Professional Documents
Culture Documents
Neuroscienceassignment 3
Uploaded by
api-5573295480 ratings0% found this document useful (0 votes)
46 views8 pages1) Bacterial meningitis is a serious infection of the membranes surrounding the brain and spinal cord that can be life-threatening. It is most common in infants, college students, and the elderly.
2) Diagnosis involves lumbar puncture to examine cerebrospinal fluid for signs of bacteria. Treatment requires antibiotics, but the blood-brain barrier can limit their effectiveness.
3) The blood-brain barrier plays a role in both the pathophysiology and treatment of bacterial meningitis. Bacteria can cross through either transcellular or paracellular pathways, disrupting the barrier and increasing permeability. Corticosteroids are given to reduce inflammation and restore barrier integrity to improve antibiotic penetration.
Original Description:
Original Title
neuroscienceassignment3
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1) Bacterial meningitis is a serious infection of the membranes surrounding the brain and spinal cord that can be life-threatening. It is most common in infants, college students, and the elderly.
2) Diagnosis involves lumbar puncture to examine cerebrospinal fluid for signs of bacteria. Treatment requires antibiotics, but the blood-brain barrier can limit their effectiveness.
3) The blood-brain barrier plays a role in both the pathophysiology and treatment of bacterial meningitis. Bacteria can cross through either transcellular or paracellular pathways, disrupting the barrier and increasing permeability. Corticosteroids are given to reduce inflammation and restore barrier integrity to improve antibiotic penetration.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
46 views8 pagesNeuroscienceassignment 3
Uploaded by
api-5573295481) Bacterial meningitis is a serious infection of the membranes surrounding the brain and spinal cord that can be life-threatening. It is most common in infants, college students, and the elderly.
2) Diagnosis involves lumbar puncture to examine cerebrospinal fluid for signs of bacteria. Treatment requires antibiotics, but the blood-brain barrier can limit their effectiveness.
3) The blood-brain barrier plays a role in both the pathophysiology and treatment of bacterial meningitis. Bacteria can cross through either transcellular or paracellular pathways, disrupting the barrier and increasing permeability. Corticosteroids are given to reduce inflammation and restore barrier integrity to improve antibiotic penetration.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 8
1
Noah Riccelli
Bacterial Meningitis and The Blood-Brain-Barrier
Noah Riccelli
Seton Hill University
SPA 220-02
October 28, 2020
2
Noah Riccelli
Meningitis is a serious and potentially life-threatening infection characterized by an
inflammation of the arachnoid and pia mater in the brain and spinal cord. 1,2 This illness can be
viral, fungal, or bacterial. On a worldwide scale, bacterial meningitis is on the top ten list of
deaths related to infectious disease. All individuals are susceptible to this infection, but infants,
college students, and the elderly are the most at-risk. Even though an effective vaccine exists
and there are proven antibiotics readily available, approximately 1.2 million individuals contract
the illness in a given year and 170,000 of these cases are fatal. 1,2 Additionally, 50% of those who
survive deal with permanent neurological impairment. 1-3 The limitations to treating this
infection based on the blood-brain-barrier (BBB) are partially explained by the BBB itself as both
a physical and functional unit. Bacterial meningitis is treated through the use of steroids and
antibiotics, but there are many potential complications involved due to the physical and
chemical selectivity of the BBB.
Diagnosis of bacterial meningitis is difficult because symptoms are varied. A severe
headache, fever, and neck tightness are most common. In more advanced cases, though, a
patient presents with neurological impairment, epileptic seizures, or even a coma. 3 The onset
and progression of the symptoms occur so rapidly that by the time a patient seeks medical
treatment the prognosis is often bleak. Though most individuals recover from bacterial
meningitis, a lack of prompt-treatment can result in death within days or hours. Although blood
tests or imaging techniques like a CT scan or MRI are common methods to suggest an infection
is present, the collection of cerebrospinal fluid (CSF) through a lumbar puncture can give a
definite answer on bacterial meningitis. Additionally, it provides physicians information on the
specific types of bacteria present so they can prescribe the correct antibiotic. Antibiotic
resistance can be the difference between life and death, so having the information to prescribe
an appropriate antibiotic is necessary. 1,3 Unlike a case of viral or fungal meningitis where the
patient is often sent home and prescribed bedrest, bacterial meningitis requires treatment with
antibiotics.3 This intervention is complicated for two reasons: one is quickly finding an antibiotic
for the specific bacteria and the second is finding an antibiotic able to cross the BBB.
The composition of the BBB provides understanding about the pathophysiology of
bacterial meningitis. Ultimately, the ability to cross the BBB depends on the size of the
3
Noah Riccelli
molecule, the positive or negative charge, how lipophilic it is, binding of certain proteins, and
flow of CSF.3 Small molecules with little to no plasma protein binding and many lipophilic
substances are ideal candidates to cross the barrier, but many other substances face a
restriction.1,3 Lipid solubility determines how fast and effective a drug can diffuse into the brain.
Some drugs with polar components are likely to experience a delayed entry while other drugs
with a high lipid solubility will leave the bloodstream and enter the CNS extremely quickly and
efficiently.3-5 Adherens junctions and tight junctions are located in endothelial cells. These
junctions control BBB permeability as well as monitor the polarity of cells, signaling proteins,
and transcription.1 These specific characteristics explain the mechanisms in which blood-borne
bacteria are able to cross the BBB.
Bacteria involved with bacterial meningitis undergo several mechanisms in order to
reach the BBB. Besides entering the BBB, the bacteria must first survive within the bloodstream
then colonize to the circulatory system of the brain. 4 There is not a complete scientific
consensus on how exactly the bacterial components are able to cross the barrier, but the
specific component involved as well as how it interacts with receptors on endothelial cells can
help scientists to make predictions.1,4 Common microbes that can cause bacterial meningitis
include N. meningitidis, S. pneumoniae, and H. influenzae. E. coli and group B Streptococcus
(GBS) are two examples that occur mainly in infants. 1,3,4 The microbiological and chemical
makeup of these microbes provide information on the characteristics and properties that
permit them to cross the BBB. There are multiple ways of gaining entry, but the two most
common are through a transcellular pathway that invades the endothelial cellular layer and a
paracellular pathway that inflicts trauma on the tight and adherens junctions. 4 For example,
GBS, N. meningitidis, and E. coli have been shown to bind to brain microvascular endothelial
cells (BMECs). Many of these bacteria contain a polysaccharide in the form of a capsule that
regulates their invasion.1 As the pathogens attach to the host receptors, regulation becomes a
factor. The laminin receptor and the platelet activating factor receptor are the two main points
at which N. meningitidis, H. influenzae, and S. pneumoniae enter the CNS.1-3 The attachment of
bacteria to the endothelium as well as the interactions between bacteria and receptors both
4
Noah Riccelli
explain the invasion aspect, but the defensive response and breakdown of BBB integrity provide
clarity on the physiology of bacterial meningitis.
There is more to the physiological process than bacteria crossing the BBB and producing
the effects on the brain and meninges. The pathophysiology of bacterial meningitis starts and
ends with the chemical and physical disruption of the BBB. The way the BBB responds to defend
itself can pose additional risks for the patient. The pathogens affect the integrity of the
endothelial cells that serve as the barrier between the brain and the outside environment. 1,4,5
This mechanism can occur through toxic effects and also by disrupting both the structure and
formation of the adherens junctions and tight junctions. In some instances, there are pore-
forming toxins given off by bacteria such as GBS and S. pneumoniae. Consequently, the risk for
developing meningitis is proportional to the secretion of these toxins. 1,3 Furthermore, the
response from the BBB to these toxins includes the formation of cytokines and chemokines,
which disrupt the integrity of the BBB.1 As this integrity becomes disrupted, the permeability of
the barrier increases.1-4 When the barrier is weakened, bacteria and other molecules can cross
over more easily. Substances previously unable to cross the barrier will be able to.
When the BBB senses the presence of harmful bacteria, there is a rush to recruit and
activate neutrophils as an initial response. How fast and effectively the neutrophils are
recruited determines both the response by the BBB and the overall outcome of the disease.
When the pathogens overtake the barrier, the common response is inflammation due to the
endothelial cells being overactivated.1,3-5 In fact, a main cause of the change in permeability is
inflammation of the BBB.1 This inflammation points to the barrier as not only a physical layer of
protection, but also a functional one. Research to help demonstrate this is ongoing. A study
done on a mouse with meningitis showed that when the neutrophils did not experience
apoptosis quick enough, the inflammation in the BBB increased and the outcome of the disease
worsened.1 In further studies, scientists want to figure out the mechanisms behind the
neutrophils acting normally in some instances and their delayed response in other cases. When
the barrier becomes inflamed, the main danger is that it will now be susceptible to foreign
bacterial elements and certain drugs.
5
Noah Riccelli
A common first line of treatment for bacterial meningitis is a corticosteroid. Often,
steroid hormones can cross the BBB by transmembrane diffusion. 6 With an extracellular
pathway, extremely large hormones cross by residual leakiness.7 The properties of these steroid
hormones explain why they can penetrate the barrier. For example, steroid hormones are
typically small and lipid soluble, which allows them to cross bidirectionally. 6,7 In addition,
binding proteins help the molecules cross the BBB. The rate and the degree of penetration are
altered by circulating half-life.6 A commonly prescribed steroid is a glucocorticoid called
dexamethasone. Patients with inflammatory issues dealing related to the immune system,
allergic reactions, and infection are given this drug. Other commonly used steroids include
prednisone, hydrocortisone, and betamethasone. 5,6,7 These steroids are not meant to be a cure
for bacterial meningitis but are meant to decrease inflammation in and outside of the CNS.
With bacterial meningitis and other diseases, the typical defensive response of the BBB is to
become inflamed. This response is similar to the body becoming inflamed as a result of certain
diseases and infection. The endothelial permeability and the diameter of vessels both increase,
so there is less regulation of substances leaking through. 1,6 An inflamed barrier will be less
effective at inhibiting the entry of unwanted molecules, so the body is susceptible to many new
hazards. Furthermore, certain antibiotics that could normally cross the BBB may not be able to
as quickly or effectively as before. Since the increase in inflammation associated with bacterial
meningitis negatively affects the integrity and permeability of the BBB, a decrease in
inflammation restores this integrity.6 Antibiotics used to treat the infection can now penetrate
the barrier without difficulty.5,7
The treatment of bacterial meningitis with antibiotics involves many factors. First, the
infection can overtake the body in days or hours, so physicians must make the proper diagnosis
and treatment decisions quickly. With diagnosing, there must be tests ordered and a lumbar
puncture performed very early on to determine the type of bacteria present in the CSF. 7 With
this knowledge, an effective antibiotic can be paired to treat the infection. Physicians must also
take into consideration the properties of each antibiotic to determine whether it will be able to
cross the BBB. One property that can determine the outcome of using the drug is whether it is
lipid or water soluble. Drugs of both solubilities are commonly used, but fat-soluble once are
6
Noah Riccelli
always preferred. Some common antibiotics used to treat bacterial meningitis include
cephalosporins like ceftriaxone and cefotaxime. Other examples include vancomycin,
meropenem, and medications in the penicillin family.4,6,7 Since antibiotics in the penicillin family
are highly water-soluble, they have difficulty crossing the BBB. 7 Additionally, meropenem and
vancomycin are also water-soluble. Since the BBB favors lipid-soluble drugs, many of these
water-soluble drugs experience more difficulty and take longer to cross the barrier than fat-
soluble drugs. To overcome this limitation, physicians give patients a combination of antibiotics
(usually two or three). Using this strategy helps combat potential antibiotic resistance,
increases the probability of the drug successfully treating the disease, and speeding up the
penetration into the BBB.6,7 More research is being conducted to discover a better option for
treatment. A lot of this research involves individual case studies and is considered anecdotal
evidence. There was a case study involving a patient with bacterial meningitis caused by
Acinetobacter baumannii. The patient was given three different antibiotics intravenously:
vancomycin, meropenem, and tigecycline. After several days, the vancomycin and meropenem
were stopped while the tigecycline doses continued. A number of tests on CSF showed the
meningeal bacteria still present, but a slight increase in the dosage resulted in negative tests for
meningitis only three days later.7 While a number of drugs are effective at treating bacterial
meningitis, scientists are searching for more effective drugs.
Due to the complexity of symptoms and how fast a patient’s condition can worsen
without proper intervention, diagnosis and treatment of bacterial meningitis can be
complicated. The BBB is used to develop understanding of the pathophysiology of bacterial
meningitis. The defensive response and loss of integrity along with the increase in permeability
and inflammation explains how the BBB acts as both a physical and functional unit.1,2,6 Steroids
are used to decrease this inflammation and prevent other unwanted molecules from
penetrating. The limitations to treating this infection stem from the specific properties of the
drugs and how they interact with the BBB. Lipophilic and smaller size molecules are best-suited
to penetrate the barrier.1,6 Besides using corticosteroids to decrease inflammation, there are a
number of antibiotic interventions to treat the symptoms. While most of these drugs are water-
7
Noah Riccelli
soluble and cannot cross the barrier very fast, physicians use combination therapy to combat
this limitation.
8
Noah Riccelli
References
1. van Sorge NM, Doran KS. Defense at the border: the blood-brain barrier versus bacterial
foreigners. Future Microbiol. 2012;7(3):383-394. doi:10.2217/fmb.12.1
2. Hoffman O, Weber RJ. Pathophysiology and treatment of bacterial meningitis. Ther Adv
Neurol Disord. 2009;2(6):1-7. doi:10.1177/1756285609337975
3. Nau R, Sörgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal
fluid/blood-brain barrier for treatment of central nervous system infections. Clin
Microbiol Rev. 2010;23(4):858-883. doi:10.1128/CMR.00007-10
4. Guennec LL, Coureuil M, Nassif X, Bourdoulous S. Strategies used by bacterial pathogens
to cross the blood–brain barrier. Cellular Microbiology. 2019;22(1).
doi:10.1111/cmi.13132
5. Yau B, Hunt NH, Mitchell AJ, Too LK. Blood‒brain barrier pathology and CNS outcomes
in streptococcus pneumoniae meningitis. Int J Mol Sci. 2018;19(11):3555. Published 2018
Nov 11. doi:10.3390/ijms19113555
6. Banks WA. Brain meets body: the blood-brain barrier as an endocrine
interface. Endocrinology. 2012;153(9):4111-4119. doi:10.1210/en.2012-1435
7. Nau R, Seele J, Djukic M, Eiffert H. Pharmacokinetics and pharmacodynamics of
antibiotics in central nervous system infections. Curr Opin Infect Dis. 2018;31(1):57-68.
doi:10.1097/QCO.0000000000000418
You might also like
- June 2023 - Scientific ArticleDocument8 pagesJune 2023 - Scientific Articlebody fayez100% (1)
- Case Study Neonatal SepsisDocument24 pagesCase Study Neonatal Sepsisreiche90% (29)
- Microbes and the Mind: The Impact of the Microbiome on Mental HealthFrom EverandMicrobes and the Mind: The Impact of the Microbiome on Mental HealthNo ratings yet
- The Nature Versus Nurture Debate Involves The Extent To Which Particular Aspects of Behavior Are A Product of Either InheritedDocument1 pageThe Nature Versus Nurture Debate Involves The Extent To Which Particular Aspects of Behavior Are A Product of Either InheritedRebeca VentocillaNo ratings yet
- Cognitive Impairments in Patients With HIV - Associated EncephalopathyDocument5 pagesCognitive Impairments in Patients With HIV - Associated EncephalopathyCentral Asian StudiesNo ratings yet
- Case Study of Neurological DisordersDocument9 pagesCase Study of Neurological DisordersSkyerexNo ratings yet
- Bacterial Meningitis Patho PaperDocument5 pagesBacterial Meningitis Patho PaperJessica BrayNo ratings yet
- Meningitis UPLOADDocument7 pagesMeningitis UPLOADNiruja SriNo ratings yet
- MeningitisDocument5 pagesMeningitisKelly KaroftisNo ratings yet
- Depressão e MicrobiomaDocument14 pagesDepressão e MicrobiomaDoc Nelson JuniorNo ratings yet
- Clinical Microbiology - (10.11)Document11 pagesClinical Microbiology - (10.11)Arthur YanezNo ratings yet
- Hussain 2024Document6 pagesHussain 2024jose mendozaNo ratings yet
- Micro Extra Credit Option Microbiome COVID 24SPDocument2 pagesMicro Extra Credit Option Microbiome COVID 24SPHandel JonathanNo ratings yet
- The Pathogenesis of Tuberculous MeningitisDocument14 pagesThe Pathogenesis of Tuberculous MeningitisGladys SuwantiNo ratings yet
- Pathophysiology Septic ShockDocument26 pagesPathophysiology Septic ShockTinea Sycillia100% (1)
- The Inflammatory ProcessDocument7 pagesThe Inflammatory ProcessDaniul ConuiNo ratings yet
- Research Review - Term PaperDocument12 pagesResearch Review - Term PaperTania RiazNo ratings yet
- Microbios Intestinales en Trastornos Neurocognitivos y de Salud Mental (Halversona y Alagiakrishnan, 2020)Document21 pagesMicrobios Intestinales en Trastornos Neurocognitivos y de Salud Mental (Halversona y Alagiakrishnan, 2020)Centro integral del desarrollo LogrosNo ratings yet
- Botulism, My ReviewDocument19 pagesBotulism, My ReviewAdrija DasNo ratings yet
- Micronutrients Influencing The Immune Response in Leprosy: RevisiónDocument11 pagesMicronutrients Influencing The Immune Response in Leprosy: RevisiónSherlocknovNo ratings yet
- 2021 Article 757Document13 pages2021 Article 757Isabely AmabilyNo ratings yet
- Wa0003.Document18 pagesWa0003.Adrija DasNo ratings yet
- A Look Beyond LymeDocument34 pagesA Look Beyond Lymetimsmith1081574100% (1)
- Ijms 22 10028Document19 pagesIjms 22 10028daniela altamiranoNo ratings yet
- Clinical Evidence On The Potential Beneficial Effects ofDocument12 pagesClinical Evidence On The Potential Beneficial Effects ofDyane VatriciaNo ratings yet
- Cytoquine Storm and SepsisDocument12 pagesCytoquine Storm and SepsisEduardo ChanonaNo ratings yet
- Wellcomeopenres 4 17007Document15 pagesWellcomeopenres 4 17007Achilles Fkundana18No ratings yet
- Microorganisms 08 00493Document18 pagesMicroorganisms 08 00493Gisa IkawaNo ratings yet
- Assign 2Document5 pagesAssign 2Julia ThindNo ratings yet
- Cutaneous Tuberculosis: Epidemiologic, Etiopathogenic and Clinical Aspects - Part IDocument10 pagesCutaneous Tuberculosis: Epidemiologic, Etiopathogenic and Clinical Aspects - Part IDellNo ratings yet
- Mjms 21 1 004Document7 pagesMjms 21 1 004Vini JRNo ratings yet
- Botulism, My Review - 213224-11-0023Document18 pagesBotulism, My Review - 213224-11-0023Adrija DasNo ratings yet
- Meningitis Thesis StatementDocument9 pagesMeningitis Thesis StatementMichele Thomas100% (1)
- Background: Pneumonia Arthritis Osteomyelitis SepsisDocument53 pagesBackground: Pneumonia Arthritis Osteomyelitis SepsisWuwun NurulhidayatiNo ratings yet
- Chapter01 ThebasicsofMicrobiologyDocument14 pagesChapter01 ThebasicsofMicrobiologyFarooq SyedNo ratings yet
- Biology Final Paper 2Document6 pagesBiology Final Paper 2Shawn Inglis-McInnisNo ratings yet
- Toxoplasma Gondii: and The Blood-Brain BarrierDocument12 pagesToxoplasma Gondii: and The Blood-Brain BarrierValentina TjandraNo ratings yet
- Fisiopatología de La Meningitis BacterianaDocument7 pagesFisiopatología de La Meningitis BacterianaGiuliano AlbizziNo ratings yet
- Pediatric Tubercular Meningitis A ReviewDocument10 pagesPediatric Tubercular Meningitis A ReviewemmyNo ratings yet
- Echevarria Jonille S. BS-Pharmacy 2 November 03, 2020: 1. Comment in House M.D. "Hunting"Document3 pagesEchevarria Jonille S. BS-Pharmacy 2 November 03, 2020: 1. Comment in House M.D. "Hunting"Jonille EchevarriaNo ratings yet
- Ibd GDDocument15 pagesIbd GDAndi SusiloNo ratings yet
- 32 - The Microbiota-Microbiome and The Gut-Brain Axis, How Much Do They Matter in PsychiatryDocument28 pages32 - The Microbiota-Microbiome and The Gut-Brain Axis, How Much Do They Matter in PsychiatryPaula CantalapiedraNo ratings yet
- The Role of Gut and Lung Microbiota in SusceptibilityDocument20 pagesThe Role of Gut and Lung Microbiota in SusceptibilityannewidiatmoNo ratings yet
- Nyarang'o Dennis Level IIIDocument29 pagesNyarang'o Dennis Level IIIBryan AmataNo ratings yet
- The Beehive Theory Role of Microorganisms in Late Sequelae o - 2019 - Medical HDocument5 pagesThe Beehive Theory Role of Microorganisms in Late Sequelae o - 2019 - Medical HBruno MañonNo ratings yet
- New 1Document12 pagesNew 1Muhammad SyaifullahNo ratings yet
- Case Study Neonatal SepsisDocument21 pagesCase Study Neonatal SepsisLenjun0% (1)
- Pharmacy - Aegrotat Supplementary - Biochemistry Microbiology Immunology - PC 221 - Feb 2022 .Document9 pagesPharmacy - Aegrotat Supplementary - Biochemistry Microbiology Immunology - PC 221 - Feb 2022 .THE MASUVHELELE POSTNo ratings yet
- Antibiotic Failure Beyond Antimicrobial Resistan - 2023 - Drug Resistance UpdatDocument28 pagesAntibiotic Failure Beyond Antimicrobial Resistan - 2023 - Drug Resistance UpdatDana MateiNo ratings yet
- COVID and Risk of Cognitive DeclineDocument6 pagesCOVID and Risk of Cognitive DeclineHelenaNo ratings yet
- Three Insights On Psychoneuroimmunology of Mood Disorders To Be TakenDocument2 pagesThree Insights On Psychoneuroimmunology of Mood Disorders To Be Takeniftekhar2005No ratings yet
- Meningitis 2016Document6 pagesMeningitis 2016Christopher YovanNo ratings yet
- Bilirubin Toxicity: January 2012Document31 pagesBilirubin Toxicity: January 2012Muhammad HabiburrahmanNo ratings yet
- Bacteriophage TherapyDocument5 pagesBacteriophage TherapyMário FernandesNo ratings yet
- Could Proteomic Research Deliverthe Next GenerationofDocument11 pagesCould Proteomic Research Deliverthe Next GenerationofHafriliantika RamadhaniNo ratings yet
- Introduction and Amino Acids and ProteinsDocument336 pagesIntroduction and Amino Acids and ProteinsDeginet MathewosNo ratings yet
- v11 Biomodulacao Celular o Futuro Da DermatologiaDocument8 pagesv11 Biomodulacao Celular o Futuro Da DermatologiaFabiana BNo ratings yet
- The Progress of Gut Microbiome Research Related To Brain DisordersDocument20 pagesThe Progress of Gut Microbiome Research Related To Brain DisordersVictoria HristovaNo ratings yet
- BSI Briefing Note 2021 Immunity COVID19Document19 pagesBSI Briefing Note 2021 Immunity COVID19Chainsaw ManNo ratings yet
- SocialjusticeprojectDocument2 pagesSocialjusticeprojectapi-557329548No ratings yet
- LA400 Senior Integrative Seminar: University Learning Objectives GridDocument5 pagesLA400 Senior Integrative Seminar: University Learning Objectives Gridapi-557329548No ratings yet
- EthicalissuesvtDocument14 pagesEthicalissuesvtapi-557329548No ratings yet
- La 150 Spring 2019 Text Readings and Question Assignment 4 On ChristianityDocument2 pagesLa 150 Spring 2019 Text Readings and Question Assignment 4 On Christianityapi-557329548No ratings yet
- OVERVIEW (4 Points) : CH116 General and Organic Principles LabDocument4 pagesOVERVIEW (4 Points) : CH116 General and Organic Principles Labapi-557329548No ratings yet
- CH 116 Steam Distillation of Orange Oil Short Form SP 2020 2Document3 pagesCH 116 Steam Distillation of Orange Oil Short Form SP 2020 2api-557329548No ratings yet
- Assignment 4 NeuroscienceDocument8 pagesAssignment 4 Neuroscienceapi-557329548No ratings yet
- Westernmedicinedocs4 6Document3 pagesWesternmedicinedocs4 6api-557329548No ratings yet
- 26 Patofisiologi Edema FK Unhas TGL 5 Mei 2015Document65 pages26 Patofisiologi Edema FK Unhas TGL 5 Mei 2015sri ayu lestari wulandariNo ratings yet
- Generalized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)Document6 pagesGeneralized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)jenNo ratings yet
- UPS RM Specification Sheet PDFDocument18 pagesUPS RM Specification Sheet PDFakashgangaaNo ratings yet
- Human Population Demography LabDocument8 pagesHuman Population Demography LabMarc DrakeNo ratings yet
- English Worksheet - The Laburnum TopDocument4 pagesEnglish Worksheet - The Laburnum TopDIVYALAKSHMINo ratings yet
- Cellrespphotopuzzle Pre ApDocument2 pagesCellrespphotopuzzle Pre Apapi-155864611No ratings yet
- Electron Transport ChainDocument5 pagesElectron Transport ChainTanya Dilshad100% (1)
- 2nd ExpositoryDocument4 pages2nd Expositoryapi-595567391No ratings yet
- Say Hello To Our Little Friends: ZOO br00011Document3 pagesSay Hello To Our Little Friends: ZOO br00011Andjela RoganovicNo ratings yet
- Neurotransmitter - Prof. RondangDocument35 pagesNeurotransmitter - Prof. RondangYoga WitularNo ratings yet
- Grapevine Water Relations: Larry E. WilliamsDocument6 pagesGrapevine Water Relations: Larry E. WilliamsFadhilah SurotoNo ratings yet
- Science 7 Compendium 2nd QTR With CoverDocument66 pagesScience 7 Compendium 2nd QTR With CoverLyra Mae De BotonNo ratings yet
- Analogy Part 2Document6 pagesAnalogy Part 2khushiNo ratings yet
- Lab 3Document23 pagesLab 3qvk8yy9pxcNo ratings yet
- Non-Vascular Flora of Black Mountain: Macrofungi, Lichens, Hornworts, Liverworts and MossesDocument29 pagesNon-Vascular Flora of Black Mountain: Macrofungi, Lichens, Hornworts, Liverworts and MossesCristopher Jimenez OrozcoNo ratings yet
- HIL IndexDocument17 pagesHIL IndexnikhilmajethiaNo ratings yet
- Lesson Plans - PYP 5 - Week 2Document15 pagesLesson Plans - PYP 5 - Week 2Nayyab ZiadNo ratings yet
- (Kenneth Tan) Pharmacologic Management For Cardiogenic Shock - EBM or Gut FeelDocument21 pages(Kenneth Tan) Pharmacologic Management For Cardiogenic Shock - EBM or Gut FeelAdriana VillarrealNo ratings yet
- Reproduction in Plants ScienceDocument3 pagesReproduction in Plants SciencegajulavarshithaaravNo ratings yet
- HSB 1 - Doritos Gmo Gene ResearchDocument10 pagesHSB 1 - Doritos Gmo Gene Researchapi-522650514No ratings yet
- Artificail Neural Network Seminar ReportDocument34 pagesArtificail Neural Network Seminar Reportankit89m25% (4)
- Hematology - KitProtocol - List of TIC KitsDocument3 pagesHematology - KitProtocol - List of TIC Kitsuzair.narcNo ratings yet
- Heme Breakdown, JAUNDICE & LFTDocument58 pagesHeme Breakdown, JAUNDICE & LFTnirmalramyaNo ratings yet
- Characteristics of Cardiac MuscDocument7 pagesCharacteristics of Cardiac Muscusman tariqNo ratings yet
- Taste: Links in The Chain From Tongue To Brain: Lucy A. Vera and Stephen P. WoodingDocument6 pagesTaste: Links in The Chain From Tongue To Brain: Lucy A. Vera and Stephen P. WoodingCelzo RozaldoNo ratings yet
- DNA Structure and FunctionDocument42 pagesDNA Structure and FunctionBenjamin Fernandez Jr.No ratings yet
- TGF BDocument16 pagesTGF BmonikaNo ratings yet
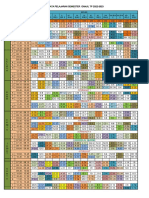
- Roster Pelajaran SMT Genap TP 2022-2023Document10 pagesRoster Pelajaran SMT Genap TP 2022-2023Kadal KodokNo ratings yet
- Notes - Ge ScienceDocument20 pagesNotes - Ge ScienceDiane RosarioNo ratings yet