Professional Documents
Culture Documents
COPD Discharge Care Bundle
Uploaded by
Shawn Gaurav JhaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
COPD Discharge Care Bundle
Uploaded by
Shawn Gaurav JhaCopyright:
Available Formats
BTS Chronic Obstructive Pulmonary Disease (COPD) Discharge Care Bundle COPD D1
Trust logo
This care bundle describes 5 high impact actions to ensure the best clinical outcome for patients admitted with an acute exacerbation of COPD (AECOPD). The aim is to
reduce the number of patients who are readmitted following discharge after an AECOPD and to ensure that all aspects of the patients COPD care is considered.
Patient sticker
1. REVIEW PATIENT’S MEDICATIONS & DEMONSTRATE USE OF INHALERS
Assess during medication rounds. Observe the patient using their inhalers and refer to if technique is inadequate. Ensure medications
have been optimised by respiratory specialist team.
ENSURE ALL ELEMENTS OF
Inhaler technique checked: Medications reviewed by respiratory team before discharge? COPD SAFE DISCHARGE
CHECKLIST COMPLETED
2. PROVIDE WRITTEN SELF MANAGEMENT PLAN & EMERGENCY DRUG PACK
Prescribe COPD emergency drug pack and provide to patient at discharge. Ensure patient has a completed self management plan describing how and when to use medications Nurse checking completion of
provided. Provide oxygen alert card if patient is at risk of CO2 retention (referral to a community team for drug pack and plan is acceptable) discharge checklist (initials):
Self management plan? Given ... Already has ... Not applicable ... Emergency drug pack provided? Yes ... No ... Not applicable ...
Oxygen alert card? Yes ... No ... Not applicable ... Referred to community team for pack or plan? Yes ... No ... Not applicable ...
PRIOR TO DISCHARGE
DAY OF DISCHARGE
Checklist completed:
3. ASSESS AND OFFER REFERRAL FOR SMOKING CESSATION
Ask every patient whether they are a current smoker and offer referral to smoking cessation service
Patient is a current smoker: Yes Ex-smoker Never smoked Date of admission:
(To be classed as an ex-smoker, patients must have abstained for 3 months)
Referral made: Yes No Declined N/A
Has smoking cessation been recorded as discussed? Yes No Date of discharge:
4. ASSESS FOR SUITABILITY FOR PULMONARY REHABILITATION
All patients who report walking slower than others on the level or who need to stop due to dyspnea after a mile or after less than 15 minutes walking should be assessed for and
offered pulmonary rehabilitation
Already completed pulmonary rehabilitation? Referral made?
Declined? Not applicable: . Not Done:
5. ARRANGE FOLLOW UP CALL WITHIN 72 HOURS OF DISCHARGE
Follow up all patients at home within 72 hours in person or by phone. A call for the patient can be booked by calling and faxing completed
discharge bundle to: .
Patient has agreed to be contacted: Patients phone number:
Date of call given to patient:
Instructions for use of bundle: Data entry: https://audits.brit-thoracic.org.uk/
Enquiries: carebundles@brit-thoracic.org.uk
v9 October 2016
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- WCLC2021 Abstract Book - Final 16310719983133277Document1,066 pagesWCLC2021 Abstract Book - Final 16310719983133277Shawn Gaurav Jha100% (1)
- Preparing For The Prescribing Safety AssessmentDocument36 pagesPreparing For The Prescribing Safety AssessmentChAndrewNo ratings yet
- Preparing For The Prescribing Safety AssessmentDocument36 pagesPreparing For The Prescribing Safety AssessmentChAndrewNo ratings yet
- Preparing For The Prescribing Safety AssessmentDocument36 pagesPreparing For The Prescribing Safety AssessmentChAndrewNo ratings yet
- ALL in 1Document1 pageALL in 1Shawn Gaurav JhaNo ratings yet
- God's PharmacyDocument18 pagesGod's PharmacyTrack and Trace Committee100% (3)
- CT For PE Breathing Technique PRESENTATIONDocument17 pagesCT For PE Breathing Technique PRESENTATIONEka JuliantaraNo ratings yet
- Health Education Interventions For Older Adults With Hypertension: A Systematic Review and Meta-AnalysisDocument9 pagesHealth Education Interventions For Older Adults With Hypertension: A Systematic Review and Meta-AnalysisJosé Carlos Sánchez-RamirezNo ratings yet
- Clinician's guide to tinnitus history and interpretationDocument1 pageClinician's guide to tinnitus history and interpretationShawn Gaurav JhaNo ratings yet
- Practical Guide: Antimicrobial StewardshipDocument22 pagesPractical Guide: Antimicrobial StewardshipTawfiq BA ABBADNo ratings yet
- Cardiac Rhythms and Dysrhythmias GuideDocument14 pagesCardiac Rhythms and Dysrhythmias GuideShawn Gaurav Jha100% (1)
- Consent For HIV TestingDocument2 pagesConsent For HIV TestingRaviraj PisheNo ratings yet
- Stroke Information Pack: Information For Patients, Families and CarersDocument56 pagesStroke Information Pack: Information For Patients, Families and CarersShawn Gaurav JhaNo ratings yet
- BBN Assessment SheetDocument2 pagesBBN Assessment SheetShawn Gaurav JhaNo ratings yet
- Discussing DNACPR: Before You Begin .Document5 pagesDiscussing DNACPR: Before You Begin .Shawn Gaurav JhaNo ratings yet
- Myfirst 3192Document3 pagesMyfirst 3192Shawn Gaurav JhaNo ratings yet
- Mechanical Thrombectomy For Acute Ischaemic Stroke: An Implementation Guide For The UKDocument99 pagesMechanical Thrombectomy For Acute Ischaemic Stroke: An Implementation Guide For The UKShawn Gaurav JhaNo ratings yet
- CSA Case Scenario Angry Patient About Strike ActionDocument4 pagesCSA Case Scenario Angry Patient About Strike ActionShawn Gaurav JhaNo ratings yet
- START Info For Potential New Regional Centres 21Document9 pagesSTART Info For Potential New Regional Centres 21Shawn Gaurav JhaNo ratings yet
- ADT Form Sample Prescription ChartDocument6 pagesADT Form Sample Prescription ChartShawn Gaurav JhaNo ratings yet
- Key Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation ProblemsDocument5 pagesKey Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation ProblemsShawn Gaurav JhaNo ratings yet
- COPD Care Bundle Action PlanDocument1 pageCOPD Care Bundle Action PlanShawn Gaurav JhaNo ratings yet
- Diabetes 1 0Document4 pagesDiabetes 1 0Yuliah AsrumNo ratings yet
- E-Portfolio Guidance For Foundation Year 1 Doctors: August 2015 - July 2016Document17 pagesE-Portfolio Guidance For Foundation Year 1 Doctors: August 2015 - July 2016Shawn Gaurav JhaNo ratings yet
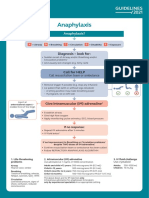
- Anaphylaxis Algorithm 2021Document1 pageAnaphylaxis Algorithm 2021Shawn Gaurav JhaNo ratings yet
- Scripts For Checking UnderstandingDocument2 pagesScripts For Checking UnderstandingShawn Gaurav JhaNo ratings yet
- BTS Guideline For Long Term Macrolide UseDocument35 pagesBTS Guideline For Long Term Macrolide UseShawn Gaurav JhaNo ratings yet
- COPD Admission Care BundleDocument1 pageCOPD Admission Care BundleShawn Gaurav JhaNo ratings yet
- Optho Diams QDocument5 pagesOptho Diams QShawn Gaurav JhaNo ratings yet
- Hospital Passport Template Example From South West London Access To Acute GroupDocument9 pagesHospital Passport Template Example From South West London Access To Acute GroupShawn Gaurav JhaNo ratings yet
- Neet PG 2019 - DR AzamDocument17 pagesNeet PG 2019 - DR AzamShawn Gaurav Jha75% (4)
- PELVIS, Student FileDocument52 pagesPELVIS, Student FileShawn Gaurav JhaNo ratings yet
- Disease and Disease TransmissionDocument48 pagesDisease and Disease TransmissionAYO NELSONNo ratings yet
- Understand Earthing by Q&ADocument22 pagesUnderstand Earthing by Q&AMohamed ElfekyNo ratings yet
- Controlling Drug Delivery SystemsDocument24 pagesControlling Drug Delivery SystemsYuppie RajNo ratings yet
- 1.1 Fundamentals of The Nervous SystemDocument18 pages1.1 Fundamentals of The Nervous Systemno nameNo ratings yet
- 1.1 Health, Safety and Security Almost Finished DocxnwDocument10 pages1.1 Health, Safety and Security Almost Finished DocxnwHilly Douwes-PostmaNo ratings yet
- Word ScoutDocument104 pagesWord ScoutMobina RadNo ratings yet
- Gems of Akbar DarbarDocument12 pagesGems of Akbar DarbarAtul DaveNo ratings yet
- Rundown Kegiatan Pearls Makassar 2021: HARI 1, 23 OKTOBER 2021 WaktuDocument12 pagesRundown Kegiatan Pearls Makassar 2021: HARI 1, 23 OKTOBER 2021 WaktuangelicaNo ratings yet
- Vet Pathol 2011 2011 ACVP Annual Meeting E1 E51Document52 pagesVet Pathol 2011 2011 ACVP Annual Meeting E1 E51Haroon RashidNo ratings yet
- Concept 3 Notes - Anatomy Basics For StudentsDocument39 pagesConcept 3 Notes - Anatomy Basics For StudentsKaranNo ratings yet
- A Short Guide to Understanding FibromyalgiaDocument188 pagesA Short Guide to Understanding FibromyalgiaDave100% (4)
- Standard Treatment GuidelinesDocument468 pagesStandard Treatment GuidelinesHarshit ChempallilNo ratings yet
- Robert Murphy DissertationDocument6 pagesRobert Murphy DissertationPaperWritingCompanyCanada100% (1)
- AHP Matlab software calculates weights for network analysisDocument9 pagesAHP Matlab software calculates weights for network analysisAllahyarNo ratings yet
- Physiology of Thermoregulation (Dr. Herman)Document59 pagesPhysiology of Thermoregulation (Dr. Herman)stella pangestikaNo ratings yet
- Drug StudyDocument2 pagesDrug StudymatthewchadNo ratings yet
- How To Write ThesisDocument22 pagesHow To Write ThesisKenneth LewisNo ratings yet
- Nephrostomy Tubes ToolkitDocument18 pagesNephrostomy Tubes Toolkitmegawati.rscmNo ratings yet
- 11 Benefits of Breastfeeding For Both Mom and BabyDocument15 pages11 Benefits of Breastfeeding For Both Mom and BabySubhranil MaityNo ratings yet
- Conservative TreatmentDocument30 pagesConservative TreatmentAlessandro AnceschiNo ratings yet
- Indian Psychiatric Society - Guideline For Management PDFDocument294 pagesIndian Psychiatric Society - Guideline For Management PDFSarbartha PramanikNo ratings yet
- Endocrine System (Lecture)Document79 pagesEndocrine System (Lecture)roselle legsonNo ratings yet
- NSTP - HealthDocument38 pagesNSTP - Healthmftaganas86% (7)
- Financing Mental Health Care in Sri LankaDocument40 pagesFinancing Mental Health Care in Sri LankajudyjeyakumarNo ratings yet
- Ceramic Veneers DR Jason WangDocument13 pagesCeramic Veneers DR Jason Wangyovita meliaNo ratings yet
- Sex Hormone Synthesis, Regulation, and Function - McMaster Pathophysiology ReviewDocument7 pagesSex Hormone Synthesis, Regulation, and Function - McMaster Pathophysiology ReviewWahyu W'cas PamungkasNo ratings yet
- Ectopic Pregnancy - CSDocument14 pagesEctopic Pregnancy - CSMASII100% (1)