Professional Documents
Culture Documents
Medical Surgical Nursing: Download
Uploaded by
Kim LeeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Surgical Nursing: Download
Uploaded by
Kim LeeCopyright:
Available Formats
Read free for 30
Search
days
Download 1 of 59 ( Search document )
Enjoy thousands of titles when you subscribe
Read free for 30 days
Only ₱129/month a/er. Cancel anytime.
Medical Surgical Nursing
Uploaded by Chey Dianne Seriña
! 100% (7) · 4K views · 59 pages
More
" # $ % & '
Save 100% 0% Embed Share Print
Download 1 of 59 ( Search document )
MEDICAL-SURGICAL NURSING REVIEW
Course Outline
I. Client in Pain
II. Perioperative Nursing Care
III. Alterations in Human Functioning
a. Disturbances in Oxygenation: Respiratory & Cardiovascular Functions
b. Disturbances in Metabolic and Endocrine Functions
c. Disturbances in Elimination: Gastrointestinal Problems
d. Disturbances in Fluids and Electrolytes: Renal & Genitourinary Functions
e. Disturbances in Cellular Functioning: Cancer and Hematologic Problems
f. Disturbances in Auditory & Visual Functions
g. Disturbances in Musculoskeletal Functions
IV. Client in Biologic Crisis: Life threatening Conditions of the Human Body
- Shock
V. Emergency & Disaster
- First-aid and Cardiopulmonary Support
--------------------------------------------------------------------------------------------------------------------------------------
I. CLIENT IN PAIN
Pain – the fifth vital sign
an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
Basic Categories of Pain:
1. Acute Pain – sudden pain which is usually relieved in seconds or after a few weeks.
2. Chronic Pain (Non-Malignant) – constant, intermittent pain which usually persists even after healing
of the injured tissue
3. Cancer-Related Pain- May be acute or chronic; may or may not be relieved by medications
Pain Transmission:
1. Nociceptors are called pain receptors. These are the free nerve endings in the skin that respond to
intense, potentially damaging stimuli.
2. Peripheral Nervous System
3. Central Nervous System
4. Descending Control System
Factors Influencing Pain Response
1. Past Experience – e.g. trauma
2. Anxiety and Depression
3. Culture - beliefs
4. Age – infants are more sensitive
5. Gender
6. Placebo Effect
Characteristics of Pain
1. Intensity –mild, moderate, excruciating
2. Timing – morning or evening, duration may be longer or shorter
3. Location
4. Quality – burning, aching, stabbing
5. Personal Meaning to pain – tolerance to pain may be different from one person to the other due to
some personal reasons such as economic reasons, work condition, etc.
6. Aggravating and Alleviating factors – patient’s environment
7. Pain Behaviors - facial expressions with pain
Pain Assessment
1. Evaluate: Cause, Location, Character and Intensity
2. Numeric Pain Scale – 5-severe pain -! 0 – no pain
3. Descriptive Pain Scales – mild, moderate, severe
4. Visual Analogue Scales
5. Faces Pain Scale
Nurse’s Role in Pain Management
1. Identify goals for Pain management
a. Decrease intensity, duration or frequency
b. Factors in identifying goals:
i. Severity of pain
115
ii. Harmful effects of pain to the client
iii. Duration of the pain
2. Establish Nurse-Patient Relationship and Teaching
a. Acknowledge the verbalization of pain by the client
b. Relieve patient’s anxiety
c. Teach measures how to relieve pain
3. Provide Physical care
a. Teach and assist in self-care
b. Environmental conditions
c. Application of ice/heat on painful area
4. Manage anxiety related to Pain
a. Teach about the nature of pain that may be felt by the client and reassure him/her
b. Teach alternative measures to relieve pain
c. Stay with the client/ frequent communication with the client
5. Pain Medications may be administered as:
a. Balanced Anesthesia – given to avoid experiencing pain
b. PRN – “Pro Re Nata” – as needed
c. Preventive – taken before pain is felt
d. Individualized Dosage
e. Patient-Controlled Analgesia (PCA) – patient takes medication if pain felt is becoming
intolerable
6. Non-pharmacologic Interventions
a. Cutaneous Simulation and Massage
b. Ice and heat therapies
c. Transcutaneous Electrical Nerve Stimulation
d. Distraction
e. Relaxation Techniques
f. Guided Imagery
g. Hypnosis
II. PERIOPERATIVE CARE
o Phases of Perioperative Nursing
a. Pre-operative Nursing
b. Inraoperative Nursing
c. Post-operative Nursing
A. Pre-operative Care
Pre-admission and Admission Test
1. Psychological support
2. Client Education:
a. Importance and practice of breathing exercises
b. Location & support of wound
c. Importance of early ambulation
d. Inform and practice leg exercises, positioning, turning
e. Anesthesia and analgesics
f. Educate regarding drains and dressings to be received post-op
g. Recovery room policies and procedures
3. Informed consent
a. At least 18 years of age
b. In sound mind- without psychologic disorder
c. Not under the influence of drugs or alcohol
d. Immediate relative over 18 years old
4. Physical Assessment and preparation
a. Physical Preparation – NPO, remove dentures, jewelries, clothesetc.
b. Nutritional & Fluid Status – should be well hydrated
c. Drug or alcohol Use – may experience delirium or intoxication to
anesthetic drugs because ormal doses do not usually take effect to
these patients and require heavier dose to achieve anesthetic effect.
d. Respiratory Status - teach breathing exercises
e. Cardiovascular Status – should have controlled and stable
cardiovascular functioning before operation to prevent intraoperative
problems
f. Hepatic & Renal Functions – normal functioning is important in
absorbing anesthetic drugs
116
g. Endocrine Functions- important in monitoring to prevent
hypo/hyperglycemia, thyrotoxicosis, acidosis
h. Immune Functions – allergies esp. to anesthetic drugs
i. Psychosocial Factors – emotional and psychological preparation to
ensure cooperation fom the patient with the procedures
j. Spiritual & Cultural Beliefs - blood transfusions, transplants, ligation,
etc are against other culture & religion.
5. Pre-operative drugs – given 20-60 mins.pre-operative
o Makes patient drowsy, keep siderails up
6. Proper positioning
Semi-Fowlers HOB elevated at 30 Head injury, pot-op cranial surgery,
degrees post-op cataract removal, increased
ICP, dyspneic patients
Fowlers HOB elevated at 45 Head injury, pot-op cranial surgery;
degrees post-op abdominal surgery; post-op
thyroidectomy, post-op cataract surgery,
increased ICP; dyspnea
High-Fowler’s HOB elevated at 90 Pneumothorax, hiatus hernia
degrees
Supine/ Dorsal Lying on back w/ small Spinal cord injury, urinary
Recumbent pillow under head catheterization
Lying on abdomen with Amputation of legs/feet, post lumbar
head turned to the side puncture, post myelogram, post
tonsillectomy & adenoidectomy (T&A)
Lateral / Side lying Lying on side, weight Post-abominal surgery, post
on the lateral side, the tonsillectomy & adenoidectomy (T&A),
lower scapula and post-liver biopsy ( right side down), post
lower iliac. pyloric stenosis (right)
Lying on side, weight Unconscious client
on the clavicle,
humerus and anterior
aspect of the iliac.
Lying on back with Perineal, rectal & vaginal procedures
knees and legs bent
and raised on a stir up
Trendelenburg Head & body lowered, Shock
feet elevated
Reverse Head elevated , feet Cervical traction
Tredelenburg lowered
Elevate extremity Support with pillows Post-op surgical procedure on
extremity, cast, edema,
thrombophlebitis
117
Prone
Supine Lateral Recumbent
Sim’s Position Reverse High-Fowler’s
Trendelenburg
Jack-Knife Lithotomy
B. Intra-operative Care
1. Ensure sterility of all instruments and supplies at the operating field
Principle: STERILE TO STERILE, CLEAN TO CLEAN
Sterile objects touches only sterile surfaces/objects
Clean objects touches only clean surfaces/objects
Sterilization techniques:
o Autoclave – Steam, Ethyl Oxide (Gas)
o Glutaraldehyde Solution- Cidex
2. Ensure safety of client in the operating table- prevent falls, drape the patient properly,
provide warmth
3. Stay with the client to relieve anxiety and support during anesthesia
Anesthesia Administration:
118
a. General Anesthesia via Inhalation
b. General Anestheisia via Intravenous
c. Regional Anesthesia - local anesthesia
d. Conduction Blocks/ Spinal Anesthesia – Epidural & Spinal Block
- for operation below the waist line
- patient is awake during operation
4. Perform sponge count, instrument count and needle count
5. Aseptic technique in handling and preparing all instruments and supplies
6. Applies grounding device to prevent electrical burn during use of electrosurgical
equipment
7. Proper documentation
C. Post-operative Care
1. Immediate assessment of VS, and Neuro VS, drainages, surgical dressing
2. Monitoring of vital signs q 15mins until stable
3. Post-operative positioning depending on the procedure performed
4. Deep breathing exercises
5. Early ambulation
6. Health teaching for Independent (self) care upon discharge
III. ALTERATIONS IN HUMAN FUNCTIONING
1. DISTURBANCES IN OXYGENATION
Arterial Blood Gas
Normal Value
pH Measure of acidity or alkalinity 7.35 – 7.45
pCO2 Partial pressure of carbon dioxide respiratory 35 -45
parameter influenced by lungs only
pO2 Partial pressure of oxygen; measure of amount 80-100
oxygen delivered to lungs
HCO3 Bicarbonate, metabolic parameter influenced only by 22-26
metabolic factors
Respiratory Normal Value Respiratory
Acidosis Alkalosis
pH 7.35 – 7.45
pCO2 35 -45
Normal Compensation HCO3 22-26 Normal Compensation
a. Administer NaHco3 Nursing Intervention a. Breathe into paper
b. Get rid of CO2 bag or cupped
c. Bronchodilators hands
d. Monitor ABG b. Oxygen
119
Metabolic Normal Value Metabolic
Acidosis Alkalosis
pH 7.35 – 7.45
Normal Compensation Normal Compensation
pCO2 35 -45
HCO3 22-26
a. Treat underlying cause Restore fluid loss which may be
(Starvation, systemic cause by vomiting, gastric
infections, renal failure, suction, alkali ingestion,
Diabetic acidosis, Nursing Intervention excessive diuretic
Keratogenic diet,
diarrhea, excessive
exercise)
b. Promote Metabolic
good air Normal Value Metabolic
exchange Acidosis 2
Alkalosis
c. Give NAHCO3 via IV
pH 3
7.35 – 7.45
pCO
Normal Compensation CHRONIC OBSTRUCTIVE PULMONARY DISEASE Normal Compensation
HCO 35 -45
- A group of conditions assoc. w/ chronic obstruction of airflow entering or leaving the lungs
Major diseases
You're Reading a Preview 22-26
1. Pulmonary Emphysema – airway is obstructed due to destroyed alveolar walls
2. Chroni a. cTreat
Bronunderlying cause mucus production that obstructs airway
chitis- increased Restore fluid loss which may be
3. Asthma Upload your documents to download. cause by vomiting, gastric
(Starvation, systemic Nursing Intervention
infections, renal failure, suction, alkali ingestion,
Cause: Diabetic acidosis, excessive diuretic
Keratogenic
3
diet, OR Medical Management:
1. Cigarette smoking 1. Bronchodilators
2. Chronic resp diarrhea,
iratoryexcessive
infections
exercise) 2. Antihistamines
3. Family hist ory of COPD 3. Steroids
4. Air pob. ionBecome
llutPromote good air a Scribd member for full
4. access.
AntibioticsYour
exchange
c. Give NAHCO via IV first 30 days are free. 5. Expectorants
Clinical Manifestations: 6. Oxygen therapy at 2LPM – use cautiously
" Few words between breaths
" Pursed-lip breathing CHRONIC OBSTRUCTIVE PULMONARY Nursing Management:
DISEASE
" Cyanosis 1. Administer meds and O2 as ordered
" Distended neck veins Continue for Free2. Promote adequate activities to enhance
" Barrel chest – increased diameter of thorax cardiovascular fitness
" Pulsus paradoxus – 3. Adequate rests
A group of conditions assoc. w/ chronic obstruction of airflow entering 4. Avoor id leaving
allergenstheorlungs
other irritants
" Clubbing of fingers
" Nicotine Stains 5. Ps yc ho lo gical Sup po rt
Major diseases
"1. Pitting
Pulmoedemanary Emphysema – airway is obstructed due to destroyed alveolar walls
"2. exertional
Chronic Bron dyspnea
chitis-orincr
dyspnea
eased at rest production that obstructs airway
mucus
- "3. Enlarged
Asthma pulsating liver
" Cough- with or without sputum production
Cause: Medical Management:
1. Cigarette smoking 1. Bronchodilators
2. Chronic respiratory infections CHRONIC BRONCHITIS
2. Antihistamines
"
3. Family history of COPD “Blue Bloater”
"
3. Steroids
4. Air pollution 4. Antibiotics
"
5. Expectorants
- "AnManifestations:
Clinical inflammation of the bronchi which causes increased mucus6.product ion athe
Oxygen ndrap
chryonic cough
at 2LP M –. use cautiously
- "Chron Few ic words
conditibetween
on is diagn osed if symptoms occur for 3 months and for 2 consecutive years.
breaths
" Pursed-lip breathing Nursing Management:
Cause:
" Cigarette
CyanosisSmoking, infection, pollution 1. Administer meds and O2 as ordered
" Distended neck veins 2. Promote adequate activities to enhance
" Barrel chest – increased diameter of thorax cardiovascular fitness
" Pulsus paradoxus – 3. Adequate rests
" Clubbing of fingers 4. Avoid allergens or other irritants
" Nicotine Stains 5. Psychological Support
Clinical Manifestations:
Pitting edema
exertional Slight gynecomastia
" dyspnea
Productiveor dyspnea
cough at rest
Enlarged Petechiae in midsternal area
" pulsating
Thicker, liver
more tenacious mucus
Cough- with or without sputum production Dyspnea
CHRONIC BRONCHITIS
“Blue Bloater”
120
- An inflammation of the bronchi which causes increased mucus production and chronic cough.
- Chronic condition is diagnosed if symptoms occur for 3 months and for 2 consecutive years.
Cause: Cigarette Smoking, infection, pollution
"
"
Clinical Manifestations:
" Decreased exercise tolerance
" Wheezes Slight gynecomastia
Productive cough Petechiae in midsternal area
Thicker,
Medical Management: more tenacious mucus
see COPD Dyspnea
Nursing Management:
1. Reduce or avoid irritants
2. Increase humidity
3. Administer medications as ordered 120
4. Chest physiotherapy
5. Postural drainage
6. Promote Breathing techniques
EMPHYSEMA
“Pink Puffer”
"
- A disorder"where the alveolar walls are destroyed causing permanent distention of air spaces.
- (+) dead areas in the lungs that do not participate in gas or blood exchange
Cause: Cigarette smoking,Decreased exercise tolerance
Alpha-anti-trypsin deficiency (an enzyme in the alveolar walls)
Wheezes
Clinical Manifestations: Nursing Management:
Medical
1. Management:
Dyspnea on ex see
ertiCOPD
on Position: Sit up and lean forward
2. Tachypnea Pulmonary toilet:
3. Management:
Nursing Barrel-chest Cough->Breathe deeply->Chest physiotherapy-> turn & position
41.. W
Rehdu
eecezesor avoid irritants Frequent rest periods
2. Pi
5. Incr
nkea
ishseski
hunmi codilotyr Nebulization
3. Sh
6. Admallo
iniwste
rarpimdedi
rescat pira s ordered IPPB – Intermittent Positive Pressure Breathing (aerosolized inhalation)
iontisonas
7.
4. Pu
Chrs
esed lip sibot
t phy rehe
athirangpy O2 @ 2LPM
You're Reading a Preview
5. Postural drainage
6. Promote Breathing techniques EMPHYSEMA
“Pink Puffer”
Asthma
Upload your documents to download.
-A condition where there is an increase responsiveness and/or spasm of the trachea and bronchi due to various stimuli
- A causes
which disordernarrowing veolar walls are destroyOR
where theofalairways ed causing permanent distention of air spaces.
- (+) dead areas in the lungs that do not participate in gas or blood exchange
Cause and Risk Factors:
Cause: Cigarette
1. FaBecome
smoking, tory oaf aScribd
mily hisAlpha-anti-trypsin member
sthma deficiency (an for
enzyme fullinaccess.
the alveolarYour
walls)
2. Allergens: dust, pollens,
Secondary smoke inhalatioNursing Management:
3.
Clinical Manifestations:
1. Dy4. spneaAoinr pex oler
lutition
on first Position: Sit are
30
n
days up and free.
lean forward
2. T 5.achypneSatress Pulmonary toilet:
3. Barrel-chest Cough->Breathe deeply->Chest physiotherapy-> turn & position
Types:
4. Wheezes Frequent rest periods
5.1. PiIm
nkmish
unsoki
longico
c alosrthma - Continue
oIPPB n cfor
Nebulization
hildhoFree
ccurs– iIntermittent od Positive Pressure Breathing (aerosolized inhalation)
6. Shallow rapid respirations
7.2. Pu
No rsn-
edimlimu
p bno lohi
reat gingc asthma - oc
O2cu@rs2LPM
in adulthood and assoc w/ recurrent resp infections.
- usually >35 y/o
3. Mixed, combined immunologic and non-immuno logic
Asthma
Clinical Manifestations: Nursing M anagement:
" Increased tightness of chest, dyspnea
" Tachycardia, tachypnea 1. Promote pulmonary ventilation
-A condition where
" thereDry, hacking, persistent
is an increase cough
responsiveness and/or spasm 2. Facilitate
of the tracheaexpectoration
and bronchi due to various stimuli
" (+) wheezes,
which causes narrowing of airwayscrackles 3. Health teaching
" Pallor, cyanosis, diaphoresis " Breathing techniques
Cause and Risk" Factors:
Chronic barrel chest, elevated shoulders " Stress management
1. Family history of asthma " Avoid allergens
2. " Alledistended
rgens: dusneck t, polveins
lens,
3. "Secorthopnea
ondary smoke inhalation
4. "Air Tenacious,
pollution mucoid sputum
5.t:
Tre atm en Stress
1. Steroids,
Types:
2. Antibiotics
3. Bro
Immnc
unho
oldi
oglaictoarss,thex
mpe
a ctoran- ts occurs in childhood
4.
1. O2, nebulization,
Non-immunologic asthma -aerosol occurs in adulthood and assoc w/ recurrent resp infections.
" - usually >35 y/o
2.
"
3. Mixed, combined immunologic and non-immunologic
Complication: STATUS
" ASTHMATICUS - a life-threatening asthmatic attack in w/c symptoms of asthma
Clinical Manifestations:
" Nursing to
continues and do not respond M atreatment
nagement:
" Increased tightness of chest, dyspnea "
II. PARENCHY M A L D ISO R D
Tachycardia, tachypnea E RS : Promote
" pulmonary ventilation
Dry, hacking, persistent cough 1. Facilitate
" expectoration
(+) wheezes, crackles 3. Health teaching
2.
"
" Pallor, cyanosis, diaphoresis Breathing techniques
"
Stress management 121
" Chronic barrel chest, elevated shoulders
Avoid allergens
distended neck veins
orthopnea
Tenacious, mucoid sputum
Tre atm en t:
1. Steroids,
2. Antibiotics
3. Bronchodilators, expectorants
O2, nebulization, aerosol
4. STATUS ASTHMATICUS -
Complication: a life-threatening asthmatic attack in w/c symptoms of asthma
continues and do not respond to treatment
PNEUMONIA
II. PARENCHYMAL DISORDERS:
- An inflammatory process of lung parenchyma assoc. w/ marked increase in alveolar and interstitial fluids
Etiology:
1. Bacterial / Viral – streptococcus pneumoniae, pseudomonas aeruginosa, influenza
2. Aspiration 121
3. Inhalation of irritating fumes
Risk factors:
1. Age: too young and elderly are most prone to develop
2. Smoking, air pollution
3. URTI
4. Altered conciousness
5. Tracheal intubation
6. Prolonged immobility: post-operative, bed-ridden patients
PNEUMONIA
Clinical Manifestations:
-
1. Chest pain, irritability, apprehensiveness, irritability, restlessness, nausea, anorexia, hx of exposure
2. Cough- productive , rusty/ yellowish/greenish sputum, splinting of affected side, chest retration
3. CXR, sputum culture, Blood culture, increased WBC, elevated sedimentation rate
An inflammatory process of lung parenchyma assoc. w/ marked increase in alveolar and interstitial fluids
Nursing Management:
Etiology:
1. Bacterial"/ Viral – streptoco
Promote ccus ventilation-
adequate pneumoniae, pseudomonas
positioning, Chestaephysiotherapy,
ruginosa, influenza
IPPB
2. Aspiration Provide rest and comfort
"
3. Inhalation of irritating fumes
" Prevent potential complications
You're Reading a Preview
Risk factors: " Health teaching: skin care, hygiene
1. Age" : tooDrug
youngtherapy:
and elderly are most prone to develop
2. Smoking, air o pollutAntibiotics:
ion penicillin, cephalosphorin, tetracycline, erythromycin
o Upload your documents to download.
3. URTI Cough suppressants
4. Altered concio o
usne ss
Expectorants
5. Tracheal intubation
" Rest and adequate activity bed-ridden patients
Prolonged immobility: post-operative, OR
6. " Proper Nutrition
Clinical Manifestations:
Become a Scribd member for full access. Your
PULMONARY EDEMA
1. Chest pain, irritability, apprehensiveness, irritability, restlessness, nausea, anorexia, hx of exposure
2. Cough- productive , rusty/ yelfirst 30
lowish/gre days
enish are
spu tum, free.
splinting of affected side, chest retration
"
3. CXR, sputum culture, Blood culture, increased WBC, elevated sedimentation rate
- often occurs"when the left side of the heart is distended and fails to pump adequately
"
Nursing Management:
Clinical Manifestation:o
o Constant irritating cough,
" Promote o
Continue
o dyspnea, crackles, cyanosis
adequate ventilation- for Free
positioning, Chest physiotherapy, IPPB
Provide rest and comfort
Pathophysiology: Prevent potential complications
"
"Health
Fluidteaching: skin care,
accumulation in thehygiene
alveolar sacs due to hypovolemia, fluid congestions in the lungs, alveoli
Drug
aretherapy:
congested
"
Antibiotics: penicillin, cephalosphorin, tetracycline, erythromycin
Nursing Management: Cough suppressants
"
1. Diuretics, low sodium diet, I&O
Expectorants
2. promote effective airway clearance, breathing patterns and ventilation
3. Rest
Moniand
tor Vadequate
S activity
4. Proper
PsychoNutrition
logical support
o
5. Administer medications PULMONARY EDEMA
TUBERCULOSIS
- often occurs when the left side of the heart is distended and fails to pump adequately
Clinical Manifestation:
Constant "cough, dyspnea, crackles, cyanosis
irritating
- A chronic lung infection that leads to consumption of alveolar tissues
EPathophysiology:
tiology: Mycobacterium tuberculosis.
Risk Factors: Fluid accumulation in the alveolar sacs due to hypovolemia, fluid congestions in the lungs, alveoli
Poor living conditions,are congested
overcrowded
1. Poor nutritional intake
Nursing
2. Pr Management:
evious infection
1. Diuretics, low sodium diet, I&O
2. promote effective airway clearance, breathing patterns and ventilation
3. Monitor VS
4. Psychological support
5. Administer medications 122
TUBERCULOSIS
You're reading a preview *
- A chronic lung infection that leads to consumption of alveolar tissues
Unlock full access (pages 9-22) by
Etiology: Mycobacterium tuberculosis.
Risk Factors:
uploading documents or with a
Poor living conditions, overcrowded
1. Poor nutritional intake
2. Previous infection 30 day free trial
Continue for Free
122
You're reading a preview *
Unlock full access (pages 26-32)
by uploading documents or with
a 30 day free trial
Continue for Free
You might also like
- Rehab Cheat SheetDocument18 pagesRehab Cheat SheetZ A100% (3)
- Medical Certificate for Cough, Sore Throat, HeadacheDocument1 pageMedical Certificate for Cough, Sore Throat, HeadacheJareena SamsonNo ratings yet
- Case HistoryDocument12 pagesCase HistoryEmmanuel Rojith Vaz0% (1)
- Eyelid Anatomy and Common Disorders GuideDocument26 pagesEyelid Anatomy and Common Disorders Guideking darkNo ratings yet
- Escoton, Kate Angel P (NCP)Document4 pagesEscoton, Kate Angel P (NCP)Kate EscotonNo ratings yet
- Bukidnon State University College of NursingDocument5 pagesBukidnon State University College of NursingAIZA MAE BANGGAY100% (1)
- Pain AssessmntDocument2 pagesPain Assessmntmohs2007100% (1)
- Medical Surgical NursingDocument59 pagesMedical Surgical Nursingnot your medz duranNo ratings yet
- Medical Surgical NursingDocument66 pagesMedical Surgical Nursing04eden100% (3)
- Andrian Dwi Herlambang (P17230181001) Acute PainDocument8 pagesAndrian Dwi Herlambang (P17230181001) Acute PainAndrian TakigawaNo ratings yet
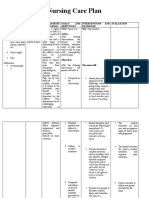
- NCP PainDocument4 pagesNCP PainFlauros Ryu JabienNo ratings yet
- Problem Scientific Basis Goals/Objectives Criteria Nursing Interventions Rationale Evaluation Date: November 9, 2021 Time: 10:00 AM Nursing Diagnosis: Goal Partially METDocument2 pagesProblem Scientific Basis Goals/Objectives Criteria Nursing Interventions Rationale Evaluation Date: November 9, 2021 Time: 10:00 AM Nursing Diagnosis: Goal Partially METGwyneth Christine TanNo ratings yet
- Typhoid Fever NCPDocument46 pagesTyphoid Fever NCPLyra Lustre RN67% (3)
- Nursing Care PlanDocument19 pagesNursing Care Planabigail gogoNo ratings yet
- Assessment NyeriDocument18 pagesAssessment NyerisnookumsnjNo ratings yet
- Nursing Care for Acute PainDocument3 pagesNursing Care for Acute PainJared Niles SantosNo ratings yet
- Diagnostic Findings:: Short Term Goal Short Term GoalDocument3 pagesDiagnostic Findings:: Short Term Goal Short Term GoalGiselle EstoquiaNo ratings yet
- Finals Notes UnfinishedDocument23 pagesFinals Notes UnfinishedNicholeGarcesCisnerosNo ratings yet
- College Nursing Care Plan TemplateDocument9 pagesCollege Nursing Care Plan TemplateCecil MonteroNo ratings yet
- Appendicitis - NCPDocument5 pagesAppendicitis - NCPEarl Joseph Deza100% (1)
- Appendicitis NCPDocument5 pagesAppendicitis NCPEarl Joseph DezaNo ratings yet
- Prioritizing Nursing Problems and Interventions for Postpartum PainDocument2 pagesPrioritizing Nursing Problems and Interventions for Postpartum PainFia GregorioNo ratings yet
- Idc NCPDocument14 pagesIdc NCPEnrique BabierraNo ratings yet
- Module 2M: Concept of PainDocument3 pagesModule 2M: Concept of PainDominic DegraciaNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainGeorge FogNo ratings yet
- Pain and Fever (Reviewer)Document5 pagesPain and Fever (Reviewer)James Lord GalangNo ratings yet
- Updated CH 30 Pain Assessment and ManagementDocument30 pagesUpdated CH 30 Pain Assessment and Managementaabbccss1.z71No ratings yet
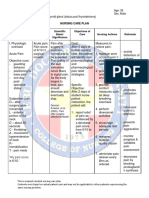
- Nursing Care Plan: Western Mindanao State University College of NursingDocument11 pagesNursing Care Plan: Western Mindanao State University College of NursingPatricia VasquezNo ratings yet
- Actual NCPDocument10 pagesActual NCPRouie Björn ABrianNo ratings yet
- NCM117 NCPDocument2 pagesNCM117 NCPHANNAH MICOLE GAERLANNo ratings yet
- Post-Operative Nursing Care Plan # 1Document14 pagesPost-Operative Nursing Care Plan # 1Vince John SevillaNo ratings yet
- Nursing Care Plan for Post-Surgical Pain ManagementDocument7 pagesNursing Care Plan for Post-Surgical Pain ManagementMacris BondocNo ratings yet
- 5 Hamad Core Comeptencies FinalDocument2 pages5 Hamad Core Comeptencies FinalvhonNo ratings yet
- PainDocument2 pagesPainAshley TwinkleNo ratings yet
- Nursing Care PlanDocument6 pagesNursing Care PlanRohmanNo ratings yet
- Ruby Mae L. Aguaviva N32 1. Acute Pain: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesRuby Mae L. Aguaviva N32 1. Acute Pain: Assessment Diagnosis Planning Intervention Rationale EvaluationRuby Mae AguavivaNo ratings yet
- Pain ManagementDocument7 pagesPain ManagementHazel ZullaNo ratings yet
- Pain Lesson PlanDocument17 pagesPain Lesson PlanbharadwajjagreetiNo ratings yet
- NCP For Case Presentation (Acute Pain, Episiotomy)Document3 pagesNCP For Case Presentation (Acute Pain, Episiotomy)Jenny Ajoc100% (2)
- GAYO C. Revised NCPDocument7 pagesGAYO C. Revised NCPCarl LacambraNo ratings yet
- Nursing Care Plan: Clustered Cues Nursing Diagnosis Rationale Outcome Criteria Nursing Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Clustered Cues Nursing Diagnosis Rationale Outcome Criteria Nursing Interventions Rationale EvaluationCLEMENT, EUGENE CHADNo ratings yet
- Sample Nursing Care PlanDocument1 pageSample Nursing Care PlanQuiannë Delos ReyesNo ratings yet
- NCP Acute PainDocument2 pagesNCP Acute PainKhleanne CastilloNo ratings yet
- Acute PainDocument5 pagesAcute PainEricka MunsayacNo ratings yet
- This Chart Contains Information Provided by PatientsDocument4 pagesThis Chart Contains Information Provided by PatientsCecilia MendezNo ratings yet
- Pain Management Nursing Skills TypesDocument4 pagesPain Management Nursing Skills TypesBrittania CorbittNo ratings yet
- Managing Chronic Pain BiopsychosocialDocument169 pagesManaging Chronic Pain BiopsychosocialGabriel DelfinoNo ratings yet
- Ncm116 Lesson2 Rle Pain ManagementDocument4 pagesNcm116 Lesson2 Rle Pain ManagementMilcah NuylesNo ratings yet
- Pain assessment toolsDocument22 pagesPain assessment toolspuchioNo ratings yet
- Demonstrate: Pain Coping TechniquesDocument4 pagesDemonstrate: Pain Coping TechniquesMae Therese B. MAGNO100% (1)
- Nursing Care Plan Preoperative Cues Nursing Diagnosis Objectives Nursing Interventions Rationale Evaluation SubjectiveDocument5 pagesNursing Care Plan Preoperative Cues Nursing Diagnosis Objectives Nursing Interventions Rationale Evaluation SubjectiveShamsa AfdalNo ratings yet
- NCP For ChronicPain PDFDocument2 pagesNCP For ChronicPain PDFjay kusainNo ratings yet
- NCP Drug Study, Ojoy Dan Joshua LDocument2 pagesNCP Drug Study, Ojoy Dan Joshua Ldan.ojoy18No ratings yet
- Chap 10 - Lewis MSN Philippine 8eDocument26 pagesChap 10 - Lewis MSN Philippine 8eCHABELITA DAVIDNo ratings yet
- Nursing Care Plan - Acute Pain Assessment Diagnosis Scientific Rationale Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan - Acute Pain Assessment Diagnosis Scientific Rationale Planning Intervention Rationale EvaluationNicole cuencosNo ratings yet
- Module 5 HA Pain Assessment The Fifth Vital SignsDocument12 pagesModule 5 HA Pain Assessment The Fifth Vital SignsCalvo AdrianNo ratings yet
- Midterms GeriaDocument18 pagesMidterms GeriaGiselle Estoquia100% (1)
- Nursing Care PlanDocument30 pagesNursing Care PlanJam CorrosNo ratings yet
- NCPDocument4 pagesNCPfairwoods90% (10)
- Question 1. Hypothetical Situation Which Includes Client's Assessment (History, Manifestations, Etc ) To Establish The ConditionDocument12 pagesQuestion 1. Hypothetical Situation Which Includes Client's Assessment (History, Manifestations, Etc ) To Establish The ConditionJoie JoieNo ratings yet
- PAIN FinalDocument23 pagesPAIN Finalneelimawanker chinnariNo ratings yet
- Nursing Intervention Reduces Abdominal PainDocument3 pagesNursing Intervention Reduces Abdominal PainNicole Mendonis LunarNo ratings yet
- NCPDocument6 pagesNCPAndrea Marie SevillaNo ratings yet
- The Somatic Toolkit: A Comprehensive Guide to Healing Trauma Through Somatic Practices: Unlock Your Body's Potential for Deep Healing and RestorationFrom EverandThe Somatic Toolkit: A Comprehensive Guide to Healing Trauma Through Somatic Practices: Unlock Your Body's Potential for Deep Healing and RestorationNo ratings yet
- Types of MalnutritionDocument8 pagesTypes of Malnutritionkazz!No ratings yet
- March 2016 (v2) QP - Paper 2 CIE Biology A-LevelDocument16 pagesMarch 2016 (v2) QP - Paper 2 CIE Biology A-LevelShazia AsifNo ratings yet
- Understanding Lewy Body DementiasDocument15 pagesUnderstanding Lewy Body DementiasCecilia Flores JaraNo ratings yet
- Acute Abdominal Pain History and Exam HPCDocument5 pagesAcute Abdominal Pain History and Exam HPCnaafNo ratings yet
- A Successful Case Study On Ayurvedic Management of HypothyroidismDocument6 pagesA Successful Case Study On Ayurvedic Management of HypothyroidismIJRASETPublicationsNo ratings yet
- Vitamin C and FatigueDocument7 pagesVitamin C and FatigueSteveNo ratings yet
- DR Vibhor PardasaniDocument19 pagesDR Vibhor PardasaniPushpanjali Crosslay HospitalNo ratings yet
- Discharge Plan Patient Teaching Pleural Effusion CastleDocument6 pagesDischarge Plan Patient Teaching Pleural Effusion Castleapi-341263362100% (2)
- MumpsDocument3 pagesMumpsAbeer FatimaNo ratings yet
- OsteoporoseDocument54 pagesOsteoporoseJandui DinizNo ratings yet
- CHD 128 Communicable Diseases and Control AssignmentDocument2 pagesCHD 128 Communicable Diseases and Control AssignmentDani AnyikaNo ratings yet
- Staphylococcus Aureus PhisiologyDocument21 pagesStaphylococcus Aureus PhisiologyJohann MuñozNo ratings yet
- Nama: Lubbul Aqil Maltuf (19010081) Dan Moh. Alvin Zalif F (19010091) Kelas: 19B Prodi: S1 Keperawatan Dialog: Asking Patient Medical HistoryDocument4 pagesNama: Lubbul Aqil Maltuf (19010081) Dan Moh. Alvin Zalif F (19010091) Kelas: 19B Prodi: S1 Keperawatan Dialog: Asking Patient Medical HistoryAll 17No ratings yet
- @slight - Cristobal v. Employees Compensation Commission, G.R. No. L-49280, Feb. 26, 1981Document9 pages@slight - Cristobal v. Employees Compensation Commission, G.R. No. L-49280, Feb. 26, 1981James OcampoNo ratings yet
- Social Determinants of HealthDocument2 pagesSocial Determinants of HealthKeerthi sanapala7278No ratings yet
- Perioralpigmentation PublishedDocument16 pagesPerioralpigmentation PublishedBrahmaiah UpputuriNo ratings yet
- Canine Viral Enteritis: Nipah and Hendra Virus InfectionsDocument9 pagesCanine Viral Enteritis: Nipah and Hendra Virus InfectionsAnnahi BcNo ratings yet
- Prepositions-Of-Time-Grammar-Guides - Sin RespuestaDocument1 pagePrepositions-Of-Time-Grammar-Guides - Sin RespuestaCarla BonanoNo ratings yet
- Assessment and Management of Patients With Endocrine DisordersDocument78 pagesAssessment and Management of Patients With Endocrine Disordershenny1620100% (1)
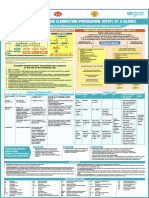
- NTEP at A Glance - Comprehensive Clinical Management Protocol For TBDocument1 pageNTEP at A Glance - Comprehensive Clinical Management Protocol For TBNael NajeebNo ratings yet
- Klebsiella Pneumoniae Pathogenesis: Etiology/BacteriologyDocument4 pagesKlebsiella Pneumoniae Pathogenesis: Etiology/Bacteriologysuper cute100% (1)
- NRSG 780 - Health Promotion and Population Health: Module 3: EpidemiologyDocument34 pagesNRSG 780 - Health Promotion and Population Health: Module 3: EpidemiologyjustdoyourNo ratings yet
- Davainea Proglottina - A Potentially Underestimated PDFDocument3 pagesDavainea Proglottina - A Potentially Underestimated PDFryan100% (1)
- Schizophrenia Clinical Presentation - History, Physical Examination, ComplicationsDocument4 pagesSchizophrenia Clinical Presentation - History, Physical Examination, ComplicationsdilaNo ratings yet
- Clinical Review: The Management of Lower Urinary Tract Symptoms in MenDocument4 pagesClinical Review: The Management of Lower Urinary Tract Symptoms in MenSan Phạm ĐìnhNo ratings yet
- CARDIOVASCULAR EXAMINATION Human DiseaseDocument4 pagesCARDIOVASCULAR EXAMINATION Human DiseaseVictoria MedfordNo ratings yet