Professional Documents
Culture Documents
PREECLAMPSIA
Uploaded by
ZAY EMCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PREECLAMPSIA
Uploaded by
ZAY EMCopyright:
Available Formats
PREECLAMPSIA
Preeclampsia is a pregnancy complication characterized by high blood pressure and
signs of damage to another organ system, most often the liver and kidneys.
Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood
pressure had been normal.
Left untreated, preeclampsia can lead to serious — even fatal — complications for
both you and your baby. If you have preeclampsia, the most effective treatment is
delivery of your baby. Even after delivering the baby, it can still take a while for you
to get better.
If you're diagnosed with preeclampsia too early in your pregnancy to deliver your
baby, you and your doctor face a challenging task. Your baby needs more time to
mature, but you need to avoid putting yourself or your baby at risk of serious
complications.
Rarely, preeclampsia develops after delivery of a baby, a condition known as
postpartum preeclampsia.
Risk factors
Preeclampsia develops only as a complication of pregnancy. Risk factors include:
History of preeclampsia. A personal or family history of preeclampsia significantly
raises your risk of preeclampsia.
Chronic hypertension. If you already have chronic hypertension, you have a higher
risk of developing preeclampsia.
First pregnancy. The risk of developing preeclampsia is highest during your first
pregnancy.
New paternity. Each pregnancy with a new partner increases the risk of preeclampsia
more than does a second or third pregnancy with the same partner.
Age. The risk of preeclampsia is higher for very young pregnant women as well as
pregnant women older than 35.
Race. Black women have a higher risk of developing preeclampsia than women of
other races.
Obesity. The risk of preeclampsia is higher if you're obese.
Multiple pregnancy. Preeclampsia is more common in women who are carrying twins,
triplets or other multiples.
Interval between pregnancies. Having babies less than two years or more than 10
years apart leads to a higher risk of preeclampsia.
History of certain conditions. Having certain conditions before you become pregnant
— such as chronic high blood pressure, migraines, type 1 or type 2 diabetes, kidney
disease, a tendency to develop blood clots, or lupus — increases your risk of
preeclampsia.
In vitro fertilization. Your risk of preeclampsia is increased if your baby was
conceived with in vitro fertilization.
Complications
The more severe your preeclampsia and the earlier it occurs in your pregnancy, the
greater the risks for you and your baby. Preeclampsia may require induced labor and
delivery.
Delivery by cesarean delivery (C-section) may be necessary if there are clinical or
obstetric conditions that require a speedy delivery. Otherwise, your doctor may
recommend a scheduled vaginal delivery. Your obstetric provider will talk with you
about what type of delivery is right for your condition.
Complications of preeclampsia may include:
Fetal growth restriction. Preeclampsia affects the arteries carrying blood to the
placenta. If the placenta doesn't get enough blood, your baby may receive
inadequate blood and oxygen and fewer nutrients. This can lead to slow growth
known as fetal growth restriction, low birth weight or preterm birth.
Preterm birth. If you have preeclampsia with severe features, you may need to
be delivered early, to save the life of you and your baby. Prematurity can lead to
breathing and other problems for your baby. Your health care provider will help
you understand when is the ideal time for your delivery.
Placental abruption. Preeclampsia increases your risk of placental abruption, a
condition in which the placenta separates from the inner wall of your uterus
before delivery. Severe abruption can cause heavy bleeding, which can be life-
threatening for both you and your baby.
HELLP syndrome. HELLP — which stands for hemolysis (the destruction of
red blood cells), elevated liver enzymes and low platelet count — syndrome is a
more severe form of preeclampsia, and can rapidly become life-threatening for
both you and your baby.
Symptoms of HELLP syndrome include nausea and vomiting, headache, and
upper right abdominal pain. HELLP syndrome is particularly dangerous because
it represents damage to several organ systems. On occasion, it may develop
suddenly, even before high blood pressure is detected or it may develop without
any symptoms at all.
Eclampsia. When preeclampsia isn't controlled, eclampsia — which is
essentially preeclampsia plus seizures — can develop. It is very difficult to
predict which patients will have preeclampsia that is severe enough to result in
eclampsia.
Often, there are no symptoms or warning signs to predict eclampsia. Because
eclampsia can have serious consequences for both mom and baby, delivery
becomes necessary, regardless of how far along the pregnancy is.
Other organ damage. Preeclampsia may result in damage to the kidneys, liver,
lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of
injury to other organs depends on the severity of preeclampsia.
Cardiovascular disease. Having preeclampsia may increase your risk of future
heart and blood vessel (cardiovascular) disease. The risk is even greater if
you've had preeclampsia more than once or you've had a preterm delivery. To
minimize this risk, after delivery try to maintain your ideal weight, eat a variety
of fruits and vegetables, exercise regularly, and don't smoke.
Prevention
Researchers continue to study ways to prevent preeclampsia, but so far, no clear
strategies have emerged. Eating less salt, changing your activities, restricting calories,
or consuming garlic or fish oil doesn't reduce your risk. Increasing your intake of
vitamins C and E hasn't been shown to have a benefit.
Some studies have reported an association between vitamin D deficiency and an
increased risk of preeclampsia. But while some studies have shown an association
between taking vitamin D supplements and a lower risk of preeclampsia, others have
failed to make the connection.
In certain cases, however, you may be able to reduce your risk of preeclampsia with:
Low-dose aspirin. If you meet certain risk factors — including a history of
preeclampsia, a multiple pregnancy, chronic high blood pressure, kidney
disease, diabetes or autoimmune disease — your doctor may recommend a daily
low-dose aspirin (81 milligrams) beginning after 12 weeks of pregnancy.
Calcium supplements. In some populations, women who have calcium
deficiency before pregnancy — and who don't get enough calcium during
pregnancy through their diets — might benefit from calcium supplements to
prevent preeclampsia. However, it's unlikely that women from the United States
or other developed countries would have calcium deficiency to the degree that
calcium supplements would benefit them.
It's important that you don't take any medications, vitamins or supplements without
first talking to your doctor.
Before you become pregnant, especially if you've had preeclampsia before, it's a good
idea to be as healthy as you can be. Lose weight if you need to, and make sure other
conditions, such as diabetes, are well-managed.
Once you're pregnant, take care of yourself — and your baby — through early and
regular prenatal care. If preeclampsia is detected early, you and your doctor can work
together to prevent complications and make the best choices for you and your baby.
You might also like
- Generic Name:: Is Used To Dissolve (Cholesterol) Gallstones and PDocument9 pagesGeneric Name:: Is Used To Dissolve (Cholesterol) Gallstones and PZAY EMNo ratings yet
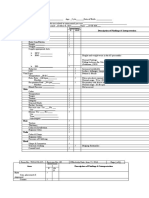
- Area Assessment Description of Findings & Interpretation General Appearance PostureDocument6 pagesArea Assessment Description of Findings & Interpretation General Appearance PostureZAY EMNo ratings yet
- FFFFDocument2 pagesFFFFZAY EMNo ratings yet
- PREECLAMPSIADocument9 pagesPREECLAMPSIAZAY EMNo ratings yet
- Diagnostic/Laborator Y Procedures Indication/Purpose S Result Analysis and Interpretation of Results Nursing ResponsibilitiesDocument2 pagesDiagnostic/Laborator Y Procedures Indication/Purpose S Result Analysis and Interpretation of Results Nursing ResponsibilitiesZAY EMNo ratings yet
- Congenital Heart DiseaseDocument2 pagesCongenital Heart DiseaseZAY EMNo ratings yet
- Congenital Heart DiseaseDocument5 pagesCongenital Heart DiseaseZAY EMNo ratings yet
- Viral GastroenteritisDocument1 pageViral GastroenteritisZAY EMNo ratings yet
- Viral GastroenteritisDocument3 pagesViral GastroenteritisZAY EMNo ratings yet
- Gestational DiabetesDocument6 pagesGestational DiabetesZAY EMNo ratings yet
- Simplifying Numerical Expressions: Rules For The Order of ExpressionDocument4 pagesSimplifying Numerical Expressions: Rules For The Order of ExpressionZAY EMNo ratings yet
- Gestational DiabetesDocument1 pageGestational DiabetesZAY EMNo ratings yet
- Speech BullyingDocument1 pageSpeech BullyingZAY EMNo ratings yet
- BasketballDocument11 pagesBasketballZAY EMNo ratings yet
- Florence Nightingale'S Environmental TheoryDocument16 pagesFlorence Nightingale'S Environmental TheoryZAY EMNo ratings yet
- Hildegard Peplau: Interpersonal Relations TheoryDocument4 pagesHildegard Peplau: Interpersonal Relations TheoryZAY EMNo ratings yet
- Hildegard Peplau: Interpersonal Relations TheoryDocument5 pagesHildegard Peplau: Interpersonal Relations TheoryZAY EMNo ratings yet
- InfographicDocument1 pageInfographicZAY EMNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Fume Cup BrochureDocument2 pagesFume Cup Brochuremfisol2000No ratings yet
- DAR Provincial Office: On-the-Job Training (OJT) Training PlanDocument3 pagesDAR Provincial Office: On-the-Job Training (OJT) Training PlanCherry Jean MaanoNo ratings yet
- Towards (De-) Financialisation: The Role of The State: Ewa KarwowskiDocument27 pagesTowards (De-) Financialisation: The Role of The State: Ewa KarwowskieconstudentNo ratings yet
- Human Computer Interaction LECTURE 1Document19 pagesHuman Computer Interaction LECTURE 1mariya ali100% (2)
- 2019 National Innovation PoliciesDocument98 pages2019 National Innovation PoliciesRashmi SinghNo ratings yet
- Policing System Indonesia PolicingDocument5 pagesPolicing System Indonesia Policingdanilo bituin jrNo ratings yet
- ECB Priority III: Deutz - Starter MotorDocument7 pagesECB Priority III: Deutz - Starter MotorMarcelo OlivaresNo ratings yet
- Chapter 1: Introduction Aviation Industry: Mini Project On Vistara AirlinesDocument84 pagesChapter 1: Introduction Aviation Industry: Mini Project On Vistara Airlinesselvaraj rapakaNo ratings yet
- NHD Process Paper 1Document2 pagesNHD Process Paper 1api-544229559No ratings yet
- Report Web AuditDocument17 pagesReport Web Auditanupprakash36No ratings yet
- Law Sample QuestionDocument2 pagesLaw Sample QuestionknmodiNo ratings yet
- Region 2Document75 pagesRegion 2yoyiyyiiyiyNo ratings yet
- Articles On Philippine Obligation and ContractsDocument114 pagesArticles On Philippine Obligation and ContractsKriz Batoto100% (1)
- 2.peace Treaties With Defeated PowersDocument13 pages2.peace Treaties With Defeated PowersTENDAI MAVHIZANo ratings yet
- Febryruthwahyuni Lds g1718 Bilphy MRDocument11 pagesFebryruthwahyuni Lds g1718 Bilphy MRfebry sihiteNo ratings yet
- Chemistry: Presented By: Mrs. Marie Nella T. VictoriaDocument75 pagesChemistry: Presented By: Mrs. Marie Nella T. VictoriaJESPHER GARCIANo ratings yet
- Coles Stategic AssessmentDocument10 pagesColes Stategic AssessmentRichardNo ratings yet
- College Physics Global 10th Edition Young Solutions ManualDocument25 pagesCollege Physics Global 10th Edition Young Solutions ManualSaraSmithdgyj100% (57)
- International Banking & Foreign Exchange ManagementDocument4 pagesInternational Banking & Foreign Exchange ManagementAnupriya HiranwalNo ratings yet
- Unit 2 Listening SkillDocument7 pagesUnit 2 Listening SkillSbgacc SojitraNo ratings yet
- The Fat Cat Called PatDocument12 pagesThe Fat Cat Called PatAlex ArroNo ratings yet
- Family Advent Devotions 1Document3 pagesFamily Advent Devotions 1collingdalenazNo ratings yet
- RSC SCST Programme Briefing For Factories enDocument4 pagesRSC SCST Programme Briefing For Factories enmanikNo ratings yet
- Andrea Falcon - Aristotle On How Animals MoveDocument333 pagesAndrea Falcon - Aristotle On How Animals MoveLigia G. DinizNo ratings yet
- Carnatic Music NotationDocument6 pagesCarnatic Music Notationksenthil kumar100% (1)
- Cb-3 Mech'l Plans 05.06.22Document12 pagesCb-3 Mech'l Plans 05.06.22Mark Vincent MoraNo ratings yet
- Swot Analysis of PiramalDocument5 pagesSwot Analysis of PiramalPalak NarangNo ratings yet
- Guidelines On Setting Up A Newman Fellowship 2017-2018Document6 pagesGuidelines On Setting Up A Newman Fellowship 2017-2018Liz McFeelyNo ratings yet
- A Proposed Approach To Handling Unbounded Dependencies in Automatic ParsersDocument149 pagesA Proposed Approach To Handling Unbounded Dependencies in Automatic ParsersRamy Al-GamalNo ratings yet
- A Study of Consumer Protection Act Related Related To Banking SectorDocument7 pagesA Study of Consumer Protection Act Related Related To Banking SectorParag SaxenaNo ratings yet