Professional Documents
Culture Documents
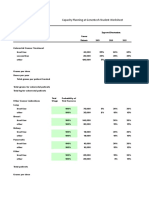
02 Covid 19 Flowchart 2 Management of Mild V6.0
Uploaded by
umarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
02 Covid 19 Flowchart 2 Management of Mild V6.0
Uploaded by
umarCopyright:
Available Formats
MANAGEMENT OF
ADULTS WITH
MILD COVID-19
VERSION 6.0
PUBLISHED
9 JULY 2020
MANAGING RISK OF INFECTION
Definition of disease severity
Follow national advice for use of PPE in non-inpatient heathcare settings Mild illness
during the COVID-19 outbreak. PP [Taskforce/AHPPC] Adults not presenting any clinical features suggestive of moderate or
severe disease or a complicated course of illness.
Characteristics:
• no symptoms
MANAGEMENT IN THE COMMUNITY
• or mild upper respiratory tract symptoms
• or cough, new myalgia or asthenia without new shortness of breath
• Patients with mild COVID-19 can be managed in the community or a reduction in oxygen saturation
with advice on self management of symptoms and self isolation.
PP [BMJ]
• Any person clinically assessed as being a likely case of COVID-19
should be managed as if they are a confirmed case until they receive
a negative test for SARS-CoV-2. PP [Taskforce] Rural and remote access to care
General
• Ensure that patients living alone have identified someone to check on This flowchart should be applied after considering features of the
them regularly, even if they are currently well. PP [BMJ] individual patient, their preferences and the context in terms of rurality/
• Assess whether or not the patient and carer(s) have the ability to remoteness, public health responses and proximity to higher level care.
manage infection control to a high standard. PP [Taskforce] Application of the flowchart will vary with local current COVID-19
prevalence and availability of testing. Early transfer to a major centre
should be considered for those at risk of deterioration.
BASELINE ASSESSMENT
Check for signs of moderate/severe disease (refer to Assessment for
suspected COVID-19 Clinical Flow Chart)
Check status of oro/nasopharyngeal swab results.
No baseline investigations are required for mild COVID-19.
Perform CXR and/or blood tests if clinically indicated.
Chest CT scan is not indicated for COVID-19, but should be performed
if clinically indicated for other reasons.
PP [Taskforce]
COVID-19 THERAPIES THERAPIES FOR PRE-EXISTING CONDITIONS
SUPPORTIVE CARE GENERAL
Manage mild COVID-19 in a similar way to seasonal flu and advise Ensure that people with suspected COVID-19 continue to receive their
patients to rest and drink fluids. PP [BMJ] usual care for pre-existing conditions. PP [Taskforce]
An antipyretic is generally not required, but paracetamol can be People advised to take NSAIDs routinely may continue with treatment.
considered for symptomatic relief. PP [ACSQHC] PP [ACSQHC]
00.10 In people with suspected or confirmed COVID-19, consider
DISEASE-MODIFYING TREATMENTS alternative routes of administration for intranasal medicines, recognising
that in some situations administration via the intranasal route may
be a safer option for affected individuals and healthcare workers. PP
44.81 Do not initiate dexamethasone or other corticosteroids for the [Taskforce/ACSQHC]
treatment of mild COVID-19. PP [Taskforce]
Baloxavir marboxil ASTHMA AND COPD
For people with COVID-19, only administer baloxavir marboxil in the
context of randomised trials with appropriate ethical approval.
EBR [Taskforce] Use inhaled or oral steroids for the management of people with
co-existing asthma or COPD and COVID-19 as you normally would for
viral exacerbation of asthma or COPD. Do not use a nebuliser.
Favipiravir CBR [Taskforce]
For people with COVID-19, only administer favipiravir in the context of
randomised trials with appropriate ethical approval.
EBR [Taskforce]
DIABETES AND CARDIOVASCULAR DISEASE
Lopinavir/ritonavir
For people with COVID-19, only administer lopinavir/ritonavir in the In patients with COVID-19 who are receiving ACE-I/ARB,
context of randomised trials with appropriate ethical approval. these medications should be continued, unless contraindicated
EBR [Taskforce] (e.g. hypotension). CBR [Taskforce]
Remdesivir Do not cease or change the dose of other treatments such as insulin,
For people with mild COVID-19, only administer remdesivir in the other diabetes medications, or statins. PP [Taskforce]
context of randomised trials with appropriate ethical approval.
EBR [Taskforce]
Treatment
CONDITIONS MANAGED WITH IMMUNOSUPPRESSANTS
Ruxolitinib
For people with COVID-19, only administer ruxolitinib in the context of
randomised trials with appropriate ethical approval. Only cease or change the dose of long term immunosuppressants such as
EBR [Taskforce] high-dose corticosteroids, chemotherapy, biologics, or disease-modifying
anti-rheumatic drugs (DMARDs) on the advice of the treating specialist.
PP [Taskforce]
Chloroquine
For people with COVID-19, only administer chloroquine in the context of
randomised trials with appropriate ethical approval. EBR [Taskforce]
Hydroxychloroquine
For people with COVID-19, only administer hydroxychloroquine in the
context of randomised trials with appropriate ethical approval.
EBR [Taskforce]
Convalescent plasma
For people with COVID-19, only administer convalescent plasma in the
context of randomised trials with appropriate ethical approval.
EBR [Taskforce]
Interferon β-1a
For people with COVID-19, only administer interferon β-1a in the context
of randomised trials with appropriate ethical approval.
EBR [Taskforce]
Colchicine
For adults with COVID-19, only administer colchicine in the context of
randomised trials with appropriate ethical approval. EBR [Taskforce]
Other disease-modifying treatments
For people with COVID-19, only administer disease-modifying
treatments in the context of randomised trials with appropriate ethical
approval. CBR [Taskforce]
ANTIBIOTICS
44.83 Do not prescribe antibiotics unless indicated for other reasons,
such as suspected CAP. PP [Taskforce]
THINGS TO WATCH FOR
Advise the person and their carer or family members to look out for
Monitoring
the development of new or worsening symptoms, especially breathing
difficulties which may indicate the development of pneumonia or
hypoxaemia.
Reassure the person that 4 out of 5 people with COVID-19 will have a
mild illness and will usually recover 2 to 3 weeks after the initial onset of
symptoms.
If symptoms do worsen, this is most likely to occur in the 2nd or 3rd week
of illness.
PP [Taskforce]
ESCALATION OF CARE TRANSFER TO HOSPITAL
Transfer to hospital is recommended if the person develops symptoms
or signs suggestive of moderate or severe COVID-19, such as: Check the person’s wishes regarding transfer, and whether they
have an Advanced Care Directive for proceeding with hospital
• symptoms or signs of pneumonia management.
• severe shortness of breath or difficulty breathing If the person wishes to stay in their place of residence, discuss care
• blue lips or face arrangements with the patient, their carer(s) and family. Involve
• pain or pressure in the chest their GP, and local palliative care services if available. Be aware that
Next steps in care
out-of-hospital care will be dependent on the capacity of carer(s)
• cold, clammy or pale and mottled skin
and family to manage infection risk at home.
• new confusion or fainting
If the person wishes to be admitted to hospital, advise the carer or
• becoming difficult to rouse family member to call an ambulance and to notify the paramedics
• little or no urine output that the person has suspected or confirmed COVID-19.
• coughing up blood PP [Taskforce]
PP [BMJ]
RELEASE FROM ISOLATION
• Refer to relevant State public health advice for the conditions that
must be met prior to release of a person from isolation.
• Review patient Care at Home advice and provide to patient if
appropriate.
PP [Taskforce]
LEGEND
Sources
ACSQHC – Australian Commission on Safety and Quality in Health Care. COVID-19 Position EBR: Evidence-Based Recommendation
Statement - Managing fever associated with COVID-19 (Revised 29 April 2020). Managing intranasal CBR: Consensus-Based Recommendation
administration of medicines for patients during COVID-19 (Revised 19 May 2020)
PP: Practice Point
AHPPC – Australian Health Protection Principal Committee (AHPPC). Guidance on use of personal
protective equipment (PPE) in non-inpatient healthcare settings, during the COVID-19 outbreak.
17 June 2020. Living Currently prioritised Not prioritised
BMJ – Covid-19: a remote assessment in primary care. BMJ 2020;368:m1182 doi: Guidance for review for review
10.1136/bmj.m1182 (25 March 2020)
Taskforce – Current guidance from the National COVID-19 Clinical Evidence Taskforce
You might also like
- Genentech Student Worksheet - ResultDocument10 pagesGenentech Student Worksheet - ResultArijit MajiNo ratings yet
- MH Exam 2 Study GuideDocument24 pagesMH Exam 2 Study Guidewn4tb100% (1)
- MoHP Protocol For COVID19 November 2020Document28 pagesMoHP Protocol For COVID19 November 2020medya dostorNo ratings yet
- Managing The Long Term Effects of Covid-19: Summary of NICE, SIGN, and RCGP Rapid GuidelineDocument4 pagesManaging The Long Term Effects of Covid-19: Summary of NICE, SIGN, and RCGP Rapid GuidelineRahmanu ReztaputraNo ratings yet
- Consensus Statement: Safe Airway Society Principles of Airway Management and Tracheal Intubation Specific To The COVID-19 Adult Patient GroupDocument10 pagesConsensus Statement: Safe Airway Society Principles of Airway Management and Tracheal Intubation Specific To The COVID-19 Adult Patient GroupMeska AmeliaNo ratings yet
- Mja2 50598Document10 pagesMja2 50598Andi Astrid AmaliaNo ratings yet
- COVID Guidelines UpdatedDocument54 pagesCOVID Guidelines UpdatedmaelisaNo ratings yet
- Covid 19 TreatmentDocument2 pagesCovid 19 TreatmentGio Tamaño BalisiNo ratings yet
- Sars Cov-2 (Covid-19) : Coronavirus Disease (COVID-19) Is An Infectious Disease Caused by A Newly Discovered CoronavirusDocument6 pagesSars Cov-2 (Covid-19) : Coronavirus Disease (COVID-19) Is An Infectious Disease Caused by A Newly Discovered CoronavirusRIZANNEMARIEL BELZANo ratings yet
- Covid-19 For MRCP ExamsDocument6 pagesCovid-19 For MRCP ExamsZara VaraNo ratings yet
- Faqs Breastfeeding and Covid 19Document5 pagesFaqs Breastfeeding and Covid 19ErikaMRSiaNo ratings yet
- COVID GuidelinesDocument54 pagesCOVID GuidelinesHBNo ratings yet
- Saudi Moh Protocol For Patients Suspected Of/Confirmed With Covid-19Document15 pagesSaudi Moh Protocol For Patients Suspected Of/Confirmed With Covid-19AldrinNo ratings yet
- FIP COVID-19 Webinar Slides Key Considerations FinalDocument49 pagesFIP COVID-19 Webinar Slides Key Considerations FinalCahyuni Saputri YusufNo ratings yet
- WHO 2019 nCoV FAQ Breast - Feeding 2020.1 PorDocument6 pagesWHO 2019 nCoV FAQ Breast - Feeding 2020.1 PorLus FerreiraNo ratings yet
- I PREVENT COVID FLU RSV SummaryDocument3 pagesI PREVENT COVID FLU RSV SummaryServaas OostrikNo ratings yet
- WPR Dse 2020 031 EngDocument5 pagesWPR Dse 2020 031 EngKyla LotaNo ratings yet
- COVID-19 Treatment Guidelines: Clinical ManagementDocument6 pagesCOVID-19 Treatment Guidelines: Clinical ManagementPetra SpringNo ratings yet
- COVID 19 Vaccine Clinical Guidance Rheumatic Diseases SummaryDocument6 pagesCOVID 19 Vaccine Clinical Guidance Rheumatic Diseases SummarySiamakNo ratings yet
- MoH Saudi Arabia COVID 19 ProtocolDocument13 pagesMoH Saudi Arabia COVID 19 Protocoladilah fazliNo ratings yet
- WHO Covid19 HomeCare 2020.3 EngDocument4 pagesWHO Covid19 HomeCare 2020.3 EngReggie CastroNo ratings yet
- Return To Work Post Covid CDCDocument5 pagesReturn To Work Post Covid CDCmikaelNo ratings yet
- Exposed To Covid19 1409Document6 pagesExposed To Covid19 1409A ShahinNo ratings yet
- Directorate General of Health Services, Mohfw, Goi Comprehensive Guidelines For Management of Covid-19 Patients Asymptomatic Mild Moderate SevereDocument2 pagesDirectorate General of Health Services, Mohfw, Goi Comprehensive Guidelines For Management of Covid-19 Patients Asymptomatic Mild Moderate SevereSpecial OPD SVMCHRCNo ratings yet
- COVID-19 Protocol July 2022Document36 pagesCOVID-19 Protocol July 2022Mobile AsdNo ratings yet
- Breastfeeding and COVID-19 For Health Care Workers: Frequently Asked QuestionsDocument5 pagesBreastfeeding and COVID-19 For Health Care Workers: Frequently Asked QuestionsDayana Dìaz BalarezoNo ratings yet
- Covid - 19 Vaccine Contraindications & Precautions Background DocumentDocument12 pagesCovid - 19 Vaccine Contraindications & Precautions Background DocumentNico Angelo CopoNo ratings yet
- EN - Management of Healthcare Workers Exposed To COVID 19 V3.2Document6 pagesEN - Management of Healthcare Workers Exposed To COVID 19 V3.2Gangotri GayatriNo ratings yet
- 2020 ACR COVID 19 Clinical Guidance Summary For Pediatric Patients With Rheumatic DiseaseDocument3 pages2020 ACR COVID 19 Clinical Guidance Summary For Pediatric Patients With Rheumatic Diseasehasan andrianNo ratings yet
- Clinical Management Guidelines For Suspected or Confirmed COVID 19 Infection in Adults Version 4 April 2023 MOH NUGDocument94 pagesClinical Management Guidelines For Suspected or Confirmed COVID 19 Infection in Adults Version 4 April 2023 MOH NUGFrozenboy. 1993No ratings yet
- Jama Murthy 2020 It 200008Document2 pagesJama Murthy 2020 It 200008jorgeNo ratings yet
- National Guidelines of COVID 19 1st June 2020Document61 pagesNational Guidelines of COVID 19 1st June 2020Rasha ElbannaNo ratings yet
- FAQs On COVID-19 From AIIMS e-ICUsDocument3 pagesFAQs On COVID-19 From AIIMS e-ICUsrakeshambasanaNo ratings yet
- WHO 2019 nCoV Clinical 2020.5 EngDocument62 pagesWHO 2019 nCoV Clinical 2020.5 EngTemis Edwin Guzman MartinezNo ratings yet
- How COVID-19 Has Changed The Management of Glomerular DiseasesDocument4 pagesHow COVID-19 Has Changed The Management of Glomerular DiseasesLouie MercadoNo ratings yet
- Enero 2022, TratamientosDocument10 pagesEnero 2022, TratamientosMari Carmen GrandasNo ratings yet
- Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is SuspectedDocument19 pagesClinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is SuspectedgustixNo ratings yet
- CAPA Poster 1Document1 pageCAPA Poster 1moNo ratings yet
- How COVID-19 Has Changed The Management of Glomerular DiseasesDocument4 pagesHow COVID-19 Has Changed The Management of Glomerular DiseasesHendri WahyudiNo ratings yet
- Infection Prevention and Control During Health Care When Coronavirus Disease (COVID-19) Is Suspected or ConfirmedDocument13 pagesInfection Prevention and Control During Health Care When Coronavirus Disease (COVID-19) Is Suspected or ConfirmedDina PrilyaNo ratings yet
- Abbott NOW HealthcareDocument3 pagesAbbott NOW HealthcareMadalina PavelNo ratings yet
- FLCCC - Alliance I RECOVER Protocol PostVaccine v1 25may2022Document2 pagesFLCCC - Alliance I RECOVER Protocol PostVaccine v1 25may2022JohnNo ratings yet
- Home Care For Patients With COVID-19 Presenting With Mild Symptoms and Management of Their ContactsDocument5 pagesHome Care For Patients With COVID-19 Presenting With Mild Symptoms and Management of Their ContactsNur MaliaNo ratings yet
- Novel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited SettingsDocument8 pagesNovel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited Settingsdiah Bayu siswantiNo ratings yet
- Treatment of Coronavirus Disease 2019.4Document5 pagesTreatment of Coronavirus Disease 2019.4Gaby VillasmilNo ratings yet
- Treatment: in Vitro Antiviral Activity Against SARSDocument2 pagesTreatment: in Vitro Antiviral Activity Against SARSCerlyn CabanitNo ratings yet
- Pedia COVID POLICIES 2023Document9 pagesPedia COVID POLICIES 2023Katrina Kristine RamosNo ratings yet
- WHO 2019 nCoV IPC 2020.4 Eng - 29june20Document13 pagesWHO 2019 nCoV IPC 2020.4 Eng - 29june20Pusat Penjaminan Mutu Poltekkes PalembangNo ratings yet
- From The Frontline of COVID-19 - How Prepared Are We As Obstetricians: A CommentaryDocument3 pagesFrom The Frontline of COVID-19 - How Prepared Are We As Obstetricians: A CommentaryMila PimentelNo ratings yet
- Nebulized Versus MDI Medication Administration in COVID-19 PatientsDocument3 pagesNebulized Versus MDI Medication Administration in COVID-19 Patientssalman683 gNo ratings yet
- Eua Fulgent Covid HCPDocument3 pagesEua Fulgent Covid HCPapi-527536875No ratings yet
- Document Can Be Found At:: /hcp/non-Us-Settings/overview/index - HTMLDocument25 pagesDocument Can Be Found At:: /hcp/non-Us-Settings/overview/index - HTMLMaqbool AlizaiNo ratings yet
- Novel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited SettingsDocument9 pagesNovel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited SettingsHanni HarahapNo ratings yet
- EUA Acupath Covid HCPDocument3 pagesEUA Acupath Covid HCPFarah AbdullahNo ratings yet
- Infection Prevention and Control Guidance January 2021Document49 pagesInfection Prevention and Control Guidance January 2021saepulloh bin amingNo ratings yet
- COVID-19 Guidelines For Renal Dialysis: 10 February 2022Document19 pagesCOVID-19 Guidelines For Renal Dialysis: 10 February 2022zulfiqarNo ratings yet
- Blue Modern Medical Center Z-Fold BrochureDocument2 pagesBlue Modern Medical Center Z-Fold BrochureAngela Shaine CruzNo ratings yet
- Resbakuna!: Benefits of Covid 19 VaccineDocument2 pagesResbakuna!: Benefits of Covid 19 VaccineAngela Shaine CruzNo ratings yet
- E. Nursing Management (Highlight The Priority Nursing Interventions)Document6 pagesE. Nursing Management (Highlight The Priority Nursing Interventions)Johanisa SultanNo ratings yet
- Pharmacological Treatment of Patients With Mild To Moderate COVID-19: A Comprehensive ReviewDocument12 pagesPharmacological Treatment of Patients With Mild To Moderate COVID-19: A Comprehensive ReviewPhạm Trịnh Công BìnhNo ratings yet
- 2022 ACR Latest COVID and Rheumatic Disease Therapies - Perritt SawDocument70 pages2022 ACR Latest COVID and Rheumatic Disease Therapies - Perritt SawLiza EgudinsNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Australia's Epidemiology and COVID-19 Vaccine RoadmapDocument7 pagesAustralia's Epidemiology and COVID-19 Vaccine RoadmapumarNo ratings yet
- FRIDAY FAST FACTS #32 - Novel Oral AntiCoagulantsDocument2 pagesFRIDAY FAST FACTS #32 - Novel Oral AntiCoagulantsumarNo ratings yet
- General Rural Pathway 2019 AGPT Eligibility FlowchartDocument1 pageGeneral Rural Pathway 2019 AGPT Eligibility FlowchartumarNo ratings yet
- Mycobacterial Infections Hcu Aug 2016 PDFDocument5 pagesMycobacterial Infections Hcu Aug 2016 PDFumarNo ratings yet
- Withdrawal+Guidelines+ +Benzodiazepine+ChapterDocument8 pagesWithdrawal+Guidelines+ +Benzodiazepine+ChapterumarNo ratings yet
- Diabetes Mellitus - Diabetic KetoacidosisDocument21 pagesDiabetes Mellitus - Diabetic KetoacidosisJamil Lorca100% (5)
- What Is Chikungunya Virus?Document12 pagesWhat Is Chikungunya Virus?Quenzil LumodNo ratings yet
- NeedleEMG Fundamentals (David Shapiro)Document36 pagesNeedleEMG Fundamentals (David Shapiro)Shauki AliNo ratings yet
- Licensed Physical Therapist Assistant in New York City Resume Tracy PhillipsDocument3 pagesLicensed Physical Therapist Assistant in New York City Resume Tracy PhillipsTracyPhillipsNo ratings yet
- HaiHua CD 9X User ManualDocument13 pagesHaiHua CD 9X User ManualEdson Cordeaca100% (1)
- WalkerDocument18 pagesWalkerNini JendeukieNo ratings yet
- R F I R: Edesigning The ALL Ncident EportDocument9 pagesR F I R: Edesigning The ALL Ncident EportSheNo ratings yet
- Proudly Presents: Malvin Giovanni 030.09.141Document27 pagesProudly Presents: Malvin Giovanni 030.09.141Malvino GiovanniNo ratings yet
- Pressure UlcersDocument43 pagesPressure UlcersZubda Butt100% (2)
- Https Examinationservices - Nic.in Examsys22part2 Downloadadmitcard AdmitCardKVS - AspxDocument1 pageHttps Examinationservices - Nic.in Examsys22part2 Downloadadmitcard AdmitCardKVS - AspxReema SinghNo ratings yet
- ResumeDocument2 pagesResumeLASONYA CHANDA ROBINSONNo ratings yet
- Visarpa PDFDocument8 pagesVisarpa PDFDr.Chetana INo ratings yet
- DR Shaf3y Neurology Revisions 6pDocument6 pagesDR Shaf3y Neurology Revisions 6pOmar HatemNo ratings yet
- Ramirez-Yañez 2008 JCPD 32 325-30Document6 pagesRamirez-Yañez 2008 JCPD 32 325-30Omer Roy MustafaNo ratings yet
- Cerebro NeonatalDocument8 pagesCerebro NeonatalRodri EspinNo ratings yet
- Fluid Resuscitation - Dita AditianingsihDocument48 pagesFluid Resuscitation - Dita AditianingsihGalih Wicaksono100% (1)
- A Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeDocument10 pagesA Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeInnani Wildania HusnaNo ratings yet
- 05 Digital Vag Exam Revised Feb 06Document2 pages05 Digital Vag Exam Revised Feb 06Musa yohanaNo ratings yet
- Par QDocument1 pagePar QMary Grace DeramasNo ratings yet
- NACO ART Guidelines 2013Document122 pagesNACO ART Guidelines 2013RohitKumarNo ratings yet
- Using The CDDR For Icd-11 Mental, Behavioural or Neurodevelopmental DisordersDocument17 pagesUsing The CDDR For Icd-11 Mental, Behavioural or Neurodevelopmental DisordersAl RamírezNo ratings yet
- Prostate CancerDocument6 pagesProstate CancerfheisanzNo ratings yet
- Type 2 Diabetes The Lancet 2022Document18 pagesType 2 Diabetes The Lancet 2022Valentina Kerguelen HernándezNo ratings yet
- Walsh The Bermuda Triangle of Autism PDFDocument6 pagesWalsh The Bermuda Triangle of Autism PDFAnupamaNo ratings yet
- Dental Clinic Management SystemDocument6 pagesDental Clinic Management Systemsevero delos reyes jrNo ratings yet
- Clinical Manifestations and Assessment of Respiratory Disease 5th Edition Jardins Test BankDocument9 pagesClinical Manifestations and Assessment of Respiratory Disease 5th Edition Jardins Test Banksarahpalmerotpdkjcwfq100% (26)
- Pneumonia in Children: IAP UG Teaching Slides 2015 16Document28 pagesPneumonia in Children: IAP UG Teaching Slides 2015 16Ananya Anaparthi100% (1)
- Cover LetterDocument1 pageCover Letterapi-639518867No ratings yet