Professional Documents
Culture Documents
Hydramnios or Polyhydramnios
Uploaded by
Angel MoncadaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hydramnios or Polyhydramnios
Uploaded by
Angel MoncadaCopyright:
Available Formats
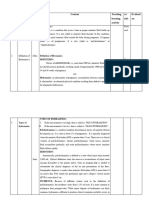
HYDRAMNIOS OR POLYHYDRAMNIOS MANAGEMENT:
• Is an excessive amount of amniotic fluid in the 1. Hospitalization if there is severe dyspnea
amniotic sac. and abdominal pain during ambulation.
• At 36 weeks of pregnancy there is usually about 2. Amniocentesis – removal of amniotic fluid
a liter of fluid present. to relieved maternal distress.
• The amount of amnioc fluid normally decreases 3. Indomethacin therapy – drug to decrease
after this time. fetal urine formation.
• The amount of amniotic fluid present is 4. Amniotomy – fluid is removed by a needle
controlled in part by fetal urination and inserted through the cervix.
swallowing. CLINICAL MANIFESTATION:
PATHOPHYSIOLOGY: 1.Excessive weight gain, dyspnea
2.Abdomen may be tense and shiny.
1. The etiology is often unknown 3.Edema of the vulva, legs and lower
2. Normal amniotic fluid volume at terms is extremities.
500 to 1,000 ml. , the volume in 4. Increased uterine size for gestational age
polyhydramnios exceed 2,000 ml. = usually accompanied by difficulty in
3. Anomalies causing impaired fetal palpating fetal parts and in auscultation of
swallowing or excessive micturition may fetal heart.
contribute to the condition. DIAGNOSTIC EVALUATION:
4. It is associated with maternal diabetes,
multiple gestation, Rh isoimmunization, 1..Present of amniotic fluid index of above
anomalies of the CNS including spina 25 cm.
bifida and anencephaly or anomalies in 2. Ultrasound evaluation will show large
the gastrointestinal tract including pocket of fluid between the fetus and
tracheoesophageal fistula. uterine wall or placenta.
Kind / Degree of Hydramnios: 3. Difficult to palpate fetal heart tone
4. Fundal height is above the age of
1. Mild Hydramnios = when amniotic fluid gestation.
pockets is between 8 to 11 cm in vertical COMPLICATION:
dimension. (85%)
2. Moderate Hydramnios – when amniotic 1.Premature labor and delivery
fluid pockets is between 12 to 15 cm 2.Postpartum hemorrhage due to uterine
vertical dimension. ( 17%) atony from gross distention of the uterus.
3. Severe Hydramnios = when amniotic fluid 3. Abruptio placenta
pockets is more than 16 cm in vertical 4. Cord prolapse
dimension. (5%) 5. malpresentation
Effects on Pregnancy: NURSING ASSESSMENT:
• Can cause fetal malpresentation due to 1. Evaluate maternal respiratory status
the additional uterine space and can 2. Inspect abdomen and evaluate uterine
allow the fetus to turn on a transverse lie height and compare with previous
• Can lead to premature rupture of the findings .
membranes from the increased pressure 3. Evaluate for abdominal pain, edema,
that can lead to risks for infection, varicosities of lower extremities and vulva.
prolapsed cord and preterm birth NURSING INTERVENTION:
Normal Process during Pregnancy:
1. Promoting effective Breathing
• Amniotic fluid is formed by a combination
a. Position to promote chest expansion
of the cells of the amniotic membrane
and from fetal urine with head elevated.
• It is evacuated by being swallowed by the
b. Provide oxygen by face mask if
fetus, absorbed across the intestinal
indicated
membrane into the fetal bloodstream and
transferred across the placenta
c. Limit activities and plan for frequent
• With polyhydramnios, accumulation of
rest period
amniotic fluid suggests difficulty with the
fetus’s ability to swallow or absorb fluid
d. Maintain adequate intake and
Causes of inability to swallow fluids:
output.
• Anencephalic
2. Promoting placental tissue perfusion and Oxygen to
• Fetus with tracheoesophageal fistula with
fetus
stenosis
• Fetus with intestinal obstruction a. Position pt. into side lying position, with
• Occurs among infant with diabetic mother head elevated
Causes: b. Encourage passive or active assisted
range of motion to the lower extremities.
1. Fetal abnormalities
c. Monitor FHR as directed and assess
2. Multiple pregnancy
abnormal FHR pattern: decreased or
3. Diabetes Mellitus
absent variability, tachycardia, prolonged, 2. Ultrasound – pockets of amniotic fluid are less
variable or late decelerations. than average
d. Provide good fluid intake and a diet
adequately in protein, iron and fluids. Effects on the fetus after birth:
e. Administer oxygen at 8 to 10 L/min. per
facemask • Muscles are weak due to cramped space
3. Promoting mobility during pregnancy
• Lungs fail to develop that can lead to
a. Assist woman with position changes and hypoplastic lungs- difficulty of breathing
ambulation • Potter syndrome- distorted features of the
b. Advise on alternating activity with rest face
periods for legs Causes:
c. Instruct woman to wear loose-fitting
clothing and low-heeled shoes with good 1.
Fetal Renal anomalies that results in
support. anuria.
4. Deceasing Anxiety 2. Premature rupture o membrane
3. Exposure to angiotensin converting
a.
Explain the cause of hydramnios if known. enzyme inhibitors.
b.
Encourage patient and family to ask MANAGEMENT:
question regarding any treatment or
procedure. 1. Observed newborn for complication
c. Encourage expression of feeling throughout the remainder of pregnancy.
d. Prepare patient for type of delivery 2. Clubfoot
e. Encourage presence of support person. 3. Amputation- due to adhesion of fetal parts
OLIGOHYDRAMNIOS to the amnion.
4. Abortion
• Is marked a decrease of amniotic fluid in 5. Fetal growth retardation
the amniotic sac.cord compression and 6. Abruptio placenta
fetal compromise may occur and lead to a 2. During labor and delivery
poor outcome.
• The infant will suffer from pulmonary a.
Cord compression
hypoplasia and skeletal abnormalities due b.
Fetal hypoxia as a result of cord
to a lack of fluid in the terminal air sac. compression
• Amniotic fluid less than 300 ml amniotic c. Prolonged labor.
fluid index of less than 5 cm. COMPLICATION:
• The abdomen appears too small for
gestational age. a. Umbilical Cord Compression
• New born of women with b. Passage of meconium
oligohydramnios have characteristic c. Fetal/ neonatal death
appearance of dry skin, leathery and NURSING INTERVENTION:
wrinkled.
Refers to a pregnancy with less than the average amount a. Evaluate fetal status by way of fetal
monitoring
of amniotic fluid.
b. Evaluate maternal vital sign for sign of
Part of the volume of amniotic fluid is formed by the infection, especially if oligohydramnios is
secondary to PROM.
addition of fetal urine, this reduced amount of fluid is
c. Assist with an amnioinfusion as indicated
usually caused by a bladder or renal disorder in the fetus
d. Inform health care provider of fetal
that is interfering with voiding compromise, assist woman to a side lying
position.
Another cause: due to growth restriction of the fetus,
Potter syndrome
he/she is not voiding as much as usual.
Nursing Consideration:
Diagnosis:
> Careful inspection among infants at birth to
rule out kidney disease and compromised
lung development
> Therapeutic Management:
1.Hospitalization or home care Goal:
a. .For adequate rest
b. For further evaluation
c. .To maintain adequate uteroplacental
circulation
d. To reduce pressure on the cervix and
prevent preterm labor
2. Advice woman to report any sign of ruptured
membranes or uterine contractions
1. Physical Assessment: Inspection: suspected
during pregnancy if the uterus fails to meet its 3. Advice woman to have high fiber diet and
expected growth rate consult her doctor for stool softener if diet is
ineffective-to prevent constipation and 1.Assess newborn for meconium aspiration
straining during defecation to prevent uterine
pressure > Establish and maintain patent airway
4. Monitor vital signs if in the hospital 2. Assess for polycythemia – due to decreased
5. Monitor presence of edema in the lower oxygenation in the final weeks
extremities
6. Amniocentesis – to remove excess some > hematocrit may be elevated due to polycythemia and
of the extra fluid dehydration that leads to lowered circulating plasma
7. Tocolytics- to prevent or halt preterm level.
labor
If preterm rupture of the membranes occurs: 3. Asess for hypoglycemia-because fetus had to
use stores of glycogen for nourishment in the
• Membranes can be “Needled” (insertion final weeks of intrauterine life
of a thin needle vaginally to pierce them) 4. Maintain an adequate temperature
to slow, control the release of fluid and to ➢ Newborn has low subcutaneous fats levels
prevent prolapsed cord during labor
• Assess infant after birth for gastrointestinal 5. Follow up care until at least school age to track
blockage. their developmental abilities
Postterm Pregnancy Care of the Woman:
• A term pregnancy is 38 to 42 weeks ➢ Allow woman to stay a longer period of time
• Any pregnancy that extends this period is with her newborn and let her or assist her in
postterm providing appropriate interventions to her
Causes: newborn
1. Women who have long menstrual cycle Rh Incompatibility
• 40 to 45 days: they do not ovulate on day Occurs when the mother is Rh negative and the
14 which is the normal period fetus is Rh positive
• They ovulate 14 days from the end of their
cycle, or on day 26 or 31, children will be Fetal blood and maternal blood are separate.
considered “late” by 12 to 17 days Sometimes accidental breaks in the placental villi
• Women who are receiving high dose of results in fetal blood entering the maternal
salicylates for their severe sinus
bloodstream.
headaches or rheumatoid arthritis- this
interferes with the synthesis of If the fetal blood is Rh negative and the maternal
prostaglandin
blood is Rh positive, the mother will recognize the
• Myometrial quiescence-uterus that does
fetal blood as foreign bodies and will produce
not respond to normal labor stimulation
antibodies against it. Only a few antibodies are
Danger to the fetus:
formed this way so that it usually does not affect the
1. Meconium aspiration first infant.
2. Macrosomia
3. Lack of growth-placenta is functioning for
only 40-42 weeks-exposes the fetus to
decreased blood perfusion, oxygen, fluid
and nutrients
Management:
1. Biophysical profile- to evaluate the placental
perfusion and amount of amniotic fluid present;
• if normal, it is assumed miscalculation
occurs
• If abnormal result or physical examination
or biparietal diameter on ultrasound
result the fetus is in term size, labor will be
induced
How to induce labor:
1. Prostaglandin gel or misoprostol–applied to • During placental separation a great amount of
the vagina to initiate uterine contraction maternal and fetal blood are mixed, causing
the mother to produced large amounts of
followed by an oxytocin infusion
antibodies during the first 72 hrs after placental
2. if oxytocin is ineffective, C/S is performed delivery. Since the infants is already delivered
at this time, the infant will not be affected.
Nursing Consideration during the labor process: • If the fetus is subsequent pregnancies is Rh
positive, the antibodies already present in the
1.Monitor FHR, V/S maternal blood stream will attack and destroy
the fetal red blood cells resulting in fetal
After Birth: anemia.
DIAGNOSIS IS MADE BY: 3. Provide good skin care because stool is
irritating to the skin.
a. Indirect Coomb’s test- presence of antibodies 4. Expect the urine to be dark colored
in maternal serum because of urobilinogen formation.
b. Direct Coomb’s test- presence of antibodies in
the fetal cord blood 5. Assess for dehydration by skin turgor
PREVENTION: identifying. Fluid loss may occur due
to heat from the fluorescent light
ADMINISTRATION OF Rh ( ANTI-D) GLOBULIN WITHIN above the infant.
THE FIRST 72 HRS AFTER DELIVERY TO WOMAN WHO: 6. Offer glucose water every 2 hrs to prevent
dehydration
1.Have delivered Rh positive fetus 7. 7. Maintain body temperature between 36
2.Have had untypeable pregnancies such as degree to 37 degree
ectopic pregnancies, stillbirth and 8. Infant should removed from the isolette
abortion. during feeding and eye patches
3. Have received ABO compatible Rh removed to allow interaction and
positive blood visual stimulation.
4. Have had invasive diagnostic procedure FETAL DEATH
such as amniocentesis.
ABO Incompatibility ONE OF THE MOST SEVERE COMPLICATION OF
PREGNANCY.
• Occurs when maternal blood type is O and
fetus is CAUSES FOR FETAL DEATH
TYPE A – MOST COMMON • CHROMOSOMAL ABNORMALITIES
• CONGENITAL MALFORMATION
TYPE B – MOST SERIOUS • INFECTIONS SUCH AS:
1. HEPATITIS B
TYPE AB - RARE 2. IMMUNOLOGIC CAUSES
3. COMPLICATION OF MATERNAL DISEASE
•
A and B antibodies are present in
Signs and Symptoms:
maternal bloodstream at birth so
hemolysis of fetal blood occur during the • Painless spotting
first pregnancy. • Uterine contractions with cervical
• The antibodies are the large Ig M type so effacement and dilatation
it does not cross the placenta during
• Fetus is born lifeless and emaciated
pregnancy.
Dx:
• During separation of the placenta
maternal blood mixes with fetal blood ➢ (-) fetal movement
resulting in antibodies of the mother ➢ (-) FHB
entering the bloodstream of the infant. ➢ Uterine growth ceases
These antibodies begin to hemolyze the ➢ Uterine size decrease
fetal RBC after birth. ➢ Fetal heart movement cannot be visualized by
MANAGEMENT FOR HD UTZ
➢ X-ray detected by the appearance of
• Suspension of breastfeeding during first 24 hrs intravascular or intra abdominal fetal gas
(Robert’s sign)
• – to prevent prenanediol
(breakdown product of progesterone excreted in
Management:
breastmilk) from interfering with the conjugation of
indirect bilirubin to direct bilirubin. 1. Induced labor- combination of
misoprostol (Cytotec) applied to the
PHOTOTHERAPY: vagina to effect cervical ripening and
oxytocin administration to begin uterine
1.
Destruction of RBC result in the formation contraction
of indirect bilirubin.
2. Blood studies: test for DIC
2. Phototherapy speeds up the maturation of
red blood cells - to prevent accumulation
of indirect bilirubin.
3. Uses of single quarts halogen lamp or a
bank of 4 to 8 cool white, day bright, or
special blue fluorescent lights positioned
12 to 30 inches above the infant.
NURSING CARE DURING PHOTOTHERAPY
1. Close eyes and cover with dressing
2. Expect the stool to loose and bright green
from excessive bilirubin excretion and skin
to be dark brown ( bronze baby
syndrome)
You might also like
- Case Simulation 118Document4 pagesCase Simulation 118Rica AvendañoNo ratings yet
- Anatomy and Physiology of Female For Cesarean SectionDocument8 pagesAnatomy and Physiology of Female For Cesarean SectionGrace Mellaine100% (1)
- Ateneo de Naga Nursing Students Study Case of Abruptio PlacentaDocument14 pagesAteneo de Naga Nursing Students Study Case of Abruptio PlacentaLexy Milante80% (10)
- Pathophysiology of Postpartum HemorrhageDocument2 pagesPathophysiology of Postpartum HemorrhageroxaynnnNo ratings yet
- 109Document3 pages109Angel MoncadaNo ratings yet
- Hydra Mi NosDocument8 pagesHydra Mi NosSudha DeviNo ratings yet
- PROBLEMS OF GESTATIONAL WEIGHTDocument11 pagesPROBLEMS OF GESTATIONAL WEIGHTODESSA GALOLONo ratings yet
- Chapter 23 ContinuationDocument7 pagesChapter 23 ContinuationArabelle GO100% (1)
- Polyhydramnios 10Document4 pagesPolyhydramnios 10hussain AltaherNo ratings yet
- HIGH RISK AND SICK MOTHER 5PsDocument16 pagesHIGH RISK AND SICK MOTHER 5Psbaracream.exeNo ratings yet
- POLYHYDRAMNIOSDocument4 pagesPOLYHYDRAMNIOSmohammed alkanani100% (1)
- HrpregnancyDocument13 pagesHrpregnancyAriane RegaladoNo ratings yet
- LP PolihidrDocument13 pagesLP PolihidrMas UupilNo ratings yet
- Inversion of The UterusDocument15 pagesInversion of The UterusRitamariaNo ratings yet
- 8 Priorities of Care for High-Risk NeonatesDocument30 pages8 Priorities of Care for High-Risk NeonatesregNo ratings yet
- MCN Report Polyhydramnios 1Document24 pagesMCN Report Polyhydramnios 1Vincent CuyucaNo ratings yet
- Reviewer in NCMDocument12 pagesReviewer in NCMtamsmadjad18No ratings yet
- 3 Each QDocument6 pages3 Each QShane PangilinanNo ratings yet
- Antepartum HaemorrhageDocument74 pagesAntepartum HaemorrhageApex College of Nursing100% (1)
- Nursing Care of Postpartum ComplicationsDocument13 pagesNursing Care of Postpartum ComplicationsLyca Mae AurelioNo ratings yet
- Puperium ComplicationDocument75 pagesPuperium Complicationvarshasharma05100% (1)
- MANAGEMENT OF HYDRAMNIOS AND OLIGOHYDRAMNIOSDocument12 pagesMANAGEMENT OF HYDRAMNIOS AND OLIGOHYDRAMNIOSEaster Soma HageNo ratings yet
- Ward TeachingDocument23 pagesWard Teachingvani reddyNo ratings yet
- Nursing Care of The Client With High-Risk Labor & DeliveryDocument10 pagesNursing Care of The Client With High-Risk Labor & DeliveryWilbert CabanbanNo ratings yet
- A Woman Who Develops A Complication of PregnancyDocument24 pagesA Woman Who Develops A Complication of PregnancyLady Jane CaguladaNo ratings yet
- Hydatidiform Mole OutlineDocument3 pagesHydatidiform Mole Outlineyxly imperialNo ratings yet
- Adiel Joy P. Calsa ASYNCHRONOUS ACTIVITY (WEEK 2 - 3)Document2 pagesAdiel Joy P. Calsa ASYNCHRONOUS ACTIVITY (WEEK 2 - 3)Adiel CalsaNo ratings yet
- Obstetrics Emergencies: By: Farah Mashitah Hafiz AdeebDocument96 pagesObstetrics Emergencies: By: Farah Mashitah Hafiz AdeebAriff MahdzubNo ratings yet
- Handouts of Complications of PostnatalDocument12 pagesHandouts of Complications of PostnatalAshish GuptaNo ratings yet
- Estabilizacion de PotrillosDocument6 pagesEstabilizacion de PotrillosCarlos Pedro VillaNo ratings yet
- Problems Related To Gestational WeightDocument15 pagesProblems Related To Gestational WeightJkimNo ratings yet
- Polyhydramnious and oligohydramnious: Causes, effects and managementDocument34 pagesPolyhydramnious and oligohydramnious: Causes, effects and managementEdward Munyaradzi KutsanziraNo ratings yet
- Prolonged Labor Complications and Fetal MalpositionsDocument9 pagesProlonged Labor Complications and Fetal Malpositionslarissedeleon100% (1)
- ArlineDocument16 pagesArlinearline beshraNo ratings yet
- Managing Pica, Polyhydramnios, Oligohydramnios, and Hyperemesis GravidarumDocument29 pagesManaging Pica, Polyhydramnios, Oligohydramnios, and Hyperemesis GravidarumKyle Ethan De la RiarteNo ratings yet
- Signs Indicating Possible Complications of PregnancyDocument6 pagesSigns Indicating Possible Complications of Pregnancygerald polopotNo ratings yet
- Definition: Related Diagnostic TestsDocument8 pagesDefinition: Related Diagnostic TestsQuinn Xylon VillanuevaNo ratings yet
- Puerperium and ManagementDocument38 pagesPuerperium and ManagementWadhha AlsenaidiNo ratings yet
- Changes in PregnancyDocument13 pagesChanges in PregnancyZarlyn MirafloresNo ratings yet
- Changes in PregnancyDocument13 pagesChanges in PregnancyZarlyn MirafloresNo ratings yet
- Breech DeliveryDocument35 pagesBreech Deliverytam mei100% (1)
- Complications during labor and deliveryDocument16 pagesComplications during labor and deliveryEden NatividadNo ratings yet
- Protocol:: Rachel TwelmeyerDocument5 pagesProtocol:: Rachel Twelmeyerapi-384858632No ratings yet
- Labor Process and Nursing Care GuideDocument9 pagesLabor Process and Nursing Care GuideMary Florence VelardeNo ratings yet
- Puerperum Notes 1Document7 pagesPuerperum Notes 1Google SecurityNo ratings yet
- Multiple PregnancyDocument26 pagesMultiple PregnancyRaj PatelNo ratings yet
- Examining the Pregnant AbdomenDocument6 pagesExamining the Pregnant AbdomenArvind SeecharanNo ratings yet
- Amniotic FluidDocument29 pagesAmniotic FluidZeytun AbdullahiNo ratings yet
- Problems With The PassageDocument13 pagesProblems With The PassageMaria Theresa BuscasNo ratings yet
- Maternal High Risk Factors (High Risk Pregnancies)Document20 pagesMaternal High Risk Factors (High Risk Pregnancies)Charmy UbiñaNo ratings yet
- Displacement of The UterusDocument32 pagesDisplacement of The UterusRaja100% (1)
- Abruptio Placentae Nursing Care PlanDocument10 pagesAbruptio Placentae Nursing Care PlanLizabell TumlosNo ratings yet
- Online Skills Lab Pa of A Normal Pregnant Client Jamosmos 1 1Document12 pagesOnline Skills Lab Pa of A Normal Pregnant Client Jamosmos 1 1Aries BautistaNo ratings yet
- Placenta Previa Case StudyDocument5 pagesPlacenta Previa Case StudyKristine Castillo100% (2)
- Obstetric Emergencies 1Document38 pagesObstetric Emergencies 1bmukiri62No ratings yet
- Module 2 - Maternal TransesDocument6 pagesModule 2 - Maternal TransesCarl UyNo ratings yet
- MCN 2Document7 pagesMCN 2GabNo ratings yet
- Postpartum PeriodDocument4 pagesPostpartum PeriodMiccah Angjela UyNo ratings yet
- MCN ObDocument7 pagesMCN ObJoshua SaelNo ratings yet
- 2M Intrapartal Complications Written Report 109Document72 pages2M Intrapartal Complications Written Report 109kai xoxoNo ratings yet
- Review UNIT XI High Risk NewbornDocument20 pagesReview UNIT XI High Risk NewbornShehana ShihabNo ratings yet
- 2 Topics at RiskDocument5 pages2 Topics at RiskGeraldine PatayanNo ratings yet
- ABORTIONDocument3 pagesABORTIONAngel MoncadaNo ratings yet
- Diagnosing and Treating Ectopic PregnancyDocument14 pagesDiagnosing and Treating Ectopic PregnancyAngel MoncadaNo ratings yet
- Respiratory S-A (Sept. 6)Document37 pagesRespiratory S-A (Sept. 6)Angel MoncadaNo ratings yet
- Skeletal System Functions in 206 BonesDocument6 pagesSkeletal System Functions in 206 BonesAngel MoncadaNo ratings yet
- 109 Bleeding Disorder To DIC NotesDocument7 pages109 Bleeding Disorder To DIC NotesAngel MoncadaNo ratings yet
- NCM 109 High Risk PregnancyDocument8 pagesNCM 109 High Risk PregnancyAngel MoncadaNo ratings yet
- RS-2N Final Exam 2021-2022Document3 pagesRS-2N Final Exam 2021-2022Angel MoncadaNo ratings yet
- PharmaDocument4 pagesPharmaAngel MoncadaNo ratings yet
- Preventive ObstetricsDocument8 pagesPreventive ObstetricsAnn Merlin JobinNo ratings yet
- ETD Nicole Bourbonnais PDFDocument387 pagesETD Nicole Bourbonnais PDFJavier Castro ArcosNo ratings yet
- Prenatal Care Guide for Diagnosis, Exams, and MonitoringDocument43 pagesPrenatal Care Guide for Diagnosis, Exams, and Monitoringgayon09No ratings yet
- Incompetent CervixDocument20 pagesIncompetent CervixTiffany AdriasNo ratings yet
- STI College Nursing Program ExamDocument2 pagesSTI College Nursing Program ExamKarren FernandezNo ratings yet
- 18 - Oligohydramnios and PolyhydramniosDocument3 pages18 - Oligohydramnios and PolyhydramniosSu OoNo ratings yet
- Adolescencents Pregnanncy in Baranggay Kimadzil, Carmen, CotabatoDocument9 pagesAdolescencents Pregnanncy in Baranggay Kimadzil, Carmen, CotabatoRonnie OmarNo ratings yet
- Understanding Normal Lochia Flow After ChildbirthDocument2 pagesUnderstanding Normal Lochia Flow After Childbirthbing bongNo ratings yet
- Hormonal of Child BearingDocument249 pagesHormonal of Child BearingNorma JeepiNo ratings yet
- Scope and Standards of Maternal and Child Practice in The PhilippinesDocument33 pagesScope and Standards of Maternal and Child Practice in The PhilippinesSana ChanNo ratings yet
- Newborn AssessmentDocument12 pagesNewborn AssessmentstellaclarkNo ratings yet
- Leopold's Maneuvers: Assessing Fetal PositionDocument6 pagesLeopold's Maneuvers: Assessing Fetal PositionJoeyca Shien PiolNo ratings yet
- Ats Menjawab Super Brankas Soal Unas 2020-2015Document424 pagesAts Menjawab Super Brankas Soal Unas 2020-2015anton suponoNo ratings yet
- Prenatal Postpartum CareDocument4 pagesPrenatal Postpartum CareJamie PalmeriNo ratings yet
- Sistem Pengurusan Kualiti: Jadual Pengajaran TerperinciDocument3 pagesSistem Pengurusan Kualiti: Jadual Pengajaran TerperinciNurul IrhamnaNo ratings yet
- 1a. Obstetric Emergencies Koros E.KDocument225 pages1a. Obstetric Emergencies Koros E.KSalman KhanNo ratings yet
- Entry FormsDocument2 pagesEntry FormsMarlon FernandoNo ratings yet
- Cpy - Labour and PostnatalDocument16 pagesCpy - Labour and PostnatalSELVA S (DA2132311010011)No ratings yet
- Newborn AssessmentDocument4 pagesNewborn Assessmentapi-543734210No ratings yet
- Persalinan. Yogyakarta: Yayasan Essentia MedicaDocument2 pagesPersalinan. Yogyakarta: Yayasan Essentia MedicaYemimaNo ratings yet
- Fluid Electrolytes Bablance 150308Document17 pagesFluid Electrolytes Bablance 150308Laura ReyesNo ratings yet
- A Study of Maternal and Fetal Outcome in Antepartum HaemorrhageDocument4 pagesA Study of Maternal and Fetal Outcome in Antepartum HaemorrhagechairulNo ratings yet
- College of Our Lady of Mt. Carmel: Midwifery DepartmentDocument10 pagesCollege of Our Lady of Mt. Carmel: Midwifery DepartmentMA. JYRELL BONITONo ratings yet
- Chapter 2Document9 pagesChapter 2andro De PioNo ratings yet
- MCN Test DrillsDocument20 pagesMCN Test DrillsFamily PlanningNo ratings yet
- Badan UniformDocument21 pagesBadan UniformMahenthiranNo ratings yet
- International Journal of Health Sciences and ResearchDocument7 pagesInternational Journal of Health Sciences and ResearchTabrani. ZANo ratings yet