Professional Documents
Culture Documents
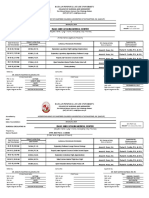
EFP - Systemic and Other Periodontal Conditions
EFP - Systemic and Other Periodontal Conditions
Uploaded by
Roshan PatelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EFP - Systemic and Other Periodontal Conditions
EFP - Systemic and Other Periodontal Conditions
Uploaded by
Roshan PatelCopyright:
Available Formats
•
Numerous systemic disorders can affect the initiation and progression of periodontitis, or can
negatively impact the periodontal structures.
• The new classification of gingival recession is based on interproximal attachment loss and combines
clinical parameters, including gingival phenotype, and characteristics of the exposed root surface.
• Occlusal forces can damage teeth and the periodontal attachment apparatus.
• Developmental or acquired conditions associated with teeth or prostheses may predispose to
diseases of the periodontium.
• Periodontal abscesses and endo-periodontal lesions can also affect the periodontium.
Author Søren Jepsen
Published March 2019 European
Federation of
© European Federation of Periodontology Periodontology
Introduction
Human periodontal diseases encompass a wide spectrum of conditions in addition
to gingival diseases and periodontitis. Some of these are related to plaque biofilm
while others arise independently of biofilm accumulation and may either be modified
by the biofilm or be uninfluenced by it.
It was the remit of working group 3 of the 2017 World Workshop to review and
update the 1999 classification on periodontal manifestations of systemic diseases
and developmental and acquired conditions, and to develop case definitions and
diagnostic considerations.
Periodontal manifestations of systemic diseases and conditions
There are rare systemic disorders, such as Papillon–Lefèvre syndrome, that result
in the early presentation of severe periodontitis. They have a major impact on the
loss of periodontal tissues by influencing periodontal inflammation. Such conditions
are grouped together as “periodontitis as a manifestation of systemic disease” and
classification is based on the primary systemic disease (using ICD-10 codes).
There are more common systemic diseases – such as diabetes mellitus – that are
important modifiers of the course of periodontitis. However, diabetes-associated
periodontitis should not be regarded as a distinct diagnosis – diabetes is now included
in the new clinical classification of periodontitis as a descriptor in the grading process.
In a similar way, smoking – now regarded as nicotine dependence and as a chronic
relapsing medical disorder with major negative effects on the periodontium – is now
also included as a descriptor in the grading process.
Other systemic conditions, such as neoplastic diseases, can affect the periodontal
tissues independently of biofilm-induced inflammation. They are also classified
based on the primary systemic disease (using ICD-10 codes) and are now grouped
together as “systemic diseases or conditions that affect the periodontal supporting
tissues.”
A case of
“periodontitis”
in a patient with
uncontrolled
diabetes mellitus.
This is not a case of
“periodontitis as a
direct manifestation
of systemic disease”
Systemic and other periodontal conditions Guidance for clinicians 2
Periodontitis as a manifestation of systemic disease
Systemic disorders with major impact on loss of periodontal tissues by influencing
periodontal inflammation:
• Genetic disorders
-- Diseases associated with immunological disorders (e.g. Papillon-Lefèvre syndrome)
-- Diseases affecting the oral mucosa and gingival tissue (e.g. epidermolysis bullosa)
-- Diseases affecting connective tissues (e.g. Ehlers-Danlos syndromes)
-- Metabolic and endocrine disorders (e.g. hypophosphatasia)
• Acquired immunodeficiency diseases (e.g. HIV infection)
• Inflammatory diseases (e.g. inflammatory bowel disease)
Other systemic disorders that influence the pathogenesis of periodontal diseases:
• Diabetes mellitus
• Obesity
• Smoking (nicotine dependence)
Systemic diseases or conditions that affect the periodontal supporting tissues
Systemic disorders that can result in loss of periodontal tissues independently
of periodontitis:
• Neoplasms (e.g. oral squamous-cell carcinoma)
• Other disorders that may affect periodontal tissues (e.g. Langerhans cell histiocytosis)
Mucogingival conditions
The importance of the gingival phenotype – including gingival thickness
and width – is now recognised and a new classification for gingival recessions
has been introduced. This combines clinical parameters such as the gingival
phenotype, the interproximal attachment loss, and the characteristics of the
exposed root surface.
Classification of mucogingival conditions (gingival phenotype) and gingival recessions
Gingival site Tooth site
Recession Gingiva Width of CEJ Step
RT = recession type (Cairo et al. 2011) depth thickness keratinised (A/B) (+/-)
gingiva
CEJ = cemento-enamel junction
(Class A = detectable CEJ, No recession
Class B = undetectable CEJ)
Step = root-surface concavity RT1
(Class + = presence of a cervical step
> 0.5mm. RT2
Class – = absence of a cervical step
> 0.5mm) RT3
(Pini Prato et al. 2010)
Systemic and other periodontal conditions Guidance for clinicians 3
RT1 RT2 RT3
-- REC with no loss of -- REC with loss of -- REC with loss of
interproximal CAL interproximal CAL interproximal CAL
-- Interproximal CEJ is not -- Interproximal loss of CAL -- Interproximal loss of CAL
visible is less than or equal to is greater than loss of
buccal CAL loss buccal CAL
A patient with multiple
gingival recession defects
of various recession types,
gingival phenotypes
and root-surface
conditions. Individual
case assessments (tooth
by tooth) are required
to facilitate adequate
treatment planning.
(Photo: K. Jepsen).
Graphics RT1, RT2, RT3 courtesy H. Dommisch.
Occlusal trauma and traumatic occlusal forces
Traumatic occlusal force, which replaces the term “excessive occlusal force” of the
previous (1999) classification, is any occlusal force that results in injury to teeth (such
as excessive wear or fracture) and/or to the periodontal attachment apparatus.
Occlusal trauma is a histological term to describe the injury of the periodontal
attachment apparatus.
The presence of traumatic occlusal forces and occlusal trauma may be indicated
by one or more of the following: (a) fremitus (adaptive tooth mobility), (b) progressive
tooth mobility, (c) thermal sensitivity, (d) excessive occlusal wear, (e) tooth migration,
(f) discomfort/pain on chewing, (g) fractured teeth, (h) radiographically widened
periodontal ligament space, (i) root resportion, (j) hypercementosis.
It should be noted that some of the signs and symptoms of traumatic occlusal
forces and occlusal trauma may also be associated with other conditions. Therefore,
an appropriate differential analysis must be performed to rule out alternative
aetiological factors.Traumatic occlusal forces lead to adaptive mobility in teeth with
Systemic and other periodontal conditions Guidance for clinicians 4
normal support (primary occlusal trauma) and to progressive mobility in teeth with
reduced support (secondary occlusal trauma), usually requiring splinting.
There is no evidence from human studies that traumatic occlusal forces accelerate
the progression of periodontitis or that they can cause non-carious cervical lesions
or gingival recessions.
Cervical enamel
projections are an example
of tooth-related factors
that can predispose to loss
of periodontal supporting
tissues – in this case
severe buccal furcation
involvement of the first
molar.
(Photo: K. & S. Jepsen).
Prosthesis-related and tooth-related factors
Classification of factors related to teeth and to dental prostheses
that can affect the periodontium
A. Localised tooth-related factors that modify or predispose
to biofilm-induced gingival diseases/periodontitis
1. Tooth anatomical factors
2. Root fractures
3. Cervical root resorption, cemental tears
4. Root proximity
5. Altered passive eruption
B. Localised dental-prosthesis-related factors
1. Restoration margins placed within the supracrestal attached tissues
2. Clinical procedures related to the fabrication of indirect restorations
3. Hypersensitivity/toxicity reactions to dental materials
This section is expanded in the new classification. It comprises all factors that
modify or predispose to biofilm-induced gingival diseases/periodontitis.
• The term “biologic width” is replaced by “supracrestal tissue attachment”, consisting
of junctional-epithelium and supracrestal connective tissue.
• An infringement of restorative margins within the supracrestal connective-tissue
attachment is associated with inflammation and loss of periodontal supporting tissue.
Systemic and other periodontal conditions Guidance for clinicians 5
• The design, fabrication, delivery, and materials used for tooth-supported/retained
restorations and fixed dental prosthetic procedures can be associated with
plaque retention, gingival recession, and loss of periodontal supporting tissue.
• Tooth anatomical factors (i.e. cervical enamel projections, enamel pearls,
developmental grooves), root proximity, abnormalities and fractures, and tooth
relationships in the dental arch are related to gingival inflammation induced by
dental-plaque biofilm and loss of periodontal supporting tissues.
Periodontal abscesses
Case definition: A periodontal abscess is a localised accumulation of pus located
within the gingival wall of the periodontal pocket/sulcus, resulting in a significant
tissue breakdown. The primary detectable signs or symptoms associated with a
periodontal abscess may involve ovoid elevation in the gingiva, along the lateral
part of the root, and bleeding on probing. Other signs and symptoms include pain,
suppuration on probing, deep periodontal pockets, and increased tooth mobility.
A periodontal abscess may develop in a pre-existing periodontal pocket – for
example, in patients with untreated periodontitis, under supportive therapy, after
scaling and root planing, or after systemic antimicrobial therapy. A periodontal
abscess occurring at a site that was previously periodontally healthy is commonly
associated with a history of impaction or harmful habits.
Classification of periodontal abscesses based on the aetiological factors involved
Untreated periodontitis
Periodontal Acute Non-responsive to
abscess in exacerbation periodontitis therapy
periodontitis
patients (in Supportive periodontal therapy
a pre-existing Post-scaling
periodontal Post-surgery
pocket) After
treatment Systemic antimicrobials
Post-medication
Other drugs: nifedipine
Dental floss, orthodontic
Impaction elastic, toothpick, rubber
dam or popcorn hulls
Harmful habits Wire or nail biting and
clenching
Periodontal Orthodontic factors Orthodontic forces or a
abscess in non cross-bite
periodontitis
Gingival overgrowth
patients (not
mandatory Invaginated tooth,
to have a Severe anatomic alterations dens evaginatus,
a pre-existing or odontodysplasia
periodontal Minor anatomic alterations Cemental tears, enamel
pocket) pearls, or development
Alteration of
root surface grooves
Iatrogenic conditions Perforations
Severe root damage Fissure or fracture,
cracked-tooth syndrome
Post-surgery
Systemic and other periodontal conditions Guidance for clinicians 6
Endo-periodontal lesions
Endo-periodontal lesions should be classified according to signs and symptoms
that have direct impact on their prognosis and treatment (such as the presence
or absence of fractures and perforations, and the presence or absence of
periodontitis).
Case definition: An endo-periodontal lesion is a pathological communication
between the pulpal and periodontal tissues at a given tooth that may occur in
an acute or a chronic form. The primary signs associated with this lesion are
deep periodontal pockets extending to the root apex and/or a negative/altered
response to pulp-vitality tests.
Other signs/symptoms may include: (a) radiographic evidence of bone loss in the
apical or furcation region, (b) spontaneous pain or pain on palpation/percussion,
(c) purulent exudate/suppuration, (d) tooth mobility, (e) sinus tract/fistula, (f)
crown and/or gingival colour alterations.
Signs observed in endo-periodontal lesions associated with traumatic and/or
iatrogenic factors may include root perforation, fracture/cracking, or external
root resorption. These conditions drastically impair the prognosis of the involved
tooth.
Classification of endo-periodontal lesions
Endo-periodontal Root fracture or cracking
lesion with root Root-canal or pulp-chamber perforation
damage External root resorption
Grade 1 - narrow deep periodontal pocket
in one tooth surface
Endo-periodontal
lesion in Grade 2 - wide deep periodontal pocket
periodontitis in one tooth surface
patients
Grade 3 - deep periodontal pocket
Endo-periodontal in more than one tooth surface
lesion without root
damage Grade 1 - narrow deep periodontal pocket
Endo-periodontal in one tooth surface
lesion in Grade 2 - wide deep periodontal pocket
non-periodontitis in one tooth surface
patients
Grade 3 - deep periodontal pocket
in more than one tooth surface
Endo-periodontal
lesion (Grade 3) in a
periodontitis patient
(Photo: H. Dommisch)
Systemic and other periodontal conditions Guidance for clinicians 7
Further reading Proceedings of the World Workshop on the Classification of Periodontal and Peri-implant
Diseases and Conditions,
co-edited by Kenneth S. Kornman and Maurizio S. Tonetti.
Journal of Clinical Periodontology, Volume 45, Issue S20, June 2018.
Proceedings include:
--Jepsen S, Caton JG, et al. Periodontal manifestations of systemic diseases and
developmental and acquired conditions: Consensus report of workgroup 3 of the 2017
World Workshop on the Classification of Periodontal and Peri-Implant Diseases and
Conditions: S219-S229.
--Albandar JM, Susin C, Hughes FJ. Manifestations of systemic diseases and conditions
that affect the periodontal attachment apparatus: case definitions and diagnostic
considerations: S171-S189.
--Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: narrative
review, case definitions and diagnostic considerations: S190-S198.
--Fan J, Caton JG. Occlusal trauma and excessive occlusal forces: narrative review, case
definitions, and diagnostic considerations: S199-S206.
--Ercoli C, Caton JG. Dental prostheses and tooth-related factors: S207-S218.
--Herrera D, Retamal-Valdes B, Alonso B, Feres M. Acute periodontal lesions (periodontal
abscesses and necrotising periodontal diseases) and endo-periodontal lesions: S78-S94.
--Papapanou PN, Sanz M, et al. Periodontitis: Consensus report of workgroup 2 of the
2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases
and Conditions, S162-S170.
Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. The interproximal clinical attachment
level to classify gingival recessions and predict root coverage outcomes: an explorative and
reliability study. J Clin Periodontol. 2011; 38: 661-666.
Pini-Prato G, Franceschi D, Cairo F, Nieri M, Rotundo R. Classification of dental surface
defects in areas of gingival recession. J Periodontol. 2010; 81: 885-890.
Author
Søren Jepsen
Søren Jepsen is professor and chair of the Department of Periodontology, Operative
and Preventive Dentistry at the University of Bonn, Germany. He has served on
the executive committee of the European Federation of Periodontology (EFP) as
chair of its research committee (2004-2010), as a board member (2012-2017),
and as president (2015-2016). He was also co-chair of the organising committee
for the AAP/EFP World Workshop on the Classification of Periodontal and
Peri-implant Diseases and Conditions (2017), and scientific chair of EuroPerio9
(2018). Prof Jepsen has lectured and published extensively, has received
numerous awards, and is associate editor of the Journal of Clinical Periodontology
and an editorial-board member of Clinical Oral Implants Research, the European
Journal of Oral Implantology, and the Chinese Journal of Dental Research.
Systemic and other periodontal conditions Guidance for clinicians 8
New Classification of periodontal and peri-implant diseases and conditions
The New Classification is the product of the World Workshop on the Classification of
Periodontal and Peri-implant Diseases and Conditions, held in Chicago in November
2017. The World Workshop was organised jointly by the American Academy of
Periodontology (AAP) and the European Federation of Periodontology (EFP) to create
a consensus knowledge base for a new classification to be promoted globally. The
New Classification updates the previous classification made in 1999. The research
papers and consensus reports of the World Workshop were published simultaneously
in June 2018 in the EFP’s Journal of Clinical Periodontology and the AAP’s Journal of
Periodontology. The new classification was presented formally by the two organisations
at the EuroPerio9 congress in Amsterdam in June 2018.
European
Federation of
Periodontology
About the EFP
The European Federation of Periodontology (EFP) is an umbrella organisation of 35
national scientific societies devoted to promoting research, education, and awareness
of periodontal science and practice. It represents more than 14,000 periodontists and
gum-health professionals in Europe alone. In addition to 31 European members,
the EFP has recently welcomed four international associate members from Asia, the
Middle East, and Latin America.
www.efp.org
www.efp.org/newclassification
European Federation of Periodontology
Avenida Doctor Arce, 14. Office 38
28002 Madrid
Spain
You might also like
- Prevmed Reaction PaperDocument2 pagesPrevmed Reaction Paperapi-3801039100% (5)
- Textbook of Orthodontics - Samir Bishara - 599 - 52MBDocument599 pagesTextbook of Orthodontics - Samir Bishara - 599 - 52MBPratyusha Vallam96% (45)
- Chcage001 Student Workbook (Word) (c3) .v1.2Document55 pagesChcage001 Student Workbook (Word) (c3) .v1.2Saima Rashid100% (1)
- Critical Health Concerns of The 21st CenturyDocument2 pagesCritical Health Concerns of The 21st CenturySafa AamirNo ratings yet
- Periodontitis As A Risk Factor For Systemic DiseaseDocument13 pagesPeriodontitis As A Risk Factor For Systemic DiseaseRussia Al ShboulNo ratings yet
- Tonetti Et Al-2018-Journal of Periodontology TDocument14 pagesTonetti Et Al-2018-Journal of Periodontology TJonathan Meza MauricioNo ratings yet
- English CurriculumDocument9 pagesEnglish CurriculumsunilbijlaniNo ratings yet
- 03 Enf. SistemicasDocument12 pages03 Enf. SistemicasAgustin BuryakNo ratings yet
- Diagnosis and Classification of Periodontal Disease and PrognosisDocument40 pagesDiagnosis and Classification of Periodontal Disease and PrognosishayiarNo ratings yet
- Manifestations of Systemic Diseases and Conditions That Affect The Periodontal Attachment Apparatus: Case Definitions and Diagnostic ConsiderationsDocument22 pagesManifestations of Systemic Diseases and Conditions That Affect The Periodontal Attachment Apparatus: Case Definitions and Diagnostic ConsiderationsMarco Antonio García LunaNo ratings yet
- Clasificacion de Enf 2017Document10 pagesClasificacion de Enf 2017Jonathan Meza MauricioNo ratings yet
- Jper 17-0733Document12 pagesJper 17-0733Jonathan Meza MauricioNo ratings yet
- Journal of Controlled ReleaseDocument14 pagesJournal of Controlled ReleaseRachmawati Dian PuspitasariNo ratings yet
- Albandar Et Al-2018-Journal of PeriodontologyDocument21 pagesAlbandar Et Al-2018-Journal of PeriodontologyVixente MontNo ratings yet
- Albandar Et Al-2018-Journal of Clinical PeriodontologyDocument19 pagesAlbandar Et Al-2018-Journal of Clinical PeriodontologyCristian CulcitchiNo ratings yet
- The Classification of Periodontal and Peri-Implant Diseases and ConditionsDocument98 pagesThe Classification of Periodontal and Peri-Implant Diseases and ConditionsKieru BuiNo ratings yet
- Chronic PeriodontitisDocument33 pagesChronic Periodontitissidra malikNo ratings yet
- Periodontitis: Foreign-Body ReactionsDocument25 pagesPeriodontitis: Foreign-Body ReactionsAisyah Arina NurhafizahNo ratings yet
- Dental Update New Perio ClassificationDocument4 pagesDental Update New Perio ClassificationJosé Antonio Alarcón VergaraNo ratings yet
- Periodontitis Classification and Staging PDFDocument9 pagesPeriodontitis Classification and Staging PDFAnonymous 7YkiHucQlONo ratings yet
- fileadminuploadsefpDocumentsCampaignsNew ClassificationGuidance Notesreport-02 PDFDocument9 pagesfileadminuploadsefpDocumentsCampaignsNew ClassificationGuidance Notesreport-02 PDFAufa AyshaNo ratings yet
- Journal of Periodontology - 2018 - Papapanou - Periodontitis Consensus Report of Workgroup 2 of The 2017 World Workshop OnDocument10 pagesJournal of Periodontology - 2018 - Papapanou - Periodontitis Consensus Report of Workgroup 2 of The 2017 World Workshop OnMonica MartínezNo ratings yet
- Systemic Diseases or Conditions Affecting The Periodontal Tissue SupportDocument47 pagesSystemic Diseases or Conditions Affecting The Periodontal Tissue SupportVikhilPatelNo ratings yet
- Periodontitis and Systemic DiseasesDocument55 pagesPeriodontitis and Systemic DiseasesDr.Arshad SayedNo ratings yet
- Periodontal DiseaseDocument4 pagesPeriodontal Diseasemojako_badboysNo ratings yet
- Aap 2017Document3 pagesAap 2017Meithasya Radya Putri KamalNo ratings yet
- PeriodontologyDocument28 pagesPeriodontologytresfour2No ratings yet
- Enf Periondoltal 2017 PDFDocument15 pagesEnf Periondoltal 2017 PDFyenny2No ratings yet
- Papapanou Et Al 2018 Periodontitis Consensus Report of Workgroup 2 of The 2017 World Workshop On The ClassificationDocument9 pagesPapapanou Et Al 2018 Periodontitis Consensus Report of Workgroup 2 of The 2017 World Workshop On The ClassificationAnatole DuqueleNo ratings yet
- Periodontitis and Systemic Disease: BDJ Team November 2015Document5 pagesPeriodontitis and Systemic Disease: BDJ Team November 2015Jenea CapsamunNo ratings yet
- Classification of Periodontal Diseases and Conditions 2018Document15 pagesClassification of Periodontal Diseases and Conditions 2018Jean DatorNo ratings yet
- A Case Report On Generalized Aggressive Periodontitis: June 2014Document8 pagesA Case Report On Generalized Aggressive Periodontitis: June 2014Natasya AngelynaNo ratings yet
- Klasifikasi Penyakit PeriodontiumDocument15 pagesKlasifikasi Penyakit PeriodontiumDenanda Eka NugraheniNo ratings yet
- Periodontitis As A Component of Hyperinflammation:: Treating Periodontitis in Obese Diabetic PatientsDocument7 pagesPeriodontitis As A Component of Hyperinflammation:: Treating Periodontitis in Obese Diabetic PatientsbetziiNo ratings yet
- Capítulo 4 Carranza 11 Ed.Document21 pagesCapítulo 4 Carranza 11 Ed.Estefanía Paz Torrejón GuzmánNo ratings yet
- PART 1 Biologic Basis of PeriodontologyDocument3 pagesPART 1 Biologic Basis of PeriodontologyNurul HidayatiNo ratings yet
- 03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumDocument16 pages03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumFloba Ika SianturiNo ratings yet
- 2000 Controlled and Targeted Drug Delivery Strategies Towards Intraperiodontal Pocket DiseasesDocument22 pages2000 Controlled and Targeted Drug Delivery Strategies Towards Intraperiodontal Pocket DiseasesK KNo ratings yet
- J Clinic Periodontology - 2018 - Papapanou - Periodontitis Consensus Report of Workgroup 2 of The 2017 World Workshop OnDocument9 pagesJ Clinic Periodontology - 2018 - Papapanou - Periodontitis Consensus Report of Workgroup 2 of The 2017 World Workshop OnTesis Luisa MariaNo ratings yet
- Periodontology Research PaperDocument10 pagesPeriodontology Research Paperapi-511115589No ratings yet
- Grace Girgis - DissertationDocument53 pagesGrace Girgis - DissertationGraceNo ratings yet
- Staging and Grading of PeriodontitisDocument17 pagesStaging and Grading of PeriodontitisAndy HeNo ratings yet
- Hematological Pathology Between Diagnosis and Treatment in The Context of Oral Manifestations. Management of The Patient With Leukemia in The Dental Practice. ReviewDocument10 pagesHematological Pathology Between Diagnosis and Treatment in The Context of Oral Manifestations. Management of The Patient With Leukemia in The Dental Practice. ReviewoanaNo ratings yet
- Sindromi Pulpo - PeriodontalDocument12 pagesSindromi Pulpo - PeriodontalErisa BllakajNo ratings yet
- Artigo Periodontia 2Document13 pagesArtigo Periodontia 2DANIELA MARTINS LEITENo ratings yet
- Periodontitis Diseases Periodontal Tissues Alveolar Bone Periodontal Ligament Cementum Gingiva PlaqueDocument26 pagesPeriodontitis Diseases Periodontal Tissues Alveolar Bone Periodontal Ligament Cementum Gingiva PlaqueNaro HassanNo ratings yet
- Diabetes and Periodontal Diseases: An Established Two-Way RelationshipDocument21 pagesDiabetes and Periodontal Diseases: An Established Two-Way RelationshipReza Fachrial SyaifulNo ratings yet
- 4 - Staging and Grading of Periodontitis Framework and Proposal of A NewDocument14 pages4 - Staging and Grading of Periodontitis Framework and Proposal of A NewSalma HelmyNo ratings yet
- J Clinic Periodontology - 2018 - Chapple - Periodontal Health and Gingival Diseases and Conditions On An Intact and ADocument10 pagesJ Clinic Periodontology - 2018 - Chapple - Periodontal Health and Gingival Diseases and Conditions On An Intact and AAndreaNo ratings yet
- Chronic Marginal PeriodontitisDocument21 pagesChronic Marginal PeriodontitisLaslo Mihaela Larisa100% (1)
- Klasifikasi 1999 PDFDocument50 pagesKlasifikasi 1999 PDFintanNo ratings yet
- 2017 Staging Grading PerioDocument48 pages2017 Staging Grading PerioTooTiredToThinkOfANameNo ratings yet
- Journal of Periodontology - 2018 - Tonetti - Staging and Grading of Periodontitis Framework and Proposal of A NewDocument14 pagesJournal of Periodontology - 2018 - Tonetti - Staging and Grading of Periodontitis Framework and Proposal of A NewxixiyciciNo ratings yet
- Journal of Periodontology - 2018 - Tonetti - Staging and Grading of Periodontitis Framework and Proposal of A NewDocument14 pagesJournal of Periodontology - 2018 - Tonetti - Staging and Grading of Periodontitis Framework and Proposal of A NewMonica MartínezNo ratings yet
- PERIODONTITIS Systemic AntibioticsDocument6 pagesPERIODONTITIS Systemic AntibioticsPrabhjot KaurNo ratings yet
- Gingivitis: November 2018Document14 pagesGingivitis: November 2018RamonaNo ratings yet
- Classification of DiseasesDocument20 pagesClassification of Diseasesarun perioNo ratings yet
- Periodontology - IntroductionDocument11 pagesPeriodontology - IntroductionMatthew SenyahNo ratings yet
- Risk Assessment in Periodontal DiseasesDocument8 pagesRisk Assessment in Periodontal Diseasesahmedkhalidzzxx000No ratings yet
- Local and Systemic Mechanisms Linking Periodontal Disease and Inflammatory ComorbiditiesDocument15 pagesLocal and Systemic Mechanisms Linking Periodontal Disease and Inflammatory ComorbiditiesGeorgi GugicevNo ratings yet
- Ilovepdf Merged CompressedDocument99 pagesIlovepdf Merged CompressedCarina AidetNo ratings yet
- Chapple Et Al-2018-Journal of Clinical Periodontology Grupo 1Document10 pagesChapple Et Al-2018-Journal of Clinical Periodontology Grupo 1Genesis Lopez torresNo ratings yet
- Copia de Journal of Periodontology - 2018 - Tonetti - Staging and Grading of Periodontitis Framework and Proposal of A New 2Document14 pagesCopia de Journal of Periodontology - 2018 - Tonetti - Staging and Grading of Periodontitis Framework and Proposal of A New 2Javiera SepulvedaNo ratings yet
- Understanding Periodontitis: A Comprehensive Guide to Periodontal Disease for Dentists, Dental Hygienists and Dental PatientsFrom EverandUnderstanding Periodontitis: A Comprehensive Guide to Periodontal Disease for Dentists, Dental Hygienists and Dental PatientsNo ratings yet
- Your Dental Health Can Save Your Life: Unlocking the Secrets of Oral-Systemic Health: All About DentistryFrom EverandYour Dental Health Can Save Your Life: Unlocking the Secrets of Oral-Systemic Health: All About DentistryNo ratings yet
- Endo-Perio Lesions Diagnosis and InterdisciplinaryDocument5 pagesEndo-Perio Lesions Diagnosis and InterdisciplinaryGabriela ArgeseanuNo ratings yet
- Clinical and Radiographic Evaluation of The Periodontium With Biologic Width Invasion by Overextending Restoration Margins - A Pilot StudyDocument7 pagesClinical and Radiographic Evaluation of The Periodontium With Biologic Width Invasion by Overextending Restoration Margins - A Pilot StudyGabriela ArgeseanuNo ratings yet
- What Does Perio Treatment InvolveDocument2 pagesWhat Does Perio Treatment InvolveGabriela ArgeseanuNo ratings yet
- Implementingsocketsealsurgery JP2008Document11 pagesImplementingsocketsealsurgery JP2008Gabriela ArgeseanuNo ratings yet
- Perio TreatmentDocument15 pagesPerio TreatmentGabriela ArgeseanuNo ratings yet
- In The Dental Implant Era, Why Do We Still Bother Saving Teeth?Document8 pagesIn The Dental Implant Era, Why Do We Still Bother Saving Teeth?Gabriela ArgeseanuNo ratings yet
- Tord Berglundh: AuthorDocument9 pagesTord Berglundh: AuthorGabriela ArgeseanuNo ratings yet
- Ghid PracticaDocument36 pagesGhid PracticaGabriela ArgeseanuNo ratings yet
- Partial Dentures PDFDocument1 pagePartial Dentures PDFGabriela ArgeseanuNo ratings yet
- Cipla .Document14 pagesCipla .SreedhuNo ratings yet
- Manual of POCT (Point of Care Testing) : PrefaceDocument17 pagesManual of POCT (Point of Care Testing) : PrefaceSatria UtomoNo ratings yet
- DR Sally BoaDocument42 pagesDR Sally BoaInna PuriceNo ratings yet
- Isaac and Catalina Medical Center: Bataan Peninsula State University College of Nursing and MidwiferyDocument4 pagesIsaac and Catalina Medical Center: Bataan Peninsula State University College of Nursing and MidwiferyArra BeatrizNo ratings yet
- Emotional Impacts of Covid-19 To Medical Practitioners: Universidad de ManilaDocument18 pagesEmotional Impacts of Covid-19 To Medical Practitioners: Universidad de ManilaEduardo MabiniNo ratings yet
- Is A Mask Necessary in The Operating TheatreDocument3 pagesIs A Mask Necessary in The Operating TheatreGermano MatiasNo ratings yet
- TELEMEDICINE AND TELEDIAGNOSIS - General Perception RomaniaDocument8 pagesTELEMEDICINE AND TELEDIAGNOSIS - General Perception RomaniaDelia NiculaNo ratings yet
- Mental Health 2Document1 pageMental Health 2Meshael HernandezNo ratings yet
- Drugs Easily Explained by Roland SeifertDocument280 pagesDrugs Easily Explained by Roland SeifertMark Chang100% (2)
- Press Release - Breast Cancer Awareness Drive - EditedDocument2 pagesPress Release - Breast Cancer Awareness Drive - EditedParag DhurkeNo ratings yet
- Self AdministrationDocument4 pagesSelf AdministrationellaNo ratings yet
- Abnormal PsychologyDocument2 pagesAbnormal PsychologyBernard MachokaNo ratings yet
- Physical Activity Readiness Questionnaire (PAR Q) : When Using This Form, You Need To StateDocument3 pagesPhysical Activity Readiness Questionnaire (PAR Q) : When Using This Form, You Need To StateF-dawgNo ratings yet
- Delivering Race Equality in Mental Health Care: Report On The Findings and Outcomes of The Community Engagement Programme 2005-2008 Jane Fountain and Joanna Hicks FULL REPORT 2010Document152 pagesDelivering Race Equality in Mental Health Care: Report On The Findings and Outcomes of The Community Engagement Programme 2005-2008 Jane Fountain and Joanna Hicks FULL REPORT 2010tony_jameson-allenNo ratings yet
- NURS FPX 6026 Assessment 3 Population Health Policy AdvocacyDocument4 pagesNURS FPX 6026 Assessment 3 Population Health Policy Advocacyjoohnsmith070No ratings yet
- Musculoskeletal Disorders, Disability and WorkDocument130 pagesMusculoskeletal Disorders, Disability and Workpmontanher100% (1)
- Consenso de Cirurgia em Retocolite Ulcerativa e D de Crohn 2023 GEDIIBDocument19 pagesConsenso de Cirurgia em Retocolite Ulcerativa e D de Crohn 2023 GEDIIBCarla MartinsNo ratings yet
- Flyer Jump 2024Document8 pagesFlyer Jump 2024hasanyahyadrNo ratings yet
- Lsmubrochure2019 PDFDocument26 pagesLsmubrochure2019 PDFAlberto MayorgaNo ratings yet
- Health Care Delivery Concerns, National Health andDocument26 pagesHealth Care Delivery Concerns, National Health and421Karanbir KaurNo ratings yet
- USMLE Overview PDFDocument1 pageUSMLE Overview PDFYossef HammamNo ratings yet
- Breaking or Crushing TabletsDocument2 pagesBreaking or Crushing TabletsRahmaNo ratings yet
- Ra 2382Document12 pagesRa 2382Remy BedañaNo ratings yet
- CDPH Survey With Plan of CorrectionDocument67 pagesCDPH Survey With Plan of CorrectionJames WardNo ratings yet
- Goals of Patient Care GuidelineDocument12 pagesGoals of Patient Care GuidelineangelaNo ratings yet
- Surgical Product Catelog With Images Full ListDocument97 pagesSurgical Product Catelog With Images Full ListhyvasNo ratings yet