Professional Documents
Culture Documents
2017 Relevance of Cerebral
Uploaded by
Tote Cifuentes AmigoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2017 Relevance of Cerebral
Uploaded by
Tote Cifuentes AmigoCopyright:
Available Formats
Review article: Biomedical intelligence | Published 11 December 2017 | doi:10.4414/smw.2017.
14538
Cite this as: Swiss Med Wkly. 2017;147:w14538
Relevance of the cerebral collateral circulation in
ischaemic stroke: time is brain, but collaterals
set the pace
Jung Simonab, Wiest Rolandc, Gralla Janc, McKinley Richardc, Mattle Heinrich Pa, Liebeskind Davidb
a
Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Switzerland
b
Neurovascular Imaging Research Core and the Department of Neurology, University of California, Los Angeles, USA
c
University Institute for Diagnostic and Interventional Neuroradiology, Inselspital, Bern University Hospital, University of Bern, Switzerland
Summary teries to each other (fig. 1). The secondary routes include
all external to internal carotid artery connections through
Blood supply to the brain is secured by an extensive collat-
facial, maxillary, middle meningeal, and occipital arteries.
eral circulation system, which can be divided into primary
The most common one is the connection through the oph-
routes, i.e., the Circle of Willis, and secondary routes, e.g.,
thalmic artery: retrograde blood flow via the ophthalmic
collaterals from the external to the internal carotid artery
artery allows supply from the external carotid artery to the
and leptomeningeal collaterals. Collateral flow is the basis
internal carotid artery (ICA) in the case of proximal occlu-
for acute stroke treatment, since neurones will only sur-
sion of the ICA. In addition, the secondary routes comprise
vive long enough to be rescued with reperfusion therapies
leptomeningeal collaterals, perforator collaterals, the tectal
if there is sufficient collateral flow. Poor collateral flow is
plexus and the ophthalmic plexus. Leptomeningeal collat-
associated with worse outcome and faster growth of larger
erals are small pial arterioles connecting the territories of
infarcts in acute stroke treatment. Therapeutic promotion
the middle cerebral artery (MCA) with those of the anteri-
of collateral flow theoretically offers the chance for out-
or (ACA) and posterior cerebral artery (PCA) (fig. 2). Lep-
come improvement, but randomised trials are lacking. The
tomeningeal collaterals are very important in occlusions
extent of collateral flow is highly variable between individ-
of the intracranial arteries. Perforator collaterals connect
uals. As a consequence, the speeds of infarct growth are
lenticulostriate and thalamostriate arteries with branches of
highly variable, resulting in varying individual treatment
the MCA and PCA and can be recruited in addition to lep-
time windows until the whole salvageable tissue has be-
tomeningeal collaterals in MCA occlusions.
come infarcted. An ideal patient selection for reperfusion
The extent of collaterals is highly variable between indi-
therapies should be based on imaging of the salvageable
viduals, but there is also intraindividual variability during
tissue, the so called penumbra. The penumbra can be
the lifetime: rarefaction of the collaterals is observed with
approximately visualised by computed tomography (CT)
aging and as a result of vascular risk factors [1].
and magnetic resonance imaging (MRI), but both methods
are significantly inaccurate in about 25% of the patients.
The role of collaterals in acute ischaemic
There is a need for improved penumbra imaging by CT
stroke
and MRI, and first studies applying machine learning tech-
niques have shown promising results. Intravenous thrombolysis (IVT) and endovascular treat-
ment (EVT) have been proven to have considerable thera-
Key words: acute stroke, treatment, anaemia, haemoglo-
peutic effect in acute ischaemic stroke in several large clin-
bin decrease, infarct growth, haemodilution
ical trials [2–10]. The treatment effect of these reperfusion
therapies is based on the penumbral concept, which as-
The cerebral collateral system sumes the existence of salvageable tissue due to gradual in-
Collateral blood circulation is common in most species as a farct growth within the territory of the occluded vessel (fig.
system of vascular redundancy designed to preserve blood 3) [11, 12]. Theoretical considerations quantify this grad-
supply in the event of failure of the primary blood supply- ual infarct growth to be 1.9 million neurones dying every
ing system. In humans, collateral circulation can be found minute in occlusion of one of the large arteries [13]. This
Correspondence: in most organs, and the blood supply to the brain especial- is fast – but why do neurones not die all at once after a few
Simon Jung, MD, Depart- ly is secured by an extensive collateral circulation system. minutes, given results from in-vitro experiments that have
ment of Neurology, Univer- The collateral circuits to the brain can be divided into pri- shown that neuronal cell death occurs already minutes after
sity Hospital Inselspital,
mary and secondary routes. The primary route consists of interruption of energy supply? Neuronal cell death can
Freiburgstrasse 18,
CH-3010 Bern, si- the Circle of Willis, which mainly links the anterior with only be delayed by ongoing energy supply – that is, the
mon.jung[at]insel.ch the posterior circulation and the nearby main cerebral ar- whole penumbral concept as well as the therapeutic effect
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 1 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
Review article: Biomedical intelligence Swiss Med Wkly. 2017;147:w14538
of reperfusion therapies relies on collateral blood flow. De- tremely fast: it takes only 12 seconds after ICA occlusion
pending on the extent of collateral blood flow, neuronal in rats until maximal dilatation of the leptomeningeal col-
death can be delayed in a variable manner or even prevent- laterals [16].
ed. The extent of collateral flow is highly variable between The extent of collateral flow has major impact on the out-
individuals, but it is usually greatest in the case of occlu- come of conservatively treated patients and of patients
sion of the extracranial vessels: almost 60% of patients tol- treated with IVT or EVT. Even at hospital admission, the
erate even complete ICA occlusion without infarct devel- severity of neurological deficits already depends on the ex-
opment because of sufficient blood supply through primary tent of collaterals [17, 18], which is revealed by variable
and secondary collateral circuits [14, 15]. The recruitment infarct sizes in baseline imaging, depending on the collat-
of inactive, vasoconstricted collaterals can take place ex- eral quality [19, 20]. Several studies demonstrated that the
Figure 1: Intracranial vessels. Yellow: Circle of Willis (adapted from the Stroke Guidelines of the University Hospital of Bern 2017, www.stroke-
center.ch).
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 2 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
Review article: Biomedical intelligence Swiss Med Wkly. 2017;147:w14538
outcome after IVT and EVT is also highly dependent on patients on average may not benefit from later therapy, pa-
the extent of collateral flow [21–33]: not only the volume tient selection based on these time windows would neglect
of the final infarct [19, 20, 24, 34–38], but also the success the large interindividual variability of the extent of collat-
of reperfusion [20, 27, 39, 40] are influenced by the collat- eral flow. This regimen would lead to the exclusion from
eral quality. In addition, the risk for symptomatic bleeding therapy of many patients who would, in fact, benefit. In-
after reperfusion therapy seems to rise with poor collateral deed, infarct growth is much less dependent on the elapsed
flow [30, 41, 42]. time than on the quality of collaterals: good collaterals
slow down infarct growth and poor collaterals accelerate
Implications of the collateral variability on it [19, 45–48]. Of course reperfusion treatment should al-
time windows for acute stroke treatment ways be initiated as early as possible because “time is
brain”, but the collaterals set the pace of neuronal loss,
Reperfusion therapy by means of IVT and EVT is highly
and with this the individual time window until infarction of
effective. In large randomised trials only 5–14 patients had
all tissue at risk. Figure 4 illustrates two patients in whom
to be treated with IVT and 3–7 patients with EVT to pre-
the approximated velocity of neuronal cell loss differed be-
vent one patient from death or dependency [2–10]. The
tween 9000 neurones/min and more than 460 billion neu-
therapeutic effect of these therapies is not only dependent
rones/min. This large variability of the velocity of neuronal
on the success of reperfusion, but is also highly time de-
cell loss implies that there are probably many patients el-
pendent. Treatment time windows of 4.5 hours for IVT and
igible for therapy far beyond time windows that were cal-
7.3 hours for EVT have been defined by pooled analysis
culated on the average of patients. Patient selection based
of the patients treated in the large trials [43, 44]. Although
Figure 2: Leptomeningeal collateral flow in occlusion of the proximal middle cerebral artery as seen in conventional angiography (sagittal
plane). (A1–A3): serial images after contrast agent application into the internal carotid artery showing proximal middle cerebral artery occlu-
sion (red arrow in A1) with subsequent filling of leptomeningeal collaterals 2.5 sec thereafter fed by the anterior (above and right of blue line in
A2) and posterior circulation. After 5.3 sec retrograde collateral flow filled the superior (red dots) and inferior branch (green dots) of the occlud-
ed middle cerebral artery (A3 + A3 zoomed). (B) After windowing A3 capillary filling visualised supply of the whole middle cerebral artery terri-
tory by collaterals. (C) The same branches filled retrogradely by collaterals in A3 are filled anterogradely after reperfusion of the occlusion.
(Pictures: Stroke Centre Bern)
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 3 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
Review article: Biomedical intelligence Swiss Med Wkly. 2017;147:w14538
on restricted time windows would not only exclude from That imaging-based patient selection is a promising con-
therapy eligible patients outside the time windows, but also cept has recently been demonstrated by the DAWN trial
all patients with wake-up stroke and with unknown symp- (not yet published), which included patients with large
tom onset, who account for at least one third of all stroke artery occlusion between 6 and 24 hours after symptom
patients. Therefore, patient selection for reperfusion thera- onset for EVT, if they presented with a so called clinical-
py should be individualised by imaging salvageable tissue, image mismatch: patients had to be clinically severely af-
rather than being restricted by strict time windows. fected (NIHSS ≥10) but infarct core had to be restricted
Figure 3: Illustration of the penumbra concept. Infarct core (red): infarcted tissue. Penumbra (orange): salvageable tissue at risk for infarction
in case of persistence vessel occlusion. Oligaemia (yellow): hypoperfused tissue without risk for infarction. Cerebral blood flow decreases in
direction to the infarct core. Decreased blood flow can be compensated by an increased oxygen extraction fraction and vasodilation of collater-
al vessels sufficiently enough in the oligaemia but not in the penumbra. (Picture: Stroke Centre Bern)
Figure 4: Variable velocities of infarct growth. Patient A: carotid T occlusion and fetal type posterior cerebral artery, 2 hours after symptom on-
set hyperintensity of the whole hemisphere in diffusion-weighted imaging (DWI) with corresponding hypodensity in CT perfusion (CBV). Pa-
tient B: persistent carotid occlusion, slow infarct growth in DWI over 17 days. Neuronal cell loss was estimated based on volumetric measure-
ment of the lesion and the average neuronal density described in Saver et al. [13] (Pictures: Stroke Centre Bern)
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 4 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
Review article: Biomedical intelligence Swiss Med Wkly. 2017;147:w14538
(<21 cc if patients was ≥80 years, <31 cc if patients was pared with previous maps [60]. Nevertheless, estimation
<80 years and NIHSS ≥10 or <51 cc if patient was <80 of the tissue at risk based on maps derived from simple
years and NIHSS ≥20). The trial revealed a clear effect of thresholding is prone to errors in about 25% of patients,
reperfusion therapy in these selected patients: the number with variations of the predicted penumbra of up to 100 ml
needed to treat was reported to be 2.8 for 90-day functional [61]. In most cases the penumbra is overestimated owing
independence. Future trials will hopefully allow the inclu- to inclusion of parts of the oligaemia. Newer studies ap-
sion of even more patients by a more detailed visualisation plying machine learning techniques instead of using only
of salvageable tissue. the somewhat arbitrary thresholds of surrogate parameters
have shown first promising results with improved accura-
Assessment of cerebral collaterals and salvage- cy of the penumbra imaging [62].
able tissue
Collaterals can be visualised most accurately by use of
Potential treatment options for improving col-
conventional angiography, which is the gold standard due
lateral flow
to its high temporal and spatial resolution [49–51]. Unfor- Given the association of poor collateral flow with poor out-
tunately, there are several systems for grading collateral come, and larger and faster infarct growth, therapeutic pro-
flow, which hampers the comparability of study results. motion of collateral flow may offer the chance to improve
One of the scoring systems most often used is the one outcome beyond efforts to raise reperfusion success rates
described by the Society of NeuroInterventional Surgery and to minimise treatment delay. Up to now, mainly in-vivo
(formally ASITN/SIR) [52]. In clinical practice, therapeu- data support the potential benefit from promoting collat-
tic decisions are usually made in advance of conventional eral flow [63, 64]. Possible treatment options include in-
angiography, on the basis of noninvasive imaging with duced hypertension (e.g. by phenylephrine), selective cere-
magnetic resonance (MR) or computed tomography (CT). bral vasodilation (e.g., by nitric oxide or sphenopalatine
Although grading of collaterals is also possible by CT and ganglion stimulation), external counterpulsation, and en-
MR imaging, it is less accurate [53, 54]. Furthermore, there dovascular partial occlusion of the abdominal aorta [63,
is more a need for an accurate visualisation of salvageable 64]. On the one hand, induced hypertension and partial oc-
tissue at risk for infarction, rather than pure information on clusion of the abdominal aorta aim to improve collateral
collateral flow. circulation by raising the perfusion pressure through an in-
Positron emission tomography (PET) is the gold standard creased systemic pressure and flow diversion, respectively.
for imaging of the penumbra because it allows the most External counterpulsation aims also to raise the perfusion
accurate visualisation of the infarct core and the hypop- pressure of collaterals, but through augmented diastolic
erfused tissue [55]. A cerebral blood flow (CBF) below flow. On the other hand, selective cerebral vasodilatation
12 ml/100g/min defines the area of infarct core, a flow of aims to increase collateral flow by reducing the vessel re-
12–22 ml/100g/min identifies the tissue at risk for infarc- sistance within collateral arterioles.
tion in the case of persistence vessel occlusion, and a flow
greater than 22 ml/100g/min defines an area of oligaemia, Disclosure statement
Jan Gralla is the Global Principal Investigator of the SWIFT DIRECT
i.e., hypoperfused tissue without risk for infarction [56].
Trial. No other potential conflict of interest relevant to this article was
Although very accurate, PET imaging is not a practica- reported.
ble technique in the acute setting of stroke. Both MR and
CT allow approximation of the penumbra, but show a rele- References
vant inaccuracy of the imaging techniques used up to now 1 Menon BK, Smith EE, Coutts SB, Welsh DG, Faber JE, Goyal M, et al.
Leptomeningeal collaterals are associated with modifiable metabolic
[56–58]. The core is defined with MR imaging of the le-
risk factors. Ann Neurol. 2013;74(2):241–8. doi:http://doi.wiley.com/
sion in diffusion-weighted imaging (DWI) and the hypop- 10.1002/ana.23906. PubMed.
erfused area by perfusion imaging. With CT, the core is vi- 2 National Institute of Neurological Disorders and Stroke rt-PA Stroke
sualised by means of cerebral blood volume (CBV) and the Study Group. Tissue plasminogen activator for acute ischemic stroke. N
Engl J Med. 1995;333(24):1581–8. doi: http://dx.doi.org/10.1056/NE-
hypoperfused area by perfusion imaging. Visualisation of
JM199512143332401. PubMed.
the infarct core with MRI is more accurate than with CT, 3 Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et
but diffusion lesion reversal can occur because the DWI le- al.; ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours af-
sion may overestimate the infarct core and contain up to ter acute ischemic stroke. N Engl J Med. 2008;359(13):1317–29. doi:
http://dx.doi.org/10.1056/NEJMoa0804656. PubMed.
25% false positive, surviving, tissue [59]. Definition of the
4 Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J,
core by use of quantitative analysis of the calculated Ap- et al.; ESCAPE Trial Investigators. Randomized assessment of rapid en-
parent Diffusion Coefficient (ADC) maps is more accurate dovascular treatment of ischemic stroke. N Engl J Med.
[59]. 2015;372(11):1019–30. doi: http://dx.doi.org/10.1056/NEJ-
Moa1414905. PubMed.
Imaging of the hypoperfused tissue at risk by use of MR
5 Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A,
and CT perfusion imaging relies on surrogates of perfusion et al.; REVASCAT Trial Investigators. Thrombectomy within 8 hours af-
parameters calculated from nondeconvolved (e.g, time to ter symptom onset in ischemic stroke. N Engl J Med.
peak TTP]) or deconvolved (e.g. CBF, mean transit time 2015;372(24):2296–306. doi: http://dx.doi.org/10.1056/NEJ-
Moa1503780. PubMed.
[MTT], time to maximum [Tmax]) tissue residue function
6 Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al.;
(time contrast curve) of the intravascular contrast bolus SWIFT PRIME Investigators. Stent-retriever thrombectomy after intra-
[56]. Different maps computed from MR and CT imaging venous t-PA vs. t-PA alone in stroke. N Engl J Med.
have been developed and compared with PET measure- 2015;372(24):2285–95. doi: http://dx.doi.org/10.1056/NEJ-
Moa1415061. PubMed.
ments. Recent studies indicate that Tmax thresholds of
7 Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF,
>6 sec improves the prediction of salvageable tissue com- Yoo AJ, et al.; MR CLEAN Investigators. A randomized trial of intraar-
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 5 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
Review article: Biomedical intelligence Swiss Med Wkly. 2017;147:w14538
terial treatment for acute ischemic stroke. N Engl J Med. tients. Ann Neurol. 2007;61(6):533–43. doi: http://dx.doi.org/10.1002/
2015;372(1):11–20. PubMed. ana.21130. PubMed.
8 Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi 26 Tan IYL, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et
N, et al.; EXTEND-IA Investigators. Endovascular therapy for ischemic al. CT angiography clot burden score and collateral score: correlation
stroke with perfusion-imaging selection. N Engl J Med. with clinical and radiologic outcomes in acute middle cerebral artery in-
2015;372(11):1009–18. doi: http://dx.doi.org/10.1056/NEJ- farct. AJNR Am J Neuroradiol. 2009;30(3):525–31. doi:
Moa1414792. PubMed. http://dx.doi.org/10.3174/ajnr.A1408. PubMed.
9 Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et 27 Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, Ovbiagele B, et al.
al.; THRACE investigators. Mechanical thrombectomy after intravenous Collateral flow predicts response to endovascular therapy for acute is-
alteplase versus alteplase alone after stroke (THRACE): a randomised chemic stroke. Stroke. 2011;42(3):693–9. doi: http://dx.doi.org/10.1161/
controlled trial. Lancet Neurol. 2016;15(11):1138–47. doi: STROKEAHA.110.595256. PubMed.
http://dx.doi.org/10.1016/S1474-4422(16)30177-6. PubMed. 28 Gerber JC, Petrova M, Krukowski P, Kuhn M, Abramyuk A, Bodechtel
10 Mocco J, Zaidat OO, von Kummer R, Yoo AJ, Gupta R, Lopes D, et al.; U, et al. Collateral state and the effect of endovascular reperfusion thera-
THERAPY Trial Investigators*. Aspiration Thrombectomy After Intra- py on clinical outcome in ischemic stroke patients. Brain Behav.
venous Alteplase Versus Intravenous Alteplase Alone. Stroke. 2016;6(9):e00513. doi: http://dx.doi.org/10.1002/brb3.513. PubMed.
2016;47(9):2331–8. doi: http://dx.doi.org/10.1161/STROKEA- 29 Leng X, Lan L, Liu L, Leung TW, Wong KS. Good collateral circulation
HA.116.013372. PubMed. predicts favorable outcomes in intravenous thrombolysis: a systematic
11 Baron JC. Mapping the ischaemic penumbra with PET: implications for review and meta-analysis. Eur J Neurol. 2016;23(12):1738–49. doi:
acute stroke treatment. Cerebrovasc Dis. 1999;9(4):193–201. doi: http://dx.doi.org/10.1111/ene.13111. PubMed.
http://dx.doi.org/10.1159/000015955. PubMed. 30 Leng X, Fang H, Leung TWH, Mao C, Miao Z, Liu L, et al. Impact of
12 Astrup J, Siesjö BK, Symon L. Thresholds in cerebral ischemia - the is- collaterals on the efficacy and safety of endovascular treatment in acute
chemic penumbra. Stroke. 1981;12(6):723–5. doi: http://dx.doi.org/ ischaemic stroke: a systematic review and meta-analysis. J Neurol Neu-
10.1161/01.STR.12.6.723. PubMed. rosurg Psychiatry. 2016;87(5):537–44. doi: http://dx.doi.org/10.1136/jn-
13 Saver JL. Time is brain--quantified. Stroke. 2006;37(1):263–6. doi: np-2015-310965. PubMed.
http://dx.doi.org/10.1161/01.STR.0000196957.55928.ab. PubMed. 31 Liebeskind DS, Jahan R, Nogueira RG, Zaidat OO, Saver JL; SWIFT
14 Powers WJ. Cerebral hemodynamics in ischemic cerebrovascular dis- Investigators. Impact of collaterals on successful revascularization in
ease. Ann Neurol. 1991;29(3):231–40. doi: http://dx.doi.org/10.1002/ Solitaire FR with the intention for thrombectomy. Stroke.
ana.410290302. PubMed. 2014;45(7):2036–40. doi: http://dx.doi.org/10.1161/STROKEA-
15 Arnold M, Slezak A, El-Koussy M, Lüdi R, Findling O, Mono ML, et HA.114.004781. PubMed.
al. Occlusion Location of Middle Cerebral Artery Stroke and Outcome 32 Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J,
after Endovascular Treatment. Eur Neurol. 2015;74(5-6):315–21. doi: et al.; ESCAPE Trial Investigators. Randomized assessment of rapid en-
http://dx.doi.org/10.1159/000441445. PubMed. dovascular treatment of ischemic stroke. N Engl J Med.
16 Morita Y, Fukuuchi Y, Koto A, Suzuki N, Isozumi K, Gotoh J, et al. 2015;372(11):1019–30. doi: http://dx.doi.org/10.1056/NEJ-
Rapid changes in pial arterial diameter and cerebral blood flow caused Moa1414905. PubMed.
by ipsilateral carotid artery occlusion in rats. Keio J Med. 33 Tan BYQ, Wan-Yee K, Paliwal P, Gopinathan A, Nadarajah M, Ting E,
1997;46(3):120–7. doi: http://dx.doi.org/10.2302/kjm.46.120. PubMed. et al. Good Intracranial Collaterals Trump Poor ASPECTS (Alberta
17 Roberts HC, Dillon WP, Furlan AJ, Wechsler LR, Rowley HA, Fis- Stroke Program Early CT Score) for Intravenous Thrombolysis in Ante-
chbein NJ, et al. Computed tomographic findings in patients undergoing rior Circulation Acute Ischemic Stroke. Stroke. 2016;47(9):2292–8. doi:
intra-arterial thrombolysis for acute ischemic stroke due to middle cere- http://dx.doi.org/10.1161/STROKEAHA.116.013879. PubMed.
bral artery occlusion: results from the PROACT II trial. Stroke. 34 Ovbiagele B, Buck BH, Liebeskind DS, Starkman S, Bang OY, Ali LK,
2002;33(6):1557–65. doi: http://dx.doi.org/10.1161/ et al. Prior antiplatelet use and infarct volume in ischemic stroke. J Neu-
01.STR.0000018011.66817.41. PubMed. rol Sci. 2008;264(1-2):140–4. doi: http://dx.doi.org/10.1016/
18 Marks MP, Lansberg MG, Mlynash M, Olivot JM, Straka M, Kemp S, j.jns.2007.08.033. PubMed.
et al.; Diffusion and Perfusion Imaging Evaluation for Understanding 35 Boers AM, Jansen IG, Berkhemer OA, Yoo AJ, Lingsma HF, Slump
Stroke Evolution 2 Investigators. Effect of collateral blood flow on pa- CH, et al.; MR CLEAN trial investigators †. Collateral status and tissue
tients undergoing endovascular therapy for acute ischemic stroke. outcome after intra-arterial therapy for patients with acute ischemic
Stroke. 2014;45(4):1035–9. doi: http://dx.doi.org/10.1161/STROKEA- stroke. J Cereb Blood Flow Metab. 2016;Jan 1:X16678874.
HA.113.004085. PubMed. doi:http://journals.sagepub.com/doi/10.1177/0271678X16678874.
19 Jung S, Gilgen M, Slotboom J, El-Koussy M, Zubler C, Kiefer C, et al. PubMed.
Factors that determine penumbral tissue loss in acute ischaemic stroke. 36 Christoforidis GA, Vakil P, Ansari SA, Dehkordi FH, Carroll TJ. Impact
Brain. 2013;136(Pt 12):3554–60. doi: http://dx.doi.org/10.1093/brain/ of pial collaterals on infarct growth rate in experimental acute ischemic
awt246. PubMed. stroke. AJNR Am J Neuroradiol. 2017;38(2):270–5. doi:
20 Marks MP, Lansberg MG, Mlynash M, Olivot JM, Straka M, Kemp S, http://dx.doi.org/10.3174/ajnr.A5003. PubMed.
et al.; Diffusion and Perfusion Imaging Evaluation for Understanding 37 Son JP, Lee MJ, Kim SJ, Chung JW, Cha J, Kim GM, et al. Impact of
Stroke Evolution 2 Investigators. Effect of collateral blood flow on pa- Slow Blood Filling via Collaterals on Infarct Growth: Comparison of
tients undergoing endovascular therapy for acute ischemic stroke. Mismatch and Collateral Status. J Stroke. 2017;19(1):88–96. doi:
Stroke. 2014;45(4):1035–9. doi: http://dx.doi.org/10.1161/STROKEA- http://dx.doi.org/10.5853/jos.2016.00955. PubMed.
HA.113.004085. PubMed. 38 Vagal A, Menon BK, Foster LD, Livorine A, Yeatts SD, Qazi E, et al.
21 Galimanis A, Jung S, Mono M-L, Fischer U, Findling O, Weck A, et al. Association Between CT Angiogram Collaterals and CT Perfusion in
Endovascular therapy of 623 patients with anterior circulation stroke. the Interventional Management of Stroke III Trial. Stroke.
Stroke. 2012;43(4):1052–7. doi: http://dx.doi.org/10.1161/STROKEA- 2016;47(2):535–8. doi: http://dx.doi.org/10.1161/STROKEA-
HA.111.639112. PubMed. HA.115.011461. PubMed.
22 Kucinski T, Koch C, Eckert B, Becker V, Krömer H, Heesen C, et al. 39 Leng X, Fang H, Leung TWH, Mao C, Xu Y, Miao Z, et al. Impact of
Collateral circulation is an independent radiological predictor of out- Collateral Status on Successful Revascularization in Endovascular
come after thrombolysis in acute ischaemic stroke. Neuroradiology. Treatment: A Systematic Review and Meta-Analysis. Cerebrovasc Dis.
2003;45(1):11–8. doi: http://dx.doi.org/10.1007/s00234-002-0881-0. 2016;41(1-2):27–34. doi: http://dx.doi.org/10.1159/000441803.
PubMed. PubMed.
23 Toni D, Fiorelli M, Bastianello S, Falcou A, Sette G, Ceschin V, et al. 40 Liebeskind DS, Jahan R, Nogueira RG, Zaidat OO, Saver JL; SWIFT
Acute ischemic strokes improving during the first 48 hours of onset: Investigators. Impact of collaterals on successful revascularization in
predictability, outcome, and possible mechanisms. A comparison with Solitaire FR with the intention for thrombectomy. Stroke.
early deteriorating strokes. Stroke. 1997;28(1):10–4. doi: 2014;45(7):2036–40. doi: http://dx.doi.org/10.1161/STROKEA-
http://dx.doi.org/10.1161/01.STR.28.1.10. PubMed. HA.114.004781. PubMed.
24 Rosenthal ES, Schwamm LH, Roccatagliata L, Coutts SB, Demchuk 41 Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, Ovbiagele B, et al.;
AM, Schaefer PW, et al. Role of recanalization in acute stroke outcome: UCLA-Samsung Stroke Collaborators. Collateral flow averts hemor-
rationale for a CT angiogram-based “benefit of recanalization” model. rhagic transformation after endovascular therapy for acute ischemic
AJNR Am J Neuroradiol. 2008;29(8):1471–5. doi: http://dx.doi.org/ stroke. Stroke. 2011;42(8):2235–9. doi: http://dx.doi.org/10.1161/
10.3174/ajnr.A1153. PubMed. STROKEAHA.110.604603. PubMed.
25 Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M. System- 42 Liebeskind DS, Tomsick TA, Foster LD, Yeatts SD, Carrozzella J, Dem-
atic comparison of perfusion-CT and CT-angiography in acute stroke pa- chuk AM, et al.; IMS III Investigators. Collaterals at angiography and
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 6 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
Review article: Biomedical intelligence Swiss Med Wkly. 2017;147:w14538
outcomes in the Interventional Management of Stroke (IMS) III trial. 53 Baird AE, Warach S. Magnetic resonance imaging of acute stroke. J
Stroke. 2014;45(3):759–64. doi: http://dx.doi.org/10.1161/STROKEA- Cereb Blood Flow Metab. 1998;18(6):583–609. doi: http://dx.doi.org/
HA.113.004072. PubMed. 10.1097/00004647-199806000-00001. PubMed.
43 Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick 54 Wintermark M, Reichhart M, Thiran J-P, Maeder P, Chalaron M, Schny-
JP, et al., NINDS rt-PA Study Group Investigators. Association of out- der P, et al. Prognostic accuracy of cerebral blood flow measurement by
come with early stroke treatment: pooled analysis of ATLANTIS, perfusion computed tomography, at the time of emergency room admis-
ECASS, and NINDS rt-PA stroke trials. Lancet. sion, in acute stroke patients. Ann Neurol. 2002;51(4):417–32. doi:
2004;363(9411):768–74. doi: http://dx.doi.org/10.1016/ http://dx.doi.org/10.1002/ana.10136. PubMed.
S0140-6736(04)15692-4. PubMed. 55 Heiss W-D. PET imaging in ischemic cerebrovascular disease: current
44 Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel status and future directions. Neurosci Bull. 2014;30(5):713–32. doi:
DW, et al.; HERMES Collaborators. Time to Treatment With Endovas- http://dx.doi.org/10.1007/s12264-014-1463-y. PubMed.
cular Thrombectomy and Outcomes From Ischemic Stroke: A Meta- 56 Heiss W-D, Zaro Weber O. Validation of MRI Determination of the
analysis. JAMA. 2016;316(12):1279–88. doi: http://dx.doi.org/10.1001/ Penumbra by PET Measurements in Ischemic Stroke. J Nucl Med.
jama.2016.13647. PubMed. 2017;58(2):187–93. doi: http://dx.doi.org/10.2967/jnumed.116.185975.
45 Cheng-Ching E, Frontera JA, Man S, Aoki J, Tateishi Y, Hui FK, et al. PubMed.
Degree of collaterals and not time is the determining factor of core in- 57 Donnan GA, Baron JC, Ma H, Davis SM. Penumbral selection of pa-
farct volume within 6 hours of stroke onset. AJNR Am J Neuroradiol. tients for trials of acute stroke therapy. Lancet Neurol. 2009;8(3):261–9.
2015;36(7):1272–6. doi: http://dx.doi.org/10.3174/ajnr.A4274. PubMed. doi: http://dx.doi.org/10.1016/S1474-4422(09)70041-9. PubMed.
46 Cheripelli BK, Huang X, McVerry F, Muir KW. What is the relationship 58 Heit JJ, Wintermark M. Perfusion Computed Tomography for the Evalu-
among penumbra volume, collaterals, and time since onset in the first 6 ation of Acute Ischemic Stroke: Strengths and Pitfalls. Stroke.
h after acute ischemic stroke? Int J Stroke. 2016;11(3):338–46. doi: 2016;47(4):1153–8. doi: http://dx.doi.org/10.1161/STROKEA-
http://dx.doi.org/10.1177/1747493015620807. PubMed. HA.116.011873. PubMed.
47 Hwang Y-H, Kang D-H, Kim Y-W, Kim Y-S, Park S-P, Liebeskind DS. 59 Heiss W-D, Sobesky J, Smekal U, Kracht LW, Lehnhardt FG, Thiel A,
Impact of time-to-reperfusion on outcome in patients with poor collater- et al. Probability of cortical infarction predicted by flumazenil binding
als. AJNR Am J Neuroradiol. 2015;36(3):495–500. doi: and diffusion-weighted imaging signal intensity: a comparative positron
http://dx.doi.org/10.3174/ajnr.A4151. PubMed. emission tomography/magnetic resonance imaging study in early is-
48 Maurer CJ, Egger K, Dempfle AK, Reinhard M, Meckel S, Urbach H. chemic stroke. Stroke. 2004;35(8):1892–8. doi: http://dx.doi.org/
Facing the Time Window in Acute Ischemic Stroke: The Infarct Core. 10.1161/01.STR.0000134746.93535.9b. PubMed.
Clin Neuroradiol. 2016;26(2):153–8. doi: http://dx.doi.org/10.1007/ 60 Olivot JM, Mlynash M, Thijs VN, Kemp S, Lansberg MG, Wechsler L,
s00062-016-0501-8. PubMed. et al. Optimal Tmax threshold for predicting penumbral tissue in acute
49 McVerry F, Liebeskind DS, Muir KW. Systematic review of methods stroke. Stroke. 2009;40(2):469–75. doi: http://dx.doi.org/10.1161/
for assessing leptomeningeal collateral flow. AJNR Am J Neuroradiol. STROKEAHA.108.526954. PubMed.
2012;33(3):576–82. doi: http://dx.doi.org/10.3174/ajnr.A2794. PubMed. 61 Forkert ND, Kaesemann P, Treszl A, Siemonsen S, Cheng B, Handels
50 Martinon E, Lefevre PH, Thouant P, Osseby GV, Ricolfi F, Chavent A. H, et al. Comparison of 10 TTP and Tmax estimation techniques for MR
Collateral circulation in acute stroke: assessing methods and impact: a perfusion-diffusion mismatch quantification in acute stroke. AJNR Am J
literature review. J Neuroradiol. 2014;41(2):97–107. doi: Neuroradiol. 2013;34(9):1697–703. doi: http://dx.doi.org/10.3174/
http://dx.doi.org/10.1016/j.neurad.2014.02.001. PubMed. ajnr.A3460. PubMed.
51 Raymond SB, Schaefer PW. Imaging Brain Collaterals: Quantification, 62 McKinley R, Häni L, Gralla J, El-Koussy M, Bauer S, Arnold M, et al.
Scoring, and Potential Significance. Top Magn Reson Imaging. Fully automated stroke tissue estimation using random forest classifiers
2017;26(2):67–75. doi: http://dx.doi.org/10.1097/ (FASTER). J Cereb Blood Flow Metab. 2017;37(8):2728–41. doi:
RMR.0000000000000123. PubMed. http://dx.doi.org/10.1177/0271678X16674221. PubMed.
52 Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et 63 Cuccione E, Padovano G, Versace A, Ferrarese C, Beretta S. Cerebral
al.; Technology Assessment Committee of the American Society of In- collateral circulation in experimental ischemic stroke. Exp Transl Stroke
terventional and Therapeutic Neuroradiology; Technology Assessment Med. 2016;8(1):2. doi: http://dx.doi.org/10.1186/s13231-016-0015-0.
Committee of the Society of Interventional Radiology. Trial design and PubMed.
reporting standards for intra-arterial cerebral thrombolysis for acute is- 64 Nishijima Y, Akamatsu Y, Weinstein PR, Liu J. Collaterals: Implica-
chemic stroke. Stroke. 2003;34(8):e109–37. doi: http://dx.doi.org/ tions in cerebral ischemic diseases and therapeutic interventions. Brain
10.1161/01.STR.0000082721.62796.09. PubMed. Res. 2015;1623:18–29. doi: http://dx.doi.org/10.1016/j.brain-
res.2015.03.006. PubMed.
Swiss Medical Weekly · PDF of the online version · www.smw.ch Page 7 of 7
Published under the copyright license “Attribution – Non-Commercial – No Derivatives 4.0”.
No commercial reuse without permission. See http://emh.ch/en/services/permissions.html.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 2020 Muscle Atrophy and The SestrinsDocument4 pages2020 Muscle Atrophy and The SestrinsTote Cifuentes AmigoNo ratings yet
- Muscle Atrophy书Document618 pagesMuscle Atrophy书xiangyu RenNo ratings yet
- 2021 Shared and Distinct Mechanisms of Skeletal Muscle AtrophyDocument23 pages2021 Shared and Distinct Mechanisms of Skeletal Muscle AtrophyTote Cifuentes AmigoNo ratings yet
- 2020 Skeletal Muscle Atrophy. Multiple Pathways Leading To A Common OutcomeDocument11 pages2020 Skeletal Muscle Atrophy. Multiple Pathways Leading To A Common OutcomeTote Cifuentes AmigoNo ratings yet
- 2021 Mechanisms of Muscle Atrophy and Hypertrophy. Implications in Health and DiseaseDocument12 pages2021 Mechanisms of Muscle Atrophy and Hypertrophy. Implications in Health and DiseaseTote Cifuentes AmigoNo ratings yet
- 2018 Weight Loss Increases All Cause Mortality in Overwight or Obese Patients With DiabetesDocument10 pages2018 Weight Loss Increases All Cause Mortality in Overwight or Obese Patients With DiabetesTote Cifuentes AmigoNo ratings yet
- HTTPSWWW Who Intpublicationsiitem9789240015128Document104 pagesHTTPSWWW Who Intpublicationsiitem9789240015128Miguel Reis CostaNo ratings yet
- 1985 Scale MAS StrokeDocument6 pages1985 Scale MAS StrokeTote Cifuentes AmigoNo ratings yet
- Advances in Geroscience-Springer International Publishing (2016)Document637 pagesAdvances in Geroscience-Springer International Publishing (2016)Tote Cifuentes AmigoNo ratings yet
- The End of PhysiotherapyDocument66 pagesThe End of PhysiotherapyTote Cifuentes AmigoNo ratings yet
- Treatment of Acute Ischemic StrokeDocument13 pagesTreatment of Acute Ischemic Strokeamania jeumpa nur alamNo ratings yet
- 10 1016@J Jphys 2019 08 005Document1 page10 1016@J Jphys 2019 08 005Tote Cifuentes AmigoNo ratings yet
- 2016 Ischemic Stroke. Basic Pathophysiology and Clinical ImplicationDocument21 pages2016 Ischemic Stroke. Basic Pathophysiology and Clinical ImplicationTote Cifuentes AmigoNo ratings yet
- The Balance Evaluation Systems Test (Bestest) To Differentiate Balance DeficitsDocument16 pagesThe Balance Evaluation Systems Test (Bestest) To Differentiate Balance DeficitsTote Cifuentes AmigoNo ratings yet
- 2011 Neurological Principles and Rehabilitation of Action Disorders. Common Clinical DeficitsDocument12 pages2011 Neurological Principles and Rehabilitation of Action Disorders. Common Clinical DeficitsTote Cifuentes AmigoNo ratings yet
- HHS Public Access: Early Rehabilitation After Stroke: A Narrative ReviewDocument20 pagesHHS Public Access: Early Rehabilitation After Stroke: A Narrative ReviewfransAPNo ratings yet
- 2016 Accessing Rehabilitation After Stroke - A Guessing Game.Document6 pages2016 Accessing Rehabilitation After Stroke - A Guessing Game.Tote Cifuentes AmigoNo ratings yet
- 2016 Chapter 6 Stroke PathophysiologyDocument8 pages2016 Chapter 6 Stroke PathophysiologyTote Cifuentes AmigoNo ratings yet
- 2006 Issues in Selecting Ourtome Measures To Assess Functional Recovery After StrokeDocument20 pages2006 Issues in Selecting Ourtome Measures To Assess Functional Recovery After StrokeTote Cifuentes AmigoNo ratings yet
- Rehabilitation After Stroke PDFDocument8 pagesRehabilitation After Stroke PDFBetaNo ratings yet
- 2019 Aerobic Training and Mobilization Early Post Stroke. Cautions and ConsiderationsDocument26 pages2019 Aerobic Training and Mobilization Early Post Stroke. Cautions and ConsiderationsTote Cifuentes AmigoNo ratings yet
- 2018 Oligemia, Penumbra, Infarction. Understanding Hypoperfusion With NeuroimagingDocument11 pages2018 Oligemia, Penumbra, Infarction. Understanding Hypoperfusion With NeuroimagingTote Cifuentes AmigoNo ratings yet
- Paper NSciencesDocument15 pagesPaper NSciencesTote Cifuentes AmigoNo ratings yet
- 2017 Relevance of CerebralDocument7 pages2017 Relevance of CerebralTote Cifuentes AmigoNo ratings yet
- Dalise 2014 Brain Plasticity and Recovery in Preclinical Models of StrokeDocument26 pagesDalise 2014 Brain Plasticity and Recovery in Preclinical Models of StrokeTote Cifuentes AmigoNo ratings yet
- Reimagining and Empowering The Design of Projects A ProJect - Based Learning Goals FrameworkDocument10 pagesReimagining and Empowering The Design of Projects A ProJect - Based Learning Goals FrameworkTote Cifuentes AmigoNo ratings yet
- 2013 The Physiological Demands of Table Tennis A ReviewDocument9 pages2013 The Physiological Demands of Table Tennis A ReviewTote Cifuentes AmigoNo ratings yet
- Impact of Habitual Physical Activity and Type of Exercise On Physical Performance Across Ages in Community-Living PeopleDocument12 pagesImpact of Habitual Physical Activity and Type of Exercise On Physical Performance Across Ages in Community-Living PeopleTote Cifuentes AmigoNo ratings yet
- 2011 The Playing Posture, Activities and Health of The Table Tennis PlayerDocument6 pages2011 The Playing Posture, Activities and Health of The Table Tennis PlayerTote Cifuentes AmigoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Intertrigo and Secondary Skin InfectionsDocument5 pagesIntertrigo and Secondary Skin Infectionskhalizamaulina100% (1)
- Soal Bahasa Inggris - Evaluasi TestDocument9 pagesSoal Bahasa Inggris - Evaluasi TestHamdani IlhamNo ratings yet
- Dissertation 7Document18 pagesDissertation 7Sidhartha KumarNo ratings yet
- Understanding Receiver Operating Characteristic Roc CurvesDocument2 pagesUnderstanding Receiver Operating Characteristic Roc CurvesOlievia Herinda AdhiafebriantyNo ratings yet
- Hamza DissertDocument108 pagesHamza DissertMobin Ur Rehman KhanNo ratings yet
- Female PelvisDocument11 pagesFemale PelvisAhmed Gh Al-zechrawi100% (1)
- Biometric Insulin PumpDocument25 pagesBiometric Insulin PumpvenkatNo ratings yet
- Brain CTDocument83 pagesBrain CTArvind Jha100% (2)
- Pernicious Anemia - MitchDocument18 pagesPernicious Anemia - Mitchthalafuj100% (1)
- Osteomalasia GujaratiDocument4 pagesOsteomalasia Gujaratidhavalb20No ratings yet
- Notes From The Lecture by DR Hiromi ShinyaDocument3 pagesNotes From The Lecture by DR Hiromi ShinyaAfianti Sulastri100% (1)
- Blood Cold ChainDocument74 pagesBlood Cold Chainشريف عبد المنعمNo ratings yet
- Errors in Cephalometry - WordDocument39 pagesErrors in Cephalometry - WordSrinivasan BoovaraghavanNo ratings yet
- What's Bugging Your Teen?-The Microbiota and Adolescent Mental HealthDocument13 pagesWhat's Bugging Your Teen?-The Microbiota and Adolescent Mental HealthPaula Manalo-SuliguinNo ratings yet
- Tanganyika Nacte Past Paper-1Document116 pagesTanganyika Nacte Past Paper-1Mnawaru KhalfaniNo ratings yet
- Setting Fire On The MountainDocument5 pagesSetting Fire On The MountainElizabeth Durkee NeilNo ratings yet
- 03 Orlando D. Garcia, JR., Et Al. vs. Ranida Salvador, Et Al.Document2 pages03 Orlando D. Garcia, JR., Et Al. vs. Ranida Salvador, Et Al.Raj AtmanNo ratings yet
- Quality Control in Homoeopathy: DefinitionDocument3 pagesQuality Control in Homoeopathy: Definition11 Isha ChitnisNo ratings yet
- CV - Updated April 2023Document6 pagesCV - Updated April 2023api-641524095No ratings yet
- Menastil Complete Clinical Trials - Pain Relief That Works.Document43 pagesMenastil Complete Clinical Trials - Pain Relief That Works.emoryholstNo ratings yet
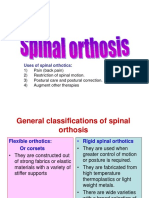
- Spinal OrthosisDocument16 pagesSpinal OrthosisChristya Ari NugrahaNo ratings yet
- Running Head: Normal Saline vs. Heparin 1Document9 pagesRunning Head: Normal Saline vs. Heparin 1MaureenAmilcaNo ratings yet
- SOAP Notes: AuthorsDocument6 pagesSOAP Notes: AuthorsRanita Kumalasari100% (4)
- Common Medical AbbreviationsDocument1 pageCommon Medical Abbreviationskedwards108No ratings yet
- Soil Transmitted Helminth Infections: The Nature, Causes and Burden of The ConditionDocument79 pagesSoil Transmitted Helminth Infections: The Nature, Causes and Burden of The ConditionYokaiCO100% (1)
- INTRODUCTION of Tuberculosis Final NewDocument2 pagesINTRODUCTION of Tuberculosis Final Newbatch1No ratings yet
- 200 Bed Hospital Project ReportDocument59 pages200 Bed Hospital Project ReporttonyNo ratings yet
- Ayurveda PDFDocument12 pagesAyurveda PDFsanjit0907_982377739No ratings yet
- Chemistry in Everyday LifeDocument398 pagesChemistry in Everyday LifeArsh DhawanNo ratings yet
- HemoCue Plasma Low HB Overview 131123Document22 pagesHemoCue Plasma Low HB Overview 131123Trung LeNo ratings yet