Professional Documents
Culture Documents
INFORMATION SHEET 1. - Risk Categorisation Guidelines: Protection Against The Specified Infectious Diseases Is Required
Uploaded by
jacksonzchenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
INFORMATION SHEET 1. - Risk Categorisation Guidelines: Protection Against The Specified Infectious Diseases Is Required
Uploaded by
jacksonzchenCopyright:
Available Formats
Occupational assessment, screening and vaccination
against specified infectious diseases PROCEDURES
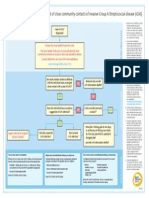
INFORMATION SHEET 1. – Risk categorisation guidelines
Category A
Protection against the specified infectious diseases is required
Direct physical contact with:
− patients/clients
− deceased persons, body parts
− blood, body substances, infectious material or surfaces or equipment that might contain these (eg soiled
linen, surgical equipment, syringes)
Contact that would allow the acquisition or transmission of diseases that are spread by respiratory means.
Includes persons:
− whose work requires frequent/prolonged face-to-face contact with patients or clients eg interviewing or
counselling individual clients or small groups; performing reception duties in an emergency/outpatients
department;
− whose normal work location is in a clinical area such as a ward, emergency department, outpatient clinic
(including, for example, ward clerks and patient transport officers); or
− who frequently throughout their working week are required to attend clinical areas, eg food services staff
who deliver meals.
All persons working with the following high risk client groups or in the following high risk clinical areas are
automatically considered to be Category A, regardless of duties.
High risk client groups High risk clinical areas
− Children less than 2 years of age − Ante-natal, peri-natal and post-natal areas including labour
including neonates and wards and recovery rooms
premature infants − Neonatal Intensive Care Units and Special Care Units
− Pregnant women − Paediatric wards
− Immunocompromised clients − Transplant and oncology wards
− Intensive Care Units
− Emergency Departments
− Operating theatres, and recovery rooms treating restricted
client groups
− Ambulance and paramedic care services
− Laboratories
All health care students are Category A.
Category B
Does not require protection against the specified infectious diseases as
level of risk is no greater than that of the general community
− Does not work with the high risk client groups or in the high risk clinical areas listed above.
− No direct physical contact with patients/clients, deceased persons, blood, body substances or infectious
material or surfaces/equipment that might contain these.
− Normal work location is not in a clinical area, eg administrative staff not working in a ward environment,
food services staff in kitchens.
− Only attends clinical areas infrequently and for short periods of time eg visits a ward occasionally on
administrative duties; is a maintenance contractor undertaking work in a clinical area.
− Although such persons may come into incidental contact with patients (eg in elevators, cafeteria, etc) this
would not normally constitute a greater level of risk than for the general community.
PD2011_005 Issue date: January 2011 Page 19
Occupational assessment, screening and vaccination
against specified infectious diseases PROCEDURES
INFORMATION SHEET 2. – Checklist: Evidence required from
Category A applicants
Evidence required to demonstrate protection against the specified infectious diseases
1. Acceptable evidence of protection against specified infectious diseases includes:
a written record of vaccination signed by the medical practitioner, and/or
serological confirmation of protection, and/or
other evidence, as specified in the table below.
NB: the health facility may require further evidence of protection, eg serology, if the vaccination record does
not contain vaccine brand and batch or official certification from vaccination provider (eg clinic/practice stamp)
2. TST screening is required if the person was born in a country with a high incidence of TB, or has resided
for a cumulative time of 3 months or longer in a country with a high incidence of TB, as listed
at: http://www.health.nsw.gov.au/Infectious/tuberculosis/Documents/countries-incidence.pdf
3. In certain specialised clinical settings, for example, in transplant, oncology or neonatal wards, the health facility
may require serological evidence of protection (in addition to evidence of vaccination or other evidence) to ensure
that the risk to vulnerable patients is minimised.
Disease Evidence of vaccination Documented serology results Other acceptable
evidence
Diphtheria,
tetanus,
One adult dose of
Serology will not be accepted Not applicable
diphtheria/ tetanus/
pertussis pertussis vaccine
(whooping (dTpa). Not ADT.
cough)
Hepatitis B
History of completed age- Anti-HBs greater than or Documented
appropriate course of equal to 10mIU/mL evidence of anti-
hepatitis B vaccine. Not HBc, indicating
“accelerated” course. and or past hepatitis B
infection
Measles,
mumps,
2 doses of MMR vaccine Positive IgG for measles, Birth date before
at least one month apart mumps and rubella 1966
rubella or or
(MMR)
Varicella
(chickenpox)
2 doses of varicella vaccine Positive IgG for varicella History of
at least one month apart chickenpox or
(evidence of one dose is physician-
sufficient if the person was diagnosed
vaccinated before shingles (serotest
or or
14 years of age) if uncertain)
Tuberculosis
(TB) Not applicable
Tuberculin skin
test (TST)
See note 2 Note: interferon-gamma release immunoassay (IGRA) is not
above for list generally accepted. In the event that an IGRA has been
of persons Not applicable performed, screening by TST will be required if the IGRA result
requiring is negative or equivocal.
TST Persons with positive TST/IGRA must be fully assessed by a TB
screening service within 3 months of commencement of clinical duties or
clinical placement and must be asymptomatic when
commencing clinical duties or clinical placement.
Influenza Annual influenza vaccination is not a requirement, but is strongly recommended
PD2011_005 Issue date: January 2011 Page 20
Occupational assessment, screening and vaccination
against specified infectious diseases PROCEDURES
INFORMATION SHEET 3. – Specified infectious diseases: risks,
consequences of exposure and protective measures
The following table provides a brief description of the infectious diseases specified in this
policy directive and links to further information, including risks of infection, consequences of
infection and, where relevant, management in the event of exposure.
Fact sheets on each of the listed diseases are available in an A-Z list on the NSW Health
website at: http://www.health.nsw.gov.au/Infectious/factsheets/Pages/default.aspx
The Australian Immunisation Handbook (current edition) is available online
at: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook10
-home
Hepatitis B Blood-borne viral disease. Can lead to a range of diseases including chronic
(HBV) hepatitis B infection, cirrhosis and liver cancer. Anyone not immune through
vaccination or previous infection is at risk of infection via blood or other body fluids
entering through broken skin, mucous membrane, injection/ needlestick,
unprotected sex or from HBV positive mother to child during birth. Specific at risk
groups include: health care workers, sex partners of infected people, injecting drug
users, haemodialysis patients. Management in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/hepb.aspx
Diphtheria Contagious, potentially life-threatening bacterial infection, now rare in Australia
because of immunisation. Spread via respiratory droplets and discharges from the
nose, mouth or skin. Infectious for up to 4 weeks from onset of symptoms. Anyone
not immune through vaccination or previous infection is at risk. Diphtheria toxin
(produced by the bacteria) can cause inflammation of the heart muscle, leading to
death. Management in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/diphtheria.aspx
Tetanus Infection from a bacterium usually found in soil, dust and animal faeces. Toxin from
the bacterium can attack the nervous system. Although the disease is now fairly
uncommon, it can be fatal. Not spread from person to person. Generally occurs
through injury. Neonatal tetanus can occur in babies of inadequately immunised
mothers. Mostly older adults who were never adequately immunised. Management
in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/tetanus.aspx
Pertussis Highly infectious bacterial infection, spread by respiratory droplets through
(Whooping coughing or sneezing. Cough that persists for more than 3 weeks and, in children,
cough) may be accompanied by paroxysms, resulting in a “whoop” sound or vomiting.
Anyone not immune through vaccination is at risk of infection and/or transmission.
Can be fatal, especially in babies under 12 months of age. Management in the
event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/pertussis.aspx
PD2011_005 Issue date: January 2011 Page 21
Occupational assessment, screening and vaccination
against specified infectious diseases PROCEDURES
Measles Highly infectious viral disease, spread by respiratory droplets - infectious before
symptoms appear and for several days afterwards. Serious complications such as
ear infection, pneumonia, or encephalitis can occur in up to 1/3 of cases. At risk are
persons born during or after 1966 who haven’t had 2 doses of MMR vaccine, babies
st
under 12 months of age, before they have had a 1 dose and children over 4 years
nd
of age who have not had a 2 dose. Management in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/measles.aspx
Mumps Viral disease, spread by respiratory droplets. Now relatively uncommon in Australia
because of immunisation. Anyone not immune through vaccination or previous
infection is at risk. Persons who have the infection after puberty can have serious
complications, eg swelling of testes or ovaries; encephalitis or meningitis may occur
rarely. Management in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/mumps.aspx
Rubella Viral disease, spread by respiratory droplets and direct contact. Infectious before
(German symptoms appear and for several days afterwards. Anyone not immune through
Measles) vaccination or previous infection is at risk. In early pregnancy, can cause birth
defects or miscarriage. Management in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/rubella.aspx
Varicella Viral disease, relatively minor in children, but can be severe in adults and
(Chicken immunosuppressed persons, leading to pneumonia or inflammation of the brain. In
pox) pregnancy, can cause foetal malformations. Early in the infection, varicella can be
spread through coughing and respiratory droplets; later in the infection, it is spread
through contact with fluid in the blisters. Anyone not immune through vaccination or
previous infection is at risk. Management in the event of exposure:
see http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/han
dbook10-4-22
Tuberculosis A bacterial infection that can attack any part of the body, but the lungs are the most
(TB) common site. Spread via respiratory droplets when an infected person sneezes,
coughs or speaks. At risk are those who spend time with a person with TB infection
of the lung or respiratory tract or anyone who was born in, or has lived or travelled for
more than 3 months in, a high TB incidence country. Management in the event of
exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/tuberculosis.asp
x
Seasonal Viral infection, with the virus regularly changing. Mainly affects the lungs, but can
influenza affect the heart or other body systems, particularly in people with other health
(Flu) problems, leading to pneumonia and/or heart failure. Spread via respiratory droplets
when an infected person sneezes or coughs, or through touch, eg handshake.
Spreads most easily in confined and crowded spaces. Anyone not immune through
annual vaccination is at risk, but the elderly and small children are at most risk of
infection. Management in the event of exposure:
see http://www.health.nsw.gov.au/Infectious/controlguideline/Pages/influenza.aspx
PD2011_005 Issue date: January 2011 Page 22
You might also like
- INFECTIOUS DISEASES: INFLUENZA, SEPTICEMIA, DIPHTHERIA, PERTUSSISDocument8 pagesINFECTIOUS DISEASES: INFLUENZA, SEPTICEMIA, DIPHTHERIA, PERTUSSISSoojung NamNo ratings yet
- Policy Vaccination Record CardDocument2 pagesPolicy Vaccination Record CardGurpreetNo ratings yet
- Module 2 - Community Health NursingDocument9 pagesModule 2 - Community Health NursingMarie Kelsey Acena Macaraig100% (1)
- Elements of EPIDocument2 pagesElements of EPIMichelle Gambol50% (2)
- Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino WomenDocument7 pagesOb 1.05 Clinical Practice Guidelines On Immunization For Filipino Womenotartil_niman50% (2)
- Renal Vegetarian NutritionDocument2 pagesRenal Vegetarian NutritionSg Balaji100% (1)
- MCQs blood & cell physiology blogDocument8 pagesMCQs blood & cell physiology bloglubna malikNo ratings yet
- Family Case Study For HydrocephalusDocument9 pagesFamily Case Study For HydrocephalusjaegergranNo ratings yet
- PSYC1001 Unit of Study OutlineDocument84 pagesPSYC1001 Unit of Study OutlinejacksonzchenNo ratings yet
- Tilak Shah MD-NMS Medicine Casebook (2008)Document1,207 pagesTilak Shah MD-NMS Medicine Casebook (2008)John Link100% (1)
- Childhood Immunization & Catch Up Immunization-2Document53 pagesChildhood Immunization & Catch Up Immunization-2Haters ExterminatorNo ratings yet
- Disease Prediction Using Machine LearningDocument10 pagesDisease Prediction Using Machine LearningIJRASETPublicationsNo ratings yet
- Diseases Under Surveillance: PIDSR ObjectivesDocument61 pagesDiseases Under Surveillance: PIDSR ObjectivesGina BoligaoNo ratings yet
- FundaDocument5 pagesFundaGreggy Francisco LaraNo ratings yet
- Asthma Lesson PlanDocument26 pagesAsthma Lesson PlanBharat Singh BanshiwalNo ratings yet
- Identification and classification of infections in neonatesDocument62 pagesIdentification and classification of infections in neonatesvisuinsvu100% (7)
- Host Defenses To Infection: Tarek Amin DR Amira GamalDocument44 pagesHost Defenses To Infection: Tarek Amin DR Amira GamalWira SundokoNo ratings yet
- Adult Immunization Recommendations SummaryDocument5 pagesAdult Immunization Recommendations SummaryHannah Caburian RemoNo ratings yet
- Neonatal Infection Prevention and ControlDocument2 pagesNeonatal Infection Prevention and ControlJaymeeNo ratings yet
- TBDocument5 pagesTBQuezon D. Lerog Jr.No ratings yet
- 1.CD Control Program: RD RDDocument18 pages1.CD Control Program: RD RDKen Mark CatubigNo ratings yet
- Herpes GuideDocument12 pagesHerpes GuidesDamnNo ratings yet
- What Is PlagueDocument3 pagesWhat Is Plagueanon_959000253No ratings yet
- 1 CombineDocument726 pages1 CombineSong Hành Vạn KiếpNo ratings yet
- Pulmonary TB, Lung AbscessDocument47 pagesPulmonary TB, Lung AbscessCC Samson, Caesar AnthonyNo ratings yet
- Tetanus: Acute Communicable Disease Control Manual (B-73) Revision - February 2012Document2 pagesTetanus: Acute Communicable Disease Control Manual (B-73) Revision - February 2012Hisashi Ren MinamotoNo ratings yet
- IMMUNIZATIONDocument2 pagesIMMUNIZATIONdomo domoNo ratings yet
- Immunization - Dr. SarahDocument14 pagesImmunization - Dr. Sarahf6bk6xnppyNo ratings yet
- TetanusDocument4 pagesTetanusΔΗΜΗΤΡΙΟΣ ΔΟΥΚΑΣNo ratings yet
- CDC Diphtheria Surveillance WorksheetDocument6 pagesCDC Diphtheria Surveillance WorksheetLuna WhiteNo ratings yet
- Community WrittenDocument23 pagesCommunity WrittenImPrint CenterNo ratings yet
- Stay Healthy, Stay On Top of Vaccinations: CDC Click Here For The CDC's Full Vaccination ChartDocument4 pagesStay Healthy, Stay On Top of Vaccinations: CDC Click Here For The CDC's Full Vaccination ChartcircularreasoningNo ratings yet
- Introduction: Hepatitis A Maurice HillemanDocument19 pagesIntroduction: Hepatitis A Maurice Hillemanahmed solimanNo ratings yet
- Jurnal 882Document1 pageJurnal 882saddamNo ratings yet
- NR 224 Week 1 Instuctor Unit 1 Questions and AnswersDocument7 pagesNR 224 Week 1 Instuctor Unit 1 Questions and AnswersJesse JohnsonNo ratings yet
- Tuberculin Skin TestingDocument4 pagesTuberculin Skin Testingmick saNo ratings yet
- Immunization and Prophylaxis: Childhood Immunization Has Reduced The Impact - Active Immunization Is TheDocument18 pagesImmunization and Prophylaxis: Childhood Immunization Has Reduced The Impact - Active Immunization Is TheCabdiNo ratings yet
- Module 3 Triage SARIDocument26 pagesModule 3 Triage SARIEstefania Cuta HernandezNo ratings yet
- TB Guidance Chapter 2Document15 pagesTB Guidance Chapter 2dindaNo ratings yet
- Measles Aug 2014Document23 pagesMeasles Aug 2014Shahab UddinNo ratings yet
- Annexure-XX Clinical Management Protocol: (Novel Influenza A H1N1)Document3 pagesAnnexure-XX Clinical Management Protocol: (Novel Influenza A H1N1)Ramadi PrameelaNo ratings yet
- Lecture 2 - MeaslesDocument33 pagesLecture 2 - MeaslesShaimaa AbdulkadirNo ratings yet
- Igas Flow ChartDocument1 pageIgas Flow ChartYi Wei KoNo ratings yet
- Pms SummaryDocument40 pagesPms SummaryRoscelie KhoNo ratings yet
- Measles: Investigative GuidelinesDocument17 pagesMeasles: Investigative GuidelinesDennis DennisNo ratings yet
- TB in Children: Department of Pediatrics College of Medicine Cagayan State UniversityDocument49 pagesTB in Children: Department of Pediatrics College of Medicine Cagayan State UniversityyayayanizaNo ratings yet
- V.3 21195 Sinopharm Vaccine Explainer 24Document6 pagesV.3 21195 Sinopharm Vaccine Explainer 24Mohammad Hisham BhawpalNo ratings yet
- DM2016-0337: Confirmed Diphtheria Investigation and ResponseDocument6 pagesDM2016-0337: Confirmed Diphtheria Investigation and ResponseJezza Jonah AclanNo ratings yet
- COVID-19 InterimGuidelines Treatment ENGDocument24 pagesCOVID-19 InterimGuidelines Treatment ENGHouda LaatabiNo ratings yet
- Pentaxim-Pi-Sg Pen 0118 Spc0914Document10 pagesPentaxim-Pi-Sg Pen 0118 Spc0914walkrogNo ratings yet
- Immunization EPI Huda 201212Document5 pagesImmunization EPI Huda 201212Aerish TupazNo ratings yet
- UF Immunization Cheat Sheet PDFDocument8 pagesUF Immunization Cheat Sheet PDFJag UnathNo ratings yet
- Adult ImmunizationDocument6 pagesAdult ImmunizationAmit GoelNo ratings yet
- COVID-19 InterimGuidelines Treatment ENGDocument25 pagesCOVID-19 InterimGuidelines Treatment ENGMartin PaturlanneNo ratings yet
- 47 Antimycobacterial DrugsDocument77 pages47 Antimycobacterial DrugsKriziaoumo P. OrpiaNo ratings yet
- LiphDocument33 pagesLiphMaritess Margarico ClaritoNo ratings yet
- Vaccination 2023-1Document59 pagesVaccination 2023-1Mohammad Moufaq El-BashabshehNo ratings yet
- Intra-Uterine and Perinatal InfectionDocument72 pagesIntra-Uterine and Perinatal InfectionsabrinaNo ratings yet
- PTB Grand Case Pres Group A 1Document46 pagesPTB Grand Case Pres Group A 1Community BNo ratings yet
- Highly Pathogenic Avian InfluenzaDocument25 pagesHighly Pathogenic Avian Influenzaainzahir94No ratings yet
- COMMUNICABLE DISEASES PREVENTIONDocument136 pagesCOMMUNICABLE DISEASES PREVENTIONCharmaine BonifacioNo ratings yet
- Neonatal Tetanus SurveillanceDocument14 pagesNeonatal Tetanus SurveillanceNadiah Husnul KhotimahNo ratings yet
- Wisconsin Varicella Surveillance GuidelineDocument4 pagesWisconsin Varicella Surveillance GuidelineVidinikusumaNo ratings yet
- CasefindingDocument52 pagesCasefindingdecebelle alabaNo ratings yet
- Good Health in the Tropics: Advice to Travellers and SettlersFrom EverandGood Health in the Tropics: Advice to Travellers and SettlersNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- Coronavirus Crisis: Information and Help in the 2020 Pandemic - What Everyone Should KnowFrom EverandCoronavirus Crisis: Information and Help in the 2020 Pandemic - What Everyone Should KnowNo ratings yet
- Corona Virus: Information You Need and How to Protect Yourself and Your Fellow Human BeingsFrom EverandCorona Virus: Information You Need and How to Protect Yourself and Your Fellow Human BeingsNo ratings yet
- 433-Article Text-1208-1-10-20181126Document7 pages433-Article Text-1208-1-10-20181126jacksonzchenNo ratings yet
- Depression TheoryDocument2 pagesDepression Theoryأحمد نور الهدايةNo ratings yet
- Alcohol Consumption During Pregnancy:: Results From The 2010 National Drug Strategy Household SurveyDocument27 pagesAlcohol Consumption During Pregnancy:: Results From The 2010 National Drug Strategy Household SurveyjacksonzchenNo ratings yet
- IJP Volume 5 Issue 9 Pages 5751-5778Document27 pagesIJP Volume 5 Issue 9 Pages 5751-5778jacksonzchenNo ratings yet
- Fetal Alcohol Spectrum Disorder: Knowledge, Attitudes and Practice Within The Western Australian Justice SystemDocument118 pagesFetal Alcohol Spectrum Disorder: Knowledge, Attitudes and Practice Within The Western Australian Justice SystemjacksonzchenNo ratings yet
- Fact Sheet-Voluntary and Involuntary AdmissionDocument2 pagesFact Sheet-Voluntary and Involuntary AdmissionjacksonzchenNo ratings yet
- Examining Trends in Alcohol Consumption During Pregnancy in Australia, 2001-2016Document18 pagesExamining Trends in Alcohol Consumption During Pregnancy in Australia, 2001-2016jacksonzchenNo ratings yet
- I'm Sure It's Fine: Why Highly Educated Women Report Higher Rates of Alcohol Consumption During PregnancyDocument50 pagesI'm Sure It's Fine: Why Highly Educated Women Report Higher Rates of Alcohol Consumption During PregnancyjacksonzchenNo ratings yet
- Trainee in Difficulty 2ndDocument44 pagesTrainee in Difficulty 2ndsiriopa08No ratings yet
- NEUR3005 Dementia 2019 NotesDocument42 pagesNEUR3005 Dementia 2019 NotesjacksonzchenNo ratings yet
- Eval Rep 4 SMSICDocument49 pagesEval Rep 4 SMSICjacksonzchenNo ratings yet
- Prescribing Drugs of Dependence in General Practice Part B BenzodiazepinesDocument101 pagesPrescribing Drugs of Dependence in General Practice Part B BenzodiazepinesjacksonzchenNo ratings yet
- Report AnticoagulationDocument171 pagesReport AnticoagulationjacksonzchenNo ratings yet
- Altered Resting-State Functional Connectivity of Default-Mode Network and Sensorimotor Network in Heavy Metal Music LoversDocument6 pagesAltered Resting-State Functional Connectivity of Default-Mode Network and Sensorimotor Network in Heavy Metal Music LoversjacksonzchenNo ratings yet
- A Simple Framework For Behavioral Experiments Using The Psychophysics Toolbox For MATLABDocument32 pagesA Simple Framework For Behavioral Experiments Using The Psychophysics Toolbox For MATLABjacksonzchenNo ratings yet
- CPAT3201 Adaptive and Innate Immune ResponsesDocument20 pagesCPAT3201 Adaptive and Innate Immune ResponsesjacksonzchenNo ratings yet
- 2019 Anatomy of A Memory Second Lecture Without AnswersDocument30 pages2019 Anatomy of A Memory Second Lecture Without AnswersjacksonzchenNo ratings yet
- Faculty of Science: PHSI2005@physiol - Usyd.edu - AuDocument27 pagesFaculty of Science: PHSI2005@physiol - Usyd.edu - AujacksonzchenNo ratings yet
- 2019 NEUR3005 3905 Hypothalamus - AggressionDocument34 pages2019 NEUR3005 3905 Hypothalamus - AggressionjacksonzchenNo ratings yet
- Psychology, 54, 292-342Document1 pagePsychology, 54, 292-342jacksonzchenNo ratings yet
- 1 s2.0 S0896627318307414 MainDocument14 pages1 s2.0 S0896627318307414 MainjacksonzchenNo ratings yet
- Microbes Impact Global Food SupplyDocument8 pagesMicrobes Impact Global Food SupplyjacksonzchenNo ratings yet
- CodeDocument7 pagesCodejacksonzchenNo ratings yet
- Ethics Tutorial NotesDocument1 pageEthics Tutorial NotesjacksonzchenNo ratings yet
- Code-Breaking Techniques for Common CiphersDocument7 pagesCode-Breaking Techniques for Common CiphersjacksonzchenNo ratings yet
- 2014 HSC Chemistry PDFDocument42 pages2014 HSC Chemistry PDFlillianaNo ratings yet
- SSP Dna GelsDocument10 pagesSSP Dna GelsjacksonzchenNo ratings yet
- Bio CalcsDocument4 pagesBio CalcsjacksonzchenNo ratings yet
- The Function and Anatomy of the LungsDocument20 pagesThe Function and Anatomy of the LungsNkosinathi ShongweNo ratings yet
- To Remember The Four Causes of Cell InjuryDocument43 pagesTo Remember The Four Causes of Cell Injuryapi-3825096No ratings yet
- Dementia Presentation Feb 19Document28 pagesDementia Presentation Feb 19Rhu Pugo, La UnionNo ratings yet
- Antibióticos para La Neumonía Asociada Al Ventilador.Document96 pagesAntibióticos para La Neumonía Asociada Al Ventilador.Julio GonzalesNo ratings yet
- Biochemistry Assignment: On Acid-Base BalanceDocument4 pagesBiochemistry Assignment: On Acid-Base BalanceMuhammed ElRakabawiNo ratings yet
- Peritoneal DialysisDocument9 pagesPeritoneal Dialysispinkygurlz1990No ratings yet
- Acute and Chronic PyelonephritisDocument7 pagesAcute and Chronic PyelonephritisMatthew Ryan100% (1)
- 3 Ceramic Pot Water FilterDocument32 pages3 Ceramic Pot Water Filtermohammed abdellaNo ratings yet
- CHAPTER II Open BurningDocument6 pagesCHAPTER II Open Burningjedric_14100% (1)
- A 55-Year-Old Woman With Shock and Labile Blood PressureDocument11 pagesA 55-Year-Old Woman With Shock and Labile Blood PressureMr. LNo ratings yet
- Unseen PassageDocument7 pagesUnseen PassageVinay OjhaNo ratings yet
- Discussion Topics: Seafood Red ListDocument3 pagesDiscussion Topics: Seafood Red ListНадія ЛупійNo ratings yet
- Rundown Iomu 071019 - 08.10 PDFDocument13 pagesRundown Iomu 071019 - 08.10 PDFEfi OctavianyNo ratings yet
- Venipuncture Techniques and ProceduresDocument66 pagesVenipuncture Techniques and ProceduresAngelica Camille B. AbaoNo ratings yet
- AcupunctureDocument15 pagesAcupuncturezextorcNo ratings yet
- Emropub 2016 en 19266Document45 pagesEmropub 2016 en 19266jamshaidjiNo ratings yet
- WORKSHEET 3 Lymphocyte ActivationDocument5 pagesWORKSHEET 3 Lymphocyte ActivationNeha ChoudharyNo ratings yet
- 2019-04-01 Good Housekeeping PDFDocument126 pages2019-04-01 Good Housekeeping PDFTiểu MyNo ratings yet
- Iet Me Introduce My Name Najib MahfuzhDocument2 pagesIet Me Introduce My Name Najib MahfuzhnajibNo ratings yet
- Dhatupaushtik ChurnaDocument6 pagesDhatupaushtik ChurnaShoeb MirzaNo ratings yet
- Bio SafetyDocument57 pagesBio SafetySatyaveer SinghNo ratings yet
- Group 2 Research G8Document24 pagesGroup 2 Research G8aurasaliseNo ratings yet
- Medicinal Properties of GarlicDocument7 pagesMedicinal Properties of GarlicFawzia Haznah Nurul Imani0% (1)