Professional Documents
Culture Documents
2023 LabDx Trans03 Basic-Examinations-of-Urine
Uploaded by
stella0 ratings0% found this document useful (0 votes)
36 views5 pagesOriginal Title
2023.LabDx.Trans03.Basic-Examinations-of-Urine
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
36 views5 pages2023 LabDx Trans03 Basic-Examinations-of-Urine
Uploaded by
stellaCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
Basic Examinations of Urine
Mila Amor V. Reyes, MD, FPSP | September 12, 2020
Trans by: Agleham, Cayabas, Laggui, Soriano
OUTLINE • Sample of choice in cases of suspected UTI, less likely to be
contaminated by the epithelium and bacterial flora
I. Introduction to Urinalysis II. Routine Analysis
• External genitalia are cleansed with antiseptic soap and rinsed
A. Abnormalities A. Physical Properties
with sterile water prior to voiding
B. Types of Urine B. Chemical Properties
Specimens C. Sediment Constituents • After micturition is begun, first few ml of urine is discarded, and
III. Review on Key Points a midstream sample is collected in a sterile container
5. Catheterized (In-Out)
IV. Reference
• Sterile urine specimen
I. INTRODUCTION TO URINALYSIS • Obtained safely by inserting a catheter into the bladder, useful
in infants, young children, or debilitated patients
• One of the most commonly performed laboratory procedures
6. Timed urine collection
• Provides important information about primary disease of the
• Used to quantitate excretion of a particular analyte during a
kidneys and urinary tract and impact of various systemic
fixed period
diseases on this organ system
• Sample must be preserved to prevent bacterial overgrowth
→ Adults excrete 1000 to 1500 mL of urine/day
and to limit deterioration of solutes (refrigeration, chemical
→ Inverse relationship between volume excreted and preservatives e.g., formaldehyde, thymol, toluene)
specific gravity of urine
Notes:
• A properly collected and promptly analyzed specimen is an
absolute prerequisite if useful information is to be obtained • Improper specimen collection is the most common source of
from a urinalysis error
• Once the specimen is collected, examination should begin
A. ABNORMALITIES promptly
• Polyuria • Significant changes occur when urine is left standing at room
→ Abnormally increased urine volume (>2000mL/day) temperature (principal cause for inaccurate results)
→ Causes: • If delay is anticipated, urine must be refrigerated or preserved
▪ Diabetes mellitus • Urine changes at room temperature:
▪ Diabetes insipidus → Increased pH
▪ Drugs (caffeine, diuretic, ethanol) → Formation or dissolution of crystals
▪ Chronic renal failure → Destruction of RBCs and WBCs
▪ Renal tubular damage → Bacterial overgrowth
▪ Primary aldosteronism
→ Decrease in ketones, glucose, bilirubin, and urobilinogen
▪ Adrenocortical insufficiency
→ Development of turbidity and pungent odor
▪ Hyperparathyroidism
▪ High salt or protein intake → Dissolution of casts
▪ Psychiatric disorders (psychogenic polydipsia) → Darkening of color
• Oliguria II. ROUTINE ANALYSIS
→ Abnormally decreased urine volume of 100-500mL/day that is
• Set of chemical assays using a dipstick that contains a set of
insufficient to excrete the normal daily solute load
reagent pads
→ Can result from renal diseases and intravascular fluid volume
• Some laboratories perform an automated urinalysis including
contraction
microscopic screening of the specimen
• Anuria
→ Virtual absence of renal function with urine production of <100 • Many factors not associated with disease (e.g., ingestion of
mL/day vitamin C) may affect the physical and chemical properties of
→ Associated with severe renal disease (e.g., complete and urine and interfere with urine dipstick tests.
long-standing urinary tract obstruction, bilateral renal cortical • A patient with significant ketoacidosis and ketonuria may have
necrosis) a negative dipstick reaction for urine ketones because the
• Proper specimen collection is mandatory for an accurate dipstick detects only acetoacetic acid.
urinalysis A. PHYSICAL PROPERTIES
• Minimum of 12 to 15 mL is required
1. Color
• Specimen should be collected in a clean, dry, wide-mouth,
disposable plastic container • Normal: Pale yellow to dark amber
→ Due to the presence of urochrome, uroerythrin and urobilin
B. TYPES OF URINE SPECIMENS pigments
1. First voided urine • Intensity of color is proportional to the concentration of solutes
• First voided urine in the morning: preferred specimen for • Medication – most common cause of abnormal urine color
assessing the concentrating capacity of the kidneys
Table 1. Causes of abnormal urine color.
• Provides the best preserved and most concentrated urinary Abnormal color Causes
sediment
Red, red-brown Blood (smoky), hemoglobin (clear),
2. Random urine
myoglobin, methemoglobin, porphyrins,
• Most commonly obtained specimen beets, phenazopyridine HCI,
• May not reveal abnormalities in urine solute and protein phenolphthalein
contents, or formed elements Yellow-brown, Bile pigments
• Any time of the day green-brown
3. Post-prandial urine Orange Phenazopyridine HCl
• Best detects glucosuria (glucose in urine) Bright orange- Riboflavin and metabolites
• Two hours after meal yellow (multivitamins)
4. Midstream clean-catch specimen
Trans # 3 Basic Examinations of Urine 1 of 5
Brown Melanin, homogentisic acid, rhubarb, ▪ Increased volume and SG due to excessive glucose
cascara, senna excretion, which increases the urinary solute load
Green Acriflavine → Diabetes Insipidus (DI)
Blue-green Methylene blue, azure blue ▪ Large urine volume with low SG, loss of ADH impairs the
renal concentrating mechanism
2. Clarity
• Normal: Clear • The condition glucosuria may result from many conditions
Table 2. Causes of cloudy urine. other than diabetes mellitus.
Conditions Urine constituents 6. Osmolality
Alkaline pH Phosphates • Normal: 500-800 mOsm/kg of water
Acidic pH Urates • It is the ratio of the number of solute molecules to the weight of
Pyuria Leukocytes the solution
Hematuria Erythrocytes • Freezing point depression method – method of measurement
Bacteriuria Bacteria for osmolality
Chyluria Lymph Table 5. Factors affecting urine osmolality.
Alkaline pH Phosphates Factor Urine osmolality
3. Odor High-protein diet Increased urine osmolality
• Normal: Faint, aromatic odor Salt-free diet Decreased urine osmolality
Table 3. Causes of unusual urine odors.
Dehydration Increased urine osmolality
(800-1400 mOsm/kg of water)
Unusual urine odor Causes
Water diuresis Decreased urine osmolality
Ammonia Bacterial contamination
(20-80 mOsm/kg of water)
Musty Phenylketonuria
Pungent Advanced cirrhosis B. CHEMICAL CHARACTERISTICS
Maple syrup Maple syrup disease 1. Protein
Sweaty feet Glutaric acidemia, isovaleric academia • Normal upper limit is 150 mg/day
Acetone Ketonuria • 50-70% comes from plasma and the rest from renal tubular
4. Urinary pH (Tamm-Horsfall mucoprotein) and lower urinary tract sources
• Normal: slightly acidic pH 6 (4.5-8.0) (proteins of seminal, prostatic, and urethra)
• Kidney and lungs – responsible for maintaining acid-base • Proteinuria – greater than 150 mg/day
hemostasis in the plasma • Types of Proteinuria
• Lungs – involved in the expiration of CO2 1. Transient Proteinuria – does not indicate renal disease;
• Kidneys – reabsorb HCO3- filtered by the glomeruli, excrete proteinuria disappears when the causative factor is removed;
nonvolatile organic acids caused by alterations in renal hemodynamics than to changes
in glomerular permeability
Table 4. Non-pathologic changes in urine pH.
a. Postural proteinuria
Alkaline urine Acid urine → 3-5% of healthy adolescents and young adults, occurs
Bacterial contamination Acid contamination of when the person is upright and disappears when the
(pH>8) container person is recumbent
Vegetable diet High-protein diet b. Functional proteinuria
Postprandial (alkaline tide) Sleep (respiratory acidosis) → Associated with physiologic conditions, caused by fever,
5. Specific gravity (SG) strenuous exercise, exposure to heat or cold, emotional
• Normal: 1.016 to 1.022 stress, or CHF
• Used for estimating the concentrating capacity of the kidneys, 2. Persistent proteinuria – usually indicates renal disease
other than test for urine osmolality a. Severe (>3.5 g/day) – renal diseases that greatly increase
• Most important urine solutes: glomerular permeability, e.g., NS, AGN, CGN, lupus
→ Urea nephritis, amyloidosis, renal vein obstruction
b. Moderate (0.5—3.5 g/day) – nephrosclerosis,
→ Sodium (Na+)
pyelonephritis with HPN, preeclampsia, diabetic
→ Chlorine (Cl-)
nephropathy, multiple myeloma, and toxic renal damage
• SG usually measured by: c. Minimal (<0.5 g/day) – CPN, renal tubular disorders,
→ Colorimetric test polycystic renal disease, inactive phases of glomerular
▪ Incorporated in dipsticks diseases, and transient proteinuria
− Based on a pKa change of certain pretreated • Tests for the presence of protein
polyelectrolytes in relation to ionic concentration → Colorimetric Methods
− Affected by protein and highly buffered alkaline urine, ▪ Screening test dipstick pad with pH indicator dye that
but not by glucose or radiographic dyes changes color in proportion to the protein concentration
→ Refractometer and Urinometer/Hydrometer method ▪ Fairly specific for protein; drugs and radiographic contrast
• Clinical correlations: media will not interfere
→ Normal concentrating capacity ▪ Contamination with quaternary ammonium compounds
▪ First morning urine with SG of ≥ 1.023 after fluid deprivation (antiseptics, detergents) or chlorhexidine (skin cleansers),
→ Hypersthenuria and highly buffered alkaline urine may produce false
▪ High urine specific gravity positive results
▪ Presence of high molecular weight substance (e.g., ▪ May not detect other proteins (hemoglobin, Bence-Jones
radiographic contrast media) proteins, globulins)
→ Hyposthenuria → Precipitation Methods
▪ Low urine specific gravity ▪ Used to confirm the presence of proteinuria
▪ Suggests renal tubular injury or excessive fluid intake ▪ Heat and acetic acid, SSA, or TCA
→ Isosthenuria ▪ Resulting turbidity is proportional to the protein
▪ Fixed urine specific gravity of 1.010 concentration
▪ Indicates severe renal damage ▪ Presence of certain drugs (tolbutamide) or radiographic
→ Diabetes Mellitus (DM) contrast media may produce false positive results
Trans # 3 Basic Examinations of Urine 2 of 5
▪ More sensitive and detects all forms of protein • Microscopic examination of the urine sediment is more
→ Bence-Jones Proteins sensitive than a dipstick test for the detection of hematuria.
▪ Best detected by protein electrophoresis or
• Interfering situations of test for hemoglobin
immunoelectrophoresis
▪ Gradual heating of urine precipitates the protein at 40-60°C → Large amounts of urine vitamin C will inhibit the test and
and redissolves near 100°C cause false negative result
2. Glucose and other sugars → Samples with significant bacterial contamination may
contain sufficient peroxidase activity to produce false
• Freely filtered by the glomeruli and resorbed by the tubules
positive result
• Glucosuria
→ Specimen containers contaminated with hypochlorite bleach
→ Blood glucose concentration of >8.3 to 10 mmol/L is the renal
may cause false positive reaction
threshold
• Myoglobin
▪ Glucosuria induces osmotic diuresis – results in 3P's and
high urine SG typical of DM → Not present in normal urine
▪ Glucosuria in the absence of hyperglycemia – defect in → Severe traumatic injury to muscle (crush syndrome), thermal
renal tubular resorptive mechanism, can occur as primary burns, toxic muscle injury (snake venom), primary muscle
renal disorder or secondary to toxic renal injury diseases, strenuous exercise ("march" myoglobinuria), and
spontaneous paroxysmal myoglobinuria
Table 6. Causes of glucosuria.
→ Contains peroxidase-like activity; produces positive dipstick
Causes of glucosuria
test result for hemoglobin
Diabetes mellitus Islet cell tumor
→ Tested by salt precipitation or spectrophotometry
Cushing’s syndrome Hyperthyroidism
Exogenous corticosteroids Pheochromocytoma 4. Bile pigments (Bilirubin and Urobilinogen)
Destructive pancreatic disease CNS disease Table 8. Bile pigments found in urine.
Glycogen storage disease Liver disease Bile pigments in urine
Uremia Trauma Urobilinogen Bilirubin
Severe infection Renal tubular disease Normal Normal (-)
Hemolytic States Increased (-)
• Methods for detecting glucosuria
Hepatocellular Disease Increased (+)/(-)
1. Copper reduction tests
Biliary Obstruction (-)/Decreased (+)
→ not specific, rely on the reducing properties of glucose
→ Benedict's test or Clinitest • Bilirubinuria
→ Other reducing sugars, non-sugar reducing agents may → Conjugated (water-soluble) bilirubin – >1-2 mg/dL is excreted
give a false positive result into the urine
→ Lowest detectable amount is 8.3-13.0 mmol/L → Dipstick test – detect urine levels of 0.8 mg/dL
Table 7. List of non-glucose reducing substances. → Ictotest tablet – detect urine levels of 0.05-0.1 mg/dL
Non-glucose reducing substances → Based on diazo reaction – coupling of bilirubin with diazonium
Galactose Ascorbic acid salt
Lactose Uric acid → False positive tests occur with chlorpromazine metabolites
Fructose Creatinine → False negative tests occur with high levels of vitamin C or
Pentose Drug metabolites urine exposed to light for several hours
Maltose • Urobilinogen
→ Produced within the intestinal lumen by bacterial action on
2. Enzymatic tests
bilirubin, partially absorbed into the portal circulation, small
→ Enzyme glucose oxidase, specific for glucose; amount is excreted in the urine
incorporated in dipsticks reagents
→ Fresh urine must be examined for urobilinogen – based on
→ More specific and sensitive (2.8-5.6 mmol/L) than copper Ehrlich's aldehyde reaction
reduction tests ▪ False negative results with phenazopyridine HCl or azo
→ Substance that causes false positive reaction: dyes
hypochlorite bleach, used to clean urine specimen → Watson-Schwartz test – presence of urobilinogen or
containers porphobilinogen (PBG)
→ High concentration of vitamin C may inhibit the reaction → Hoesch's test – confirmatory test for PBG
and cause false negative result
5. Ketones
3. Blood hemoglobin and related pigments
• Produced when fatty acids are incompletely metabolized by the
• Normal urine contains 0-2 RBCs/HPF liver, e.g., poorly controlled DM, starvation, dehydration,
• Blood occurs in two (2) forms: prolonged vomiting, fever, and rare hereditary metabolic
→ Intact RBC (Hematuria) diseases
▪ Result from renal disease or lower urinary tract disease • Ketonuria – ketones are readily excreted in urine
→ Hemoglobin (Hemoglobinuria) → 3 types of ketones produced:
▪ Result from urinary tract bleeding with hemolysis of cells ▪ β-hydroxybutyric acid (78%)
within the urine; or from intravascular hemolysis, which ▪ Acetoacetic acid (20%)
releases hemoglobin into the plasma ▪ Acetone (2%)
→ Note: Hemoglobinuria without hematuria in fresh urine sample → Detected using alkaline nitroprusside, reacts with
indicates significant hemoglobinemia, or long-standing acetoacetic acid (but not other ketones)
specimen (resulting in cell lysis), or myoglobin is present ▪ Conversion of β-hydroxybutyric acid and acetone to
• Dipstick Test diacetic acid must be incorporated to the reagent strips
→ Based on peroxidase-like activity of heme from free → False positive results with levodopa metabolites, sulfhydryl
hemoglobin, lysed RBCs, or myoglobin containing compounds, and concentrated highly pigmented
→ Less sensitive than microscopic exam (detects 5-20 urine
RBCs/HPF or 0.15-0.62 g/L of hemoglobin) • A patient with significant ketoacidosis and ketonuria may have
→ Microscopic exam must be performed regardless of the a negative dipstick reaction for urine ketones because the
dipstick result dipstick detects only acetoacetic acid.
Trans # 3 Basic Examinations of Urine 3 of 5
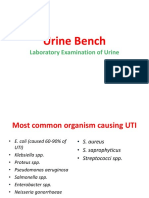
6. Nitrite and Leukocyte esterase 1. Cells
• Nitrite test • Erythrocytes
→ Screening test for UTI/bacteriuria → Hemolyzed in alkaline or dilute urine, and crenated in
→ Reduction of urine nitrate to nitrite by bacteria concentrated urine
→ Test performed ASAP on first morning specimen or on sample → Hematuria with proteinuria suggests renal origin
collected at least 4 hours following the previous voiding Table 9. Causes of gross hematuria.
(allows bacteria in the bladder sufficient time to metabolize Causes of gross hematuria
urine nitrate) Viral cystitis IgA nephropathy
→ False positive test due to bacterial proliferation and Urinary calculi Polycystic kidney disease
metabolism within the specimen container left standing, and Neoplasms Poststreptococcal glomerulonephritis
with phenazopyridine Hypercalciuria
→ False negative test occurs with pathogens that do not form
nitrite from nitrate (e.g., Enterococci, Streptococci, or • Leukocytes
Staphylococci) → Usually neutrophils; rapidly lysed in alkaline or hypotonic
→ Specific for gram negative organisms urine
→ False negative test occurs with large amount of vitamin C, lack → >50 WBCs/HPF or clumps of leukocytes in the sediment
of urine nitrate for bacteria to metabolize, or insufficient suggest acute infection
incubation time within the bladder → >5 WBCs/HPF may be the earliest sign of acute
→ Sensitivity is 60% compared with microbiologic procedures, glomerulonephritis (AGN)
but a positive test suggests significant bacteriuria (>105 → Repeated episodes of pyuria despite negative culture &
organisms/mL) sensitivity suggest renal tuberculosis (TB), lupus nephritis,
• Leukocyte esterase test chlamydial urethritis
→ Detects presence of leukocytes (pyuria) in the urine → Eosinophils – allergic interstitial nephritis
→ Detects both lysed and intact WBCs equivalent to 5-15 → Lymphocytes – TB or chronic inflammatory disorder
cells/HPF • Epithelial cells
→ Interferences: high glucose level (3 g/dL), high SG, presence → Renal tubular cells
of cephalexin, cephalothin, oxalic acid, nitrofurantoin ▪ Smallest, slightly larger than leukocyte; round cells with
→ False negative test results with tetracycline, and neutropenia round nucleus; abundant, clear cytoplasm
→ False positive test results with contamination from vaginal ▪ Increased numbers seen in acute tubular damage [e.g.,
neutrophils acute tubular necrosis (ATN), acute pyelonephritis,
necrotizing papillitis, acute renal allograft rejection]
B. CHEMICAL CHARACTERISTICS → Oval fat bodies
• First-voided morning urine – specimen of choice for ▪ Renal tubular cells or macrophages containing lipid
microscopic exam because urine is most concentrated and ▪ Refractile or exhibit ‘Maltese cross’ formation under
cellular elements are best preserved polarized light
• Urine is centrifuged and the sediment examined ASAP → Transitional cells
▪ From renal pelvis, ureter, or bladder epithelium
▪ More cytoplasm than renal tubular cells; cuboidal cells
with large nucleus; seen in inflammatory states
→ Squamous cells
▪ From the urethra and are of no diagnostic importance
▪ Very large, polygonal cells with angulated margins
2. Casts
• Cylindrical, agglutinated masses formed in the lumen of the
nephron; believed to originate in the DCTs or first part of the
collecting ducts
• Casts may contain large number of cells (cellular cast). Cells
soon disintegrate, their cytoplasmic and nuclear materials
appear as granular fragments (granular cast). Eventually,
cellular debris becomes retractile, homogenous mass (waxy
cast).
• “Telescoped” urinary sediment – sediments that contains a
mixture of all types of casts and inflammatory cells
Table 10. Types of urinary casts.
Types of casts Description
Broad casts • Formed by stasis in the distal portion of
the collecting ducts
• Aka “renal failure casts because of their
association with advanced renal disease
Hyaline casts • Composed of gelled Tamm-Horsfall
protein; transparent, homogenous, and
colorless; soluble in hypotonic urine
• May entrap other elements within the
matrix during their formation –hyaline
cellular casts, hyaline granular casts,
and hyaline fatty casts
• May be found in small numbers in normal
individuals
• Increased excretion after exercise, with
Figure 1. Sediments seen in urine specimen.
dehydration, and with proteinuria
[©2006, The McGraw-Hill Companies, Inc.]
Trans # 3 Basic Examinations of Urine 4 of 5
Erythrocyte • Collections of RBCs within a protein • Cystine – hexagonal plates
casts matrix • Leucine – yellow refractile spheres with radial and concentric
• Yellow-brown to red-brown in fresh urine striations
• Indicate glomerular disease, malignant • Tyrosine – fine, dark-yellow needles arranged in sheaves or
nephrosclerosis, ATN clumps
• Pigmented/Hemoglobin casts – • Ampicillin – masses of long, thin, colorless needles; seen in
degenerated RBC casts that retain acid urine
hemoglobin pigment; suggest glomerular • Radiographic contrast material – flat, 4-sided plates, or long,
disease or intravascular hemolysis thin rectangles
Leukocyte casts • Aggregates of WBCs within a protein • Cholesterol – notched, rectangular plates
matrix 5. Microorganisms
• Renal tubular and interstitial diseases, • Clean-catch specimen with quantitative urine culture
esp. acute inflammation (e.g., acute and → Most reliable way to document significant bacteriuria (105
chronic pyelonephritis, interstitial bacteria/mL)
nephritis, AGN)
• Identification of bacteria in Gram stained smears of uncentrifuged
Epithelial cell • Composed of renal tubular epithelial specimen indicates significant bacteriuria
casts cells → Sensitive but not specific preliminary screening for infection
• Suggest severe tubular damage → Specificity is increased by counting the number of
Granular casts • Result from degeneration of cellular bacteria/OIF in a centrifuged specimen
casts or by direct aggregation of plasma → Negative result does not exclude infection, especially in
proteins into the Tamm-Horsfall matrix females with urethrocystitis with low bacterial counts
• Colorless, dense, with sharp outlines → Culture & sensitivity is used as confirmatory test
• Coarse or fine granular casts • Fungi
• Observed in acute or chronic renal → Most common: Candida albicans, especially in diabetics
disease, CHF in association with ▪ Budding yeasts are characteristic, also, pseudohyphal
proteinuria forms
Waxy casts • Represent end-stage degeneration of ▪ Vaginal candidiasis may contaminate urine
cellular casts • Parasites
• Yellow, highly refractile, homogenous → Most common: Trichomonas vaginalis, indicates vaginal
with sharp outlines, irregular ends, and infection
prominent cracks or fissures → Ova of Schistosoma haematobium may enter urine from the
• Long-standing nephron obstruction and bladder
advanced renal disease → Fecal contamination may contain ova of intestinal parasites
Fatty casts • Coarse granular casts composed mainly e.g., pinworm eggs
of lipid highly refractile and anisotropic • Viral Inclusions
under polarized light → Epithelial cells with viral inclusions
• RBC casts distinguish hematuria of renal origin from bleeding → Nuclear and cytoplasmic inclusions of CMV
more distal in the urinary tract. 6. Tumor cells
3. Lipiduria • Exfoliated cells from the renal pelvis, bladder wall, or urethra
• Three (3) forms • Stained preparations are required
→ Free fat droplets 7. Contaminants
→ Oval fat bodies • Common: spermatozoa, mucus strands, fabric, pollen, hair, talc,
→ Fatty casts cotton fibers, and starch granules
• Nephrotic syndrome
→ Lipiduria with heavy proteinuria, hypoalbuminemia, edema, III. REVIEW ON KEY POINTS
hyperlipidemia • A properly collected and promptly analyzed specimen is an
• Free fat droplets absolute prerequisite if useful information is to be obtained from
→ Also occur with nonrenal conditions (e.g., fractures, a urinalysis.
atheromatous emboli) • Many factors not associated with disease (e.g., ingestion of
4. Crystals vitamin C) may affect the physical and chemical properties of
I. Crystals found in normal urine urine and interfere with urine dipstick tests.
a. Normal alkaline urine • Glucosuria may result from many conditions other than DM.
• Ammonium biurate – yellow-brown spheres, often with • A patient with significant ketoacidosis and ketonuria may have a
spines ("thorn apple" crystals) negative dipstick reaction for urine ketones because the dipstick
• Ammonium magnesium phosphate (triple phosphate) detects only acetoacetic acid.
– colorless, 3-6 sided prisms (“coffin lid” crystals) • Microscopic examination of the urine sediment is more sensitive
• Calcium phosphate – stellate prisms or wedge shapes than a dipstick test for the detection of hematuria.
• Calcium carbonate – tiny, colorless spheres or “dumbbells” • RBC casts distinguish hematuria of renal origin from bleeding
• Amorphous phosphates – fine yellow-brown precipitate more distal in the urinary tract.
of crystalline material of varying sizes and shapes IV. REFERENCE
b. Normal acidic urine
Lecture of Dr. Reyes
• Amorphous urates – tiny, yellow-brown granules of
varying shape but generally uniform size
• Uric acid – most polymorphic, usually yellow or red-brown
prisms or rhomboids
• Calcium oxalate – refractile, often tiny, octahedrons
("envelops")
II. Crystals found in abnormal urine
• Sulfonamides – needle-like sheaves or round forms with
radial striations
Trans # 3 Basic Examinations of Urine 5 of 5
You might also like
- Hematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesFrom EverandHematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesRating: 5 out of 5 stars5/5 (2)
- The Ideal Dialysis Diet Cookbook; The Superb Diet Guide To Managing Kidney Problems And Soothing Dialysis With Nutritious Low Sodium Low Potassium RecipesFrom EverandThe Ideal Dialysis Diet Cookbook; The Superb Diet Guide To Managing Kidney Problems And Soothing Dialysis With Nutritious Low Sodium Low Potassium RecipesNo ratings yet
- URINALYSISDocument6 pagesURINALYSISmaeNo ratings yet
- L2-SCBM 343-2 Urine-WJDocument42 pagesL2-SCBM 343-2 Urine-WJpond_1993No ratings yet
- Introduction To Urinalysis: Student Notes: AubfDocument3 pagesIntroduction To Urinalysis: Student Notes: AubfMelody Jane PardilloNo ratings yet
- AUBFDocument28 pagesAUBFMichelle San Miguel FeguroNo ratings yet
- URINARY SYSTEM New One After DeletDocument36 pagesURINARY SYSTEM New One After DeletyaraNo ratings yet
- AUBF Lesson UrinalysisDocument5 pagesAUBF Lesson UrinalysisReyn CrisostomoNo ratings yet
- Nursing Foundation: Mrs. Neha Babru Asst - ProfessorDocument29 pagesNursing Foundation: Mrs. Neha Babru Asst - ProfessorSharon LawrenceNo ratings yet
- MLSP MidtermDocument14 pagesMLSP MidtermANGELICA ROMAWAKNo ratings yet
- Clinical MicrosDocument14 pagesClinical MicrosKRISTINE JOY PANGAHINNo ratings yet
- AUBF HandoutsDocument11 pagesAUBF Handoutsmika de guzmanNo ratings yet
- Genito-Urinary SystemDocument7 pagesGenito-Urinary Systemugaban.rhaine.bNo ratings yet
- AUBF - Chapter 2Document5 pagesAUBF - Chapter 2Kristin SoquilloNo ratings yet
- 4 - Urine BenchDocument37 pages4 - Urine BenchChiizu iraNo ratings yet
- Intro To Urinalysis TransDocument5 pagesIntro To Urinalysis Transapril jholynna garroNo ratings yet
- Urinary Tract Infection: Jenniferlee Dibernardo Pathophysiology ProjectDocument19 pagesUrinary Tract Infection: Jenniferlee Dibernardo Pathophysiology ProjectAhmad MatterNo ratings yet
- By: Dr. Yoavita Moderator: Dr. Anik Widijanti, SP - PK (K)Document61 pagesBy: Dr. Yoavita Moderator: Dr. Anik Widijanti, SP - PK (K)Gilang KusdinarNo ratings yet
- Urine Examination# DivyaDocument69 pagesUrine Examination# DivyaMedicine 0786No ratings yet
- Shifting Exam Finals TransDocument38 pagesShifting Exam Finals Transjustine vidallonNo ratings yet
- Clinical Microscopy - MTDocument200 pagesClinical Microscopy - MTJihrus MendozaNo ratings yet
- Lesson 5 The UrineDocument44 pagesLesson 5 The UrineFaith TambongNo ratings yet
- Urine Specimen Collection: Ms. Sneha SehrawatDocument36 pagesUrine Specimen Collection: Ms. Sneha SehrawatRajaNo ratings yet
- Urinalysis Chapter 5Document178 pagesUrinalysis Chapter 5Sanket GuptaNo ratings yet
- Urinary Tract InfectionsDocument15 pagesUrinary Tract InfectionsJohir ChowdhuryNo ratings yet
- Clinical Analytical MethodsDocument47 pagesClinical Analytical MethodsDesta Yakob Doda 18BML0121No ratings yet
- Urinary Tract InfectionsDocument43 pagesUrinary Tract InfectionshendraNo ratings yet
- Assessment of Kidney DiseaseDocument23 pagesAssessment of Kidney DiseaserakaNo ratings yet
- Topic 9 The Clinical Microscopy SectionDocument4 pagesTopic 9 The Clinical Microscopy SectionHanna EstebanNo ratings yet
- Nutrition Lab Alcantara, Nikah Pauline F. BSN-2A: UrinalysisDocument12 pagesNutrition Lab Alcantara, Nikah Pauline F. BSN-2A: UrinalysisNIKAH PAULINE ALCANTARANo ratings yet
- Fecalysis LaboratoryDocument7 pagesFecalysis LaboratoryFRANCESCA ALEXANDRIA PAREDESNo ratings yet
- Urinalysis PDFDocument34 pagesUrinalysis PDFAzeli SiquianNo ratings yet
- Urine ExaminationDocument45 pagesUrine ExaminationSalwa FaisalNo ratings yet
- Urinary Elimination: Ma. Tosca Cybil A. Torres, RN, MANDocument37 pagesUrinary Elimination: Ma. Tosca Cybil A. Torres, RN, MANጀኔራል አሳምነው ፅጌNo ratings yet
- Urine Analysis FinalDocument112 pagesUrine Analysis FinalNischita JayarajNo ratings yet
- Genito Urinary TractDocument199 pagesGenito Urinary TractKim GonzalesNo ratings yet
- 2.physical ch. urine د.هناديDocument22 pages2.physical ch. urine د.هناديAbdulmalik Al-harthyNo ratings yet
- URINALYSISDocument5 pagesURINALYSISanaodtohanNo ratings yet
- Clinical Microscopy: Capture All The POO/PEE!!!Document54 pagesClinical Microscopy: Capture All The POO/PEE!!!VenomNo ratings yet
- WEEK 7 Clinical Microscopy - UrinalysisDocument11 pagesWEEK 7 Clinical Microscopy - Urinalysisioperez1868qcNo ratings yet
- Urine Analysis: Sbmitted To:dr - Jayganeesh Asst - Professor Dept - of Modern Diagnosis Submitted By:manisha Nandan 3 Year BNYSDocument30 pagesUrine Analysis: Sbmitted To:dr - Jayganeesh Asst - Professor Dept - of Modern Diagnosis Submitted By:manisha Nandan 3 Year BNYSMeera NandanNo ratings yet
- Aubf LecDocument66 pagesAubf Lec12 Newton - Cayetano, Arafe Nicole A.No ratings yet
- Urinary AssessmentDocument5 pagesUrinary AssessmentStephanie Prue YeeNo ratings yet
- Aubf TransDocument12 pagesAubf TransRai Mohammad AliNo ratings yet
- 24 Hour Urine CollectionDocument11 pages24 Hour Urine CollectionKRIZIA ANE A. SULONGNo ratings yet
- GlomerulonefritisDocument43 pagesGlomerulonefritisdian nofitaNo ratings yet
- Clinical Analytical MethodsDocument47 pagesClinical Analytical MethodsCathrine CruzNo ratings yet
- Fecal Elimination and Urinary EliminationDocument6 pagesFecal Elimination and Urinary Eliminationincent100% (1)
- Urine TestingDocument2 pagesUrine Testingayreensomelhig25No ratings yet
- Physical Characteristics of UrineDocument36 pagesPhysical Characteristics of Urinemuhammad saad100% (1)
- تحليل البول بالصور والشرحDocument72 pagesتحليل البول بالصور والشرحDaouai TaaouanouNo ratings yet
- Analysis of UrineDocument5 pagesAnalysis of UrineHARIDHA SREE.C 18BMB018No ratings yet
- Analysis of UrineDocument5 pagesAnalysis of UrineHaridha ChandranNo ratings yet
- Urinalysis PDFDocument56 pagesUrinalysis PDFTio AjhaNo ratings yet
- MS 1 - Renal SystemDocument11 pagesMS 1 - Renal SystemClaire LimosNo ratings yet
- 1 - Introduction To UrinalysisDocument6 pages1 - Introduction To UrinalysisKunware TropaNo ratings yet
- Chapter 2 Introduction To Urinalysis PDFDocument4 pagesChapter 2 Introduction To Urinalysis PDFJulie Anne Soro ValdezNo ratings yet
- 1st Week Aubf Mtap and Semr FinalsDocument48 pages1st Week Aubf Mtap and Semr FinalsKrenz CatiboNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- 2023.LabDx - Trans05.Serous Effusion & Synovial FluidDocument4 pages2023.LabDx - Trans05.Serous Effusion & Synovial FluidstellaNo ratings yet
- Cerebrospinal Fluid: Figure 2. Lumbar PunctureDocument4 pagesCerebrospinal Fluid: Figure 2. Lumbar PuncturestellaNo ratings yet
- 2023.LabDx - Trans02.Hemostasis and ThrombosisDocument4 pages2023.LabDx - Trans02.Hemostasis and ThrombosisstellaNo ratings yet
- 2023.neuroscience - trans11.PosteriorFossaLevelCerebellar Vestibular and Auditory SystemDocument15 pages2023.neuroscience - trans11.PosteriorFossaLevelCerebellar Vestibular and Auditory SystemstellaNo ratings yet
- 2023.LabDx - Trans01.basic Examination of BloodDocument4 pages2023.LabDx - Trans01.basic Examination of BloodstellaNo ratings yet
- 2023.neuroscience - Trans12.diencephalon & Visual SystemDocument13 pages2023.neuroscience - Trans12.diencephalon & Visual SystemstellaNo ratings yet
- 2023.neuroscience - Trans15.Neurologic ExaminationDocument6 pages2023.neuroscience - Trans15.Neurologic ExaminationstellaNo ratings yet
- Telencephalon: Lecturer: Dr. Lara - June 25,2021 Trans By: Zingapan, Dumelod, Matila, CalaycayDocument17 pagesTelencephalon: Lecturer: Dr. Lara - June 25,2021 Trans By: Zingapan, Dumelod, Matila, CalaycaystellaNo ratings yet
- 2023.neuroscience - Trans10.posterior Fossa Level Brainstem Cranial Nuclei and NervesDocument7 pages2023.neuroscience - Trans10.posterior Fossa Level Brainstem Cranial Nuclei and NervesstellaNo ratings yet
- 2023.neuroscience - Trans14.autonomic Nervous SystemDocument13 pages2023.neuroscience - Trans14.autonomic Nervous SystemstellaNo ratings yet
- Metacognitive TherapyDocument13 pagesMetacognitive Therapyzoey1mNo ratings yet
- Internship - REPORTDocument32 pagesInternship - REPORTMadhukumarNo ratings yet
- RDPL Royal Diagnostics Pvt. Ltd.Document6 pagesRDPL Royal Diagnostics Pvt. Ltd.Royal Diagnostic Centre in Vaishali Nagar JaipurNo ratings yet
- Biology Paper 2 SLDocument16 pagesBiology Paper 2 SLCandela HerreraNo ratings yet
- Printable Flashcard On Normal Lab Values - Free Flash CardsDocument6 pagesPrintable Flashcard On Normal Lab Values - Free Flash CardsCharity T.100% (1)
- A Study On Patient Satisfaction and Quality Evaluation of Health Care ServicesDocument50 pagesA Study On Patient Satisfaction and Quality Evaluation of Health Care ServicesNaresh Kumar100% (1)
- IGNOU Block 3 Unit 4 Communicable Diseases 3 - Zoonotic DiseasesDocument17 pagesIGNOU Block 3 Unit 4 Communicable Diseases 3 - Zoonotic Diseaseserice.researchNo ratings yet
- 3 Study DesignDocument60 pages3 Study DesignNour KoraneNo ratings yet
- Drug Study Format For RLEDocument2 pagesDrug Study Format For RLESheryl Ann Barit PedinesNo ratings yet
- Breast Cancer Related Lymphedema2.pdfL P 4Document12 pagesBreast Cancer Related Lymphedema2.pdfL P 4LýNo ratings yet
- Transcript Foundational Herbcraft Part 1Document32 pagesTranscript Foundational Herbcraft Part 1Stacey DianeNo ratings yet
- Ventilador Philips Trilogy Evo FichaDocument89 pagesVentilador Philips Trilogy Evo FichaSarai PalafoxNo ratings yet
- The Role of High Sugar Consumption On Diabetes Development Among Adults Living in The United States Research PaperDocument12 pagesThe Role of High Sugar Consumption On Diabetes Development Among Adults Living in The United States Research Paperapi-301801285No ratings yet
- Medial Plantar Flap For Hand ReconstructionDocument7 pagesMedial Plantar Flap For Hand ReconstructionMiguel JohnsonNo ratings yet
- 19 - Symptoms, Signs and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified (R00-R99) - 1Document23 pages19 - Symptoms, Signs and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified (R00-R99) - 1Wardatul MukhlishohNo ratings yet
- Artis Zee EP Suite Final PDFDocument20 pagesArtis Zee EP Suite Final PDFTòng Tiêu ThanhNo ratings yet
- Chapter 1Document18 pagesChapter 1Mehar IndiNo ratings yet
- MSDocument49 pagesMSJenniffer Matitu VisdaNo ratings yet
- Frontotemporal Dementia (FTD)Document27 pagesFrontotemporal Dementia (FTD)Wikawee SirisukNo ratings yet
- Shafer's Textbook of Oral Pathology (PDFDrive) - 282-298Document17 pagesShafer's Textbook of Oral Pathology (PDFDrive) - 282-298iWellyFoxNo ratings yet
- Curvas NCDocument3 pagesCurvas NCOscarPazRamirezNo ratings yet
- Forsaken LivesDocument66 pagesForsaken LivesAlbert DomingoNo ratings yet
- Cerebro Vaskuler Disease Pada Kasus FashduDocument60 pagesCerebro Vaskuler Disease Pada Kasus Fashduotha polmedNo ratings yet
- Case3 Case StudyDocument6 pagesCase3 Case StudyKrizzia Angela BacotocNo ratings yet
- Liver Abscess, Hepatic TumoursDocument29 pagesLiver Abscess, Hepatic TumoursNadun MethwadaneNo ratings yet
- Plastic Surgery Board NotesDocument69 pagesPlastic Surgery Board Notesseandarcy600100% (1)
- Broken Family ResearchDocument20 pagesBroken Family Researchmaryie lapeceros87% (38)
- Thyroid DiseasesDocument44 pagesThyroid DiseasesPLDT HOMENo ratings yet
- Evaluation Abutment Tooth:: Prof. Adel Farhan IbraheemDocument12 pagesEvaluation Abutment Tooth:: Prof. Adel Farhan IbraheemMohammad ANo ratings yet
- T2R Survival Guide - 2019Document22 pagesT2R Survival Guide - 2019chioNo ratings yet