Professional Documents
Culture Documents
Cognitive Behavior Therapy in The Posthospitalization Treatment of Anorexia Nervosa
Uploaded by
D 13 Risna KhoirunnisaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cognitive Behavior Therapy in The Posthospitalization Treatment of Anorexia Nervosa
Uploaded by
D 13 Risna KhoirunnisaCopyright:
Available Formats
Brief Report
Cognitive Behavior Therapy in the Posthospitalization
Treatment of Anorexia Nervosa
Kathleen M. Pike, Ph.D. Results: The group receiving nutritional counseling relapsed
significantly earlier and at a higher rate than the group receiv-
B. Timothy Walsh, M.D. ing cognitive behavior therapy (53% versus 22%). The overall
Kelly Vitousek, Ph.D. treatment failure rate (relapse and dropping out combined) was
significantly lower for cognitive behavior therapy (22%) than for
G. Terence Wilson, Ph.D. nutritional counseling (73%). The criteria for “good outcome”
Joy Bauer, M.S., R.D. were met by significantly more of the patients receiving cogni-
tive behavior therapy (44%) than nutritional counseling (7%).
Objective: This study provides what the authors believe is the Conclusions: Cognitive behavior therapy was significantly
first empirical evaluation of cognitive behavior therapy as a more effective than nutritional counseling in improving out-
posthospitalization treatment for anorexia nervosa in adults. come and preventing relapse. To the authors’ knowledge, these
data provide the first empirical documentation of the efficacy
Method: After hospitalization, 33 patients with DSM-IV anor- of any psychotherapy, and cognitive behavior therapy in partic-
exia nervosa were randomly assigned to 1 year of outpatient ular, in posthospitalization care and relapse prevention of adult
cognitive behavior therapy or nutritional counseling. anorexia nervosa.
(Am J Psychiatry 2003; 160:2046–2049)
A dult anorexia nervosa is associated with a high rate
of relapse (1–3), extreme morbidity, and a mortality esti-
The cognitive behavior therapy and nutritional counsel-
ing in this trial consisted of 50 individual sessions deliv-
mate of 5% per decade of follow-up (4). However, we know ered over the 1 year after hospitalization. The goals of both
of no empirical support for any intervention for adult an- interventions were maintenance and consolidation of
orexia nervosa. In the present study we assessed the effi- gains achieved on the inpatient unit, continued improve-
cacy of cognitive behavior therapy in the posthospitaliza- ment and recovery, and relapse prevention.
tion treatment of adult anorexia nervosa. Cognitive behavior therapy is widely implemented in
anorexia nervosa treatment; however, we have found no
Method empirical data for its application to adult anorexia ner-
vosa. Given the well-documented efficacy of cognitive be-
Patients were eligible to participate in this outpatient havior therapy for bulimia nervosa (5), in this study we
trial if they 1) successfully completed inpatient treatment evaluated a manual-based method (available on request
(defined as achievement of at least 90% of ideal body from Dr. Pike) consistent with recommendations specific
weight based on the 1959 Metropolitan Life Insurance Ta- to cognitive behavior therapy for anorexia nervosa (6).
bles for a minimum of 2 weeks, normalization of eating, Cognitive behavior therapy for anorexia nervosa focuses
and resolution of acute medical problems) and 2) lived on cognitive and behavioral features associated with the
within commuting distance of the hospital. During the re- maintenance of eating pathology and uses a schema-
cruitment period, 43 women met these eligibility criteria, based approach to address a range of issues related to self-
and 33 were randomly assigned to treatment. Of the 10 esteem, self-schema, and interpersonal functioning.
women who did not enter the study, four were referred to The nutritional counseling intervention was a manual-
long-term inpatient or day treatment programs because of based treatment (available on request from Dr. Pike) built
severe comorbid psychopathology, and six returned to on well-established principles of nutritional education
prehospitalization therapists. and food exchanges (7, 8). Nutritional counseling is
The 33 study participants were between the ages of 18 psychoeducational and supportive, and it focuses on spe-
and 45 years, had DSM-IV diagnoses of anorexia nervosa, cific dietary analyses and balanced meal planning. Nutri-
and had successfully completed inpatient hospitalization tional counseling was used as the comparison treatment
at New York State Psychiatric Institute. The study was ex- because, in the absence of scientifically established treat-
plained to potential participants, and written informed ment standards, it is a credible clinical intervention that is
consent was obtained at the time of random assignment a standard component of anorexia nervosa treatment (9).
to treatment. This study was approved by the New York Cognitive behavior therapy and nutritional counseling
State Psychiatric Institute institutional review board. were conducted by four doctorate-level licensed, experi-
2046 http://ajp.psychiatryonline.org Am J Psychiatry 160:11, November 2003
BRIEF REPORTS
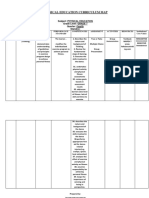
enced psychologists. The therapists in both modalities FIGURE 1. Survival Analysis of Time to Relapse for Patients
participated in extensive training and supervision and With Anorexia Nervosa Who Received 1-Year Posthospital-
ization Treatment With Cognitive Behavior Therapy or Nu-
met competency criteria, and all sessions were audio- tritional Counselinga
taped. Senior supervisors (G.T.W., K.V., and J.B.) evaluated
a portion of the tapes for integrity and adherence to treat- 1.0
Cumulative Proportion Without Relapse
ment protocols and conducted bimonthly supervision.
On-site supervision was conducted weekly.
0.8
The participants were randomly assigned to their treat-
ment conditions immediately before their first session in
the outpatient trial, which was scheduled within 1 week of 0.6
successful completion of hospitalization. Random assign-
ment to treatment condition was based on an adaptive 0.4
stratification procedure (10) to control for possible effects
of duration of illness (2), illness subtype (11), and medica-
tion status at time of discharge. Eighteen women were 0.2
Cognitive behavior therapy (N=18)
randomly assigned to cognitive behavior therapy, and 15 Nutritional counseling (N=15)
were assigned to nutritional counseling. 0.0
0 10 20 30 40 50
Study physicians met with the patients monthly to
monitor their medical condition. If treatment with antide- Session Number
a The patients receiving cognitive behavior therapy remained in
pressant medication was initiated in the hospital because
treatment significantly longer without relapsing (mean session=
of a continuing mood disorder despite weight restoration,
43.79, SD=2.9) than those receiving nutritional counseling (mean
it was continued throughout the outpatient trial and mon- session=27.21, SD=5.9) (log-rank statistic=8.39, p<0.004).
itored by the study physician. No psychopharmacological
interventions were initiated during the randomized trial. the mean numbers of previous hospitalizations were 1.8
Study participation was terminated if 1) the subject’s (SD=2.6) and 1.1 (SD=1.2), the mean body mass indexes at
weight fell below a body mass index of 17.5 kg/m2 (ap- evaluation were 16.0 (SD=2.1) and 15.2 (SD=1.5) kg/m2,
proximately 80% of ideal) for more than 10 days; 2) medi- the highest body mass indexes at the subjects’ current
cal status was compromised by exacerbation of anorexia heights were 22.1 (SD=3.8) and 21.1 (SD=2.6), and the low-
nervosa pathology to the extent that alternative, inpatient est body mass indexes at the current heights were 13.9
care was required (e.g., laxative overdose resulting in an (SD=2.4) and 14.4 (SD=1.4). The rates of the restricting
emergency hospitalization); or 3) exacerbation of non- subtype were 56% (10 of 18) and 40% (six of 15), respec-
eating-disorder psychopathology (e.g., attempted suicide) tively, and were not significantly different (χ2=0.79, df=1,
required alternative care. p<0.37).
At randomization and end of treatment, eating pathol- The patients receiving cognitive behavior therapy did
ogy was assessed by interview with the Eating Disorder not differ significantly (according to Mann-Whitney t
Examination (12). The complete Structured Clinical In- tests) from those receiving nutritional counseling on any
terview for DSM-IV Axis I Disorders (SCID) (13) was ad- of the four measures of treatment credibility or expect-
ministered at the prehospitalization evaluation. A modi- ancy: the mean scores for treatment logic were 11.18 (SD=
fied SCID was administered at randomization and end of 3.0) and 10.61 (SD=3.3) for cognitive behavior therapy and
treatment to assess current comorbid psychopathology. nutritional counseling, respectively. The mean scores for
Height and weight were measured at the time of initial
treatment relevance were 10.6 (SD=3.6) versus 10.0 (SD=
evaluation. Weight was measured weekly during the trial
2.8), the mean scores for expectation of success were 10.2
to calculate body mass index.
(SD=3.0) versus 11.6 (SD=2.5), and the mean scores for
At the end of session 1, four self-report questions about treatment response were 11.1 (SD=2.0) versus 11.7 (SD=
treatment credibility and expectancy were completed by 1.3) for cognitive behavior therapy and nutritional coun-
using a 15-point visual analogue scale. seling, respectively.
A Kaplan-Meier survival analysis (Figure 1) comparing
Results the time to relapse for the two treatment groups indicated
According to two-tailed t tests, the group receiving cog- a significant difference (long-rank statistic=8.39, p<0.004).
nitive behavior therapy did not differ significantly from Those receiving cognitive behavior therapy remained in
the group receiving nutritional counseling on any baseline treatment significantly longer without relapsing (mean
characteristic: the mean ages were 26.1 (SD=6.2) and 24.3 session=43.79, SD=2.9) than those receiving nutritional
(SD=6.9) years, respectively, the mean ages at illness onset counseling (mean session=27.21, SD=5.9).
were 17.4 (SD=5.2) and 16.5 (SD=3.1) years, the mean du- During the 1-year trial, the criteria for relapse were met
rations of illness were 7.6 (SD=5.9) and 7.3 (SD=5.8) years, by 53% of the patients in the nutritional counseling group
Am J Psychiatry 160:11, November 2003 http://ajp.psychiatryonline.org 2047
BRIEF REPORTS
(eight of 15) and 22% of those in the cognitive behavior ascertain whether medication appeared to affect outcome
therapy group (four of 18) (χ2=3.42, df=1, p<0.06). In the at this stage of treatment. A chi-square analysis of medica-
cognitive behavior therapy group, three women relapsed tion status by outcome status (“good” versus “fair,” “poor,”
because of weight loss and one relapsed because of both and “other” combined) was conducted for each treatment
weight loss and increased suicidality. In the nutritional condition. No significant medication effects were identi-
counseling group, five women relapsed because of weight fied for nutritional counseling (χ2=0.71, df=1, p<0.39). The
loss and three were referred to alternative care because of findings for cognitive behavior therapy suggested a medi-
severe depression, including active suicidal ideation in cation effect: seven of the eight patients who met the crite-
two participants. ria for good outcome were receiving medication, com-
In the survival analysis, individuals who voluntarily pared to four of the 10 who did not meet the criteria for
dropped out of treatment were not considered to have had good outcome (χ2=4.21, df=1, p<0.04).
relapses. The number of early dropouts, defined as pa- Chi-square analyses indicated that subtype did not have
tients who discontinued treatment before session 10, was a significant impact on outcome for the overall study (χ2=
higher for nutritional counseling (three of 15, 20%) than for 0.08, df=1, p<0.78) nor when examined by treatment con-
cognitive behavior therapy (N=0) (χ2=3.96, df=1, p<0.05). dition (cognitive behavior therapy: χ2=0.18, df=1, p<0.67;
nutritional counseling: χ2=0.71, df=1, p<0.39).
Overall treatment failure represents both individuals who
relapsed and those who dropped out of treatment within
the first 10 sessions. A chi-square comparison revealed a Discussion
significantly lower overall treatment failure rate for cogni- The findings from this study offer preliminary support
tive behavior therapy (22%, four of 18) than for nutritional for the use of cognitive behavior therapy in posthospital-
counseling (73%, 11 of 15) (χ2=8.62, df=1, p<0.003). ization treatment of adult anorexia nervosa. The group re-
A significantly higher percentage of individuals in the ceiving cognitive behavior therapy had lower dropout and
cognitive behavior therapy condition (44%, eight of 18) relapse rates and better overall clinical outcome than did
than in the nutritional counseling group (7%, one of 15) the comparison group receiving nutritional counseling
met modified Morgan-Russell criteria (1, 2) for “good out- combined with medical monitoring. We believe this to be
come” (χ2=5.89, df=1, p<0.02). However, a limitation of the first empirical documentation of therapeutic efficacy
these criteria is that they do not cover related psychologi- for any posthospitalization treatment for adult anorexia
cal and behavioral variables that are core criteria of anor- nervosa.
exia nervosa. As a result, an individual could meet the cri-
teria for good outcome but still be symptomatic in terms Received May 3, 2002; revisions received Aug. 9 and Nov. 22, 2002;
accepted April 14, 2003. Revised version of papers presented at the
of weight concerns, shape concerns, and eating behavior. Third International Congress of Neuropsychiatry, Kyoto, Japan, April
Following the practice in other studies (1, 3), we estab- 10–11, 2000, and the Ninth International Conference on Eating Dis-
lished an operational definition of “full recovery” by using orders, New York, May 4–7, 2000. From the Department of Psychia-
try, Columbia University College of Physicians and Surgeons. Address
the Eating Disorder Examination interview. Patients had reprint requests to Dr. Pike, Department of Psychiatry, Unit 98, Co-
to meet the criteria for good outcome and 1) eating atti- lumbia University, 1051 Riverside Dr., New York, NY 10032; kmp2@
tudes and weight concerns had to be less than one stan- columbia.edu (e-mail).
Supported in part by NIMH grant MH-01185 to Dr. Pike.
dard deviation above the mean of a comparison group The authors thank Laurel Mayer, M.D., Michael Devlin, M.D., Rachel
without eating disorders and 2) binge eating or purging Levy, Ph.D., Pamela Raizman, Ph.D., and Wendy Worth, Ph.D., for
behaviors had to be absent. These criteria for full recovery clinical contributions to this study and Andrew Leon, Ph.D., and
Laura Portera, M.S., for statistical consultation.
were met by 17% (three of 18) of the cognitive behavior
therapy group and none of the individuals in the nutri-
tional counseling group (χ2=2.75, df=1, p<0.10). References
At the time of random assignment, 17 participants were
1. Eckert ED, Halmi KA, Marchi P, Grove W, Crosby R: Ten-year fol-
taking antidepressant medication (fluoxetine: N=13, ven- low-up of anorexia nervosa: clinical course and outcome. Psy-
lafaxine: N=2, fluvoxamine: N=1, paroxetine: N=1). All chol Med 1995; 25:143–156
medications were initiated on the inpatient unit because 2. Russell GFM, Szmukler GI, Dare C, Eisler I: An evaluation of fam-
significant mood disturbance continued despite weight ily therapy in anorexia nervosa and bulimia nervosa. Arch Gen
Psychiatry 1987; 44:1047–1056
restoration, and four patients continued to meet criteria
3. Strober M, Freeman R, Morrell W: The long-term course of se-
for mood disorder despite medication. vere anorexia nervosa in adolescents: survival analysis of re-
The primary purpose of this clinical trial was not to ex- covery, relapse, and outcome predictors over 10–15 years in a
amine medication effects, so adaptive stratification proce- prospective study. Int J Eat Disord 1997; 22:339–360
4. Sullivan PF: Mortality in anorexia nervosa. Am J Psychiatry
dures accounted for medication status in the assignment
1995; 152:1073–1074
of patients to the treatment conditions. However, given
5. Fairburn CG: Cognitive behavioral therapy for bulimia nervosa,
that 17 of the 33 patients were taking medication during in Eating Disorders and Obesity. Edited by Fairburn CG,
the clinical trial, exploratory analyses were conducted to Brownell KD. New York, Guilford, 2002, pp 302–307
2048 http://ajp.psychiatryonline.org Am J Psychiatry 160:11, November 2003
BRIEF REPORTS
6. Garner DM, Vitousek K, Pike KM: Cognitive behavioral therapy 10. Friedman LM, Furberg CD, DeMets DL: Fundamentals of Clini-
for anorexia nervosa, in Handbook of Treatment for Eating Dis- cal Trials. Littleton, Mass, PSG Publishing, 1985
orders, 2nd ed. Edited by Garner DM, Garfinkel PE. New York, 11. Garner DM, Garner MV, Rosen LW: Anorexia nervosa “restrict-
Guilford, 1997, pp 94–144 ers” who purge: implications for subtyping anorexia nervosa.
7. Williams SR: Nutrition and Diet Therapy, 7th ed. St Louis, Int J Eat Disord 1993; 13:171–185
Mosby, 1993
12. Fairburn CG, Cooper Z: The Eating Disorder Examination, 12th
8. Sizer FS, Whitney EN: Hamilton and Whitney’s Nutrition Con-
ed, in Binge Eating: Nature, Assessment and Treatment. Edited
cepts and Controversies, 6th ed. St Paul, Minn, West Publishing,
1994 by Fairburn CG, Wilson GT. New York, Guilford, 1993, pp 317–
9. Beumont PJV: Nutritional management of anorexia and bu- 360
limia nervosa, in Eating Disorders and Obesity. Edited by 13. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clini-
Brownell KD, Fairburn GC. New York, Guilford, 1995, pp 306– cal Interview for DSM-IV Axis I Disorders (SCID). New York, New
313 York State Psychiatric Institute, Biometrics Research, 1994
Brief Report
Unipolar Mania Over the Course
of a 20-Year Follow-Up Study
David A. Solomon, M.D. Objective: Using data from a longitudinal study of the mood
disorders, the investigators address the phenomenon of unipo-
Andrew C. Leon, Ph.D. lar mania.
Jean Endicott, Ph.D. Method: Subjects diagnosed as having Research Diagnostic Cri-
William H. Coryell, M.D. teria mania at intake into the study were prospectively followed
for up to 20 years.
Timothy I. Mueller, M.D.
Results: Twenty-seven subjects had the diagnosis of unipolar
Michael A. Posternak, M.D. mania at the time they entered the study and had no history of
major depression before enrolling in the study. Seven of these
Martin B. Keller, M.D.
subjects did not suffer any episodes of major depression during
the 15- to 20-year follow-up.
Conclusions: These data support the diagnostic validity of
unipolar mania.
(Am J Psychiatry 2003; 160:2049–2051)
N early every study of unipolar mania has used retro-
spective methods. In the one prospective study of unipo-
tion. After the study was completely described to subjects, written
informed consent was obtained from all who participated.
lar mania to our knowledge that has been published (1), At intake into the study, current and past psychiatric history
were assessed with the Schedule for Affective Disorders and
the average length of follow-up was 5.6 years. Findings
Schizophrenia (2). Diagnoses were then made according to Re-
based on retrospective methods have led some authorities search Diagnostic Criteria (RDC) (3).
to question the existence of unipolar mania as a separate A total of 163 patients with bipolar I disorder entered the Col-
diagnostic entity. laborative Depression Study, including 14 who enrolled during an
episode of mania and who had no previous history of major or
minor depression. Sixty-six subjects with schizoaffective disorder,
Method mainly affective subtype, also entered the Collaborative Depres-
From 1978 to 1981, the NIMH Collaborative Depression Study— sion Study, and this group included 13 subjects who were experi-
a prospective, longitudinal, observational study of the mood encing an episode of mania and had no previous history of major
disorders—recruited individuals seeking treatment for major de- or minor depression. (Subjects with RDC-diagnosed schizoaffec-
pression, mania, schizoaffective mania, or schizoaffective depres- tive disorder, mainly affective subtype, were included in the
sion at five U.S. academic medical centers (in Boston, Chicago, present analyses because the RDC definition of schizoaffective
Iowa City, New York, and St. Louis). Inclusion criteria included age mania, mainly affective subtype [3], is nearly identical to the def-
of at least 17 years, IQ greater than 70, ability to speak English, inition of bipolar I mania in DSM-IV.)
white race (genetic hypotheses were tested), and no signs of a For the purposes of the present study, a minimum of 15 years of
mood or psychotic disorder secondary to a general medical condi- prospective follow-up was required for each subject. Follow-up
Am J Psychiatry 160:11, November 2003 http://ajp.psychiatryonline.org 2049
You might also like
- Kurdonia Structural Design ReportDocument341 pagesKurdonia Structural Design ReportAnonymous nQ9RqmNo ratings yet
- The Lucky Symbol of A Fish On The PalmDocument4 pagesThe Lucky Symbol of A Fish On The PalmANTHONY WRITER80% (5)
- Cognitive Behavioral Psychopharmacology: The Clinical Practice of Evidence-Based Biopsychosocial IntegrationFrom EverandCognitive Behavioral Psychopharmacology: The Clinical Practice of Evidence-Based Biopsychosocial IntegrationMark MuseNo ratings yet
- Costa, António Pedro, Luís Paulo Reis, António Moreira. 2019. (Advances in Intelligent Systems and Computing 861) Computer Supported Qualitative Research - New Trends On Qualitative Research-SpringerDocument330 pagesCosta, António Pedro, Luís Paulo Reis, António Moreira. 2019. (Advances in Intelligent Systems and Computing 861) Computer Supported Qualitative Research - New Trends On Qualitative Research-SpringerClarisse ReinfildNo ratings yet
- Leyte Department of Education Personal Development DocumentDocument2 pagesLeyte Department of Education Personal Development DocumentMaricar Cesista NicartNo ratings yet
- SUCCESSION CHAMP Notes (BALANE)Document91 pagesSUCCESSION CHAMP Notes (BALANE)carlee01483% (6)
- Complementary Therapies in Medicine: Matthew Krouwel, Amanda Farley, Sheila Greenfield, Tariq Ismail, Kate JollyDocument9 pagesComplementary Therapies in Medicine: Matthew Krouwel, Amanda Farley, Sheila Greenfield, Tariq Ismail, Kate JollyPhilippe MirasNo ratings yet
- Ethics and Social ResponsibilityDocument16 pagesEthics and Social Responsibilitypallavi50% (2)
- Effect of Sahaja Yoga Meditation On Quality of Lif PDFDocument9 pagesEffect of Sahaja Yoga Meditation On Quality of Lif PDFSwapnil RaautNo ratings yet
- Article Abt HypertensionDocument8 pagesArticle Abt HypertensionG HarshythaNo ratings yet
- CBT More Effective Than Nutrition Counseling for Anorexia RelapseDocument5 pagesCBT More Effective Than Nutrition Counseling for Anorexia RelapseAlexa AbendanoNo ratings yet
- Anorexia NervosaDocument4 pagesAnorexia NervosaFarida RahmaNo ratings yet
- Ensayo BMJDocument6 pagesEnsayo BMJoscuralizthNo ratings yet
- Does Mindfulness Improve Outcomes in Patients With Chronic PainDocument14 pagesDoes Mindfulness Improve Outcomes in Patients With Chronic Painiker1303No ratings yet
- Adherence With Psychotherapy and Treatment Outcomes With Psychogenic Nonepileptic SeizuresDocument6 pagesAdherence With Psychotherapy and Treatment Outcomes With Psychogenic Nonepileptic SeizuresNely M. RosyidiNo ratings yet
- A Randomized Controlled Trial of Medication and Cognitive-Behavioral Therapy For HypochondriasisDocument9 pagesA Randomized Controlled Trial of Medication and Cognitive-Behavioral Therapy For HypochondriasisDewina Dyani Rosari IINo ratings yet
- Sap 28 195Document9 pagesSap 28 195IntanAgustiFernandesNo ratings yet
- BMC Psychiatry: Non-Adherence To Antipsychotic Medication, Relapse and Rehospitalisation in Recent-Onset SchizophreniaDocument7 pagesBMC Psychiatry: Non-Adherence To Antipsychotic Medication, Relapse and Rehospitalisation in Recent-Onset SchizophreniaKamaruzzamanNo ratings yet
- A Multicenter CBT Vs ItpDocument8 pagesA Multicenter CBT Vs ItploloasbNo ratings yet
- Ger - Errington-Evans, Nick. (2015)Document5 pagesGer - Errington-Evans, Nick. (2015)Rafael ConcursoNo ratings yet
- Cairns 2006Document12 pagesCairns 2006David LorencNo ratings yet
- Federici 2007Document10 pagesFederici 2007Tomáš MartínekNo ratings yet
- Trastorno Límite ChenDocument10 pagesTrastorno Límite ChenGabyMaría DelValle Cordero Gómez ⃝⃤No ratings yet
- PDF on effects of community occupational therapyDocument22 pagesPDF on effects of community occupational therapyalwanNo ratings yet
- A Comparison of Osteopathic Spinal Manipulation With Standard Nejm199911043411903Document6 pagesA Comparison of Osteopathic Spinal Manipulation With Standard Nejm199911043411903Paola GuerraNo ratings yet
- Qigong Exercise For The Symptoms of Parkinson's Disease: A Randomized, Controlled Pilot StudyDocument6 pagesQigong Exercise For The Symptoms of Parkinson's Disease: A Randomized, Controlled Pilot StudySanta Maria PangaribuanNo ratings yet
- Resistance, early engagement and outcome in psychoanalytic psychotherapy of patients with psychosomatic disordersDocument11 pagesResistance, early engagement and outcome in psychoanalytic psychotherapy of patients with psychosomatic disordersMeykaNo ratings yet
- Jurnal Disfagia LagiDocument8 pagesJurnal Disfagia LagiNadewdewNo ratings yet
- Treatment For Eating DisordersDocument13 pagesTreatment For Eating DisordersPsihoterapeut Alina VranăuNo ratings yet
- Qigong Heroin Detox StudyDocument9 pagesQigong Heroin Detox StudyLaurentiu M.No ratings yet
- Nejmoa 2300184Document11 pagesNejmoa 2300184Hector RivasNo ratings yet
- ENERGY PSYCH THERAPY EVIDENCEDocument19 pagesENERGY PSYCH THERAPY EVIDENCElandburender100% (1)
- Effect of Sahaja Yoga Meditation On Quality of LifeDocument8 pagesEffect of Sahaja Yoga Meditation On Quality of LifeVladimir SutanovacNo ratings yet
- Clinical GuidelinesDocument34 pagesClinical GuidelinesAlberto PachecoNo ratings yet
- Ningalsri PDFDocument8 pagesNingalsri PDFCaesar CeblonkNo ratings yet
- Physiotherapy Improves Eating Disorders and Quality of Life in Bulimia and Anorexia NervosaDocument3 pagesPhysiotherapy Improves Eating Disorders and Quality of Life in Bulimia and Anorexia NervosaAzul MarinoNo ratings yet
- Clinical GuidelinesDocument34 pagesClinical GuidelinesSandro PerilloNo ratings yet
- Intervencionbueno FullDocument6 pagesIntervencionbueno FullfafiscribdNo ratings yet
- Predictors of Relapse in Chinese Schizophrenia Patients: A Prospective, Multi-Center StudyDocument7 pagesPredictors of Relapse in Chinese Schizophrenia Patients: A Prospective, Multi-Center StudyDhienWhieNo ratings yet
- Efficacy of Combined Cognitive Behavior Therapy and Hypnotherapy in Anorexia Nervosa A Case StudyDocument8 pagesEfficacy of Combined Cognitive Behavior Therapy and Hypnotherapy in Anorexia Nervosa A Case StudyCarol Rio AguirreNo ratings yet
- Jurnal JiwaDocument6 pagesJurnal JiwaoldDEUSNo ratings yet
- Rou Saud 2007Document11 pagesRou Saud 2007healliz36912No ratings yet
- Depression and TelepsychiatryDocument6 pagesDepression and TelepsychiatryMaria Von ShaftNo ratings yet
- velligan-et-al-2000-randomized-controlled-trial-of-the-use-of-compensatory-strategies-to-enhance-adaptive-functioning (1)Document7 pagesvelligan-et-al-2000-randomized-controlled-trial-of-the-use-of-compensatory-strategies-to-enhance-adaptive-functioning (1)Katerina ChatzNo ratings yet
- Copia de 09enero Sedacion Prot Vs No ProtDocument22 pagesCopia de 09enero Sedacion Prot Vs No ProtMartin LafuenteNo ratings yet
- Mind-Body Medicine Yang-Sheng 2012-05Document6 pagesMind-Body Medicine Yang-Sheng 2012-05Budo MediaNo ratings yet
- Cognitive Behavior Therapy For Schizophrenia 2006Document9 pagesCognitive Behavior Therapy For Schizophrenia 2006Patri SanchezNo ratings yet
- 007Document3 pages007Ed RibeiroNo ratings yet
- Safer Et Al 2001Document3 pagesSafer Et Al 2001Flavia DenisaNo ratings yet
- The Association Between Personality and Eating Psychopathology in Inpatients With Anorexia NervosaDocument8 pagesThe Association Between Personality and Eating Psychopathology in Inpatients With Anorexia NervosaDaniela Sánchez AcostaNo ratings yet
- Behavioural Intervention For Dysphagia in Acute Stroke A Randomised Controlled Trial PDFDocument7 pagesBehavioural Intervention For Dysphagia in Acute Stroke A Randomised Controlled Trial PDFmichelle montesNo ratings yet
- Evaluating Effect of Cognitive Behavioral Nursing On Quality of Life in Hemodialysis PatientsDocument4 pagesEvaluating Effect of Cognitive Behavioral Nursing On Quality of Life in Hemodialysis PatientsZiall MalikaNo ratings yet
- Physiotherapists' Pain Beliefs and Their Influence On Back Pain - Daykin2004Document13 pagesPhysiotherapists' Pain Beliefs and Their Influence On Back Pain - Daykin2004Paolo NavNo ratings yet
- Fluoxetine BulimiaDocument7 pagesFluoxetine BulimiaIroner'z Puroner'zNo ratings yet
- Standardized Vs Individualized Acupuncture For Chronic Back PainDocument8 pagesStandardized Vs Individualized Acupuncture For Chronic Back PainAHNo ratings yet
- 2011 - BBAT en Trastornos Alimentarios PDFDocument10 pages2011 - BBAT en Trastornos Alimentarios PDFMargarita CorreaNo ratings yet
- Adherencia Al Tratamiento de Crisis Funcionales DisociativasDocument7 pagesAdherencia Al Tratamiento de Crisis Funcionales DisociativasluciaNo ratings yet
- Content ServerDocument9 pagesContent ServerJohn SteplNo ratings yet
- Cognitivebehavioural Therapy V Structured Care For Medically Unexplained Symptoms Randomised Controlled Trial PDFDocument9 pagesCognitivebehavioural Therapy V Structured Care For Medically Unexplained Symptoms Randomised Controlled Trial PDFChica MirandaNo ratings yet
- 2011-Transdiagnostic Cognitive-Behavioral Therapy For Patients With Eating Disorders - A Two-Site Trial With 60-Week Follow-UpDocument18 pages2011-Transdiagnostic Cognitive-Behavioral Therapy For Patients With Eating Disorders - A Two-Site Trial With 60-Week Follow-UpRenata CarvalhoNo ratings yet
- 128 FullDocument9 pages128 FullAhtarunnisa Fauzia HanifaNo ratings yet
- Effectiveness of Acupuncture in The Treatment of Hyperemesis Gravidarum - A Systematic Review and Meta-AnalysisDocument14 pagesEffectiveness of Acupuncture in The Treatment of Hyperemesis Gravidarum - A Systematic Review and Meta-Analysiswiwit vitaniaNo ratings yet
- Take Charge Personality As Predictor of Recovery From Eating DisorderDocument6 pagesTake Charge Personality As Predictor of Recovery From Eating DisorderRokas JonasNo ratings yet
- Acupuncture For Acute Non-Specific Low Back Pain: A Pilot Randomised Non-Penetrating Sham Controlled TrialDocument9 pagesAcupuncture For Acute Non-Specific Low Back Pain: A Pilot Randomised Non-Penetrating Sham Controlled TrialArista AnggrainiNo ratings yet
- Psychological And Behavioral Treatment Of Insomnia UpdateDocument17 pagesPsychological And Behavioral Treatment Of Insomnia UpdateIta Punya ShintaNo ratings yet
- Integrative Headache Medicine: An Evidence-Based Guide for CliniciansFrom EverandIntegrative Headache Medicine: An Evidence-Based Guide for CliniciansLauren R. NatbonyNo ratings yet
- 1 SMDocument17 pages1 SMD 13 Risna KhoirunnisaNo ratings yet
- Procedure TextDocument4 pagesProcedure TextD 13 Risna KhoirunnisaNo ratings yet
- Virtual Classroom Kit by SlidesgoDocument61 pagesVirtual Classroom Kit by SlidesgoRogerNo ratings yet
- Depression Breakthrough - by SlidesgoDocument82 pagesDepression Breakthrough - by SlidesgoD 13 Risna KhoirunnisaNo ratings yet
- St. Mary'S University School of Graduate Studies: OCTOBER 2013, Addis Ababa, EthiopiaDocument88 pagesSt. Mary'S University School of Graduate Studies: OCTOBER 2013, Addis Ababa, EthiopiaRachel HaileNo ratings yet
- Kumpulan Soal SynonymDocument10 pagesKumpulan Soal SynonymMuhammad Abi PrasetyoNo ratings yet
- Contact Session Slides Rubber Manufacture, Processing and Value Addition - 2015Document27 pagesContact Session Slides Rubber Manufacture, Processing and Value Addition - 2015Chathura Thennakoon100% (1)
- Why Eye Is The Important Sensory Organ in Our LifeDocument3 pagesWhy Eye Is The Important Sensory Organ in Our LifeAljhon DelfinNo ratings yet
- Biography: Rex NettlefordDocument1 pageBiography: Rex NettlefordYohan_NNo ratings yet
- Geriatrics Trauma Power Point Presentation Dr. BarbaDocument23 pagesGeriatrics Trauma Power Point Presentation Dr. BarbagiscaamiliaNo ratings yet
- SCA No. 8220-R - Petitioner's MemorandumDocument9 pagesSCA No. 8220-R - Petitioner's MemorandumElizerNo ratings yet
- Leading culturally diverse global teamsDocument20 pagesLeading culturally diverse global teamsEdrick SoegiantoNo ratings yet
- Hedge Fund Modelling and Analysis Using Excel and VBA: WorksheetsDocument6 pagesHedge Fund Modelling and Analysis Using Excel and VBA: WorksheetsmarcoNo ratings yet
- Curriculum Vitae: About MyselfDocument5 pagesCurriculum Vitae: About MyselfRahat Singh KachhwahaNo ratings yet
- Question Bank Topic 1 Economic Thinking and Choice in A World of ScarcityDocument19 pagesQuestion Bank Topic 1 Economic Thinking and Choice in A World of ScarcityHide Yasu NakajimaNo ratings yet
- Physical Education Curriculum MapDocument20 pagesPhysical Education Curriculum MapdyonaraNo ratings yet
- Concrete Mix DesignDocument21 pagesConcrete Mix DesignIftikhar KamranNo ratings yet
- Right Triangle Activity For Quiz #2 - RetakeDocument4 pagesRight Triangle Activity For Quiz #2 - Retakeapi-16147700No ratings yet
- BCOM SyllabusDocument67 pagesBCOM SyllabusvjayarajuNo ratings yet
- l2 Unit 8 Statement of Aims Blank 2023 Templa 1Document8 pagesl2 Unit 8 Statement of Aims Blank 2023 Templa 1api-631701024No ratings yet
- MDBUSDocument20 pagesMDBUSjvaldiviesopNo ratings yet
- Born 1925 EngDocument30 pagesBorn 1925 EngFranz SchindlerNo ratings yet
- Un Ejercicio para 2º BACHILLERATO. (An Exercise For Advanced Students.)Document4 pagesUn Ejercicio para 2º BACHILLERATO. (An Exercise For Advanced Students.)Herber HerberNo ratings yet
- Four Theories of the Press - Libertarian vs AuthoritarianDocument8 pagesFour Theories of the Press - Libertarian vs Authoritarianআলটাফ হুছেইনNo ratings yet
- Understanding Balance of PaymentsDocument8 pagesUnderstanding Balance of PaymentsMurtaza JamaliNo ratings yet
- LP 3 Stylistics and DiscourseDocument12 pagesLP 3 Stylistics and DiscourseJonathan JaboyaNo ratings yet
- Philippines Supreme Court rules on robbery and double homicide caseDocument13 pagesPhilippines Supreme Court rules on robbery and double homicide caseNadzlah BandilaNo ratings yet
- Pem735 D00084 D XxenDocument6 pagesPem735 D00084 D XxenYigit SarıkayaNo ratings yet