygfaefrearfet34tr3r53No ratings yet
- Int J Clinical Practice - 2014 - Kröger - Venous Thromboembolism in Germany Results of The GermAn VTE RegistryDocument6 pagesInt J Clinical Practice - 2014 - Kröger - Venous Thromboembolism in Germany Results of The GermAn VTE Registrysanto sNo ratings yet
- 10-Mog Vs SPH in InvasiveDocument8 pages10-Mog Vs SPH in InvasiveYasmine AbbaouiNo ratings yet
- Guidance Version 17 On MNGMT of Vitt 20210420Document5 pagesGuidance Version 17 On MNGMT of Vitt 20210420Abd El-rahman MohamedNo ratings yet
- Cytokine Septic ShockDocument13 pagesCytokine Septic ShockEduardo ChanonaNo ratings yet
- 2020 Thromb J Thrombosis Management in Times of COVID-19 Epidemy A Dutch PerspectiveDocument2 pages2020 Thromb J Thrombosis Management in Times of COVID-19 Epidemy A Dutch Perspectivenilmania_01No ratings yet
- Clinical Practice Guideline: Tonsillitis I. Diagnostics and Nonsurgical ManagementDocument15 pagesClinical Practice Guideline: Tonsillitis I. Diagnostics and Nonsurgical ManagementTuti Nursyah PutriNo ratings yet
- Balam I 2012 Compli HipDocument18 pagesBalam I 2012 Compli HipRosario RosarioNo ratings yet
- 508 - 7 CardiologyDocument9 pages508 - 7 CardiologymlinaballerinaNo ratings yet
- COVID 19 in People Living With Human Immunodeficiency Virus: A Case Series of 33 PatientsDocument6 pagesCOVID 19 in People Living With Human Immunodeficiency Virus: A Case Series of 33 PatientsherrerachaimNo ratings yet
- Common Procedures and Conditions Leading To Inpatient Hospital Admissions in Adults With and Without Diabetes From 2015 To 2019 in GermanyDocument11 pagesCommon Procedures and Conditions Leading To Inpatient Hospital Admissions in Adults With and Without Diabetes From 2015 To 2019 in GermanyEva ArdianahNo ratings yet
- Bilateral Massive Pulmonary Embolism On Disseminated Intravascular Coagulation (DIVC) After Severe Postpartum HaemorrhageDocument8 pagesBilateral Massive Pulmonary Embolism On Disseminated Intravascular Coagulation (DIVC) After Severe Postpartum HaemorrhageAji NugrozzNo ratings yet
- Hemoptysis Revealing Intracardiac Thrombosis: A Case Report of Behcets DiseaseDocument5 pagesHemoptysis Revealing Intracardiac Thrombosis: A Case Report of Behcets DiseaseIJAR JOURNALNo ratings yet
- 2019 European Stroke Organisation Guideline On Reversal of Oral Anticoagulants in Acute Intracerebral HaemorrhageDocument13 pages2019 European Stroke Organisation Guideline On Reversal of Oral Anticoagulants in Acute Intracerebral HaemorrhageSoda SodaNo ratings yet
- Vaccine-Induced Immune Thrombocytopenia and Thrombosis (VITT)Document4 pagesVaccine-Induced Immune Thrombocytopenia and Thrombosis (VITT)Ravi KumarNo ratings yet
- Journal of Critical Care: Matthew F. Whelihan, PHD, Armin Kiankhooy, MD, Kathleen E. Brummel-Ziedins, PHDDocument7 pagesJournal of Critical Care: Matthew F. Whelihan, PHD, Armin Kiankhooy, MD, Kathleen E. Brummel-Ziedins, PHDJoséRafaelArmasNo ratings yet
- A Practical Guide For The Prevention and Treatment of VTE and Management of Anaemia and Coagulopathy in COVID-19Document14 pagesA Practical Guide For The Prevention and Treatment of VTE and Management of Anaemia and Coagulopathy in COVID-19Jye yiNo ratings yet
- SICH MGMTDocument12 pagesSICH MGMTLennon Ponta-oyNo ratings yet
- Ehac 515Document18 pagesEhac 515Phuoc NguyenNo ratings yet
- Lesoes Cisticas HIVDocument5 pagesLesoes Cisticas HIVAndrey Barbosa PimentaNo ratings yet
- Hta (G4)Document9 pagesHta (G4)Juan LeonNo ratings yet
- Elevada Variabilidad Interpersonal en AlemaniaDocument11 pagesElevada Variabilidad Interpersonal en AlemaniaFernando DominguezNo ratings yet
- Bibliografia 14850 PDFDocument16 pagesBibliografia 14850 PDFMahtosurup GodavarthyNo ratings yet
- Monte Cuc Co 2015Document21 pagesMonte Cuc Co 2015Silvana Reyes ZavaletaNo ratings yet
- JurnalDocument6 pagesJurnalSiska SulistiyowatiNo ratings yet
- Chronic Immune Thrombocytopenia in ChildhoodDocument3 pagesChronic Immune Thrombocytopenia in Childhoodfitri asymidaNo ratings yet
- Evw Adq ManucciDocument6 pagesEvw Adq Manuccimaria perezNo ratings yet
- Thomalla, G (2013) - WAKE - UP ACVDocument8 pagesThomalla, G (2013) - WAKE - UP ACVVictorNo ratings yet
- Moreau Et Al. - 2023 - The Use of Induced Hypothermia in Extracorporeal MDocument13 pagesMoreau Et Al. - 2023 - The Use of Induced Hypothermia in Extracorporeal Mgavain.ferronsNo ratings yet
- COVID-19-associated Immune ThrombocytopeniaDocument7 pagesCOVID-19-associated Immune ThrombocytopeniaDr Varshil ShahNo ratings yet
- Article: Ferrata Storti FoundationDocument10 pagesArticle: Ferrata Storti FoundationAbdurrahman HasanuddinNo ratings yet
- Hypotheses Behind The Very Rare Cases of Thrombosis With Thrombocytopenia Syndrome After SARS-CoV-2 VaccinationDocument10 pagesHypotheses Behind The Very Rare Cases of Thrombosis With Thrombocytopenia Syndrome After SARS-CoV-2 VaccinationAna-Maria AursuleseiNo ratings yet
- Management of Hemoptysis in Inflammatory Chest Diseases: Tugba Cosgun, Alper TokerDocument6 pagesManagement of Hemoptysis in Inflammatory Chest Diseases: Tugba Cosgun, Alper TokerNatalindah Jokiem Woecandra T. D.No ratings yet
- Wa0009.Document10 pagesWa0009.JoelGámezNo ratings yet
- British Columbia (Public Service Employee ReDocument32 pagesBritish Columbia (Public Service Employee ReChristine GildensternNo ratings yet
- Unit 2. The Vital Functions of Human BeingsDocument11 pagesUnit 2. The Vital Functions of Human BeingsAlfonso Macias Martin100% (1)
- Regulation of ErythropoiesisDocument3 pagesRegulation of ErythropoiesisFlowerNo ratings yet
- AVIATION Flight Physiology: - Kirk Michael WebsterDocument56 pagesAVIATION Flight Physiology: - Kirk Michael WebsterabriowaisNo ratings yet
- Biology C - Lesson 1 - Circulatory SystemDocument46 pagesBiology C - Lesson 1 - Circulatory SystemMuhammad Azrie0% (1)
- Mark Scheme (Results) January 2013: International GCSE Biology (4BI0) Paper 1BDocument20 pagesMark Scheme (Results) January 2013: International GCSE Biology (4BI0) Paper 1BJohn HopkinsNo ratings yet
- Autoregulation and Capillary Dynamics: Graphics Are Used With Permission ofDocument10 pagesAutoregulation and Capillary Dynamics: Graphics Are Used With Permission ofUta Provinsiana SukmaraNo ratings yet
- Anatomy and Physiology of NeonatesDocument17 pagesAnatomy and Physiology of NeonatesYu ShiNo ratings yet
- Lab Report 1 (Hematology)Document8 pagesLab Report 1 (Hematology)Romanda GreeneNo ratings yet
- Haematology Test Result Unit Biological Ref. Interval Prothrombin TimeDocument6 pagesHaematology Test Result Unit Biological Ref. Interval Prothrombin TimeNidhi RakeshNo ratings yet
- CLS Aipmt 18 19 XIII Zoo Study Package 3 SET 1 Chapter 12Document30 pagesCLS Aipmt 18 19 XIII Zoo Study Package 3 SET 1 Chapter 12Saravanan Raju100% (1)
- Amphibian HematologyDocument18 pagesAmphibian HematologyGabi OliveiraNo ratings yet
- IJSO Biology Module - 3Document207 pagesIJSO Biology Module - 3Ikhbaat Atiqur RehmanNo ratings yet
- Hyper Bilirubin Emi ADocument36 pagesHyper Bilirubin Emi ASai Krishna MaddiralaNo ratings yet
- Blood Pressure ChartDocument4 pagesBlood Pressure ChartMelvyn Chavez MauricoNo ratings yet
- ANATOMYDocument3 pagesANATOMYKara Faith DeocadesNo ratings yet
- Collection TubeDocument6 pagesCollection TubeChristiane ReaNo ratings yet
- FOLIO: Biology Form 4 Chapter 2: Cell Structure and OrganisationDocument51 pagesFOLIO: Biology Form 4 Chapter 2: Cell Structure and OrganisationSashimi 刺身 Chebby100% (1)
- Episode No. 8 Title: The Circulatory System: No Erasures of Any FormDocument3 pagesEpisode No. 8 Title: The Circulatory System: No Erasures of Any FormRalph Martin S. RIVERANo ratings yet
- Science Sample Paper 2Document8 pagesScience Sample Paper 2LVAM GAMINGNo ratings yet