Professional Documents
Culture Documents
Current Concepts in The Management of Enterocutane
Current Concepts in The Management of Enterocutane
Uploaded by
nur hasnahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Current Concepts in The Management of Enterocutane
Current Concepts in The Management of Enterocutane
Uploaded by
nur hasnahCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/324762302
Current concepts in the management of enterocutaneous fistula
Article in International Surgery Journal · April 2018
DOI: 10.18203/2349-2902.isj20181836
CITATION READS
1 1,122
2 authors, including:
Promise Nnamd Wichendu
University of Port Harcourt Teaching Hospital
13 PUBLICATIONS 21 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Management of symptomatic gall stone disease in a tertiary care hospital in southern Nigeria View project
All content following this page was uploaded by Promise Nnamd Wichendu on 30 May 2018.
The user has requested enhancement of the downloaded file.
International Surgery Journal
Dodiyi-Manuel A et al. Int Surg J. 2018 Jun;5(6):1981-1985
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20181836
Review Article
Current concepts in the management of enterocutaneous fistula
Amabra Dodiyi-Manuel*, Promise N. Wichendu
Department of Surgery, University of Port Harcourt Teaching Hospital, Port Harcourt, Rivers State, Nigeria
Received: 23 March 2018
Accepted: 17 April 2018
*Correspondence:
Dr. Amabra Dodiyi-Manuel,
E-mail: dodman_05@yahoo.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Enterocutaneous fistula is an abnormal connection between the intra-abdominal gastrointestinal tract and skin. It
causes considerable morbidity and mortality. The goals of management are restoration of gastrointestinal continuity
and allowance of enteral nutrition with minimal morbidity and mortality. A multidisciplinary approach is essential in
the successful management and this has led to closure rates ranging from 5-20% following conservative management
and 75-85% with operative treatment. This article seeks to review the current concepts in the management of
enterocutaneous fistula. A systematic search of literature on enterocutaneous fistula was conducted. Relevant
materials were selected and selected references from relevant books, journal articles and abstracts using Medline,
Google scholar and Pubmed databases were critically reviewed. Enterocutaneous fistulas can be classified by the
anatomy, aetiology or physiology. Anatomically, enterocutaneous fistula has been classified based on the organ of
origin and this is useful in the consideration of management options: type l (abdominal oesophageal and
gastroduodenal fistula), type ll (small bowel fistula), type lll (large bowel fistula) and type IV (enteroatmospheric,
regardless of origin. The anatomy also depends on the presence or absence of associated abscess cavity and the length
and characteristics of the fistula tract. Aetiologically, the majority of enterocutaneous fistulas are iatrogenic (75-85%)
while between 15 and 25% occur spontaneously. The physiological classification is based on the volume of its output.
High output fistulas drain more than 500mls in 24 hours, moderate output between 200 and 500mls in 24 hours and
low output less than 200mls in 24 hours. Successful management requires a multidisciplinary approach and would
consist of initial resuscitaion with fluids and electrolytes, control of sepsis, good and adequate nutrition, wound care
and skin protection and definitive management. The treatment of enterocutaneous fistula is multidisciplinary and
remains a challenge despite the recent improvement in supportive care. Once enterocutaneous fistula occurs, adequate
stabilization of the patient and non-operative management should be commenced. If surgery is required, careful
planning, meticulous dissection, restoration of bowel continuity and reconstruction of abdominal wall are critical.
Keywords: Closure, Enterocutaneous fistula, Management
INTRODUCTION remains a challenge to surgeons today with mortality
remaining at 5-15%.1,2 The goals of management are
Enterocutaneous fistula is an abnormal connection restoration of gastrointestinal continuity and allowance of
between the intra-abdominal gastrointestinal tract and enteral nutrition with minimal morbidity and mortality. A
skin.It is one of the most disheartening experiences to multidisciplinary approach is essential in the successful
both the surgeon and the physician. In spite of the management which is either by operative and non-
advances made in critical care, antibiotics and nutritional operative means. This involves optimal medical
support, the management of enterocutaneous fistula management, good and meticulous surgical technique
where indicated with social and emotional support for
International Surgery Journal | June 2018 | Vol 5 | Issue 6 Page 1981
Dodiyi-Manuel A et al. Int Surg J. 2018 Jun;5(6):1981-1985
patients and their families. This has led to closure rates MANAGEMENT
ranging from 5-20% following conservative management
and 75-85% with operative treatment.3,4 In spite of the Successful management of enterocutaneous fistula
improvement in mortality rates over the past 4 decades, requires a multidisciplinary approach involving the
leading institutions have reported high morbidity rates of surgeon, wound and ostomy nurses, specialized nutrition
over 85%.5 Mortality has been attributed to sepsis, support team, intensive care and general floor nursing,
malnutrition and fluid and electrolyte imbalance.6,7 physiological and occupational therapy, medical social
Predictive factors of high mortality are infectious and non workers, pain management, psychiatry, palliative care
infectious complications, high output fistula and age.8-10 and spiritual support services.17 This multidisciplinary
approach has led to 50% decrease in mortality.18
This article seeks to review the current concepts in the
management of enterocutaneous fistula. Initial resuscitation
METHODS The aim of resuscitation is to restore intravascular
volume and optimize oxygen carrying capacity.12 Fluid
A systematic search of literature on enterocutaneous and electrolyte losses should be replaced with
fistula was conducted. Relevant materials were selected crystalloids. Patients that are severely dehydrated and
and selected references from relevant books, journal have electrolyte derrangements will require assessment of
articles and abstracts using Medline, Google scholar and their renal functions and electrolytes regularly. There
Pubmed databases were critically reviewed. should be daily assessment of intake and output. Sodium,
potassium and magnesium are the electrolytes that often
CLASSIFICATION require significant supplementation.19 Replacement
should be done in high output small intestinal fistula with
Enterocutaneous fistulas can be classified by the normal saline and 10mmol of potassium chloride.20
anatomy, aetiology or physiology and these will Placement of central venous catheter may be required for
contribute to the morbidity, mortality and likelihood of haemodynamic monitoring especially when sepsis is
spontaneous closure.8,11-12 suspected.
Anatomically, enterocutaneous fistula has been classified Control of sepsis
based on the organ of origin and this is useful in the
consideration of management options: type l (abdominal Sepsis is a major source of morbidity and responsible for
oesophageal and gastroduodenal fistula), type ll (small about 77% of mortality in patients with enterocutaneous
bowel fistula), type lll (large bowel fistula) and type IV fistula.9 Computerized tomography (CT) scan of the
(enteroatmospheric, regardless of origin.11 The anatomy abdomen and pelvis together with percutaneous drainage
also depends on the presence or absence of associated with radiological guidance is essential to evaluate and
abscess cavity and the length and characteristics of the treat the source of infection. When enhancing contrast
fistula tract i.e. simple fistula has single and direct tract media are used, CT scan has an accuracy of greater than
while complex fistula has multiple tracts or an associated 97%.21 Ultrasound scan and magnetic resonance imaging
abscess cavity. It is also classified into an end fistula (the (MRI) can also be used as adjuncts. Percutaneous
entire circumference of the bowel wall is involved in the drainage may also decompress a complex fistula and
fistula) and lateral fistula (part of the bowel wall is convert it to a simple one. In cases of peritonitis and
involved). Aetiologically, the majority of inability to control the source with conservative
enterocutaneous fistulas are iatrogenic (75-85%) while measures, prompt fluid resuscitation, antibiotics
between 15 and 25% occur spontaneously.13 Causes of administration and operative control of infection are
spontaneous fistula include inflammatory bowel diseases essential.9
(commonest), malignancy, appendicitis, diverticulitis,
radiation, tuberculosis/actinomycosis and ischaemia.13 Broad spectrum antibiotics should be started at the onset
of sepsis and cultures taken from all possible sources of
The physiological classification is based on the volume of infection.22 Antibiotics should then be tailored to the
its output. High output fistulas drain more than 500mls in results from culture and sensitivity and reserved for
24 hours, moderate output between 200 and 500mls in 24 patients with ongoing sepsis with special consideration
hours and low output less than 200mls in 24 hours.12,13 given to fungal infections.12 The indiscriminate use of
Monitoring of the volume and character of output of the antibiotics should be avoided as this may lead to selection
fistula can guide nutritional support and resuscitation. of highly resistant pathogens that may cause untreatable
Fistula output has been documented to predict likelihood overwhelming infections. Empiric antibiotic coverage
of spontaneous closure and mortality.9,14,15 Other should not exceed 4 to 7 days.23,24 There is no role for
physiologic features that predict spontaneous closure rate antibiotic coverage in patients whose sepsis is fully
include absence of sepsis, good nutritional status and low controlled with percutaneous drainage.23 Resolution of
C- reactive protein to albumin ratio.16 sepsis is essential to achieve spontaneous closure of
enterocutaneous fistula.19
International Surgery Journal | June 2018 | Vol 5 | Issue 6 Page 1982
Dodiyi-Manuel A et al. Int Surg J. 2018 Jun;5(6):1981-1985
Nutrition increase the rate of fistula closure.19 However, they
decrease acidity and quantity of gastric secretions and are
Basically, there are 3 sources of malnutrition in patients recommended as part of atandard treatment regimen in
with enterocutaneous fistula: inadequate calorie intake, high output fistula.6,12,17 Sucrafate can also be used for its
catabolism related to ongoing sepsis and ongoing losses gastric neutralizing and constipating effects.12
from the gastrointestinal tract.25 The basal energy needs Antidiarrheal agents like loperamide,
of a healthy adult can be estimated using the Harris- codeine,diphenoxylate/atropine have been used to
Benedict equation and a patient with enterocutaneous decrease fistula output.19 In a British Intestinal Failure
fistula will require 1 to 2.5 times of the basal energy Centre, up to 40mg/day of loperamide and 240mg/day of
needs.25 codeine are being used to control refractory high output
fistulas with success.17,28
Generally, patients with enterocutaneous fistula require
25-32 kcal/kg/day, with a calorie to nitrogen ratio ranging Somatostatin and its long acting analogue octreotide have
from 150 to 200:1, and a protein intake of 1.5g/kg/day, been useful in reducing fistula effluent. In fistulas that are
taking into account adjustments for metabolic stress and more likely to close on conservative management,
fistula losses.12,26 After initial resuscitation with fluids somastostatin and octreotide will decrease output and
and electrolytes and control of sepsis, parenteral nutrition time to closure but there will be no increase in non-
is started in high output fistula and enteral nutrition in operative closure rate.2,12,31-33 Some complications that
low output fistula patients.19 may occur following the use of octreotide decrease
perfusion in the splanchnic and portal circulation,
Parenteral nutrition is an established part of management worsening cholestasis and possible adverse effect on
of enterocutaneous fistula.15 Its institution can help meet immune system.34,35
the nutritional demands of the patient while minimizing
the flow of enteric contents through the fistula. Despite Wound care and skin protection
the fact that reduction of flow through the intestinal tract
and fistula output are associated with increased non- Skin care and control of fistula output should be started
operative closure rates, enteral nutrition remains an as soon as the diagnosis is made to decrease local skin
important factor in the maintenance of mucosal barrier excoriation and inflammation, pain and infection. Low
and integrity, optimization of the immune and hormonal output fistulas can be controlled with wet to dry dressing
function of the bowel and prevention of sepsis by or dry gauze, while moderate output fistulas with an
improving hepatic protein synthesis.12,27 As little as 20% ostomy appliance with appropriate skin protection around
of calorie requirement administered administered the fistula in the form of adhesive ring paste, powder or
enterally can achieve these effects.12 For enteral feeding hydrophilic dressing.36 In high output fistulas, several
to be moderately successful, about 4 feet of healthy types of collection device exist such as ostomy
intestine is needed from the ligament of Treitz to the appliances, wound managers, pouching systems that can
external fistula opening.19 be collected to wall sunction. Negative pressure dressings
are a relatively recent development in the management of
Attempts at oral nutrition can be made in high output complex wounds. While some authors have published
fistula with the following modifications28: i) Limit intake their experience with vacuum assisted closure (VAC)
of low sodium fluids to 500mls/kg/day, ii) Provide devices to protect the skin, promote wound contraction or
patient with oral solution high in sodium (90-120mmol/l close the fistula some others raised the concern that these
sodium content), iii) Small volume of fluid intake with devices can cause recurrent enterocutaneous fistula with
solid meals, iv) Protein pump inhibitor therapy, increased mortality. 2,37-39
antimotility drugs and octreotide. Relative
contraindications to enteral nutrition include insufficient As a result of the fact that negative pressure therapy can
bowel length (˂75cm), intestinal discontinuity, cause bowel injury and lead to fistula formation,
symptomatic intolerance to enteral nutrition, significant interposition of a layer of material between bowel and the
increases in fistula output leading to electrolyte sponge of the device when in use has been recommended
disturbances at start of enteral nutrition and inability to as a cautionary measure.22 The use of fibrin glue has been
establish/maintain feeding access.29 reported in carefully selected patients with favourable
anatomy and physiology.2,40
Fistuloclysis (feeding through the fistula) has been
described and is possible if the fistula is proximal enough Only case series are available for fistula plugs in the
to allow at least 5 feet of small bowel absorption to occur treatment of enterocutaneous fistula. However, they have
in the absence of distal obstruction.22,30 been utilized with some successes in anrectal fistulas.19,22
Medical management Investigations
Acid reduction therapies like H2 receptor antagonists and Fistulogram is done once the patient is stabilized. This
proton pump inhibitors (PPIs) have been shown to will define the source of fistula, the length and course of
International Surgery Journal | June 2018 | Vol 5 | Issue 6 Page 1983
Dodiyi-Manuel A et al. Int Surg J. 2018 Jun;5(6):1981-1985
its tract, presence or absence of bowel continuity, 3. Lynch AC, Delaney CP, Senagore AJ, Connor JT,
presence of distal obstruction and associated abscess Remi FH. Fazio VW. Clinical outcome and factors
cavity.22 Water soluble contrast enemas will rule out predictive of recurrence after enterocutaneous
colonic or small bowel obstruction. CT scan can visualize fistula surgery. Ann Surg. 2004;240:825-31.
abscess cavities and shows abdominal wall defect. MRI is 4. Brenner M, Clayton JL, Tillou A, Hiatt JR, Cryer
helpful when enterocutaneous fistula is due to HG. Risk factors for recurrence after repair of
malignancy or crohn’s disease and helps to define pre enterocutaneous fistula. Arch Surg 2009;144:500-5.
existing shortened intestine.22 5. Connolly PT, Teubner A, Lees LP, Anderson ID,
Scott NA, Carlson GL. Outcome of reconstructive
Definitive management surgery for intestinal fistula in the open abdomen.
Am Surg. 2008;247:440-4.
The conservative measures lasting at least 4 weeks are 6. Lloyd DA, Gabe SM, Windsor AC. Nutrition and
done in almost all patients. These measures allow for management of enterocutaneous fistula. Br J Surg
fistula closure in approximately 4-6 weeks. About 90% of 2006;93:1045-55.
the fistulas destined to close spontaneously will do so 7. Martinez JL, Luque-de-Leon E, Mier J, Blanco-
within this period. However, this occurs in only 30% of Benavides R, Robledo F. Systematic management of
fistulas,41,42 post-operative enterocutaneous fistula: factors
related to outcomes. World J Surg. 2008;323:436-
Conservative management is considered to have failed if 43.
decreased output or fistula closure is not observed after 4 8. Sitges-Sera A, Jaurrieta E, Sitges-Creus A.
weeks of sepsis control, nutritional supplementation and Management of post-operative enterocutaneous
establishing wound care and planning of operative fistulas: the role of parenteral nutrition and surgery.
intervention should be done.12 Requirements before Br J Surg. 1982;69:147-50.
definitive fistula operative intervention include 9. Campos AC, Andrade DF, Campos GM, Matias JE,
nutritional optimization and eradication of sepsis, Coellio JC. A multivariate model to determine
addressing psychological morbidity and clinical evidence prognostic factors in gastrointestinal fistulas. J Am
of softening scars and abdominal wall on examination.19 Coll Surg. 1999;188:483-90.
10. Mawdsley JE, Hollington P, Bassett P, Windsor AJ,
The goal of surgery is reestablishment of gastrointestinal Forbes A, Gabe SM. An analysis of predictive
continuity and soft tissue coverage of intra-abdominal factors for healing and mortality in patients with
contents with abdominal wall closure. Recurrence rates enterocutaneous fistulas. Aliment Pharmacol Ther
are minimized (18%) when the involved bowel is fully 2008;28:1111-21.
mobilized and resected.19 Oversewing or wedge 11. Schein M, Decker GA. Post operative external
resection/bowel repair results in higher recurrence rates at alimentary tract fistulas. Am J Surg. 1991;161:435-
33%.3 8.
12. Evenson AR, Fischer JE. Current management of
CONCLUSION enterocutaneous fistula. J Gastrointest Surg. 2006;
10:455-64.
The treatment of enterocutaneous fistula is 13. Berry SM, Fischer JE. Classification and
multidisciplinary and remains a challenge despite the pathophysiology of enterocutaneous fistula. Surg
recent improvement in supportive care. Once Clin North Am. 1996;76:1009-18.
enterocutaneous fistula occurs, adequate stabilization of 14. Levy E, Frileux P, Cugnenc PH, Honiger J, Oliver
the patient and non-operative management should be JM, Parc R. High-output external fistula of the small
commenced. If surgery is required, careful planning, bowel: management of continuous enteral nutrition.
meticulous dissection, restoration of bowel continuity and Br J Surg. 1989;76:676-9.
reconstruction of abdominal wall are critical. 15. Soeters PB, Ebeid AM, Fischer JE. Review of 404
patients with gastrointestinal fistulas. Impact of
Funding: No funding sources parenteral nutrition. Am Surg. 1979;190:189-202.
Conflict of interest: None declared 16. Harriman S, Rodych N, Hayes P, Moser MA. The
Ethical approval: Not required C-reactive protein to albumin ratio predicts fistula
closure. Am J Surg. 2011;202:175-8.
REFERENCES 17. Hollington P, Mawdsley J, Lim W, Gabe SM,
Forbes A, Windsor AJ. An 11 year experience of
1. Joyce MR, Dietz W. Management of complex enterocutaneous fistula. Br J Surg. 2004;91:1646-
gastrointestinal fistula. Curr Probl Surg 51.
2009;46:384-430. 18. Irving M, White R, Tresadern J. Three years
2. Draus JM Jr, Huss SA, Harty NJ, Cheadle WG, experience with an intestinal failure unit. Am R Coll
Larson GM. Enterocutaneous fistulas: are treatments Surg Engl. 1985;67:2-5.
improving? Surg. 2006;140:570-6.
International Surgery Journal | June 2018 | Vol 5 | Issue 6 Page 1984
Dodiyi-Manuel A et al. Int Surg J. 2018 Jun;5(6):1981-1985
19. Gribovskaja-Rupp I, Melton GB. Enterocutaneous 32. Sancho JJ, diCostanzo J, Nubiola P, Larrad A,
fistula: proven strategies and updates. Clin Colon Bequiristain A, Roqueta F. Randomized double-
Rectal Surg. 2016;29:130-7. blind placebo controlled trial of early octreotide in
20. Schecter WP, Hirshberg A, Chang DS, Harris HW, patients with enterocutaneous fistula. Br J Surg
Napolitano LM, Wexner SD, et al. Enteric fistulas: 1995;82:638-41.
principles of management. J Am Coll Surg. 2009; 33. Torres AJ, Landa JI, Moreno-Azcoita M, Arguello
209:484-91. JM, Sillecchia G, Castro J, et al. SAomatostatin in
21. Kaushal M, Carlson GL. Management of the management of gastrointestinal fistulas. A
enterocutaneous fistula. Clin Colon Rectal Surg multicenter trial. Arch Surg. 1992;127:97-9.
2004;17:79-88. 34. Cooper AM, Braatvedt GD, Qanear MI, Brown H,
22. Haack CI, Gallloway JR, Srinivasan J. Thomas DM, Halliwell M. Fasting and post-prandial
Enterocutaneous fistulas: A look at the causes and splanchnic blood flow is reduced by somatostatin
management. Current Surg Reports. 2014:2:71 analogue (octreotide) in man. Clin Sci.
23. Bleier JI, Hedrick T. Metabolic support of the 1991;81:169-75.
enterocutaneous fistula patient. Clin Colon Rectal 35. Lattuada D, Casnici C, Crotta K, Mastrotto C,
Surg 2010;23:142-8. Franco P, Schmid HA. Inhibitory effect of
24. Dellinger RP, Levy MM, Rhodes A, Annane D, pasireotide and octreotide on lymphocyte activation.
Geriach H, Opal SM, et al. Surviving sepsis J Neuroimmunol. 2007;182:153-9.
campaign: international guidelines for the 36. Brindle CT, Blankenship J. Management of
management of severe sepsis and septic shock: complex wounds with small bowel fistulae: isolation
2012. Crit Care Med. 2013;41:580-637. techniques and exudate control to improve
25. Dudrick SJ, Maharaj AR, Mckelvey aa. Artificial outcomes. J Wound Ostomy Continence Nurs
nutritional support in patients with gastrointestinal 2009;36:396-403.
fistulas. World J Surg. 1999;23:570-6. 37. Alvarez AA, Maxwell GL, Rodriquez GC. Vacuum-
26. Majercik S, Kinikini M, White T. assisted closure for cutaneous gastrointestinal fistula
Enteroatmospheric fistula: from soup to nuts. Nutr management. Gynecol Oncol. 2001;80:413-6.
Clin Pract. 2012;27:507-12. 38. Fischer J. A cautionary note: the use of vacuum-
27. Gianotti L, Alexander JW, Nelson JL, Fukushima R, assisted closure systems in the treatment of
Pyles T, Chalk CL. Role of early enteral feeding and gastrointestinal cutaneous fistula may be associated
acute starvation of post burn bacterial translocation with higher mortality from subsequent fistula
and host defence: prospective randomized trials. development. Am J Surg. 2008;196:1-2.
Crit Care Med. 1994;22:265-72. 39. Rao M, Burke D, Finan PJ, Sagar PM. The use of
28. Datta V, Engledow A, Chan S, Forbes A, Cohen vacuum-assisted closure of abdominal wounds: a
CR, Windsor A. The management of word of caution. Colorectal Dis. 2007;9:266-8.
enterocutaneous fistula in a regional unit in the 40. Rabago LR, Ventosa N, Castro JL, Marco J, Herrera
United Kingdom: a prospective study. Dis Colon N, Gea F. Endoscopic treatment of post operative
Rectum. 2010;53:192-9. fistulas resistant to conservative management using
29. Polk TM, Schwab CW. Metabolic and nutritional biological fibrin glue. Endoscopy. 2002;34:632-8.
support of enterocutaneous fistula patient: a three 41. Roben G. Treatment strategies in 135 consecutive
phase approach. World J Surg. 2012;6:524-33. patients with enterocutaneous fistulas. World J Surg
30. Teubner A, Morrison K, Ravishankar HR, Anderson 2008;32:445-53.
ID, Scott NA, Carlson GL. Fistuloclysis can 42. Murphy M, Hotouraw A, Koers L, Bhan C, Glym
successfully replace parenteral feeding in the M, Chan CL. Establishing a regional
nutritional support of patients with enterocutaneous enterocutaneous fistula service: The Royal London
fistula. Br J Surg. 2004;91:625-31. Hospital Experience. Int J Surg. 2013;11:952-6.
31. Nubiola P, Badia JM, Martinez-Rodenas F, Gil MJ,
Segura M, Sancho J, et al. Treatment of 27 post Cite this article as: Dodiyi-Manuel A, Wichendu
operative enterocutaneous fistulas with long half- PN. Current concepts in the management of
life somatostatin analogue SMS 201-995. Am Surg enterocutaneous fistula. Int Surg J 2018;5:1981-5.
1989;210:56-8.
International Surgery Journal | June 2018 | Vol 5 | Issue 6 Page 1985
View publication stats
You might also like
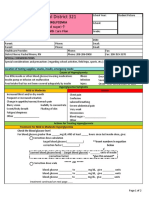
- Diabetes Hyperglycemia Emergency Care PlanDocument2 pagesDiabetes Hyperglycemia Emergency Care Planapi-405196113No ratings yet
- 15 Principles of Management and Prevention of Odontogenic inDocument24 pages15 Principles of Management and Prevention of Odontogenic inVukasin VostinicNo ratings yet
- Summary Performance Evaluation Achieving Intra-Partal Care Competency in Accordance With PRC Board of Nursing Memorandum No. 01 Series 2009Document8 pagesSummary Performance Evaluation Achieving Intra-Partal Care Competency in Accordance With PRC Board of Nursing Memorandum No. 01 Series 2009Fleo GardivoNo ratings yet
- A Modified Open Omental Plugging of Peptic Ulcer Perforation in A Mission Hospital, Northwestern CameroonDocument10 pagesA Modified Open Omental Plugging of Peptic Ulcer Perforation in A Mission Hospital, Northwestern CameroonRony RonyNo ratings yet
- GCSMC jms2014v3n1p18Document4 pagesGCSMC jms2014v3n1p18Yacine Tarik AizelNo ratings yet
- APPENDIC CASES Cuenco2020Document3 pagesAPPENDIC CASES Cuenco2020Nicole cuencosNo ratings yet
- The Surgical Anatomy and Etiology of Gastrointestinal FistulasDocument5 pagesThe Surgical Anatomy and Etiology of Gastrointestinal FistulasYacine Tarik AizelNo ratings yet
- Fistula Enterokutan 1Document8 pagesFistula Enterokutan 1Amalia GrahaniNo ratings yet
- Fistula Enterokutan 1Document8 pagesFistula Enterokutan 1Amalia GrahaniNo ratings yet
- Montravers2016 PDFDocument14 pagesMontravers2016 PDFraysellaNo ratings yet
- Anesthesia and Perioperative Management of Colorectal Surgical Patients - Specific Issues (Part 2)Document10 pagesAnesthesia and Perioperative Management of Colorectal Surgical Patients - Specific Issues (Part 2)Syauqi DarussalamNo ratings yet
- Hemorragia Tubo DigestivoDocument23 pagesHemorragia Tubo DigestivoNadia DeschampsNo ratings yet
- Cth artikel Final Efficacy and Cost Analysis of a Fish Skin Graft vs Standard of Care in the Management of Chronic Diabetic Foot Ulcers: A Prospective, Multicenter, Randomized Controlled Clinical TrialDocument21 pagesCth artikel Final Efficacy and Cost Analysis of a Fish Skin Graft vs Standard of Care in the Management of Chronic Diabetic Foot Ulcers: A Prospective, Multicenter, Randomized Controlled Clinical TrialanabkddosenNo ratings yet
- Intensive & Critical Care Nursing: Review ArticleDocument7 pagesIntensive & Critical Care Nursing: Review Articlefara annisaNo ratings yet
- Randomized Comparison of SubcuDocument11 pagesRandomized Comparison of SubcuRafael MarvinNo ratings yet
- Acute Gastroenteritis in Children of The World: What Needs To Be Done?Document8 pagesAcute Gastroenteritis in Children of The World: What Needs To Be Done?yoonie catNo ratings yet
- Treatment of Localized Aggressive Periodontitis With Platelet-Rich Plasma and Bone Allograft. Clinical Case ReportDocument8 pagesTreatment of Localized Aggressive Periodontitis With Platelet-Rich Plasma and Bone Allograft. Clinical Case ReportLori SimmonsNo ratings yet
- Nutritional Management of Patients With Enterocutaneous Fistulas: Practice and ProgressionDocument12 pagesNutritional Management of Patients With Enterocutaneous Fistulas: Practice and ProgressionKevin Howser T. ViNo ratings yet
- Optimising The Treatment of Upper Gastrointestinal FistulaeDocument9 pagesOptimising The Treatment of Upper Gastrointestinal FistulaeYacine Tarik AizelNo ratings yet
- Collado Boira2021Document10 pagesCollado Boira2021Andreia LopesNo ratings yet
- Nutrition in Pancreatic Surg ISGPS 2018Document14 pagesNutrition in Pancreatic Surg ISGPS 2018Dr Ankit SharmaNo ratings yet
- Int J of Nursing Knowl - 2021 - Capilla D AzDocument9 pagesInt J of Nursing Knowl - 2021 - Capilla D AzSuharyatno nizarNo ratings yet
- DiverticulitisDocument8 pagesDiverticulitisjennifer.hd.mfNo ratings yet
- Incidence of Histopathological Findings in Appendectomy Specimens in A Tertiary Care Hospital in Two-Year TimeDocument5 pagesIncidence of Histopathological Findings in Appendectomy Specimens in A Tertiary Care Hospital in Two-Year Timepatolog32No ratings yet
- Esophageal EmergenciesDocument15 pagesEsophageal EmergenciesOmar SolisNo ratings yet
- Perioperative Nutrition Recommendations From The ESPEN ExpertDocument17 pagesPerioperative Nutrition Recommendations From The ESPEN ExpertDomenica BritoNo ratings yet
- International Journal of SurgeryDocument4 pagesInternational Journal of SurgeryNatalindah Jokiem Woecandra T. D.No ratings yet
- Management of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and BeyondFrom EverandManagement of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and BeyondAditi BhattNo ratings yet
- Guia IDSA Prevencion ICVCDocument32 pagesGuia IDSA Prevencion ICVCmaturana61No ratings yet
- Dream 2020Document4 pagesDream 2020Karlito Dela CruzNo ratings yet
- Enterocutaneous Fistula: Medical and Surgical Management Including Patients With Crohn's DiseaseDocument7 pagesEnterocutaneous Fistula: Medical and Surgical Management Including Patients With Crohn's DiseaseAmanqui Alex DerlyNo ratings yet
- Manejo GistDocument7 pagesManejo GistRicardo Uzcategui ArreguiNo ratings yet
- BMJ k1407 Full PDFDocument14 pagesBMJ k1407 Full PDFraysellaNo ratings yet
- 2015 Anaesthesiology Intensive Therapy ManagementofabdomminalsepsisaparadigmshiftDocument10 pages2015 Anaesthesiology Intensive Therapy ManagementofabdomminalsepsisaparadigmshiftdwimellyndaNo ratings yet
- Small Bowel ObstructionDocument8 pagesSmall Bowel ObstructionChristopher AdhisasmitaNo ratings yet
- Đặc tính bảo vệ chuyển hóa và chống viêm của huyết thanh giàu dưỡng chất cho con người sau khi hấp thụ chiết xuất từ lá atisô Kết quả từ một thử nghiệm lâm sàng Ex Vivo cải tiếnDocument23 pagesĐặc tính bảo vệ chuyển hóa và chống viêm của huyết thanh giàu dưỡng chất cho con người sau khi hấp thụ chiết xuất từ lá atisô Kết quả từ một thử nghiệm lâm sàng Ex Vivo cải tiếnLại Ngọc MaiNo ratings yet
- Abdominal AdhesionsDocument21 pagesAbdominal Adhesionspkjunaid313No ratings yet
- Intraabdominal SepsisDocument6 pagesIntraabdominal SepsisPablo O. Cisneros FlorNo ratings yet
- Fluid Resuscitation in Acute PancreatitisDocument7 pagesFluid Resuscitation in Acute PancreatitisRicardo Isique SantillanNo ratings yet
- Diverticulitis NEJMDocument8 pagesDiverticulitis NEJMAlfredo MartínezNo ratings yet
- Percutaneus Endoscopic Gatrotomy PDFDocument15 pagesPercutaneus Endoscopic Gatrotomy PDFJosé Moreira Lima NetoNo ratings yet
- Mayumi Et Al-2018-Journal of Hepato-Biliary-Pancreatic SciencesDocument5 pagesMayumi Et Al-2018-Journal of Hepato-Biliary-Pancreatic SciencesAndres RiveraNo ratings yet
- 1 s2.0 S1521691822000038 MainDocument1 page1 s2.0 S1521691822000038 Mainafg_19No ratings yet
- Drenaje Quirurgico Vs Endoscopico PsudoquisteDocument9 pagesDrenaje Quirurgico Vs Endoscopico Psudoquistecore6406No ratings yet
- Gutjnl 2020 321372.fullDocument15 pagesGutjnl 2020 321372.fullBojan TepesNo ratings yet
- Influence of The Intestinal Microbiome On Anastomotic Healing in The Colon and RectumDocument25 pagesInfluence of The Intestinal Microbiome On Anastomotic Healing in The Colon and RectumDumitru RadulescuNo ratings yet
- Manejo Del ResangradoDocument13 pagesManejo Del ResangradoRudy J CoradoNo ratings yet
- Acute Appendicitis: Evidence Based Management: January 2016Document5 pagesAcute Appendicitis: Evidence Based Management: January 2016putraNo ratings yet
- Treatment of Enterocutaneous Fistula A Systematic Review and MetaanalysisDocument12 pagesTreatment of Enterocutaneous Fistula A Systematic Review and MetaanalysisMarcus CezilloNo ratings yet
- Research Paper On Tuberculosis in IndiaDocument8 pagesResearch Paper On Tuberculosis in Indiakcjzgcsif100% (1)
- Comparison of MUST and Nutriscore For The Screening of Malnutrition in Hospitalized Oncology PatientsDocument7 pagesComparison of MUST and Nutriscore For The Screening of Malnutrition in Hospitalized Oncology Patientssergedemirdjian1990No ratings yet
- February - Peritonitis and Intra-Abdominal AbscessDocument16 pagesFebruary - Peritonitis and Intra-Abdominal AbscessPekerja KesunyianNo ratings yet
- Original Article: Key WordsDocument9 pagesOriginal Article: Key WordsykommNo ratings yet
- Octreotide 2017Document10 pagesOctreotide 2017Issa AbuzeidNo ratings yet
- Diagnosis and Management of Klatskin Tumor: April 2010Document6 pagesDiagnosis and Management of Klatskin Tumor: April 2010Feby Kurnia PutriNo ratings yet
- Non Operative Treatment in AppendicitisDocument9 pagesNon Operative Treatment in AppendicitisCarla GarcíaNo ratings yet
- Diarrhea For CancerDocument17 pagesDiarrhea For Cancerpalomazul007No ratings yet
- Final Ugib Sec To BpudDocument17 pagesFinal Ugib Sec To BpudBaby Kate BONGCARASNo ratings yet
- 01 Editorial 6042 IngDocument2 pages01 Editorial 6042 IngJuan Mendia OssioNo ratings yet
- Perforated Peptic Ulcer - An Update: ArticleDocument14 pagesPerforated Peptic Ulcer - An Update: ArticleMuhammad ibnu kaesar PurbaNo ratings yet
- Classification and Management of Bile Duct Injuries: EditorialDocument6 pagesClassification and Management of Bile Duct Injuries: EditorialSINAN SHAWKATNo ratings yet
- E023064 FullDocument8 pagesE023064 FullChiperi CristinaNo ratings yet
- Nutritional Support after Gastrointestinal SurgeryFrom EverandNutritional Support after Gastrointestinal SurgeryDonato Francesco AltomareNo ratings yet
- Self-Assessment Color Review Moriello's Small Animal Dermatology Fundamental Cases and Concepts 2nd Edition PDFDocument307 pagesSelf-Assessment Color Review Moriello's Small Animal Dermatology Fundamental Cases and Concepts 2nd Edition PDFGiulia Nădășan-Cozma100% (1)
- Listening TestDocument3 pagesListening TestKhông Trà Trà ĐàoNo ratings yet
- Lymph Node PathologyDocument4 pagesLymph Node PathologyGerardLum0% (1)
- Obgyn OspeDocument21 pagesObgyn OspeAbrar HasanNo ratings yet
- Hymenal MorphologyDocument5 pagesHymenal MorphologyDimple Marie CabiasNo ratings yet
- Therapeutic Effect of Date Fruit PDFDocument10 pagesTherapeutic Effect of Date Fruit PDFMerdiana SafitriNo ratings yet
- Seminar On Shock: IntroductionDocument22 pagesSeminar On Shock: Introductionmahendra singhNo ratings yet
- NIPT - BeSHG 2014Document70 pagesNIPT - BeSHG 2014Mohamed ElsawyNo ratings yet
- MMDST PDFDocument50 pagesMMDST PDFChristopher OlipasNo ratings yet
- DR Nadia AhmadDocument4 pagesDR Nadia AhmadNadia AhmadNo ratings yet
- Anestesia y Analgesia Veterinaria Lumb Adjuvant Analgesics in Acute Pain ManagementDocument3 pagesAnestesia y Analgesia Veterinaria Lumb Adjuvant Analgesics in Acute Pain ManagementGilliNo ratings yet
- Man Week Vii PDFDocument2 pagesMan Week Vii PDFLewis GwytherNo ratings yet
- International Journal of Respiratory and Pulmonary Medicine Ijrpm 5 087Document7 pagesInternational Journal of Respiratory and Pulmonary Medicine Ijrpm 5 087ZuraidaNo ratings yet
- Subcortical AphasiaDocument4 pagesSubcortical AphasiaCris RaNo ratings yet
- 3D Guided Comprehensive Approach ToDocument12 pages3D Guided Comprehensive Approach ToAna Maria Montoya GomezNo ratings yet
- Nervous System Diagnostic Tests: Dr. Odilon A. Maglasang Learning FacilitatorDocument40 pagesNervous System Diagnostic Tests: Dr. Odilon A. Maglasang Learning FacilitatorMr rawrNo ratings yet
- Manual de Neuropatía Periférica (2005)Document727 pagesManual de Neuropatía Periférica (2005)histoginoNo ratings yet
- 6277-Article Text-44963-1-10-20221231Document10 pages6277-Article Text-44963-1-10-20221231Agus KarismaNo ratings yet
- Medical For Athletes 2Document2 pagesMedical For Athletes 2RICXIENo ratings yet
- 1.d 2.d 3.a 4.c 5.a 6.c 7.c 8d. 9.d 10. B: Answer Key For MCQ MicrobiologyDocument9 pages1.d 2.d 3.a 4.c 5.a 6.c 7.c 8d. 9.d 10. B: Answer Key For MCQ Microbiologymenah ayyashNo ratings yet
- ADA Radiography GuidelinesDocument27 pagesADA Radiography GuidelinesJames ChenNo ratings yet
- Study Designs in Epidemiologic Research Chronic DiseasesDocument51 pagesStudy Designs in Epidemiologic Research Chronic DiseasesLeonel Nkweti100% (2)
- Slcog Abstracts 2012Document133 pagesSlcog Abstracts 2012Indika WithanageNo ratings yet
- Depression Anxiety Stress ScaleDocument2 pagesDepression Anxiety Stress ScaleYanna LozanoNo ratings yet
- Basic Foods 2-FLOUR AND FLOUR MIXTURESDocument3 pagesBasic Foods 2-FLOUR AND FLOUR MIXTURESBernadette YurongNo ratings yet
- NSAIDsDocument27 pagesNSAIDsshatz_014No ratings yet
- Helminthes PDFDocument24 pagesHelminthes PDFMatt Joseph CabantingNo ratings yet