Professional Documents
Culture Documents
Eficacia de Lamparas
Eficacia de Lamparas
Uploaded by
Johnnys GonzalezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Eficacia de Lamparas
Eficacia de Lamparas
Uploaded by
Johnnys GonzalezCopyright:
Available Formats
[Downloaded free from http://www.ijds.in on Friday, July 19, 2019, IP: 186.66.190.
122]
Original Article
Assessment of Efficacy and Maintenance of Light‑curing Units
in Dental Offices Across Punjab: A Clinical Survey
Rajinder Bansal, Manu Bansal, Shilpa Walia, Loveena Bansal, Karanvir Singh, Ridhi Aggarwal
Department of Conservative Dentistry and Endodontics, Guru Nanak Dev Dental College and Research Institute, Sunam, Punjab, India
Abstract
Aims and Objectives: Curing units in dental offices across Punjab are analyzed for a practical purpose. Materials and Methods: One
thousand light‑curing units regularly used by the dentists in dental offices across the state of Punjab were examined for their output intensity.
Various factors include as follows: type, power of light‑curing unit, material molecule formation on tip (YES/NO), diameter of guide tip,
and frequency of bulb replacement. A radiometer, a magnifying glass, and a Vernier caliper were used. Data were collected and analyzed.
Results: About 75.80% of dentists use light‑emitting diode (LED) lights, while 24.20% utilize halogen lamps to cure dental composites.
36.60% of light‑curing units of the state had light intensity below 300 mW/cm2, out of which 61.60% were quartz–tungsten–halogen (QTH)
and 28.60% LED light‑curing units. 17.40% of light‑curing units recorded light intensity between 301 and 400 mW/cm2. 46% of light‑curing
units registered an output intensity of >400 mW/cm2. 79.60% of light units showed material particle buildup on light‑curing tips. 62.40% of
dentists never replaced the bulbs of their light‑curing units. Two‑third of dental the practitioners avoided infection control barriers on the tips
of curing units. Conclusions: There is a deficit of knowledge among dental practitioners in Punjab regarding care of light‑curing units. Dental
light‑curing units should be regularly checked and infection control remedies should be opted.
Keywords: Light intensity, light‑curing unit, radiometer
Introduction are depicted in the literature as inadequate.[6] The strength of
light‑curing unit conversely corresponds to the diameter of
The utilization of visible light to cure dental materials has
light‑curing tip.[7]
extended over ongoing years to include a wide range of
items, including luting cements, temporary filling materials, The power of curing lights is essentially lessened due to
periodontal pack materials, reline and impression materials, the presence of composite material development on curing
composite resins, glass ionomers, and bonding agents. tip.[7] Light‑curing units are inclined to bacterial tainting after
Effective utilization of these items specifically depends repeated utilization and various measures can be undertaken
on correct working of the visible light‑curing unit.[1] Light to decrease and prevent this.
restored composite resins depend on adequate light to
A dental radiometer ought to be utilized intermittently to
accomplish satisfactory polymerization. The effect of the
gauge light intensity and decide if there is a requirement
adequate intensity yield of curing lights in guaranteeing
for bulb replacement. This estimation is made on a regular
the life span of filling materials and keeping away from
timetable either weekly or monthly, depending on frequency
unfortunate clinical results is all around accepted.[2,3] As the
of utilization of the curing light.[8]
curing light unit ages, the light yield reduces which prompts
deficient polymerization causing minor breakdown, expanded
wear, diminished quality, poor shading steadiness and Address for correspondence: Dr. Rajinder Bansal,
expanded water sorption, secondary caries, pulpal sensitivity, Department of Conservative Dentistry and Endodontics, Guru Nanak Dev
Dental College and Research Institute, Sunam ‑ 148 028, Punjab, India.
and diminished life span of the restoration.[1,3,4] To cure E‑mail: drrajinderbansal@hotmail.com
composite of 2‑mm thick increment, a power of 400 mW/cm2
is acceptable.[5] Light units with powers of under 300 mW/cm2
This is an open access journal, and articles are distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which allows others to remix,
Access this article online tweak, and build upon the work non‑commercially, as long as appropriate credit is given and
Quick Response Code: the new creations are licensed under the identical terms.
Website:
For reprints contact: reprints@medknow.com
www.ijds.in
How to cite this article: Bansal R, Bansal M, Walia S, Bansal L, Singh K,
DOI: Aggarwal R. Assessment of efficacy and maintenance of light‑curing units
10.4103/IJDS.IJDS_63_18 in dental offices across Punjab: A clinical survey. Indian J Dent Sci
2019;11:42-5.
42 © 2019 Indian Journal of Dental Sciences | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.ijds.in on Friday, July 19, 2019, IP: 186.66.190.122]
Bansal, et al.: A clinical survey for assessment of efficacy and maintenance of light‑curing units in dental offices across Punjab
Materials and Methods • Diameter of light guide tip – Diameter of the light‑curing
tip was estimated with digital Vernier caliper
One thousand light‑curing units routinely utilized by the dental
• Frequency of bulb replacement – Dental practitioners
practitioners in dental workplaces crosswise over Punjab were
were addressed about the history of bulb replacement
analyzed. Consent of the dental practitioner was obtained
and their reaction was recorded likewise in months
so as to inspect the light‑curing unit in the operatory. Type,
• Exercising with infection control on the light‑curing
output power, diameter of light‑curing unit, tip of curing unit,
device tip – Dental practitioners were put to the
frequency of bulb replacement, and infection control barrier
question about the application of protection barriers
on the device tip were examined.
on the light‑curing device tip and their reaction was
The radiometer was standardized by estimating the intensity documented.
of two curing lights of known intensity. One light‑curing unit
was light‑emitting diode (LED) [Figure 1], while other was
quartz‑tungsten-halogen (QTH) [Figure 2]. The radiometer Results
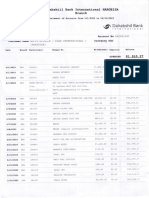
[Figure 3] was consistently checked against these light sources. The information gathered and analyzed demonstrated that
75.80% of dental practitioners utilize LED‑curing lights, while
The yield intensity (mW/cm ) of all the examined light‑curing
2
24.20% utilize QTH restoring lights to cure dental composites
units was sorted into three groups:
[Figure 4]. About 36.60% of light‑curing units of the state had
a. <300 mW/cm2
light intensity beneath 300 mW/cm2, 17.40% of light‑curing
b. In the middle of 301–400 mW/cm2
units recorded light intensity between 301 and 400 mW/cm2,
c. >401 mW/cm2
while 46% of light restoring units demonstrated a yield intensity
• Examination of light‑curing tip – Tip of the
of more than 400 mW/cm2 [Figure 5]. 79.60% of light units
light‑curing unit was inspected with magnifying glass
showed material particle buildup on light‑curing tips [Figure 6].
for the presence/absence of material particles
Only one‑third of dentists used infection control barriers, while
two‑thirds did not use infection control barriers on the tips of
Figure 1: Light‑emitting diode
Figure 2: Quartz–tungsten–halogen
80 75.80
70
60
50
Percentage(%)
40
30 24.20
20
10
0
QTH Lights LED Lights
Number of QTH and LED light-curing units
Figure 3: Radiometer Figure 4: Percentage of practitioners utilizing QTH and LED light‑curing units
Indian Journal of Dental Sciences ¦ Volume 11 ¦ Issue 1 ¦ January-March 2019 43
[Downloaded free from http://www.ijds.in on Friday, July 19, 2019, IP: 186.66.190.122]
Bansal, et al.: A clinical survey for assessment of efficacy and maintenance of light‑curing units in dental offices across Punjab
50 90
46 79.60
80
40 36.60 70
60
Percantage(%)
Percentage(%)
30
50
40
20 17.40
30 20.40
10 20
10
0 0
<300 301-400 >400 NO YES
Material particle buildup
Intensity of light-curing units in mW/cm2
Figure 6: Material particle buildup on light‑curing tips
Figure 5: Intensity of light‑curing units used
68.10 70
70 62.40
60
60
50
50
Percentage(%)
40
Percentage(%)
40
31.90 30
30
20 17.70
13.30
20
6.60
10
10
0
0 6 months or less 7-12 months 13-18 months Never
YES NO Time Period
Use of infection control barriers
Figure 8: Percentage of dentists who never replaced bulbs of their
Figure 7: Percentage of dentists using infection control barrier on tips light‑curing units
of light‑curing units
Light‑cured resin composites depend on adequate intensity of
light‑curing units [Figure 7]. Nearly 62.40% of dentists never light to accomplish satisfactory polymerization.[13] Yield force
replaced the bulbs of their light‑curing units [Figure 8]. About of 400 mW/cm2 for 40 s is acceptable to completely cure a
91.30% of dentists use light guide tip with 8‑mm diameter, 2‑mm thick increment.[5] Under experimental conditions, light
while only 8.70% of dentists use light guide with diameter of units with intensities of under 300 mW/cm2 are considered as
10 mm to cure composite resins [Figure 9]. inadequate.[14] The intensity of light‑curing units ought to never
dip under 300 mW/cm2 to sufficiently polymerize a 2‑mm thick
Discussion increment of universal shade composite resin.[15] Deficient
The utilization of composite resins has expanded in the modern polymerization of composite resins in more deeper layers
era as a result of expanding patient’s interest for all the more cause diminished mechanical properties prompting minor
esthetically satisfying restorations[9] and visible light‑curing breakdown, expanded wear, diminished quality, poor shading
units have turned into an integral component of modern stability, expanded water sorption, and secondary caries.[6]
adhesive dentistry.[10] QTH lights and LED units are utilized The adherence of composite resin to the light tip diminishes
most often in everyday clinical practice.[11] Three‑fourth the productivity of light‑curing tip tends to dissipate the light,
of dental practitioners of the state utilize LED, while just extensively decreasing the yield power. In this way, the tip
one‑fourth utilize QTH‑curing lights in dental facilities ought to be free of composite resin.[13,16]
crosswise over Punjab.
About 79.60% of light‑curing units indicated composite resin
LED technology has a few points of interest contrasted with
material buildup on light‑curing tip. Resin‑based composite
halogen relieving lights. To start with, unlike halogen lights,
development has a critical negative impact on irradiance on
LED delivers light inside a limited spectral range. This energy
the grounds that the resin‑based composite material hinders
range is almost perfect for activating materials that utilize
the light output.[15,17]
camphorquinone as a photoactivator. LED requires less power
to work; therefore, these are with rechargeable batteries. This Light‑curing units are utilized for a more extensive scope of
component makes them cordless, versatile, and moderately clinical applications. As a result of lower irradiance values,
lightweight. Moreover, low‑power requirement wipes out bigger diameter tips might be less powerful than smaller
the need for a cooling fan since heat delivering infrared diameter tips in polymerizing light‑activated materials.[18]
wavelengths are eliminated.[12] Most commonly utilized diameter of light guide tips was
44 Indian Journal of Dental Sciences ¦ Volume 11 ¦ Issue 1 ¦ January-March 2019
[Downloaded free from http://www.ijds.in on Friday, July 19, 2019, IP: 186.66.190.122]
Bansal, et al.: A clinical survey for assessment of efficacy and maintenance of light‑curing units in dental offices across Punjab
100 91.30 Conflicts of interest
There are no conflicts of interest.
80
60 References
Percentage(%)
1. Martin FE. A survey of the efficiency of visible light curing units. J Dent
40
1998;26:239‑43.
2. Hegde V, Jadhav S, Aher GB. A clinical survey of the output intensity
20 8.70 of 200 light curing units in dental offices across Maharashtra. J Conserv
Dent 2009;12:105‑8.
0
3. Pearson GJ, Longman CM. Water sorption and solubility of resin‑based
10mm 8mm materials following inadequate polymerization by a visible‑light curing
Tip Diameter of QTH and LED light curing units in millimeter
system. J Oral Rehab 1989;16:57‑61.
4. Leung RL, Fan PL, Johnston WM. Post irradiation polymerization of
Figure 9: Percentage of dentists using different tip diameters of
visible light‑activated composite resin. J Dent Res 1983;62:363‑5.
light‑curing units 5. Jadhav S, Hegde V, Aher G, Fajandar N. Influence of light curing units on
failure of directcomposite restorations. J Conserv Dent 2011;14:225‑7.
8 mm (91.30%) followed by 10 mm (8.70%) among dental 6. Bansal R, Hora BS, Kumar A, Bansal M, Gupta C, Singla S. Are we
doing justice? A clinical survey of the output intensity of light curing
practitioners crosswise over Punjab. The QTH lights have a
units in dental offices. Int J Dent Sci 2012;4:9‑11.
constrained life expectancy of 100 h because of consecutive 7. Christensen R. Practice made perfect dental infection control – Can we
degradation during repeated working cycles. QTH bulb call the changes progress. J Esthet Dent 1994;6:135‑8.
replacement ought to be supplanted every 6 months to 8. Corciolani G, Vichi A, Davidson CL, Ferrari M. The influence
guarantee ideal performance.[19] of tip geometry and distance on light‑curing efficacy. Oper Dent
2008;33:325‑31.
Tainting of light guides and light control unit (LCU) handles 9. El‑Mowafy O, El‑Badrawy W, Lewis DW, Shokati B, Soliman O,
Kermalli J, et al. Efficacy of halogen photopolymerization units in
is common after clinical utilize. LCU and light guides utilized
private dental offices in Toronto. J Can Dent Assoc 2005;71:587.
for curing resins ought not be in direct contact with oral tissues, 10. Dunn WJ, Bush AC. A comparison of polymerization by light‑emitting
which can be responsible of transmission of infectious agents diode and halogen‑based light‑curing units. J Am Dent Assoc
from one patient to another.[18,20,21] 2002;133:335‑41.
11. Jung H, Friedl KH, Hiller KA, Furch H, Bernhart S, Schmalz G,
About 68.10% dental specialists did not utilize contamination et al. Polymerization efficiency of different photocuring units through
control barrier on the tip of light‑curing units. The presentation ceramic discs. Oper Dent 2006;31:68‑77.
12. Leonard DL, Charlton DG, Roberts HW, Cohen ME. Polymerization
of dental practitioners and auxiliaries to a variety of infectious efficiency of LED curing lights. J Esthet Restor Dent 2002;14:286‑95.
agents is generally ignored. Light‑curing devices are a potential 13. Mehta P, Bansal R, Dhawan R, Khatri A. Dental light curing units – A
wellspring of infectious diseases because of tainting of the light review. Int J Dent Sci 2014;6:125‑8.
tip, which specifically contacts oral tissues. 14. Fan PL, Schumacher RM, Azzolin K, Geary R, Eichmiller FC.
Curing‑light intensity and depth of cure of resin‑based composites tested
according to international standards. J Am Dent Assoc 2002;133:429‑34.
Conclusions 15. Bayne SC. Dental Materials. Sturdvents, Art and Science of Operative
Dentistry. 4th ed. USA: Mosby; 2002. p. 200.
From the present investigation, it can be presumed that there is 16. McAndrew R, Lynch CD, Pavli M, Bannon A, Milward P. The effect of
an absence of awareness among dental practitioners in Punjab disposable infection control barriers and physical damage on the power
with respect to intensity and maintenance of light‑curing output of light curing units and light curing tips. Br Dent J 2011;210:E12.
units. Radiometer ought to be accessible in each dental office 17. Maghaireh GA, Alzraikat H, Taha NA. Assessing the irradiance
delivered from light‑curing units in private dental offices in Jordan.
for occasional checking of light force of curing unit. Bulb of J Am Dent Assoc 2013;144:922‑7.
light‑curing unit ought to be supplanted when the intensity of 18. Rueggeberg FA, Caughman WF. Factors affecting light transmission of
the light‑curing unit falls beneath 400 mW/cm2. Tips of ought single‑use, plastic light‑curing tips. Oper Dent 1998;23:179‑84.
to be free from any sort of material molecule development. 19. Friedman J. Variability of lamp characteristics in dental curing lights.
J Esthet Dent 1989;1:189‑90.
Light‑curing tip of minimum diameter and disposable barrier 20. Shortall AC, Harrington E, Wilson HJ. Light curing unit effectiveness
tips ought to be utilized. assessed by dental radiometers. J Dent 1995;23:227‑32.
21. Chong SL, Lam YK, Lee FK, Ramalingam L, Yeo AC, Lim CC, et al.
Financial support and sponsorship Effect of various infection‑control methods for light‑cure units on the
Nil. cure of composite resins. Oper Dent 1998;23:150‑4.
Indian Journal of Dental Sciences ¦ Volume 11 ¦ Issue 1 ¦ January-March 2019 45
You might also like
- Gl-300 Gps Tracker User Manual Rev2Document28 pagesGl-300 Gps Tracker User Manual Rev2ravelsteinNo ratings yet
- IAAD Working Instructions - Light CuringDocument3 pagesIAAD Working Instructions - Light CuringgabyNo ratings yet
- From Direct Versus Indirect' Toward An Integrated Restorative Concept in The Posterior Dentition Opdam2016 PDFDocument8 pagesFrom Direct Versus Indirect' Toward An Integrated Restorative Concept in The Posterior Dentition Opdam2016 PDFLeandroMartinsNo ratings yet
- Adhesive Restoration of Endodontically Treated TeethFrom EverandAdhesive Restoration of Endodontically Treated TeethRating: 3 out of 5 stars3/5 (2)
- IFC2x3 TC1 Entity Hierarchy PDFDocument17 pagesIFC2x3 TC1 Entity Hierarchy PDFthouartuNo ratings yet
- 1756 0500 7 416Document9 pages1756 0500 7 416dr.m3.abazaNo ratings yet
- 6840 27220 1 PBDocument3 pages6840 27220 1 PBPercy Andree Bayona GuillermoNo ratings yet
- Effectiveness of Low-Level Laser Therapy On Stability of Dental Implants A Systematic ReviewDocument6 pagesEffectiveness of Low-Level Laser Therapy On Stability of Dental Implants A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Regenerative Endodontics: A Paradigm Shift in Clinical EndodonticsDocument7 pagesRegenerative Endodontics: A Paradigm Shift in Clinical EndodonticsCyber MagicNo ratings yet
- SaudiEndodJ9127-1446986 040109Document7 pagesSaudiEndodJ9127-1446986 040109umar talibNo ratings yet
- Variations in Flexural Strength of Heat-Polymerized Acrylic Resin After The Usage of Denture CleanserDocument5 pagesVariations in Flexural Strength of Heat-Polymerized Acrylic Resin After The Usage of Denture Cleanserhafidh akbarNo ratings yet
- Laser and Its Use in Pediatric Dentistry: A Review of Literature and A Recent UpdateDocument5 pagesLaser and Its Use in Pediatric Dentistry: A Review of Literature and A Recent UpdateTiaraNo ratings yet
- Journal Laser and Its Use in Pediatric Dentistry A ReviewDocument5 pagesJournal Laser and Its Use in Pediatric Dentistry A ReviewTiaraNo ratings yet
- The Advantages of The Dental Operative MicroscopeDocument6 pagesThe Advantages of The Dental Operative MicroscopeMarielEsmeraldaNo ratings yet
- Evolution of Indirect Restorations For Fixed Prosthodontics: Planning, Preparation and CementationDocument16 pagesEvolution of Indirect Restorations For Fixed Prosthodontics: Planning, Preparation and CementationImane HNo ratings yet
- JPharmBioallSci95295-3690707 101507Document4 pagesJPharmBioallSci95295-3690707 101507ayoubNo ratings yet
- DR IbadatDocument10 pagesDR IbadatVinod ViswanathanNo ratings yet
- SJODR 48 555 556 CDocument2 pagesSJODR 48 555 556 Cyasser bedirNo ratings yet
- Tugas Resume Jurnal Resin KompositDocument9 pagesTugas Resume Jurnal Resin Kompositdhea wirantiNo ratings yet
- Single Visit Apexification Procedure of A Traumatically Injured Tooth With A Novel Bioinductive Material (Biodentine)Document5 pagesSingle Visit Apexification Procedure of A Traumatically Injured Tooth With A Novel Bioinductive Material (Biodentine)fatimahNo ratings yet
- Clinical Evaluation and Comparison of Quality of Obturation and Instrumentation Time For Pulpectomy in Primary Molars With or Without A Magnifying Loupe An Invivo StudyDocument9 pagesClinical Evaluation and Comparison of Quality of Obturation and Instrumentation Time For Pulpectomy in Primary Molars With or Without A Magnifying Loupe An Invivo StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Regenerative Endodontics-Potential Approaches in Revitalizing The Tooth Pulp - A Review ArticleDocument7 pagesRegenerative Endodontics-Potential Approaches in Revitalizing The Tooth Pulp - A Review ArticleMelliya heptaniaNo ratings yet
- IndianJDentSci12268-3597318 095933Document5 pagesIndianJDentSci12268-3597318 095933TriptiLath DentalNo ratings yet
- IndianJDentSci10129-2612313 071523Document8 pagesIndianJDentSci10129-2612313 071523Anukrity PathakNo ratings yet
- Light-Curing Units: A Review of What We Need To Know: R.B. Price, J.L. Ferracane, and A.C. ShortallDocument8 pagesLight-Curing Units: A Review of What We Need To Know: R.B. Price, J.L. Ferracane, and A.C. ShortallpoojaNo ratings yet
- Intracanal Medicaments - Their Use in Modern Endodontics: A Narrative ReviewDocument6 pagesIntracanal Medicaments - Their Use in Modern Endodontics: A Narrative ReviewDarío Pérez VillalbaNo ratings yet
- Evolution of Magnifications in Endodontics A RevieDocument5 pagesEvolution of Magnifications in Endodontics A RevieAnjali SatsangiNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument5 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- A Review of The Regenerative Endodontic Treatment ProcedureDocument9 pagesA Review of The Regenerative Endodontic Treatment ProcedureOmar TalibNo ratings yet
- How Do You Treat A Severely Resor BedDocument5 pagesHow Do You Treat A Severely Resor BedpoetraNo ratings yet
- The World of Oral Cavity Through The Eye of The LoupeDocument3 pagesThe World of Oral Cavity Through The Eye of The LoupeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Endo VacDocument5 pagesEndo Vacisha MehtaNo ratings yet
- Provisional Restorations in Fixed ProsthodonticsDocument4 pagesProvisional Restorations in Fixed ProsthodonticsPhoebe David100% (1)
- Articol Cariologie 2020 ENGDocument9 pagesArticol Cariologie 2020 ENGAndi TabacariuNo ratings yet
- Journal Homepage: - : IntroductionDocument7 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Denu 2014 41 10 912 PDFDocument6 pagesDenu 2014 41 10 912 PDFhasanNo ratings yet
- Denu 2014 41 10 912Document6 pagesDenu 2014 41 10 912hasanNo ratings yet
- Ceramic Resin BondDocument5 pagesCeramic Resin BondStefan PopescuNo ratings yet
- Endodontology31168-7965184 220731Document4 pagesEndodontology31168-7965184 220731Asmita SonawneNo ratings yet
- Comparative Evaluation of Newer Remineralizing AgeDocument7 pagesComparative Evaluation of Newer Remineralizing AgeBhargavi H naikNo ratings yet
- Jadun2019 Endodontic Microsurgery Part 2Document11 pagesJadun2019 Endodontic Microsurgery Part 2Shirley Granados LauraNo ratings yet
- Additive Effects of Touchactivated Polymerization andDocument9 pagesAdditive Effects of Touchactivated Polymerization anddr.gonzalezcalvinoNo ratings yet
- Anodized Dental Implant Surface: Systematic ReviewDocument24 pagesAnodized Dental Implant Surface: Systematic ReviewRik ChatterjeeNo ratings yet
- Thesis - Synopsis: Dr. Abhilash.ADocument12 pagesThesis - Synopsis: Dr. Abhilash.ARajesh SNo ratings yet
- Diode Laser Frenectomy: A Case Report With Review of LiteratureDocument6 pagesDiode Laser Frenectomy: A Case Report With Review of LiteraturemmputraNo ratings yet
- PCL SilverDocument9 pagesPCL SilverMinh Khuê Trần LêNo ratings yet
- InstrumentationDocument12 pagesInstrumentationMaiush JbNo ratings yet
- Novel Dental Composite Resin Derived From Rice Husk Natural Biowaste - A Systematic Review and Recommendation For Future AdvancementDocument10 pagesNovel Dental Composite Resin Derived From Rice Husk Natural Biowaste - A Systematic Review and Recommendation For Future Advancementnafsiyah xyzNo ratings yet
- Adhesion 2Document6 pagesAdhesion 2Deisy Angarita FlorezNo ratings yet
- Protesis Fija Con Ataches. Rep Caso. 2020. Cureus. SivakumarDocument13 pagesProtesis Fija Con Ataches. Rep Caso. 2020. Cureus. SivakumarAngela AcostaNo ratings yet
- Light Curing Matters: Vol 14, No 6, 2012Document2 pagesLight Curing Matters: Vol 14, No 6, 2012poojaNo ratings yet
- Idjsr Se 0168Document4 pagesIdjsr Se 0168Alfan MaulanaNo ratings yet
- Research ArticleDocument8 pagesResearch ArticleIrzam PratamaNo ratings yet
- 65 JPR D 20 00275Document8 pages65 JPR D 20 00275Loredana BarbaneagraNo ratings yet
- Consensus Statement On Curing LightsDocument2 pagesConsensus Statement On Curing Lightssergio ataydeNo ratings yet
- 3.publication - Green ReviewDocument4 pages3.publication - Green ReviewDr Reema AgrawalNo ratings yet
- Restoring Non-Restorable With The Help of Customized Digital Solutions: A ReviewDocument4 pagesRestoring Non-Restorable With The Help of Customized Digital Solutions: A ReviewDey AzzNo ratings yet
- 0 JConservDent215495-4005111 110731Document5 pages0 JConservDent215495-4005111 110731DarshilNo ratings yet
- IJISRT19AP150Document9 pagesIJISRT19AP150International Journal of Innovative Science and Research TechnologyNo ratings yet
- A Comparison of Efficacy of Lingual Retainer Wires Bonded With Different Adhesive Systems - An In-Vitro StudyDocument9 pagesA Comparison of Efficacy of Lingual Retainer Wires Bonded With Different Adhesive Systems - An In-Vitro StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Comparative Effect of Self VS Dual Curing On Antibacterial Property in A Novel Dental Restorative Material - An Invitro StudyDocument5 pagesComparative Effect of Self VS Dual Curing On Antibacterial Property in A Novel Dental Restorative Material - An Invitro StudyIJAR JOURNALNo ratings yet
- Worksheet 3Document2 pagesWorksheet 3Anmol guptaNo ratings yet
- Airline Reservation SystemDocument81 pagesAirline Reservation SystemBanagiri AkhilNo ratings yet
- Ocean Bottom Node Processing in Deep Offshore Environment For Reservoir MonitoringDocument4 pagesOcean Bottom Node Processing in Deep Offshore Environment For Reservoir MonitoringNadia CorinnaNo ratings yet
- Rules: Manual of The First Competition at Higher Technological Institute (6 October Branch)Document8 pagesRules: Manual of The First Competition at Higher Technological Institute (6 October Branch)Ahmed SaidNo ratings yet
- MaterialismDocument3 pagesMaterialismAce AceNo ratings yet
- Lesson PlanDocument5 pagesLesson PlanPrincess Kylah Chua TorresNo ratings yet
- Ibrahim Kalin - The Age of UnreasonDocument4 pagesIbrahim Kalin - The Age of UnreasonKhaled Aryan ArmanNo ratings yet
- SG - Closed Sets in Topological Spaces: Pauline Mary Helen MDocument11 pagesSG - Closed Sets in Topological Spaces: Pauline Mary Helen MArnav GudduNo ratings yet
- lp33 User ManualDocument94 pageslp33 User ManualAndrew SisonNo ratings yet
- Graphic Design in The Age of Interactive Media: January 2005Document11 pagesGraphic Design in The Age of Interactive Media: January 2005Vlad GavrilasNo ratings yet
- Old English Part 8Document5 pagesOld English Part 8eliseo_dNo ratings yet
- RIA Collaborative Robots White Paper October 2014Document13 pagesRIA Collaborative Robots White Paper October 2014solomonlazioNo ratings yet
- PhotomicrographyDocument73 pagesPhotomicrographyanastatataNo ratings yet
- Task 1 Stratbusana Holy Angel UniversityDocument3 pagesTask 1 Stratbusana Holy Angel UniversityJane DizonNo ratings yet
- Kollmorgen AKM - ServomotorDocument44 pagesKollmorgen AKM - ServomotorMiguel GonzalezNo ratings yet
- Xcell Ammonia (NH) Sensor: Technical Data SheetDocument2 pagesXcell Ammonia (NH) Sensor: Technical Data SheetPaulo HeideckeNo ratings yet
- Samruddhi Thopate ViitDocument1 pageSamruddhi Thopate ViitROHANT NARANGNo ratings yet
- Type-Certificate Data Sheet: An Agency of The European UnionDocument32 pagesType-Certificate Data Sheet: An Agency of The European UnionPrzemekBarnaśNo ratings yet
- Grade 5 DLL English 5 Q4 Week 7Document7 pagesGrade 5 DLL English 5 Q4 Week 7JaniceNo ratings yet
- Plan Child Bank Statement Year001Document7 pagesPlan Child Bank Statement Year001Naima AbdulrahmanNo ratings yet
- Mystic Class v1 2Document16 pagesMystic Class v1 2Raphael CostaNo ratings yet
- Kevilton Price List With Effect From 01st of July 2021Document13 pagesKevilton Price List With Effect From 01st of July 2021chinthaka1234No ratings yet
- FrontDocument6 pagesFrontlokesh_045No ratings yet
- Labsheet - 4 - More - Classes - and - ObjectsDocument15 pagesLabsheet - 4 - More - Classes - and - Objectssarah smithNo ratings yet
- Public Spanish 2 Course Map - Spanish 2Document2 pagesPublic Spanish 2 Course Map - Spanish 2api-534094065No ratings yet
- Sensitivity and SpecificityDocument3 pagesSensitivity and SpecificityPrisia AnantamaNo ratings yet
- Mountain Province State Polytechnic College: Vision Course SyllabusDocument5 pagesMountain Province State Polytechnic College: Vision Course SyllabusArnold Leand BatulNo ratings yet
- Antenna L InEDocument2 pagesAntenna L InERasheed Yaser RabahNo ratings yet