Professional Documents
Culture Documents
IJP Volume 4 Issue 1 Pages 1233-1242
IJP Volume 4 Issue 1 Pages 1233-1242
Uploaded by
Anca AdamCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IJP Volume 4 Issue 1 Pages 1233-1242
IJP Volume 4 Issue 1 Pages 1233-1242
Uploaded by
Anca AdamCopyright:
Available Formats
http:// ijp.mums.ac.
ir
Original Article (Pages: 1233-1242)
Children with Steroid-resistant Nephrotic Syndrome: a Single-
Center Study
*Rahime Renda11, Özlem Aydoğ 2, Mehmet Bülbül 3, Evrim Kargın Çakıcı 4
1
Pediatric Nephrology Department, Antalya Research and Education Hospital, Antalya, Turkey.
2
Associate Professor, Pediatric Nephrology Department, Ankara Dr. Sami Ulus Research and Education
Hospital, Ankara, Turkey.
2
Associate Professor, Pediatric Nephrology Department, Ankara Dr. Sami Ulus Research and Education
Hospital, Ankara, Turkey.
4
Pediatric Nephrology Department, Ankara Dr. Sami Ulus Research and Education Hospital, Ankara, Turkey.
Abstract
Background
Steroid-resistant nephrotic syndrome (SRNS) accounts for 10%-20% of all cases of idiopathic
nephrotic syndrome. These patients are at risk of developing end-stage renal disease. The aim of this
study was to determine the demographic characteristics, renal biopsy findings, response to
immunosuppressive treatment, and prognosis in pediatric patients with SRNS.
Materials and Methods
This retrospective study included 31 patients diagnosed as primary SRNS. Age at first episode,
gender, parental consanguinity, and familial history of nephrotic syndrome were recorded.
Demographic characteristics, renal biopsy findings, response to immunosuppressive treatment and
prognosis were analyzed, as were the number of and treatment of relapses, extra-renal manifestations
and complications of disease and treatment. Data were analyzed using SPSS version 15.0
Results
Mean age at first episode of nephrotic syndrome was 4.1±2.9 years. At the end of the first
immunosuppressive treatment cycle, 14 (51.8%) patients achieved complete remission, 4 (14.8%)
patients achieved partial remission and 9 patients (33.3%) did not achieve remission. Analysis of the
final status of the patients showed that 16 patients (51.6%) developed remission, 5 patients (16%)
continued to have nephrotic range proteinuria and 10 patients (32%) developed chronic renal failure
(CRF).
Conclusion
The treatment of SRNS remains controversial. Early genetic testing can help the inevitable
immunosuppressive treatments which may not be effective and have several side effects. Calcineurin
inhibitors and mycophenolate mofetil are known to be effective immunosuppressive drugs for treating
steroid resistant nephrotic syndrome.
Key Words: Focal segmental glomerulosclerosis, Mutations, Steroid-resistant nephrotic syndrome.
*Please cite this article as: Renda R, Aydoğ Ö, Bülbül M, Kargın Çakıcı E. Children with Steroid-resistant
Nephrotic Syndrome: a Single-Center Study. Int J Pediatr 2016; 4(1): 1233-42.
*Corresponding Author:
Rahime Renda, MD, Department of Pediatric Nephrology, Antalya Research and Education Hospital, Varlık
Mah. Kazık Karabekir Cad. 07100 Soğuksu/Muratpaşa/Antalya, Turkey. Fax: +90 (242) 249 00 62
Email: rahimeg@yahoo.com
Received date Nov 29, 2015 ; Accepted date: Dec 28, 2015
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1233
Children with Steroid-Resistant Nephrotic Syndrome
1- INTRODUCTION hypoalbuminemia ≥2.5 g/dL. Complete
remission was defined as 24-h protein
The majority of children with idiopathic
excretion <4 mg/m2/h, uPCR <0.2 mg/ mg,
nephrotic syndrome (NS) respond to
or a trace-negative dipstick. Partial
steroid therapy, but about 10%-20% have
remission was defined as a ≥50%
steroid-resistant nephrotic syndrome
reduction in the basal proteinuria value or
(SRNS) (1). In 50%-60% of children with
uPCR: 0.2-2mg/mg. Non-response was
SRNS the cause cannot be determined,
defined as a reduction in the basal
whereas one third of patients have a single
proteinuria value <50% or a uPCR >2 mg/
genetic defect that affects glomerular
mg. Relapse was defined as 3 consecutive
podocyte structure or function. Moreover,
days of ≥3+ proteinuria based on dipstick
most patients with SRNS are unresponsive
or a uPCR >2mg/mg in patients that were
to immunosuppressive treatments (2). The
previously in remission. Chronic renal
most common mutations in patients with
failure (CRF) was defined as an estimated
SRNS are in the NPHS1 gene that encodes
glomerular filtration rate (eGFR) <80
nephrin, the NPHS2 gene that encodes
mL/min/1.73 m² (irreversibly impaired
podocin, and the WT1 gene that encodes
kidney function). ESRD was defined as the
transcription tumor suppressor protein.
need for renal replacement treatment or an
The most common observed histological
eGFR <15 mL/min/1.73 m2. Also, eGFR
lesion in SRNS patients is focal segmental
was determined by Schwartz equation (3).
glomerulosclerosis (FSGS) (2). SRNS in
general and FSGS specifically are 2-2. Patients
associated with a 50% risk of end-stage This retrospective study included 31
renal disease (ESRD) within 5 years of patients diagnosed as primary SRNS.
diagnosis in patients that do not achieve Patients with secondary SRNS were
partial or complete remission (38). The excluded from the study. Patient gender,
aims of treatment are to correct proteinuria
age at first episode, parental consanguinity
and preserve kidney function, but the and family history of nephrotic syndrome
optimal treatment method remains were recorded. Renal biopsy was
controversial. The present study aimed to performed in 29 of the patients. Mutation
determine the demographic characteristics,
analysis was performed in all patients
renal biopsy findings, genetic mutations, using Sanger sequencing. All patients were
response to treatment, and prognosis in investigated for NPHS2 and WT1
pediatric patients with SRNS. mutations, NPHS1 mutation was
2- MATERIALS AND METHODS investigated in 4 patients that had
congenital nephrotic syndrome (CNS), and
2-1. Definitions LAMB2 mutation was investigated in one
patient with CNS that was thought to have
SRNS was diagnosed in patients with
clinical Pierson syndrome. Patient
idiopathic NS based on lack of complete
demographic characteristics, renal biopsy
remission despite treatment with oral
findings, response to immunosuppressive
steroids 60 mg/m²/day (maximum: 60
treatment and prognosis were also
mg/d) for 8 weeks or 60 mg/m²/day for 4
analyzed. The study protocol was
weeks followed by Intravenous (IV) pulse
conducted in accordance with the
methylprednisolone (MPZ) 30 mg/kg/day
Declaration of Helsinki and approved by
for 3 days (maximum: 1 g/ day). NS was
the Dr. Sami Ulus Children’s Hospital
defined as 24-h protein excretion >40
Ethics Committee. Written informed
mg/m²/h, a urine protein/creatinine ratio
consent was provided by the patients’
(uPCR)>2 mg/mg or dipstick≥2+ and
families before the start of study.
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1234
Renda et al.
2-3. Treatment converting enzyme inhibitor and/or
angiotensin receptor blocker, and anti-
Immunosuppressive treatments, dosages
lipidemics) were administered when
and durations are shown in (Tables 1 and
necessary in all patients. Patients with
2). Due to its side-effects,
CRF were given supportive treatment and
cyclophosphamide (CYC) was not
appropriate renal replacement therapy was
administered for a period exceeding 12
administered in those with ESRD.
weeks. After 6 months, patients that did
not respond to cyclosporine A (CsA) were 2-4. Statistical analysis
switched to mycophenolate mofetil (MMF) Data were analyzed using SPSS version
and if a response was achieved the 15.0 for Windows (SPSS Inc., Chicago,
treatment was continued for at least 12 IL). Data are expressed as frequency and
months. Immunosuppressive treatment was percentage. Relationships between
not administered to the patients with CNS. variables were analyzed via the chi-square
In addition to immunosuppressive drugs,
test and Mann-whitney U test. The level of
statistical significance was set at P < 0.05.
oral prednisolone at tapering doses) and
renoprotective treatment (angiotensin-
Table 1: The Tune-Mendoza protocol.
Weeks IV Pulse MPZ* Oral Prednisolone
1-2 30 mg kg–1 QWK** -
3-10 30 mg kg–1 QWK 1.5 mg kg–1 eod***
11-18 30 mg kg–1 once every 2 weeks 1 mg kg–1 eod
19-50 30 mg kg–1 once per month 0.5 mg kg–1 eod
51-82 30 mg kg–1 once every 2 months 0.5 mg kg–1 eod
*MPZ: Methylprednisolone, **QWK: Every week; ***eod: every other day.
Table 2: Other immunosuppressive treatment protocols.
Immunosuppressive drugs Dose Dose interval (duration)
Cyclophosphamide 2 mg kg-1 day-1 Single dose (8-12 weeks)
Cyclosporine A 3-6 mg kg-1 day-1 2 doses (6-24 months)
Mycophenolate mofetil 1000-1200 mg/m2/day 2 doses (6-48 months)
3-RESULTS Renal biopsy was performed in 29 of the
31 SRNS patients and the findings were as
The study included 31 (17 male and 14
follows: FSGS: n = 18 (62%); mesangial
female) SRNS patients. The male-female
proliferation: n = 8 (27%); minimal change
ratio was 1.2:1; the difference in the
disease (MCD): n = 2 (6.8%); diffuse
number of males and females was not
mesangial sclerosis (DMS): n = 1 (3.4%).
significant (P > 0.05). Mean age at the first
A mutation was noted in only 4 (12.9%)
episode of SRNS was 4.1±2.9 years. The
patients (Table.4), of which 2 had NPHS2
mean follow-up period was 63.06 ± 60.12
homozygous mutation. Mutation was
months. Parental consanguinity was noted
detected in only 2 of the 4 patients with
in 13 (41.9%) of the patients and 5 (16%)
CNS: patient no. 1, who was diagnosed as
patients had a family history of nephrotic
Denys-drash Syndrome (DDS), had WT1
syndrome. Patient demographic
heterozygous mutation and patient no. 2,
characteristics are shown in (Table. 3).
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1235
Children with Steroid-Resistant Nephrotic Syndrome
who was diagnosed as Pierson syndrome, relapses another immunosuppressive
had a homozygous mutation in the treatment (CsA or MMF) was required. In
LAMB2 gene. Extrarenal abnormalities patients in which the duration of CsA
were noted in 2 patients. Ambigous treatment was administered for 2- year and
genitalia and bilateral Wilms tumors were in patients that did not respond to CsA for
noted in the patient with DDS, and eye 6 months, the treatment was changed to
abnormalities were observed in the patient MMF. At the time of the last follow-up 9
with Pierson syndrome. Supportive (51.6%) patients had achieved complete
treatment only (no immunosuppressive remission and 7 had achieved partial
treatment) was administered to the 4 remission. Of the 15 (48.4%) patients that
patients with CNS, whereas various did not respond to immunosuppressive
immunosuppressive treatment protocols treatment, or had CNS, 4 of them
were administered to the remaining 27 continued nephrotic range proteinuria and
SRNS patients. The response to the first 11 of them developed CRF. During
immunosuppressive treatment, number of follow-up period, CRF occurred mean in
relapses, relapse treatment, final status of 29.4 ± 46.8 months. Among the 11 patients
the patients at the last follow-up, renal with CRF, 5 developed ESRD and
biopsy findings and mutation analysis subsequently received continuous
findings are shown at the end page of ambulatory peritoneal dialysis (CAPD). Of
article (Table.5). the 5 patients with ESRD, 3 died due to
CAPD and/or primary disease-associated
At least one immunosuppressive treatment
complications and 2 previously had
protocol was administered to 27 of the
undergone renal transplantation. Of the 2
patients with SRNS. The Mendoza
patients that underwent renal
protocol was administered to 6 patients of
transplantation, 1 had CNS and a family
which 1 had partial remission and 5 had no
history of nephrotic syndrome, but no
response. CYC was administered to 8
mutation was found both in the patient and
patients, none of whom achieved
her parents. This patient renal biopsy
remission. CsA was administered to 24
showed mesangial proliferation. Renal
patients; 10 achieved complete remission,
transplantation from her father was
4 had partial remission, and 10 had no
performed 3 years ago, there was no post-
response. MMF was administered to 9
transplant recurrence of disease and the
patients of which 2 achieved complete
patient is in complete remission. The other
remission, 1 achieved partial remission,
patient that had undergone renal
and 6 had no response. In total, 14 (51.8%)
transplantation had no mutation or family
of the 27 patients achieved complete
history of nephrotic syndrome. His renal
remission, 4 (14.8%) achieved partial
biopsy showed FSGS. He underwent renal
remission, and 9 (33.3%) did not have
transplantation from his father 5 years ago
remission.
and 1 month post transplantation disease
During follow-up, 12 relapses developed recurrence developed, but following acute
in 9 of the 14 patients that had achieved humoral rejection treatment the patient is
complete remission. In addition, 9 relapses now in complete remission. The most
occurred in 8 patients after the termination common complications in patients with
of CsA treatment. Treatment for all the SRNS were retarded growth and
relapses was 3 days of IV pulse development (26%), osteoporosis (22.5%),
Methylprednisolone (MPZ) 30 mg/kg/day cushingoid changes (16%), infections
followed by oral prednisolone. In 2 (16%) and hirsutism (13%). These
relapses complete remission was achieved complications were due to long-term, high-
with only pulse MPZ; for the other 10 dose steroid use.
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1236
Renda et al.
Table 3: Patient demographic characteristics
Gender (male/female) Number (17/14)
Age at first episode
0-4 months 4
4-12 months 1
13 months-5 years 20
6-12 years 6
Parental consanguinity 13 (41.9%)
Family history of similar disease 5 (16%)
Table 4: Genetic mutation findings
Patient no. Genetic Mutations
1 WT1 gene, 9th exon c.1186G>C (p.Asp396His) heterozygous
2 LAMB2 gene, homozygous IVS4+2T > C donor splice site mutation
3 NPHS2 gene, 5th exon c.538G>A homozygous p.V180M protein change
4 NPHS2 gene, 4th exon 467delT homozygous L156fsX180
4- DISCUSSION
(10, 11). In the present study, the patients
SRNS constitutes 10%-20% of all cases who have a mutation, age at onset of NS
of idiopathic NS. In majority of children was lower. One third of SRNS cases are
with SRNS the underlying cause cannot be associated with a mutation in genes
determined, whereas one third of patients encoding proteins that negatively affect
had single- genetic defects (2). The present podocyte structure or function (12). The
study aimed to evaluate SRNS patients, in likelihood of a genetic mutation was
terms of demographic characteristics, renal significantly higher in SRNS patients with
biopsy findings, underlying genetic parental consanguinity or a family history
abnormalities, response to treatment, of nephrotic syndrome (14). Among the
relapses, prognosis and complications. present study’s SRNS patients with a
Previous studies reported that NS was disease causing mutation, two had
more common in males than females (4, consanguineous parents and one had a
5). In a study of children in Nigeria by family history of nephrotic syndrome.
Anochie et al. (6) the male-female ratio Renal biopsy is recommended for
was 1:1, whereas Mekahli et al. (7) histological diagnosis of children with
reported a ratio of 1:4 and in the present SRNS and for determining treatment
study it was 1:2. NS emerges most often options and prognosis (15,16). The 3 most
around the age of 2 years and 70%-80% of frequently seen histological findings are
cases occur before age 6 years (8). With FSGS, mesangial proliferation and MCD
increasing age at the time of the first (16). Several recent studies reported that as
episode of NS, the frequency of FSGS the FSGS rate increases, the steroid
increases and the response to steroid response rate decreases (17, 18). The best
treatment decreases (9). In the present example of this was shown in a study by
study mean age at first episode of NS was Balanszak et al. (19), in which 102 patients
4.1±2.9 years; 3.18 years in males, vs. 4.86 were evaluated during 2 distinct time
years in females. These findings are periods (1986-1995 [period 1] and 1996-
similar to those reported earlier in Turkey
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1237
Children with Steroid-Resistant Nephrotic Syndrome
2005[ period 2]). Renal biopsy was present study. SRNS patients with multi-
performed in 28 patients during period 1 drug resistance thought there is to be an
and in 44 patients during period 2. During underlying genetic pathology (24).
period 2, the number of patients with MCD Similarly, in the current study SRNS
was lower and the number of those with patients that were multidrug resistant, but
mesangial proliferation and FSGS was not determined to have a genetic mutation
significantly higher, as compared to period or polymorphism, were thought to have an
1. In the present study mesangial undetermined mutation. Among the
proliferation and FSGS were found to be present study, of 4 patients with CNS, 2
significantly high in our patients. had a heterozygous WT1 mutation and a
homozygous LAMB2 mutation; the same
Genetic mutations are frequently seen in
heterozygous mutations were in both
patients with CNS, hereditary NS and
patients’ mothers. The father of the patient
syndromic NS (20). Previous studies have
with Pierson syndrome could not undergo
recommended that to prevent unnecessary
genetic analysis. When evaluated together
use of immunosuppressive drugs and the
with extra-renal findings, the patient with
associated side-effects in SRNS patients,
WT1 heterozygous mutation was
mutation analysis should be conducted,
diagnosed as DDS (25) and the patient
taking into consideration the age at onset
with LAMB2 homozygous mutation was
of NS, renal histopathological findings and
diagnosed as Pierson syndrome (26).
extra-renal anomalies (13,21). Risk factors
for the development of SRNS associated SRNS causes significant morbidity, the
with genetic causes include family history treatment of which is extremely difficult.
of nephrotic syndrome, the occurrence of Pulse IV MPZ was first recommended for
proteinuria during the first year of life, and the treatment of SRNS by Mendoza and
the presence of syndromic SRNS (22). Tune (27) in 1990; however, more recent
studies have reported severe side-effects
After diagnosis of SRNS, the first step is
associated with high-dose, long-term
recommended to perform NPHS1, NPHS2
steroid use. High dose and long-term
and WT1 gene mutation analysis in
steroid administration involves
patients with CNS and NPHS2 and WT1
hospitalization and insufficient response;
gene mutation analysis in patients without
therefore, this treatment is no longer
CNS. In syndromic patients with extra-
recommended (23). In the present study
renal findings specific genes, including
the Mendoza protocol was administered to
LAMB2, SMARCAL1 and LMX1B,
6 patients; of them, one had partial
should be analyzed (23). Reported SRNS
response and five had no response. In
mutation rates varied by country (24).
addition, multiple side-effect of long-term,
Genetic analysis of 110 patients with
high-dose steroid use were noted. Several
SRNS in Spain (22) showed that 33% of
studies reported that alkylating agents are
patients with a family history of nephrotic
highly toxic and not effective for obtaining
syndrome had a genetic mutation, vs. 25%
remission in patients with SRNS (28, 29).
of patients with a negative family history
In the present study CYC was
and that all 15 CNS patients had a
administered to 8 patients, none of which
mutation (NPHS1: n = 12; NPHS2: n = 1;
achieved remission.
WT1: n = 2). In the present study 4
(12.9%) of the 31 patients had mutation CsA has been shown to have a non-
(NPHS2: n = 2; WT1: n = 1; LAMB2: n = immunological, anti-proteinuric effect, in
1); the 2 patients with NPHS2 mutation addition to its immunosuppressive effect
were homozygous. Polymorphism in the (30); in support of this, CsA was shown to
podocin gene was noted in 5 patients in the be effective in SRNS patients with NPHS2
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1238
Renda et al.
mutation (31) and in patients with genetic testing may prevent the inevitable
hereditary nephritis (32). Remission rates immunosuppressive treatments, which may
of 25%-87% were reported for CsA, which not be effective and have several side
is commonly used drug for treating SRNS effects. Despite the small patient
(33). Similarly, in the present study population, the present study’s findings
remission was achieved in 14 (58.3%) of show that age at the first episode of SRNS,
24 patients treated with CsA, but no parental consanguinity and family history
response was obtained in two NPHS2 of nephrotic syndrome did not have a
homozygous patients. Among patients significant effect on prognosis. The most
treated with CsA, 50%-85% develop important factor that affected morbidity
relapse post CsA treatment and 25%-50% and mortality in the patients with SRNS
of patients develop drug resistance (33). In was the response to immunosuppressive
the present study 12 relapses occurred in 9 treatment. CNI and MMF were effective
of 14 patients that had achieved complete immunosuppressive drugs; however,
remission; 9 of these relapses occurred additional, large-scale prospective and
after termination of CsA treatment. controlled studies are needed to more
clearly determine which are the most
The literature includes only a few studies
effectivness immunosuppressive
on MMF treatment in SRNS patients. A
treatments for SRNS.
Brazilian study that included 52 SRNS
patients treated with MMF reported that 6-CONFLICT OF INTEREST
complete remission was achieved in 12 The authors declare that there are no
patients and partial remission in 19 (34). conflicts of interest.
Gipson et al. (35) treated one group of
SRNS patients with CNI and another 7-FINANCIAL SUPORT: No relevant
group with MMF and oral dexamethasone. financial relationship exists.
Complete or partial remission was noted in
33% of the patients in the MMF group and 8-ACKNOWLEDGMENT
in 45.8% of those in the CNI group. In the We wish to thank Prof. Fatih Özaltın for
present study, 9 patients were treated with his support at the Nephrogenetics
MMF, with a remission rate of 33.3%. Laboratory, Hacettepe University, Ankara-
In total, 15 (48.4%) of the present study’s Turky.
patients did not respond to treatment, NS
continued in 4 patients, and CRF 9-REFERENCES
developed in 11 (35.5%). Mean time from 1. Niaudet P. Treatment of childhood
first attack of NS to the development of steroid-resistant idiopatic nephrosis with a
CRF was 29.4 ± 46.8 months. This time combination of cyclosporine and prednisone.
period was similar to those previously French society of pediatric nephrology. J
reported from Turkey (10). ESRD was Pediatr 1994; 125:981-6.
accounted for more than 10% of SRNS 2. Kim JS, Bellew CA, Silverstein DM,
patients (36, 37) and in the present study Aviles DH, Boineau FG, Vehaskari VM. High
16.1% of the patients developed ESRD. incidence of initial and late steroid resistance
in childhood nephrotic syndrome. Kidney Int
5-CONCLUSION 2005; 68(3):1275-81.
In conclusion, the optimal treatment of 3. Schwartz GJ, Haycock GB, Edelmann
SRNS remains controversial. Identification CM Jr, Spitzer A. A simple estimate of
of a genetic mutation is important factor glomerular filtration rate in children derived
for predicting responsiveness to from body length and plasma creatinine.
Pediatrics 1976; 58:259-263.
immunosuppressive treatment. Early
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1239
Children with Steroid-Resistant Nephrotic Syndrome
4. Niaudet P. Steroid sensitive idiopatic nephrotic syndrome. Pediatr Nephrol 2010;
syndrome in children. In: Avner ED, Harmon 25(2):241-52.
WE (eds). Pediatric Nephrology, 5th ed.
15. Gbadegesin R, Lavin P, Foreman J,
Philadelphia: Lippinccott, Wiliams-Wilkins,
Winn M. Pathogenesis and therapy of focal
2004. p. 543.
segmental glomerulosclerosis: an update.
5. Lahdenkari AT et al. Clinical features Pediatr Nephrol 2011; 26(7):1001-15.
and outcome of childhood minimal change
16. Lombel RM, Hodson EM, Gipson
nephrotic syndrome: Is genetics involved?
DS; Kidney Disease: Improving Global
Pediatr Nephrol 2005; 20:1073-80.
Outcomes. Treatment of steroid-resistant
6. Anochie I, Eke F, Okpere A. nephrotic syndrome in children: new
Childhood nephrotic syndrome: change in guidelines from KDIGO. Pediatr Nephrol
pattern and response to steroids. J Natl Med 2013; 28(3):409-14.
Assoc 2006; 98(12):1977-81.
17. Dragovic D, Rosenstock JL, Wahl SJ,
7. Mekahli D, Liutkus A, Ranchin B, Yu Panagopoulos G, DeVita MV, Michelis MF.
A, Bessenay L, Girardin E et al. Long-term Increasing incidence of focal segmental
outcome of idiopathic steroid-resistant glomerulosclerosis and an examination of
nephrotic syndrome: a multicenter study. demographic patterns. Clin Nephrol 2005;
Pediatr Nephrol 2009; 24(8):1525-32. 63(1):1-7.
8. Nash MA, Edelmann CM, Bernstein J, 18. Kari JA, Halawani M, Mokhtar G,
Barnett HL. The nephrotic syndrome. In: Jalalah SM, Anshasi W. Pattern of steroid
Edelmann CM (ed). Pediatric Kidney Disease, resistant nephrotic syndrome in
2 th ed, Vol. II, Boston: Little Brown and CO, children living in the kingdom of Saudi
1992. p.1247. Arabia: a single center study. Saudi J Kidney
Dis Transpl 2009; 20(5):854-57.
9. Davutoglu M, Ece A, Bilici M, Dagli
A. Steroid responsiveness of children with 19. Banaszak B, Banaszak P. The
idiopathic nephrotic syndrome in southeastern increasing incidence of initial steroid
region of Turkey. Ren Fail 2007; 29(7):855- resistance in childhood nephrotic syndrome.
59. Pediatr Nephrol 2012; 27(6):927-32.
10. Berdeli A, Mir S, Yavascan O, 20. Hinkes B, Vlangos C, Heeringa S,
Serdaroglu E, Bak M, Aksu N et al. NPHS2 Mucha B, Gbadegesin R, Liu J et al; APN
(podocin) mutations in Turkish children with Study Group. Specific podocin mutations
idiopathic nephrotic syndrome. Pediatr correlate with age of onset in steroid-resistant
Nephrol 2007; 22(12):2031-40. nephrotic syndrome. J Am Soc Nephrol 2008;
19(2):365-71.
11. Mir S, Yavascan O, Berdeli A, Sozeri
B. TRPC6 gene variants in Turkish children 21. Benoit G, Machuca E, Antignac C.
with steroid-resistant nephrotic syndrome. Hereditary nephrotic syndrome: a systematic
Nephrol Dial Transplant 2012; 27(1):205-9. approach for genetic testing and a review of
associated podocyte gene mutations. Pediatr
12. Büscher AK, Kranz B, Büscher R,
Nephrol 2010; 25(9):1621-3.
Hildebrandt F, Dworniczak B, Pennekamp P et
al. Immunosuppression and renal outcome in 22. Santín S, Bullich G, Tazón-Vega B,
congenital and pediatric steroid-resistant García-Maset R, Giménez I, Silva I et el.
nephrotic syndrome. Clin J Am Soc Nephrol Clinical utility of genetic testing in children
2010; 5(11):2075-84. and adults with steroid-resistant nephrotic
syndrome. Clin J Am Soc Nephrol 2011;
13. Niaudet P. Genetic forms of nephrotic
6(5):1139-48.
syndrome. Pediatr Nephrol 2004; 19(12):1313-
18. 23. Niaudet P. Steroid-resistant idiopatic
nephrotic syndrome in children. 2012
14. Caridi G, Trivelli A, Sanna-Cherchi
www.UpToDate.com
S, Perfumo F, Ghiggeri GM. Familial forms of
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1240
Renda et al.
24. Trautmann A, Bodria M, Ozaltin F, 31. Ruf RG, Lichtenberger A, Karle SM,
Gheisari A, Melk A, Azocar M, et al; PodoNet Haas JP, Anacleto FE, Schultheiss M, et al;
Consortium. Spectrum of steroid-resistant and Arbeitsgemeinschaft Für Pädiatrische
congenital nephrotic syndrome in children: the Nephrologie Study Group. Patients with
PodoNet registry cohort. Clin J Am Soc mutations in NPHS2 (podocin) do not respond
Nephrol 2015; 10(4):592-600. to standard steroid treatment of nephrotic
syndrome. J Am Soc Nephrol 2004; 15(3):722-
25. Hakan N, Aydin M, Erdogan O,
32.
Cavusoglu YH, Aycan Z, Ozaltin F, et al. A
novel WT1 gene mutation in a newborn infant 32. Callís L, Vila A, Carrera M, Nieto J.
diagnosed with Denys-Drash syndrome. Long-term effects of cyclosporine A in Alport's
Genet. Couns 2012; 23(2):255-61. syndrome. Kidney Int 1999; 55(3):1051-56.
26. Aydin B, Ipek MS, Ozaltin F, 33. Mahmoud I, Basuni F, Sabry A, El-
Zenciroğlu A, Dilli D, Beken S, et al. A novel Husseini A, Hassan N, Ahmad NS, et al.
mutation of laminin β-2 gene in Pierson Single-centre experience with cyclosporin in
syndrome manifested with nephrotic syndrome 106 children with idiopathic focal segmental
in the early neonatal period. Genet Couns glomerulosclerosis. Nephrol Dial Transplant
2013; 24(2):141-47. 2005; 20(4):735-42.
27. Mendoza SA, Reznik VM, Griswold 34. de Mello VR, Rodrigues MT,
WR, Krensky AM, Yorgin PD, Tune BM. Mastrocinque TH, Martins SP, de Andrade OV,
Treatment of steroid-resistant focal segmental Guidoni EB et al. Mycophenolate mofetil in
glomerulosclerosis with pulse children with steroid/cyclophosphamide-
methylprednisolone and alkylating agents. resistant nephrotic syndrome. Pediatr Nephrol
Pediatr Nephrol 1990; 4(4):303-7. 2010; 25(3):453-60.
28. Hodson EM, Willis NS, Craig JC. 35. Gipson DS, Trachtman H, Kaskel FJ,
Interventions for idiopathic steroid-resistant Greene TH, Radeva MK et al. Clinical trial of
nephrotic syndrome in children. Cochrane focal segmental glomerulosclerosis in children
Database Syst Rev 2010;(11):CD003594. and young adults. Kidney İnt 2011; 80:868-78.
29. Steroid-resistant nephrotic syndrome 36. Otukesh H, Otukesh S, Mojtahedzadeh
in children. Kidney International Supplements M, Hoseini R, Fereshtehnejad SM, Riahi Fard
2012; 2:172-6. A, et al. Management and outcome of steroid-
resistant nephrotic syndrome in children. Iran J
30. Faul C, Donnelly M, Merscher-Gomez
Kidney Dis 2009; 3(4):210-7.
S, Chang YH, Franz S, Delfgaauw J et al. The
actin cytoskeleton of kidney podocytes is a 37. Cattran DC, Rao P. Long-term
direct target of the antiproteinuric effect of outcome in children and adults with classic
cyclosporine A. Nat Med 2008; 14(9):931-8. focal segmental glomerulosclerosis. Am J
Kidney Dis 1998; 32(1):72-9.
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1241
http:// ijp.mums.ac.ir
Original Article (Pages: 1233-1242)
Table 5: The response to the first immunosuppressive treatment and final status of the patients at the last follow-up
n. 1st ISD 2nd ISD 3rd ISD Response to first treatment Relapse frequency Relapse treatment Final status Final treatment Renal biopsy Mutation
1.
Mendoza CR 1 Pulse MPZ CRF CAPD FSGS -
CNI - MMF Renal tx
2. CsA- NR MMF CR CR FSGS NPHS2
Mendoza- NR polymorphism
3. Mendoza- PR CsA CR CR FSGS -
4. Mendoza- NR CsA- NR MMF NR CRF CAPD FSGS -
Ex.
5. CsA- NR 6 months pulse MPZ CR CR FSGS -
6. CsA- NR Mendoza- NR CsA NR CRF Supportivetreatment FSGS -
7. NPHS2
CsA- NR Mendoza- NR CsA PR PR CsA FSGS polymorphism
8. CsA- NR CsA PR PR CsA FSGS -
9. CsA- NR CsA- NR MMF NR NS Supportivetreatment MCD NPHS2
homozygote
10. Mesangial -
CsA- NR CsA CR 1 Pulse MPZ CR Proliferation
11. CsA- NR CsA- NR MMF PR PR MMF FSGS -
12. CsA- NR CsA CR 2 Pulse MPZ PR MMF FSGS NPHS2
CNI - MMF Polymorphism
13. Mesangial
CsA CR CR Proliferation
14. CR 1 Pulse MPZ CR Mesangial NPHS2
CsA proliferation polymorphism
15. CR Pulse MPZ PR MMF FSGS
CsA 1 MMF -
16. CsA- NR MMF NR NS Supportivetreatment MCD -
17. CR 1 Pulse MPZ CR MMF Mesangial -
CsA MMF proliferation
18. Pulse MPZ
CsA CR 1 CNI - MMF NS Supportivetreatment FSGS
19. MMF NR CRF Supportivetreatment Mesangial NPHS2
CsA- NR proliferation homozygote
20. CsA PR PR CsA FSGS -
21. CsA NR CRF Supportivetreatment FSGS -
22. CsA NR NS Supportivetreatment Mesangial -
proliferation
23. CsA CR 3 Pulse MPZ CR FSGS -
CNI
24. CsA- NR MMF NR CRF Supportivetreatment Mesangial NPHS2
proliferation polymorphism
25. CsA CR 1 Pulse MPZ PR CsA FSGS -
CNI
26 CsA- NR MMF NR CRF Supportivetreatment FSGS -
27. CsA- PR MMF CR CR FSGS -
Int J Pediatr, Vol.4, N.1, Serial No.25, Jan 2016 1242
You might also like
- Renal Pathology Lectures - PPT SeriesDocument267 pagesRenal Pathology Lectures - PPT SeriesMarc Imhotep Cray, M.D.100% (12)
- Pathology PDFDocument28 pagesPathology PDFRoman PanditNo ratings yet
- DUTIES OF NURSING PERSONALS IN HOSPITAL WordDocument25 pagesDUTIES OF NURSING PERSONALS IN HOSPITAL Wordpooja singh100% (1)
- ACP Board Review Nephrology 20052ndDocument35 pagesACP Board Review Nephrology 20052nddoctormido2010100% (1)
- Urinary and Renal Worksheet Answer KeyDocument6 pagesUrinary and Renal Worksheet Answer KeyF6imNo ratings yet
- Glomerulopatias Secundarias PDFDocument80 pagesGlomerulopatias Secundarias PDFOscar Morales100% (1)
- (Mebooksfree Net) Chr&kid&dis&dia&tre&yan&he&1st PDFDocument250 pages(Mebooksfree Net) Chr&kid&dis&dia&tre&yan&he&1st PDFmainoNo ratings yet
- CKD - For Concept MappingDocument7 pagesCKD - For Concept MappingKennette Lim0% (1)
- Pathophysiology CKDDocument3 pagesPathophysiology CKDCyndi Jane Bandin CruzataNo ratings yet
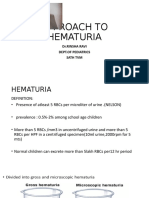
- Approach To Hematuria: DR - Rinsha Ravi Dept - of Pediatrics Sath TVMDocument40 pagesApproach To Hematuria: DR - Rinsha Ravi Dept - of Pediatrics Sath TVMAnoop ThoombayilNo ratings yet
- Gene Therapy in Neurological DisordersFrom EverandGene Therapy in Neurological DisordersMingjie LiNo ratings yet
- CGHS Chennai Hco March 21Document12 pagesCGHS Chennai Hco March 21Harini MNo ratings yet
- Childhood Idiopathic Nephrotic Syndrome in Turkey: Original ArticleDocument4 pagesChildhood Idiopathic Nephrotic Syndrome in Turkey: Original ArticleDrago BakovicNo ratings yet
- The Importance of Genetic Testing in Adolescent-Onset Steroid-Resistant Nephrotic Syndrome - Case ReportDocument9 pagesThe Importance of Genetic Testing in Adolescent-Onset Steroid-Resistant Nephrotic Syndrome - Case ReportAlrista MawarNo ratings yet
- Molecular Genetic Analysis of Steroid Resistant NephroticDocument8 pagesMolecular Genetic Analysis of Steroid Resistant NephroticBeatri AyuzaNo ratings yet
- Efficacy of Higher-Dose Levamisole in Maintaining Remission in Steroid-Dependant Nephrotic SyndromeDocument6 pagesEfficacy of Higher-Dose Levamisole in Maintaining Remission in Steroid-Dependant Nephrotic Syndromechandra maslikhaNo ratings yet
- Iran J Kidney Dis 2020 14 6 478 481 EngDocument4 pagesIran J Kidney Dis 2020 14 6 478 481 EngFachri PopopNo ratings yet
- 2018 Tto Del SN CorticoresistenteDocument11 pages2018 Tto Del SN CorticoresistenteJeff Daniel Landauro PanayNo ratings yet
- Epi 12739Document8 pagesEpi 12739Juan Diego De La Cruz MiñanoNo ratings yet
- Treatment-Associated Side Effects in Patients With Steroid-Dependent Nephrotic SyndromeDocument6 pagesTreatment-Associated Side Effects in Patients With Steroid-Dependent Nephrotic SyndromeIndah SolehaNo ratings yet
- Short-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyDocument12 pagesShort-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyTJPRC PublicationsNo ratings yet
- Poster: Effect of Mendoza Protocol Therapy in Children With Steroid-Resistant Nephrotic Syndrome. A Case Series in DR - Kariadi Hospital SemarangDocument1 pagePoster: Effect of Mendoza Protocol Therapy in Children With Steroid-Resistant Nephrotic Syndrome. A Case Series in DR - Kariadi Hospital SemarangSondang Herikson PanjaitanNo ratings yet
- Dose, Plasma Concentrations, (Sirdaludo) : Correlations Between and Action of TizanidineDocument6 pagesDose, Plasma Concentrations, (Sirdaludo) : Correlations Between and Action of TizanidineApriani MargastutieNo ratings yet
- Medip, IJCP-2856 ODocument6 pagesMedip, IJCP-2856 OMarcelita DuwiriNo ratings yet
- Jurnal ANCADocument22 pagesJurnal ANCAMuthia FaurinNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- A Single-Centre Retrospective Study of The Safety and Ef Ficacy of Mycophenolate Mofetil in Children and Adolescents With Nephrotic SyndromeDocument6 pagesA Single-Centre Retrospective Study of The Safety and Ef Ficacy of Mycophenolate Mofetil in Children and Adolescents With Nephrotic SyndromeBakul TapeNo ratings yet
- Levamisole Therapy in Children With Frequently Relapsing and Steroid-Dependent Nephrotic Syndrome - A Single-Center ExperienceDocument5 pagesLevamisole Therapy in Children With Frequently Relapsing and Steroid-Dependent Nephrotic Syndrome - A Single-Center ExperienceGading AuroraNo ratings yet
- Mycophenolate MofetilDocument3 pagesMycophenolate MofetilRAMESH HAOLADAR100% (2)
- Sindrome NefroticoDocument8 pagesSindrome NefroticoRudy Espejo del ArcaNo ratings yet
- Long-Term Clinical Outcome of Fetal Cell Transplantation For Parkinson Disease Two Case ReportsDocument5 pagesLong-Term Clinical Outcome of Fetal Cell Transplantation For Parkinson Disease Two Case Reportsjust for download matterNo ratings yet
- Nephrotic Syndrome Guidelines 2019Document14 pagesNephrotic Syndrome Guidelines 2019Sara Ilyas KhanNo ratings yet
- A Prospective Cohort Study of Rituximab in The Treatment of Refractory Nephrotic SyndromeDocument10 pagesA Prospective Cohort Study of Rituximab in The Treatment of Refractory Nephrotic SyndromeMuh Deriyatmiko BastamanNo ratings yet
- AKI Child W NS 2018Document4 pagesAKI Child W NS 2018Indah Nur LathifahNo ratings yet
- Ijcp-5459 oDocument5 pagesIjcp-5459 oDrkaleembrimsNo ratings yet
- CyclophospamideDocument4 pagesCyclophospamidemrkoyoNo ratings yet
- Final NS Guidelines August 26 2019-1Document17 pagesFinal NS Guidelines August 26 2019-1Nido MalghaniNo ratings yet
- 2018 Article 31727Document11 pages2018 Article 31727Jackson HakimNo ratings yet
- Ejhpharm 2017 001285.fullDocument1 pageEjhpharm 2017 001285.fullTauqeer Hussain MallhiNo ratings yet
- PIIS008525381546747XDocument15 pagesPIIS008525381546747XBintiNo ratings yet
- Out (2) .TranslateDocument4 pagesOut (2) .TranslateElang SudewaNo ratings yet
- Tau-Targeting Antisense Oligonucleotide Mapt in Mild Alzheimer's Disease: A Phase 1b, Randomized, Placebo-Controlled TrialDocument20 pagesTau-Targeting Antisense Oligonucleotide Mapt in Mild Alzheimer's Disease: A Phase 1b, Randomized, Placebo-Controlled TrialSiddharth NarsipurNo ratings yet
- 1899 FullDocument6 pages1899 Fullmelanita_99No ratings yet
- Intravenous Cyclophosphamide in Steroid-Resistant Nephrotic SyndromeDocument6 pagesIntravenous Cyclophosphamide in Steroid-Resistant Nephrotic SyndromeRicho WijayaNo ratings yet
- Immunosuppressive Treatment in Children With Iga Nephropathy and The Clinical Value of Podocytopathic FeaturesDocument10 pagesImmunosuppressive Treatment in Children With Iga Nephropathy and The Clinical Value of Podocytopathic FeaturesFrida RasyidNo ratings yet
- Second-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceDocument10 pagesSecond-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceSitaNo ratings yet
- Rogers 1993Document4 pagesRogers 1993Nadia SaiNo ratings yet
- Single-Nucleotide Polymorphism of The UMOD Promoter Is Associated With The Outcome of Chronic Kidney Disease PatientsDocument5 pagesSingle-Nucleotide Polymorphism of The UMOD Promoter Is Associated With The Outcome of Chronic Kidney Disease Patientssylvi293No ratings yet
- RCT ArticleDocument8 pagesRCT ArticleelpisNo ratings yet
- Jdi 13061 PDFDocument6 pagesJdi 13061 PDFOlga BabiiNo ratings yet
- A Randomized Controlled Clinical Trial To Compare The Safety and Effi Cacy of Edaravone in Acute Ischemic StrokeDocument5 pagesA Randomized Controlled Clinical Trial To Compare The Safety and Effi Cacy of Edaravone in Acute Ischemic StrokeWahyuni SetiawatiNo ratings yet
- Lec - S32 Injuria RenalDocument8 pagesLec - S32 Injuria RenalEvelyn EstradaNo ratings yet
- Ten Common Mistakes in The Management of Lupus Nephritis. 2014Document10 pagesTen Common Mistakes in The Management of Lupus Nephritis. 2014Alejandro Rivera IbarraNo ratings yet
- Primary Nephrotic Syndrome NewDocument15 pagesPrimary Nephrotic Syndrome Newpj rakNo ratings yet
- Cilia 2018Document1 pageCilia 2018Anna Beatriz Silva EspindolaNo ratings yet
- On Research ArticleDocument10 pagesOn Research ArticleTanya MesheryakovNo ratings yet
- Use of A LowDocument8 pagesUse of A Lowirma suwandi sadikinNo ratings yet
- Calin 2004 PDFDocument8 pagesCalin 2004 PDFRafaela Queiroz MascarenhasNo ratings yet
- Neurourology and Urodynamics - 2022 - Martin - Is Sacral Neuromodulation Effective in Patients With Parkinson S Disease ADocument7 pagesNeurourology and Urodynamics - 2022 - Martin - Is Sacral Neuromodulation Effective in Patients With Parkinson S Disease AElkin JNo ratings yet
- The Efficacy of Propofol and Midazolam in Treatment of Refractory Status Epilepticus in ChildrenDocument6 pagesThe Efficacy of Propofol and Midazolam in Treatment of Refractory Status Epilepticus in ChildrenReci MaulitaNo ratings yet
- Artigo 3Document17 pagesArtigo 3Raquel BastosNo ratings yet
- Remdesivir in Patients With Acute or Chronic Kidney Disease and COVID-19Document3 pagesRemdesivir in Patients With Acute or Chronic Kidney Disease and COVID-19lucianarottyNo ratings yet
- Gene Therapy For Spinal Muscular Atrophy: The Qatari ExperienceDocument5 pagesGene Therapy For Spinal Muscular Atrophy: The Qatari ExperienceCarlos Meza HernandezNo ratings yet
- 1Document11 pages1Valentina Cortes MoralesNo ratings yet
- 8 Sivakumar Et AlDocument7 pages8 Sivakumar Et Alkhalid alharbiNo ratings yet
- Effects of An Antithrombin Drug in Patients With Subacute Exacerbations of Binswanger DiseaseDocument4 pagesEffects of An Antithrombin Drug in Patients With Subacute Exacerbations of Binswanger DiseaseFortune FireNo ratings yet
- Evaluation Dose of AntibioticDocument3 pagesEvaluation Dose of AntibioticrachmafitriNo ratings yet
- MagnascoDocument8 pagesMagnascoMeliana SulistioNo ratings yet
- 101-Article For Submission-298-1-10-20210207Document21 pages101-Article For Submission-298-1-10-20210207Umer RazaqNo ratings yet
- Risperidone Induced Seizures After Cessation of ClozapineDocument1 pageRisperidone Induced Seizures After Cessation of ClozapineAttaufiq IrawanNo ratings yet
- Bartels 2014Document6 pagesBartels 2014docadax848No ratings yet
- Archnutrients 2291092 SupplementaryDocument3 pagesArchnutrients 2291092 SupplementaryAnca AdamNo ratings yet
- 2 PH Metrie Esofagite GerdDocument6 pages2 PH Metrie Esofagite GerdAnca AdamNo ratings yet
- Intrauterine Growth RestrictionDocument13 pagesIntrauterine Growth RestrictionAnca AdamNo ratings yet
- IUGRDocument6 pagesIUGRAnca AdamNo ratings yet
- Spitalul Clinic de Urgenta Pentru Copii SF Maria IasiDocument38 pagesSpitalul Clinic de Urgenta Pentru Copii SF Maria IasiAnca AdamNo ratings yet
- Adult Sequelae of Intrauterine Growth RestrictionDocument6 pagesAdult Sequelae of Intrauterine Growth RestrictionAnca AdamNo ratings yet
- Neonatal Hyperbilirubinaemia 5.0Document25 pagesNeonatal Hyperbilirubinaemia 5.0Anca AdamNo ratings yet
- Renovascular Hypertension 42 Cases AnalysisDocument33 pagesRenovascular Hypertension 42 Cases AnalysisAnca AdamNo ratings yet
- Schema Reechilibrare HeDocument2 pagesSchema Reechilibrare HeAnca AdamNo ratings yet
- PK Hofmann ADocument20 pagesPK Hofmann AAnca AdamNo ratings yet
- Nations' Kidney Community Announces Major Initiative To Develop Quality Metrics To Assess Dialysis Provider PerformanceDocument3 pagesNations' Kidney Community Announces Major Initiative To Develop Quality Metrics To Assess Dialysis Provider PerformancePR.comNo ratings yet
- Dialysis and Disasters PresentationDocument21 pagesDialysis and Disasters Presentationapi-24755251No ratings yet
- Automated Peritoneal Dialysis: Clinical Prescription and TechnologyDocument8 pagesAutomated Peritoneal Dialysis: Clinical Prescription and Technologyamalia puspita dewiNo ratings yet
- Evidence Based Approach To The Patient With Hypertensive Disorders - Gülçin Kantarcı - NEPHROLOGYDocument2 pagesEvidence Based Approach To The Patient With Hypertensive Disorders - Gülçin Kantarcı - NEPHROLOGYGÖKSU SAYGILINo ratings yet
- Cue and Clue Problem List Idx PDX PTX Pmo PedDocument5 pagesCue and Clue Problem List Idx PDX PTX Pmo PedEmma FitrianaNo ratings yet
- 2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)Document7 pages2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)elleinas100% (1)
- National Kidney Foundation Position PaperDocument4 pagesNational Kidney Foundation Position PaperGenesis HendraNo ratings yet
- Glomerular Disease: Acute Nephritic Syndrome Nephrotic Syndrome Chronic GlomerulonephritisDocument18 pagesGlomerular Disease: Acute Nephritic Syndrome Nephrotic Syndrome Chronic GlomerulonephritisironNo ratings yet
- Lawrence Owino Okongo Paediatric Rheumatologist: List of Privileges Allergy/Immunology DisordersDocument5 pagesLawrence Owino Okongo Paediatric Rheumatologist: List of Privileges Allergy/Immunology DisordersMARTINNo ratings yet
- Daftar PustakaDocument3 pagesDaftar Pustakagayuh rizkyNo ratings yet
- Chronic Kidney Disease - ClinicalKeyDocument53 pagesChronic Kidney Disease - ClinicalKeyMariel Patricia CapunoNo ratings yet
- Module 1: Acute Care Hemodialysis Orientation Manual and Assessment ToolsDocument33 pagesModule 1: Acute Care Hemodialysis Orientation Manual and Assessment Toolsmarlon armamentoNo ratings yet
- Data Dictionary For Quarterly Dialysis Facility Compare: Release Date: October 2019Document34 pagesData Dictionary For Quarterly Dialysis Facility Compare: Release Date: October 2019Yasmin RassoulNo ratings yet
- DialysisDocument6 pagesDialysisPrincess Joy Torrijas Factora0% (1)
- EmphospitalDocument47 pagesEmphospitaljayakrishna173157No ratings yet
- Pathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaDocument7 pagesPathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaIJAR JOURNALNo ratings yet
- CGHS Chennai Empanelled Hospital List As On Apr 23Document7 pagesCGHS Chennai Empanelled Hospital List As On Apr 23Banumathy RajappaNo ratings yet
- Semio Renal DiaposDocument143 pagesSemio Renal DiaposMaria jose Pesantez abadNo ratings yet
- Nephrology Case StudyDocument8 pagesNephrology Case StudyAmina Tariq100% (1)