Professional Documents
Culture Documents
Dipeptidyl Peptidaseiv A Brief Review 1 6
Uploaded by
GREESTYOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dipeptidyl Peptidaseiv A Brief Review 1 6
Uploaded by
GREESTYCopyright:
Available Formats
ISSN: 2319-9849
Research and Reviews: Journal of Chemistry
Dipeptidyl Peptidase–IV: A Brief Review.
Bhavya K*, and Madhusudan N Purohit
Department of Pharmaceutical Chemistry, JSS College of Pharmacy, JSS University, Mysore-15, Karnataka, India.
Review Article
Received: 28/05/2013 ABSTRACT
Revised: 04/06/2013
Accepted: 14/06/2013 Diabetes mellitus-2 [NIDDM/T2D] is a metabolic disorder that is
characterized by Insulin resistance and hyperglycemia. DPP IV inhibitors have been
*For Correspondence investigated as new target for T2D treatment. DPP IV inhibition improves the impaired
insulin secretion and decrease postprandial concentrations of glucagon by enhancing
Department of Pharmaceutical the incretin hormone levels of Glucagon like peptide-1(GLP-1) and Glucose dependent
Chemistry, JSS College of Pharmacy, insulinotropic polypeptide (GIP). Many research activities in this area resulted in the
JSS University, Mysore-15, Karnataka, introduction of Sitagliptin and Vildagliptin (Only in Europe) and few active molecules
India. entered into clinical trials, for example Alogliptin. Treatment of this metabolic
Mobile: +91 9964585681 disorder especially in the early stages of the disease by DPP IV inhibition has been
recognized as a validated and large numbers of inhibitors are currently in various
Keywords: DPP-IV inhibitors, GLP, GIP, stages of preclinical or clinical development. This review summarizes the development
Incretin. of DPP IV inhibitors, molecular mechanism, and etc.
INTRODUCTION
Diabetes is an emerging epidemic of the 21st century and has become a major health problem throughout the globe. It is a
metabolic disease characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. After digestion,
glucose passes into the bloodstream, where it is used by cells for growth and energy. For glucose to get into cells, insulin must be
present. Insulin (51 amino acid residue) is a hormone produced by the pancreas, a large gland behind the stomach (Pancreas) [1, 2]. In
diabetes, the pancreas either produces little or no insulin, or the cells do not respond appropriately to the insulin that is produced.
Glucose builds up in the blood, overflows into the urine, and passes out of the body. Thus, the body loses its main source of fuel even
though the blood contains large amounts of sugar. The three main types of (Chart-1) diabetes are (1) Type-1diabetes(T1D) (2) Type-
2 diabetes(T2D) (3) Gestational diabetes, Out of this T2D, often called Non-Insulin Dependent Diabetes and is the most common
form of diabetes, affecting 90% - 95% people in the world. Metabolic syndrome is associated with a markedly increased incidence of
coronary, cerebral and peripheral artery disease. The current oral hypoglycemic agents against T2D include metformin, sulfonylurea,
thiazolidinedione and α-glycosidase inhibitors, although effective in increasing insulin secretion, are associated with undesirable
side effects, Weight gain, edema, gastrointestinal toxicities and hypoglycemia are the few side effects of existing oral antidiabetic
agents. List of existing oral antidiabetic agents along with their molecular target, mechanism of action and adverse effects related to
their use are summerised in Table 1. Patients having T2D are at high risk of vascular complications including coronary heart disease,
stroke, hypertension, peripheral vascular disease, neuropathy, retinopathy and nephropathy [2]. According to World Health
Organization (WHO) this public health problem affecting 366 million people by 2030. Inhibition of Dipeptidyl Peptidase IV (DPP IV) has
emerged as a new treatment for T2D. Inhibition of DPP-IV has shown to increase the half life of GLP-1 and to prolong the beneficial
effects of incretin hormone. Moreover, DPP-IV inhibitors did not show the undesirable side effects, as observed in other oral
antidiabetic agents [2, 3].
Chart 1: Classification Diabetes
Types of Diabetes
Type-1 Type-2
Insulin dependent diabetes(IDDM) Non insulin dependent diabetes (NIDDM)
Caused by destruction of beta cells Caused by target cell resistance to insulin
Appears in childhood appears to reduce the number of insulin receptor Mostly appears in obese person, obesity
Dependent on insulin replacement Treated with oral hypoglycemic drugs
RRJC | Volume 2 | Issue 3 | July – September 2013 1
ISSN: 2319-9849
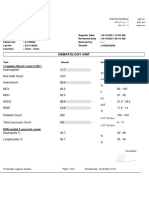
Table 1: DPP-IV inhibitors status and availability
Drug Chemical nature Status Trade name Pharmaceutical company
Sitagliptin Β-amino acid based blockbuster drug Approved in the United JanuviaTM, Merck & Co., Inc
States and Europe Janumet®
Saxagliptin Methanoprolinenitrile based inhibitor Approved in the United OnglyzaTM Bristol-Meyers
(BMS-477118) States and Europe Squibb/AstraZeneca
Linagliptin --- Approved in United Ondero® , Boehringer Ingelheim
States and Europe Tradjenta ™
Vildagliptin Cyanopyrrolidine based inhibitor Approved in Europe Galvus® Novartis AG
Alogliptin Non-peptidomimetic series drug Under investigation Nesina® Takeda Pharmaceutical
(SYR-322) Company Limited
Dutogliptin Boronic acid based inhibitor Phase III Not officially Phenomix/Forest
(PHX-1149) disclosed Laboratories, Ind.
Melogliptin Fluropyrrolidine based inhibitor Phase II Not officially Glenmark
(GRC-8200) disclosed Pharmaceuticals, Europe
Teneligliptin Cyanopyrrolidinebased inhibitor Phase II (Japan) Not officially Mitsubishi Tanabe
(MP-513) Phase III(US/EU) disclosed Pharma Corporation.
Denagliptin Cyanopyrrolidine based bis-aryl inhibitor Phase II Not officially Glaxosmith Kline
(GW-823093) disclosed Pharmaceuticals Ltd
K-579 Pyrrolidine carbonitrile derivative ----- ----- Tocris Bioscience
ABT-341 Alkylcyanopyrrolidine based inhibitor ----- ----- Abbott laboratories
Incretin System
Incretins are a group of gastrointestinal hormones released during meals from gut endocrine cells. They cause an increase in
the amount of insulin released from β-cells of the Islets of Langerhans after intake of food, they also inhibit glucagon release from
the α-cells of the Islets of Langerhans. The incretin hormones include glucagon-like peptide-1(GLP-1) and glucose dependent
insulinotropic polypeptide (GIP). Both hormones contribute to insulin secretion from the beginning of a meal and their effects are
progressively amplified as plasma glucose concentration rises. In response of food ingestion GLP-1 (7-36 amide) is a 30 amino acid
polypeptide which is rapidly secreted into the small intestine and the colon. Half life of GLP is 1- 1.5 minutes and shortly after its
secretion it is rapidly degraded by the enzyme DPP-IV, by cleaving the two N-terminal residues ogGLP-1[4,5]. K cells of the duodenum
are responsible to release GIP with the response of nutrient ingestion and also enhance glucose-stimulated insulin secretion. Half life
of GIP is 5-7 minutes [6,7,8,9].
Dipeptidyl Peptidase-IV Inhibitors
Dipeptidyl peptidase IV (DPP IV) was identified in 1966 by Hopsu-Hovu and Glenner as glycylproline napthylamidase and was
purified from rat liver and pig kidney in 1967 and 1968, respectively. The first inhibitor were characterized in the late 1980s and
1990s [10]. DPP-IV is circular membrane protein with ubiquitous expression, its activity has been recorded in rats, mice and humans in
epithelial cells of the intestine, kidney, liver, lung, thymus, spleen and etc. It is also known as the T-cell antigen CD26, a serine
exopeptidase. Members of protease family include DPP I-IV; DPP IV is a key regulator of incretin hormones. DPP IV is a non classical
serine protease, membrane associated peptidase of 766 amino acids, widely distributed in numerous tissues and DPP-IV inhibitors
prevents the degradation of GLP-1 and increases its concentration in blood [11,12].
Mechanism of Action
DPP-IV is a 766 amino acid amino peptidase. It is a tetramer with each subunit comprising of two domains, N-terminal β-
propeller domain & C-terminal catalytic domain. The active site of the enzyme is covered by the β-propeller domain or a side opening
formed at the interface of β-propeller domain and catalytic domain [13]. Based on In-vitro studies DPP-IV has a preference to cleave X-
proline dipeptides at the N-terminus of polypeptides. GLP-1 and related glucagon family members contain alanine at this position [13].
DPP-IV inhibitors competitively inhibit the enzyme DPP IV, this enzyme breaks down the incretin GLP-1 and GIP, which are
released in response to a meal. By preventing GLP-1 and GIP inactivation, insulin secretion increases and suppresses the release of
glucagon by the pancreas which brings the blood glucose levels to normal. As the blood glucose level attained normal, the amount of
insulin released and glucagon suppressed diminishes and prevents hypoglycemia which is seen with some oral hypoglycemic agents
[15].
There are three class of DPP-IV inhibitors are under investigation, reversible product analogue inhibitors (pyrrolidines and
thiazolidines), covalently modifying product analogues (Cyanopyrrolidines) and reversible non-peptidic heterocyclic inhibitors
(xanthines and aminomethylpyrimidines) [14,15].
RRJC | Volume 2 | Issue 3 | July – September 2013 2
ISSN: 2319-9849
Sitagliptin (JANUVIA TM):
Sitagliptin (Figure-1) (Merck Pharmaceuticals, USA) is a highly potent, competitive; a highly selective triazolopiprazine based
reversible inhibitor of DPP-IV enzyme. It is the first compound of its class introduced in the market and its chemical structure is (2R)-
4-oxo-4[3-(trifluoromethyl)-5,6-dihydro[1,2,4]-triazolo-[4,3]-pyrazin-7-(8H)-yl]-1-(2,4,5-trifluorophenyl)-butan-2-amide. In
October 2006, the US FDA approved sitagliptin as monotherapy and in combination with other oral diabetic medications, metformin,
pioglitazone to improve blood glucose controlin T2D [16, 17]. In March 2007 it was approved in European Union. The normal dose is
100mg at once a day. Currently it is approved in 42 countries as an anti-diabetic agent [18, 19].
Figure.1: Structures of selected DPP-IV inhibitors
F
F
NH2 O O CN
N N
HO N
N
F N NH2
Sitagliptin CF3 Saxagliptin
CN
NH2 N
N O C
N N
N N
O N
N N N
O N
H3C O H NH2
Alogliptin Linagliptin
F
C N
O
H
N N
O C N
F
N N N
Melogliptin
F NH2 N
Denagliptin F
Pharmacokinetics and Drug Interaction
38% of sitagliptin is bound to plasma protein and its bioavailability is approximately 87%. Its halflife is 8-14hours, it
undergoes metabolism via CYP3A4 and CYP2C8. Dose of sitagliptin should not be changed when it is combined with other
antidiabetic drugs (metformin/glitazones). Elimination is mainly through urine.
Combination of sitagliptin with pioglitazone results in peripheral oedema. According to reports on glitazones, it posses
cardio toxic effect. Although sitagliptin is not as likely to cause hypoglycemia as other oral diabetes medications [20,21,22].
Side Effects
Side effects of sitagliptin are cold, stuffy nose, diarrhea, headache, skin irritation, anaphylaxis, angioedema, hypersensitivity
and rashes.
Vildagliptin (Galvus®):
Vildagliptin (Figure-1) is a potent, selective and orally active 2nd generation pyrrolidine based reversible inhibitor of DPP-IV.
Reversible binding forms a complex with DPP-IV, causing its inhibition. Its chemical structure is (S)-1-[N-(3-hydroxy-1-adamantyl)
glycyl]pyrrolidine-2-carbonitrile. In December 2011, the EU FDA approved Vildagliptin as monotherapy and in combination with other
existing oral antidiabetc agents (metformin, sulfonylureas and glitazones) to treat T2D [23]. The approval of Galvus in the US remains
uncertain, however presently it is using in 37 countries as an antidiabetic agent [23, 24].
Pharmacokinetics and Drug Interaction
Vildagliptin bioavailability is 85% and rapidly absorbed within 1-2 hours. It undergoes metabolism via CYP450, with a half
life of 1.5-4.5 hrs but it does not appear to induce or inhibit the CYP450 enzyme. Dose of 50mg to be taken twice daily. So,
Vildagliptin dose frequency is higher than Sitagliptin. Vildagliptin is used as a monotherapy or in combination with metformin [25, 26, 27,
RRJC | Volume 2 | Issue 3 | July – September 2013 3
ISSN: 2319-9849
31] (50mg of Galvus and 850mg of metfomin) and rosiglitazone [30]. Major antidiabetic action appears to be an enhancement of glucose
stimulated insulin release, mediated via increasein GLP-1 levels. Most of the published evidence shows that Vildagliptin 50mg/day is
more effective in reducing both fasting plasma glucose and postprandial plasma glucose [25,26,27,28,29,30,31].
Side effects
Head ache, dizziness, upper respiratory infection, high blood pressure, nose and throat infection, pain in the extremities.
Swelling of the face, lips, mouth, tongue and allergic reaction known as anaphylactic shock.
Saxagliptin (Onglyza™)
Saxagliptin (Figure-1) was approved by US Food and Drug administration in July 2009 and by European Medicines Evaluation
Agency in October 2009 for use as monotherapy or in combination for the treatment of T2D [32, 33]. Its chemical structure is (1S, 3S,
5S)-2-[(2S)-2-amino-2-(3-hydroxy-1-adamantyl) acetyl]-2-azabicyclo hexane-3-carbonitrile.The combination product of
saxagliptin/ metformin was approved in November 2010 [33]. Presently it is using in 68 countries as anti diabetic agent. It is also
approved to use as monotherapy (Dose of 50mg) and in combination with other drugs, metformin (100mg),
sulfonyl urea and glitazones [34, 35, 36, 37, 38, 39, 40, 41].
Pharmacokinetics and Drug interactions
Saxagliptin is a cyannopyrrolidine P-glycoprotein (P-gp) substrate. It is metabolized hepatically by cytochrome P450 (CYP)
3A4/5 to an active metabolite, 5-hydroxy saxagliptin [34]. This active metabolite is also a selective, reversible, competitive DPP-4
inhibitor. According to reports on saxagliptin, it does not inhibit the T-cell activity in In vivo study [38, 39, 40, 41].
Linagliptin (Tradjenta ™)
Linagliptin (Figure-1) (Boehringer Ingelheim Research) is a structurally novel dipeptidyl-peptidase-4 (DPP-4) inhibitor[42]. Its
chemical structure is 1H-Purine-2, 6-dione -8- [(3R)-3-amino-1-piperidinyl] – 7 - (2-butyn-1-yl) - 3, 7-dihydro-3-methyl-1-1[(4-
methyl-2-quinazolinyl)-methyl]. In May 2011, US FDA approved Linagliptin for clinical use. Combination of linagliptin plus metformin
(Jentadueto, Eli Lilly) was approved for clinical use on February 2012 [43, 44, 45].
Pharmacokinetics and Drug Interaction
Dose of 5mg to be administered daily and its bioavailability is 30% of the administered drug [45]. 90% of linagliptin is excreted
in unchanged form. According to reported datas on Combination therapy of linagliptin with other diabetic drugs (metformin,
sulfonylurea, glitazones) were also showed significant reduction of blood glucose level. Combination of linagliptin plus metformin
hydrochloride received approval from US FDA on February 2012 [46, 47, 48].
Alogliptin (Nesina ®)
Alogliptin (Figure-1) is an orally available quinazolinonebased noncovalent inhibitor of DPP 4.It is under investigation in the
US for the treatment of T2DM. It is being sold in Japan. It failed to receive the approval from European FDA; on April 2012 regulators
of Europe have agreed to review its T2D therapy of Alogliptin. Regard this in the month of April, the FDA issued a second complete
response letter for the drug and fixed dose combination of alogliptin with pioglitazone [49, 50].
CONCLUSION
DPP-IV inhibitors are a novel class of orally available molecules for the treatment of type 2 diabetes. Even though they are
structurally different, they share a common mechanism of action by extending half-life endogenous Incretins and potentially reduce
blood glucose level. Because GLP-1 secreted in glucose-dependent manner, DPP-IV inhibitors which prolong its half-life.
ACKNOWLEDGEMENT
Authors are thankful to the principal, JSS college of Pharmacy, JSS University, Mysore, for providing necessary facilities.
REFERENCES
1. Giovanni A, David PF. Protease inhibitors in the clinic. Med Chem. 2005; 1: 71-104.
2. Yan IC, Lee MC. Dipeptidyl Peptidase IV Inhibitors: An Evolving Treatment for Type 2 Diabetes from the Incretin Concept.
Recent Pat Endocr Metab Immune Drug Discov. 2007; 1: 15-24.
3. Drucker DJ. Therapeutic potential of dipeptidyl peptidase IV inhibitors for type 2 diabetes. Expert Opin Inv Drug. 2003; 12:
87-100.
RRJC | Volume 2 | Issue 3 | July – September 2013 4
ISSN: 2319-9849
4. Christopher HS. Incretin based therapies for type 2 diabetes. Canadian J diabetes. 2008; 32(2):131-139.
5. http//eme.medscape.com/view article/ 732272.
6. Michael AN, Tina VB, Baptist Gall W, Alan G. Incretin based therapies. Diabetes Care. 2009; 32(2): S223-S231.
7. Daniel C, Stephanie LL, Robert AP. IARS. 2009; 108(6): 1803.
8. Renee EA, Joseph L, Anas Fassios GP. Efficacy and safety of incretin therapy in type 2 diabetes-systematic review and meta-
analysis. J Am Med Assoc. 2007; 298(2):194-206.
9. Davidson JA. Incorporating incretin-based therapies into clinical practice: differences between glucagon-like peptide 1
receptor agonists and dipeptidyl peptidase 4 inhibitors. Mayo Clin Proc. 2010; 85(12): S27-S37.
10. Sebokova E, Christ A, Boehringer M, Mizrahi J. Dipeptidyl peptidase-4 inhibitors- A new approach in diabetes. Curr Top Med
Chem. 2006; 7: 547-555.
11. Monika G, Sarbjot S, Punam G. Dipeptidyl peptidase-4 inhibitors: A new approach in diabetes treatment. Int J Drug Dev Res.
2009; 1(1): 146-156.
12. Boehringer . DPP IV Inhibitors. US7314884 B2. January 1st. 2008.
13. Mentlein R. Mechanisms underlying the rapid degradation and elimination of the incretin hormones GLP-1 and GIP. Best
Pract. Res Clin Endocrinol Metab. 2009; 23: 443-452.
14. Gupta R, Waluni SS, Tokala RK, Parsa KV, Singh SK, Pal M. Emerging drug candidates of dipeptidyl peptidase IV (DPP IV)
inhibitor class for the treatment of type 2 diabetes. Curr Drug Targets. 2009; 10: 71-87.
15. Patel KD, Patel GM. Role of DPP-IV inhibitors in treatment of type II diabetes. IRJP. 2010; 1(1):19-28.
16. Miller SA, St.Onge EL. Sitagliptin: A dipeptidyl peptidase IV inhibitor for the treatment of Type 2 diabetes. Ann Pharmacother.
2006; 40:1336-1343.
17. Thornberry NA, Weber AE. Discovery of JANUVIA (Sitagliptin), a selective dipeptidyl peptidase IV inhibitor for the treatment of
type 2 diabetes. Curr Top Med Chem. 2007; 7(6): 557-568.
18. Drucker D, Easley C, Kirkpatrick P. Sitagliptin. Nat.Rev. Drug Disco. 2007; 6: 109-10.
19. Decon CF. Dipeptidyl peptidase 4 inhibition with sitagliptin: a new therapy for type 2 diabetes. Expert Opin Investig Drugs.
2007; 16(4): 535-545.
20. Hermann GA, Stein PP, Thornberry NA, Wagner JA. Dipeptidyl peptidase -4 inhibitors for the treatment of type 2 diabetes:
focus on sitagliptin. Clin Pharmacol Ther. 2007; 81(5): 761-767.
21. Rajesh K, Gary H, John AW. Accelerating drug development using Biomarkers: A case study with sitagliptin, a novel DPP4
inhibitor for type 2 diabetes. AAPS J. 2008; 10(2): 401-409.
22. Baptist G. Review of Sitagliptin phosphate: a novel treatment for type 2 diabetes. Vasc.Health. Risk Manag. 2007; 3(2): 203-
210.
23. Andrea OEl, Rehring E, Jens Holst J, Anja S, James F, David H. The Dipeptidyl peptidase 4 inhibitor Vildagliptin does not
accentuate Glibenclamide-Induced hypoglycemia but reduces Glucose-Induced Glucagon- Like peptide 1 and Gastric
Inhibitory polypeptide Secretion. J Clin Endocrinol Metab. 2007; 92(11): 4165-4171.
24. Claudia F, Sherwyn S, James EF. Effect of Vildagliptin as add-on therapy to a low-dose metformin. World J Diabetes. 2010;
1(1):19-26.
25. Ahren B, Pacini G, Foley JE, Schweizer A. Improved meal-related beta cell function and insulin sensitivity by the dipeptidyl
peptidase-IV inhibitor vildagliptin in metformin-treated patients with type 2 diabetes over 1 year. Diabetes Care. 2005;
28(8):1936-1940.
26. Balas B, Baig MR, Watson C, Dunning BE, Ligueros-Saylan M, Wang Y. The dipeptidyl peptidase IV inhibitor Vildagliptin
suppresses endogenous glucose production and enhances islet function after single-dose administration in type 2 diabetic
patients. J Clin Endocrinol Metab. 2007; 92(4): 1249-1255.
27. Emanuele B, Erika R, Riccardo PC, Alan JG, Carole C. Effects of vildagliptin on glucose control over 24 weeks in patients with
type 2 Diabetes Inadequately controlled with metformin. Diabetes Care. 2007; 30: 890-895.
28. Burkey BF, Bolognese L, Balkan B, Mone M, Russell M, Hughes TE. Acute and chronic effects of the incretin enhancer
vildagliptin in insulin-resistant rats. J Pharm Exp Ther. 2005; 315(2): 688-695.
29. Dale SE, Kathryn SJ, Doss WN, Melanie S, Charles HH, Xia Z. Inhibition of dipeptidyl peptidase 4 by vildagliptin during
Glucagon-Like peptide 1 fusion Increases Liver glucose uptake in the conscious Dog. Diabetes. 2009; 58:243-249.
30. Julio R, David M, Michelle AB, Sylvie D, Anja S. Comparison of Vildagliptin and rosaglitazone monotherapy in patients with
type 2 diabetes: A 24 week, double blind, randomized trial. Diabetes Care. 2007; 30: 217-223.
31. Claudia F, Sherwyn S, James EF. Effect of vildagliptin as add-on therapy to a low-dose metformin. World J Diabetes. 2010;
1(1): 19.
32. www.fda.gov/downloads/UCM149587.
33. www.onglyza.org
34. Kim YB, Kopcho LM, Kirby MS, Hamann LG, Weigelt CA, Metzler WJ. Mechanism of Gly-Pro-pNA cleavage catalyzed by
dipeptidyl peptidase-IV and its inhibition by saxagliptin (BMS-477118). Young BK, Lisa MK, Mark SK. Arch Biochem Biophys.
2006; 445: 9-18.
35. Tahrani AA, Piya MK, Barnett AH. Saxagliptin: a new DPP-4 inhibitor for the treatment of type 2 diabetes mellitus. Adv Ther.
2009; 26(3): 249-262.
36. Rosenstock J, Sankoh S, List JF. Glucose-lowering activity of the dipeptidyl peptidase-4 inhibitor saxagliptin in drug-naïve
patients with type 2 diabetes. Diabetes Obes Metab. 2008; 10(5): 376-386.
RRJC | Volume 2 | Issue 3 | July – September 2013 5
ISSN: 2319-9849
37. Rosenstock J, Salinas CA, Klein E, Nepal S, List J. Effect of saxagliptin monotherapy in treatment-naïve patients with type 2
diabetes. Curr Med Res Opin. 2009; 25: 2401-2411.
38. De Fronzo RA, Hissa MN, Garber AJ, Luiz Gross J, Yuyan DR, Ravichandra S. The efficacy and safety of saxagliptin when
added to metformin therapy in patients with inadequately collected type 2 diabetes with metformin alone. Diabetes Care.
2009; 32: 1649-1655.
39. Hollander P, Li J, Allen E, Chen R. Saxagliptin added to a thiazolidinedione improves Glycemic control in patients with type 2
diabetes and inadequate control on thiazolidinedione alone. J Clin Endocrinol Metab. 2009; 94: 4810-4819.
40. Chacra AR, Tan GH, Apanovitch A, Ravichandran S, List J, Chen R. Saxagliptin added to a submaximal dose of sulphonylurea
improves glycemic control compared with uptitration of sulfonylurea in patients with type 2 diabetes: a randomized
controlled trial . Int J Clin Pract. 2009; 63: 1395-1406.
41. Scheen AJ, Charpentier G, Ostgren CJ, Hellqvist A, Nilsson IG. Efficacy and safety of saxagliptin in combination with
metformin compared with sitagliptin in combination with metformin in adult patients with type 2 diabetes mellitus. Diabetes
Metab Res Rev. 2010; 26(7): 540-549.
42. Weber AE. Dipeptidyl peptidase IV inhibitors for the treatment of diabetes. J Med Chem. 2004; 47(17): 4135-4141.
43. McIntosh CH, Demuth HU, Pospisilik JA, Pederson R. Dipeptidyl peptidase IV Inhibitors: how do they work as new antidiabetic
agents. Regul Pept. 2005; 128(2):159-165.
44. Eckhardt M, Langkopf E, Mark M, Tadayyon M, Thomas L, Nar H. 8-(3-(R)-aminoprperidin-1-yl)-7-but-2-ynyl-3-methyl-1-
(4-methyl-quinazolin-2-ylmethyl)-3,7-dihydropurine-2,6-dione (BI 1356), a highly potent, selective, long acting, and orally
bioavailable DPP-4 inhibitor for the treatment of type 2 diabetes. J Med Chem. 2007; 50(26): 6450-6453.
45. Joshua JN, Stephen MS. Review of linagliptin for the treatment of type 2 diabetes mellitus. Clin Therapeutics. 2012; 34(5):
993-1005.
46. Del Prato S, Barnett AH, Huisman H, Neubacher D, Woerle HJ, Dugi KA. Effect of linagliptin monotheraphy on glycaemic
control and markers of beta cell function in patients with inadequately controlled type 2 diabetes: a randomized controlled
trial. Diabetes Obes Metab. 2011; 13: 258-267.
47. Taskinen MR, Rosenstock J, Tamminen I, Kubiak R, Patel S, Duqi KA. Safety and efficacy of linagliptin as add-on therapy to
metformin in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled study. Diabetes Obes Metab.
2011; 13: 65-74.
48. Prato SD, Barnett AH, Huisman H, Neubacher D, Woerle HJ, Dugi KA. Effect of linagliptin monotherapy on glycemic and
markers of E-cell function tesDiain patients with inadequately controlled type 2 diabetes: a randomized controlled trial. Obes
Metab. 2011; 13: 258-267.
49. DeFronzo RA, Fleck PR, Wilson CA, Mekki Q. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin in patients
with type 2 diabetes and inadequate glycemic control: a randomized, double-blind, placebo-controlled study. Diabetes Care.
2008; 31: 2315-2317.
50. Nauck MA, Ellis GC, Fleck PR, Wilson CA, Mekki Q. efficacy and safety of adding the dipeptidyl peptidase-4 inhibitor
alogliptin to metformin therapy in patients with type 2 diabetes inadequately controlled with metformin monotherapy: a
multicentre, randomised, double-blind, placebo-controlled study. Int J Clin Practice. 2009;63 (1): 46-55.
RRJC | Volume 2 | Issue 3 | July – September 2013 6
You might also like
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- IJAMSCR-17-223 - 426-433 Review On Adverse Drug Reaction of Antidiabetic Drugs PDFDocument8 pagesIJAMSCR-17-223 - 426-433 Review On Adverse Drug Reaction of Antidiabetic Drugs PDFtrupetiNo ratings yet
- Dipeptidyl Peptidase-4 Inhibitors: Their Role in The Management of Type 2 DiabetesDocument3 pagesDipeptidyl Peptidase-4 Inhibitors: Their Role in The Management of Type 2 DiabetesRidha Surya NugrahaNo ratings yet
- Safety and Efficacy of Linagliptin in Type 2 Diabetes Patients With Common Renal and Cardiovascular Risk FactorsDocument11 pagesSafety and Efficacy of Linagliptin in Type 2 Diabetes Patients With Common Renal and Cardiovascular Risk FactorsmichaelwillsonNo ratings yet
- Antidiabetic DrugsDocument14 pagesAntidiabetic DrugsAswini sreenarayanaNo ratings yet
- 02 Ijpscr 123 23Document12 pages02 Ijpscr 123 23BRNSS Publication Hub InfoNo ratings yet
- Pharmaceuticals 03 03005Document16 pagesPharmaceuticals 03 03005vigneshkumar.r3850No ratings yet
- Diabetes LinagliptinaDocument7 pagesDiabetes LinagliptinaFatimaNo ratings yet
- An Overview On Tirzepatide, Dual-Targeted Treatment For Diabetes and ObesityDocument6 pagesAn Overview On Tirzepatide, Dual-Targeted Treatment For Diabetes and ObesityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Chapter 1 - IntroductionDocument61 pagesChapter 1 - IntroductionAmir HamzahNo ratings yet
- Role of Dipeptidyl Peptidase-Iv (Dpp-4) Inhibitor in The Management of Type 2 DiabetesDocument16 pagesRole of Dipeptidyl Peptidase-Iv (Dpp-4) Inhibitor in The Management of Type 2 Diabeteshar1977No ratings yet
- لقطة شاشة ٢٠٢١-٠٢-٠٥ في ١.٤٦.٥٧ مDocument2 pagesلقطة شاشة ٢٠٢١-٠٢-٠٥ في ١.٤٦.٥٧ مDr. Emad Elbadawy د عماد البدويNo ratings yet
- IT 5 - Diabetes Melitus & Sindrom Metabolik 1 - YULDocument45 pagesIT 5 - Diabetes Melitus & Sindrom Metabolik 1 - YULAnikusaSaniariNo ratings yet
- Five Steps in Management of DMDocument62 pagesFive Steps in Management of DMarti tyagitaNo ratings yet
- Diabetes Type 2 HassanDocument26 pagesDiabetes Type 2 Hassanyash_acharya007100% (1)
- Ijnpr 10 (4) 227-237Document11 pagesIjnpr 10 (4) 227-237GREESTYNo ratings yet
- Pharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaDocument3 pagesPharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaiajpsNo ratings yet
- A Comprehensive Review and Perspective On Natural Sources As Dipeptidyl Peptidase-4 Inhibitors For Management of DiabetesDocument18 pagesA Comprehensive Review and Perspective On Natural Sources As Dipeptidyl Peptidase-4 Inhibitors For Management of DiabetesPuspaNo ratings yet
- Antidiabetic Drugs. 12 May Modified 2016 of 2015 - 2017 11 17 MayDocument54 pagesAntidiabetic Drugs. 12 May Modified 2016 of 2015 - 2017 11 17 Mayblue sapphireNo ratings yet
- Effi Cacy and Safety of Sitagliptin in The Treatment of Type 2 DiabetesDocument10 pagesEffi Cacy and Safety of Sitagliptin in The Treatment of Type 2 DiabetesAnjeli KhairunnisaNo ratings yet
- Chapter-3 Drug ProfileDocument3 pagesChapter-3 Drug ProfileManish NaharNo ratings yet
- Dipeptidyl Peptidase 4 (DPP-4) Inhibitors For The Treatment of Type 2 Diabetes MellitusDocument12 pagesDipeptidyl Peptidase 4 (DPP-4) Inhibitors For The Treatment of Type 2 Diabetes MellitusAdi PrayogaNo ratings yet
- Linagliptin in Type 2 Diabetes Media Fact Sheet: June 2010Document3 pagesLinagliptin in Type 2 Diabetes Media Fact Sheet: June 2010Mike StevensNo ratings yet
- Drug Interaction DMT2Document12 pagesDrug Interaction DMT2Dhonat FlashNo ratings yet
- Diabetes MellitusDocument30 pagesDiabetes MellitusjohanNo ratings yet
- MPT2081Document11 pagesMPT2081debkantha gopeNo ratings yet
- Mitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic SyndromeDocument9 pagesMitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic Syndromerajesh sumanNo ratings yet
- Insulin and Antidiabetic Drugs: BSC Nursing Online and Offline Lecture SeriesDocument27 pagesInsulin and Antidiabetic Drugs: BSC Nursing Online and Offline Lecture SeriesSayan ChatterjeeNo ratings yet
- Treating Diabetes: Dr. S. P. Mathew M. D. (Med) Ashok HospitalDocument57 pagesTreating Diabetes: Dr. S. P. Mathew M. D. (Med) Ashok HospitalMathew S Peedikayil100% (1)
- Name Accession Number Type Groups Description: Show EntriesDocument14 pagesName Accession Number Type Groups Description: Show EntriesIndrayansah SiahaanNo ratings yet
- Evolution of Gliptins Over The Last 5 Years: Apurba Kumar MukherjeeDocument6 pagesEvolution of Gliptins Over The Last 5 Years: Apurba Kumar MukherjeeHoàng Hải PhạmNo ratings yet
- European Journal of Biomedical AND Pharmaceutical SciencesDocument9 pagesEuropean Journal of Biomedical AND Pharmaceutical SciencesRobert ChristevenNo ratings yet
- The Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in The Management of Type 2 Diabetes: The SURPASS Clinical TrialsDocument15 pagesThe Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in The Management of Type 2 Diabetes: The SURPASS Clinical TrialsLilian Aracely Gaspar caceresNo ratings yet
- 02 - Update Article New Oral Antidiabetic AgentsDocument7 pages02 - Update Article New Oral Antidiabetic AgentsMuhammad Lutfi Al AyubiNo ratings yet
- Incretin PharmDocument3 pagesIncretin PharmSlim SaaryNo ratings yet
- Linagliptin - Farmacology, Efficacy and SafetyDocument7 pagesLinagliptin - Farmacology, Efficacy and SafetyMisaelDominguezNo ratings yet
- Life Cycle Strategic PlanDocument78 pagesLife Cycle Strategic PlanTancheto111No ratings yet
- Meglitinides ProjectDocument10 pagesMeglitinides Projectarmaan kaltaNo ratings yet
- MethylprednisoloneDocument4 pagesMethylprednisoloneadryananestesiNo ratings yet
- FDA Analysis PDFDocument7 pagesFDA Analysis PDFAdson AlcantaraNo ratings yet
- Ozempic Product Monograph PDFDocument59 pagesOzempic Product Monograph PDFAnonymous Complainer0% (1)
- Sitagliptin 1Document2 pagesSitagliptin 1Raju Teach KapsNo ratings yet
- Incretin-Based Therapies: Joshua J. NeumillerDocument23 pagesIncretin-Based Therapies: Joshua J. NeumillerAbulHasan Idrus IstarNo ratings yet
- Mulher in 2011Document10 pagesMulher in 2011Zulvina FaozanudinNo ratings yet
- Profile of Tirzepatide in The Management of Type 2 Diabetes Mellitus: Design, Development, and Place in TherapyDocument13 pagesProfile of Tirzepatide in The Management of Type 2 Diabetes Mellitus: Design, Development, and Place in TherapyDiego Andres Garcia RochaNo ratings yet
- Drug Study ProglinDocument2 pagesDrug Study ProglinChris Denver BancaleNo ratings yet
- Dipeptidyl Peptidase IV (DPP IV) : A Novel Emerging Target For The Treatment of Type 2 DiabetesDocument8 pagesDipeptidyl Peptidase IV (DPP IV) : A Novel Emerging Target For The Treatment of Type 2 DiabetesGREESTYNo ratings yet
- Managent DMT2 KabDocument49 pagesManagent DMT2 KabNoorvita SRNo ratings yet
- Lecture 7 Diabetes Mellitus 2021Document39 pagesLecture 7 Diabetes Mellitus 2021Ahmed ShakerNo ratings yet
- Drug Name Mechanism of Action Indication Side Effects Nursing Reponsibilities Generic NameDocument4 pagesDrug Name Mechanism of Action Indication Side Effects Nursing Reponsibilities Generic NamehahahaNo ratings yet
- Oral Antidiabetic Drugs: Ullmann's Encyclopedia of Industrial ChemistryDocument14 pagesOral Antidiabetic Drugs: Ullmann's Encyclopedia of Industrial ChemistryjaimeNo ratings yet
- Omcij MS Id 555853Document10 pagesOmcij MS Id 555853Drkrishnasarma pathyNo ratings yet
- Drug Study Anthemether Lumefrantine and RifampincineDocument12 pagesDrug Study Anthemether Lumefrantine and RifampincineAnonymous K99UIf1No ratings yet
- Comparison of The Glimepiride Brand Name Medication and Generic Medications in The Simple Suspension Method and Their Dissolution BehaviorDocument8 pagesComparison of The Glimepiride Brand Name Medication and Generic Medications in The Simple Suspension Method and Their Dissolution BehaviorMohammad BakrNo ratings yet
- Antihyperglycemic Effect of Short Term Resveratrol Supplementation in Type Ii Diabetes PatientsDocument28 pagesAntihyperglycemic Effect of Short Term Resveratrol Supplementation in Type Ii Diabetes PatientssowjanyaNo ratings yet
- Incretin-Based Therapy For Diabetes: What A Cardiologist Needs To KnowDocument9 pagesIncretin-Based Therapy For Diabetes: What A Cardiologist Needs To KnowmdmmmNo ratings yet
- St. Paul University Philippines: /almarallag/v01/2020-21Document3 pagesSt. Paul University Philippines: /almarallag/v01/2020-21Suzete PagaduanNo ratings yet
- Pharmacology LectureDocument5 pagesPharmacology LectureAbdullahayad farouqNo ratings yet
- Endocrine PharmacologyDocument42 pagesEndocrine PharmacologyAhmed El SharkawyNo ratings yet
- Pangestuti, Arifin - 2018 - Medicinal and Health Benefit Effects of Functional Sea CucumbersDocument11 pagesPangestuti, Arifin - 2018 - Medicinal and Health Benefit Effects of Functional Sea CucumbersGREESTYNo ratings yet
- PJ 11 4 50Document6 pagesPJ 11 4 50GREESTYNo ratings yet
- Nutritional, Healthical and Therapeutic Efficacy of Black Cumin (Nigella Sativa) in Animals, Poultry and HumansDocument19 pagesNutritional, Healthical and Therapeutic Efficacy of Black Cumin (Nigella Sativa) in Animals, Poultry and HumansGREESTYNo ratings yet
- Pangkey Et Al. - 2012 - Prospect of Sea Cucumber Culture in Indonesia As Potential Food SourcesDocument16 pagesPangkey Et Al. - 2012 - Prospect of Sea Cucumber Culture in Indonesia As Potential Food SourcesGREESTYNo ratings yet
- Journal Pre-Proofs Serum Albumin-Mediated Strategy For The Effective Targeting of Sars-Cov-2Document4 pagesJournal Pre-Proofs Serum Albumin-Mediated Strategy For The Effective Targeting of Sars-Cov-2GREESTYNo ratings yet
- Dipeptidyl Peptidase IV (DPP IV) : A Novel Emerging Target For The Treatment of Type 2 DiabetesDocument8 pagesDipeptidyl Peptidase IV (DPP IV) : A Novel Emerging Target For The Treatment of Type 2 DiabetesGREESTYNo ratings yet
- Review: Zebrafish (Danio Rerio) Sebagai Model Obesitas Dan Diabetes Melitus Tipe 2Document12 pagesReview: Zebrafish (Danio Rerio) Sebagai Model Obesitas Dan Diabetes Melitus Tipe 2GREESTYNo ratings yet
- Chemopreventive Effect of Xanthorrhizol From: Curcuma XanthorrhizaDocument7 pagesChemopreventive Effect of Xanthorrhizol From: Curcuma XanthorrhizaGREESTYNo ratings yet
- Potensi Temulawak SBG Agen Antivirus Covid-19Document10 pagesPotensi Temulawak SBG Agen Antivirus Covid-19GREESTYNo ratings yet
- Wang Shilei, 2020Document8 pagesWang Shilei, 2020GREESTYNo ratings yet
- Collagen Animal Sources and Biomedical ApplicationDocument5 pagesCollagen Animal Sources and Biomedical ApplicationDanielGonzalezNo ratings yet
- 1688 3737 1 PB PDFDocument4 pages1688 3737 1 PB PDFputri firda erlinaNo ratings yet
- Aphrodisiac Effect of Areca Catechu L. and Pedalium Murex in RatsDocument6 pagesAphrodisiac Effect of Areca Catechu L. and Pedalium Murex in RatsGREESTYNo ratings yet
- 1207-Article Text-3856-2-10-20210722Document4 pages1207-Article Text-3856-2-10-20210722GREESTYNo ratings yet
- Curcuma Anti KankerDocument4 pagesCurcuma Anti KankerTrisnawati AmaliaNo ratings yet
- Titrasi IodometriDocument42 pagesTitrasi IodometriGREESTYNo ratings yet
- Bioactive Proteins in Channa Striata Promote Wound Healing Through Angiogenesis and Cell ProliferationDocument12 pagesBioactive Proteins in Channa Striata Promote Wound Healing Through Angiogenesis and Cell ProliferationGREESTYNo ratings yet
- Hyperalbuminemia and Elevated Transaminases Associated With High Protein DietDocument3 pagesHyperalbuminemia and Elevated Transaminases Associated With High Protein DietGREESTYNo ratings yet
- 1 s2.0 S0006291X04025331 MainDocument8 pages1 s2.0 S0006291X04025331 MainGREESTYNo ratings yet
- The Alkaloid Contents of Sixty Nzcotzmva Species: Phyrochemufry, Vol 24, No 3, PP 477-480, 1985 Pnnted UtDocument4 pagesThe Alkaloid Contents of Sixty Nzcotzmva Species: Phyrochemufry, Vol 24, No 3, PP 477-480, 1985 Pnnted UtGREESTYNo ratings yet
- Comparative Evaluation of Polysaccharides Isolated From As-Tragalus, Oyster Mushroom, and Yacon As Inhibitors ofDocument4 pagesComparative Evaluation of Polysaccharides Isolated From As-Tragalus, Oyster Mushroom, and Yacon As Inhibitors ofGREESTYNo ratings yet
- The Antioxidant Properties of Serum Albumin: MinireviewDocument5 pagesThe Antioxidant Properties of Serum Albumin: MinireviewGREESTYNo ratings yet
- Neuroprotective Effects of Moringa Oleifera Leaf ExtractDocument11 pagesNeuroprotective Effects of Moringa Oleifera Leaf ExtractGREESTYNo ratings yet
- Immunomodulator Effect of RiceDocument4 pagesImmunomodulator Effect of RiceGREESTYNo ratings yet
- The Use of Phyllanthus Niruri L As An ImmunomodulaDocument10 pagesThe Use of Phyllanthus Niruri L As An ImmunomodulaMuhammad Arif MahfudinNo ratings yet
- Moringa Oleifera:: A Review On Nutritive Importance and Its Medicinal ApplicationDocument8 pagesMoringa Oleifera:: A Review On Nutritive Importance and Its Medicinal ApplicationIndah TaemintshawolNo ratings yet
- Channa Striata PDFDocument9 pagesChanna Striata PDFM Husni MubarokNo ratings yet
- Albumin Biochemical and Therapeutic EffextDocument9 pagesAlbumin Biochemical and Therapeutic EffextGREESTYNo ratings yet
- Albumin and Its Application in Drug DeliveryDocument20 pagesAlbumin and Its Application in Drug DeliveryGREESTYNo ratings yet
- Neuroprotective Effects of Moringa Oleifera Leaf ExtractDocument11 pagesNeuroprotective Effects of Moringa Oleifera Leaf ExtractGREESTYNo ratings yet
- Concept PaperDocument12 pagesConcept Paperjlventigan100% (1)
- Exercise Tolerance TestDocument15 pagesExercise Tolerance TestahmedNo ratings yet
- Therapeutic Management of Clinical Mastitis in Goat: A Case StudyDocument5 pagesTherapeutic Management of Clinical Mastitis in Goat: A Case StudyIJAR JOURNALNo ratings yet
- Case Presentation: - Vuppu BhavaniDocument53 pagesCase Presentation: - Vuppu BhavaniLohith Kumar MenchuNo ratings yet
- Yaman Walid KassabDocument282 pagesYaman Walid KassabHeryanti PusparisaNo ratings yet
- Long-Term Evaluation of Periodontal TherapyDocument16 pagesLong-Term Evaluation of Periodontal TherapyRanuch TakNo ratings yet
- T2DM PracticalGuide 20190718 FA Ebook2Document80 pagesT2DM PracticalGuide 20190718 FA Ebook2Nokoline HuNo ratings yet
- TALLY 79 Respondents FinalDocument7 pagesTALLY 79 Respondents FinalMarissa AsimNo ratings yet
- The Prevention and Cure Effects of Aspirin Eugenol Ester On Hyperlipidemia and Its MetabonomicsDocument108 pagesThe Prevention and Cure Effects of Aspirin Eugenol Ester On Hyperlipidemia and Its MetabonomicsKavisa GhoshNo ratings yet
- Antenatal CareDocument13 pagesAntenatal CareOjambo Flavia50% (2)
- Obstetric Nursing Study GuideDocument69 pagesObstetric Nursing Study GuideValerie100% (3)
- Canine and Feline Skin Cytology - A Comprehensive and Illustrated Guide To The Interpretation of Skin Lesions Via Cytological ExaminationDocument535 pagesCanine and Feline Skin Cytology - A Comprehensive and Illustrated Guide To The Interpretation of Skin Lesions Via Cytological ExaminationCandelaria Rosa Alvarez100% (2)
- Intestinal and Colonic Physiology and Biochemistry (Part 2 - Secretion, Digestion, Absorption) (Slides With Notes)Document69 pagesIntestinal and Colonic Physiology and Biochemistry (Part 2 - Secretion, Digestion, Absorption) (Slides With Notes)kuchipuchi12No ratings yet
- Jaw Fractures Managing The Whole PatientDocument2 pagesJaw Fractures Managing The Whole PatientElisa BaronNo ratings yet
- 2021 Va Ers DataDocument1,788 pages2021 Va Ers DataasdasdasdNo ratings yet
- EBMDocument6 pagesEBMjoyce_garcia_10No ratings yet
- Gastric GavageDocument3 pagesGastric GavageRico Delgado of WorldbexNo ratings yet
- ANEXA Nr. 9 Certificat Medical Medical Fitness CertificateDocument1 pageANEXA Nr. 9 Certificat Medical Medical Fitness CertificatePrisacaru MarianNo ratings yet
- Acute Complications of Diabetes Mellitus: Hypoglycemia and Hypoglycemic ComaDocument30 pagesAcute Complications of Diabetes Mellitus: Hypoglycemia and Hypoglycemic ComaCristinaGheorgheNo ratings yet
- Clinical Pharma 2Document156 pagesClinical Pharma 2RebwarNo ratings yet
- Complete Medical TermsDocument32 pagesComplete Medical TermsSharifa Darayan100% (1)
- Thrombocytopenia: Decreased Production Increased Destruction Sequestration PseudothrombocytopeniaDocument43 pagesThrombocytopenia: Decreased Production Increased Destruction Sequestration PseudothrombocytopeniaDea Tasha MeicitaNo ratings yet
- BIOLOGYDocument5 pagesBIOLOGYDiana NurulNo ratings yet
- Hematology Unit: Complete Blood Count (CBC)Document2 pagesHematology Unit: Complete Blood Count (CBC)Rasha ElbannaNo ratings yet
- Drugs For Diarrhea and ConstipationDocument24 pagesDrugs For Diarrhea and ConstipationFaddi BoyNo ratings yet
- Insuficienta Renala Acuta, Leziunea Acuta RenalaDocument40 pagesInsuficienta Renala Acuta, Leziunea Acuta RenalaLeoveanu MirelNo ratings yet
- Anti Diare SGDocument17 pagesAnti Diare SGludoy03No ratings yet
- Immature GranulocytesDocument10 pagesImmature Granulocytespieterinpretoria391No ratings yet
- Osteoconduction and OsteoinductionDocument6 pagesOsteoconduction and OsteoinductiontofssbiNo ratings yet
- Pathology Review BookDocument5 pagesPathology Review BookAnas AliagaNo ratings yet