Professional Documents
Culture Documents
Jesena Procedure Study Week 3 1
Jesena Procedure Study Week 3 1
Uploaded by
Jesena SalveCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jesena Procedure Study Week 3 1
Jesena Procedure Study Week 3 1
Uploaded by
Jesena SalveCopyright:
Available Formats
VELEZ COLLEGE
COLLEGE OF NURSING
F. Ramos St. Cebu City
NURSING CARE MANAGEMENT 109 RLE:
Care of Mother and Child at Risk or With Problems (Acute and Chronic)
Procedure Study
Procedure Indications Contraindications Results and Nursing Considerations
Implications
OGT Feeding • Nutrition/feeding • Suspected/known Tube misplacement can • Mummy restraints
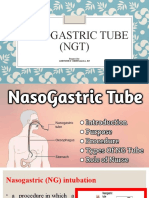
Nasogastric (NG) tubes or administration basilar skull fracture result in adverse patient effectively contain
Orogastric (OG) tubes are (prematurity, critical • Maxillofacial trauma outcomes including arms and legs
small tubes placed either illness, anatomic • The postoperative severe disability and without causing any
through the nose or the defects) period – any reinsertion death. These risks include: unwarranted
mouth and end with the tip • Medication of a gastric tube • Pneumonitis from pressure on infant
in the stomach. NG/OG tubes administration required following gastric feeds being • Measuring the tube
may be used for feedings, • Evacuation of recent deposited into the lungs ensures that it will be
medication administration, stomach contents • surgery to the mouth, • Intracranial insertion in long enough to enter
or removal of contents from pharynx, oesophagus or infant/child with base of the stomach. If a
the stomach via aspiration, stomach skull disruption tube is passed too
suction, or gravity drainage. • Known structural • Aspiration associated far, it will curl and
Procedure for insertion abnormality e.g. choanal with tube dislodgement end up in the
1. Loosely swaddle the atresia • Trauma to surrounding esophagus; if not
infant using a • Recent caustic ingestion tissues passed for enough it
mummy restraint • Suspected spinal injury • Pneumothorax will also be in the
2. Measure the space • Known or suspected • Spontaneous passage esophagus. Botha
from the infant’s oesophageal varices, through pylorus, causing can lead to aspiration
nose to earlobe to a chronic liver disease or feeding intolerance, in feeding.
point halfway liver failure abdominal pain, poor • Lubrication helps
between the xiphoid • Upper gastrointestinal absorption of medications tube pass the
process and stricture/oesophageal given via tube and esophagus without
umbilicus using a stricture /obstruction diarrhoea. trauma. Never use oil
no.8/no.10 feeding lubricants because it
tube. If infant is older • Suspected nasal, can pass the trachea
than 1 year, measure maxillary, oropharyngeal could lead to lipoid
from the bridge of the or oesophageal trauma pneumonia.
nose to the earlobe to • Suspected base of skull • Gentle pressure
xiphoid process. fractures helps to ensure
3. Mark the tube at the • Bleeding disorder. comfort and safety
measured point with • Assessing proper
a small clump or tape. placement helps to
Lubricate tip or ensure that the
catheter with water. feeding will enter the
4. Pass the catheter stomach, not the
with gentle pressure infant’s respiratory
to the point of clamp tract.
tape. If catheter is • Assessing stomach
passed to trachea content amounts
rather than aides in determining
esophagus, the infant if the previous
usually coughs and feeding was
becomes dyspneic. If absorbed. Replacing
this happens, stomach secretions
withdraws replace rather than
catheter. discarding them
5. Assess the catheter helps prevent
for position (confirm electrolyte loss.
that if it is nit in the • Elevating the infant’s
trachea) before upper body allows
administering the feeding to flow by
feeding using a bulb gravity.
syringe administer air • Elevating the infant’s
through the tubing upper body allows
and using a feeding to flow by
stethoscope gravity.
auscultate and listen • Excessive elevation
for gangling noise in can cause the
the xiphoid process. feeding to flow too
6. Aspirate stomach quickly, filling the
contents to assess esophagus and
amount if amount is increasing the risk for
small, replace it at the aspiration. Hurrying
beginning of feeding.
If large, replace it feeding by missing
through the tubing the plunger of then
and reduce the syringe or bulb
amount of feeding by attachment to add
amount. pressure that can
7. After being certain lead to aspiration.
that the catheter is in • Clamping the tube
the stomach, attach a before it is
syringe or special withdrawn is
feeding funnel to important to prevent
tube. Elevate the any milk remaining in
infants head and the tube from
chest slightly to flowing out and
encourage fluid to redness risk of
flow downwards to aspiration.
the stomach. • Flushing a tube helps
8. Flush water into the prevent clogging and
tube before adding plugging of the tube
feeding mixture. with feeding
9. Add specific kind and solution. Capping the
amount of feeding tube helps to prevent
prescribed to the air and bacteria from
syringe or funnel and entering.
allow it to flow by • Taping a tube to the
gravity into the forehead can put
infant’s stomach pressure on the
don’t elevate the anterior nan’s,
syringe end of the leading to ulceration.
tube more than 12 • Bubbling helps in
inches above the preventing air
infant’s abdomen. accumulation and
10. When the feeding has regurgitation of
passed through the feeding.
tube, reclamp the • Placing baby in this
tube securely and position helps the
gently and rapidly feeding solution
withdraws it. enjoy pyloric value,
11. If the tube is to be in promoting stomach
place flush it with 1-5 emptying.
ml of clear water and • Aids in outcome
cap it. evaluation.
12. If the tube is to be left
in place, tape it below
the nose and to the
cheek. Do not tape it
to the forehead.
13. Bubbly baby after
enteral feeding
14. Unswaddle and place
infant on right side
with head slightly
elevated or hold or
rack baby in this
position.
15. Assess infant comfort
References:
Wayne, G. (2018, December 29). Nasogastric Intubation: Insertion procedures & technique. Retrieved March 13, 2021, from https://nurseslabs.com/nasogastric-
intubation/#nursing_considerations
Farrington, M., Lang, S., Cullen, L., & Stewart, S. (2009). Nasogastric tube placement verification in pediatric and neonatal patients. Pediatric Nursing, 35, 17-24.
Marcdante, K. J., & Kliegman, R. (2019). Nelson essentials of pediatrics. Philadelphia, PA, 19103: Elsevier.
Jeffries, L., Ratoni, T., Roberts, D., Stevens, H., & Winskil, R. (2016). Infants and Children Insertion and Confirmation of Placement of Nasogastric and Orogastric
Tubes [Ebook] (1st ed., p. 1-16).
Dartford and Gravesham NHS Trust, 2007. Paediatric enteral feeding guidelines & operational policy (infants & children). 1st ed. p.1-13.
You might also like
- Neuropsychology Study Guide & Board Review (2014)Document666 pagesNeuropsychology Study Guide & Board Review (2014)pachozal100% (6)
- Gavage, Enteral Feeding or Tube Feeding. Placement May Be Temporary For TheDocument5 pagesGavage, Enteral Feeding or Tube Feeding. Placement May Be Temporary For TheWillen May Delopere Lomarda100% (1)
- Med Cert TemplateDocument1 pageMed Cert TemplateKatrizia Fauni50% (2)
- Fundamentals of NursingDocument40 pagesFundamentals of NursingCamille ParedesNo ratings yet
- Nasogastric Tubes/Gastric Decompression: Tube Position Visual Identification of The Tube NG TubeDocument6 pagesNasogastric Tubes/Gastric Decompression: Tube Position Visual Identification of The Tube NG Tubeemseph07No ratings yet
- Nasogastric Tube InsertionDocument62 pagesNasogastric Tube Insertionyhanne100% (22)
- Benign and Malignant Ovarian Tumors (Gynaecology)Document70 pagesBenign and Malignant Ovarian Tumors (Gynaecology)Dr Ali MehdiNo ratings yet
- NGT Ogt-FeedingDocument14 pagesNGT Ogt-Feedingnibbles nibblesNo ratings yet
- Imperforate AnusDocument17 pagesImperforate AnusNalzaro Emyril100% (1)
- Umbilical HerniaDocument19 pagesUmbilical HerniabonopazioNo ratings yet
- Nasogastric Tube (NGT)Document31 pagesNasogastric Tube (NGT)annyeong_123No ratings yet
- Elderly Care 101-NGT and PEGDocument92 pagesElderly Care 101-NGT and PEGBecky GalanoNo ratings yet
- Nasogastric Tube InsertionDocument18 pagesNasogastric Tube InsertionSandya PallapotuNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Congenital Anomalies of GiDocument94 pagesCongenital Anomalies of GiPadmaNo ratings yet
- Hearing-Impairment Case StudyDocument10 pagesHearing-Impairment Case StudyIrish Eunice Felix100% (1)
- NGT LavageDocument16 pagesNGT Lavageapi-3722454100% (4)
- Tube FeedingDocument55 pagesTube Feedingrhimineecat71No ratings yet
- Pyloric Stenosis: CLASS:-B.Sc. Nursing 3 YearDocument38 pagesPyloric Stenosis: CLASS:-B.Sc. Nursing 3 YearshikhaNo ratings yet
- NGT Feeding ChecklistDocument4 pagesNGT Feeding ChecklistCee Sanchez100% (6)
- Hirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshDocument48 pagesHirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshArchana Mahata100% (1)
- Regaining Bladder Control: For Incontinence on Exertion or Following Pelvic SurgeryFrom EverandRegaining Bladder Control: For Incontinence on Exertion or Following Pelvic SurgeryNo ratings yet
- NGT LavageDocument16 pagesNGT LavageTina Alteran100% (1)
- NGT Feeding and and CatherizationDocument9 pagesNGT Feeding and and Catherizationrussellnicoabendanabendan1234No ratings yet
- Day 12 - Ncm-109 7b InfancyDocument59 pagesDay 12 - Ncm-109 7b InfancySheena Patricia ArasulaNo ratings yet
- Congenital Gastrointestinal DisorderDocument7 pagesCongenital Gastrointestinal DisorderDONA, Randel John T.No ratings yet
- Ncm116 Skills LabDocument17 pagesNcm116 Skills LabMarie Isabelle HerveraNo ratings yet
- Enteral Nutrition: Course OutlineDocument3 pagesEnteral Nutrition: Course OutlineAngeli IdrisNo ratings yet
- Common Neonatal Surgical Conditions: Intensive Care Nursery House Staff ManualDocument6 pagesCommon Neonatal Surgical Conditions: Intensive Care Nursery House Staff ManualSayf QisthiNo ratings yet
- Jose, Leana Louisse D. BSN 2B1 Title: Enteric Nutrition Care of The Mother and Child at Risk or With ProblemsDocument3 pagesJose, Leana Louisse D. BSN 2B1 Title: Enteric Nutrition Care of The Mother and Child at Risk or With ProblemsLiana Louisse JoseNo ratings yet
- TracheoesophagealDocument2 pagesTracheoesophagealLuigi GeduqueNo ratings yet
- Imperforate AnusDocument24 pagesImperforate AnusGrace EspinoNo ratings yet
- Pyloric StenosisDocument5 pagesPyloric StenosisfdgrgNo ratings yet
- HandoutDocument13 pagesHandoutshaneleenrNo ratings yet
- Nasogastric TubeDocument3 pagesNasogastric TubeFreddy PanjaitanNo ratings yet
- 24 Upper GIDocument61 pages24 Upper GIMahmoud AbuAwadNo ratings yet
- Assessment of The Pediatric PatientDocument12 pagesAssessment of The Pediatric PatientiskoriahNo ratings yet
- Ob2 Sas 19Document9 pagesOb2 Sas 19Ralph Louie ManagoNo ratings yet
- NCM 104 Rle Final TermDocument15 pagesNCM 104 Rle Final TermJiro Luis KatindigNo ratings yet
- 20 PediatricDocument31 pages20 PediatricMahmoud AbuAwadNo ratings yet
- Management of Prolapse: Preventive Conservativ e SurgeryDocument16 pagesManagement of Prolapse: Preventive Conservativ e Surgerysanjay kashyapNo ratings yet
- Cayabyab, Natasha Alaine E. BSN Iv-E2: Gastrointestinal Diseases Description Management Esophageal AtresiaDocument9 pagesCayabyab, Natasha Alaine E. BSN Iv-E2: Gastrointestinal Diseases Description Management Esophageal AtresiaNatasha Alaine E. CayabyabNo ratings yet
- (Aganglionic Megacolon) : Hirschsprung'S DiseaseDocument2 pages(Aganglionic Megacolon) : Hirschsprung'S DiseaseLalisaM ActivityNo ratings yet
- Enteral Tube Feeding in Adults: Continuing Medical EducationDocument6 pagesEnteral Tube Feeding in Adults: Continuing Medical EducationMaca GallardoNo ratings yet
- Gavage Feeding 2Document10 pagesGavage Feeding 2Tiffany AdriasNo ratings yet
- Handout # 10 Part 4Document5 pagesHandout # 10 Part 4Ram AugustNo ratings yet
- Shoulder Dystocia NCPDocument6 pagesShoulder Dystocia NCPNicole Genevie MallariNo ratings yet
- Imperforate Anus: Preoperative CareDocument2 pagesImperforate Anus: Preoperative CareLalisaM ActivityNo ratings yet
- 1 s2.0 S2213576613000110 MainDocument3 pages1 s2.0 S2213576613000110 MainAria Andhyka YudhadiNo ratings yet
- Colombo, J. M., Wassom, M. C., & Rosen, J. M. (2015) - Constipation and Encopresis in Childhood. Pediatrics in ReviewDocument13 pagesColombo, J. M., Wassom, M. C., & Rosen, J. M. (2015) - Constipation and Encopresis in Childhood. Pediatrics in ReviewJorge Mario LujanNo ratings yet
- Topics Pediatric SurgeryDocument6 pagesTopics Pediatric SurgeryPatrycjaSkierkaNo ratings yet
- Second Stage of LaborDocument25 pagesSecond Stage of LaborAna67% (6)
- Delivery Room ProcedureDocument5 pagesDelivery Room ProcedureAparicio, Samantha Nicole D.No ratings yet
- Pediatrics (Inguinal Hernia)Document2 pagesPediatrics (Inguinal Hernia)fathima7910No ratings yet
- Nutrition Review: Dysphasia Enteral Tube FeedingDocument31 pagesNutrition Review: Dysphasia Enteral Tube Feedingcharm4991No ratings yet
- Hydramnios or PolyhydramniosDocument4 pagesHydramnios or PolyhydramniosAngel MoncadaNo ratings yet
- Intestinal Atresia: A Case ReportDocument3 pagesIntestinal Atresia: A Case ReportOvamelia JulioNo ratings yet
- NGT Procedure With RationaleDocument4 pagesNGT Procedure With Rationaleyuuki konnoNo ratings yet
- Hirsch SprungDocument3 pagesHirsch SprungBheru LalNo ratings yet
- Colic SyndromeDocument4 pagesColic SyndromeKenneth UbaldeNo ratings yet
- Percutaneous Gastrostomy: EndoscopicDocument3 pagesPercutaneous Gastrostomy: EndoscopicRaluca CondreaNo ratings yet
- Gavage Syringe or Funnel MethodDocument2 pagesGavage Syringe or Funnel MethodLea Jean Lobrigo OleaNo ratings yet
- Lavage Assisting With Gastric IntubationDocument3 pagesLavage Assisting With Gastric IntubationLea Jean Lobrigo OleaNo ratings yet
- Pyloric Stenosis: CLASS:-B.Sc. Nursing 3 YearDocument38 pagesPyloric Stenosis: CLASS:-B.Sc. Nursing 3 Yearshikha100% (1)
- Disease Prevention & ControlDocument23 pagesDisease Prevention & ControlNokatNo ratings yet
- Model Curriculum Handbook RadiotDocument157 pagesModel Curriculum Handbook RadiotYuda FhunkshyangNo ratings yet
- Mental Health in The Canadian Construction IndustryDocument14 pagesMental Health in The Canadian Construction IndustryTwinkle RamnialNo ratings yet
- 1 Anjeli Ratih Syamlingga Putri-DikonversiDocument10 pages1 Anjeli Ratih Syamlingga Putri-DikonversifirmianisaNo ratings yet
- The Culture of CrossFit. A Lifestyle Prescription For Optimal Health and Fitness (Inglés) Autor Steven KuhnDocument15 pagesThe Culture of CrossFit. A Lifestyle Prescription For Optimal Health and Fitness (Inglés) Autor Steven KuhnRosa Martin HuelvesNo ratings yet
- Water Treatment Plant Visit ReportDocument6 pagesWater Treatment Plant Visit ReportManmohan Singh Khadka100% (1)
- Beating ValentineDocument3 pagesBeating Valentinenitu roxanaNo ratings yet
- Theories of Growth and DevelopmentDocument3 pagesTheories of Growth and DevelopmentReyjan ApolonioNo ratings yet
- Handouts EIM SS1. Week 10Document1 pageHandouts EIM SS1. Week 10myco sauraNo ratings yet
- A Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDocument9 pagesA Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- The Philippine National Red Cross Valenzuela City Chapter: Nurses' Pad Ivteam Philippines HubDocument3 pagesThe Philippine National Red Cross Valenzuela City Chapter: Nurses' Pad Ivteam Philippines HubNoel100% (1)
- Name: Date: Grade: Week: Work Immersion Module 3: Safety in The WorkplaceDocument2 pagesName: Date: Grade: Week: Work Immersion Module 3: Safety in The WorkplaceGabrelle OgayonNo ratings yet
- DMH Long Quiz ReviewerDocument9 pagesDMH Long Quiz ReviewerKIM ABIGAIL ABAGNo ratings yet
- OTIFA External Newsletter Vol. 1 - 15 October 2018Document2 pagesOTIFA External Newsletter Vol. 1 - 15 October 2018Keisha Marsha TuffahatiNo ratings yet
- Test Bank For Nursing Research in Canada 3rd Edition Geri Lobiondo WoodDocument10 pagesTest Bank For Nursing Research in Canada 3rd Edition Geri Lobiondo WoodDonaldSmithwrmc100% (42)
- Malas Are The MetabolicDocument34 pagesMalas Are The MetabolicallenNo ratings yet
- RPMT 2011Document3 pagesRPMT 2011Prashant Kumar NeelratanNo ratings yet
- Health Econ 2013Document235 pagesHealth Econ 2013James SchneiderNo ratings yet
- Ammonium Chloride: Safety Data SheetDocument8 pagesAmmonium Chloride: Safety Data Sheetpippo2378793No ratings yet
- The Movie Patch AdamsDocument2 pagesThe Movie Patch AdamsPrincess TolentinoNo ratings yet
- Diabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: DiagnosisDocument1 pageDiabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: Diagnosislouglee9174100% (1)
- F4 CDPR 12-2-10Document167 pagesF4 CDPR 12-2-10Bonjack ReyesNo ratings yet
- A Review of Instruments Measuring Nurse-Physician CollaborationDocument10 pagesA Review of Instruments Measuring Nurse-Physician CollaborationMin MinNo ratings yet
- Nuremburg 2.0 in America - It Is Time: Renz LawDocument43 pagesNuremburg 2.0 in America - It Is Time: Renz LawJohn CokkrainNo ratings yet
- Tissue Salts Calc Fluor: DownloadDocument3 pagesTissue Salts Calc Fluor: DownloadDivyajyoti DevaNo ratings yet
- Useful Sources of InformationDocument28 pagesUseful Sources of InformationbobocmihailNo ratings yet