Professional Documents
Culture Documents
Pathophysiology: Hemolytic Diseases of The Fetus and Newborn
Pathophysiology: Hemolytic Diseases of The Fetus and Newborn
Uploaded by
pixiedustOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathophysiology: Hemolytic Diseases of The Fetus and Newborn
Pathophysiology: Hemolytic Diseases of The Fetus and Newborn
Uploaded by
pixiedustCopyright:
Available Formats
Francisco Frances Lorraine R.
Immunohematology
17-2-00897 Ms. KATELYN JOY DAÑO
Hemolytic Diseases of the Fetus and Newborn
Pathophysiology
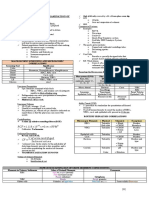
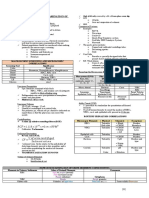
Maternal alloantibodies cross the placenta, enter the fetal circulation and cause hemolysis. Depending on
severity, hemolysis can lead to bilirubin in amniotic fluid, fetal anemia and hydrops fetalis.
Alloimmnunization via
Previous transfusion
Previous pregnancy
Current pregnancy (CVS, amniocentesis, trauma, spontaneous/elective abortion
Severity of disease determined by
IgG subclass
Amount of antibody
Number of antigenic sites on red cells
Etiology
ABO HDFN - Leading cause of HDFN. Usually group O mom and group A or B child. Unlike other groups, O
patients have IgG (antiA,B antibody) that crosses the placenta into fetal circulation – Since these ABO antibodies are
naturally occurring, interaction can occur during the first pregnancy. Hemolysis is very mild since fetal/neonatal RBC’s
only have weak ABO antigen expression. HDFN due to Kell is the most common cause of severe HDFN followed by anti-c
– Kell is present on fetal RBC’s, unlike other antigens. Classic HDFN is caused by anti-D antibodies which is usually not
seen in first pregnancy.
Diagnosis
Titers less than 1:16 have very low risk of hemolysis. Titers greater than 1:16 warrant monitoring for fetal
hemolysis. Indications for RhIG D- woman with a D+ or D-unknown fetus – Ppx= 300 μg (full vial) at 28 wks and at term –
Fetomaternal hemorrhage of unknown qty (ectopic, amnio, CVS)= 50 μg (small vial) in first 12 wks of gestation and 300
μg (full vial) after 12 wks
Prevention
D- women should be checked for anti-D ab:
– If she does not have anti-D antibodies, give prophylactic doses of RhIg at 28 weeks gestation and anytime there is
fetomaternal hemorrhage
– If she does have anti-D antibodies, maternal antibody titer is determined; if titer is high,
monitor fetal hemolysis -- intrauterine transfusion or early delivery may be necessary
You might also like
- RH and Abo IncompatibilityDocument10 pagesRH and Abo IncompatibilityamitNo ratings yet
- 2001-Haemolytic Disease of Newborn.Document6 pages2001-Haemolytic Disease of Newborn.蔡黑面No ratings yet
- Rhalloimmunization 180317110948Document57 pagesRhalloimmunization 180317110948BIRHANE TESFAYNo ratings yet
- BB OriginalDocument14 pagesBB Originalstone siehNo ratings yet
- Iso-Immunization in Pregnancy: Hydrops FoetalisDocument4 pagesIso-Immunization in Pregnancy: Hydrops FoetalisRaju PariharNo ratings yet
- CP Conference Hemolytic Disease of The Fetus and Newborn (HDFN)Document17 pagesCP Conference Hemolytic Disease of The Fetus and Newborn (HDFN)fathogNo ratings yet
- Topic Rhesus IncompatibilityDocument4 pagesTopic Rhesus IncompatibilityMechkar KatherinNo ratings yet
- Share 'RH Neg Final - 23.6Document80 pagesShare 'RH Neg Final - 23.6AppuNo ratings yet
- RH. Lesson PlanDocument14 pagesRH. Lesson PlanNithiya NadesanNo ratings yet
- Hemolytic Disease of The NewbornDocument7 pagesHemolytic Disease of The NewbornLara CarisaNo ratings yet
- Haemolytic Disease of The NewbornDocument46 pagesHaemolytic Disease of The Newborntan_kit_1100% (1)
- Introduction To Alloimmune Disorders of PregnancyDocument46 pagesIntroduction To Alloimmune Disorders of PregnancyDr.Marva YusafzaiNo ratings yet
- RH IsoimmunizationDocument47 pagesRH IsoimmunizationDuncan JacksonNo ratings yet
- Rhesus Iso-ImmunizationDocument20 pagesRhesus Iso-Immunizationahmed shorshNo ratings yet
- RH Incompatibility New For MDDocument65 pagesRH Incompatibility New For MDMd AtifNo ratings yet
- Jurnal Internasional 3Document4 pagesJurnal Internasional 3P17312215223 LINDA ANISANo ratings yet
- RH DiseaseDocument25 pagesRH Diseasepoongodi cNo ratings yet
- The High Risk Prenatal ClientDocument25 pagesThe High Risk Prenatal ClientAngelie RojasNo ratings yet
- Republic of The Philippines University of Northern Philippines College of NursingDocument3 pagesRepublic of The Philippines University of Northern Philippines College of NursingCatherine PradoNo ratings yet
- Erythroblastosis FetalisDocument3 pagesErythroblastosis Fetalisdanica jeanNo ratings yet
- Chapter 10 - Hemolytic Disease of The Fetus and New BornDocument79 pagesChapter 10 - Hemolytic Disease of The Fetus and New BornKorsaNo ratings yet
- TUGAS DR - Chris - BAB 48 - Neonatal Alloimmune ThrombocytopeniaDocument11 pagesTUGAS DR - Chris - BAB 48 - Neonatal Alloimmune ThrombocytopeniaGrindin' ShoeNo ratings yet
- Haemolytic Disease of The Fetus and Newborn: ReviewDocument15 pagesHaemolytic Disease of The Fetus and Newborn: ReviewBEREKETNo ratings yet
- RH Incompatability FinalDocument27 pagesRH Incompatability Finalsanthiyasandy100% (2)
- 1Document4 pages1James Victor Villanueva100% (2)
- Allofetus of NewbornDocument9 pagesAllofetus of NewbornSameerKHNo ratings yet
- RH DiseaseDocument9 pagesRH DiseaseYerra SukumalaNo ratings yet
- RhAbo IncompamtabilityDocument19 pagesRhAbo Incompamtability22-56354No ratings yet
- Rhesus Isoimmunization: DR Esgair Alzahra MBBCH, Dog, AbogDocument58 pagesRhesus Isoimmunization: DR Esgair Alzahra MBBCH, Dog, AbogWendy Evans100% (1)
- Nascimento Et Al. - 2012 - Bloody Nipple Discharge in Infancy - Report of Two CasesDocument3 pagesNascimento Et Al. - 2012 - Bloody Nipple Discharge in Infancy - Report of Two CasesflashjetNo ratings yet
- Evaluation and Treatment of Fetal Exposure To Toxoplasmosis 2015Document6 pagesEvaluation and Treatment of Fetal Exposure To Toxoplasmosis 2015Khalila DiantiNo ratings yet
- Sam,+frequency and Types of Red Cell Alloantibodies in Pregnant Females 6Document5 pagesSam,+frequency and Types of Red Cell Alloantibodies in Pregnant Females 6Luján GómezNo ratings yet
- Iufd Bali 2006Document26 pagesIufd Bali 2006Andy YusrizalNo ratings yet
- Erythroblastosis Case StudyDocument19 pagesErythroblastosis Case StudyMaricel Agcaoili GallatoNo ratings yet
- Haemolytic Disease of The Fetus andDocument16 pagesHaemolytic Disease of The Fetus andkallaliNo ratings yet
- Hemolytic Disease of The Newborn A ReviewDocument11 pagesHemolytic Disease of The Newborn A ReviewririlibertiNo ratings yet
- Immunology in Pregnancy & Coagulation Failure in PregnancyDocument30 pagesImmunology in Pregnancy & Coagulation Failure in PregnancySrikutty DevuNo ratings yet
- Red Cell AlloimmunizationDocument54 pagesRed Cell Alloimmunizationበአምላክ ጋሻዬ በዛNo ratings yet
- Hemolytic Disease of The NewbornDocument43 pagesHemolytic Disease of The Newbornalibayaty1No ratings yet
- RH Negative Pregnancy: DR ShwetaDocument30 pagesRH Negative Pregnancy: DR ShwetaZaenNiasNo ratings yet
- 11pediatrics in Review 2011 Del Pizzo 537 42Document8 pages11pediatrics in Review 2011 Del Pizzo 537 42Minerva StanciuNo ratings yet
- Hemolytic Diseases of The Newborn PDFDocument9 pagesHemolytic Diseases of The Newborn PDFsaritha OrugantiNo ratings yet
- Amniotic Fluid - Fetal DistressDocument26 pagesAmniotic Fluid - Fetal DistressJanielle FajardoNo ratings yet
- Alloimmunization in PregnancyDocument26 pagesAlloimmunization in PregnancyYona MbalibulhaNo ratings yet
- Government College of Nursing Jodhpur (Raj.) : Procedure On-Amniocentesis Subject-Obstetrics & Gynaecology Specialty-IDocument7 pagesGovernment College of Nursing Jodhpur (Raj.) : Procedure On-Amniocentesis Subject-Obstetrics & Gynaecology Specialty-Ipriyanka100% (1)
- Lucena2019 PDFDocument7 pagesLucena2019 PDFSaddam FuadNo ratings yet
- Inkompatibilitas DarahDocument3 pagesInkompatibilitas DarahIntan PermataNo ratings yet
- Hemolytic Disease of The FetusDocument14 pagesHemolytic Disease of The FetusGrindin' ShoeNo ratings yet
- 11 - HDNDocument16 pages11 - HDNجير يكو (جيريكو)No ratings yet
- Abortion: Pregnancy Termination or Loss Before 20 Weeks' Gestation or With A Fetus Delivered Weighing 500 G Early Pregnancy LostDocument2 pagesAbortion: Pregnancy Termination or Loss Before 20 Weeks' Gestation or With A Fetus Delivered Weighing 500 G Early Pregnancy LostKristine Jade OdtujanNo ratings yet
- Clinical Case Analysis - PromDocument4 pagesClinical Case Analysis - PromSiobhan GreeneNo ratings yet
- Pregnancy Embryo Fetus Survive Outside The Uterus Miscarriage Induced AbortionDocument29 pagesPregnancy Embryo Fetus Survive Outside The Uterus Miscarriage Induced AbortionAleena DavisNo ratings yet
- Wa0015.Document50 pagesWa0015.LUCKYNo ratings yet
- Pre EclampsiaDocument12 pagesPre EclampsiaJohn Mark PocsidioNo ratings yet
- 2003 - 01 - 01 Steinborn-Scharf-Soluble HLA-DR Levels in The Maternal CirculationDocument7 pages2003 - 01 - 01 Steinborn-Scharf-Soluble HLA-DR Levels in The Maternal CirculationAlexander ScharfNo ratings yet
- NCM 109 ReviewerDocument8 pagesNCM 109 ReviewerAlma Janella TOSINO100% (2)
- HEMOLYTIC DISEASE OF THE NEWBORN - Docx PrintDocument6 pagesHEMOLYTIC DISEASE OF THE NEWBORN - Docx PrintJudy HandlyNo ratings yet
- Congenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementFrom EverandCongenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDiva D. De León-CrutchlowNo ratings yet
- Food Protein Induced Enterocolitis (FPIES): Diagnosis and ManagementFrom EverandFood Protein Induced Enterocolitis (FPIES): Diagnosis and ManagementTerri Faye Brown-WhitehornNo ratings yet
- Alert Medical Series: USMLE Alert I, II, IIIFrom EverandAlert Medical Series: USMLE Alert I, II, IIIRating: 2 out of 5 stars2/5 (1)
- Holy Child Jesus Montessori: School of Dasmariñas, Incorporated S.Y.2020-2021Document2 pagesHoly Child Jesus Montessori: School of Dasmariñas, Incorporated S.Y.2020-2021pixiedustNo ratings yet
- Rarwardqaarmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwardqaarmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedust100% (1)
- Rarwrdqaarmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwrdqaarmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedustNo ratings yet
- Rarwrdqrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwrdqrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedustNo ratings yet
- Rarwrdrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwrdrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedustNo ratings yet
- Rarwrrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwrrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedustNo ratings yet
- Rarwrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMDocument13 pagesRarwrmicroscopic Examination of Urine: RCF 1.118 X 10 XR CMXRPMpixiedustNo ratings yet
- Blood Components (E-Learning Activity) : Francisco, Frances Lorraine RDocument3 pagesBlood Components (E-Learning Activity) : Francisco, Frances Lorraine RpixiedustNo ratings yet
- GAS LAWS - QUIZ 1lolDocument1 pageGAS LAWS - QUIZ 1lolpixiedustNo ratings yet
- Nasugbu: Commission Slip Commission SlipDocument1 pageNasugbu: Commission Slip Commission SlippixiedustNo ratings yet