Professional Documents
Culture Documents
Hypertension in CKD: Core Curriculum 2019
Hypertension in CKD: Core Curriculum 2019
Uploaded by
yongky amaloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertension in CKD: Core Curriculum 2019
Hypertension in CKD: Core Curriculum 2019
Uploaded by
yongky amaloCopyright:
Available Formats
Core Curriculum
Hypertension in CKD: Core Curriculum 2019
Elaine Ku, Benjamin J. Lee, Jenny Wei, and Matthew R. Weir
Hypertension and chronic kidney disease (CKD) are closely interlinked pathophysiologic states, such Complete author and article
that sustained hypertension can lead to worsening kidney function and progressive decline in kidney information provided at the
end of the article.
function can conversely lead to worsening blood pressure (BP) control. The pathophysiology of hy-
pertension in CKD is complex and is a sequela of multiple factors, including reduced nephron mass, Am J Kidney Dis. 74(1):
increased sodium retention and extracellular volume expansion, sympathetic nervous system over- 120-131. Published online
March 19, 2019.
activity, activation of hormones including the renin-angiotensin-aldosterone system, and endothelial
dysfunction. Currently, the treatment target for patients with CKD is a clinic systolic BP < 130 mm Hg. doi: 10.1053/
The main approaches to the management of hypertension in CKD include dietary salt restriction, j.ajkd.2018.12.044
initiation of treatment with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, © 2019 by the National
and diuretic therapy. Uncontrolled hypertension can lead to significant cardiovascular morbidity and Kidney Foundation, Inc.
mortality and accelerate progression to end-stage kidney disease. Although intensive BP control has
not been shown in clinical trials to slow the progression of CKD, intensive BP control reduces the risk
for adverse cardiovascular outcomes and mortality in the CKD population.
Introduction Several putative mechanisms contribute to
FEATURE EDITOR:
Hypertension is common in patients with chronic elevated BP in patients with CKD, including Asghar Rastegar
kidney disease (CKD). The prevalence ranges neural and hormonal changes that often act in
from 60% to 90% depending on the stage of concert to disrupt appropriate BP regulation ADVISORY BOARD:
CKD and its cause. The mechanisms of hyper- (Fig 1). Ursula C. Brewster
CKD is associated with increased activity Michael Choi
tension in CKD include volume overload, sym- Ann O’Hare
pathetic overactivity, salt retention, endothelial of the RAAS. There is reduced blood flow in
Manoocher Soleimani
dysfunction, and alterations in hormonal systems peritubular capillaries downstream of scle-
that regulate blood pressure (BP). Hypertension rosed glomeruli. As a result of this reduced The Core Curriculum
remains a leading attributed cause of end-stage effective (perceived) blood flow, glomeruli aims to give trainees
kidney disease (ESKD) in the United States. Un- in these regions hypersecrete renin, thereby in nephrology a
increasing circulating angiotensin II levels. strong knowledge
controlled hypertension is also associated with base in core topics in
higher risk for cardiovascular (CV) morbidity and Angiotensin II has a direct vasoconstrictor
the specialty by
mortality. In this Core Curriculum, we review the effect, which increases systemic vascular providing an over-
pathophysiology, diagnosis, and management resistance and BP. Because there are fewer view of the topic and
of hypertension in patients with CKD. functioning glomeruli in CKD, each citing key references,
remaining glomerulus must increase its including the founda-
glomerular filtration rate (GFR): increasing tional literature that
led to current clinical
Pathophysiology of Hypertension in systemic arterial pressure helps bolster approaches.
CKD perfusion pressure and GFR.
Angiotensin II also promotes sodium reab-
Question 1: All of the following mechanisms sorption in the proximal tubule and (through
have been implicated in the development of aldosterone) the collecting duct. Moreover, net
hypertension in patients with CKD except loss of overall GFR impairs sodium excretion,
(choose 1): which also leads to sodium retention. Sodium
a) Sympathetic nervous system (SNS)
retention causes hypertension through volume-
overactivity
b) Increased intracellular calcium level
dependent and volume-independent mecha-
c) Sodium retention nisms. Excess extracellular volume leads to
d) Reversal of hypoxia-induced vasodilation increased perfusion of peripheral tissues, which
e) Increased activity of the renin-angiotensin- stimulates vasoconstriction, increases peripheral
aldosterone system (RAAS) vascular resistance, and therefore increases BP.
f) None of the above; all these mechanisms Extracellular volume expansion also leads to the
have been implicated production of ouabain-like steroids that induce
For the answer to this question, see the
vasoconstriction and therefore increase periph-
following text. eral vascular resistance. Volume-independent
mechanisms include increased vascular stiffness
120 AJKD Vol 74 | Iss 1 | July 2019
Core Curriculum
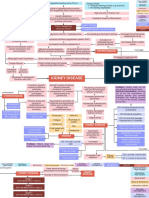
Reduced
glomerular mass
Endothelial
dysfunction Decreased Na+
Increased renin
production excretion
Increased Sympathetic
angiotensin II nervous system
overactivity
Increased Na+
resorption
Na+ retention
Increased
peripheral Increased
Extracellular
vasoconstriction arterial stiffness
volume
expansion
Increased systemic
blood pressure
Figure 1. Pathophysiologic mechanisms of hypertension in chronic kidney disease.
and increased central sympathetic outflow (a direct sequela of and sodium chloride delivery to the macula densa (tubulo-
increased extracellular sodium). glomerular feedback) are part of the autoregulatory
Overactivity of the SNS in CKD stimulates renin pro- process that helps maintain intraglomerular pressure
duction by the renal juxtaglomerular cells. Beyond SNS and therefore GFR. However, in hypertensive patients,
activation by sodium retention, renal ischemia also leads to chronically elevated systemic arterial pressures cause
renal afferent nerve excitation through adenosine. Finally, remodeling of the afferent arteriole and reduce its ability to
experimental and clinical studies suggest that angiotensin constrict and dilate. Over time, elevated systemic arterial
II levels (which are higher in patients with CKD as detailed pressures transmitted to the kidney lead to glomerular
above) directly stimulate SNS activity. hypertension, nephrosclerosis, and progressive loss of
Endothelial dysfunction (including impaired nitrous kidney function.
oxide production), oxidative stress, and elevated endo- As the discussion shows, multiple mechanisms have
thelin levels are also implicated in the pathogenesis of been implicated in the development of hypertension in
hypertension in patients with CKD. CKD. Therefore, the correct answer to question 1 is (f).
Several factors related to CKD complications may also
contribute to the high prevalence of hypertension among Additional Readings
patients with CKD. In anemic patients, treatment with ► Neumann J, Ligtenberg G, Klein II, Koomans HA, Blankestijn PJ.
Sympathetic hyperactivity in chronic kidney disease: pathogen-
erythropoietin and erythropoiesis-stimulating agents can
esis, clinical relevance, and treatment. Kidney Int. 2004;65:
reverse hypoxia-induced vasodilation as hemoglobin 1568-1576.
concentration increases. There is also evidence that these ► Rodriguez-Iturbe B, Romero F, Johnson RJ. Pathophysiological
agents may acutely cause vasoconstriction, even before mechanisms of salt-dependent hypertension. Am J Kidney Dis.
anemia is corrected. Furthermore, secondary hyperpara- 2007;50:655-672.
thyroidism increases intracellular calcium levels, leading to
vasoconstriction. Because progressive CKD is associated Defining Normal and Abnormal BP in CKD
with vascular calcification, isolated systolic hypertension
that is resistant to antihypertensive therapy is relatively Question 2: A 54-year-old woman with a medical history of
common. Finally, uremia may impair vasodilation by stage 3 CKD and dyslipidemia presents to the clinic. BP
inhibiting nitric oxide synthase. readings taken in triage are 138/78 mm Hg and 134/80 mm
While CKD contributes to the development of hyper- Hg. Which of the following would be the best next step:
tension, hypertension is also a major factor in the progres- a) Repeat the BP in the clinic after 5 minutes of quiet rest
sion of CKD. Normally, the glomerular capillary loops are b) Initiate therapy with an angiotensin-converting enzyme
shielded from elevated systemic arterial pressures by a (ACE) inhibitor
c) Order a 24-hour ambulatory BP monitor
process called autoregulation. Afferent arteriole caliber
d) Tell the patient her BP is appropriate for age
changes in response to systemic pressure (myogenic reflex)
AJKD Vol 74 | Iss 1 | July 2019 121
Core Curriculum
higher risk for adverse CV outcomes, as well as CKD
Question 3: The 24-hour ambulatory BP monitoring
progression.
(ABPM) is considered a preferred metric of BPs because: A substantial proportion of patients with CKD have white
a) Clinical trials have shown that lowering ambulatory BPs coat (10%-20%) and masked hypertension (10%-30%),
reduced the risk for CV events which would not be detected in the absence of ABPM
b) White coat hypertension is considered to be completely (Table 1). However, ABPM is not widely available and
benign and should never be treated reimbursement for its performance is poor. When available,
c) ABPM measurements are more strongly associated with elevated BPs obtained using an appropriate technique in the
risk for adverse outcomes compared with clinic BP clinic can be confirmed with 24-hour ABPM, especially in
measurements settings of suspected white coat or masked hypertension.
d) Home BP measurements are usually not performed ABPM can also be useful for confirmation of BP control
correctly by patients and are not associated with risk for
and help detect hypotension that may be occurring outside
adverse outcomes
the office setting in symptomatic patients.
For the answers to these questions, see the following text.
Home BP Monitoring
Out-of-office BP measurements (eg, home BP monitoring)
are more practical than ABPM and can be a useful tool for
Accurate BP measurement is critical to the diagnosis monitoring BPs during therapy. Automated devices that
and management of CKD. Most clinical BP measurements have been validated should be used, and individuals should
are obtained in the office and these measurements are be trained to measure BP in the appropriate fashion (as for
commonly used during treatment decisions, although office BP measurements). Two readings should be taken at
24-hour ABPM is preferred for the confirmation of each sitting, twice a day. Although the evidence is less
abnormal BPs. Office BP measurements should be ob- robust than 24-hour ABPM, home BP measurements have
tained in standardized fashion after 5 minutes of quiet also been associated with risk for adverse outcomes in a
rest using a validated device that is routinely calibrated. similar fashion as ABPM and can be a useful adjunct for
The cuff should be placed on the arm at the level of the improving BP control, especially if combined with tele-
atrium with the correct cuff size (the bladder of the cuff health counseling.
should encircle 80% of the arm), and the patient should
be sitting with feet flat on the ground and back supported
BP Classification and Correlations Between BPs
by a chair. At least 2 readings should be obtained in
Taken in Different Settings
the office. Caffeine and exercise should be avoided 30
minutes before BP measurement. BP measurement errors Based on the most recent American Heart Association/
are common in routine clinical practice, so accurate American College of Cardiology (AHA/ACC) guidelines,
assessment of BP is critical during the diagnosis and
monitoring of hypertension. All major adult clinical Table 1. Definitions of Normal and Abnormal BP Based on the
trial data related to the effect of BP treatment on 2017 AHA/ACC Guideline in Patients With CKD
renal and CV outcomes have used BPs obtained in the Daytime
clinic setting under standardized protocols with serial BP Classificationa Office BP ABPM or Home BP
measurements. Normal or elevated <130/80 mm <130/80 mm Hg
BP Hg
Sustained hypertension ≥130/80 mm ≥130/80 mm Hg
Ambulatory BP Monitoring Hg
Because of the stronger association between BPs obtained White coat hypertension ≥130/80 mm <130/80 mm Hg
from ABPM with CV and renal outcomes, 24-hour ABPM Hg
has been considered the preferred metric of BP in both Masked hypertension <130/80 mm ≥130/80 mm Hg
the general population and patients with CKD. During Hg
24-hour ABPM, an appropriate-size BP cuff is worn for Difficult-to-Control
24 hours, with measurements taken every 15 to 20 mi- BP Definition
nutes during the daytime and every 30 to 60 minutes Resistant Receiving ≥3 antihypertensive agents,
during sleep. Thus, an advantage of ABPM is the provi- hypertension 1 of which is a diuretic, without
sion of readings during sleep that allows for assessment adequate BP control
of appropriate nocturnal physiologic dipping (BP should Refractory Receiving ≥3 antihypertensive agents,
hypertension 1 of which is a thiazide-type diuretic
decrease by >10% during sleep) and BP variability. The and another of which is spironolactone,
presence of masked hypertension (defined as normal without adequate BP control
office BPs but elevated out-of-office BPs) has been Abbreviations: ABPM, ambulatory blood pressure monitoring; AHA/ACC,
associated with higher risk for CV disease in patients American Heart Association/American College of Cardiology; BP, blood pressure;
CKD, chronic kidney disease.
with and without CKD. Both nocturnal hypertension a
As recommended by 2017 ACC/AHA guideline (Whelton et al. J Am Coll Cardiol.
and nondipping status have also been associated with 2018;71(19):2199-2269).
122 AJKD Vol 74 | Iss 1 | July 2019
Core Curriculum
an office BP < 120/80 mm Hg is considered to be Additional Readings
normal, and office BPs in the range of 120- to <130/ ► Agarwal R, Andersen MJ. Prognostic importance of ambulatory
<80 mm Hg are considered to be elevated. An office BP ≥ blood pressure recordings in patients with chronic kidney disease.
130/80 mm Hg would meet the threshold for hyper- Kidney Int. 2006;69:1175-1180.
tension. Although the Systolic BP Intervention Trial ► Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship be-
tween clinic and ambulatory blood-pressure measurements and
(SPRINT) found that assignment to a systolic BP treat-
mortality. N Engl J Med. 2018;378:1509-1520. + ESSENTIAL
ment goal < 120 mm Hg lowered the risk for CV events READING
and death, given that the BPs measured in routine clinic ► Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood
visits are unlikely to be obtained in the same standard- pressure measurement in humans and experimental animals: part
ized approach as in trials such as SPRINT (eg, unob- 1: blood pressure measurement in humans: a statement for pro-
served using an automated device), routine clinic BPs fessionals from the Subcommittee of Professional and Public
could be 5 to 10 mm Hg higher than BPs obtained in Education of the American Heart Association Council on High
Blood Pressure Research. Circulation. 2005;111:697-716.
clinical trials such as SPRINT. Thus, treatment to a sys-
+ ESSENTIAL READING
tolic BP target < 120 mm Hg based on BPs obtained in ► Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/
routine clinical practice could potentially lead to over- AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA
treatment of BP. guideline for the prevention, detection, evaluation, and man-
An office BP of 140/90 mm Hg is thought to correlate agement of high blood pressure in adults: executive summary:
with an ABPM 24-hour average BP of 130/80 mm Hg a report of the American College of Cardiology/American
(135/85 mm Hg daytime and 120/70 mm Hg nighttime Heart Association Task Force on Clinical Practice Guidelines.
J Am Soc Hypertens. 2018;12:579 e571-579 e573.
mean BPs) and a mean home BP of 135/85 mm Hg. The
+ ESSENTIAL READING
appropriate classification of BPs using a combination of
office and ambulatory BPs (when available) are shown in Hypertension Workup and Differential Diagnosis in
Table 1. CKD
Resistant and refractory hypertension (Table 1) in
CKD are common, especially in CKD stages 4 to 5, Question 4: A 42-year-old woman with stage 3 CKD and
for which multiple classes of complementary antihyper- previously well-controlled hypertension for 10 years has
tensive agents are frequently needed to achieve BP required escalation of antihypertensive therapy from 1 to 4
control. medications in the last few months. She is asymptomatic. She
Because the majority of clinical trials in patients with does not have a family history of hypertension. BP measured
and without CKD have targeted office-measured BPs, in the clinic is 160/90 mm Hg in both arms and legs. On
most guidelines (including KDIGO) continue to recom- laboratory evaluation, she has metabolic alkalosis but has
never been hypokalemic. Kidney sizes on renal ultrasound are
mend treatment of hypertension based on office-
normal and symmetric. What is the most appropriate next
measured BPs in adults with CKD. To date, there have step?
been no large clinical trials of adults with CKD that have a) Doppler ultrasound
targeted 24-hour ABPM-derived BPs. Because of the b) Check aldosterone-to-renin ratio
logistical complexity associated with routine ABPM c) Echocardiogram to evaluate for coarctation of the aorta
performance and lack of solid evidence to support ABPM- d) Check serum metanephrine levels
based BPs, we currently recommend routine treatment of e) Reduce dietary sodium intake
hypertension based on office BP measurements ascer- Question 5: All of the following are indications for workup of
tained using standardized protocols. However, in our secondary hypertension in patients with CKD except:
opinion, in the setting of resistant or refractory hyper- a) Onset of elevated BP before puberty but after the
tension, symptoms of orthostasis or hypotension among development of CKD
those receiving antihypertensive therapy and concern for b) Hypertension unresponsive to 3 antihypertensive medi-
autonomic dysfunction or white coat hypertension, cations, including a diuretic
ABPM- or home-based BPs should be obtained to help c) Acute worsening of previously well-controlled
further guide treatment of hypertension in patients with hypertension
CKD. Home BP monitoring may be especially useful d) Persistent hypokalemia off diuretic treatment
for achieving appropriate BP control among patients e) Concomitant development of tremors and palpitations
f) Flash pulmonary edema
with CKD.
In the scenario raised in question 2, the patient’s BP of Question 6: The STAR, ASTRAL, and CORAL trials suggest
137/78 mm Hg is only mildly elevated. It is also a single that renal angioplasty with stenting may not be superior to
visit reading and therefore it is best to repeat this reading medical therapy for renal artery stenosis. As a result, workup
several months later before any treatment is considered. for renovascular hypertension should be reserved for patients
Therefore, the correct answer is (a). who are more likely to improve their BP with revasculariza-
tion. Which of the following patient characteristics
Regarding question 3, because multiple studies have
suggests a higher probability of improvement in BPs after
shown that ABPM more strongly correlates with adverse
revascularization?
outcomes compared to office BP, the correct answer is (c).
AJKD Vol 74 | Iss 1 | July 2019 123
Core Curriculum
a) Resistant hypertension
hypertension, increased risk of CV events, and a higher
b) Flash pulmonary edema incidence of end-organ damage. Although hypokalemia
c) Abrupt onset of hypertension is more frequent in primary aldosteronism, it is detected
d) a) and c) only in <50% of patients with primary aldosteronism. Thus,
e) a), b), and c) the absence of hypokalemia should not deter providers
from screening for primary aldosteronism if there are
For the answers to these questions, see the following text.
other reasons to justify this evaluation. Hyper-
aldosteronism may occur as often in patients with CKD as
in the general population.
As both a cause and consequence of CKD, hypertension is BP measurements in all 4 extremities should be
highly prevalent among patients with CKD. Additional compared to rule out coarctation of the aorta. Patients with
workup for other causes of hypertension is warranted if episodic severe hypertension (with or without headache or
there are reasons to suspect a secondary cause of hyperten- flushing) or a family history concerning for genetic pre-
sion (Box 1). In general, further evaluation is recommended disposition should have serum metanephrine levels
in patients with CKD if the onset of elevated BPs occurred checked to rule out pheochromocytoma.
before puberty (and preceded the development of CKD), Asymmetric kidney sizes, worsening estimated GFR
severe or malignant hypertension that is out of proportion to (eGFR) with ACE inhibition or angiotensin receptor
the degree of CKD is present, sudden worsening of BP blockade, presence of an abdominal bruit, or flash pul-
control occurs in a previously hypertensive patient with monary edema may suggest the presence of renovascular
good BP control, or resistant hypertension is present hypertension. The initial screening test for renal artery
(Table 1). Workup and prioritization of testing should be stenosis is Doppler ultrasonography, and peak systolic
guided by cause-specific signs or symptoms. velocity in the main renal artery is the best parameter for
For example, patients with spontaneous or diuretic- the detection of significant stenosis. To detect ≥60%
induced hypokalemia should be screened for primary reduction in renal artery diameter, a peak systolic velocity
aldosteronism using aldosterone-to-renin ratio. In addi- cutoff of 180 to 200 cm/s has been proposed.
tion, compared with other causes of hypertension, pri- Three randomized trials comparing medical therapy and
mary aldosteronism is characterized by more severe renal angioplasty with stenting in patients with athero-
sclerotic renal artery stenosis did not demonstrate differ-
Box 1. Causes of Secondary Hypertension
ences in mortality, CV events, or progression of CKD: the
STAR (Stent Placement in Patients With Atherosclerotic
• Renovascular hypertension (atherosclerosis, fibromuscular Renal Artery Stenosis and Impaired Renal Function),
dysplasia) ASTRAL (Angioplasty and Stenting for Renal Artery Le-
• Coarctation of the aorta sions), and CORAL (Cardiovascular Outcomes With Renal
• Primary aldosteronism Atherosclerotic Lesions) trials. Although selection bias may
• Pheochromocytoma have led to underestimation of the therapeutic benefits of
• Polycystic ovary syndrome
angioplasty, based on these results, only patients with a
• Cushing syndrome
• Hyperthyroidism, hypothyroidism
higher likelihood of improvement in BPs with revascu-
• Obstructive sleep apnea larization should be evaluated for renovascular hyperten-
> Chemical or medication induced sion because angioplasty is not without risks and medical
> Caffeine, coffee management would otherwise be the primary approach to
> Alcohol treatment. Patient factors that may increase the chances of
> NSAIDs improving BP control with revascularization include recent
> Oral contraceptives onset/progression of hypertension, resistant hypertension,
> Steroids and flash pulmonary edema. In addition, patients with a
> Calcineurin inhibitors
solitary kidney and renal artery stenosis or bilateral renal
> Chemotherapeutic agents (gemcitabine, VEGF receptor
artery stenosis with worsening kidney function could also
inhibitors)
be considered for revascularization.
> Illicit drugs (amphetamines, cocaine)
• Monogenic disorders
In the vignette described in question 4, the patient has
> Liddle syndrome
resistant hypertension with poor control despite the use of 4
> Syndrome of apparent mineralocorticoid excess antihypertensive medications. It is therefore important to
> Glucocorticoid-remediable hypertension (familial hyper- consider secondary causes of hypertension. The key finding
aldosteronism type I) is persistent metabolic alkalosis despite CKD. Although she is
> Familial hyperaldosteronism type III not hypokalemic, it is important to rule out primary
> Gordon syndrome hyperaldosteronism. The correct answer is therefore (b).
> Subtypes of congenital adrenal hyperplasia Regarding question 5, although hypertension in the
Abbreviations: NSAID, nonsteroidal anti-inflammatory drug; VEGF, vascular pre-pubescent period is an indication for further workup,
endothelial growth factor.
hypertension after the development of CKD in this period
124 AJKD Vol 74 | Iss 1 | July 2019
Core Curriculum
is common and in itself should not trigger further workup. hypertensive patients, although a high-potassium intake
All other options require further workup. Therefore, the may be difficult to maintain without provoking hyper-
correct answer is (a). kalemia in patients with more advanced CKD (eg, stage 4
Relevant to question 6, multiple studies have shown a or 5). It is unknown whether a higher potassium diet
correlation between the presence of resistant hypertension, would lower BP in patients with CKD. Limiting alcohol
abrupt onset of severe hypertension and flash pulmonary intake to no more than 2 drinks per day in men and 1
edema, and higher likelihood of responding to revascu- drink per day in women can also help improve BP control.
larization. Therefore, the correct answer is (e). Reducing sodium intake also has the added benefit of
reducing proteinuria.
Additional Readings
Weight loss can reduce BP by w5 mm Hg for every
► ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revas-
5-kg weight loss, and bariatric surgery may be a potential
cularization versus medical therapy for renal-artery stenosis. option in those deemed to be suitable candidates for this
N Engl J Med. 2009;361:1953-1962. procedure. For those with sleep apnea, treatment with
► Cooper CJ, Murphy TP, Cutlip DE, et al. Stenting and medical continuous positive airway pressure may also lead to
therapy for atherosclerotic renal-artery stenosis. N Engl J Med. modest improvements in BP. In addition, both aerobic and
2014;370:13-22. isometric resistance exercise can improve BPs in patients
► Textor SC, Lerman LO. Reality and renovascular disease: when with hypertension. Currently, 90 to 150 minutes of
does renal artery stenosis warrant revascularization? Am J Kidney
Dis. 2014;63:175-177. + ESSENTIAL READING
aerobic exercise is recommended per week. Use of
over-the-counter medications such as nonsteroidal
anti-inflammatory pain medications should be avoided
Management of Hypertension because they may increase BP and also adversely affect
kidney function.
Question 7: Which of the following dietary or behavioral
modifications has not been shown to improve BP control, Renal Denervation
especially in patients with CKD? Renal denervation involves radiofrequency ablation of
a) A <2-g/d sodium diet the network of nerves that innervate the renal artery.
b) Reduction in alcohol intake The role of renal denervation for the treatment of
c) Weight loss resistant (or refractory) hypertension among patients
d) High-potassium diet with CKD is unclear. Although the procedure itself
e) Diet low in unsaturated fats appears to be safe, early randomized trials initially
Question 8: A 60-year-old man with CKD, diabetes, and failed to demonstrate the superiority of renal denerva-
hypertension is on treatment with a maximum-dose ACE tion over sham procedures among patients with resis-
inhibitor, but both his BP and proteinuria are still not at tant hypertension and normal or mildly reduced eGFRs
therapeutic targets. Which of the following would be the best (>45 mL/min/1.73 m2) in terms of reducing office or
choice for antihypertensive therapy, assuming that additional ambulatory BPs 6 months postintervention. However,
proteinuria reduction is a goal and the same BP target could more recent trials have shown more promising results,
be achieved with any of these agents?
including the SPYRAL HTN-ON MED trial, which
a) Add an angiotensin receptor blocker (ARB)
demonstrated that renal denervation was effective in
b) Add clonidine
c) Add amlodipine reducing office systolic BPs by w7 mm Hg compared to
d) Add diltiazem a sham procedure among patients with elevated BPs
e) Add hydralazine who were receiving pharmacotherapy at baseline. A
small study of patients with CKD also showed remark-
For the answers to these questions, see the following text. able reductions in BP (>30 mm Hg) after renal dener-
vation in more advanced CKD (stages 3-4), and some
studies have shown reductions in albuminuria and
Nonpharmacologic Therapy slower progression of CKD with renal denervation.
Dietary and Behavioral Modification However, no device is currently approved in the United
Nonpharmacologic therapy should be the first step to the States for routine clinical use.
treatment of hypertension, even among patients with CKD,
and the mainstays of nonpharmacologic therapy are dietary Baroreceptor Activation
interventions. Diets rich in fruits and vegetables and low in Pacing of the carotid baroreceptors to increase their activity
saturated or unsaturated fats (such as the DASH [Dietary and therefore reduce SNS activity has also been attempted
Approaches to Stop Hypertension] diet) can lead to as a treatment strategy for resistant hypertension. How-
moderate declines in BP by w10 mm Hg in hypertensive ever, this method has not been shown to be efficacious. No
patients. Increasing potassium intake to 3 to 4 g/d and device is currently approved in the United States, and there
reducing sodium intake to <1.5 g/d can also lead to re- are no data on the effectiveness of such devices in patients
ductions in BP by w5 mm Hg with both interventions in with CKD.
AJKD Vol 74 | Iss 1 | July 2019 125
Core Curriculum
Pharmacologic Therapy There has been some suggestion that moving the
In general, for patients with CKD, ACE inhibitors and timing of once-daily antihypertensive therapy from
ARBs are considered first-line antihypertensive agents by morning to nighttime may be beneficial for reducing CV
most guidelines, especially in the presence of concurrent risk, purportedly by restoring physiologic nocturnal
albuminuria (albumin excretion > 300 mg/d). Evidence dipping and the circadian rhythm of BP variation.
to support their benefit over other classes of antihyper- However, the effect of changing only the timing of
tensive agents in those without proteinuria is less robust. antihypertensive medications remains controversial in
ACE inhibitors and ARBs induce efferent arteriolar terms of its long-term CV benefits. In a Cochrane Review
vasodilation, which leads to reductions in intra- of this issue conducted in 2011 that included mostly
glomerular pressure and therefore suppresses proteinuria. studies of patients without CKD, bedtime dosing of
This renal benefit is applicable to both patients with and antihypertensive medications was associated with better
without diabetes. However, the combination of ACE in- BP control, but not with a decrease in risk for adverse
hibitors with ARBs has not been shown to be effective at CV or mortality outcomes.
slowing the progression of CKD or reducing CV events in Table 2 provides recommendations regarding antihy-
patients with CKD (with or without diabetes). Because pertensive therapy selection among patients with CKD. In
this combination may predispose to hyperkalemia and general, ACE inhibitors and ARBs are preferred first-line
acute kidney injury, dual blockade with ACE inhibitors agents in patients with albuminuria or proteinuria, and
and ARBs has generally fallen out of favor. Similarly, diuretics may be useful in combination with ACE in-
although there is some evidence to support the use of hibitors and ARBs to balance the risk for hyperkalemia and
ACE inhibitors or ARBs with aldosterone antagonists in enhance albuminuria or proteinuria reduction. In the
certain conditions such as heart failure, patients with absence of albuminuria or proteinuria, the optimal first-
CKD receiving this regimen need to be monitored care- line agent for patients with CKD is debated and may be
fully for hyperkalemia. selected based on concurrent indications, including the
There is less consensus regarding the optimal second- cause of hypertension, need to treat hyperkalemia, or fluid
line class of antihypertensive agents in patients with overload.
CKD, but diuretics are a reasonable choice for most pa- More recently, a new class of antihyperglycemic
tients with CKD, especially in the setting of volume medications, the SGLT2 inhibitors, has been shown to
overload. Whereas loop diuretics may be preferred as be effective in reducing risk for adverse CV and
GFR declines, especially if there is evidence of kidney disease outcomes. They also possess antihyper-
volume overload, there is evidence that thiazide and tensive effects that do not appear to be related to
thiazide-like diuretics are effective antihypertensive glucosuria.
agents, likely through indirect vasodilatory mechanisms. Medication nonadherence is one of the major reasons
Of the loop diuretics, bumetanide or torsemide may be for inadequate BP control in patients with CKD. More
preferred due to its superior bioavailability. Torsemide than 50% of patients with CKD require 3 or more
also has a longer half-life than furosemide and bumeta- medications to control their BP, and many patients
nide and can be administered once daily. Diuretics may with CKD have a high pill burden because of
be less optimal as the antihypertensive agent of choice for concurrent treatment needed for metabolic acidosis,
patients with CKD due to polycystic kidney disease if hyperphosphatemia, and other sequelae of CKD. It is
they trigger volume depletion and vasopressin release, important to assess for nonadherence to medications as
which may contribute to cyst enlargement. Non- a cause of uncontrolled BPs and to simplify regimens
dihydropyridine calcium channel blockers (eg, diltiazem when possible.
or verapamil) may also have antiproteinuric effects and In terms of question 7, although higher potassium
may be useful in patients with CKD and proteinuria. intake is associated with decreased BP in healthy in-
Among patients with cardiac disease, there may be in- dividuals, it is not known whether a high-potassium diet
dications for other classes of antihypertensive agents, has the same effect in patients with CKD. The correct
such as β-blockers. answer is therefore (d).
For resistant hypertension, regimens that include a Regarding question 8, the nondihydropyridine calcium
diuretic or spironolactone may be considered. When BP is channel blocker diltiazem has been shown to have an
thought to be resistant, confirmation of the accuracy of antiproteinuric effect. Therefore, the best answer is (d).
BP measurements and adherence to BP medications is
important because often BPs are “pseudo-resistant” due to Additional Readings
► Agodoa LY, Appel L, Bakris GL, et al. Effect of ramipril vs amlo-
measurement error or nonadherence to therapy. For pa-
dipine on renal outcomes in hypertensive nephrosclerosis: a
tients who report symptoms of hypotension while randomized controlled trial. JAMA. 2001;285:2719-2728.
receiving antihypertensive therapy, ABPM may be useful to ► Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of
confirm whether these symptoms are related to decreases renal denervation for resistant hypertension. N Engl J Med.
in BP that may not be detected in the office. 2014;370:1393-1401.
126 AJKD Vol 74 | Iss 1 | July 2019
Core Curriculum
Table 2. Selected Indications and Considerations in the Choice of Antihypertensive Agents for Patients With CKD
CKD-Related Other Potential Common Side Potential Other
Medications Indications Indications Effects Contraindications Considerations
Diuretics
Thiazide (eg, Fluid overload; may Kidney stone Hyperuricemia; Gout; hypercalcemia May be less effective
hydrochlorothiazide, improve proteinuria if prevention hypercalcemia; when eGFR is <30
chlorthalidone, used in combination (hypercalciuria); hyponatremia; although some
metolazone) with RAS inhibitors Gordon syndrome; hypokalemia; studies have shown
NDI hyperglycemia these agents remain
(with long-term effective even with
use) low eGFR
Loop (eg, Fluid overload Heart failure; Hearing loss; Gout; sulfonamide- Bumetanide and
furosemide, hypercalcemia hypokalemia; related torsemide have better
bumetanide, hypocalcemia; hypersensitivity intestinal absorption
torsemide) hyponatremia than furosemide
Potassium-sparing Fluid overload; Refractory Hyperkalemia; Pregnancy
(triamterene, hypokalemia hypomagnesemia; metabolic
amiloride) lithium toxicity/NDI acidosis
RAS Blockade
ACEi (first-line Proteinuria Heart failure with Cough; Pregnancy; bilateral
agents if proteinuria) reduction; delays reduced ejection angioedema; renal artery stenosis
progression of CKD fraction; hyperkalemia;
post–myocardial leukopenia;
infarction anemia
ARBs (first-line Proteinuria Uric acid lowering Cough (less than Pregnancy; bilateral
agents if proteinuria) reduction; delays (losartan) or gout; with ACEi); renal artery stenosis
progression of CKD similar to ACEi angioedema;
hyperkalemia
β-Blockers
Selective Heart failure; atrial Bradycardia; Asthma; COPD; 2nd
(metoprolol, fibrillation; hyperkalemia; or 3rd degree heart
nebivolol) migraines; essential fatigue; block
tremors; anxiety depression; sexual
disorders; angina dysfunction
Combined α-β Heart failure; atrial Bradycardia; 2nd or 3rd degree May be better
(carvedilol, labetalol) fibrillation hyperkalemia; heart block tolerated in lung
fatigue; disease than
depression; sexual selective β-blockers
dysfunction
Calcium Channel Blockers
Dihydropyridine Raynaud, Lower-extremity May worsen
(amlodipine, esophageal spasms edema; gingival proteinuria
nifedipine) hypertrophy
Nondihydropyridine Proteinuria reduction Atrial fibrillation Constipation; 2nd or 3rd degree ↑ calcineurin and
(diltiazem, verapamil) gingival heart block mTOR inhibitor levels
hyperplasia
Other
α-Blockers Benign prostatic Orthostasis
hypertrophy; kidney
stone passage
Central α-adrenergic Sedation; Depression
agonists (clonidine) bradycardia; dry
mouth; rebound
hypertension
Vasodilators Headache; Post–myocardial
(minoxidil, tachycardia; lupus- infarction; heart failure
hydralazine) like syndrome
(hydralazine);
edema; pericardial
effusion
Direct renin inhibitors Proteinuria Bilateral renal artery Not recommended for
(aliskiren) reduction; if not stenosis use in combination
tolerating ACEi or with ACEi or ARBs
ARB
(Continued)
AJKD Vol 74 | Iss 1 | July 2019 127
Core Curriculum
Table 2 (Cont'd). Selected Indications and Considerations in the Choice of Antihypertensive Agents for Patients With CKD
CKD-Related Other Potential Common Side Potential Other
Medications Indications Indications Effects Contraindications Considerations
Aldosterone Proteinuria reduction Cirrhosis with Hyperkalemia; May be useful in
antagonists ascites; polycystic metabolic addition to ACEi or
(spironolactone, ovarian syndrome; acidosis; ARB for proteinuria
eplerenone) hyperaldosteronism gynecomastia reduction
Abbreviations: ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary
disease; eGFR, estimated glomerular filtration rate (in mL/min/.173 m2); mTOR, mammalian target of rapamycin; NDI, nephrogenic diabetes insipidus; RAS, renin-
angiotensin system.
► Ruggenenti P, Perna A, Gherardi G, et al. Renoprotective of <140/90 mm Hg. However, in the MDRD Study,
properties of ACE-inhibition in non-diabetic nephropathies assignment to the lower BP goal slowed GFR decline among
with non-nephrotic proteinuria. Lancet. 1999;354:359-364.
+ ESSENTIAL READING
the subset of patients with urinary protein excretion > 1 g/d.
In the ACCORD (Action to Control Cardiovascular Risk in
Diabetes) trial, which included patients with diabetes (but
Effect of Hypertension Treatment on Outcomes and excluded patients with CKD stage 4 or 5), lowering of sys-
Treatment Targets tolic BP to <120 mm Hg was not superior compared to
a <140 mm Hg target for either CV outcomes or kidney
Question 9: Tight BP control (to systolic BP < 120 mm Hg) disease progression, although the majority of patients
has been shown to:
enrolled did not have CKD. The HALT-PKD (HALT Pro-
a) Reduce the risk for death from any cause
gression of Polycystic Kidney Disease) trials randomly
b) Reduce the risk for heart failure
c) Reduce the risk for CKD progression assigned more than 500 hypertensive patients with auto-
d) Improve quality of life somal dominant polycystic kidney disease (baseline eGFR ≥
e) Both a) and b) 60 mL/min/1.73 m2) to a low BP target (95/60-110/
75 mm Hg) versus standard BP target (120/70-130/
Question 10: Largely as a result of SPRINT, the current 80 mm Hg) groups. During follow-up periods ranging from
AHA/ACC- recommended BP goal for patients with nondi-
5 to 8 years, the lower BP group had a 14.2% slower annual
abetic nonproteinuric CKD is:
a) <130/80 mm Hg
increase in total kidney volume, but there were no differ-
b) <130/90 mm Hg ences in change in eGFR. As a consequence, for many years
c) <135/85 mm Hg the recommended BP target for patients with CKD without
d) <140/80 mm Hg significant proteinuria was <140/90 mm Hg; this changed
e) <140/90 mm Hg with the recent publication of SPRINT.
In SPRINT, 9,361 participants (w2,600 with stage 3
For the answers to these questions, see the following text.
CKD) were assigned to a systolic BP target <120 mm Hg
versus <140 mm Hg. SPRINT participants were older than
50 years and the subset with CKD had mildly to moderately
There is strong observational evidence that uncontrolled decreased GFRs. Patients with significant proteinuria or
hypertension is associated with worse renal and CV out- ESKD were excluded from the study. This study population
comes across all age groups. Regardless of the cause of differed from that of the MDRD Study and the REIN-2 trial,
CKD, uncontrolled (and potentially severe) hypertension which recruited patients with more advanced CKD and
accelerates loss of GFR. However, whether intensive greater degrees of proteinuria. Overall, patients assigned to
lowering of BP slows GFR decline is less clear. Patients the lower BP treatment target had lower risk for CV events
with CKD are at elevated CV risk, and hypertension is one (myocardial infarction, other acute coronary syndromes,
of the leading risk factors for CV events and stroke. Several stroke, heart failure, or death from CV causes) and all-cause
randomized trials have compared the effects of varying BP mortality, although no difference in CKD progression was
goals on renal and CV outcomes. As a result of these noted. The trial was stopped prematurely because of the
studies, BP treatment targets for patients with CKD have benefit of intensive BP lowering on CV events. In a subset of
evolved over the last 2 decades. SPRINT participants, those assigned to lower BP targets were
Three large randomized controlled trials of patients also noted to have lower risk for mild cognitive impairment
with nondiabetic CKD (the MDRD [Modification of Diet in and dementia. Largely as a result of data from this trial, in
Renal Disease] Study, AASK [African American Study of 2017, the AHA/ACC released new guidelines recommend-
Kidney Disease in Hypertension], and the REIN-2 [Ram- ing a <130/80 mm Hg BP target for patients with CKD
ipril Efficacy in Nephropathy 2] trial) that assigned BP given the CV benefits from this threshold, regardless of the
targets of approximately <130/80 mm Hg failed to degree of proteinuria present. However, the appropriate BP
demonstrate a benefit for renal (eGFR decline or ESKD risk) target for patients with CKD who do not fit the SPRINT
or CV outcomes compared with BP targets in the range inclusion criteria (including those with diabetes mellitus)
128 AJKD Vol 74 | Iss 1 | July 2019
Core Curriculum
remains a subject of debate. Overall, individualized BP CKD. Because there are physiologic increases in BP with
targets should be set only after weighing potential risks and growth, the threshold for normal BP changes with age
benefits of treatment. and depends on the sex and height of the patient. As in
For question 9, SPRINT showed that tight control was adults, hypertension and proteinuria are strong pre-
associated with a decrease in all-cause mortality and CV dictors of CKD progression in children. Hence, adequate
events but had no effect on progression of CKD; thus, the BP control remains an important focus of CKD manage-
answer to this question is (e). For question 10, the current ment in children.
AHA/ACC recommendation is BP < 130/80 mm Hg, so BP evaluation should be performed at every clinical
the correct answer is (a). encounter for pediatric patients with CKD. However,
even if clinic BP measurements are within the normal
Additional Readings range, more than one-third of children and adolescents
► Cheung AK, Rahman M, Reboussin DM, et al. Effects of intensive with CKD have masked hypertension. White coat hy-
BP control in CKD. J Am Soc Nephrol. 2017;28:2812-2823. pertension is also common in children and affects
+ ESSENTIAL READING
approximately half the children with elevated office BPs.
► Cushman WC, Evans GW, Byington RP, et al. Effects of intensive
blood-pressure control in type 2 diabetes mellitus. N Engl J Med.
Thus, the American Academy of Pediatrics (AAP) rec-
2010;362:1575-1585. + ESSENTIAL READING ommends the performance of 24-hour ABPM at least
► Klahr S, Levey AS, Beck GJ, et al. The effects of dietary protein annually for the detection of white coat and masked
restriction and blood-pressure control on the progression of hypertension in all children with CKD (Table 3). These
chronic renal disease. Modification of Diet in Renal Disease Study recommendations differ from those for adults, for
Group. N Engl J Med. 1994;330:877-884. whom ABPM is not routinely recommended as in the
► Ruggenenti P, Perna A, Loriga G, et al. Blood-pressure control for AAP guidelines.
renoprotection in patients with non-diabetic chronic renal disease
(REIN-2): multicentre, randomised controlled trial. Lancet.
The overall goal for treating hypertension in childhood
2005;365:939-946. is to reduce the risk for target organ damage. The KDIGO
► Schrier RW, Abebe KZ, Perrone RD, et al. Blood pressure in early and AAP clinical practice guidelines currently recommend
autosomal dominant polycystic kidney disease. N Engl J Med. that a child with CKD begin antihypertensive therapy when
2014;371:2255-2266. BP measurements are consistently above the 90th percen-
► Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure tile for the child’s age, sex, and height or ≥130/80 mm
lowering and antihypertensive drug class on progression of Hg.
hypertensive kidney disease: results from the AASK trial. JAMA.
2002;288:2421-2431.
Lifestyle and dietary modifications for the treatment of
hypertension are similar for children as they are for
adults. Initial antihypertensive medications for children
Treatment of Hypertension in Special Populations with CKD and hypertension is either ACE inhibitors or
With CKD ARBs unless there are contradictions to the use of these
agents. If a pediatric patient is not responding to the
Question 11: For which of the following groups is ABPM preferred agents, other antihypertensive treatments such
recommended routinely during the assessment and treat- as α-blockers, β-blockers, calcium channel blockers, or
ment of hypertension?
direct vasodilators can be used. Lifestyle modifications
a) Children and adolescents
b) Patients with a functional allograft
c) Patients older than 65 years
d) Pregnant women Table 3. Hypertension Classification in Children and
Question 12: The BP treatment target for a kidney trans- Adolescents With CKD
plant recipient is: BP Measurements
a) Systolic BP < 120 mm Hg HTN Adolescents
b) Systolic BP < 130 mm Hg Classification Children (1-<13 y) (≥13 y)
c) Systolic BP < 140 mm Hg Hypertension ≥95th percentile for age, sex, ≥ 130/80
d) Dependent on the age of the patient and height or ≥130/80 mm mm Hg
g, whichever is lower
For the answers to these questions, see the following text.
Stage 1 ≥95th percentile to <95th 130-139/80-89
hypertension percentile + 12 mm Hg, or mm Hg
130-139/80-89 mm Hg,
Children and Adolescents whichever is lower
Stage 2 ≥95th percentile + 12 mm ≥ 140/90
Approximately 1% of all patients with CKD are children hypertension Hg, or ≥140/90 mm Hg, mm Hg
and adolescents. Hypertension is found in a considerable whichever is lower
proportion of pediatric patients with CKD and ESKD, Abbreviations: BP, blood pressure; CKD, chronic kidney disease; HTN,
ranging from 50% to 80% depending on the stage of hypertension.
Based on information in Flynn et al (Clinical Practice Guideline for Screening
disease. Currently, thresholds for the diagnosis of hy- and Management of High Blood Pressure in Children and Adolescents.
pertension do not differ for children with or without Pediatrics. 2017;140[3]:e20171904).
AJKD Vol 74 | Iss 1 | July 2019 129
Core Curriculum
should be sustained in combination with pharmacologic high-risk apolipoprotein L1 (APOL1) gene variant, vitamin
treatments. Repeat ABPM should be conducted at least D deficiency, greater degree of sympathetic overactivity,
annually to reassess hypertension treatment response. different dietary patterns, and higher prevalence of obesity
In the ESCAPE (Effect of Strict Blood Pressure Control and metabolic syndrome.
and ACE Inhibition on the Progression of Chronic Renal Currently, BP treatment targets do not vary by race or
Failure in Pediatric Patients) trial, 385 children taking ACE ethnicity, but there are known significant racial and ethnic
inhibitors were randomly assigned to 2 BP targets: inten- disparities in hypertension control. Nonpharmacologic
sified (24-hour mean arterial BP < 50th percentile by treatment for all patients regardless of race and ethnicity
ABPM) or conventional (mean arterial BP from 50th-95th remains the first step to therapy. Lifestyle modifications are
percentile). The intensified treatment arm had slower especially important for the black and Hispanic pop-
progression of their CKD. Hence, tight BP control to a ulations, but adoption of these lifestyle changes is often
24-hour mean arterial BP < 50th percentile by ABPM using difficult due to social and financial barriers in these at-risk
ACE inhibitors as the first-line antihypertensive agent is populations.
currently recommended. Both the AHA/ACC and JNC 8 guidelines recommend
ACE inhibitors or ARBs as initial pharmacologic treatment
Additional Readings for hypertensive patients with CKD regardless of race or
► Flynn JT, Kaelber DC, Baker-Smith CM, et al; Subcommittee on ethnicity. However, it should be noted that there is a
Screening and Management of High Blood Pressure in Children. slightly higher incidence of angioedema with ACE in-
Clinical practice guideline for screening and management of high hibitors in blacks and higher incidence of ACE-induced
blood pressure in children and adolescents. Pediatrics. cough in Asian Americans.
2017;140: e20171904. + ESSENTIAL READING
► ESCAPE Trial Group; Wuhl E, Trivelli A, Picca S, et al. Strict
blood-pressure control and progression of renal failure in children. Additional Readings
N Engl J Med. 2009;361:1639-1650. + ESSENTIAL READING ► Duru OK, Li S, Jurkovitz C, et al. Race and sex differences
► Mitsnefes M, Flynn J, Cohn S, et al; CKiD Study Group. Masked in hypertension control in CKD: results from the Kidney
hypertension associates with left ventricular hypertrophy in chil- Early Evaluation Program (KEEP). Am J Kidney Dis.
dren with CKD. J Am Soc Nephrol. 2010;21:137-144. 2008;51:192-198.
► Samuels J, Ng D, Flynn JT, et al; Chronic Kidney Disease in ► Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure
Children Study Group. Ambulatory blood pressure patterns lowering and antihypertensive drug class on progression of
in children with chronic kidney disease. Hypertension. 2012;60: hypertensive kidney disease: results from the AASK trial. JAMA.
43-50. 2002;288:2421-2431.
Older Patients Women and Pregnancy
Although the Joint National Committee 8 (JNC 8) Although the definition of normal BP differs by sex in
guidelines set a higher BP treatment target of <150/ children, in adults, no sex-specific BP treatment targets have
90 mm Hg for older patients, with the recent publication been developed and the effect of BP treatment on outcomes
of SPRINT, it is now the recommendation that BP has not been shown to differ by sex. Women planning to
be <130/80 mm Hg in adults 65 years and older in the become pregnant should avoid ACE inhibitors or ARBs due
community who are ambulatory. Most trials that have to their teratogenic potential, especially if these agents are
included patients 65 years and older have consistently continued beyond the first trimester of pregnancy.
shown CV benefits to tighter BP control. However, current The optimal BP target for pregnant women with CKD is
AHA/ACC guidelines note that individualization of BP unclear. The goal of antihypertensive therapy is to prevent
treatment targets may be reasonable depending on co- severe hypertension and its sequelae. Agents acceptable for
morbid conditions, life expectancy, and the presence of use during pregnancy for the control of BP include
cognitive impairment. These recommendations do not nifedipine, labetalol, and methyldopa. RAAS inhibitors are
differ for elderly patients 65 years and older who also have contraindicated during pregnancy. Calcium channel
concurrent CKD. blockers and β-blockers may potentially reduce the risk for
preeclampsia during pregnancy.
Race and Ethnicity Considerations in the Treatment
of Hypertension BP Treatment After Kidney Transplantation
The prevalence of uncontrolled hypertension in CKD varies There have been no large-scale randomized controlled
considerably by race or ethnicity and is more prevalent in trials of alternate BP targets in patients with functional
blacks, Hispanics, and Asians. Blacks develop hypertension allografts. In general, both KDIGO and the ACC/AHA
at an earlier age than non-Hispanic whites, have a 4-fold guidelines currently recommend a BP target < 130/80 mm
higher rate of hypertension-related ESKD, and have a Hg, although whether lower BP targets would slow the
higher prevalence of resistant hypertension. These differ- progression of CKD or reduce CV risk remains unclear.
ences may be attributable to genetic and physiologic dif- One observational study of the association between base-
ferences observed in blacks, including the presence of the line BPs of participants from the FAVORIT (Folic Acid for
130 AJKD Vol 74 | Iss 1 | July 2019
Core Curriculum
Vascular Outcome Reduction in Transplantation) trial
Article Information
suggested higher risk for CV disease and mortality with
every 20–mm Hg increase in systolic BP, whereas every Authors’ Full Names and Academic Degrees: Elaine Ku, MD,
MAS, Benjamin J. Lee, MD, MAS, Jenny Wei, BA, and Matthew R.
10–mm Hg lower diastolic BP (if diastolic BP was <70 mm Weir, MD.
Hg) was associated with higher risk for CV disease and
Authors’ Affiliations: Division of Nephrology and Pediatric
mortality. Nephrology, Departments of Medicine and Pediatrics, University
In terms of antihypertensive agent selection, no specific of California San Francisco, San Francisco, CA (EK); Houston
first-line agents are recommended. Although the use of Kidney Consultants, Houston Methodist Institute for Academic
ACE inhibitors and ARBs may be reasonable as first-line Medicine, Houston, TX (BJL); School of Medicine, University of
agents in the kidney transplant population, especially if Southern California, Los Angeles, CA (JW); and Division of
Nephrology and Hypertension, Department of Medicine,
there is proteinuria, risk for hyperkalemia and acute kidney University of Maryland, Baltimore, MD (MRW).
injury may be high with concurrent calcineurin inhibitor Address for Correspondence: Elaine Ku, MD, MAS, Division of
use. Small-scale trials that randomly assigned patients with Nephrology, University of California, San Francisco, 533
functional allografts to ACE-inhibitor or ARB therapy Parnassus Ave, U404, Box 0532, San Francisco, CA 94143-
versus placebo have not shown definitive benefit on 0532. E-mail: elaine.ku@ucsf.edu
pathologic changes, kidney disease progression, or death Support: Dr Ku is funded by NHLBI HL131023.
in this population. Financial Disclosure: Dr Weir has received payments from Vifor,
Returning to question 11, children and adolescents with Merck, Janssen, Relypsa, Abbvie, Ablative Solns, Novo Nordisk,
CKD have a high rate of both masked and white coat hy- Sanofi-Aventis, Boston Scientific, AstraZeneca, Opko, Boehringer
Ingelheim, Vifor Fresenius, Bayer, and Dr. Ku serves as a
pertension. The AAP has recommended that ABPM be consultant to Tricida. The other authors declare that they have no
performed annually in this group; thus, the best answer is relevant financial interests.
(a). For question 12, although no large-scale randomized Peer Review: Received September 7, 2018, in response to an
studies have been performed in kidney transplant re- invitation from the journal. Evaluated by 2 external peer reviewers
cipients to define the best BP level in transplant recipients, and a member of the Feature Advisory Board, with direct editorial
the KDIGO and AHA/ACC guidelines both recommend a input from the Feature Editor and a Deputy Editor. Accepted in
target of <130/80 mm Hg; thus, the best answer is (b). revised form December 20, 2018.
AJKD Vol 74 | Iss 1 | July 2019 131
You might also like
- Mechanistic Insights in Cardiorenal Syndrome: Published August 23, 2022Document13 pagesMechanistic Insights in Cardiorenal Syndrome: Published August 23, 2022Raul Fernando100% (1)
- Consumer Chemistry: Quarter 4 - Module 1Document29 pagesConsumer Chemistry: Quarter 4 - Module 1wetlog lolololim67% (3)
- Fisiopatología HTA en CKDDocument7 pagesFisiopatología HTA en CKDCesar Limón SierraNo ratings yet
- How To Determine Dry Weight'?: Ali I. GunalDocument3 pagesHow To Determine Dry Weight'?: Ali I. GunalEunice P. Immanuella HidayatNo ratings yet
- Medicine Update 2021 Section 11Document62 pagesMedicine Update 2021 Section 11Huda AminNo ratings yet
- Search Termsearch Database: Limits Advanced Journal List HelpDocument21 pagesSearch Termsearch Database: Limits Advanced Journal List Helpحسام جبار مجيدNo ratings yet
- RAAS CKD ProgressionDocument86 pagesRAAS CKD ProgressionNikesh DoshiNo ratings yet
- Therenin-Angiotensin-Aldosteronesystemandheart Failure: Gabriel Sayer,, Geetha BhatDocument12 pagesTherenin-Angiotensin-Aldosteronesystemandheart Failure: Gabriel Sayer,, Geetha BhatHefie RahmaniarNo ratings yet
- Jcom Feb10 HypertensionDocument9 pagesJcom Feb10 HypertensionrchristevenNo ratings yet
- Natriuresis Por PresionDocument8 pagesNatriuresis Por PresionESTEBAN ALEJANDRO PERALTA ROJASNo ratings yet
- Hypertension TanDocument20 pagesHypertension TanBEA RADANo ratings yet
- Biomarkers of Volume Overload and Edema in HFDocument14 pagesBiomarkers of Volume Overload and Edema in HFalcasan63No ratings yet
- Fisiopatologia HtaDocument15 pagesFisiopatologia HtadeisynoriegaNo ratings yet
- KUIPER Et Al-2007-Alimentary Pharmacology & TherapeuticsDocument11 pagesKUIPER Et Al-2007-Alimentary Pharmacology & TherapeuticsJhonatan Efrain Lopez CarbajalNo ratings yet
- Articulo 1 HTADocument15 pagesArticulo 1 HTAMateo VisbalNo ratings yet
- Essential Hypertension Pathogen Es Is and Path o PhysiologyDocument23 pagesEssential Hypertension Pathogen Es Is and Path o Physiology1910149 Yemima Elshantika SyNo ratings yet
- Congestive Renal FailureDocument9 pagesCongestive Renal FailureSayf QisthiNo ratings yet
- Essensial Hypertension Pathogenesis and PathophsiologyDocument22 pagesEssensial Hypertension Pathogenesis and PathophsiologyAmeliana KamaludinNo ratings yet
- Hepatorenal SyndromeDocument10 pagesHepatorenal SyndromeAmaiiranii GarciiaNo ratings yet
- Hepato Renal SyndromeDocument3 pagesHepato Renal SyndromepraveenbhavniNo ratings yet
- NCM 106 - Week 2 (Cardiovascular P1) (Midterm)Document7 pagesNCM 106 - Week 2 (Cardiovascular P1) (Midterm)MARIA KAWILANNo ratings yet
- Update of Pathophysiology and Management of Diabetic Kidney DiseaseDocument14 pagesUpdate of Pathophysiology and Management of Diabetic Kidney DiseasesoniNo ratings yet
- 6 HypertensionDocument95 pages6 HypertensionZeleke temechewNo ratings yet
- Hypertension: S F Vascular SystemDocument12 pagesHypertension: S F Vascular SystemSNo ratings yet
- Liver International - 2017 - M Ller - The Pathophysiology of Arterial Vasodilatation and Hyperdynamic Circulation inDocument11 pagesLiver International - 2017 - M Ller - The Pathophysiology of Arterial Vasodilatation and Hyperdynamic Circulation inVero GiraldoNo ratings yet
- Management of Hypertension in CKD 2015Document9 pagesManagement of Hypertension in CKD 2015Alexander BallesterosNo ratings yet
- The Pathophysiology of HypertensionDocument5 pagesThe Pathophysiology of HypertensionVani OhmanNo ratings yet
- Hypertension in Diabetes PDFDocument6 pagesHypertension in Diabetes PDFNorma González CervantesNo ratings yet
- Materi Koas GinjalDocument30 pagesMateri Koas GinjalRichard 151289No ratings yet
- Im HypertensionDocument4 pagesIm HypertensionNeil Vincent De AsisNo ratings yet
- Renovascular HypertensionDocument20 pagesRenovascular Hypertensionalul847474No ratings yet
- Pathophysiology of Hypertensive Renal DamageDocument7 pagesPathophysiology of Hypertensive Renal DamageXtineNo ratings yet
- Pharma 7 To 13Document212 pagesPharma 7 To 13Loai Mohammed IssaNo ratings yet
- Neurohumoral Blockade in CHF ManagementDocument9 pagesNeurohumoral Blockade in CHF ManagementluongcongthucNo ratings yet
- Reduced Renal Sodium Excretion: Forced Through A Narrow LumenDocument5 pagesReduced Renal Sodium Excretion: Forced Through A Narrow LumenFlowerNo ratings yet
- Hyponatrrmia in A Patient With Hypertensive EmergencyDocument2 pagesHyponatrrmia in A Patient With Hypertensive EmergencybugsfilesNo ratings yet
- Pathophysiology of Acute Renal FailureDocument1 pagePathophysiology of Acute Renal FailureAina HaravataNo ratings yet
- ABC of Heart FailureDocument12 pagesABC of Heart FailureJane PowerNo ratings yet
- Fluid Retention in Cirrhosis: Pathophysiology and ManagementDocument16 pagesFluid Retention in Cirrhosis: Pathophysiology and ManagementÃßD ÔûñîNo ratings yet
- CKD Part 2Document49 pagesCKD Part 2Pao AliNo ratings yet
- Hypertension and Chronic Kidney Disease: Respective Contribution of Mean and Pulse Pressure and Arterial StiffnessDocument6 pagesHypertension and Chronic Kidney Disease: Respective Contribution of Mean and Pulse Pressure and Arterial StiffnessLis Borda MuñozNo ratings yet
- Ascites: Fredric D. GordonDocument15 pagesAscites: Fredric D. GordonNancy Mac Lean BalboaNo ratings yet
- Питание и Гипертония 2013Document7 pagesПитание и Гипертония 2013dr.martynchukNo ratings yet
- The Pathophysiology of Hypertension: Abdul Majid/ Eka Roina MDocument51 pagesThe Pathophysiology of Hypertension: Abdul Majid/ Eka Roina MYohanna SinuhajiNo ratings yet
- ABC of Heart FailureDocument4 pagesABC of Heart Failurekunalprabhu148No ratings yet
- Peripheral Autoregulatory ComponentsDocument2 pagesPeripheral Autoregulatory ComponentsDebbyNovriozaNo ratings yet
- Inotropes and Vasopressors - Circulation. 2008Document11 pagesInotropes and Vasopressors - Circulation. 2008Dani AguirreNo ratings yet
- NIH Public Access: Pathophysiology of Portal HypertensionDocument13 pagesNIH Public Access: Pathophysiology of Portal HypertensionBianeth SantafeNo ratings yet
- Hypertension: Definition and Classification of HypertensionDocument13 pagesHypertension: Definition and Classification of HypertensionnivethitaNo ratings yet
- Genogram Patho 2 PDFDocument3 pagesGenogram Patho 2 PDFLester Jade BOCANo ratings yet
- Cortical NeprhonDocument3 pagesCortical NeprhonProfessingProfessorNo ratings yet
- Evidence-Based Hyponatremia Management in Liver DiseaseDocument21 pagesEvidence-Based Hyponatremia Management in Liver DiseaseDea Fiesta JatikusumaNo ratings yet
- Mechanism of HypertensionDocument4 pagesMechanism of HypertensionAlya Putri KhairaniNo ratings yet
- Hypertension: Risk Associated With "Normal" Blood PressureDocument2 pagesHypertension: Risk Associated With "Normal" Blood PressureAkama BetaNo ratings yet
- HCVDDocument99 pagesHCVDMiguel CuevasNo ratings yet
- Increase in Serum Creatinine: Acute Kidney Injury (AKI)Document5 pagesIncrease in Serum Creatinine: Acute Kidney Injury (AKI)Kurisu AadenNo ratings yet
- Fluid Overload Contributing To Heart FailureDocument4 pagesFluid Overload Contributing To Heart FailureSholihatul AmaliyaNo ratings yet
- Electrolyte and Acid-Base Disturbances Associated With Non-Steroidal Anti-Inflammatory DrugsDocument10 pagesElectrolyte and Acid-Base Disturbances Associated With Non-Steroidal Anti-Inflammatory DrugsMelda Usman Al FatihNo ratings yet
- Entresto in Insuficienta CardiacaDocument2 pagesEntresto in Insuficienta CardiacaRadu AndreiNo ratings yet
- Artigo - Hellen 01Document6 pagesArtigo - Hellen 01YuchungLeeNo ratings yet
- The IDEAL Study: Towards Personalized Drug Treatment of HypertensionDocument10 pagesThe IDEAL Study: Towards Personalized Drug Treatment of HypertensionDi Fon Panse'wNo ratings yet
- Risk Factors, Clinical Presentations and Predictors of Stroke Among Adult Patients Admitted To Stroke Unit of Jimma University Medical Center, South West Ethiopia: Prospective Observational StudyDocument11 pagesRisk Factors, Clinical Presentations and Predictors of Stroke Among Adult Patients Admitted To Stroke Unit of Jimma University Medical Center, South West Ethiopia: Prospective Observational StudyReyhan AristoNo ratings yet
- HAAD Exam 06-08-2020Document16 pagesHAAD Exam 06-08-2020Sandeep Kanneganti100% (2)
- Acute Hypertension-Hypertensive Urgency and Hypertensive EmergencyDocument13 pagesAcute Hypertension-Hypertensive Urgency and Hypertensive EmergencyAmitKumarNo ratings yet
- Research Proposal Form FINALDocument5 pagesResearch Proposal Form FINALJohn Felix AgdaNo ratings yet
- The Different Therapeutic Choices With Arbs. Which One To Give? When? Why?Document12 pagesThe Different Therapeutic Choices With Arbs. Which One To Give? When? Why?Jonathan Ian ArinsolNo ratings yet
- Classification: HypertensionDocument13 pagesClassification: HypertensiontermskipopNo ratings yet
- Seminar: Rany Shamloul, Hussein GhanemDocument14 pagesSeminar: Rany Shamloul, Hussein GhanemApitri PurnomoNo ratings yet
- Hypertension - CSA322 Therapeutics in Practice 3ADocument33 pagesHypertension - CSA322 Therapeutics in Practice 3AV MNo ratings yet
- Morley-Senkler Et Al-2022-Cochrane Database of Systematic ReviewsDocument12 pagesMorley-Senkler Et Al-2022-Cochrane Database of Systematic ReviewsVenessaEdeNo ratings yet
- Histamine 5-ht Angiotensin Kinin Endothelins Eicosanoids Interleukins TNF Interferones Growth FCDocument57 pagesHistamine 5-ht Angiotensin Kinin Endothelins Eicosanoids Interleukins TNF Interferones Growth FCFaisal 'arifNo ratings yet
- Hipertensi PBLDocument56 pagesHipertensi PBLVandra PrinosaNo ratings yet
- Esrd 2 To Interstitial Nep EditedDocument68 pagesEsrd 2 To Interstitial Nep EditedThe GreatNo ratings yet
- Potensi Interaksi Obat Amlodipine Pada Pasien Hipertensi Disalah Satu Puskesmas Kabupaten SumedangDocument7 pagesPotensi Interaksi Obat Amlodipine Pada Pasien Hipertensi Disalah Satu Puskesmas Kabupaten SumedangElisabeth RahmaNo ratings yet
- Hypertension in ElderlyDocument13 pagesHypertension in ElderlybookwormMD100% (2)
- Hypertension Management GuidelineDocument11 pagesHypertension Management GuidelineAdeNeaNo ratings yet
- BenazeprilDocument2 pagesBenazeprilFeliciaDorghamNo ratings yet
- Requirements For European Class 3 Medical Certification of Air Traffic ControllersDocument56 pagesRequirements For European Class 3 Medical Certification of Air Traffic ControllersmalidalkiranNo ratings yet
- Efficacy and Safety of Amlodipine Versus Captopril and Their Combination Inhypertensive Urgency A Randomized Controlled Trial 2329 9126 1000274 PDFDocument7 pagesEfficacy and Safety of Amlodipine Versus Captopril and Their Combination Inhypertensive Urgency A Randomized Controlled Trial 2329 9126 1000274 PDFMaya sariNo ratings yet
- Nursing Care PlanDocument5 pagesNursing Care PlanCharlie AbagonNo ratings yet
- HypertensionDocument17 pagesHypertensionMico AprueboNo ratings yet
- NCM 106 - Week 2 (Cardiovascular P1) (Midterm)Document7 pagesNCM 106 - Week 2 (Cardiovascular P1) (Midterm)MARIA KAWILANNo ratings yet
- Hypertension and Herbal Plant For Its Treatment: A ReviewDocument1 pageHypertension and Herbal Plant For Its Treatment: A Reviewdyan ayu puspariniNo ratings yet
- Redifining Product Management: Suresh Sukheja Is A Pune Based WriterDocument37 pagesRedifining Product Management: Suresh Sukheja Is A Pune Based WriterrahulNo ratings yet
- Atenolol TenorminDocument3 pagesAtenolol TenorminLIEZEL GRACE VELAYONo ratings yet
- HypertensionDocument28 pagesHypertensionSanthoshi Sadhanaa SankarNo ratings yet
- HypertensionDocument27 pagesHypertensionAnamika ChoudharyNo ratings yet
- US Hypertension Review GuidelinesDocument12 pagesUS Hypertension Review Guidelinesmefav7778520100% (1)
- Prediction, Prevention, and Prognosis of Preeclampsia: RecommendationsDocument8 pagesPrediction, Prevention, and Prognosis of Preeclampsia: RecommendationskunkkonkNo ratings yet