Professional Documents
Culture Documents
HIF-1 Mediates Pathogenic Inflammatory Responses To Intestinal Ischemia-Reperfusion Injury
HIF-1 Mediates Pathogenic Inflammatory Responses To Intestinal Ischemia-Reperfusion Injury
Uploaded by
Yusrinabilla -Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HIF-1 Mediates Pathogenic Inflammatory Responses To Intestinal Ischemia-Reperfusion Injury
HIF-1 Mediates Pathogenic Inflammatory Responses To Intestinal Ischemia-Reperfusion Injury
Uploaded by
Yusrinabilla -Copyright:
Available Formats
Am J Physiol Gastrointest Liver Physiol 299: G833–G843, 2010.
First published August 5, 2010; doi:10.1152/ajpgi.00065.2010.
HIF-1 mediates pathogenic inflammatory responses to intestinal
ischemia-reperfusion injury
Rena Feinman,1 Edwin A. Deitch,1 Anthony C. Watkins,1 Billy Abungu,1 Iriana Colorado,1
Kolenkode B. Kannan,1 Sharvil U. Sheth,1 Francis J. Caputo,1 Qi Lu,1 Madhuri Ramanathan,1
Shirhan Attan,1 Chirag D. Badami,1 Danielle Doucet,1 Dimitrios Barlos,1 Marta Bosch-Marce,2
Gregg L. Semenza,2 and Da-Zhong Xu1
1
Department of Surgery, University of Medicine and Dentistry of New Jersey-New Jersey Medical School, Newark, New
Jersey; and 2Vascular Program, Institute for Cell Engineering, and McKusick-Nathans Institute of Genetic Medicine, John
Hopkins University School of Medicine, Baltimore, Maryland
Submitted 17 February 2010; accepted in final form 27 July 2010
Feinman R, Deitch EA, Watkins AC, Abungu B, Colorado I, generated several working hypotheses, one of which is the gut
Kannan KB, Sheth SU, Caputo FJ, Lu Q, Ramanathan M, Attan S, hypothesis of MODS. A key element in the gut hypothesis of
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
Badami CD, Doucet D, Barlos D, Bosch-Marce M, Semenza GL, MODS is that a splanchnic ischemia-reperfusion (I/R) insult
Xu D. HIF-1 mediates pathogenic inflammatory responses to leading to gut inflammation and loss of barrier function is the
intestinal ischemia-reperfusion injury. Am J Physiol Gastroin- initial triggering event that turns the gut into the “motor” of
test Liver Physiol 299: G833–G843, 2010. First published August
MODS (19). However, the exact mechanisms by which gut I/R
5, 2010; doi:10.1152/ajpgi.00065.2010.—Acute lung injury (ALI)
and the development of the multiple organ dysfunction syndrome leads to intestinal injury and how an intestinal ischemic insult
(MODS) are major causes of death in trauma patients. Gut inflam- is transduced into a systemic inflammatory response remains
mation and loss of gut barrier function as a consequence of splanchnic incomplete. To date, the majority of the molecular and cellular
ischemia-reperfusion (I/R) have been implicated as the initial trigger- studies investigating shock-induced gut injury and gut-induced
ing events that contribute to the development of the systemic inflam- MODS have focused primarily on the reperfusion phase of the
matory response, ALI, and MODS. Since hypoxia-inducible factor intestinal I/R insult and the consequent production of proin-
(HIF-1) is a key regulator of the physiological and pathophysiological flammatory mediators such as inducible nitric oxide synthase
response to hypoxia, we asked whether HIF-1 plays a proximal role in (iNOS)-derived nitric oxide (22), reactive oxygen species,
the induction of gut injury and subsequent lung injury. Utilizing cytokines (IL-6) (48), transcription factors (NF-B, AP-1)
partially HIF-1␣-deficient mice in a global trauma hemorrhagic shock (72), cyclooxygenase-2 (COX-2) (31), and poly(ADP-ribose)
(T/HS) model, we found that HIF-1 activation was necessary for the polymerase (44). Yet, because the induction of many of these
development of gut injury and that the prevention of gut injury was
factors is secondary to or accentuated by hypoxia and because
associated with an abrogation of lung injury. Specifically, in vivo
studies demonstrated that partial HIF-1␣ deficiency ameliorated ischemia precedes reperfusion, it seemed likely that the mo-
T/HS-induced increases in intestinal permeability, bacterial translo- lecular response triggered by the ischemic component of the
cation, and caspase-3 activation. Lastly, partial HIF-1␣ deficiency I/R insult is a critical step in initiating the sequence of events
reduced TNF-␣, IL-1, cyclooxygenase-2, and inducible nitric oxide that lead to the development of gut injury and MODS.
synthase levels in the ileal mucosa after T/HS whereas IL-1 mRNA The adaptive response to hypoxia or ischemia has been
levels were reduced in the lung after T/HS. This study indicates that shown to be primarily regulated by hypoxia-inducible factor
prolonged intestinal HIF-1 activation is a proximal regulator of (HIF-1). The HIF-1 heterodimer consists of an oxygen-labile
I/R-induced gut mucosal injury and gut-induced lung injury. Conse- HIF-1␣ subunit and a constitutively expressed HIF-1 subunit
quently, these results provide unique information on the initiating that mediates a wide spectrum of physiological and cellular
events in trauma-hemorrhagic shock-induced ALI and MODS as well adaptive responses such as angiogenesis, metabolic adaption,
as potential therapeutic insights. erythropoiesis, and vascular tone (67). In the presence of
hemorrhagic shock; inflammation; multiple organ dysfunction syn- oxygen, prolyl hydroxylation of the oxygen-dependent degra-
drome; acute lung injury dation domain of HIF-1␣ marks it for ubiquitin-proteasomal
degradation (34, 36) and asparaginyl hydroxylation of the
COOH-terminal transactivation domain of HIF-1␣ prevents
IN PATIENTS SUSTAINING major trauma, the development of the interaction with the transcriptional coactivator p300 (42, 47).
systemic inflammatory response syndrome (SIRS) and multi- In the context of ischemic injury, HIF-1 was originally
ple organ dysfunction (MODS) is a major clinical problem shown to protect organs that are highly sensitive to energy
resulting in 50 – 80% of all deaths in surgical intensive care deprivation such as the brain, heart, and kidney from ischemic
units. Since the pathophysiology of this syndrome remains damage in I/R preconditioning models (23). Thus one accepted
incompletely understood and therapy remains largely support- role for HIF-1 is that it acts as an adaptive and survival factor
ive (16), studies focusing on the basic biology of trauma- for cells exposed to hypoxia or cells undergoing stress such as
induced SIRS, organ injury/dysfunction, and MODS have been ischemic injury, especially in models of ischemic precondition-
major areas of investigation. These mechanistic studies have ing (23, 45). However, in response to prolonged ischemic
stress as well as in various nonpreconditioning models, HIF-1
Address for reprint requests and other correspondence: R. Feinman,
may be deleterious because of its ability to augment both
UMDNJ-New Jersey Medical School, Dept. of Surgery, 185 South Orange apoptotic (1, 26) and inflammatory processes (13, 45), espe-
Ave. MSB-G594, Newark, NJ 07103 (e-mail: feinmarr@umdnj.edu). cially via upregulation of iNOS. In fact, our earlier studies
http://www.ajpgi.org 0193-1857/10 Copyright © 2010 the American Physiological Society G833
G834 HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY
demonstrated that the in vivo intestinal mucosal response to gut vein until a mean arterial pressure (MAP) between 35 and 40 mmHg
I/R was associated with a prolonged increase in HIF-1␣ ex- was obtained and maintained for 60 min. After 60 min, the mice were
pression that was not rapidly lost during reperfusion when the resuscitated with their shed blood for 3 h. Sham-shock animals (T/SS)
gut becomes reoxygenated (41). These results were surprising underwent cannulation of the femoral artery and jugular vein followed
by a laparotomy; however, no blood was withdrawn and the MAP was
since cellular HIF-1 levels rapidly decrease to normoxic levels
kept within normal limits.
within minutes of reoxygenation (32). This relatively unique Morphological analysis of gut and lung injury. At euthanasia,
prolonged HIF-1␣ response to I/R in the intestine appeared to terminal ileum or lung was fixed in 10% buffered formalin, processed,
be mediated by bacteria and bacterial products within the gut stained with hematoxylin and eosin, and examined by light micros-
lumen coming into direct contact with the stressed intestinal copy. For each animal, the percentage of villous injury was a gross
mucosa (41). In this study, we hypothesized that prolongation assessment of the number of damaged villus tips per 200 villus tips
of the intestinal HIF-1 response could be potentially maladap- (⬃20 –25 visual fields at ⫻100 magnification), which ranged from
tive or injurious and contribute to loss of gut barrier function blunting and vacuolation of villus tips to denuded villi and mucosal
and the development of distant organ injury. Using partially ulceration. According to the grading systems for villous injury as
HIF-1␣-deficient mice, we tested the functional significance of described by Refs. 9, 49, 74, the numerical scores were the following:
HIF-1 in a trauma hemorrhagic shock (T/HS)-mediated gut I/R 0 ⫽ normal mucosa, 1 ⫽ development of subepithelial Gruenhagen’s
space and vacuolization at the villus tip, 2 ⫽ extension of the
injury model.
subepithelial space with moderate lifting of epithelial layer from the
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
MATERIALS AND METHODS lamina propria, 3 ⫽ massive subepithelial lifting/sloughing and in-
creased vacuolization from the tip to midportion of villi, 4 ⫽ epithelial
Mice. The generation and genotyping of HIF-1␣⫹/⫺ and HIF- lifting and vacuolization from the tip to lower portion of villi, and 5 ⫽
⫹/⫹ mucosal ulceration and disintegration of the lamina propria (Fig. 1).
1␣ mice on a C57B6/129 genetic background was described
previously (35) and provided by G. L. Semenza (John Hopkins Similarly, lung injury was determined by using a modified lung injury
University School of Medicine, Baltimore, MD). All animal proce- grading scale (10) that assessed the magnitude of interstitial edema
dures were approved by the University of Medical and Dentistry of (0 –2), pulmonary edema (0 –2), and alveolar integrity (0 –1). In this
New Jersey Animal Care and Use Committee and maintained in grading system, 0 indicates no injury and the lung injury score is
accordance with the recommendations of the “National Institutes of calculated by adding the injury grades of each component (maximal
Health Guide for Care and Use of Laboratory Animals.” lung injury score is 5). All slides were evaluated by two examiners in
T/HS model. Male mice were anesthetized with pentobarbital a blinded fashion.
(60 – 80 mg/kg ip) and under strict asepsis, a 2.5-cm midline laparot- In vivo intestinal permeability assay. Under anesthetized condi-
omy was performed. Isoflurane was given if needed to maintain tions, at 30 min before euthanasia, a 5-cm segment of distal ileum was
surgical level of anesthesia. Blood was withdrawn from the jugular isolated, beginning at 3 cm proximal to the cecum and bilateral end of
Fig. 1. Histological criteria used to grade villous damage following trauma hemorrhagic shock (T/HS). 0 ⫽ normal mucosa, 1 ⫽ development of subepithelial
Gruenhagen’s space and vacuolization at the villus tip, 2 ⫽ extension of the subepithelial space with moderate lifting of epithelial layer from the lamina propria,
3 ⫽ massive subepithelial lifting/ sloughing and increased vacuolization from the tip to midportion of villi, 4 ⫽ epithelial lifting and vacuolization from the tip
to lower portion of villi, and 5 ⫽ mucosal ulceration and disintegration of the lamina propria. The shorter arrows depict the presence of vacuoles, the longer
arrows depict the subepithelial and epithelial lifting, and the stars depict mucosal ulceration. Magnification ⫻400.
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY G835
ileum, and then ligated with a 4-0 silk suture to prevent leakage of at 37°C. The colonies were counted on the plates and recorded as the
4.4-kDa fluorescein isothiocyanate-dextran (FD-4; Sigma-Aldrich). number of colony forming units per gram of MLN.
PBS (200 l) containing 25 mg/ml FD-4 was injected into the lumen, Real-time PCR. Total RNA was prepared from ileal mucosa or lung
which was returned to the abdominal cavity and then closed. After 30 tissue by using the RNeasy kit (Qiagen) and cDNA synthesis was
min, the mouse was euthanized and a blood sample (100 l) was taken reverse transcribed by using the high-capacity cDNA reverse tran-
by cardiac puncture. The concentration of FD-4 in the plasma was scription kit (Applied Biosystems) according to manufacturer’s pro-
measured by a fluorescence spectrophotometer. tocols. cDNA was then amplified with TaqMan gene expression
MPO activity. Frozen ileal mucosa and lung tissue was homoge- Master Mix and predesigned TaqMan probes for murine GLUT1,
nized and processed for myeloperoxidase (MPO) activity measure- COX-2, TNF-␣, IL-1, IL-6, and IL-10 as recommended by Applied
ment as previously described (73). The MPO activity in these super- Biosystems. Within each experimental group, mRNA expression was
natants was determined by measuring the H2O2-mediated oxidation of normalized to 18S amplification (⌬Ct) and then fold changes in
o-dianisidine hydrochloride at 460 nm. MPO activity was determined expression relative to wild-type (WT) T/SS (⌬⌬Ct) was determined
by using a standard curve from MPO derived from human leukocytes by use of 2⫺(⫺⌬⌬Ct) (54).
(Sigma Aldrich) and normalized to milligrams of protein determined Western blotting. Whole cell extracts prepared from ileal mucosal
by bicinchoninic acid protein assay (Pierce). scrapings as described (41) were resolved by SDS-PAGE and detected
Bacterial translocation. The mesenteric lymph node (MLN) com- by Western blotting. The following antibodies were used: iNOS,
plex was harvested and the level of translocating bacterial quantified HIF-1␣ (BD Biosciences), cleaved Asp175 caspase-3, p42/p44 (Cell
as previously described (17). Briefly, using sterile technique, the MLN Signaling), and HIF-1␣ (Novus Biologicals). As reported by others
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
complex was harvested, weighed, and homogenized in 0.2 ml of (38), total p42/p44 was used as a our loading control since the
sterile saline. Aliquots were plated onto both blood and MacConkey expression of commonly used loading controls such as actin and
agar plates. These plates were examined at 24 h of aerobic incubation tubulin have been shown to be altered in tissues of animals subjected
Fig. 2. Induction of hypoxia-inducible factor
(HIF)-1␣- and HIF-1-dependent genes in the
ileal mucosa after T/HS. Wild-type (WT) and
HIF-1␣⫹/⫺ mice were subjected to T/HS or
sham shock (T/SS) for 60 min and 3 h reper-
fusion. A: relative levels of HIF-1␣, GLUT1,
and cyclooxygenase-2 (COX-2) mRNA levels
in the ileal mucosa were determined by real-
time PCR using the ⌬⌬Ct method by using a
log2 scale. Mean values ⫾ SE are shown (n ⫽
4 –15 mice/group). B: whole cell extracts
(WCEs) prepared from mucosal scrapings
from the distal ileum were examined for HIF-
1␣, inducible nitric oxide synthase (iNOS),
and total MAPK expression by Western blot
analysis. A nonspecific (NS) band (70 kDa)
recognized by iNOS antibody also confirmed
equal loading of our samples. Numbers refer to
individual mice.
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
G836 HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY
to I/R injury (63) and intestinal cytoskeleton degradation has been ANOVA analysis followed by Tukey-Kramer or Newman-Keuls. For
shown to precede tight junction loss (64). Ponceau S staining of the lung injury score and real-time PCR analysis, data were analyzed by
membranes was also done to validate transfer efficiency as well as Mann-Whitney test and bacterial translocation by 2 analysis with
equal protein loading. The Western blots were developed with Immo- Fisher exact test. P values less than 0.05 were considered statistically
bilon Western chemiluminescent HRP substrate (Millipore) and ana- significant.
lyzed by densitometry using an AlphaImager 3400 imaging system
and AlphaEase FC software (Alpha Innotech).
RESULTS
Caspase-3 activity and caspase-3/7 activity assays. For in vivo
studies, caspase-3 activity was determined according to the instruc- Partial HIF-1␣ deficiency attenuates gut and lung I/R
tions provided by the caspase-3/CPP32 colorimetric assay kit with
DEVD-pNA substrate (Biovision). For in vitro studies, caspase-3/7
injury. To establish the functional significance of HIF-1 in gut
was determined according to the instructions provided by the I/R injury, we utilized mice that were heterozygous for a
sensoLyte homogenous Rh110 caspase-3/7 assay kit (AnaSpec). knockout allele at the HIF-1␣ locus (HIF-1␣⫹/⫺) in a com-
Generation of HIF-1␣ stable transfectants. Using the Nucleofector bined T/HS model. The T/HS model (laparotomy plus 60 min
T kit (Amaxa), Caco-2 cells (ATCC) were nucleofected with p of hemorrhagic shock at 35– 40 mmHg) and 3 h of reperfusion
(HA)HIF-1␣ or pcDNA3 (empty) expression vector provided by H. F. represents a global I/R injury. The addition of a laparotomy is
Bunn (Harvard Medical School, Boston, MA). Pools of HIF-1␣ or important because tissue injury is a component of traumatic
control Caco-2 stable transfectants were selected in the presence of hemorrhage and the combined insult of hemorrhage and tissue
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
G418 (1 mg/ml) for 14 days. To confirm HIF-1␣ expression, control injury results in an inflammatory response that more closely
and HIF-1␣ transfectants were starved overnight in DMEM contain-
ing 0.1% FBS and exposed to normoxia or hypoxia (1% O2) for 3 h mimics the clinical situation than hemorrhage alone (15). We
as described (41). first determined the effects of T/HS on the induction of HIF-1␣
Statistical analysis. Statistical significance among groups for vil- mRNA and protein expression in the ileal mucosa of WT and
lous injury, in vivo intestinal permeability, polymorphonuclear cell HIF-1␣⫹/⫺ mice. As shown in Fig. 2A, real-time PCR analysis
(PMN) infiltration, and MPO activity was determined by one-way demonstrated a modest increase in mucosal HIF-1␣ expression
Fig. 3. Partial HIF-1␣ deficiency attenuates T/HS-induced gut injury. WT and HIF-1␣⫹/⫺ mice were subjected to T/HS or T/SS for 60 min and 3 h reperfusion.
A: representative sections of hematoxylin and eosin (H&E) staining of the distal ileum (⫻200). Arrows depict subepithelial lifting sloughing and mucosal edema
in the villi. B: percentage of villous injury. C: histological scoring of villous damage. Values in B and C are expressed as means ⫾ SE (n ⫽ 7–11 mice/group).
D: MPO activity (U/mg of protein) was measured in the ileal mucosa. Values are expressed as means ⫾ SE (n ⫽ 5–10 mice/group).
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY G837
in WT mice subjected to T/HS compared with their T/SS subepithelial lifting, mucosal edema, and sloughing in WT
counterparts. In contrast, HIF-1␣ expression was not evident in mice subjected to T/HS whereas the ileal mucosa of the
HIF-1␣⫹/⫺ mice after T/HS. T/HS was also capable of induc- T/HS-challenged HIF-1␣⫹/⫺ mice had minimal mucosal dam-
ing the expression of two HIF-1 targets, GLUT1 and COX-2, age and resembled the T/SS groups, regardless of genotype.
in WT but not HIF-1␣⫹/⫺ mice after T/HS. In agreement with The magnitude of T/HS-induced villous injury was approxi-
earlier studies (5, 35, 52), the baseline mRNA levels of HIF-1␣ mately fourfold greater in WT mice than in HIF-1␣⫹/⫺ mice
were significantly lower in the T/SS group of HIF-1␣⫹/⫺ (Fig. 3B). Although the percentage of villous injury in HIF-
relative to the T/SS WT group. Consistent with these findings, 1␣⫹/⫺ mice was the same for T/SS and T/HS groups, the
both HIF-1␣ and iNOS protein levels were increased in the percentage of villous injury was twofold higher in the HIF-
ileal mucosa of WT mice after T/HS compared with T/SS- 1␣⫹/⫺ mice subjected to T/SS as compared its WT counterpart.
operated mice (Fig. 2B). In contrast, the HIF-1␣ and iNOS The villous injury score was also markedly higher in WT than
responses were markedly lower in the ileal mucosa of HIF- HIF-1␣⫹/⫺ mice after T/HS (Fig. 3C). We also determined
1␣⫹/⫺ mice after T/HS. Negligible HIF-1␣ and iNOS protein whether HIF-1 modulated the sequestration of PMN into the
levels were detected in WT or HIF-1␣⫹/⫺ mice subjected to ileal mucosa after T/HS. Although MPO levels were extremely
T/SS. We chose to characterize the iNOS response since iNOS low in the ileal mucosa, T/HS elevated MPO levels in WT
has been identified as a HIF-1 target and is a key effector in the mice by approximately threefold compared with their T/SS
pathophysiology of gut barrier failure during shocked states. counterpart (P ⬍ 0.02; Fig. 3D). However, there was no
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
These findings are in agreement with earlier studies demon- difference between MPO levels in HIF-1␣⫹/⫺ mice subjected
strating reduced expression of endogenous HIF-1␣ protein and to T/SS and T/HS.
downstream targets in HIF-1␣⫹/⫺ cells under hypoxic condi- On the basis of earlier studies demonstrating that T/HS-
tions (5, 35, 52) and HIF-1␣⫹/⫺ mice manifesting impaired induced gut injury leads to the development of a systemic
physiological responses to ischemia and hypoxia (5, 52, 60). inflammatory response and lung injury, we asked whether
Since our findings demonstrated that T/HS induced an in- HIF-1 played a maladaptive role in T/HS-induced lung injury.
testinal HIF-1␣ response, we assessed the effect of partial As a consequence of T/HS, loss of alveolar integrity, increased
HIF-1␣ deficiency on T/HS-induced villous injury. Histologi- inflammation, and red blood cell congestion are evident in the
cal sections of the ileal mucosa (Fig. 3A) showed evidence of lungs of WT mice but not of HIF-1␣⫹/⫺ mice (Fig. 4A). No
Fig. 4. Partial HIF-1␣ deficiency attenuates T/HS-induced lung injury. WT and HIF-1␣⫹/⫺ mice were subjected to T/HS or T/SS for 60 min and 3 h reperfusion.
A: representative section of H&E staining of the lung. B: lung injury score. C: number of infiltrating polymorphonuclear cells (PMNs) per high-power field (hpf).
D: MPO activity (U/mg of protein) was measured in the lung. Values in B–D are expressed as means ⫾ SE (n ⫽ 6 –13 mice/group).
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
G838 HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY
evidence of lung injury is seen in WT or HIF-1␣⫹/⫺ mice contrast, no translocation was evident in HIF-1␣⫹/⫺ mice after
subjected to T/SS. The lung injury score (Fig. 4B), the number T/HS and as expected no translocation was found in either WT
of infiltrating PMN per high-power field (Fig. 4C), and MPO or HIF-1␣⫹/⫺ mice after T/SS. Taken together, our findings
levels (Fig. 4D) were markedly elevated in WT mice subjected suggest that partial HIF-1␣ deficiency ameliorated intestinal
to T/HS compared with T/SS. In contrast, there was no signif- barrier dysfunction during T/HS, thereby supporting the con-
icant difference in lung injury and PMN influx in the lungs of cept that HIF-1 mediates gut injury.
HIF-1␣⫹/⫺ mice subjected to T/HS or T/SS. Thus partial HIF-1 promotes apoptosis during gut I/R injury. We next
HIF-1␣ deficiency significantly attenuated T/HS-induced gut studied caspase-3 activation since it has been implicated in gut
and lung injury, thereby supporting the concept that elevation injury models of T/HS (39, 40), hypoxia (20), and ischemia (7,
of HIF-1␣ after gut I/R is deleterious and contributes to both 25) and the caspase-3 promoter contains a functional HIF-1
local gut and distant lung organ damage. response element (65). A significant decrease in the cleavage
Persistent HIF-1 activation is linked to loss of gut barrier of caspase-3 (Fig. 6, A and B) and caspase-3/7 activity (Fig.
function. Since functional studies of intestinal barrier function 6C) was found in the ileal mucosa of HIF-1␣⫹/⫺ mice sub-
have demonstrated that intestinal permeability increases after jected to T/HS compared with their WT counterparts. Simi-
gut I/R (57, 70), we tested the hypothesis that HIF-1␣ activa- larly, a progressive increase in caspase-3 activity was found in
tion contributes to T/HS-induced increased intestinal perme- our HIF-1␣ Caco-2 transfectants exposed to normoxia, hyp-
ability. With use of an in vivo FD-4 intestinal permeability oxia, or hypoxia/reoxygenation compared with control Caco-2
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
assay, T/HS increased intestinal permeability by 3.8-fold in transfectants (Fig. 6D). These findings suggest that HIF-1 also
WT mice compared with their T/SS counterparts (Fig. 5A). manifests a proapoptotic role during T/HS-induced gut injury.
However, T/HS was only capable of increasing intestinal HIF-1 differentially regulates proinflammatory cytokines in
permeability by 1.8-fold in HIF-1␣⫹/⫺ mice vs. their T/SS the ileal mucosa and lung after T/HS. In T/HS models, loss of
counterparts. The baseline level of intestinal permeability for gut barrier function has been associated with a gut inflamma-
the T/SS HIF-1␣⫹/⫺ group was approximately twofold higher tory response (18, 21). The translocation of bacteria or their
than the WT T/SS group (P ⬍ 0.05). products have also been shown to trigger or sustain gut inflam-
Consistent with these results, bacterial translocation to the mation (21, 62), and our recent studies have demonstrated that
mesenteric lymph node was markedly increased in WT mice bacteria and LPS upregulated HIF-1 expression in intestinal
subjected to T/HS relative to their T/SS group (Fig. 5B). In epithelial cells under normoxic conditions (41). Given that
HIF-1 is capable of modulating the innate immune and inflam-
matory responses in hematopoietic and nonhematopoietic cells,
we determined whether HIF-1 activation modulated the intes-
tinal and lung inflammatory response after T/HS. As shown in
Fig. 7, T/HS increased TNF-␣ and IL-1 mRNA levels in the
ileal mucosa of WT mice compared with their T/SS group (P ⬍
0.007 and P ⬍ 0.05, respectively). In contrast, partial HIF-1␣
deficiency attenuated the induction of mucosal TNF-␣ and
IL-1 gene expression after T/HS compared with WT mice
after T/HS (P ⬍ 0.05). Ileal IL-6 gene expression was not
modulated after T/HS in either genotype, but its baseline level
of expression as well as IL-1 were significantly lower in
HIF-1␣⫹/⫺ mice than in WT mice (P ⬍ 0.05). We then asked
whether HIF-1 activation affected the pulmonary inflammatory
response. Lung TNF-␣, IL-1, and IL-6 levels were markedly
higher in WT mice after T/HS. However, in contrast to the
intestinal inflammatory response, only the increase in T/HS-
induced lung IL-1 expression was prevented in HIF-1␣⫹/⫺
mice (P ⬍ 0.03). IL-10 levels were also measured to determine
whether T/HS induced higher levels of IL-10 in HIF-1␣⫹/⫺
mice compared with WT mice since IL-10 was described as an
anti-inflammatory cytokine (46, 68). IL-10 levels were equally
elevated in both the ileum and lungs of WT and HIF-1␣⫹/⫺
mice subjected to T/HS compared with their T/SS counterparts.
Thus the attenuation of gut and subsequent lung injury by
partial HIF-1␣ deficiency was not due to an increased IL-10
Fig. 5. HIF-1 directly impairs gut barrier function. A: in vivo intestinal response. Taken together, our results suggest that HIF-1 dif-
permeability was assessed in WT and HIF-1␣⫹/⫺ mice subjected to T/SS or ferentially regulates intestinal and lung-derived inflammation
T/HS for 60 min and 3 h reperfusion by quantifying 4.4-kDa fluorescein after T/HS.
isothiocyanate-dextran (FD-4) concentration (g/ml) in the serum. Values are
expressed as means ⫾ SE (n ⫽ 5– 8 mice/group). B: bacterial translocation to
the mesenteric lymph nodes (MLN) was measured in WT and HIF-1␣⫹/⫺ mice DISCUSSION
subjected to T/SS or T/HS. Number of colony forming units of bacteria per
gram MLN (CFU/g) and values are expressed as means ⫾ SD (n ⫽ 6 – 8 The major observation of the present work is that prolonged
mice/group). HIF-1 activation significantly contributes to splanchnic ische-
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY G839
Fig. 6. HIF-1 promotes apoptosis during gut isch-
emia-reperfusion (I/R) injury. A and B: WCEs
were prepared from ileal mucosa of WT and HIF-
1␣⫹/⫺ mice subjected to T/HS or T/SS for 60 min
and 3 h reperfusion. A: cleaved caspase-3 and total
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
p42/p44 expression was determined by Western
blotting. B: densitometry was performed to quan-
tify cleaved caspase-3 and total p42/p44 expres-
sion. Data are represented as means ⫾ SE (4 – 6
mice/group). C: caspase-3 activity is expressed as
absorbance at 405 nm per 50 g of protein. Values
are expressed as means ⫾ SE (n ⫽ 4 –5/group).
D: caspase-3/7 activity assay using WCEs derived
from HIF-1␣ and control (Ctl) Caco-2 transfec-
tants exposed to normoxia (N), hypoxia (H) for 3
h, or H followed by reoxygenation for 3 h (H/R).
RFU, relative fluorescence units. Mean values ⫾
SE are shown (n ⫽ 3– 4/condition).
mia-reperfusion-induced loss of gut barrier function, bacterial patient populations (18). The reason why gut injury and loss of
translocation, apoptosis, and gut-derived inflammatory response, barrier function appear to be clinically important in these
subsequently resulting in villous injury. A second major observa- patient populations is related to its increased susceptibility to
tion is that resistance to gut injury was associated with resistance injury during stress states (11, 18) and the fact that the gut and
to lung inflammation and injury in the HIF-1␣⫹/⫺ mice. These its contents are a major source of factors that contribute to the
observations expand our earlier studies demonstrating that gut development of a systemic inflammatory state and distant
ischemia in vivo induces a prolonged intestinal mucosal HIF-1 organ including acute lung injury (19).
response that does not disappear upon reoxygenation of the Although cytokines (58), bacteria (41, 51), and LPS (41, 59)
intestine and that this persistence of the HIF-1 response ap- as well as hypoxia have been shown to activate HIF-1 in
pears to be mediated, at least in part, by intestinal bacteria enterocytes, our knowledge of HIF-1 activation and its func-
and/or bacterial products, such as LPS (41). Thus the present tional sequelae in gut injury models is limited and to some
study provides evidence that a prolonged intestinal mucosal extent controversial. For example, in contrast to our acute gut
HIF-1 response, which persists after gut reperfusion, plays a I/R results, HIF-1␣ was found to be protective in more chronic
role in the pathogenesis of gut-mediated I/R injury. These gut injury models utilizing colon-specific HIF-1␣-deficient
results are of potential clinical importance because gut injury mice. These models included 2,4,6-trinitrobenzene sulfonic
and loss of normal intestinal barrier function have been asso- acid -induced colitis (12, 37, 56), chronic hypoxia (24), and
ciated with the development of SIRS, acute respiratory distress Yersinia enterocolitica orogastric infection (28). In the context
syndrome (ARDS), and MODS as well as worse clinical of gut I/R injury, one study found that mice administered the
outcomes in severely injured as well as intensive care unit hydroxylase inhibitor, dimethyloxalglycine (DMOG) was pro-
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
G840 HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
Fig. 7. HIF-1 differentially regulates proin-
flammatory cytokines in the ileal mucosa
and lung after T/HS. RNA was prepared
from ileal mucosa and lung of WT and
HIF-1␣⫹/⫺ mice subjected to T/HS or T/SS
for 60 min and 3 h reperfusion. Relative
mRNA expression for TNF-␣, IL-1, IL-6,
and IL-10 was quantified by real-time PCR
using the ⌬⌬Ct method using a log2 scale.
Mean values ⫾ SE are shown (n ⫽ 4 –7
mice/group).
tective in a localized gut I/R injury model (superior mesenteric in necrotizing enterocolitis (2) and in dextran sulfate sodium-
artery occlusion for 15 min and 3 h reperfusion), and HIF-1 induced colitis in von Hippel-Lindau-deficient mice character-
mediated its protective effects via CD73 (27). One possible ized for their constitutive HIF-1 expression (61). Thus the role
explanation for this discrepancy may be due to differences in of HIF-1, as protective or deleterious, may depend on whether
our models of gut I/R injury and a second explanation is that the insult is acute or chronic, the segments of the intestine
the pretreatment of mice with DMOG may have precondi- injured, as well as on whether the loss of HIF-1␣ is partial or
tioned their intestine to subsequent gut I/R injury. However, total. For example, the chronic studies, where HIF-1 was
consistent with our studies, HIF-1␣ was found to be detrimental protective, utilized conditional intestinal and colonic epithelial
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY G841
HIF-1␣ mice (28, 37, 56), whereas our studies were performed in myeloid cells afforded protection against LPS-induced mor-
in mice with a partial HIF-1␣ deficiency that involves the tality (53). Although ileal IL-6 levels were not significantly
entire gut. These differences may be important, since the elevated in WT mice subjected to T/HS as reported previously
segment of the gut that is susceptible to acute gut I/R-mediated (71), the baseline levels of intestinal IL-6 level and IL-1 were
injury is the distal small intestine (33, 69). This increased significantly lower in HIF-1␣⫹/⫺ mice than WT mice. Whether
susceptibility of the ileum to I/R-mediated injury is consistent partially HIF-1␣ deficient mice have a less primed or less
with the observation that the levels of proinflammatory genes, active immune status remains to be determined since we only
such as iNOS, and apoptotic cell death were markedly in- profiled a limited number of proinflammatory cytokines. Al-
creased after hemorrhagic shock in the ileum compared with though our findings suggest that HIF-1 activation exacerbates
duodenum, jejunum, and colon (33). Thus acute and chronic the T/HS-induced gut-and lung-derived inflammatory response
gut injury models differ not only in their mechanism of injury, and HIF-1 differentially regulates cytokine expression in the
but also in the segments of the guts that are at highest risk of ileal mucosa and lung, a more extensive analysis of the HIF-
injury. Additionally, the use of partially HIF-1␣⫹/⫺-deficient 1-driven intestinal and lung inflammatory response is needed to
mice has the advantage that only a partial HIF-1␣ deficiency resolve this issue.
exists whereas complete deficiency of HIF-1␣ in a specific cell Since SIRS, ARDS, and MODS remain common causes of
type, as with the conditional deletion of HIF-1␣ in intestinal morbidity and mortality, understanding the mechanisms by
and colonic cells, may result in a phenotype that is not as which shock and gut ischemic states, such as trauma, lead to
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
clinically relevant, since such a state is unlikely to exist in any gut injury and gut-induced acute lung injury are critical to
human disease state. Thus although HIF-1 appears to be advancing the care of these patients. In this context, our study
involved in the regulation of intestinal homeostasis, it appears showing for the first time that prolonged HIF-1 activation is the
to have dichotomous roles in gut inflammatory diseases in that proximal regulator of T/HS-induced gut mucosal injury and
it can be injurious or protective depending on the exact phys- inflammation provides novel insights into the biology of this
iological conditions studied as well as the nature and duration clinically important syndrome as well as potential therapeutic
of the insult. insights.
This dichotomous effect of HIF-1 activation has also been
observed in studies focusing on the heart and brain as well as GRANTS
the gut. For example, HIF-1 has been implicated as a cardio- This research was supported by National Institutes of Health grants
protective factor in ischemic preconditioning models, since 1P50GM069790 (to R. Feinman and E. A. Deitch), T32-GM069330 (to F. J.
cardioprotection by intermittent ischemia was impaired in Caputo and D. Doucet) and R01-HL55338 (to G. L. Semenza).
partially deficient HIF-1␣ mice (6). However, while HIF-1 is
cardioprotective in preconditioning models, where HIF-1 is DISCLOSURES
only transiently elevated, chronic activation of HIF-1 signaling No conflicts of interest, financial or otherwise, are declared by the author (s).
was found to be deleterious in ischemic hearts (43). Similarly,
HIF-1␣ was found to mediate ischemic tolerance in the neo- REFERENCES
natal rat brain (3) as well as in transient (55) and permanent (4)
focal cerebral ischemia models. However, in contrast to its 1. Bakker WJ, Harris IS, Mak TW. FOXO3a is activated in response to
hypoxic stress and inhibits HIF1-induced apoptosis via regulation of
protective effects in models of preconditioning or tolerance, CITED2. Mol Cell 28: 941–953, 2007.
ablation of HIF-1 in the brain was associated with neuropro- 2. Baregamian N, Rychahou PG, Hawkins HK, Evers BM, Chung DH.
tection to an acute ischemic insult (30) and loss of HIF-1␣ in Phosphatidylinositol 3-kinase pathway regulates hypoxia-inducible fac-
astrocytes markedly protected neurons from hypoxia-induced tor-1 to protect from intestinal injury during necrotizing enterocolitis.
Surgery 142: 295–302, 2007.
neuronal death (8, 66). Thus HIF-1␣ activation has been shown 3. Bergeron M, Gidday JM, Yu AY, Semenza GL, Ferriero DM, Sharp
to be either beneficial or deleterious in several organ systems FR. Role of hypoxia-inducible factor-1 in hypoxia-induced ischemic
depending on the physiological context of the model. tolerance in neonatal rat brain. Ann Neurol 48: 285–296, 2000.
There is evidence that the relationship between HIF-1 acti- 4. Bernaudin M, Nedelec A, Divoux D, MacKenzie E, Petit E, Schumann-Bard
vation and inflammation appears to be bidirectional since P. Normobaric hypoxia induces tolerance to focal permanent cerebral isch-
emia in association with an increased expression of hypoxia-inducible factor-1
numerous studies have shown that HIF-1 is a central regulator and its target genes, erythropoietin and VEGF, in the adult mouse brain. J
of inflammation and innate immunity (50), whereas at the same Cereb Blood Flow Metab 22: 393–403, 2002.
time proinflammatory mediators such as TNF-␣, IL-1, nitric 5. Bosch-Marce M, Okuyama H, Wesley J, Sarkar K, Kimura H, Liu Y,
oxide, and LPS have been shown to induce HIF-1␣ expression Zhang H, Strazza M, Rey S, Savino L, Zhou Y, McDonald K, Na Y,
Vandiver S, Rabi A, Shaked Y, Kerbel R, LaVallee T, Semenza G.
in cells, including enterocytes, even under normoxic conditions Effects of aging and hypoxia-inducible factor-1 activity on angiogenic cell
(29, 41, 58, 59). In this context, our findings suggest that the mobilization and recovery of perfusion after limb ischemia. Circ Res 101:
diminished intestinal TNF-␣, IL-1, and iNOS responses as 1310 –1318, 2007.
well as the reduced pulmonary IL-1 response in partially 6. Cai Z, Zhong H, Bosch-Marce M, Fox-Talbot K, Wang L, Wei C,
deficient HIF-1␣ mice after T/HS may be linked to the atten- Trush MA, Semenza GL. Complete loss of ischaemic preconditioning-
induced cardioprotection in mice with partial deficiency of HIF-1␣.
uation of villous and lung injury. Support for this concept Cardiovasc Res 77: 463–470, 2008.
stems from earlier studies linking gut-derived factors such as 7. Chaitanya GV, Babu PP. Activation of calpain, cathepsin-B and
IL-1, TNF-␣, and iNOS as well as enteric bacteria to intes- caspase-3 during transient focal cerebral ischemia in rat model. Neuro-
tinal barrier dysfunction and the development of both sepsis- chem Res 33: 2178 –2186, 2008.
8. Chen C, Hu Q, Yan J, Yang X, Shi X, Lei J, Chen L, Huang H, Han
and T/HS-mediated distant organ injury (14, 70). Additionally, J, Zhang JH, Zhou C. Early inhibition of HIF-1␣ with small interfering
HIF-1 activation has been implicated in the proinflammatory RNA reduces ischemic-reperfused brain injury in rats. Neurobiol Dis 33:
response of myeloid cells during sepsis and deletion of HIF-1␣ 509 –517, 2009.
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
G842 HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY
9. Chiu C, McArdle A, Brown R, Scott H, Gurd F. Intestinal mucosal reperfusion-independent inflammatory events. Arch Orthop Trauma Surg
lesions in low-flow states. Arch Surg 101: 478 –483, 1970. 121: 219 –222, 2001.
10. Claridge JA, Enelow RI, Young JS. Hemorrhage and resuscitation 32. Huang LE, Gu J, Schau M, Bunn HF. Regulation of hypoxia-inducible
induce delayed inflammation and pulmonary dysfunction in mice. J Surg factor 1alpha is mediated by an O2-dependent degradation domain via the
Res 92: 206 –213, 2000. ubiquitin-proteasome pathway. Proc Natl Acad Sci USA 95: 7987–7992,
11. Clark JA, Coopersmith CM. Intestinal crosstalk: a new paradigm for 1998.
understanding the gut as the “motor” of critical illness. Shock 28: 384 – 33. Inoue K, Takahashi T, Uehara K, Shimuzu H, Ido K, Morimatsu H,
393, 2007. Omori E, Katayama H, Akagi R, KM. Protective role of heme oxygen-
12. Cummins EP, Seeballuck F, Keely SJ, Mangan NE, Callanan JJ, ase 1 in the intestinal tissue injury in hemorrhagic shock in rats. Shock 29:
Fallon PG, Taylor CT. The hydroxylase inhibitor dimethyloxalylglycine 252–261, 2008.
is protective in a murine model of colitis. Gastroenterology 134: 156 –165, 34. Ivan M, Kondo K, Yang H, Kim W, Valiando J, Ohh M, Salic A,
2008. Asara JM, Lane WS, Kaelin WG Jr. HIF-1␣ targeted for VHL-mediated
13. Dehne N, Brüne B. HIF-1 in the inflammatory microenvironment. Exp destruction by proline hydroxylation: implications for O2 sensing. Science
Cell Res 315: 1791–1797, 2009. 292: 464 –468, 2001.
14. Deitch E, Xu DZ, Franko L, Ayala A, Chaudry I. Evidence favoring the 35. Iyer NV, Kotch LE, Agani F, Leung SW, Laughner E, Wenger RH,
role of the gut as a cytokine generating organ in rats subjected to Gassmann M, Gearhart JD, Lawler AM, Yu AY, Semenza GL.
hemorrhagic shock. Shock 1: 141–146, 1994. Cellular and developmental control of O2 homeostasis by hypoxia-induc-
15. Deitch EA. Animal models of sepsis and shock: a review and lessons ible factor 1 alpha. Genes Dev 12: 149 –162, 1998.
learned. Shock 9: 1–11, 1998. 36. Jaakkola P, Mole D, Tian Y, Wilson M, Gielbert J, Gaskell S,
16. Deitch EA. Multiple organ failure: pathophysiology and potential future Kriegsheim A, Hebestreit H, Mukherji M, Schofield C, Maxwell P,
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
therapy. Ann Surg 216: 117–134, 1992. Pugh C, Ratcliffe P. Targeting of HIF-alpha to the von Hippel-Lindau
17. Deitch EA, Berg R, RS. Endotoxin promotes the translocation of bacteria ubiquitylation complex by O2-regulated prolyl hydroxylation. Science
from the gut. Arch Surg 122: 185–190, 1987. 292: 468 –472, 2001.
18. Deitch EA, Sambol JT. The gut origin hypothesis of MODS. In: Sepsis 37. Karhausen J, Furuta GT, Tomaszewski JE, Johnson RS, Colgan SP,
and Multiple Organ Dysfunction: A Multidisciplinary Approach, edited by Haase VH. Epithelial hypoxia-inducible factor-1 is protective in murine
Deitch EA, Vincent J-L, Windsor A. Philadelphia, PA: Saunders, 2002, p. experimental colitis. J Clin Invest 114: 1098 –1106, 2004.
105–116. 38. Kawagoe T, Sato S, Jung A, Yamamoto M, Matsui K, Kato H,
19. Deitch EA, Xu D, Lu Q. Gut lymph hypothesis of early shock and Uematsu S, Takeuchi O, Akira S. Essential role of IRAK-4 protein and
trauma-induced multiple organ dysfunction: a new look at gut origin of its kinase activity in Toll-like receptor-mediated immune responses but not
sepsis. J Org Dys 2: 70 –70, 2006. in TCR signaling. J Exp Med 204: 1013–1024, 2007.
20. Dhanasekaran A, Gruenloh SK, Buonaccorsi JN, Zhang R, Gross GJ, 39. Kiang JG, Bowman PD, Lu X, Li Y, Wu BW, Loh HH, Tsen KT,
Falck JR, Patel PK, Jacobs ER, Medhora M. Multiple antiapoptotic Tsokos GC. Geldanamycin inhibits hemorrhage-induced increases in
targets of the PI3K/Akt survival pathway are activated by epoxyeicosa- caspase-3 activity: role of inducible nitric oxide synthase. J Appl Physiol
trienoic acids to protect cardiomyocytes from hypoxia/anoxia. Am J 103: 1045–1055, 2007.
Physiol Heart Circ Physiol 294: H724 –H735, 2008. 40. Kiang JG, Peckham RM, Duke LE, Shimizu T, Chaudry IH, Tsokos
21. Fink MP, Delude RL. Epithelial barrier dysfunction: a unifying theme to GC. Androstenediol inhibits the trauma-hemorrhage-induced increase in
explain the pathogenesis of multiple organ dysfunction at the cellular caspase-3 by downregulating the inducible nitric oxide synthase pathway.
level. Crit Care Clin 21: 177–196, 2005. J Appl Physiol 102: 933–941, 2007.
22. Forsythe RM, Xu DZ, QL, Deitch EA. LPS-induced enterocyte-derived 41. Koury J, Deitch EA, Homma H, Abungu B, Gangurde P, Condon MR,
nitric oxide induces intestinal monolayer permeability in an autocrine Lu Q, Xu DZ, RF. Persistent HIF-1␣ activation in gut ischemia/reperfu-
fashion. Shock 17: 180 –184, 2002. sion injury: potential role of bacteria and lipopolysaccharide. Shock 22:
23. Fraisl P, Aragones J, Carmeliet P. Inhibition of oxygen sensors as a 270 –277, 2004.
therapeutic strategy for ischaemic and inflammatory disease. Nat Rev 42. Lando D, Peet DJ, Gorman JJ, Whelan DA, Whitelaw ML, Bruick
Drug Discov 8: 139 –152, 2009. RK. FIH-1 is an asparaginyl hydroxylase enzyme that regulates the
24. Furuta GT, Turner JR, Taylor CT, Hershberg RM, Comerford K, transcriptional activity of hypoxia-inducible factor. Genes Dev 16: 1466 –
Narravula S, Podolsky DK, Colgan SP. Hypoxia-inducible factor 1-de- 1471, 2002.
pendent induction of intestinal trefoil factor protects barrier function 43. Lei L, Mason S, Liu D, Huang Y, Marks C, Hickey R, Jovin IS,
during hypoxia. J Exp Med 193: 1027–1034, 2001. Pypaert M, Johnson RS, Giordano FJ. Hypoxia-inducible factor-depen-
25. Giakoustidis AE, Giakoustidis DE, Koliakou K, Kaldrymidou E, dent degeneration, failure, and malignant transformation of the heart in the
Iliadis S, Antoniadis N, Kontos N, Papanikolaou V, Papageorgiou G, absence of the von Hippel-Lindau protein. Mol Cell Biol 28: 3790 –3803,
Atmatzidis K, Takoudis D. Inhibition of intestinal ischemia/reperfusion 2008.
induced apoptosis and necrosis via down-regulation of the NF-kB, c-Jun 44. Liaudet L, Szabo A, Soriano F, Zingarelli B, Szabo C, Salzman A.
and caspase-3 expression by epigallocatechin-3-gallate administration. Poly(ADP-ribose) synthetase mediates intestinal mucosal barrier dysfunc-
Free Radic Res 42: 180 –188, 2008. tion after mesenteric ischemia. Shock 14: 142–143, 2000.
26. Greijer A, van der Wall E. The role of hypoxia inducible factor (HIF-1) 45. Loor G, Schumacker PT. Role of hypoxia-inducible factor in cell
in hypoxia induced apoptosis. J Clin Pathol 57: 1009 –1014, 2004. survival during myocardial ischemia-reperfusion. Cell Death Differ 15:
27. Hart ML, Henn M, Kohler D, Kloor D, Mittelbronn M, Gorzolla IC, 686 –690, 2008.
Stahl GL, Eltzschig HK. Role of extracellular nucleotide phosphohy- 46. Madsen KL, Malfair D, Gray D, Doyle JS, Jewell LD, Fedorak RN.
drolysis in intestinal ischemia-reperfusion injury. FASEB J 22: 2784 – Interleukin-10 gene-deficient mice develop a primary intestinal permeabil-
2797, 2008. ity defect in response to enteric microflora. Inflamm Bowel Dis 5: 262–
28. Hartmann H, Eltzschig HK, Wurz H, Hantke K, Rakin A, Yazdi AS, 270, 1999.
Matteoli G, Bohn E, Autenrieth IB, Karhausen J, Neumann D, Colgan 47. Mahon PC, Hirota K, Semenza GL. FIH-1: a novel protein that interacts
SP, Kempf VAJ. Hypoxia-independent activation of HIF-1 by Enterobac- with HIF-1alpha and VHL to mediate repression of HIF-1 transcriptional
teriaceae and their siderophores. Gastroenterology 134: 756 –767, 2008. activity. Genes Dev 15: 2675–2686, 2001.
29. Hellwig-Burgel T, Rutkowski K, Metzen E, Fandrey J, Jelkmann W. 48. Michalsky MP, Deitch EA, Ding J, Lu Q, Huang Q. Interleukin-6 and
Interleukin-1beta and tumor necrosis factor-alpha stimulate DNA binding tumor necrosis factor production in an enterocyte cell model (Caco-2)
of hypoxia-inducible factor-1. Blood 94: 1561–1567, 1999. during exposure to Escherichia coli. Shock 7: 139 –146, 1997.
30. Helton R, Cui J, Scheel JR, Ellison JA, Ames C, Gibson C, Blouw B, 49. Murao Y, Loomis W, Wolf P, Hoyt DB, Junger WG. Effect of dose of
Ouyang L, Dragatsis I, Zeitlin S, Johnson RS, Lipton SA, Barlow C. hypertonic saline on its potential to prevent lung tissue damage in a mouse
Brain-specific knock-out of hypoxia-inducible factor-1␣ reduces rather model of hemorrhagic shock. Shock 20: 29 –34, 2003.
than increases hypoxic-ischemic damage. J Neurosci 25: 4099 –4107, 50. Nizet V, Johnson RS. Interdependence of hypoxic and innate immune
2005. responses. Nat Rev Immunol 9: 609 –617, 2009.
31. Hierholzer C, Harbrecht BG, Billiar TR, Tweardy DJ. Hypoxia- 51. Patel NJ, Zaborina O, Wu L, Wang Y, Wolfgeher DJ, Valuckaite V,
inducible factor-1 activation and cyclo-oxygenase-2 induction are early Ciancio MJ, Kohler JE, Shevchenko O, Colgan SP, Chang EB, Turner
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
HIF MEDIATES GUT ISCHEMIA-REPERFUSION INJURY G843
JR, Alverdy JC. Recognition of intestinal epithelial HIF-1␣ activation by HIF-1␣ and pVHL under physiological conditions and after ischemia-
Pseudomonas aeruginosa. Am J Physiol Gastrointest Liver Physiol 292: reperfusion injury. Am J Physiol Renal Physiol 295: F1666 –F1677, 2008.
G134 –G142, 2007. 64. Thuijls G, de Haan J, Derikx J, Daissormont I, Hadfoune M, Heine-
52. Peng YJ, Yuan G, Ramakrishnan D, Sharma SD, Bosch-Marce M, man E, Buurman W. Intestinal cytoskeleton degradation precedes tight
Kumar GK, Semenza GL, Prabhakar NR. Heterozygous HIF1␣ defi- junction loss following hemorrhagic shock. Shock 31: 164 –169, 2009.
ciency impairs carotid body-mediated systemic responses and reactive 65. Van Hoecke M, Pringent-Tessier A, Garnier P, Bertrand N,
oxygen species generation in mice exposed to intermittent hypoxia. J Filomenko R, Bettaieb A, Marie C, Beley A. Evidence of HIF-1
Physiol 577: 705–716, 2006. functional binding activity to caspase-3 promoter after photothrombotic
53. Peyssonnaux C, Cejudo-Martin P, Doedens A, Zinkernagel AS, John- cerebral ischemia. Mol Cell Neurosci 34: 40 –47, 2007.
son RS, Nizet V. Cutting edge: essential role of hypoxia inducible
66. Vangeison G, Carr D, Federoff HJ, Rempe DA. The good, the bad, and
factor-1␣ in development of lipopolysaccharide-induced sepsis. J Immu-
the cell type-specific roles of hypoxia inducible factor-1␣ in neurons and
nol 178: 7516 –7519, 2007.
54. Pfaffl M. A new mathematical model for relative quantification in real- astrocytes. J Neurosci 28: 1988 –1993, 2008.
time RT-PCR. Nucleic Acids Res 29: e45, 2001. 67. Wang GL, Semenza GL. Characterization of hypoxia-inducible factor 1
55. Prass K, Scharff A, Ruscher K, Lowl D, Muselmann C, Victorov I, and regulation of DNA binding activity by hypoxia. J Biol Chem 268:
Kapinya K, Dirnagl U, Meisel A. Hypoxia-induced stroke tolerance in 21513–21518, 1993.
the mouse is mediated by erythropoietin. Stroke 34: 1981–1986, 2003. 68. Wang Q, Fang CH, Hasselgren PO. Intestinal permeability is reduced
56. Robinson A, Keely S, Karhausen J, Gerich ME, Furuta GT, Colgan and IL-10 levels are increased in septic IL-6 knockout mice. Am J Physiol
SP. Mucosal protection by hypoxia-inducible factor (HIF) prolyl hydrox- Regul Integr Comp Physiol 281: R1013–R1023, 2001.
ylase inhibition. Gastroenterology 134: 144 –155, 2008. 69. Xu DZ, Lu Q, Guillory D, Cruz N, Berg R, Deitch EA. Mechanisms of
Downloaded from http://ajpgi.physiology.org/ at EBSCO on May 6, 2013
57. Rupani B, Caputo F, Watkins A, Vega D, Magnotti L, Lu Q, Xu D, endotoxin-induced intestinal injury in a hyperdynamic model of sepsis. J
Deitch E. Relationship between disruption of the unstirred mucus layer Trauma 34: 676 –683, 1993.
and intestinal restitution in loss of gut barrier function after trauma 70. Yang R, Gallo DJ, Baust JJ, Watkins SK, Delude RL, Fink MP. Effect
hemorrhagic shock. Surgery 141: 481–489, 2007. of hemorrhagic shock on gut barrier function and expression of stress-
58. Scharte M, Han X, Bertges DJ, Fink MP, Delude RL. Cytokines induce related genes in normal and gnotobiotic mice. Am J Physiol Regul Integr
HIF-1 DNA binding and the expression of HIF-1-dependent genes in Comp Physiol 283: R1263–R1274, 2002.
cultured rat enterocytes. Am J Physiol Gastrointest Liver Physiol 284: 71. Yang R, Han X, Uchiyama T, Watkins SK, Yaguchi A, Delude RL,
G373–G384, 2003. Fink MP. IL-6 is essential for development of gut barrier dysfunction
59. Scharte M, Han X, Uchiyama T, Tawadrous Z, Delude RL, Fink MP. after hemorrhagic shock and resuscitation in mice. Am J Physiol Gastroin-
LPS Increases hepatic HIF-1␣ protein and expression of the HIF-1- test Liver Physiol 285: G621–G629, 2003.
dependent gene aldolase A in rats. J Surg Res 135: 262–267, 2006.
72. Yeh KY, Yeh M, Glass J, Granger DN. Rapid activation of NF-kappaB
60. Semenza GL. Regulation of physiological responses to continuous and
and AP-1 and target gene expression in postischemic rat intestine. Gas-
intermittent hypoxia by hypoxia-inducible factor 1. Exp Physiol 91:
803–806, 2006. troenterology 118: 525–534, 2000.
61. Shah YM, Ito S, Morimura K, Chen C, Yim SH, Haase VH, Gonzalez 73. Yu HP, Hsieh YC, Suzuki T, Choudhry MA, Schwacha MG, Bland
FJ. Hypoxia-inducible factor augments experimental colitis through an KI, Chaudry IH. Mechanism of the nongenomic effects of estrogen on
MIF-dependent inflammatory signaling cascade. Gastroenterology 134: intestinal myeloperoxidase activity following trauma-hemorrhage: up-
2036 –2048, 2008. regulation of the PI-3K/Akt pathway. J Leukoc Biol 82: 774 –780, 2007.
62. Strober W, Fuss IJ, Blumberg RS. The immunology of mucosal models 74. Zhang HY, Radulescu A, Besner GE. Heparin-binding epidermal
of inflammation. Annu Rev Immunol 20: 495–549, 2002. growth factor-like growth factor is essential for preservation of gut barrier
63. Sutton TA, Wilkinson J, Mang HE, Knipe NL, Plotkin Z, Hosein M, function after hemorrhagic shock and resuscitation in mice. Surgery 146:
Zak K, Wittenborn J, Dagher PC. p53 regulates renal expression of 334 –339, 2009.
AJP-Gastrointest Liver Physiol • VOL 299 • OCTOBER 2010 • www.ajpgi.org
Copyright of American Journal of Physiology: Gastrointestinal & Liver Physiology is the
property of American Physiological Society and its content may not be copied or emailed to
multiple sites or posted to a listserv without the copyright holder's express written permission.
However, users may print, download, or email articles for individual use.
You might also like
- The Effect of Coffee Arabica Coffea Arabica L FruiDocument11 pagesThe Effect of Coffee Arabica Coffea Arabica L FruiYusrinabilla -No ratings yet
- A Review of Dietary and Non-Dietary Exposure To Bisphenol-A: ArticleDocument18 pagesA Review of Dietary and Non-Dietary Exposure To Bisphenol-A: ArticleYusrinabilla -No ratings yet
- Animal Models of Ischemia-Reperfusion Induced Intestinal Injury: Progress and Promise For Translational ResearchDocument53 pagesAnimal Models of Ischemia-Reperfusion Induced Intestinal Injury: Progress and Promise For Translational ResearchYusrinabilla -No ratings yet
- Effects of Chronic IngestionDocument7 pagesEffects of Chronic IngestionYusrinabilla -No ratings yet
- ErosikkkDocument20 pagesErosikkkYusrinabilla -No ratings yet
- Determination of Urinary Levels of Bisphenol A in A Turkish PopulationDocument10 pagesDetermination of Urinary Levels of Bisphenol A in A Turkish PopulationYusrinabilla -No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Preservative Challenge TestDocument8 pagesPreservative Challenge TestBernardo100% (1)
- Coming of Chaperone Mediated AutophagyDocument17 pagesComing of Chaperone Mediated AutophagyUlikNo ratings yet
- Epigenetics: - Epi'genetics - On' or Over' The Genetic Information Encoded in The DNADocument14 pagesEpigenetics: - Epi'genetics - On' or Over' The Genetic Information Encoded in The DNAlordniklausNo ratings yet
- 3.6.8 SOP - Stool CultureDocument5 pages3.6.8 SOP - Stool CultureSemeeeJunior100% (1)
- Topical Revision Notes Biology O Level PDFDocument140 pagesTopical Revision Notes Biology O Level PDFBilal Akram80% (20)
- Brain Arteriovenous MalformationsDocument20 pagesBrain Arteriovenous MalformationsTony NgNo ratings yet
- Sim - Science 4 Animal ReproductionbinmaleyDocument12 pagesSim - Science 4 Animal ReproductionbinmaleyEvelyn Torrero100% (1)
- Cell Theory ActivityDocument1 pageCell Theory ActivityLawrence StilinskiNo ratings yet
- Archives of Biochemistry and BiophysicsDocument10 pagesArchives of Biochemistry and BiophysicsJuanNo ratings yet
- Biology PaperDocument42 pagesBiology PaperPratyay BhaumikNo ratings yet
- Gender Role, Gender Identity, Core Gender Identity. Usage and Definition of Terms PDFDocument10 pagesGender Role, Gender Identity, Core Gender Identity. Usage and Definition of Terms PDFRodolfo Hitch100% (2)
- AntibacterialactivityofRhoeodiscolorHance JournalDocument5 pagesAntibacterialactivityofRhoeodiscolorHance JournalOktoNo ratings yet
- Graphical Presentation of Applications in Microbial TechnologyDocument1 pageGraphical Presentation of Applications in Microbial TechnologyMariam ShafiqueNo ratings yet
- Assessment of Immunohistochemical Expression of p16 in Head and Neck Squamous Cell Carcinoma and Their Correlation With Clinicopathological ParametersDocument8 pagesAssessment of Immunohistochemical Expression of p16 in Head and Neck Squamous Cell Carcinoma and Their Correlation With Clinicopathological ParametersMadhura ShekatkarNo ratings yet
- Photosynthesis Exam QuestionsDocument4 pagesPhotosynthesis Exam QuestionsInvincible Nasir The ProNo ratings yet
- DDBJ, Bilogical Data Bases, Bioinformatics Data BaseDocument2 pagesDDBJ, Bilogical Data Bases, Bioinformatics Data BaseRajesh GuruNo ratings yet
- Malaria Best Investigatory ProjectDocument37 pagesMalaria Best Investigatory ProjectDivyansh PandeyNo ratings yet
- Sessions 4 - 2023Document13 pagesSessions 4 - 2023Chen ZhonghaoNo ratings yet
- Edco Biology Sample Paper 3 HL SolutionsDocument8 pagesEdco Biology Sample Paper 3 HL SolutionsgopodNo ratings yet
- Jism Al InsaanDocument26 pagesJism Al InsaantisuchiNo ratings yet
- Blue-White Colony ScreeningDocument1 pageBlue-White Colony ScreeningShalizma Khandaker OrniNo ratings yet
- Em Steep CGDocument4 pagesEm Steep CGGsbsggsbsjysbsnshsbNo ratings yet
- Novel Coronavirus Landscape Covid 19Document9 pagesNovel Coronavirus Landscape Covid 19kenNo ratings yet
- Nutrition in Plants PART 1Document11 pagesNutrition in Plants PART 1Sarika AhujaNo ratings yet
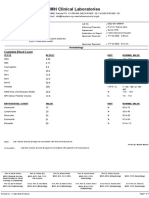
- FMH Clinical Laboratories: Complete Blood CountDocument1 pageFMH Clinical Laboratories: Complete Blood CountZahid AliNo ratings yet
- The Role of Autophagy in CancerDocument7 pagesThe Role of Autophagy in CancerAlexander VigenNo ratings yet
- Cell CycleDocument12 pagesCell CycleAmNo ratings yet
- Haralambos SexandGenderDocument52 pagesHaralambos SexandGenderBob Jiggins83% (6)
- Terminator Gene TechnologyDocument8 pagesTerminator Gene TechnologyKDNo ratings yet
- Exsc 223 Practice Exam 2Document11 pagesExsc 223 Practice Exam 2kimber brownNo ratings yet