Professional Documents
Culture Documents
Bladder Cancer Basics
Uploaded by
Aziz Khalid0 ratings0% found this document useful (0 votes)
12 views1 pageBladder cancer is the most common tumor of the urinary tract. Smoking is the most well-established risk factor, causing 50-65% of cases in men and 20-30% of cases in women. Grading and staging are the most important prognostic factors, with high-grade and muscle-invasive tumors having the worst prognosis. Diagnosis involves instrumental tests like ultrasound and cystoscopy, though cystoscopy is necessary for diagnosis and ultrasound cannot detect carcinoma in situ. Biopsy during cystoscopy is recommended for abnormal-looking mucosa or normal mucosa with risk factors.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBladder cancer is the most common tumor of the urinary tract. Smoking is the most well-established risk factor, causing 50-65% of cases in men and 20-30% of cases in women. Grading and staging are the most important prognostic factors, with high-grade and muscle-invasive tumors having the worst prognosis. Diagnosis involves instrumental tests like ultrasound and cystoscopy, though cystoscopy is necessary for diagnosis and ultrasound cannot detect carcinoma in situ. Biopsy during cystoscopy is recommended for abnormal-looking mucosa or normal mucosa with risk factors.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views1 pageBladder Cancer Basics
Uploaded by
Aziz KhalidBladder cancer is the most common tumor of the urinary tract. Smoking is the most well-established risk factor, causing 50-65% of cases in men and 20-30% of cases in women. Grading and staging are the most important prognostic factors, with high-grade and muscle-invasive tumors having the worst prognosis. Diagnosis involves instrumental tests like ultrasound and cystoscopy, though cystoscopy is necessary for diagnosis and ultrasound cannot detect carcinoma in situ. Biopsy during cystoscopy is recommended for abnormal-looking mucosa or normal mucosa with risk factors.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
By María J.
Ribal , @MaríaJRibal
Head of Uro-Oncology Unit Hospital Clinic, Barcelona, Spain
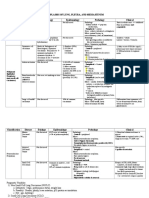
BLADDER CANCER (BC), BASICS
RISK FACTORS
EPIDEMIOLOGY SMOKING Most well-established risk factor (causing 50-65% of male cases and 20-30% of female cases)
The most common tumour of the urinary tract Incidence is directly related to the duration of smoking and the number of cigarettes per day
More frequent in men and Caucasians Decrease in the risk after smoking cessation (40% within one to four years, 60% after 25 years)
4th for incidence and 8th for mortality in American man AROMATIC Occupational exposure (dyes, rubbers, textiles, paints, leathers, chemicals)
Maximum incidence after 55 years AMINES Risk significantly greater after 10 years or more of exposure
Mean latency period usually exceeds 30 years
WHO CLASSIFICATION 2016 SCHISTOSOMA Second most common parasitic infection after malaria
HAEMATOBIUM Endemic in some regions (e.g., Egypt)
• Urothelial tumours (90%)
Related with squamous cell carcinoma
• Squamous cell neoplasm OTHERS Familiarity, cyclophosphamide, pioglitazone, radiotherapy
• Glandular neoplasm (e.g., adenocarcinoma)
• Neuroendocrine tumours (e.g., small cell carcinoma) TNM 2017
• Others: urachal carcinoma, tumours of Müllerian type, melanocytic tumours, Tx Primary tumour cannot be assessed
mesenchymal tumours, haematopoietic and lymphoid tumours, miscellaneous tumours T0 No evidence of primary tumour
Ta Non-invasive papillary carcinoma
GRADING AND STAGING Tis Carcinoma in situ (CIS)
Non-invasive Invasive T1 Tumour invades subepithelial connective tissue
T2 T2a - Tumour invades superficial muscle (inner half)
(Ta, T1, Tis) (T2, T3, T4)
T2b - Tumour invades deep muscle (outer half)
T3 T3a - Tumour invades perivesical tissue microscop.
High-grade T3b - Tumour invades perivesical tissue macroscop.
Flat (CIS) Papillary
(most)
T4 T4a - Tumour invades prostate stroma, seminal vesicles,
uterus or vagina
High-grade (by T4b - Tumour invades pelvic wall or abdominal wall
PUNLMP
definition) Nx Regional lymph nodes cannot be assessed
N0 No regional lymph node metastasis
N1 Metastasis in a single lymph node in the true pelvis
Low-grade
(hypogastric, obturator, external iliac, or presacral)
N2 Metastasis in multiple regional lymph nodes in the true
pelvis (hypogastric, obturator, external iliac, or presacral)
High-grade
N3 Metastasis in common iliac lymph node(s)
M0 No distant metastasis
Grading and staging are the most important prognostic factors: high-grade and muscle-invasive tumours M1 M1a -Non-regional lymph nodes
M1b -Other distant metastases (lungs, liver, bones)
have the worst prognosis!
CLINICAL PRESENTATION BIOPSY DURING CYSTOSCOPY
MACROHAEMATURIA is the most frequent sign
- Abnormal-looking mucosa
ASSOCIATED STORAGE LUTS should suggest CIS
URINARY OBSTRUCTION and PELVIC PAIN may appear in advanced cases
- Normal-looking mucosa in selected cases (positive
Tumour may be ASYMPTOMATIC and accidentally diagnosed with ultrasound cytology, history of HG tumours, tumours with non-
papillary appearance). In these cases, mapping biopsies
DIAGNOSIS (trigone, bladder dome, right, left, anterior and posterior
INSTRUMENTAL AND LABORATORY TESTS FOR DIAGNOSIS bladder wall) should be performed. Fluorescence-guided
ULTRASOUND First level examination in case of haematuria. It cannot detect CIS (PDD) biopsies should be performed if available.
- Prostatic urethra in selected cases (CIS is present or
CYSTOSCOPY Necessary for the diagnosis. It cannot be replaced by any other non-invasive test.
Flexible cystoscopy is preferable in men if available. A comprehensive description of the suspected, positive cytology without evidence of tumour in
tumour and the use of a bladder diagram are recommended. CIS can present as a velvet-like, the bladder, visible abnormalities of the prostatic urethra).
reddish area, indistinguishable from inflammation, or it may not be visible at all! Resection loop should be used.
URINARY CYTOLOGY Useful to detect high-grade tumours (e.g., CIS). High sensitivity in high-grade tumours (84%),
but low sensitivity in low-grade tumours (16%). Specificity exceeds 90%.
Three consecutive samples can increase sensitivity. Paris system for cytology reporting. Morning
urine not suitable for cytolysis
CT UROGRAPHY In selected cases (e.g., tumours located in the trigone, multiple- or high-risk tumours) TREATMENT
TURB
Indicated for non-muscle-invasive tumours to reduce recurrence rate (RR).
Non-muscle- INTRAVESICAL Single instillation of Mitomycin C reduces the RR in low-risk patients
Muscle-invasive ADJUVANT Repeat Mitomycin C instillations reduce the RR in intermediate-risk patients
invasive
TREATMENT Repeat BCG instillations reduce the RR in intermediate-risk and high-risk patients.
Three-year maintenance is more effective than one year to reduce RR in patients with high-
risk tumours but not with intermediate-risk tumours
Staging
Indicated for T2-T4a, N0M0 tumours. Do not defer more than 3 months.
Risk Removal of bladder, regional lymph nodes regional, prostate and seminal vesicles in man,
stratification uterus ovaries and anterior part of the vagina in woman. Continent or non-continent urinary
Non-metastatic Metastatic diversion (type of urinary diversion does not affect oncological outcomes).
RADICAL CYSTECTOMY: gold standard treatment. Whether ORC or RARC, should be
Intravesical RADICAL performed only in high-volume centres (at least 10, preferably > 20, RCs hospital/per year.)
adjuvant
treatment CYSTECTOMY NEOADJUVANT CISPLATIN-BASED COMBINATION THERAPY FOR T2-T4A, CN0M0 TUMOURS.
Radical cystectomy Systemic ADJUVANT CISPLATIN-BASED COMBINATION THERAPY TO PATIENTS WITH PT3/4 AND/OR
NEOADJUVANT CT therapy
PN+ DISEASE IF NO NEOADJUVANT THERAPY WAS GIVEN.
Radical Palliative purpose for patients with T4b tumours.
cystectomy Multimodal Indicated for NON-MUSCLE-INVASIVE TUMOURS IN SELECTED CASES (BCG-refractory /
bladder-sparing unresponsive / relapsing tumours, highest-risk tumours)
therapy
MULTIMODAL Alternative for patients with T2N0M0 tumour unfit for cystectomy.
BLADDER-SPARING In a highly selected patient population, long-term survival rates of multimodality treatment
FOLLOW-UP THERAPY are comparable to those of early cystectomy.
TURB + RADIOTHERAPY + CHEMOTHERAPY
As a result of the risk of recurrence and progression, non-muscle- - FIRST-LINE TREATMENT FOR CISPLATIN-ELIGIBLE PATIENTS
invasive need for follow-up after TURB Use cisplatin-containing combination chemotherapy with GC, MVAC, preferably with G-CSF,
Duration: 5 years (low-risk) or lifetime (intermediate-to-high risk) HD-MVAC with G-CSF or PCG.
Do not offer carboplatin and non-platinum combination chemotherapy.
First cystoscopy at 3 months is an important prognostic indicator -FIRST-LINE TREATMENT IN PATIENTS INELIGIBLE (UNFIT) FOR CISPLATIN
• Low-risk: cystoscopy (3 months from TURB, 9 months from SYSTEMIC THERAPY Offer checkpoint inhibitors pembrolizumab or atezolizumab to PD-L1-positive patients.
previous cystoscopy, yearly until five years) Offer carboplatin combination chemotherapy if PD-L1 is negative.
• Intermediate-risk: individualized -SECOND-LINE TREATMENT
• High-risk: cystoscopy and urinary cytology (every 3 months for 2 Offer checkpoint inhibitor pembrolizumab to patients progressing during, or after, platinum-
based combination chemotherapy for metastatic disease. Alternatively, offer treatment
years, every 6 months until five years, yearly) + CT urography
within a clinical trial setting.
(yearly)
You might also like
- bb2 Chap7Document12 pagesbb2 Chap7NurRahmaMusdalifaNo ratings yet
- Soft Tissue Tumors: A Practical and Comprehensive Guide to Sarcomas and Benign NeoplasmsFrom EverandSoft Tissue Tumors: A Practical and Comprehensive Guide to Sarcomas and Benign NeoplasmsNo ratings yet
- URO 3 - Neoplasm in The Genitourinary TractDocument8 pagesURO 3 - Neoplasm in The Genitourinary TractHa Jae kyeongNo ratings yet
- Lungs Benign and MalignantDocument7 pagesLungs Benign and MalignantNestley TiongsonNo ratings yet
- L O C S F: IP ND RAL Avity Taging ORMDocument4 pagesL O C S F: IP ND RAL Avity Taging ORMalysonNo ratings yet
- Neoplasms of Lung, Pleura, and Mediastinum Classification Disease Etiology Epidemiology Pathology ClinicalDocument4 pagesNeoplasms of Lung, Pleura, and Mediastinum Classification Disease Etiology Epidemiology Pathology ClinicalMrSomnambululNo ratings yet
- Neoplasms of Lung, Pleura, and Mediastinum Classification Disease Etiology Epidemiology Pathology ClinicalDocument4 pagesNeoplasms of Lung, Pleura, and Mediastinum Classification Disease Etiology Epidemiology Pathology ClinicalMrSomnambululNo ratings yet
- Chapter 11Document10 pagesChapter 11sybico.xray.abadclinicNo ratings yet
- Pathology and Prognostic Determinants of Colorectal Cancer - UpToDateDocument1 pagePathology and Prognostic Determinants of Colorectal Cancer - UpToDateamanuelNo ratings yet
- Salivary Gland TumorsDocument16 pagesSalivary Gland Tumorsmaria del mar RoblesNo ratings yet
- Carcinoma of The LungDocument50 pagesCarcinoma of The LungTristen TanNo ratings yet
- Lung Ca Small Bx2 PDFDocument4 pagesLung Ca Small Bx2 PDFJose SirittNo ratings yet
- 13 AppendixDocument3 pages13 AppendixGibi SupitNo ratings yet
- Nose and Paranasal Sinus Tumours: United Kingdom National Multidisciplinary GuidelinesDocument8 pagesNose and Paranasal Sinus Tumours: United Kingdom National Multidisciplinary GuidelinesRidho RifhansyahNo ratings yet
- EENTDocument11 pagesEENTJohn Christopher LucesNo ratings yet
- TNM Ca de MamaDocument4 pagesTNM Ca de MamaacademiaNo ratings yet
- Urinary Bladder PathologyDocument16 pagesUrinary Bladder Pathologyv@r0_5No ratings yet
- Recto y Ano TraducidoDocument19 pagesRecto y Ano TraducidoJacqueline GómezNo ratings yet
- Chapter 4 - NasopharynxDocument13 pagesChapter 4 - Nasopharynxmaaddy001No ratings yet
- TracheaDocument90 pagesTracheaLpsuedjNo ratings yet
- Testicular Cancer: Basic InformationDocument3 pagesTesticular Cancer: Basic InformationAnonymous eF8cmVvJaNo ratings yet
- TNM - Classifications (1) : 1) UICC-TNM-classification of NETS According To Different Primary TumorsDocument2 pagesTNM - Classifications (1) : 1) UICC-TNM-classification of NETS According To Different Primary TumorsRiaNo ratings yet
- Patologi Tumor Sistim UrogenitalDocument29 pagesPatologi Tumor Sistim UrogenitalSiddiq Blackhell CakepNo ratings yet
- RCJ Finals - Non Epithelial Ovarian CaDocument4 pagesRCJ Finals - Non Epithelial Ovarian CaJohn Paulo Catacutan100% (1)
- Calarynx 130814125710 Phpapp01Document33 pagesCalarynx 130814125710 Phpapp01Wael ShamyNo ratings yet
- Breast Cancer UG Lecture 1Document60 pagesBreast Cancer UG Lecture 1Ribhav GuptaNo ratings yet
- Rect 2Document28 pagesRect 2Miruna GhigeanuNo ratings yet
- " Chest:: by Definition Malignant Tumor of The Lung Primary Its EtiologyDocument10 pages" Chest:: by Definition Malignant Tumor of The Lung Primary Its EtiologyAhmed GaberNo ratings yet
- Soft Tissue SarcomasDocument79 pagesSoft Tissue Sarcomasvinitha kattaNo ratings yet
- Thyroid Malignancy With MRNDDocument25 pagesThyroid Malignancy With MRNDRashma JosephNo ratings yet
- Lung Cancer: I Gede Ketut SajinadiyasaDocument81 pagesLung Cancer: I Gede Ketut Sajinadiyasadr.Dewi Shintaher100% (1)
- 27 Mediastinal and Other Neoplasms Part 2 Other Lung NeoplasmsDocument25 pages27 Mediastinal and Other Neoplasms Part 2 Other Lung NeoplasmsjimmyneumologiaNo ratings yet
- Tumor Laring DannyDocument31 pagesTumor Laring DannyCicha Aulia WardaniNo ratings yet
- SARCOMA Bimbingan KoasDocument41 pagesSARCOMA Bimbingan KoasWarung MamakNo ratings yet
- Female GUDocument18 pagesFemale GULauren LaMonicaNo ratings yet
- DR Sagar Rathod Drddwagh: Presented by GuideDocument1 pageDR Sagar Rathod Drddwagh: Presented by GuideSagarRathodNo ratings yet
- 298658Document44 pages298658Rohan GargNo ratings yet
- Management of Rhabdomyosarco MA: Presenter: DR Manas Dubey Moderator: DR Rakesh DhankharDocument64 pagesManagement of Rhabdomyosarco MA: Presenter: DR Manas Dubey Moderator: DR Rakesh DhankharRebuma MegersaNo ratings yet
- 3-3-08 KnudsonDocument27 pages3-3-08 KnudsonNurRahmaMusdalifaNo ratings yet
- MediastinumDocument38 pagesMediastinumAndreea RalucaNo ratings yet
- Askep CA Paru OkDocument70 pagesAskep CA Paru OkLisa KurniaNo ratings yet
- Oncology NursingDocument6 pagesOncology NursingreooooNo ratings yet
- DR 180114164748Document43 pagesDR 180114164748Hasnain ToheedNo ratings yet
- Imaging in Lung Cancer: Mashuri, Dr. SP - Rad., M.KesDocument54 pagesImaging in Lung Cancer: Mashuri, Dr. SP - Rad., M.KesmirzasullivanNo ratings yet
- CarcinomarectumDocument45 pagesCarcinomarectumHuzefa MemonNo ratings yet
- Presented By: Moderator: Dr. Vikas KumarDocument104 pagesPresented By: Moderator: Dr. Vikas KumarWorku KifleNo ratings yet
- CA M1 RVWR HshsDocument5 pagesCA M1 RVWR HshscharmiemabaoNo ratings yet
- Y1.6 Neoplasia - Malignant Tumors 2022 PDFDocument41 pagesY1.6 Neoplasia - Malignant Tumors 2022 PDFlina hossamNo ratings yet
- Tumors of The Testis: S. Vahidi M.DDocument21 pagesTumors of The Testis: S. Vahidi M.DsuciNo ratings yet
- Squamous Cell CarcinomaDocument5 pagesSquamous Cell CarcinomaNuman QureshiNo ratings yet
- 2010 TNM Staging Colorectal CADocument2 pages2010 TNM Staging Colorectal CAbubbrubb20063998No ratings yet
- Ca of The Respiratory System NCM 112 Cell Ab Final TopicsDocument95 pagesCa of The Respiratory System NCM 112 Cell Ab Final TopicsA. Lizette PabloNo ratings yet
- Rectal Cancer StagingDocument10 pagesRectal Cancer StagingI G. A. Ratna DewiNo ratings yet
- Oleh: DR - Hans Marpaung, SPB, FicsDocument75 pagesOleh: DR - Hans Marpaung, SPB, FicsIrma Julyanti PanggabeanNo ratings yet
- Carcinoma Rectum - Janak - NEWDocument74 pagesCarcinoma Rectum - Janak - NEWTowhidulIslamNo ratings yet
- Case ReportDocument8 pagesCase ReportPradhana FwNo ratings yet
- Family HistoryDocument24 pagesFamily HistoryMARY CLAIRE SUMILHIGNo ratings yet
- Staging Dan Tatalaksana CRDocument13 pagesStaging Dan Tatalaksana CRAyu AnggrainiNo ratings yet
- General Stages and TX of Malignant Cells? Naming TumorsDocument11 pagesGeneral Stages and TX of Malignant Cells? Naming TumorsRyan TurnerNo ratings yet
- Arellano University Senior High School DepartmentDocument3 pagesArellano University Senior High School DepartmentMia QuimsonNo ratings yet
- Disorders of Sexual DevelopmentDocument19 pagesDisorders of Sexual DevelopmentJoanne May100% (1)
- Acne VulgarisDocument58 pagesAcne VulgarisNargisNo ratings yet
- Pharmacology For Nurses A Pathophysiologic Approach 5th Edition Adams Test Bank 1Document34 pagesPharmacology For Nurses A Pathophysiologic Approach 5th Edition Adams Test Bank 1matthew100% (51)
- Support Individuals With Specific Communication NeedsDocument21 pagesSupport Individuals With Specific Communication NeedsRamona Lazurca100% (2)
- MDS Prosthodontics New CurriculumDocument54 pagesMDS Prosthodontics New CurriculumPriyanka GandhiNo ratings yet
- Obesity Research PaperDocument10 pagesObesity Research PaperPaige-Hill88% (16)
- 6 ParoDocument9 pages6 ParoDiana TanasaNo ratings yet
- Full Download Ebook PDF How Writing Works A Guide To Composing Genres PDFDocument41 pagesFull Download Ebook PDF How Writing Works A Guide To Composing Genres PDFpaul.medford293100% (41)
- 5.a. Health Is Wealth LectureDocument62 pages5.a. Health Is Wealth LectureYüshîa Rivás GōmëźNo ratings yet
- Etiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsDocument33 pagesEtiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsNatasya Ayusandra MahersaputriNo ratings yet
- A Project Report ON ''Stress Management'' IN: Master of Business Administration (SESSION 2016-2017)Document73 pagesA Project Report ON ''Stress Management'' IN: Master of Business Administration (SESSION 2016-2017)Sao PutNo ratings yet
- Rekam MedikDocument4 pagesRekam MedikRusmin NoryadinNo ratings yet
- Chapter 84 - Insomnia - Restless Nights and The Blue Moon Level IIDocument6 pagesChapter 84 - Insomnia - Restless Nights and The Blue Moon Level IIaleksme88No ratings yet
- Material Safety Data Sheet Organic Virgin Coconut OilDocument4 pagesMaterial Safety Data Sheet Organic Virgin Coconut OilIda Nur AiniNo ratings yet
- Peperiksaan Pertengahan Tahun 1/2021 Tingkatan 1: SMK Bukit Bandaraya Lorong Maarof, Bangsar, 59000 Kuala LumpurDocument10 pagesPeperiksaan Pertengahan Tahun 1/2021 Tingkatan 1: SMK Bukit Bandaraya Lorong Maarof, Bangsar, 59000 Kuala LumpurjayaselanNo ratings yet
- BRAP PAMET Biosafety Guidance On COVID 19 Testing For Laboratorians EDocument179 pagesBRAP PAMET Biosafety Guidance On COVID 19 Testing For Laboratorians EMM ReyesNo ratings yet
- Case 2 Acute Ischemic Stroke wk.6Document3 pagesCase 2 Acute Ischemic Stroke wk.6Nader AbdurasadNo ratings yet
- Clinical DeathDocument2 pagesClinical DeathIoNo ratings yet
- Emergency First Aid Made Easy Training PresentationDocument92 pagesEmergency First Aid Made Easy Training PresentationRyan-Jay AbolenciaNo ratings yet
- Risk For InfectionDocument5 pagesRisk For InfectionRochelle Corneta JoreNo ratings yet
- ACTIVITY 3: Lifestyle Self-AssessmentDocument5 pagesACTIVITY 3: Lifestyle Self-AssessmentJohn Lloyd SuizoNo ratings yet
- Swanson 2012Document6 pagesSwanson 2012Ramjan KhandelwalNo ratings yet
- Hancock County Needs Assessment 1Document20 pagesHancock County Needs Assessment 1api-622005669No ratings yet
- Previous Gate Questions: Reading ComprehensionDocument17 pagesPrevious Gate Questions: Reading Comprehensionअभिषेक सिंह पटेलNo ratings yet
- Covid 19 Letter To AwaremedDocument2 pagesCovid 19 Letter To AwaremedWMBF NewsNo ratings yet
- Long Covid in PediatricsDocument25 pagesLong Covid in PediatricsAC Vallester100% (1)
- Case 1 Block NBSSDocument13 pagesCase 1 Block NBSSRuswinata ApitoNo ratings yet
- 2 Bedside Case Discussion Evaluation SheetDocument1 page2 Bedside Case Discussion Evaluation Sheetمهند الرحيليNo ratings yet
- Material On Language and Disability PDFDocument25 pagesMaterial On Language and Disability PDFpriyankaNo ratings yet