Professional Documents
Culture Documents
Reverse Epidemiology of Hypertension-Mortality Associations in Hemodialysis Patients - A Long-Term Population-Based Study
Uploaded by
nuvitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Reverse Epidemiology of Hypertension-Mortality Associations in Hemodialysis Patients - A Long-Term Population-Based Study
Uploaded by
nuvitaCopyright:
Available Formats
original contributions nature publishing group
Reverse Epidemiology of Hypertension-Mortality
Associations in Hemodialysis Patients: A Long-Term
Population-Based Study
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
Chih-Chiang Chien1,2, Chun-Sheng Yen1, Jhi-Joung Wang3, Hung-An Chen4, Ming-Ting Chou5,6, Chin-Chen
Chu3, Chung-Ching Chio7, Jyh-Chang Hwang1,6, Hsien-Yi Wang1,6, Yi-Hua Lu1 and Wei-Chih Kan1,8
Background without HTN (log-rank test: P <0.001). Multivariate analysis showed
Although hypertension (HTN) is a predictor of mortality, recent that patients with baseline HTN may have a higher survival rate (hazard
data have questioned the link between baseline HTN and mortality ratio (HR) 0.901, 95% confidence interval (CI): 0.819–0.992). After
in incident hemodialysis (HD) patients. We used Taiwan’s National stratification by age and DM, only elderly (≥65) patients without DM
Health Insurance claim data (NHRI-NHIRD-99182) to investigate had a significantly higher survival rate (HR 0.769, 95% CI: 0.637–0.927).
the association. HTN predicts lower mortality with increasing age in patients with
congestive heart failure (CHF) or coronary artery disease (CAD).
Methods
In 1999, this longitudinal cohort study enrolled 5752 new HD Conclusions
patients. Follow-up began from the initiation of HD until death, the There is a reverse (counterintuitive) association between baseline
end of HD, or the end of 2008. A Kaplan–Meier survival analysis was HTN and mortality in elderly HD patients without DM and a clear
done. Cox proportional hazard analysis was used to identify the risk tendency for a reverse association with increasing age in patients
factors for mortality. with CHF or CAD. Further study of the association between HTN and
mortality in older HD patients may be warranted.
Results
The prevalence of baseline HTN was 75.47%. Patients with HTN had Keywords: blood pressure; hemodialysis; hypertension; mortality;
a higher prevalence of diabetic mellitus (DM) and cardiovascular reverse epidemiology
diseases. The 1-, 5-, and 9-year cumulative survival rates were 95.5, 63.7
American Journal of Hypertension, advance online publication 31 May 2012.
and 41.8% in patients with HTN, and 95.5, 71.0, and 52.0% in those doi:10.1038/ajh.2012.60
Introduction cardiovascular mortality, several studies1,5,6 have questioned
Hypertension (HTN) is an important public health problem the link between HTN and mortality in HD patients. Some
and affects 24% of the general population.1 The prevalence of studies7–11 report a counterintuitive association between HTN
HTN in patients with chronic kidney disease (CKD) signifi- and mortality in HD patients: a normal-to-low blood pressure
cantly exceeds that seen in the general population; it is esti- (BP) is associated with increased all-cause and cardiovascular
mated to be more than 70% in patients with end-stage renal death, whereas a high BP confers survival advantages.7–10 The
disease (ESRD) and undergoing hemodialysis (HD).2,3 phenomenon is referred to as “reverse epidemiology”,12 which
Patients with CKD are in the highest risk group for cardio- has been proposed to address the observation of a counterin-
vascular events.4 Although HTN is an important predictor of tuitive association between an exposure and outcome. Foley et
al.6 found that elevated BP was associated with an increase in
1Department of Nephrology, Chi-Mei Medical Center, Tainan, Taiwan;
left ventricular mass index, heart failure, and coronary artery
2Department of Food Nutrition, Chung Hwa University of Medical Technology, disease (CAD), but that low BP was independently associated
Tainan, Taiwan; 3Department of Medical Research, Chi-Mei Medical Center, with increased mortality. However, there are still conflicting
Tainan, Taiwan; 4Department of Rheumatology, Chi-Mei Medical Center,
Tainan, Taiwan; 5Department of Cardiology, Chi-Mei Medical Center, Tainan,
effects on the impact of HTN. Tomita et al.11 reported that
Taiwan; 6Department of Sport Management, College of Leisure and Recreation the survival rate was higher in patients with a systolic BP <
Management, Chia Nan University of Pharmacy and Science, Tainan, Taiwan; 160 mm Hg than those with a systolic BP ≥ 160 mm Hg.
7Department of Neurological Surgery, Chi-Mei Medical Center, Tainan, Taiwan;
8Department of Medical Laboratory Science and Biotechnology, Chung Hwa
The primary goal of HD is to prolong patient survival.
University of Medical Technology, Tainan, Taiwan. Correspondence: Wei-Chih Age, diabetes mellitus (DM) and heart disease are important
Kan (rockiekan@ntu.edu.tw) factors.13 We hypothesized that baseline HTN has a differ-
Received 2 December 2012; first decision 11 February 2012; accepted 13 April 2012. ent impact on subsequent mortality in HD patients stratified
© 2012 American Journal of Hypertension, Ltd by age, DM, and heart disease. Publications on this subject
900 august 2012 | VOLUME 25 NUMBER 8 | 900-906 | AMERICAN JOURNAL OF HYPERTENSION
Hypertension-Mortality Associations in HD Patients original contributions
are still inconclusive,14 especially epidemiological data for than 60 days is not recorded as a “switch” in the database).16 A
national cohort studies of incident HD patients. To explore total of 5,752 HD patients were analyzed in this study.
this hypothesis, we used the Taiwan National Health Insurance
(NHI) database to investigate the association between baseline Ascertaining the demographic and comorbid variables
HTN and mortality in HD patients. We linked to the diagnostic codes through the inpatient and
outpatient claims databases of the NHI. Our research included
Methods not only survival status, but also date of death, patient demo-
Database graphics, and baseline comorbidities. Baseline comorbidi-
NHI program has provided compulsory universal health ties—such as HTN, DM, congestive heart failure (CHF), CAD,
insurance in Taiwan since 1995. With the exception of prison cerebrovascular accident, peripheral vascular disease, chronic
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
inmates, all citizens are enrolled in the program. All contracted lung disease, chronic liver disease, and cancer—were impor-
medical institutions must submit standard computerized claim tant factors affecting mortality and were assessed at the start of
documents for medical expenses. Patients with ESRD are dialysis. These characteristics are consistent with those in pre-
eligible for any type of renal replacement therapy free of any vious studies and demonstrate the need to adjust when com-
charge; all chronic dialysis patients are covered by NHI. paring mortality rates among dialysis patients. The ICD-9-CM
Data were obtained from the National Health Insurance codes used to define each condition are shown in Appendix 1.
Research Database15 and released for research by the Taiwan An individual was classified as an HTN patient if he or she had
National Health Research Institute. The National Health essential HTN, secondary HTN, hypertensive heart disease,
Insurance Research Database covers nearly all (99%) inpatient hypertensive renal disease, or hypertensive retinopathy. An
and outpatient medical benefit claims for Taiwan’s 23 million individual was classified as a DM patient if he or she had type 1
residents, is one of the largest and most comprehensive data- DM, type 2 DM, DM without mention of complication, or DM
bases in the world, and has been used extensively in various with mention of complications (ketoacidosis, hyperosmolarity,
studies.15 Patient identification numbers, gender, birthday, coma, nephropathy, neuropathy, peripheral circulatory disor-
dates of admission, and discharge, medical institutions provid- ders, hypoglycemia, retinopathy, and cataract). An individual
ing the services, the ICD-9-CM (International Classification of was classified as a CAD patient if he or she had acute myocar-
Diseases, 9th Revision, Clinical Modification) diagnostic and dial infarction, old myocardial infarction, angina pectoris or
procedure codes (up to five each), and outcomes are encrypted. another acute, subacute, or chronic form of ischemic heart dis-
The dataset was released with de-identified secondary data ease. An individual was classified as a CHF patient if he or she
for public research purposes. All types of personal identifi- had left heart failure, right heart failure, systolic heat failure,
cation on files connected with the present study were scram- diastolic heart failure, rheumatic heart failure, acute myocar-
bled using surrogate identification numbers to secure patient ditis, cardiomyopathy, hypertensive heart failure, or any other
privacy. The present study was exempted from ethical review. form of heart failure. An individual was classified as a periph-
The Bureau of National Health Insurance approves the appli- eral vascular disease patient if he or she had atherosclerosis,
cation (NHRI-NHIRD-99182) after reviewing all the required aortic aneurysm and dissection, other aneurysms, arterial
medical documents. We used the National Health Insurance embolism and thrombosis, phlebitis and thrombophlebitis,
Research Database for ambulatory care claims, all inpatient portal vein thrombosis, or other peripheral vascular disease.
claims, and the updated registry for beneficiaries from 1998 Comorbidities, which the patients had, were determined by
to 2008 for this study. All datasets can be interlinked through whether they fit one of the following two definitions: (i) diag-
each individual’s unique personal identification number. nostic codes from outpatient visits if the patient had an initial
diagnosis at any time in the 1 year before the start of dialysis
Patient selection and definition and then had one or more additional diagnoses within the
We designed a longitudinal cohort study and selected all adult subsequent 12 months. The first and last outpatient visit within
ESRD patients (≥18 years old) on maintenance dialysis who 1 year had to have been >30 days apart to avoid accidental
began renal replacement therapy between 1 January 1999, and inclusion of miscoded patients; (ii) diagnostic codes in hospi-
31 December 1999 (n = 6,170). ESRD patients on maintenance talization databases at least once in the 1 year before the start
dialysis were defined as having undergone dialysis for more of dialysis.
than 90 days. Patients who had undergone renal transplantation
before beginning dialysis were excluded (n = 36). Patients were Statistical analyses
followed-up from the first reported date of HD to the date of The data were analyzed using the Statistical Package for Social
death, a switch to peritoneal dialysis, renal transplantation, or 31 Sciences for Windows 17.0 (SPSS, Chicago, IL). Baseline char-
December 2008. Data on patients were censored if they switched acteristics of groups of patients with and without HTN were
to peritoneal dialysis, underwent renal transplantation, or 31 compared using Pearson χ2 tests. Age was entered as a categor-
December 2008. The primary outcome (event) was death from ical variable (18–44, 45–64, and 65 years or older). Significance
any cause. The predictor was HTN. The determination of modal- was set at P < 0.05. Overall patient survival was described using
ity switches after the initial modality choice followed the “60-day the Kaplan–Meier method based on dialysis modality. Hazard
rule” used by the USRDS (i.e., any change in modality lasting less ratios (HRs) and 95% confidence intervals (CIs) were derived
AMERICAN JOURNAL OF HYPERTENSION | VOLUME 25 NUMBER 8 | august 2012 901
original contributions Hypertension-Mortality Associations in HD Patients
from Cox proportional hazards models. Cox models met the female patients. With increasing age, the proportion of HTN
assumption of proportionality of risks. To adjust for potential increased. Patients with baseline HTN tended to have more
confounding in the association between comorbidities and the comorbidities than those without baseline HTN (Table 1).
risk of mortality, multivariate analyses were used to model all-
cause mortality. To test the hypothesis that being in different Cumulative survival rate
age groups and having DM have a different effect on mortality During the follow-up period, 2,775 patients died (Figure 1).
in HD patients with and without HTN, we further stratified The mean follow-up time alive on dialysis was 87.13 months
these HD patients by age-group and DM. (95% CI: 84.94–89.32) in patients without HTN and 80.45
months (95% CI: 79.18–81.72) for patients with HTN.
Results The cumulative survival rate for patients without HTN
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
Demographics and clinical characteristics was 95.5% at 1 year, 71.0% at 5 years, and 52.0% at 9 years,
Of 5,752 HD patients, 4,341 patients (75.47%) had baseline and for patients with HTN was 95.5% at 1 year, 63.7% at 5
HTN. There were no significant differences between male and years, and 41.8% at 9 years. The log-rank test showed a sig-
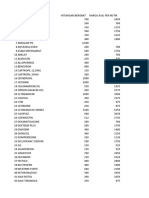
Table 1 | Patient characteristics and association with and without hypertension on hemodialysis
HD without HTN HD with HTN P value
n (%) n (%)
Gender 0.958
Female 751 (53.2) 2307 (53.1)
Male 660 (46.8) 2034 (46.9)
Age at start of HD <0.001
18-44 years old 328 (23.20) 566 (13.00)
45-64 years old 578 (41.00) 1991 (45.90)
≥ 65 years old 505 (35.80) 1784 (41.10)
Baseline comorbidity
Diabetes mellitus <0.001
No 999 (70.8) 1666 (38.4)
Yes 412 (29.20) 2675 (61.60)
Congestive heart failure <0.001
No 1286 (91.10) 3445 (79.40)
Yes 125 (8.90) 896 (20.60)
Coronary artery disease <0.001
No 1275 (90.40) 3172 (73.10)
Yes 136 (9.60) 1169 (26.90)
Cerebrovascular disease <0.001
No 1349 (95.60) 3728 (85.90)
Yes 62 (4.40) 613 (14.10)
Peripheral vascular disease <0.001
No 1373 (97.3) 4141 (95.4)
Yes 38 (2.7) 200 (4.6)
Chronic lung disease <0.001
No 1335 (94.60) 3931 (90.60)
Yes 76 (5.40) 410 (9.40)
Chronic Liver Disease 0.208
No 1278 (90.60) 3980 (91.70)
Yes 133 (9.40) 361 (8.30)
Cancer <0.001
No 1320 (93.60) 4211 (97.0)
Yes 91 (6.40) 130 (3.0)
HD, hemodialysis; HTN, hypertension.
902 august 2012 | VOLUME 25 NUMBER 8 | AMERICAN JOURNAL OF HYPERTENSION
Hypertension-Mortality Associations in HD Patients original contributions
nificant difference in survival rates between the two groups in patients 18–44 years old, 0.934 in those 45–64 years old,
(log-rank: P < 0.001). Although crude survival was better in and 0.697 in those ≥65 years old. There was a clear tendency
patients without HTN, there was a reverse outcome in long- toward HTN’s predicting lower mortality with increasing age
term mortality between the two groups after adjusting for in patients with CHF.
age, gender, and comorbidities (HR: 0.901, 95% CI: 0.819–
0.992) (Table 2). Risk factors for all-cause mortality in HD patients stratified by
CAD and different age groups
Risk factors for all-cause mortality in HD patients We further stratified patients by CAD and different age groups
A multivariate Cox proportional hazards analysis of baseline (Table 5). After a multivariate analysis, baseline HTN was an
data showed that male gender, being ≥45 years old, DM, CHF, independent predictor for lower mortality only in nonCAD
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
CAD, cerebrovascular accident, peripheral vascular disease, HD patients ≥65 years old (HR: 0.840, 95% CI: 0.721–0.97).
chronic lung disease, chronic liver disease, and cancer were The HR decreased with increasing age in patients with CAD;
associated with a significantly higher mortality rate (Table 2). the HR was 1.134 in patients 18–44 years old, 1.029 in those
However, the mortality rate for patients with baseline HTN 45–64 years old, and 0.74 in those ≥65 years old. There was a
was lower than for those without HTN. clear tendency toward HTN’s predicting lower mortality with
increasing age in patients with CAD.
Risk factors for all-cause mortality in HD patients stratified by
DM and different age groups Discussion
We further stratified patients by DM and different age groups This study used the Taiwan NHI database to investigate the
(Table 3). After multivariate analysis, baseline HTN was an association between baseline HTN and subsequent long-term
independent predictor for lower mortality only in nonDM mortality in chronic HD patients. The population studied was
HD patients ≥ 65 years old (HR: 0.769, 95% CI: 0.637–0.927). nationwide and representative. There was a high prevalence of
Mortality was higher for male than female patients only in baseline HTN (75.47%) in incident HD patients in our registry.
the nonDM group. A history of CHF was a significant predic- Patients with a history of HTN also had a higher rate of DM
tor of mortality in the DM group and the elderly (≥65 years
old).
Table 2 | Adjusted hazard ratio a for all-cause mortality in
Risk factors for all-cause mortality in HD patients stratified by hemodialysis patients
CHF and different age groups Covariate Univariate analysis Multivariate analysis
We further stratified patients by CHF and different age groups HR (95% CI) HR (95% CI)
(Table 4). After a multivariate analysis, baseline HTN was an Sex (male vs. female) 1.228 (1.140–1.323)* 1.175 (1.090-1.266)*
independent predictor for lower mortality in elderly patients Age at initiation of
both with (HR: 0.849, 95% CI: 0.733–0.983) and without hemodialysis
(HR: 0.697, 95% CI: 0.489–0.995) CHF. The HR decreased 18–44 years old Referent Referent
with increasing age in patients with CHF; the HR was 5.492 45–64 years old 2.659 (2.300–3.075)* 2.142 (1.849–2.482)*
≥ 65 years old 5.637 (4.878–6.515)* 4.384 (3.780–5.084)*
1.0
Log-rank P < 0.001 Diabetes mellitus (yes vs. no) 2.197 (2.033–2.375)* 1.776 (1.636–1.928)*
Hypertension (yes vs. no) 1.312 (1.199–1.436)* 0.901 (0.819–0.992)*
0.8
Congestive heart failure 1.988 (1.817–2.175)* 1.514 (1.374–1.668)*
Cumulative survival rate
Without HTN (yes vs. no)
0.6
With HTN Coronary artery disease 1.860 (1.711–2.022)* 1.139 (1.040–1.248)*
(yes vs. no)
0.4 Cerebrovascular disease 1.862 (1.674–2.071)* 1.354 (1.216–1.509)*
(yes vs. no)
0.2 Peripheral vascular disease 2.141 (1.567–2.926)* 1.648 (1.203–2.256)*
(yes vs. no)
0.0 Chronic lung disease 1.805 (1.599–2.037)* 1.278 (1.130–1.446)*
(yes vs. no)
0 12 24 36 48 60 72 84 96 108 120
Chronic liver disease 1.467 (1.293–1.663)* 1.334 (1.176–1.513)*
Number at risk Survival time (months) (yes vs. no)
With HTN patients 4341 3960 3443 2908 2561 2209 1933 1733 1552 1371
Cancer (yes vs. no) 1.521 (1.268–1.825)* 1.273 (1.059–1.532)*
Without HTN patients 1411 1288 1133 996 906 827 758 684 636 588
CI, confidence interval; HR, hazard ratio.
aThe analyses were adjusted for age, gender, diabetic mellitus, hypertension, congestive
Figure 1 | Crude overall Kaplan–Meier survival curves for incident end-stage heart failure, coronary artery disease, cerebrovascular disease, peripheral vascular disease,
renal disease hemodialysis patients stratified by the presence and absence of chronic lung disease and cancer. *P < 0.05.
hypertension (HTN) at the start of dialysis.
AMERICAN JOURNAL OF HYPERTENSION | VOLUME 25 NUMBER 8 | august 2012 903
original contributions Hypertension-Mortality Associations in HD Patients
Table 3 | Numbers and adjusted hazard ratioa for all-cause mortality in hemodialysis patients stratified by diabetes mellitus and
age-group
Covariate Age 18–44 Age 45–64 Age ≥65
NonDM DM NonDM DM NonDM DM
(n = 640) (n = 254) (n = 1039) (n = 1530) (n = 986) (n = 1303)
Sex (male vs. 1.777 (1.218–2.592)* 1.122 (0.734–1.713) 1.725 (1.385–2.149)* 1.094 (0.954–1.254) 1.182 (1.000–1.398)* 0.994 (0.865–1.142)
female)
Hypertension 0.692 (0.478–1.002) 1.293 (0.714–2.343) 0.964 (0.769–1.208) 0.958 (0.779–1.179) 0.769 (0.637–0.927)* 0.879 (0.718–1.078)
(yes vs. no)
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
Congestive heart 1.431 (0.656–3.121) 1.799(1.070–3.025)* 1.352 (0.946–1.932) 1.427 (1.204–1.691)* 1.416 (1.132–1.771)* 1.633 (1.382–1.929)*
failure (yes vs. no)
Coronary artery 0.811 (0.254–2.585) 1.220 (0.714–2.085) 1.213 (0.881–1.671) 1.305 (1.107–1.538)* 1.241 (1.011–1.523)* 0.966 (0.831–1.123)
disease (yes vs. no)
Cerebrovascular 0.580 (0.134–2.512) 1.845 (0.983–3.461) 1.476 (0.980–2.221) 1.468 (1.224–1.761)* 1.196 (0.907–1.578) 1.271 (1.066–1.514)*
disease (yes vs. no)
Peripheral vascular 25.655 (2.951–223.04)*10.209 (1.356–76.862)*2.360 (0.323–17.242) 1.226 (0.785–1.916) 2.300 (0.951–5.670) 2.127 (1.193–3.793)*
disease (yes vs. no)
Chronic lung 0.755 (0.098–5.831) 1.212 (0.487–3.020) 1.631 (1.093–2.436)* 0.895 (0.693–1.155) 1.361 (1.069–1.735)* 1.434 (1.171–1.757)*
disease (yes vs. no)
Chronic liver 2.530 (1.394–4.592)* 0.912 (0.429–1.937) 1.887 (1.349–2.639)* 1.302(1.043–1.626)* 1.286 (0.941–1.757) 1.118 (0.880–1.420)
disease (yes vs. no)
Cancer (yes vs. no) 4.371 (1.583–12.072) 2.570 (0620–10.657) 3.300 (2.141–5.088)* 1.093 (0.743–1.608) 0.976 (0.681–1.400) 1.060 (0.739–1.521)
DM, diabetic mellitus; n, the number of patients in each subgroup.
aThe analyses were adjusted for gender, hypertension, congestive heart failure, coronary artery disease, cerebrovascular disease, peripheral vascular disease, chronic lung disease
and cancer. All data are hazard ratio (95% confidence interval).
*P < 0.05.
Table 4 | Numbers and adjusted hazard ratioa for all-cause mortality in hemodialysis patients stratified by congestive heart failure
and age-group
Covariate Age 18–44 Age 45–64 Age ≥65
NonCHF CHF NonCHF CHF NonCHF CHF
(n = 823) (n = 71) (n = 2133) (n = 436) (n = 1775) (n = 514)
Sex (male vs. female) 1.613 (1.202–2.165)* 0.989 (0.407–2.403) 1.276 (1.120–1.454)* 1.149 (0.894–1.476) 1.076 (0.952–1.216) 1.037 (0.829–1.298)
Hypertension 0.733 (0.539–1.013) 5.492 (0.709–42.537) 0.964 (0.818–1.137) 0.934 (0.618–1.410) 0.849 (0.733–0.983)* 0.697 (0.489–0.995)*
(yes vs. no)
Diabetic mellitus 2.420 (1.782–3.288)* 2.786 (1.000–7.766) 2.204 (1.906–2.548)* 2.236 (1.546–3.232)* 1.392 (1.225–1.581)* 1.531 (1.203–1.948)*
(yes vs. no)
Coronary artery 0.819 (0.438–1.528) 2.286 (0.974–5.369) 1.344 (1.128–1.601)* 1.251 (0.968–1.618) 0.973 (0.839–1.127) 1.244 (0.991–1.561)
disease (yes vs. no)
Cerebrovascular 1.522 (0.819–2.830) 0.599 (0.163–2.198) 1.411 (1.161–1.714)* 1.600 (1.158–2.212)* 1.329 (1.118–1.579)* 1.092 (0.818–1.457)
disease (yes vs. no)
Peripheral vascular 21.855 (5.186– – 1.121 (0.659–1.906) 1.630 (0.758–3.509) 2.306 (1.350–3.939)* 2.226 (0.698–7.104)
disease (yes vs. no) 92.105)*
Chronic lung disease 1.385 (0.563–3.410) 0.848 (0.097–7.409) 1.317 (1.020–1.700)* 0.688 (0.465–1.018) 1.481 (1.221–1.798)* 1.344 (1.034–1.747)*
(yes vs. no)
Chronic liver disease 1.869 (1.151–3.033)* 0.636 (0.126–3.215) 1.534 (1.247–1.888)* 1.162 (0.770–1.752) 1.161 (0.936–1.440) 1.175 (0.777–1.776)
(yes vs. no)
Cancer (yes vs. no) 3.636 (1.589–8.319)* – 1.663 (1.225–2.258)* 1.210 (0.531–2.757) 0.934 (0.696–1.252) 1.274 (0.761–2.132)
CHF, congestive heart failure; n, the number of patients in each subgroup.
aThe analyses were adjusted for gender, hypertension, congestive heart failure, coronary artery disease, cerebrovascular disease, peripheral vascular disease, chronic lung disease
and cancer. All data are hazard ratio (95% confidence interval).
*P < 0.05.
904 august 2012 | VOLUME 25 NUMBER 8 | AMERICAN JOURNAL OF HYPERTENSION
Hypertension-Mortality Associations in HD Patients original contributions
Table 5 | Numbers and adjusted hazard ratioa for all-cause mortality in hemodialysis patients stratified by coronary artery disease
and age-group
Covariate Age 18–44 Age 45–64 Age≥65
NonCAD CAD NonCAD CAD NonCAD CAD
(n = 830) (n = 64) (n = 2046) (n = 523) (n = 1571) (n = 718)
Sex (male vs. 1.513 (1.132–2.023)* 1.617 (0.480–5.443) 1.284 (1.123–1.469)* 1.176 (0.934–1.480) 1.094 (0.961–1.246) 1.003 (0.829–1.213)
female)
Hypertension 0.787 (0.578–1.071) 1.134 (0.220–5.580) 0.944 (0.801–1.113) 1.029 (0.679–1.561) 0.840 (0.721–0.978)* 0.749 (0.551–1.019)
(yes vs. no)
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
Diabetic mellitus 2.323 (1.715–3.145)* 4.074 (1.058–15.679)* 2.208 (1.903–2.562)* 2.227 (1.611–3.079)* 1.508 (1.318–1.726)* 1.226 (1.003–1.498)*
(yes vs. no)
Congestive heart 1.219 (0.722–2.059) 4.106 (1.630–10.343)* 1.470 (1.205–1.794)* 1.365 (1.078–1.727)* 1.364 (1.128–1.651)* 0.966 (0.831–1.123)*
failure (yes vs. no)
Cerebrovascular 1.651 (0.874–3.120) 0.649 (0.207–2.032) 1.503 (1.226–1.843)* 1.375 (1.031–1.833)* 1.187 (0.979–1.440) 1.387 (1.097–1.752)*
disease (yes vs. no)
Peripheral vascular 22.091 (5.268–92.641)* – 1.030 (0.580–1.828) 1.677 (0.859–3.273) 2.785 (1.316–5.897)* 1.966 (1.041–3.712)*
disease (yes vs. no)
Chronic lung 1.330 (0.576–3.072) – 1.309 (1.005–1.703)* 0.724 (0.501–1.046) 1.548 (1.270–1.887)* 1.216 (0.947–1.562)
disease (yes vs. no)
Chronic liver 1.571 (0.967–2.551) 3.490 (0.544–22.406) 1.729 (1.399–2.137)* 0.950 (0.654–1.380) 1.237 (0.986–1.552) 1.000 (0.708–1.413)
disease (yes vs. no)
Cancer (yes vs. no) 3.515 (1.583–8.033)* – 1.512 (1.094–2.090)* 1.889 (1.027–3.474)* 0.986 (0.732–1.329) 1.060 (0.643–1.747)
CAD, coronary artery disease; n, the number of patients in each subgroup.
aThe analyses were adjusted for gender, hypertension, congestive heart failure, coronary artery disease, cerebrovascular disease, peripheral vascular disease, chronic lung disease
and cancer. All data are hazard ratio (95% confidence interval).
*P < 0.05.
and cardiovascular diseases, including CHF, CAD, cerebrov- during follow-up. Patients who died in the initial stage (within
ascular accident, and peripheral vascular disease. We found a 90 days after initiation of HD) were excluded from our study; the
tendency of reverse epidemiology between baseline HTN and HR was 0.769 (95% CI: 0.637–0.927) (Table 3). We performed
subsequent lower mortality; however, it was significant in HD an additional analysis of mortality excluding death within 1 year
patients ≥65 years old without DM. There was a clear tendency after the initiation of HD. A multivariate analysis showed that
for a reverse association with increasing age in patients with baseline HTN was also an independent predictor for lower mor-
CHF or CAD. tality only in nonDM HD patients ≥65 years old (HR: 0.784, 95%
We, like Kimura et al.,17 found that baseline normal BP was CI: 0.642–0.956). The HR increased from 0.769 to 0.784, which
associated with poor outcomes in nonDM HD patients ≥65 indicated that serious health conditions may be partially respon-
years old. Kimura et al. also reported that HTN had no signifi- sible for mortality in elderly patients; other reasons for mortality
cant effect on elderly patients. Elderly dialysis patients have a are yet to be determined. Thus, the reason for an inverse associa-
much higher mortality rate.13 In the presence of strong factors tion between baseline HTN and mortality may be that a higher
other than BP that affect mortality, the effect of HTN might nei- BP “protective” in the elderly; in contrast, normal-to-low BP may
ther be discovered nor be as important. We also found there was reflect the fact that organ failure or other events leading to hypo-
a clear tendency for a reverse association with increasing age tension had occurred before death.
in patients with CHF or CAD. It is also possible that a higher Some reports7 refer to the tendency of an inverse associa-
BP could be “protective” in the elderly, especially with CHF or tion between baseline HTN and subsequent mortality in dial-
CAD, by improving cardiac perfusion or overcoming the resist- ysis patients as “reverse epidemiology”, a term first used in
ance of stiff arteries.9 In addition, the normal-to-low BP may 1999 by Josef Coresh (cited in Levin et al. 2007)12. However,
be a marker of the already poor survival rate of elderly dialysis the term appears to have generated confusion and inaccurate
patients,18,19 especially with CHF or CAD. Older patients with usages over the past decade. Levin et al.12 clarified that the
no HTN might have latent heart failure and thus be more likely epidemiology is not reversed. Most ESRD dialysis patients
to die.17 The association of normal-to-low BP with mortality have subclinical manifestations of the disease process and
was a marker for having had cardiac failure before death.6,19 A often they and their physicians are unaware, until very late in
recent study20 also showed that the association between low BP the course of the disease, of how their disease and treatment
and death was especially evident in the short term. To evaluate are affecting them. There appears to be a counterintuitive
the hypothesis that elderly dialysis patients without DM, but with association between baseline BP and subsequent mortality
one or more other serious conditions, have a poor survival rate, partly because of unmeasured baseline disease manifesta-
we analyzed mortality, but excluded death in the initial stage, tions of risk factors and partly because of the methods used
AMERICAN JOURNAL OF HYPERTENSION | VOLUME 25 NUMBER 8 | august 2012 905
original contributions Hypertension-Mortality Associations in HD Patients
Disclosure: The authors declared no conflicts of interest.
to analyze disease progression and treatment efficacy7; there
may be other reasons. Acknowledgment: The study was supported by grant CMFHR10078 from
There are several limitations to this study. First, although we Chi-Mei Medical Center and grant NHRI-NHIRD-99182 from the National
Health Research Institutes in Taiwan. We are grateful to the staff in Professor
stratified our patients by age and DM status, like other stud-
Jhi-Joung Wang’s Department of Medical Research, especially Chin-Li Lu and
ies that have used administrative data, we did not control for Shih-Feng Weng, who helped with statistical analyses.
some unmeasured confounding variables: antihypertensive
treatment, BP levels in hypertensive patients, etc. Whether this 1. Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ,
Labarthe D. Prevalence of hypertension in the US adult population. Results
is based on latent confounding or whether there is a biologi- from the Third National Health and Nutrition Examination Survey, 1988-1991.
cal basis remains to be determined. Second, the comorbidi- Hypertension 1995; 25:305–313.
ties relied on the claim data and ICD-9-CM diagnosis codes, 2. VanDeVoorde RG, Mitsnefes MM. Hypertension and CKD. Adv Chronic Kidney Dis
Downloaded from https://academic.oup.com/ajh/article/25/8/900/2282145 by Joongbu University user on 13 August 2020
2011; 18:355–361.
but it is possible that some of the diseases were misclassified. 3. United States Renal Data System <http://www.usrds.org>. Accessed 25 October
Third, we were unable to take into account the severity of the 2011.
diseases, which reduced our chances of showing the severity- 4. Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL,
White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD,
related effects of comorbidities. Fourth, our study lacked spe- Califf RM, Pfeffer MA. Relation between renal dysfunction and cardiovascular
cific data on dialysis adequacy, patient compliance, nutritional outcomes after myocardial infarction. N Engl J Med 2004; 351:1285–1295.
status, biochemical data, and socioeconomic characteristics. 5. Fernández JM, Carbonell ME, Mazzuchi N, Petruccelli D. Simultaneous analysis of
morbidity and mortality factors in chronic hemodialysis patients. Kidney Int 1992;
Finally, it would be better to describe the causes of death and 41:1029–1034.
analyze the mortalities of cardiovascular and noncardiovascu- 6. Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barre PE. Impact of
lar diseases; however, the Taiwan Bureau of National Health hypertension on cardiomyopathy, morbidity and mortality in end-stage renal
disease. Kidney Int 1996; 49:1379–1385.
Insurance does not afford the cross-link information between 7. Agarwal R. Hypertension and survival in chronic hemodialysis patients–past
this and the database with “causes of death”. lessons and future opportunities. Kidney Int 2005; 67:1–13.
In conclusion, maintenance of HD patients have a high 8. Zager PG, Nikolic J, Brown RH, Campbell MA, Hunt WC, Peterson D, Van Stone J,
Levey A, Meyer KB, Klag MJ, Johnson HK, Clark E, Sadler JH, Teredesai P. “U” curve
prevalence of HTN. Using the Taiwan NHI claim data, we association of blood pressure and mortality in hemodialysis patients. Medical
found a counterintuitive reverse association between base- Directors of Dialysis Clinic, Inc. Kidney Int 1998; 54:561–569.
line HTN and mortality in nonDM chronic HD patients 9. Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD. Reverse
epidemiology of hypertension and cardiovascular death in the hemodialysis
≥65 years old. There was a clear tendency for a reverse asso- population: the 58th annual fall conference and scientific sessions. Hypertension
ciation with increasing age in patients with CHF or CAD. 2005; 45:811–817.
Additional studies of this counterintuitive reverse associa- 10. Li Z, Lacson E Jr, Lowrie EG, Ofsthun NJ, Kuhlmann MK, Lazarus JM, Levin NW. The
epidemiology of systolic blood pressure and death risk in hemodialysis patients.
tion between HTN and mortality in elderly HD patients may Am J Kidney Dis 2006; 48:606–615.
be warranted. 11. Tomita J, Kimura G, Inoue T, Inenaga T, Sanai T, Kawano Y, Nakamura S, Baba S,
Matsuoka H, Omae T. Role of systolic blood pressure in determining prognosis of
hemodialyzed patients. Am J Kidney Dis 1995; 25:405–412.
Appendix 1 | ICD-9-CM codes used to identify clinical 12. Levin NW, Handelman GJ, Coresh J, Port FK, Kaysen GA. Reverse epidemiology: a
confusing, confounding, and inaccurate term. Semin Dial 2007; 20:586–592.
conditions 13. Vonesh EF, Snyder JJ, Foley RN, Collins AJ. The differential impact of risk factors on
Conditions ICD-9-CM code mortality in hemodialysis and peritoneal dialysis. Kidney Int 2004; 66:2389–2401.
14. Lacson E Jr, Lazarus JM. The association between blood pressure and mortality
Diabetes mellitus 250.a, 357.2, 362.0a, 366.41 in ESRD-not different from the general population? Semin Dial 2007; 20:510–517.
Hypertension 362.11, 401.a–405.a, 437.2 15. Bureau of National Health Insurance <www.doh.gov.tw/statistic/index.htm>
[In Chinese]; <http://www.doh.gov.tw/EN2006/index_EN.aspx> [In English].
Congestive heart failure 428, 398.91, 422, 425, 402.a1, 404.a1, 404.a3 Accessed 25 September 2011.
Coronary artery disease 410.a–414.a 16. United States Renal Data System. Treatment history (chapter V). In: Researcher’s
Guide to the USRDS Database 1999. <http://www.usrds.org>. Accessed 25
Cerebrovascular accident/TIA 430–438 October 2011.
Peripheral vascular disease 440–444, 447, 451–453, 557 17. Kimura G, Tomita J, Nakamura S, Uzu T, Inenaga T. Interaction between
hypertension and other cardiovascular risk factors in survival of hemodialyzed
Chronic lung disease 490–496a, 500-505a, 506.4a patients. Am J Hypertens 1996; 9:1006–1012.
Chronic liver disease 570, 571, 572.1, 572.4, 573.1–573.3 18. Loyke HF. Disease states in which blood pressure is lowered. South Med J 1989;
82:864–867.
Cancer 140–208; 230–231; 233–234 19. Covic A, Goldsmith DJ. Ambulatory blood pressure measurement in the renal
ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; patient. Curr Hypertens Rep 2002; 4:369–376.
TIA, Transient ischemic attack. 20. Bos WJ, van Manen JG, Noordzij M, Boeschoten EW, Krediet RT, Dekker FW. Is the
aCan be any number or missing. inverse relation between blood pressure and mortality normalized in ‘low-risk’
dialysis patients? J Hypertens 2010; 28:439–445.
906 august 2012 | VOLUME 25 NUMBER 8 | AMERICAN JOURNAL OF HYPERTENSION
You might also like
- 4170-Article Text-31215-2-10-20200702Document8 pages4170-Article Text-31215-2-10-20200702nuvitaNo ratings yet
- JEM Guideline For Writers 2023Document4 pagesJEM Guideline For Writers 2023nuvitaNo ratings yet
- Outcome Research, Nutrition, and Reverse Epidemiology in Maintenance Dialysis PatientsDocument9 pagesOutcome Research, Nutrition, and Reverse Epidemiology in Maintenance Dialysis PatientsnuvitaNo ratings yet
- Study Comparatif Kualitas Hidup Antara Pasien Hemodialisis Dengan Pasien Continuous Ambulatory Peritoneal DialysisDocument6 pagesStudy Comparatif Kualitas Hidup Antara Pasien Hemodialisis Dengan Pasien Continuous Ambulatory Peritoneal DialysisnuvitaNo ratings yet
- Prevalence of Chronic Kidney Disease in Patients With or at A High Risk of Cardiovascular DiseaseDocument4 pagesPrevalence of Chronic Kidney Disease in Patients With or at A High Risk of Cardiovascular DiseasenuvitaNo ratings yet
- Evaluation of Protein-Energy Wasting and Inflammation On Patients Undergoing Continuous Ambulatory Peritoneal Dialysis and Its CorrelationsDocument8 pagesEvaluation of Protein-Energy Wasting and Inflammation On Patients Undergoing Continuous Ambulatory Peritoneal Dialysis and Its CorrelationsnuvitaNo ratings yet
- Clinical Practice Guideline Undernutrition in Chronic Kidney DiseaseDocument27 pagesClinical Practice Guideline Undernutrition in Chronic Kidney DiseasenuvitaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bacteriophage Therapy SummitDocument12 pagesBacteriophage Therapy SummitZhibek AbyshevaNo ratings yet
- The Importance of Proteinuria in Preeclampsia and Its Predictive Role in Maternal and Neonatal OutcomesDocument9 pagesThe Importance of Proteinuria in Preeclampsia and Its Predictive Role in Maternal and Neonatal OutcomesimuhammadfahmiNo ratings yet
- Multi Organ Dysfunction SyndromeDocument40 pagesMulti Organ Dysfunction SyndromeDr. Jayesh PatidarNo ratings yet
- Errors 2Document5 pagesErrors 2Anggun rahmi PutriNo ratings yet
- List of Philhealth Accredited Level 3 Hospital As of October 31, 2019Document35 pagesList of Philhealth Accredited Level 3 Hospital As of October 31, 2019Lex CatNo ratings yet
- BronchiectasisDocument30 pagesBronchiectasisMark Gizle PapagayoNo ratings yet
- Laporan Kasus Neurogenic ShockDocument44 pagesLaporan Kasus Neurogenic ShockAkbar TaufikNo ratings yet
- Acute PancreatitisDocument11 pagesAcute PancreatitisJunaid Masoodi100% (4)
- Working With Addicted PopulationsDocument9 pagesWorking With Addicted PopulationsWhimsical BrunetteNo ratings yet
- Case Presentation On Parkinson'S Disease: Presented By: T.Avinash Vith Pharm D Y13PHD0721Document21 pagesCase Presentation On Parkinson'S Disease: Presented By: T.Avinash Vith Pharm D Y13PHD0721AVINASH TALAPALA100% (1)
- PHARMACOLOGYDocument44 pagesPHARMACOLOGYshruti sangwan100% (1)
- Parameter For Mindray Reagent On BS-400 (V12.0)Document3 pagesParameter For Mindray Reagent On BS-400 (V12.0)НиколайКрылов100% (1)
- Carboplatin MonographDocument9 pagesCarboplatin Monographmerkuri100% (1)
- Common Dermatology Multiple Choice Questions and Answers - 6Document3 pagesCommon Dermatology Multiple Choice Questions and Answers - 6Atul Kumar Mishra100% (1)
- m3 Act3 Emotional DisabilitiesDocument7 pagesm3 Act3 Emotional Disabilitiesapi-516574894No ratings yet
- Diagnosis Treatment of Back Pain MedicationsDocument41 pagesDiagnosis Treatment of Back Pain Medicationsrabin1994No ratings yet
- Topic 5. MEDICAL TECHNOLOGY EDUCATIONDocument7 pagesTopic 5. MEDICAL TECHNOLOGY EDUCATIONSophia GarciaNo ratings yet
- Fetal Colonic GradeDocument7 pagesFetal Colonic Gradedgina8800No ratings yet
- The Use of Pycnogenol in The Treatment of Melasma: Original ArticlesDocument5 pagesThe Use of Pycnogenol in The Treatment of Melasma: Original ArticlesfreitasjonashenriqueNo ratings yet
- NCLEX Fluids & ElectrolytesDocument6 pagesNCLEX Fluids & ElectrolytesNathalee Walker100% (1)
- Keith Edwards Score For Diagnosis of Tuberculosis. IJP.03Document3 pagesKeith Edwards Score For Diagnosis of Tuberculosis. IJP.03Diego Bedon AscurraNo ratings yet
- Some Oncology Tips & Tricks by DR Khaled MagdyDocument8 pagesSome Oncology Tips & Tricks by DR Khaled MagdyA.h.Murad100% (1)
- EpsiotomyDocument2 pagesEpsiotomyJazzlyneNo ratings yet
- 4D CT With Respiratory GatingDocument2 pages4D CT With Respiratory GatingLaura Karina Sanchez ColinNo ratings yet
- Daftar Harga Obat ApotekDocument7 pagesDaftar Harga Obat ApoteksalmaegaNo ratings yet
- 30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFDocument10 pages30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFRicovially DavyaNo ratings yet
- Osteoporosis PhilippinesDocument3 pagesOsteoporosis PhilippinesMia DangaNo ratings yet
- Myasthenia GravisDocument11 pagesMyasthenia GravisParvathy RNo ratings yet
- A Modified Supine Position Facilitates Bladder Function in Patient Undergoing Percutaneous Coronary InterventionDocument8 pagesA Modified Supine Position Facilitates Bladder Function in Patient Undergoing Percutaneous Coronary InterventionVelicia MargarethaNo ratings yet
- Nguyen 2021Document8 pagesNguyen 2021Yaseen MohamnadNo ratings yet