Professional Documents
Culture Documents
Beezhold Sawyer Lynch 2020 ENERGYEXPENDITUREINASYMESAMPUTEETRIATHLETE1
Uploaded by
Raissa NoorOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Beezhold Sawyer Lynch 2020 ENERGYEXPENDITUREINASYMESAMPUTEETRIATHLETE1
Uploaded by
Raissa NoorCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/345271285
ENERGY EXPENDITURE IN A SYME'S AMPUTEE TRIATHLETE
Article · August 2020
CITATIONS READS
0 38
3 authors, including:
Brandon J Sawyer Heidi Lynch
Point Loma Nazarene University Point Loma Nazarene University
48 PUBLICATIONS 466 CITATIONS 12 PUBLICATIONS 89 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Differences in strength, power, body composition, diet, and physical activity between females following plant-based or omnivorous diets View project
All content following this page was uploaded by Heidi Lynch on 04 November 2020.
The user has requested enhancement of the downloaded file.
Journal of Kinesiology and Wellness - Student Edition
A Publication of the Western Society for Kinesiology and Wellness
Volume 9, Number 2, Pages 47-55, 2020
ISSN# 2332-4503
ENERGY EXPENDITURE IN A SYME’S AMPUTEE TRIATHLETE
Erin J. Beezhold*, Brandon J. Sawyer, and Heidi M. Lynch*
Department of Kinesiology
Point Loma Nazarene University
Submitted May 2020; Accepted in final form August 2020
Beezhold EJ, et. al. Energy expenditure prediction equations developed for able-bodied populations may be
inaccurate for para-athletes, a population characterized by different types of impairments. Sufficient data do not
exist currently to generate or validate energy expenditure predictive equations for para-athletes to establish dietary
recommendations to cover the demands of sport. The purpose of this observational study was to assess energy
expenditure and substrate usage from a trained para-athlete at rest and while performing the athlete’s specific
mode of exercise. One para-athlete recruited from the Challenged Athletes Foundation (female; age 32)
participated in the study. The participant was a left leg Syme’s amputee triathlete. Resting metabolic rate was
measured for the triathlete. Energy expenditure was also measured at moderate (64-76% of age-predicted HRmax)
and vigorous intensity exercise (77-95% of age-predicted HRmax) on a stationary cycle ergometer on a separate
day. The triathlete’s energy expenditure during exercise was higher than that predicted by the metabolic equivalent
of task (MET) matched by exercise type at a moderate (measured: 7.0 kcal/min, predicted: 5.0 kcal/min) and
vigorous intensity (measured: 9.3 kcal/min, predicted: 7.0 kcal/min). The Revised Harris-Benedict and the Mifflin-
St Jeor equations underestimated resting metabolic rate in the triathlete (measured: 2,194 kcal/day, predicted:
1,348 ± 39 kcal/day). This study indicates that equations developed for able-bodied populations underestimate
energy expenditure in a Syme’s amputee when compared to the measured energy expenditure values assessed by
indirect calorimetry at rest and during a workout on both a stationary cycle ergometer and while running on the
track.
Key Words: para-athlete, able-bodied, energy expenditure, resting metabolic rate
INTRODUCTION leg strength difference are examples of impairments
that influence the rate and quantity of substrate
Energy expenditure (EE) describes the rate
utilization (Goosey-Tolfrey et al., 2014). Thereby, it
and quantity of substrate utilization in the body for
excludes this population from the accurate usage of
energy (Haugen et al., 2007; Levine, 2005). Para-
standard EE prediction equations developed for AB
athletes are a population characterized by different
athletes (Farkas et al., 2019; Price, 2010).
types of impairments. Depending on the type and
EE in the clinical and field setting is well
severity, the disability can result in a change in EE
understood for AB athletes (Levine, 2005; Hall et al.,
(either increased or decreased) when compared to
2004). However, data on EE in physically impaired
able-bodied (AB) athletes (Gjovaag et al., 2017;
athletes is sparse (Goosey-Tolfrey & Leicht, 2013).
Schmalz et al., 2002; Ward & Merers, 1995). Standard
This is because there are several limitations when
EE prediction equations that were developed for AB
working with a population characterized by a wide
populations are inaccurate for para-athletes
variety of types and degrees of impairment (Goosey-
(Czerniecki et al., 2017; Farkas et al., 2019).
Tolfrey et al., 2014). For example, not all protocols
Decreased muscle power, a limb deficiency or loss, or
designed for an AB population are transferable to
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 47
Beezhold et. al., Energy Expenditure of Syme’s Amputee
physically impaired athletes and some testing account for the diverse range of degrees and types of
equipment cannot accommodate prosthesis or impairments that exist in para-athletes (Goosey-
wheelchairs (Goosey-Tolfrey et al., 2016). Tolfrey at al.,2013; Price, 2010). However, individual
Opportunities are growing for physically EE data is important for each para-athlete in order for
impaired individuals to participate in exercise and each athlete to understand his or her energy needs
sport (Goosey-Tolfrey et al., 2014). Consequently, during training for optimal fueling and weight
efforts are being made to better understand EE at rest management (Gjovaag et al., 2017). Over time, as
and during exercise to enhance training and more para-athletes’ EE is documented, it may
performance through nutrition and body-weight become possible to develop population-specific EE
regulation in the expanding para-athlete population prediction equations.
(Edwards et al., 2018). It is valuable to have an Therefore, the purpose of this observational
estimate of energy requirement to decide the study was to assess EE and substrate usage from a
sufficiency of energy intake for sport demands trained para-athlete at rest and during a training
(Goosey-Tolfrey et al., 2016). This can help prevent session. This information can help dietitians to
the likelihood of low energy availability and offers estimate appropriate energy intake of a Syme’s
direction in prescribing diet and training to support amputee to cover energy costs of the sport. This can
changes in physique and performance (Blauwet et al., provide direction for changes in diet and training to
2017; Goosey-Tolfrey et al., 2014). While there are regulate body composition and enhance training and
predictive equations for AB people to estimate performance. This study also serves as a foundation
energy expenditure, rate of EE during exercise is less upon which future research may build. Data from
studied for para-athletes (Czerniecki et al., 2017). The individuals should be matched by type and degree of
majority of research looking at individuals specifically impairment and mode of exercise to assist in the
with amputation takes place in a clinical setting with generation of population-specific EE prediction
non-athletes (Ward & Merers, 1995). Such studies equations.
lack ecological validity, an important factor in the
practicality of data utilization (Czerniecki et al., 2017). METHODS
Athletes with a lower extremity amputation Participants
tend to have a higher respiratory exchange ratio
(RER), rating of perceived exertion (RPE), oxygen Criteria for inclusion were: reporting “no” to
uptake (VO2), and heart rate (HR) compared to AB all questions on the Physical Activity Readiness
athletes at a given submaximal intensity (Gjovaag et Questionnaire (PAR-Q), being at least 18 years of age,
al., 2017). The higher energy cost is likely because an athlete with a physical disability, and currently
movement with prosthetics can be inefficient training for a competitive event or race at a
(Goosey-Tolfrey et al., 2014). The location of the recreational or elite level. The study was approved by
amputation also can determine EE because greater an Institutional Review Board and athletes provided
tissue loss results in higher levels of energy expended written informed consent. One healthy participant
during movement, but lower RMR levels in was recruited from Challenged Athletes Foundation
comparison to an AB individual (Schmalz et al., 2002). (Table 1): a recreational triathlete with a left leg
Despite emerging efforts in understanding EE Syme’s amputation (removal of the foot at the ankle
characteristics in athletes with amputation, currently joint). The triathlete was training for a marathon 8
there are insufficient data to generate or validate EE months from the testing date, building mileage
predictive equations for these athletes in order to through an average of 6 hours of self-reported
establish dietary recommendations for appropriate training per week, excluding resistance training. She
energy intake or sport performance enhancement had no history of smoking and reported no usage of
(Blauwet et al., 2017; Joaguim et al., 2018). The wide medications affecting HR during rest and exercise.
variety of impairment types precludes this possibility
at present because most studies available involve
small subject numbers and do not adequately
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 48
Beezhold et. al., Energy Expenditure of Syme’s Amputee
Procedures and impairment history for the participant were
documented. Since the participant was able to
The triathlete was asked to participate in
assume a standing position, a Seca 206 wall-mounted
three different testing days. For each visit, the
stadiometer (Seca, Birmingham, United Kingdom)
triathlete was instructed to refrain from alcohol and
was used to measure height. A Cosmed integrated
vigorous exercise 24 hours prior to testing and from
digital scale (Cosmed, Concord, CA, USA) was used to
caffeine the day of testing. The tests took place one
measure weight, subtracting prosthetic weight from
week apart in the exercise science laboratory and on
total body mass. The triathlete’s everyday prosthetic
the track of a local university.
used for cycling was a Seattle Kinetic Light (0.50 kg)
Table 1 and her running prosthetic was an Ossur Cheetah foot
(0.51 kg). The participant was then fitted with the
Athlete Demographics and Energy Expenditure at Rest Cosmed K4b2 portable breath-by-breath gas
exchange analyzer. The K4b2 was calibrated using
Description Athlete manufacturer guidelines before each test. A Polar
Impairment type Syme’s amputation (L) Unisex Adult Heart Rate Sensor and Pro Chest Strap
(Polar, NY, USA) recorded heart rate (HR). Time was
Sport triathlon
tracked using a digital Pro Survivor Stopwatch
Sex female (Accusplit, Livermore, CA, USA). RMR testing took 45
Age (yr) 32 minutes while the athlete rested in a supine position.
The first 20-30 minutes allowed the subject to reach
Height (cm) 160
a steady-state while resting comfortably. Gas
Weight (kg), excluding 63 exchange and ventilatory data were collected in a
prostheses breath-by-breath fashion and then 30-second
averages were used for analysis. Steady-state oxygen
Current training (excluding 6 uptake was defined as 10 minutes during which VO2
resistance training) and ventilation did not vary by >10%. The last five
minutes of those 10 minutes of steady state were
(hours/week)
used for RMR assessment. The following two
Measured resting metabolic 2,194 equations commonly used to predict RMR in an AB
rate (kcal/day) population (Frankenfield et al., 2005; Mifflin et al.,
1990) were used to predict the RMR of the triathlete
Resting VO2 ml/kg/min 5.0
and to compare with their directly measured RMR:
RER 0.80
Kcal/min 1.5 Revised Harris-Benedict equation: 447.6 + [9.25 x
weight (kg)] + [3.10 x height (cm)] – [4.33 x age (y)]
Kcal/kg/min 0.02
% of energy used from 67 Mifflin-St Jeor formula: [10 x weight (kg)] + [6.25 x
height (cm)] – [5 x age (y)] – 161
fats at rest
% of energy used from 33 On visit two, the triathlete was asked to
carbohydrates at rest prepare nutritionally and warm up for a workout as
normal to mimic a regular practice. The test was
Resting HR 43 bpm
conducted using a stationary cycle ergometer
(Monark L7, Varberg, Sweden) to match the
Note: Metabolic values are averages taken from the last
5-minutes of the resting metabolic test. triathlete’s primary mode of exercise. Once fitted
with the K4b2, the triathlete performed in a HR and
On visit one, the triathlete was instructed to RPE range (Borg, 1982) according to the American
fast for at least 8 hours prior. Sex, age, height, weight, College of Sports Medicine (ACSM) (Garber et al.,
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 49
Beezhold et. al., Energy Expenditure of Syme’s Amputee
2011) at a moderate (64-76% of HRmax and RPE score Kcal/kg/min = kcal/hour ÷ weight in kilograms ÷ 60
between 12-13) and vigorous intensity (77-95% of minutes
HRmax and RPE score between 14-17) using age-
Statistical Analysis
predicted HRmax (220 – age = HRmax). The exercise
test took approximately 45 minutes. EE data were Descriptive statistics are presented for EE,
continuously collected for five minutes at rest, during VO2, and RER at rest and during exercise for the
a 1-minute self-paced warm-up, during 15 minutes of athlete. As this was a case study (N=1), we are
moderate intensity exercise, during 15 minutes of reporting the descriptive statistics and visually
vigorous intensity exercise, and during a 5-minute comparing measured energy expenditure to that
cool-down at a self-selected pace. RPE was recorded estimated by predictive equations.
every minute, and HR levels were closely monitored
during exercise to keep the triathlete’s HR within the RESULTS
intensity zones by manipulating bike resistance and Group Characteristics
encouraging the triathlete to pedal at a consistent
rate. Data were used from the last two minutes of The triathlete showed a higher measured
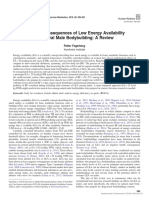
each stage after steady-state was reached to RMR (2,194 kcal/day) compared to that predicted by
calculate EE at the given exercise intensity. RER and the Revised Harris-Benedict equation (1,387
caloric expenditure values (kcal/min) were calculated kcal/day) or the Mifflin-St Jeor formula (1,309
using the following standard metabolic conversion kcal/day) (see Figure 1). The triathlete primarily
equations used in indirect calorimetry: utilized fat (67%) as a substrate for energy in
comparison to carbohydrates (33%) during rest.
RER = Average VCO2/VO2, EE = VO2 x caloric
equivalent Figure 1
A Comparison of Measured and Predicted Resting
On visit three, the triathlete was again asked Energy Expenditure
to prepare nutritionally and to warm up for a workout
as normal to mimic a regular practice. While wearing Measured Mifflin-St Jeor Revised Harris-Benedict
the K4b2 on the track, the triathlete ran a mile warm- 2,500
up, 2x800 m and 1x400 m with a 4-minute recovery 2,000
between repetitions at a tempo pace, described as
kcals per day
“comfortably hard” (Daniels, 2013). The triathlete 1,500
helped decide the workout to mirror an abbreviated
1,000
version of her training. EE data was the average of the
last minute of each 800 m run and the last 30 seconds 500
of the 400 m run.
0
Data from both exercise tests were then Triathlete
compared to the metabolic equivalent of task (MET)
adopted by ACSM to express the rate of energy Resting Energy Expenditure Assessment Methods
expended for a given activity (Ainsworth et al., 2011). Energy Expenditure Tests
Closely matched exercise descriptions with a
corresponding MET value were selected from the Heart rate, RPE, rate of EE, and carbohydrate
2011 Compendium of Physical Activities. Kilocalorie usage increased as intensity increased (see Table 2).
(kcal) values were calculated from METs using the The athlete expended higher amounts of energy than
following equations (Ainsworth et al., 2011): the MET equation predicted at a moderate (7.0
kcal/min vs. 5.0 kcal/min, respectively) and vigorous
Kcal/hour = MET x weight in kilograms x duration in intensity (9.3 kcal/min vs. 7.1 kcal/min, respectively).
hours The METs selected and compared to the exercise test
were described as 51-89 watts (W) on a stationary
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 50
Beezhold et. al., Energy Expenditure of Syme’s Amputee
bike at a light-to-moderate effort (4.8 METs) and 90- triathlete expended more energy during the 2x800 m
100 W at a moderate-to-vigorous effort (6.8 METs) compared to that predicted by the MET equation
(Ainsworth et al. 2011). (13.4 kcal/min average vs. 12.7 kcal/min average,
respectively), but less energy during the 400 m
Table 2 compared to that predicted by the MET equation
(13.7 kcal/min vs. 15.2 kcal/min, respectively). The
Measured Cardiorespiratory Responses and an
METs selected and compared to the field-test paces
Estimate of Energy Expenditure using Metabolic
were described as running at 8 mph or 7.5 min/mile
Equivalents (METs) of a Cycling Workout in a
(11.8 METs), running at 8.6 mph or 7 min/mile (12.3
Triathlete with a Syme’s Amputation
METs), and running at 10 mph or 6 min/mile (14.5
Variable Moderate Vigorous METs) (Ainsworth et al. 2011).
Intensity Intensity
DISCUSSION
(64-76% of (77-95% of
predicted predicted For the triathlete with a Syme’s amputation,
HRmax) HRmax) substrate utilization occurred similar to an AB athlete,
increasing carbohydrate reliance and caloric
VO2 ml/kg/min 23.0 30.1 expenditure with increased intensity (Bergman &
RER 0.8 0.9 Brooks, 1999; Hawley & Leckey, 2015). The triathlete
ate a snack before both tests to prepare for the
Kcal/hour 419 558
workout, leading to the assumption that the
Kcal/min 7.0 9.3 carbohydrates in the snack were used for fuel and
Kcal/kg/min 0.1 0.2 suppressed lipolysis, contributing to the increase in
% of energy used carbohydrate reliance (Hawley & Leckey, 2015). MET
56 35 values under-estimated EE for the triathlete in both
from fats
% of energy used cycling and running, with the exception of the 400 m
from 44 65 run, which over-estimated EE by 1.5 kcal/min.
carbohydrates Measured EE during cycling at a moderate intensity
HR, beats per (7.0 kcal/min) was also higher than EE (4.52 ± 0.55
108 153
minute (bpm) kcal/min) reported in a study looking at cycling
Pace: watts (W), efficiency with a sample of 96 healthy young adults
rotations per 45W, 88 RPM 91W, 87 RPM (18-40 yr.) cycling at 50W (Gaesser et al., 2018). This
minute (RPM)
is consistent with studies that show athletes with
Rating of
amputation have higher energy costs during exercise
perceived 12 16
exertion (RPE)
at a given submaximal intensity (Gjovaag et al., 2017,
Schmalz et al., 2002).
METs kcal/hour 302 428
A lower extremity amputation is
METs kcal/min 5.0 7.1 characterized by the loss of the ankle joint, the
METs kcal/kg/min 0.1 0.1 muscles that control the joint structure, and the
sensory input of the musculature, changing the
Note. Metabolic values are averages taken from the last biomechanics for the cyclist when compared to an AB
two-minutes of each stage. cyclist (Childers, 2009). Cycling with one intact limb
and one prosthetic limb leads to asymmetric work
In-Field Assessment (torque) production (Childers, 2011), which could
The triathlete ran an untimed, self-selected account for a higher EE than an AB cyclist at a given
pace for a warm-up mile, 2x800 m at 7:28 and 7:06 intensity. Future research needs to assess how
min/mile pace, and a 400 m at 6:04 min/mile pace asymmetric torque in amputees affects EE during
with a 4-minute recovery between (see Table 3). The cycling.
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 51
Beezhold et. al., Energy Expenditure of Syme’s Amputee
Amputees also have higher energy costs Czerniecki et al., 2017). Schmalz et al. (2002) found
during walking and running when compared to an AB that the style of prosthesis can affect the EE cost of
person because the use of a prosthetic results in an amputee.
lower energy efficiency (Gjovaag et al., 2018;
Table 3
Measured Cardiorespiratory Responses and an Estimate of Energy Expenditure using Metabolic Equivalents (METs)
of a Track Workout in a Triathlete with a Syme’s Amputation
Measurement Warm-up 1st 800 m 2nd 800 m 400 m
Pace (min/mile) untimed 7:28 7:06 6:04
Average HR, beats per minute (bpm) 137 161 170 175
Exercise domain Moderate Vigorous Vigorous Vigorous
VO2 ml/kg/min 34.0 41.6 42.9 43.1
RER 0.9 1.0 1.2 1.2
Kcal/hour 635 795 818 821
Kcal/min 10.6 13.2 13.6 13.7
Kcal/kg/min 0.2 0.2 0.2 0.2
% of energy used from fat 31 0.0 0.0 0.0
% of energy used from carbohydrates 69 100 100 100
METs kcal/hour N/A 743 775 914
METs kcal/min N/A 12.4 12.9 15.2
METs kcal/kg/min N/A 0.2 0.2 0.2
Note. The values are averages taken from the last 6 minutes of the warm-up mile, the last minute of the 800 m, and the last
30 s of the 400 m.
Blair (2018) made a comparison of EE between a exercise with his or her specific gear is critical because
lower limb amputee using a running-specific an impairment can be more or less of a caloric burden
prosthesis compared with a non-amputee similar in in one mode of exercise versus another. Likewise, the
age, sex, and activity level. Results showed that the type of sport equipment used, such as type of
amputee, while using that specific running prosthesis, prosthetic, influences movement efficiency which can
did not expend more energy than the matched impact energy cost. We would expect to see the
control or the metabolic calculation. The triathlete triathlete with the Syme’s amputation expend higher
with a Syme’s amputation who participated in the amounts of energy while running when compared to
current study ran wearing an Ossur Cheetah foot, the AB person accomplishing the same amount of
designed to be lightweight and for gait efficiency. work (Czerniecki et al., 2017; Gjovaag et al.,
Although measured EE values were above predicted 2018). However, a running-specific prosthetic can
values, we would expect to see an even higher energy make energy cost lower than if she used a non-
cost at the given intensity if she used a non- running- specific prosthetic, creating less of a difference
specific prosthesis. between energy cost of an amputee and an AB
These observations suggest that assessing person. The triathlete wore a running-specific
the athlete performing in his or her specific mode of prosthetic, which likely lowered her energy cost
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 52
Beezhold et. al., Energy Expenditure of Syme’s Amputee
compared to if she wore her every-day prosthetic and on the track. This provides valuable training
while running. information to the athlete and shows how the
The results of this study showed that the RMR athlete’s EE compares with the predictive equations
of the Syme’s amputee was greater than that for AB people. The primary limitation of this study
predicted by the Revised Harris-Benedict and the was the sample size of one. Therefore, no
Mifflin-St Jeor equations. This is contrary to past generalizations can be made. Lastly, the participant
studies that found that estimated RMR formulas used was asked verbally before each visit to confirm
for AB individuals in amputees to overestimate by 5- abstinence from food (8 hours), alcohol, caffeine and
32% (Schmalz et al., 2002; Buchholz et al., 2004). vigorous exercise (24 hours) before the RMR test and
However, Jagmin et al. (2018) found that RMR alcohol (24 hours) before the ExEE tests; however, we
prediction equations, including the Revised Harris- cannot be certain of compliance.
Benedict and the Mifflin-St Jeor formula, consistently
underestimate RMR in male and female AB athletes. CONCLUSION
It was found that the prediction equation with the This study found that in a Syme’s amputee
smallest mean difference (-165 kcals) was the triathlete, while EE and substrate utilization during
Cunningham equation, which is based upon fat-free exercise are similar to that of an AB athlete, the
mass (FFM) instead of total body mass. Highly active triathlete expended energy at a higher rate than the
individuals are expected to have higher metabolism predicted MET values in both cycling and running,
at rest than sedentary individuals due to an increased with exception to the 400 m run. Measured RMR was
amount of fat-free mass (Jagim et al., 2018). This higher than estimations from the Revised Harris-
could explain why the triathlete showed a higher RMR Benedict and the Mifflin-St Jeor equations for the
value than the prediction equations despite the triathlete with a Syme’s amputation. Future studies
physical impairment. This could mean that an should build upon these data by profiling athletes
increased metabolism from high levels of physical with similar impairments to assist in the generation of
activity makes up for the lower energy cost of the population-specific EE prediction equations. Defining
missing or dysfunctional muscle mass of an amputee energy requirements for para-athletes may aid in
or paraplegic, respectively. Because we were unable healthy lifestyles, body weight regulation, and
to measure body composition for the triathlete, we performance enhancement.
could not use the Cunningham equation to estimate
the triathlete’s resting EE. ACKNOWLEDGMENTS
Goosey-Tolfrey et al. (2014) found that RMR
prediction equations cannot be applied to amputees We thank Patrick Lawrence with the Challenged
unless the amputation is small in magnitude. Athletes Foundation who notified their sponsored
However, the magnitude of amputation is not defined athletes of our research opportunity in aid of
to help determine when an amputee should not use recruitment. We also thank the undergraduate
resting rate prediction equations that are based off assistant, Justin Waller, who offered his time to help
AB estimations (Goosey-Tolfrey et al., 2014). Because with data collection. Finally, we gratefully
a Syme’s amputation is only the removal of the foot acknowledge the athlete who participated in the
from the ankle down, this could explain why the study.
triathlete’s RMR was higher than the predicted
FUNDING
equation’s estimate and what we might expect to see
with other types of amputation. The energy No funding declared to complete this research.
requirements of the foot are only 1.5% of the whole
body (Goosey-Tolfrey et al., 2014).
A strength of this study was that we assessed
the individual energy needs of a para-athlete at rest
and during her sport-specific workout at different
exercise intensities in both a controlled lab setting
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 53
Beezhold et. al., Energy Expenditure of Syme’s Amputee
REFERENCES and Rehabilitation, 39(2), 143-151.
https://doi:10.3109/09638288.2015.1095948
Ainsworth, B.E., Haskell, W.L., Herrmann, S.D.,
Daniels, J. (2013). Training runs and intensities. In T.
Meckes, N., Bassett, D.R., Tudor-Locke, C., Greer,
Hanlon, & C. Marty (Eds.), Daniel’s running
J.L., Vezina, J., Whitt-Glover, M.C., & Leon, A.S.
formula (3 ed., pp. 91-135). Human Kinetics, Inc.
(2011). Compendium of Physical Activities: a
Edwards, T., Barfield, Niemiro, G.M., Beals, J.W.,
second update of codes and MET values.
Broad, E.M., Molt, R.W., Lisio, M.D., Burd, N.A.,
Medicine and Science in Sports and Exercise,
& Pilutti, L.A. (2018). Physiological responses
43(8), 1575-1581.
during a 25-km time trial in elite wheelchair
https://doi:10.1249/MSS.0b013e31821ece12
athletes. Spinal Cord Series and Cases, 4(77).
Bergman, B.C., & Brooks, G.A. (1999). Respiratory
https://doi.org/10.1038/s41394-018-0114-3
gas-exchange ratios during graded exercise in
Farkas, G.J., Pitot, M.A., & Gater, Jr. D.R. (2019). A
fed and fasted trained and untrained men.
systematic review of the accuracy of estimated
Journal of Applied Physiology, 6, 479–87.
and measured resting metabolic rate in chronic
https://doi.org/10.1152/jappl.1999.86.2.479
spinal cord injury. International Journal of Sport
Blair, M. (2018). A case study of energy expenditure
Nutrition and Exercise Metabolism, 29(5), 548-
of a lower limb amputee using a running blade
558. https://doi:10.1123/ijsnem.2018-0242.
compared to a non-amputee. ProQuest
Frankenfield, D., Roth-Yousey, L., Compher, C.
Dissertations Publishing.
(2005). Comparison of predictive equations for
Blauwet, C.A., Brook, E.M., Tenforde, A.S. et al.
resting metabolic rate in healthy nonobese and
(2017). Low energy availability, menstrual
obese adults: a systematic review. Journal of the
dysfunction, and low bone mineral density in
American Dietetic Association, 105(5), 775-789.
individuals with a disability: implications for the
https://doi.org/10.1016/j.jada.2005.02.005
Para Athlete population. Sports Medicine, 47,
Gaesser, G. A., Tucker, W. J., Sawyer, B. J., Bhammar,
1697-1708. https://doi.org/10.1007/s40279-
D. M., & Angadi, S. S. (2018). Cycling efficiency
017-0696-0
and energy cost of walking in young and older
Buchholz, A.C., Pencharz, P.B. (2004). Energy
adults. Journal of Applied Physiology, 124(2),
expenditure in chronic spinal cord injury. Current
414–420.
Opinion in Clinical Nutrition Care, 6, 635-637.
https://doi.org/10.1152/japplphysiol.00789.201
https://doi.org/10.1097/00075197-200411000-
7
00008
Garber C.E., Blissmer B., Deschenes M.R., Franklin
Childers, W.L., Kistenberg, R.S., & Gregor R.J. (2009).
B.A., Lamonte M.J., Lee I.M., Nieman D.C., &
The biomechanics of cycling with a transtibial
Swain D.P. (2011). American College of Sports M.
amputation: recommendations for prosthetic
American college of sports medicine position
design and direction for future research.
stand. Quantity and quality of exercise for
Prosthetics and Orthotics International, 33(3),
developing and maintaining cardiorespiratory,
256-271.
musculoskeletal, and neuromotor fitness in
https://doi.org/10.1080/03093640903067234
apparently healthy adults: Guidance for
Childers, W. L., Kistenberg, R. S., & Gregor, R. J.
prescribing exercise. Medicine & Science in
(2011). Pedaling asymmetries in cyclists with
Sports Exercise, 43,1334–1359.
unilateral transtibial amputation: effect of
https://doi:10.1249/MSS.0b013e318213fefb
prosthetic foot stiffness. Journal of Applied
Gjovaag, T., Mirtaheri, P., & Starholm, I. M. (2017).
Biomechanics, 27(4), 314–321.
Carbohydrate and fat oxidation in persons with
https://doi.org/10.1123/jab.27.4.314
lower limb amputation during walking with
Czerniecki, J.M., & Morgenroth, D.C. (2017).
different speeds. Prosthetics and Orthotics
Metabolic energy expenditure of ambulation in
International, 42(3), 304-310.
lower extremity amputees: what have we
https://doi.org/10.1177/0309364617740237
learned and what are the next steps? Disability
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 54
Beezhold et. al., Energy Expenditure of Syme’s Amputee
Goosey-Tolfrey V., Keil M., & Booke-Wavell K. 32(7), 1875-1881.
(2016). A comparison of methods for the https://doi:10.1519/JSC.0000000000002111
estimation of body composition in highly trained Joaquim, D.P., Juzwiak, C.R., & Winckler, C. (2018).
wheelchair game players. International Journal Do Paralympic track and field athletes have low
of Sports Medicine, 37(10), 799-806. energy availability? Revista Brasileira de
https://doi.org/10.1055/s-0042-104061 Cineantropometria & Desempenho Humano,
Goosey-Tolfrey, V., Krempien, J., & Price, M. (2014). 20(1), 71-81. https://doi.org/10.5007/1980-
Spinal cord injuries. In E. Broad (Ed). Sports 0037.2018v20n1p71
Nutrition for Paralympic Athletes (1 ed., pp. 67- Levine, J. (2005). Measurement of energy
90). Boca Raton: CRC Press. expenditure. Public Health Nutrition, 8(7a),
https://doi.org/10.1201/b16375 1123-1132. https://doi:10.1079/PHN2005800
Goosey-Tolfrey, V., & Leicht, C.A. (2013). Field-based Mifflin, M.D., St Jeor, S.T., Hill, L.A., Scott, B.J.,
physiological testing of wheelchair athletes. Daugherty, S.A., & Koh, Y.O. (1990). A new
Sports Medicine, 43, 77-91. predictive equation for resting energy
https://doi.org/10.1007/s40279-012-0009-6 expenditure in healthy individuals. The American
Hall, C, Figueroa, A., Fernhall, B., & Kanaley, J. Journal of Clinical Nutrition, 5(2), 241–247.
(2004). Energy expenditure of walking and https://doi:10.1093/ajcn/51.2.241.
running: comparison with prediction equations. Price, M. (2010). Energy expenditure and
Medicine & Science in Sports & Exercise, 36(12), metabolism during exercise in persons with a
2128-2134. https://doi: spinal cord injury. Sports Medicine, 40, 681–696.
10.1249/01.MSS.0000147584.87788.0E https://doi.org/10.2165/11531960-000000000-
Haugen, H.A., Chan, L.‐N. & Li, F. (2007). Indirect 00000
calorimetry: A practical guide for clinicians. Schmalz, T., Blumentritt, S., & Jarasch, R. (2002).
Nutrition Clinical Practice, 22, 377-388. Energy expenditure and biomechanical
https://doi:10.1177/0115426507022004377 characteristics of lower limb influence of
Hawley, J.A., & Leckey, J.J. (2015). Carbohydrate prosthetic alignment and different prosthetic
dependence during prolonged, intense components. Gait & Posture, 16(3), 255-263.
endurance exercise. Sports Medicine. 45, 5–12. https://doi.org/10.1016/S0966-6362(02)00008-5
https://doi:10.1007/s40279-015-0400-1 Ward, K.H., & Merers, M.C. (1995). Exercise
Jagim, A.R., Camic, C.L., Kisiolek, J., Erickson, J., performance of lower-extremity amputees.
Jones, M.T., & Oliver, J.M. (2018). Accuracy of Sports Medicine, 20(4), 207-214.
resting metabolic rate prediction equations in https://doi.org/10.2165/00007256-199520040-
athletes. The Journal of Strength & Conditioning, 0000
*Address correspondence to:
Erin Beezhold
Email: erinjeannebeezhold@gmail.com
Heidi M. Lynch, Ph.D., RDN
Email: hlynch@pointloma.edu
Journal of Kinesiology and Wellness - Student Edition, Volume 9, Number 2, 2020 55
View publication stats
You might also like
- ACSM Guidelines DownloadDocument11 pagesACSM Guidelines DownloadGOLDEN FIZZIK GYM14% (14)
- (Aquatic Exercise Association) Aquatic Fitness Pro (B-Ok - CC) PDFDocument422 pages(Aquatic Exercise Association) Aquatic Fitness Pro (B-Ok - CC) PDFVadim Gaivoronschi100% (1)
- Vital Signs of AnimalsDocument9 pagesVital Signs of AnimalsCherry Luz Linco RezagaNo ratings yet
- NCLEX Cardiovascular Exam 2020 - Questions and AnswersDocument74 pagesNCLEX Cardiovascular Exam 2020 - Questions and AnswersNeoGellin83% (6)
- Energy Expenditure Estimation of A Moderate Intensity Strength Training SessionDocument14 pagesEnergy Expenditure Estimation of A Moderate Intensity Strength Training SessionNelson Carvas JrNo ratings yet
- ErtDocument18 pagesErtRon FranklinNo ratings yet
- Fphys 12 668055Document9 pagesFphys 12 668055tilahunNo ratings yet
- Dose-Response Relationship Between Weekly Resistance Training Volume and Increases in Muscle Mass - A Systematic Review and Meta-Analysis PDFDocument10 pagesDose-Response Relationship Between Weekly Resistance Training Volume and Increases in Muscle Mass - A Systematic Review and Meta-Analysis PDFThiago Leal100% (1)
- Moderators of Strength Gains and Hypertrophy in Resistance Training: A Systematic Review and Meta-AnalysisDocument11 pagesModerators of Strength Gains and Hypertrophy in Resistance Training: A Systematic Review and Meta-AnalysisJoão Rangel MiguelNo ratings yet
- Revisão - Efeito Da Ordem Dos Exercícios Na Força e HipertrofiaDocument10 pagesRevisão - Efeito Da Ordem Dos Exercícios Na Força e HipertrofiaEverton GomesNo ratings yet
- Comparison of The Effects of Velocity Based Vs Traditional Resistance Training Methods On Adaptations in Strength Power and Sprint Speed A SystematicDocument16 pagesComparison of The Effects of Velocity Based Vs Traditional Resistance Training Methods On Adaptations in Strength Power and Sprint Speed A SystematicbvgqptkhshNo ratings yet
- Sutton 2009Document9 pagesSutton 2009dinhopitalugaNo ratings yet
- ArtigoNovo Carlos e Ronei FutsalDocument5 pagesArtigoNovo Carlos e Ronei FutsalWesley DamacenoNo ratings yet
- What Influence Does Resistance Exercise Order Have On Muscular Strength Gains and Muscle Hypertrophy? A Systematic Review and Meta-AnalysisDocument23 pagesWhat Influence Does Resistance Exercise Order Have On Muscular Strength Gains and Muscle Hypertrophy? A Systematic Review and Meta-AnalysisTiago FernandesNo ratings yet
- European Journal of Sport Science - 2024 - Enes - The Effects of Squat Variations On Strength and Quadriceps HypertrophyDocument10 pagesEuropean Journal of Sport Science - 2024 - Enes - The Effects of Squat Variations On Strength and Quadriceps HypertrophyLukas RenannNo ratings yet
- Effects of Linear and Daily UndulatingDocument20 pagesEffects of Linear and Daily UndulatingNATHALIA MARIA TORRES DA SILVANo ratings yet
- Do Lower Limb Previous Injuries Affect Balance Performance - Sarto2019Document5 pagesDo Lower Limb Previous Injuries Affect Balance Performance - Sarto2019Jaime Fernandez FernandezNo ratings yet
- Fspor 03 803366Document8 pagesFspor 03 803366BorisJoséChacónLópezNo ratings yet
- Indoor Cycling Energy Expenditure: Does Sequence Matter?: Environmental Research and Public HealthDocument8 pagesIndoor Cycling Energy Expenditure: Does Sequence Matter?: Environmental Research and Public HealthHOME ASSISTANTNo ratings yet
- Relationship Between Training Load and Recovery in Collegiate American Football Players During Pre-Season TrainingDocument10 pagesRelationship Between Training Load and Recovery in Collegiate American Football Players During Pre-Season TrainingtayfunertebelNo ratings yet
- Comparison of The Effects of Velocity Based Vs Traditional Resistance Training Methods On Adaptations in Strength Power and Sprint Speed A SystematicDocument16 pagesComparison of The Effects of Velocity Based Vs Traditional Resistance Training Methods On Adaptations in Strength Power and Sprint Speed A SystematicSergi ManzanoNo ratings yet
- Reduced Energy Availability Implications For Bone Health in Physically Active PopulationsEuropean Journal of NutritionDocument13 pagesReduced Energy Availability Implications For Bone Health in Physically Active PopulationsEuropean Journal of NutritionAri YulistiNo ratings yet
- Nunesetal2020Meta AnalysisexerciseorDocument10 pagesNunesetal2020Meta AnalysisexerciseorRichard Mezadri ViebrantzNo ratings yet
- Ijsnem Article p403Document9 pagesIjsnem Article p403Jonathan ValenzuelaNo ratings yet
- Fpsyg 11 01888Document11 pagesFpsyg 11 01888ceydaalyazhotamisNo ratings yet
- Return To Play Protocols For Musculoskeletal Upper and Lower Limb Injuries in Tackle-Collision Team Sports A Systematic ReviewDocument15 pagesReturn To Play Protocols For Musculoskeletal Upper and Lower Limb Injuries in Tackle-Collision Team Sports A Systematic ReviewtayfunertebelNo ratings yet
- Armes, C Et Al. Just One More Rep! – Ability to Predict Proximity to Momentary Failure in Resistance Trained Persons_ a Deception Study of Predictive Ability During the Gestalt Experience of Resistance TrainingDocument28 pagesArmes, C Et Al. Just One More Rep! – Ability to Predict Proximity to Momentary Failure in Resistance Trained Persons_ a Deception Study of Predictive Ability During the Gestalt Experience of Resistance TrainingYunusNo ratings yet
- Elderly Resistance Training Loads MetaAnalysisDocument12 pagesElderly Resistance Training Loads MetaAnalysisCatarina PiresNo ratings yet
- Single Joint Exercises Do Not Provide Benefits in Performance and Anthropometric Changes in Recreational BodybuildersDocument9 pagesSingle Joint Exercises Do Not Provide Benefits in Performance and Anthropometric Changes in Recreational BodybuildersTem ginastica?No ratings yet
- Kadyan & Maman 2022Document14 pagesKadyan & Maman 2022Taha IliasNo ratings yet
- Analysis of An ESSA Position StatementDocument2 pagesAnalysis of An ESSA Position Statementnargis yahyaNo ratings yet
- Sports 09 00013Document2 pagesSports 09 00013taglio87No ratings yet
- Study of Physical Fitness Index Using Modified Harvard Step Test in Relation With Body Mass Index in Physiotherapy StudentsDocument4 pagesStudy of Physical Fitness Index Using Modified Harvard Step Test in Relation With Body Mass Index in Physiotherapy StudentsUswatun HasanahNo ratings yet
- Journal of Sports Sciences: Martin C. Refalo, Eric R. Helms, D. Lee Hamilton & Jackson J. FyfeDocument24 pagesJournal of Sports Sciences: Martin C. Refalo, Eric R. Helms, D. Lee Hamilton & Jackson J. FyfeVasco BastosNo ratings yet
- Peter WagerbergDocument18 pagesPeter WagerbergjuanNo ratings yet
- Grgic 2021Document10 pagesGrgic 2021rodrigo vieiraNo ratings yet
- Relationships Between Muscular Performance and Markers of Well-Being in Elite Rugby Union PlayersDocument27 pagesRelationships Between Muscular Performance and Markers of Well-Being in Elite Rugby Union PlayersTpacNo ratings yet
- Ajmg 185 1023Document10 pagesAjmg 185 1023Luis Briones Lau.LiNo ratings yet
- 2018 Peeyoosha Et Al. Differences in Balance, Proprioception and Reaction Time in Land and Water Based AthletesDocument10 pages2018 Peeyoosha Et Al. Differences in Balance, Proprioception and Reaction Time in Land and Water Based AthletesNathalia Bakes TeodoroNo ratings yet
- Sensitivity Oi 3kysiolojical and 3syckolojical Markers To 7raininj /oad, Ntensi Iication in Volleyball 3layersDocument14 pagesSensitivity Oi 3kysiolojical and 3syckolojical Markers To 7raininj /oad, Ntensi Iication in Volleyball 3layersSarah Aida SilvianaNo ratings yet
- Effect of Training Cessation On Muscular Performance A Meta AnalysisDocument10 pagesEffect of Training Cessation On Muscular Performance A Meta AnalysisGutoGonçalvesNo ratings yet
- Prevalence of Eating Disorders and The Predictive Power of Risk Models in Female Elite Athletes - A Controlled StudyDocument11 pagesPrevalence of Eating Disorders and The Predictive Power of Risk Models in Female Elite Athletes - A Controlled Studyfpetrelli_857303250No ratings yet
- Tabla Periodica OrtografiaDocument10 pagesTabla Periodica OrtografiacsolismNo ratings yet
- Effects of Resistance Training Performed To Repetition Failure or Non-Failure On Muscular Strength and Hypertrophy: A Systematic Review and Meta-AnalysisDocument10 pagesEffects of Resistance Training Performed To Repetition Failure or Non-Failure On Muscular Strength and Hypertrophy: A Systematic Review and Meta-AnalysisCristhian P. EcheverríaNo ratings yet
- Articulo APA2Document8 pagesArticulo APA2Maria Isabel AmorteguiNo ratings yet
- Quantification of In-Season Training Load Relative To Match Load in Professional Dutch Eredivisie Football PlayersDocument11 pagesQuantification of In-Season Training Load Relative To Match Load in Professional Dutch Eredivisie Football PlayersAmin CherbitiNo ratings yet
- 1543 2742 Article p428Document6 pages1543 2742 Article p428Jorge Rubio LopezNo ratings yet
- Training Intensity Distribution Analysis by Race Pace vs. Physiological Approach in World-Class Middle - and Long-Distance RunnersDocument9 pagesTraining Intensity Distribution Analysis by Race Pace vs. Physiological Approach in World-Class Middle - and Long-Distance RunnersultraminingNo ratings yet
- RISE Scale Concurrent and Construct Validation of A New Scale For Rating Perceived Exertion During Elastic Resistance Training in The ElderlyDocument12 pagesRISE Scale Concurrent and Construct Validation of A New Scale For Rating Perceived Exertion During Elastic Resistance Training in The ElderlyLeonardo MacedaNo ratings yet
- Practicas. Alvarez. BelenDocument40 pagesPracticas. Alvarez. BelenBelen AlvarezNo ratings yet
- Bruno Fernandez (2020) The Influence of Functional Flywheel Resistance Training On Movement Variability and Movement Velocity in Elite Rugby PlayersDocument9 pagesBruno Fernandez (2020) The Influence of Functional Flywheel Resistance Training On Movement Variability and Movement Velocity in Elite Rugby PlayersmikilampreNo ratings yet
- OndulatorioDocument20 pagesOndulatorioAnderson SanchesNo ratings yet
- 肢体间不对称Document8 pages肢体间不对称Dongting JiangNo ratings yet
- Overreaching and Overtraining in Strength Sports and Resistance Training: A Scoping ReviewDocument17 pagesOverreaching and Overtraining in Strength Sports and Resistance Training: A Scoping ReviewIvan Lucas PiconeNo ratings yet
- Single Muscle Bre Contractile Properties Differ Between Subjects - Meier Et Al. 2015Document11 pagesSingle Muscle Bre Contractile Properties Differ Between Subjects - Meier Et Al. 2015Frangolho JoãoNo ratings yet
- Vosburg 2022Document6 pagesVosburg 2022Jayne PereiraNo ratings yet
- Does Pre-Exercise Static Stretching Inhibit Maximal Muscular PerformanceDocument19 pagesDoes Pre-Exercise Static Stretching Inhibit Maximal Muscular Performancealexandra nascimentoNo ratings yet
- 4 FFBDocument7 pages4 FFBDian Ika CahyaniNo ratings yet
- Effects of Different Intensities of Resistance Training With Equated Volume Load On Muscle Strength and HypertrophyDocument11 pagesEffects of Different Intensities of Resistance Training With Equated Volume Load On Muscle Strength and HypertrophyVince CarlosNo ratings yet
- Interaction Between Caffeine and Creatine When Used As ConcurrentDocument11 pagesInteraction Between Caffeine and Creatine When Used As ConcurrentMaría Martínez FerránNo ratings yet
- Volume de Treino (Recomendações)Document12 pagesVolume de Treino (Recomendações)Henrique HungriaNo ratings yet
- The Effect of Skipping Rope Exercise On Physical and Cardiovascular Fitness Among Collegiate MalesDocument6 pagesThe Effect of Skipping Rope Exercise On Physical and Cardiovascular Fitness Among Collegiate MalesK. M. Junayed AhmedNo ratings yet
- Perancangan Dan Pengembangan Produk Helm MenggunakDocument11 pagesPerancangan Dan Pengembangan Produk Helm MenggunakRaissa NoorNo ratings yet
- Perancangan Dan Pengembangan Produk Helm MenggunakDocument11 pagesPerancangan Dan Pengembangan Produk Helm MenggunakRaissa NoorNo ratings yet
- REFERENSI: Jurnal Ilmu Manajemen Dan Akuntansi Vol.5 No.2 Desember 2017Document17 pagesREFERENSI: Jurnal Ilmu Manajemen Dan Akuntansi Vol.5 No.2 Desember 2017Raissa NoorNo ratings yet
- Sarah SharplesDocument9 pagesSarah SharplesRaissa NoorNo ratings yet
- Pengelolaan Retribusi Pelayanan Pasar Di Kabupaten Pemalang Anita Noviani PascasarjanaDocument13 pagesPengelolaan Retribusi Pelayanan Pasar Di Kabupaten Pemalang Anita Noviani PascasarjanaRaissa NoorNo ratings yet
- PreviewpdfDocument40 pagesPreviewpdfRaissa NoorNo ratings yet
- Social Science & MedicineDocument9 pagesSocial Science & MedicineRaissa NoorNo ratings yet
- A Conceptual Framework To Evaluate The Environmental Sustainability Performance of Mining Industrial FacilitiesDocument20 pagesA Conceptual Framework To Evaluate The Environmental Sustainability Performance of Mining Industrial FacilitiesRaissa NoorNo ratings yet
- Sustainable Development, Governance and Performance Measurement in Public Private Partnerships (PPPS) : A Methodological ProposalDocument25 pagesSustainable Development, Governance and Performance Measurement in Public Private Partnerships (PPPS) : A Methodological ProposalRaissa NoorNo ratings yet
- Journal Pre-Proof: Safety and Health at WorkDocument16 pagesJournal Pre-Proof: Safety and Health at WorkRaissa NoorNo ratings yet
- Social Science & Medicine 246 (2020) 112774Document11 pagesSocial Science & Medicine 246 (2020) 112774Raissa NoorNo ratings yet
- Learning and Individual Differences:, Anton AlujaDocument5 pagesLearning and Individual Differences:, Anton AlujaRaissa NoorNo ratings yet
- International Journal of Information Management Data InsightsDocument11 pagesInternational Journal of Information Management Data InsightsRaissa NoorNo ratings yet
- International Journal of Africa Nursing Sciences: Bayisa Bereka Negussie, Gebisa Bayisa OliksaDocument6 pagesInternational Journal of Africa Nursing Sciences: Bayisa Bereka Negussie, Gebisa Bayisa OliksaRaissa NoorNo ratings yet
- Analisis Beban Kerja Fisiologis Sebagai Dasar Penentuan Waktu Istirahat Untuk Mengurangi Kelelahan KerjaDocument8 pagesAnalisis Beban Kerja Fisiologis Sebagai Dasar Penentuan Waktu Istirahat Untuk Mengurangi Kelelahan KerjaJohny Iskandar Arsyad NstNo ratings yet
- Fundamentals of Work PhysiologyDocument26 pagesFundamentals of Work PhysiologyEl morroNo ratings yet
- Analisis Beban Kerja Fisiologis Sebagai Dasar Penentuan Waktu Istirahat Untuk Mengurangi Kelelahan KerjaDocument8 pagesAnalisis Beban Kerja Fisiologis Sebagai Dasar Penentuan Waktu Istirahat Untuk Mengurangi Kelelahan KerjaJohny Iskandar Arsyad NstNo ratings yet
- International Journal of Hospitality ManagementDocument6 pagesInternational Journal of Hospitality ManagementRaissa NoorNo ratings yet
- Metal Welding ProcessesDocument51 pagesMetal Welding ProcessespandiyaNo ratings yet
- What Ies Do Iie-Iab v2Document15 pagesWhat Ies Do Iie-Iab v2Abduletif HeboNo ratings yet
- Hope 2 - ReviewerDocument3 pagesHope 2 - ReviewerYianna SibayanNo ratings yet
- Edge 605 705 Owners-Manual enDocument76 pagesEdge 605 705 Owners-Manual enocondutorNo ratings yet
- Information 13 00059 v2Document18 pagesInformation 13 00059 v2hendranatjNo ratings yet
- FC-Age-predicted Maximal Heart Rate in Healthy Subjects-The HUNT Fitness Study-NESDocument8 pagesFC-Age-predicted Maximal Heart Rate in Healthy Subjects-The HUNT Fitness Study-NESDaiane DravanzNo ratings yet
- Heartrate Zones: Calculation of Heart Rate Zones Formula For Calculating Maximum Heart RateDocument3 pagesHeartrate Zones: Calculation of Heart Rate Zones Formula For Calculating Maximum Heart RateVennia PapadipoulouNo ratings yet
- 2.2 - Powerpoint D - Effects of Exercise On The Cardiovascular SystemDocument23 pages2.2 - Powerpoint D - Effects of Exercise On The Cardiovascular SystemAshraf ShaikhNo ratings yet
- Block PlanDocument3 pagesBlock Planapi-535386658No ratings yet
- Stress of Nursing Students in Clinical Simulation: A Randomized Clinical TrialDocument8 pagesStress of Nursing Students in Clinical Simulation: A Randomized Clinical Trialanon_843050552No ratings yet
- Physiology & Behavior: Xi Zhang, Zhiwei Lian, Yong WuDocument8 pagesPhysiology & Behavior: Xi Zhang, Zhiwei Lian, Yong WupestaNo ratings yet
- Module and Activities in P.E Week 3Document4 pagesModule and Activities in P.E Week 3Eloisa Jane BituinNo ratings yet
- Training Zone Calculations: Run Cycle SwimDocument7 pagesTraining Zone Calculations: Run Cycle SwimMoreno LuponiNo ratings yet
- Physio Ex Exercise 6 Activity 2Document3 pagesPhysio Ex Exercise 6 Activity 2Roland Calipayan Jr.No ratings yet
- Normal Sinus RhythmDocument97 pagesNormal Sinus RhythmNatasha LiberisNo ratings yet
- Amazfit Pace User Manual: Downloaded From Manuals Search EngineDocument17 pagesAmazfit Pace User Manual: Downloaded From Manuals Search EngineChinmi GokuNo ratings yet
- Role of Pets in Enhancing Human Well-Being PDFDocument16 pagesRole of Pets in Enhancing Human Well-Being PDFKanchan GhoshNo ratings yet
- Hill Hass Physiology of Small Sided Games Training In.3Document23 pagesHill Hass Physiology of Small Sided Games Training In.3Ali ÖZGELNo ratings yet
- p90x ExcelDocument288 pagesp90x ExcelCristhian Camilo Gómez NarváezNo ratings yet
- Exercise Stress TestingDocument54 pagesExercise Stress TestingSaranya R S100% (2)
- Atrial Fibrillation: Classification, Pathophysiology, Mechanisms and Drug Treatment PDFDocument6 pagesAtrial Fibrillation: Classification, Pathophysiology, Mechanisms and Drug Treatment PDFAlya MaulidaNo ratings yet
- EDAN Holter System V1.2Document27 pagesEDAN Holter System V1.2Suciu FlorinNo ratings yet
- Vívosmart HR/HR+: Owner's ManualDocument16 pagesVívosmart HR/HR+: Owner's ManualSimon BirdNo ratings yet
- Pulse Rate ResearchDocument5 pagesPulse Rate ResearchJhanna LouNo ratings yet
- Cardiac Rehab OTDocument24 pagesCardiac Rehab OTJacintha GohNo ratings yet
- G11 STATPRB Q3 Module4 W4Document24 pagesG11 STATPRB Q3 Module4 W4Dylan Federico BonoanNo ratings yet
- Minerva Anestesiol 2017 GruenewaldDocument15 pagesMinerva Anestesiol 2017 GruenewaldMarjorie Lisseth Calderón LozanoNo ratings yet
- Quantifying Training Load: A Comparison of Subjective and Objective MethodsDocument15 pagesQuantifying Training Load: A Comparison of Subjective and Objective MethodsStefan WintersNo ratings yet
- The Effect of Cilostazol On Right Heart FunctionDocument43 pagesThe Effect of Cilostazol On Right Heart FunctionGunawan YogaNo ratings yet