Professional Documents
Culture Documents
Volume 10, No. 5 January 2020
Volume 10, No. 5 January 2020
Uploaded by
zoran cukovicOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Volume 10, No. 5 January 2020
Volume 10, No. 5 January 2020
Uploaded by
zoran cukovicCopyright:
Available Formats
Volume 10, No.
5 January 2020
This Medicines Information Leaflet is produced locally to optimise the use of medicines by
encouraging prescribing that is safe, clinically appropriate and cost-effective to the NHS.
The management of patients who are receiving oral therapy if they are regarded as at high risk of
anticoagulation with warfarin or a Direct Oral thrombosis (see table 1). The dose of dalteparin
Anticoagulant (DOAC e.g. dabigatran, rivaroxaban, recommended for bridging is outlined in table 2.
apixaban, edoxaban) who require surgery or are All patients who do not require bridging with full
undergoing a procedure depends on the underlying treatment dose heparin peri-operatively should be
thrombotic risk, the intended surgical intervention, risk assessed and given prophylactic dose LMWH as
and the risk of bleeding associated with it. This MIL appropriate.
covers the management of patients on warfarin or a
DOAC undergoing elective procedures, grouped into Table 1: Consider bridging with full treatment dose
three categories: major surgery (excluding vascular heparin in patients who stop warfarin if thrombotic
surgery), minor surgery and endoscopy. risk is high
Note: Patients within 3 months of acute venous Consider bridging with full treatment dose
thromboembolism (VTE) are at high risk of recurrent heparin in:
VTE if anticoagulation is stopped; it is estimated that VTE Patients with a VTE within previous 3
cessation of anticoagulation in the first month after months.
an acute VTE is associated with a 40% one-month
risk of recurrent VTE, and 10% for the subsequent Very high risk patients such as patients with
two months. Therefore, wherever possible elective a previous VTE whilst on therapeutic
surgery should be delayed until 3 months after an anticoagulation who now have a target INR
acute VTE. If this is not possible then please speak of 3.5.
with haematology (bleep 5529). AF Patients with a previous stroke/TIA in last
three months.
1) WARFARIN
Patients with a previous stroke/TIA and
a. Major surgery or procedure which requires
three or more of the following risk factors:
the INR to be normalised
Congestive cardiac failure
(i) Pre-operation Hypertension (greater than
For patients on warfarin the pre-operative 140/90 mmHg or on medication)
assessment team must liaise with the patient’s Age over 75 years
anticoagulation service (bleep 1857 for Oxfordshire Diabetes mellitus
patients). Warfarin should be stopped 5 days before MHV All Mechanical Heart Valve patients except
surgery.
those with a bileaflet aortic valve and no
The main decision is whether to give bridging other risk factors (AF, prior stroke or TIA,
therapy, with full treatment doses of low molecular hypertension, diabetes, congestive cardiac
weight heparin (LMWH) or, less commonly with failure or age over 75 years).
unfractionated heparin (UFH) once the INR is
subtherapeutic. Patients on warfarin for mechanical
heart valves (MHV), atrial fibrillation (AF) or for
treatment or prevention of venous
thromboembolism (VTE) are considered for bridging
Medicines Management and Therapeutics Committee January 2020
Oxford University Hospitals NHS Foundation Trust
2 Medicines Information Leaflet
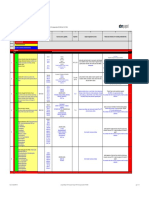
Table 2: Dose of dalteparin for bridging therapy Following major surgery, or procedure with high
bleeding risk, therapeutic anticoagulation with
Body weight (kg) Dose of dalteparin (units) LMWH should not be started until at least 48 hours
(pre-filled syringe) post procedure. Consider prophylactic dose LMWH
after surgery once haemostasis has been secured
Less than 46 7,500 once daily
until therapeutic anticoagulation can be
46-56 10,000 once daily reintroduced. Instruction for the provision of post-
57-68 12,500 once daily operative heparin is the responsibility of the
operating surgeon and should be documented in
69-82 15,000 once daily the patient notes.
83-98 18,000 once daily
Warfarin can be resumed, at the normal
99-112 10,000 twice daily maintenance dose, the evening of surgery or the
next day if there is adequate haemostasis, following
113-137 12,500 twice daily
discussion with the operating surgeon.
138-165 15,000 twice daily
b. Minor surgery or procedure with low bleeding
166 or more 18,000 twice daily
risk
There is no need to monitor the INR in patients who For some operations the surgeon may advise that
are at home for the 5 days before surgery. The last the INR need only be reduced (e.g. to 1.5‐2) for the
dose of warfarin should be taken on the evening of procedure in which case bridging anticoagulation
day -6. LMWH is started on the morning of day -3 may not be required. In these cases, the surgical
and is continued until day -1 (i.e. 24 hours before team should liaise with the anticoagulation service in
surgery). If the surgery poses a high risk of bleeding, good time to make necessary dose adjustments and
this final dose of LMWH on day -1 should only be half arrange an INR test the day before surgery as
the full anticoagulant dose. N.B. according to described above.
Oxfordshire Shared Care guidelines, supply of LMWH Some procedures, such as joint injections and
for patients who need bridging at home should come cataract surgery, can be carried out without
from the hospital. This should be discussed and interrupting warfarin therapy. However, the person
arranged during the pre-operative assessment. performing the procedure may advise that the INR is
In patients who are in hospital in the run up to reduced to 1.5‐2.
surgery and who are receiving bridging
anticoagulation with therapeutic dose UFH, heparin c. Gastrointestinal (GI) endoscopy in patients on
should be stopped 4-6 hours before surgery (discuss warfarin
timing with the operating surgeon). Refer to In general, low risk diagnostic procedures including
MIL vol.5 no.6 “Guidelines on when to use and how mucosal biopsy can be performed when the INR is up
to monitor unfractionated heparin in adults” for full to and including 3 without altering anticoagulation.
guidance on the use of UFH. For therapeutic procedures, the risk of post-
procedure bleeding is higher and reduction of
In all patients whose warfarin has been stopped 5
anticoagulation is preferred. However, there are no
days before surgery, the INR should be measured on
absolute rules and the risks and benefits should be
the day before surgery, allowing correction with oral
discussed with the patient prior to the procedure
phytomenadione (vitamin K) if it is greater than or
and an individual decision made.
equal to 1.5 (suggested dose 2mg). If correction with
phytomenadione is required, the INR should be If warfarin is stopped, it is safe to reinstate
re-checked on the morning of surgery. anticoagulation on the evening of the procedure
unless the endoscopist advises otherwise.
(ii) Post- operation/procedure The risk of thromboembolism and risk of bleeding
In patients undergoing a procedure which carries a after a procedure can be divided into high and low,
high risk of bleeding, the perioperative see table 3. The recommendations for action
anticoagulation depends on a balance between the following risk assessment are summarised below:
risk of bleeding and the risk of thrombosis.
Medicines Management and Therapeutics Committee January 2020
Oxford University Hospitals NHS Foundation Trust
3 Medicines Information Leaflet
High Risk Procedure Due to their short half-lives bridging with heparin is
Warfarin should be discontinued 5 days before the not required. Suggested periods for discontinuation
procedure. Bridging therapy with heparin (UFH or are in table 4. Note: eGFR is a reasonable guide to
LMWH) should be considered for high risk conditions GFR in most patients. However, in patients at
whilst the INR is subtherapeutic. No bridging is extremes of body weight a GFR should be should
needed if low risk condition. be calculated using the Cockcroft-Gault formula.
Low Risk Procedure
No change in anticoagulation is recommended unless Table 4: Discontinuation of DOACs for elective
the INR is greater than 3 either due to over- procedures
anticoagulation or a previously desired higher target Renal Function Low bleeding High bleeding
range. eGFR (ml/min) risk procedure risk procedure
Dabigatran
Table 3: Risk evaluation for GI endoscopic procedures 80 or more 24 hours 48 hours
Procedure Condition 50 to 79 24-48 hours 48-72 hours
High Risk Procedures High Risk Conditions
30 to 49 48-72 hours 96 hours
Polypectomy Prosthetic metal heart Dabigatran is not licensed for use with an eGFR below 30ml/min
ERCP with sphincterotomy valve in mitral position
Apixaban,
Ampullectomy Prosthetic heart valve and Rivaroxaban
AF and Edoxaban
EMR/ESD AF and mitral stenosis 30 or more 24 hours 48 hours
Dilation of strictures Less than 3 months after 15-29 48 hours 72 hours
Therapy of varices VTE Apixaban, rivaroxaban and edoxaban are not licensed for use with
PEG an eGFR below 15ml/min
EUS with FNA
Oesophageal, enteral or Following low bleeding risk procedures, treatment
colonic stenting dose anticoagulation can be recommenced once
Low Risk Procedures Low Risk Conditions haemostasis is secured, usually at 24 hours.
Diagnostic procedures +/- Prosthetic metal heart Following major surgery, or procedure with high
biopsy valve in aortic position bleeding risk, DOACs should not be re-introduced at
full dose until at least 48 hours post procedure.
Biliary or pancreatic Xenograft heart valve
stenting In patients with a high thrombosis risk it is
AF without valvular disease
Device-assisted appropriate to give prophylactic dose LMWH until it
Greater than 3months is safe to switch the patient back onto a DOAC:
enteroscopy without after VTE
polypectomy When using prophylactic LMWH, it should usually be
administered 6-12 hours post-surgery provided
haemostasis is secure. For high bleeding risk surgery
2) DOACs
(such as spinal and cranial surgery) prophylactic
The approach to the peri-operative or peri-
dalteparin should be delayed for 24-48 hours. LMWH
procedure management of patients on DOACs is
and DOAC should not overlap; they should be
based on an approximate calculation of the half-life
switched directly by giving the DOAC when the next
of the drug and so its persistence in the circulation,
dose of LMWH would have been due.
taking into account renal function. This is combined
with consideration of the bleeding risk of the
proposed procedure and a clinical evaluation of the References
patient’s individual risk factors for thrombosis and Douketis, J.D et al. (2015) Perioperative Bridging
bleeding. Current strategies for elective surgery do Anticoagulation in Patients with Atrial Fibrillation. N
not routinely include measurement of either non- Engl J Med, 373, 823-833.
specific or specific coagulation parameters to assist
in quantification of DOAC levels.
Medicines Management and Therapeutics Committee January 2020
Oxford University Hospitals NHS Foundation Trust
4 Medicines Information Leaflet
Keeling, D.M., et al. (2016). Peri-operative
management of anticoagulation and antiplatelet
therapy. Br. J. Haematol, 175, 602-613.
Spyropoulos, A.C et al, (2016) Periprocedural
management of patients receiving a vitamin K
antagonist or a direct oral anticoagulant requiring an
elective procedure or surgery. J Thromb Haemost,
14, 875-885.
Tafur A and Douketis J (2018) Perioperative
management of anticoagulant and antiplatelet
therapy. Heart 104, 1461-1467
Veitch, A.M., et al. (2016) Endoscopy in patients on
antiplatelet or anticoagulant therapy, including
direct oral anticoagulants: British Society of
Gastroenterology (BSG) and European Society of
Gastrointestinal Endoscopy (ESGE) guidelines. Gut,
65, 374-389.
Prepared by:
Susie Shapiro, Consultant Haematologist and Vicki
Price, Lead Anticoagulation Pharmacist
With advice from: Anticoagulation Team
Review date: Jan 2023
Medicines Management and Therapeutics Committee January 2020
Oxford University Hospitals NHS Foundation Trust
You might also like
- WarfarinDocument23 pagesWarfarinminaNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- Assignment 2Document4 pagesAssignment 2JafinNo ratings yet
- MILgfgsd V1Document4 pagesMILgfgsd V1garywall.ukNo ratings yet
- Peri-Operative Management of Patients Receiving AnticoagulantsDocument22 pagesPeri-Operative Management of Patients Receiving AnticoagulantsCheuk Hei LauNo ratings yet
- MILV10Document4 pagesMILV10garywall.ukNo ratings yet
- UHS Anticoagulation Therapy Guideline Y12 04Document7 pagesUHS Anticoagulation Therapy Guideline Y12 04staylor235No ratings yet
- MIL Vol 5 No 8 (Initiating Oral Anticoagulation)Document3 pagesMIL Vol 5 No 8 (Initiating Oral Anticoagulation)garywall.ukNo ratings yet
- Anticoagulations in Surgery: Sharifah Naiemah BT Syed MansorDocument20 pagesAnticoagulations in Surgery: Sharifah Naiemah BT Syed MansorSharifah NaiemahNo ratings yet
- Antiplatelet Drugs, Anticoagulants and Elective SurgeryDocument5 pagesAntiplatelet Drugs, Anticoagulants and Elective SurgeryJanice WongNo ratings yet
- Vit KguidelinesDocument2 pagesVit KguidelinesMayer Rosenberg100% (1)
- CCJM Warfarin PDFDocument12 pagesCCJM Warfarin PDFmyscribeNo ratings yet
- Anticoag GuidelinesDocument22 pagesAnticoag Guidelinesyusuf100% (1)
- 2.anticoag Si Anti Agreg in Dermatologie-2009Document10 pages2.anticoag Si Anti Agreg in Dermatologie-2009Gabriela Catana TurcuNo ratings yet
- Anticoag Antipla in Endoscopic ProceduresDocument14 pagesAnticoag Antipla in Endoscopic ProceduresAnonymous ZUaUz1wwNo ratings yet
- Anticoagulants and The Perioper - 2006 - Continuing Education in Anaesthesia CriDocument4 pagesAnticoagulants and The Perioper - 2006 - Continuing Education in Anaesthesia Crironaldquezada038No ratings yet
- Pre and Post Operative CareDocument9 pagesPre and Post Operative CareSara Abdi OsmanNo ratings yet
- Warfarin Therapy Management: ScopeDocument9 pagesWarfarin Therapy Management: ScopesastiraNo ratings yet
- Official Reprint From Uptodate ©2018 Uptodate, Inc. And/Or Its Affiliates. All Rights ReservedDocument43 pagesOfficial Reprint From Uptodate ©2018 Uptodate, Inc. And/Or Its Affiliates. All Rights ReservedVictor M' PimentelNo ratings yet
- Procoagulantes Guias PDFDocument30 pagesProcoagulantes Guias PDFtsntbNo ratings yet
- Chest Guidelines - WarfarinDocument41 pagesChest Guidelines - Warfarinkedaw100% (1)
- Perioperative Management of Patients Receiving Anticoagulants. UpToDate. 2017.Document40 pagesPerioperative Management of Patients Receiving Anticoagulants. UpToDate. 2017.radiomedicNo ratings yet
- The Perioperative Management of AnticoagulationDocument4 pagesThe Perioperative Management of AnticoagulationEliana Castañeda MarínNo ratings yet
- Fondaparinux UPDATE 19 1Document2 pagesFondaparinux UPDATE 19 1Aldi Harry RamdaniNo ratings yet
- Perioperative Management of Patients Receiving Anticoagulants - UpToDateDocument69 pagesPerioperative Management of Patients Receiving Anticoagulants - UpToDatePhúc NguyễnNo ratings yet
- Bleeding After Dental Extractions in Patients Taking Warfarin.Document4 pagesBleeding After Dental Extractions in Patients Taking Warfarin.saeint.peterNo ratings yet
- Mini Warfarin GuidelinesDocument2 pagesMini Warfarin GuidelinesPeunn NattaphatNo ratings yet
- Perioperative Management of AnticoagulationDocument33 pagesPerioperative Management of Anticoagulationmonge20No ratings yet
- Vitamin K Antagonists: American College of Pharmacology and Management of TheDocument41 pagesVitamin K Antagonists: American College of Pharmacology and Management of TheCatalina VallejoNo ratings yet
- Dental Management of Patients On Warfarin Therapy: O M /O & M SDocument5 pagesDental Management of Patients On Warfarin Therapy: O M /O & M SdrsalmanazizNo ratings yet
- Haematology DrugsDocument17 pagesHaematology DrugsParyNo ratings yet
- Head Injury in Anticoagulated Patients: Trauma Clinical GuidelineDocument6 pagesHead Injury in Anticoagulated Patients: Trauma Clinical GuidelinearifbudipraNo ratings yet
- QRG AntithromboticDocument6 pagesQRG AntithromboticthapanNo ratings yet
- Preoperative AnticoagulantDocument59 pagesPreoperative AnticoagulantMahmoud SaghaeiNo ratings yet
- Handbook of Surgical Care For House OfficersDocument20 pagesHandbook of Surgical Care For House OfficersCharity AtsuNo ratings yet
- DVT Prophylaxis Safety ContraindicatDocument1 pageDVT Prophylaxis Safety Contraindicata1b14No ratings yet
- Handbook of Surgical Care For House OfficersDocument22 pagesHandbook of Surgical Care For House OfficersDeep SleepNo ratings yet
- Guidelines On The Diagnosis and Management of Heparin-Induced Thrombocytopenia: Second EditionDocument13 pagesGuidelines On The Diagnosis and Management of Heparin-Induced Thrombocytopenia: Second EditionManzoorAlamKhattakNo ratings yet
- Guidelines On The Diagnosis and Management of Heparin-Induced Thrombocytopenia: Second EditionDocument13 pagesGuidelines On The Diagnosis and Management of Heparin-Induced Thrombocytopenia: Second EditionManzoorAlamKhattakNo ratings yet
- Deep Vein ThrombosisDocument22 pagesDeep Vein ThrombosisEznal MahidinNo ratings yet
- Anticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveDocument3 pagesAnticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveShoyeb KhanNo ratings yet
- Perioperative Management of Patients Receiving Anticoagulants - UpToDateDocument65 pagesPerioperative Management of Patients Receiving Anticoagulants - UpToDatejames lxNo ratings yet
- Periprocedural Anticoagulation v2Document27 pagesPeriprocedural Anticoagulation v2Joanne HoNo ratings yet
- ACCP Anticoagulation Guidelines SummaryDocument11 pagesACCP Anticoagulation Guidelines Summaryd40sithui100% (3)
- Name of The Medicinal Product: Prescribing Information Coumadin TabletsDocument13 pagesName of The Medicinal Product: Prescribing Information Coumadin Tabletsddandan_2No ratings yet
- Algorithm For Perioperative Management of Anticoagulation1Document8 pagesAlgorithm For Perioperative Management of Anticoagulation1andi namirah100% (1)
- A NTICOAGULANTDocument48 pagesA NTICOAGULANTSharliza S100% (1)
- Anticoagulation Protocol For PostDocument8 pagesAnticoagulation Protocol For PostMohammed IbrahimNo ratings yet
- Anx 135796 enDocument108 pagesAnx 135796 enMohamed RawyNo ratings yet
- Deep Vein Thrombosis - 2003Document34 pagesDeep Vein Thrombosis - 2003farmasi_hm100% (1)
- Perioperative ManagementDocument15 pagesPerioperative Managementalfi syahrinNo ratings yet
- Chest: Treatment and Prevention of Heparin-Induced ThrombocytopeniaDocument36 pagesChest: Treatment and Prevention of Heparin-Induced ThrombocytopeniaDonia ShadyNo ratings yet
- Anticoagulants Preoperative InstructionsDocument3 pagesAnticoagulants Preoperative InstructionsDevaki VisvalingamNo ratings yet
- Warfarin Perioperative ManagementDocument8 pagesWarfarin Perioperative Managementzoran cukovicNo ratings yet
- WARFARIN Prescribing Guidelines For The Management of Patients On Anticoagulant Therapy WIRRAL NHSDocument14 pagesWARFARIN Prescribing Guidelines For The Management of Patients On Anticoagulant Therapy WIRRAL NHSNavojit ChowdhuryNo ratings yet
- Clinical Review: Target-Specific Oral Anticoagulants in The Emergency DepartmentDocument12 pagesClinical Review: Target-Specific Oral Anticoagulants in The Emergency Departmentrosariris94No ratings yet
- Arfarin: Arget UdienceDocument4 pagesArfarin: Arget UdienceMano cempakaNo ratings yet
- Anticoagulantele Si Explorarile Invazive 2021Document33 pagesAnticoagulantele Si Explorarile Invazive 2021GabrielaOaneNo ratings yet
- Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)Document40 pagesDeep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)Shahab AlamNo ratings yet
- Cardiovascular Center Pocket Guide Use of Warfarin in Thrombotic Cardiovascular DiseaseDocument2 pagesCardiovascular Center Pocket Guide Use of Warfarin in Thrombotic Cardiovascular Diseasemicheal1960No ratings yet
- UFH LMWH Fonda - 06september2020Document7 pagesUFH LMWH Fonda - 06september2020gabrimarteNo ratings yet
- Atmospherc Pressure Vs AltitudeDocument1 pageAtmospherc Pressure Vs Altitudezoran cukovicNo ratings yet
- From The Perspective of Battery Production: Energy-Environment-Economy (3E) Analysis of Lithium-Ion Batteries in ChinaDocument12 pagesFrom The Perspective of Battery Production: Energy-Environment-Economy (3E) Analysis of Lithium-Ion Batteries in Chinazoran cukovicNo ratings yet
- New Guidance On The Design of Offshore StructuresDocument8 pagesNew Guidance On The Design of Offshore Structureszoran cukovicNo ratings yet
- Wmo 188eDocument327 pagesWmo 188ezoran cukovicNo ratings yet
- Warfarin Perioperative ManagementDocument8 pagesWarfarin Perioperative Managementzoran cukovicNo ratings yet
- Api 650 Technical Queries PDFDocument21 pagesApi 650 Technical Queries PDFzoran cukovicNo ratings yet
- Diet Guidelines While Taking Warfarin or Coumadin™: Tips To Keep Your Vitamin K Intake ConsistentDocument2 pagesDiet Guidelines While Taking Warfarin or Coumadin™: Tips To Keep Your Vitamin K Intake Consistentzoran cukovicNo ratings yet
- List of Substances Subject To Prohibited / Undesirable / DeclarationDocument13 pagesList of Substances Subject To Prohibited / Undesirable / Declarationzoran cukovicNo ratings yet
- Roadrunner Hybrid 3 HP / 2 Stage Dry VacuumDocument8 pagesRoadrunner Hybrid 3 HP / 2 Stage Dry Vacuumzoran cukovicNo ratings yet
- STEAMGEN - PED - Calculations PDFDocument177 pagesSTEAMGEN - PED - Calculations PDFzoran cukovicNo ratings yet
- 1352 PDFDocument115 pages1352 PDFzoran cukovicNo ratings yet
- Chemical Storage Guidelines: Acids (PH 7.0)Document3 pagesChemical Storage Guidelines: Acids (PH 7.0)zoran cukovicNo ratings yet
- Foundations Ambient Temperature Storage Tanks: ContentsDocument8 pagesFoundations Ambient Temperature Storage Tanks: Contentszoran cukovicNo ratings yet
- 9117-15-7154 Addendum 1Document240 pages9117-15-7154 Addendum 1zoran cukovicNo ratings yet
- How Does Your Comp Air Cost - P-2010-ED-tcm131-6752Document21 pagesHow Does Your Comp Air Cost - P-2010-ED-tcm131-6752zoran cukovicNo ratings yet
- Optimal System Design For Weigh-In-Motion Measurements Using In-Pavement Strain SensorsDocument8 pagesOptimal System Design For Weigh-In-Motion Measurements Using In-Pavement Strain Sensorszoran cukovicNo ratings yet
- First Aid - NotesDocument10 pagesFirst Aid - NotesRoisin McdonnellNo ratings yet
- Rheumatic and Systemic DiseaseDocument37 pagesRheumatic and Systemic DiseasesallyNo ratings yet
- Susunan Acara Simposium Pertemuan Ilmiah Ilmu Penyakit Dalam (Pit Ipd) 2020Document4 pagesSusunan Acara Simposium Pertemuan Ilmiah Ilmu Penyakit Dalam (Pit Ipd) 2020Ulfa MutiaraNo ratings yet
- Core, Care, Cure ModelDocument33 pagesCore, Care, Cure ModelThushara Krishnas50% (2)
- HemorrhoidsDocument32 pagesHemorrhoidsSimon Peter MollanedaNo ratings yet
- Tamil Nadu - Management QuotaDocument602 pagesTamil Nadu - Management Quotakaushik ghoshNo ratings yet
- Case-Scenario No. 2 Ectopic-PregnancyDocument2 pagesCase-Scenario No. 2 Ectopic-PregnancyJoegie ArioNo ratings yet
- Waiters Newborn Care PDFDocument1 pageWaiters Newborn Care PDFmp1757No ratings yet
- Crown Lengthening Procedures - A Review ArticleDocument11 pagesCrown Lengthening Procedures - A Review ArticleIOSRjournalNo ratings yet
- Morphine Titration GuideDocument1 pageMorphine Titration GuideDaniel Jonathan LimNo ratings yet
- Quality Standards Acute Care Equipment and Drug ListsDocument34 pagesQuality Standards Acute Care Equipment and Drug ListsGul NazNo ratings yet
- Integrated Management of Childhood Illness (IMCI) PDFDocument7 pagesIntegrated Management of Childhood Illness (IMCI) PDFLOVELY ANN GIGANTENo ratings yet
- NCP 2Document2 pagesNCP 2Aneeza Musa IndananNo ratings yet
- Post-Operative Instructions Hemorrhoidectomy: Comfort MeasuresDocument3 pagesPost-Operative Instructions Hemorrhoidectomy: Comfort MeasuresKath ReignNo ratings yet
- QuizDocument16 pagesQuizAmy Ramirez100% (1)
- Gap Analysis Between 4010 and 5010 TransactionDocument6 pagesGap Analysis Between 4010 and 5010 TransactionNikhil SatavNo ratings yet
- Clinical GuidlinesDocument200 pagesClinical GuidlinesMujtaba NadeemNo ratings yet
- Drug Study For HepatitisDocument4 pagesDrug Study For Hepatitisunyokies100% (1)
- Kyyrönen IidaDocument114 pagesKyyrönen IidaNopri JayaNo ratings yet
- KEIZINAN - ZDocument52 pagesKEIZINAN - ZMisya SafinaNo ratings yet
- White Island in The Red SeaDocument1 pageWhite Island in The Red SeaIndach RatnaNo ratings yet
- Varicella in PregDocument5 pagesVaricella in PregYwagar YwagarNo ratings yet
- Concept Map: End Stage Renal DiseaseDocument4 pagesConcept Map: End Stage Renal DiseaseAziil LiizaNo ratings yet
- International Symposium: On Human Factors andDocument25 pagesInternational Symposium: On Human Factors andSusmitha CLNo ratings yet
- Slide Kombinasi Antibiotik MedicalDocument62 pagesSlide Kombinasi Antibiotik MedicalyamtotlNo ratings yet
- Recomendacions ERC 2015 Resumo Executivo (Galego)Document100 pagesRecomendacions ERC 2015 Resumo Executivo (Galego)Leonel MeloNo ratings yet
- G.R. No.146891. July 30, 2002 Ruben T. Limbo, Petitioner, V. Employees Compensation Commission and Social SecurityDocument3 pagesG.R. No.146891. July 30, 2002 Ruben T. Limbo, Petitioner, V. Employees Compensation Commission and Social Securityfritzie abellaNo ratings yet
- Emea Thiomersal Vaccines Human Use Recent Evidence Supports Safety Thiomersal - enDocument2 pagesEmea Thiomersal Vaccines Human Use Recent Evidence Supports Safety Thiomersal - enAntonio MoncayoNo ratings yet
- CSS Form 2016 PDFDocument1 pageCSS Form 2016 PDFikenxhee liNo ratings yet