Professional Documents
Culture Documents
TAHBSO Concept Map
Uploaded by
Sherika Mariz Moreno GuarinCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TAHBSO Concept Map
Uploaded by
Sherika Mariz Moreno GuarinCopyright:
Available Formats
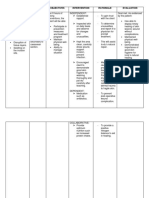
LEGEND:
RISK FACTORS
CLINICAL
MANIFESTATIONS
PATHOPHYSIOLOGY
c ar e o f a pat i e nt u nde r g o i ng t o t al abdo mi nal
DIAGNOSTIC TESTS
MEDICAL MANAGEMENT
NURSING DIAGNOSIS
NURSING
INTERVENTIONS
hy s t e r e c t o my w i t h bi l at e r al s al pi ng o -o o pho r e c t o my
COMPLICATIONS
THEORIES
(t ahbs o o )
SURGICAL PROCEDURE PREDISPOSING FCTORS
- Reproductive age
- Early menarche PRECIPITATING FCTORS
- Family history of endometriosis - Low body weight
- Late menopause - Obesity
- Prolonged menstrual flow - Intercourse during menses
- Short cycle interval PRECIPITATING FCTORS
- Genetics - Multiple sexual partners
- Infertility
Mircoogranisms
Pituitary gland PREDISPOSING FCTORS - IUD Insertion
- Reproductive age (Escherichia coli, Bacteroides fragilis, other - Sexual activity with an infected partner
- History of prior episode of PID Bacteroidesspecies, Peptostreptococcus, - Past surgery
Peptococcus, andaerobic streptococci) - Abortion
produces Luteinizing - Vaginal childbirth
Hormone (LH) and
Follicle-stimulating hormone
(FSH) Enters lower genital tract
DEMOGRAPHI C DATA
Ovulation
Name: Patient N.S.A. Enters uterus
Age: 41 years old
Retrograde menstruation
Gender: Female or sexual intercourse
ruptured follicle closes and
Nationality: Filipino Ovaries release egg
forms into corpus luteum Infection reaches fallopian
Birthdate: September 6, 1976 tubes and ovaries
Religion: Roman Catholic
Address: Tinayunan Beach, Guihulngan City, Negros Oriental Egg travels through fallopian High levels of progesterone
Educational status: College level tube and estrogen
Marital status: Married Triggers the immune system
Occupation: Housewife
Date of admission: September 13, 2020; 11:40 PM Not fertilized by sperm
Chief complaint: Vaginal bleeding Neutrophils, plasma cells,
and lymphocytes in fallopian
Physician-in-charge: Dr. GC Austria (attending physician); Dr. LS Serillo tubes
(co-managing physician) Shedding of endometrial Estrogen and progesterone
lining levels drop
History of Present illness: 3 months ago, patient had experienced Damages tubal epithelium
prolonged bleeding (used 5-10 pads/day) that lasted for 2 months. Patient and filled with pus
sought consult in attending physician's clinic and was given Althea, GnRH Menstruation
agonist, and Visanne for a month. Vaginal bleeding resolved until 4 days PTA,
vaginal bleeding recurred (used 5-10 pads/day). An hour PTA, patient had Scar tissues form
profuse vaginal bleeding fully soaking 3 pads in an hour associated with blood
clot, headache, dizziness, and pallor. Persistence of symptoms promted her
to seek consult. Vascular and lymphatic Coelomic metaplasia of Damaged epithelium binds
Dysfunction with the Immune
Retrograde menstruation dissemination of endometrial multipotential cells in the to one another
system
Past Health History: In 2008, client had observed she was experiencing cells peritoneal cavity
signs and symptoms of having irregular menstruation, severe blood loss
formation of pockets and
during menstruation and hypogastric pain. Within the same year, she Endometrial tissue endometrial tissues move
coelomic cells undergo little "dead-end" pouches
consulted with an internal medicine and was then diagnosed with right retrograde along fallopian via vasculature or lymphatic
metaplasia
tubes from uterus
ovarian cyst. The client had undergone surgery? salpingo oophorectomy
(right). After 10 years (2018), client got pregnant, however, was not aware
until 8th weeks of AOG, she had a threatened abortion. She had also Transform into endometrial Antibiotics
profuse vaginal bleeding
undergone Dilatation and Curettage and experienced positive chest pains. cells
Tubo-ovarian abscess Hypogastric pain Fever
LMP = September 11, 2020; experienced dysmenorrhea. Had fever for 2 days Corticosteroids
and cough and colds for a week. Abdominal and Reported ovarian new
Frozen Section Biopsy
Transvaginal ultrasound growth
Diagnosis: G1P0 (0010) Abnormal Uterine Bleeding-A (Adenomyoma). Left Combined Oral Laparascopy Complete Blood Count
Endometriosis External with Tubo-Ovarian Abscess by Frozen Section Biopsy Contraceptives
with very severe anemia secondary to Acute Blood Loss. Status post Gonadotropin Agonists
Abdominal and
Transvaginal ultrasound
Reported enlarged uterus
with adenomyosis uteri
salpingo-oophorectomy right pelvic endometriosis
Laparascopy
Endometrial tissues located Pap smear
CASE SCENARI O outside of uterine cavity
Endometrial biopsy
Changes in hormone levels
and chronic inflammation
Patient N.S.A., 41-year-old woman, was admitted due to profuse
vaginal bleeding associated with hypogastric pain with blood clot, Shed or bleed during
profuse vaginal bleeding
headache, dizziness, and pallor. Her diagnostic exams reported an menstruation
enlarged uterus with adenomyosis uteri. Her diagnosis was G1P0
(0010) Abnormal Uterine Bleeding-A (Adenomyoma). Left Endometriosis TOTAL ABDOMINAL
External with Tubo-Ovarian Abscess by Frozen Section Biopsy with very Hypogastric pain
Causing more inflammation, HYSTERECTOMY WITH BILATERAL
scarring, adhesions, and
severe anemia secondary to Acute Blood Loss. The patient was later on endometriomas SALPINGO-OOPHORECTOMY
Dysmenorrhea (TAHBSO)
referred for surgical evaluation and co-management. Thus, the need for
surgical treatment.
Development of
Infertility
adhesions due to
inflammation
PREOPERATIVE ROLES OF THE NURSE:
1.Final preoperative teaching.
2.Explain to the mother that after a hysterectomy, the mother will no longer have periods or be able to become pregnant.
3.Assessment and communication of pertinent findings
4.Ensuring that records and reports are present and complete to accompany the patient to the OR.
5.It is important to verify the presence of a signed informed consent, laboratory and diagnostic data, a history and
physical examination, a record of any consultations, baseline vital signs, and completed nursing notes.
6.Site and side of the anticipated surgery will be identified and marked with an indelible marker and documented to
indicate agreement with the patient.
7.If the patient is an inpatient, ensure that the patient is ready and appropriately prepared for surgery.
8.If patient is an ambulatory surgical patient, the patient or caregiver will share the responsibility for preoperative
preparation.
9.Dress patient in hospital gown that is left untied and open in the back. Hospitals may require patients to wear a hospital
gown with no underclothes, whereas some surgical centers may allow patients to wear underwear, depending on the
surgical procedure performed.
10.Patient should not wear cosmetics. Also, nail polish and artificial nails should be removed.
11.Identification band should be identified or placed on the patient.
12.Cover patient?s hair completely with a disposable paper cap; if patient has long hair, it may be braided; hairpins are PREOPERATIVE NURSING DIAGNOSIS:
Anxiety r/t surgical procedure and outcome of surgery
removed.
13.Remove jewelry. If patient prefers not to remove wedding ring, the ring can be taped securely to the finger to prevent
loss. 1. Explain all activities, procedures, and issues that involve the patient; use nonmedical terms and calm,
14.All prostheses, including dentures, glasses, contact lenses, are generally removed to prevent loss or damage. slow speech. Do this in advance of procedures when possible and validate patient?s understanding.
2. Identify patient?s perception of the threat represented by the situation.
15.If electrocautery devices are to be used during surgery, jewelry in body piercings should be removed as a safety
3. Monitor physical responses (palpitation/rapid pulse, repetitive movements, pacing)
measure.
4. Observe how the patient uses coping techniques and defense mechanisms to cope with anxiety.
16.Hearing aids may be left in place to allow the patient to better follow instructions. 5. Use presence, touch (with permission), verbalization, and demeanor to remind patients that they are not
17.Encourage patient to void before preoperative medications are administered if the medications will interfere with alone and to encourage expression or clarification of needs, concerns, unknowns, and questions.
maintaining balance and increase risk of falling when ambulating to the bathroom. 6. Interact with patient in a peaceful manner.
18.Have patient empty bladder before transferring to the OR to prevent involuntary elimination under anesthesia and 7. Accept patient?s defenses: do not argue, dare or debate with them.
reduce the possibility of urinary retention during early postoperative recovery. 8. Encourage patient to acknowledge and to express feelings.
19.Administer preanesthetic medication as ordered and keep the patient in bed with side rails raised. Observe for any 9. Acknowledge patient?s anxiety or fear. Do not deny or reassure patient that everything will be all right.
untoward reaction to the medications. Keep the immediate surroundings quiet to promote relaxation. 10. Lessen sensory stimuli by keeping a quiet and peaceful environment.
20.Assist the patient in transferring from the hospital bed to the OR stretcher, raise the side rails, and ensure that the 11. If the situational response is rational, use empathy to encourage patient to interpret the anxiety
completed chart and any ordered preoperative equipment goes with the patient. symptoms as normal.
21.Responsible for the ?hand off? of communication to the nurse receiving the patient.
22.Caregiver should be shown where to wait for the patient during surgery.
INTRAOPERATIVE ROLES OF THE CIRCULATING NURSE:
1.Reviews anatomy, physiology, and surgical procedure.
2.Assists with preparing the OR.
3.Practices aseptic technique in all required activities.
4.Monitors practices of aseptic technique in self and others.
5.Ensures that needed items are available and sterile (if required).
6.Checks mechanical and electrical equipment and environmental factors
7.Identifies and admits patient to OR suite.
8.Assesses patient?s physical and emotional status.
9.Plans and coordinates intraoperative nursing care.
10.Checks chart and relates pertinent data.
11.Assists with transferring patient to OR bed and ensures patient safety in transferring and positioning patient.
12.Participates in insertion and application of monitoring devices. INTRAOPERATIVE NURSING DIAGNOSIS:
13.Assists with induction of anesthesia. Provide a vital communication link for the ACP to ancillary departments such as Risk for hypothermia r/t cool surgical environment
the laboratory or blood bank during the procedure.
14.Prepares the surgical site. 1. Monitor vital signs to obtain baseline data.
15.Monitors draping procedure. 2. Assess environmental temperature and modify as needed: providing warming and cooling blankets,
16.Documents intraoperative care. increasing room temperature.
17.Records, labels, and sends blood and tissue specimens to proper locations. 3. If possible, cover skin areas (legs, arms, head) outside of operative field.
18.Measures blood and fluid loss. 4. Remove wet clothing and prevent pooling of antiseptic solutions under client in the OR
19.Records amounts of medications, including local anesthetics. 5. Avoid the use of heat clamps or hot water bottles. Surface rewarming can lead to rewarming shock due
to surface vasodilation.
20.Coordinates all activities in room with team members and other health-related staff and departments.
6. Increase ambient room temperature at conclusion of procedure.
21.Counts sponges, needles, instruments, and small medical devices.
7. Apply warming blankets at emergence from anesthesia.
22.Accompanies patient to PACU. 8. Monitor temperature throughout intraoperative phase.
23.Reports information relevant to care of patient to PACU nurses.
24.Ongoing assessment of the patient is essential because the patient?s condition may change quickly.
POSTOPERATIVE ROLES OF THE NURSE:
1.Initial admission of the patient to the PACU.
2.Monitoring and managing respiratory and circulatory function, pain, temperature, and the surgical site.
3.Asses air exchange status and note patient?s skin color.
4.Verify patient?s identity.
5.Assess patient?s level of consciousness.
6.Asses patient?s vital signs (temperature, apical/heart rate, respiration, blood pressure, and pain) every 15 minutes.
7.Encourage patient to take deep breaths.
8.Monitor intake and output closely. POSTOPERATIVE NURSING DIAGNOSIS:
9.Assist in positioning patient in an appropriate position for him or her based on the location of incision site and Acute pain r/t surgical incision
presence of draining tubes.
10.Protect and ensure patent airway. 1. Assess patient?s vital signs.
2. Note patient?s age, weight, coexisting medical or psychological conditions, idiosyncratic sensitivity to
11.Maintain ventilation and circulation.
analgesics, and intraoperative course.
12.Monitor oxygen and level of consciousness. 3. Review intraoperative or recovery room record for type of anesthesia and medications previously
13.Prevent shock. administered.
14.Manage pain. 4. Evaluate pain regularly (every 2 hours noting characteristics, location, and intensity using 0-10 scale)
15.Prevent complications. emphasize patient?s responsibility for reporting pain/relief of pain completely.
16.Maintain patient safety. 5. Assess causes of possible discomfort other than operative procedure.
6. Reposition patient as indicated.
7. Provide additional comfort measures (backrubs, heat or cold applications)
8. Encourage use of relaxation techniques such as deep breathing exercises, guided imagery, visualization,
music, etc.
9. Document effectiveness and side and/or adverse effects of analgesia. Administer analgesics and other
postoperative drugs as prescribed by physician.
Damage to adjacent
Blood clots Hemorrhage Infection Depression Constipation Urinary retention
organs
Death
You might also like
- Nursing Care Plan On Creutzfeldt-Jakob DiseaseDocument7 pagesNursing Care Plan On Creutzfeldt-Jakob DiseaseUjean Santos Sagaral100% (1)
- NCP Skin IntegrityDocument3 pagesNCP Skin IntegrityAlfie Ayro50% (2)
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNo ratings yet
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDocument6 pagesAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasNo ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument2 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestNo ratings yet
- Impaired Physical Mobility: Date/ Time Focus DARDocument1 pageImpaired Physical Mobility: Date/ Time Focus DARMaria Chrislyn Marcos GenorgaNo ratings yet
- COLLEGE OF ST. JOHN - ROXAS Member: Association ofDocument6 pagesCOLLEGE OF ST. JOHN - ROXAS Member: Association ofCrisha Ann Billones BacutaNo ratings yet
- NCP Acute Pain Related To Presence of Postoperative Surgical IncisionDocument2 pagesNCP Acute Pain Related To Presence of Postoperative Surgical IncisionPebbles PangilinanNo ratings yet
- Impaired Physical Mobility...Document3 pagesImpaired Physical Mobility...Christy BerryNo ratings yet
- NCP 3Document3 pagesNCP 3Grae TaclobNo ratings yet
- NCP (Acute Pain)Document2 pagesNCP (Acute Pain)jennilois100% (1)
- Risk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.Document2 pagesRisk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.eleinsamNo ratings yet
- This Study Resource Was: Date/Time Focus Progress Note (D-A-R)Document1 pageThis Study Resource Was: Date/Time Focus Progress Note (D-A-R)Michelle Gliselle Guinto MallareNo ratings yet
- NCP ErDocument4 pagesNCP ErljarseniornNo ratings yet
- Drug-Study NCPDocument5 pagesDrug-Study NCPMURILLO, FRANK JOMARI C.No ratings yet
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanNo ratings yet
- Nursing Care for Surgical Incision HealingDocument2 pagesNursing Care for Surgical Incision HealingJrose CuerpoNo ratings yet
- Nursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationDocument2 pagesNursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationGrace MellaineNo ratings yet
- Pathophysiology of Uterine FibroidsDocument1 pagePathophysiology of Uterine FibroidsJurilyne Rose TundagNo ratings yet
- Nursing Care for Fracture PatientDocument2 pagesNursing Care for Fracture Patientbanyenye25No ratings yet
- Post-Op Wrist Pain ManagementDocument13 pagesPost-Op Wrist Pain ManagementJay Jay JayyiNo ratings yet
- SP CSDocument4 pagesSP CSKhan HansNo ratings yet
- NCP Modified Radical MastectomyDocument5 pagesNCP Modified Radical MastectomyIvan Jules P. PALMARESNo ratings yet
- NCP Con ConstipationDocument2 pagesNCP Con ConstipationChristine Marie Bucio OraizNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- 3011-1 - NCP & Drug Study - AMCDocument5 pages3011-1 - NCP & Drug Study - AMCAngie MandeoyaNo ratings yet
- Reaction Paper ERDocument1 pageReaction Paper ERVann Anthony FuentesNo ratings yet
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Don Mariano Marcos Memorial State University Nursing CaseDocument9 pagesDon Mariano Marcos Memorial State University Nursing CaseJoselyn M. LachicaNo ratings yet
- Assessing Nursing Diagnoses and Expected OutcomesDocument20 pagesAssessing Nursing Diagnoses and Expected OutcomesZamranosNo ratings yet
- Nursing Care Plan for Bronchial Asthma PatientDocument3 pagesNursing Care Plan for Bronchial Asthma PatientissaiahnicolleNo ratings yet
- NCP-Acute PainDocument2 pagesNCP-Acute PainMatt Reyes Del CastilloNo ratings yet
- Seizure NCPDocument2 pagesSeizure NCPChristine Dela CruzNo ratings yet
- DRUG-STUDY - BALLON, Karlo CDocument6 pagesDRUG-STUDY - BALLON, Karlo CMelinda Cariño BallonNo ratings yet
- Incomplete Spinal Cord Injury Nursing CareDocument6 pagesIncomplete Spinal Cord Injury Nursing CareTherese MargaretNo ratings yet
- COURSE OBJECTIVES or NursingDocument5 pagesCOURSE OBJECTIVES or NursingFil AquinoNo ratings yet
- Doctors Order LoveDocument4 pagesDoctors Order LoveAubrey Unique EvangelistaNo ratings yet
- Kardex: GCS: 12-13/15 (M:5, V:4-5, E:3)Document11 pagesKardex: GCS: 12-13/15 (M:5, V:4-5, E:3)Dienizs Labini TadenaNo ratings yet
- Daily MNGT Plan3Document4 pagesDaily MNGT Plan3Christian Apple Angwas GonzalesNo ratings yet
- NCP HemothoraxDocument3 pagesNCP HemothoraxMichael John F. NatividadNo ratings yet
- NCM 114 - NCPDocument3 pagesNCM 114 - NCPReysiela Mae ValinoNo ratings yet
- Date/Time Focus Progress NotesDocument2 pagesDate/Time Focus Progress Notesanna jean oliquianoNo ratings yet
- Normal Spontaneous DeliveryDocument11 pagesNormal Spontaneous DeliveryAyah GarciaNo ratings yet
- Ov Ov OvDocument15 pagesOv Ov OvHayyana Mae Taguba LadiaNo ratings yet
- Module 2Document2 pagesModule 2Duchess Juliane Jose MirambelNo ratings yet
- Nursing Care Plan for Cholelithiasis Patient Undergoing ECGDocument2 pagesNursing Care Plan for Cholelithiasis Patient Undergoing ECGJenny Ajoc0% (1)
- GERD and PUD Nursing CareDocument6 pagesGERD and PUD Nursing CareDexel Lorren ValdezNo ratings yet
- Resource Unit On Common Drugs (LRDR Rotation)Document37 pagesResource Unit On Common Drugs (LRDR Rotation)kiamoiNo ratings yet
- 13 Areas of Assessment FrejDocument3 pages13 Areas of Assessment FrejJoMa TuazonNo ratings yet
- Self Task For English Lesson Part 2THDocument1 pageSelf Task For English Lesson Part 2THistiningrum0% (1)
- DolcetDocument2 pagesDolcetmarc_hansen_1312No ratings yet
- NCP Proper - Obstructive JaundiceDocument8 pagesNCP Proper - Obstructive JaundiceWyen Cabatbat100% (1)
- NP4 Nursing Board ExamDocument7 pagesNP4 Nursing Board ExamNewb TobikkoNo ratings yet
- NCP Risk For InfectionDocument6 pagesNCP Risk For InfectionCazze SunioNo ratings yet
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNo ratings yet
- NCP Self Care DeficitDocument3 pagesNCP Self Care DeficitLeizel ApolonioNo ratings yet
- Schematic PDFDocument1 pageSchematic PDFAngela BarcebalNo ratings yet
- Breast Cancer Male Concept MapDocument1 pageBreast Cancer Male Concept MapJed ArominNo ratings yet
- Myoma PathoniixDocument1 pageMyoma PathoniixRendel FernandezNo ratings yet
- Thesis Jur ErbrinkDocument245 pagesThesis Jur Erbrinkgmb09140No ratings yet
- Samsung Mobile: Market Share & Profitability in SmartphonesDocument15 pagesSamsung Mobile: Market Share & Profitability in SmartphonesTanmay WadhwaNo ratings yet
- Ratio Method For Calculating A RatioDocument5 pagesRatio Method For Calculating A RatioFareeha KhanNo ratings yet
- On The Metres of Poetry and Related Matters According To AristotleDocument61 pagesOn The Metres of Poetry and Related Matters According To AristotleBart MazzettiNo ratings yet
- Spare Order 28.03Document27 pagesSpare Order 28.03Ankit AgarwalNo ratings yet
- TASK 9adhDocument5 pagesTASK 9adhAyan FaridiNo ratings yet
- ChatGpt For AccountantsDocument29 pagesChatGpt For Accountantssamreen khanNo ratings yet
- ART. Dworkin - in Praise of Theory PDFDocument16 pagesART. Dworkin - in Praise of Theory PDFmaiasilva70No ratings yet
- Skema Pppa Kimia k2 2014 (Set 1)Document10 pagesSkema Pppa Kimia k2 2014 (Set 1)Siva Guru0% (1)
- TFN RVWDocument145 pagesTFN RVWmftaganasNo ratings yet
- Readme P006Document7 pagesReadme P006paras99No ratings yet
- Fulbright-Hays Dissertation Research AbroadDocument8 pagesFulbright-Hays Dissertation Research AbroadHelpMeWriteMyPaperPortSaintLucie100% (1)
- Slingfox RC NotesDocument2 pagesSlingfox RC NotesgauravwordsNo ratings yet
- Batra, Kanika - Kipps, Belsey, and Jegede - Cosmopolitanism, Transnationalism, and Black Studies in Zadie Smith's On BeautyDocument15 pagesBatra, Kanika - Kipps, Belsey, and Jegede - Cosmopolitanism, Transnationalism, and Black Studies in Zadie Smith's On Beautyjen-leeNo ratings yet
- Sources of Strength For Mental Wellness by Sheryl Boswell, Youth Mental Health Canada (YMHC)Document11 pagesSources of Strength For Mental Wellness by Sheryl Boswell, Youth Mental Health Canada (YMHC)Youth Mental Health CanadaNo ratings yet
- Finale 2005b - (Holly Mass of ST Peter DamianDocument6 pagesFinale 2005b - (Holly Mass of ST Peter DamianArmelNo ratings yet
- Pre-Lab: Ahnaf Habib Khan 40079665 TJ-XDocument2 pagesPre-Lab: Ahnaf Habib Khan 40079665 TJ-XAhnafHabibKhanNo ratings yet
- Chapter5 EthDocument30 pagesChapter5 EthVictoriasecret PerfumeNo ratings yet
- Partner With Rittal: It's Easy To Become A Rittal PartnerDocument10 pagesPartner With Rittal: It's Easy To Become A Rittal PartnerBhanu Uday SinghNo ratings yet
- Admin Case DigestDocument8 pagesAdmin Case DigestlenvfNo ratings yet
- Concept of Peace in Peace Studies: A Short Historical SketchDocument14 pagesConcept of Peace in Peace Studies: A Short Historical SketchTrieu Huy HaNo ratings yet
- Curriculum Vitae: Radhey ShyamDocument3 pagesCurriculum Vitae: Radhey ShyamGaurav SinghNo ratings yet
- Injera Production and Export Business PlanDocument50 pagesInjera Production and Export Business PlanTumim84% (44)
- Secrets of The Knights Templar The Knights of John The BaptistDocument7 pagesSecrets of The Knights Templar The Knights of John The BaptistP NielsenNo ratings yet
- Republic Planters Bank Vs CADocument2 pagesRepublic Planters Bank Vs CAMohammad Yusof Mauna MacalandapNo ratings yet
- 05 AHP and Scoring ModelsDocument32 pages05 AHP and Scoring ModelsIhjaz VarikkodanNo ratings yet
- United Kindom: Stefan Casian, 5BDocument14 pagesUnited Kindom: Stefan Casian, 5BClaudia Ramona StefanNo ratings yet
- Target Mature Men with Luxury Watch MarketingDocument13 pagesTarget Mature Men with Luxury Watch MarketingAndriDwisondiNo ratings yet
- Labor 4th Construction in Favor of LaborDocument25 pagesLabor 4th Construction in Favor of LaborLiee RaineNo ratings yet
- Element Six v. Novatek Et. Al.Document26 pagesElement Six v. Novatek Et. Al.PriorSmartNo ratings yet